UNIT 1: POSTNATAL CARE
Key Unit competence:Monitor a mother during postnatal period
1.1 General assessment of the mother and its importance in theimmediate postnatal period.
Introductory activity 1
a) Observe these images and describe what you see.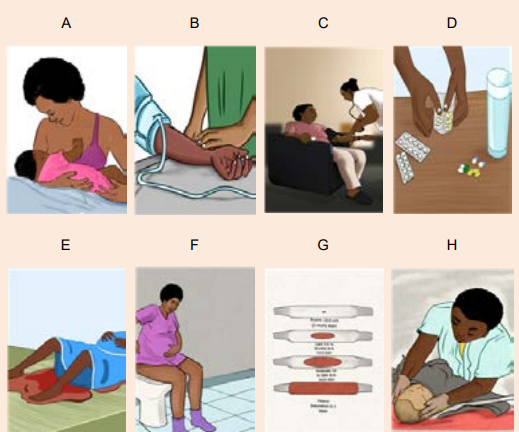
b) What are the needed materials to monitor a mother in postnatal period?
c) What is the importance of voiding in the immediate postnatal period?d) How can you explain blood loss in the immediate postnatal period?
Learning Activity 1.1
Observe these images illustrating a health care provider who is assessing themother in the postnatal period.
From the observation of above pictures,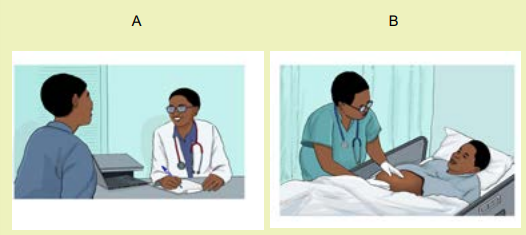
After child birth, the mother needs close monitoring where the health care
provider has to perform her assessment.
e) What do you think that could be the meaning of these images during the
assessment to this mother?
f) What do you think that could be an advantage of the assessment to thismother?
Obstetrics is the field of study concentrated on pregnancy, childbirth and the
postpartum period.
Postnatal period is the period beginning immediately after birth of a child and
extends for about six weeks of life. According to the World Health Organization,
(WHO) immediate postnatal period covers the first 24 hours from delivery of
the placenta while early postnatal period refers to the period from day 2 to 7 th
day and late postnatal period ranges from day 8 to 42nd day after birth. Therefore,
immediate postnatal care is the care given to the mother and the new born baby
immediately after the delivery of placenta until 24hours. The care includes the
prevention, early detection and treatment of complications, and the provision ofcounselling on breastfeeding, birth spacing, immunization and maternal nutrition.
Postnatal period is the time after birth, a time in which the mother’s body, including
hormone levels and uterus size return to a non-pregnant state.
During the assessment, the health care provider obtains the information from
the mother and this is called subjective data while the information obtained after
performing the physical examination is also called objective data.
Immediate postnatal assessment always starts from general assessment. The
assessment must be done in a way that the associate nurse starts from head totoes.
a) Importance of general assessment in immediate postnatal period
The importance of general assessment in the immediate postnatal period:
• To have the general picture of the mother’s well being
• To find out the level of consciousness
• To find out if the woman’s condition gives rise to concern• To find out the woman’s and baby’s urgent need of care
b) Safety considerations of general assessment in immediate postnatal
period
The safety considerations while performing general assessment in immediate
postnatal period are various but the following are considered to be essential:• Perform hand hygieneSelf-assessment 1.1
• Check room for contact precautions
• Introduce yourself to patient.
• Confirm patient ID using
• Explain process to patient.
• Be organized and systematic in your assessment.
• Use appropriate listening and questioning skills.
• Listen and attend to patient cues.
• Ensure patient’s privacy and dignity.
• Assess ABCCS (airway, breathing, circulation, consciousness, safety)
• Apply principles of asepsis and safety.
• Check vital signs• Complete necessary focused assessments
1. What is the importance of general assessment in immediate postnatal
period?
2. Enumerate 5 safety considerations before conducting general assessmentof the other in immediate postnatal period.
1.2 Techniques and elements of general assessment of the motherin immediate postnatal period.
Learning Activity 1.2
Observe these images showing the techniques that a health care can use duringthe assessment of the mother in postnatal period.
The health care provider may use different methods in order to obtain information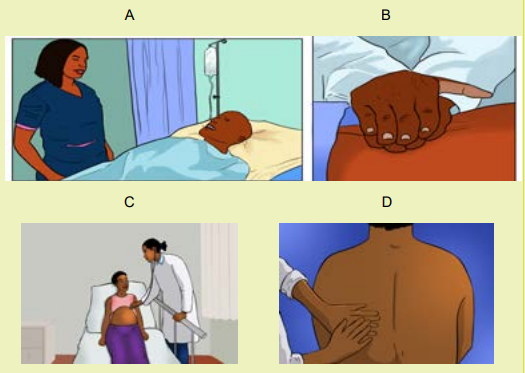
from the mother.
1. Which image that is showing an associate nurse receiving information by
looking the mother?
2. Which image that is demonstrating an associate nurse obtaining information
of the mother with the help of stethoscope and what does stethoscope helpduring the assessment?
There different techniques used in assessing the general status of the other in
immediate postnatal period including inspection, palpation and auscultation
Inspection:
In immediate postnatal period, observations should be performed as often asindicated by the woman’s clinical condition.
During the inspection, observe the mother’s: overall sense of wellbeing and
mobility. It is necessary to observe the general appearance, skin colour, level of
consciousness or mental status, and vaginal bleeding. Observe dyspnea-laboredbreathing, shortness of breath, and chest pain
On the breast, inspect for the redness and engorgement. On the abdomen;
inspect for the presence of visible scars, whether the abdomen is distended and itsmovement during the respiration.
Palpation
During the assessment of the mother, the associate nurse can use palpation for
assessing different parts like:• Skin (moist and cold skin indicate the mother is falling into the shock statusAuscultation
which can be related to postpartum haemorrhage)
• The conjunctiva (pale/whitish conjunctiva indicate anaemia and that might be
having postpartum haemorrhage)
• Pulse rate (fast and rising pulse indicate potential shock to the mother)
• Breast nipple for ensuring the presence of colostrum breast
• Bladder fullness
• Lower limbs for pitting oedema, warmth and signs of inflammation for negativeHoman’s sign.
Auscultation of bowel sounds with stethoscope for the mother in postpartumdelivered by caesarean section.
Self-assessment 1.2
1. What are the elements that can be assessed during inspection of the
mother in the postnatal period?
2. On lower limbs, what will you inspect and palpate for the mother?
3. Regarding Homan’s sign, what is the meaning of Homan’s sign in postnatal
care
4. What are the elements of auscultation to the mother in the immediatepostnatal period?
1.3. Nursing interventions during general assessment of themother in postnatal period.
Learning Activity 1.3
First 24 hours after birth: All postpartum women should have regular assessment
of vaginal bleeding, uterine contraction, fundal height, temperature and heart
rate (pulse) routinely during the first 24 hours starting from the first hour after
birth. Blood pressure should be measured shortly after birth.
a) What do you think about general assessment to the mother in immediate
postnatal period?
b) What do you think about advantages of regular assessment in immediatepostnatal period?
