UNIT 7: MEDICAL IMAGING
Key Unit Competence:Generate the processes in medical imaging.
Introductory activity
Years ago, the only way to get information from inside of human bodies was
through surgery. In modern medicine, medical imaging has undergone major
advancements and this ability to obtain information about different parts of the
human body and has many useful clinical applications.
Observe and interpret, clearly the pictures above and answer to the following
questions:
1. Describe the phenomena happening in each figures above (A, B, C, D
and E)
2. Propose the technique that is being used for each image?
3. Suggest a detailed working principle of the mentioned techniques in
each image
4. Are there other techniques that are not indicated in the figure above? If
yes, state and explain them.
5. In your own view, what do you think are the effects of these techniquesin general?
7.1. CONCEPT OF MEDICAL IMAGING.
Activity 7.1
Imagine you were in internship in a certain primary school in your district and
while teaching in P3, a pupil happens to swallow a 20 Francs coin. You and
fellow teachers gave her first aid and later your Head teacher assigned you to
take her to the nearest hospital.
a) In your own view, how do you think a doctor will be able to locate the
swallowed coin without operating her?
b) Explain using scientific reasoning, why a doctor needs to use method(s)you suggested in (a) above.
The technique and process of producing visual representations of the interior areas
inside the human body (function of some organs or tissues) to diagnose medical
problems and monitor treatment is known as Medical imaging.
There are many types of medical imaging, and more methods for imaging are being
invented as technology advances. The main types of imaging used in modern
medicine include
• Radiography.
• Mammography
• Magnetic resonance imaging.
• Nuclear medicine.
• Ultrasound.
• Endoscopy
• Elastography.
• Photoacoustic imaging.
• Tomography.
• Echocardiography, etc
In this unit, we shall focus on only the following: Radiography and
Mammography, Magnetic Resonance Imaging, Ultrasound and Endoscopy.
SPECIFIC PURPOSES OF IMAGING TECHNIQUES
Each technique is used in different conditions. For example:
• Ultrasound is used to study the development of fetus in the mother’s womb
and to take images of internal organs when high resolution is not needed.
• Radiography is often used when we want images of bone structures to look
for breakages.
• MRI scanners are often used to take images of the brain or other internal
tissues, particularly when high-resolution images are needed.
• Nuclear medicine is used when you need to look inside the digestive or
circulatory systems, such as to look for blockages. It uses radioactive materialsthat are injected or swallowed.
Application activity 7.1
1. Explain the meaning of medical imaging
2. Medical imaging being a new technique of examining internal parts of
a body under examination, has been emphasized and used in different
medical places. What are different methods of medical imaging you
know and where are they used?
3. Highlight the purpose(s) of each of the methods mentions in question2 above.
7.2 ULTRASONIC IMAGING
Activity 7.2
Mutesi is a young mother who was pregnant used to feel pain in her lower
abdomen and she happened to go to the hospital for medical checkup. As she
reached the hospital, she underwent a medical testing and her doctor referred
her to undergo ultrasound scan.
What she noticed was a doctor moving a piezoelectric crystal on her abdomen.At the end, she was given image of affected part.
a) As a physics student, explain why the technique used is regarded as
ultrasound?
b) From your understanding, how the emitted rays are used to capture the
image of intended part and feed it back to the computer.
c) If you were a doctor, would you advise someone to always visit ultrasound
scans every time he/she feels pain? If No explain why? If yes, defend youropinion.
7.2.1 Interaction of sound waves with different structure inside
the body
Ultrasound imaging uses ultra-high-frequency sound waves to produce cross
sectional images of the body. Ultrasound is actually sound with a frequency in
excess of 20 kHz, which is the upper limit of human hearing. The frequency range
of normal person hearing is between 20 Hz to 20 KHz. In fact, the frequencies
used in medicine are much higher than this, typically between 1 MHz and 15 MHz
like all sound waves, ultrasound consists of longitudinal, elastic or pressure waves,
capable of traveling through solids, liquids and gases. This makes them ideal for
penetrating the body, unlike transverse mechanical waves, which cannot travel to
any great extent through fluids.
Different tissues in a human or animal body alter the ultra sound waves in different
ways. Some waves are reflected directly while others scatter the waves before they
return to the transducer as echoes. The reflected ultrasound pulses detected by
the transducer need to be amplified in the scanner or ultrasonic probe. The echoes
that come from deep within the body are more attenuated than those from the more
superficial parts and therefore required more amplification. When echoes return to
the transducer, it is possible to reconstruct a two-dimensional map of all the tissues
that have been in the beams. The information is stored in a computer and displayed
on a video (television) monitor. Strong echoes are said to be of the high intensity
and appear as brighter dots on the screen.
Normally in medicine, Doctors commonly use ultrasound to study a developing
fetus (unborn baby), a person›s abdominal and pelvic organs, muscles and tendons,or their heart and blood vessels
7.2.2 Reflection of ultrasound
When the pulse of ultrasound is sent into the body and meets a boundary between
two media, of different specific acoustic impedance Z, the sound wave needs to
change gear in order to continue. If the difference in Z across the boundary is large
the wave cannot easily adjust: there is an “acoustic mismatch”. Most of the waveis reflected and a strong echo is recorded. The fraction of intensity reflected back
 at the normal incidence, is known as the intensity of
at the normal incidence, is known as the intensity of reflection coefficient α
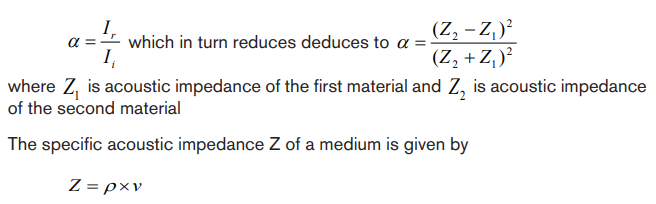
Where ρ is the density of the medium and v is he velocity of sound in medium.

