Topic outline
UNIT 1 SIMPLE WOUND CARE
Key Unit competence
Perform the techniques of simple wound dressing
Introductory activity 1.0Observe the picture provided and respond to the questions below
1. What do the following picture have in common?
2. What did you notice in the picture A, B, C, and D?
3. If you were an associate nurse, what could you do to care for patient in
picture D
The picture shown above represent a wound, process of wound healing and
related wound care. The wound is the breaking of the skin, underlying tissues
or an organ (break of skin integrity). A wound occurs when the integrity of any
tissue is compromised (e.g. skin breaks, muscle tears, burns, or bone fractures.
A wound may be caused by an act, such as a gunshot, fall, or surgical procedure.
1.1 PRINCIPLES OF SIMPLE WOUND CARE
1. What do you think should guide a comprehensive wound care?
2. According to what you have experienced, seen or heard regarding
wounds, relate causes and types of wounds
Learning activity 1.1
1.1.1.Types of wounds
There are several ways of classifying types of wounds, such as the source of the
wound, the state of skin integrity, the likelihood and degree of contamination and
how much time the wound have been existing.
a) Types of wound per etiology
Wounds are either intentional or unintentional.
• Intentional wound occurs as a result of therapeutic reasons. Examples are
surgical incisions or venipuncture. This wound is created under the sterile
conditions.
• Unintentional wound occurs as a result of unplanned event such as a
wound caused by an accident. Examples include traumatic wounds, fall, a
gunshot wound, and violence, unusual wound (snake or insect bite) or the
result of an allergic reaction.
Furthermore, unintentional wound may result from an illness such as vascular an
or neuropathic impairment. Thus, the wound may result from either ischemia or
blood stasis. Ischemia comes from reduced blood supply caused by the tightening
or blockage of blood vessels, and this leads to poor circulation.
Wounds caused by being immobile, such as bed sores or pressure injuries this is
caused by immobilization (or difficulty moving) for long periods.
The wound can be caused by friction when a body part rubs or scrapes across arough or hard surface
b) Types of wound per skin integrity
Wounds are mainly open or closed.
A closed wound is an injury that does not break the surface of the skin butcauses damage to the underlying tissues.
Open wounds break the surface of the skin and may also damage underlying
tissues.
Some examples of open wounds include
Abrasions: These form as a result of rubbing or scraping the skin against a hardsurface.
Lacerations: These are deeper cuts caused by sharp objects, such as a knife, or
sharp edges.
Punctures: These are small deep holes caused by a long, pointed object, such
as a nail.
Burns: These result from contact with an open flame, a strong heat source,
severe cold, certain chemicals, or electricity.
Avulsions: This refers to the partial or complete tearing away of skin and
tissues.
c) Types of wound per likelihood and degree of contamination
Considering the likelihood and degree of contamination, there are four types of
wounds:
• Clean wounds - are uninfected wounds in which no or minimal inflammation
is encountered and the respiratory, alimentary, genital and urinary tracts are
not entered. Clean wounds are primarily closed and surgical wounds.
• Clean contaminated wounds - are surgical wounds in which the respiratory,
alimentary, genital or urinary tract has been entered. Such wounds show no
evidence of infection.
• Contaminated wounds - include open, fresh, accidental wounds and
surgical wounds involving a major break in sterile technique or a large
amount of spillage from the gastrointestinal tract. Contaminated wounds
show evidence of inflammation.
• Dirty or infected wounds - include wounds containing dead tissue and
wounds with evidence of a clinical infection, such as purulent drainage.
d) Types of wound per wound age
Considering how long the wound has been existing, the wound is either acute or
chronic:
• Acute wounds are relatively new and occur suddenly in nature as result of
surgery or trauma. Their healing move through the stages of healing within
the predicted time-frame.
• Chronic wounds may develop over time as results of underling chronic
condition such as diabetes, ischemic disease, pressure damage resulting
from prolonged immobilization, and inflammatory diseases and or as a resultof failed healing of an acute wound leading to a lengthened recovery.
1.1.2. Principle of simple wound care
Wound healing is a complex and dynamic physiological process that is affected by
various factors. Healthcare providers must understand how to assess these and be
able to address them accordingly to optimize the wound healing process. Though
wound care is often focused primarily on topical treatment, a comprehensive plan
of care should address three areas concerning wound healing affecting factors.
Therefore, general principles for holistic wound care are (1) correction of etiologic
factors, (2) provision of systematic support for wound healing and (3) topical
treatment that create and maintain an optimal healing environment.
Correctly identifying the cause of the wound is key to developing a comprehensive
management plan. Failure to addressing the causative factor(s) will result in failure
to heal, even if systematic support is provided and topical therapy is appropriate.
Thus, initial assessment and intervention must include identification of the etiologic
factors and initiation of measures to address these. For example, the most the most
critical intervention in the management plan of a pressure ulcer is to eliminate or
minimize the pressure that caused the wound.
Systematic support for wound healing is important as wound healing requires
increased calorie, protein, and vitamin and mineral intake; sufficient blood flow
and oxygen to support repair process; and relatively normal glycemic levels. Thus
assessment and correction of systematic conditions that adversely affect repair is
the second priority in wound healing.
The goal of topical therapy in wound care is to create a local environment that
supports healing, through appropriate cleansing and dressing selected based on
individual wound assessment and it should be matched evidence-based guidelines.
For instance, if a wound’s assessment reveals that it is in proliferative phase,
cleansing it should aim at removing exudate without damaging the proliferative
cells and newly formed tissues. Moreover, providing topical wound therapy should
ensure comfort and dignity of the patient.Self-assessment 1.1
1. Your sister accidentally cut her finger while slicing tomatoes. This injury is
a(1) ___________________ (2) _______________ (3) _____________
(4) ____________________wound
2. After finishing a wound dressing, the associated nurse undertook a five
minutes’ patient education activity regarding a balanced diet and smoking
cessation.
a. Which principle of wound care was she addressing?
b. What other wound care principles should be implemented for acomprehensive and holistic wound care?
1.2. PHASE OF WOUND HEALINGAnalyze carefully the following images and respond to the questions below
a. What do you understand with the term wound healing?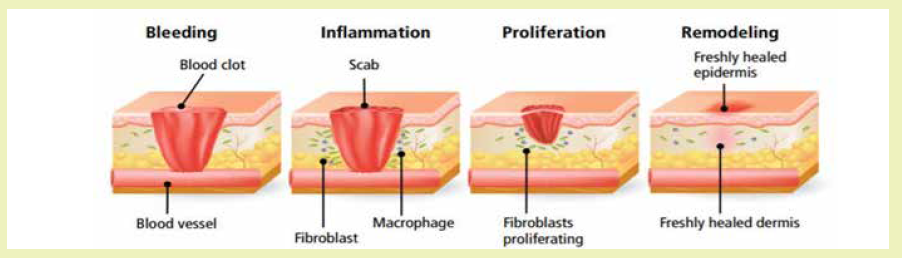
b. According to the image above showing biological changes in body tissues
during wound healing process, describe what happen in each picture
c. Imagine what would happen if one phase of wound healing did not occur?
Wound healing is the complex process in which the skin goes through as it repairs
damage from wounds. Destroyed or damaged tissue is replaced by new produced
tissue in stepwise fashion and involves the stage of hemostasis, inflammation,
proliferation, and maturation.a) Phase 1 - Hemostasis
This phase has the aim of stopping any bleeding where the body activates its blood
clotting system. When the blood clots at the opening of a wound, it prevents the
patient from losing too much blood and therefore it become the first step of the wound
closing up. Briefly when tissue is damaged, serotonin, histamine, prostaglandins,
and blood from the injured vessels fill the area. Blood platelets form a clot, and fibrin
in the clot binds the wound edges together. This step can last up 2 days depending
on the part of the skin which is affected.
b) Phase 2 - Inflammation
When phase one is complete and the body is no longer bleeding, the body activatesits key defense mechanism inflammation.
This phase works to kill bacteria and remove debris with white and other blood
cells. Inflammation ensures that the wound is clean and ready for new tissue to
start growing. This phase is the most painful. Lymphocytes initiate the inflammatory
response and this causes increasing capillary permeability. White blood cells from
surrounding vessels move in and ingest bacteria and cellular debris, demolishing
the clot and healing the wound. Redness, warmth, swelling, pain, and loss of
function may occur. Platelets heavily secrete growth factors during this phase. This
phase takes up to six days and should go away.
c) Phase 3 - Proliferation or repair
When the wound is clean, the body will begin the proliferation phase of woundhealing. This stage involves closing of the wound.