In the postnatal period, all these dynamic body systems (uterus, heart, lungs, blood
volume and blood contents, reproductive system, breasts, immune system and
hormones) have to adjust from the pregnant state back to the pre-pregnant state,
and there is potential risks of complications as these adjustments occur. Common
examples are postpartum haemorrhage, deep vein thrombosis (blood clots in the
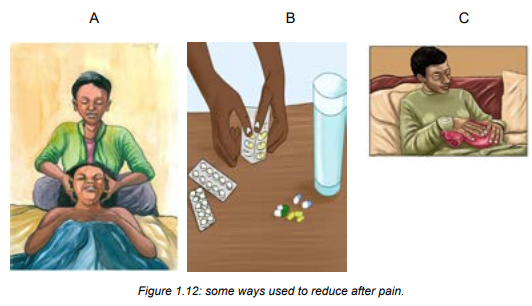
veins of the legs), infections and others. Additionally, women in the postnatal periodare often coping with stressful conditions (example is after pain, new born care).
To avoid and overcome complications related to physiological adjustments after
delivery, all mothers and their babies must receive active and ongoing assessment
and care in the immediate postnatal period. This is called ‘immediate postnatalcare’
In immediate postnatal care period the associate nurse must do the following
essential care:
• Assess the mother’s general status, vital signs, bladder fullness, uterine
retraction(involution), and vaginal bleeding
• Rehydration and nutrition support to the mother
• Provide hygiene (genital and perineal care, bed bath, bed making) to the
mother,
• Assess the psychological status of the mother focuses on three aspects:
mother’s reaction to the birth experience, the mother’s adaptation to the
infant and the family’s reaction to the infant. Then, provide education and
psychological support to the mother
• Assess degree of pain and provide pharmacological and non-pharmacological
pain relief method based on cause (episiotomy, lacerations or caesarean
section pain, breastfeeding, uterine involution.)
• Assess if no family centered care constraints( family support and involvement
in the care)
• Assess and ensure cleanliness of the mother(poor hygiene can lead to risk ofperipheral infections and patients’ discomfort)
Self-assessment 1.3
1. State the associate nurse interventions in the immediate postnatal period
care2. What is postnatal period?
1.4 General assessment of the baby in immediate postnatal periodPostnatal care encompasses aspects of obser
Learning Activity 1.4
Observe the following images which are showing the care provided to the babyin the postnatal period.
It is necessary to perform new born assessment after birth as it helps to rule out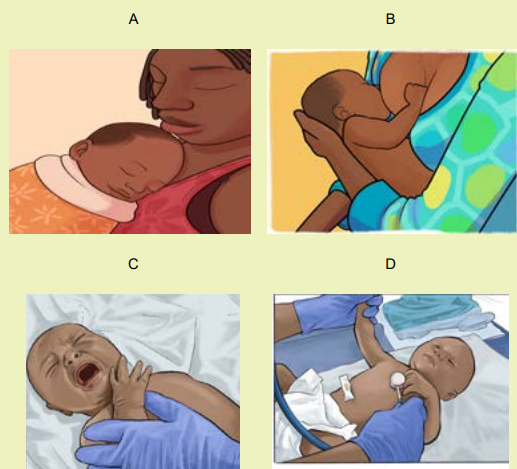
any abnormality.a) What are the general elements that you think the associate nurse can basePostnatal care encompasses aspects of observing and monitoring the health of theon in order to conduct the assessment of this baby?
mother and her baby, as well as offering support and guidance in breastfeeding andparenting skills.
Monitoring successful transition to extra-uterine life begins from the moment of
birth with an assessment of the APGAR score. This is measured at 1, 5, and if
needed, 10 minutes after birth, and is followed by an initial examination soon after
birth. A baby’s interactions with the parents during the first weeks of life are an
important pre-requisite for the continued wellbeing. The main elements of general
assessment for the baby in the immediate postnatal period include:• Skin colour (palor/ whitish color indicate the baby’s umbilical cord isSelf-assessment 1.4
bleeding, blue skin or cyanosis indicate respiratory distress)
• Respiratory rate (very or low respiration movement, noisy respiration, chest
indrawing, nasal flaring).
• Temperature (low body temperature is caused by exposure to coldness)
• Tone and activity (floppy and inactive baby is caused by hypoglycemia)
• Ability to breastfeed/feed (inability to breastfeed for the baby can expose
to hypoglycaemia, sudden death)
• Umbilical cord bleeding (cord bleeding cause anaemia and/or death of the
baby).
1. While assessing the baby in immediate postnatal period, what are the
causes of the following?
a) Paleness of the skin
b) Blue skin(cyanosis)
c) Floppy and inactive baby
d) Low body temperature
e) Very or low respiration movement, noisy respiration, chest indrawing,
nasal flaring.
2. What are the elements will you inspect on the baby in immediate postnatalperiod?
1.5 Practice of rapid general assessment of the baby
Learning Activity 1.5
Read the following case study of a newborn in immediate postnatal period.
Term baby boy born by spontaneous vaginal delivery, it’s now 4hours postdelivery.
the baby is number 1, baby is crying when associate nurse arrived
mother told her that the baby didn’t breast feed since birth, she has no knowledge
about breastfeeding.
a) By reading this scenario what do you think about this baby?
b) What do you think about this baby’s rapid assessment?
c) What do you think about help to this mother about baby feeding?
A key part of every postnatal nursing visit is to assess the new born for danger
signs, the common danger signs include; not feeding, lethargy (abnormal body
movements), fast breathing with chest in drawing, fever, hypothermia, jaundice and
convulsions.
Assessment of new born in immediate postnatal care includes;• Observe the baby’s general condition, including colour, responsiveness,
activity, spontaneous movement, feeding, and posture and muscle tone. ...
• Assess the head and skull for any abnormal findings (bulging or depressed
fontanelle). Depressed fontanelle indicates dehydration or bleeding. Bulging
fontanelle indicate intracranial bleeding or hematoma• Assess the eyes and sleepiness.
Assess for any of the following danger signs:
• History of difficulty feeding or unable to feed now; asks the mother about theobserved on the palms of the hands and soles of the feet.
baby’s feeding pattern.
• History of convulsion or convulsing now; asks the mother, has the baby had
any fits?
• Newborn seems lethargic or unconscious.
• Movement only when stimulated.
• Fast breathing.
• Severe lower chest in-drawing.
• Fever.
• Hypothermia (baby is cold to the touch).• Baby developed yellowish discoloration before 24 hours of age; jaundice
• There is swelling of the eyes or eye discharge.
• Umbilicus is bleeding or tie loosen
• More than 10 pustules (spots) are found on the skin
• Record findings, if anything unusual noted notify to the senior staff immediatelyand reassure the parents
Education to the mother about
• Baby care includes; breastfeeding, cord care, baby birth and clothing,Self-assessment 1.5
prevention of hypoglycemia and immunization.
• Hygiene and nutrition of the mother this includes; hand hygiene, body, perineal
care and balanced diet.
• Education about birth spacing and possible ovulation return.
• Education about danger signs to both mother and baby and when to comeback to hospital or when to alert care provider.
1. After assessing new born what education will you give to the mother?2. What will you do after noticing anything unusual?
1.6 Physiological changes and importance of vital signs monitoringin immediate postnatal period
Learning Activity 1.6
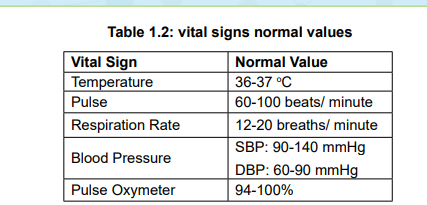
Image showing the materials used to take the vital signs like BP machine,thermometer, pulse oxymeter, watch, and stethoscope and pain scale.

