Topic outline
UNIT 1: POSTNATAL CARE
Key Unit competence:Monitor a mother during postnatal period
1.1 General assessment of the mother and its importance in theimmediate postnatal period.
Introductory activity 1
a) Observe these images and describe what you see.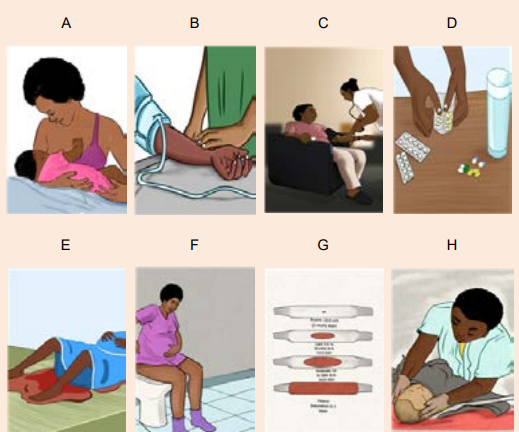
b) What are the needed materials to monitor a mother in postnatal period?
c) What is the importance of voiding in the immediate postnatal period?d) How can you explain blood loss in the immediate postnatal period?
Learning Activity 1.1
Observe these images illustrating a health care provider who is assessing themother in the postnatal period.
From the observation of above pictures,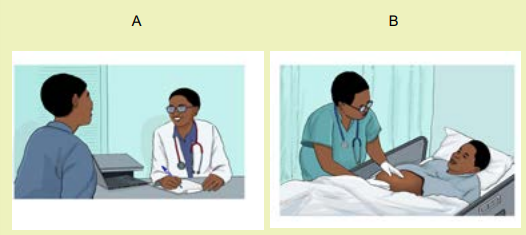
After child birth, the mother needs close monitoring where the health care
provider has to perform her assessment.
e) What do you think that could be the meaning of these images during the
assessment to this mother?
f) What do you think that could be an advantage of the assessment to thismother?
Obstetrics is the field of study concentrated on pregnancy, childbirth and the
postpartum period.
Postnatal period is the period beginning immediately after birth of a child and
extends for about six weeks of life. According to the World Health Organization,
(WHO) immediate postnatal period covers the first 24 hours from delivery of
the placenta while early postnatal period refers to the period from day 2 to 7 th
day and late postnatal period ranges from day 8 to 42nd day after birth. Therefore,
immediate postnatal care is the care given to the mother and the new born baby
immediately after the delivery of placenta until 24hours. The care includes the
prevention, early detection and treatment of complications, and the provision ofcounselling on breastfeeding, birth spacing, immunization and maternal nutrition.
Postnatal period is the time after birth, a time in which the mother’s body, including
hormone levels and uterus size return to a non-pregnant state.
During the assessment, the health care provider obtains the information from
the mother and this is called subjective data while the information obtained after
performing the physical examination is also called objective data.
Immediate postnatal assessment always starts from general assessment. The
assessment must be done in a way that the associate nurse starts from head totoes.
a) Importance of general assessment in immediate postnatal period
The importance of general assessment in the immediate postnatal period:
• To have the general picture of the mother’s well being
• To find out the level of consciousness
• To find out if the woman’s condition gives rise to concern• To find out the woman’s and baby’s urgent need of care
b) Safety considerations of general assessment in immediate postnatal
period
The safety considerations while performing general assessment in immediate
postnatal period are various but the following are considered to be essential:• Perform hand hygieneSelf-assessment 1.1
• Check room for contact precautions
• Introduce yourself to patient.
• Confirm patient ID using
• Explain process to patient.
• Be organized and systematic in your assessment.
• Use appropriate listening and questioning skills.
• Listen and attend to patient cues.
• Ensure patient’s privacy and dignity.
• Assess ABCCS (airway, breathing, circulation, consciousness, safety)
• Apply principles of asepsis and safety.
• Check vital signs• Complete necessary focused assessments
1. What is the importance of general assessment in immediate postnatal
period?
2. Enumerate 5 safety considerations before conducting general assessmentof the other in immediate postnatal period.
1.2 Techniques and elements of general assessment of the motherin immediate postnatal period.
Learning Activity 1.2
Observe these images showing the techniques that a health care can use duringthe assessment of the mother in postnatal period.
The health care provider may use different methods in order to obtain information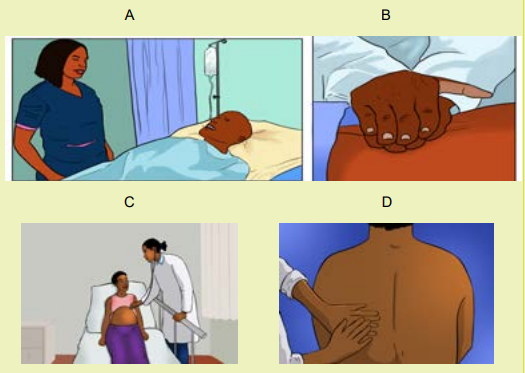
from the mother.
1. Which image that is showing an associate nurse receiving information by
looking the mother?
2. Which image that is demonstrating an associate nurse obtaining information
of the mother with the help of stethoscope and what does stethoscope helpduring the assessment?
There different techniques used in assessing the general status of the other in
immediate postnatal period including inspection, palpation and auscultation
Inspection:
In immediate postnatal period, observations should be performed as often asindicated by the woman’s clinical condition.
During the inspection, observe the mother’s: overall sense of wellbeing and
mobility. It is necessary to observe the general appearance, skin colour, level of
consciousness or mental status, and vaginal bleeding. Observe dyspnea-laboredbreathing, shortness of breath, and chest pain
On the breast, inspect for the redness and engorgement. On the abdomen;
inspect for the presence of visible scars, whether the abdomen is distended and itsmovement during the respiration.
Palpation
During the assessment of the mother, the associate nurse can use palpation for
assessing different parts like:• Skin (moist and cold skin indicate the mother is falling into the shock statusAuscultation
which can be related to postpartum haemorrhage)
• The conjunctiva (pale/whitish conjunctiva indicate anaemia and that might be
having postpartum haemorrhage)
• Pulse rate (fast and rising pulse indicate potential shock to the mother)
• Breast nipple for ensuring the presence of colostrum breast
• Bladder fullness
• Lower limbs for pitting oedema, warmth and signs of inflammation for negativeHoman’s sign.
Auscultation of bowel sounds with stethoscope for the mother in postpartumdelivered by caesarean section.
Self-assessment 1.2
1. What are the elements that can be assessed during inspection of the
mother in the postnatal period?
2. On lower limbs, what will you inspect and palpate for the mother?
3. Regarding Homan’s sign, what is the meaning of Homan’s sign in postnatal
care
4. What are the elements of auscultation to the mother in the immediatepostnatal period?
1.3. Nursing interventions during general assessment of themother in postnatal period.
Learning Activity 1.3
First 24 hours after birth: All postpartum women should have regular assessment
of vaginal bleeding, uterine contraction, fundal height, temperature and heart
rate (pulse) routinely during the first 24 hours starting from the first hour after
birth. Blood pressure should be measured shortly after birth.
a) What do you think about general assessment to the mother in immediate
postnatal period?
b) What do you think about advantages of regular assessment in immediatepostnatal period?
In the postnatal period, all these dynamic body systems (uterus, heart, lungs, blood
volume and blood contents, reproductive system, breasts, immune system and
hormones) have to adjust from the pregnant state back to the pre-pregnant state,
and there is potential risks of complications as these adjustments occur. Common
examples are postpartum haemorrhage, deep vein thrombosis (blood clots in the
veins of the legs), infections and others. Additionally, women in the postnatal periodare often coping with stressful conditions (example is after pain, new born care).
To avoid and overcome complications related to physiological adjustments after
delivery, all mothers and their babies must receive active and ongoing assessment
and care in the immediate postnatal period. This is called ‘immediate postnatalcare’
In immediate postnatal care period the associate nurse must do the following
essential care:
• Assess the mother’s general status, vital signs, bladder fullness, uterine
retraction(involution), and vaginal bleeding
• Rehydration and nutrition support to the mother
• Provide hygiene (genital and perineal care, bed bath, bed making) to the
mother,
• Assess the psychological status of the mother focuses on three aspects:
mother’s reaction to the birth experience, the mother’s adaptation to the
infant and the family’s reaction to the infant. Then, provide education and
psychological support to the mother
• Assess degree of pain and provide pharmacological and non-pharmacological
pain relief method based on cause (episiotomy, lacerations or caesarean
section pain, breastfeeding, uterine involution.)
• Assess if no family centered care constraints( family support and involvement
in the care)
• Assess and ensure cleanliness of the mother(poor hygiene can lead to risk ofperipheral infections and patients’ discomfort)
Self-assessment 1.3
1. State the associate nurse interventions in the immediate postnatal period
care2. What is postnatal period?
1.4 General assessment of the baby in immediate postnatal periodPostnatal care encompasses aspects of obser
Learning Activity 1.4
Observe the following images which are showing the care provided to the babyin the postnatal period.
It is necessary to perform new born assessment after birth as it helps to rule out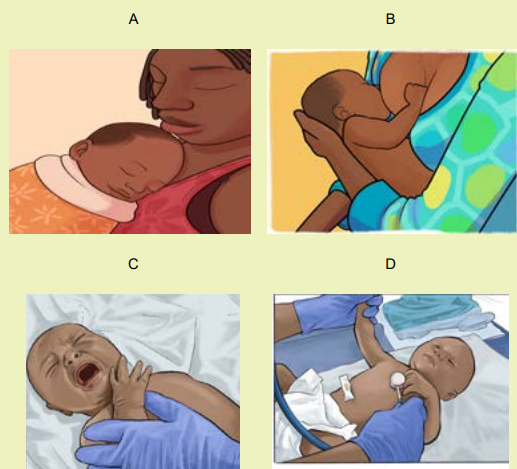
any abnormality.a) What are the general elements that you think the associate nurse can basePostnatal care encompasses aspects of observing and monitoring the health of theon in order to conduct the assessment of this baby?
mother and her baby, as well as offering support and guidance in breastfeeding andparenting skills.
Monitoring successful transition to extra-uterine life begins from the moment of
birth with an assessment of the APGAR score. This is measured at 1, 5, and if
needed, 10 minutes after birth, and is followed by an initial examination soon after
birth. A baby’s interactions with the parents during the first weeks of life are an
important pre-requisite for the continued wellbeing. The main elements of general
assessment for the baby in the immediate postnatal period include:• Skin colour (palor/ whitish color indicate the baby’s umbilical cord isSelf-assessment 1.4
bleeding, blue skin or cyanosis indicate respiratory distress)
• Respiratory rate (very or low respiration movement, noisy respiration, chest
indrawing, nasal flaring).
• Temperature (low body temperature is caused by exposure to coldness)
• Tone and activity (floppy and inactive baby is caused by hypoglycemia)
• Ability to breastfeed/feed (inability to breastfeed for the baby can expose
to hypoglycaemia, sudden death)
• Umbilical cord bleeding (cord bleeding cause anaemia and/or death of the
baby).
1. While assessing the baby in immediate postnatal period, what are the
causes of the following?
a) Paleness of the skin
b) Blue skin(cyanosis)
c) Floppy and inactive baby
d) Low body temperature
e) Very or low respiration movement, noisy respiration, chest indrawing,
nasal flaring.
2. What are the elements will you inspect on the baby in immediate postnatalperiod?
1.5 Practice of rapid general assessment of the baby
Learning Activity 1.5
Read the following case study of a newborn in immediate postnatal period.
Term baby boy born by spontaneous vaginal delivery, it’s now 4hours postdelivery.
the baby is number 1, baby is crying when associate nurse arrived
mother told her that the baby didn’t breast feed since birth, she has no knowledge
about breastfeeding.
a) By reading this scenario what do you think about this baby?
b) What do you think about this baby’s rapid assessment?
c) What do you think about help to this mother about baby feeding?
A key part of every postnatal nursing visit is to assess the new born for danger
signs, the common danger signs include; not feeding, lethargy (abnormal body
movements), fast breathing with chest in drawing, fever, hypothermia, jaundice and
convulsions.
Assessment of new born in immediate postnatal care includes;• Observe the baby’s general condition, including colour, responsiveness,
activity, spontaneous movement, feeding, and posture and muscle tone. ...
• Assess the head and skull for any abnormal findings (bulging or depressed
fontanelle). Depressed fontanelle indicates dehydration or bleeding. Bulging
fontanelle indicate intracranial bleeding or hematoma• Assess the eyes and sleepiness.
Assess for any of the following danger signs:
• History of difficulty feeding or unable to feed now; asks the mother about theobserved on the palms of the hands and soles of the feet.
baby’s feeding pattern.
• History of convulsion or convulsing now; asks the mother, has the baby had
any fits?
• Newborn seems lethargic or unconscious.
• Movement only when stimulated.
• Fast breathing.
• Severe lower chest in-drawing.
• Fever.
• Hypothermia (baby is cold to the touch).• Baby developed yellowish discoloration before 24 hours of age; jaundice
• There is swelling of the eyes or eye discharge.
• Umbilicus is bleeding or tie loosen
• More than 10 pustules (spots) are found on the skin
• Record findings, if anything unusual noted notify to the senior staff immediatelyand reassure the parents
Education to the mother about
• Baby care includes; breastfeeding, cord care, baby birth and clothing,Self-assessment 1.5
prevention of hypoglycemia and immunization.
• Hygiene and nutrition of the mother this includes; hand hygiene, body, perineal
care and balanced diet.
• Education about birth spacing and possible ovulation return.
• Education about danger signs to both mother and baby and when to comeback to hospital or when to alert care provider.
1. After assessing new born what education will you give to the mother?2. What will you do after noticing anything unusual?
1.6 Physiological changes and importance of vital signs monitoringin immediate postnatal period
Learning Activity 1.6
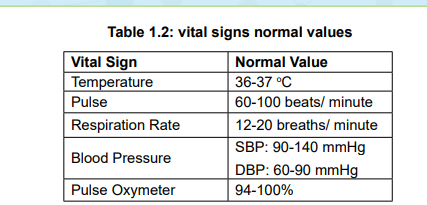
Image showing the materials used to take the vital signs like BP machine,thermometer, pulse oxymeter, watch, and stethoscope and pain scale.

You learned how to check the vital signs in Fundamentals of Nursing in S4.
a) What do you think that could be the importance of taking the vital signs of
the mother in the postnatal period?
b) What do you think about the use of thermometer?
c) What do you think about the frequency of taking vital signs in the immediate
postnatal period?
Vital signs are considered vital to the rapid assessment of the mother when it
is necessary to determine major changes in the mother’s basic physiological
functioning.
Physiological changes of vital signs monitoring in immediate postnatalperiod
Like other body systems change also vital signs undergo changes after delivery.
The following are changes that occur:
• Blood pressure
In immediate postnatal period, decreased blood pressure may result from the
physiological changes associated with the decrease in intra-pelvic pressure, or
it may be indicative of uterine haemorrhage. An increase in the systolic blood
pressure of 30 mm Hg or 5 mm Hg in the diastolic blood pressure, especially
when associated with headaches or visual changes, may be a sign of gestational
hypertension. Orthostatic hypotension may occur when the patient moves from asupine to a sitting position.
- Pulse rate
(bradycardia) commonly occur during the first 6 to10 days of the postpartum period.
During pregnancy, the weight of the gravid uterus causes a decreased flow of
venous blood to the heart. The elevated stroke volume leads to a decreased heart
rate. Postnatal tachycardia may result from a complication, prolonged labour, bloodloss, temperature elevation, or infection.
• Respiratory rate
The respiratory rate normal range of 12 to 20 respirations per minute elevated
respirations may occur due to pain, fear, excitement, exertion, or excessive blood
loss. Tachypnea, abnormal lung sounds, shortness of breath, chest pain, anxiety, or
restlessness are abnormal findings that must be reported. Immediately, these signs
and symptoms may be indicative of pulmonary oedema or emboli.
• Temperature
During the first 24 hours postpartum, some women experience an increase in
body temperature up to (38°C). High temperature at this time may be indicative ofinfection.
Self-assessment 1.6
1. What are the abnormal findings that must be reported while assessing the
respiration rate in immediate postnatal period?
2. While taking vital signs, when will you suspect that the mother is havingpostpartum haemorrhage?
1.7 Practice on the taking vital signs in the immediate postnatalperiod.
Learning Activity 1.7
Read the following scenario and with the aid of mannequin monitor this mother’s
vital signs.
28 years old mother P2 delivered by spontaneous vaginal delivery 1hour ago,
monitor Bp, pulse rate, body temperature, respiration, oxygen saturation and
pain score, every 30minutes for 2 hours and once every hour for next 3hours.
a) With aid of mannequin apply vital signs monitoring in immediate postnatal
period and record the findings and indicate rationale behind each vital sign
taking.
b) What do you think that the thermometer will help to the mother?
c) c) Which instrument do you think that it can help to auscultate the bowel
sound?
Vital signs monitoring is a fundamental component of nursing care because they
are essential in identifying clinical deterioration and that those vital parameters
must be measured consistently and recorded accurately in postnatal period.
Vital signs (blood pressure, heart rate, temperature, oxygen saturation, pain and
respiratory rate) are thought to undergo changes during and immediately afterdelivery.
Importance of vital signs monitoring in immediate postnatal period
Monitoring vital signs in immediate postnatal period and play the following role:• Help to detect the likely possible signs of shock
• Helps to prevent immediate postnatal related complication including
postpartum haemorrhage• Helps to intervene earlier if postpartumSelf-assessment 1.7• To promote maternal safety
1. What is the importance of monitoring vital signs to the mother in postnatal1.8 Protocol of vital signs monitoring in the immediate postnatal
period?2. List 6 vital signs you should monitor in immediate post-natal period.
period
Learning Activity 1.8
Read the case study below of mother in immediate postpartum period.
A 35 years old mother P3 in postpartum room 324 its now 1 hour postdelivery,
delivered by spontaneous vaginal delivery with intact perineum, she
is breastfeeding her baby boy without any problem and the nurse came in to
assess her wellbeing by monitoring of vital signs that is to say blood pressure
126/68mmhg, pulse rate 80bts/ min, respiration 20 cycles, oxygen saturation
98%, temperature 36oc, pain 4/10.a) Why do you think that it’s necessary to monitor vital signs of the mother in
the immediate postnatal period?
b) What do you reflect on the above pain score?
Monitoring vital signs in immediate postnatal period requires a close follow up.
Below is the protocol that can used for vital signs monitoring in the immediatepostpartum period.
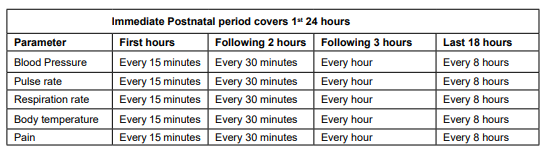
Table 1.1: Frequency of vital signs monitoring in the immediate postnatalperiod
Interpretation of vital signs in immediate postnatal period
If her blood pressure is too low and falling, and her pulse and respiration rates
are too fast and rising, she is going into shock. The most likely cause is a l
life-threatening haemorrhage. If there are no signs of bleeding from the vagina, she
may be losing blood internally. The associate nurse can help the mother by telling
her on a scale of 0 to 10 and she may state how she feels pain. Having no pain is
characterized by 0 (zero) and 10 is the worst possible pain.
This tool can be used during pain assessment to the mother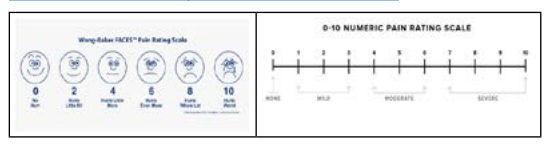
Self-assessment 1.8
1. Show the protocol of vital signs monitoring in immediate postpartum to 3
hours?
2. Interpret the following vital signs found from a mother who delivered 2
hours ago: Blood pressure (85/50), and pulse rate (120 beats/min) andrespiration rates (25 movements/minutes)
1.9 Techniques and importance of assessing bladder fullness inthe immediate postnatal period
Learning Activity 1.9
Read the following case study related to bladder fullness in immediate postnatal
period.
A 28-year-old primipara gave birth to a term 3 350 g baby in a maternity hospital.
She is admitted in postpartum ward and we are at 6 hour post-delivery. She is
complaining of abdominal pain, unable to void. She is sometimes having slight
bleeding. On examination, it was revealed that the episiotomy scar was intact and
there was no sign of perineal laceration. Physical examination of the abdomen
revealed a palpable and painful mass. Also the uterus is boggy and displaced on
lateral side of the abdomen. A urinary catheter was inserted and 3000 ml clear
urine was drained. After urine was drained, her pain was instantly relieved and
bleeding started to stop.Using the case described in the above scenario:
a) What do you think that could be the cause of distended abdomen to thisa. Techniques of assessing bladder fullness in the immediate postnatal
mother?
b) How long do you think that the spontaneous voiding should return to this
mother after birth?
c) What volume of the urine do you think that the mother is supposed to pass
per void in postnatal period?
period
To rule out the signs and symptoms of bladder fullness in the immediate postnatal
period, the associate nurse must do the following:• Observe if the mother has a full bladder (bulging or distension of the lowerSigns of bladder distension:
abdomen, displaced uterine fundus from the midline)
• Palpate the lower abdomen for assessing the bladder fullness tenderness
• Check for voidance amount. Expected volume is 150 ml for each void.• Location of the fundus above baseline level (determined with empty bladder)• Fundus displaced from midlineA full bladder will push the uterus up and toward the mother’s right side. Observing
• Excessive lochia
• Bladder discomfort
• Bulge of the bladder above the symphysis• Frequent voiding of less than 150ml each time
from the side, you might see what appears to be ‘camel humps’: the lower hump is
the bladder and the upper hump is the uterus.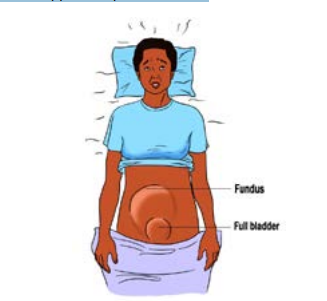
Figure 1.1: Image showing a mother with full bladder in immediate postnatal period
Importance of assessment and emptying full bladder in the immediate
postnatal period
Profound diuresis can begin immediately after delivery and spontaneous voiding
usually returns within 6-8 hours post-delivery. In immediate postnatal period,
the bladder fills rapidly after delivery due to the marked increase in urine production.
The urine volume should return to pre-pregnant levels by 2-3 days after delivery.
The importance of assessing and emptying the full bladder is:
• A full bladder can displace the uterus and lead to postpartum haemorrhage.
Therefore, assessing and emptying the full bladder can help in prevention of
postpartum haemorrhage.
• The woman who voids frequent, small amount of urine may have increased
residual urine because her bladder does not fully empty. Consequently,
residual urine in bladder may promote the growth of microorganisms and
formation of renal calculi if it takes long time. Therefore, assessing and
emptying the full bladder may help in prevention of postpartum urinary
tract infections.
• To promote optimal bladder function after delivery
• Reduce risks of uterine atone (bladder distension causes uterine atone)
• Reduce and manage postpartum after pains
• Reduce immediate postnatal stress to the mother due to increase after
pains related to full bladder
• Promote the wellbeing of the mother in postnatal period
• Assessment of the bladder function
• Assessment of the bladder function to the mother in postnatal period includes:
• Return of urination, which should occur within six to eight hours of delivery
• For approximately 8 hours after delivery, amount of urine at each void.
Patients should void a minimum of 150 mL per void; less than 150 mL
per void could indicate urinary retention due to decreased bladder tone
post-delivery (in the absence of preeclampsia or other significant health
problems).
• Signs and symptoms of a urinary tract infection (UTI), including frequent
urination, bladder spasm, cloudy urine, persistent urge to urinate, and
pain with urination
• The bladder should be not palpable above the symphysis pubis. Mothers
are encouraged to drink adequate fluid each day and to report signs and
symptoms of a urinary tract infection, including frequency, urgency, painful
urination, and hematuria.
Self-assessment 1.9
a. What is the importance of emptying urinary bladder in the immediate
postnatal period?
b. What are the techniques used to assess full bladder in the immediate
postnatal period?
c. What are the consequences of full bladder to the mother in immediatepostnatal period
1.10 Nursing interventions for full bladder in the immediatepostnatal period.
Learning Activity 1.10
Read this case study for the mother in postnatal period with a health
problem.
A mother called KD whose 31 years old, P2, G2 complained of unusual vaginal
bleeding and difficult in passing out the urine, abdominal pain, general body
weakness and distended abdomen at 4 hours after delivery. The vital signs
during the assessment revealed that the BP: 108/96 mmHg, pulse: 78 beats/
minute, temperature: 36.8 oc, respiration: 18 breaths/ minute. This mother has
delivered also by vaginal delivery without any episiotomy or perineal tear. Her
baby is breastfeeding with no problem.a) From this case study.The associate nurse must play a major role to ensure the bladder is empty. The
b) What do you think that may be the cause of that vaginal bleedingc) What do you suggest that can be done to help this mother?
following are the role of the nurses while emptying the bladder in immediatepostnatal period:
• Ask the mother to urinate within the first two to three hours. If she is too
tired to get up and walk, she can squat over a bowel on the bed or on the
floor, if she has urine retention she may need urinary catheter in place. If the
mother cannot urinate after four hours, and her bladder is not full, she may
be dehydrated.
• Help her to drink fluids
• Check bladder fullness frequently in post-delivery period.
• Encourage the woman to empty her bladder regularly
• Check the amount of voiding for measuring input and output
• If no void in 4-6 hours, encourage the mother to go to void
• Stimulate voiding by running tap water or pouring warm water over the
perineum if possible.
• Provide or help the mother to take plenty fluid
• If over 6 hours and the bladder is still full, refer her where the urinary cathetercan be used to empty the bladder.Self-assessment 1.10
• In setting where urinary catheterization is done for distended bladder (avoid
rapid emptying and do not remove more than 800 ml at one time – This prevents
a precipitous drop in intra-abdominal pressure and splenic engorgement andhypotension).
a) What are the strategies used to empty full bladder in the immediate
postnatal period?
b) What are the roles of the associate nurse during the technique of bladder
emptying?
c) When do you decide to refer the mother to go where the urinary cathetercan be inserted?
1.11 Concepts, physiology and importance of measuring fundalheight in immediate postnatal period.
Learning Activity 1.11
Techniques of measuring fundal height (In skills lab by use of mannequin)
Place the zero mark of the tape measure at the uppermost border of the uterine
fundus to uppermost border of the symphysis pubis. To locate the fundus, the
hand is moved down the abdomen below the symphysis pubis until the curved
upper border of the fundus is felt.a) What do you think that could be the importance of measuring the fundalConcepts, physiology and importance of measuring fundal height in
height in the immediate postnatal period?
b) Where do you think that the fundus may be located immediately after birth?
immediate postnatal period
Concepts
Fundal height: is the distance from the pubic bone to the top of the uterus measured
in centimeters.
Boggy uterus: refers to a clinical finding in which the uterus is identified as
enlarged and soft.
Uterine atony: is defined as failure of the myometrium to contract and retract
around the open blood vessels of the utero-placental implantation site following
childbirth. A hypotonic uterus, or “boggy” uterus, is among the most common
obstetrical conditions which may cause postpartum infection and postpartumhaemorrhage (PPH).
Uterine retraction: Retraction of the uterus is a phenomenon of the uterus in labour
or after delivery in which the uterine muscle fibers are permanently shortened.
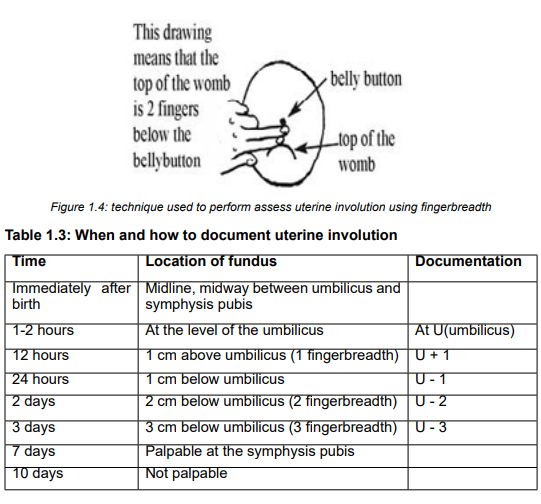
Physiology of fundal height after delivery
Usually, the progression of uterine descent into the pelvis is 1cm/day. Immediately
after delivery, the fundus is in the midway between umbilicus and symphysis
pubis. 1hour postpartum, the fundus is at umbilicus level or just slightly below
it. At 12 hours, the fundus is at 1cm above the umbilicus. At 24hours, it is at
1cm below the umbilicus. Day 2 to day 7, it decreases about 1cm/day. Day 7,
just palpable at the symphysis, Day 10-14, not palpable, Weeks 6, it returns to
non-pregnancy size.
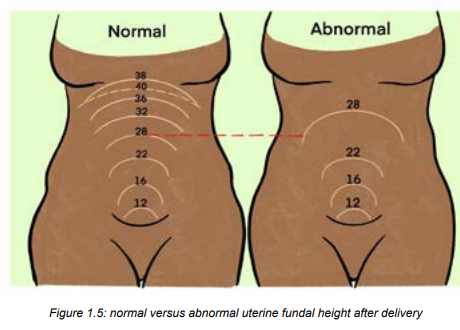
Importance/role of measuring fundal height in immediate postnatal period
Assessing the fundal height allows identify:• The state of uterine involution progress
• Identify uterine tone and the cause of uterine atony related bleeding
• Prevent uterine atony related bleeding
• Help the other reducing after pains through uterine massage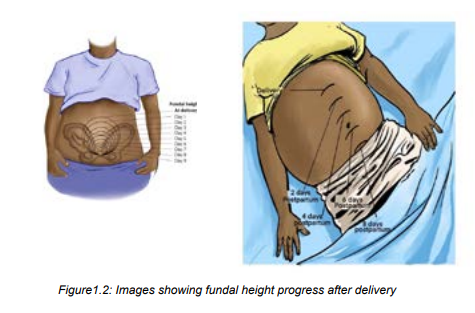

Self-assessment 1.11
Define the following terms:a) Fundal height1.12 Technique of assessing the fundal height in the immediate
b) Boggy uterus
c) Uterine retractiond) Uterine atony
postnatal period.
Learning Activity 1.12
Techniques of assessing uterine retraction (In skills lab by use of mannequin)
The mother GA delivered a baby boy in 45 minutes ago. When looking at her
abdomen, the uterus area still looks big, the mother is having slight bleeding. On
palpation, the associate nurse realizes the uterus is very soft and deviated at
lateral side of the abdomen.
By relating to the scenario described above, answer the following questions:a) What can be proposed as the materials to be used while measuring the
fundal height?
b) What do you think about the time of checking for the uterus contraction inWhile assessing the fundal height, below is the procedure of measuring the fundal height inthe postnatal period?
immediate postnatal period:• The fundus is assessed for approximately one hour post-delivery
• Ensure the bladder is empty before palpation of the uterine fundus.
• If the fundus is deviated or elevated above the level of umbilicus always rule
out distended bladder.
• Massage prior palpation and assess for any blood discharged during massage
• Using hand palpate the uterus and check if the fundus is firm
• Apply fingerbreadths (each fingerbreadth=1cm) or tape measure on uterus
and precise the fundus level of descent• Interpret and document findings on the patient’s file
Self-assessment 1.12
a) At what time does the fundus take to be located at 1 cm below the umbilicus
after delivery?
b) If the fundus is deviated or elevated above the level of umbilicus, what the
associate nurse will do prior to progress to further step of fundal height
assessment?
c) The fundus is palpable at the symphysis pubis at what time?
1.13 Physiology and importance of uterine retraction in immediatepostnatal period
Learning Activity 1.13
The mother GA 26 years old P1 delivered a baby boy, it’s now 2 hours and30 minutes
postpartum. When associate nurse palpates her abdomen during obstetrical assessment,
realises that; the uterus is still big 2 cm above the umbilicus and soft the mother is having
moderate vaginal bleeding, when the nurse takes vital signs they are in normal range
except pulse of 118bts/min.
By relating to the scenario described above, answer the following questions:a) What do you think about importance of checking softness or firmness of
the uterus in the postnatal period?b) What you think should be done before palpating the mother’s abdomen?
Physiology of uterine retraction in immediate postnatal period
Immediately after the placenta delivery, it begins to involute with contractions of the smooth
muscle of the uterus. It contracts midline with the umbilicus. The uterine contractions come
from effect of oxytocin. The fundus contracts downward towards the pelvis. The uterus
becomes firm and retracted with alternate hardening and softening. The failure of the uterus
to retract (uterine atone) leads to increased risk of postpartum hemorrhage.