This phase can have 3 semi phase which are: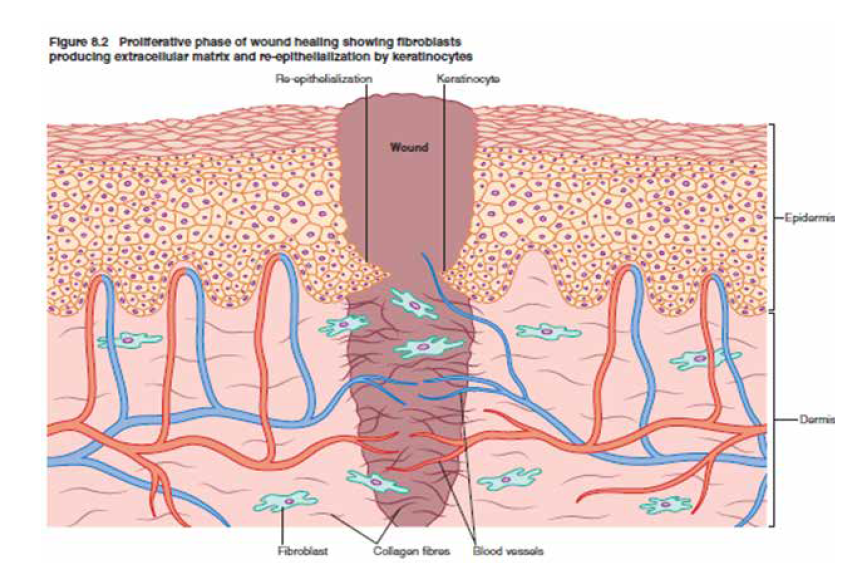
Filling the wound: with new connective tissue and blood vessels.
Contracting the edges of the wound: this will feel like the wound is tightening
towards the center.
Covering the wound: epithelial cells (cells that create a protective barrier between
the inside and outside of your body) flood in and multiply to close your wound
completely.
This phase can last four days to almost a month, depending on the surface area of
your wound.
d) Phase 4 - Maturation or remodeling
During this phase, the new tissue that body built in phase three, needs to strengthenand build flexibility.
This stage can take the longest, sometimes taking over a year to fully repair. But,
once fully recovered, the skin should be pretty close to as strong as it was before
it was wounded.
The healing process is one of the body’s most surprising functions, but it can be
delayed by aggravators like infection and poor wound care. It is good to learn how
to properly dress a wound so health care provide can maximize the body’s ability.
Self-assessment 1.2
Match phases of wound healing in column A with their respective definitions incolumn B
1.3.FACTORS AFFECTING WOUND HEALING
Learning activity 1.3Observe the following images and answer to questions below
1) After observing the above images ABCD, list different factors affecting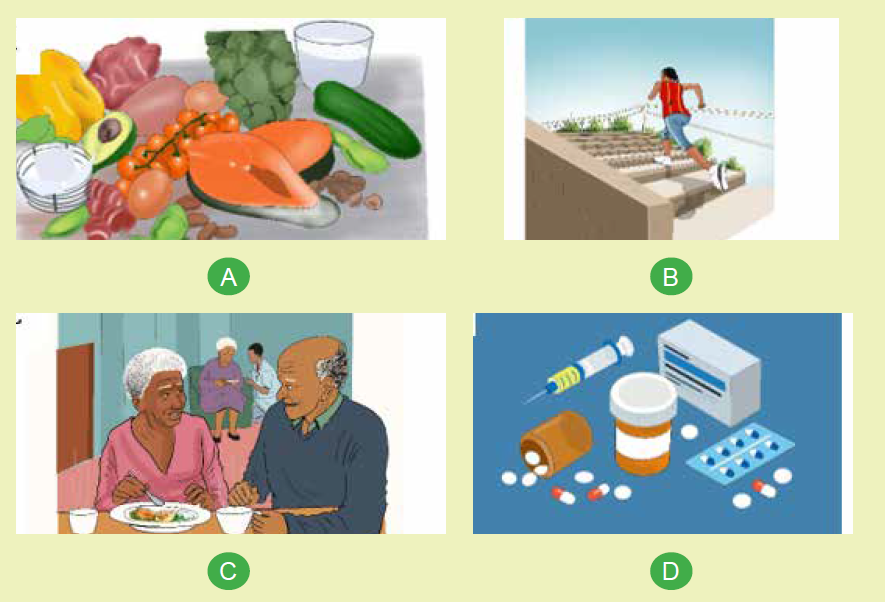
wound healing.
2) In group discussion, explain the factors affecting wound healing separately.
There are many reasons why wounds do not heal in a straightforward manner;
these reasons can be classified as intrinsic (something internal to the individual) or
extrinsic (something external to the individual).
a) Intrinsic factors of wound healing
• Age: as we age cell regeneration rates slowdown, which means that wounds
usually take longer to heal the older we get. A wound that might take 3 weeks
to heal in a youth may take 6 weeks to heal in the older individual. It is therefore
important to set realistic goals when planning care.
• Gender: the fluctuating hormone levels in females during their lifetime appear
to affect skin integrity and therefore healing rates, though in a mild way.
• Psychological: it is thought that the psychological state can impact on wound
healing, such as high levels of emotional stress, worry and negative thought
processes. Evidence of this can be seen where a person develops mouth
ulcer or cold sores when they are experiencing such emotional pressures.
• Physical/structure: the human form itself can be a factor in wound healing
rates, and one example of this is where pressure ulcers exist; the underlying
bone that caused the ulcer in the first instance will continue to delay wound
healing if pressure relief is not ensured. Other physical factors that must be
considered are for example scar tissue, physical deformities, particularly of
limbs, amputations, mobility and reduced mobility.
• Lifestyle: smoking, alcohol and drug use, although an extrinsic factor, can
impact intrinsically on the individual, which could delay healing rates.
• Nutrition: this can be both an intrinsic factor (e.g. due to malabsorption
conditions or gastric surgery) and an extrinsic factor (due to dietary choices) all
of which can result in poor nutritional intake. As wounds require an increased
nutritional intake, any reduction will impact on healing rates.
• Medications, common medications that impact on wound healing processes
and rates are steroids, anti-inflammatory and cytotoxic drugs.
• Comorbidities common medical conditions that affect wound healing rates
are:
i. Diabetes, peripheral artery disease and other conditions that affect
the blood circulation such as heart disease and hypertension means a
reduced blood supply reaches the wound bed.
ii. An inefficient cardiopulmonary circulation due to heart or lung disease
means that the wound will receive a reduced supply of essential oxygen
and nutrients that will reduce healing rates.
iii. Inflammatory diseases, such as rheumatoid arthritis and ulcerative colitis;
these conditions affect the inflammatory phase of a wound healing if
the condition is in ‘flare-up’, which can cause a prolonged inflammatory
phase; alternatively, if the condition is in remission the patient is usually
taking prescribed steroids, which also delay the healing process by
delaying or stopping the inflammatory phase. Patients on steroids who
are due to have surgery are often required to stop steroids for a short
time before and after surgery.
iv. Cancer.
v. Major or multi-organ failure.
b) Extrinsic factors
• Environment – this may include the surface the patient is lying or sitting on;
the environment they live in; the support networks available to the patient;
social and financial factors. It can also refer to the environment the wound is
kept in (see below).
• Clothing and footwear – these can impact on healing rates by causing
• pressure or restriction of blood supply, which means that there is a reduce
supply of essential oxygen and nutrients supplied to the wound.
• Wound site – wounds sited over joints (e.g. elbows, knees) will usually take
slightly longer to heal than wounds over non-mobile areas.
• Temperature – of particular importance is the temperature of the wound bed;
ideally a wound ought to be retained at body temperature (i.e. 36.9°C). If the
wound is not dressed with an appropriate (insulating) dressing the wound bed
will cool according to the atmosphere and will result in a reduced blood supply.
The temperature of an individual is also important; if a person is allowed to
cool the peripheral circulation will be reduced in order to preserve the core
temperature. This in turn reduces the amount of blood (and therefore oxygen
and nutrients) reaching the wound bed.
• Nutrition – it is vital that the patient with a wound takes in additional calories
in order to increase healing rates, particularly with regards to increased
proteins.
• Wound care skill/technique: one of the most common reasons for delayed
wound healing is the wound care technique of health professionals. This may
include the use of inappropriate dressings, causing trauma on removal of the
dressing (causing the wound to revert back to the beginning of the healing
process); leaving a dressing in situ for too long, causing saturation and
subsequent maceration/excoriation of the wound and peri-wound tissues.
• Infection: Both bacteria and endotoxins can lead to the prolonged elevation
of pro-inflammatory cytokins such as interleukin-1 and TNF-α and elongate
the inflammatory phaseSelf-assessment 1.3
Discuss the ways that intrinsic factors (age, lifestyle and medications) and
extrinsic factors (nutrition, wound site and wound care skill) affect the woundhealing process.
1.4.OVERVIEW ON SIMPLE WOUND CARE
Learning activity 1.4
Patient H. is coming to the health facility where you work as an associate nurse.
He is having the bleeding simple wound on elbow after road traffic accident. The
senior nurse decided that the wound dressing will be performed.
1) Why wound dressing will be done?2) Which type of wound dressing will be performed?
The wounds are different and therefore their dressing differ also. There is:
• Aseptic dry wound dressing - is the most common type of dressing for
simple wound, it is done using dry gauzes without products and held in place
using a tap or a bandage if a non-adhesive dressing material is used. The
wound is previously cleaned with sterile gauzes soaked in an appropriate
fluid like normal saline 0.9%.
