UNIT 8: RADIATIONS AND MEDICINE
Key Unit Competence:Categorize hazards and safety precautions of radiation in medicine
Introductory activity
Radiation has always been present and is all around us. Life has evolved in a
world containing significant levels of ionizing radiation. Our bodies are adapted
to it.
People are constantly exposed to small amounts of ionizing radiation from the
environment as they carry out their normal daily activities; this is known as
background radiation. We are also exposed to radiations through some medical
treatments and through other activities involving radioactive substances.
The figure above identifies four major sources of public exposure to natural
radiation: cosmic radiation, terrestrial radiation, inhalation and ingestion.Brainstorm and try to answer the following questions:
a) From your own understanding, how is artificial source of radiation different
from natural source of radiation?
b) Using your physics knowledge, what do you think are major sources of
radiation that are mostly preferred to be used in medicine? Defend your
opinion.
c) Do you think exposure to heavy ions at the level that would occur during
deep-space missions for a long duration pose a risk to the integrity and
function of the central nervous system? Explain to support your idea.
d) As a physics student-teacher, what do you think are the symptoms,effects and jeopardy of radiation exposure to human body?
8.1. RADIATION DOSE
Activity 8.1
Radiation is the emission of particles or electromagnetic waves from a source.
Radiation from radioactive materials has the ability to interact with atoms and
molecules of living objects.
a) From your understanding, what makes these radiations able to penetrate
matter?
b) Do you think any amount of radiation should be applied to human body in
case it is to be used to examine a certain part under study or investigation?
Defend your reasoning.
c) Using your prior knowledge about use of radiation in hospitals, what are
common used radiations?
d) Suggest the possible side effects of these radiations to human body.
e) From your suggestions in (d) above, what do you think are precaution
measures one should take to avoid dangers that may be caused by theseradiations?
8.1.1 Ionization and non-ionization radiations.
Radiation is the emission of particles or electromagnetic waves from a source.
Also it is amount of energy deposited in a given mass of medium by ionization
radiation. Radiation from radioactive materials has the ability to interact with atoms
and molecules of living objects.
In a neutral atom, the positive charge of the nucleus is equal and opposite to the
total negative charge of the orbital electrons. If such an atom loses or gains an
electron, it becomes an ion. The atom will now have a net positive or negative
charge and is called an ion. This process is called ionization, and the radiation
responsible for it is called ionizing radiation. When discussing the interaction of
radiations with matter in particularly in relation to health,
two basic types of radiation can be considered.
a. Ionizing radiation.
Ionization radiation refers to a radiation that carries sufficient energy to release
electrons from atoms or molecules, in that way ionizing them. It is made up of
energetic subatomic particles,ion or atoms that moving at high speeds. As the more
powerful form of radiation, ionizing radiation is more likely to damage tissue than
non-ionizing radiation. The main source of exposure to ionizing radiation is the
radiation used during medical exams such as X-ray radiography or computed
tomography scans.
However, the amounts of radiation used are so small that the risk of any damaging
effects is minimal. Even when radiotherapy is used to treat cancer, the amount of
ionizing radiation used is so carefully controlled that the risk of problems associated
with exposure is tiny.
All forms of living things emit a certain amount of radiation, with humans, plants and
animals accumulating radioisotopes as they ingest food, air and water. Some forms
of radiation such as potassium-40 emit high-energy rays that can be detected using
measurement systems. Together with the background radiation, these sources of
internal radiation add to a person’s total radiation dose.
Background radiation is emitted from both naturally and man-made sources. Natural
sources include cosmic radiation, radon radiation in the body, solar radiation and
external terrestrial radiation. Man-made forms of radiation are used in cancer
treatment, nuclear facilities and nuclear weapons.
Globally, the average exposure to ionizing radiation per year is around 3 milli
Sieverts (mSv), with the main sources being natural (around 80%). The remaining
exposure is due to man-made forms such as those used in medical imaging
techniques. Exposure to man-made forms of ionizing radiations is generally much
higher in developed countries where the use of nuclear imaging techniques is
much more common than in developing countries.
b. Non-ionizing radiations
Non-ionizing radiationis any type of electromagnetic radiation that does not carry
enough energy to ionize atoms or molecules. Examples of non-ionizing radiations
include visible light, microwaves, ultraviolet (UV) radiation, infrared radiation, radio
waves, radar waves, mobile phone signals and wireless internet connections.
Although UV has been classified as a non-ionizing radiation but it has been
confirmed. High levels of UV-radiation can cause sunburn and increase the risk ofskin cancer developing.
Scientific investigations suggest that the use of telecommunications devices such
as mobile phones may be damaging, but no risk associated with the use of these
devices has yet been identified in any scientific studies. This energy is emitted bothinside the body and externally, through both natural and man-made processes.
8.1.2 Radiation penetration in body tissue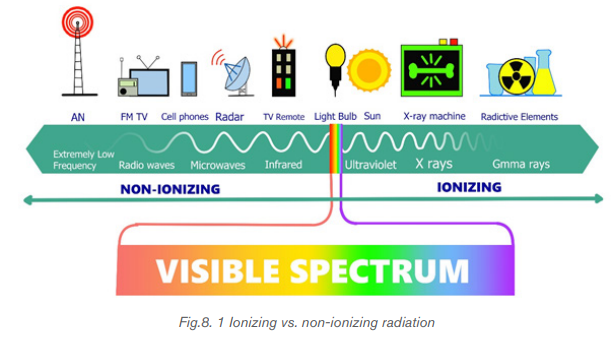
Radiation cannot be spread from person to person. Small quantities of radioactive
material occur naturally in the air, drinking water, food and our own bodies. People
can come into contact with radiation through medical procedures. An important
characteristic of the various ionizing radiations is how deeply they can penetrate
the body tissues. X-rays, gamma rays, and neutrons of sufficient energy described
below can reach all tissues of the body from an external source.
• Alpha Radiation
Alpha radiation refers to a form of particle radiation that occurs when an atom
undergoes radioactive decay. They consist of two protons and two neutrons
(essentially the nucleus of a helium-4 atom). Due to their charge and mass, alpha
particles interact strongly with matter, and can only travel a few centimeters in air.
A thin sheet of paper, on the other hand, stops alpha particles. Alpha radiation can
only penetrate the outer layers of human skin. Therefore, radionuclides that emit
only alpha particles are harmless unless you take them into the body. This you might
do by inhalation (breathing in) or ingestion (eating and drinking).