You learned how to check the vital signs in Fundamentals of Nursing in S4.
a) What do you think that could be the importance of taking the vital signs of
the mother in the postnatal period?
b) What do you think about the use of thermometer?
c) What do you think about the frequency of taking vital signs in the immediate
postnatal period?
Vital signs are considered vital to the rapid assessment of the mother when it
is necessary to determine major changes in the mother’s basic physiological
functioning.
Physiological changes of vital signs monitoring in immediate postnatalperiod
Like other body systems change also vital signs undergo changes after delivery.
The following are changes that occur:
• Blood pressure
In immediate postnatal period, decreased blood pressure may result from the
physiological changes associated with the decrease in intra-pelvic pressure, or
it may be indicative of uterine haemorrhage. An increase in the systolic blood
pressure of 30 mm Hg or 5 mm Hg in the diastolic blood pressure, especially
when associated with headaches or visual changes, may be a sign of gestational
hypertension. Orthostatic hypotension may occur when the patient moves from asupine to a sitting position.
- Pulse rate
(bradycardia) commonly occur during the first 6 to10 days of the postpartum period.
During pregnancy, the weight of the gravid uterus causes a decreased flow of
venous blood to the heart. The elevated stroke volume leads to a decreased heart
rate. Postnatal tachycardia may result from a complication, prolonged labour, bloodloss, temperature elevation, or infection.
• Respiratory rate
The respiratory rate normal range of 12 to 20 respirations per minute elevated
respirations may occur due to pain, fear, excitement, exertion, or excessive blood
loss. Tachypnea, abnormal lung sounds, shortness of breath, chest pain, anxiety, or
restlessness are abnormal findings that must be reported. Immediately, these signs
and symptoms may be indicative of pulmonary oedema or emboli.
• Temperature
During the first 24 hours postpartum, some women experience an increase in
body temperature up to (38°C). High temperature at this time may be indicative ofinfection.
Self-assessment 1.6
1. What are the abnormal findings that must be reported while assessing the
respiration rate in immediate postnatal period?
2. While taking vital signs, when will you suspect that the mother is havingpostpartum haemorrhage?
1.7 Practice on the taking vital signs in the immediate postnatalperiod.
Learning Activity 1.7
Read the following scenario and with the aid of mannequin monitor this mother’s
vital signs.
28 years old mother P2 delivered by spontaneous vaginal delivery 1hour ago,
monitor Bp, pulse rate, body temperature, respiration, oxygen saturation and
pain score, every 30minutes for 2 hours and once every hour for next 3hours.
a) With aid of mannequin apply vital signs monitoring in immediate postnatal
period and record the findings and indicate rationale behind each vital sign
taking.
b) What do you think that the thermometer will help to the mother?
c) c) Which instrument do you think that it can help to auscultate the bowel
sound?
Vital signs monitoring is a fundamental component of nursing care because they
are essential in identifying clinical deterioration and that those vital parameters
must be measured consistently and recorded accurately in postnatal period.
Vital signs (blood pressure, heart rate, temperature, oxygen saturation, pain and
respiratory rate) are thought to undergo changes during and immediately afterdelivery.
Importance of vital signs monitoring in immediate postnatal period
Monitoring vital signs in immediate postnatal period and play the following role:• Help to detect the likely possible signs of shock
• Helps to prevent immediate postnatal related complication including
postpartum haemorrhage• Helps to intervene earlier if postpartumSelf-assessment 1.7• To promote maternal safety
1. What is the importance of monitoring vital signs to the mother in postnatal1.8 Protocol of vital signs monitoring in the immediate postnatal
period?2. List 6 vital signs you should monitor in immediate post-natal period.
period
Learning Activity 1.8
Read the case study below of mother in immediate postpartum period.
A 35 years old mother P3 in postpartum room 324 its now 1 hour postdelivery,
delivered by spontaneous vaginal delivery with intact perineum, she
is breastfeeding her baby boy without any problem and the nurse came in to
assess her wellbeing by monitoring of vital signs that is to say blood pressure
126/68mmhg, pulse rate 80bts/ min, respiration 20 cycles, oxygen saturation
98%, temperature 36oc, pain 4/10.a) Why do you think that it’s necessary to monitor vital signs of the mother in
the immediate postnatal period?
b) What do you reflect on the above pain score?
Monitoring vital signs in immediate postnatal period requires a close follow up.
Below is the protocol that can used for vital signs monitoring in the immediatepostpartum period.
Table 1.1: Frequency of vital signs monitoring in the immediate postnatalperiod
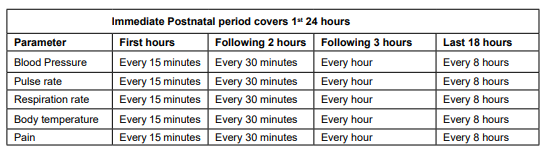
Interpretation of vital signs in immediate postnatal period
If her blood pressure is too low and falling, and her pulse and respiration rates
are too fast and rising, she is going into shock. The most likely cause is a l
life-threatening haemorrhage. If there are no signs of bleeding from the vagina, she
may be losing blood internally. The associate nurse can help the mother by telling
her on a scale of 0 to 10 and she may state how she feels pain. Having no pain is
characterized by 0 (zero) and 10 is the worst possible pain.
This tool can be used during pain assessment to the mother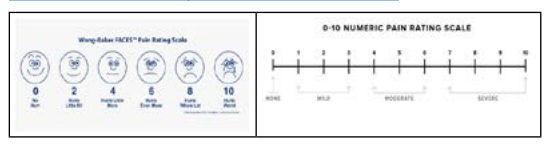
Self-assessment 1.8
1. Show the protocol of vital signs monitoring in immediate postpartum to 3
hours?
2. Interpret the following vital signs found from a mother who delivered 2
hours ago: Blood pressure (85/50), and pulse rate (120 beats/min) andrespiration rates (25 movements/minutes)
1.9 Techniques and importance of assessing bladder fullness inthe immediate postnatal period
Learning Activity 1.9
Read the following case study related to bladder fullness in immediate postnatal
period.
A 28-year-old primipara gave birth to a term 3 350 g baby in a maternity hospital.
