UNIT 3: NEW BORN DANGER SIGNS
Key Unit Competence:
Detect, manage and refer a newborn with danger
Introductory activity 3.0Observe the following pictures showing the new born danger signs and reflect on them.
From the observation of the above mentioned images;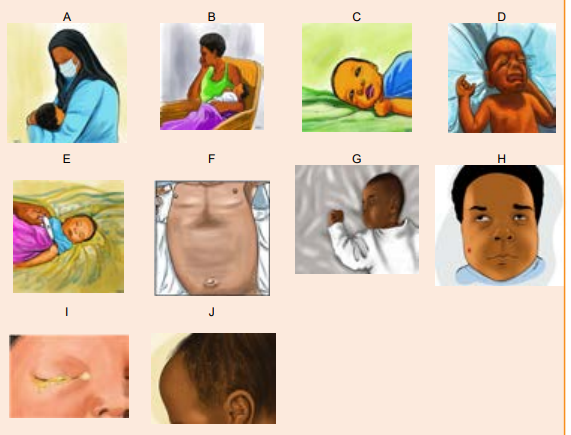
 a) Which danger sign do you think image A is showing?3.1 General assessment of the New born danger signs.
a) Which danger sign do you think image A is showing?3.1 General assessment of the New born danger signs.
b) Which danger sign do you think image B is showing?
c) Which danger sign do you think image C is showing?
d) Which danger sign do you think image D is showing?
e) Which danger sign do you think image E is showing?
f) Which danger sign do you think image F is showing?
g) Which danger sign do you think image G is showing?
h) Which danger sign do you think image H is showing?
i) Which danger sign do you think image I is showing?
j) Which danger sign do you think image J Is showing?
Learning Activity 3.1
12 hours old female newborn found to be having difficult in breathing with
respiratory rate of 70 movements /min, axillary temperature of 34 , hypotonic,
unable to breastfeed but the health care provider observed that the baby has
breastfeed well earlier as reported by the mother, baby’s birth weight is 2.2kg
and born at 3 weeks before term.a) What do you think about the cause of difficult in breathing?Newborn danger signs are the clinical signs that indicate a high risk of neonatal
b) What do you think that can be the cause of unable to breast feed?c) What do you think can cause very low body temperature to this newborn?
morbidity and mortality and require immediate therapeutic interventions. They are
also signs that show the neonate is sick. Early identification by the nurse and the
parents is an important step toward improving newborn survival. The World Health
Organization (WHO) described nine neonatal danger signs which includes not
able to feed or stopped feeding well, convulsions, fast breathing, severe chest indrawing,
fever, hypothermia, yellow soles, movement only when stimulated or no
movement, and signs of local infection (umbilicus red or draining pus, skin infection,
or eyes draining with pus.or eyes draining with pus.
The neonatal period is the first four weeks of an infant’s life, whether the baby was
carried to term or born prematurely. It’s a time of rapid change and development
where patterns for infancy, like feeding and bonding, are developed.
Danger signs in the neonatal period (0–28 days) are non-specific and that indicates
severe illness. They are used in integrated management of neonatal and childillness (IMNCI) by practitioners to identify children who need medical care.
It has been noted that one-third of all neonatal deaths occur on the first day of life,
almost half within 3 days and nearly three-quarters within the first week of life.
Therefore, effective strategies to improve newborn survival in developing countries
require a clear understanding of the patterns and determinants of newborn-care
seeking by mothers, families and other newborn caregivers.
Improving families’ care-seeking behavior is one of the important strategies to
reduce child death in developing nations. The WHO estimates that seeking prompt
and appropriate care could reduce child mortality due to acute respiratory infections
by 20%.An important method to reduce newborn death is early recognition of NDSsand the provision of quality of curative health services for sick newborns.
The majority of neonatal deaths in developing countries occur at home. Many of
these deaths are related to late recognition of the signs of a serious illness by
parents and a delay in the decision to seek medical care. Since the health-seeking
behaviour of mothers for neonatal care depends on the mothers’ knowledge
Although many babies will have a healthy birth and will breathe easily and begin
feeding soon after being placed on the mother’s breast, other babies will have a
range of needs, some urgent, in order to ensure their safety and wellbeing.
It is very important to assess the new-born for the danger signs in order to take
actions to help the newborn are crucial to ensure prompt and safe care. Mothers
should be taught to look for these signs in the newborn and advised to seek earlymedical care if they observe any one of the danger signs.
Self-assessment 3.1
1) Define neonatal period?
2) What does it mean new born danger signs?3) Where does the majority of neonatal death occur in developing countries?
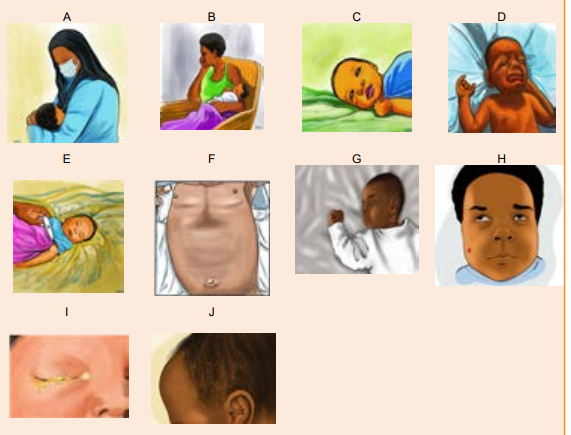
3.2 Respiratory problems in newborns and hypoxiaLearning Activity 3.2
Observe and compare the pictures above that show 2 neonate’ respiratory
features;a) Reflect on the difference between the 2 new borns.Respiratory disorders in newborns are conditions characterized by abnormal
b) Characterize the baby A mouth and the baby B mouth
c) Close your nose and stop breathing in, how will you manage to try breathing?
d) Characterize and reflect on the baby A chest and the baby B cheste) What should happen if the baby is not receiving enough Oxygen?
respiratory rate (RR), increased work of breathing that result in hypoxia.
Abnormal respiratory rate (RR)
The newborn presents a breathing that is abnormally rapid and often shallow known
as Tachypnea with a respiratory rate > 60breaths/minute or a slow respiratory rate
< 30breaths/minute called Bradypnea. Dramatically the baby can cease breathing
for a period > 20 seconds or less when associated with bradycardia or cyanosis this
is known as apnea.
Breathing less than or equal to 30 or more than or equal to 60 breaths per minute,grunting, severe chest in drawing, blue tongue and lips, or gasping.
Increased work of breathing
A newborn with respiratory distress struggles to breathe and exhales against
a partially closed glottis this produces a sound termed as grunting. This effort
causes widening of nostrils when breathing in, called nasal flaring and the chest
undergoes a marked inward movements of the muscles between the ribs during
inspiration. This is termed as chest retraction (chest indrawing).
Classification of respiratory disorders:
Mild
Physical Examination:• Minimal grunting on expiration, flaring and retractionsModerate to severe• Vital Signs: RR in 60–70, Oxygen saturation >90%
Physical Examination:
Moderate to severe grunting, flaring, retractionsVital Signs: RR > 70 or < 30 or saturation <90%
The role of the associate nurse in the management of respiratory distress in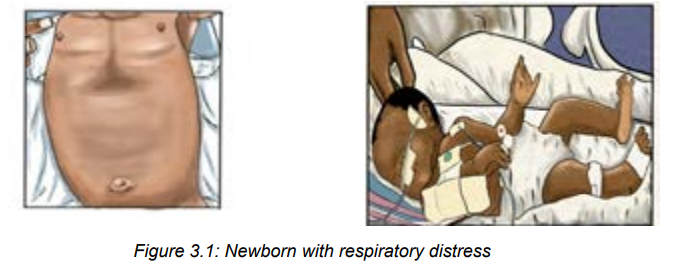
neonates
Most neonates with respiratory distress can be treated with respiratory support
and noninvasive methods. Oxygen can be provided via bag/mask, nasal
cannula, oxygen hood, and nasal continuous positive airway pressure. Ventilatorsupport may be used in more severe cases.
A baby in respiratory distress needs to be resuscitated and the associate nurse will
first call for help from experienced caregivers and following actions will be done:• Immediately resuscitate the newborn using current guidelinesSelf-assessment 3.2
• Stabilize and admit to neonatal unit
• Monitor Vital signs with focus on respiratory rate and oxygen saturation
frequently.
• Initial evaluation includes a detailed history and physical examination. The
clinician should monitor vital signs and measure oxygen saturation with pulse
oximetry.
• The blood gas measurement may be considered;
• Lab exams (Full blood count)
• Take pulse oximetry after 24 hours but before hospital discharge to screen for
any critical congenital heart
• Always assess for cyanosis
• Assess for feeding or nutrition possibilities
• Avoid hypothermia1) Explain the respiratory problems in new born.3.3 Breastfeeding /feeding disorders (inability to breastfeed/poor
2) Identify the respiratory rate deviation in the new born.