• Sterile wet wound dressing - Gauze or other dressing materials is be
moistened with saline to keep the surface of open wounds moist. A moist
wound surface enhances the cellular migration necessary for tissue repair
and healing.
Purpose of wound dressing
• To keep the wound clean
• To prevent the wound from injury and contamination
• To keep in position, the drugs applied locally
• To keep the edges of the wound together
• To apply pressure
Self-assessment 1.4
Mr. J. underwent hernia repair and was discharged home the following day. He
presents to you with a discharge summary at a health center.
1) What is the type of wound dressing is indicated for Mr. J.?
2) Differentiate aseptic dry dressing from sterile wet wound dressing3) What is the purpose of wound dressing for Mr. J?
1.5 ASEPTIC DRY WOUND DRESSING TECHNIQUES
Learning activity 1.5
1) According to your understanding, what do you think the health care
provider should do in order to keep the aseptic wound dry?
2) What do you think should be attention of nurse to make aseptic wound
dressing procedure?
3) Perform dry aseptic wound dressing technique to a mannequin aswatched on video
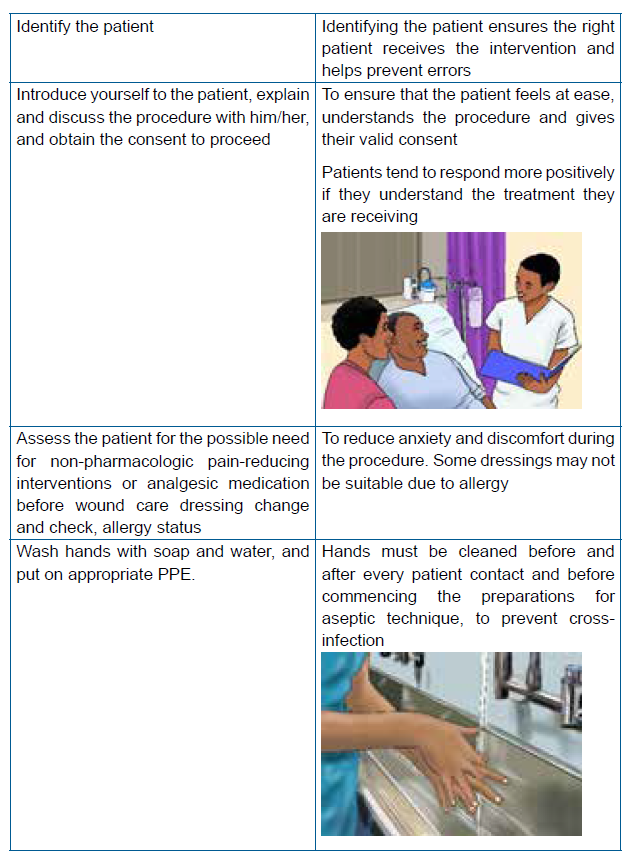
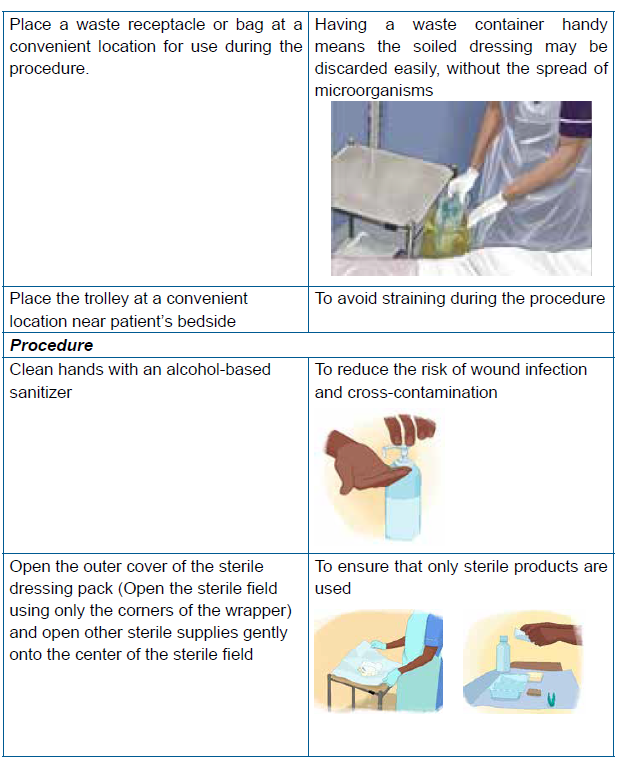
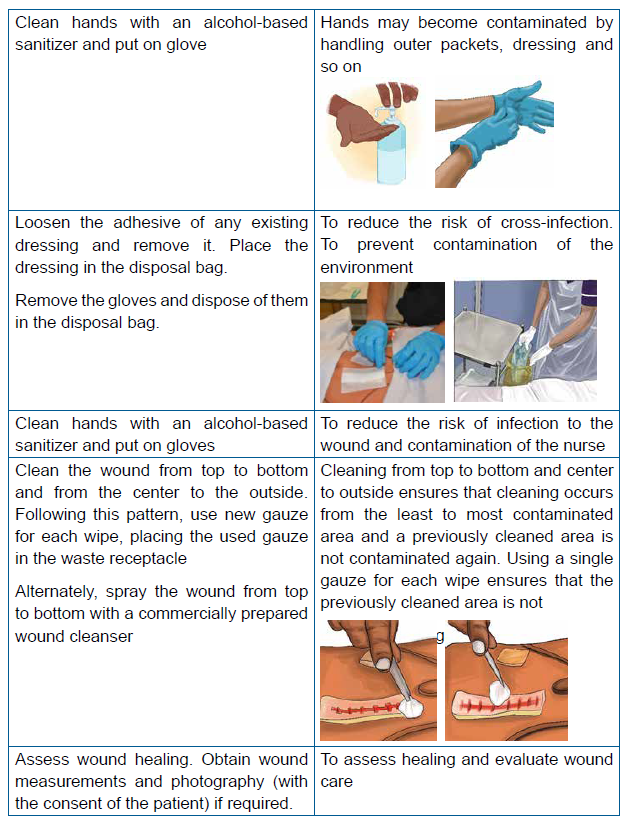
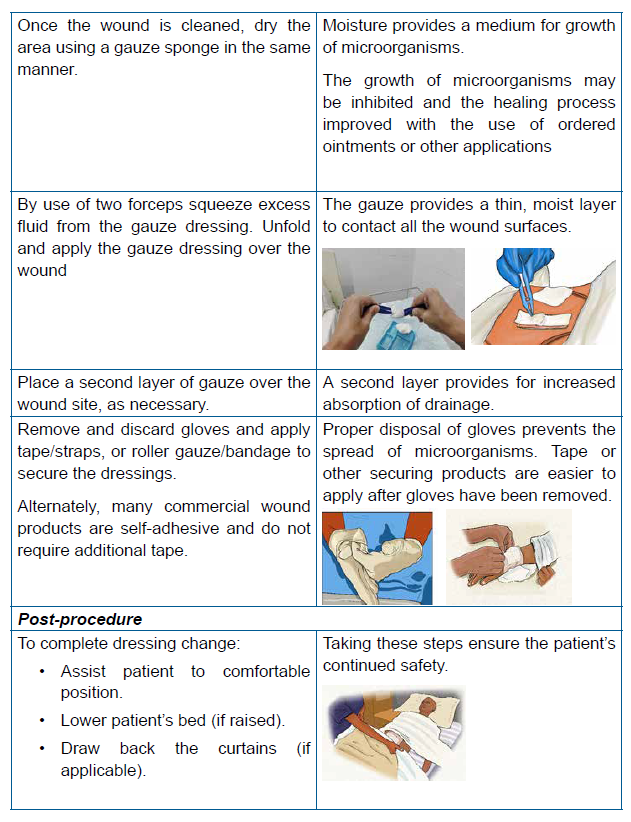
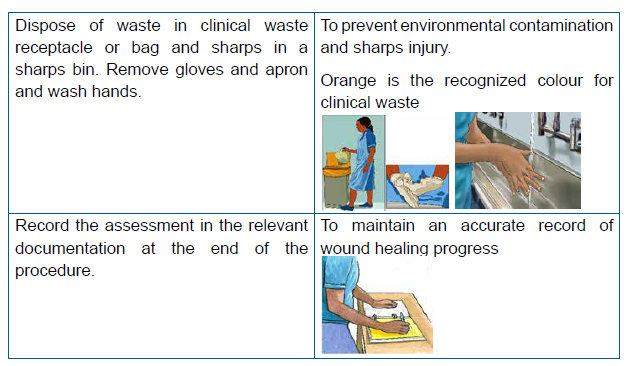
Steps of dry wound dressing technique


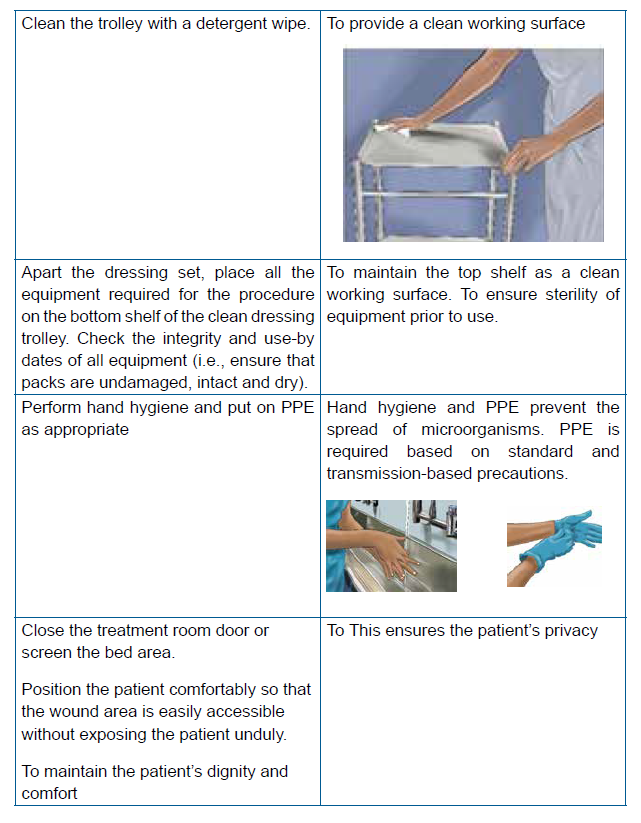


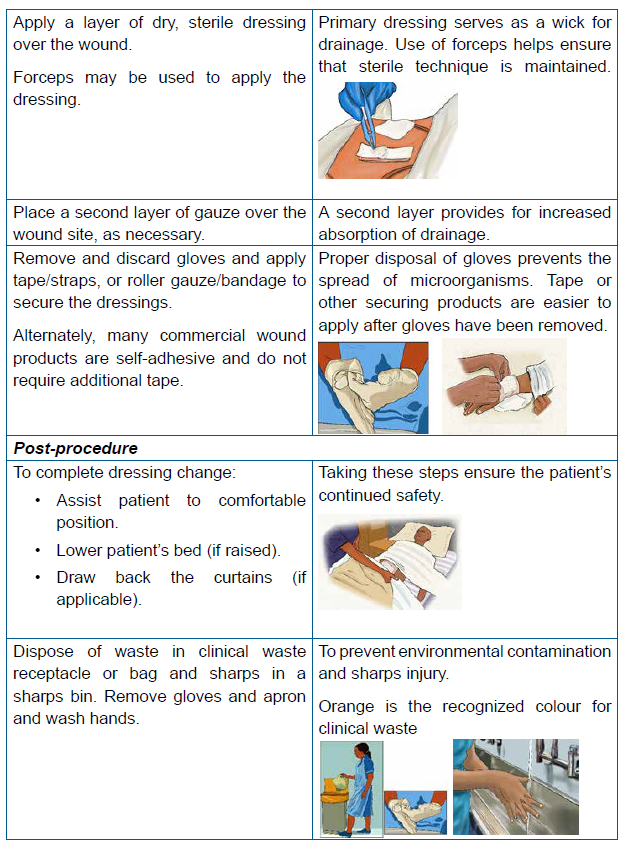

Self-assessment 1.5
Use the simulation lab and perform aseptic dry wound dressing technique on themannequin respecting the steps of aseptic dry wound dressing.
1.6.WET DRESSING TECHNIQUE
Learning activity 1.6
After having an overview on techniques of wound dressing
1) Which techniques do you find as mostly indicated for the illustrated wound
image?
2) Explain the rationale of choosing that wound dressing technique?3) Perform the indicated wound dressing technique
A saline-moistened dressing promotes moist wound healing and protects the wound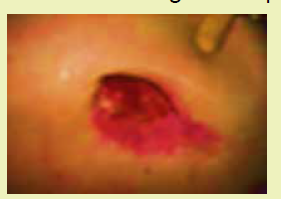
from contamination and trauma. A moist wound surface enhances the cellular
migration necessary for tissue repair and healing. It is important that the dressing
material be moist, not wet, when placed in open wounds. Dressing materials are
soaked in normal saline solution and squeezed to remove excess saline so that the
dressing is only slightly moist.Steps of wet wound dressing


Self Assessment 1.6
Mr. P. A 29 years old male is a patient who comes regularly at the health center
for wound dressing of his right heel which he got from a road traffic accident from
his motorcycle. Today is his day-10 to be dressed, and in his small book from
the health center (carnet), it is indicated that Mr. P.’s wound is mildly infected. On
your observation after removing the old dressing, you find that there are some
yellowish discharges coming from the wound in small amount
1) Identify the type of dressing technique indicated2) Perform the indicated wound dressing technique
End unit assessment 1
1. Why good hand hygiene is important in wound care?
a) Clean hands smell nicer for the patient.
b) Prevent the spread of infection
c) Dressings don’t work if there is any dirt on a wound.
d) Nurses don’t like dirty hands
2. Which of the following is the correct sequential order of the phases of
wound healing?