Table 7. 1 Values ρ,v and Z for various substances
Note that large differences in Z give rise to large values for intensity of reflectioncoefficient (α), producing strong echoes.
7.2.3 Attenuation of ultrasound
The combined effect of scattering and absorption is called attenuation. The
attenuation of the waves describes the reduction in its intensity as they travel
through a medium. This loss is due to a number of factors:
• The wave simply “spreads out” and suffers an “inverse square law type”
reduction in intensity.
• The wave is scattered away from its original direction
• The wave is absorbed in the medium.
The amount of absorption of ultrasound beam in a medium is described by the
absorption coefficient, which is intensity level per unit length. It is expressed in
decibels per cm and it firstly depends on the type of medium the wave is propagating
into. As example whilst water absorbs very little ultrasound, bone is a strong
absorber, putting it at risk, for example, during high- power ultrasound therapy.
Secondly, higher frequencies suffer greater absorption. In fact if the frequency is
doubled, the absorption increases by the factor of four.
7.2.4 Ultrasonic imaging techniques
The basic component of the ultrasound probe is the piezoelectric crystal. Excitation
of this crystal by electrical signals causes it to emit ultra-high-frequency sound
waves; this is the piezoelectric effect. The emitted ultrasound waves are reflected
back to the crystal by the various tissues of the body. These reflected sound waves
also called the “echoes” act on the piezoelectric crystal in the ultrasound probe to
produce an electric signal, again by the piezoelectric effect. It is this electric signal
which is analysed by a computer produces a cross-sectional image.
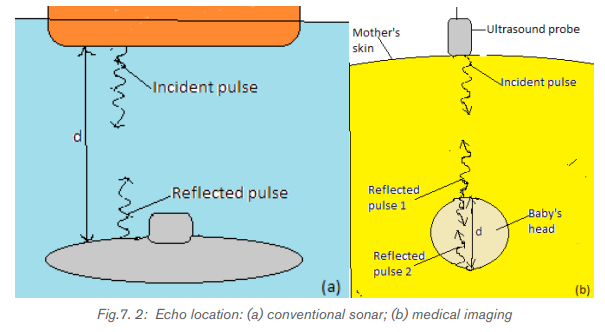
The process of imaging is the same as the echo-locating sonar of a submarine or
a bat. The observer sends out a brief pulse of ultrasound and waits for an echo.
The pulse travels out, reflects off the target and returns. The ultrasound machine
uses pulses because the same device acts as both transmitter and receiver. If it
continually sent out sounds, then the receiver would not hear the much softer echoover the louder transmission.
Sonar is an acronym for Sound Navigation and Ranging. It relies on the reflection of
ultrasound pulses. A short pulse of ultrasound is directed towards the object interest,
which then reflects it back as an echo. The total time between transmission of pulse
and reception of an echo is measured, often using a cathode ray oscilloscope(CRO). The sonar principle is used to estimate the depth of a structure, using
Where t is the time taken to go and back and is the velocity of ultrasound in the
medium.
The factor of 2 is necessary because the pulse must travel “there and back”
An ultrasound beam structure is directly into the body. The reflection or echoes
from different body structure are then detected and analyzed, yielding information
about the locations. For example if the time delays between the reception of echo
pulse1 and 2 (Figure below) is, then the diameter of the baby’s head can befound using the above formula.
As ultrasound imaging uses sound waves to produce pictures of inside of the body.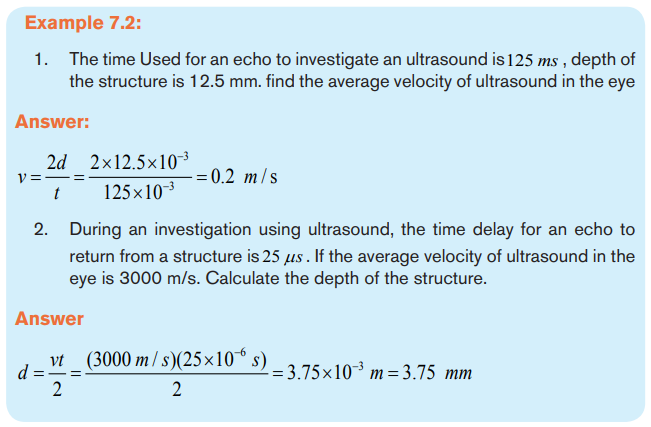
It is used to help diagnose the cause of pain, swelling and infection in the body’s
internal organs and to examine a baby in pregnant woman and the brain and hips in
infants. It is also used to help guide biopsies, diagnose heart conditions and assess
damage after a heart attack.
Ultrasound examinations do not use ionizing radiation (x-rays), there is no radiation
exposure to the patient. Because ultrasound images are captured in real time, they
can show the structure and movement of the body’s internal organs, as well asblood flowing through blood vessels.
7.2.5 Risk and benefit associated to ultrasounds
Ultrasound imaging uses high-frequency sound waves, not used x-ray and no
radiation exposure to the patient does not mean the at ultrasound is mostly safe. It
has some dangers.
Some of them are:
• Cannot penetrate bone, so the adult skeletal system and head cannot be
imaged.
• Clarity of image is poorer than in many other techniques.
• It cannot be used in areas that contain gas (such as lungs)
• Scan can take a long time and demand greater skills and experience to
produce a clear result.Etc.
Apart from its dangers, ultrasound is helpful because:
No known harmful effects of diagnostic ultrasound.
Clear examination of soft tissues, e.g.Obstetric and abdomen studies
More cost effective than other imaging modalities
Real time imaging means required quick procedure.
