UNIT 9 NURSING ASSESSMENT OF GENITO-URINARY SYSTEM
Key Unit Competence:
Take appropriate action based on findings of nursing assessment of genito-urinary
system.Introductory activity 9.0
Observe the images above and answer the following questions:
a. What do images above means to you?
b. Guess the lesson we are going to study.
c. List the anatomical parts illustrated on image B and D
Genito-urinary system combines both reproductive and urinary system. The
reproductive system serves to ensure the survival of species. To do so, it produces
ovum and sperm cells, transport and sustain these cells, nurture the growing offspring
and produce hormones. Gonads are the primary organs of the reproductive system;
it consists of ovaries and testes in female and male respectively. These organs
are responsible for producing the ovum and sperm cells and hormones. These
hormones function in the maturation of the reproductive system, the development of
sexual characteristics, and regulation of the normal physiology of the reproductive
system. The remaining organs, ducts, and glands in the reproductive system
are considered secondary, or accessory, reproductive organs. These structures
transport and sustain the gametes and nurture the developing offspring.
The urinary system has its upper part composed of two kidneys and two ureters
while its lower part consists of a urinary bladder and a urethra. The kidneys serve
as principal organs of the urinary system. The main functions of the kidneys are
to (1) regulate the volume and composition of the blood and (2) excrete waste
products from the body in the form of urine. The kidneys also function to control
blood pressure, produce erythropoietin, activate vitamin D, and regulate acid-base
balance. Urine is formed in the kidneys, drains through the ureters to be stored in
the bladder, and then passes from the body through the urethra.9.1. History taking of genitourinary system
Learning activity 9.1
Observe the image above and respond to the following question
a. What does the image A illustrate?b. What can be the reason behind the posture on image B
9.1.1. History taking of the genitourinary system
After greeting, introduction and listening the chief complaint of the patient,
the examiner will decide to ask specific questions to know the health status of
genitourinary system. The patient may report frequency, urgency, nocturia, dysuria,
hesitancy, straining, urine color change, penis pain, lesion and discharge, scrotal pain
and swelling, reduced sexual activity and sexual desire, contraception measures
and past genitourinary history. Menstrual history, obstetric history, menopause,
lower abdominal pain, vaginal discharge, and painful sexual intercourse are usually
female specific.
Here are questions to be used for appropriate history taking of the genitourinary
system:
1. Are you urinating more often than usual? Frequency said when an adult
patient reports to urinate more than 5-6 times per a day. Polyuria is the
excessive quantity of the urine, oliguria is a diminished quantity of the urine
< 400ml/24 hours, whereas anuria is the absence of urine or quantity <
100ml/24 hours. Urgency is when a patient can’t wait to urinate. Awakening
desire to urinate during the night is known as nocturia. The examiner will
go in deep and ask how many times per a night and if it is a recent change.
Frequency, urgency and nocturia mostly happen in urinary tract conditions
2. Do you feel pain or burning sensation during urination? Dysuria is common
in acute cystitis, prostatitis and urethritis.
3. Do you have difficult starting urine stream? Or do you need to strain to start
or maintain urine stream? Hesitancy and straining respectively indicate that
the patient has outlet obstruction due to benign prostatic hyperplasia.
4. What is the color, smell and consistency of the urine? The intensive
yellow to dark color of the urine indicates dehydration, cloudy in urinary
tract infection. Hematuria: presence of blood in the urine is a danger sign
that warrants further investigations. Some color changes are temporary or
harmless. However, for blood in urine or for a color change lasting longer
than a day, seek health care. Hematuria may signal glomerulonephritis,
cancers of prostate or bladder.
5. Do you have difficulty controlling urine? Urge incontinence is when the
detrusor muscle of the bladder is overactive and cause involuntary urine
loss. Stress incontinence is when physical effort, sneezing or coughing
causes involuntary urine falls due to weakness in pelvic floor.
6. Any problem with the penis? These problem can be pain, lesion or discharge.
Urethral discharge is more frequent in urinary tract infection and sexually
transmitted infections.
