UNIT 11: MEDICAL IMAGING
Key unit Competence: Analyze the processes in medical imaging.
Learning objectives:• Outline specific purposes of imaging techniquesINTRODUCTORY ACTIVITY
• Explain the effects of various imaging techniques for particular
purposes.
• Explain the basic functioning principles of major medical imaging
techniques• Identify advantages and disadvantages of medical imaging techniques
Investigation on the use of medical imaging techniques:
Years ago, the only way to get information from inside of human bodies was
through surgery. In modern medicine, medical imaging has undergone major
advancements and this ability to obtain information about different parts of
the human body has many useful clinical applications.
Using information provided on the above pictures, answer to the following
questions:
1. Observe the image A, B, and C (Fig.12.1) and describe what is happening.
2. Suggest the technique that is being used for each image?
3. Explain the working principle of the mentioned techniques in question2?
11.1 X-RAY IMAGING.
11.1.1 Interaction of X-rays with matter.
a. Introduction
In unit 10, we learnt that X-rays are electromagnetic radiation produced by
focusing a beam of high energy electron on a target material in x-ray tube. Since
the major part of the energy of the electrons is converted into heat in the target
(only about 1% will appear as X-rays), the target material should have a high
melting point and good heat conduction ability. To get a high relative amount of
X-ray energy, the anode material should be of high atomic number. Tungsten is
the dominating anode material and is in modern X-ray tubes often mixed withRhenium.
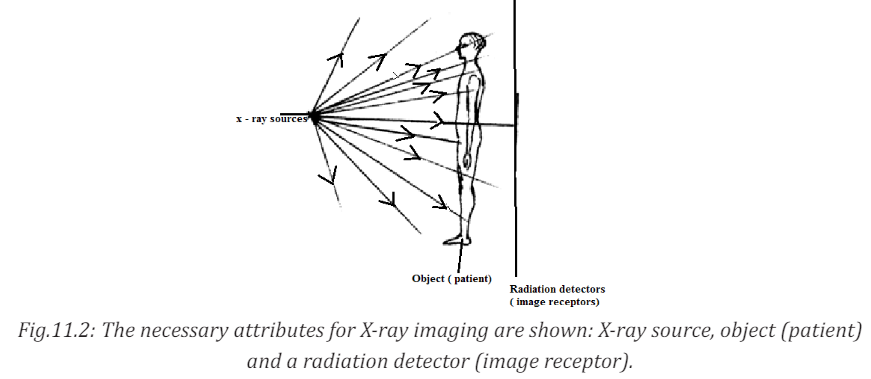
In X-ray diagnostics, radiation that is partly transmitted through and partly
absorbed in the irradiated object is utilized. An X-ray image shows the variations
in transmission caused by structures in the object of varying thickness, densityor atomic composition.
b. Attenuation and Absorption of X-rays
There are principally two interaction processes that give rise to the x-ray
attenuation (variation in photon transmission) through the patient which is
the basis of X-ray imaging. These are photoelectric absorption and scatteringprocesses.
A photon which has experienced an interaction process has either been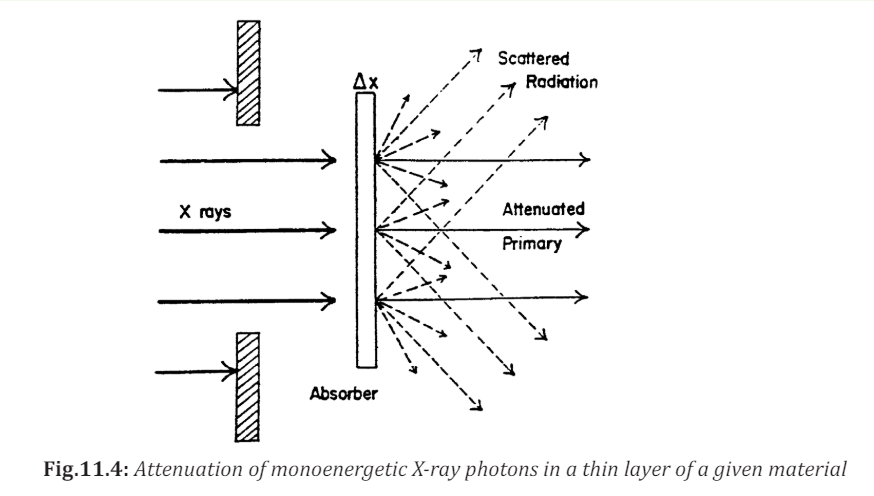
absorbed or has changed its energy and/or direction of motion. A photon that
changes its direction of motion is called a scattered photon. For monoenergetic
x-ray photons, the number of photons that experience such interactions and
therefore removed from the primary beam when this is incident on a thin
layer of material is proportional to the number of incident photons (N) and thethickness of the layer (dx) following the expression :
where µ is a constant of proportionality called the linear attenuation coefficient.
Integrating the above equation will result in

where
It can be seen that the incident beam photons (or the beam energy) is attenuated is the initial number of photons in the incident beam.
is the initial number of photons in the incident beam.
exponentially as the X-rays travel through the material. The different interaction
processes involved, that are absorption, coherent and incoherent scattering
and pair production, add their contributions to the total linear attenuationcoefficient
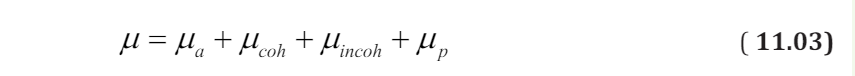
where µa, µcoh, µincoh, and µp are the contributions to the attenuation from photoelectric absorption, coherent scattering, incoherent scattering and pair production.
C. Contrast
The contrast is a measure of the difference in radiation transmission or
other parameters between two adjacent areas in a radiographic image.
Contrast plays an important role in the ability of a radiologist to perceiveimage detail.
where ε1and ε2 are energies of the monoenergetic X-ray photons per unit area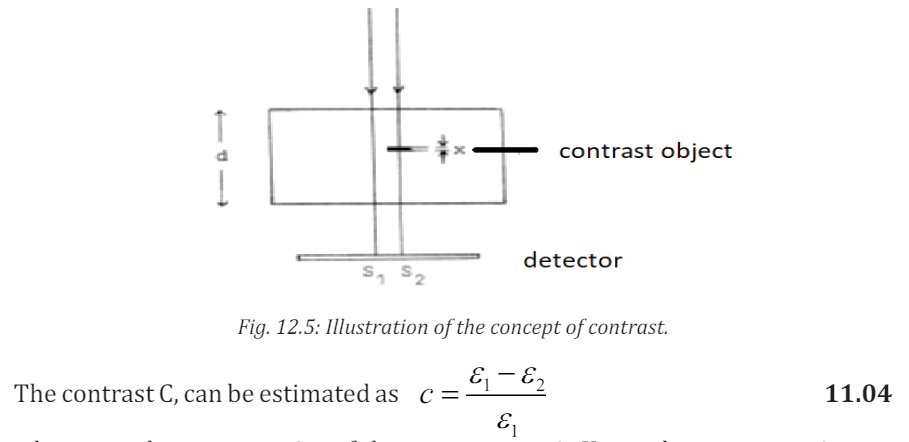
reaching the detector and therefore absorbed in the detector without and
with the contrasting detail respectively. In the case where the film is used as
image receptor, the signal is obtained in terms of the optical density. The image
contrast is then usually defined as the optical density difference beside andbehind the contrasting detail.