3) What is the grunting in abnormal work of breathing of a new born?
4) The term hypoxia is often used in respiratory patterns; how can it bedefined?
feeding)
Learning Activity 3.3
A student mother comes to the health facility with her 3weeks baby because 2
days ago baby stopped to nurse, the baby is crying for hunger but cannot suck
and the mother prefers to use a bottle. As an associate nurse:a) Reflect on why the breast milk is the best aliment of the baby?
b) What do you think about the causes that can interrupt breastfeeding onthe neonate?
A change in behavior may be one of the first signs of illness in a newborn. It’s
normal for a baby’s activity, appetite, and cries to vary from day to day, even hour to
hour. But a distinct change in any of these areas may signal illness.
Exclusive breastfeeding is strongly recommended for the first six months. The
healthy newborn does not need water, other fluids, or foods during this time.
Mother’s milk is healthy because it contains antibodies that actively protects
against infection and allergies. Newborn who are not breastfed become sick and
may die from hypoglycemia, neonatal jaundice, and infections such as diarrhea,
gastrointestinal infections. Baby cannot suck due to newborn itself or from maternalcauses.
Poor sucking; In a term baby who was feeding earlier ® indicates neonatal illness
(as perceived by mother). In a preterm baby ® needs careful assessment because
it may be due to cold stress or immaturity.
In case the baby refuses or misses several feedings due to that she/he is having
trouble of sucking at breast or bottle, doesn’t seem to be hungry, is having problems
spitting up, or is losing weight, that is a sign of illness. Immediate attention must be
taken.
If the baby is bottle-fed, a weak suck may require the bottle nipple to be “worked”
or pumped to stimulate a suck. Either type of feeding, whether by breast or bottle,
may take a very long time often longer than 45 minutes.
Spitting up and dribbling milk with burps or after feedings is fairly common in
new-borns. This is because the sphincter muscle between the stomach and the
oesophagus (the tube from the mouth to stomach) is weak and immature. However,
forceful or projectile vomiting, or spitting up large amounts of milk after most
feedings, can indicate a problem. If the baby is formula-fed, vomiting may occur
after overfeeding or because of intolerance to formula. If the baby is breastfed or
formula-fed, he or she may have a physical condition that prevents normal digestionand may cause vomiting.
Causes and factors associated with new born inability to feed/breast
feeding;• The baby is sick from a general illness or abdominal distentionManagement of the new born with inability to feed/poor feeding:
• Preterm babies due to immature or the absence of sucking reflex
• New born who have congenital malformations ex: cleft palate and lips.
There are a few reasons that a neonate baby may not be feeding enough/ unable
to feed such as a tongue-tie, blocked nose, stomach flu, illness or being born
prematurely. However, regardless of the reason, if the newborn is not feeding
normally, a neonatologist or neonatal care specialist must be called, especially if
the baby is sleepy and dull. This can be a sign of illness, infection or low bloodsugar.
The following techniques have proven helpful for babies refusing the breast/
unable to feed:• The first choice to feed a non-nursing baby is the mother’s own milk. The
second choice is banked breast milk from mother and the third choice
is formula if possible.
• Very careful, supportive positioning can be very helpful when the baby is
having breastfeeding issues. For example, a cross-cradle hold or modified
football hold can be useful. Make sure the baby’s head is at a higher level
than the rest of their body. If the baby is tolerating it, then work on latching
for up to 10 minutes or so. If the neonate is getting upset, then go with
shorter sessions. It is not a good idea to keep trying for more than about 10
minutes. The baby may get tired and latching will be harder. In addition, the
baby may be at risk of here is a risk of developing breastfeeding aversion ifyou persist too much.
• Continue to offer expressed mother’s milk, banked milk, formula for short
times, but gradually help the mother to put the baby on closer and closer to
the nursing position, skin-to-skin, etc.
• Educate and help the mother to wear clothing that allows very easy access
to the breasts. Baby may get very impatient in the split-second that it takes
a mother to lift her blouse and undo her bra. Tell the mother to spend time, if
possible, in a warm place that allows both mother and baby to be naked fromthe waist up.
• Educate the mother to offer the breast often. Try breastfeeding in baby’s
favourite place, in favourite position, in the bath, while walking around, while
lying down, with the baby being in upright, with baby being flat on their back
position.
• If the neonate is completely unable to feed or vomit all the times, it is an
emergency and parenteral feedings must be considered at an advanced
health setting through Nasogastric tube.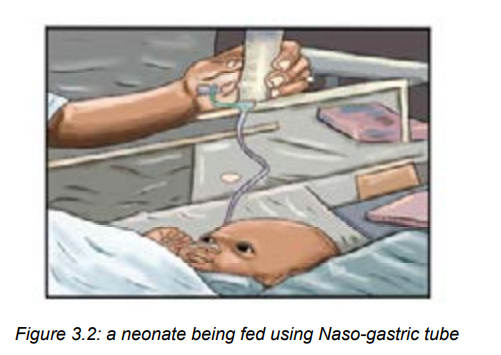
Self-assessment 3.3
1. Poor sucking in a baby who was feeding well earlier indicates the following
except one:
a) Neonatal illness
b) It is a preterm baby it may be due to cold stress or immaturity.
c) Maternal causes
d) Congenital malformations
2. What does spitting up and dribbling milk with burps or after feedings means
to the neonate
3. What does a forceful or projectile vomiting, or spitting up large amounts ofmilk after most feedings means to the neonate?
3.4 Lethargy/ Hypotonia
Learning Activity 3.4
A 2-day old term male infant was found too sleepy and with few movement and
sometimes refuse to breastfeed.a) What do you reflect is this situation?Lethargy is the pathological state of sleepiness or deep unresponsiveness. It
b) What do you think that could be the cause of this new born’s hypotonic?
may be a sign of infection or other conditions such as low blood sugar. If neonate
becomes lethargic or is not as active, inactivity, so it’s necessary to seek medical
care as soon as possible.
Lethargy is noticed when the neonate seems to have little or no energy, is drowsy
or sluggish, or is sleeping longer than usual. He or she may be hard to wake for
feedings, and won’t be alert or attentive to sounds and visual stimulation. Sometimes
this develops slowly, so the gradual change will be noticed. Lethargy may be a sign
of infection, anemia, low blood sugar or hypoxic ischemic encephalopathy (HIE)
and it is among neonatal emergency.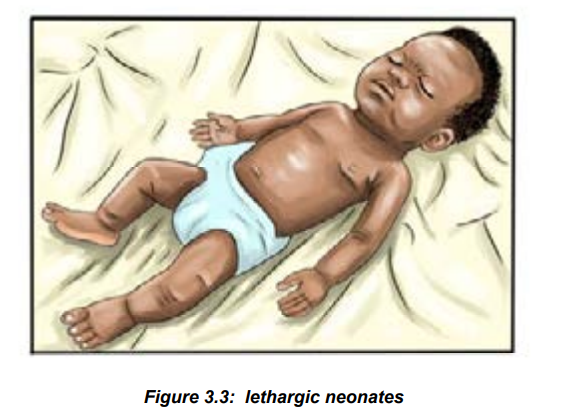
Nursing management of hypotonic/lethargy in the neonate:• Initial management should be focused on stabilizing the infant and then
evaluate the most likely causes of illness.• start with evaluation for hypoglycemia and sepsis and provide respiratory1) Define term lethargy?
support.
• Take laboratory samples for checking blood glucose and FBC to rule out
infection and anemia
• Take and monitor closely vital signs• Manage and care the neonate according to the cause of hypotonia.
Self-assessment 3.4
2) What can be done initially when noticed that the neonate is lethargic?3) State 3 causes of lethargy in new borns.
PROBLEM OF THERMOREGULATION
3.5 Neonatal hypothermiaLearning Activity 3.5
A 5-day old male term new born is bathed in a cold ward. Afterwards the new born
appears not well, has rapid breathing, pale skin, lethargic and is not accepting
breastfeeding. A thermometer reading over the right upper abdomen gives a
result of 34 °C. His birth weight is 2400 grams but has wasted 200grams.a) What do you think is the situation to that neonate baby?A baby is hypothermic when axillary temperature is below 35.5°C or core temperature
b) What do you think could be the reason of low body temperature to this new
born?
is below 36°C. As the rectal temperature is normally higher than that at other sites,
a rectal temperature below 35 °C is particularly dangerous. It results into metabolic
disorders such as dyspnea, poor feeding, hypoglycemia and lethargy. Once the
body temperature falls below 35 °C the infant is in danger of complications relatedto being too cold.