• Beta Radiation
Beta radiation occurs when radioactive atomic nuclei emit electrons (negatively
charged) or frequently positron (positively charged particles with the same mass of
electron).Due to their smaller mass, they are able to travel further in air, up to a few
meters, and can be stopped by a thick piece of plastic, or even a stack of paper
i.e can penetrate the skin a few centimeters to metres in air and few millimetres to
centimetre in soft tissue and plastic. Posing somewhat of an external health risk.
The depth to which beta particles can penetrate the body depends on their energy.
High-energy beta particles (several MeV) may penetrate a centimeter of a tissue,
although most are absorbed in the first few mm. As a result, beta emitters outside
the body are hazardous only to surface tissues such as the skin or the lenses of the
eye. When you take beta emitters into the body, they will irradiate internal tissues
and then become a much more serious hazard.
• Gamma Radiation
In the case of gamma radiation, energy is transferred as an electromagnetic wave.
Electromagnetic radiation can be described in terms of its frequency or wavelength
( the high frequency and the shorter the wavelength, the more energetic radiation).
Gamma radiation is at high energy end of electromagnetic spectrum. Gamma
radiation, unlike alpha or beta, does not consist of any particles, instead consisting
of a photon of energy being emitted from an unstable nucleus. Having no mass or
charge, gamma radiation can travel much farther through air than alpha or beta,
losing (on average) half its energy.
Gamma waves can be stopped by a thick or dense enough layer material, with high
atomic number. Materials such as lead can be used as the most effective form of
shielding.
• X-Rays
X-rays are similar to gamma radiation, with the primary difference being that they
originate from the electron cloud. This is generally caused by energy changes in
an electron, such as moving from a higher energy level to a lower one, causing the
excess energy to be released. X-Rays are longer-wavelength and (usually) lower
energy than gamma radiation, as well.
• Neutron Radiation
Neutron radiation consists of a free neutron that is mainly released in nuclear
fission. They are able to travel hundreds or even thousands of meters in air, they are
however able to be effectively stopped if blocked by a hydrogen material, such as
concrete or water.
Neutron radiation occurs when neutrons are ejected from the nucleus by nuclear
fission and other processes. The nuclear chain reaction is an example of nuclear
fission, where a neutron being ejected from one fission atom will cause another
atom to fission, ejecting more neutrons. Unlike other radiations, neutron radiation isabsorbed by materials with lots of hydrogen atoms, like paraffin wax and plastics.
8.1.3 Radiation dosimetry
Just as for drugs, the effect of radiation depends on the amount a person has
received. Therefore, amounts of radiation received are referred to as doses, and
the measurement of such doses is known as dosimetry.
A radiation dosimeter refers to a device the measures dose uptake of external
ionizing radiation. Dosimeters are used to monitor your occupational dose from
radioactive material or radiation-producing equipment. Most individuals working
with X-ray producing equipment in the hospital will be issued with a dosimeter.
For those individuals working in the research laboratory setting, dosimeters will be
issued based on the nuclide and total activity that will be used.
Dosimeters are integrating detectors; that is, they accumulate the radiation dose
and give off an amount of light which is proportional to that dose.
The energy absorption properties of dosimeters are designed to be very similar to
tissue, so they are very effective as personnel dosimeters. These devices are used
to measure exposures from x-ray, gamma ray and high energy beta particles.
Dosimeters are not suitable for measuring exposures to low energy beta particles
or alpha particles.
8.1.4. Radiation exposure.
Exposure is a measure of the ionization produced in air by X-rays or gamma rays,
and it is defined in the following manner. A beam of X-rays or gamma rays is sent
through a mass m of dry air at standard temperature and pressure
In passing through the air, the beam produces positive ions whose total charge is q.
Exposure is defined the total charge per unit mass of air. The SI unit for exposure
is coulomb per unit mass . The unit for exposure E is the roentgen(R). 1R
. The unit for exposure E is the roentgen(R). 1R
is the amount of electromagnetic radiation which produces in one gram of air ( ) at normal temperature (22 and pressure (760mmHg) conditions.
) at normal temperature (22 and pressure (760mmHg) conditions.
Since the concept of exposure is defined in terms of the ionizing abilities of X-rays
and gamma rays in air, it does not specify the effect of radiation on living tissue. For
biological purposes, the absorbed dose is more suitable quantity, because it is theenergy absorbed from the radiation per unit mass of absorbing material.
Long-term exposure to small amounts of radiation can lead to gene mutations
and increase the risk of cancer, while exposure to a large amount over a briefperiod of time can cause burns or radiation sickness.
Radiation sickness is a damage human body caused by a large dose
of radiation often received over a short period of time (acute). It isn’t caused by
common tests that use low-dose radiation such as x-rays or CT-Scans. Radiationsickness also called acute radiation syndrome or radiation poisoning.
8.1.5. Absorbed radiation dose.
Radiation dose is a quantity of the energy measured which is deposited in matter by
ionizing radiation per unit mass. A similar approach is used in radiation protection
measurements, where the unit of absorbed dose is specified in terms of the
amount of energy deposited by radiation in 1 kg of material. International system of
unit for radiation measurement is the “gray” (Gy) and “sievert’’ (Sv). These units
can be expressed into others like “rad”, “rem” or roentgen(R). An absorbed
radiation dose of 1 Gray corresponds to the deposition of 1 joule of energy in 1kg of material (air, water, tissue or other).
It describes the physical effect of the incident radiation, but it tells us nothing about
the biological consequences of such energy deposition in tissue. Studies have
shown that alpha and neutron radiation cause greater biological damage for a given
energy deposition per kg of tissue than gamma radiation does. A person who has
absorbed a whole body dose of 1 Gy has absorbed one joule of energy in each
kg of its body tissue. Absorbed dose is used in calculation of dose uptake in livingtissues in both radiation protections.
In other words, equal doses of, say, alpha and gamma radiation produce unequal
biological effects. This is because the body can more easily repair damage from
radiation that is spread over a large area than that which is concentrated in a small
area. Because more biological damage are caused for the same physical dose.
When we analyze the effect of radiation on human being is not so much the total
dose to the whole system but the dose per kg. That’s why a doctor will recommendsmaller doses of medicine for children than for adults.
8.1.6 Quality factors
Quality factors are used to compare the biological effects from different types
of radiation. For example, fast neutron radiation is considered to be 20 times as
damaging as X-rays or gamma radiation. You can also think of fast neutron radiation
as being of “higher quality”, since you need less absorbed dose to produce
equivalent biological effects. This quality is expressed in terms of the Quality Factor
(Q). The quality factor of a radiation type is defined as the ratio of the biological
damage produced by the absorption of 1 Gy of that radiation to the biological
damage produced by 1 Gy of X or gamma radiation.