Factors enhancing the uterine retraction include: uncomplicated labor, early initiation of
breastfeeding, complete delivery of the placenta.
Then, factors hindering the uterine involution include prolonged labor, incomplete separation
and expulsion of placenta, grand multiparty, full bladder and anesthesia.
Importance of uterine retraction in immediate postnatal period
Therefore, the following are importance of assessing uterine retraction:• Early prevention of postpartum hemorrhage caused by uterine atone orSelf-assessment 1.13
placenta retains
• Reducing risks of postpartum deaths due to postpartum hemorrhage
• Reducing the intensity of severe postpartum after pains as uterine massage
is always in the process of assessment of uterine retraction.
1. Which hormone is involved in immediate postnatal period uterine retraction?
2. Enumerate factors hindering the uterine retraction in immediate postnatal
period
3. What is the importance of uterine retraction assessment to the mother inpostnatal period?
1.14 Monitoring protocol and technique used in uterine retractionassessment and care
Learning Activity 1.14
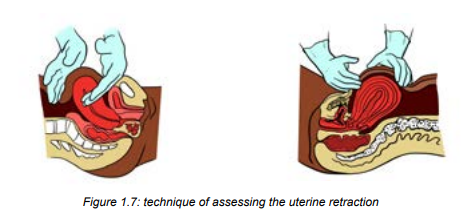
Observe the image below and read the technics used to assess uterineretraction.
Have the bladder empty prior to assessment
Make sure the woman is in a supine position
The health care provider should have one hand at the level of the umbilicus and
the other hand right about the symphysis pubis to stabilize the uterus
Palpate her abdomen to check contraction of the uterus to make sure it is firm.
Immediately after birth, you should be able to feel it is contracting near the
mother’s umbilicus.a. What do you think about stabilising of uterus during palpation and massaging?
b. What do you think about the time and frequency of checking the softness orfirmness of the uterus in the postnatal period?
a) Monitoring of uterine retraction in immediate postnatal period
The uterine retraction combined with uterine massage is generally performed every 10-15
minutes for the first hour after birth, and every 30 minutes during the second hour.
After the first two hours this massage usually happens every 4-8 hours until discharge.
b) Technique of uterine retraction assessment
• Have the bladder empty prior to assessment, a distended bladder may delay
the uterine retraction
• Make sure the woman is in a supine position
• The health care provider should have one hand at the level of the umbilicus
and the other hand right about the symphysis pubis to stabilize the uterus
• Palpate her abdomen to check contraction of the uterus to make sure it is
firm. Immediately after birth, you should be able to feel it is contracting nearthe mother’s umbilicus.
a) Monitoring of uterine retraction in immediate postnatal period
The uterine retraction combined with uterine massage is generally performed every 10-15
minutes for the first hour after birth, and every 30 minutes during the second hour.After the first two hours this massage usually happens every 4-8 hours until discharge.
b) Technique of uterine retraction assessment
• Have the bladder empty prior to assessment, a distended bladder may delay
the uterine retraction
• Make sure the woman is in a supine position
• The health care provider should have one hand at the level of the umbilicus
and the other hand right about the symphysis pubis to stabilize the uterus
• Palpate her abdomen to check contraction of the uterus to make sure it is
firm. Immediately after birth, you should be able to feel it is contracting near
the mother’s umbilicus.
• A boggy uterus, soft, displaced or associated with bleeding from midline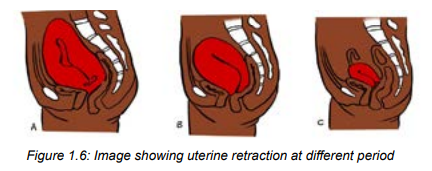
needs to be investigated
• Attention: The hand at the umbilicus will push down and in to feel the fundus
(feel if the uterus is firm or hard, soft or displaced laterally). The support is
need to help prevent uterine inversion and prolapse
• If the uterus is hard, leave it alone between checks. If it feels soft, rub/
massage the abdomen at the top of the uterus to help it to contract. (see the
video on YouTube)
• If the uterus is soft/boggy and resisting to uterine massage, misoprostol or
oxytocin may be administered
• At the end teach and demonstrate the mother how to do to self-massage• Thank the mother and record findings
Self-assessment 1.14a) Which schedule that can be respected during uterine massage after birth1.15 Physiology, causes and signs of blood loss immediate
for the first 48 hours?
b) What is the impact of full bladder on the uterine retraction?
c) What will the associate nurse do to prevent the uterine inversion while
checking and performing the uterine massage in postnatal period?
d) What will be the signs of a well retracted uterus in immediate postnatalperiod?
postnatal period
Learning Activity 1.15
Observe the image above and then read the following case study :
DM is 30 years old with G6, P6 mother who delivered a baby girl in 1hour ago the
associate nurse come to notice that the mother looks unhappy, reports feeling
cold, thirsty and sometimes feels dizzy. She has also; vaginal bleeding and her
bed sheets are soiled with blood. On examination the associate nurse finds
bleeding from vagina and the BP of 80/60, PR of 110beats/minute with signs of
increased respiratory movements.
By using the scenario above answer the following questions:a) What do you think can indicate unusual blood loss to that mother inPhysiology of postnatal blood loss
scenario?
b) What do you think about benefits of estimating the amount of blood loss inimmediate postnatal period?
After birth, it is normal for a woman to bleed the same amount as a heavy monthly period.
The blood should also look like monthly blood; old and dark, or pinkish. Immediately after
birth, the first the blood comes out in little spurts or gushes (lochia rubra) when the uterus
contracts, or when the mother coughs, moves, or stands up, but the flow should reduce over
the next two to three days.
Normally after delivery of placenta the expected blood loss 250mls therefore the nurse has
to monitor blood loss every 30 minutes for next 3hours, once an hour for next 3 hours.
It is important to recognize whether there is no excessive blood loss during childbirth, which
is a significant cause of morbidity and mortality.
Lochia
Lochia is normal discharge from the uterus after childbirth; it contains blood, mucous and
placenta tissue. Lochia discharge typically continues for 4-6weeks after childbirth (while the
reproductive organs return to their pre pregnancy state). Inspect the colour, odour and the
amount of lochia.
Types of lochia
Lochia is described using 3 names. Lochia rubra is the first vagina discharge colour lost
following birth of baby, it is dark red (red) in colour because it contains large amount of
blood, this amount comes from the wound left behind inside the uterus where the placenta
sheared away, it occurs for 3-5 days after birth. Lochia serosa is the term for lochia that has
thinned and turned brownish/ pink in colour, it continues until around the 10th day post birth.
Lochia alba is described as vaginal loss which has turned yellow /whitish. This typically
occurs after the 10th day and may last from the 2nd through to the 3rd and up to 6weeks afterbirth.
Lochia should not become offensive in smell or turn bright red after becoming serosa or
alba. If possible or happened, the mother should seek the health professional for additional
advice and care. When lochia subsides, the uterus is considered as closed, partial infection
is less likely. It is important to note that patients who had a C-section will typically have lesslochia than patients who delivered vaginally; however, some lochia should be present.
After discharge, patients should report any abnormal progressions of lochia, excessive
bleeding, foul-smelling lochia, or large blood clots to their physician immediately. Patientsare instructed to avoid sexual activity until lochia flow has ceased.
Patients who had a C-section typically have less lochia than patients who delivered vaginally;
however, some lochia should be present.
Signs and symptoms of blood loss in immediate postnatal periodSigns and symptoms of blood loss in immediate postnatal period vary depending on the
amount lost
The follow are the most common symptoms of postpartum haemorrhage:• Uncontrolled bleeding.• For heavy bleeding, the patient may experience loss of consciousness and
• Decreased blood pressure.
• Increased heart rate.
• Decrease in the red blood cell count.
• Swelling and pain in the vagina and nearby area if bleeding is from ahematoma.
other signs of symptoms of hypovolemic shock
Self-assessment 1.15
1. Explain the normal pattern of blood loss in immediate postnatal period
2. Normally after delivery of placenta the expected blood loss is:a) 600mls3. Explain signs and symptoms of mild blood loss in immediate postnatal
b) 500mls
c) 250mlsperiod
1.16 Methods of blood loss assessment in the immediate postnatal
period
Learning Activity 1.16
Observe the image below showing blood loss with in 1 hour after delivery.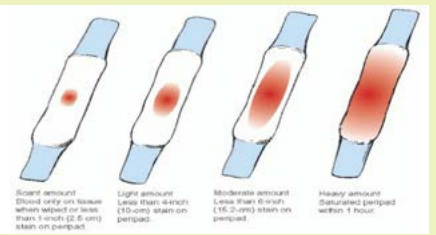
a) What do you think about image D?b) How do you think that the blood loss can be estimated?
In many instances, the birth attendant assesses blood loss by looking at the
amount of blood lost, and estimating its volume (visual estimation). This method
is available in all birth settings. In another method, the birth attendant places a
shallow bedpan below the mother’s buttocks, and then weighs the collected blood,
along with blood that has soaked into any pads and material. This is referred to
as an indirect method. In one direct method, a ‘calibrated delivery drape’ is placed
under the mother’s buttocks and tied around her waist, with the calibrated funnel
portion (that indicates how much blood she has lost) hanging down between her
legs. Other methods are also available, such as dye dilutions and radioactivetechniques, but these are not practical in many birth settings.
There are two methods of measuring blood loss:
One is by direct measurement of collected blood (swabs, pads, pampers etc) and
the other is by indirect measurement and later reflects blood loss by assessment of
haemoglobin concentration in the blood.
Very heavy bleeding is dangerous. To check for heavy bleeding in the first six hours
after birth and check the mother’s pads often, 500ml (about two cups) of blood loss
is too much. If she soaks one pad per hour, it is considered heavy bleeding. If the
mother is bleeding heavily, and you cannot stop it, take her to the hospital or ask for
help from other health care providers. Remember that postpartum haemorrhage is
a major cause of maternal mortality and it can happen at any time in the postnatalperiod.
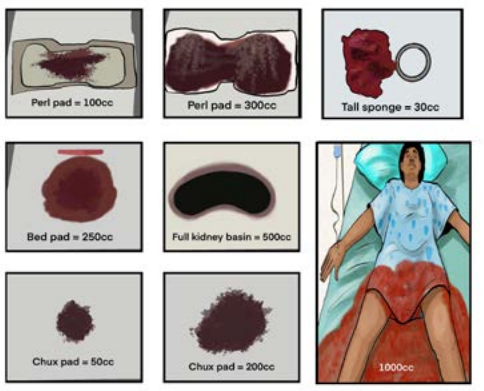
Figure 1.9: blood loss visual estimation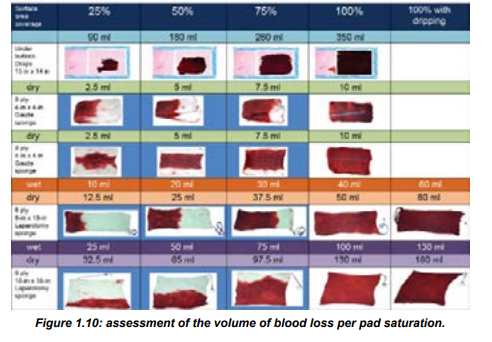
Lochia is assessed during the postpartum period:
Saturating one pad in less than an hour, a constant trickle of lochia, or the presence
of large (i.e., golf-ball sized) blood clots is indicative of more serious complications
and should be investigated immediately. A significant amount of lochia despite a
firm fundus may indicate a laceration in the birth canal, which should be addressedimmediately.
Foul-smelling lochia typically indicates an infection and needs to be addressed as
soon as possible
Episiotomy/perineal tear blood loss assessment and care
To assess episiotomy or perineal tear, the associate nurse must use a gloved hand
to gently examine the mother’s genitals for tears, haemorrhage, or a haematoma
(bleeding under the skin).
The acronym REEDA is often used to assess an episiotomy or laceration of the
perineum.
REEDA stands for:
R: Redness
E: Edema
E: Ecchymosis
D: Discharge
A: Approximation
Redness is considered normal with episiotomies and lacerations; however, if there
is significant pain present, further assessment is necessary. The use of ice packs
during the immediate postpartum period is generally indicated. There should be an
absence of discharge from the episiotomy or laceration, and the wound edges should
be well approximated. Perineal pain must be assessed and treated. Performing
Kegel exercises are an important component of strengthening the perineal muscles
after delivery and may be begun as soon as it is comfortable to do so. If a woman
has a tear that needs to be repaired, apply pressure on it for 10 minutes with a
clean cloth or pad and manage accordingly. If the tear is small, it can probably healwithout being sutured, as long as it is kept clean.
Self-assessment 1.16
1. What are the methods used for blood loss assessment in the immediate
postnatal period
2. Define the term lochia3. Differentiate the term lochia rubra from lochia serosa
1.17 Perineal and genital care
Learning Activity 1.17
Observe the images below showing perineal and genital care to themother in the immediate postnatal period.
a) What do you think about perineal and genital care in immediate postnatal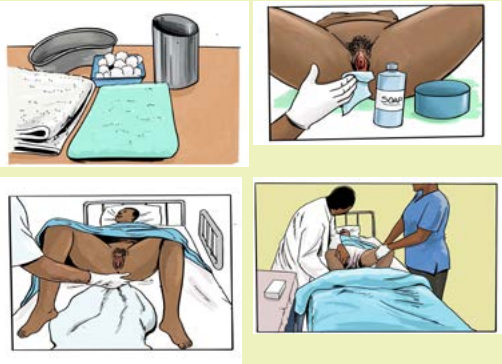
period?b) What do you think about changing pads and bedmaking in this period?\
In immediate postnatal period most of the time mothers are very tired due to labour
process and cannot care by themselves. The perineal care also helps to prevent
infection. Rinse the perineum with water after the use the toilet and before the
putting on a new peripad.
Therefore, it is the responsibility of the associate nurse to care those mothers, In
caring perineal and genital area, the associate nurse must always wash hands first
and put on surgical gloves before touching the mother’s genitals parts;
• Washing and cleaning the perineal and genital parts and changing pads after
birth must be done every 4-6 hours, or more frequently in case of heavy
bleeding or lochia and/or and after passing the stool.
• The associate nurse must clean the mother’s genitals very gently, using a
soap and very clean water and soap
• After cleaning the perineum and genital parts, the mother is dressed with
clean clothes and sanitary pad and changing of bed sheets for good hygiene,
infection prevention and making her comfortable.
• Cleaning perineal and genital area must be done in anteroposterior direction
from vulva to the anus. This is because even a too small piece of stool in
genital area can cause infection. Be careful not to bring anything up from the
anus toward the vagina.
• Disinfection of the episiotomy site or tear must be done if applicable.• Do not use alcohol or any other irritant disinfectants in genital area.
Self-assessment 1.17
1. Why is it necessary to clean perineum in anteroposterior direction?
2. Why is it discouraged to use alcohol or any other disinfectants to cleangenital area?
1.18 After pains care and education to the mother in the immediatepostnatal period.
Learning Activity 1.18
Read the following case study that is showing a mother having after pains in
postnatal period.
MD whose 28 years old with G4, P4 and lying on the bed in 5 hours postdelivery
by the arrival of associate nurse noticed that mother looks unhappy, and
complains lower abdominal most often when the baby is put on breast and she
fears to put the baby on breast. In addition to that episiotomy was done to her
while delivering and she fears to go to toilet. On palpation, the associate nurse
felt some contractions like at the uterine area and the uterus started to descend.
After the associate nurse helped her to relieve after pain, the associate nurse
started providing health education
Referring to the case described above, answer the following questions:a) What do you think it is after pains?The associate nurse is called to assist alleviating after pains and provide health
b) What do you think that may be the predisposing factors of after pain to
mother in postnatal period?
c) What can you suggest as at least one method to use in order to relieve
after pain?
d) What kind of education do you think should be provided by the associate
nurse to that mother?education to the mother in immediate postnatal period.
After pains care in immediate postnatal care
After delivery the uterus contract and relax as it shrinks back to its pre-pregnancy
status. This cramping also is called “after pains” It may feel like menstrual cramps
or even labor contractions. After-pains are contractions that occur after labor and
delivery. In addition, the perineum may be bruised, or the mother may have some
episiotomy stitches which can increase the pain in the immediate postnatal period.
The primiparous woman typically has mild after pains, if she notices them at all,
because her uterus is able to maintain a contracted state. Multiparas and patients
with uterine over distention (eg., large baby, multifetal gestation, hydramnios) are
more likely to experience after pains, due to the continuous pattern of uterine
relaxation and vigorous contractions.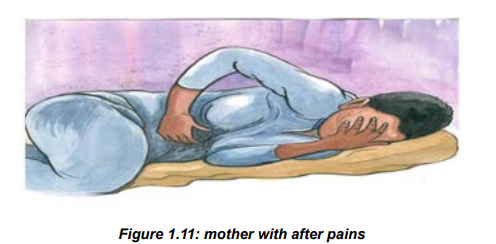
While providing emotional support, the associate nurse must do the following:
In addition to pain medication (ibuprofen, diclofenac) prescribed by the physician or
a midwife, the associate nurse can provide non pharmacological comfort techniquessuch as;
• Help the mother to place ice on the perineum to reduce swelling and pain• Apply warm compress or water bottle to lower abdomen
• Assist the mother to sitting and/or lie in positions that can help her feeling
more comfortable
• Prone position with small pillow under abdomen (that position applies pressure
to uterus and stimulates contraction.
• Guide relaxation and breathing techniques to the mother (read books on
relaxation and breathing technics)
• Keep the mother’s bladder empty
• Assisting the mother to immediately start breastfeeding after birth and
frequently as it helps alleviating after pains, for breast milk production and
helps and preventing hypoglycemia to the newborn.• Help if possible or advise the mother to start walking soon after delivery.
 The associate nurse is called to assist alleviating afterpains and provide healtheducation to the mother in immediate postnatal period.Education (hygiene, nutrition, breastfeeding, baby care, immunization, birth spacingand emotional support).In immediate postnatal period, the associate nurse should teach the mother about
The associate nurse is called to assist alleviating afterpains and provide healtheducation to the mother in immediate postnatal period.Education (hygiene, nutrition, breastfeeding, baby care, immunization, birth spacingand emotional support).In immediate postnatal period, the associate nurse should teach the mother about
the following:• Delaying the baby’s first bath to after the first 24 hours• Baby’s warmth through putting the baby skin-to-skin on mother’s abdomen,the hat on the baby’s head and dressing the baby not cold clothes.• Observing frequently umbilical cord for any bleeding and ensure hygieniccare of the baby’s umbilical cord stump.• Motivate the mother to stay closely to the baby for maintaining the bondbetween them• Encourage the mother to increase the fluid and food intake with increasingintake of fruits and vegetables in order to gain strength and maintain hydration.• Encourage her to go to void frequently for at least 2hours urine• Encourage mother early breast feeding especially in the first hour of life• Tell the mother to report immediately anything unusual like bleeding, severeheadache to her or umbilical cord bleeding, inability to breastfeed, anddifficulty breathing to her baby• Tell the mother to wash hands every time she comes from toilet beforechanging her pad or breastfeeding her baby• Encourage the mother have a shower if dirty to prevent risk of infection• Encourage the mother to change sanitary pads if dirty• Talk with mother during the assessment and care, teach her the thingsSelf-assessment 1.18
about her care as you go along, baby care, and ask her what she needs,
if she needs help let her have it. Example: perineal care when checking
the perineum, rationale for sits bath, use of local analgesics, rationale for
ambulation especially if a C-section, baby care like changing diapers, baby
bath, latching etc.
• Encourage the mother to limit visitors in order to get the rest, encourage her
to believe in herself and think positively about parental hood.
• Rest is usually encouraged during the first hours preferably in prone position
as this aids drainage from the uterus and vagina.
• Educate the mother about birth spacing and its benefits to mother, her baby,
family, community and entire nation.
Summary of the unit:A good method to remember how to check and care the mother in immediatepostnatal period is the use of the acronym BUBBLEHE:B: Breast.U: Uterus.B: Bladder.B: Bowel.L: Lochia.E: Episiotomy.H: Homans’ sign (to detect early DVT)E: Emotional response.1. Regarding after pains care answer the following questions:1.19. End of unit assessment 1
a) What are the non-pharmacologic comfort measures used to relieve
afterpains?
b) What will the associate nurse do to reduce swelling and pain on perineum
with tears or episiotomy?
c) What will the associate nurse do to reduce pain through positioning the
mother?
2. In teaching the mother in postnatal period answer the following questions:
a) What will you teach the mother regarding the baby’s warm and umbilical
cord
b) How would you instruct the mother on the time and frequency of
breastfeeding?
c) What can you teach the mother regarding taking fluid and food?
d) What are you supposed to teach the mother regarding elimination and
hygiene after elimination?
End of unit assessment 1
SECTION A: Multiple choice and true or false
1. A postpartum nurse is preparing to care for a woman who has just delivered a
healthy new born infant. In the immediate postpartum period the nurse plans to
take the woman’s vital signs:a) Every 30 minutes during the first hour and then every hour for the next2. A postpartum nurse is taking the vital signs of a woman who delivered a healthy
two hours
b) Every 15 minutes during the first hour and then every 30 minutes for the
next two hours.
c) Every hour for the first 2 hours and then every 4 hours
d) Every 5 minutes for the first 30 minutes and then every hour for the next4 hours.
new born infant 4 hours ago. The nurse notes that the mother’s temperature is
37.8°C3.
Which of the following actions would be most appropriate?a) Retake the temperature in 15 minutes3. The nurse is assessing a client who is 6 hours postpartum after delivering a
b) Notify the physician or the senior nurse
c) Document the findingsd) Increase hydration by encouraging oral fluids
full-term healthy infant. The client complains to the nurse of feelings of faintness
and dizziness. Which of the following nursing actions would be most appropriate?a) Empty the bladder for that mother4. What vital signs findings will be indicative of unusual vaginal bleeding in
b) Instruct the mother to request help when getting out of bed
c) Elevate the mother’s legs
d) Avoid bringing the new born infant to the mother until the feelings of lightheadedness and dizziness have diminished
immediate postnatal period?a) Hypertension5. What will indicate that the bladder is full in immediate postpartum?
b) Rapid pulse
c) Hypotensiond) Both b and c
a) Soft and flat abdomen.6. Answer by true or false. By assessing the uterine retraction, the following
b) Bulging and distended lower abdomen with painful on touch and displace
c) Distended uterus.d) Lower abdominal pain with urinary frequency.
statements will indicate to the associate nurse that the uterus in not well retracted
in immediate postnatal period.a) The uterus becomes firm and retracted.SECTION B: Short answers
b) The uterus becomes big in size but palpable.
c) The uterus becomes soft and boggy.
d) Unusual vaginal bleeding with bulging of lower abdomen.e) Hard uterus, non-tender and mild vaginal bleeding.
7. What an associate nurse will do in case he/finds the uterus is hard? -------
-- soft? ………………
8. While measuring the fundal height, where will the associate nurse
expect the uterine fundus: immediately after birth? …….. 2hours?
12hours…………………Interpret and document those findings.
9. In which situation is it necessary to wash and clean more frequently the
perineal and genital in immediate postnatal period?
10. What will be the techniques that the associate nurse will use to empty the
full bladder in immediate postnatal period?
11. In palpation, what will the moist and cold skin indicate to the mother?
12. In palpation, what will whitish (pale) conjunctiva indicate to the mother?
13. Which mothers are more likely to experience after pains compared to their
peers? Explain why
14. What medications can be given to the mother experiencing after pains
resisting to non-pharmacological methods?
15. To differentiate after pains with other abdominal pains, describe the
characteristics of after pains in postpartum period
16. While teaching the mother about rest in immediate postnatal period why
do we advise the mother to rest in prone position? Explain.
17. Briefly explain the components of inspection during general examination
of the mother in the immediate postnatal period.
18. Describe the physical checks you should do on postnatal mother soon
after delivery.
19. Describe the importance and expected normal findings for each vital sign
taken during immediate postnatal period.20. Describe how full bladder may cause postpartum bleeding
UNIT 2: POSTNATAL OBSTETRIC DANGER SIGNS
Key Unit Competence:
Identify obstetrical danger signs in women during postnatal period and manage the
woman accordingly.
2.0 Introductory activityIntroductory activity 2
Observe the following pictures showing a mother with postnatal obstetric dangersigns.
1. What do you think on a mother who may deliver and continues to have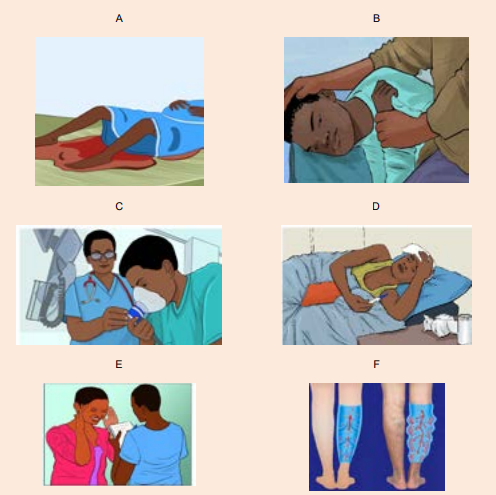
vagina bleeding? Which image that is expressing that situation?
2. What are the complications that are likely to occur to the picture A situation?
3. Did you have an exposure with the person who was presenting seizures?
What do you think that can be done to this person with seizures?
4. Have you seen a person with difficult in breathing? What do you suggest
that can help this person with breating difficulties?
5. Have you ever had hotness of the body? What do you think that can help
to reduce the body temperature for this person with hotnes of the body like
in image D situation?
6. Have youever been in contact with the person with headache? What do
you suggest that can be done in order to help this person with headache
like in picture E?
7. What do you think to the mother who may deliver and develop deep vein
thrombosis at the lower limbs? What do you suggest that can help theperson with this condition like picture F state?
2.1 Assessment of vaginal bleeding as an obstetric danger signin the postnatal period.
Learning Activity 2.1
Observe the following image and try to think about the medical condition thatcan be reflected on it.
a) Which obstetrical condition do you think that looks like this image above?
b) Have you ever seen acondition like this?c) Which clinical manifestations do you observe from this mother?
Obstetrics: is the field of study concentrated on pregnancy, childbirth and the
postpartum period.Hemorrhage means excessive bleeding.
In postnatal period, blood loss of 500 ml or less following a delivery is generally
considered as physiologically normal. However, severe postnatal blood loss is life
a threatening situation to the other. In immediate postnatal period, bleeding also
called ‘postpartum haemorrhage’ (PPH) is defined as:• Bleeding more than 500mls following vaginal delivery and 1000mls following
Caesarean section in the first 24 hours following birth.
• Constant trickling of blood after delivery in the first 24 hours following birth. or
• Blood loss sufficient to cause hemodynamic instability in the first 24 hours
following birth.
• Postpartum haemorrhage is the leading cause of morbidity and mortality
among pregnant women (approximately one third of deaths of maternal
mortality) worldwide. Therefore, early recognition of these danger signs isvery important in order to avoid delay
Vaginal bleeding risk factors
The following are the risk factors that should be watched out to the mother inpostnatal period:
•Conditions that distend the uterus beyond average capacity. Multiple
gestations, hydramnios, a large baby, and the presence of uterine myomas
predispose to postpartum haemorrhage.• Conditions that could have caused cervical or uterine lacerations. Awoman who underwent operative birth (caesarean section) or rapid birthCauses of vaginal bleeding
could develop lacerations that would cause bleeding.
• Conditions with varied placental site attachment: Placenta praevia and
abruption placenta also cause heavy maternal bleeding.
• Uterus could not contract readily: Conditions such as deep anesthesia during
caesarean delivery, advanced maternal age, and high parity could cause the
uterus not to contract and therefore result in bleeding.
• Inadequate blood coagulation: Disseminated intravascular coagulation
(DIC) in a woman could cause heavy bleeding postpartum.
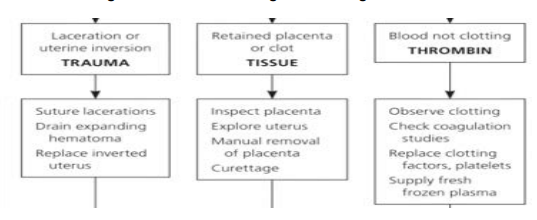
Vaginal bleeding has many potential causes but the common known 4Ts are the
following. They are arranged according to frequency:• Tone (70%)• Trauma (20%)Tone: uterine atone is the inability of the uterus to contract and may lead to continuous
• Tissue (9%)• Thrombin (1%)
bleeding. Retained placental tissue and infection may contribute to uterine atone.
Uterine atone is the most common cause of postpartum haemorrhage
Trauma: Injury to the birth canal which includes the uterus, cervix, vagina andthe perineum which can happen even if the delivery is monitored properly
Tissue: retention of tissue from theplacenta orfetusas well as placental abnormalitiessuch as placenta accreta and pericreta may lead to bleeding.
Thrombin: a bleeding disorder occurs when there is a failure of clotting, such aswith diseases known as coagulopathies.
Signs and symptoms of vaginal bleeding in postnatal period
Signs and symptoms of vaginal bleeding generally include heavy bleeding from the
vagina that doesn’t slow or stop over time. Initially there may be an increased heart
rate, feeling faint upon standing, and an increased respiratory rate. As more blood
is lost, the patient may feel cold, blood pressure drop (hypotension), and they may
become unconscious in case of severe vaginal bleeding.
Self-assessment 2.1
1. Define postpartum haemorrhage.
2. Explain the risk factors of postpartum haemorrhage.
3. Enumerate causes of postpartum haemorrhage.
2.2 Management of vaginal bleeding as an obstetric danger signin the postnatal period.
Learning Activity 2.2
Observe the following image and try to think about the management of PPH
 a) To rescue the mother with severe vaginal bleeding, what do you think canAppropriate management of postpartum haemorrhage requires prompt diagnosis
a) To rescue the mother with severe vaginal bleeding, what do you think canAppropriate management of postpartum haemorrhage requires prompt diagnosis
be done to the patient?
b) After they finish rescuing the patient in critical condition, they have to
continue close monitoring, what do you think can be closely monitored?
c) What do you think about this condition in case blood transfusion may beneeded?
and treatment.
Massive transfusion protocols allow for rapid and appropriate response to
haemorrhages exceeding 1500ml of blood loss. However, blood transfusion is donein highly equipped health setting.
a. Initial management and resuscitation
Table 2.1: Initial management of PPH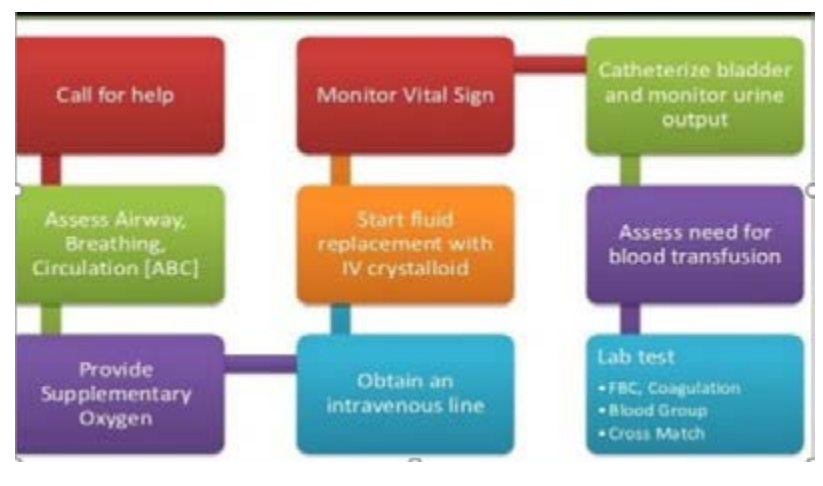
b. Management for uterine atony
Uterine Massage, bladder emptying + the following drugs
Table 2.2: Drugs used in uterine atony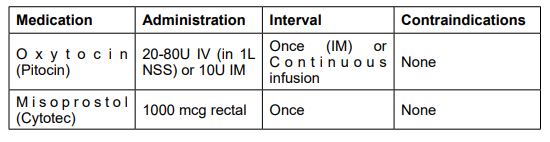
c. Management of other causes of vaginal bleedingTable 2.3: Management of causes of vaginal bleeding
d. Management of severe vaginal bleeding
The severe postpartum haemorrhage is managed through:• Transfusion of red blood cells, platelets and clotting factorse. After care
• Blood pressure vasopressor drugs to raise up blood pressure
• Uterine packing, aorta compression, balloon tamponade, and bimanualcompression of the uterus
• Monitor for ongoing blood loss (preferably quantitative measurement and vitalSelf-assessment 2.2
signs
• Assess for signs of anaemia (fatigue, shortness of breath, chest pain, lactation
problems.
