UNIT 5: Counselling in Reproductive Health related conditions
Key Unit competenceProvide counselling in reproductive health related conditions
Introductory activity 5
Using textbook or other sources of information discuss in group of 5 about the
images A, B and C and answer the following questions.a. What do you know about PMTCT?5.1. PMTCT (Prevention of mother to child transmission)
b. According to you, why do you think is the difference between STIs and HIV
counselling?
c. What do you think is involved in counselling for STIs and HIV?d. Mention the stages of counselling for STIs and HIV.
5.1.1 Introduction to PMTCT (Prevention of mother to childtransmission)
Learning Activity 5.1.1
Using different source of information (internet, books or any other source of
information), answer the following terms:
1. Explain how HIV can be transmitted to babies through the mother.
2. What do you understand by the term Prevention mother to child transmissionof HIV?
Knowledge of HIV status, through HIV testing and counselling, is especially important
during pregnancy, childbirth, and breastfeeding, since women with HIV can transmit
the virus to their babies during these times. These different transmission routes of
HIV from the mother to the baby is termed ‘mother-to-child transmission of HIV’.
In HIV-positive pregnant women, the virus is found abundantly in the birth canal
(cervix and vagina) and in the mother’s blood.
Therefore, if the baby is exposed to vaginal fluid or to the mother’s blood during
labour and delivery, there is an increased chance of mother to child transmission(MTCT) occurring.
If anything breaks the barrier between the placenta and the wall of the uterus, there
will be an increased the risk of MTCT of HIV.
As a nurse, you should encourage all pregnant women to consent to be tested for
HIV. Explain to every pregnant woman that if her HIV test result is positive, she
can receive effective services to prevent her baby from getting HIV before or after
birth. The main PMTCT goals include early identification of pregnant women with
HIV, to reduce new pediatric HIV infections, and providing mothers and babies with
appropriately and timely manner to prevention, care, and treatment services. To
achieve these goals, health providers should provide counselling to women and
their families through the following activities:• To help clients to understand what actions they can take to prevent the
transmission of HIV to their children.
• To assist women and men to minimize the risk of HIV infection during
conception and pregnancy.
• To provide information on the extra risk of transmission to the child if mother
is infected during pregnancy or breast-feeding.
• To help mothers and families to weigh up the benefits and risks of differentinfant feeding options.
Self-assessment 5.1.1
1. What is the PMTCT main goal?2. What are the objectives of PMTCT?
5.1.2. Counselling pregnant women and their partners about PMTCT
Learning Activity 5.1.2
In a group of 5, Using different source of information (internet, books or any
other source of information) search and discuss PMTCT approaches and be
prepared for class presentation.
i) Describe how you can provide counselling to the pregnant woman and her
male partner.
Efforts to prevent mother to child transmission of HIV should be as comprehensive
as possible and acknowledge that both mothers and fathers have an impact on
transmission of HIV to the infant:• Both partners need to be aware of the importance of safer sex throughout
pregnancy and breastfeeding.• Both partners should be tested and counselled for HIV.
• Both partners should be made aware of and provided with PMTCT
interventions.• Both partners should be provided with condoms.
When the male partner is involved and informed, the woman is more likely to be able
to participate in PMTCT interventions. Some things that help prevent transmission
from mother-to-child, such as exclusive replacement feeding or exclusive
breastfeeding, can be difficult for women to adopt, especially if they do not share
their HIV status with family. Not only men will be supportive but also it is very crucial
that the partner’s HIV status in case of discordant couple. The partner’s serologicalstatus helps in provision of health education for HIV prevention or management.
Although the woman’s partner’s involvement is vital, as a nurse, you should
appreciate that when providing counselling to pregnant women, you need to assure
her of confidentiality. This means that only health staff directly involved in her care
will know her test results. Otherwise, let the woman decide herself if and when she
wants to share her test results with anyone else including so they can then talk with
you as a couple about these issues, to help them better understand risks, and findsolutions that are agreeable to both.
Many couples are successful in adopting safer sexual practices. It is often helpfulto offer to counsel the couple together
Self-assessment 5.1.2
i) What the nurse should appreciate when providing counselling to the
pregnant woman?ii) Why it is important to counsel the couple together?