In such situation where monoenergetic photons are considered and no scattered
radiation is reaching the detector, the absorbed energy in the detector can bewritten as
Where d, is the thickness of the object with linear attenuation coefficient

The energy through the contrasting detail can be expressed as
where ε0 is the energy absorbed in the detector with no object present, x is the
thickness of the contrasting detail with its linear attenuation coefficient µ2
Replacing equation 12.05 and 12.06 into equation 12.04 we obtain the contrast
The contrast is then proportional to the difference in the linear attenuation
coefficients and the thickness of the contrasting detail. Therefore, when
scattered radiation is neglected in the process, the contrast is independent of
the thickness d of the object but also it does not depend on where in the object
the contrasting detail is situated.
The ability of conventional radiography to display a range of organs and
structures may be enhanced by the use of various contrast materials, also
known as contrast media. The most common contrast materials are based on
barium or iodine. Barium and iodine are high atomic number materials thatstrongly absorb X-rays and are therefore seen as dense white on radiography.
11.1.2 X-rays Imaging Techniques
a. Conventional Radiography
X-rays are able to pass through the human body and produce an image of internal
structures. The resulting image is called a radiograph, more commonly known
as an ‘X-ray’ or ‘plain film’. The common terms ‘chest X-ray’ and ‘abdomen X-ray’are widely accepted and abbreviated to CXR and AXR.
As a beam of X-rays passes through the human body, some of the X-rays photons
are absorbed or scattered producing reduction or attenuation of the beam withthe internal human structure acting as contrasting details.
Therefore tissues of high density and/or high atomic number cause more X-ray
beam attenuation and are shown as lighter grey or white on radiographs. Less
dense tissues and structures cause less attenuation of the X-ray beam, and
appear darker on radiographs than tissues of higher density. The figure belowshows the typical conventional radiograph of a human body
Fig.11.6: The five principal radiographic densities. This radiograph of a benign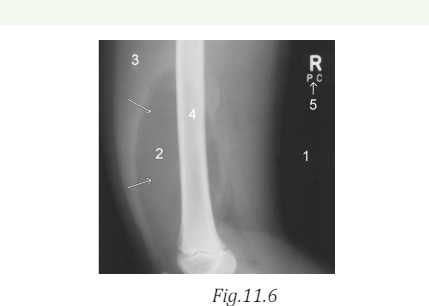
lipoma (arrows) in a child’s thigh demonstrates the five basic radiographic
densities: (1) air; (2) fat; (3) soft tissue; (4) bone; (5) metal. (David A Disle
(2012) Imaging for students. Fourth Edition. (Page 1))
Five principal densities are easily recognized on this plain radiograph due to
the increase in their densities:
1. Air/gas appears as black, e.g. lungs, bowel and stomach
2. Fat is shown by dark grey, e.g. subcutaneous tissue layer, retroperitoneal
fat
3. Soft tissues/water appears as light grey, e.g. solid organs, heart, blood
vessels, muscle and fluid-filled organs such as bladder
4. Bone appears as off-white
5. Contrast material/metal: bright white.
In the past, X-ray films were processed in a darkroom or in freestanding
daylight processors. In modern practice, radiographic images are produced
digitally using one of two processes, computed radiography (CR) and digital
radiography (DR).
DR uses a detector screen containing silicon detectors that produce an electrical
signal when exposed to X-rays. This signal is analyzed to produce a digital
image. Digital images obtained by CR and DR are sent to viewing workstations
for interpretation. Images may also be recorded on X-ray film for portability
and remote viewing.
The image given by a computer radiography may be reviewed and reported
on a computer workstation. This allows various manipulations of images as
well as application of functions such as measurements of length and angles
measurements.
The relative variance of the shadows depends upon the density of the materials
within the object or body part. Dense, calcium – rich bone absorbs X-rays to a
higher degree than soft tissues that permit more X-rays to pass through them,
making X-rays very useful for capturing images of bone.
In projection radiography, there is much room for adjusting the energy level of
the X-rays depending on the relative densities of the tissues being imaged and
also how deep through a body the waves must travel in order to achieve theimaging.
• Images of bones (for instance, to examine a fracture or for diagnosticb. Mammography
measures related to bone conditions like osteoarthritis or certain
cancers) require high-energy X-rays because of the high density of
bone.
• Images of soft tissues like lungs, heart and breasts (both chest X-rays
and mammography are very common diagnostic applications of X-rays)
require relatively less energy from the X-rays in order to penetrate
properly and achieve excellent images.
• In order to achieve these different energies, technologists use X-ray
generators of different voltages and equipped with anodes made ofdifferent metals.
ACTIVITY 11.2
One day a girl suffering from the breast tells her mother about the
problem. And her mother advises her to go to the hospital to consult a
doctor.a. Think of the problem that girl may have.Mammography is a specialized medical imaging that uses low-dose X-rays to
b. Try to explain what may be the cause of that problem.
c. If you are a doctor how can you detect such problem?
d. Which advise can you give to other people who are not suffering
froe. m that problem in order to prevent it?
investigate the internal structure of the breast. A mammography exam, called
a mammogram, helps in the early detection and diagnosis of women’s breast
diseases such as breast cancer before even experiencing any symptom. Below
is a typical mammography test showing the presence of abnormal areas ofdensity, mass, or calcification that may indicate the presence of cancer.
Mammography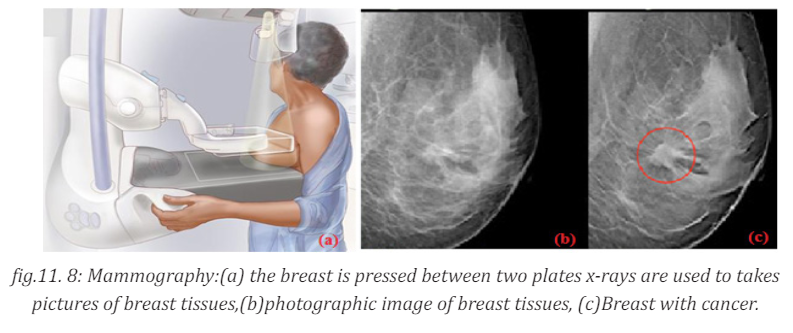
a) the breast is pressed between two plates x-rays are used
to takes pictures of breast tissues,(b)photographic image of breast tissues, (c)
Breast with cancer. A mammography unit is a rectangular box that houses the
tube in which X-rays are produced. The unit is used exclusively for X-ray exams
of the breast, with special accessories that allow only the breast to be exposed
to the X-rays. Attached to the unit is a device that holds and compresses thebreast and positions it so images can be obtained at different angles.
In conventional film and digital mammography, a stationery X-ray tube
captures an image from the side and an image from above the compressed breast.
Breast tomosynthesis, also called three-dimensional (3-D) mammography
and digital breast tomosynthesis (DBT), is an advanced form of breast imaging
where multiple images of the breast from different angles are captured and
reconstructed (“synthesized”) into a three-dimensional image set. In this way,
3-D breast imaging is similar to computed tomography (CT) imaging in which
a series of thin “slices” are assembled together to create a 3-D reconstructionof the body.
c. Computer tomography scan (ct scan)
CT terminology
In 1970s, a revolutionary new X-ray technique was developed called Computer
tomography (CT), which produce an image of a slice through the body. Theword tomography comes from the Greek: tomos =slice, graph= picture.)