a) Inflammation, remodeling, hemostasis, and repair
b) Inflammation, hemostasis, proliferation, and maturation
c) Hemostasis, inflammation, repair, and remodeling
d) Inflammation, maturation, proliferation, and hemostasis
3. Why is it important to include the patient in your selection of wound
dressing?
a) Because the ward manager has told you to talk to patients
b) Because the league of friends won’t supply any more extras for the
ward if you don’t talk to patients
c) Because patients will respond to treatment in a more positive manner
if they understand what you are doing and the likely outcomes.
d) Because talking to your patient helps the time to pass more quickly
when you’re doing the dressing explain and discuss the procedure
with the patient
True or false questions
1) Normal saline solution is the only completely safe cleansing agent and is
the treatment of choice for use of wounds
2) Use the same swab to cleanse a circular wound more than once
3) As long as the aseptic wound dressing is done properly, documentation is
unnecessary after performing it
Short answer questions
1) Mention the principles of performing wound dressing
2) Explain how comorbidities as intrinsic factors affect wound healing
process
Case Scenario
Mr. T with 30 years old comes to the health facility where you work, he has
bleeding wound on left tibia after road traffic accident. Your senior prescribe for
him daily Wound dressing with Normal saline. As a student future associate
nurse assigned to take care of Mr.
1) List at list 3 purpose of wound dressing
2) Outline at least 5 precautions that you are going to implement for
preventing infections to Mr. T during performing wound dressing
3) During the procedure, explain to him the role of diet as well as the example
of most preferred nutrient in promoting wound healing4) Which phase of wound healing for Mr. T,s wound
UNIT 2 BANDAGING TECHNIQUES
Key unit competence
Apply correctly the techniques of bandaging
Introductory activity 2Observe the picture provided and respond to the questions below
1. What does the above image A show to you?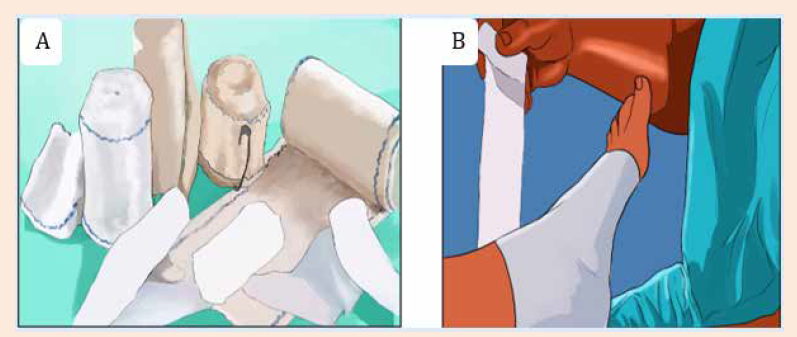
2. Which technique is being performed on image B?
3. What do you think the technique performed will help the casualty
2.1.INTRODUCTION TO BANDAGING TECHNIQUES
A bandage applied properly can aid in the recovery of a patient while a carelessly or
improperly applied bandage can cause discomfort to the patient, expose the wound
to danger of infection and even imperil the life of the patient.
Bandaging is a process of covering a wound or an injured body parts.
A bandage is a strip of cloth used to wrap some part of the body. Applying the right
type of bandage for a particular injury is necessary. Moreover, a bandage protects
the injury from any kind of germs that might slow down the healing process.
Learning activity 2.1Observe the illustrated images and answer the following questions
1) What do the images give you an idea about?
2) What was the purpose of the procedure done?
3) Describe the differences in the images illustrated above
4) Suggest the types of bandages used5) Comment on the way different body parts bandaged are tightened
2.1.1. Purpose of Bandaging
Bandaging can be done purposefully to immobilize an injured part and relieve pain,
to protect a wound and secure dressing, to control bleeding from wounds, and to
reduce or prevent swelling.