Newborns at risk of developing hypothermia• Preterm <35 weeks of gestation
• Low birth weight
• Small for gestational age
• Sick newborns
• Any newborn not adequately kept warm
• Wet infants (after delivery or bathing).
• Infants requiring resuscitation.
• Sick infants, particularly if there is infection.
• Infants who are in a cold room.
• Infants who are not fed.
• Hypoglycemic infants. »Infants undergoing medical procedures.• Infants born before arrival at a health facility, home delivery
Nursing management of hypothermia
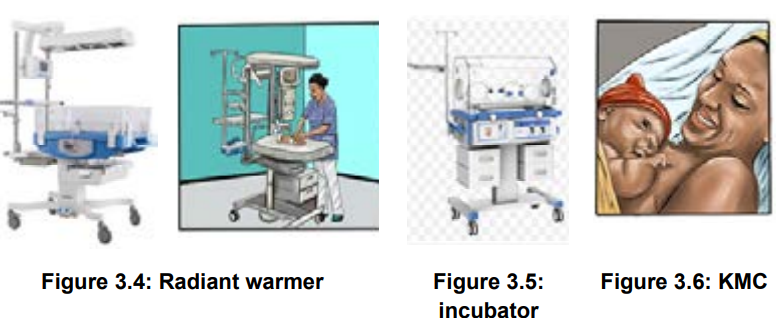
• Warm the infant in a closed incubator, overhead radiant warmer or warmDifferent ways used to keep the new born warm:
room. Skin-to-skin care is a very effective method of warming a cold infant.
• Provide energy while the infant is being warmed.
• Monitor closely vital signs, oxygen saturation and color of skin
• Ensure neonate adequate breastfeeding
• Avoid cold infusions
• Educate the mother how to keep warm the baby and avoid cold bathing.
1. Maternal body heat (skin-to-skin care). Infants can very easily and
effectively be kept warm by placing them naked against the mother’s bare
breasts. The infant should wear a woollen cap and nappy. Both mother and
infant should be covered. The mother’s body heat will keep the infant warm.
This simple method is an important part of kangaroo mother care (KMC). It isthe best method of keeping a well infant warm.
2. A closed incubator. This is the traditional way of warming smallest or sick
infants as the temperature can be carefully controlled. Today more and more
infants are being warmed with KMC rather than in an incubator.
3. Radiant warmers (overhead radiant heaters). A radiant warmer is used for
warming very sick infant in an intensive care unit. Water loss by evaporation
is higher than in a closed incubator. A thick plastic sheet or ‘bubble wrap’ over
the infant reduces water loss. As soon as ill baby has improved they should
be moved out of a radiant heater and into a closed incubator.
4. Warm room. Most healthy, term infants can be warmed in a cot or bassinet in
a warm caring environment (ward or home). The room temperature should be
about 20 °C. The infant should be dressed to prevent heat loss by radiation
to cold windows or walls.
5. Hot room. Many low birth weight infants can be kept warm in a bassinet if
they are cared in a room where the temperature is kept at 25–30 °C. The
smaller the infant, the higher the required room temperature will be. However,
keeping the mother and infant together with KMC is preferable.
6. Dressing the infant. The infant can be kept warm by covering the body with
an insulating layer and, thereby, preventing heat loss by convection to cold air
and radiation to cold objects in the room. This is done by dressing the infant
in a nappy, jacket, woollen hat and booties. A woollen cap is most important
in preventing heat loss by radiation.
7. Thermal blanket. An infant can be kept warm for hours if wrapped in a
thermal blanket, silver swaddler or heavy gauge aluminium foil normally
used for cooking. This is an effective method of preventing heat loss during
transport if KMC or a transport incubator is not available. The infant must be
warm and dry before being wrapped in a thermal blanket.
8. Perspex heat shield. A transparent Perspex shield can be placed over aninfant in an incubator to reduce heat loss by radiation.
Self-assessment 3.5
1. Define hypothermia?2. State 5 methods of warming baby?
3.6 Neonatal hyperthermia
Learning Activity 3.6
4 days old male new born, born by spontaneous vaginal delivery brought at
emergency department by his mother complaining of, baby is hot on touch, body
temperature 39.8c0
. She also says that baby had inability to breastfeed since 2
days ago. The baby looked weak and dehydrated.a. What do you think could be the condition to this new born?Hyperthermia is defined as body temperature above 37.6 oC. Hyperthermia is
b. What do you think can be the cause of elevated body temperature to theneonate?
frequently a result of environmental factors that cause overheating. It is a sign of aserious infection in newborn termed as sepsis and must be ruled out for adequate
treatment. However, regardless of cause, hyperthermia can have detrimentalconsequences.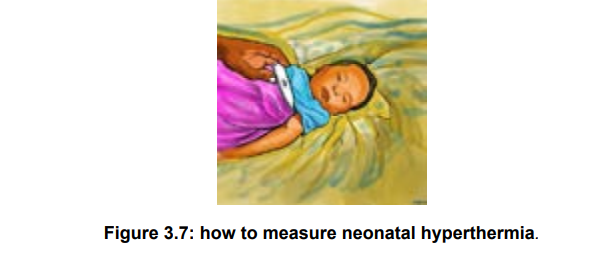
Causes of newborn hyperthermia• Overheating from incubators, radiant warmers, or hot ambient environmentalSigns and symptoms of hyperthermia in the new born
temperature
• Maternal fever
• Maternal epidural anesthesia
• Phototherapy lights, sunlight
• Excessive bundling or swaddling
• Infection
• CNS disorders (i.e. asphyxia)
• Dehydration• Tachycardia, tachypnea, apnea, warm extremities, flushing, perspiration.Nursing management of neonatal hyperthermia
• Dehydration.
• Lethargic, poor feeding, Irritability, Weak cry.• The usual approach to treating the hyper-thermic newborn is to adjust
environmental conditions.
• The newborn should be moved away from the source of heat, and undressed
partially or fully, if necessary.
• If the newborn is in an incubator, the air temperature should be lowered. It is
important that the newborn be breastfed frequently to replace fluids.• During the cooling process, the newborn’s temperature must be monitored
every 15-30 minutes until stable.
• Never turn off the incubator to cool off the newborn. When hyperthermia is
severe (i.e. body temperature above 40°C), the newborn can be given a bath.
• The water should be warm (about 2°C lower than the newborn’s body
temperature).
• Cooling devices are not recommended, if the newborn cannot breastfeed
extra fluids should be given intravenously or by tube.
• The treatment of hyperthermia in the new-born consists also exposing him or
her to room temperature.
• If the skin temperature is higher than 39.0°C, sponging with tepid water
at about 35.0°C should be initiated until the skin temperature approaches37.0°C.
Self-assessment 3.6
1) Define the term hyperthermia
2) State the causes of hyperthermia in the newborns
3) Briefly, explain the signs of hyperthermia in newborns3.7 Umbilical cord infection (Omphilitis)
Learning Activity 3.7
8 days old male neonate born by spontaneous vaginal delivery at home un
planed brought by his mother to the health facility with the following complaints;
umbilical stump draining pus, smelling discharge, swollen area around umbilical
cord, un usual temperature and baby is sleepy, she also reported that her baby’s
umbilical cord bleeds after birth and they re-tied it with cloth- thread.a) What do you think that could be the problem?In most cases, the umbilical cord stump dries up and falls off the newborn within the
b) What do you think that could be the cause?
first few weeks of life. It’s also normal for the clamped cord to develop a scab at its
end. It may even bleed a little bit, especially around the base of the stump when it’s
ready to fall off. But the bleeding should be light and quickly stop when you apply
gentle pressure. But sometimes an infection can develop. This may cause the area
around the cord to swell and become inflamed, red, or tender. There may be cloudy,
discolored, or bad-smelling discharge from the cord. There may also be oozing or
slight bleeding. That situation is called umbilical cord infection(omphilitis).
Omphalitis is an infection of the umbilical stump. It typically presents as a superficial
cellulitis that can spread to involve the entire abdominal wall and may progress tonecrotizing fasciitis, myonecrosis, or systemic disease.
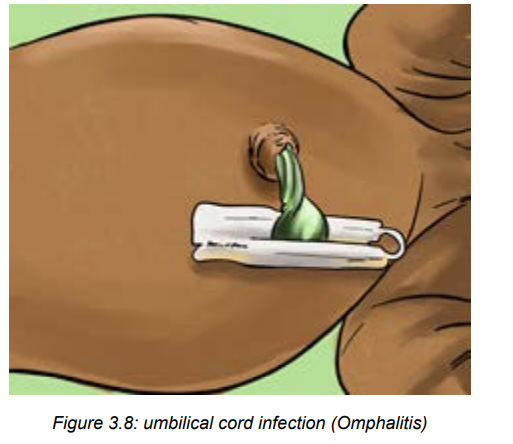
Signs of omphilitis include:
• Red, swollen, warm, or tender skin around the cordTo treat the umbilical cord infection, the healthcare provider may prescribe medicine
• Pus (a yellow-greenish liquid) oozing from the skin around the cord
• Bad smell coming from the cord
• Fever• A fussy, uncomfortable, or very sleepy baby
(antibiotics and anti-inflammatory drugs) and give instructions for cord care at home.