The Q of a certain type of radiation is related to the density of the ion tracks it leavesbehind it in tissue; the closer together the ion pairs, the higher the Q.
8.1.7 Equivalent dose
The measure of biological damage that is calculated by multiplying absorbeddosebyquality factor for the type of radiation involved is known as equivalent dose.
The unit of equivalent dose H is the Sievert (Sv). An equivalent dose of one Sievert
represents that quantity of radiation dose that is equivalent, in terms of specified
biological damage, to one gray of X or gamma rays. Normally, we use the millisievert
(mSv) and microsievert (µSv). Few other instruments can read in mGy or µGy, butthey measure only gamma radiation.
The Calculation of Equivalent Dose and Effective dose is given by:
The effective dose is a measure of cancer risk, it adjusts the equivalent dose based
on the susceptibility of the tissue exposed to the radiation. It is expressed in Sv andmSv.
8.1.8 Radiation protection
The effects of radiation at high doses and dose rates are reasonably well
documented. A very large dose delivered to the whole body over a short time willresult in the death of the exposed person within days.
We know from these that some of the health effects of exposure to radiation do
not appear unless a certain quite large dose is absorbed. However, many other
effects, especially cancers are readily detectable and occur more often in those
with moderate doses. At lower doses and dose rates, there is a degree of recoveryin cells and in tissues.
Radiation protection sets examples for other safety disciplines in two unique
respects:
• First, there is the assumption that any increased level of radiation above
natural background will carry some risk of harm to health.
• Second, it aims to protect future generations from activities conducted today.
The use of radiation and nuclear techniques in medicine, industry, agriculture, energy
and other scientific and technological fields has brought tremendous benefits to
society. The benefits in medicine for diagnosis and treatment in terms of human
lives saved are large in size.
No human activity or practice is totally devoid of associated risks. Radiation should
be viewed from the perspective that the benefit from it to mankind is less harmfulthan from many other agents.
Note: The optimization of patients’ protection is based on a principle that the dose
to the irradiated target (tumor) must be as high as it is necessary for effectivetreatment while protecting the healthy tissues to the maximum extent possible.
Application activity 8.1
1. a) How ionization differs from non-ionization radiations
b) Give any two examples of each.
2. What does the following terms mean in medical treatment?
a) absorbed dose
b) radiation dose
c) The quality factor
3. In the application of radiation in medicine, we use the statement “Ameasure of the risk of biological harm”. Clearly explain this statement
8.2. HAZARDS AND SAFETY PRECAUTIONS WHEN HANDLING
RADIATIONS
Activity 8.2
1. The picture below show doctors’ meeting and they are discussing on
a therapeutic treatment due to the wrong exposure to radiation that
normally occur in their hospital. These radiations happened in unintendedevent occurring as a radiation accident.
a) In your own words, what does radiation accident mean?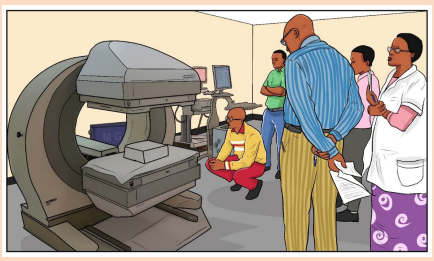
b) What do you think are the radiation accident (unintended events)
which may happen due to wrong exposure radiation?
c) That radiation exposure may be computed in fewer and greater
amount. What do you think are the negative effects that may be as a
result of exposure of these amounts of radiations?
d) Based on unintended event you think might have happened in (b)
above, what do you think are preventive measures that should be
taken to reduce or stop the occurrence of unintended radiationaccident?
2. You happen to interact with a man who was diagnosed and found to
have cancer cells in one of his fingers. He was advised by the doctor
that the cells can be killed by X-rays’ radiations. He had previously
been told that X-rays have a lot of negative effects if exposed to human
body. He at first resisted and was given 2 days to decide. It’s one day
remaining and you happen to interact with him and he is seeking advicefrom you. Advise this man on what do.
8.2.1 Deterministic and stochastic effects:
Effects of radiations due to cell killing have a practical threshold dose below
which the effect is not evident but in general when the effect is present its severityincreases with the radiation dose.
The threshold doses are not an absolute number and vary somewhat by individual.
Effects due to mutations (such as cancer) have a probability of occurrence thatincreases with dose.
a. Deterministic effects:
These effects are observed after large absorbed doses of radiation and are
mainly a consequence of radiation induced cellular death. They occur only if a large
proportion of cells in an irradiated tissue have been killed by radiation, and the losscan be compensated by increasing cellular proliferation.
b. Stochastic effects:
They are associated with long term, low level (chronic) exposure to radiation. They
have no apparent threshold. The risk from exposure increases with increasing dose,
but the severity of the effect is independent of the dose.
Irradiated and surviving cells may become modified by induced mutations (somatic,
hereditary). These modifications may lead to two clinically significant effects:
malignant neoplasm (cancer) and hereditary mutations.
In evaluating biological effects of radiation after partial exposure of the body further
factors such as the varying sensitivity of different tissues and absorbed doses
to different organs have to be taken into consideration. The lifetime value for the
average person is roughly a 5% increase in fatal cancer after a whole body dose
of 1 Sv. It appears that the risk in fetal life, in children and adolescents exceeds
somewhat this average level (by a factor of 2 or 3) and in persons above the age of
60 it should be lower roughly by a factor of ~ 5.
Animal models and knowledge of human genetics, the risk of hereditary deleterious
effects have been estimated to not be greater than 10% of the radiation induced
carcinogenic risk.
All living organisms on this planet, including humans, are exposed to radiation from
natural sources. An average yearly effective dose from natural background amounts
to about 2.5 mSv. This exposure varies substantially geographically (from 1.5 to
several tens of mSv in limited geographical areas).
Various diagnostic radiology and nuclear medicine procedures cover a wide dose
range based upon the procedure. Doses can be expressed either as absorbed
dose to a single tissue or as effective dose to the entire body which facilitates
comparison of doses to other radiation sources (such as natural background
radiation. Quality assurance and quality control in diagnostic radiology and nuclear
medicine play also a fundamental role in the provision of appropriate, sound
radiological protection of the patient.