A computed tomography scan also known as CT scan, makes use of computer
processed combinations of many X-ray measurements taken from different
angles to produce cross-sectional (tomographic) images (virtual “slices”) of
specific areas of a scanned object, allowing the user to see inside the object
without cutting it. Other terms include computed axial tomography (CAT scan)
and computer aided tomography. The term “computed tomography” (CT) is
often used to refer to X-ray CT, because it is the most commonly known formbut many other types of CT exist.
CT is an imaging technique whereby cross-sectional images are obtained with
the use of X-rays. In CT scanning, the patient is passed through a rotating
gantry that has an X-ray tube on one side and a set of detectors on the other.
Information from the detectors is analysed by computer and displayed as a
grey-scale image. Owing to the use of computer analysis, a much greater arrayof densities can be displayed than on conventional X-ray films.
This allows accurate display of cross-sectional anatomy, differentiation of
organs and pathology, and sensitivity to the presence of specific materials such
as fat or calcium. As with plain radiography, high- density objects cause more
attenuation of the X-ray beam and are therefore displayed as lighter grey thanobjects of lower density.
Principle behind of computer tomography scan (CT scan).
Computer Tomography is shown in below figure: a thin collimated beam of
X- ray(“ to collimate” means to “make straight”) passes through the body to adetector that measures the transmitted intensity. Measurements are made at
a large number of points as the source and detector are moved past the body
together. The apparatus is rotated slightly about the body axis and again scanned;
this is repeated at 1 intervals for 180 . The intensity of the transmitted beam for
the many points of each scan, and for each angles, are sent to a computer that
reconstructs the image of the slice. Note that the imaged slice is perpendicular
to the long axis of the body. For this reason, CT is sometimes called computerizeaxial tomography.
The use of single detector would require a few minutes for many scans needed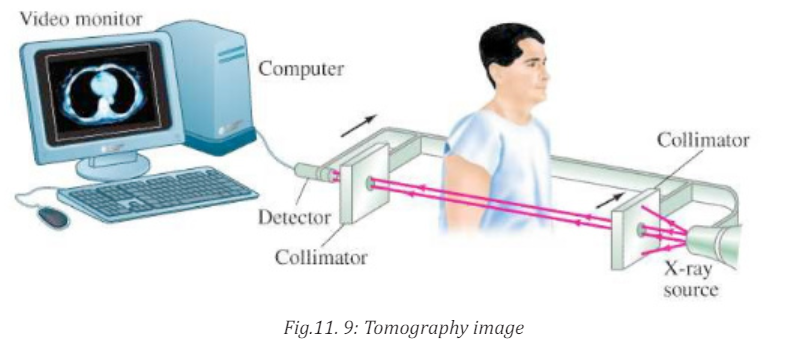
to form a complete image. Much faster scanner use a fan beam in which passing
through the entire cross section of the body are detected simultaneously by
many detectors. The x-ray source and the detectors are rotated about the
patient and an image requires only few seconds to be seen. This means that
rays transmitted through the entire body are measured simultaneously at each
angle where the source and detector rotate to take measurements at differentangles.
CT images of internal organs, bones, soft tissue, and blood vessels provide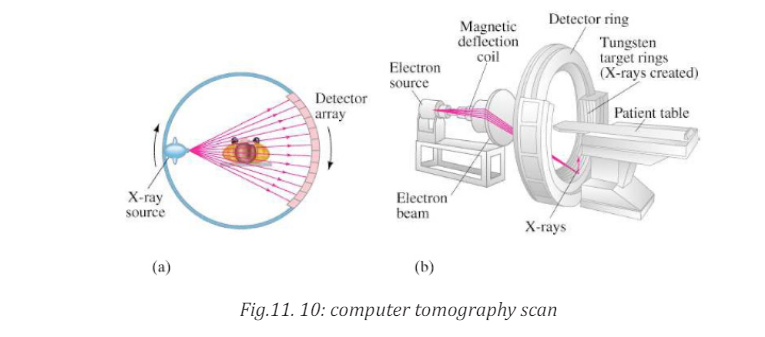
greater clarity and more details than conventional X-ray images, such as a chestX-Ray
Function of CT scan• A motorized table moves the patient through a circular opening in theNote that, it is advisable to avoid unnecessary radiation exposure; a medically
CT imaging system.
• While the patient is inside the opening, an X-ray source and a detector
assembly within the system rotate around the patient. A single rotation
typically takes a second or less. During rotation the X-ray source
produces a narrow, fan-shaped beam of X-rays that passes through a
section of the patient’s body.
• Detectors in rows opposite the X-ray source register the X-rays that
pass through the patient’s body as a snapshot in the process of creating
an image. Many different “snapshots” (at many angles through the
patient) are collected during one complete rotation.
• For each rotation of the X-ray source and detector assembly, the
image data are sent to a computer to reconstruct all of the individual
“snapshots” into one or multiple cross-sectional images (slices) of theinternal organs and tissues.
needed CT scan obtained with appropriate acquisition parameter has benefitsthat outweigh the radiation risks.
11.1.3 Checking my progress1. Outline the advantage and disadvantages CT scan11.2 ULTRASONIC IMAGING
2. Explain the types of x-ray imaging used in mammography.
3. In mammography exams, is the breast compression necessary? Why
4. A beam of X-rays passes through the human body of tissues with
different densities; explain the production of X-rays on less densetissues?
11.2.1 Basics of Ultra sound and its production
ACTIVITY 11.3
1. Distinguish ultrasound from infrasound?
2. Where do you think ultrasound may be applied in daily life?3. Advise on how ultrasound be used in medicine?
Sound can refer to either an auditory sensation in the brain or the disturbance
in a medium that causes this sensation. Hearing is the process by which the ear
transforms sound vibrations into nerve impulses that are delivered to the brain
and interpreted as sounds. Sound waves are produced when vibrating objects
produce pressure pulses of vibrating air. The auditory system can distinguishdifferent subjective aspects of a sound, such as its loudness and pitch.
Pitch is the subjective perception of the frequency, which in turn is measured in
cycles per second, or Hertz (Hz). The normal human audible range extends from
about 20 Hz to 20 000 Hz, but the human ear is most sensitive to frequencies
of 1 000 Hz to 4 000 Hz. Loudness is the perception of the intensity of sound,
related to the pressure produced by sound waves on the tympanic membrane.
The pressure level of sound is measured in decibels (dB), a unit for comparing
the intensity of a given sound with a sound that is just perceptible to the normal
human ear at a frequency in the range to which the ear is most sensitive. On the
decibel scale, the range of human hearing extends from 0 dB, which represents
the auditory threshold, to about 130 dB, the level at which sound becomespainful.
11.2.2 Interaction of sound waves with different structure inside the body
a. Introduction
Ultrasound imaging uses ultra-high-frequency sound waves to produce cross sectional
images of the body. Ultrasound is actually sound with a frequency in
excess of 20 kHz, which is the upper limit of human hearing. Typical ultrasoundfrequencies used for clinical purposes are in the 2 MHz to 10 MHz range.