• Frequently assess for bladder fullness• Report findings and hindrances met
1. What are the interventions that must be provided for initial
management of vaginal bleeding?
2. What drugs are used in management of PPH caused by uterine atony?3. Write PPH in full.
2.3 Complications and prevention of vaginal bleeding in postnatalperiod
Learning Activity 2.3
Read the following case study
24years old mother P2 delivered by spontaneous vaginal delivery, delivered
baby girl weighing 4.5kg in good condition, with in 1 hour of delivery mother
developed sudden gush of blood from the vagina. When the nurse arrived for
post-natal care realises that the uterus becomes soft, estimated amount of blood
loss is 1000mls by visual estimation.
a) What do you think about this scenario?b) What do you think about likely complications?
a) Complications of vaginal bleeding in the postnatal period
Vaginal bleeding after delivery has various complications to the mother including
but not limited to anaemia, dilutional coagulopathy, fatigue, myocardial disorders,
orthostatic hypotension, postpartum depression, anterior pituitary ischemia with
delay or failure of lactation (Sheehan syndrome or postpartum pituitary necrosis),hypovolemic shock when not detected and managed early.
b) Prevention of vaginal bleeding in the postnatal period
Postpartum haemorrhage to the mother is very critical but it can be prevented. The
following are preventive measures of postpartum haemorrhage from pregnancy,during labour and postpartum:
During pregnancy• Identification of risk factorsDuring labour
• Identification and treatment of maternal anaemia and iron deficiency during
antenatal care visit.
• Education of the mother to deliver in health setting area• Avoid routine unnecessary episiotomyAfter delivery
• Limit instrumented deliveries, especially forceps.
• Perform Active management of the third stage of labor (AMTSL) with controlled
cord traction (see the video on youtube.com), intramuscular oxytocin injection,and delivery of the placenta.
• Uterine massage and uterine retraction checking in first 6 hours postpartum
• Close blood loss amount checking
• Close monitoring of postpartum.
• Vital signs
• Emptying the bladder and avoid bladder fullness in first 6 hours postpartum• Ensuring rest of the other in first 6 hours postpartum
Self-assessment 2.3
1. What does it mean AMTSL?
2. What are the preventive measures of postpartum haemorrhage afterdelivery?
2.4 Assessment of the mother with seizures as an obstetric dangersign in postnatal period
Learning Activity 2.4
Read the following case study
A 32 years old mother presented at the accident and emergency department
on day 5 post normal delivery with a history of headache which is not relieved
by analgesics, her husband reports that she had one episode of convulsion at
home.
On arrival the vital signs revealed that BP was 178/114mmHg, pulse: 108beats
per minute, SPO2: 86% on room air and respiration rate: 18 breaths per minute.
After 10 minutes of arrival, she experienced another episode of convulsions
and these were characterised by generalised muscle spasms which terminated
spontaneously. There was no bowel or urinary incontinence during the episode.
a) After reading this case study, what do you think about this condition?
b) What do you think could be the reason of that convulsion?
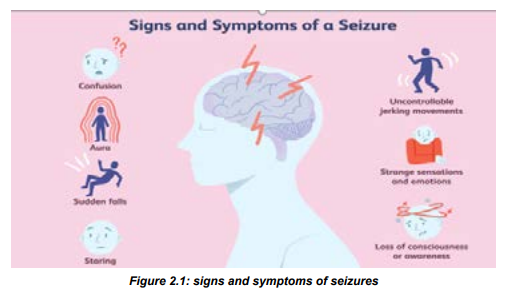
A seizure (the medical term for a fit or convulsion) is a burst of uncontrolled
electrical activity between brain cells (neurons or nerve cells) that causes temporary
abnormalities in muscle tone or movements (stiffness, twitching or limpness),
behaviours, sensations or states of awareness. Seizures may range from focal
(involve one area of your brain) or generalized (involve all areas of the brain). In
postpartum seizures are most common during the first 48 hours after delivery.
However, sudden seizures can come up at any time from delivery up to 6 weeks
after delivery.Symptoms of seizures in postnatal period
Postpartum seizures start from prodromal or early signs (Aura)that indicate that the
patient is going to enter in convulsion status. Those symptoms include:• Fear and anxiety
• Vertigo,
• Visual illusions, including flashing bright lights, spots, or wavy lines and• Nausea.
After aura, the mother may experience the followings:
• Uncontrolled convulsions,During a seizure, a woman with eclampsia has a type of seizure called a grand mal
• Rapid eye movements or staring,
• Sudden falling, stiffening of the body,
• Confusion,
• Uncontrolled convulsions,
• Loss of bladder or bowel control,
• Temporary stop in breathing,
• Entire body shaking,• Mood changes
seizure, which begins with a sudden loss of consciousness. Throughout the first 15
to 30 seconds of a seizure, the entire body stiffens as the muscles contract. The
back and neck arch. The woman may cry out as the vocal cords contract or may
turn blue if she is having difficulty breathing.
During the next 30 to 45 seconds, the muscles jerk, or convulse, in a rhythmic
pattern. While the muscles are jerking, the woman may bite her tongue or lose
bladder or bowel control. An entire seizure lasts 1 to 2 minutes or longer. After the
seizure, the woman will be unresponsive at first but will gradually wake up within
10 to 15 minutes. She may be sleepy, confused, or dazed. She may also feel tired,
weak, or moody and may have a headache and muscle aches for the next 24 hours.
Causes of seizures
Seizures are episodes of disturbed brain activity that cause changes in attention
or behavior. Among the causes of postnatal seizures are the following; toxemia of
pregnancy ( preeclampsia and eclampsia), drug abuse, epilepsy, high fever, head
injury, heart disease, stroke, poisoning, very high blood pressure, brain tumor.
Preeclampsia: is a pregnancy related complication characterized by high blood
pressure and signs of damage to another organ system, most often the liver and
kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in women whoseblood pressure had been normal.
Eclampsia: is the new onset of seizures or coma in a pregnant woman withpreeclampsia. These seizures are not related to an existing brain condition.
Table 2.4: Causes of postpartum seizures
Diagnosis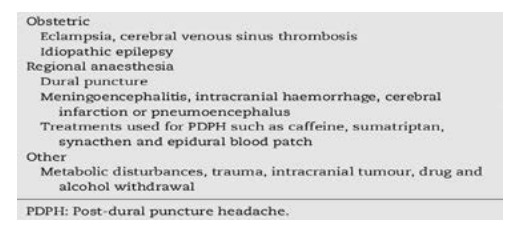
Seizures in postnatal period to the mother can be diagnosed according to the
following: Clinical manifestations, Routine blood tests, and urinalysis, Magnetic
resonance imaging (MRI) or computerized tomography (CT) scans in order to
evaluate your brain activity.
Preventive measures and management of seizures
An accurate diagnosis is important as many of these conditions are life-threatening
and require specific treatment. Convulsions in postpartum period should be treated
as eclampsia until proven otherwise. However, opportunities to identify other causes
of convulsions should be vigorously pursued.
If the mother has postpartum preeclampsia, the following treatments might be
prescribed: blood pressure lowering medicine (nifedipine), anti-seizure medicine,
such as magnesium sulfate.Self-assessment 2.4
1. Briefly state the risk factors of seizures in postpartum period.2. Identify 5 signs of seizures in postpartum period are
2.5 Nursing management of the mother with seizures in thepostnatal period
Learning Activity 2.5
Read the following case study and try to think about it.
I G is 30 years P4 in room 245 postpartum delivered by spontaneous vaginal
delivery with history of pre- eclampsia she delivered a baby boy in good condition
at 36 weeks of pregnancy, it’s now 3 hours, when nurse arrived in her room
noticed that mother is having convulsions.c) After reading this case study what do you think about it?While managing postpartum seizures, the first associate nurse ‘responsibility is tod) What do you think about this mother’s safety?
do the following:• Ensure the patient’ safety (it is one of the main considerations during seizure• Remember DRSABC: (Danger; Response; Send for help; Airway; Breathing;activity)
Circulation)
• Stay with the patient and call for help.
• Time the seizure and note its characteristics
• Protect the patient’s head, especially with any convulsive movements
occurring that may injure the patient.
• The nurse can protect the patient from harming themselves by placing
something soft under their head and shoulders.
• The surrounding area must be made clear to decrease the risk of injury,
however, do not try to physically restrict the movement of the patient’s limbs as
this can cause musculoskeletal damage, Do not put anything in the patient’s
mouth or attempt to move them.
• As soon as you are able to do so, roll the patient onto their side in the recovery
position to prevent aspiration due to excessive saliva production and ensure
their airway remains patent. If the patient has vomited or has food or fluids in
their mouth, it is crucial to do this immediately.
• Clean and clear the mouth and nose and provide oxygen
• Monitoring of vital signs is imperative, especially respiratory function.
• Following the seizure, manage any resulting injuries.
• Continue to monitor the patient’s airway, using suction as needed, and do not
disturb the patient if they fall sleep.
• When she wakes, calmly tell her where she is and she is safe.
• Provide reassurance, as this can understandably be quite distressing for the
patient
• Frequent monitoring of vital signs and neurological observations will need tobe performed in order to monitor the patient’s condition.
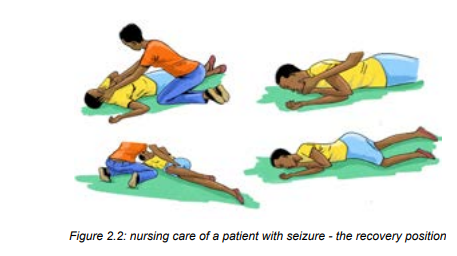
Self-assessment 2.5
1. What are the common causes of seizures in postnatal period?
2. Describe the nursing management of seizures in postnatal period.3. How should seizures in postpartum be treated?
2.6 Fast or difficult breathing as an obstetric danger sign in thepostnatal period
Learning Activity 2.6
 a) Basing to your observation, what do you think that can be one of theAcute dyspnea after delivery is a common symptom that can signify a wide variety
a) Basing to your observation, what do you think that can be one of theAcute dyspnea after delivery is a common symptom that can signify a wide variety
postnatal obstetric danger signs?
b) What do you think about the position that can be given to the mother with
difficulty of breathing in postpartum?
c) What do you think about oxygen administration to that mother?
of underlying etiologies.
Signs and symptoms of fast/ difficult breathing
A mother with fast breathing may present with some of the following signs andsymptoms:
• Increase in number of breaths/minute (it means that the person is havingCauses of fast or shortness of breath in postpartum period
trouble breathing or not getting enough oxygen.
• Skin color changes.
• Grunting or wheezing, and nasal flaring.
• Other signs accompanying shortness of breath include: coughing up blood,dizziness, and feeling faint.
Acute dyspnea after delivery is a common symptom that can signify variety of
underlying etiologies like: thromboembolism like thrombus and pulmonary embolism,
pulmonary edema, cardiomyopathy. I t can also be due to fluid accumulation in thelungs.
Diagnosis of difficulty in breathing in postnatal period
Clinical manifestations, laboratory investigations like FBC, Imaging like chest x-rayand CT scan.
Management of fast/ breathing difficulties
Position the mother in semi sitting position, monitor vital signs closely if the oxygen
saturation is below the 90%, the mother has to receive oxyenotherapy, encourage
the mother to perform regular breathing exercises. Request the mother to report
any breathing difficulties during this kind of exercise and manage according to thecause.
Self-assessment 2.6
1. What are signs and symptoms of fast breathing of a mother in postpartum
period?
2. What are the laboratory investigations that can be done?
3. Explain the management of fast breathing of a mother in postpartumperiod?
2.7 Pathogenesis, causes, symptoms and management ofpuerperal fever
Learning Activity 2.7
 a) By observing images above what do you think will be the condition?
a) By observing images above what do you think will be the condition?b) What do you think about this patient will present?
a. Pathogenesis
Postpartum fever (Puerperal fever) is defined as a temperature of 38.7 degrees
C (101.6 degrees F) or greater for the first 24 hours or greater than 38.0 degrees
C (100.4 degrees F) on any two of the first 10 days postpartum. It often results
from endometritis but can also be caused by urinary tract infection, wound infection
or phlebitis. The most common symptoms of postpartum illnesses are high fever
(21%), heavy vaginal bleeding (14%), and foul smelling vaginal discharge (10%),
and breast problems (18%).
b. Causes of fever in post-partum
The most common causes associated with postpartum fever are endometritis
(higher among patients who have a cesarean delivery, compared with those
who have a vaginal delivery), wound infections (e.g., surgical site infection),
and urinary tract infections, genital tract infection (painful inflamed perineum),
Mastitis(breast inflammation caused by nipple trauma and cellulitis) , deep venous
thrombosis(Painful, swollen calf), viral infection or chest infections.
c. Signs and symptoms of postpartum fever
Clinical manifestations of puerperal fever include; fever greater than 38 o
c, chills,
feelings of discomfort or illness, headache, loss of appetite, pain in the lower
abdomen or pelvis caused by a swollen uterus, foul-smelling vaginal discharge
In addition to fever, the following signs and symptoms should prompt urgent action
or urgent referral for hospital assessment by emergency ambulance:• Pyrexia (greater than or equal to 39°C).d) Management of fever in postpartum period
• Sustained tachycardia (≥90 beats/minute).
• Breathlessness (respiratory rate ≥20 breaths/minute).
• Abdominal or chest pain.
• Diarrhea and/or vomiting - may be due to endotoxins.
• Uterine or renal angle pain and tenderness.
• The woman is generally unwell or seems unduly anxious or distressed
Management and treatment of fever will depend on the cause.• Postpartum febrile episodes in which temperatures are less than 38.4 degrees
C (101.1 degrees F) often resolve without intervention, especially when they
occur in the first 24 hours after delivery.
• Treatment options for patients whose febrile episodes do not resolve
spontaneously or are higher than 38.7 degrees C (101.6 degrees F) during
the first 24 hours or higher than 38.0 degrees C (100.4 degrees F)
• General measures must be used: Ice packs may be helpful for pain from
perineal wounds or mastitis. Rest and adequate fluid intake are required,
particularly for mothers who are breastfeeding
• Pharmacological
• Administration of broad-spectrum antibiotics is recommended (Antibiotics
should be commenced after taking specimens and should not be delayeduntil the results are available).
Attention: Breastfeeding limits the use of some antimicrobials; hence, the advice of
a consultant should be sought at an early stage.Administration of antipyretic and analgesia may be required.
Self-assessment 2.7
1. What are the causes of fever to the mother in postpartum period?
2. What are the signs of fever to the mother in postpartum period?
3. Explain the possible management of fever to the mother in postpartumperiod?
2.8 Nursing intervention and prevention of puerperal fever
Learning Activity 2.8
Read the following case study and try to answer questions
MK 27 years readmitted in postpartum ward with temperature of 39.5oc on
D5 post caesarian section delivery, presenting chills loss of appetite and pain,
swelling S at surgical site, feeling un well and these symptoms started 3days
ago, her bay is well feeding on breast.
a) what do you think are interventions that an associate nurse must do for
that patients to relieve fever?b) what do you think can be the cause of fever to this mother in scenario?
Nursing intervention during puerperal fever• The associate nurse must play essential role in management of puerperal
fever. Therefore, the following are essential interventions and their rationale
for the associate nurse in management of puerperal fever:
• Review prenatal, intrapartum, and postpartum record. This helps to identify
factors that place client in high-risk category for development/spread of
postpartum infection.
• Demonstrate and maintain a strict hand-washing policy for staff, client, and
visitors. It helps prevent cross-contamination
• Instruct the proper disposal of contaminated linens, dressings, and peripads.
Maintain isolation, if indicated. It helps preventing the spread of infection
• Demonstrate correct perineal cleaning after voiding and defecation,
and frequent changing of peripads. Cleaning removes urinary/fecal
contaminants. Changing pad removes moist medium that favors bacterial
growth
• Demonstrate proper fundal massage. Enhances uterine contractility;
promotes involution and passage of any retained placental fragments
• Monitor temperature, pulse, and respirations. Note presence of chills
or reports of anorexia or malaise. Elevations in vital signs accompany
infection; fluctuations, or changes in symptoms, suggest alterations in client
status.
• Observe perineum/incision for other signs of infection (e.g., redness, edema,
ecchymosis, discharge and approximation [REEDA scale]). Allows early
identification and treatment; promotes resolution of infectionday. Note urine output, degree of hydration, and presence of nausea, vomiting,• Monitor oral/parenteral intake, stressing the need for at least 2000 ml fluid per
or diarrhea. Increased intake replaces losses and enhances circulating
volume, preventing dehydration and aiding in fever reduction.
• Encourage and or help the patient to be in semi-Fowler’s position. Enhances
flow of lochia and uterine/pelvic drainage.
• Promote early ambulation, balanced with adequate rest. Advance activity
as appropriate. It increases circulation; promotes clearing of respiratory
secretions and lochia drainage; enhances healing and general well-being.
Note: Presence of pelvic/femoral thrombophlebitis may require strict bed rest.
• Investigate reports of leg or chest pain. Note pallor, swelling, or stiffness
of lower extremity. These signs and symptoms are suggestive of
septic thrombus formation.
• Recommend that breastfeeding mother periodically check infant’s mouth for
presence of white patches. Oral thrush in the newborn is a common side effect
of maternal antibiotic therapy
• Instruct in proper medication use (e.g., with or without meals, take entire course
of antibiotic, as prescribed). Oral antibiotics may be continued after discharge.
Failure to complete medication may lead to relapse
• Discuss the importance of pelvic rest as appropriate (avoidance of douching,
tampons, and intercourse). Promotes healing and reduces the risk of
reinfection
• Ensure laboratory studies results are available. Helps identifying infectious
process/causative organism and appropriate treatment
• Encourage application of moist heat in the form of sitz baths and of dry heat
in the form of perineal lights for 15 min 2–4 times daily. Water promotes
cleansing. Heat dilates perineal blood vessels, increasing localized blood
flow and promotes healing.
• Demonstrate perineal application of antibiotic creams, as appropriate. It helps
eradicating local infectious organisms, reducing risk of spreading infection
• Administer medications as indicated (Antibiotics, oxytocics, such as Pitocin)• Arrange for transfer to intensive care setting as appropriate. May be necessary
for client with severe infection (e.g., peritonitis, sepsis) or pulmonary emboli.• Assist with procedures, such as incision and drainage (I&D) if necessary.
Prevention of puerperal fever
• Scrupulous attention to hygiene should be used during all examinations and
use of instrumentation during and after labour.Self-assessment 2.8• The use of prophylactic antibiotics during prolonged labour or caesarian• Any infection identified during pregnancy or labor should be treated
section should be done.
• Catheterization should be avoided where possible or should be done with
strict hygiene.
• Perineal wound should be cleaned and sutured as soon as possible after
delivery.
• All blood losses and the completeness of the placenta should be recorded at
all deliveries.
• Early mobilization of delivered mothers will help to protect against venous
thrombosis.
• New mothers should be helped to acquire the skills required for successful
hygiene, and breastfeeding in order to reduce the risk of mastitis and otherpossible infections.
1. Why the associate nurse must review prenatal, intrapartum, and postpartum2.9 Postpartum hypotension
record while managing puerperal fever?
2. Why the associate nurse must promote early ambulation, balanced with
adequate rest while managing puerperal fever.
3. Enumerate at least 5 measures that an associate nurse can do to preventpuerperal fever
Learning Activity 2.9
Read the following case study on one of the obstetric danger signs and try to think on it.
A 34 years old mother; Para 1, at 8 hours post normal delivery developed sudden
dizziness, generalised body weakness and feeling like going to faint while sitting on her
bed. Her vital signed showed that BP; 86/48mmHg, pulse; 118beats per minute, SPO2;
96%, body temperature; 36oC, respiration rate; 18 cycles per minute.
The associate nurse was told that the mother experienced unusual vaginal bleeding
2 hours post-delivery and the whole pamper was soaked unfortunately the bleeding
stopped after receiving misoprostol.a) What do you think to be the condition for this mother?After childbirth, the blood pressure remains about the same as it was during labour,
b) After reading this case study, what do you think can be the cause of the abovecondition?
and the pulse gradually decrease. A low blood pressure is helpful in diagnosing
potential complications such as hemorrhaging or spinal anesthesia complications.
Severe hypotension is related to shock. Shock occurs when vital organs do not
get the blood and oxygen they need to function properly. Severe hypotension, in
postnatal period can be life-threatening if not treated promptly. When the maternal
blood pressure suddenly drops in postnatal period, for whatever reason, it can havefrom short to long term harmful effects to the mother.
Signs and symptoms of hypotension
Signs and symptoms of postpartum hypotension include the following:• Severe lightheadedness when standingCauses of hypotension in postpartum period
• Dizziness.
• Feeling sick.
• Blurred vision.
• Generally feeling weak.
• Confusion.• Faintness
• Severe postpartum hemorrhageManagement of postnatal period hypotension
• Inadequate intake of fluids
• Severe nauseous and vomiting• spinal anesthesia
The management will depend on the underlying cause of hypotension. Treatment
could include:• medications for heart disease, diabetes, or infectionSelf-assessment 2.9
• Assist and encourage drinking plenty of water to avoid hypotension due to
dehydration
• Provision of IV fluids (normal saline)
• Blood transfusions in case of severe postpartum related to hypervolemia
caused by postpartum hemorrhage
• Encourage the patient to take salty food
• Taking and monitoring frequently blood pressure and pulse rate of the patient• Take safety measures to avoid risks for falling.
1. What are the signs and symptoms of hypotension in mothers during2.10 Assessment of the severe headache as an obstetric danger
postnatal period?
2. What are the causes of hypotension in mothers during postnatal period?
3. Explain briefly what will be done in case the postpartum hypotension isdiscovered to the mother
sign in the postnatal period.
Learning Activity 2.10
Look at the following picture and try to think on this obstetric danger sign.
 a) What do you think that can be the obstetric danger sign basing on thePostpartum headache or postnatal headaches refers to the appearance or increase
a) What do you think that can be the obstetric danger sign basing on thePostpartum headache or postnatal headaches refers to the appearance or increase
above image?b) What do you think about the link of above condition in postnatal period?
in headaches in women who have just had a baby, typically within the first six weeks
after they deliver. Headaches affect approximately 40% of women in the postpartum
period and are more common in women with a prior headache history, older age,
increased parity, or a shorter second stage of labor. Postnatal headaches areclosely linked to significant oestrogen and progesterone levels drop after delivery
Types of postpartum headaches
There are primary headaches and secondary headaches. Both can happen in the
postpartum period.
A primary headache is not caused by another condition. The pain can be hard to livewith, but the headache is not dangerous. In in this headache, the brain can’t sense
pain, the pain felt by the client is caused by swelling in blood vessels, muscles, and
nerves of the neck and head. Primary headaches are divided into:• Migraines: Typically felt on one side of the head and they cause throbbingA secondary headache is more serious. They usually come from underlying condition
pain, nausea, and sensitivity to light, noise, and smells.
• Tension headache: This usually includes the pain on both sides and sometimes
sensitivity to light and sound.
• Cluster headache: Often felt on one side of your head, behind one eye. It can
happen at the same time of day for several weeks.
• Hypnic headache: This occurs at night, typically in people between the agesof 40 and 80.
cause severe pain. They trigger pain in your neck and head, like; Head injury, Neckinjury; Brain infection; Brain tumor; High blood pressure; Aneurysm; etc.
Causes and risk factors of postpartum headaches
Almost half of all women have a headache in the first few weeks after they give birth
to their baby, and it’s especially common in the first week. Causes of postpartum
headaches include: A sharp drop in hormones, Not enough fluids, Not eating
enough, Not enough sleep, Muscle tension from pushing out your baby, High
blood pressure, Preeclampsia (high blood pressure in pregnancy), Sinus infection,
Blood clot, Major bleeding, Having an epidural or spinal anesthesia, cortical veinthrombosis, some medications, caffeine withdrawal.
Patterns of headaches to be reported immediately
Although headaches are a relatively common occurrence in postnatal period, the
following are patterns of headache that should be reported immediately to the
senior or transferred to high level of care: are severe, peak in intensity after a short
period of time, are accompanied by other concerning symptoms like fever, neck
stiffness, nausea or vomiting, visual changes, or cognitive problems, change over
time or when the patient moves into a different position, wake the patient up fromsleep, occur after physical activity
In addition, the sharp drop in estrogen and progesterone levels after delivery can
also cause postpartum night sweats. A combination of hormone changes, waterloss from sweating, and not enough sleep can cause a postpartum headache.
Women with headaches before being pregnant, older, or have had many births, arealso at risk of having a postpartum headache.
Self-assessment 2.10
1. What are the causes of headache to the mothers in postpartum period?
2. Explain the types of headache to the mothers in postpartum period.3. What are the mothers that are more likely to have postpartum headache?
2.11 Management and prevention of postpartum headaches
Learning Activity 2.11Read the case and answer questions in the box
a. What do you think that can be the treatment of her headaches?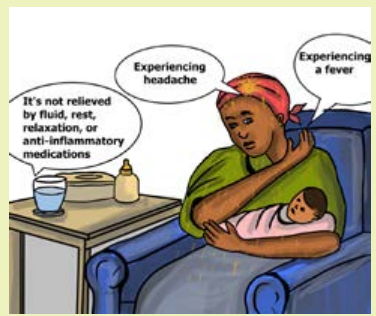
b. What do you think can be done to prevent this headache for next time tothis mother?
Management of postpartum headaches
Management of postpartum headaches varies and most of the time depend on
severity and cause the headache. In addition, most often, postpartum headaches
can treat at home. But, more severe secondary headaches should be seen by the
doctor immediately and may require a higher level of treatment to prevent moreserious symptoms or complications from occurring.
Tension and migraine headaches can be treated with over-the-counter non steroidal
anti-inflammatories, such as naproxen (Aleve) and ibuprofen (Advil). Most of these
are safe to take while breastfeeding, with the exception of aspirin. Beyond analgesia,
the bed rest and intravenous hydration, and caffeine supplementation are also
methods of management of postpartum headaches in health setting area. Patients
who do not respond to the treatment within 48 hours require a quick transfer to thesuperior level of care.
The treatment of secondary causes of headache in the postpartum period often
requires collaboration with consulting services both for acute management and risk
factor modification. Headaches caused by preeclampsia resolve with treatment
of the condition, including initiation of magnesium sulfate and anti-hypertensive
medications and admission to an obstetrics service for monitoring.
Ischemic and thrombolytic related headache the management will be done with
the aid of the cardiologist and neurologist. For puerperal stress related headache,
the management can be done through psychological counseling and relationtechniques.
Prevention of postpartum headache
For the side of health care provider:• Prompt recognition of vital sign abnormalities and risk factors assessmentTaking of self-care is an important way to prevent tension and migraine headaches.
by nursing and immediate physician notification can help reduce delays in
diagnosis or misdiagnosis.
• Identification of social stressors contributing to or causing the patient’s
presentation with subsequent referral to case management professionals or
social support services prevent bounce-back visits and readmission.
• Recognition of traumatic causes of headache by members of the healthcare
team can lead to a referral to resources for safe-houses .
• Assisting the patient to get enough and adequate fluids and food can help
reducing risks of postpartum headaches.For the side of the patient
Here are some tips to teach the patient for preventing the occurrence of primary
headaches:• Get enough rest: Try to take naps when the baby naps and ask the partner or
a friend to watch over the baby between feedings.
• Drink plenty of fluid: Put a large water bottle around or make sure you have a
glass of water by your side.• Eat healthy foods regularly: Stock the refrigerator and pantry with nutritiousSelf-assessment 2.11
foods that are convenient to prepare and eat.
• Try to relax in order to reduce stress: Take an easy walk, read a book, or chatwith a friend to alleviate stress.
1. Explain briefly the management of puerperal headaches.2.12 Blurred vision as an obstetric danger sign in the postnatal
2. What are the tips of education that can the associate nurse teach thepatient in order to prevent puerperal headaches?
period
Learning Activity 2.12
Read the following case study for the mother with postnatal obstetric danger
sign.
A 26 years old mother arrived at accident and emergency department at 8th day
of postpartum period. This mother delivered by c/section and on arrival, she was
complaining of severe headache, unable to see variety of things clearly, during
assessment, the associate nurse asked this mother to state what he was holding
in his hand and the mother responded that she was not seeing it clearly. Then he
rushes to take vital signs of this mother; the findings were: BP: 154/102 mmHg,
Pulse rate: 101 beats/ minute, respiration: 20 cycles, body temperature: 36.2 o
c,
oxygen saturation: 98%, pain score: 3/10.a) After reading the scenario above, what do you think about this motherPhysiology of vision after delivery
condition?b) What do you think can be done to this mother?
A woman’s body goes through a lot of changes during and after pregnancy, and
hormones are responsible for these changes. One such change that most new
mothers would notice is related to their vision. The changing levels of hormones and
fluids within the body can cause changes in vision. About fifty percent of pregnant
women are prone to these changes. Changes in vision become more prominent
in the second trimester and postpartum. Hormonal changes can also lead to dry
eyes after pregnancy. Most of the changes abate the vision and the vision becomenormal after a few months of childbirth.
Postpartum blurred vision is defined as a type of vision impairment that affects
the sharpness or focus of an image and experience a decreased clarity in vision
after delivery. The frequency of blurred vision depends on the underlying cause and
may only occur in certain situations. The intensity also varies and can be unilateral
or bilateral with other visual distortions.Causes of blurred vision in postpartum period
Postpartum blurred vision is caused by hormonal changes after delivery. However,
it may also be due to a cause not related to pregnancy or postpartum changes. The
following are some causes or risk factors of postpartum blurred vision:• Preeclampsia (Due to high blood pressure, there is CNS irritation or cerebralSymptoms of blurred vision in postpartum period
edema which result in blurred vision)
• Gestational diabetes (due to diabetes, the blood vessels attached to the
retina may get damaged. This affect the eyesight and cause blurred vision)
• Pituitary Adenoma (tumor in the pituitary gland of the women may alter the
functioning of the hormone secretion and lead to vision problems)
• Lower Fluid Retention (After delivery, the fluid retention capacity of a woman’s
eye ducts lowers. This can alter the shape of the cornea, leading to blurred
or distorted vision).• Certain medications
The symptoms of postpartum vision loss or eye problems include:• Sensitivity to light: Bright lights may irritate the eyes.Management of blurred vision
• Dizziness: Blurred vision may lead to a feeling of dizziness and nausea.
• Double vision: Outlines may seem blurred and the mother might see images
overlapping.
• Intermittent blur: This can happen occasionally, where certain things, like
road signs, appear blurred.
• Strain on eyes: The eyes will feel tired and stressed all the time.
• Flashes and floaters: Bright flashes of light or wavy lines in the sight of the
vision and may appear due to retinal detachment, caused by strained pushingduring labour.
Postpartum vision problems rarely cause permanent vision changes after pregnancy.
Many of the changes can go back to normal a few months after the baby is born.
But, in a few women, this warrants a new prescription, due to permanent changes
in vision.
Despite best way to manage blurred vision is to avoid triggers and making
some simple changes can make vision clear again, the following are some tips of
postpartum blurred vision management.
For Dry Eyes
Dry eyes can be one of the main reasons for blurred vision. saline drops, like the
ones used by contact lens users.
For Blurred Vision
Blurred vision often abates after pregnancy, but if it continues, refer the patient to
the ophthalmologist to get eyes tested.
For Preeclampsia.
It is important to send the patient to the gynecologist to keep blood pressure
managed
For Gestational Diabetes.
The first step is to switch to a healthy diet and lifestyle to avoid the risk factors of
gestational diabetes. If you already have high sugar levels, the gynecologist can
prescribe medications to keep it under control.
Regardless of the cause, informing and teaching about postpartum blurred vision,it is the best way to deal with the problem.
Self-assessment 2.12
1. Define the term postpartum blurred vision2. Enumerate the symptoms of blurred vision in postnatal period.
2.13 Assessment of the signs of deep vein thrombosis (DVT) as anobstetric danger sign in the postnatal period.
Learning Activity 2.13
Observe the following images and start thinking on the postnatal obstetricdanger signs that this mother may present.
a) From your observation, what do you think that this mother is suffering from?
b) Have you ever come in contact with condition like this?
Deep vein thrombosis (DVT),is the development of a blood clot in a deep vein.
blood clots occur in a deep vein of the leg, calf or pelvis. 90% of DVTs occur in the
left leg. Deep venous thrombosis (DVT) during pregnancy is associated with high
mortality, morbidity, and costs. The risk of developing blood clots (thrombophlebitis)
is increased for about 6 to 8 weeks after delivery. Pulmonary embolism (PE), is
the most feared complication, and it is the leading cause of maternal death in the
developed world. Other complications include post-thrombotic syndrome, chronic
venous insufficiency, and vein valve destruction.