7. Do you have any problem on the scrotum or testicles? Problems can be
lumps or swelling. A list of complains may be reported by the clients such as
spermatocele, hydrocele, varicocele and rarely testicular cancer.
8. Are you in relationship that involves sexual intercourse? This question is
relevant when assessing genitourinary system and should be gender neutral
to avoid embracing people with different sexual orientation. Ensure that thepatient accept individual’s sexual activity and believe that it is important.
Self-assessment 9.1
1. M.R. is a 19-year-old male student who 2 days noted acute onset of painful
urination, frequency, and urgency. Noted some thick penile discharge. He
is worried because of unprotected sexual intercourse he had last week
with one of his girlfriend.
a. Ask this patient 5 additional questions to ruler out complete subjective
information?
b. What medical condition will you think first to fit the patient’s complaints?
2. I.C. urinates 4 or 5 times/day, clear, straw-colored. No nocturia, dysuria,
or hesitancy. No pain, lesions, or discharge from penis. Does not do
testicular self-examination. No history of genitourinary disease. Sexually
active in a monogamous relationship. Sexual life satisfactory to self and
partner. Uses birth control via barrier method (partner uses diaphragm).
No known STI contact. Objective no lesions, inflammation, or discharge
from penis. Testes descended, symmetric, no masses. No inguinal hernia.
3. What is your conclusion as an associate nurse after getting the aboveinformation from your patient.
9.2. Physical assessment of genitourinary systemLearning activity 9.2
Observe the image above and respond to the following questions
a. What does this image A represent?
b. What is being done by gloved hangs on image B
c. In your own word, comment on abnormalities seen on image C, D, E, Fd. Enumerate the organs sees on image A and B.
The assessment of urinary system will start with inspection then percussion and
palpation of the abdomen. The abdomen must the soft, flat, concave and symmetric.
Observe the color of the costo-vertebral angle and hypogastric region where the
kidneys and urinary bladder are located respectively.
The examiner will make sure that the room is prepared with availability of necessary
materials such as gynecological table, sheets, pillow, gloves, and sample collection
items as needed. The temperature of the room should be warm and privacy is
mandatory to stop any movement in and out of the room during examination.
Clean your hands and don examination gloves. Women may feel apprehensive
about having their genitalia examined, especially if the nurse is male. If necessary,
arrange for a female assistant. Before bringing the woman to the examination room,
ask her to empty her bladder. She should be instructed to undress completely and
put on a gown. Most of the time, the woman will be in the lithotomy position and
asked to remove clothes. The lithotomy position may make her feel embarrassed
and vulnerable. If she seems uncomfortable or embarrassed, you may ask her if
she would like her head elevated so she can see you better. Position her with her
buttocks at the edge of the examination table. Ask her to place her arms at her sides
or across her chest but not over her head (this tightens the abdominal muscles).
Position the sheet completely over the patient’s lower abdomen and upper legs,
exposing only the vulva for your examination. Push the sheet down so you can see
the woman’s face as you proceed. As you start the examination, reassure her that
you will tell her everything that you are going to do before you actually do it. Help
the woman relax and assure her that, if she becomes too uncomfortable, you will
stop what you are doing and reassess what is happening. Please, every step here
must be objective and matter of facts; don’t be tentative with your touch; once you
make physical contact, maintain it for assessment purpose. Be sure to talk to the
woman throughout the examination to tell her what you are doing, what you are
seeing or feeling, and how long it will be until you are finished.
The assessment of GU in both male and female starts by external genitalia. Pubic
area is inspected for normal characteristic and distribution hair per age category.
The skin should be intact, inguinal regions with no erythema fissure or enlarged
lymph nodes. For female, each type of labia is symmetric and equal size to its
homologous. The clitoris allocated above urinary meatus measures about 1 to
1.5cm. The vaginal opening should not show swelling, redness or any protrusion.
Inspect the urethra through its meatus for patency and position. Inspect the
perineum, skin must be intact with no lesion or tears. Note that female who had
episiotomy manifests healed scars. The available findings will direct the examiner
to the advanced assessment cervix and vaginal wall by using the speculum.