Different tissues in a human or animal body alter the ultra sound waves in
different ways. Some waves are reflected directly while others scatter the
waves before they return to the transducer as echoes. The reflected ultrasound
pulses detected by the transducer need to be amplified in the scanner or
ultrasonic probe. The echoes that come from deep within the body are more
attenuated than those from the more superficial parts and therefore requiredmore amplification.
When echoes return to the transducer, it is possible to reconstruct a two
dimensional map of all the tissues that have been in the beams. The information
is stored in a computer and displayed on a video (television) monitor. Strong
echoes are said to be of the high intensity and appear as brighter dots on thescreen.
b. Reflection of ultrasound
When the pulse of ultrasound is sent into the body and meets a boundary between
two media, of different specific acoustic impedance Z, the sound wave needs to
change gear in order to continue. If the difference in Z across the boundary is
large the wave cannot easily adjust: there is an “acoustic mismatch”. Most of
the wave is reflected and a strong echo is recorded. The fraction of intensity
reflected back to that incident at the normal incidence, is known as theintensity of reflection coefficient
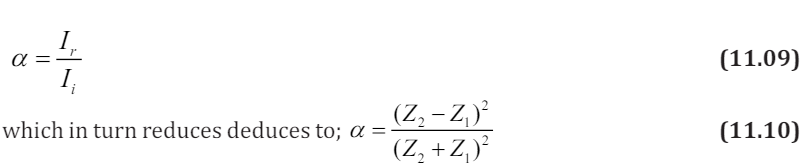
where Z is acoustic impedance
Note that large difference in Z give rise to large values for α, producing strongechoes
Ultrasounds are high-frequency sound waves above the human ear’s audible
range: that is with frequency sound waves greater than 20 kHz. In fact, the
frequencies used in medicine are much higher than this, typically between
1 MHz and 15 MHz. like all sound waves, ultrasound consists of longitudinal,
elastic or pressure waves, capable of traveling through solids, liquids and gases.This makes them ideal for penetrating the body, unlike transverse mechanical
waves, which cannot travel to any great extent through fluids.
c. Attenuation of ultrasound
The attenuation of the waves describes the reduction in its intensity as they
travel through a medium. This loss is due to a number of factors:• The wave simply “spreads out” and suffers an “inverse square law type”The amount of absorption of ultrasound beam in a medium is described by the
reduction in intensity.
• The wave is scattered away from its original direction
• The wave is absorbed in the medium.
absorption coefficientα , which is intensity level per unit length. It is expressed
in decibels per cm and it firstly depends on the type of medium the wave is
propagating into. As example whilst water absorbs very little ultrasound,
bone is a strong absorber, putting it at risk, for example, during high- powerultrasound therapy.
Secondly, higher frequencies suffer greater absorption. In fact if the frequency is
doubled, the absorption increases by the factor of four. This has very important
consequences when choosing the best frequency at which to image the body. If
the selected frequency is too high, the ultrasound will not be able to penetrateto the regions under investigation.
11.2.3 Ultrasonic imaging techniques
The basic component of the ultrasound probe is the piezoelectric crystal.
Excitation of this crystal by electrical signals causes it to emit ultra-high frequency
sound waves; this is the piezoelectric effect. The emitted ultrasound
waves are reflected back to the crystal by the various tissues of the body. These
reflected sound waves also called the “echoes” act on the piezoelectric crystal
in the ultrasound probe to produce an electric signal, again by the piezoelectriceffect. It is this electric signal which is analysed by a computer produces a cross sectional image.
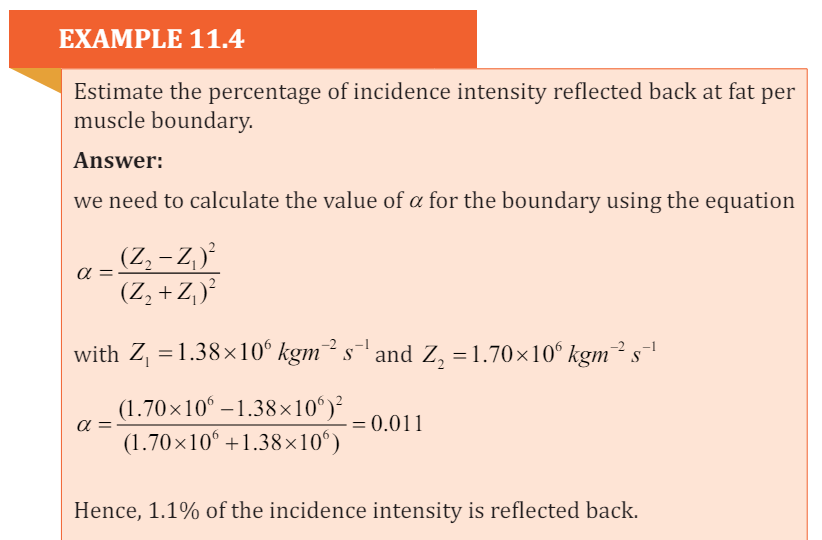
The process of imaging is the same as the echo-locating sonar of a submarine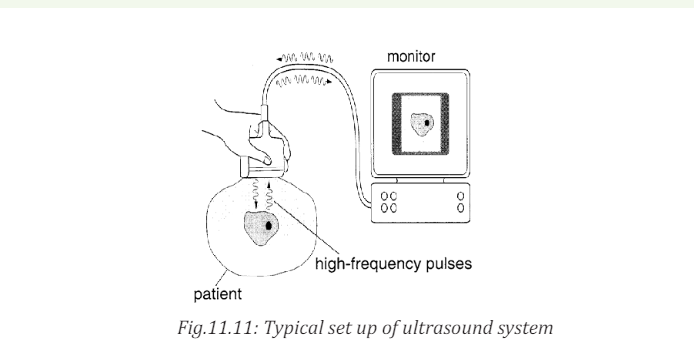
or a bat. The observer sends out a brief pulse of ultrasound and waits for an
echo. The pulse travels out, reflects off the target and returns. The ultrasound
machine uses pulses because the same device acts as both transmitter and
receiver. If it continually sent out sounds, then the receiver would not hear themuch softer echo over the louder transmission.
The duty cycle of the ultrasound imager is the amount of time spent transmittingcompared to the total time of transmitting and listening.
Sonar is an acronym for Sound Navigation and Ranging. It relies on the
reflection of ultrasound pulses. A short pulse of ultrasound is directed towards
the object interest, which then reflects it back as an echo. The total time
between transmission of pulse and reception of an echo is measured, often
using a cathode ray oscilloscope (CRO). The sonar principle is used to estimatethe depth of a structure, using
Where t is the time taken to go and back and v is the velocity of ultrasound in
the medium.
The factor of 2 is necessary because the pulse must travel “there and back”
An ultrasound beam structure is directly into the body. The reflection or
echoes from different body structure are then detected and analyzed, yielding
information about the locations. For example if the time delays between the
reception of echo pulse1 and 2 (Fig.11.12 below) is t , then the diameter of thebaby’s head can be found using the above formula.