Risk factors of omphilitis
Risk factors for omphalitis included septic delivery, unplanned home delivery,
maternal chorioamnionitis, prolonged rupture of membranes, low birth weight,
and umbilical vessel catheterization. Mainly lack of hygiene from the mothers
and caregivers. Aerobic bacteria are present in approximately 85% of infections,
predominated by Staphylococcus aureus, group A streptococcus, escherichia coli,
klebsiella pneumoniae, and Proteus mirabilis. Methicillin-resistant S aureus has
also been described in association with omphalitis.
Nursing management of omphilitis• Wash the hands well before and after caring for the cord.Self-assessment 3.7
• Clean the area around the cord using disinfectant solutions
• Use a clean, moist cloth.
• Remove all drainage and clean an inch around the base. If there is a little
drainage is present you may be advised to use antibiotic ointment after each
cleaning.
• Roll the neonate’s diapers down below the belly button (navel) until the
infection has healed. This helps prevent contamination from urine and stool. If
needed, cut a notch in the front of the diapers to make a space for the cord.
• Don’t dress the baby in clothing that is tight across the cord.
• Don’t put the baby in bathwater until the infection has cleared and the cord
has fallen off. Instead, bathe the baby with a sponge or damp washcloth.
• Don’t use talc or other powders on the cord.
• Don’t try to remove the cord. It will fall off on its own.
• Watch for continuing signs of infection (redness, swelling, and cloudy,
discolored, or bad smelling drainage in the area around the cord) and othervital signs. This includes.
1) Define the term omphalitis3.8 Neonatal umbilical cord bleeding
2) State clinical manifestations of omphilitis3) Briefly explain the risk factors for omphilitis
Learning Activity 3.8
Observe the images above and reflect on them.
a) What do you reflect on that condition?b) What do you think that are the causes of that condition?
Bleeding umbilical cord on the neonate can lead to serious cardiovascular and
neurological effects. Routine administration of vitamin K has reduced the incidence
of hemorrhagic disease of the newborn, but abnormal bleeding can occur in neonate
babies from many causes.
Causes and risk factors of neonatal umbilical cord bleeding
Bleeding from the umbilical cord in the newborn can be caused by improper tying
of the umbilical cord, an inherited coagulation disorder, vitamin K deficiency or
immune-mediated thrombocytopenia. Disseminated intravascular coagulation
(DIC) is more common in the sick newborn.
Signs of umbilical cord bleeding
During the healing process, it’s normal to see a little blood near the cord. Much like
a scab, the cord might bleed a little when it falls off.
In case of severe hemorrhage, severity signs may include pale heavy bleeding
crossing the diaper from umbilicus, pale skin, lethargy, inability to breastfeed and
sometimes signs of shock and anemia.
Management of bleeding umbilical cord
Treat normal umbilical cord bleeding by cleaning the area around the umbilical cord
and applying a small amount of pressure to the umbilical stump to slow and stopthe bleeding.
If the bleeding is heavy, the following interventions should be done:• Call for helpSelf-assessment 3.8
• Retie the umbilical cord thoroughly
• Take vital signs
• Resuscitate the neonate in case of shock and respiratory problems
• Monitor closely vital signs
• Draw blood for lab examination (if possible)
• Ensure the nutrition (breastfeeding or parenteral)
• Remember to transfer the neonate to the neonatology or pediatrics specialist
1) What are the causes and risk factors of neonatal umbilical cord bleeding?
2) What are the signs of severe neonatal umbilical cord bleeding?3) State the complications of severe neonatal umbilical cord bleeding.
3.9 Skin infections in newborns
Learning Activity 3.9
From the observation of the above images;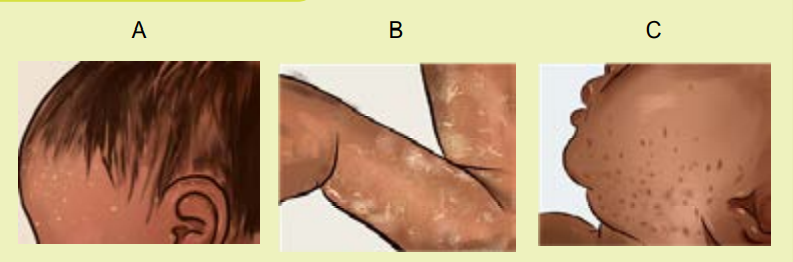
Among the skin infections, which one do you think that affect the skin like thosementioned on these images?
Skin forms a barrier with the external environment and is formed by structures that
have well defined functions. Although the stratum corneum of full-term neonates is
analogous to that of adult skin, structural and compositional differences of the skinmake the newborn more susceptible to bacterial colonization. Particularly for the
preterm neonate, impaired cutaneous barrier function and an immature immune
syii. Presentation• Nonbullous impetigo accounts for 70% of all cases and appears as tiny fluidfilled blisters that develop into honey–colored, crusty lesions. Generally, they
do not cause any pain or redness to the surrounding skin.
• Bullous impetigo is more common in infants and appears as larger, clear
blisters filled with fluid. When these blisters rupture, they may leave a scale
behind.
iii. Neonatal staphylococcal skin infectionsstem reduce the capacity to defend against bacterial pathogens.
The majority of cutaneous bacterial infections is localized to the skin and is easily
treated; however, systemic bacterial infection and disseminated disease in the
neonatal period may be life-threatening.
Pustular disorders are common in the neonatal period. Most of these conditions are
benign, but several serious and infectious diseases can present in the neonate as
pustular disorders.
Causes of neonatal skin infections
Vesiculo-bullous and pustular lesions in neonates can be due to
miscellaneous benign conditions, an infection, a genodermatosis, or
transient autoimmune bullous disorder.
Pustular eruptions in a neonate are due to a variety of causes, the benign causes
include erythema toxicum neonatorum, transient neonatal pustular melanosis, and
neonatal acne. The most common causes of infectious pustular skin lesions include
bacterial infections, which may be initially localized (Staphylococcus aureus) or
septicaemic (Listeria monocytogenes); viral infections (herpes simplex, varicellazoster);
fungal infections (Candidiasis, Malassezia furfur); or parasitic disorders(scabies).
Variety of serious neonatal skin infections
i. Impetigo
Definition: Impetigo, a common skin infection in both neonates and children caused
by bacteria (Staphylococcus or Streptococcus) entering a cut or break in the skin.
Although impetigo is usually a minor infection that can be easily treated, it could
progress to more severe symptoms including deep skin infections (cellulitis), kidney
inflammation, or meningitis. It causes distinctive blisters or sores, which can be
itchy or uncomfortable for your baby. Impetigo can be further classified into 2 types:bullous and non bullous.
ii. Presentation• Non bullous impetigo accounts for 70% of all cases and appears as tinyfluid filled blisters that develop into honey–colored, crusty lesions. Generally, theyiii. Neonatal staphylococcal skin infections
do not cause any pain or redness to the surrounding skin.
• Bullous impetigo is more common in infants and appears as larger, clear
blisters filled with fluid. When these blisters rupture, they may leave a scale
behind.
In full-term newborns, S. aureus infection usually first appears as a skin and soft
tissue infection, but may rapidly progress to osteomyelitis and pneumonia or cause
bacteremia.
Direct infection of the skin results in staphylococcal pyoderma, manifests as
vesicles, pustules, erythematous papules; folliculitis; bullous impetigo with large,flaccid bullae; honey-coloured crusted areas of nonbullous impetigo and cellulites
Manifestations of neonatal staphylococcal skin infections may be local or
generalized
iv. Pustula melanosis
Definition: Transient neonatal pustular melanosis is defined as harmless skin
condition in newborn that begins with superficial, vesiculopustular lesions often
causing some alarm when present at birth. Transient neonatal pustular melanosis
is an uncommon benign pustular condition presenting in newborn infants. It is also
known as transient neonatal pustular dermatosis and transient neonatal pustulosis.
Pustula melanosis vesicles rupture within 12 to 48 hours, leaving small pigmented
macules. The macules are often surrounded by a ring of very fine white scales. Any
stage or combination of stages (vesicles, pustules, or scaling of ruptured vesicles)
may be present at birth. These small hyper pigmented macules may remain for up
to 3 months after birth. Transient neonatal pustular melanosis is benign, requiring
no treatment.