2.1.2. Rules of applying bandages
The rules of applying bandaging are but not limited to; selecting a bandage of
appropriate size and suitable material, putting the patient in a comfortable position,
support the injured area while bandaging, if a joint is involved; flex it slightly, face
the patient while applying the bandage, except when applying it on the head, hold
the roll of the bandage in the dominant hand when applying the bandage and check
the circulation in the area distal to the bandage, If necessary, unroll the bandageuntil the blood supply returns, and reapply it more loosely.
2.1.3.Types of bandages
The types of bandages include the following:
A. Triangular bandage
Triangular bandage consists of a wide
triangular piece of cloth usually made
from meter square tissue that is cut in half
diagonally. The bandage can be used in
various ways as sling to support an injured
limb, to secure splint or for immobilization
of broken bones and soft tissue injuries.
It is valuable in emergency bandaging
since it is quickly, easily applied and stays
on well They are used also for applyingpressure to a wound to control bleeding.
When opened up, they make slings to support, elevate or immobilize upper limbs.
For example, this may be necessary with a broken bone or strain or to protect a
limb after an operation.
Folded narrowly, a triangular bandage becomes a cold compress that can help
reduce swelling.
B. Roller bandage
A roller bandage is a long strip of gauze or
cotton material prepared on a roll. Roller
bandages can be used to immobilize
injured body parts, provide pressure
to control internal or external bleeding,
absorb drainage, and secure dressings.
Basically, there are two types of roller
bandages; an elastic roller bandage
which is used to apply support a strain
or sprain and is wrapped around the joint
or limb many times, another type of roller
bandage is linen roller bandages which
are used to cover gauze dressings.
They come in many different widths and are held in place with tape or pins; they
can also be used for wound compression as they are typically sterile.Bandages should be applied firmly but not tightly enough to reduce circulation.
C. Tubular bandage
Tubular bandages are used for supporting
purpose in case of contusions, light sprains
and post-plaster casting, hold dressings on
fingers or toes because those areas are
difficult to bandage, prevents slipping down
in joints and allows full freedom of movement
and saves Healthcare provider’s time.
They’re made of seamless fabric tube. You
can get elasticized ones to place over joints
such as the ankle.Size of bandages by body part to be bandaged


Self-assessment 2.1
A 9 years male child X is brought to the health center by her mother saying that
he fallen down while he was climbing avocado tree and the child is complaining
for left arm pain; through observation you realize that there is a deformity of the
left forearm and while you try to palpate the arm this act increases the pain to the
child. After consultation you suspect closed fracture and you decide to transfer
the child to the nearest District Hospital for full diagnosis and management.
Questions:
1) Choose the best type of bandage you can use for supporting the injured
upper limb of child X.
a) Roller bandage
b) Triangular bandage
c) Tubular bandage
2) Explain the reason why you choose that type of bandage?
2.2. TECHNIQUES OF BANDAGING2.2.1. Spiral bandage
Learning activity 2.2.1
A male patient Y. has a wound on his left lower arm and his wound is to be
dressed and supported by a spiral bandage. Referring to the aside image of
spiral bandage, use the model in simulation lab and make a spiral bandage ofthe lower arm of the patient.
a) Description
A bandage rounds a part of the body, overlapping the previous section at each
turn.Spiral turns are used to bandage parts of the body that are fairly uniform in
circumference.
Example: Upper arm, upper leg.
b) Implementation
• Make two spiral turns to anchor the bandage,
• Continue spiral turns at an oblique angle about a 30 degree,
• Each turn overlapping the preceding one by two third the width of the bandage,• Terminate the bandage with two circular turns and secure the end.
Self-assessment 2.2.1
Respecting principles and steps of bandaging techniques,
Perform the spiral bandage of upper arm using the mannequin in simulation laband respecting principles and steps of bandaging techniques
2.2.2. Spica bandage
Learning activity 2.2.2
A female patient D has fallen down and got a wound on her right upper arm.
The wound is to be dressed and supported by a spica bandage to stop bleeding.
Referring to the aside image of spica bandage, use the model for bandaging inthe simulation lab and make a spica bandage of the upper arm of patient D.
a) Description
A bandage in which a figure of eight turns are applied, each a little higher or lower,
overlapping a portion of each preceding turn so as to give an imbricated appearance.
b) Implementation
• Hold the roll in the dominant hand, and the beginning of the bandage in the
other hand and face the patient.
• Make 2 circles, the 1st slightly at an oblique angle, then fold up the formed
point and maintain it by the 2nd circle.
• Wrap progressively by crossing the bandage towards the top, in a figure 8
fashions.
• Make sure that the crosses are well one above the other.• End by 2 wraps. Secure bandages with adhesive plaster or a safety pin.
Self-assessment 2.2.2
Perform the spica bandage of the lower arm of mannequin in simulation lab by
following the steps of spica bandaging correctly and respecting the rules andprinciples of applying bandages.
2.2.3. Earlobe bandage
Learning activity 2.2.3
A 20 years female K. had a left earlobe wound infection after piercing her
ears. The wound care was done and you are asked to help by covering the
dressing using earlobe bandage. Following the image illustrated of earlobebandage aside, use the mannequin and make an earlobe bandage for K.
a) Description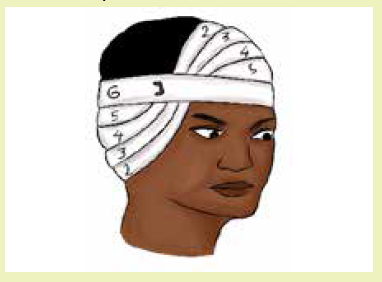
Earlobe bandage consists of use of a strip of material such as gauze or cloth used
to protect, compress, or support a wound dressing of the ear.
b) Implementation
• Make 2 circles facing the patient, the 1st slightly at an oblique angle, then
• Fold up the formed point and maintain it by the 2nd circle.
• Make three oblique drops as for the eye, which means upward from the ear
and downward on the parietal region of the opposite side, in order to have a
crossing at the location of the brow just above the eye.
• When bandaging the left ear, start from the top of the head at the right side;
When bandaging the right ear, start under the ear and avoid covering the eye.
• Secure bandages with adhesive plaster or a safety pin.
Self-assessment 2.2.3
Form groups of two learners and make the earlobe bandage for each other by
following steps of earlobe bandage, respecting rules and principles of applicationof bandages.
2.2.4. Cranial bandage
Learning activity 2.2.4
A 30 years old cyclist had road traffic accident and got head injuries; the multiple
wounds cover his head and it is necessary to support the wound dressings using
bandage. Referring to the image of cranial bandage also known as capeline of
head illustrated, Work in pairs and perform a cranial bandage of your colleagueshowing the way you can bandage the patient after wound care.
a) Description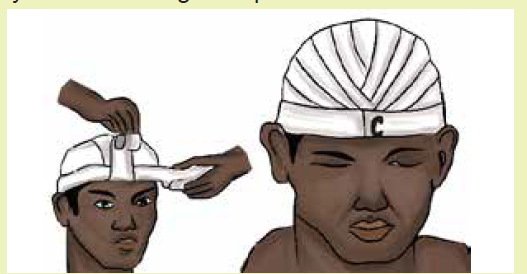
Cranial bandage is sometimes used when the whole scalp is to be covered. A
double headed roller bandage is used. The patient should be seated and the nurse
should stand behind the patient.
b) Implementation
• Place a center of the outer surface of the bandage in the center of the
forehead, the lower border of the bandage lying just above the eyebrows.
• The head of the bandage as brought over the temples and above the ears to
the nape of the neck where the ends are crossed.
• The upper bandage being carried, round the head and another brought over
the center of the top of the scalp to the root of the nose.
• The bandage which encircles head is now brought over the forehead, covering
and fixing the bandage which could cross the scalp.
• This bandage is then brought back over the scalp.
• Slightly to one side of the center, thus covering one margin of the original turn.
• At the back, it is again crossed and fixed by the encircling bandage and is turn
back over the scalp to the opposite side of center line,
• Now covering the other margin of its original turn.
• These backward and forward turns are repeated to alternate side of the
center, each one being, in turn, fixed by encircling bandage until the whole
scalp is covered.
• The bandage is completed by a circular turn around the head and pinned in
the center of the forehead.Self-assessment 2.2.4
In groups of two learners perform capeline of head bandage to each other
following all steps of the procedure and respecting the rules and principles ofbandages application.
2.2.5. Monocular bandage
Learning activity 2.2.5
Mr. G had an injury of the left eye and he needs a monocular bandage to prevent
swelling of his injuries.
Referring to the illustrated image, perform a monocular bandage of the left eyefor Mr. M.
a) Description
Monocular bandage also known as “Crossed bandage of one eye” is the way of
bandaging used to hold dressing of the eye.
b) Implementation
A bandage of 1.5-2width is required for monocle bandage.
• Start on the forehead by a first circular, turned at an angle, at which it is fold
back between first and the second circular without tightening too much.
• Oblique wraps are made, ascending while passing under the earlobe.
• Go up to the interior angle of the affected eye and at the opposite top of the
head.
• Cover the first jet of the 2/3rd while moving away from the center, which
means, crossing on the face then move away from the nose on the eye-level.