During an investigation using ultrasound, the time delay for an echo to return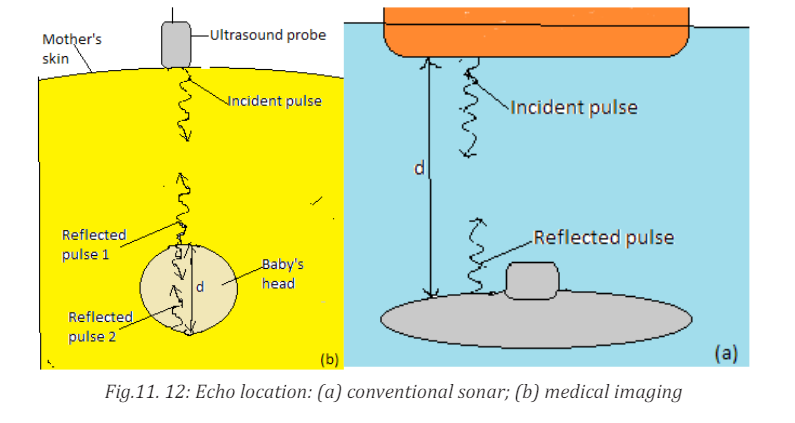
from a structure is 10.5µs If the average velocity of ultrasound in the eye is 1510m/s. Calculate the depth of the structure.
a. Doppler ultrasonic
An object travelling towards the listener causes sound waves to be compressed
giving a higher frequency; an object travelling away from the listener gives a
lower frequency. The Doppler effect has been applied to ultrasound imaging.
Flowing blood causes an alteration to the frequency of sound waves returning
to the ultra sound probe. This frequency change or shift is calculated allowing
quantization of blood flow. The combination of conventional two-dimensionalultra sound imaging with Doppler ultra sound is known as Duplex ultra sound.
The Doppler sample gate is positioned in the artery (arrow) and the frequency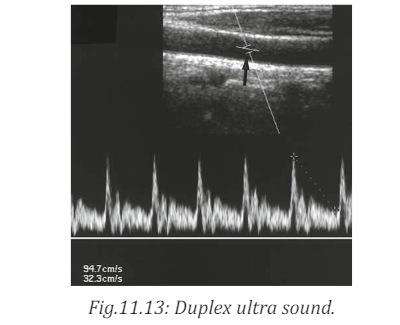
shifts displayed as a graph. Peak systolic and end diastolic velocities arecalculated and also displayed on the image in centimeters per second.
As ultrasound imaging uses sound waves to produce pictures of inside of the
body. It is used to help diagnose the cause of pain, swelling and infection in
the body’s internal organs and to examine a baby in pregnant woman and the
brain and hips in infants. It is also used to help guide biopsies, diagnose heartconditions and assess damage after a heart attack.
Ultrasound examinations do not use ionizing radiation (x-rays), there is no
radiation exposure to the patient. Because ultrasound image are captured in
real time, they can show the structure and movement of the body’s internalorgans, as well as blood flowing through blood vessels.
b. Advantages and Disadvantages of ultrasounds
The advantages of ultrasound over other imaging modalities include:• Lack of ionizing radiation.Some disadvantages of ultrasound include:
• Relatively low cost
• It is noninvasive (of medicine procedures not involving the introduction
of instruments into the body)
• Quick procedure
• Good for examining soft tissues.• Portability of equipment.
• It is highly operator dependent as it relies on the operator to produce11.2.4 Checking my progress
and interpret images at the time of examination
• Not as much details as X-rays and MRI
• It cannot be used in areas that contain gas (such as lungs)
• Doesn’t pass through bones.• Can be wrong in detecting physical abnormalities.
1. Explain how ultrasound imaging is used?11.3 SCINTIGRAPHY (NUCLEAR MEDICINE)
2. Who take the decision to scan or not to scan in normal pregnancy?
3. What are the risks and side effects to the mother or baby during
ultrasound?
4. If an ultrasound is done at 6 to 7 weeks and a heartbeat is not detected,does
ACTIVITY 11.4a. What do you understand by ‘radionuclide imaging’?11.3.1 Physics of scintigraphy and terminology
b. What is a radionuclide scan used for?c. Compare radionuclide scan with mammography scan?
Scintigraphy refers to the use of gamma radiation to form images following the
injection of various radiopharmaceuticals. The key word to understanding of
scintigraphy is radiopharmaceutical. ‘Radio’ refers to the radionuclide, i.e. theemitter of gamma rays.
The most commonly used radionuclide in clinical practice is technetium,
written in this text as mTc 9 , where 99 is the atomic mass, and the ‘m’ stands for
metastable. Metastable means that the technetium atom has two basic energy
states: high and low energy states. As the technetium transforms from the highenergy state to the low-energy state, it emits a quantum of energy in the form of
a gamma ray, which has energy of 140 keV. Other commonly used radionuclidesinclude gallium citrate (67Ga), thallium (201TI), indium (111In) and iodine ( 131 I).
11.3.2 Basic functioning of radionuclide scan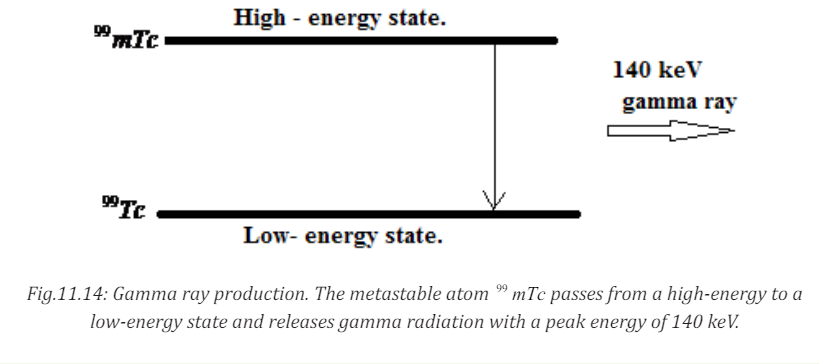
ACTIVITY 11.5
For radionuclide imaging, it is advisable for the patient to consume a
small quantity of radionuclide, or it is injected into a vein in your arm.a. How long does it take?A radionuclide scan is a way of imaging bones, organs and other parts of the
b. What is the purpose of those radionuclide chemicals?
c. Assuming the patient has already consumed the radionuclide for
him/her to be scanned and wants to take another scan on another
part of the body, will the patient be required to take another dose
of the nuclide?
d. You as a student, what advice can you give to a patient whodevelops allergies after taking the radio nuclear chemical?
body by using a small dose of a radioactive chemical. There are different types
of radionuclide chemical. The one used depends on which organ or part of thebody need to be scanned.
A radionuclide (sometimes called a radioisotope or isotope) is a chemical which
emits a type of radioactivity called gamma rays. A tiny amount of radionuclide
is put into the body, usually by an injection into a vein. Sometimes it is breathedin, or swallowed, or given as eye drops, depending on the test.
Gamma rays are similar to X-rays and are detected by a device called a gamma
camera. The gamma rays which are emitted from inside the body are detected
by the gamma camera, are converted into an electrical signal and sent to a
computer. The computer builds a picture by converting the differing intensitiesof radioactivity emitted into different colors or shades of grey.
However, radionuclide imaging techniques do not depict structural anatomy like
ultrasound, X-ray computed tomography (XCT) or conventional radiographs.
It is the only established noninvasive technique available to investigate organ
physiology, although recently Nuclear magnetic resonance (NMR) imaging
technique has shown its capability to probe organ physiology and anatomywithout ionizing radiation.
Radionuclide scans do not generally cause any after effects. Through the natural
process of radioactive decay, the small amount of radioactive chemical in your
body will lose its radioactivity over time. Although the levels of radiation usedin the scan are small, patients may be advised to observe special precautions.