5.1.3. PMTCT pre-test counselling
Learning Activity 5.1.3
i) Mention at least three topics covered during the pre-test counselling of the
PMTCT sessions.
ii) What precautions do you need to take if the woman refuses to take an HIVtest?
Counselling during routine antenatal and postpartum care is an important way to
reach women with information about HIV/AIDS and encourage HIV testing. Women
receive pre-test counseling that covers comprehensive information on HIV/AIDS,
including the difference between HIV and AIDS, the importance of being tested,
modes of transmission, means of prevention, possible results and their implications,availability of care and treatment services.
HIV counselling and testing (HTC) is recommended for pregnant women as a key
component of the package of care in all antenatal services. All pregnant mothers
attending ANC will receive HTC preferably with their partners at the time of their
first visit to ANC.
Strong emphasis will continue being put in male partners’ involvement in PMTCT
cascade, starting by ANC together with couple’s HIV counselling and testing. Some
of the topics covered during the PMTCT counselling include:• basics of HIV transmission and prevention;• HIV testing processes;
benefits and risks of HIV testing;
• right to refuse testing (opt-out);• implications of positive and negative test results;At some time, a woman may refuse testing and counselling. In that case, as
• identification of supportive HIV services and treatment available;
• identification of PMTCT services and treatment available;
• identification of sexual risks and plan for reduction of risks;• Importance of infant feeding and nutrition.
a counsellor, you need to spend a bit of extra time with her to find out why she
refused. Use open questioning and active listening skills, and see if you can help
her with any problems related to accepting the HIV test. But remember to present
the information in a neutral, non-biased way without judgement. As a counsellor,
you should appreciate that some women may be afraid to get an HIV test, do not
want to know their HIV status, or do not want to discuss results with their partner.
Counselling women about the benefits and risks of knowing their HIV status, not
only for themselves but for their infant and partner, can help to overcome the fearof stigma, discrimination and other barriers.
Self-assessment 5.1.3
i) Why is it important to provide counselling during routine antenatal care?
ii) What are some of the reasons that may lead some women to not test
themselves of HIV?
iii) How can you address those issues during your pre-test counsellingsession?
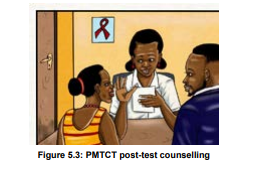
5.1.4. PMTCT Post-Test counselling
Learning Activity 5.1.4
i) What are the goals of posttest PMTCT counselling?ii) What topics are covered during the post-test PMTCT counselling?
Post-test counseling should be provided by the same person who gave the pretest
counseling. Post-test counselling for a pregnant woman who has tested
HIV-negative should focus on helping the woman decide how she can stay HIV negative.
If the woman is not with her partner, support should also be provided to
help her decide if she will discuss her results with her partner. Post-test counseling
will insist on the risk reduction and HIV prevention strategies and the counselorshould explain to the client about the seroconversion period and its implications.
Negative clients who are not at high risk of HIV infection should be advised to keep
protecting themselves against HIV seroconversion and plan to retest only after any
other risky contact. Negative clients who are at high risk should be advised to
get tested every six months.
The main ways to prevent HIV infection and STIs:
• Correct and consistent use of condoms during every sexual act;
• Practising safer sex (choosing sexual activities that do not allow semen, fluid
from the vagina, or blood to enter the mouth, anus or vagina of the partner, or
to touch the skin of the partner where there is an open cut or sore.)
• Reducing the number of partners
• Sexual fidelity• Abstinence.
In case of Positive results, posttest counselling will insist on linkage to care and
treatment. Post-test counselling for pregnant women who are diagnosed with an
HIV infection should include the following, in addition to the standard messages
described above for all people diagnosed with HIV infection:• childbirth plans: providers should encourage HIV-positive pregnant womeni) What should be done in case of HIV negative results?
to deliver in a health facility for their own well-being as well as to ensure
access to PMTCT services;
• use of ARVs for the client’s health, when indicated and available, as well
as the use of ARVs to prevent transmission to the infant;
• the importance of partner testing and information on the availability of
couples testing services;
• ensuring screening for TB and testing for other infections such as syphilis;
• counselling on adequate maternal nutrition, including iron and folic acid;
• advice on infant feeding options and support to carry out the mother’s infant
feeding choice;
• HIV testing for the infant and needed follow-up for HIV-exposed infantsSelf-assessment 5.1.4
ii) What other messages would you focus on when counselling a woman witha positive HIV test?