• Make 3 wraps.
• End by a frontal circle.
• Secure bandages with adhesive plaster or a safety pin.
• It is necessary to systematically move up on the ear, and down on the top
from the head.
Some people prefer to take the bandage around the forehead between each turn
covering the dressing, but this makes a heavy bulk around the head which is notreally necessary.
Self-assessment 2.2.5
A 10 years old male child had left eye problem, after being operated, a wound
dressing is to be done and supported by a left eye bandage. Use group of twolearners and perform eye bandage
2.2.6. Binocular bandage
Learning activity 2.2.6
Mrs. N. a 56 years old woman underwent a surgery of both eyes and there was
need for binocular bandage to support the dressing and prevent swelling.Perform the binocular bandage as illustrated in the aside image.
a) Description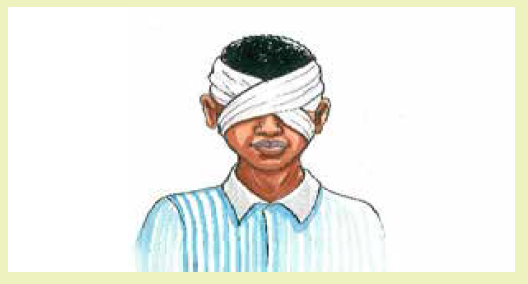
Binocular bandage also known as “Crossed bandage of both eyes” is the way of
bandaging used to hold dressings of both eyes.
b) Implementation
• A figure of eight technique is used.
• Start on the forehead and make two circles; the first slight at an oblique angle,
then fold up the formed point and maintain it by the second cycle.
• From the nape of neck pass through the right top of the head, the interior
angle of the left eye and under the left earlobe.
• Go down in the nape of the neck, under the right earlobe, the interior angle
of right eye and pass at the left top of the head.
• Make a frontal circle. Three times, repeat the movement while deviating, on
the one hand from the top of the head, on the other hand from the nose: the
wraps cross on the face above the nose.
• Do not tighten on the eyes.• End by two wraps and secure bandages with adhesive plaster or safety pin.
Self-assessment 2.2.6
In classroom and in pair, perform binocular bandage to each other following
all steps of binocular bandage and respecting rules and principles of bandageapplication.
2.2.7. Hand gloved bandage
Learning activity 2.2.7
K. a 10 years old child has a dressing on the back of his hand and there is
need to do a hand-gloved bandage in order to protect the wound and supportthe dressing. Perform a hand gloved bandage of the left arm as illustrated aside.
a) Description
Hand gloved bandage also called complete bandage of hand is used to retain
dressings on the back of the hand.
b) Implementation
• Hold the roll in the dominant hand, and the beginning of the bandage in the
other hand and face the patient.
• Make 2 circles, the 1st slightly at an oblique angle, then fold up the formed
point and maintain it by the 2nd circle.
• If hand is pronated: start with the small finger of the right hand or start with
the thumb of the left hand.
• If hand is supinated: start with the thumb of the right hand or start with the
small finger of the left hand.
• Form a spiral at each finger, starting with the distal part of each finger.
• Each time, make the bandage pass over the back of the hand before returning
to the wrist.
• Make a circle at the wrist before to start wrapping next finger.
• End by 2 circles at the wrist. Secure bandages with adhesive plaster or a
safety pin.
Self-assessment 2.2.7
In simulation lab, using the mannequin perform hand gloved bandage using
appropriate bandage type, following steps of hand gloved bandage and
respecting rules and principles of bandage application.
2.2.8. Triangular Bandage
Learning activity 2.2.8
A 32years old male was injured on his elbow in a motorcycle accident and you
are among the people gathering around the accident site.
Work in pairs and perform a triangular bandage of the right arm as illustratedaside.
a) Description
Triangular bandage, also known as handkerchief bandage is used for temporary
or permanent dressing of wounds, fractures, dislocations and slings.
It is very valuable in first-aid work since it is quickly and easily applied and can be
improvised from any kind of cloth such as a piece of cloth such as a shirt, a sheet,
a large handkerchief etc.
b) Implementation
• Ask the patient to bend his arm to be placed in a sling bringing the forearm on
the chest, so that the hand is placed higher than the elbow.
• Place the bandage under the Patient’s arm on his chest (the center of the
triangle base under the wrist, angle point at the level of the elbow, neck scarf
at the level of the neck).
• Hold upward lower the sling of the arm, above the wrist.
• Fix a reef knot on the unaffected side (never fix it on the spinal column).
• Fold the excess cloth on the level of the elbow and fix it with safety pins.
• Check the correct setting of the scarf (hand and forearm maintained abovethe elbow).
Self-assessment 2.2.8
Mr. F. has injured in road traffic accident and he has injured his right elbow, make
pairs in class and perform triangular bandage simulating to support Mr. F’s arm
before evacuation from the accident point.
2.2.9. Stump bandage
Learning activity 2.2.9
Mr. M.’s left leg has been amputated below the knee due to a malignant disease
condition. After the surgical operation the stump was sutured, dressed and
bandaged. On the 3rd day post-operative, there is need to change the dressing
and do a stump bandaging. After the wound dressing, you have to apply a stump
bandage.
Perform a stump bandage of Mr. M’s left leg on the model in the simulation labas illustrated in the image.
a) Description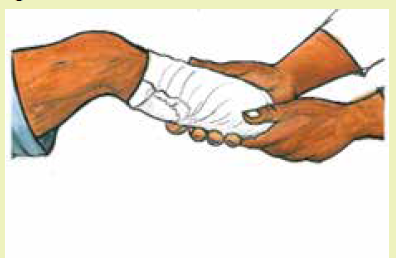
Stump bandage also known as recurrent bandage of the stump is used to control
postoperative edema and to shape the stump, hold the dressing around the stump
of arm, leg or around finger. The elastic bandage is applied in a recurrent or figure
of eight fashion with more pressure applied to the distal, rather than the proximal
portion of the limb.
b) Implementation
• Use a four-inch bandage and make two circular turns round the limb and
place the end of the bandage in the center of the upper side of the limb.
• Carry the bandage over the center of the stump to the same level behind
holding the turns back and front with the thumb and finger of the other hand.
• Repeat the recurrent turns over the end of the stump first on the left and then
on the right side of the original turn, until the whole of the dressing is covered.
• Fix the loop with a straight turn round the stump and continue the bandage with
figure of eight turns round the limb until the dressing is completely covered.• Secure with a safety pin.
Self-assessment 2.2.9
In simulation lab, using a mannequin of stump, perform stump bandage andterminate with spica following steps of stump bandage application.
End unit assessment 2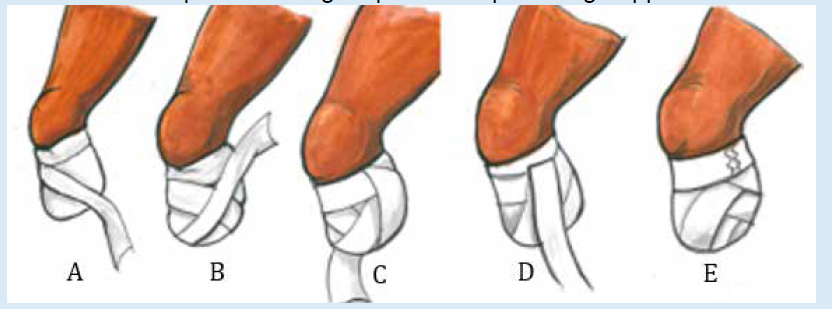
Match the item in column A with the appropriate statement in column B
(2) Outline at least five rules of bandage application.
(3) Give two specific examples of roller bandaging techniques.
(4) Point out 3 purposes of bandaging.
(5) Appraise why a bandage have to be anchored as a rule of bandaging.
(6) Describe the consequences of tightening the bandage.(7) Indicate the type of bandage performed on the images below.
(8) Reorder the shuffled order of steps followed to make a triangular bandage.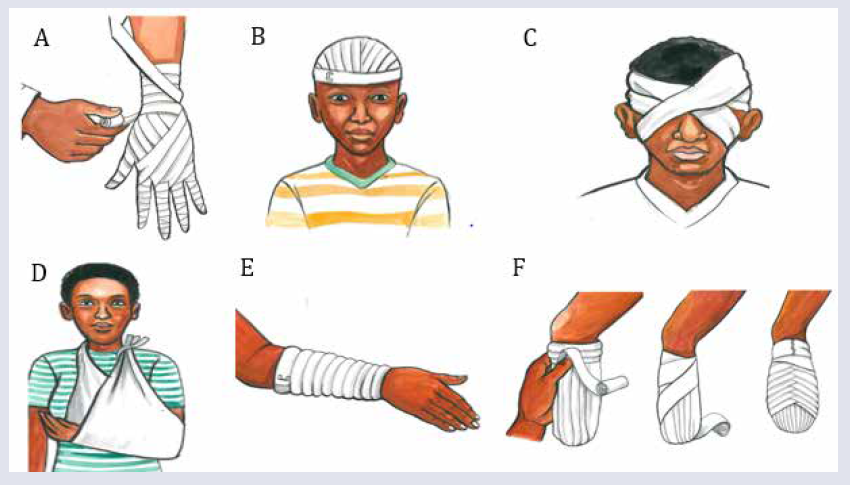
Shuffled order of triangle bandaging technique
f) Hold upward lower the sling of the arm, above the wrist.
g) Ask to the patient to bend his arm to be placed in a sling bringing the
forearm on the chest, so that the hand is placed higher than the elbow.
h) Fix a reef knot on the unaffected side (never fix it on the spinal column).