11.3.3 Limitations and disadvantages of scintigraphy
The main advantages of scintigraphy are its high sensitivity and the fact that the
functional information is provided as well as anatomical information. However
it has some disadvantages that are listed below:i. Generally poor resolution compared with other imaging techniques.11.3.4 Checking my progress
ii. Radiation risks due to the administered radionuclide
iii. Can be invasive, sometimes requiring an injection into the bloodstream
iv. Disposal for radioactive waste, including that from patients, requires
special procedures.
v. Relatively high costs associated with radiotracer production andadministration.
Choose the correct answers
1. Scintigraphy refers to the use of:a. Gamma radiation to form images2. The radionuclide in clinical practice are
b. X- ray radiation to form images
c. X- rays and gamma radiations to form images
d. None of radiation to form images.a. Technetium11.4 MAGNETIC RESONANCE IMAGING (MRI)
b. Thallium
c. Galliumd. ALL of them
ACTIVITY 11.6:Principles of MRI1. What does MRI mean?11.4.1. MRI physics and terminology.
2. What is it used for?
3. What makes MRI to be powerful compared to other imaging
techniques?
4. is it advisable for a pregnant woman to be placed in MRI Scanner?Explain your view?
Magnetic resonance (MR) imaging has become the dominant clinical imaging
modality with widespread, primarily noninvasive, applicability throughout the
body and across many disease processes. The progress of MR imaging has been
rapid compared with other imaging technologies and it can be attributed in part
to physics and in part to the timing of the development of MR imaging, whichcorresponded to an important period of advances in computing technology.
Initially let us described how magnetic resonance can be demonstrated with
a pair of magnets and a compass. If a compass happens to find itself near a
powerful magnet, the compass needle will align with the field. In a normal
pocket compass, the needle is embedded in liquid to dampen its oscillations.
Without liquid, the needle will vibrate through the north direction for a period
before coming to rest. The frequency of the oscillations depends on the magneticfield and of the strength of the magnetic needle.
Let us focus on what made the needle oscillate. It was the small movements of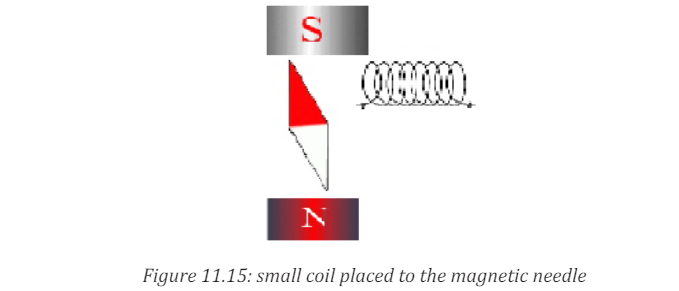
the magnet, back and forth, or more precisely the oscillation of a weak magnetic
field perpendicular to the powerful stationary magnetic field caused by the
movement of the magnet. But oscillating magnetic field is what we understand
by “radio waves”, which means that in reality, we could replace the weak magnet
with other types of radio wave emitters.
This could, for example, be a small coil subject to an alternating current, as shown
in figure above. Such a coil will create a magnetic field perpendicular to the
magnetic needle. The field changes direction in synchrony with the oscillation
of the alternating current, so if the frequency of the current is adjusted to the
resonance frequency of the magnetic needle, the current will set the needle
in motion. This is also applied in an MR scanner. In summary, the needle can
be set in motion from a distance by either waving a magnet or by applying an
alternating current to a coil. In both situations, magnetic resonance is achieved
when the magnetic field that motion or alternating currents produce, oscillates
at the resonance frequency. When the waving or the alternating current is
stopped, the radio waves that are subsequently produced by the oscillatingneedle will induce a voltage over the coil.
MRI uses the magnetic properties of spinning hydrogen atoms to produce
images. The first step in MRI is the application of a strong, external magnetic
field. For this purpose, the patient is placed within a large powerful magnet.
Most current medical MRI machines have field strengths of 1.5 or 3.0 Tesla.
The hydrogen atoms within the patient align in a direction either parallel orantiparallel to the strong external field.
A greater proportion aligns in the parallel direction so that the net vector of
their alignment, and therefore the net magnetic vector, will be in the direction
of the external field. This is known as longitudinal magnetization. A second
magnetic field is applied at right angles to the original external field. This second
magnetic field is known as the radiofrequency pulse (RF pulse), because it is
applied at a frequency in the same part of the electromagnetic spectrum asradio waves. A magnetic coil, known as the RF coil, applies the RF pulse.
The RF pulse causes the net magnetization vector of the hydrogen atoms to
turn towards the transverse plane, i.e. a plane at right angles to the direction
of the original, strong external field. The component of the net magnetization
vector in the transverse plane induces an electrical current in the RF coil. This
current is known as the MR signal and is the basis for formation of an image.
Computer analysis of the complex MR signal from the RF receiver coils is used
to produce an MR image.
11.4.2. The magnetism of the body
Let‘s see how magnet needles with and without spin are affected by radio
waves, we now turn to the “compass needles” in our own bodies.a. Most frequently, the MR signal is derived from hydrogen nuclei (meaning
the atomic nuclei in the hydrogen atoms). Most of the body’s hydrogen is
found in the water molecules. Few other nuclei are used for MR.
b. Hydrogen nuclei (also called protons) behave as small compass needles
that align themselves parallel to the field.
c. The compass needles (the spins) are aligned in the field, but due to
movements and nuclear interactions in the soup, the alignment only
happens partially.
d. The nuclei in the body move among each other (thermal motion) and the11.4.3. Magnetic Resonance Imaging (MRI).net magnetization in equilibrium is thus temperature dependent.
e. Due to the number of hydrogen nuclei (about 1027 ) found in the body,
the net magnetization still becomes measurable. It is proportional to the
field: A large field produces a high degree of alignment and thus a largemagnetization and better signal to noise ratio.
In MRI, a particular type of nucleus is selected and its distribution in the body
is monitored. Hydrogen is the most commonly imaged element, not only due to
its abundance in the body but also because it gives the strongest MRI signals.
The technique uses a very powerful magnet to align the nuclei of atoms inside
the body, and a variable magnetic field that causes the atoms to resonate, a
phenomenon called nuclear magnetic resonance. The nuclei produce their own
rotating magnetic fields that a scanner detects and uses to create an image.
MRI is used to diagnose a variety of disorders, such as strokes, tumors,
aneurysms, spinal cord injuries, multiple sclerosis and eye or inner ear
problems. It is also widely used in research to measure brain structure andfunction, among other things.

An MRI scan can be used to examine almost any part of the body, including the:• Brain and spinal cord
• Bones and joints
• Breasts
• Heart and blood vessels
• Internal organs, such as the liver, womb or prostate gland ,etcThe results of an MRI scan can be used to help diagnose conditions, plantreatments and assess how effective previous treatment has been.
11.4.4. Functional of MRI Scan
ACTIVITY 11.7a. Explain the function of MRI Scan.There are many forms of MRI, some of them are:
b. What are the advantages and disadvantages of MRI Scan?c. What are the hazards associated with MRI?
a. Diffusion-weighted imaging.