Pathogenesis of DVT
Pregnancy is a prothrombotic state; it has all components of Virchow’s triad: venous
stasis, endothelial damage and hypercoagulability. Thus, during normal pregnancy,
a hypercoagulable state is initiated. This is the most important risk factor contributing
to thrombosis (DVT after delivery). Pulmonary embolism results from the blood
clots that breaks, loose and travels through the bloodstream into the lungs, where itlodges in a blood vessel in the lung and blocks the blood lung’s flow.
DVT risk factors
The risk for DVT increases in the postpartum period. Factors that increase the risk
of developing DVT in the postpartum period include:• Cesarean sectionSigns and symptoms of deep vein thrombosis (DVT) during postpartum
• Stillbirth
• High blood pressure (hypertension)
• Eclampsia or preeclampsia
• Postpartum infection
• Obstetric hemorrhage
• Preterm delivery at less than 36 weeks
• Other underlying medical conditions (diabetes, infections, pre-eclampsia, etc)
• BMI (body mass index) of 25 or greater
• Over 35 years of age
• Smoking
• BMI of 25 or greater
• Over 35 years of age• Smoking
The most common symptoms of deep vein thrombosis during pregnancy and
postpartum usually occur in just one leg and include:• A heavy or painful feeling in the leg (a lot of people say that it feels like a really
bad pulled muscle that doesn’t go away)
• Calf or thigh is painful, tender to the touch, warm, and swollen.
• redness in the calf or thigh
• Slight to severe swelling of the calf or thigh
• A fever that develops after delivery may be caused by a blood clot.• A blood clot in the pelvis may not cause symptoms.
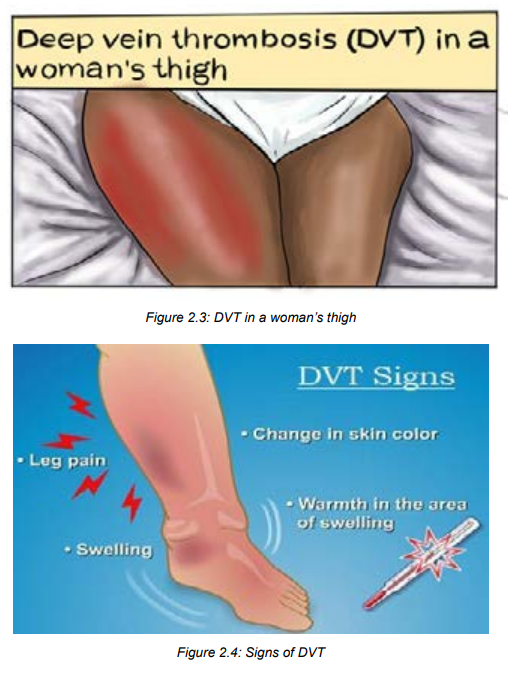
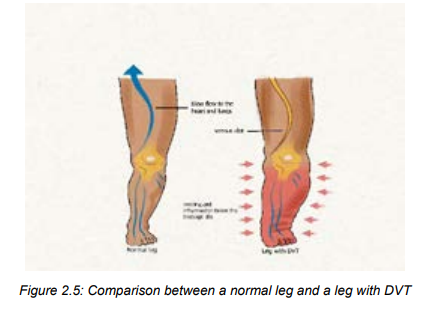
Self-assessment 2.13
1. Define the term deep vein thrombosis.2. What are the signs of deep vein thrombosis?
2.14 Nursing management of deep vein thrombosis as an obstetric
danger sign in the postnatal period.
Learning Activity 2.14
Read the following case study and start thinking on the management, preventionand nursing interventions that can be done
During puerperium period following caesarean section in a referral teaching hospital,
a woman a DVT with superficial blood clots diagnosis was made after finding that that
patient had unilateral leg oedema and pelvic and lower left limb pain The attending
obstetrician on duty started to tell the nurse on shift that the DVT management must be
initiated immediately. In addition, the Doctor told to that nurse that the other patient who
was lying at the opposite bed was at risk of developing DVT too. Then, the nurse was
asked to remain vigilant and start doing preventive measures to that other patient.
Based on the scenario described abovea) What do you think can be done to that mother to attenuate the pain, oedema andManagement of postpartum DVT
blood clot?
b) What do you think can be done to prevent the occurrence of DVT to that mother
lying in the opposite bed?
Early assessment of DVT risks factors and complications and prompt treatment
can keep a clot from breaking off and traveling through the circulatory system to the
lungs (pulmonary embolism). PE is the life-threatening in postpartum period.• For superficial blood clots: The associate nurse can apply warm compresses,Prevention of deep vein thrombosis
compression bandages, and elevation of the limb.
• For deep vein thrombosis or pulmonary embolism: At hospital the gynecologist
and cardiologist prescribe drugs such as: Heparin (subcutaneous) or Warfarin
Among the preventive measures for clots and deep vein thrombosis, keep the blood
flow in the following ways:• Getting plenty of pregnancy-safe exercise.Nursing interventions in management and prevention of DVT
• Encourage early ambulation
• Walking and stretching if the mother has been sitting for more than two to
three hours
• Moving the legs while the mother is sitting (elevates and lowers the heels and
then the toes).
• Taking extra precautions when the mother is on travel, including drinking lots
of water, getting up frequently to walk (or stretching the legs from a seated
position).
• Use of anti-embolism stockings for those women at risk• Encourage the woman not to smoke
The goal of nursing care for a client with postpartum DVT include enhance tissue
perfusion, facilitate resolution of thrombus, promote optimal comfort, preventcomplications and provide information and emotional support.
The following are nursing care interventions to manage and prevent
postpartum DVT:• Monitor capillary refill time; Assess for positive Homans’ sign (calf pain at
dorsiflexion of the foot)
• Assess circulation, asymmetry, sensory and motor function of extremity;
Observe edema from groin to foot; Measure and record calf/thigh circumference
of both legs as appropriate. Report proximal progression of inflammation,
traveling pain.
• Assess respiration and auscultate for lung sounds, noting crackles or friction
rub.• Investigate reports of chest pain or feelings of anxiety.
• Instruct client to avoid massaging or rubbing the affected extremity. Instruct
client to avoid massaging or rubbing the affected extremity.
• Maintain bed rest with elevation of feet and lower legs in above heart level
during the acute phase.
• Elevate client’s legs when resting or sitting in a chair. Elevate client’s legs
when resting or sitting in a chair. Elevate client’s legs when resting or sitting
in a chair.
• Instruct client to avoid crossing the legs or wear constrictive clothing. Instruct
client to avoid crossing the legs or wear constrictive clothing.
• Encourage increased fluid intake of 2500 ml/day unless contraindicated
• Emphasize the importance of deep-breathing exercises.
• Facilitate and assist with active or passive (Range of motion) ROM while on
bed rest; Assist with gradual resumption of ambulation as advised.
• Apply warm, moist compresses or heating pad to affected extremity as
ordered.
• Apply elastic support hose. Caution is advised to prevent a tourniquet effect.• Apply mechanical devices such as sequential compression stockings,Self-assessment 2.14
thromboembolic (TED) stockings as indicated.
• Monitor laboratory studies
• Administer medication as indicated• Prepare client for surgical intervention as indicated.
1. What intervention will the associate nurse do if the the superficial blood
clots are detected in postpartum?
2. How the mother moves the legs while in sitting in order to prevent
postpartum DVT?3. Enumerate at least 4 ways that can be used to prevent Postpartum DVT
2.15End unit assessment for unit 2
End of unit assessment
SECTION A
Multiple choice questions.
4. The following statements defines postpartum hemorrhage excepta) Bleeding of 350mls- 500mls following vaginal delivery and 850mls-1000mls
post caesarian section.
b) Bleeding more than 500mls following vaginal delivery and 1000mls
following Caesarean section in the first 24 hours following birth.
c) Blood loss sufficient to cause hemodynamic instability in the first 24 hours
following birth.d) A and C.2. Among the causes of postpartum heamorrhage known as 4Ts the
fallowing are not correct except.a) Tone (70%), Trauma (30%), Tissue (10%) and Thrombin (1%)3. The following are not medications used in prevention of convulsions
b) Tone (70%), Trauma (20%), Tissue (9%) and Thrombin (1%)
c) Tone (70%), Trauma (20%), Tissue (10%) and Thrombin (1%) .
d) A and C.
except.a) Nifedipine4. Acute dyspnea after delivery is a common symptom that can signify variety
b) Aldomet
c) Magnesium sulphate
d) Adalate
of underlying etiologies and can lead to low oxygen supply in the blood .
so the following measures shows you when to administer oxygen, pic the
correct answer.a) oxygen saturation of 95%5. The risk factors of postpartum hemorrhage are grouped into 2(ante natal
b) oxygen saturation of less than 90%
c) oxygen saturation of more than 90%
d) oxygen saturation of 92-94%
risk factors and intrapartum risk factors) so the following are antenatal risk
factors except.a) Antepartum haemorrhag6. The most feared complication of the Deep Venous thrombosis (DVT):
b) Previous macrosomic baby above 4500g
c) Incomplete 3 rd stage of labor.
d) Polyhyramnios.a) DeathANSWER THE FOLLOWING STATEMENTS BY TRUE OR FALSE.
b) Pulmonary embolism (PE)
c) Chronic venous insufficiency
d) Vein valve destruction.
7. Bleeding disorder occurs when there is a failure of clotting is called embolism.
8. Sheehan syndrome is defined as postpartum pituitary necrosis secondary to
postpartum hemorrhaged.
9. The type of headache typically felt on one side of the head and they cause
throbbing pain, nausea, and sensitivity to light, noise, and smells is called
Tension headache.
10. The type of headache characterized the pain on both sides and sometimes
sensitivity to light and sound is called Migraine headache.
11. The type of headache often felt on one side of your head, behind one eye iscalled Cluster headache.
SECTION B: Short answer questions.
12. Define the term postpartum blurred vision.
13. Describe general measures to be used while managing puerperal fever
14. Describe the pharmacological method while managing puerperal fever
15. In assessing puerperal fever for the mother, what are the signs and symptoms
that should prompt urgent action or urgent referral for hospital assessment?
16. What will the associate nurse suspect if he/she finds the blood pressure of
60/30 mmHg associated with severe lightheadedness and vomiting? The blood
loss amount after delivery is < 500ml and a caesarian section was done to the
mother.
17. Explain Flashes and floaters
18. What is the cause of Flashes and floaters?
19. Why the associate nurse must monitor oral/parenteral intake, assessing the
need for at least 2000 ml fluid per day?
20. Enumerate at least 5 interventions that the associate nurse can do in
management and prevention of postpartum DVT.
UNIT 3: NEW BORN DANGER SIGNS
Key Unit Competence:
Detect, manage and refer a newborn with danger
Introductory activity 3.0Observe the following pictures showing the new born danger signs and reflect on them.
From the observation of the above mentioned images;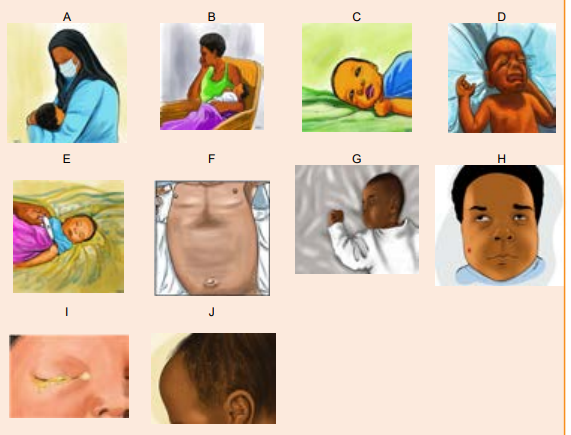
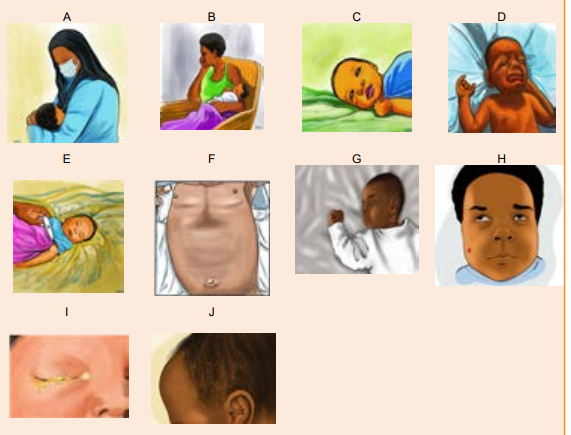 a) Which danger sign do you think image A is showing?3.1 General assessment of the New born danger signs.
a) Which danger sign do you think image A is showing?3.1 General assessment of the New born danger signs.
b) Which danger sign do you think image B is showing?
c) Which danger sign do you think image C is showing?
d) Which danger sign do you think image D is showing?
e) Which danger sign do you think image E is showing?
f) Which danger sign do you think image F is showing?
g) Which danger sign do you think image G is showing?
h) Which danger sign do you think image H is showing?
i) Which danger sign do you think image I is showing?
j) Which danger sign do you think image J Is showing?
Learning Activity 3.1
12 hours old female newborn found to be having difficult in breathing with
respiratory rate of 70 movements /min, axillary temperature of 34 , hypotonic,
unable to breastfeed but the health care provider observed that the baby has
breastfeed well earlier as reported by the mother, baby’s birth weight is 2.2kg
and born at 3 weeks before term.a) What do you think about the cause of difficult in breathing?Newborn danger signs are the clinical signs that indicate a high risk of neonatal
b) What do you think that can be the cause of unable to breast feed?c) What do you think can cause very low body temperature to this newborn?
morbidity and mortality and require immediate therapeutic interventions. They are
also signs that show the neonate is sick. Early identification by the nurse and the
parents is an important step toward improving newborn survival. The World Health
Organization (WHO) described nine neonatal danger signs which includes not
able to feed or stopped feeding well, convulsions, fast breathing, severe chest indrawing,
fever, hypothermia, yellow soles, movement only when stimulated or no
movement, and signs of local infection (umbilicus red or draining pus, skin infection,
or eyes draining with pus.or eyes draining with pus.
The neonatal period is the first four weeks of an infant’s life, whether the baby was
carried to term or born prematurely. It’s a time of rapid change and development
where patterns for infancy, like feeding and bonding, are developed.
Danger signs in the neonatal period (0–28 days) are non-specific and that indicates
severe illness. They are used in integrated management of neonatal and childillness (IMNCI) by practitioners to identify children who need medical care.
It has been noted that one-third of all neonatal deaths occur on the first day of life,
almost half within 3 days and nearly three-quarters within the first week of life.
Therefore, effective strategies to improve newborn survival in developing countries
require a clear understanding of the patterns and determinants of newborn-care
seeking by mothers, families and other newborn caregivers.
Improving families’ care-seeking behavior is one of the important strategies to
reduce child death in developing nations. The WHO estimates that seeking prompt
and appropriate care could reduce child mortality due to acute respiratory infections
by 20%.An important method to reduce newborn death is early recognition of NDSsand the provision of quality of curative health services for sick newborns.
The majority of neonatal deaths in developing countries occur at home. Many of
these deaths are related to late recognition of the signs of a serious illness by
parents and a delay in the decision to seek medical care. Since the health-seeking
behaviour of mothers for neonatal care depends on the mothers’ knowledge
Although many babies will have a healthy birth and will breathe easily and begin
feeding soon after being placed on the mother’s breast, other babies will have a
range of needs, some urgent, in order to ensure their safety and wellbeing.
It is very important to assess the new-born for the danger signs in order to take
actions to help the newborn are crucial to ensure prompt and safe care. Mothers
should be taught to look for these signs in the newborn and advised to seek earlymedical care if they observe any one of the danger signs.
Self-assessment 3.1
1) Define neonatal period?
2) What does it mean new born danger signs?3) Where does the majority of neonatal death occur in developing countries?
3.2 Respiratory problems in newborns and hypoxiaLearning Activity 3.2
Observe and compare the pictures above that show 2 neonate’ respiratory
features;a) Reflect on the difference between the 2 new borns.Respiratory disorders in newborns are conditions characterized by abnormal
b) Characterize the baby A mouth and the baby B mouth
c) Close your nose and stop breathing in, how will you manage to try breathing?
d) Characterize and reflect on the baby A chest and the baby B cheste) What should happen if the baby is not receiving enough Oxygen?
respiratory rate (RR), increased work of breathing that result in hypoxia.
Abnormal respiratory rate (RR)
The newborn presents a breathing that is abnormally rapid and often shallow known
as Tachypnea with a respiratory rate > 60breaths/minute or a slow respiratory rate
< 30breaths/minute called Bradypnea. Dramatically the baby can cease breathing
for a period > 20 seconds or less when associated with bradycardia or cyanosis this
is known as apnea.
Breathing less than or equal to 30 or more than or equal to 60 breaths per minute,grunting, severe chest in drawing, blue tongue and lips, or gasping.
Increased work of breathing
A newborn with respiratory distress struggles to breathe and exhales against
a partially closed glottis this produces a sound termed as grunting. This effort
causes widening of nostrils when breathing in, called nasal flaring and the chest
undergoes a marked inward movements of the muscles between the ribs during
inspiration. This is termed as chest retraction (chest indrawing).
Classification of respiratory disorders:
Mild
Physical Examination:• Minimal grunting on expiration, flaring and retractionsModerate to severe• Vital Signs: RR in 60–70, Oxygen saturation >90%
Physical Examination:
Moderate to severe grunting, flaring, retractionsVital Signs: RR > 70 or < 30 or saturation <90%
The role of the associate nurse in the management of respiratory distress in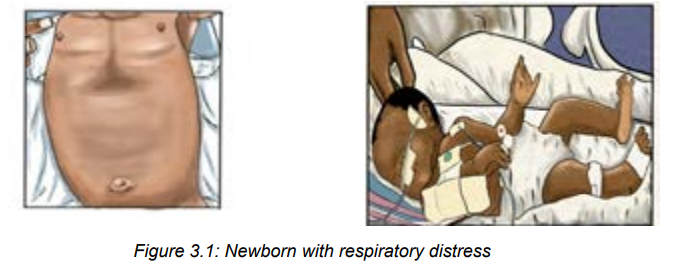
neonates
Most neonates with respiratory distress can be treated with respiratory support
and noninvasive methods. Oxygen can be provided via bag/mask, nasal
cannula, oxygen hood, and nasal continuous positive airway pressure. Ventilatorsupport may be used in more severe cases.
A baby in respiratory distress needs to be resuscitated and the associate nurse will
first call for help from experienced caregivers and following actions will be done:• Immediately resuscitate the newborn using current guidelinesSelf-assessment 3.2
• Stabilize and admit to neonatal unit
• Monitor Vital signs with focus on respiratory rate and oxygen saturation
frequently.
• Initial evaluation includes a detailed history and physical examination. The
clinician should monitor vital signs and measure oxygen saturation with pulse
oximetry.
• The blood gas measurement may be considered;
• Lab exams (Full blood count)
• Take pulse oximetry after 24 hours but before hospital discharge to screen for
any critical congenital heart
• Always assess for cyanosis
• Assess for feeding or nutrition possibilities
• Avoid hypothermia1) Explain the respiratory problems in new born.3.3 Breastfeeding /feeding disorders (inability to breastfeed/poor
2) Identify the respiratory rate deviation in the new born.
3) What is the grunting in abnormal work of breathing of a new born?
4) The term hypoxia is often used in respiratory patterns; how can it bedefined?
feeding)
Learning Activity 3.3
A student mother comes to the health facility with her 3weeks baby because 2
days ago baby stopped to nurse, the baby is crying for hunger but cannot suck
and the mother prefers to use a bottle. As an associate nurse:a) Reflect on why the breast milk is the best aliment of the baby?
b) What do you think about the causes that can interrupt breastfeeding onthe neonate?
A change in behavior may be one of the first signs of illness in a newborn. It’s
normal for a baby’s activity, appetite, and cries to vary from day to day, even hour to
hour. But a distinct change in any of these areas may signal illness.
Exclusive breastfeeding is strongly recommended for the first six months. The
healthy newborn does not need water, other fluids, or foods during this time.
Mother’s milk is healthy because it contains antibodies that actively protects
against infection and allergies. Newborn who are not breastfed become sick and
may die from hypoglycemia, neonatal jaundice, and infections such as diarrhea,
gastrointestinal infections. Baby cannot suck due to newborn itself or from maternalcauses.
Poor sucking; In a term baby who was feeding earlier ® indicates neonatal illness
(as perceived by mother). In a preterm baby ® needs careful assessment because
it may be due to cold stress or immaturity.
In case the baby refuses or misses several feedings due to that she/he is having
trouble of sucking at breast or bottle, doesn’t seem to be hungry, is having problems
spitting up, or is losing weight, that is a sign of illness. Immediate attention must be
taken.
If the baby is bottle-fed, a weak suck may require the bottle nipple to be “worked”
or pumped to stimulate a suck. Either type of feeding, whether by breast or bottle,
may take a very long time often longer than 45 minutes.
Spitting up and dribbling milk with burps or after feedings is fairly common in
new-borns. This is because the sphincter muscle between the stomach and the
oesophagus (the tube from the mouth to stomach) is weak and immature. However,
forceful or projectile vomiting, or spitting up large amounts of milk after most
feedings, can indicate a problem. If the baby is formula-fed, vomiting may occur
after overfeeding or because of intolerance to formula. If the baby is breastfed or
formula-fed, he or she may have a physical condition that prevents normal digestionand may cause vomiting.
Causes and factors associated with new born inability to feed/breast
feeding;• The baby is sick from a general illness or abdominal distentionManagement of the new born with inability to feed/poor feeding:
• Preterm babies due to immature or the absence of sucking reflex
• New born who have congenital malformations ex: cleft palate and lips.
There are a few reasons that a neonate baby may not be feeding enough/ unable
to feed such as a tongue-tie, blocked nose, stomach flu, illness or being born
prematurely. However, regardless of the reason, if the newborn is not feeding
normally, a neonatologist or neonatal care specialist must be called, especially if
the baby is sleepy and dull. This can be a sign of illness, infection or low bloodsugar.
The following techniques have proven helpful for babies refusing the breast/
unable to feed:• The first choice to feed a non-nursing baby is the mother’s own milk. The
second choice is banked breast milk from mother and the third choice
is formula if possible.
• Very careful, supportive positioning can be very helpful when the baby is
having breastfeeding issues. For example, a cross-cradle hold or modified
football hold can be useful. Make sure the baby’s head is at a higher level
than the rest of their body. If the baby is tolerating it, then work on latching
for up to 10 minutes or so. If the neonate is getting upset, then go with
shorter sessions. It is not a good idea to keep trying for more than about 10
minutes. The baby may get tired and latching will be harder. In addition, the
baby may be at risk of here is a risk of developing breastfeeding aversion ifyou persist too much.
• Continue to offer expressed mother’s milk, banked milk, formula for short
times, but gradually help the mother to put the baby on closer and closer to
the nursing position, skin-to-skin, etc.
• Educate and help the mother to wear clothing that allows very easy access
to the breasts. Baby may get very impatient in the split-second that it takes
a mother to lift her blouse and undo her bra. Tell the mother to spend time, if
possible, in a warm place that allows both mother and baby to be naked fromthe waist up.
• Educate the mother to offer the breast often. Try breastfeeding in baby’s
favourite place, in favourite position, in the bath, while walking around, while
lying down, with the baby being in upright, with baby being flat on their back
position.
• If the neonate is completely unable to feed or vomit all the times, it is an
emergency and parenteral feedings must be considered at an advanced
health setting through Nasogastric tube.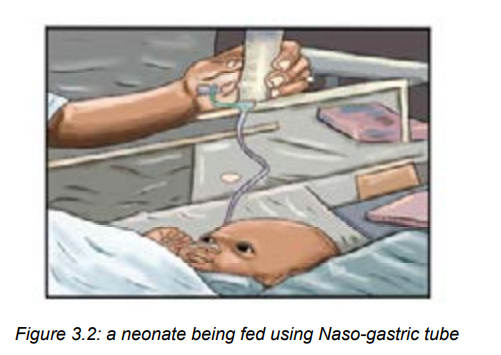
Self-assessment 3.3
1. Poor sucking in a baby who was feeding well earlier indicates the following
except one:
a) Neonatal illness
b) It is a preterm baby it may be due to cold stress or immaturity.
c) Maternal causes
d) Congenital malformations
2. What does spitting up and dribbling milk with burps or after feedings means
to the neonate
3. What does a forceful or projectile vomiting, or spitting up large amounts ofmilk after most feedings means to the neonate?
3.4 Lethargy/ Hypotonia
Learning Activity 3.4
A 2-day old term male infant was found too sleepy and with few movement and
sometimes refuse to breastfeed.a) What do you reflect is this situation?Lethargy is the pathological state of sleepiness or deep unresponsiveness. It
b) What do you think that could be the cause of this new born’s hypotonic?
may be a sign of infection or other conditions such as low blood sugar. If neonate
becomes lethargic or is not as active, inactivity, so it’s necessary to seek medical
care as soon as possible.
Lethargy is noticed when the neonate seems to have little or no energy, is drowsy
or sluggish, or is sleeping longer than usual. He or she may be hard to wake for
feedings, and won’t be alert or attentive to sounds and visual stimulation. Sometimes
this develops slowly, so the gradual change will be noticed. Lethargy may be a sign
of infection, anemia, low blood sugar or hypoxic ischemic encephalopathy (HIE)
and it is among neonatal emergency.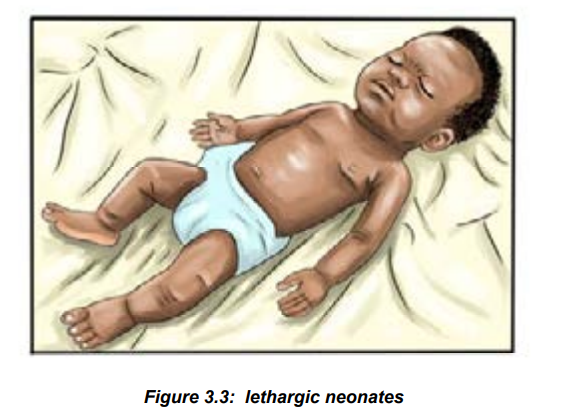
Nursing management of hypotonic/lethargy in the neonate:• Initial management should be focused on stabilizing the infant and then
evaluate the most likely causes of illness.• start with evaluation for hypoglycemia and sepsis and provide respiratory1) Define term lethargy?
support.
• Take laboratory samples for checking blood glucose and FBC to rule out
infection and anemia
• Take and monitor closely vital signs• Manage and care the neonate according to the cause of hypotonia.
Self-assessment 3.4
2) What can be done initially when noticed that the neonate is lethargic?3) State 3 causes of lethargy in new borns.
PROBLEM OF THERMOREGULATION
3.5 Neonatal hypothermiaLearning Activity 3.5
A 5-day old male term new born is bathed in a cold ward. Afterwards the new born
appears not well, has rapid breathing, pale skin, lethargic and is not accepting
breastfeeding. A thermometer reading over the right upper abdomen gives a
result of 34 °C. His birth weight is 2400 grams but has wasted 200grams.a) What do you think is the situation to that neonate baby?A baby is hypothermic when axillary temperature is below 35.5°C or core temperature
b) What do you think could be the reason of low body temperature to this new
born?
is below 36°C. As the rectal temperature is normally higher than that at other sites,
a rectal temperature below 35 °C is particularly dangerous. It results into metabolic
disorders such as dyspnea, poor feeding, hypoglycemia and lethargy. Once the
body temperature falls below 35 °C the infant is in danger of complications relatedto being too cold.
Newborns at risk of developing hypothermia• Preterm <35 weeks of gestation
• Low birth weight
• Small for gestational age
• Sick newborns
• Any newborn not adequately kept warm
• Wet infants (after delivery or bathing).
• Infants requiring resuscitation.
• Sick infants, particularly if there is infection.
• Infants who are in a cold room.
• Infants who are not fed.
• Hypoglycemic infants. »Infants undergoing medical procedures.• Infants born before arrival at a health facility, home delivery
Nursing management of hypothermia
• Warm the infant in a closed incubator, overhead radiant warmer or warmDifferent ways used to keep the new born warm:
room. Skin-to-skin care is a very effective method of warming a cold infant.
• Provide energy while the infant is being warmed.
• Monitor closely vital signs, oxygen saturation and color of skin
• Ensure neonate adequate breastfeeding
• Avoid cold infusions
• Educate the mother how to keep warm the baby and avoid cold bathing.
1. Maternal body heat (skin-to-skin care). Infants can very easily and
effectively be kept warm by placing them naked against the mother’s bare
breasts. The infant should wear a woollen cap and nappy. Both mother and
infant should be covered. The mother’s body heat will keep the infant warm.
This simple method is an important part of kangaroo mother care (KMC). It isthe best method of keeping a well infant warm.
2. A closed incubator. This is the traditional way of warming smallest or sick
infants as the temperature can be carefully controlled. Today more and more
infants are being warmed with KMC rather than in an incubator.
3. Radiant warmers (overhead radiant heaters). A radiant warmer is used for
warming very sick infant in an intensive care unit. Water loss by evaporation
is higher than in a closed incubator. A thick plastic sheet or ‘bubble wrap’ over
the infant reduces water loss. As soon as ill baby has improved they should
be moved out of a radiant heater and into a closed incubator.
4. Warm room. Most healthy, term infants can be warmed in a cot or bassinet in
a warm caring environment (ward or home). The room temperature should be
about 20 °C. The infant should be dressed to prevent heat loss by radiation
to cold windows or walls.
5. Hot room. Many low birth weight infants can be kept warm in a bassinet if
they are cared in a room where the temperature is kept at 25–30 °C. The
smaller the infant, the higher the required room temperature will be. However,
keeping the mother and infant together with KMC is preferable.
6. Dressing the infant. The infant can be kept warm by covering the body with
an insulating layer and, thereby, preventing heat loss by convection to cold air
and radiation to cold objects in the room. This is done by dressing the infant
in a nappy, jacket, woollen hat and booties. A woollen cap is most important
in preventing heat loss by radiation.
7. Thermal blanket. An infant can be kept warm for hours if wrapped in a
thermal blanket, silver swaddler or heavy gauge aluminium foil normally
used for cooking. This is an effective method of preventing heat loss during
transport if KMC or a transport incubator is not available. The infant must be
warm and dry before being wrapped in a thermal blanket.
8. Perspex heat shield. A transparent Perspex shield can be placed over aninfant in an incubator to reduce heat loss by radiation.
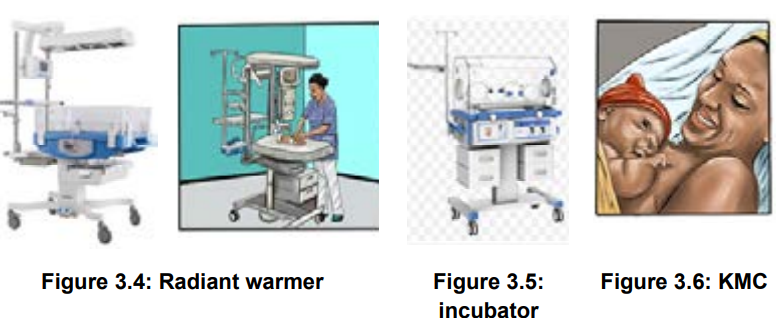
Self-assessment 3.5
1. Define hypothermia?2. State 5 methods of warming baby?
3.6 Neonatal hyperthermia
Learning Activity 3.6
4 days old male new born, born by spontaneous vaginal delivery brought at
emergency department by his mother complaining of, baby is hot on touch, body
temperature 39.8c0
. She also says that baby had inability to breastfeed since 2
days ago. The baby looked weak and dehydrated.a. What do you think could be the condition to this new born?Hyperthermia is defined as body temperature above 37.6 oC. Hyperthermia is
b. What do you think can be the cause of elevated body temperature to theneonate?
frequently a result of environmental factors that cause overheating. It is a sign of aserious infection in newborn termed as sepsis and must be ruled out for adequate
treatment. However, regardless of cause, hyperthermia can have detrimentalconsequences.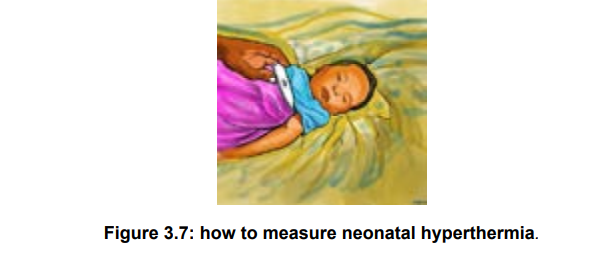
Causes of newborn hyperthermia• Overheating from incubators, radiant warmers, or hot ambient environmentalSigns and symptoms of hyperthermia in the new born
temperature
• Maternal fever
• Maternal epidural anesthesia
• Phototherapy lights, sunlight
• Excessive bundling or swaddling
• Infection
• CNS disorders (i.e. asphyxia)
• Dehydration• Tachycardia, tachypnea, apnea, warm extremities, flushing, perspiration.Nursing management of neonatal hyperthermia
• Dehydration.