There are several ways that will minimize the risk without sacrificing the valuable
information that can be obtained for patients’ benefit. Among the possible measures
it is necessary to justify the examination before referring a patient to the radiologist
or nuclear medicine physician. Failure to provide adequate clinical information at
referral may result in a wrong procedure or technique being chosen by radiologist
or nuclear medicine specialist.
An investigation may be seen as a useful one if its outcome - positive or negative
- influences management of the patient. Another factor, which potentially adds
to usefulness of the investigation, is strengthening confidence in the diagnosis.
Irradiation for legal reasons and for purposes of insurance should be carefully
limited or excluded.
While all medical uses of radiation should be justified, it stands to reason that
the higher the dose and risk of a procedure, the more the medical practitioner
should consider whether there is a greater benefit to be obtained.Among these
special position is occupied by computed tomography (CT), and particularly its
most advanced variants like spiral or multi slice CT.
If an examination is typically at the high end of the diagnostic dose range and the
fetus is in or near the radiation beam or source, care should be taken to minimize
the dose to the fetus while still making the diagnosis. For children, dose reduction in
achieved by using technical factors specific for children and not using routine adult
factors, because children are small, in nuclear medicine the use of administered
activity lower than that used for an adult will still result in acceptable images and
reduced dose to the child.
The most powerful tool for minimizing the risk is appropriate performance of the test
and optimization of radiological protection of the patient. These are the responsibility
of the radiologist or nuclear medicine physician and medical physicist.
The basic principle of patients’ protection in radiological X-ray investigations and
nuclear medicine diagnostics is that necessary diagnostic information of clinically
satisfactory quality should be obtained at the expense of a dose as low as reasonablyachievable, taking into account social and financial factors.
8.2.2 Effects of radiation exposure
Some effects may occur immediately (days or months) while others might take tens
of years or even get passed to the next generation. Effects of interest for the person
being exposed to radiation are called somatic effects and effects of interest that
affect our children are called genetic effects.
i. Radiation Health Effects
Ionizing radiation has sufficient energy to cause chemical changes in cells and
damage them. Some cells may die or become abnormal, either temporarily or
permanently. By damaging the genetic material (DNA) contained in the body’scells, radiation can cause cancer.
Fortunately, our bodies are extremely efficient at repairing cell damage. The extent
of the damage to the cells depends upon the amount and duration of the exposure,
as well as the organs exposed.
Exposure to an amount of radiation all at once or from multiple exposures in a
short period of time. In most cases, a large acute exposure to radiation causes
both immediate (radiation sickness) and delayed effects (cancer or death), can
cause sickness or even death within hours or days. Such acute exposures areextremely rare.
ii. Chronic Exposure
With chronic exposure, there is a delay between the exposure and the observed
health effect. These effects can include cancer and other health outcomes such asbenign tumors, cataracts, and potentially harmful genetic changes.
a. Low levels of radiation exposure
Radiation risks refer to all excess cancers caused by radiation exposure (incidence
risk) or only excess fatal cancers (mortality risk). Risk may be expressed as a
percent, a fraction, or a decimal value.
For example, a 1% excess risk of cancer incidence is the same as a 1 in a hundred
(1/100) risk or a risk of 0.01. However, it is very hard to tell whether a particular
cancer was caused by very low doses of radiation or by something else.
While experts disagree over the exact definition and effects of “low dose.”
Radiation protection standards are based on the premise that any radiation
dose carries some risk, and that risk increases directly with dose.
Note:
• The risk of cancer from radiation also depends on age, sex, and factors such
as tobacco use.
• Doubling the dose doubles the risk.
Acute health effects occur when large parts of the body are exposed to a large
amount of radiation. The large exposure can occur all at once or from multiple
exposures in a short period of time. Instances of acute effects from environmentalsources are very rare.
8.2.3 Safety precautions for handling radiations
Shortening the time of exposure, increasing distance from a radiation source and
shielding are the basic countermeasures (or protective measures) to reduce dosesfrom external exposure.
Note:
• Time: The less time that people are exposed to a radiation source, the less
the absorbed dose.
• Distance: The farther away that people are from a radiation source, the lessthe absorbed dose.
Note: Shielding: Barriers of lead, concrete or water can stop radiation or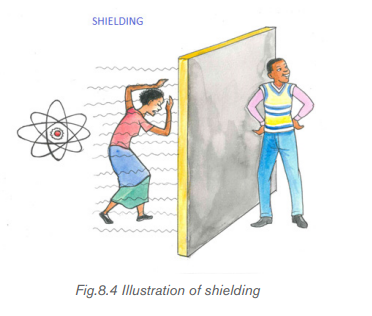
reduce radiation intensity.
There are four main factors that contribute to how much radiation a person absorbs
from a source. The following factors can be controlled to minimize exposure toradiation:
i. The distance from the source of radiation
The intensity of radiation falls sharply with greater distance, as per the inverse
square law. Increasing the distance of an individual from the source of radiation
can therefore reduce the dose of radiation they are exposed to. For example, such
distance increases can be achieved simply by using forceps to make contact with
a radioactive source, rather than the fingers.
ii. Duration of exposure
The time spent exposed to radiation should be limited as much as possible. The
longer an individual is subjected to radiation, the larger the dose from the source
will be. One example of how the time exposed to radiation and therefore radiation
dose may be reduced is through improving training so that any operators who need
to handle a radioactive source only do so for the minimum possible time.
iii. Reducing incorporation into the human body
Potassium iodide can be given orally immediately after exposure to radiation. This
helps protect the thyroid from the effects of ingesting radioactive iodine if an
accident occurs at a nuclear power plant. Taking Potassium iodide in such an eventcan reduce the risk of thyroid cancer developing.
iv. Shielding
Shielding refers to the use of absorbent material to cover the source of radiation,
so that less radiation is emitted in the environment where humans may be exposed
to it. These biological shields vary in effectiveness, depending on the material’s
cross-section for scattering and absorption. The thickness (shielding strength) of
the material is measured in Any amount of radiation that does penetrate the
Any amount of radiation that does penetrate the
material falls exponentially with increasing thickness of the shield.
Some examples of the steps taken to minimize the effects of radiation exposure are
described below;
- The exposed individual is removed from the source of radiation.
- If radiation exposure has led to destruction of the bone marrow, the number
of healthy white blood cells produced in the bone marrow will be depleted.
- If only part of the body has been exposed to radiation rather than the whole
body, treatment may be easier because humans can withstand radiation
exposure in large amounts to non-vital body parts.
In every medicine there is a little poison. If we use radiation safely, there are benefits
and if we use radiation carelessly and high doses result, there are consequences.