5.2. Counselling for Sexually Transmitted Infections
5.2.1. Counselling a client before taking a STI test
Learning Activity 5.2.1
i) Why is it important to provide counselling to a client before taking the STI
test?ii) Explain with examples counselling targeting the prevention of STIs.
Globally, more than 1 million sexually transmitted infections (STIs) are acquired
every day worldwide, the majority of which are asymptomatic. Every year, an
estimated 374 million new infections with 1 of 4 STIs: chlamydia, gonorrhoea,
syphilis and Trichomoniasis occur. Research shows that about one million pregnant
women get infected with syphilis which in turn results in over 350, 000 adverse birth
outcomes including 200,000 stillbirths and newborn deaths. When left untreated,
STIs have direct impact on sexual and reproductive health through stigmatization,infertility, cancers and pregnancy complications and can increase the risk of HIV.
Counselling a client before taking a test of STIs is important for both the primary
and secondary prevention of STIs. Counselling to prevent STIs includes any
intervention that aims to reduce an individual’s likelihood of acquiring an STI. The
primary prevention is very significant because it reduces the risk of acquiring an STI
and it aims to promote the following behaviours:– Reduction of the number of partners;For the secondary prevention, counselling aims at reducing the complications of
– Advise an individual to adapt low risk sexual practices;
– Consistent and correct use of condoms when in engaged in sexual
intercourses.
STIs. It seeks to promote treatment seeking behaviours among people who suspect
they have been infected and further promote safe sex behaviours outlined in Figure
below.
Table 5.1 Sexual activities with their risk of STIs/ HIV infection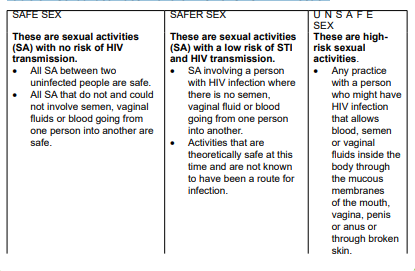
Self-assessment 5.2.1
i) With examples, explain the term ‘unsafe sex practices.
ii) Why is primary prevention needed when offering counselling about STIs?
iii) Learn to provide counselling for STIs testing. Using a role play, create a
sketch of five minutes in which you counsel a client coming to seek STIstesting services.
5.2.2. Helping clients to assess their risk of STI and HIV infection
Learning Activity 5.2.2
When helping a client to assess his/her risk of STI and HIV infection:
i) How do you start the counselling?ii) What are the sexual activities a client may not talk about easily?
Once the client accepts to proceed with counselling, as a nurse, you may find it
easier to begin to talk about the risk of STI. To proceed, a counsellor shares with the
client knowledge about how STI/HIV is transmitted and then explores the possibility
of transmission in clients’ lives. This is done through helping the client reflect on
their past and present sexual practices and drug-using behaviour and further reflect
on whether this may have put them at risk of STI. Moreover, the counsellor needs to
also guide the client to recall on their medical history and whether there might havebeen any risk of contracting HIV from blood transfusions.
While assessing the risk of HIV transmission, help clients to talk about all their sexual
activities and partners. Do not make any assumptions about clients’ sexual activity
nor the activity of their sexual partners. The client may have or have had partners
of the same sex or the opposite sex now or in the past. A married person may have
relationships outside marriage or their partner may have such relationships. An
adolescent may be abused at home.
As you explore this, provide information on the level of risk of different sexual
activities. Probe about other possible activities that the client may not have thought
significant or may not like to mention. Discuss each of their concerns in detail,
learning about their understanding of HIV and adding information as needed. When
you have covered all their concerns, ask about any risk factors that they have not
mentioned. When you have talked over all the issues, summarise the main pointsand ask how the client feels about their likely risk.