It is noninvasive (of medicine procedures not involving the introduction of instruments
into the body)
• Lack of ionizing radiation.• Equipment is safe, easy to handle, can be operated and be portable. Etc
Application activity 7.2
1. Calculate the percentage of incidence intensity reflected back at:
a) Air per soft tissues boundary
b) Bone per softy tissues boundary.
2. Discuss on the purpose of using ultrasound in medicine
3. Outline the application of ultrasound scan?4. Why ultrasound is performed
7.3 X-RAY IMAGING.
Activity 7.3
1. The figure below is what a Doctor got after X-rays scan in order tocheck a problem that was suspected to be in ribs.
a) Using the picture above, how do you think the doctor was able to get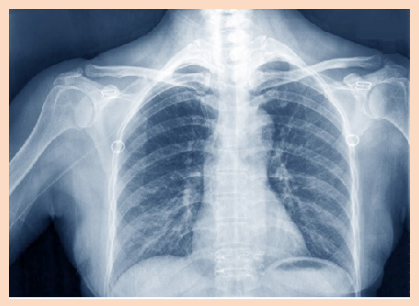
the image
b) Why do you think devices like cameras cannot give such images?
2. One day a girl suffering from the breast tells her mother about the
problem. And her mother advises her to go to the hospital to consult
a doctor. After examined by the doctor, she was referred to the X-ray
room for further checking.
a) Imagine you are the doctor operating the X-ray device, explain all that
you can do to detect the problem a girl had.
b) There are many methods of X-ray imaging techniques that may be
used. Can you suggest one that can be used to examine breastproblems? Defend your suggestion.
7.3.1 Interaction of X-rays with matter.
a. Introduction
In unit 5, we learnt that X-rays are electromagnetic radiation produced by focusing
a beam of high energy electron on a target material in x-ray tube. Since the major
part of the energy of the electrons is converted into heat in the target (only about
1% will appear as X-rays), the target material should have a high melting point and
good heat conduction ability. To get a high relative amount of X-ray energy, the
anode material should be of high atomic number. Tungsten is the dominating anodematerial and is in modern X-ray tubes often mixed with Rhenium.
In X-ray diagnostics, radiation that is partly transmitted through and partly
absorbed in the irradiated object is utilized. An X-ray image shows the variations
in transmission caused by structures in the object of varying thickness, density or
atomic composition.
b. Attenuation and Absorption of X-rays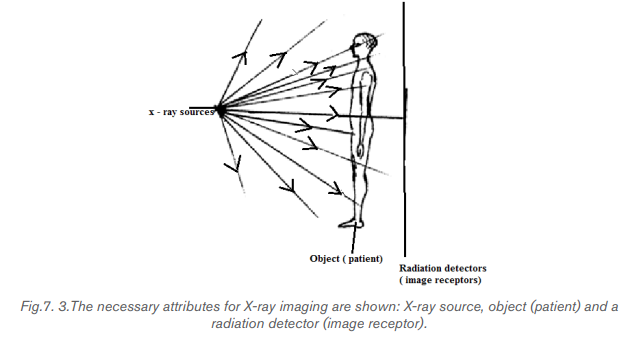
There are principally two interaction processes that give rise to the x-ray attenuation
(variation in photon transmission) through the patient which is the basis of X-rayimaging. These are photoelectric absorption and scattering processes.
A photon which has experienced an interaction process has either been absorbed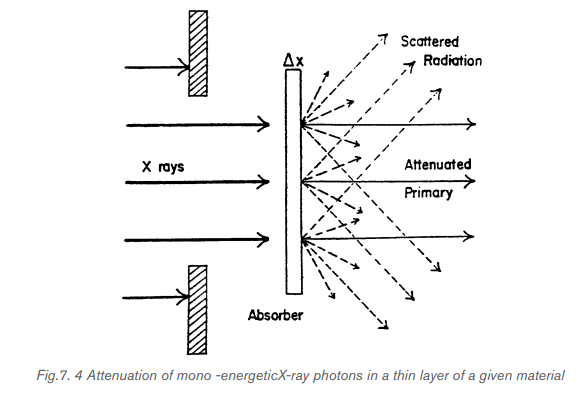
or has changed its energy and/or direction of motion. A photon that changes its
direction of motion is called a scattered photon. For mono-energetic x-ray photons,
the number of photons that experience such interactions and therefore removed
from the primary beam when this is incident on a thin layer of material is proportional
to the number of incident photons (N) and the thickness of the layer (dx) followingthe expression :
where µ is a constant of proportionality called the linear attenuation coefficient.
Integrating the above equation will result in
Where
 is the initial number of photons in the incident beam.
is the initial number of photons in the incident beam.
It can be seen that the incident beam photons (or the beam energy) is attenuated
exponentially as the x-rays travel through the material. The different interaction
processes involved, that are absorption, coherent and incoherent scattering andpair production, add their contributions to the total linear attenuation coefficient
Where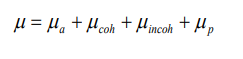
 and µ p are the contributions to the attenuation from
and µ p are the contributions to the attenuation from
photoelectric absorption, coherent scattering, incoherent scattering and pairproduction.
7.3.2 X-rays Imaging Techniques
a. Conventional Radiography
X-rays are able to pass through the human body and produce an image of internal
structures. The resulting image is called a radiograph, more commonly known
as an ‘X-ray’ or ‘plain film’. The common terms ‘chest X-ray’ and ‘abdomen
X-ray’ are widely accepted and abbreviated to CXR and AXR.
As a beam of X-rays passes through the human body, some of the X-rays photons
are absorbed or scattered producing reduction or attenuation of the beam with the
internal human structure acting as contrasting details. Therefore, tissues of high
density and/or high atomic number cause more X-ray beam attenuation and are
shown as lighter grey or white on radiographs. Less dense tissues and structures
cause less attenuation of the X-ray beam, and appear darker on radiographs
than tissues of higher density. The figure below shows the typical conventionalradiograph of a human body.