Ionizing radiation can change the structure of the cells, sometimes creating
potentially harmful effects that are more likely to cause changes in tissue. These
changes can interfere with cellular processes so cells might not be able to divideor they might divide too much.
Radioactive rays are penetrating and emit ionizing radiation in the form of
electromagnetic waves or energetic particles and can therefore destroy living
cells. Small doses of radiation over an extended period may cause cancer and
eventually death. Strong doses can kill instantly. Marie Curie and Enrico Fermi died
due to exposure to radiation.
Several precautions should be observed while handling radioisotopes. Some of
these are listed in the following:
• No radioactive substance should be handled with bare hands. Alpha and
beta emitters can be handled using thick gloves. Gamma ray emitters must
be handled only by remote control that is by mechanical means. Gamma rays
are the most dangerous and over exposure can lead to serious biological
damage.
• Radioactive materials must be stored in thick lead containers.
• Reactor and laboratories dealing with and conducting experiments with
radioactive metals must be surrounded with thick concrete lined with lead.
• People working with radioactive isotopes must wear protective clothing
which is left in the laboratory. The workers must be checked regularly with
dosimeters, and appropriate measures should be taken in cases of overdose.
• Radioactive waste must be sealed and buried deep in the ground.
Rules to remember when working with radiation
Everyone must take radiation overexposure seriously. Hence, preventive measures
and rules must be strictly followed to avoid critical health conditions.
b. Acquire adequate training to better understand the nature of radiation hazards.
a. Reduce handling time of radioactive materials and equipment.
b. Be mindful of your distance from sources of radiation. Increase distance as
much as possible.
c. Use proper shielding for the type of radiation.
d. Isolate or contain harmful radioactive materials properly.
e. Armor yourself with appropriate protective clothing and dosimeters.
f. Conduct contamination surveys in the work area.
g. Do not eat, drink, smoke, or apply cosmetics in an area where unsealed
radioactive substances are handled.
h. Observe proper radioactive waste disposal.i. Conduct usual radiation safety self-inspection
8.2.4 Concept of balanced risk
a. Risks of ionizing radiation in medical treatment
Risk in the area of radiation medicine has several dimensions that are less common
in other areas of medicine. First, there may be risks from overexposure that do
not cause immediate injury. For example, the causal connection, if any, may be
difficult or impossible to verify for a malignancy that surfaces several years after
an inappropriate exposure. Second, the risks associated with the medical use of
ionizing radiation extend beyond the patient and can affect health care workers
and the public.
In amplifying these and other aspects of the risks that attend medical uses of
ionizing radiation, the discussion addresses the following issues: human error and
unintended events; rates of misadministration in radiation medicine; inappropriate
and unnecessary care; and efforts that reduce misadministration and inappropriate
care.
b. Human Error and Unintended Events
Errors occur throughout health care: A pharmacist fills a prescription with the wrong
medicine; an x-ray technician takes a film of the wrong leg; a surgeon replaces
the wrong hip. The advent of complex medical technology has increased the
opportunity for error even as it has increased the opportunity for effecting cures.
By educating health care workers, and by circumscribing their actions, human error
may be minimized. However, some number of mistakes will always, unavoidably, be
made, and no amount of training or double-checking can erase that fact.
c. Comparison of risks in the use of ionizing radiation
The comparison of relative risks of misadministration in by-product radiation
medicine to error rates and events in other medical practice settings, as well
as the comparison of disease and death rates with the risks of the therapeutic
administration itself, help to some extent to place ionizing radiation use in a broader
context.
To achieve this success requires the highest standards of performance (accuracy
of delivered dose), both when planning irradiation for an individual patient and in
actual delivery of the dose.
In a large number of cases, decreasing the dose to the target volume is not possible
since it would unacceptably decrease the cure rate. In these cases present
technological developments aim at optimizing the patients’ protection, keeping
the absorbed tumor dose as high as is necessary for effective treatment while
protecting nearby healthy tissues.
It should be remembered that successful eradication of a malignant tumor by
radiation therapy requires high-absorbed doses and there is a delayed (and usually
low) risk of late complication. The above mention techniques are used to provide
the best benefit/risk ratio.
A malignant tumor in a pregnant woman may require radiotherapy in attempt to
save life of the patient. If a tumor is located in a distant part of the body, the therapy
- with individually tailored protection of the abdomen (screening) may proceed.
When thyroid cancer with metastases is diagnosed in a pregnant woman, treatment
with 131 I is not compatible with continuation of the pregnancy. The treatment should
then be delayed until delivery if doing so wouldn’t put the mother’s life in danger.
Medical radiation can be delivered to the patient from a radiation source outside the
patient. Regardless of how much dose the patient received, they do not become
radioactive or emit radiation.
Balancing risks are often summarized in the following:
• The demand for imaging, especially computed tomography, that has increased
vastly over the past 20 years
• An estimated 30% of computed tomography tests that may be unnecessary
• Ionizing radiation that may be associated with cancer.
• The risks of radiation exposure that is often overlooked and patients are
seldom made aware of these risks
• The requesting doctor who must balance the risks and benefits of any
high radiation dose imaging test, adhering to guideline recommendations if
possible
• Difficult cases that should be discussed with a radiologist, ideally at a clinicradiological or multidisciplinary team meeting.
Application activity 8.2
1. How do you understand by the term balance risk?
2. What is magnitude of the risk for cancer and hereditary effects?
3. Is ionizing radiation from medical sources the only one radiation for
which people are expected to be exposed?
4. What are typical doses from medical diagnostic procedures?
5. Can radiation doses in diagnosis be managed without affecting the
diagnostic benefit? Explain to support your decision.
6. Explain clearly how radiation can be reduced by three principles for
radiation safety: time, distance and shielding
8.3. BASICS OF RADIATION THERAPY FOR CANCER
TREATMENT
Activity 8.3The figure below shows the radiotherapy of breast cancer treatment
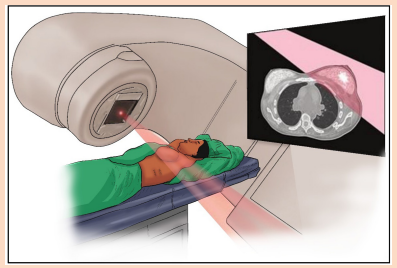
Use the diagram above to answer the following questions.
i) Use a pencil, re-draw the picture in your notebook and locate points
that may be affected by cancer cells.
ii) From your reasoning, does the breast cancer affect only women?