Figure 3.9: pustula melanosis evolution:
Step 1. Pustule/Vesicles
Step2.Ruptured Pustule/VesiclesStep3.pigmented macules
Figure 3.10: Fluid-filled neonatal skin lesions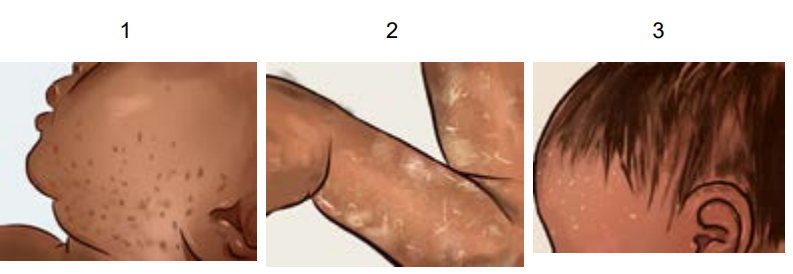
a) Vesicles due to eczema
b) Pustule due to herpes simplexc) Bulla in bullous pemphigoid.
Fluid-filled neonatal skin lesions are other types of neonatal skin infection to report.
They can be originating from all earlier described causes or idiopathic reasons.
Management of neonatal skin infections• For management of pustula melanosis: No treatment is indicated. ReassureThe skin and body hygiene are of paramount for all types of neonatal skin
parents that neonatal pustular melanosis is a benign finding and that it
disappears.
• For neonatal staphylococcal skin infections: Blebs should be punctured as
soon as formed and topical ointment/lotion should be applied. Full recovery
usually occurs in 2-3 week.
• For management of impetigo: In most cases, the antibiotic cream is
prescribed to speed up the healing process. With antibiotic treatment, the
baby’s impetigo should clear up within a week to 10 days. If the symptoms
don’t start to improve within five days of starting treatment, take back to the
dermatologist and peditrician.
• For management of transient neonatal pustular melanosis: It is benign,requiring no treatment apart from only local cleansing and washing.
infections
Self-assessment 3.9
1) What are the causes for Pustular eruptions in a neonate?
2) What are the symptoms of severe impetigo to the neonate?
3) Briefly, discuss on the neonatal staphylococcal skin infections caused byS. aureus in full term babies.
3.10 Seizures or convulsions in newbornsLearning Activity 3.10
Read the following scenario and reflect on it.
A 16-day-old female infant was brought to the emergency room because
of twitching, jaw movements, jerking movements of her arms and legs the
movements did not stop with restraint, these signs started since day 2 of life.
The parents hope to be recovered on its own but continued. There was cyanosis
of limbs and lips. They had been no fever, and she had been bottle feeding fairly,
her mother reported that she accidentary delivered from home and baby didn’t
cry for some minutes, latterly baby cried with weak voice as mentioned by her
mother.a) What do you think about the new born described in scenario’s condition?A neonatal seizure is an occurrence of abnormal, paroxysmal, and persistent
b) What do you think could be the cause of the above new born’s condition?
movements on the neonate. A neonatal seizure may or may not be epileptic.
Clinical manifestation of seizure• A neonate will present one or more of the following signs and symptoms:
twitching, rhythmic lip or jaw movements, eye twitching, extension of
extremities, clenching of fists, stiffening or jerking of limbs or trunk, lip
smacking movements may be observed.
• Accompanying signs may include the change in vital signs such as alteration
in heart rate, blood pressure, respiration, salivation, pupillary dilation, and
other associated paroxysmal changes in the autonomic nervous system of
infants may be caused due to these seizures.
• Common etiologies of neonatal seizures• The commonest cause is asphyxia due to hypoxic ischemic encephalopathy
but others are intra uterine and central nervous system (CNS) infections.
Lack of oxygen before or during birth due to placental abruption (premature
detachment of the placenta from the uterus), a difficult or prolonged labor, orcompression of the umbilical cord.
• Metabolic disorders that occur before (inborn error of metabolism) or around
birth such as hypo glycaemia, Hypocalcaemia, Hypomagnesaemia, Hypo/
hypernatremia may cause convulsions in newborn babies.
• Congenital abnormalities that involve the CNS, neonatal ‘stroke’ andintracranial hemorrhage are responsible of convulsions in newborn.
• Infection acquired before or after birth, such as bacterial meningitis, viral
encephalitis, toxoplasmosis, syphilis or rubella.
• Stroke before or after birth.
• Blood clot in the brain.
• Bleeding in the brain.
• Brain birth defects.
• Blood sugar or electrolyte imbalances Rarely Seizures in newborn can be a
precursor factor of neonatal onset epilepsy.Management of seizures• To control the seizures, anticonvulsant medications may be prescribed,
including phenobarbital, lorazepam and phenytoin. Seizures in neonates are
often subtle, featured as any unusual repetitive or stereotypic movement.
• Check blood glucose and/or treat for hypoglycemia.
• Treat with phenobarbital IV if the seizure lasts more than 3 minutes, or recurs
(> 2 to 3 episodes in one hour), or is associated with cardiorespiratory
disturbance:• First dose: 20 mg/kg by slow IV infusion over 30 minutes. Phenobarbital
should never be administered as a rapid direct IV injection. Phenobarbital
may be given IM (undiluted) if there is no IV access.
• If seizures persist 30 minutes after, administer a second dose
of phenobarbital 10 mg/kg by slow IV infusion over 30 minutes. If still no IV
access, give the second dose of phenobarbital 10 mg/kg (undiluted) IM at
least 60 minutes after the first IM dose. Do not give more than 40 mg/kg in
total.• Any neonate that required treatment with phenobarbital should be transferredSelf-assessment 3.10
to a neonatal care unit.
• Babies are closely monitored during treatment, and then slowly re-warmed to
normal body temperature.
• Monitor the neonate closely while awaiting transfer. Ensure ventilation
equipment is available as there is a risk of respiratory depression.
• Vital signs should be monitored closely.
1. Describe how you will recognize that a baby is having seizures orconvulsion.2. Briefly discuss metabolic causes of newborns convulsions3. When to start treating seizures with phenobarbital on the neonates?3.11 Neonatal jaundice
Read the following case study and think about it.
A full-term female baby was delivered through Caesarian Section due to
prolonged labor with birth weight 4.2 kg at 39th week of gestational age. Baby
cried soon after birth and the APGAR score at birth was 9/10 and 10/10 first and
fifth minutes respectively. No any congenital anomalies seen at the time of birth.
Also, early breastfeeding was initiated on the 3rd hour from birth because the
mother delayed in the operating room due to complicated surgical operation.
After 48 hours, the neonate baby was brought in neonatal unit complaining the
baby was not breastfeeding well, is falling sleepy every time and that the color of
the baby’s skin has turned into yellow color.a) What do you think could be the condition to neonate baby described above?
b) What do you think could be the risk factor or cause of that condition?Learning Activity 3.11
Neonatal jaundice is defined as the presence of yellowish coloration of the sclera
and the skin in a neonate, caused by bilirubin accumulation in the blood. Neonatal
jaundice is a common event that occurs especially in the first week of birth and is
one of the most common causes of hospitalization of the term and preterm neonates
in neonatal wards. It is also called “Hyperbilirubinemia “
Neonatal jaundice usually occurs on the second day of birth and is not usually
harmful, and a self-limiting condition, where disease usually improves without
treatment after reaching the normal amount of bilirubin, however very high levels of
bilirubin may lead to kernicterus as permanent brain damage.
Kernicterus is a type of brain damage that can result from high levels of bilirubin in
a baby’s blood. It can cause athetoid cerebral palsy and hearing loss. Kernicterus
also causes problems with vision and teeth and sometimes can cause intellectual
disabilities. Jaundice on the first day of life is always pathologic, and urgent attentionis needed to find its cause.
Assessment of neonatal jaundice by using of Modified Kramer ‘scale
• Perform the physical examination starting with eye sclera, face, and downward.
• Jaundice may be hard to see especially in newborns with dark skin.
• Kramer rule helps to estimate the degree of neonatal jaundice depending onthe body parts presenting with jaundice.
Causes and risk factors of neonatal jaundice
The known risk factors for neonatal hyperbilirubinemia include:• Delayed breast feeding and Lactation failureWhen red blood cells break down, a chemical called ‘bilirubin’ is released,
• ABO incompatibility (simply maternal–infant incompatibility in ABO system.
and this makes the skin to become yellow.
Premature birth (<38 week). A newborn’s immature liver often can’t remove
bilirubin quickly enough, causing an excess of bilirubin.• Post-term and macrosomia. Those newborn babies are born with high amountModerate signs and symptoms of neonatal jaundice
of RBC and need to break down them. Therefore, a lot of red blood cells, but
their liver isn’t developed enough to get rid of the bilirubin. This results in a
bilirubin overload, which leads to jaundice.