She is admitted in postpartum ward and we are at 6 hour post-delivery. She is
complaining of abdominal pain, unable to void. She is sometimes having slight
bleeding. On examination, it was revealed that the episiotomy scar was intact and
there was no sign of perineal laceration. Physical examination of the abdomen
revealed a palpable and painful mass. Also the uterus is boggy and displaced on
lateral side of the abdomen. A urinary catheter was inserted and 3000 ml clear
urine was drained. After urine was drained, her pain was instantly relieved and
bleeding started to stop.Using the case described in the above scenario:
a) What do you think that could be the cause of distended abdomen to thisa. Techniques of assessing bladder fullness in the immediate postnatal
mother?
b) How long do you think that the spontaneous voiding should return to this
mother after birth?
c) What volume of the urine do you think that the mother is supposed to pass
per void in postnatal period?
period
To rule out the signs and symptoms of bladder fullness in the immediate postnatal
period, the associate nurse must do the following:• Observe if the mother has a full bladder (bulging or distension of the lowerSigns of bladder distension:
abdomen, displaced uterine fundus from the midline)
• Palpate the lower abdomen for assessing the bladder fullness tenderness
• Check for voidance amount. Expected volume is 150 ml for each void.• Location of the fundus above baseline level (determined with empty bladder)• Fundus displaced from midlineA full bladder will push the uterus up and toward the mother’s right side. Observing
• Excessive lochia
• Bladder discomfort
• Bulge of the bladder above the symphysis• Frequent voiding of less than 150ml each time
from the side, you might see what appears to be ‘camel humps’: the lower hump is
the bladder and the upper hump is the uterus.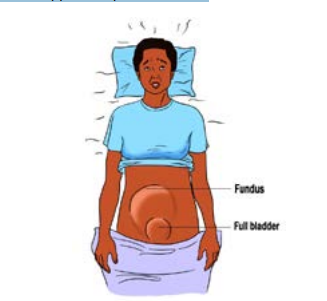
Figure 1.1: Image showing a mother with full bladder in immediate postnatal period
Importance of assessment and emptying full bladder in the immediate
postnatal period
Profound diuresis can begin immediately after delivery and spontaneous voiding
usually returns within 6-8 hours post-delivery. In immediate postnatal period,
the bladder fills rapidly after delivery due to the marked increase in urine production.
The urine volume should return to pre-pregnant levels by 2-3 days after delivery.
The importance of assessing and emptying the full bladder is:
• A full bladder can displace the uterus and lead to postpartum haemorrhage.
Therefore, assessing and emptying the full bladder can help in prevention of
postpartum haemorrhage.
• The woman who voids frequent, small amount of urine may have increased
residual urine because her bladder does not fully empty. Consequently,
residual urine in bladder may promote the growth of microorganisms and
formation of renal calculi if it takes long time. Therefore, assessing and
emptying the full bladder may help in prevention of postpartum urinary
tract infections.
• To promote optimal bladder function after delivery
• Reduce risks of uterine atone (bladder distension causes uterine atone)
• Reduce and manage postpartum after pains
• Reduce immediate postnatal stress to the mother due to increase after
pains related to full bladder
• Promote the wellbeing of the mother in postnatal period
• Assessment of the bladder function
• Assessment of the bladder function to the mother in postnatal period includes:
• Return of urination, which should occur within six to eight hours of delivery
• For approximately 8 hours after delivery, amount of urine at each void.
Patients should void a minimum of 150 mL per void; less than 150 mL
per void could indicate urinary retention due to decreased bladder tone
post-delivery (in the absence of preeclampsia or other significant health
problems).
• Signs and symptoms of a urinary tract infection (UTI), including frequent
urination, bladder spasm, cloudy urine, persistent urge to urinate, and
pain with urination
• The bladder should be not palpable above the symphysis pubis. Mothers
are encouraged to drink adequate fluid each day and to report signs and
symptoms of a urinary tract infection, including frequency, urgency, painful
urination, and hematuria.
Self-assessment 1.9
a. What is the importance of emptying urinary bladder in the immediate
postnatal period?
b. What are the techniques used to assess full bladder in the immediate
postnatal period?
c. What are the consequences of full bladder to the mother in immediatepostnatal period
1.10 Nursing interventions for full bladder in the immediatepostnatal period.
Learning Activity 1.10
Read this case study for the mother in postnatal period with a health
problem.
A mother called KD whose 31 years old, P2, G2 complained of unusual vaginal
bleeding and difficult in passing out the urine, abdominal pain, general body
weakness and distended abdomen at 4 hours after delivery. The vital signs
during the assessment revealed that the BP: 108/96 mmHg, pulse: 78 beats/
minute, temperature: 36.8 oc, respiration: 18 breaths/ minute. This mother has
delivered also by vaginal delivery without any episiotomy or perineal tear. Her
baby is breastfeeding with no problem.a) From this case study.The associate nurse must play a major role to ensure the bladder is empty. The
b) What do you think that may be the cause of that vaginal bleedingc) What do you suggest that can be done to help this mother?
following are the role of the nurses while emptying the bladder in immediatepostnatal period:
• Ask the mother to urinate within the first two to three hours. If she is too
tired to get up and walk, she can squat over a bowel on the bed or on the
floor, if she has urine retention she may need urinary catheter in place. If the
mother cannot urinate after four hours, and her bladder is not full, she may
be dehydrated.
• Help her to drink fluids
• Check bladder fullness frequently in post-delivery period.
• Encourage the woman to empty her bladder regularly
• Check the amount of voiding for measuring input and output
• If no void in 4-6 hours, encourage the mother to go to void
• Stimulate voiding by running tap water or pouring warm water over the
perineum if possible.
• Provide or help the mother to take plenty fluid
• If over 6 hours and the bladder is still full, refer her where the urinary cathetercan be used to empty the bladder.Self-assessment 1.10
• In setting where urinary catheterization is done for distended bladder (avoid
rapid emptying and do not remove more than 800 ml at one time – This prevents
a precipitous drop in intra-abdominal pressure and splenic engorgement andhypotension).
a) What are the strategies used to empty full bladder in the immediate
postnatal period?
b) What are the roles of the associate nurse during the technique of bladder
emptying?
c) When do you decide to refer the mother to go where the urinary cathetercan be inserted?
1.11 Concepts, physiology and importance of measuring fundalheight in immediate postnatal period.
Learning Activity 1.11
Techniques of measuring fundal height (In skills lab by use of mannequin)
Place the zero mark of the tape measure at the uppermost border of the uterine
fundus to uppermost border of the symphysis pubis. To locate the fundus, the
hand is moved down the abdomen below the symphysis pubis until the curved
upper border of the fundus is felt.a) What do you think that could be the importance of measuring the fundalConcepts, physiology and importance of measuring fundal height in
height in the immediate postnatal period?
b) Where do you think that the fundus may be located immediately after birth?
immediate postnatal period
Concepts
Fundal height: is the distance from the pubic bone to the top of the uterus measured
in centimeters.
Boggy uterus: refers to a clinical finding in which the uterus is identified as
enlarged and soft.
Uterine atony: is defined as failure of the myometrium to contract and retract
around the open blood vessels of the utero-placental implantation site following
childbirth. A hypotonic uterus, or “boggy” uterus, is among the most common
obstetrical conditions which may cause postpartum infection and postpartumhaemorrhage (PPH).
Uterine retraction: Retraction of the uterus is a phenomenon of the uterus in labour
or after delivery in which the uterine muscle fibers are permanently shortened.