Five principal densities are easily recognized on this plain radiograph due to the
increase in their densities:
• Air/gas appears as black, e.g. lungs, bowel and stomach
• Fat is shown by dark grey, e.g. subcutaneous tissue layer, retroperitoneal fat
• Soft tissues/water appears as light grey, e.g. solid organs, heart, blood
vessels, muscle and fluid-filled organs such as bladder
• Bone appears as off-white
• Contrast material/metal: bright white.
In the past, X-ray films were processed in a darkroom or in freestanding daylight
processors. In modern practice, radiographic images are produced digitally using
one of two processes, computed radiography (CR) and digital radiography (DR).
DR uses a detector screen containing silicon detectors that produce an electrical
signal when exposed to X-rays. This signal is analyzed to produce a digital image.
Digital images obtained by CR and DR are sent to viewing workstations for
interpretation. Images may also be recorded on X-ray film for portability and remoteviewing.
The image given by a computer radiography may be reviewed and reported on
a computer workstation. This allows various manipulations of images as well as
application of functions such as measurements of length and angles measurements.
The relative variance of the shadows depends upon the density of the materials
within the object or body part. Dense, calcium – rich bone absorbs X-rays to a
higher degree than soft tissues that permit more X-rays to pass through them,
making X-rays very useful for capturing images of bone.
In projection radiography, there is much room for adjusting the energy level of the
X-rays depending on the relative densities of the tissues being imaged and also
how deep through a body the waves must travel in order to achieve the imaging.
• Images of bones (for instance, to examine a fracture or for diagnostic measures
related to bone conditions like osteoarthritis or certain cancers) require high
energy X-rays because of the high density of bone.
• Images of soft tissues like lungs, heart and breasts (both chest X-rays and
mammography are very common diagnostic applications of X-rays) require
relatively less energy from the X-rays in order to penetrate properly and
achieve excellent images.
• In order to achieve these different energies, technologists use X-ray generatorsof different voltages and equipped with anodes made of different metals.
Advantages and disadvantages of conventional radiography.
b. Mammography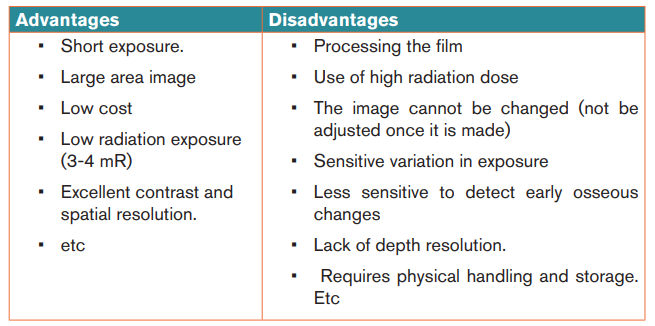
Mammography is a specialized medical imaging that uses low-dose X-rays to
investigate the internal structure of the breast. A mammography exam, called a
mammogram, helps in the early detection and diagnosis of women’s breast diseases
such as breast cancer before even experiencing any symptom. Below is a typical
mammography test showing the presence of abnormal areas of density, mass, orcalcification that may indicate the presence of cancer.
A mammography unit is a rectangular box that houses the tube in which X-rays are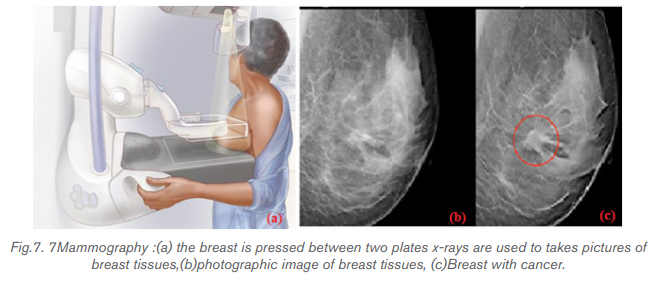
produced. The unit is used exclusively for X-ray exams of the breast, with special
accessories that allow only the breast to be exposed to the X-rays. Attached to the
unit is a device that holds and compresses the breast and positions it so imagescan be obtained at different angles.
In conventional film and digital mammography, a stationery X-ray tube
captures an image from the side and an image from above the compressed breast.
Breast tomosynthesis, also called three-dimensional (3-D) mammography and
digital breast tomosynthesis (DBT), is an advanced form of breast imaging where
multiple images of the breast from different angles are captured and reconstructed
(“synthesized”) into a three-dimensional image set. In this way, 3-D breast imaging
is similar to computed tomography (CT) imaging in which a series of thin “slices”
are assembled together to create a 3-D reconstruction of the body.
Advantages and disadvantages of mammography
Advantages are:
• Non-invasive procedure
• Minimum hazard of radiation.
• Increase in cancer detection rate.
• Improved positive predictive values for recall and biopsy.
• Etc.
Disadvantages are:
• May increase radiation dosage patient receivers.
• May require new equipment / training for techs and radiologist
• Is inconclusive in women under 35 years old due to dense breast tissue.
• Etc.
c. Computer Tomography scan (CT scan)
i) CT terminology
In 1970s, a revolutionary new X-ray technique was developed called Computer
tomography (CT), which produce an image of a slice through the body. The word
tomography comes from the Greek: tomos =slice, graph= picture.)
A computed tomography scan also known as CT scan, makes use of computer
processed combinations of many X-ray measurements taken from different angles
to produce cross-sectional (tomographic) images (virtual “slices”) of specific areas
of a scanned object, allowing the user to see inside the object without cutting it.
Other terms include computed axial tomography (CAT scan) and computer aided
tomography
The term “computed tomography” (CT) is often used to refer to X-ray CT, because
it is the most commonly known form but many other types of CT exist.