Physical assessment of the penis need both inspection and palpation of the its
surface to look at and feel its consistence. It has a visible vein on the dorsal part
identified when inspecting the posterior part. Penis has no edema, discharge, pain,
lesions or nodules. For uncircumcised male the foreskin covers the gland, it is
easily retracted by the patient, some smegma are present. For circumcised male,
the gland is visible, lighter than the shaft and free of smegma.
The external urinary meatus is located centrally on the glands on the tip of the
penis. The external urethral meatus has no discharge, stenosis, or warts. The
glands can be opened by pressing it between thumb and forefinger. The patient can
be instructed to do this. Then request him to milk the penis from the base toward
the glands or head. Note color, consistency, or odor of any discharge. The glands
is smooth and pink with no discharge. Inspect and palpate the scrotum on both its
sides. It is divided into two sacs. The scrotum is hanged asymmetrically, with the
left side lower than the right. The anterior and posterior skin appears darker with
a rugous or wrinkled surface. Palpate each testicle separately. Note the smooth,
rubbery consistency of each testicle; no nodules should be felt. Irregularities in
texture or size may indicate an infection, tumor, or cyst. Palpate the epididymis on
the posterolateral surface of each testicle. It feels smooth and non tender.
In this unit, we are going to learn GU findings that need clinical attention. Starting on
the pubic area, there may be no hair, presence of patchy growth, skin inflammation,
lesions, dermatitis, or infestations. Candidiasis (infection due to candida albicans)
causes crusty, multiple, red, round erosions and pustules. Whereas, Tinea curis, a
fungal infection with large red, scaly, and extremely itchy patches. Bulges or masses
in inguinal areas for male suggest a hernia. Hernias occur when a loop of intestine
prolapses through the inguinal wall or canal or abdominal musculature. The patient
will report pain on exertion or lifting. On examination, pain increases when position
increases intra-abdominal pressure. Testicular irregularities in texture or size may
indicate an infection, tumor, or cyst. The foreskin or prepuce can develop either
phimosis or paraphimosis. Phimosis is when the foreskin can’t be retracted from
the tip of the penis. Paraphimosis is when the foreskin is retracted but can’t move
back up to the tip of the penis. Both phimosis and paraphimosis affect blood flow
in the penis and cause inflammation. Management of these conditions involves
non-steroid anti inflammatory to control pain and inflammation and allow chance
circumcision. Urinary meatus can be allocated upper or lower than the normal
location, these conditions are epispadias and hypospadias respectively. Contact
dermatitis is common in childhood and manifests red, itchy rash caused by direct
contact with a substance or an allergic reaction to it. The rash isn’t contagious or
life-threatening, but it can be very uncomfortable. Various substances can cause
such reactions, including soaps, cosmetics, fragrances, jewelry and plants. The
management of contact dermatitis involves identification and avoidance of thecause, apply skin soothing product or anti histaminic medications.
Self-assessment 9.2
1. Mr. N.S. is entering consultation room in a bent over position, anxious
and guarding genital area. Physical examination revealed redness that
urethral meatus has mild edema with purulent urethral discharge. No pain
on palpation of genitalia. Testes symmetric with no masses.
a. What will you record from the above physical assessment?
b. What will be your nursing intervention to this patient?
2. D.C. 27-year-old married woman with Parity 1. Presents at clinic with
urinary burning, vaginal itching, and whitish curdy discharge since 4
days ago. After physical examination, vaginal sample showed spores of
Candida Albicans.
a. Which medical condition would you pose for this woman?
3. B.L., 17-year-old female high school student, comes to clinic for oral
contraceptives. She had menarche at 12 years, cycle every 30 days,
duration 4 days, mild cramps relieved by Ibuprofen. LMP 7 days ago.
No dysuria, vaginal discharge, vaginal itching. Relationship involving
vaginal intercourse with one boyfriend for since 6 months. She thinks
that her boyfriend is involved in other heterosexual contacts. For birth
control boyfriend uses condoms sometimes. Wants to start birth control
pills. Never had pelvic examination. Never had teaching about breast
self-examination or STIs except AIDS. Smokes cigarettes, PPD; started
age 11 years. Has not had HPV vaccines.
a. Depending on the information and suggestions of this girl, what is the best
family planning method would you advise her?
b. After physical assessment, what is your clinical decision or diagnosis?c. Which interventions do you think to be important in this case?