Support your answer.
iii) In Medicine, the concern of breast tissue cancer can be solved by
radiation therapy. It should be delivered in two ways i.e. External andinternal, why do think a doctor may opt one method over another?
8.3.1. Background of Radiation therapy
Radiation therapy plays an important role in curative treatment of many cancers. It
can be used alone or in conjunction with the surgery, chemotherapy or both in order
to eradicate cancer.
Cancer is the name given to a range of diseases where there is malignant tumour.
A malignant tumour may grow slowly for a time and then faster; it infiltrates
surrounding structure and will destroy them. Many cancers are treated successfully
with radiation.
Radiation therapy (also called radiotherapy) refers to the cancer treatment which
uses high dose of radiation to kill cancer cells and tumors. It can be used to cure
cancer, control the growth or spread of cancer and to provide comfort by alleviating
thesymptoms cancer can sometimes cause.The specification for the radiotherapylead to the complicated cancer like: painful bone and soft tissue metastases,
hemoptysis, dyspnea, dysphagia, brain metastases, and spinal cord compression,
etc.
Long exposure of radiation or spent the total dose of radiation over time, allow
tissue cells to be destroyed and be damaged by cancer cells. This is not a big issue
for palliative radiotherapy, but is critical for curative treatment.
Radiotherapy consists/ focuses of treating cancer without removing organs and
tissues. It can be used alone or in conjunction with the surgery and systemic
therapies(e.g., chemotherapy, hormones). The intent is either to cure with radical
radiotherapy or to control symptoms with palliative radiotherapy.
Radiotherapy is usually given over several minutes and is similar to having an
x-ray examination. Patients need to be cooperative and able to lie still for 10 to 15
minutes. As it is a localized treatment, benefits and side effects are generally limitedto the areas being treated.
Radiation therapy had the following types:
• 3D conformal radiation therapy
• Intensity-modulated radiation therapy(IMRT)
• Volumetric-guided radiation therapy(VGRT)
• Image-guided radiation therapy(IGRT)
• Stereotactic radiosurgery(SRS)
• Brachytherapy
• Superficial x-ray radiation therapy(SXRT)
• Intraoperative radiation therapy (IORT)
8.3.2 Cancer treatment
a. Destruction
Radiation damages cells through ionization. This may bea direct ionization of
important molecules such as DNA, in the cell nucleus (shown in below figure) orindirect action through ionization of the more abundant water within the cell.
DNA is a complex responsible for protein synthesis and growth pattern. In some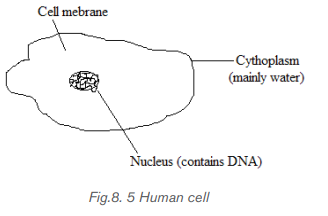
case, the cells begin to grow uncontrollably (cancer), whilst in others its ability toproduce is destroyed(sterilization).
The ionization of water results in the formation of free radicals H and OH. These
are very reactive and potentially damaging, often leading to cell death or onset of
mutation. Cells are most vulnerable to radiation damage when they are reproducing,
so that fast growing cells are very radiation sensitive, for example the developing
fetus, the reproductive organs and bone marrow. In contrast, brain and bone tissues,which do not replace themselves rapidly, are least affected.
b. The cure
Cancerous cells tend to reproduce more rapidly than normal cell, making them
relatively more radiation sensitive and capable of being selectively destroyed
through ionization. The target is always the DNA within the nucleus: breaks in the
DNA stands can result in cell death or loss of reproductive capacity either of which
stops the spread of the disease. Healthy cells recover from irradiation more quickly
than cancer cells. In order to achieve the greatest destruction of cancer cells, with
the least damaged to surrounding healthy tissue, the radiation should therefore be
delivered in short treatment or fractions of relative high doses over a period of time.
A typical fractionation scheme might be involved daily treatment for five days in fiveweeks.
c. The care
Certain organisms in the body are very weak to radiation damage and during
therapy, it is important to keep dose delivered to these tissues to a minimum. Such
critical organism include the:
• Eye(cataracts)
• Spinal cord(paralysis)
• Reproductive organs(sterility)
• Kidney, liver, rectum.
The treatment depends on the nature of the tumor and its location. There are four
basic methods and treatment for any one patient may involve two or more of them.
• Surgery: if the tumor is easily located, it may simply be removed.
• Chemotherapy: the patient is given dose of cell destroying drugs.
• Hormone therapy: some hormone dependent tumor can be treated by altering
the hormone balance within the body.
• Radiotherapy: tumor cells are destroyed with high-energy radiation, eithergamma-rays from a radioactive source or x-rays.
There are three steps to follow radiotherapy treatment:
The first step in radiotherapy is to meet with a radiation oncologist so that an informed
decision can be made regarding the overall prognosis and goals of treatment and
so that patients and physicians can proceed with planning treatment.
The next step is to determine the area to be treated. This process is called
simulation. The simulation is done with fluoroscopy, x-ray films, CT-Scan and
MRIs can.
The third step is treatment. Radiation treatments are usually given 5 days a week
over several weeks.
During the treatment planning, the doctor or radiotherapist analyses the information
about the size and position of the tumors using various imaging techniques available
like x-ray films, CT-Scan and MRI scan, even ultrasound imaging sometime can be
applied for example in assessing the thickness of the chest wall when planning
breast treatment.
The total quantity of radiation required to destroy the tumors depends on the many
factors, such as:
• Types of cell irradiated(some cancer cells are more radiation-sensitive than
others)
• Environment of the cell(its blood and oxygen supply are important)
• Extent of cancer
• Fractionation scheme selected (a large total dose is needed for more, smallerfractions).
Treatment for certain condition
a. spinal cord compression
Spinal cord compression coming from tumor growth is an oncologic emergency that
should be treated in 24hours of diagnosis with aim of maintaining patient’s ability to
walk, continence and comfort. People with spinal cord compression (about 95%)
had back pain and neurologic signs and symptoms including weakness, paresthesia,
Incontinence, spasticity and hyperreflexia.
Patients’ neurologic deficits sometimes increase rapidly, and early detection is of
highest importance. Magnetic resonance imaging is the modality of choice for this.
A radiation oncologist should be consulted on an emergency basis for spinal cordcompression.
Prognosis is largely dependent on a patient’s overall condition, pretreatment ability
to walk, rate of symptom progression, and the extent of the block. Most patient’s
ambulatory at diagnosis of spinal cord compression remain ambulatory if treated
promptly; only half of those who can move their legs but are not walking become
ambulatory after treatment.