Diffusion-weighted imaging (DWI) is sensitive to the random Brownian
motion (diffusion) of water molecules within tissue. The greater the amount of
diffusion, the greater the signal loss on DWI. Areas of reduced water molecule
diffusion show on DWI as relatively high signal. Diffusion-weighted imaging
is the most sensitive imaging test available for the diagnosis of acute
cerebral infarction. With the onset of acute ischaemia and cell death there
is increased intracellular water (cytotoxicoedema) with restricted diffusion
of water molecules. An acute infarct therefore shows on DWI as an area ofrelatively high signal.
b. Perfusion-weighted imaging
In perfusion-weighted imaging (PWI) the brain is rapidly scanned following
injection of a bolus of contrast material (gadolinium). The data obtained may
be represented in a number of ways including maps of regional cerebral blood
volume, cerebral blood flow, and mean transit time of the contrast bolus. PWI
may be used in patients with cerebral infarct to map out areas of brain at risk of
ischaemia that may be salvageable with thrombolysis.c. Magnetic resonance spectroscopy
Magnetic resonance spectroscopy (MRS) uses different frequencies to identify
certain molecules in a selected volume of tissue, known as a voxel. Following data
analysis, a spectrographic graph of certain metabolites is drawn. Metabolites
of interest include lipid, lactate, NAA (N-acetylaspartate), choline, creatinine,citrate and myoinositol.
Uses of MRS include characterization of metabolic brain disorders in children,
imaging of dementias, differentiation of recurrent cerebral tumour fromradiation necrosis, and diagnosis of prostatic carcinoma.
d. Blood oxygen level-dependent imaging
Blood oxygen level-dependent (BOLD) imaging is a non-invasive functional MRI
(fMRI) technique used for localizing regional brain signal intensity changes in
response to task performance. BOLD imaging depends on regional changes
in concentration of deoxyhemoglobin, and is therefore a tool to investigate
regional cerebral physiology in response to a variety of stimuli. BOLD fMRI may
be used prior to surgery for brain tumor or arteriovenous malformation (AVM),as a prognostic indicator of the degree of postsurgical deficit.
11.4.5 Advantage and disadvantages of MRI.
Advantages of MRI in clinical practice include:
1. Excellent soft tissue contrast and characterization
2. Lack of ionizing radiation.
3. Noninvasive machine.
4. Lack of artefact from adjacent bones, e.g. pituitary fossa
Disadvantages of MRI:
1. High capital and running costs.
2. Image selected and interpretation is complex.
3. Examination can be difficult for some people who are claustrophobic
4. The examination is noisy and takes long.
5. Hazards with implants, particularly pacemakers.6. Practical problems associated with large superconducting magnets.
11.4.7. Checking my progress
1. What is meant by relaxation in the context of MRI?
2. Give the reasons why the hydrogen nucleus is most used in MRI.
3. What does NMR stand for? Explain carefully the role of the three terms
involved4. Draw the basic steps in the formation of MRI image
11.5 ENDOSCOPY
ACTIVITY 11.81. How can we examine inside the stomach by using light rays?11.3.1 Description2. How is endoscope performed?
Endoscopy is a nonsurgical procedure used to examine a person’s digestive tract.
Using an endoscope, which is a flexible tube with a light and camera attached to
it, the specialist can view pictures of your digestive tract on a monitor.
During an upper endoscopy, an endoscope is easily passed through the mouth
and throat and into the esophagus, allowing the specialist to view the esophagus,
stomach, and upper part of the small intestine. Similarly, endoscopes can be
passed into the large intestine (colon) through the rectum to examine this area
of the intestine.
11.3.2 Upper endoscopy
Upper Endoscopy (also known as gastroscopy, EGD, or
esophagogastroduodenoscopy) is a procedure that enables your surgeon
to examine the lining of the esophagus (swallowing tube), stomach and
duodenum (first portion of the small intestine). A bendable, lighted tube about
the thickness of your little finger is placed through your mouth and into thestomach and duodenum.
11.3.3. How is the upper endoscopy performed?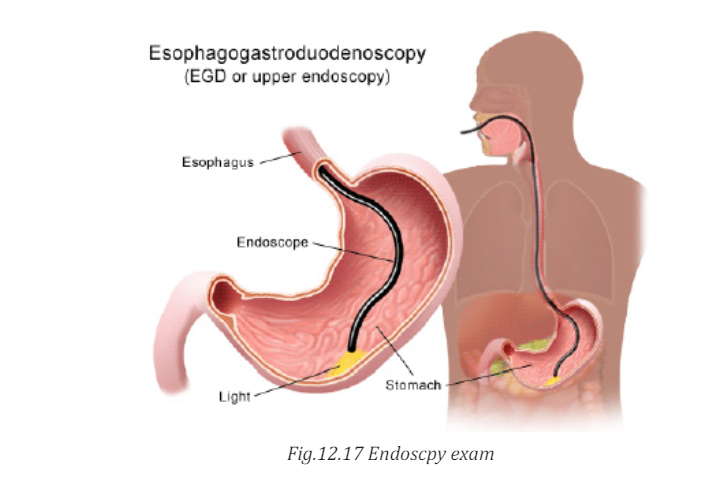
Upper endoscopy is performed to evaluate symptoms of persistent upper
abdominal pain, nausea, vomiting, difficulty swallowing or heartburn. It is an
excellent method for finding the cause of bleeding from the upper gastrointestinaltract. It can be used to evaluate the esophagus or stomach after major surgery.
It is more accurate than X-rays for detecting inflammation, ulcers or tumors
of the esophagus, stomach and duodenum. Upper endoscopy can detect early
cancer and can distinguish between cancerous and noncancerous conditionsby performing biopsies of suspicious areas.
A variety of instruments can be passed through the endoscope that allows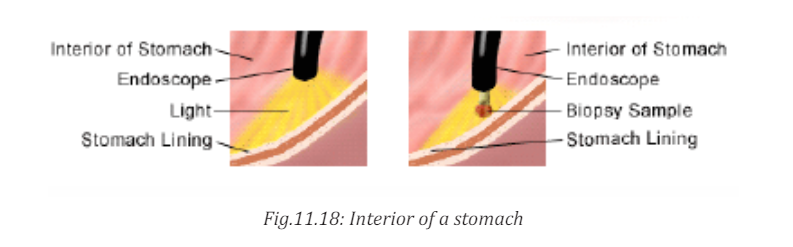
the surgeon to treat many abnormalities with little or no discomfort, remove
swallowed objects, or treat upper gastrointestinal bleeding. Safe and effective
control of bleeding has reduced the need for transfusions and surgery in manypatients.
11.3.4. Advantages and disadvantages of endoscopy
Advantages• Complete visualization of the entire stomach or digestive tract.Disadvantages:
• It is very safe and effective tool in diagnosis
• Does not leave any scar because it uses natural body openings.
• It is cost effective and has low risk
• They are generally painless.
• Can do therapeutic interventions
• Allows for sampling/biopsying of small bowel mucosa• Allows for resection of polyps.
• Although the endoscope is very safe; however, the procedure has a few
potential complications which may include:
• Bleeding
• Perforation (tear in the gut wall)
• Infection
• Reaction to sedation (action of administering a sedative drug to
produce a state of calm or sleep.
• Technically difficult procedure
• Very time consuming (Procedure can take > 3 hours)• Patient may need to be admitted to the hospital
• Higher risk of small bowel perforation11.3.5 Checking my progress
• Case reports of pancreatitis and intestinal necrosis• Reported incidents of aspiration and pneumonia
1. What are instruments used to view the esophagus, stomach and upper11.3.6. hazards associated with medical imaging
small intestine of human body?