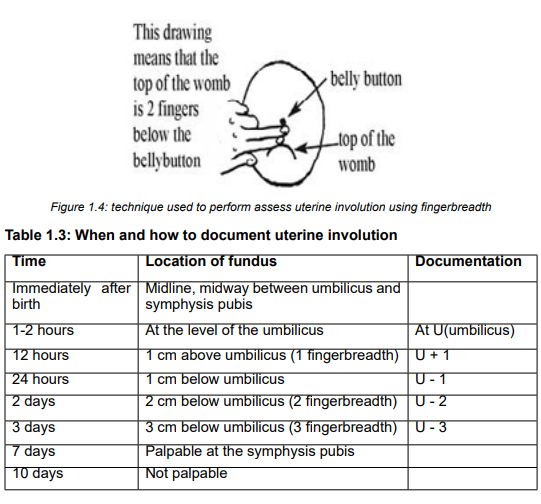
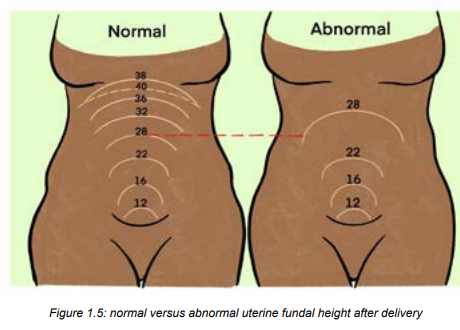
Physiology of fundal height after delivery
Usually, the progression of uterine descent into the pelvis is 1cm/day. Immediately
after delivery, the fundus is in the midway between umbilicus and symphysis
pubis. 1hour postpartum, the fundus is at umbilicus level or just slightly below
it. At 12 hours, the fundus is at 1cm above the umbilicus. At 24hours, it is at
1cm below the umbilicus. Day 2 to day 7, it decreases about 1cm/day. Day 7,
just palpable at the symphysis, Day 10-14, not palpable, Weeks 6, it returns to
non-pregnancy size.
Importance/role of measuring fundal height in immediate postnatal period
Assessing the fundal height allows identify:• The state of uterine involution progress
• Identify uterine tone and the cause of uterine atony related bleeding
• Prevent uterine atony related bleeding
• Help the other reducing after pains through uterine massage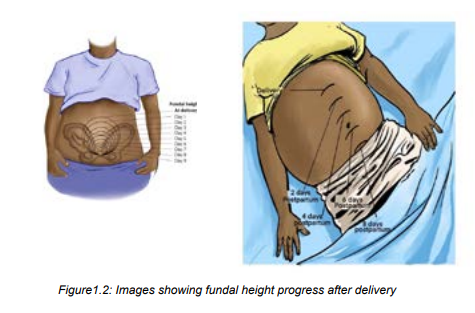

Self-assessment 1.11
Define the following terms:a) Fundal height1.12 Technique of assessing the fundal height in the immediate
b) Boggy uterus
c) Uterine retractiond) Uterine atony
postnatal period.
Learning Activity 1.12
Techniques of assessing uterine retraction (In skills lab by use of mannequin)
The mother GA delivered a baby boy in 45 minutes ago. When looking at her
abdomen, the uterus area still looks big, the mother is having slight bleeding. On
palpation, the associate nurse realizes the uterus is very soft and deviated at
lateral side of the abdomen.
By relating to the scenario described above, answer the following questions:a) What can be proposed as the materials to be used while measuring the
fundal height?
b) What do you think about the time of checking for the uterus contraction inWhile assessing the fundal height, below is the procedure of measuring the fundal height inthe postnatal period?
immediate postnatal period:• The fundus is assessed for approximately one hour post-delivery
• Ensure the bladder is empty before palpation of the uterine fundus.
• If the fundus is deviated or elevated above the level of umbilicus always rule
out distended bladder.
• Massage prior palpation and assess for any blood discharged during massage
• Using hand palpate the uterus and check if the fundus is firm
• Apply fingerbreadths (each fingerbreadth=1cm) or tape measure on uterus
and precise the fundus level of descent• Interpret and document findings on the patient’s file
Self-assessment 1.12
a) At what time does the fundus take to be located at 1 cm below the umbilicus
after delivery?
b) If the fundus is deviated or elevated above the level of umbilicus, what the
associate nurse will do prior to progress to further step of fundal height
assessment?
c) The fundus is palpable at the symphysis pubis at what time?
1.13 Physiology and importance of uterine retraction in immediatepostnatal period
Learning Activity 1.13
The mother GA 26 years old P1 delivered a baby boy, it’s now 2 hours and30 minutes
postpartum. When associate nurse palpates her abdomen during obstetrical assessment,
realises that; the uterus is still big 2 cm above the umbilicus and soft the mother is having
moderate vaginal bleeding, when the nurse takes vital signs they are in normal range
except pulse of 118bts/min.
By relating to the scenario described above, answer the following questions:a) What do you think about importance of checking softness or firmness of
the uterus in the postnatal period?b) What you think should be done before palpating the mother’s abdomen?
Physiology of uterine retraction in immediate postnatal period
Immediately after the placenta delivery, it begins to involute with contractions of the smooth
muscle of the uterus. It contracts midline with the umbilicus. The uterine contractions come
from effect of oxytocin. The fundus contracts downward towards the pelvis. The uterus
becomes firm and retracted with alternate hardening and softening. The failure of the uterus
to retract (uterine atone) leads to increased risk of postpartum hemorrhage.
Factors enhancing the uterine retraction include: uncomplicated labor, early initiation of
breastfeeding, complete delivery of the placenta.
Then, factors hindering the uterine involution include prolonged labor, incomplete separation
and expulsion of placenta, grand multiparty, full bladder and anesthesia.
Importance of uterine retraction in immediate postnatal period
Therefore, the following are importance of assessing uterine retraction:• Early prevention of postpartum hemorrhage caused by uterine atone orSelf-assessment 1.13
placenta retains
• Reducing risks of postpartum deaths due to postpartum hemorrhage
• Reducing the intensity of severe postpartum after pains as uterine massage
is always in the process of assessment of uterine retraction.
1. Which hormone is involved in immediate postnatal period uterine retraction?
2. Enumerate factors hindering the uterine retraction in immediate postnatal
period
3. What is the importance of uterine retraction assessment to the mother inpostnatal period?
1.14 Monitoring protocol and technique used in uterine retractionassessment and care
Learning Activity 1.14
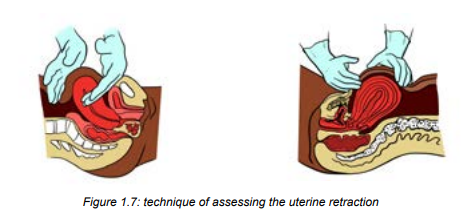
Observe the image below and read the technics used to assess uterineretraction.
Have the bladder empty prior to assessment
Make sure the woman is in a supine position
The health care provider should have one hand at the level of the umbilicus and
the other hand right about the symphysis pubis to stabilize the uterus
Palpate her abdomen to check contraction of the uterus to make sure it is firm.
Immediately after birth, you should be able to feel it is contracting near the
mother’s umbilicus.a. What do you think about stabilising of uterus during palpation and massaging?
b. What do you think about the time and frequency of checking the softness orfirmness of the uterus in the postnatal period?
a) Monitoring of uterine retraction in immediate postnatal period
The uterine retraction combined with uterine massage is generally performed every 10-15
minutes for the first hour after birth, and every 30 minutes during the second hour.
After the first two hours this massage usually happens every 4-8 hours until discharge.
b) Technique of uterine retraction assessment
• Have the bladder empty prior to assessment, a distended bladder may delay
the uterine retraction
• Make sure the woman is in a supine position
• The health care provider should have one hand at the level of the umbilicus
and the other hand right about the symphysis pubis to stabilize the uterus
• Palpate her abdomen to check contraction of the uterus to make sure it is
firm. Immediately after birth, you should be able to feel it is contracting nearthe mother’s umbilicus.
a) Monitoring of uterine retraction in immediate postnatal period
The uterine retraction combined with uterine massage is generally performed every 10-15
minutes for the first hour after birth, and every 30 minutes during the second hour.After the first two hours this massage usually happens every 4-8 hours until discharge.
b) Technique of uterine retraction assessment
• Have the bladder empty prior to assessment, a distended bladder may delay
the uterine retraction
• Make sure the woman is in a supine position
• The health care provider should have one hand at the level of the umbilicus
and the other hand right about the symphysis pubis to stabilize the uterus
• Palpate her abdomen to check contraction of the uterus to make sure it is
firm. Immediately after birth, you should be able to feel it is contracting near
the mother’s umbilicus.