Ambulatory means able to walk but ambulatory care or outpatient care is medical
care provided on an outpatient basis, including diagnosis, observation, consultation,
treatment, intervention, and rehabilitation services. This care can include advanced
medical technology and produces even when provided outside of hospitals.
b. Superior vena cava obstruction
Superior vena cava obstruction caused by cancer also requires urgent, though not
emergency, treatment. Patients with superior vein cava obstruction present with
neck and facial swelling, dilated neck veins, orthopnea, and shortness of breath,
and sometimes progress to headaches and cerebral edema. The treatment usually
varies within 1 to 2 weeks depending on the severity of presenting symptoms. Some
chemotherapy-responsive malignancies, such as lymphomas and small cell lung
cancers, can also cause superior vena cava obstruction and are primarily treatedwith chemotherapy.
c. Bone metastasis
Bone metastases are usually sign for palliative radiotherapy. About 80% of patients
who receive radiation therapy for bone pain experience fewer symptoms; maximum
effect is noticed on average 1 to 3 weeks after treatment. Breast, prostate and
lung are common primary cancer places for bone metastases. Diagnosis is usually
made using bone scans and plain x-ray films, but occasionally magnetic resonanceimaging or computed tomography scans are needed.
d. Brain metastasis
Brain metastases occur around 10% to 30% to all cancer patients. Patient with
brain metastases present the symptoms like: headache, cognitive dysfunction,
neurologic deficits, and seizures. The diagnosis duration given over 1 to 2 weeks
to the entire brain, can improve symptoms and extend survival. Contrast-enhanced
computed tomography (CT-Scan) or magnetic resonance imaging (MRI) scans are
used to diagnose brain metastases.
Conclusion
Radiotherapy has fundamental role in both curative and palliative management
of cancer patients. So that family physicians will be better aware of the appropriateness
of referring patients for such treatment and participating in care of cancer patient
can help facilitate for radiotherapy when they encounter patients with oncologicproblems or complications amenable to radiotherapy treatment.
Application activity 8.3
1. What does a radiation therapy mean?
2. What is radiotherapy used for?
3. How long does it take for radiation therapy treatment to work?4. At what stage of cancer is radiotherapy used?
Skills Lab 8
In this activity you will invite a medical doctor that has expertise in radiationand medicine.
What to do?
• Invite the doctor (using a written letter).Your class tutor or class leaders
may help you in doing this. You may target different doctors so that if
disappointed by one, you do not miss it all. Remember these doctors are
always busy at their work.
• When he/she comes, make sure you give him points of discussion.
These may include: Radiation and dosimetry, balanced risk, Hazards and
safety precautions while handling radiations, and radiation therapy for
cancer treatment. You can still send him/her these topics before so that
he/she can do enough preparations.
• While he/she is presenting, make sure you note down important
information in your notebooks.
• You may ask questions in case you do not understand what the doctor
is explaining.
• Compare what the doctor explained to what you have been discussing
in this unit.
• Develop a comprehensive report including all what you have been
studying and information from the doctor.• Submit your report to your tutor for marking or checking.
End of unit 8 assessment
1. The large amount of radiation absorbed by the body can lead to the
radiation sickness. What do you think is the symptoms and complications
of the radiation sickness?
2. Cleary explain what kind of radiation causes radiation sickness.
3. Is it possible that radiation spread from person to person?
4. What are the risks associated with radiation from diagnostic X-ray
imaging and nuclear medicine procedures?
5. Does receiving external-beam radiation make a person radioactive or
able to expose others to radiation?
6. Is there any risk that internal radiation implants (brachytherapy) will leak
or break free from where they are placed and move around my body?
7. I’m having an imaging test using radioactive materials. Will I be
radioactive after the test?
8. Are there situations when diagnostic radiological investigations shouldbe avoided? Explain to support your decision.
BIBLIOGRAPHY
1. Abbot, A. F., & Cockcroft, J. (1989). Physics (5 ed.). Heinemann: Educational
Publishers.
2. Atkins, K. R. ( 1972). Physics-Once over Lightly. New York : New York.
3. Avison, J. (1989). The world of PHYSICS. Cheltenham: Thomas Nelson and
Sons Ltd.
4. AVISON, J. (1989). The world of PHYSICS. Cheltenham: Thomas Nelson
and Sons Ltd.
5. BIPM. (2006). The International System of Units (SI). (8 ed.). Sevres,
France: International Bureau of Weights and Measures.
6. Breithaupt, J. (2000). Understanding Physics For Advanced Level. (4 ed.).
Ellenborough House, Italy: Stanley Thorners.
7. Chand, S., & S.N., G. S. (2003). Atomic Physics (Modern Physics) (1 ed.).
India.
8. CPMD. (2015). Advanced Level Physics Sylabus. Kigali: REB.
9. Cunningham, & William, P. (2000). Environmental science (6 ed.). Mc
Graw-Hill.
10. Cutnell, J. D., & Johnson, K. W. (2006). Essentials of Physics. USA: John
Wlley &Sons, Inc.
11. Cutnell, J. D., & Johnson, K. W. (2007). Physics. (7 ed.). USA: John Wiley;
Sons, Inc.
12. Cuttnell, J. D., & kennety, W. J. (2007). Physics (7 ed.). United State of
America: John Willey & Sons . Inc.
13. David, A. D. (2012). Child’s thigh demonstrate the five basic radiographic
densities: Imaging for students (4 ed.).
14. Douglass, C. G. (2014). PHYSICS, Principles with applications. (7 ed.).
Pearson Education.
15. Douglass, C. G. (2014). PHYSICS, Principles with applications. (8 ed.).
Pearson Education.
16. Duncan, T., & Kennett, H. (2000). Advanced Physics (5 ed.). London, UK:
Holder Education.
17. eschooltoday. (2008-2018). Retrieved February 19, 2018, from natural
diseasters: http
18. eschooltoday. (2008-2018). Retrieved February 19, 2018, from Climate
change: http
19. Giancoli, D. (2005). PHYSICS: Principles with applications. New Jersey:
Pearson Education, Inc.
20. Giancoli, D. C. (2005). Physics principals with application. Upper Saddle
River, NJ 07458: Pearson Education, Inc.
21. Giancoli, D. C. (2005). Physics: principals with application. Upper Saddle
River, NJ 07458: Pearson Education, Inc.
22. Giancoli, D. C. (2005). Physics: Principles with applications. New Jersey:
Pearson Education, Inc.