• Maternal and neonatal infection /sepsis
• Cephalohematoma,
• Birth asphyxia (Apgar score ≤6)
• G6PD enzyme deficiency,
• Other causes and risk factors are: low birth weight, Neonates from diabetic
mothers, neonates with siblings ‘history of severe neonatal jaundice,
hypothermia and hypoglycemia.
jaundice usually appears first on the face and then moves to the chest, belly, arms,
and legs as bilirubin levels get higher. Symptoms include yellowing of the skin and
eye conjunctiva within days after birth. In most cases, treatment isn’t required. Light
therapy (phototherapy) can help resolve moderate or severe cases.
Self-assessment 3.11
1. What are are the complications of very high levels of bilirubin to the
neonate?
2. What is Kernicterus?3. Which babies are more likely to develop jaundice than others?
3.12 Classification, diagnosis and management of neonataljaundice
Learning Activity 3.12 a. What do you think about the above image?Classification of neonatal jaundice
a. What do you think about the above image?Classification of neonatal jaundice
b. What do you think about how that blue light on image can help in neonataljaundice management?
Physiological jaundice: A newborn’s immature liver often can’t remove bilirubin
quickly enough, causing an excess of bilirubin. Jaundice due to these normal
newborn conditions is called physiologic jaundice, and it typically appears on the
second or third day of life it also characterized by the following;• Appears after at least 24 hours of birth,Pathological jaundice: is the most serious type of jaundice. It occurs within 24
• Peak after four or five days.• It later disappears after about 2 weeks of life.
hours after birth, and is characterized by a rapid rise in a baby’s bilirubin level. The
most likely cause is blood incompatibility or liver disease. Prompt medical attention
is necessary, and blood transfusions may be required and characterized by the
following:
• Appears within less 24hours
• Indirect bilirubin elevated
• Colored stools and urine
• Poor feeding
• Lethargy and excessive sleepiness• Change in muscle tone.
Symptoms of severe neonatal jaundice
The following symptoms will indicate that the baby has sever jaundice:• Crying inconsolably or with a high pitch.Diagnosis of neonatal jaundice
• Arched like a bow (the head or neck and heels are bent backward and the
body forward).
• Has a stiff, limp, or floppy body.• Have strange eye movements.
At a minimum, babies should be checked for jaundice every 8 to 12 hours in the
first 48 hours of life. The baby may be seen by a specialized nurse or physician
when the baby is between 3 and 5 days old, because this is usually when a baby’s
bilirubin level is highest. If the baby is discharged before age 72 hours, the baby
should be seen within 2 days of discharge.
Jaundice diagnosis is firstly based on symptoms such as yellowish of the skin,
eye conjunctiva and the whites of the eyes. All newborns are checked for jaundice
before leaving the hospital or birth center. However, on the other side, the bilirubin
tests may be done through blood sample collection to laboratory and bilirubin check
machines.
The associate nurse may check the baby’s bilirubin using a light meter that is placed
on the baby’s head. This results in a transcutaneous bilirubin (TcB) level. If it is high,
a blood test will likely be ordered.
The best way to accurately measure bilirubin is with a small blood sample from
the baby’s heel. This results in a total serum bilirubin (TSB) level. If the level is
high, based upon the baby’s age in hours and other risk factors, treatment will
likely follow. Repeat blood samples will also likely be taken to ensure that the TSBdecreases with the prescribed treatment.
Management of neonatal jaundice
The management of neonatal jaundice depends on the cause of the jaundice, the
bilirubin levels, and a baby’s age.– Mild jaundice goes away after 1 or 2 weeks as a baby’s body gets rid of the
extra bilirubin on its own. For newborns with breastfeeding jaundice, mothers
should breastfeed the baby more often. If the baby is not getting enough
breast milk, the specialized health care provider may suggest supplementing
with formula.
– For more serious cases of jaundice, treatment should start as soon as
possible at hospital.
– Always, encourage and support for frequent lactation and breastfeeding in
case of jaundice
• Ensure good hydration, (dehydration will cause bilirubin levels to rise moreup)
• Monitor vital signs as frequent as possible.Self-assessment 3.12
• Phototherapy. Babies lie under lights with little clothing so their skin is exposed.
The light changes the bilirubin to a form that can easily pass out of the body.• Light therapy blankets may also be used.
1) Why is it necessary to ensure good hydration on the neonate with jaundice?
2) What will be done to manage mild jaundice?
3) How phototherapy treats neonatal jaundice?4) What is the best way to accurately measure neonatal hyperbilirubinemia?
3.13 Neonatal hypoglycemia
Learning Activity 3.13
Baby MD was born one hour ago, at 40 weeks’ gestation, to a mother with
gestational diabetes. The birth weight was 4200gms and the APGAR score
of 10/10. Two days after birth, the neonate baby was brought in neonatology
unity presenting lethargy, irritability, jitteriness, high-pitched cry sometimes andinability to suck on breast.
Read the scenario and think about it:
a) What do you think about the condition of the baby described in scenario?Neonatal hypoglycemia, defined as a plasma glucose level of less than 30 mg/b) What do you think could be the risk factor to the condition of that baby?
dL (1.65 mmol/L) in the first 24 hours of life and less than 45 mg/dL (2.5 mmol/L)
thereafter, is the most common metabolic problem in newborns.
Hypoglycemia is common in neonates but often asymptomatic or presents with
non-specific signs. Recurrent or persistent hypoglycemia can lead to neurologicalsequelae.
Causes of hypoglycemia in a newborn baby
Hypoglycemia can be caused by conditions such as:• Poor nutrition for the mother during pregnancyThe newborns at risk for hypoglycemia:
• Making too much insulin because the mother has poorly controlled diabetes
Incompatible blood types of mothers and baby (severe hemolytic disease of
the newborn)
• More insulin in the baby’s blood for other reasons, such as a tumor of the
pancreas
• Birth defects
• Congenital metabolic diseases or hormone deficiencies. Some of these run
in families.
• Not enough oxygen at birth (birth asphyxia)
• Liver disease
• Infection (certain medicines the mother may have been taking for diabetes at
the time of birth, such as sulfonylurea medicines, can cause sepsis or other
severe infections).
Babies who are more likely to have hypoglycemia include those who are:• Born to mothers with diabetesSymptoms of hypoglycemia in a newborn baby
• Small for gestational age or growth-restricted
• Preterm babies, especially those with low birth weights
• Born under significant stress
• Large for their gestational age
Signs of low blood sugar may not be easy to see in newborn babies. The most
common signs include:
• Shakiness
• Blue color to skin and lips (cyanosis) or pallor
• Stopping breathing (apnea) or fast breathing
• Low body temperature (hypothermia)
• Floppy muscles (poor muscle tone)
• Not interested in feeding
• Lack of movement and energy (lethargy)
• Seizures
• Weak or high-pitched cry
Diagnosis
• Blood glucose < 2.5 mmol/l or < 45 mg/dl. Blood glucose is measured on a
sample of capillary blood taken from the lateral aspect of the heel using a
lancet or 24G needle.
• Always check blood glucose:• In neonates at risk of hypoglycemia
In neonates presenting with one of these signs:• HypothermiaComplications of neonatal hypoglycemia
• Irritability or tremors
• Bradypnoea or apnoea or cyanosis
• Hypotonia or poor response to stimulation or impaired consciousnessSeizures.
Major long-term sequelae include neurologic damage resulting in mental retardation,
recurrent seizure activity, developmental delay, and personality disorders. Someevidence suggests that severe hypoglycemia may impair cardiovascular function.
Management of hypo glycaemia
• Feed neonate immediately (preferably breast milk).
• If no milk is available, give 5 ml/kg of 10% glucose PO over 5 to 10 minutes.
Check blood glucose after 30 minutes:
• If it is normal (≥ 2.5 mmol/litre or ≥ 45 mg/dl), ensure the neonate feeds
regularly and check blood glucose again before each feed until there are 3
consecutive normal results.
• If it remains < 2.5 mmol/litre or < 45 mg/dl), treat as recurrent hypoglycaemia.
• Note: only if it is impossible to give an infusion or place a gastric tube, 1 ml/
kg of 50% glucose can be administered sublingually.• Frequent monitoring of vital signs is necessary
Self-assessment 3.13
1) Briefly explain which babies are at risk for neonatal hypoglycaemia
2) State the signs and symptoms of neonatal hypoglycaemia3) Explain which neonates should be screened for neonatal hypoglycemia.
3.14 Neonatal cyanosis
Learning Activity 3.14
What do you reflect on image A?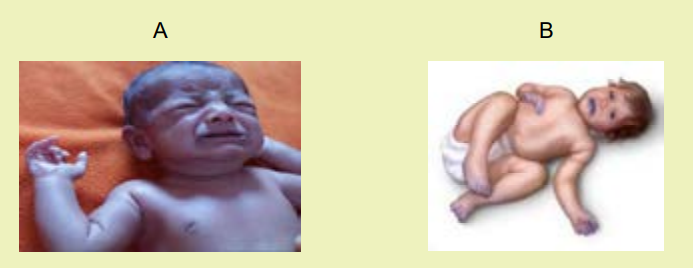
What do you reflect while observing image B?