• A boggy uterus, soft, displaced or associated with bleeding from midline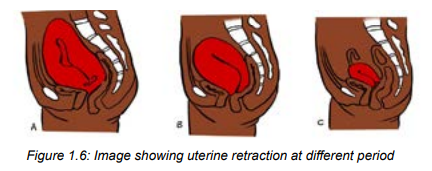
needs to be investigated
• Attention: The hand at the umbilicus will push down and in to feel the fundus
(feel if the uterus is firm or hard, soft or displaced laterally). The support is
need to help prevent uterine inversion and prolapse
• If the uterus is hard, leave it alone between checks. If it feels soft, rub/
massage the abdomen at the top of the uterus to help it to contract. (see the
video on YouTube)
• If the uterus is soft/boggy and resisting to uterine massage, misoprostol or
oxytocin may be administered
• At the end teach and demonstrate the mother how to do to self-massage• Thank the mother and record findings
Self-assessment 1.14a) Which schedule that can be respected during uterine massage after birth1.15 Physiology, causes and signs of blood loss immediate
for the first 48 hours?
b) What is the impact of full bladder on the uterine retraction?
c) What will the associate nurse do to prevent the uterine inversion while
checking and performing the uterine massage in postnatal period?
d) What will be the signs of a well retracted uterus in immediate postnatalperiod?
postnatal period
Learning Activity 1.15
Observe the image above and then read the following case study :
DM is 30 years old with G6, P6 mother who delivered a baby girl in 1hour ago the
associate nurse come to notice that the mother looks unhappy, reports feeling
cold, thirsty and sometimes feels dizzy. She has also; vaginal bleeding and her
bed sheets are soiled with blood. On examination the associate nurse finds
bleeding from vagina and the BP of 80/60, PR of 110beats/minute with signs of
increased respiratory movements.
By using the scenario above answer the following questions:a) What do you think can indicate unusual blood loss to that mother inPhysiology of postnatal blood loss
scenario?
b) What do you think about benefits of estimating the amount of blood loss inimmediate postnatal period?
After birth, it is normal for a woman to bleed the same amount as a heavy monthly period.
The blood should also look like monthly blood; old and dark, or pinkish. Immediately after
birth, the first the blood comes out in little spurts or gushes (lochia rubra) when the uterus
contracts, or when the mother coughs, moves, or stands up, but the flow should reduce over
the next two to three days.
Normally after delivery of placenta the expected blood loss 250mls therefore the nurse has
to monitor blood loss every 30 minutes for next 3hours, once an hour for next 3 hours.
It is important to recognize whether there is no excessive blood loss during childbirth, which
is a significant cause of morbidity and mortality.
Lochia
Lochia is normal discharge from the uterus after childbirth; it contains blood, mucous and
placenta tissue. Lochia discharge typically continues for 4-6weeks after childbirth (while the
reproductive organs return to their pre pregnancy state). Inspect the colour, odour and the
amount of lochia.
Types of lochia
Lochia is described using 3 names. Lochia rubra is the first vagina discharge colour lost
following birth of baby, it is dark red (red) in colour because it contains large amount of
blood, this amount comes from the wound left behind inside the uterus where the placenta
sheared away, it occurs for 3-5 days after birth. Lochia serosa is the term for lochia that has
thinned and turned brownish/ pink in colour, it continues until around the 10th day post birth.
Lochia alba is described as vaginal loss which has turned yellow /whitish. This typically
occurs after the 10th day and may last from the 2nd through to the 3rd and up to 6weeks afterbirth.
Lochia should not become offensive in smell or turn bright red after becoming serosa or
alba. If possible or happened, the mother should seek the health professional for additional
advice and care. When lochia subsides, the uterus is considered as closed, partial infection
is less likely. It is important to note that patients who had a C-section will typically have lesslochia than patients who delivered vaginally; however, some lochia should be present.
After discharge, patients should report any abnormal progressions of lochia, excessive
bleeding, foul-smelling lochia, or large blood clots to their physician immediately. Patientsare instructed to avoid sexual activity until lochia flow has ceased.
Patients who had a C-section typically have less lochia than patients who delivered vaginally;
however, some lochia should be present.
Signs and symptoms of blood loss in immediate postnatal periodSigns and symptoms of blood loss in immediate postnatal period vary depending on the
amount lost
The follow are the most common symptoms of postpartum haemorrhage:• Uncontrolled bleeding.• For heavy bleeding, the patient may experience loss of consciousness and
• Decreased blood pressure.
• Increased heart rate.
• Decrease in the red blood cell count.
• Swelling and pain in the vagina and nearby area if bleeding is from ahematoma.
other signs of symptoms of hypovolemic shock
Self-assessment 1.15
1. Explain the normal pattern of blood loss in immediate postnatal period
2. Normally after delivery of placenta the expected blood loss is:a) 600mls3. Explain signs and symptoms of mild blood loss in immediate postnatal
b) 500mls
c) 250mlsperiod
1.16 Methods of blood loss assessment in the immediate postnatal
period
Learning Activity 1.16
Observe the image below showing blood loss with in 1 hour after delivery.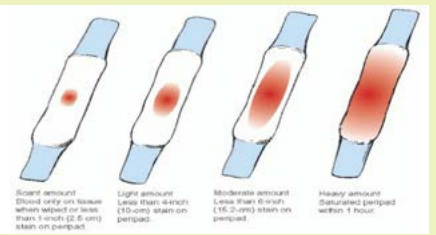
a) What do you think about image D?b) How do you think that the blood loss can be estimated?
In many instances, the birth attendant assesses blood loss by looking at the
amount of blood lost, and estimating its volume (visual estimation). This method
is available in all birth settings. In another method, the birth attendant places a
shallow bedpan below the mother’s buttocks, and then weighs the collected blood,
along with blood that has soaked into any pads and material. This is referred to
as an indirect method. In one direct method, a ‘calibrated delivery drape’ is placed
under the mother’s buttocks and tied around her waist, with the calibrated funnel
portion (that indicates how much blood she has lost) hanging down between her
legs. Other methods are also available, such as dye dilutions and radioactivetechniques, but these are not practical in many birth settings.
There are two methods of measuring blood loss:
One is by direct measurement of collected blood (swabs, pads, pampers etc) and
the other is by indirect measurement and later reflects blood loss by assessment of
haemoglobin concentration in the blood.
Very heavy bleeding is dangerous. To check for heavy bleeding in the first six hours
after birth and check the mother’s pads often, 500ml (about two cups) of blood loss
is too much. If she soaks one pad per hour, it is considered heavy bleeding. If the
mother is bleeding heavily, and you cannot stop it, take her to the hospital or ask for
help from other health care providers. Remember that postpartum haemorrhage is
a major cause of maternal mortality and it can happen at any time in the postnatalperiod.