Fold the excess cloth on the level of the elbow and fix it with safety pins.
i) Face the patient and ensure good communication with the patient
j) Check the correct setting of the scarf (hand and forearm maintained above
the elbow).
Place the bandage under the patient’s arm on his chest (the center of the triangle
base under the wrist, angle point at the level of the elbow, neck scarf at the levelof the neck).
(9) Reorder the shuffled order of steps followed to make a stump bandage
Shuffled order - stump
a) Repeat the recurrent turns over the end of the stump first on the left and
then on the right side of the original turn, until the whole of the dressing iscovered.
b) Make two circular turns round the limb and place the end of the bandage
in the center of the upper side of the limb.
c) Carry the bandage over the center of the stump to the same level behind
holding the turns back and front with the thumb and finger of the other
hand.
d) Secure with a safety pin.
e) Fix the loop with a straight turn round the stump
f) Continue the bandage with figure of eight turns round the limb until thedressing is completely covered.
UNIT 3 BASIC LABORATORY INVESTIGATIONS FOR COMMON CONDITIONS
Key unit competence
Perform basic Laboratory investigations for common conditions
Introductory activity 3
The following pictures illustrate different procedures. Critically analyze them andrespond to the following questions
1. Describe the procedure you think is being done in picture A and picture B
2. Which procedure do you think is invasive and why do you think so.
3. With clear rationale explain the procedure you think can produce results
as quick as possible between A and B
4. What do you think the technique performed will help the casualty
3.1. BASIC LABORATORY INVESTIGATIONS FOR
COMMON CONDITIONS
Learning activity 3.1
Search the book of nursing laboratory and diagnostic investigations then
define and explain the rationale for each of the following test.
a) Rapid disgnostic test
b) Glycemia test
c) Glucosuria test
d) Albuminuria test
3.1.1. Rapid Diagnostic Test for Malaria (RDT)
Malaria is among serious threat killing many people worldwide. Since infection
with Plasmodium parasites causes clinical presentation indistinguishable from
other fever-causing pathogens, rapid, accurate diagnosis is a crucial component of
effective case management.
Malaria rapid diagnostic tests (RDTs) assist in the diagnosis of malaria by detecting
evidence of malaria parasites (antigens) in human blood. These tests require a
drop of peripheral blood, normally collected from a finger or heel prick. Visual readouts
are available typically within 20 minutes or less.
Malaria rapid diagnostic test are frequently used in high malaria endemic area
such as sub-Saharan Africa and in low to moderate transmission area such as Asia
and South America, where maintenance of capacity for malaria microscopy and its
quality control are obvious burdens for malaria control programs.a) Parts of a malaria rapid diagnostic devices
b) Interpretation of RDT for Malaria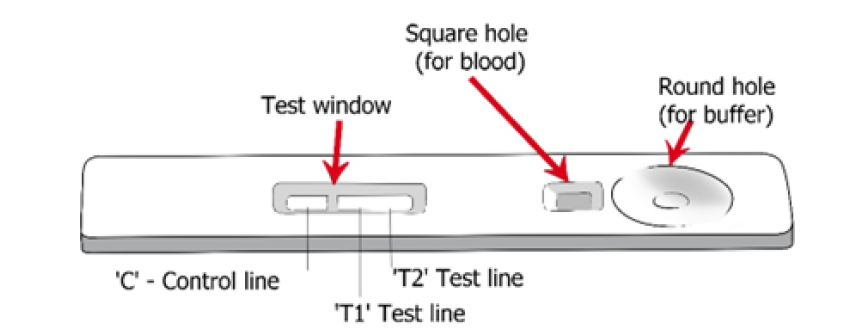
In interpreting rapid diagnostic test for malaria, one of the three possible outcome
should be revealed.
When the device shows the appearance of a line near T and C means that there
evidence of plasmodium parasites (Positive). Line near C and no line near T
means that there is no evidence of parasites (Negative). Line near T and or no line
means that the results is invalid. A studies assessing the sensitivity and specificity
of two different brand of RDT for malaria used Rwanda has demonstrated that the
sensitivity of RDT for malaria were around (80.2%-89.5%) while the specificity was
(86.2 %-94.3).
Such interpretation can be challenging, especially when compared with microscopy
exam. There are instances where RDT will be positive but no parasites will be seen
on microscopy, conversely, there are instances where RDT will be negative but
microscopy will detect parasites in the blood. There are instances too, when RDT
will be positive but there is no clinical malaria or, the fever is not caused by malaria.
Despite the fact that RDTs are recommended as a means of laboratory confirmation
of malaria before the prescription of antimalarial, the interpretation of test results
should be done with caution to ensure better malaria case management.Table illustrating possible Malaria Rapid diagnostic results
3.1.2 Glycemia test
Glycemia test also referred to as blood glucose test is a test used to measure the
level of glucose within the blood, again it is used to find out if the blood sugar levels
are in the healthy range.
The highlighted materials will be used in measuring glycaemia: Glucose meter
or glucometer measures how much sugar is in the blood sample. Test Strips,
Lancets, and Lancet Device: each small plastic strip contains chemicals that
convert the sugar in the blood into an electric current that the meter can read. It is
used by putting a test strip into the meter. Prick the side of the fingertip with a small
needle called a lancet. The results will be visible on glucometer machine within 1
minute.
If the level of sugar in the blood is high it will be referred as hyperglycemia, and
hypoglycemia for low level. Blood glucose test is often used to help diagnose and
monitor diabetes. People with diabetes require regular monitoring of their blood
glucose to help them achieve as close to normal blood glucose levels as possible for
as much of the time as possible. The benefits of maintaining a blood glucose level
that is consistently within the normal range will reduce the short-term, potentially
life-threatening complications of hypoglycemia as well as the occurrence rate and
severity of the long-term complications of hyperglycemia.
a) Fasting glucose Level
We say fasting glucose when the blood sample is obtained after 8 hours of fasting.
In non-diabetic patient, glucose levels vary between 70 mg/dl to 110mg/dl (4.0
to 5.4 mmol/L). In diabetic patient glucose level is more above110mg/dl but less
126mg/dl or 7.0 mmol/L.
b) Random glucose level
Random glucose level refers to the glucose level checked without regard to the last
meal. It is useful for people who need a speedy diagnosis, such as those with type 1
diabetes who require medication as a matter of emergency. Diabetes is diagnosed
if random glucose level is above 200 mg/ dl or above 11.1 mmol/l with symptoms
of diabetes.
c) Principles of measuring glycemia
The measurement of glucose is one of the longest established and most frequently
performed tests in the clinical biochemistry laboratory. Although conventional
laboratory techniques measure blood glucose as concentration in plasma or whole
blood, not that direct-reading electrode systems measure it as molality in mmol/kg
water, which is numerically greater, but results are often factorized and expressed,
e.g. as plasma glucose concentration.
In measuring glycemia as an associate nurse, you need to know that glycemia can
measured by two main methods. A blood drop sample is usually collected from a
fingertip prick. Alternatively, the glycaemia may be measured by taking the blood
from the vein.
Ensure that the patient has fasted for at least 8 hours in case of fasting blood
glucose. The patient should not eat or drink anything other than water for at least 8
hours before the blood sample is taken.
If random blood glucose, the glycemia is taken regardless of when the patient
last ate. In this case, several random measurements may be taken throughout
the day to allow for identification of fluctuations in blood glucose levels. When the
fluctuations vary widely, this may mean a problem.
A 2-hour postprandial blood sugar test measures blood sugar exactly 2 hours
after the patient starts eating a meal. This is useful for diabetic patients who may
need to inquire about the efficacy of insulin being taken, and if the right amount of
insulin is being taken with meals.
Sites for rapid blood glucose checking may be alternated and apart from pricking
the fingers, there is a way to prick the earlobe, heel, forearm or palm. Alternate
site testing provides similar results to finger-prick testing, especially in the fasting
and two-hour post meal times. Using alternate sites may be less painful but may
need a deeper lance. Ensure that the blood glucose machine and its equipment
allow the alternate sites. It is recommended to respect principles of asepsis in
measuring blood sugar level.