Cyanosis is a blue discoloration of the skin and mucus membranes caused by an
increased concentration of reduced hemoglobin (>1.9–3.1mmol/L) in the blood. It
is most easily seen where the skin is thin, such as the lips, mouth, earlobes and
fingernails. Cyanosis indicates there may be decreased oxygen attached to redblood cells in the bloodstream. It may suggest a problem with the lungs or heart.
Cyanosis is a common clinical finding in newborn infants. Neonatal cyanosis,
particularly central cyanosis, can be associated with significant and potentially
life-threatening diseases due to cardiac, metabolic, neurologic, infectious, andparenchymal and non-parenchymal pulmonary disorders
Types of neonatal cyanosis
• Acrocyanosis/ Peripheral cyanosis: refers to the cyanosis found in the
extremities, particularly the palms of the hands and the soles of the feet. It
can also be seen on the skin around the lips. Acrocyanosis is often normal
in babies, as long as no cyanosis is present in the central part of the body.
This is relatively common in neonates, and is generally a physiologic finding
due to the large arteriovenous oxygen difference that results during slow flowthrough peripheral capillary beds.
• Central cyanosis: refers to cyanosis found on “central” parts of the body,
including the mouth, head and torso. Central cyanosis is never normal in the
newborn period, and is almost always linked to a lower amount of oxygen in
the blood. Central cyanosis indicates the presence of potentially serious and
life-threatening disease, and requires immediate evaluation. It could be dueto a problem of the heart, lungs or blood.
Causes and conditions triggering the neonatal cyanosis
The following may be the causes and conditions triggering the neonatal cyanosis:• Primary pulmonary disease on the neonate.Cyanosis is usually caused by abnormalities of the heart, the lungs or the blood.
• Congenital cardiac malformations.
• Upper airway obstruction on the neonate.
• Persistent pulmonary hypertension of the newborn (PPHN)
• Neonatal sepsis.
• Neonatal anemia.
• Neonatal polycythemia.
• Birth asphyxia.
Under normal conditions, after receiving oxygen from the lungs, red (oxygen rich)
blood is delivered from the heart to the rest of the body. When it returns to the heart,the blue (oxygen poor) blood is shipped to the lungs to collect more oxygen.
Abnormalities in the lungs that can prevent oxygen from entering the blood,which can lead to cyanosis.
Some examples of lung abnormalities that can lead to cyanosis include:• Events that limit the amount of oxygen (smoke inhalation from house fires,
carbon monoxide poisoning, etc.)
• A blockage in the airway that limits the amount of oxygen getting into your
lungs (choking on a foreign body, croup, etc.)
• Primary lung disease (asthma, pneumonia, bronchiolitis, etc.)
• Congenital heart abnormalities can cause some blue (oxygen poor) blood
to bypass the lungs altogether and never collect oxygen (see below).
Abnormalities in the blood can decrease its ability to absorb oxygen. All of
these abnormalities cause blue (oxygen poor) blood to get pumped to the
body.Management of neonatal cyanosis
• Most cyanosis in neonates is a result of “acrocyanosis” and does not needincreasing concerns about the potential risks associated with this therapy
treatment. If there is a primary lung or heart issue, cyanosis will go away
when the neonate has the underlying condition treated either medically or
surgically.
• Severe cyanosis requires urgent supportive therapy while a diagnosis is
established. The infant should be maintained in a thermos-neutral environment
using a radiant warmer. Oxygen should be provided, although there are• Close monitoring of vital signs is requiredNeonatal pallor
• Ensuring adequate breastfeeding to the neonate is also important• Prevention of hypothermia and hypoglycemia is necessary
The neonatal pallor (whitish color) indicates a perceived decrease in rubor in the
skin and mucous membranes of a neonate, which is associated with decreased
oxyhemoglobin delivery to the skin or mucous membranes. it is more evident onface and palms.
Causes of neonatal pallor:
• Illness,
• Emotional stress,
• Anemia and• Any other condition that can reduce the amount of ox hemoglobin.
Management of neonatal pallor
• The management of neonatal pallor is based on its etiology
• Close monitoring of vital signs is required
• Ensuring adequate breastfeeding to the neonate is also important• Prevention of hypothermia and hypoglycemia is necessary
Self-assessment 3.14
1) Diferentiate acrocyanosis and central cyanosis.
2) Describe conditions that may cause cyanosis to the neonate.
3) What can be the cause of neonatal pallor?
3.15 Neonatal gastro intestinal problems
Learning Activity 3.15Read the scenario below and reflect on it.
The new-born baby boy on day 8 of life was brought to the hospital by his mother
who reported that it’s now 36hours since her baby developed vomiting, abdominal
distension. She added that it is becoming more repeated and she is worried.
Upon the nurses’ observation the neonate looks weak, and vomits every after
poorly feeding. Respiratory rate 30cycles, heart rate 138bts/min, temperature
350c, spo2 96%. Immediately, the baby was admitted and the management
started. Then, after 6 hours of admission, the neonate baby developed diarrhoea
where he passed watery stool 4 x in 1 hour.a) What do you think about this baby?Vomiting or more often, regurgitation is a relatively frequent symptom during the
b) What do you think that can show you that this baby is critically sick?
newborn period. In most cases this is unimportant and rarely persists beyond the
first few feeds. However, there are circumstances when the type of vomiting is
important.
Many newborns vomit; in most cases when vomiting is significant.
The following conditions can signify severe signs:
• Vomitus contains blood (red or black, the colour of the blood will depend upon
how long the blood has been in the stomach)
• Vomiting green bile can indicate a bowel obstruction, which needs immediate
attention.
• The baby is projectile vomiting
• The baby is failing to thrive,
• The baby has gastro esophageal reflux and could be aspirating,
• The baby also has diarrhea
• The abdomen is distended.
• Delay in passage of meconium
• The baby is dehydrated (dry mouth, decreased wet nappies, hypotonic).• Vomiting causing choking and aspiration.
The commonest cause of vomit containing blood is swallowed maternal
blood. Swallowed blood often irritates the stomach and causes vomiting. Bloodmay be swallowed during: child birth and breastfeeding.
Causes of vomiting
The most common causes of vomiting in the neonatal period include gastroenteritis,malrotation, pyloric stenosis and necrotizing entero-colitis
Vomiting Scale:
• Mild: 1 - 2 times/day
• Moderate: 3 - 7 times/day
• Severe: Vomits everything, nearly everything or 8 or more times/day
• Severity relates even more to how long the vomiting goes on for. At the start
of the illness, it’s common for a neonate to vomit everything. This can last
for 3 or 4 hours. The neonate then often become stable and change to mildvomiting.
The main risk of vomiting is dehydrationManagement of vomiting
• Rehydrating the neonate is well-hydrated is the first step,ABDOMINAL DISTENSION IN THE NEW BORNS
• If the new born is repeatedly vomiting and is unable to hold down fluids
provide IV fluids (Normal saline).
• Search for causes of diarrhea and vomiting and treat or refer for treatment in
a specialized health setting.
• The associate nurse should refer this baby urgently,
• Close monitoring of vital signs is required,
• Ensuring adequate breastfeeding to the neonate is also important,• Prevention of hypothermia and hypoglycemia is necessary.
Abdominal distension is a common clinical presentation in neonates admitted
to neonatal intensive care units (NICUs), especially preterm infants. Neonates can
present with abdominal distention during a feed advance or a change in type offeed.
Causes of abdominal distension in the new borns
Congenital malformations may be the major cause of abdominal distension in
early newborns. Sepsis and congenital megacolon are the single disease most
frequently associated with abdominal distention in preterm and full-term newbornsrespectively
Other causes: failure to pass meconium majority pass within 24 hrs, delayedpassage of meconium (lubricated per-rectal thermometer may be therapeutic).
Management of neonatal abdominal distension
The management of neonatal distended abdomen. However, the nurse must ensureclose monitoring of vital signs is required and adequate breastfeeding
NEONATAL DIARRHEA
Neonatal diarrhea is when the newborn baby passes very runny, watery stools,
sometimes at an increased frequency or more volume than normal. There may be
mucus in the stool. Diarrhea is sometimes associated with vomiting. Diarrhea isoften caused by a bacterial or viral infection.