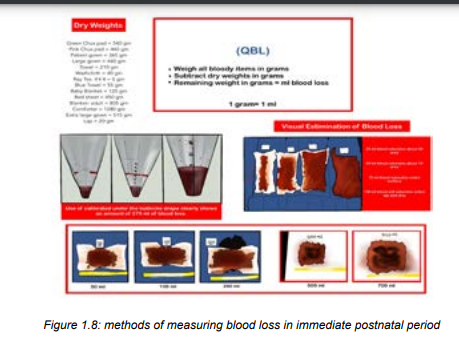
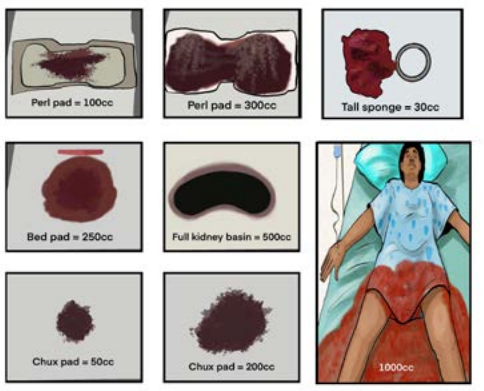
Figure 1.9: blood loss visual estimation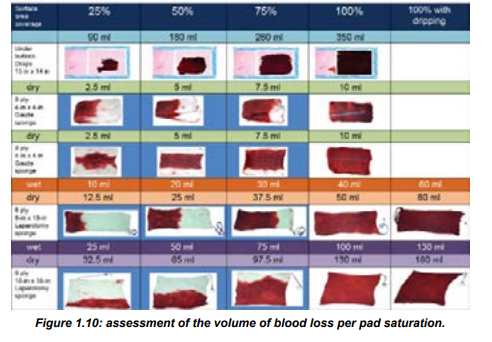
Lochia is assessed during the postpartum period:
Saturating one pad in less than an hour, a constant trickle of lochia, or the presence
of large (i.e., golf-ball sized) blood clots is indicative of more serious complications
and should be investigated immediately. A significant amount of lochia despite a
firm fundus may indicate a laceration in the birth canal, which should be addressedimmediately.
Foul-smelling lochia typically indicates an infection and needs to be addressed as
soon as possible
Episiotomy/perineal tear blood loss assessment and care
To assess episiotomy or perineal tear, the associate nurse must use a gloved hand
to gently examine the mother’s genitals for tears, haemorrhage, or a haematoma
(bleeding under the skin).
The acronym REEDA is often used to assess an episiotomy or laceration of the
perineum.
REEDA stands for:
R: Redness
E: Edema
E: Ecchymosis
D: Discharge
A: Approximation
Redness is considered normal with episiotomies and lacerations; however, if there
is significant pain present, further assessment is necessary. The use of ice packs
during the immediate postpartum period is generally indicated. There should be an
absence of discharge from the episiotomy or laceration, and the wound edges should
be well approximated. Perineal pain must be assessed and treated. Performing
Kegel exercises are an important component of strengthening the perineal muscles
after delivery and may be begun as soon as it is comfortable to do so. If a woman
has a tear that needs to be repaired, apply pressure on it for 10 minutes with a
clean cloth or pad and manage accordingly. If the tear is small, it can probably healwithout being sutured, as long as it is kept clean.
Self-assessment 1.16
1. What are the methods used for blood loss assessment in the immediate
postnatal period
2. Define the term lochia3. Differentiate the term lochia rubra from lochia serosa
1.17 Perineal and genital care
Learning Activity 1.17
Observe the images below showing perineal and genital care to themother in the immediate postnatal period.
a) What do you think about perineal and genital care in immediate postnatal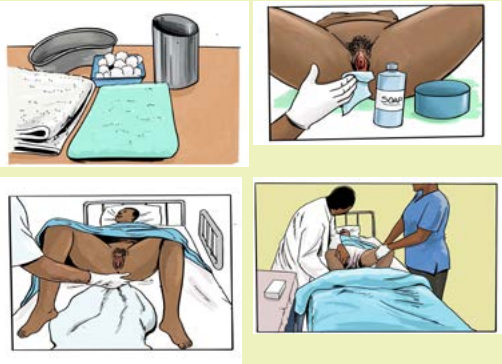
period?b) What do you think about changing pads and bedmaking in this period?\
In immediate postnatal period most of the time mothers are very tired due to labour
process and cannot care by themselves. The perineal care also helps to prevent
infection. Rinse the perineum with water after the use the toilet and before the
putting on a new peripad.
Therefore, it is the responsibility of the associate nurse to care those mothers, In
caring perineal and genital area, the associate nurse must always wash hands first
and put on surgical gloves before touching the mother’s genitals parts;
• Washing and cleaning the perineal and genital parts and changing pads after
birth must be done every 4-6 hours, or more frequently in case of heavy
bleeding or lochia and/or and after passing the stool.
• The associate nurse must clean the mother’s genitals very gently, using a
soap and very clean water and soap
• After cleaning the perineum and genital parts, the mother is dressed with
clean clothes and sanitary pad and changing of bed sheets for good hygiene,
infection prevention and making her comfortable.
• Cleaning perineal and genital area must be done in anteroposterior direction
from vulva to the anus. This is because even a too small piece of stool in
genital area can cause infection. Be careful not to bring anything up from the
anus toward the vagina.
• Disinfection of the episiotomy site or tear must be done if applicable.• Do not use alcohol or any other irritant disinfectants in genital area.
Self-assessment 1.17
1. Why is it necessary to clean perineum in anteroposterior direction?
2. Why is it discouraged to use alcohol or any other disinfectants to cleangenital area?
1.18 After pains care and education to the mother in the immediatepostnatal period.
Learning Activity 1.18
Read the following case study that is showing a mother having after pains in
postnatal period.
MD whose 28 years old with G4, P4 and lying on the bed in 5 hours postdelivery
by the arrival of associate nurse noticed that mother looks unhappy, and
complains lower abdominal most often when the baby is put on breast and she
fears to put the baby on breast. In addition to that episiotomy was done to her
while delivering and she fears to go to toilet. On palpation, the associate nurse
felt some contractions like at the uterine area and the uterus started to descend.
After the associate nurse helped her to relieve after pain, the associate nurse
started providing health education
Referring to the case described above, answer the following questions:a) What do you think it is after pains?The associate nurse is called to assist alleviating after pains and provide health
b) What do you think that may be the predisposing factors of after pain to
mother in postnatal period?
c) What can you suggest as at least one method to use in order to relieve
after pain?
d) What kind of education do you think should be provided by the associate
nurse to that mother?education to the mother in immediate postnatal period.
After pains care in immediate postnatal care
After delivery the uterus contract and relax as it shrinks back to its pre-pregnancy
status. This cramping also is called “after pains” It may feel like menstrual cramps
or even labor contractions. After-pains are contractions that occur after labor and
delivery. In addition, the perineum may be bruised, or the mother may have some
episiotomy stitches which can increase the pain in the immediate postnatal period.
The primiparous woman typically has mild after pains, if she notices them at all,
because her uterus is able to maintain a contracted state. Multiparas and patients
with uterine over distention (eg., large baby, multifetal gestation, hydramnios) are
more likely to experience after pains, due to the continuous pattern of uterine
relaxation and vigorous contractions.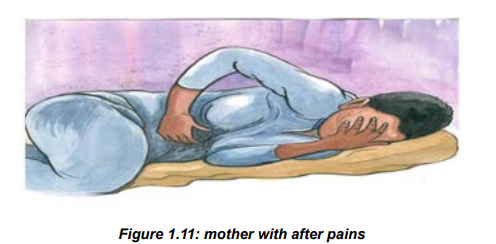
While providing emotional support, the associate nurse must do the following:
In addition to pain medication (ibuprofen, diclofenac) prescribed by the physician or
a midwife, the associate nurse can provide non pharmacological comfort techniquessuch as;
• Help the mother to place ice on the perineum to reduce swelling and pain• Apply warm compress or water bottle to lower abdomen
• Assist the mother to sitting and/or lie in positions that can help her feeling
more comfortable
• Prone position with small pillow under abdomen (that position applies pressure
to uterus and stimulates contraction.