9.3.Interpretation of specific findings on Urogenital
system.
Learning activity 9.3
1. After history taking and physical examination, the nurse decides to take
urine sample. The patient reported dysuria and genital itching. The urine
looks bloody and has a very bad odor.
a. Is it normal to have blood in the urine?b. What does dysuria means?
Following the history taking and physical examination of GU, we are going to attach
the meaning on some special findings. Urinary frequency (increased number
of urination) can originate from urinary tract infection, bladder calculi and urethra
stricture. In older male, urinary frequency is the sign of benign prostatic hyperplasia
or prostate cancer which compress the bladder. Urgency known as strong need
to urinate is an indicator to urinary tract infection, chronic prostatitis, urethritis,
obstruction of lower urinary tract leading to residual urine and overflow, anxiety, use
of diuretics, benign prostatic hyperplasia, urethral stricture, and diabetic neuropathy.
Hesitancy is the delayed or difficult starting urination. The main causes are benign
prostatic hyperplasia, compression of urethra, outlet obstruction, and neurogenic
bladder. Enuresis is the involuntary urination when someone is sleeping sleep.
Enuresis is said when bladder control can’t achieved by 5 years of age due to
delayed functional maturation of the central nervous system. Other causes of
enuresis are obstructive disease of lower urinary tract, genetic factors, failure to
concentrate urine, urinary tract infection and psychological stress.
Nocturia or excessive urination during the night indicates renal or lower urinary
tract. It can also indicate metabolic disorders as well as side effects of diuretic
medications. Urinary incontinence as the inability to voluntarily control urine
is linked to stress incontinence, tumor, bladder cancer, calculi and neurological
conditions such as spinal cord injury and Guillain-Barré syndrome. Normal urine
output in a healthy individual must be between 0.5-1.5 mL/kg/hour, and patients
should generally be urinating at least every 6 hours. On the other side oliguria is
defined as the production of inadequate volumes of urine (<500 ml/day in adults,
<0.5 mL/kg/hour in children, and <1.0 mL/kg/hour in infants. Oliguria is caused by
acute or chronic kidney failure and inadequate fluid intake. Polyuria is the increased
volume of urine. The main causes of are diabetes mellitus, diabetes insipidus, use
of diuretics, excess fluid intake. Anuria is the absence of urine or urine output of
less than 100ml per 24 hours. Anuria is due to acute or chronic kidney failure and
complete obstruction. Hematuria is the presence of red blood cells in the urine. The
causes of hematuria are cancer of genitourinary tract, acute glomerulonephritis,
renal stones, renal tuberculosis, trauma and extreme exercise. Proteinuria is the
presence proteins in the urine. Proteinuria may the sign of acute and chronic renal
disease, nephrotic syndrome, vigorous exercise, severe heart failure and diabetic
nephropathy. Kidney enlargement is palpable in the costo-vertebral angle in case
of cyst, hydronephrosis or tumor.
Syphilitic chancre is an initial sign of the infestation of Treponema Pallidum. The
chancre appears in red, painless, eroding lesion with raised boarder. It is located
inside the vagina in female or to the other parts of external genitalia in both sexes.
Vaginitis is the inflammation of the vagina resulting from overgrowth infectious microorganisms.
Vaginitis is categorized under bacterial vaginosis, Candida albicans
infection, trichomoniasis, and mucopurulent cervicitis depending on infecting agent.
Bacterial vaginosis is identified as thin grayish white discharge. Vaginal candidiasis
appears as thick, white, curdlike discharge and appears in patches on the cervix
and vaginal walls. Another form is mucopurulent cervitis originating from gonorrhea
or Chlamydia. They both produce purulent yellow discharge from the cervix.
Trichomoniasis may generate a malodorous yellow or green, foamy or watery, foulsmelling
discharge. It can also create red papules on the cervix and vaginal walls,
giving the tissue a strawberry appearance.