• Lethargic, poor feeding, Irritability, Weak cry.• The usual approach to treating the hyper-thermic newborn is to adjust
environmental conditions.
• The newborn should be moved away from the source of heat, and undressed
partially or fully, if necessary.
• If the newborn is in an incubator, the air temperature should be lowered. It is
important that the newborn be breastfed frequently to replace fluids.• During the cooling process, the newborn’s temperature must be monitored
every 15-30 minutes until stable.
• Never turn off the incubator to cool off the newborn. When hyperthermia is
severe (i.e. body temperature above 40°C), the newborn can be given a bath.
• The water should be warm (about 2°C lower than the newborn’s body
temperature).
• Cooling devices are not recommended, if the newborn cannot breastfeed
extra fluids should be given intravenously or by tube.
• The treatment of hyperthermia in the new-born consists also exposing him or
her to room temperature.
• If the skin temperature is higher than 39.0°C, sponging with tepid water
at about 35.0°C should be initiated until the skin temperature approaches37.0°C.
Self-assessment 3.6
1) Define the term hyperthermia
2) State the causes of hyperthermia in the newborns
3) Briefly, explain the signs of hyperthermia in newborns3.7 Umbilical cord infection (Omphilitis)
Learning Activity 3.7
8 days old male neonate born by spontaneous vaginal delivery at home un
planed brought by his mother to the health facility with the following complaints;
umbilical stump draining pus, smelling discharge, swollen area around umbilical
cord, un usual temperature and baby is sleepy, she also reported that her baby’s
umbilical cord bleeds after birth and they re-tied it with cloth- thread.a) What do you think that could be the problem?In most cases, the umbilical cord stump dries up and falls off the newborn within the
b) What do you think that could be the cause?
first few weeks of life. It’s also normal for the clamped cord to develop a scab at its
end. It may even bleed a little bit, especially around the base of the stump when it’s
ready to fall off. But the bleeding should be light and quickly stop when you apply
gentle pressure. But sometimes an infection can develop. This may cause the area
around the cord to swell and become inflamed, red, or tender. There may be cloudy,
discolored, or bad-smelling discharge from the cord. There may also be oozing or
slight bleeding. That situation is called umbilical cord infection(omphilitis).
Omphalitis is an infection of the umbilical stump. It typically presents as a superficial
cellulitis that can spread to involve the entire abdominal wall and may progress tonecrotizing fasciitis, myonecrosis, or systemic disease.
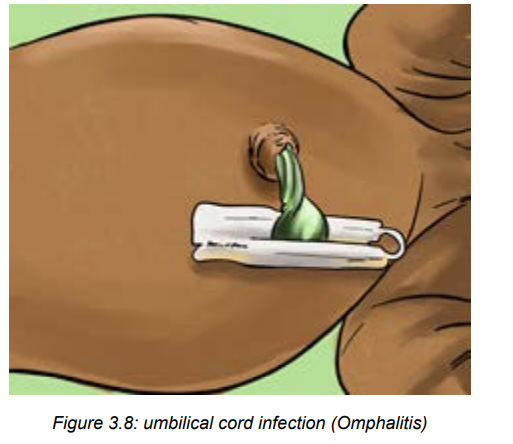
Signs of omphilitis include:
• Red, swollen, warm, or tender skin around the cordTo treat the umbilical cord infection, the healthcare provider may prescribe medicine
• Pus (a yellow-greenish liquid) oozing from the skin around the cord
• Bad smell coming from the cord
• Fever• A fussy, uncomfortable, or very sleepy baby
(antibiotics and anti-inflammatory drugs) and give instructions for cord care at home.
Risk factors of omphilitis
Risk factors for omphalitis included septic delivery, unplanned home delivery,
maternal chorioamnionitis, prolonged rupture of membranes, low birth weight,
and umbilical vessel catheterization. Mainly lack of hygiene from the mothers
and caregivers. Aerobic bacteria are present in approximately 85% of infections,
predominated by Staphylococcus aureus, group A streptococcus, escherichia coli,
klebsiella pneumoniae, and Proteus mirabilis. Methicillin-resistant S aureus has
also been described in association with omphalitis.
Nursing management of omphilitis• Wash the hands well before and after caring for the cord.Self-assessment 3.7
• Clean the area around the cord using disinfectant solutions
• Use a clean, moist cloth.
• Remove all drainage and clean an inch around the base. If there is a little
drainage is present you may be advised to use antibiotic ointment after each
cleaning.
• Roll the neonate’s diapers down below the belly button (navel) until the
infection has healed. This helps prevent contamination from urine and stool. If
needed, cut a notch in the front of the diapers to make a space for the cord.
• Don’t dress the baby in clothing that is tight across the cord.
• Don’t put the baby in bathwater until the infection has cleared and the cord
has fallen off. Instead, bathe the baby with a sponge or damp washcloth.
• Don’t use talc or other powders on the cord.
• Don’t try to remove the cord. It will fall off on its own.
• Watch for continuing signs of infection (redness, swelling, and cloudy,
discolored, or bad smelling drainage in the area around the cord) and othervital signs. This includes.
1) Define the term omphalitis3.8 Neonatal umbilical cord bleeding
2) State clinical manifestations of omphilitis3) Briefly explain the risk factors for omphilitis
Learning Activity 3.8
Observe the images above and reflect on them.
a) What do you reflect on that condition?b) What do you think that are the causes of that condition?
Bleeding umbilical cord on the neonate can lead to serious cardiovascular and
neurological effects. Routine administration of vitamin K has reduced the incidence
of hemorrhagic disease of the newborn, but abnormal bleeding can occur in neonate
babies from many causes.
Causes and risk factors of neonatal umbilical cord bleeding
Bleeding from the umbilical cord in the newborn can be caused by improper tying
of the umbilical cord, an inherited coagulation disorder, vitamin K deficiency or
immune-mediated thrombocytopenia. Disseminated intravascular coagulation
(DIC) is more common in the sick newborn.
Signs of umbilical cord bleeding
During the healing process, it’s normal to see a little blood near the cord. Much like
a scab, the cord might bleed a little when it falls off.
In case of severe hemorrhage, severity signs may include pale heavy bleeding
crossing the diaper from umbilicus, pale skin, lethargy, inability to breastfeed and
sometimes signs of shock and anemia.
Management of bleeding umbilical cord
Treat normal umbilical cord bleeding by cleaning the area around the umbilical cord
and applying a small amount of pressure to the umbilical stump to slow and stopthe bleeding.
If the bleeding is heavy, the following interventions should be done:• Call for helpSelf-assessment 3.8
• Retie the umbilical cord thoroughly
• Take vital signs
• Resuscitate the neonate in case of shock and respiratory problems
• Monitor closely vital signs
• Draw blood for lab examination (if possible)
• Ensure the nutrition (breastfeeding or parenteral)
• Remember to transfer the neonate to the neonatology or pediatrics specialist
1) What are the causes and risk factors of neonatal umbilical cord bleeding?
2) What are the signs of severe neonatal umbilical cord bleeding?3) State the complications of severe neonatal umbilical cord bleeding.
3.9 Skin infections in newborns
Learning Activity 3.9
From the observation of the above images;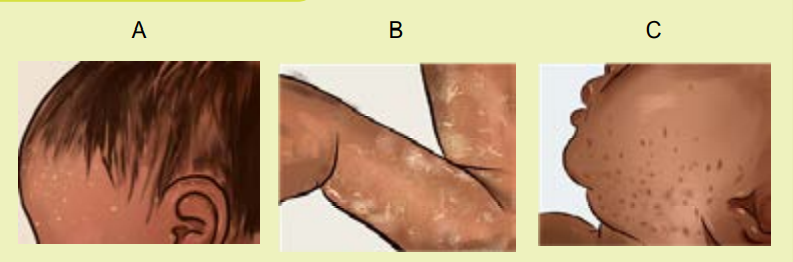
Among the skin infections, which one do you think that affect the skin like thosementioned on these images?
Skin forms a barrier with the external environment and is formed by structures that
have well defined functions. Although the stratum corneum of full-term neonates is
analogous to that of adult skin, structural and compositional differences of the skinmake the newborn more susceptible to bacterial colonization. Particularly for the
preterm neonate, impaired cutaneous barrier function and an immature immune
syii. Presentation• Nonbullous impetigo accounts for 70% of all cases and appears as tiny fluidfilled blisters that develop into honey–colored, crusty lesions. Generally, they
do not cause any pain or redness to the surrounding skin.
• Bullous impetigo is more common in infants and appears as larger, clear
blisters filled with fluid. When these blisters rupture, they may leave a scale
behind.
iii. Neonatal staphylococcal skin infectionsstem reduce the capacity to defend against bacterial pathogens.
The majority of cutaneous bacterial infections is localized to the skin and is easily
treated; however, systemic bacterial infection and disseminated disease in the
neonatal period may be life-threatening.
Pustular disorders are common in the neonatal period. Most of these conditions are
benign, but several serious and infectious diseases can present in the neonate as
pustular disorders.
Causes of neonatal skin infections
Vesiculo-bullous and pustular lesions in neonates can be due to
miscellaneous benign conditions, an infection, a genodermatosis, or
transient autoimmune bullous disorder.
Pustular eruptions in a neonate are due to a variety of causes, the benign causes
include erythema toxicum neonatorum, transient neonatal pustular melanosis, and
neonatal acne. The most common causes of infectious pustular skin lesions include
bacterial infections, which may be initially localized (Staphylococcus aureus) or
septicaemic (Listeria monocytogenes); viral infections (herpes simplex, varicellazoster);
fungal infections (Candidiasis, Malassezia furfur); or parasitic disorders(scabies).
Variety of serious neonatal skin infections
i. Impetigo
Definition: Impetigo, a common skin infection in both neonates and children caused
by bacteria (Staphylococcus or Streptococcus) entering a cut or break in the skin.
Although impetigo is usually a minor infection that can be easily treated, it could
progress to more severe symptoms including deep skin infections (cellulitis), kidney
inflammation, or meningitis. It causes distinctive blisters or sores, which can be
itchy or uncomfortable for your baby. Impetigo can be further classified into 2 types:bullous and non bullous.
ii. Presentation• Non bullous impetigo accounts for 70% of all cases and appears as tinyfluid filled blisters that develop into honey–colored, crusty lesions. Generally, theyiii. Neonatal staphylococcal skin infections
do not cause any pain or redness to the surrounding skin.
• Bullous impetigo is more common in infants and appears as larger, clear
blisters filled with fluid. When these blisters rupture, they may leave a scale
behind.
In full-term newborns, S. aureus infection usually first appears as a skin and soft
tissue infection, but may rapidly progress to osteomyelitis and pneumonia or cause
bacteremia.
Direct infection of the skin results in staphylococcal pyoderma, manifests as
vesicles, pustules, erythematous papules; folliculitis; bullous impetigo with large,flaccid bullae; honey-coloured crusted areas of nonbullous impetigo and cellulites
Manifestations of neonatal staphylococcal skin infections may be local or
generalized
iv. Pustula melanosis
Definition: Transient neonatal pustular melanosis is defined as harmless skin
condition in newborn that begins with superficial, vesiculopustular lesions often
causing some alarm when present at birth. Transient neonatal pustular melanosis
is an uncommon benign pustular condition presenting in newborn infants. It is also
known as transient neonatal pustular dermatosis and transient neonatal pustulosis.
Pustula melanosis vesicles rupture within 12 to 48 hours, leaving small pigmented
macules. The macules are often surrounded by a ring of very fine white scales. Any
stage or combination of stages (vesicles, pustules, or scaling of ruptured vesicles)
may be present at birth. These small hyper pigmented macules may remain for up
to 3 months after birth. Transient neonatal pustular melanosis is benign, requiring
no treatment.
Figure 3.9: pustula melanosis evolution:
Step 1. Pustule/Vesicles
Step2.Ruptured Pustule/VesiclesStep3.pigmented macules
Figure 3.10: Fluid-filled neonatal skin lesions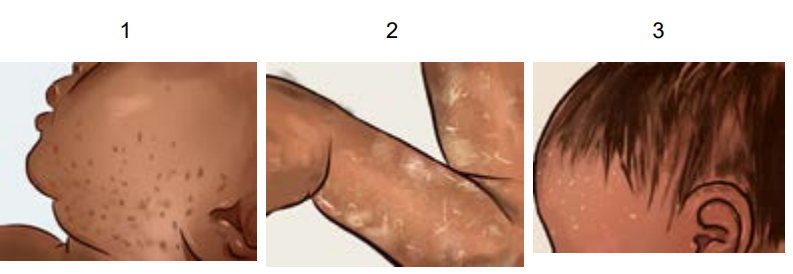
a) Vesicles due to eczema
b) Pustule due to herpes simplexc) Bulla in bullous pemphigoid.
Fluid-filled neonatal skin lesions are other types of neonatal skin infection to report.
They can be originating from all earlier described causes or idiopathic reasons.
Management of neonatal skin infections• For management of pustula melanosis: No treatment is indicated. ReassureThe skin and body hygiene are of paramount for all types of neonatal skin
parents that neonatal pustular melanosis is a benign finding and that it
disappears.
• For neonatal staphylococcal skin infections: Blebs should be punctured as
soon as formed and topical ointment/lotion should be applied. Full recovery
usually occurs in 2-3 week.
• For management of impetigo: In most cases, the antibiotic cream is
prescribed to speed up the healing process. With antibiotic treatment, the
baby’s impetigo should clear up within a week to 10 days. If the symptoms
don’t start to improve within five days of starting treatment, take back to the
dermatologist and peditrician.
• For management of transient neonatal pustular melanosis: It is benign,requiring no treatment apart from only local cleansing and washing.
infections
Self-assessment 3.9
1) What are the causes for Pustular eruptions in a neonate?
2) What are the symptoms of severe impetigo to the neonate?
3) Briefly, discuss on the neonatal staphylococcal skin infections caused byS. aureus in full term babies.
3.10 Seizures or convulsions in newbornsLearning Activity 3.10
Read the following scenario and reflect on it.
A 16-day-old female infant was brought to the emergency room because
of twitching, jaw movements, jerking movements of her arms and legs the
movements did not stop with restraint, these signs started since day 2 of life.
The parents hope to be recovered on its own but continued. There was cyanosis
of limbs and lips. They had been no fever, and she had been bottle feeding fairly,
her mother reported that she accidentary delivered from home and baby didn’t
cry for some minutes, latterly baby cried with weak voice as mentioned by her
mother.a) What do you think about the new born described in scenario’s condition?A neonatal seizure is an occurrence of abnormal, paroxysmal, and persistent
b) What do you think could be the cause of the above new born’s condition?
movements on the neonate. A neonatal seizure may or may not be epileptic.
Clinical manifestation of seizure• A neonate will present one or more of the following signs and symptoms:
twitching, rhythmic lip or jaw movements, eye twitching, extension of
extremities, clenching of fists, stiffening or jerking of limbs or trunk, lip
smacking movements may be observed.
• Accompanying signs may include the change in vital signs such as alteration
in heart rate, blood pressure, respiration, salivation, pupillary dilation, and
other associated paroxysmal changes in the autonomic nervous system of
infants may be caused due to these seizures.
• Common etiologies of neonatal seizures• The commonest cause is asphyxia due to hypoxic ischemic encephalopathy
but others are intra uterine and central nervous system (CNS) infections.
Lack of oxygen before or during birth due to placental abruption (premature
detachment of the placenta from the uterus), a difficult or prolonged labor, orcompression of the umbilical cord.
• Metabolic disorders that occur before (inborn error of metabolism) or around
birth such as hypo glycaemia, Hypocalcaemia, Hypomagnesaemia, Hypo/
hypernatremia may cause convulsions in newborn babies.
• Congenital abnormalities that involve the CNS, neonatal ‘stroke’ andintracranial hemorrhage are responsible of convulsions in newborn.
• Infection acquired before or after birth, such as bacterial meningitis, viral
encephalitis, toxoplasmosis, syphilis or rubella.
• Stroke before or after birth.
• Blood clot in the brain.
• Bleeding in the brain.
• Brain birth defects.
• Blood sugar or electrolyte imbalances Rarely Seizures in newborn can be a
precursor factor of neonatal onset epilepsy.Management of seizures• To control the seizures, anticonvulsant medications may be prescribed,
including phenobarbital, lorazepam and phenytoin. Seizures in neonates are
often subtle, featured as any unusual repetitive or stereotypic movement.
• Check blood glucose and/or treat for hypoglycemia.
• Treat with phenobarbital IV if the seizure lasts more than 3 minutes, or recurs
(> 2 to 3 episodes in one hour), or is associated with cardiorespiratory
disturbance:• First dose: 20 mg/kg by slow IV infusion over 30 minutes. Phenobarbital
should never be administered as a rapid direct IV injection. Phenobarbital
may be given IM (undiluted) if there is no IV access.
• If seizures persist 30 minutes after, administer a second dose
of phenobarbital 10 mg/kg by slow IV infusion over 30 minutes. If still no IV
access, give the second dose of phenobarbital 10 mg/kg (undiluted) IM at
least 60 minutes after the first IM dose. Do not give more than 40 mg/kg in
total.• Any neonate that required treatment with phenobarbital should be transferredSelf-assessment 3.10
to a neonatal care unit.
• Babies are closely monitored during treatment, and then slowly re-warmed to
normal body temperature.
• Monitor the neonate closely while awaiting transfer. Ensure ventilation
equipment is available as there is a risk of respiratory depression.
• Vital signs should be monitored closely.
1. Describe how you will recognize that a baby is having seizures orconvulsion.2. Briefly discuss metabolic causes of newborns convulsions3. When to start treating seizures with phenobarbital on the neonates?3.11 Neonatal jaundice
Read the following case study and think about it.
A full-term female baby was delivered through Caesarian Section due to
prolonged labor with birth weight 4.2 kg at 39th week of gestational age. Baby
cried soon after birth and the APGAR score at birth was 9/10 and 10/10 first and
fifth minutes respectively. No any congenital anomalies seen at the time of birth.
Also, early breastfeeding was initiated on the 3rd hour from birth because the
mother delayed in the operating room due to complicated surgical operation.
After 48 hours, the neonate baby was brought in neonatal unit complaining the
baby was not breastfeeding well, is falling sleepy every time and that the color of
the baby’s skin has turned into yellow color.a) What do you think could be the condition to neonate baby described above?
b) What do you think could be the risk factor or cause of that condition?Learning Activity 3.11
Neonatal jaundice is defined as the presence of yellowish coloration of the sclera
and the skin in a neonate, caused by bilirubin accumulation in the blood. Neonatal
jaundice is a common event that occurs especially in the first week of birth and is
one of the most common causes of hospitalization of the term and preterm neonates
in neonatal wards. It is also called “Hyperbilirubinemia “
Neonatal jaundice usually occurs on the second day of birth and is not usually
harmful, and a self-limiting condition, where disease usually improves without
treatment after reaching the normal amount of bilirubin, however very high levels of
bilirubin may lead to kernicterus as permanent brain damage.
Kernicterus is a type of brain damage that can result from high levels of bilirubin in
a baby’s blood. It can cause athetoid cerebral palsy and hearing loss. Kernicterus
also causes problems with vision and teeth and sometimes can cause intellectual
disabilities. Jaundice on the first day of life is always pathologic, and urgent attentionis needed to find its cause.
Assessment of neonatal jaundice by using of Modified Kramer ‘scale
• Perform the physical examination starting with eye sclera, face, and downward.
• Jaundice may be hard to see especially in newborns with dark skin.
• Kramer rule helps to estimate the degree of neonatal jaundice depending onthe body parts presenting with jaundice.
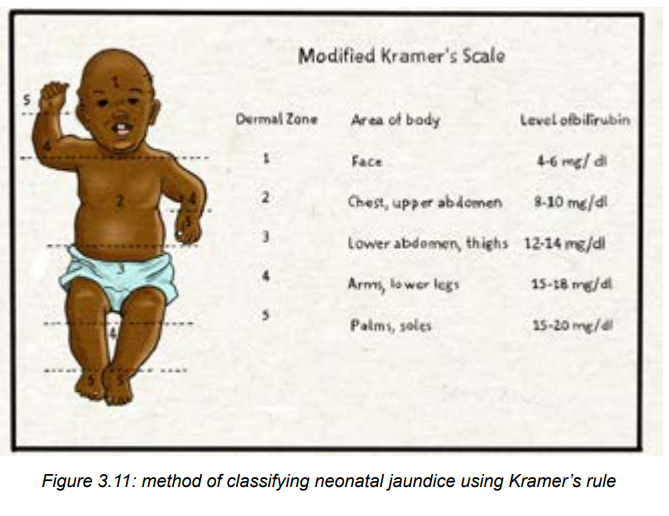
Causes and risk factors of neonatal jaundice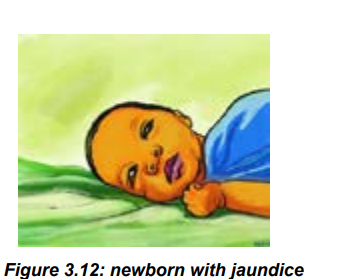
The known risk factors for neonatal hyperbilirubinemia include:• Delayed breast feeding and Lactation failureWhen red blood cells break down, a chemical called ‘bilirubin’ is released,
• ABO incompatibility (simply maternal–infant incompatibility in ABO system.
and this makes the skin to become yellow.
Premature birth (<38 week). A newborn’s immature liver often can’t remove
bilirubin quickly enough, causing an excess of bilirubin.• Post-term and macrosomia. Those newborn babies are born with high amountModerate signs and symptoms of neonatal jaundice
of RBC and need to break down them. Therefore, a lot of red blood cells, but
their liver isn’t developed enough to get rid of the bilirubin. This results in a
bilirubin overload, which leads to jaundice.
• Maternal and neonatal infection /sepsis
• Cephalohematoma,
• Birth asphyxia (Apgar score ≤6)
• G6PD enzyme deficiency,
• Other causes and risk factors are: low birth weight, Neonates from diabetic
mothers, neonates with siblings ‘history of severe neonatal jaundice,
hypothermia and hypoglycemia.
jaundice usually appears first on the face and then moves to the chest, belly, arms,
and legs as bilirubin levels get higher. Symptoms include yellowing of the skin and
eye conjunctiva within days after birth. In most cases, treatment isn’t required. Light
therapy (phototherapy) can help resolve moderate or severe cases.
Self-assessment 3.11
1. What are are the complications of very high levels of bilirubin to the
neonate?
2. What is Kernicterus?3. Which babies are more likely to develop jaundice than others?
3.12 Classification, diagnosis and management of neonataljaundice
Learning Activity 3.12 a. What do you think about the above image?Classification of neonatal jaundice
a. What do you think about the above image?Classification of neonatal jaundice
b. What do you think about how that blue light on image can help in neonataljaundice management?
Physiological jaundice: A newborn’s immature liver often can’t remove bilirubin
quickly enough, causing an excess of bilirubin. Jaundice due to these normal
newborn conditions is called physiologic jaundice, and it typically appears on the
second or third day of life it also characterized by the following;• Appears after at least 24 hours of birth,Pathological jaundice: is the most serious type of jaundice. It occurs within 24
• Peak after four or five days.• It later disappears after about 2 weeks of life.
hours after birth, and is characterized by a rapid rise in a baby’s bilirubin level. The
most likely cause is blood incompatibility or liver disease. Prompt medical attention
is necessary, and blood transfusions may be required and characterized by the
following:
• Appears within less 24hours
• Indirect bilirubin elevated
• Colored stools and urine
• Poor feeding
• Lethargy and excessive sleepiness• Change in muscle tone.
Symptoms of severe neonatal jaundice
The following symptoms will indicate that the baby has sever jaundice:• Crying inconsolably or with a high pitch.Diagnosis of neonatal jaundice
• Arched like a bow (the head or neck and heels are bent backward and the
body forward).
• Has a stiff, limp, or floppy body.• Have strange eye movements.
At a minimum, babies should be checked for jaundice every 8 to 12 hours in the
first 48 hours of life. The baby may be seen by a specialized nurse or physician
when the baby is between 3 and 5 days old, because this is usually when a baby’s
bilirubin level is highest. If the baby is discharged before age 72 hours, the baby
should be seen within 2 days of discharge.
Jaundice diagnosis is firstly based on symptoms such as yellowish of the skin,
eye conjunctiva and the whites of the eyes. All newborns are checked for jaundice
before leaving the hospital or birth center. However, on the other side, the bilirubin
tests may be done through blood sample collection to laboratory and bilirubin check
machines.
The associate nurse may check the baby’s bilirubin using a light meter that is placed
on the baby’s head. This results in a transcutaneous bilirubin (TcB) level. If it is high,
a blood test will likely be ordered.
The best way to accurately measure bilirubin is with a small blood sample from
the baby’s heel. This results in a total serum bilirubin (TSB) level. If the level is
high, based upon the baby’s age in hours and other risk factors, treatment will
likely follow. Repeat blood samples will also likely be taken to ensure that the TSBdecreases with the prescribed treatment.
Management of neonatal jaundice
The management of neonatal jaundice depends on the cause of the jaundice, the
bilirubin levels, and a baby’s age.– Mild jaundice goes away after 1 or 2 weeks as a baby’s body gets rid of the
extra bilirubin on its own. For newborns with breastfeeding jaundice, mothers
should breastfeed the baby more often. If the baby is not getting enough
breast milk, the specialized health care provider may suggest supplementing
with formula.
– For more serious cases of jaundice, treatment should start as soon as
possible at hospital.
– Always, encourage and support for frequent lactation and breastfeeding in
case of jaundice
• Ensure good hydration, (dehydration will cause bilirubin levels to rise moreup)
• Monitor vital signs as frequent as possible.Self-assessment 3.12
• Phototherapy. Babies lie under lights with little clothing so their skin is exposed.
The light changes the bilirubin to a form that can easily pass out of the body.• Light therapy blankets may also be used.
1) Why is it necessary to ensure good hydration on the neonate with jaundice?
2) What will be done to manage mild jaundice?
3) How phototherapy treats neonatal jaundice?4) What is the best way to accurately measure neonatal hyperbilirubinemia?
3.13 Neonatal hypoglycemia
Learning Activity 3.13
Baby MD was born one hour ago, at 40 weeks’ gestation, to a mother with
gestational diabetes. The birth weight was 4200gms and the APGAR score
of 10/10. Two days after birth, the neonate baby was brought in neonatology
unity presenting lethargy, irritability, jitteriness, high-pitched cry sometimes andinability to suck on breast.
Read the scenario and think about it:
a) What do you think about the condition of the baby described in scenario?Neonatal hypoglycemia, defined as a plasma glucose level of less than 30 mg/b) What do you think could be the risk factor to the condition of that baby?
dL (1.65 mmol/L) in the first 24 hours of life and less than 45 mg/dL (2.5 mmol/L)
thereafter, is the most common metabolic problem in newborns.
Hypoglycemia is common in neonates but often asymptomatic or presents with
non-specific signs. Recurrent or persistent hypoglycemia can lead to neurologicalsequelae.
Causes of hypoglycemia in a newborn baby
Hypoglycemia can be caused by conditions such as:• Poor nutrition for the mother during pregnancyThe newborns at risk for hypoglycemia:
• Making too much insulin because the mother has poorly controlled diabetes
Incompatible blood types of mothers and baby (severe hemolytic disease of
the newborn)
• More insulin in the baby’s blood for other reasons, such as a tumor of the
pancreas
• Birth defects
• Congenital metabolic diseases or hormone deficiencies. Some of these run
in families.
• Not enough oxygen at birth (birth asphyxia)
• Liver disease
• Infection (certain medicines the mother may have been taking for diabetes at
the time of birth, such as sulfonylurea medicines, can cause sepsis or other
severe infections).
Babies who are more likely to have hypoglycemia include those who are:• Born to mothers with diabetesSymptoms of hypoglycemia in a newborn baby
• Small for gestational age or growth-restricted
• Preterm babies, especially those with low birth weights
• Born under significant stress
• Large for their gestational age
Signs of low blood sugar may not be easy to see in newborn babies. The most
common signs include:
• Shakiness
• Blue color to skin and lips (cyanosis) or pallor
• Stopping breathing (apnea) or fast breathing
• Low body temperature (hypothermia)
• Floppy muscles (poor muscle tone)
• Not interested in feeding
• Lack of movement and energy (lethargy)
• Seizures
• Weak or high-pitched cry
Diagnosis
• Blood glucose < 2.5 mmol/l or < 45 mg/dl. Blood glucose is measured on a
sample of capillary blood taken from the lateral aspect of the heel using a
lancet or 24G needle.
• Always check blood glucose:• In neonates at risk of hypoglycemia
In neonates presenting with one of these signs:• HypothermiaComplications of neonatal hypoglycemia
• Irritability or tremors
• Bradypnoea or apnoea or cyanosis
• Hypotonia or poor response to stimulation or impaired consciousnessSeizures.
Major long-term sequelae include neurologic damage resulting in mental retardation,
recurrent seizure activity, developmental delay, and personality disorders. Someevidence suggests that severe hypoglycemia may impair cardiovascular function.
Management of hypo glycaemia
• Feed neonate immediately (preferably breast milk).
• If no milk is available, give 5 ml/kg of 10% glucose PO over 5 to 10 minutes.
Check blood glucose after 30 minutes:
• If it is normal (≥ 2.5 mmol/litre or ≥ 45 mg/dl), ensure the neonate feeds
regularly and check blood glucose again before each feed until there are 3
consecutive normal results.
• If it remains < 2.5 mmol/litre or < 45 mg/dl), treat as recurrent hypoglycaemia.
• Note: only if it is impossible to give an infusion or place a gastric tube, 1 ml/
kg of 50% glucose can be administered sublingually.• Frequent monitoring of vital signs is necessary
Self-assessment 3.13
1) Briefly explain which babies are at risk for neonatal hypoglycaemia
2) State the signs and symptoms of neonatal hypoglycaemia3) Explain which neonates should be screened for neonatal hypoglycemia.
3.14 Neonatal cyanosis
Learning Activity 3.14
What do you reflect on image A?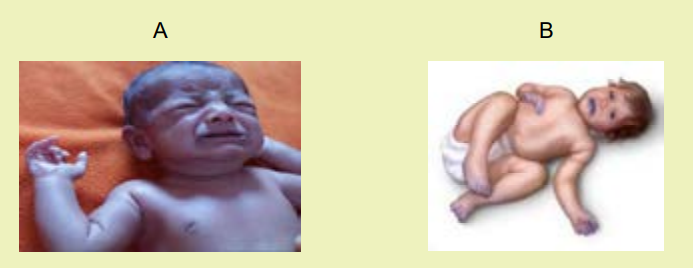
What do you reflect while observing image B?
Cyanosis is a blue discoloration of the skin and mucus membranes caused by an
increased concentration of reduced hemoglobin (>1.9–3.1mmol/L) in the blood. It
is most easily seen where the skin is thin, such as the lips, mouth, earlobes and
fingernails. Cyanosis indicates there may be decreased oxygen attached to redblood cells in the bloodstream. It may suggest a problem with the lungs or heart.
Cyanosis is a common clinical finding in newborn infants. Neonatal cyanosis,
particularly central cyanosis, can be associated with significant and potentially
life-threatening diseases due to cardiac, metabolic, neurologic, infectious, andparenchymal and non-parenchymal pulmonary disorders
Types of neonatal cyanosis
• Acrocyanosis/ Peripheral cyanosis: refers to the cyanosis found in the
extremities, particularly the palms of the hands and the soles of the feet. It
can also be seen on the skin around the lips. Acrocyanosis is often normal
in babies, as long as no cyanosis is present in the central part of the body.
This is relatively common in neonates, and is generally a physiologic finding
due to the large arteriovenous oxygen difference that results during slow flowthrough peripheral capillary beds.
• Central cyanosis: refers to cyanosis found on “central” parts of the body,
including the mouth, head and torso. Central cyanosis is never normal in the
newborn period, and is almost always linked to a lower amount of oxygen in
the blood. Central cyanosis indicates the presence of potentially serious and
life-threatening disease, and requires immediate evaluation. It could be dueto a problem of the heart, lungs or blood.
Causes and conditions triggering the neonatal cyanosis
The following may be the causes and conditions triggering the neonatal cyanosis:• Primary pulmonary disease on the neonate.Cyanosis is usually caused by abnormalities of the heart, the lungs or the blood.