If clients come to you expressing concerns about STI, affirm their sense of
responsibility and decision to take action, and assure them of confidentiality. Each
client will have their particular needs, so as a counsellor, you should acknowledge
and appreciate individuals’ differences when providing counselling. For this reason,
it is essential to give all clients an opportunity to discuss and get help on any aspect
of their sexual lives. To achieve this, the counsellor asks a question like “Would you
like to discuss anything concerning STIs? If you are busy today, we could arrangeanother time”.
If clients do not wish to talk about STI or HIV, only do what you can to ensure that
they are aware of the potential risk of STI and what they can do to reduce thoserisks.
Self-assessment 5.2.2
i) Using role play, create a scenario on how you can encourage a client todiscuss their concerns about STIs fears
5.2.3. Counselling a client with an STI diagnosis
Learning Activity 5.2.3
Mr Gakuru was aged 30 years and married. He was worried about STIs because
of symptoms he had. He informed his counsellor during the risk assessment for
STIs that he had unprotected sex with other three different women. He was
diagnosed to have signs of STIs but the HIV test was negative.i) Why do you think it is important to assure privacy and confidentiality when
taking client STIs history?
ii) Which precautions to be taken when providing post STI is diagnosis?iii) Why informing the partners the STI diagnosis is necessary?
When providing counselling for a person already diagnosed of STIs, complete
privacy is necessary. To facilitate open communication between the counsellor and
the client, the following steps need to be) followed:– Affirm your client and assure her or him of confidentiality.their genitals passed through sexual intercourse. Explain and answer the
– Encourage your client to tell you about any signs and symptoms, recent
sexual interactions, fears and what they have already done to try to solve the
problem.– Explain that the examination or test showed that they have an infection in
client’s questions about it.– Explain that STIs can have serious consequences if they are not treated asWhen announcing the results of the screening STI test, as a counsellor you need
quickly as possible.
– Explain the potential consequences of your client’s particular STIs if they are
not treated.
– Explain that most STIs are curable if they are treated early with a complete
course of the correct drugs.
– Explain about the prognosis for your clients STI. Stress the importance oftaking the full course of correct drugs.
to acknowledge the following:
– Explain to the clients why they need to tell all their sexual partners about the
infection so that they get treatment because partners can re-infect each other
every time they have sex if they are not both treated.
– Acknowledge that for some people, it is difficult to disclose their STI infection.
You need to foster trust while providing counselling so that individuals
understand the importance of disclosing their STIs infection to their partners.
– If clients are anxious about telling their partners or are not able to do so,
explore alternatives with them. Take great care not to push them into a
potentially dangerous situation.
Ask:
– “Is there a relative, friend or community member who could help you to do this
and mediate in any quarrels?”
– “Would it be helpful to counsel your partner alone or together with you?”
– Both partners should abstain from sex until they are completely cured. If they
are unable to do this, they should use condoms each time they have sex.
– Explain that STIs increase the risk of HIV. Stress the importance of preventionof STI and ask if clients wish to consider taking an HIV test.
If the clients are in a relationship, you will need to counsel them on how they
need to restore and maintain harmony in their relationship. This is because STIs
frequently result in conflicts because they imply that one or both parties have had a
relationship outside. While offering STI counselling, you will need to ask the client
how she or he is feeling. Give her or him time to express their feelings about the
situation. Some ways to express that include asking questions like:
“I see that you are feeling very angry that your partner has given you this infection,is that right?
Would you like to tell me more about what you are feeling”?
– If you are counselling a couple, give them a chance to say how they feel to
each other while the other person really listens.
– Give positive examples of couples who have been in this situation and comethrough it and are still together.
Self-assessment 5.2.3
i) Why the follow-up plan is necessary when counselling a STI client?
ii) Mention the key steps you can follow when offering counselling post STIs
screening.
iii) Mrs X is a married woman. She has come for STIs test and the results of
the screening shows that she has gonorrhoea. She is afraid of disclosing
her result to her male partner because she fears she will be stigmatized.
Create a scenario on how you will counsel her to disclose her result.