Genital warts, a sexually transmitted disease caused by human papilloma virus.
They produce painless warts on the penis, vulva, vagina, cervix, or anus. Warts
start as tiny red or pink swellings that grow. They become multiple swellings with a
cauliflower appearance.
Genital herpes is due to herpes simplex virus type 2. It produces multiple,
superficial vesicles, lesions, or crusts inside the vagina, on the external genitalia in
both sexes, on the buttocks and, sometimes, on the thighs. Symptoms of genital
warts are dysuria, regional lymph node inflammation, pain, edema, and sometimes
with fever.
Vaginal prolapse occurs when the anterior vaginal wall and bladder prolapse into
the vagina. The uterus may prolapse into the vagina and can even be seen outside
the body.
The testicular tumor is identified as painless lump in the testicles which causes
weight in the scrotum. Prostate gland enlargement is identified using digital rectal
examination. It can be categorized as benign prostatic hyperplasia (BPH) or acute
prostatitis. The BPH usually starts after age 50 with signs and symptoms of nocturia,
urinary hesitancy, frequency and recurring urinary tract infections. In the acute
prostatitis, the prostate gland is firm, warm, and extremely tender and swollen withfever as the condition originate from infection.
Self-assessment 9.3
1. How can you differentiate vulvovaginal candidiasis to contact dermatitis
by using inspection?
2. What is the causative agent of genital warts?
3. State the characteristics of paraphimosis
4. Differentiate inguinal hernia to testicular torsion
9.4. Identification of client problemsLearning activity 9.4
a. Mention possible patient problems being identified by the nurse after the
assessment of the patient’s abdomen.
b. Which anatomical organs of the internal female reproductive herementioned?
The problems of genitourinary system can be allocated under structural, functional,
infectious and tumor based origin. One of the common infection of GU is candidiasis
identified as vulvovaginal edema, erythema, and excoriation; thick white secretions.
The microscopy will show pseudohyphae, occasional budding yeast. Bacterial
vaginosis is another infection with whitish to grayish creamy secretions that coat
the vaginal walls with a strong fishy odor and vaginal itching or burning.
Laboratory investigation will show clue cells on microscopy and possibly WBCs are
present. Gonnorhea, one of the STIs, clinically present yellow purulent discharge
from the cervix; tenderness or pain with the pelvic examination. Diagnostic test
using Gram stain shows intracellular diplococcic.
Syphilis, an infection resulting from Treponema Pallidum inoculation which
penetrates intact skin or mucous membrane during sexual contact. In its early
stage it demonstrates a chancre: a painless ulceration at the point of entry which
can be on the penis or vulva.
Pediculosis pubis presents with mild to severe itching, especially in the mons pubis
and perineum. The external genitalia are excoriated. Tiny spots of blood and lice
may be seen on the underwear. Eggs normally adhere to the pubic hair and can
appear as small dark spot. The risk factors for pediculosis pubic are direct contact
with the infected person especially during sexual contact, sharing personal items
such as bed linen and living in institutionalized condition.
Uterine prolapsed is when the uterus fall into the vagina due to gradual weakening
of uterine ligaments. It may be a consequence of multiple vaginal births or an
enlarging uterus. The patient presents with low pressure, fecal impaction, and
vaginal and uterine irritation.
Ectopic Pregnancy happens when a fertilized ovum implants outside uterine
endometrium mostly in the fallopian tubes and cervix. Risk factors include previous
ectopic pregnancy, past pelvic infection, endometriosis, or tube abnormalities. The
patient presents with symptoms of a normal pregnancy initially. As the ectopic
pregnancy grows larger, there is internal hemorrhage and subsequent lower
quadrant pain.
Testicular torsion is another male related condition manifested as a sudden twisting
of the spermatic cord, usually on the left side, is rare after 20 years. It results
from poor attachment of the testis on the scrotal wall. Signs and symptoms involve
impaired blood supply which leads to ischemia and venous engorgement. Because
the testis can become gangrenous within a few hours, this is a surgical emergency.