CT is an imaging technique whereby cross-sectional images are obtained with the
use of X-rays. In CT scanning, the patient is passed through a rotating gantry that
has an X-ray tube on one side and a set of detectors on the other. Information from
the detectors is analysed by computer and displayed as a grey-scale image. Owing
to the use of computer analysis, a much greater array of densities can be displayed
than on conventional X-ray films. This allows accurate display of cross-sectional
anatomy, differentiation of organs and pathology, and sensitivity to the presence of
specific materials such as fat or calcium. As with plain radiography, high- density
objects cause more attenuation of the X-ray beam and are therefore displayed aslighter grey than objects of lower density.
ii) Principle behind of computer tomography scan (CT scan).
Computer Tomography is shown in below figure: a thin collimated beam of X- ray (“
to collimate” means to “make straight”) passes through the body to a detector that
measures the transmitted intensity. The apparatus is rotated slightly about the body
axis and again scanned; this is repeated at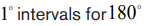 . The intensity of the
. The intensity of the
transmitted beam for the many points of each scan, and for each angles, are sent
to a computer that reconstructs the image of the slice. Note that the imaged slice is
perpendicular to the long axis of the body. For this reason, CT is sometimes calledcomputerize axial tomography.
The use of single detector would require a few minutes for many scans needed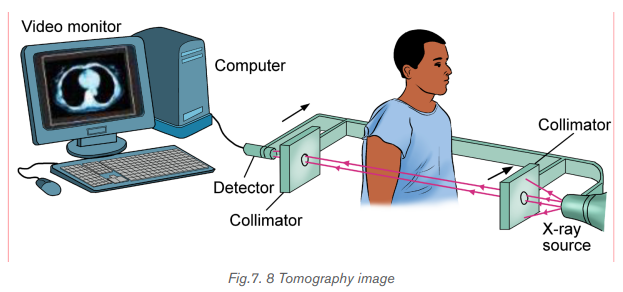
to form a complete image. Much faster scanner use a fan beam in which passing
through the entire cross section of the body are detected simultaneously by many
detectors. The x-ray source and the detectors are rotated about the patient and
an image requires only few seconds to be seen. This means that rays transmitted
through the entire body are measured simultaneously at each angle where thesource and detector rotate to take measurements at different angles.
CT images of internal organs, bones, soft tissue, and blood vessels provide greater
clarity and more details than conventional X-ray images, such as a chest X-Ray.
iii) Function of CT scan
• A motorized table moves the patient through a circular opening in the CT
imaging system.
• While the patient is inside the opening, an X-ray source and a detector
assembly within the system rotate around the patient. A single rotation
typically takes a second or less. During rotation the X-ray source produces
a narrow, fan-shaped beam of X-rays that passes through a section of the
patient’s body.
• Detectors in rows opposite the X-ray source register the X-rays that pass
through the patient’s body as a snapshot in the process of creating an image.
Many different “snapshots” (at many angles through the patient) are collected
during one complete rotation.
• For each rotation of the X-ray source and detector assembly, the image data
are sent to a computer to reconstruct all of the individual “snapshots” into one
or multiple cross-sectional images (slices) of the internal organs and tissues.
Note that, it is advisable to avoid unnecessary radiation exposure; a medically
needed CT scan obtained with appropriate acquisition parameter has benefits that
outweigh the radiation risks.
iv) Advantages and disadvantages of CT-Scan
CT-Scan has Advantages and disadvantages.
Disadvantages include:
• Risk to the patient because of the high radiation dose.
• Very expensive.
• Not commonly used to image painful joints modality
• Poor soft-tissue contrast.
• Higher radiation exposure.
• Involves exposure to ionising radiation(gamma-rays)
• Radiation material may cause allergic injection-site reactions in some people.
• etc
Advantages include:
• Images can be scored in a computer memory.
• The computer can also be used to construct a slide in a different plane using
other visual data.
• Widely available
• Quick exam.
• CT-Scan give a good contrast images
• High spatial resolution (bone/lung).
• Unlike most other imaging types, can show how different parts of the body
are working and can detect problem earlier.
• Can check how far a cancer has spread and how well treatment is working.• etc
Application activity 7.3
1. Outline the advantages and disadvantages of CT scan
2. Explain the types of x-ray imaging used in mammography.
3. In mammography exams, is the breast compression necessary? Why
4. A beam of X-rays passes through the human body of tissues with
different densities; explain the production of X-rays on less dense
tissues?
5. If you are getting a mammogram for the first time, what are the specific
questions you are expected to be asked by a doctor.
6. What does a biopsy mean?
7. Explain reasons why people do not attend breast screening (screeningmammography)
7.4 ENDOSCOPY
Activity 7.4
The picture below show the procedure that enables doctor to examine the
lining of esophagus and stomach. Examine it well and answer the followingquestion.
1. Name parts labelled letters A, B, C and D.
2. How do you call the examination technique taken by a doctor?
3. How can we examine inside the stomach by using light rays?
4. How is endoscopy performed?
5. What do you think are the advantages and disadvantages of thistechnique?
7.4.1 Description
Endoscopy is a nonsurgical procedure used to examine a person’s digestive tract.
Using an endoscope, which is a flexible tube with a light and camera attached to
it, the specialist can view pictures of your digestive tract on a monitor. During an
upper endoscopy, an endoscope is easily passed through the mouth and throat
and into the esophagus, allowing the specialist to view the esophagus, stomach,
and upper part of the small intestine. Similarly, endoscopes can be passed into thelarge intestine (colon) through the rectum to examine this area of the intestine.
7.4.2 Upper endoscopy
Upper Endoscopy (also known as gastroscopy, EGD, or
esophagogastroduodenoscopy) is a procedure that enables your surgeon to
examine the lining of the esophagus (swallowing tube), stomach and duodenum
(first portion of the small intestine). A bendable, lighted tube about the thickness ofyour little finger is placed through your mouth and into the stomach and duodenum.