• Congenital cardiac malformations.
• Upper airway obstruction on the neonate.
• Persistent pulmonary hypertension of the newborn (PPHN)
• Neonatal sepsis.
• Neonatal anemia.
• Neonatal polycythemia.
• Birth asphyxia.
Under normal conditions, after receiving oxygen from the lungs, red (oxygen rich)
blood is delivered from the heart to the rest of the body. When it returns to the heart,the blue (oxygen poor) blood is shipped to the lungs to collect more oxygen.
Abnormalities in the lungs that can prevent oxygen from entering the blood,which can lead to cyanosis.
Some examples of lung abnormalities that can lead to cyanosis include:• Events that limit the amount of oxygen (smoke inhalation from house fires,
carbon monoxide poisoning, etc.)
• A blockage in the airway that limits the amount of oxygen getting into your
lungs (choking on a foreign body, croup, etc.)
• Primary lung disease (asthma, pneumonia, bronchiolitis, etc.)
• Congenital heart abnormalities can cause some blue (oxygen poor) blood
to bypass the lungs altogether and never collect oxygen (see below).
Abnormalities in the blood can decrease its ability to absorb oxygen. All of
these abnormalities cause blue (oxygen poor) blood to get pumped to the
body.Management of neonatal cyanosis
• Most cyanosis in neonates is a result of “acrocyanosis” and does not needincreasing concerns about the potential risks associated with this therapy
treatment. If there is a primary lung or heart issue, cyanosis will go away
when the neonate has the underlying condition treated either medically or
surgically.
• Severe cyanosis requires urgent supportive therapy while a diagnosis is
established. The infant should be maintained in a thermos-neutral environment
using a radiant warmer. Oxygen should be provided, although there are• Close monitoring of vital signs is requiredNeonatal pallor
• Ensuring adequate breastfeeding to the neonate is also important• Prevention of hypothermia and hypoglycemia is necessary
The neonatal pallor (whitish color) indicates a perceived decrease in rubor in the
skin and mucous membranes of a neonate, which is associated with decreased
oxyhemoglobin delivery to the skin or mucous membranes. it is more evident onface and palms.
Causes of neonatal pallor:
• Illness,
• Emotional stress,
• Anemia and• Any other condition that can reduce the amount of ox hemoglobin.
Management of neonatal pallor
• The management of neonatal pallor is based on its etiology
• Close monitoring of vital signs is required
• Ensuring adequate breastfeeding to the neonate is also important• Prevention of hypothermia and hypoglycemia is necessary
Self-assessment 3.14
1) Diferentiate acrocyanosis and central cyanosis.
2) Describe conditions that may cause cyanosis to the neonate.
3) What can be the cause of neonatal pallor?
3.15 Neonatal gastro intestinal problems
Learning Activity 3.15Read the scenario below and reflect on it.
The new-born baby boy on day 8 of life was brought to the hospital by his mother
who reported that it’s now 36hours since her baby developed vomiting, abdominal
distension. She added that it is becoming more repeated and she is worried.
Upon the nurses’ observation the neonate looks weak, and vomits every after
poorly feeding. Respiratory rate 30cycles, heart rate 138bts/min, temperature
350c, spo2 96%. Immediately, the baby was admitted and the management
started. Then, after 6 hours of admission, the neonate baby developed diarrhoea
where he passed watery stool 4 x in 1 hour.a) What do you think about this baby?Vomiting or more often, regurgitation is a relatively frequent symptom during the
b) What do you think that can show you that this baby is critically sick?
newborn period. In most cases this is unimportant and rarely persists beyond the
first few feeds. However, there are circumstances when the type of vomiting is
important.
Many newborns vomit; in most cases when vomiting is significant.
The following conditions can signify severe signs:
• Vomitus contains blood (red or black, the colour of the blood will depend upon
how long the blood has been in the stomach)
• Vomiting green bile can indicate a bowel obstruction, which needs immediate
attention.
• The baby is projectile vomiting
• The baby is failing to thrive,
• The baby has gastro esophageal reflux and could be aspirating,
• The baby also has diarrhea
• The abdomen is distended.
• Delay in passage of meconium
• The baby is dehydrated (dry mouth, decreased wet nappies, hypotonic).• Vomiting causing choking and aspiration.
The commonest cause of vomit containing blood is swallowed maternal
blood. Swallowed blood often irritates the stomach and causes vomiting. Bloodmay be swallowed during: child birth and breastfeeding.
Causes of vomiting
The most common causes of vomiting in the neonatal period include gastroenteritis,malrotation, pyloric stenosis and necrotizing entero-colitis
Vomiting Scale:
• Mild: 1 - 2 times/day
• Moderate: 3 - 7 times/day
• Severe: Vomits everything, nearly everything or 8 or more times/day
• Severity relates even more to how long the vomiting goes on for. At the start
of the illness, it’s common for a neonate to vomit everything. This can last
for 3 or 4 hours. The neonate then often become stable and change to mildvomiting.
The main risk of vomiting is dehydrationManagement of vomiting
• Rehydrating the neonate is well-hydrated is the first step,ABDOMINAL DISTENSION IN THE NEW BORNS
• If the new born is repeatedly vomiting and is unable to hold down fluids
provide IV fluids (Normal saline).
• Search for causes of diarrhea and vomiting and treat or refer for treatment in
a specialized health setting.
• The associate nurse should refer this baby urgently,
• Close monitoring of vital signs is required,
• Ensuring adequate breastfeeding to the neonate is also important,• Prevention of hypothermia and hypoglycemia is necessary.
Abdominal distension is a common clinical presentation in neonates admitted
to neonatal intensive care units (NICUs), especially preterm infants. Neonates can
present with abdominal distention during a feed advance or a change in type offeed.
Causes of abdominal distension in the new borns
Congenital malformations may be the major cause of abdominal distension in
early newborns. Sepsis and congenital megacolon are the single disease most
frequently associated with abdominal distention in preterm and full-term newbornsrespectively
Other causes: failure to pass meconium majority pass within 24 hrs, delayedpassage of meconium (lubricated per-rectal thermometer may be therapeutic).
Management of neonatal abdominal distension
The management of neonatal distended abdomen. However, the nurse must ensureclose monitoring of vital signs is required and adequate breastfeeding
NEONATAL DIARRHEA
Neonatal diarrhea is when the newborn baby passes very runny, watery stools,
sometimes at an increased frequency or more volume than normal. There may be
mucus in the stool. Diarrhea is sometimes associated with vomiting. Diarrhea isoften caused by a bacterial or viral infection.
Management of neonatal diarrhoea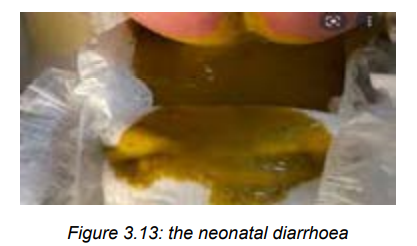
– The management is based on dealing with the cause of diarrhoea
– Hand hygiene is important in management of neonatal diarrhoea,
– Rehydrating the neonate is well-hydrated is the first step,
– If the neonate has severe diarrhea and is unable to hold down fluids provide
IV fluids (Normal saline).
– Search for causes of diarrhea and vomiting and treat or refer for treatment in
a specialized health setting.
– The associate nurse should refer this baby urgently,
– Close monitoring of vital signs is required,
– Ensuring adequate breastfeeding to the neonate is also important,
– Prevention of hypothermia and hypoglycemia is necessary.
Self-assessment 3.15
1) What the nurse will fear if the neonate baby vomits greenish like vomit?
2) When vomiting may be significant to the neonate baby?3) Using a scale, classify the neonatal vomiting.
3.16 Red, swollen eyelids and pus discharge from the eyes in thenewborns.
Learning Activity 3.16
From the observation of the mentioned above pictures, reflect to them;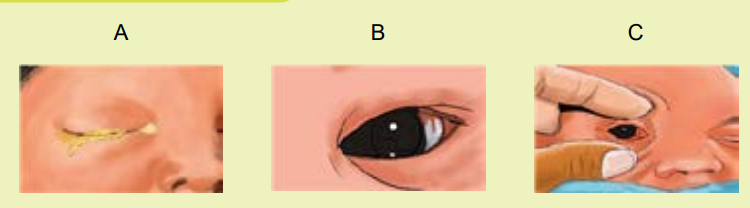 a) What do you think on the newborn’s eyes seen on image A?Neonatal red eye/ Neonatal conjunctivitis: is a red eye in a neonate caused by
a) What do you think on the newborn’s eyes seen on image A?Neonatal red eye/ Neonatal conjunctivitis: is a red eye in a neonate caused byb) What do you reflect on image B and C?
infection, irritation, or a blocked tear duct. When caused by an infection, neonatal
conjunctivitis can be very serious.
Conjunctivitis, or pink eye: is an irritation or inflammation of the conjunctiva, which
covers the white part of the eyeball. Conjunctivitis can be extremely contagious and
is spread by contact with eye secretions from someone who is infected.
Sub-conjunctival hemorrhages of the neonate: are red spots or bruises of the
eye that are common in new-borns and typically result from the normal trauma of
birth. As new-borns are squeezed through the birth canal blood vessels (on the
eyes and elsewhere) can rupture.
Causes of neonatal conjunctivitis
Conjunctivitis in neonate can be caused by an infection (bacteria or viruses.) or by
a reaction to chemicals put into the eyes (called chemical conjunctivitis).
If certain bacteria are present in the mother’s vagina, they can be passed to
the new-born during delivery. Such bacteria include Chlamydia, Streptococcus
pneumonia, Haemophilus influenza, Neisseria gonorrhoea, and others. Chemicalconjunctivitis is a reaction to the eye drops that neonates receive to prevent infection.
Symptoms neonatal conjunctivitis
Symptoms of conjunctivitis may vary depending on the cause of the infection.
Symptoms include redness, itching, swelling, or tenderness and tearing of the eyes.
Eye discharge or crusting around the eyes can be present.
Sub-conjunctival haemorrhage may present a bright red patch appearing in the
white of the eye.
Conjunctivitis caused by chlamydia usually begins 5 to 14 days after delivery but
sometimes as late as 6 weeks after. New-borns have swollen eyelids and a watery
discharge from the eyes that contains increasing amounts of pus. The infection cansometimes be severe.
Conjunctivitis caused by gonorrhoea usually begins 2 to 5 days after delivery.
New-borns have severe inflammation of the eyelids and discharge of pus from theeyes. Without treatment, blindness may occur.
Conjunctivitis caused by chemicals, such as eye drops, usually begins within 6 to8 hours after the drops are put in and goes away by itself within 2 to 4 days.
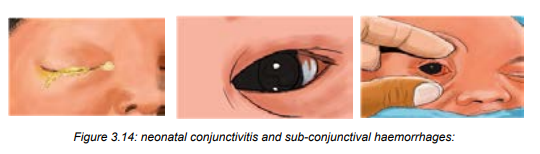
General prevention and treatment
• The tiny, delicate eyes of a neonate baby need proper care because it is
important to keep them clean and healthy.
• Using a soft a cotton ball (wool) and plain water, one can carefully cleanse
the baby’s eyes.
• Dampen the cotton ball with a little bit of lukewarm water.
• With the baby’s eyes closed, gently wipe the eyes from the inside to the
outside corners. Use a new cotton ball for each eye.
• Teach pregnant women the importance of treating sexually transmitted
infections, such as herpes simplex, gonorrhoea, and chlamydia in order to
decrease the incidence of neonatal conjunctivitis.• In Rwanda, tetracycline or silver nitrate eye ointment is routinely put intoSelf-assessment 3.16
each of the new born’s eyes after delivery to prevent conjunctivitis caused
by Neisseria gonorrhoeae.
• For conjunctivitis caused by Neisseria gonorrhoeae are given
ceftriaxone or cefotaxime injection.
• Treatment for conjunctivitis caused by Chlamydia, is treated
by erythromycin or azithromycin.
• For conjunctivitis caused by other bacteria, ointments containing polymyxinplus bacitracin, erythromycin, or tetracycline are applied.
1) What are the causes of neonatal conjunctivitis?
2) What are symptoms neonatal conjunctivitis?
3) Briefly discuss on prevention of neonatal conjunctivis after delivery.4) Describe sub-conjunctival haemorrhages of the neonate.
Summary of the unit of new born danger signs
Early detection of neonatal illness is an important step towards improving new
born survival. A mother is the nearest person to a neonate to identify, present, and
manage the neonates’ problem, which ensures that neonates can lead a healthy
life. If mothers know appropriate manifestations of the causes of death in new borns
(neonatal danger signs), it is possible to avert related neonatal mortality. Because of
the health-seeking behavior of mothers highly relies on their knowledge of neonataldanger signs.
Management of the new born danger signs:
Stabilize the neonate before transfer to the neonatal unit:
• Position the head to open the airway.
• Administer oxygen with an appropriate nasal cannula, at a maximum flow rate
of 2 litres/minute (aim for SpO2 90-95%).
• In the case of apnoea or if RR < 20/minute: perform bag and mask ventilation• Check blood glucose and/or treat for hypoglycemia.
While awaiting transfer:• Keep neonate warm in a room at 23-25 °C wrapped in a blanket or under anIn the case of severe respiratory distress, abdominal distension, or coma, do not
infant warmer, and cover the head with a cap.
• Closely monitor temperature, respiratory rate and SpO2
• Start treatment for neonatal infection
• Ensure routine neonatal care
• Start or continue feeding only if necessary, compliment feeds with a
nasogastric tube and/or IV fluids.feed the neonate by mouth. Start IV fluids if possible.
Neonates suspected to have severe neonatal infection. Danger signs may indicate
an underlying severe infection which requires transfer to a neonatal unit andantibiotic therapy.
While awaiting transfer to a neonatal unit, start antibiotic therapy: The
first line treatment is the combination of ampicillin IV + gentamicin IM.
Ampicillin is preferably used IV; the IM route is an option if the context
does not permit proper IV administration. To avoid multiple IM injections.
If meningitis is suspected, do not use procaine benzyl penicillin.
If the infection is cutaneous in origin, replace the ampicillin with cloxacillin IV.
Total treatment duration is 7 to 10 days according to clinical response. Gentamicin
should be stopped after 5 days of treatment.
3.17. End unit assessment 31. What are 9 danger signs on the neonate as described by WHO?
2. How can an associate nurse care for in infant with respiratory problems?
3. What are the consequences of the baby unable to breastfeed?
4. When is the neonate fed using naso-gastric tube?
5. What can be the error while taking the new born’s temperature taking?
6. Describe management of hyperthermia in neonate baby.
7. What are the complications of omphalitis to the neonate baby?
8. Describe the management of impetigo on the neonate baby.
9. What are the signs accompanying neonatal seizures a part from jerky
movements of eyes, libs and limbs?
10. When a mother has to suspect a neonatal jaundice to his/her neonate
baby and bring her/him to health setting immediately?
11. What are the major complications of neonatal hypoglycaemia?
12. What can an associate nurse think in case a generalized or central cyanosis
is realized to the neonate baby?
13. What are the major causes of neonatal distended abdomen to early new
borns?
14. What are the causes of neonatal diarrhoea?
15. Describe the management of neonatal diarrhoea and vomiting.
16. Describe the treatment of neonatal conjunctivitis caused by chlamydia..
UNIT 4: COUNSELLING IN REPRODUCTIVE HEALTH
Key unit competence:Provide counselling in reproductive health
By looking at the above picture A, B and C, respond to the following questions: 1. Describe the situation on the above pictures.
1. Describe the situation on the above pictures.
2. What are the signs that characterize the people’ situation on pictures A, Band C?
4.1. Definition of key concepts
Learning Activity 4.1
Using different source of information (internet, books or any other source of
information) search for the definition of the following terms and be prepared for
class presentation:1. Reproductive healthReproductive Health is defined as a state of complete physical, mental and social2. Reproductive counselling
well-being and not merely the absence of disease or infirmity, in all matters relating
to the reproductive system and its functions and processes.
Reproductive health therefore implies that people are able to have a satisfying
and safe sex life, and that they have the capability to reproduce and the freedom
to decide if, when and how often to do so. Implicit in this last condition are the
right of men and women to be informed of and to have access to safe, effective,
affordable and acceptable methods of family planning of their choice, as well as
other methods of birth control which are not against the law. Men and women have
the right to access the appropriate health-care services that will enable women
to go safely through pregnancy and childbirth and provide couples with the best
chance of having a healthy infant.
A face-to-face communication or interactive process that a healthcare provider have
with a client or couple in order to help them arrive at voluntary and informed decisions
is defined as Counselling. Counselling is used in many different ways including but
not limited to counselling for maternal and new-born health, reproductive healthfamily planning, therapy, during crisis and adolescent health.
Reproductive counselling supports individuals and couples in their journey to
become parents; provides an opportunity to receive support, better understand the
reproductive options and choices, and explore the impact of these events on clientrelationships.
Self-assessment 4.1
Define the following terms:a. Counselling4.2 The process, principles, skills of counselling in Reproductiveb. Reproductive health
Health
Learning Activity 4.2
Discuss in groups of 5 the following activities:
1. The key steps in counselling process.2. The principles for a successful counselling
The counselling process takes place within a counselling context and it is important
to be familiar with it as it provides the guidance on how to act, what is appropriate
and the situation, culture and norms of the person that is being counselled. There
are a number of guiding principles and counselling skills which support thecounselling process.
1. The Counselling process
There are six steps for counselling. Through these steps, the counsellor can give
support and guidance
Steps of counselling:
1. Assess the situation: Engage the individual in interactive discussion. Ask
questions to
better understand the situation and the needs of the client
2. Define problems, needs and information gaps: Review with the client what it
is
about the situation that prevents from addressing the needs. What makes the
situation a problem, what are the causes of the problem? What does the client
know already? Assess the need of additional information.
3. Generate alternative solutions: Review with the client how can better address
the needs by looking at what is currently being done, and what else could be done.
Identify what other information, resources or support is needed.
4. Prioritize solutions: by reviewing the advantages and disadvantages of the
various
alternatives, work out with the client which of the alternatives are most feasible to
address the problem and/or meet the needs. Assist the client to work out how to
overcome potential disadvantages.
5. Develop a plan: make a plan together
6. Review and evaluate: in the following counselling sessions review implementation
of the plan with the client. Is the plan working or should another alternative be
required?
2. The principles of counselling
These are values and process that are used in provision of professional assistanceand guidance in resolving personal or psychological issues.
Principle 1. Establish and maintain rapport with the client
Establishing and maintaining rapport with a client is vital to the encounter and
achieving positive outcomes. This can begin by creating a welcoming environmentand should continue through every stage of the client encounter, including follow up.
Principle 2. Assess the client’s needs and personalize discussions accordinglyEach visit should be tailored to the client’s individual circumstances and needs.
Principle 3. Work with the client interactively to establish a plan
Working with a client interactively to establish a plan, including a plan for follow-up,
is important. Establishing a plan should include setting goals, discussing possible
difficulties with achieving goals, and developing action plans to deal with potential
difficulties.
The amount of time spent establishing a plan will differ depending on the client’s
purpose for the visit and health-care needs. A client plan that requires behavioral
change should be made on the basis of the client’s own goals, interests, andreadiness for change.
Principle 4. Provide information that can be understood and retained by the
client
Clients need information that is medically accurate, balanced, and nonjudgmental
to make informed decisions and follow through on developed plans. When speaking
with clients or providing educational materials through any medium (e.g., written,
audio/visual, or computer/web-based), the provider must present information in a
manner that can be readily understood and retained by the client.Principle 5. Confirm client understanding
It is important to ensure that clients have processed the information provided and
discussed. One technique for confirming understanding is to have the client restate
the most important messages in her or his own words. This teach-back method can
increase the likelihood of the client and provider reaching a shared understanding,and has improved compliance with treatment plans and health outcomes.
4.2.1 Counselling skills
The key skills needed for counselling are: two-way communication; forming analliance; active listening; open questioning; providing information; facilitation.
Two-way communication: Good communication is central to good counselling
and involves the exchange of information and is most productive
when it is a two way process which offers an opportunity for each
of the parties involved to clarify issues, provide feedback and discuss topics.
Many of the skills we discuss for good counselling are also important to good
communication.
2. Forming an alliance: The counsellor’s first communication task is to build an
alliance, or a partnership, with the client and this alliance serves as the foundation
that encourages the client to actively participate in the session. You can help form
an alliance with a client by identifying similarities between yourselves, sharinginformation about one another.
3. Demonstrating active listening: Listening is more than just hearing someone
else’s words; it involves being attentive and demonstrating that you have heard and
understood what is being communicated to you.
Demonstrating that you really are listening will increase the client’s trust and
confidence in you as a counsellor, and will make her feel more at ease thus helping
to form an alliance. Demonstrating that you have heard and understood what has
been said to you can be done by paraphrasing, whereby you repeat back what has
been said to you using different words
4. Providing information
As a counsellor, you need to provide clear and understandable information, pertinent
to the
client, her family and their situation. it is important to make sure that the information
you provide has been understood. You can ask if there is anything that needs further
explanation or clarification, or sometimes you may wish to ask the client to repeatback in her own words what has been discussed.
5. Facilitation
Facilitation is the word given to the process of assisting problem-solving. Facilitation
is about assisting client to find his/her own solutions, as well as supporting him/her to
take the action needed. In a counselling situation, if you make decisions for a client
then responsibility and control is taken away from her/ him and it may lead to greater
dependency and feelings of inadequacy. It is important that a client is provided with
the opportunity to think out her/his situation and try to resolve needs. One way to
facilitate is to ask the client to list all the possible solutions identified. If you can
think of others, you might suggest them to be added to the list of alternatives, but
do not push your ideas too strongly. Then explore each alternative one by one. Get
her/him to think about the advantages and disadvantages. Keep summarizing what
have discussed and feed this back. Once the client reaches a decision, you canfollow a similar process to help facilitate a plan of action to carry out the decision.
Self-assessment 4.2
Explain the principles and the skills of successfully counselling
4.3 Counselling frameworks
Learning Activity 4.3
Using different source of information (internet, libraries) answer the question
below:What are the two different frameworks of counselling in Reproductive Health?
The REDI framework
The REDI framework (which stands for Rapport-building, Exploration,
Decision making, and implementing the decision) and it is a client
centered counselling framework. • The REDI framework emphasizes the client’s responsibility for makingPhase 1: Rapport-Building
• The REDI framework emphasizes the client’s responsibility for makingPhase 1: Rapport-Building
a decision and for carrying it out; enables providers to help clients make
full, free, and informed decisions that: Consider the client’s individual
circumstances and social and gender contexts; Emphasize the client’s
rights to and responsibilities for making and implementing decisions; Identify
the challenges a client may face in implementing decisions and developing
strategies and skills to address those challenges.
• The most important thing to remember about counselling models is that the client is
more important than the framework. Frameworks can be helpful to providers in giv
ing you a structure for talking with the client, so that you do not miss important
steps and whatever framework is used for counselling, it is important to
personalize counselling sessions by exploring each client’s individual
situation.
• The REDI framework consists of four phases: The bullets below are
suggestions for areas to address in each phase of REDI. They are not meant
as a checklist to follow in strict order, nor are they to be read or recited to theclient. The interaction should always be tailored to the client’s situation.
1. Welcome the client by greeting the client warmly and helping the client to
feel comfortable and relaxed
2. Make introductions by identify the reason for the client’s visit and ask
general questions, such as name, age, number of children, category of client
(new, satisfied, etc).
3. Introduce the subject of counselling: Explain the reasons for asking
questions and explain that the client does not have to answer questions
4. Assure confidentiality: Explain the purpose of and the policy on confidentiality
and create an atmosphere of privacy by ensuring that no one can overhearyour conversation, even if you are not able to use a separate room
Phase 2: Exploration
1. Explore the client’s needs, risks, and circumstances (Identify the reason
for the visit in detail) by assessing what the client understands about his or
her situation, what worries or concerns he or she might have, and what he or
she specifically hopes to accomplish through the visit
2. Assess the client’s knowledge and give information, as needed
by assessing the client’s knowledge of the reason of visit and correct
misinformation and fill in gaps, as needed
3. Assist the client to perceive or determine his or her own problem’s risk
by asking the client if he or she feels at risk for reproductive health problems,
help the client to recognize and acknowledge his or her risks and explore thereasons.
Phase 3: Decision Making
1. Identify what decisions the client needs to make in this session by helping
the client to prioritize the decisions, to determine which are the most important to
address and explain the importance of the client’s making his or her own
decisions
2. Identify the client’s options for each decision by helping the client to
lay out the various decisions that a client could make and to explore the
consequences of each.
3. Weigh the benefits, disadvantages, and consequences of each option by
making sure the discussion centers on options that meet the clients’ individual
needs, taking into account their preferences and concerns; providing more
detailed information, as necessary, on the options that the client is considering;
considering who else would be affected by each decision.
4. Assist the client to make his or her own realistic decisions: Ask the client
what is his or her decision; why he or she is making this decision; check to see
that this decision is the choice of the client free of pressure and help the client
to assess whether his or her decision can actually be carried out, given hisor her relationships, family life, and economic situation, among other issue
Phase 4: Implementing the Decision
1. Make a concrete, specific plan for carrying out the decision: Be specific.
If a client says that he or she is going to do something, find out when, under
what circumstances, and what his or her next steps will be in each situation.
Asking a client “What will you do next?” is important in developing a plan to
reduce risk. For example, if a client says that he will start to use condoms, the
provider should ask, “How often?” “Where will you get the condoms?” “How
will you pay for them?” “How will you tell your partner that you want to use
them?” and “Where will you keep them so you will have them with you whenyou need them?”
2. Identify barriers that the client may face in implementing the plan: Ask
about possible consequences of the plan: “How will your partner(s) react?” “Do
you fear any negative consequences?” “How will the plan affect relationships
with your partners?” “Can you communicate directly about the plan with your
partners?” and “Will indirect communication be more effective at first?”
3. Develop strategies to overcome the barriers: Ask about social supports.
Who in the client’s life can help the client carry out the plan? Who might create
obstacles? How will the client deal with a lack of support or with individuals
who interfere with the client’s efforts to reduce risk? Make a “Plan B”—thatis, if the plan does not work, then what can the client do?
Make a plan for follow-up: Invite the client to return for a follow-up visit to provide
ongoing support with decision making, negotiation, and behavior change; explain
timing for medical follow-up visit; make referral for services not provided at your
facility
The GATHER framework
The GATHER framework (which stands for Greet, Ask, Tell, Help, Explain and
schedule a Return) ensures that providers are client-focused, since it emphasizes
learning about the client and having a dialogue together, rather than talking at theclient. Ensuring informed choice is a critical element of GATHER.
GATHER provides a useful framework, but this does not mean that it must be
followed exactly or in sequential order during a counseling session. GATHER is
merely a suggested guide of steps and topics to cover while the provider andclient engage in an interactive two-way discussion of the client’s needs and risks.
G = GREET the client politely and warmly. This includes praising the client for
coming in and explaining that the discussion is confidential, including the facility’s
confidentiality policy, if applicable. These are both important parts of building
“rapport” with a client developing feelings of safety and trust so that clients will feelcomfortable talking with you about their concerns.
A = ASK the client about himself or herself, his or her family members, and his or
her general life circumstances. Ask the client why he or she has come to the facility.
As the client gives you information about why he or she has come
in, ask probing questions as part of the assessment process.
T = TELL the client about what kinds of services the facility offers, to make informed
choices and good decision, clients need clear, accurate, specific information about
the range of their choices. Let clients understand their possible choices. Information
should be tailored that is important to client’s decision. Information should bepersonalized, put in term of client’s own life.
H HELP the client make the decision that is best for him or her, this does not mean
making the decision for the client; it means helping the client determine if he or she
is at risk and helping the client decide what he or she will do to reduce these risks.
In this way, the provider helps the client to reach a decision.
E = EXPLAIN whatever needs explanation or clarification: how the facility works,
how the decision taken works, explore how the client will follow through on a plan,
explore how the client will confront and address obstacles, the provider explains
to the client how to carry out client’s decision and tries to tailor and personalizeinstructions to suit the individual client’s way of life.
R = Schedule a RETURN visit: Whenever possible, schedule follow-up
appointments with clients to assess their ongoing progress in carrying out their plan
for reducing risk and to make changes in the plan, if necessary. Provide additionalinformation, resources, or referrals, as needed.
Self-assessment 4.3
Differentiate the REDI and GATHER frameworks
4.4 Premarital Counselling
Learning Activity 4.4
In groups of 5 discuss about the definition of premarital consultation and
its objectives.
Premarital counselling helps couples to prepare for marriage. By participating
in premarital counselling prior to their wedding, couples can begin to build a
healthy, strong relationship that helps provide a healthier foundation for their union.
Premarital counselling can help couples of any gender, race, or religion identify
and address potential areas of conflict in their relationship. Additionally, counselling
can prevent small issues from escalating into serious concerns at some point in
the future. Premarital therapy also helps couples identify their expectations for themarriage and address any significant differences they might have.
1. Goals and Objectives of Premarital Counselling
Change the view of the relationship: During the therapeutic process, the
counsellor helps each partner examine the relationship in a more objective manner
and assists the couple in learning how to perceive their interactions in a positive
light.
Understand how cultural issues affect a relationship: Family of origin and
cultural beliefs affect how the partners understand all the relationships in their lives.
It also affects day to day behaviors, such as eating, working, and managing money.
Differences in cultural expectations can cause difficulties in the relationship. The
sooner the couple learns to identify and manage these differences, the better. A
counsellor can help reveal these problems and teach the couple how to use the artof compromise
Eliminate dysfunctional behaviour: Premarital counselling helps couples identify
and correct dysfunctional behaviors, such as issues with dominance and controland addiction.
Improve communication: Effective communication is one of the most important
factors in a healthy relationship. A premarital therapist helps couples learn how
to talk to each other openly and express their thoughts and feelings in a healthy,supportive manner.
Identify strengths: A premarital counsellor can help the couple identify strengths in
the relationship as a whole or in each individual partner. A thorough understanding
of the stronger aspects of the union helps build resilience and a solid foundation
upon which to build the marriage.
Decrease emotional isolation and avoidance: Many people have difficulty
expressing their feelings, so some partners simply avoid doing so. This type of
isolation almost always leads to serious problems in the relationship. A premarital
therapist assists the couple in learning how to express their feelings in a way that
draws them together rather than further apart.
2. Benefits of premarital counselling
The many advantages of premarital therapy include:
Helps build and strengthen conflict resolution skills: Conflict resolution skills
are critical for a healthy marriage. Premarital therapy offers couples a way to
identify potential conflicts and how to develop the skills necessary to get throughtough battles.
Identifies issues early: Different expectations have a disastrous effect on most
marriages. Marriage therapy assists couples in determining and discussing their
expectations early on. If the couple has different expectations, then the counsellor
can work with them to identify ways to cope with those differences.
Helps couples avoid toxic anger: When couples believe they are no longer in
love, it’s usually simply that they have allowed anger to build up in the relationship.
Resentment is toxic to happiness, and during premarital therapy, couples learn
ways to avoid this type of emotional poison.
Reduces fears about the longevity of the marriage: Statistical evidence proves
that marriages end every day, which is concerning to a couple contemplating the
prospect. Premarital therapy helps the couple identify and confront fears aboutforming and maintaining a successful relationship.
3. Common issues addressed in premarital counselling
Premarital counselling addresses a broad range of topics, including these typical
issues:
Conflict resolution: How does each partner resolve conflicts? How do their
perceptions of issues correspond? How can they improve their ability to come to
terms on issues on which they disagree?
Communication: How does the couple communicate? Do they currently have an
adaptive or maladaptive method for discussing important issues? How can they
enhance their ability to communicate?
Define marital expectations and beliefs: What does each partner expect from
the relationship? People sometimes enter relationships with different expectations
as to what constitutes a successful marriage. They often are unaware that their
expectations differ until they are already married, which can lead to serious issues.
A premarital therapist encourages each partner to discuss their expectations, after
which the couple can work toward finding ways to compromise.
Personal values: Do the partners have similar personal values? Research
demonstrates that shared values are more important than common interests, and
couples with the same values have a better chance of staying together.
Finances: Can the couple talk about financial issues? Many people are uncomfortable
when discussing their personal finances, and issues with spending and budgeting
often create conflicts in marriages. The counsellor helps each partner determine his
or her own financial style and then works with the couple in resolving these issues.
Family: Do both partners want to have children? If so, how many children does
each person want? For each partner, what is the optimal time to begin a family?