• Guide relaxation and breathing techniques to the mother (read books on
relaxation and breathing technics)
• Keep the mother’s bladder empty
• Assisting the mother to immediately start breastfeeding after birth and
frequently as it helps alleviating after pains, for breast milk production and
helps and preventing hypoglycemia to the newborn.• Help if possible or advise the mother to start walking soon after delivery.
 The associate nurse is called to assist alleviating afterpains and provide healtheducation to the mother in immediate postnatal period.Education (hygiene, nutrition, breastfeeding, baby care, immunization, birth spacingand emotional support).In immediate postnatal period, the associate nurse should teach the mother about
The associate nurse is called to assist alleviating afterpains and provide healtheducation to the mother in immediate postnatal period.Education (hygiene, nutrition, breastfeeding, baby care, immunization, birth spacingand emotional support).In immediate postnatal period, the associate nurse should teach the mother about
the following:• Delaying the baby’s first bath to after the first 24 hours• Baby’s warmth through putting the baby skin-to-skin on mother’s abdomen,the hat on the baby’s head and dressing the baby not cold clothes.• Observing frequently umbilical cord for any bleeding and ensure hygieniccare of the baby’s umbilical cord stump.• Motivate the mother to stay closely to the baby for maintaining the bondbetween them• Encourage the mother to increase the fluid and food intake with increasingintake of fruits and vegetables in order to gain strength and maintain hydration.• Encourage her to go to void frequently for at least 2hours urine• Encourage mother early breast feeding especially in the first hour of life• Tell the mother to report immediately anything unusual like bleeding, severeheadache to her or umbilical cord bleeding, inability to breastfeed, anddifficulty breathing to her baby• Tell the mother to wash hands every time she comes from toilet beforechanging her pad or breastfeeding her baby• Encourage the mother have a shower if dirty to prevent risk of infection• Encourage the mother to change sanitary pads if dirty• Talk with mother during the assessment and care, teach her the thingsSelf-assessment 1.18
about her care as you go along, baby care, and ask her what she needs,
if she needs help let her have it. Example: perineal care when checking
the perineum, rationale for sits bath, use of local analgesics, rationale for
ambulation especially if a C-section, baby care like changing diapers, baby
bath, latching etc.
• Encourage the mother to limit visitors in order to get the rest, encourage her
to believe in herself and think positively about parental hood.
• Rest is usually encouraged during the first hours preferably in prone position
as this aids drainage from the uterus and vagina.
• Educate the mother about birth spacing and its benefits to mother, her baby,
family, community and entire nation.
Summary of the unit:A good method to remember how to check and care the mother in immediatepostnatal period is the use of the acronym BUBBLEHE:B: Breast.U: Uterus.B: Bladder.B: Bowel.L: Lochia.E: Episiotomy.H: Homans’ sign (to detect early DVT)E: Emotional response.1. Regarding after pains care answer the following questions:1.19. End of unit assessment 1
a) What are the non-pharmacologic comfort measures used to relieve
afterpains?
b) What will the associate nurse do to reduce swelling and pain on perineum
with tears or episiotomy?
c) What will the associate nurse do to reduce pain through positioning the
mother?
2. In teaching the mother in postnatal period answer the following questions:
a) What will you teach the mother regarding the baby’s warm and umbilical
cord
b) How would you instruct the mother on the time and frequency of
breastfeeding?
c) What can you teach the mother regarding taking fluid and food?
d) What are you supposed to teach the mother regarding elimination and
hygiene after elimination?
End of unit assessment 1
SECTION A: Multiple choice and true or false
1. A postpartum nurse is preparing to care for a woman who has just delivered a
healthy new born infant. In the immediate postpartum period the nurse plans to
take the woman’s vital signs:a) Every 30 minutes during the first hour and then every hour for the next2. A postpartum nurse is taking the vital signs of a woman who delivered a healthy
two hours
b) Every 15 minutes during the first hour and then every 30 minutes for the
next two hours.
c) Every hour for the first 2 hours and then every 4 hours
d) Every 5 minutes for the first 30 minutes and then every hour for the next4 hours.
new born infant 4 hours ago. The nurse notes that the mother’s temperature is
37.8°C3.
Which of the following actions would be most appropriate?a) Retake the temperature in 15 minutes3. The nurse is assessing a client who is 6 hours postpartum after delivering a
b) Notify the physician or the senior nurse
c) Document the findingsd) Increase hydration by encouraging oral fluids
full-term healthy infant. The client complains to the nurse of feelings of faintness
and dizziness. Which of the following nursing actions would be most appropriate?a) Empty the bladder for that mother4. What vital signs findings will be indicative of unusual vaginal bleeding in
b) Instruct the mother to request help when getting out of bed
c) Elevate the mother’s legs
d) Avoid bringing the new born infant to the mother until the feelings of lightheadedness and dizziness have diminished
immediate postnatal period?a) Hypertension5. What will indicate that the bladder is full in immediate postpartum?
b) Rapid pulse
c) Hypotensiond) Both b and c
a) Soft and flat abdomen.6. Answer by true or false. By assessing the uterine retraction, the following
b) Bulging and distended lower abdomen with painful on touch and displace
c) Distended uterus.d) Lower abdominal pain with urinary frequency.
statements will indicate to the associate nurse that the uterus in not well retracted
in immediate postnatal period.a) The uterus becomes firm and retracted.SECTION B: Short answers
b) The uterus becomes big in size but palpable.
c) The uterus becomes soft and boggy.
d) Unusual vaginal bleeding with bulging of lower abdomen.e) Hard uterus, non-tender and mild vaginal bleeding.
7. What an associate nurse will do in case he/finds the uterus is hard? -------
-- soft? ………………
8. While measuring the fundal height, where will the associate nurse
expect the uterine fundus: immediately after birth? …….. 2hours?
12hours…………………Interpret and document those findings.
9. In which situation is it necessary to wash and clean more frequently the
perineal and genital in immediate postnatal period?
10. What will be the techniques that the associate nurse will use to empty the
full bladder in immediate postnatal period?
11. In palpation, what will the moist and cold skin indicate to the mother?
12. In palpation, what will whitish (pale) conjunctiva indicate to the mother?
13. Which mothers are more likely to experience after pains compared to their
peers? Explain why
14. What medications can be given to the mother experiencing after pains
resisting to non-pharmacological methods?
15. To differentiate after pains with other abdominal pains, describe the
characteristics of after pains in postpartum period
16. While teaching the mother about rest in immediate postnatal period why
do we advise the mother to rest in prone position? Explain.
17. Briefly explain the components of inspection during general examination
of the mother in the immediate postnatal period.
18. Describe the physical checks you should do on postnatal mother soon
after delivery.
19. Describe the importance and expected normal findings for each vital sign
taken during immediate postnatal period.20. Describe how full bladder may cause postpartum bleeding