How is the upper endoscopy performed?
Upper endoscopy is performed to evaluate symptoms of persistent upper abdominal
pain, nausea, vomiting, difficulty swallowing or heartburn. It is an excellent method
for finding the cause of bleeding from the upper gastrointestinal tract. It can be
used to evaluate the esophagus or stomach after major surgery. It is more accurate
than X-rays for detecting inflammation, ulcers or tumors of the esophagus, stomach
and duodenum. Upper endoscopy can detect early cancer and can distinguish
between cancerous and noncancerous conditions by performing biopsies ofsuspicious areas.
A variety of instruments can be passed through the endoscope that allows the
surgeon to treat many abnormalities with little or no discomfort, remove swallowed
objects, or treat upper gastrointestinal bleeding. Safe and effective control ofbleeding has reduced the need for transfusions and surgery in many patients.
7.4.3 Advantages and disadvantages of endoscopy
Advantages
• Complete visualization of the entire stomach or digestive tract.
• It is very safe and effective tool in diagnosis
• Does not leave any scar because it uses natural body openings.
• It is cost effective and has low risk
• They are generally painless.
• Can do therapeutic interventions
• Allows for sampling/biopsying of small bowel mucosa
• Allows for resection of polyps.
Overall, endoscope is very safe; however, the procedure has a few potential
complications which may include:
- Bleeding
- Perforation (tear in the gut wall)
- Infection
- Reaction to sedation (action of administering a sedative drug to produce a
state of calm or sleep.
- Technically difficult procedure
- Very time consuming (Procedure can take > 3 hours)
- Patient may need to be admitted to the hospital
- Higher risk of small bowel perforation
- Case reports of pancreatitis and intestinal necrosis
- Reported incidents of aspiration and pneumonia
Application activity 7.4
1. What are instruments used to view the oesophagus, stomach and
upper small intestine of human
2. Discuss different functions of endoscope in medicine.
3. Compare and contrast colonoscopy and gastroscopy4. What are some of negative effects of using endoscopy?
7.5 MAGNETIC RESONANCE IMAGING (MRI)Activity 7.5
i) The diagram above is a Magnetic Resonance Imaging (MRI) machine.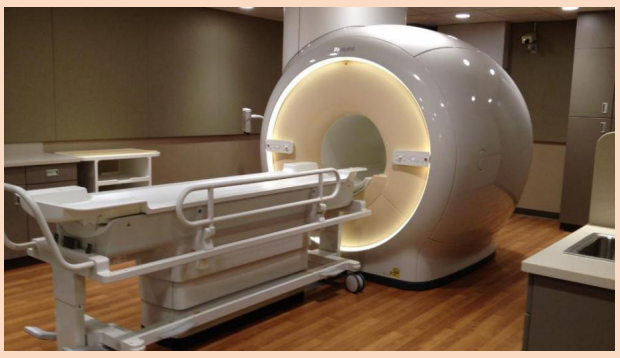
Basing on its name, explain what it does.
ii) Comparing it to other imaging techniques, explain how this machine is
different from other imaging machines.
iii) Would you advise a pregnant woman to always use this machine for a
medical checkup? Explain your view
iv) From your reasoning in iii) above, suggest advantages and disadvantagesof using MRI machine
Historically, Magnetic Resonance Imaging as with all medical imaging techniques, isa relatively new technology with its foundations beginning during the year of 1946.
Felix Bloch and Edward Purcell independently discovered the magnetic resonance
phenomena during this year, Up until the 1970s MRI was being used for chemical
and physical analysis. Then in 1971 Raymond Damadian showed that nuclear
magnetic relaxation times of tissues and tumors differed motivating scientists to
use MRI to study disease. MRI began in the central nervous system, but it has
now extended to all regions of the body. It is involving three very complex topics in
physics like: Nuclear, Magnetic and Resonance (NMR). In MRI, a particular type of
nucleus is selected and its distribution in the body is monitored. Hydrogen is the
most commonly imaged element, not only due to its abundant in the body, but also
because it gives the strongest MRI signal.
7.5.1. Concepts MRI
Magnetic Resonance (MRI) Imaging has become the dominant clinical imaging
modality with widespread, primarily noninvasive, applicability throughout the body
and across many disease processes. The progress of MR imaging has been rapid
compared with other imaging technologies and it can be attributed in part to physics
and in part to the timing of the development of MR imaging, which corresponded to
an important period of advances in computing technology.
Initially let us described how magnetic resonance can be demonstrated with a pair
of magnets and a compass. If a compass happens to find itself near a powerful
magnet, the compass needle will align with the field. In a normal pocket compass,
the needle is embedded in liquid to dampen its oscillations. Without liquid, the
needle will vibrate through the north direction for a period before coming to rest.
The frequency of the oscillations depends on the magnetic field and of the strengthof the magnetic needle.
Let us focus on what made the needle oscillate. It was the small movements of the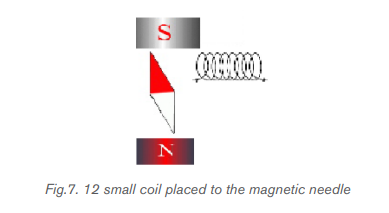
magnet, back and forth, or more precisely the oscillation of a weak magnetic field
perpendicular to the powerful stationary magnetic field caused by the movement
of the magnet. But oscillating magnetic field is what we understand by “radio
waves”, which means that in reality, we could replace the weak magnet with other
types of radio wave emitters. This could, for example, be a small coil subject to an
alternating current, as shown in figure above. Such a coil will create a magnetic
field perpendicular to the magnetic needle. The field changes direction in synchronywith the oscillation of the alternating current, so if the frequency of the current is
adjusted to the resonance frequency of the magnetic needle, the current will set
the needle in motion. This is also applied in an MR scanner. In summary, the needle
can be set in motion from a distance by either waving a magnet or by applying an
alternating current to a coil. In both situations, magnetic resonance is achieved
when the magnetic field that motion or alternating currents produce, oscillates at
the resonance frequency. When the waving or the alternating current is stopped,
the radio waves that are subsequently produced by the oscillating needle willinduce a voltage over the coil.