5.3 HIV counselling5.3.1 Introduction to HIV counselling
Learning Activity 5.3.1
Read chapter two about counselling skills and processes found in the book
‘Programme guidance on Counselling for STI/HIV prevention in sexual and
reproductive health settings’ and answer the following questions:i) According to what you have read, explain the term ‘HIV counselling’?HIV counselling is a confidential dialogue between a client and a counsellor aimedii) What are the components of HIV Counselling?
at enabling the client to cope with stress and take personal decisions related to
HIV/AIDS. The counselling process includes evaluating the personal risk of HIV
transmission, and discussing how to prevent infection. It focuses specifically on
emotional and social issues related to possible or actual infection with HIV and to
AIDS. With the consent of the client, counselling can be extended to spouses, sex
partners and relatives. As a counsellor, you need to appreciate that counselling
should only take place with the patient’s explicit consent.
HIV and AIDS counselling has two general aims: (1) the prevention of HIV
transmission and (2) the support of those affected directly and indirectly by HIV.
The topics below can be discussed during the counselling sessions:
Adjustments to sexual behaviour and other lifestyle issues;
– Misconceptions about HIV transmission;
– Safer sex practices;
– The partner’s and the patient’s psycholoogical responses to the diagnoses or
result, such as anxiety or depression;
When patients know that they have got HIV infection, they may suffer great
psychosocial and psychological stresses through a fear of rejection, social stigma,
disease progression, and the uncertainties associated with future management of
HIV. Therefore, providing counselling plays a role in addressing these concernsand helps an individual to adapt safe sexual practices.
Self-assessment 5.3.1
i) What are the aims of HIV counselling?
ii) What are the difficulties that people diagnosed of HIV may suffer?iii) How can counselling about HIV mitigates these difficulties?
5.3.2. Pre-test HIV counselling
Learning Activity 5.3.2
Watch the video titled ‘HIV Testing and counselling’ found on this link ‘https://’ and answer the following questions.
i) What to do you understand by the term pre-test counselling?
ii) Why is it important to provide pre-test counselling before screening a clientof HIV?
Pre-test counselling refers to a private session with a counsellor, who explains
the testing procedure and how the results will be given to an individual client.
During this session, the counsellor gives an individual (or a couple or group) the
opportunity to explore and analyse their situation before they an informed decision
of being tested for HIV. Pre-test counselling helps to prepare the client for the HIV
test, explains the implications of knowing that one is or is not infected with HIV, and
facilitates discussion about ways to cope with knowing one’s HIV status. It also
involves a discussion of sexuality, relationships, possible sex- and drug-related risk
behaviours, and how to prevent infection. It helps correct myths and misinformationaround the subject of AIDS.
Clients may present for testing for any number of reasons, ranging from a
generalized anxiety about health to the presence of HIV related physical symptoms.
For people at minimal risk of HIV infection, pre-test discussion provides a valuable
opportunity for health education and for safer sex messages to be made relevant to
the individual. For clients who are at risk of HIV infection, pre-test discussion is anessential part of post-test management.
Self-assessment 5.3.2
i) How does pre-test counselling contribute to HIV testing?ii) Why pre-test counselling is important for people with minimal risk of HIV?
5.3.3. Post-test counselling of HIVLearning Activity 5.3.3
Open this link ‘’
Watch the video titled ‘HIV Post-test Counselling for Medical Students’ and
answer the following questions:i) Based on the video you have watched, what is involved in providing thePost-test counselling supports people in understanding their test result and its
HIV counselling.
ii) With examples, explain how you can provide counselling to a person witha negative HIV result.
implications, whether the result is positive or negative. Counselling also helps
clients explore whom they might share the test result with, and how to approach
sharing their test result.
During the post-test counselling, the counsellor prepares the client for the result,
gives the result and then provides the client with any further information required,
if necessary, referring the person to other services. The counsellor and the client
usually discuss ways to reduce the risk of infection or transmission. HIV test results
should always be given with counselling. The form of post-test counselling will
depend on what the test result is. The same person who gave the pre-test counselling
should provide post-test counselling and this process must respect confidentiality.
Post-test counselling will encourage on risk reduction and secondary prevention ofHIV infection depending on their test result.