Sex and intimacy: Are both partners equally comfortable or uncomfortable when
discussing sex? What does each partner expect in terms of intimacy and a sexual
relationship? Couples should speak honestly and openly about sex, even if they
have chosen to remain celibate until marriage. An ability to discuss these issueswithout reservations helps lead to a successful marriage.
4. Steps of premarital counselling
Marriage is an important event of life. It is an untraversed path for the most.
However, marriage has many aspects which many people are not aware of till they
experience it. Men and women both have different physical, emotional and sexual
needs. Even, their way of thinking and perceiving usually differs from each other.
Premarital counselling is a therapy which helps to prepare the couples mentally for
marriage. The counselling helps to make sure that you and your spouse can have
a strong and healthy relationship throughout your life. Premarital counselling helps
to improve a couple’s relationship before marriage.
During the counselling, the counselor a guide that is used in other counsellingespecially in reproductive health.
During premarital counselling the provider uses the steps and topics where the
couple and the provider are engaging in an interactive two ways discussions of the
couples needs following these steps:
• Welcome: welcome the couple politely and warmly. This includes thanking
the couple for coming to the health facility, and explaining the process of
counselling for couples. the provider has to ensure to the couple that the
discussion will be private and confidential. • Provide a safe environment for the couple to feel free of discussing their
• Provide a safe environment for the couple to feel free of discussing their
issues and request for support and ask the reason of consultation
• Inform the couple about all the services that are offered in the health facility.
• Provide support or orientation to the couple depending on their needs during
counselling.
• Schedule a next visit or refer the couple to the next level if they needed
Self-assessment 4.4
1. What are the goals and objectives of premarital counselling?2. What are the steps of premarital consultation?
4.5 Voluntary Counselling and Testing
Learning Activity 4.5
Using textbooks and other resources, work in group and discuss about:
1. The definition of Voluntary counselling and testing (VCT)
2. The expected benefits of VCT for clients and society
Voluntary counselling and testing (VCT) is the process by which an individual
undergoes
confidential counselling to enable the individual to make an informed choice about
learning
his or her HIV status and to take appropriate action. If the individual decides to take
the
HIV test, VCT enables confidential HIV testing. Counselling for VCT consists of
pre-test, post-test and follow-up counselling.
Pre-test counselling includes a private session with a counsellor, who explains
the testing procedure and how the results will be given and gives an individual (or a
couple or group) the opportunity to explore and analyses their situation and consider
being tested for HIV. Each individual makes an informed decision of whether or not
to take the HIV test after they have been given information and supported to reach
an understanding of what is involved after having the chance to ask questions
about the test, and share any fears or worries. Counselling helps people identify the
implications of a negative or positive result.
Post-test counselling supports people in understanding their test result and its
implications, whether the result is positive or negative. Counselling also helps clients
explore whom they might share the test result with, and how to approach sharing
their test result. Follow-up counselling supports clients in coping with issues raised
as a result of learning HIV status, and is relevant for both clients that test positiveor negative.
Benefits of VCT for clients and society
VCT is an effective strategy for facilitating behavior change for both clients that testnegative and Positive and for the society.
To HIV NEGATIVE CLIENTS• Can be a strong motivating factor to remain negative, and supports andTo HIV POSITIVE CLIENTS
enables changes in sexual behavior to avoid infection
• Enables informed decisions about sexual relationships, informing partners of
HIV status, contraceptive methods, safer sex, pregnancy and breastfeeding
• Improves uptake of RH services through referral
• Provides opportunities and support to inform partners of the benefits of being
tested• Supports women/couples to prevent mother to child transmission
• Promotes early uptake of care and support servicesTo society
• Promotes changes in behavior to prevent infecting others with HIV and
prevent becoming re infected with HIV or other STIs
• Supports women/couples to prevent mother to child transmission
• Enables informed decisions about sexual relationships, informing partners of
HIV status, contraceptive methods, safer sex, pregnancy and breastfeeding
• Improves planning for the future
• Supports adherence to anti-retroviral therapy• Promotes awareness and knowledge of HIV/AIDS, potentially leading toCommon barriers to VCT
reduced transmission in the wider community
• Contributes to a more supportive environment for safer sexual behavior
• Encourages openness and reduces fear and stigma surrounding HIV
• Stimulates a community response in support of people with HIV, including the
development of care and support for people living with HIV/AIDS• Supports human rights
In addition to the benefits of VCT, there are also barriers to VCT. It is necessary to
acknowledge and explore these barriers in order to develop strategies to overcome
them.
Stigma
HIV is stigmatized in all countries, resulting in those with the virus experiencing
discrimination or rejection. Fear of rejection or stigma is a common reason for not
wanting to know or disclose the HIV status. VCT itself can be an important strategy
in reducing stigma because, as more people become aware of their HIV status, HIV
will become more normalized.
Lack of perceived benefit
For people living in areas with few resources, there may be a perception that little
support will be available to them if they learn they are infected with HIV. Clients and
the community have to be supported in understanding that people infected with HIV
may remain healthy for many years.
Gender inequalities
Couple counselling in VCT, when conducted in a skilled manner, may play a role
in reducing gender-based violence, discrimination, isolation, or abandonment
experienced by some women who test HIV positive.
Lack of understanding of risk
Many people, particularly in low prevalence areas where knowledge levels about
HIV/AIDS may be low may not perceive that they are at risk. In high prevalence
areas, people may believe that they are already infected. VCT services can help
people understand their personal level of risk, encourage safer sex practices, andsupport people to access care early if they are infected.
Principles of VCT
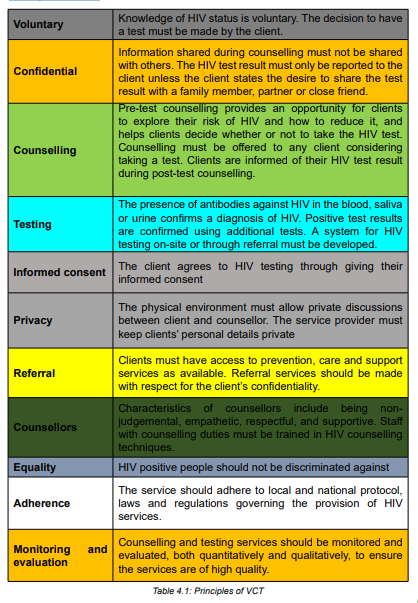
Steps of VCT
The steps of Voluntary Counselling and Testing for HIV as shown in the followingfigure include pretest counseling; testing; post-test counseling.
Pre-test Counselling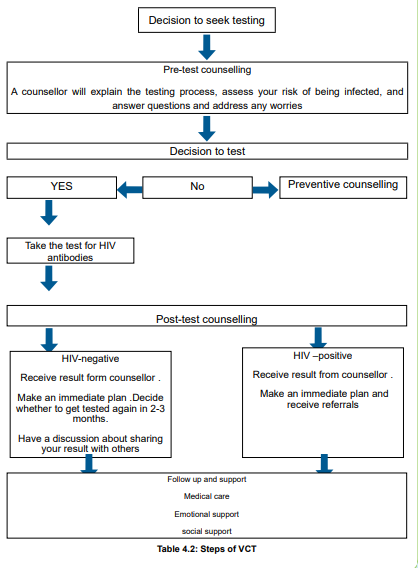
Pre-test counselling should be concise and brief as much as possible and provided
to all people seeking or requiring HIV testing. It may be provided individually, to a
couple, to a group of people or, if necessary, to a parent or guardian (for children
below 12 years, people not in command of all their mental faculties, and people with
disabilities).
Pre-test counselling provided in a group should utilize Information, Education
and Communications/Behavior Change Communication (IEC/BCC) approach and
should provide message about:• Difference between HIV and AIDS,Individual pre-test counselling takes place in a designated counselling area,
• Importance of being tested,
• Importance of index testing (which refers to a focused approach to HIV
testing in which the household, family members (including children less than
15 years for HIV positive mothers) and sexual partners of people diagnosed
with HIV (Index Case) are offered HIV testing services.)
• Partner notification process (refers to health care workers who will ask the
newly diagnosed HIV positive client, to voluntary provide a list of all his/her
sexual or injecting drug use partners, and the list of her children for diagnosing
purposes.
• Modes of transmission,
• Means of HIV prevention,
• Testing procedure and possible results and their significance,
• Availability of care and treatment services
• Demonstration on use of condoms.• The clients have an opportunity to ask questions and receive answers.
where clients are received one at a time and must follow the following steps:• Reception, introduction and screening of client’s eligibility for consentingHIV Testing
process
• Assessment of the client’s knowledge on HIV and AIDS
• HIV risk assessment (Number of sexual partners, condom use, HIV status for
the sexual partner…)
• Preparation for HIV testing and acceptance of test results and its significance
• Provision of information on availability of care and treatment services in case
of a positive result• Obtaining an informed consent for HIV testing
HIV testing can be performed using blood or oral fluids.
HIV testing using blood: uses the finger prick method and follow national HIV
Rapid Test Algorithm approved by the MOH to provide a final HIV test result.
Clients with indeterminate/ inconclusive test results according to the testing
algorithm will return for retesting after 4 weeks with the exception of special cases
required to send sample
immediately for testing using HIV ELISA to include the following: Pregnant women
attending antenatal clinics and delivery room, Couples who seek HIV testing for
marriage, Rape cases.
HIV Testing using oral fluids: Commonly known as HIV Self-Testing, this should
be done by the client him/herself using the OraQuick test kit. A positive result does
not mean that the client is definitely infected with HIV, but additional testing for
confirmation should be done in a health facility using the HIV testing method that
uses blood. If the self‑test result is negative, the individual’s HIV status should be
considered negative. If an individual self-tests and has been recently exposed or is
at ongoing risk; then retesting should be recommended.
The age to which a person is allowed to perform HIV self-testing should be for
persons aged 18 years and above.
HIV Testing algorithm: is serial algorithm that comprises of 2 stage tests:• Alere HIV Combo as First screening test (Alere TM HIV Combo)Current HIV Rapid Test Algorithm• Stat Pak as Second screening test (Chembio HIV 1/2 STAT-PAKR)
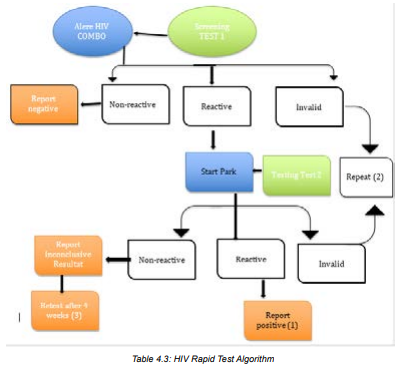
Announcement of the Result
The results of an HIV rapid test are to be given the same day and communication
of the results is verbal. Clients requesting for written results for any reason must be
received/reviewed by the management of the Health facility and provide authorized
written results. Positive or negative results may change depending on many factors
(client exposure after previous test, window period, inconclusive results, sample
and human errors) therefore written results should be interpreted with cautiousness.
Post-Test Counselling
The same person who gave the pre-test counselling should provide post-test
counselling and this process must respect confidentiality. In case the client is a child
below 12 years or an adult not in command of all of his mental faculties, post-test
counselling will be given to the parents or guardian.
In case of negative results:• Post-test counselling should insist on the risk reduction strategies for HIVIn case of positive results:
prevention and the counsellor should give information to the client about
the seroconversion period and its implications. The counsellor should also
encourage clients to bring their sexual partners for HIV testing.
• For high-risk clients who test HIV-negative such as commercial sex workers,
men who have sex with men, or HIV-negative partners in discordant couples,
the counsellor will encourage HIV risk reduction behaviors and the importance
of retesting every 12 months.
• Pregnant women in serodiscordant couple relationships should be encouraged
to retest every 3 months until the end of PMCT follow up period of 24 months’
post-partum.
• HIV Negative clients who are not at high risk of HIV infection should be
advised to keep protecting themselves against HIV and plan to retest only
after any other exposure.
• HIV Negative clients who have HIV positive partners (discordant couple) who
are not virally suppressed should be initiated on pre exposure prophylaxis
• HIV risk reduction plan (Abstinence, Being faithful to one partner
• Condom use, Don’t share needles, Education and information for behaviorchange (ABCDE)
• Post-test counselling will encourage on risk reduction and secondarySelf-assessment 4.5
prevention of HIV infection.
• HIV-positive clients should be referred to a comprehensive HIV care and
treatment unit for enrolment, ART initiation and follow-up.
• Enrolment into care and initiation to ARVs should be done the same day as the
diagnosis day taking into consideration the client’s readiness to initiate ART.
For those clients not ready requiring more preparation should be preferably
initiated on ART within a week maximum.
• Clients must be encouraged to live positively, to reduce further exposure, and
to avoid transmitting new infections to others.
• Clients are advised to disclose their status to their sexual partners and invite
them for HIV testing. For female clients who test positive and have children,they are encouraged to bring them in for testing as well.
1. What does the pre and post-test counselling includes?2. What are the steps of VCT?
4.6. End of unit assessmentEnd of unit assessment
Margarita and Martin are a young couple that want to wed anytime soon. The
lady presents herself to the health center to VCT prior to her fiancé for a VCT.
later alone the man came and they want each to have VCT and premarital
counselling.
While you plan to give a session you should be able to answer the following
questions:
1. What are the common barriers to VCT?
2. What are the principles of VCT?
3. Differentiate the REDI and GATHER counselling frameworks and decide
which one to use.
4. Name each phase of REDI:
R = ______________________________
E = ______________________________
D = ______________________________
I = ______________________________
5. The benefit of following a counseling framework, like REDI, is thatit provides a structure for talking with clients
UNIT 5: Counselling in Reproductive Health related conditions
Key Unit competenceProvide counselling in reproductive health related conditions
Introductory activity 5
Using textbook or other sources of information discuss in group of 5 about the
images A, B and C and answer the following questions.a. What do you know about PMTCT?5.1. PMTCT (Prevention of mother to child transmission)
b. According to you, why do you think is the difference between STIs and HIV
counselling?
c. What do you think is involved in counselling for STIs and HIV?d. Mention the stages of counselling for STIs and HIV.
5.1.1 Introduction to PMTCT (Prevention of mother to childtransmission)
Learning Activity 5.1.1
Using different source of information (internet, books or any other source of
information), answer the following terms:
1. Explain how HIV can be transmitted to babies through the mother.
2. What do you understand by the term Prevention mother to child transmissionof HIV?
Knowledge of HIV status, through HIV testing and counselling, is especially important
during pregnancy, childbirth, and breastfeeding, since women with HIV can transmit
the virus to their babies during these times. These different transmission routes of
HIV from the mother to the baby is termed ‘mother-to-child transmission of HIV’.
In HIV-positive pregnant women, the virus is found abundantly in the birth canal
(cervix and vagina) and in the mother’s blood.
Therefore, if the baby is exposed to vaginal fluid or to the mother’s blood during
labour and delivery, there is an increased chance of mother to child transmission(MTCT) occurring.
If anything breaks the barrier between the placenta and the wall of the uterus, there
will be an increased the risk of MTCT of HIV.
As a nurse, you should encourage all pregnant women to consent to be tested for
HIV. Explain to every pregnant woman that if her HIV test result is positive, she
can receive effective services to prevent her baby from getting HIV before or after
birth. The main PMTCT goals include early identification of pregnant women with
HIV, to reduce new pediatric HIV infections, and providing mothers and babies with
appropriately and timely manner to prevention, care, and treatment services. To
achieve these goals, health providers should provide counselling to women and
their families through the following activities:• To help clients to understand what actions they can take to prevent the
transmission of HIV to their children.
• To assist women and men to minimize the risk of HIV infection during
conception and pregnancy.
• To provide information on the extra risk of transmission to the child if mother
is infected during pregnancy or breast-feeding.
• To help mothers and families to weigh up the benefits and risks of differentinfant feeding options.
Self-assessment 5.1.1
1. What is the PMTCT main goal?2. What are the objectives of PMTCT?
5.1.2. Counselling pregnant women and their partners about PMTCT
Learning Activity 5.1.2
In a group of 5, Using different source of information (internet, books or any
other source of information) search and discuss PMTCT approaches and be
prepared for class presentation.
i) Describe how you can provide counselling to the pregnant woman and her
male partner.
Efforts to prevent mother to child transmission of HIV should be as comprehensive
as possible and acknowledge that both mothers and fathers have an impact on
transmission of HIV to the infant:• Both partners need to be aware of the importance of safer sex throughout
pregnancy and breastfeeding.• Both partners should be tested and counselled for HIV.
• Both partners should be made aware of and provided with PMTCT
interventions.• Both partners should be provided with condoms.
When the male partner is involved and informed, the woman is more likely to be able
to participate in PMTCT interventions. Some things that help prevent transmission
from mother-to-child, such as exclusive replacement feeding or exclusive
breastfeeding, can be difficult for women to adopt, especially if they do not share
their HIV status with family. Not only men will be supportive but also it is very crucial
that the partner’s HIV status in case of discordant couple. The partner’s serologicalstatus helps in provision of health education for HIV prevention or management.
Although the woman’s partner’s involvement is vital, as a nurse, you should
appreciate that when providing counselling to pregnant women, you need to assure
her of confidentiality. This means that only health staff directly involved in her care
will know her test results. Otherwise, let the woman decide herself if and when she
wants to share her test results with anyone else including so they can then talk with
you as a couple about these issues, to help them better understand risks, and findsolutions that are agreeable to both.
Many couples are successful in adopting safer sexual practices. It is often helpfulto offer to counsel the couple together
Self-assessment 5.1.2
i) What the nurse should appreciate when providing counselling to the
pregnant woman?ii) Why it is important to counsel the couple together?
5.1.3. PMTCT pre-test counselling
Learning Activity 5.1.3
i) Mention at least three topics covered during the pre-test counselling of the
PMTCT sessions.
ii) What precautions do you need to take if the woman refuses to take an HIVtest?
Counselling during routine antenatal and postpartum care is an important way to
reach women with information about HIV/AIDS and encourage HIV testing. Women
receive pre-test counseling that covers comprehensive information on HIV/AIDS,
including the difference between HIV and AIDS, the importance of being tested,
modes of transmission, means of prevention, possible results and their implications,availability of care and treatment services.
HIV counselling and testing (HTC) is recommended for pregnant women as a key
component of the package of care in all antenatal services. All pregnant mothers
attending ANC will receive HTC preferably with their partners at the time of their
first visit to ANC.
Strong emphasis will continue being put in male partners’ involvement in PMTCT
cascade, starting by ANC together with couple’s HIV counselling and testing. Some
of the topics covered during the PMTCT counselling include:• basics of HIV transmission and prevention;• HIV testing processes;
benefits and risks of HIV testing;
• right to refuse testing (opt-out);• implications of positive and negative test results;At some time, a woman may refuse testing and counselling. In that case, as
• identification of supportive HIV services and treatment available;
• identification of PMTCT services and treatment available;
• identification of sexual risks and plan for reduction of risks;• Importance of infant feeding and nutrition.
a counsellor, you need to spend a bit of extra time with her to find out why she
refused. Use open questioning and active listening skills, and see if you can help
her with any problems related to accepting the HIV test. But remember to present
the information in a neutral, non-biased way without judgement. As a counsellor,
you should appreciate that some women may be afraid to get an HIV test, do not
want to know their HIV status, or do not want to discuss results with their partner.
Counselling women about the benefits and risks of knowing their HIV status, not
only for themselves but for their infant and partner, can help to overcome the fearof stigma, discrimination and other barriers.
Self-assessment 5.1.3
i) Why is it important to provide counselling during routine antenatal care?
ii) What are some of the reasons that may lead some women to not test
themselves of HIV?
iii) How can you address those issues during your pre-test counsellingsession?
5.1.4. PMTCT Post-Test counselling
Learning Activity 5.1.4
i) What are the goals of posttest PMTCT counselling?ii) What topics are covered during the post-test PMTCT counselling?
Post-test counseling should be provided by the same person who gave the pretest
counseling. Post-test counselling for a pregnant woman who has tested
HIV-negative should focus on helping the woman decide how she can stay HIV negative.
If the woman is not with her partner, support should also be provided to
help her decide if she will discuss her results with her partner. Post-test counseling
will insist on the risk reduction and HIV prevention strategies and the counselorshould explain to the client about the seroconversion period and its implications.
Negative clients who are not at high risk of HIV infection should be advised to keep
protecting themselves against HIV seroconversion and plan to retest only after any
other risky contact. Negative clients who are at high risk should be advised to
get tested every six months.
The main ways to prevent HIV infection and STIs:
• Correct and consistent use of condoms during every sexual act;
• Practising safer sex (choosing sexual activities that do not allow semen, fluid
from the vagina, or blood to enter the mouth, anus or vagina of the partner, or
to touch the skin of the partner where there is an open cut or sore.)
• Reducing the number of partners
• Sexual fidelity• Abstinence.
In case of Positive results, posttest counselling will insist on linkage to care and
treatment. Post-test counselling for pregnant women who are diagnosed with an
HIV infection should include the following, in addition to the standard messages
described above for all people diagnosed with HIV infection:• childbirth plans: providers should encourage HIV-positive pregnant womeni) What should be done in case of HIV negative results?
to deliver in a health facility for their own well-being as well as to ensure
access to PMTCT services;
• use of ARVs for the client’s health, when indicated and available, as well
as the use of ARVs to prevent transmission to the infant;
• the importance of partner testing and information on the availability of
couples testing services;
• ensuring screening for TB and testing for other infections such as syphilis;
• counselling on adequate maternal nutrition, including iron and folic acid;
• advice on infant feeding options and support to carry out the mother’s infant
feeding choice;
• HIV testing for the infant and needed follow-up for HIV-exposed infantsSelf-assessment 5.1.4
ii) What other messages would you focus on when counselling a woman witha positive HIV test?
5.2. Counselling for Sexually Transmitted Infections
5.2.1. Counselling a client before taking a STI test
Learning Activity 5.2.1
i) Why is it important to provide counselling to a client before taking the STI
test?ii) Explain with examples counselling targeting the prevention of STIs.
Globally, more than 1 million sexually transmitted infections (STIs) are acquired
every day worldwide, the majority of which are asymptomatic. Every year, an
estimated 374 million new infections with 1 of 4 STIs: chlamydia, gonorrhoea,
syphilis and Trichomoniasis occur. Research shows that about one million pregnant
women get infected with syphilis which in turn results in over 350, 000 adverse birth
outcomes including 200,000 stillbirths and newborn deaths. When left untreated,
STIs have direct impact on sexual and reproductive health through stigmatization,infertility, cancers and pregnancy complications and can increase the risk of HIV.
Counselling a client before taking a test of STIs is important for both the primary
and secondary prevention of STIs. Counselling to prevent STIs includes any
intervention that aims to reduce an individual’s likelihood of acquiring an STI. The
primary prevention is very significant because it reduces the risk of acquiring an STI
and it aims to promote the following behaviours:– Reduction of the number of partners;For the secondary prevention, counselling aims at reducing the complications of
– Advise an individual to adapt low risk sexual practices;
– Consistent and correct use of condoms when in engaged in sexual
intercourses.
STIs. It seeks to promote treatment seeking behaviours among people who suspect
they have been infected and further promote safe sex behaviours outlined in Figure
below.
Table 5.1 Sexual activities with their risk of STIs/ HIV infection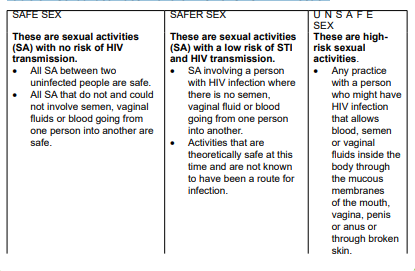
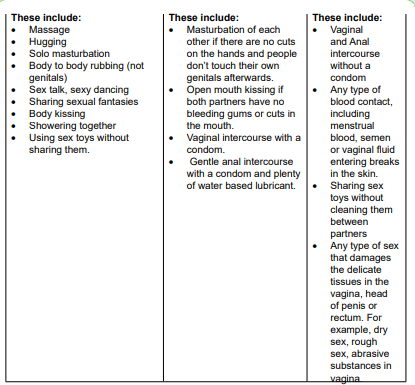
Self-assessment 5.2.1
i) With examples, explain the term ‘unsafe sex practices.
ii) Why is primary prevention needed when offering counselling about STIs?
iii) Learn to provide counselling for STIs testing. Using a role play, create a
sketch of five minutes in which you counsel a client coming to seek STIstesting services.
5.2.2. Helping clients to assess their risk of STI and HIV infection
Learning Activity 5.2.2
When helping a client to assess his/her risk of STI and HIV infection:
i) How do you start the counselling?ii) What are the sexual activities a client may not talk about easily?
Once the client accepts to proceed with counselling, as a nurse, you may find it
easier to begin to talk about the risk of STI. To proceed, a counsellor shares with the
client knowledge about how STI/HIV is transmitted and then explores the possibility
of transmission in clients’ lives. This is done through helping the client reflect on
their past and present sexual practices and drug-using behaviour and further reflect
on whether this may have put them at risk of STI. Moreover, the counsellor needs to
also guide the client to recall on their medical history and whether there might havebeen any risk of contracting HIV from blood transfusions.
While assessing the risk of HIV transmission, help clients to talk about all their sexual
activities and partners. Do not make any assumptions about clients’ sexual activity
nor the activity of their sexual partners. The client may have or have had partners
of the same sex or the opposite sex now or in the past. A married person may have
relationships outside marriage or their partner may have such relationships. An
adolescent may be abused at home.
As you explore this, provide information on the level of risk of different sexual
activities. Probe about other possible activities that the client may not have thought
significant or may not like to mention. Discuss each of their concerns in detail,
learning about their understanding of HIV and adding information as needed. When
you have covered all their concerns, ask about any risk factors that they have not
mentioned. When you have talked over all the issues, summarise the main pointsand ask how the client feels about their likely risk.
If clients come to you expressing concerns about STI, affirm their sense of
responsibility and decision to take action, and assure them of confidentiality. Each
client will have their particular needs, so as a counsellor, you should acknowledge
and appreciate individuals’ differences when providing counselling. For this reason,
it is essential to give all clients an opportunity to discuss and get help on any aspect
of their sexual lives. To achieve this, the counsellor asks a question like “Would you
like to discuss anything concerning STIs? If you are busy today, we could arrangeanother time”.
If clients do not wish to talk about STI or HIV, only do what you can to ensure that
they are aware of the potential risk of STI and what they can do to reduce thoserisks.
Self-assessment 5.2.2
i) Using role play, create a scenario on how you can encourage a client todiscuss their concerns about STIs fears
5.2.3. Counselling a client with an STI diagnosis
Learning Activity 5.2.3
Mr Gakuru was aged 30 years and married. He was worried about STIs because
of symptoms he had. He informed his counsellor during the risk assessment for
STIs that he had unprotected sex with other three different women. He was
diagnosed to have signs of STIs but the HIV test was negative.i) Why do you think it is important to assure privacy and confidentiality when
taking client STIs history?
ii) Which precautions to be taken when providing post STI is diagnosis?iii) Why informing the partners the STI diagnosis is necessary?
When providing counselling for a person already diagnosed of STIs, complete
privacy is necessary. To facilitate open communication between the counsellor and
the client, the following steps need to be) followed:– Affirm your client and assure her or him of confidentiality.their genitals passed through sexual intercourse. Explain and answer the
– Encourage your client to tell you about any signs and symptoms, recent
sexual interactions, fears and what they have already done to try to solve the
problem.– Explain that the examination or test showed that they have an infection in
client’s questions about it.– Explain that STIs can have serious consequences if they are not treated asWhen announcing the results of the screening STI test, as a counsellor you need
quickly as possible.
– Explain the potential consequences of your client’s particular STIs if they are
not treated.
– Explain that most STIs are curable if they are treated early with a complete
course of the correct drugs.
– Explain about the prognosis for your clients STI. Stress the importance oftaking the full course of correct drugs.
to acknowledge the following:
– Explain to the clients why they need to tell all their sexual partners about the
infection so that they get treatment because partners can re-infect each other
every time they have sex if they are not both treated.
– Acknowledge that for some people, it is difficult to disclose their STI infection.
You need to foster trust while providing counselling so that individuals
understand the importance of disclosing their STIs infection to their partners.
– If clients are anxious about telling their partners or are not able to do so,
explore alternatives with them. Take great care not to push them into a
potentially dangerous situation.
Ask:
– “Is there a relative, friend or community member who could help you to do this
and mediate in any quarrels?”
– “Would it be helpful to counsel your partner alone or together with you?”
– Both partners should abstain from sex until they are completely cured. If they
are unable to do this, they should use condoms each time they have sex.
– Explain that STIs increase the risk of HIV. Stress the importance of preventionof STI and ask if clients wish to consider taking an HIV test.
If the clients are in a relationship, you will need to counsel them on how they
need to restore and maintain harmony in their relationship. This is because STIs
frequently result in conflicts because they imply that one or both parties have had a
relationship outside. While offering STI counselling, you will need to ask the client
how she or he is feeling. Give her or him time to express their feelings about the
situation. Some ways to express that include asking questions like:
“I see that you are feeling very angry that your partner has given you this infection,is that right?
Would you like to tell me more about what you are feeling”?
– If you are counselling a couple, give them a chance to say how they feel to
each other while the other person really listens.
– Give positive examples of couples who have been in this situation and comethrough it and are still together.
Self-assessment 5.2.3
i) Why the follow-up plan is necessary when counselling a STI client?
ii) Mention the key steps you can follow when offering counselling post STIs
screening.
iii) Mrs X is a married woman. She has come for STIs test and the results of
the screening shows that she has gonorrhoea. She is afraid of disclosing
her result to her male partner because she fears she will be stigmatized.
Create a scenario on how you will counsel her to disclose her result.
5.3 HIV counselling5.3.1 Introduction to HIV counselling
Learning Activity 5.3.1
Read chapter two about counselling skills and processes found in the book
‘Programme guidance on Counselling for STI/HIV prevention in sexual and
reproductive health settings’ and answer the following questions:i) According to what you have read, explain the term ‘HIV counselling’?HIV counselling is a confidential dialogue between a client and a counsellor aimedii) What are the components of HIV Counselling?
at enabling the client to cope with stress and take personal decisions related to
HIV/AIDS. The counselling process includes evaluating the personal risk of HIV
transmission, and discussing how to prevent infection. It focuses specifically on
emotional and social issues related to possible or actual infection with HIV and to
AIDS. With the consent of the client, counselling can be extended to spouses, sex
partners and relatives. As a counsellor, you need to appreciate that counselling
should only take place with the patient’s explicit consent.
HIV and AIDS counselling has two general aims: (1) the prevention of HIV
transmission and (2) the support of those affected directly and indirectly by HIV.
The topics below can be discussed during the counselling sessions:
Adjustments to sexual behaviour and other lifestyle issues;
– Misconceptions about HIV transmission;
– Safer sex practices;
– The partner’s and the patient’s psycholoogical responses to the diagnoses or
result, such as anxiety or depression;
When patients know that they have got HIV infection, they may suffer great
psychosocial and psychological stresses through a fear of rejection, social stigma,
disease progression, and the uncertainties associated with future management of
HIV. Therefore, providing counselling plays a role in addressing these concernsand helps an individual to adapt safe sexual practices.
Self-assessment 5.3.1
i) What are the aims of HIV counselling?
ii) What are the difficulties that people diagnosed of HIV may suffer?iii) How can counselling about HIV mitigates these difficulties?
5.3.2. Pre-test HIV counselling
Learning Activity 5.3.2
Watch the video titled ‘HIV Testing and counselling’ found on this link ‘https://’ and answer the following questions.
i) What to do you understand by the term pre-test counselling?
ii) Why is it important to provide pre-test counselling before screening a clientof HIV?
Pre-test counselling refers to a private session with a counsellor, who explains
the testing procedure and how the results will be given to an individual client.
During this session, the counsellor gives an individual (or a couple or group) the
opportunity to explore and analyse their situation before they an informed decision
of being tested for HIV. Pre-test counselling helps to prepare the client for the HIV
test, explains the implications of knowing that one is or is not infected with HIV, and
facilitates discussion about ways to cope with knowing one’s HIV status. It also
involves a discussion of sexuality, relationships, possible sex- and drug-related risk
behaviours, and how to prevent infection. It helps correct myths and misinformationaround the subject of AIDS.
Clients may present for testing for any number of reasons, ranging from a
generalized anxiety about health to the presence of HIV related physical symptoms.
For people at minimal risk of HIV infection, pre-test discussion provides a valuable
opportunity for health education and for safer sex messages to be made relevant to
the individual. For clients who are at risk of HIV infection, pre-test discussion is anessential part of post-test management.
Self-assessment 5.3.2
i) How does pre-test counselling contribute to HIV testing?ii) Why pre-test counselling is important for people with minimal risk of HIV?