Management of neonatal diarrhoea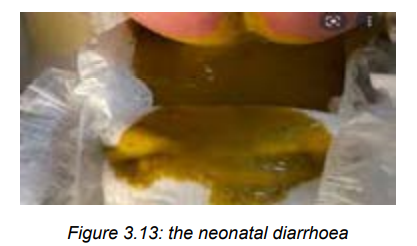
– The management is based on dealing with the cause of diarrhoea
– Hand hygiene is important in management of neonatal diarrhoea,
– Rehydrating the neonate is well-hydrated is the first step,
– If the neonate has severe diarrhea and is unable to hold down fluids provide
IV fluids (Normal saline).
– Search for causes of diarrhea and vomiting and treat or refer for treatment in
a specialized health setting.
– The associate nurse should refer this baby urgently,
– Close monitoring of vital signs is required,
– Ensuring adequate breastfeeding to the neonate is also important,
– Prevention of hypothermia and hypoglycemia is necessary.
Self-assessment 3.15
1) What the nurse will fear if the neonate baby vomits greenish like vomit?
2) When vomiting may be significant to the neonate baby?3) Using a scale, classify the neonatal vomiting.
3.16 Red, swollen eyelids and pus discharge from the eyes in thenewborns.
Learning Activity 3.16
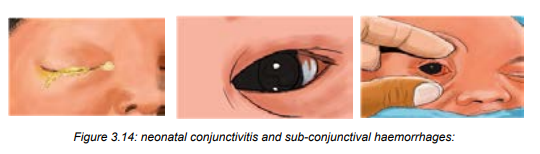
From the observation of the mentioned above pictures, reflect to them;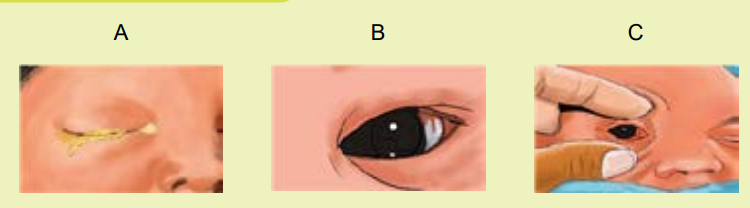 a) What do you think on the newborn’s eyes seen on image A?Neonatal red eye/ Neonatal conjunctivitis: is a red eye in a neonate caused by
a) What do you think on the newborn’s eyes seen on image A?Neonatal red eye/ Neonatal conjunctivitis: is a red eye in a neonate caused byb) What do you reflect on image B and C?
infection, irritation, or a blocked tear duct. When caused by an infection, neonatal
conjunctivitis can be very serious.
Conjunctivitis, or pink eye: is an irritation or inflammation of the conjunctiva, which
covers the white part of the eyeball. Conjunctivitis can be extremely contagious and
is spread by contact with eye secretions from someone who is infected.
Sub-conjunctival hemorrhages of the neonate: are red spots or bruises of the
eye that are common in new-borns and typically result from the normal trauma of
birth. As new-borns are squeezed through the birth canal blood vessels (on the
eyes and elsewhere) can rupture.
Causes of neonatal conjunctivitis
Conjunctivitis in neonate can be caused by an infection (bacteria or viruses.) or by
a reaction to chemicals put into the eyes (called chemical conjunctivitis).
If certain bacteria are present in the mother’s vagina, they can be passed to
the new-born during delivery. Such bacteria include Chlamydia, Streptococcus
pneumonia, Haemophilus influenza, Neisseria gonorrhoea, and others. Chemicalconjunctivitis is a reaction to the eye drops that neonates receive to prevent infection.
Symptoms neonatal conjunctivitis
Symptoms of conjunctivitis may vary depending on the cause of the infection.
Symptoms include redness, itching, swelling, or tenderness and tearing of the eyes.
Eye discharge or crusting around the eyes can be present.
Sub-conjunctival haemorrhage may present a bright red patch appearing in the
white of the eye.
Conjunctivitis caused by chlamydia usually begins 5 to 14 days after delivery but
sometimes as late as 6 weeks after. New-borns have swollen eyelids and a watery
discharge from the eyes that contains increasing amounts of pus. The infection cansometimes be severe.
Conjunctivitis caused by gonorrhoea usually begins 2 to 5 days after delivery.
New-borns have severe inflammation of the eyelids and discharge of pus from theeyes. Without treatment, blindness may occur.
Conjunctivitis caused by chemicals, such as eye drops, usually begins within 6 to8 hours after the drops are put in and goes away by itself within 2 to 4 days.
General prevention and treatment
• The tiny, delicate eyes of a neonate baby need proper care because it is
important to keep them clean and healthy.
• Using a soft a cotton ball (wool) and plain water, one can carefully cleanse
the baby’s eyes.
• Dampen the cotton ball with a little bit of lukewarm water.
• With the baby’s eyes closed, gently wipe the eyes from the inside to the
outside corners. Use a new cotton ball for each eye.
• Teach pregnant women the importance of treating sexually transmitted
infections, such as herpes simplex, gonorrhoea, and chlamydia in order to
decrease the incidence of neonatal conjunctivitis.• In Rwanda, tetracycline or silver nitrate eye ointment is routinely put intoSelf-assessment 3.16
each of the new born’s eyes after delivery to prevent conjunctivitis caused
by Neisseria gonorrhoeae.
• For conjunctivitis caused by Neisseria gonorrhoeae are given
ceftriaxone or cefotaxime injection.
• Treatment for conjunctivitis caused by Chlamydia, is treated
by erythromycin or azithromycin.
• For conjunctivitis caused by other bacteria, ointments containing polymyxinplus bacitracin, erythromycin, or tetracycline are applied.
1) What are the causes of neonatal conjunctivitis?
2) What are symptoms neonatal conjunctivitis?
3) Briefly discuss on prevention of neonatal conjunctivis after delivery.4) Describe sub-conjunctival haemorrhages of the neonate.
Summary of the unit of new born danger signs
Early detection of neonatal illness is an important step towards improving new
born survival. A mother is the nearest person to a neonate to identify, present, and
manage the neonates’ problem, which ensures that neonates can lead a healthy
life. If mothers know appropriate manifestations of the causes of death in new borns
(neonatal danger signs), it is possible to avert related neonatal mortality. Because of
the health-seeking behavior of mothers highly relies on their knowledge of neonataldanger signs.
Management of the new born danger signs:
Stabilize the neonate before transfer to the neonatal unit:
• Position the head to open the airway.
• Administer oxygen with an appropriate nasal cannula, at a maximum flow rate
of 2 litres/minute (aim for SpO2 90-95%).
• In the case of apnoea or if RR < 20/minute: perform bag and mask ventilation• Check blood glucose and/or treat for hypoglycemia.
While awaiting transfer:• Keep neonate warm in a room at 23-25 °C wrapped in a blanket or under anIn the case of severe respiratory distress, abdominal distension, or coma, do not
infant warmer, and cover the head with a cap.
• Closely monitor temperature, respiratory rate and SpO2
• Start treatment for neonatal infection
• Ensure routine neonatal care
• Start or continue feeding only if necessary, compliment feeds with a
nasogastric tube and/or IV fluids.feed the neonate by mouth. Start IV fluids if possible.
Neonates suspected to have severe neonatal infection. Danger signs may indicate
an underlying severe infection which requires transfer to a neonatal unit andantibiotic therapy.
While awaiting transfer to a neonatal unit, start antibiotic therapy: The
first line treatment is the combination of ampicillin IV + gentamicin IM.
Ampicillin is preferably used IV; the IM route is an option if the context
does not permit proper IV administration. To avoid multiple IM injections.
If meningitis is suspected, do not use procaine benzyl penicillin.
If the infection is cutaneous in origin, replace the ampicillin with cloxacillin IV.
Total treatment duration is 7 to 10 days according to clinical response. Gentamicin
should be stopped after 5 days of treatment.
3.17. End unit assessment 31. What are 9 danger signs on the neonate as described by WHO?
2. How can an associate nurse care for in infant with respiratory problems?
3. What are the consequences of the baby unable to breastfeed?
4. When is the neonate fed using naso-gastric tube?
5. What can be the error while taking the new born’s temperature taking?
6. Describe management of hyperthermia in neonate baby.
7. What are the complications of omphalitis to the neonate baby?
8. Describe the management of impetigo on the neonate baby.
9. What are the signs accompanying neonatal seizures a part from jerky
movements of eyes, libs and limbs?
10. When a mother has to suspect a neonatal jaundice to his/her neonate
baby and bring her/him to health setting immediately?
11. What are the major complications of neonatal hypoglycaemia?
12. What can an associate nurse think in case a generalized or central cyanosis
is realized to the neonate baby?
13. What are the major causes of neonatal distended abdomen to early new
borns?
14. What are the causes of neonatal diarrhoea?
15. Describe the management of neonatal diarrhoea and vomiting.
16. Describe the treatment of neonatal conjunctivitis caused by chlamydia..