For people who test HIV-negative, a counsellor provides them with health information
about their HIV status report, how to prevent acquisition of HIV in the future, and
where and how to link to HIV prevention services. People with significant ongoing
risk may need more active support and linkage to HIV prevention services. In
addition, counselling should also consider the following:• provision of male or female condoms, lubricant and guidance on their use;When the HIV test is positive, the counsellor needs to tell the client clearly, and as
• emphasis on the importance of knowing the status of sexual partner(s),
• information about the availability of partner and couples testing services;
• referral and linkage to relevant HIV prevention services, including voluntary
male medical circumcision (VMMC), Post exposure prophylaxis for people at
substantial ongoing HIV risk;
• For high-risk clients who test HIV-negative such as commercial sex workers,
men who have sex with men, or HIV-negative partners in discordant couples,
encourage HIV risk reduction behaviors and the importance of retesting every12 months.
gently and humanly as possible, providing emotional support and discussing with
the client on how to cope with the result and life thereafter. Ongoing counselling need
to be scheduled to help clients accept their HIV status, and take a positive attitude
to their lives. In those ongoing counselling sessions, the counsellor needs to help
clients understand that good medical care and nutrition are important to prolong
their life. Clients should be helped to understand that there are anti-retroviral drugs
(ARVs) which slow down the development of AIDS. In addition to ARVs, there are
vitamin supplements that clients can obtain from health services.
Indeed, the shock of learning of an HIV-positive diagnosis may make it difficult for
a person to take in further information immediately. Therefore, counselling just after
announcing the result should consider the following:• Explain the test results and diagnosis.
• Give the client time to consider the results and help the client cope with
emotions arising from the diagnosis of HIV infection.
• Discuss immediate concerns and help the client decide who in her or his
social network may be available to provide immediate support.
• Provide clear information on ART and its benefits for maintaining health and
reducing the risk of HIV transmission, as well as where and how to obtain
ART.
• Make an active referral for a specific time and date.
• Discuss barriers to linkage to care, same-day enrolment and ART eligibilityassessment.
• Arrange for follow-up of clients who are unable to enrol in HIV care on the daySelf-assessment 5.3.3
of diagnosis.
• Provide information on how to prevent transmission of HIV, including
information of the reduced transmission risk when virally suppressed on ART;
provide male or female condoms and lubricants and guidance on their use.
• Discuss possible disclosure of the result and the risks and benefits of
disclosure, particularly among couples and partners.
• Encourage and offer HIV testing for sexual partners, children and other
family members of the client if any. This can be done individually, through
couples testing, index testing or partner notification.
• Assess the risk of intimate partner violence and discuss possible steps to
ensure the physical safety of clients, particularly women, who are diagnosed
HIV-positive.
• Assess the risk of suicide, depression and other mental health consequences
of a diagnosis of HIV infection.
• Provide additional referrals for prevention, counselling, support and other
services as appropriate (for example, TB diagnosis and treatment, prophylaxis
for opportunistic infections, STI screening and treatment, contraception, ANC,and access to sterile needles and syringes, and brief sexuality counselling).
i) Mention at least two risks associated with a positive HIV test result.
ii) How can you support a high-risk client who get a negative HIV test result?
iii) Client X has been tested of HIV and his result turns to be positive. Elaborate
in a sketch of no more than six minutes how you can provide counselling tothis client while announcing the result to him.
5.4. End of unit assessmentEnd of unit assessment
Madam K came have been married to Sir K for the past 7 years. They have
3 children together and they are planning to have a last born. It was a sunny
Thursday, when Madam K planned to go to the market and pass by the children
school to pay their school fees.
On her way home, she did not feel alright and she decided to pass by the nearest
health center to consult.
After assessment, the nurse at the HC the nurse informed her that she is pregnant
and she should start ANC, and requested her to come back in morning to give
other laboratory tests with her husband. Madam K left the HC happy, ready to
announce to her family her pregnancy.
To reach home, she met a woman coming out of her room where her husband
was. She got confused and started crying.
In the next morning she convinced her husband to go with her at the HC, where
they were received by the nurse who gave them the appointment. Madam K
started by explaining to the nurse her worries that her husband may be cheating
on her while she is pregnant and requested for her help.1. What type of counselling should the nurse take this couple through and
why?
2. What are the main ways to prevent HIV infections and STIs that the nurse
provides during the couple counselling?
3. Why do nurses need to create awareness among partners on PMTCT?
4. Why is it important to involve partners during PMTCT Counselling?