MRI uses the magnetic properties of spinning hydrogen atoms to produce images.
The first step in MRI is the application of a strong, external magnetic field. For this
purpose, the patient is placed within a large powerful magnet. Most current medical
MRI machines have field strengths of 1.5 or 3.0 Tesla. The hydrogen atoms within
the patient align in a direction either parallel or antiparallel to the strong external
field. A greater proportion aligns in the parallel direction so that the net vector of
their alignment, and therefore the net magnetic vector, will be in the direction of
the external field. This is known as longitudinal magnetization. A second magnetic
field is applied at right angles to the original external field. This second magnetic
field is known as the radiofrequency pulse (RF pulse), because it is applied at a
frequency in the same part of the electromagnetic spectrum as radio waves. A
magnetic coil, known as the RF coil, applies the RF pulse. The RF pulse causes
the net magnetization vector of the hydrogen atoms to turn towards the transverse
plane, i.e. a plane at right angles to the direction of the original, strong external field.
The component of the net magnetization vector in the transverse plane induces an
electrical current in the RF coil. This current is known as the MR signal and is the
basis for formation of an image. Computer analysis of the complex MR signal fromthe RF receiver coils is used to produce an MR image.
7.5.2. The magnetism of the body
Let‘s see how magnet needles with and without spin are affected by radio waves,
we now turn to the “compass needles” in our own bodies.
a) Most frequently, the MR signal is derived from hydrogen nuclei (meaning the
atomic nuclei in the hydrogen atoms). Most of the body’s hydrogen is found
in the water molecules. Few other nuclei are used for MR.
b) Hydrogen nuclei (also called protons) behave as small compass needles that
align themselves parallel to the field.
c) The compass needles (the spins) are aligned in the field, but due to movements
and nuclear interactions in the soup, the alignment only happens partially.
d) The nuclei in the body move among each other (thermal motion) and the net
magnetization in equilibrium is thus temperature dependent.
e) Due to the number of hydrogen nuclei (about 27 10 ) found in the body, the net
magnetization still becomes measurable. It is proportional to the field: A large
field produces a high degree of alignment and thus a large magnetization andbetter signal to noise ratio.
7.5.3 Magnetic Resonance Imaging (MRI).
The hydrogen nucleus is the most use in MRI.The technique uses a very powerful
magnet to align the nuclei of atoms inside the body, and a variable magnetic field that
causes the atoms to resonate, a phenomenon called nuclear magnetic resonance.
The nuclei produce their own rotating magnetic fields that a scanner detects and
uses to create an image.
MRI is used to diagnose a variety of disorders, such as strokes, tumors, aneurysms,
spinal cord injuries, multiple sclerosis and eye or inner ear problems. It is also widelyused in research to measure brain structure and function, among other things.
An MRI scan can be used to examine almost any part of the body, including the:
• brain and spinal cord
• bones and joints
• breasts
• heart and blood vessels
• internal organs, such as the liver, womb or prostate gland ,etc
The results of an MRI scan can be used to help diagnose conditions,
plan treatments and assess how effective previous treatment has been.
7.5.4. Functional of MRI Scan
There are many forms of MRI, some of them are:
a) Diffusion weighted imaging.
Diffusion-weighted imaging (DWI) is sensitive to the random Brownian motion
(diffusion) of water molecules within tissue. The greater the amount of diffusion,
the greater the signal loss on DWI. Areas of reduced water molecule diffusion
show on DWI as relatively high signal. Diffusion-weighted imaging is the
most sensitive imaging test available for the diagnosis of acute cerebral
infarction. With the onset of acute ischaemia and cell death there is increased
intracellular water (cytotoxicoedema) with restricted diffusion of water molecules.
An acute infarct therefore shows on DWI as an area of relatively high signal.
b) Perfusion-weighted imaging
In perfusion-weighted imaging (PWI) the brain is rapidly scanned following
injection of a bolus of contrast material (gadolinium). The data obtained may be
represented in a number of ways including maps of regional cerebral blood volume,
cerebral blood flow, and mean transit time of the contrast bolus. PWI may be used
in patients with cerebral infarct to map out areas of brain at risk of ischaemia that
may be salvageable with thrombolysis.
c) Magnetic resonance spectroscopy
Magnetic resonance spectroscopy (MRS) uses different frequencies to identify
certain molecules in a selected volume of tissue, known as a voxel. Following data
analysis, a spectrographic graph of certain metabolites is drawn. Metabolites of
interest include lipid, lactate, NAA (N-acetylaspartate), choline, creatinine, citrate
and myoinositol. Uses of MRS include characterization of metabolic brain disorders
in children, imaging of dementias, differentiation of recurrent cerebral tumour from
radiation necrosis, and diagnosis of prostatic carcinoma.
d) Blood oxygen level-dependent imaging
Blood oxygen level-dependent (BOLD) imaging is a non-invasive functional MRI
(fMRI) technique used for localizing regional brain signal intensity changes in
response to task performance. BOLD imaging depends on regional changes in
concentration of deoxyhemoglobin, and is therefore a tool to investigate regional
cerebral physiology in response to a variety of stimuli. BOLD fMRI may be used prior
to surgery for brain tumor or arteriovenous malformation (AVM), as a prognosticindicator of the degree of postsurgical deficit.