5.3.3. Post-test counselling of HIVLearning Activity 5.3.3
Open this link ‘’
Watch the video titled ‘HIV Post-test Counselling for Medical Students’ and
answer the following questions:i) Based on the video you have watched, what is involved in providing thePost-test counselling supports people in understanding their test result and its
HIV counselling.
ii) With examples, explain how you can provide counselling to a person witha negative HIV result.
implications, whether the result is positive or negative. Counselling also helps
clients explore whom they might share the test result with, and how to approach
sharing their test result.
During the post-test counselling, the counsellor prepares the client for the result,
gives the result and then provides the client with any further information required,
if necessary, referring the person to other services. The counsellor and the client
usually discuss ways to reduce the risk of infection or transmission. HIV test results
should always be given with counselling. The form of post-test counselling will
depend on what the test result is. The same person who gave the pre-test counselling
should provide post-test counselling and this process must respect confidentiality.
Post-test counselling will encourage on risk reduction and secondary prevention ofHIV infection depending on their test result.
For people who test HIV-negative, a counsellor provides them with health information
about their HIV status report, how to prevent acquisition of HIV in the future, and
where and how to link to HIV prevention services. People with significant ongoing
risk may need more active support and linkage to HIV prevention services. In
addition, counselling should also consider the following:• provision of male or female condoms, lubricant and guidance on their use;When the HIV test is positive, the counsellor needs to tell the client clearly, and as
• emphasis on the importance of knowing the status of sexual partner(s),
• information about the availability of partner and couples testing services;
• referral and linkage to relevant HIV prevention services, including voluntary
male medical circumcision (VMMC), Post exposure prophylaxis for people at
substantial ongoing HIV risk;
• For high-risk clients who test HIV-negative such as commercial sex workers,
men who have sex with men, or HIV-negative partners in discordant couples,
encourage HIV risk reduction behaviors and the importance of retesting every12 months.
gently and humanly as possible, providing emotional support and discussing with
the client on how to cope with the result and life thereafter. Ongoing counselling need
to be scheduled to help clients accept their HIV status, and take a positive attitude
to their lives. In those ongoing counselling sessions, the counsellor needs to help
clients understand that good medical care and nutrition are important to prolong
their life. Clients should be helped to understand that there are anti-retroviral drugs
(ARVs) which slow down the development of AIDS. In addition to ARVs, there are
vitamin supplements that clients can obtain from health services.
Indeed, the shock of learning of an HIV-positive diagnosis may make it difficult for
a person to take in further information immediately. Therefore, counselling just after
announcing the result should consider the following:• Explain the test results and diagnosis.
• Give the client time to consider the results and help the client cope with
emotions arising from the diagnosis of HIV infection.
• Discuss immediate concerns and help the client decide who in her or his
social network may be available to provide immediate support.
• Provide clear information on ART and its benefits for maintaining health and
reducing the risk of HIV transmission, as well as where and how to obtain
ART.
• Make an active referral for a specific time and date.
• Discuss barriers to linkage to care, same-day enrolment and ART eligibilityassessment.
• Arrange for follow-up of clients who are unable to enrol in HIV care on the daySelf-assessment 5.3.3
of diagnosis.
• Provide information on how to prevent transmission of HIV, including
information of the reduced transmission risk when virally suppressed on ART;
provide male or female condoms and lubricants and guidance on their use.
• Discuss possible disclosure of the result and the risks and benefits of
disclosure, particularly among couples and partners.
• Encourage and offer HIV testing for sexual partners, children and other
family members of the client if any. This can be done individually, through
couples testing, index testing or partner notification.
• Assess the risk of intimate partner violence and discuss possible steps to
ensure the physical safety of clients, particularly women, who are diagnosed
HIV-positive.
• Assess the risk of suicide, depression and other mental health consequences
of a diagnosis of HIV infection.
• Provide additional referrals for prevention, counselling, support and other
services as appropriate (for example, TB diagnosis and treatment, prophylaxis
for opportunistic infections, STI screening and treatment, contraception, ANC,and access to sterile needles and syringes, and brief sexuality counselling).
i) Mention at least two risks associated with a positive HIV test result.
ii) How can you support a high-risk client who get a negative HIV test result?
iii) Client X has been tested of HIV and his result turns to be positive. Elaborate
in a sketch of no more than six minutes how you can provide counselling tothis client while announcing the result to him.
5.4. End of unit assessmentEnd of unit assessment
Madam K came have been married to Sir K for the past 7 years. They have
3 children together and they are planning to have a last born. It was a sunny
Thursday, when Madam K planned to go to the market and pass by the children
school to pay their school fees.
On her way home, she did not feel alright and she decided to pass by the nearest
health center to consult.
After assessment, the nurse at the HC the nurse informed her that she is pregnant
and she should start ANC, and requested her to come back in morning to give
other laboratory tests with her husband. Madam K left the HC happy, ready to
announce to her family her pregnancy.
To reach home, she met a woman coming out of her room where her husband
was. She got confused and started crying.
In the next morning she convinced her husband to go with her at the HC, where
they were received by the nurse who gave them the appointment. Madam K
started by explaining to the nurse her worries that her husband may be cheating
on her while she is pregnant and requested for her help.1. What type of counselling should the nurse take this couple through and
why?
2. What are the main ways to prevent HIV infections and STIs that the nurse
provides during the couple counselling?
3. Why do nurses need to create awareness among partners on PMTCT?
4. Why is it important to involve partners during PMTCT Counselling?
UNIT 6: COUNSELLING IN GENDER BASED VIOLENCE SITUATIONS
Key unit competence:Provide counselling in Gender Based Violence situations
Introductory activity 6
i) Based on the above pictures, would you please tell us what is happening?
ii) Mention the after effects of such society?iii) What counselling can be given in this situation?
6.1. Introduction to counselling in Gender based violence inrelated situations
Learning Activity 6.1
Watch this video on gender-based violence find it on this link: https://www.
youtube.com/watch?v=aBLsWpymxsg answer the following questions.a) What do you understand by the term gender-based violence?6.1.1. CONCEPT OF GENDER BASED VOLENCE
b) Briefly mention the types of gender-based violence according to the abovevideo.
Gender based violence is referred to any harmful acts which is directed to an
individual based on gender or sex, can be either a woman or a man.it is embedded
in gender inequality, the abuse of power and harmful norms. GBV is serious violation
of human rights and life threatening on one’s health and protection concern. They
are many forms of violence in the society e.g Violence against women and girls
(VAWG), Intimate partner violence (IPV), Domestic Violence (DV), Sexual Violence.Etc…..
GBV happens everywhere, at home, at school, in the workplace or in the community
in the broadest sense. Domestic violence, “the most prevalent form of GBV, includes
forced sexual intercourse between spouses, incest, attacks on honor, deadly
struggles for honour, female infanticide, corporal punishment of children, femalegenital mutilation.
Gender based violence can base on many factors like, Cultural factors, legal
factors, social-, economic factors and political factors. This violence is characterized
by the direct violence against an individual based on gender and breaches the
fundamental rights of life, liberty, security, dignity, equality between women and
men. Gender based violence affects a person’s sense of self-worth and self-esteem.
it also affect physical and mental health which leads to self-harm, isolation,depression and suicidal attempts.
6.1.2. TYPES OF GENDER BASED VIOLENCE
Gender-based violence is a serious human rights abuse that can lead to long-term
and life-threatening harm and trauma to the victims or survivors. It has severaltypes:
1. Intimate partner violence
An act or threat of violence or emotional harm and emotional towards a current
spouse, acquaintance or partner or Ancient.
2. Sexual violence
In this type of violence there is actual, attempted or threatened (vaginal, anal, or
oral) rape, it involves marital rape: sexual abuse and exploitation; forced prostitution;
transitional/ survival sex; sexual harassment, intimidation and humiliation.
3. Physical violence
This is when there is actual, attempt or threatened physical assault; slavery or slave
like practices and human trafficking. Some examples of physical violence are the
following: beating, kicking, biting, hair pulling, strangling, causing injury, causingdisability.
4. Emotional and psychological violence
In this category of violence, one will be abused and humiliated like assaults; cruel
and degrading treatment: convincing a person to get involved in humiliating acts
and placing restrictions on liberty and freedom of movement. The following are
examples of Emotional and psychological violence like verbal abusing, humiliating,
intimidating harassment, persecution forcing to burn forcing to suicide forcing to
use poison
5. Harmful traditional practices
Harmful traditional or cultural practice include female genital mutilation/forced
marriage; child marriage; honour or dowry killings or maiming; infanticide, sex
selective, abortion practice; sex-selective neglect and abuse; denial of education
and economic opportunities for women and girls.and economic opportunities for women and girls.
6. Social-economic violence
This involves discrimination and denial of chances or services on the basis of
gender, sex or sex orientation social exclusion, obstructive legal practice like denial
of the exercise and enjoyment of civil, social, economic, cultural and political rights,mainly to women and girls.
Self-assessment 6.1
a. What do you understand by gender-based violence?b. Explain the types of gender-based violence you know?
6.2. Main Causes of gender-based violenceLearning Activity 6.2
a) Briefly mention the causes of gender-based violence in the society?b) Enumerate the consequences of gender-based violence?
1. Lack of physical security
There is lack of physical security owing to break-down of law and order, presence
of armed forces/groups, collapse of law enforcement, justice institution and family,
social or community strictures. women and girls are particularly vulnerable when
leaving their communities in such of work, food, water and firewood. In addition,
poverty also leads to lack of education, and livelihood opportunities, and inadequate
access to shelter, food, water, fuel, and income generation can increase exposureto GBV like forced prostitution or survival sex.
2. Social, cultural, political factors
Discriminatory social, cultural or religious laws, norms and practices that disregard
women and girls, where by their rights are not respected. Failure of family, social and
communal structures and disrupted roles within the family often women and girls
to risk with limited coping mechanism avenues for protection and redress. Lack of
self-confidence and trust in social or public institutions, including law enforcement
and justice institutions that discourage victims from looking for redress.
3. Judicial barriers of factors
Lack of access to justice institutions and fairness, leading to cultural impunity for
violence and abuse.
Lack of suitable and affordable legal advice and presentation
Inadequate legal framework including national, traditional, customary and religious
law, that discriminate against women and girls, fails to guarantee their rights, or
exposes them to further harm and abuse like national law may fail to guarantee acertain right, fail to criminalise some acts like rape or narrowly explains it.
In some instances, national law criminalizes the survivor e.g. (rape defined as
adultery) or criminalizes acts that allegedly are primarily associated with women
like witchcraft or sorcery. In certain instances, victims face harassment, intimidationor severe punishment.
4. Individual barriers
There is fear of stigma, segregation and social exclusion, exposure to further
violence at the hands of the offender, the community or the authorities, including
arrest, detention, mistreatment and punishment. Lack of information on humanrights and on how and where to seek advice.
5. Humanitarian programing obstacles
Failure to address or prioritise GBV assessments, strategy development, planning
and programming because of a lack of information or understanding about the
extent or nature of GBV. Lack of gender-sensitive design programmes, services
like inadequate registration practices and distribution of food and other items.
Sexual exploitation and abuse by peacekeepers, human rights and humanitarian
workers. Lack of confidentiality, confusing reports and referral mechanisms and
GBV committees that are isolated, under-resourced and weak, and lack of supportfrom the wider community.
6.2.1. Consequences of gender-based violence.
Gender-based violence can have severe long-term and life-threatening effects
or consequences for survivors or victims. The consequences can range from
temporary, permanent disability or death to a variety of physical, psycho-social and
health related issues that often destroy the survivor’s self-worth and quality of life,and expose her to further abuse. Below are some of the consequences.
The examples of fatal consequences in gender-based violence are: homicide,suicide, maternal mortality, HIV/AIDS.
Acute physical consequences in gender-based violence include: injury including
fistulas, shock, disease, infection
Chronic physical consequences: disability, chronic pain or infection,
gastrointestinal problems, eating or sleeping disorders, alcohol or drugs abuse
Reproductive consequences: miscarriage, unwanted pregnancy, unsafe abortion,
including HIV/AIDS, menstrual disorders, pregnancy complications, gynecological
disorders, sexual disorders
Emotional and psychological consequences: post-traumatic stress, depression,
anger, anxiety and fear, shame, self-hate and self-blame, mental illness, suicidal
thoughts and behaviour.
Social and economical consequences: blaming of the victim/survivor, loss of role
or functions in society, social stigma, rejection and isolation, feminization of poverty,
increased gender inequalities, loss of livelihood and economic dependency, arrest,
detention and punishment.
Self-assessment 6.2
a) Briefly mention the causes of gender-based violence in the society?
b) Using example, discuss how the GBV has impact on Social and economicalin the society?
6.3. Counselling in gender-based violenceLearning Activity 6.3
a. In your own understanding, explain the concept counselling?
b. Enumerate the aims of the counselling in gender-based violence?c. How can you provide the counselling in case of gender-based violence?
6.3.1. Introduction to Counselling in gender-based violence
GBV is a public health issue. Addressing GBV in a health care facility is one
important means of
intervening in this public health problem. In this context, the focus for the assessment,
intervention and treatment of GBV is on secondary and tertiary prevention. This
can involve screening for early intervention (secondary prevention) and intervening
to minimize the severity of long-term abuse (tertiary prevention). The health care
providers receive the victims in case of gender-based violence who need the
counselling.
6.3.2. Concept of counselling
Counselling, also translated as “helping relationship, consists of engaging in a
sequence of verbal or non-verbal interventions with the aim of making it easier for
victim the expression, understanding and management of his or her experience. It
must make it possible to create between the victim and the service provider a climate
of trust and of interaction allowing the victim to feel comfortable in discussing the
violence suffered without shame or guilt.
Aim of counselling:– Decrease emotions that destroy the victim6.3.3. Rights of gender-based violence victims/ survivors
– Be an objective mirror: help to understand the extent of the problem as it
actually is
– Make responsible without feeling guilty
– Build new values, convictions that will permanently change your life
– Help to understand his role– Support and accompany for social reintegration
Before engaging in the counselling process, it should be noted that the victim has
the right on:
Information: Being informed of the advantages of the availability of management
of GBV and its use.
Access: To benefit from services without distinction of sex, age, religion, race,
origin, marital status or place of residence.
Safety: Refer her to an authority or a place that ensures her safety physical and
psychological
Intimacy: Having a consultation in private
Confidentiality: Be guaranteed that professional secrecy will be respected
Dignity: Being listened to and treated with respect
Comfort: Benefit from suitable reception conditions and services
Continuity: Benefit from follow-up services for as long necessary
Opinion: Freely expressing one’s opinion on the services provided
6.3.4. Elements of counselling in gender-based violence
When counselling the victim of gender-based violence, the counsellor
should consider the elements following:• Preparatory phase (suitable location, availability of everything necessary,6.3.5. Techniques used in counselling of gender-based violence
• Reception and maintenance
• Say hello, welcome and offer a seat
• Introduce yourself and others if present to put the client in confidence and
comfortable
• Reassure the victim and assure him of your willingness to help and
confidentiality of your interview (speak without raising your voice, have a
place discreet and recall the private nature of the interview).
• Ask the victim what happened
• Encourage the victim to speak up
• Listen and reassure the victim and those accompanying them
• Show availability and demonstrate attentive listening
• Ask for details on the circumstances of the acts of violence and their
frequencies
• Ask the victim if she has no questions to ask
• Assess and try to meet the needs of the victim in order to alleviate the effects
• Collect useful information
• Explain to the victim and those accompanying them the importance of urgent
PEC for the survivor and inform about the services available.
victims
Several Communication counselling techniques in gender-based violence
are used as follows:
What is encouraging: effective communication?
Look at the person appropriately
Encourage him with nods, smiles, gestures
Make small noises of encouragement (“Hmm… hmm”) and restart the story
with little words (“And after?”, “And then?– Be empathetic, patient, tolerantAsk questions to clarify a subject, ask for details
– Show interest, listen carefully
Facilitate the victim to make good decisions (concrete and specific)– Do not interruptWhat is discouraging (to avoid)
– Do not judge or criticize
– Be neutral
– Arouse the evidence that we can trust you
– Maintain an adequate physical distance• Stare with a “hard”, insistent, investigative gazeIt is important to be aware that you are expressing yourself at these two levels!
• Being apathetic
• Be aggressive
• Listening distractedly or not asking questions
• Interrupt
• Criticize and judge
• Being embarrassed or uncomfortable when emotions are expressed (verbally
or non-verbally)
• Talking instead of listening
• Contradict
• Argue, try to convince
• Talk about yourself, your experience, cite yourself as an example
• Taking care of other things while listening
• Joking or laughing inappropriately
• Keeping too much or too little distance
• Forgetting what the person said previously
How to listen well?
It is important to listen to the other person on two levels: verbally and non-verbal.
It is important to observe whether there is consistency between verbal and nonverbal messages.
Non-verbal communication
Much of communication is non-verbal. This non-verbal communication takes
different paths
6.3.6. Principles of the counselling in gender-based violence.
In order to reach the aims of fulfilling needs of traumatized victim, it is important
to follow very precise particular principles of counselling. They are three basic
principles:• Trust women’s experience
• Women victims are not guilty for the violence they experienced
• Counselling means not giving advices but trusting victim’s self- determination
• Confidentiality, implies absolute word to client that her story will not go out -
experience of each woman is equally valued
• Ethics of difference: working with victim with awareness of discrimination they
are exposed to: race, ability/disability, nationality, sexual orientation, rural/
urban, poverty.
• Ethics of care, implies caring of oneself and the others equally.
• Holistic approach of service, implies taking in account all dimensions ofvictim’s live, and supporting her in realizing different needs.
Self-assessment 6.3
a. What is the aim of counselling?b. Explain 5 rights of gender-based violence’s victims.
6.4. Advocacy in gender-based violence
Learning Activity 6.4
How do you understand the concept of advocacy?
6.4.1. Introduction of advocacy in gender-based violence
Advocacy is referred to any action that speaks in favor of others, recommends,
argues for a cause, support or defends or pleads on behalf of others and helping
people find their voice. Gender based violence affects women and men of all ages
and backgrounds. Women and girls are the primary victims like rape and other
forms of sexual violence. Also, men and boys are frequently targeted as well, as
they however face different forms of violence like to be forcibly recruited into armed
forces
Advocacy in Gender based violence should be done to the relevant actors, including
national and local authorities, traditional, cultural or religious bodies, armed forces
and security forces, law enforcement officials, civil society groups, and others, to
ensure effective prevention and response, also include advocacy with non-state
actors. For advocacy to be effective, the following points should be emphasized
on:
Assessment and analysis
Advocacy should be done to victims to have appropriate assessments must be
undertaken by trained staff with expertise in the area of gender-based violence,identification of major causes for GBV
Coordination
Ensure that GBV is addressed by the protection working group and other relevant
coordination structures. This may include appointing a focal point or a working
group on GBV. Standard operating procedures, outlining roles and responsibilities
of relevant actors, should be agreed upon and implemented. Advocacy is done with
other groups/sectors to ensure that gender concerns are taken into account and
integrated in planning and programming activities at all levels.
Information and communication activities
Ensure that information about GBV prevention and response, including how and
where to access relevant assistance and services, is readily available for all
survivors of GBV.
Referral and response mechanism.
Ensure that adequate referral and response mechanisms are put in place, including
clear and acceptable referral and reporting mechanisms that respect confidentiality
and the rights of the victim/survivor.
Physical safety and security.
Advocacy should be done to improve safety and security in and around camps,
settlements, villages and other areas, like food distribution sites, water points,
areas for firewood collection, schools, public spaces, etc. Ensure that mechanisms
are in place to guarantee the security of victims/survivors and witnesses in order to
protect them against further harm.
Health
Ensure that adequate and confidential basic health care, including physical,
reproductive and psycho-social health care, is available and fully accessible to all
women and girls, particularly victims/survivors of GBV.
Community mobilization
Build the capacity of individuals to protect themselves and recover from
acts of GBV, for instance by encouraging and promoting equal participation
of men and women in all community activities and supporting education
and vocational training program, income-generating activities and literacy
program that empower women and girls.
Livelihoods
Advocate for self-reliance and sustainable livelihood program and ensure that these
are available to victims/survivors of GBV. Such program can reduce the risk of
GBV and mitigate its effects by facilitating rehabilitation and reintegration of victims/survivors.
Shelter and physical planning
Advocate for the establishment of safe shelter for victims of GBV, in particular
single women and unaccompanied children. Where individuals or families are
provided with shelter material, ensure that gender concerns are considered.
As an example, women or girls should not have to travel long
distances to collect the material and should have the ability to erect the
shelter themselves or receive adequate assistance to do so, without being
exposed to pressures for transactional sex.
Ensure that gender concerns are taken into account in physical planning
of camps and in the design and implementation of services, such as health
care, education, water/sanitation and food distribution
Justice
Advocate for the victims/survivors to have access to free and confidential
counselling services, legal and/or other avenues for redress. This can, for instance,
include assistance with legal fees, translation, and travel to and from court, and/or
measures to ensure the safety and security of the victim/survivor. Monitor and follow
up on cases of GBV to ensure that these are investigated, prosecuted and resolved
in accordance with established laws and procedures. Help build the capacity of the
justice sector, including police, prosecutors, lawyers and judges, to deal with issuesrelated to GBV
Education
Advocate for full and equal access for internal displaced people (IDPs) and other
affected individuals to safe education, vocational and trainings that can strengthen
Self-reliance and economic independence. Promote a safe learning environment
both within and around schools and other educational facilities. This may include
awareness raising among children, parents, teachers and other educational staff,
and relevant local authorities.
Children
Ensure that child victims/survivors are provided with special care and assistance
as appropriate. Such interventions should be guided by the key principles of the
convention on the rights of the child, namely the best interests of the child and the
child’s right to life, survival and development, non-discrimination, and participation.
Durable solutions
Advocate with relevant actors to encourage attention to GBV in all return, relocation
and reintegration frameworks, developmental action plans, and disarmament,
demobilization and reintegration program. Such frameworks and action plans
should contain measures to prevent and respond to GBV and provide adequatecare, treatment and support to victims/survivors.
Self-assessment 6.4
a. List 5 points to focus on for effective advocacy.
b. Give an example where one can advocate for gender-based violence.
6.5. End of unit assessment 6
End of unit assessment
1. What do you understand by the term gender-based violence?
2. Explain the following types of gender-based violencea. Physical violence3. Briefly mention the causes of gender-based violence in the society?
b. Sexual violence
c. Emotional and psychological violence
4. Enumerate the consequences of gender-based violence?
5. What are the rights of victim in case of GBV before engaging in the
counselling process?
6. When counselling the victim of GBV, what are the elements that the
counsellor should consider?
7. Explain how the counsellor has to listen well to the victim in case of GBV?
8. How do you understand the concept of advocacy?
9. Discuss the points that counsellor should be emphasized on in order to
make advocacy to be effective:
Section two: Multiple choice questions
1. Gender based Violence can take place in the following places;
a) In homes
b) Schools
c) Work place
d) All of the above
2. Gender based violence base on many factors
a. educational factors, age factors, status factors and cultural factors.
b. religious factors, political factors, humanitarian factor and Gender factors.
c. Cultural factors, legal factors, social- economic factors and political factors.
d. None of the above
3. The consequences of gender-based violence are except
a. chronic physical consequence, acute physical consequence
b. reproductive consequences, social and economic consequences.
c. Answer is a and b
d. Answer is b only
4. counselling aims at:
a. Decrease emotions that destroy the victim, be an objective mirror: help to
understand the extent of the problem as it actually is
b. Make responsible without feeling guilty, build new values, convictions that
will permanently change your life
c. Help to understand his role, Support and accompany for social reintegration
d. All the above
5. The victims or survivors of gender-based violence has the following rights
a. Being informed of the advantages of the availability of management of GBV
and its use, to benefit from services without distinction of sex, age, religion, race,
origin, marital status or place of residence.
b. Refer her to an authority or a place that ensures her safety physical and
psychological, Having a consultation in private
c. Be guaranteed that professional secrecy will be respected., Being listened to
and treated with respect
d. All of the above
6. Advocacy in Gender based violence is defined as;
a. Advocacy is any action that speaks in favors of others, recommends, argues
for a cause, support or defends or pleads on behalf of others and helping people
find their voice.
b. Gender based violence affects women and men of all ages and backgrounds.
Women and girls are the primary victims like rape and other forms of sexual
violence.
c. Answer is ad. Answer is a and b
7. 1. REFERENCES
1. Macdonald, S., & Johnson, G. (Eds.). (2017). Mayes’ Midwifery E-Book.
Elsevier Health Sciences.
2. Henderson, C., & Macdonald, S. (2004). Maye’s Midwifery: A Textbook
for Midwives. Bailliere Tindall Limited.
3. Fraser, M. D., & Cooper, M. A. (2003). Myles text book for
midwives. Midwifery, 33(3), 752.
4. Marshall, J. E., Raynor, M. D., & Nolte, A. (Eds.). (2016). Myles Textbook
for Midwives 3E African Edition E-Book: Myles Textbook for Midwives.
Elsevier Health Sciences.
5. Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., Wilson, D., Alden,
K. R., & Cashion, M. C. (2017). Maternal child nursing care-E-Book.
Elsevier Health Sciences.
6. Ricci, S. S., & Kyle, T. (2009). Maternity and pediatric nursing. Lippincott
Williams & Wilkins.
7. Marchant, S., & Garcia, J. (1995). Routine clinical care in the immediate
postnatal period. In Aspects of Midwifery Practice (pp. 177-191). Palgrave,
London.
8. Bick, D., MacArthur, C., & Winter, H. (2008). Postnatal Care E-Book. Elsevier
Health Sciences.
9. Edmonds, K. (2018). Dewhurst’s Textbook of O
10. \bstetrics & Gynaecology. John Wiley & Sons.
11. Anderson, T., & Podkolinski, J. (2000). Reflections on Midwifery care and the
Postnatal Period. In Midwifery Practice: Core Topics 3 (pp. 1-18). Palgrave,
London.
12. Ball, J. A. (2013). Postnatal care and adjustment to. Midwives, Research and
Childbirth: Volume 1, 1, 154.
13. Jordan, R. G., Farley, C. L., & Grace, K. T. (Eds.). (2018).Prenatal and postnatal
care: a woman-centered approach. John Wiley & Sons.ng a Midwife (2014).
14. Tharpe, N. L., Farley, C. L., & Jordan, R. G. (2021). Clinical practice guidelines
for midwifery & women’s health. Jones & Bartlett Learning.
15. Jacob, A. (2018). A Comprehensive Textbook of Midwifery & Gynecological
Nursing. Jaypee Brothers Medical Publishers.
16. Murray, S. S., & McKinney, E. S. (2014). Foundations of maternal-newborn
and women’s health nursing-e-book. Elsevier Health Sciences.
17. Glazebrook, V. C. B. R. S., & Ann, J. R. M. Maternal-newborn Nursing.
18. Stillerman, E. (2007). Prenatal Massage-E-Book: A Textbook of Pregnancy,
Labor, and Postpartum Bodywork. Elsevier Health Sciences.
19. Duncan, A., & von Widekind, C. (2012). Bleeding from the lower genital tract. A
Textbook of Postpartum Hemorrhage (2nd Edition). Arulumaran S, Karoshi
M, Keith LG, Lalonde AB, B-Lynch C (Eds). Jaypee Brothers Publishers, New
Delhi, India.
20. Rao, K. A. (2011). Textbook of midwifery and obstetrics for nurses. Elsevier
India.
21. Christopher, B., Keith, L. G., Lalonde, A. B., & Karoshi, M. (Eds.). (2006). A
textbook of postpartum hemorrhage: a comprehensive guide to evaluation,
management and surgical intervention. Jaypee Brothers Publishers.
22. Khan, R. U., & El-Refaey, H. (2006). Pathophysiology of postpartum
hemorrhage and third stage of labor. Postpartum Hemorrhage, 93(3), 243-
253.
23. Francis, M. (2007). The everything health guide to postpartum care: a
complete guide to looking and feeling great after delivery and beyond. Simon
and Schuster.
24. World Health Organization. WHO technical consultation on postpartum and
postnatal care. No. WHO/MPS/10.03. World Health Organization, 2010.
25. Bick, D., MacArthur, C., & Winter, H. (2008). Postnatal Care E-Book. Elsevier
Health Sciences.
26. Byrom, S., Edwards, G., & Bick, D. (Eds.). (2009). Postnatal Care. John Wiley
& Sons.
27. Johnson, R., & Taylor, W. (2016). Skills for Midwifery Practice E-Book. Elsevier
Health Sciences.
28. Lamb, K., & Sanders, R. (2016). Bladder care in the context of motherhood:
Ensuring holistic midwifery practice. British Journal of Midwifery, 24(6), 415-
421.
29. Hall, J., & Lucas, G. (2015). Postnatal changes. RCM Midwives Journal,
(Summer), 26-27.
30. Bick, D. (2000). Organization of postnatal care and related issues. In Midwifery
practice: Core topics 3 (pp. 129-142). Palgrave, London.
31. Lewis, L. (2011). Essential midwifery practice: postnatal care. Essentially
Midirs, 2(5).
32. Baston, H., & Hall, J. (2017). Midwifery Essentials: Postnatal E-Book: Volume
4 (Vol. 4). Elsevier Health Sciences.
33. Johnson, R., & Taylor, W. (2016). Skills for Midwifery Practice E-Book. Elsevier
Health Sciences.
34. Jay, A., & Peace, M. (2014). Effective postnatal care. The Student’s Guide to
Becoming a Midwife.
35. Nunnerley, R. (1990). Quality assurance in postnatal care. In Postnatal
Care (pp. 143-167). Palgrave, London.
36. Nolte, A. G. W. (1992). The standards for postnatal care by the midwife in the
hospital and the community. Curationis, 15(4), 1-7.
37. Hall, J., & Lucas, G. (2015). Postnatal changes. RCM Midwives Journal,
(Summer), 26-27.
38. Lawrence, D. M. (1985). Postpartum Nursing: Health Care of Women
(Book). Journal of Community Health Nursing, 2(2), 121-121.
39. Arulkumaran, S., Karoshi, M., Keith, L. G., Lalonde, A. B., & Christopher,
B. (Eds.). (2012). A comprehensive textbook of postpartum hemorrhage:
an essential clinical reference for effective management. Global Library of
Women’s Medicine (www. glowm. com) by Sapiens Publishing.
40. Konar, H. (2018). DC Dutta’s Textbook of obstetrics. JP Medical Ltd.
41. Rao, K. A. (2011). Textbook of midwifery and obstetrics for nurses. Elsevier
India.
42. Jacob, A. (2018). A Comprehensive Textbook of Midwifery & Gynecological
Nursing. Jaypee Brothers Medical Publishers.
43. Firoz, T., Sotunsa, J., & Adetoro, O. O. (2016). Treatment postpartum–
immediate and long term. The FIGO Textbook of Pregnancy Hypertension: an
Evidence-Based Guide to Monitoring, Prevention and Management London:
Global Library of Women’s Medicine, 215-32.
44. Lowdermilk, D. L., Cashion, M. C., Perry, S. E., Alden, K. R., & Olshansky,
E. (2019). Maternity and Women’s Health Care E-Book. Elsevier Health
Sciences.
45. Rizvi, R. M., & Rizvi, J. (2006). Management of postpartum urinary
retention. Reviews in Gynaecological and Perinatal Practice, 6(3-4), 140-144.
46. Albers, L. L. (2000). Health problems after childbirth. The Journal of Midwifery
& Women’s Health, 45(1), 55-57.
47. Chiarelli, P., & Cockburn, J. (1999). Postpartum perineal management and
best practice. Australian College of Midwives Incorporated Journal, 12(1), 14-
18.
48. Okoror, C.E.M. and Omuemu, V.O., 2021. Knowledge of obstetric danger
signs among antenatal clinic attendees in South–South Nigeria. Health Care
for Women International, pp.1-16.
49. Thakur, R., Sharma, R.K., Kumar, L. and Pugazhendi, S., 2017. Neonatal
danger signs: attitude and practice of post-natal mothers. Journal of Nursing
& Care, 6(3), pp.2167-1168.
50. Nigatu, S.G., Worku, A.G. and Dadi, A.F., 2015. Level of mother’s knowledge
about neonatal danger signs and associated factors in North West of Ethiopia:
a community based study. BMC research notes, 8(1), pp.1-6.
51. EngenderHealth. (2003). Reproductive Health : Counseling for An Integrated.
https://www.engenderhealth.org/wp-content/uploads/imports/files/pubs/
counseling-informed-choice/ccrh_ph.pdf
52. EngenderHealth. (2018). REDI: A Client-Centered
Counseling Framework Participant ’ s Handbook.
chromeextension: //efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Frbc.gov.rw%2Ffileadmin%2Fuser_