2. Explain the function of endoscope.3. Compare and contrast colonoscopy and gastroscopy
The following are some hazards associated with medical imaging:1. Exposure to ionizing radiation1. Exposure to ionizing radiation
2. Anaphylactoid reactions to iodinated contrast media
3. Contrast-induced nephropathy (CIN)
4. MRI safety issues5. Nephrogenic systemic sclerosis (NSF) due to Gd-containing contrast media
Radiation effects and effective dose Radiography, scintigraphy and CT use
ionizing radiation. Numerous studies have shown that ionizing radiation in
large doses is harmful. The risks of harm from medical radiation are low, and
are usually expressed as the increased risk of developing cancer as a result of
exposure. Radiation effects occur as a result of damage to cells, including cell
death and genetic damage. Actively dividing cells, such as are found in the bonemarrow, lymph glands and gonads are particularly sensitive to radiation effects.
2. Anaphylactoid contrast media reactions
Most patients injected intravenously with iodinated contrast media experience
normal transient phenomena, including a mild warm feeling plus an odd taste
in the mouth. With modern iodinated contrast media, vomiting at the time of
injection is uncommon. More significant adverse reactions to contrast mediamay be classified as mild, intermediate or severe anaphylactoid reactions:
• Mild anaphylactoid reactions: mild urticaria and pruritis3. Contrast-induced nephropathy
• Intermediate reactions: more severe urticaria, hypotension and mild
bronchospasm
• Severe reactions: more severe bronchospasm, laryngeal oedema,
pulmonary oedema, unconsciousness, convulsions, pulmonarycollapse and cardiac arrest.
Contrast-induced nephropathy (CIN) refers to a reduction of renal function
(defined as greater than 25 per cent increase in serum creatinine) occurring
within 3 days of contrast medium injection. Risk factors for the developmentof CIN include:
Pre-existing impaired renal function, particularly diabetic nephropathy,
Dehydration, Sepsis, Age>60 years, Recent organ transplant , Multiple myeloma.
The risk of developing CIN may be reduced by the following measures:Risk factors should be identified by risk assessment questionnaire.
Use of other imaging modalities in patients at risk including US or noncontrast-enhanced CT.
• Use of minimum possible dose where contrast medium injection is4. MRI safety issues
required.
• Adequate hydration before and after contrast medium injection.
• Various pretreatments have been described, such as oral acetylcysteine;
however, there is currently no convincing evidence that anything otherthan hydration is beneficial.
Potential hazards associated with MRI predominantly relate to the interaction
of the magnetic fields with metallic materials and electronic devices.
Ferromagnetic materials within the patient could possibly be moved by the
magnetic field causing tissue damage. Common potential problems include
metal fragments in the eye and various medical devices such as intracerebral
aneurysm clips. Patients with a past history of penetrating eye injury are at risk
for having metal fragments in the eye and should be screened prior to entering
the MRI room with radiographs of the orbits. The presence of electrically active
implants, such as cardiac pacemakers, cochlear implants and neurostimulators,
is generally a contraindication to MRI unless the safety of an individual deviceis proven.
5. Nephrogenic systemic sclerosis
Nephrogenic systemic sclerosis (NSF) is a rare complication of some Gd-based
contrast media in patients with renal failure. Onset of symptoms may occur
from one day to three months following injection. Initial symptoms consist
of pain, pruritis and erythema, usually in the legs. As NSF progresses there is
thickening of skin and subcutaneous tissues, and fibrosis of internal organs
including heart, liver and kidneys. Identifying patients at risk, including patients
with known renal disease, diabetes, hypertension and recent organ transplant,
may reduce the risk of developing NSF following injection of Gd- based contrast
media.
Risk reduction in MRI
A standard questionnaire to be completed by the patient prior to MRI should
cover relevant factors such as:• Previous surgical historyEND UNIT ASSESSMENT 11
• Presence of metal foreign bodies including aneurysm clips, etc.
• Presence of cochlear implants and cardiac pacemakers
• Possible occupational exposure to metal fragments and history of
penetrating eye injury
• Previous allergic reaction to Gd-based contrast media• Known renal disease or other risk factors relevant to NSF.
Part I: Copy the following in your notebook and chose the correct answer
1. Which are included in the system components of gamma rays camera for
producing image of the body?a. Collimator2. Which of the following modalities does not use a form of ionizing
b. Scintillation
c. Attenuation
d. All of the above
radiation?a. Radiography.
b. Computed tomography.
c. Sonography.d. Magnetic resonance imaging3. Hazards not associated with modern medical imaging include:a. Anaphylactoid reactions to iodinated contrast media
b. Complication of some Gd-based contrast media in patients with
renal failure.
c. Imaging of the breast improves a physician’s ability to detect small
tumorsd. Radiation effects and effective dose Radiography.4. Medical imaging systems are often evaluated the characteristics which
are directly related to:a. Image noise.5. Risks associated with radionuclide imaging are:
b. Image blurring.
c. Image unsharpness.
d. Visibility of anatomical detail.a. Generally poor resolution compared with other imaging modalities.
b. Rarely receiving an overdose of chemical injected in the vein of the
body.
c. High capital and running costsd. None of them.
Part II: Structured questions
6. Write the missing word or words on the space before each number.
The term ………………….. is often used to refer to X-ray CT.a. Gastroscopy is a procedure that enables your surgeon to examine the
lining of the ………….
b. The most sensitive imaging test available for the diagnosis of acute
cerebral infarction is …………...
c. Array of …………………. to transform the flashes into amplified electrical
pulses inside the body.
d. Transducers used are different depending on ………. of a patient, one
has 5 MHz and other 3.5 MHz.
e. Hydrogen nuclei (also called protons) behave as small …………… that
align themselves parallel to the field.
f. In ………………….. there are appearance three words: nuclear, magnetic
and resonance.g. Examination can be ………………… is one of the disadvantages of MRI.7. Answer by True if it is True and by False if it is Falsea. The use of gamma radiation to form images following the injection of8. Compare endoscopy imaging and radionuclide imaging
various radiopharmaceuticals is known as Scintigraphy.
b. This decision to scan or not to scan a normal pregnancy must be made
only by the photographer. There are universally accepted guidelines at
present.
c. Tissue in the body absorbs and scatters ultrasound in the same ways.
Lower frequencies are more rapidly absorbed (attenuated) than higher
frequencies.
d. Upper endoscopy uses light and camera to view the esophagus, stomach,
and upper part of the small intestine.
e. Ultrasound is both generated and detected through high frequency
oscillations in piezoelectric crystals so there is ionizing radiation
exposure associated with ultrasound imaging.
9. What are the advantages of MRI in clinical practice?
10. Is ultrasound safe? explain.
11. What areas of the body can be imaged by ultrasound?
12. Why is ultrasound used in pregnancy?
13. Explain the advantage of CT scan
14. In mammography exams, is the breast compression necessary? Why
Essay question
Historically, MRI began in the central nervous system, but it is now extended to
all regions of the human body. The excellent resolution and contrast available in
any chosen plane in the body, makes the MRI an invaluable diagnostic tool with
which to study body structure, function and chemistry, as well as disease. Discuss
the application of MRI.