7.5.5 Advantage and disadvantages of MRI.
Advantages of MRI in clinical practice include:
1. Excellent soft tissue contrast and characterization
2. Lack of ionizing radiation.
3. Noninvasive machine.
4. Lack of artefact from adjacent bones, e.g. pituitary fossa
Disadvantages of MRI:
1. High capital and running costs.
2. Image selected and interpretation is complex.
3. Examination can be difficult for some people who are claustrophobic
4. The examination is noisy and takes long.
5. Hazards with implants, particularly pacemakers.6. Practical problems associated with large superconducting magnets.
In additional to that, out of imaging the techniques discussed above there other
imaging techniques called “radionuclide imaging/nuclear medicine/ scintigraphy”.
A radionuclide is used to collect in areas where there is a lot of bone activity.
This method uses gamma radiation to form images by injection of various
radiopharmaceuticals. The most commonly used radionuclide in clinical practice
is technetium, written in this text as where m stands for metastable.
where m stands for metastable.
Other commonly used radionuclides include gallium citrate
indium
Application activity 7.5
1. With clear explanations, explain the benefit and limitation of MRI
machine.
2. What is meant by relaxation in the context of MRI?
3. Give the reasons why the hydrogen nucleus is most used in MRI.
4. What does NMR stand for? Explain carefully the role of the three terms
involved
5. With the aid of drawing, discuss the basic steps in the formation ofMRI image.
Skills Lab 7
In this activity you will make a visit to the nearest hospital.
Note: Make inquiry either through your class leaders or class tutor to know
whether the hospital has the following.
• Ultrasound machine
• X-ray machine
• Endoscopy
• Magnetic Resonance Imaging (MRI) machine.
The main aim of the visit is to understand how these machines work.
The following are guiding questions you may ask either laboratory technician
or the doctor.
a. What is the main objective(s) of using these machines?
b. What does one need to do to use these machines?
c. What are the precautions that must be taken before using any of these
machines?
d. Are there regulations guiding any person working in the rooms where
these machines are installed?
e. Could there be negative effects of these machines on human body if
used regularly?
You can also ask any question you feel can make you understand this concept
better.
Make sure you note down something as the doctor or laboratory technician
explains the asked questions.
After leaving the hospital, Make a comprehensive report and compare the
information you got from the hospital to the one learnt in this unit.Present your findings (in the report) to your class and to your tutor.
End of unit 7 assessment
I-5: Choose the correct answer.
1. One of the medical imaging using X-ray is:
A. thermography
B. CT Scan
C. endoscopy
D. both of them
2. Magnetic Resonance Imaging uses:
A. x-rays
B. Light
C. Magnetization
D. both of them
3. The medical imaging techniques used injection of various
radiopharmaceuticals is:
A. Mammography
B. Radiography
B. Radionuclide.
D. Endoscopy
4. Mammography is used to detect:
A. Brain diseases
B. Baby diseases
C. Breast diseases
D. None of them
5. A radionuclide scan may be done for one reason:
A. A radionuclide is used to collect the areas where the infrared are
synchronized.
B. A radionuclide is used to collect in areas where there is a lot of bone
activity.
C. A radionuclide is use to collect the areas where gamma camera are
produced image
D. A radionuclide is used to collect information from the exam of lining
of esophagus.
6. Write the missing word or words on the space before each number.
A. The best human ears can respond to frequencies from about 20Hz
to almost 20 000Hz. This frequency is called the ……….
B. A variety of instruments can be passed through the endoscope
that allows the surgeon to treat many abnormalities with little or no
discomfort, remove swallowed objects
C. Equipment is safe, easy to handle, can be operated and be portable.
This in one of the ……. of ultrasound
D. When the pulse of ultrasound is sent into the body and meets a
boundary between two media, most of the wave is reflected and a
strong …… is recorded.
E. Transducers used are different depending on …… of a patient, one
has 5 MHz and other 3.5 MHz.
F. Hydrogen nuclei (also called protons) behave as small ............ that
align themselves parallel to the field.
G. In…………………. there are appearance three words: nuclear,
magnetic and resonance.
H. Lack of ……. radiation is one of the advantages of MRI.
7. Answer by True if it is true and by False if it is False
A. The use of gamma radiation to form images following the injection of
various radiopharmaceuticals is known as Scintigraphy.
B. This decision to scan or not to scan a normal pregnancy must be
made only by the photographer. There are universally accepted
guidelines at present.
C. Tissue in the body absorbs and scatters ultrasound in the same
ways. Lower frequencies are more rapidly absorbed (attenuated)
than higher frequencies.
D. Upper endoscopy uses light and camera to view the esophagus,
stomach, and upper part of the small intestine.
E. Ultrasound is both generated and detected through high frequency
oscillations in piezoelectric crystals so there is ionizing radiationexposure associated with ultrasound imaging.
iii) Determine the values of intensity of reflection coefficient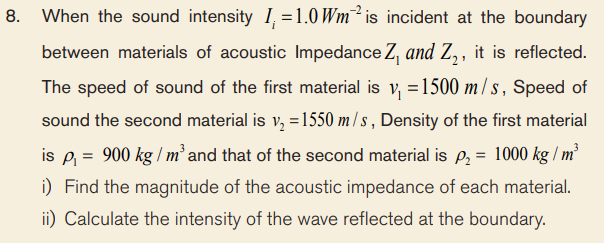
iv) Calculate the intensity of the wave transmitted into the second
material.
9. The distance between pulse representing ultrasonic reflections fromopposite sides of a fetus head was recorded on a screen of a cathode
10. Compare and contrast endoscopy imaging and radionuclide imaging
11. What are the advantages of MRI in clinical practice?
12. Why areas of the body can be imaged by ultrasound??
13. In mammography exams, is the breast compression necessary? Why
14. Historically, MRI began in the central nervous system, but it is now
extended to all regions of the human body. The excellent resolution and
contrast available in any chosen plane in the body, makes the MRI an
invaluable diagnostic tool with which to study body structure, functionand chemistry, as well as disease. Discuss the application of MRI.