Hydrocele is the collection of serous fluid develops in the tunica vaginalis
surrounding the testis. The patient presents with unilateral and intermittent edemaof the scrotum but no pain.
Self-assessment 9.4
1. Why is testicular torsion considered as a surgical emergency?
2. A patient is presenting lice like insects in his pubic area and perineum.
They cause itching at a level of skin laceration.
a. What is the medical diagnosis for this patient?b. What are the preventive measures for this condition?
9.5.Nursing intervention based on patient’s problem.Learning activity 9.5
a. Describe the above images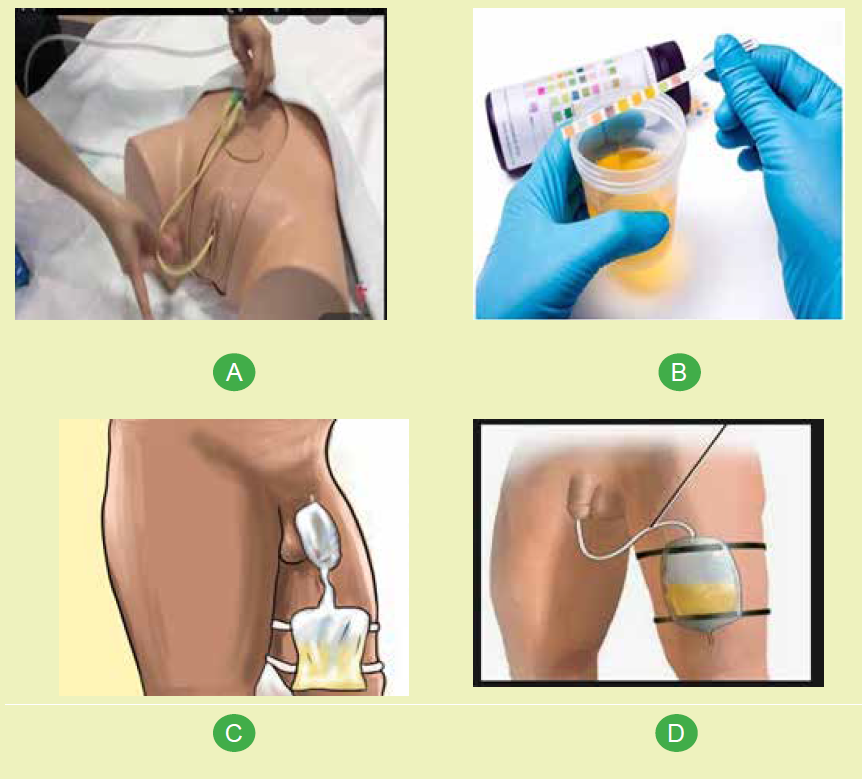
b. What are the indications of urinary catheterization?
Nurse’s activities in relations to genitourinary system are individualized and depend
on patient’s problem. After the assessment, a nurse will make priority actions which
can extend from education, advocacy or provision of nursing intervention. The
education can be safe sex practices to prevent STIs and adequate water intake to
keep urinary track flushed to prevent UTIs and renal stones. Female are advised
to clean anus after defecation from front to back to avoid contamination of feces in
the genitals which can originate from unnecessary contamination which results in
infections.
Depending on data collected from the patient, some may be alarming and require
immediate interventions such as paraphimosis and testicular torsion. The nurse
will immediately inform the physician for advanced assessment and preparation for
emergency surgery. Other nursing intervention can be urine or secretion specimen
collection, measuring urine output, provide bedpan, urinary catheter insertion and
removal as needed. The nurse also will administer prescribed orders to treat GUconditions.
Self-assessment 9.5
1. Which health education topics will you initiate after consulting a 18 year
boy used to have unprotected sex with girls of his age?
2. List the intervention a nurse can provide to manage the GU problems.3. Why is it important to drink enough water on the GU health status?
End unit 9 assessment
1. List 5 nursing interventions specific to the GU
2. Write and describe abnormalities in urination
3. List 10 clinical conditions common on GU system.4. Match the following terms to their description