23. Glencoe. (2005). Physics - Principles and Problems [textbook]. McGraw.
24. Haber-Schaim, U., Cutting, R., Kirkesey, H. G., & Pratt, H. A. (2002). Force,
Motion, and Energy. USA: Science Curriculum, Inc.
25. Halliday, D., Resneck, R., & Walker, J. (2014). Fundamentals of Physics. (10
ed.). USA: John Wiley; Sons,Inc.
26. Halliday, Resneck, & Walker. (2007). Fundamentals of Physics. (8 ed.).
Wiley.
27. Hewitt, P. G., SUCH0CKI, J., & Hewitt, L. A. (1999). Conceptual Physical
Science. (2 ed.). Addison Wesley Longman.
28. Hirsch, A. S. (2002). Nelson Physics 12. Toronto: University Preparation.
29. http://www.threastafrican.co.ke. (2017). Retrieved from rwanda/Business/
kigali.
30. Hugh, D. Y., & Roger, A. F. (2012). University Physics with Modern Physics
(13 ed.). San Francisco, USA: Pearson Education, Inc.
31. IPCC. (1996). Economics of Greenhouse Gas limitation, Main report
“Methodological Guidelines.
32. John, M. (2009). Optical Fiber Communications, Principals and Practice
(3rd Ed.). London: Pearsnon Prentice Hall.
33. Jones, E. R., & Childers, R. L. (1992). Contemporary College Physics. (2
ed.). USA: Addison-Wesley Publishing Company.
34. Kansiime, J. K. (2004). Coumpound Physical Geography: Morphology,
Climatology, Soils and Vegetation. uganda.
35. Linda, W. (2004). Earth Sceience demystified a self-teaching guide. USA:
McGraw-Hill Campanies, inc.
36. Michael, E. B. (1999). Schaum’s outline of Theory and Problems of Physics
for Engineering and Science. USA: McGRAW-HILL Companies, Inc.
37. Michael, J. P., Loannis, M., & Martha, C. (2006). Science Explorer, Florida
Comprehensive Science. Boston: Pearson Prentice Hall.
38. MIDIMAR. (2012). Disaster High Risk Zones on Floods and Landslide.
Kigali: MIDMAR.
39. Nagashima, Y. (2013). Elementary Particle Physics. Osaka University:
Deutsche Nationalbibliothek.
40. Nelkon, M., & Parker, P. (1997). Advanced level Physics. (7 ed.). Edinburgh:
Heinemann.
41. Nelkon, M., & Parker, P. (2001). Advanced Level Physics (7 ed.). Edinburgh
gate: Heinemann.
42. Office, U. M. (2011). Warming: A guide to climate change. U.K.: Met Office
Hadley Centre.
43. Orazio, S. (2010). Principles of Lasers (5 ed.). Milan, Italy: Springer.
44. Patrick, T. (2004). Mathematics standard level. (3 ed.). Victoria: Ibid Press.
45. Pope, J. (1998). Medical Physics Imaging. Heinemann.
46. R.B., B. (1984). Physical Geography in diagrams for Africa. Malaysia:
Longmann Group Limited.
47. Randall, D., & Knight. (2004). Physics for scientists and engineers: Stategic
approach (Vol. 2). San Fransisco: Pearson Education.
48. Randall, D., & Knight. (2004). Physics for scientists and engineers: Stategic
approach. (Vol. 3). San Fransisco: Pearson Education, Inc.
49. Randall, D., & Knight. (2008). Physics for scientists and engineers: Stategic
approach. (2 ed., Vol. 3). San Fransisco: Pearson Education, Inc.
50. Randall, D., & Knight. (2008). Physics for scientists and engineers: Stategic
approach. (2 ed., Vol. 3). San Fransisco: Pearson Education, Inc.
51. REMA. (n.d.). Rwanda Second National Communication Under the
UNFCCC. KIGALI: MINISTRY OF NATURAL RESOURCES,RWANDA.
52. Science, G. (2006). Florida Physical Science with Earth Science. USA: Mc
Graw Hill Glencoe Companies, Inc.
53. Serway, R. A. (1986). Physics for Scientists and Engineers (2 ed.). Saunders
College Publishing.
54. Serway, R. A. (1992). Principles of Physics. Orlando, Florida: Saunders
College Publishing.
55. Serway, R. A., & Jewett, J. J. (2008). Physics for Scientists and Engineers.
(7 ed.). USA: Thomson Learning, Inc.
56. Serway, R. A., & Jewett, J. J. (2010). Physics for Scientists and Engineers
with Modern Physics. (8 ed.).
57. Silver, B., & Ginn, I. (1990). Physical Science. Unit States of America.
58. Stephen, P., & Whitehead, P. (1996). Physics. (2 ed.). School Edition.
59. Stephen, P., & Whitehead, P. (1996). Physics. (2 ed.). School Edition.
60. Strassler, M. (2011, September 25). What’s a Proton, Anyway? Retrieved
March 05, 2018, from www.profmattstrassler.com: https://profmattstrassler.
com/articles-and-posts/largehadroncolliderfaq/whats-a-proton-anyway/
61. Subranya, K. (1993). Theory and applications of fluid mechanics. Tata
McGraw: Hill Companies.
62. Taylor, E., & Wheeler, J. A. (1992). Spacetime Physics: Introduction to
Special Relativity. (2 ed.). San Francisco: W.H.Freeman & Company,
Publishers.
63. Taylor, E., & Wheeler, J. A. (1992). Spacetime Physics: Introduction to
Special Relativity. (2 ed.). San Francisco: W.H.Freeman & Company,
Publishers.
64. Tipler, P. A. (1991). Physics for Scientists and Enginners. (3 ed., Vol. 2).
USA: Worth Publishers, Inc.
65. Tipler, P. A. (1991). Physics for Scientists and Enginners. (3 ed., Vol. 1).
USA: Worth Publishers, Inc.
66. Tom, D. (2000). Advanced Physics (5 ed.). H. Kennett.
67. Toyal, D. C. (2008). Nuclear Physics (5 ed.). Himalaya Publishing House.
68. Uichiro, M. (2001). Introduction to the electron theory of metals . Cambridge
University Press .
69. Weseda, Y., Mastubara, E., & Shinoda, K. (2011). X-rays properties-google
search. Retrieved 03 06, 2018, from www.springer.com: http://www.
springe.com/978-3-642-26634-1
70. Wysession, M., Frank, D., & Yancopoulos, S. (2004). Physical Science.
Boston, Massachusetts, Upper Saddle River, New Jersey: Pearson PrenticeHall