3.1.3. Urine test
Urine tests sometime referred to as urinalysis are laboratory investigation done
to examine the physical and chemical properties of urine and its microscopic
appearance to aid in medical diagnosis of different health conditions. Urine test is a
simple and noninvasive test that provides valuable information. An associate nurse
should be able to perform urine test using urine strips and analyses glucose and
albumin in it. After doing the technique of urine collection, Results are obtained by
direct comparison of the color blocks printed on the bottle label. The color blocks
represent nominal values; actual values will vary around the nominal values.
a) Albuminuria
Albumin is a protein found in human blood. Albumin help to maintain blood volume
and pressure. The action of the kidney is to filter the blood to remove waste products
and these filters (known as glomeruli) prevent large molecules, such as albumin,
from passing through. If these filters are damaged, albumin passes from the blood
in to the urine. If kidneys are damaged and albumin leaks into the urine in very
small amounts it will be referred as microalbuminuria. As kidney function declines
the amount of albumin in the urine increases, and larger or ‘macro’ amounts of
albumin may be present. This is known as macroalbuminuria.
In normal person, albumin is not excreted in the urine. Increase level of albumin
may cause major health risk therefore detection of albumin in urine is essential for
diagnosis albuminuria related diseases. Several methods to detect albumin in the
urine have been identified including calorimetry, radioimmunoassay, immuno enzymatic
assay, turbidimetry, and dipsticks tests. Our focus here will be dipsticks test
only. The strips technique is simple, cost effective and can give quicker results.
The albumin strip technique can be used even in rural areas where sophisticatedlaboratory testing facilities are not available.
Interpreting albumin results test is not
difficult. Results are obtained by direct
comparison of the color blocks printed on
the bottle label. The color blocks represent
nominal values; actual values will vary
around the nominal values.
False positive results may be obtained
with highly alkaline urine. Contamination
of the urine specimen with quarternary
ammonium compounds may also produce
false positive results.
In 24-hour urine, 1.0-14.0 mg/dl of protein may be excreted by the normal kidney.
A color matching any color block greater than trace indicates significant proteinuria.
For urine with high specific gravity, the test area may most closely match the trace
color block even though only normal concentrations of protein are present. Clinical
judgment is needed to evaluate the significance of trace results.
a) Glycosuria
Glycosuria meaning glucose in the urine, results from the glomerular filtration of
more glucose than the renal tubule can absorb. It occurs in all normal individuals
in amounts up to 25 mg/dl in random flesh urine. Abnormally increased glycosuria,
results from either an elevated plasma glucose, an impaired renal glucose absorptive
capacity, or both.
The plasma glucose concentration of 25mg/dl indicating glucosuria is called
the renal threshold for glucose. Its value is variable, and deviations occur both above
and below the commonly accepted «normal» threshold of 180 mg/dl. In diabetic
patients, the value is reported to vary from 54 to 300 mg/dl. Although glucosuria
greater than 25 mg/dl is considered pathologic, many commercial urine tests for
glucosuria that are available to patients fail to detect glucosuria until it reaches a
level of 50–250 mg/dl.
Techniques for measuring glucosuria are based upon either glucose oxidase
(specific for glucose) or copper sulfate reduction. Strip test are oxidase base and is
our focus in this unit. The sensitivity of commercial clinical “strip” methods can be10–15 mg/dl, although 50 mg/dl is usually detected.
The test of glucosuria using strips is based
on a double sequential enzyme reaction.
One enzyme, glucose oxidase, catalyzes
the formation of gluconic acid and hydrogen
peroxide from the oxidation of glucose. A
second enzyme, peroxidase, catalyzes the
reaction of hydrogen peroxide with potassium
iodide chromogen to oxidize the chromogen
to colors ranging from blue-green to greenishbrownthrough brown and dark brown.
Self-assessment 3.1
1) Explain how does rapid diagnostic test for malaria work?
2) How accurate are malaria rapid test?
3) In human body glucose level can be tested from the peripheral capillaries
or from the urine. Discuss on normal ranges from each method and onthe main causes of deviation from normal ranges in each method?
3.2. Techniques of performing basic laboratory investigations
for common conditions
3.2.1.The technique of performing Rapid Diagnostic Test for
malaria
Learning activity 3.2.1
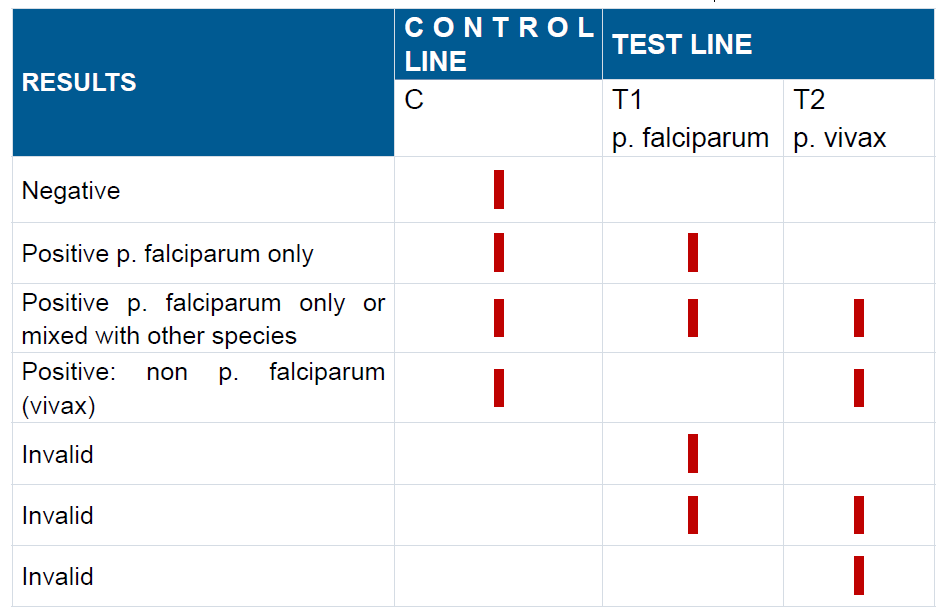
The following picture illustrate the steps of rapid diagnostic test for malaria. Byfollowing the steps as illustrated in the image:
1) Perform the technique of rapid diagnostic test on the mannequin in the
skills lab
2) What do you think would happen if you start the technique without washing
your hands?
3) After pricking the finger with a lancet it should be thrown in shaft box.
Discuss why it should not be thrown in the dustbin
4) In step 4, it is stated that the finger should be dried. What do you think as
the main reason?
a) Materials
1) Gloves
2) RDT kit
3) Safety box
4) Dustbin
5) Timerb) Procedure of Rapid diagnostic test for malaria
Self-assessment 3.2.1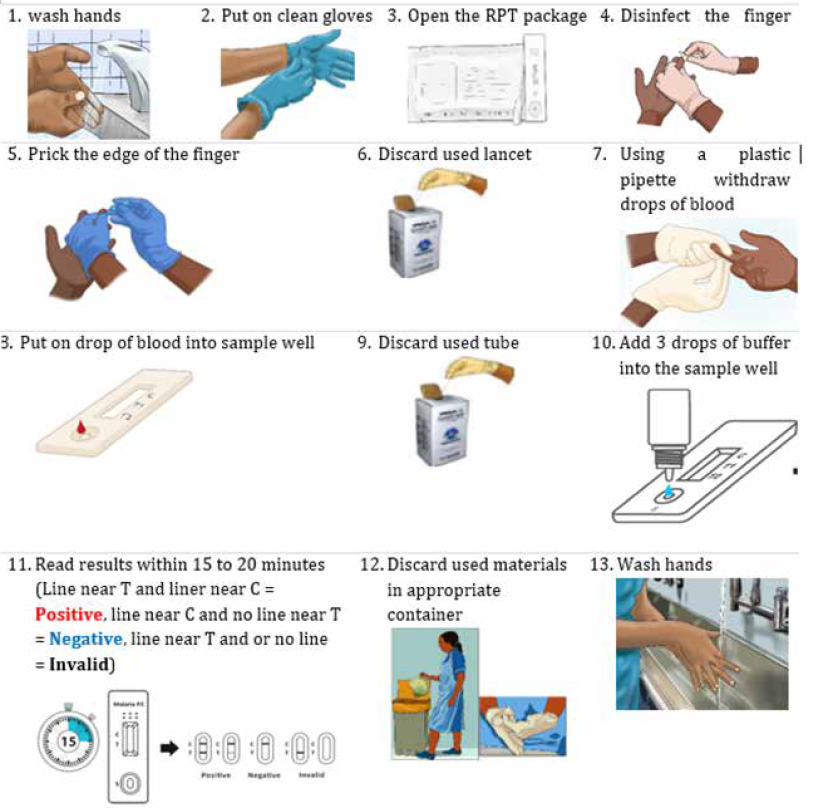
After learning the technique of rapid diagnostic test for malaria make groups of
two then go in the skills lab then screen malaria on each other using RDT. Make
sure to follow steps as you learnt them.
3.2.2.The technique of performing urine test (Albumin, Glucose)
In pairs of two and perform urine test for albumin and glucose on each other
using urine dipstrip available in the simulation lab.
The Urine must be tested within a few hours of voiding as urinary constituents can
become unstable and may affect test results.
a) Materials
1) Package insert
2) Strips
3) Specimen container
4) Glovers
5) Timeb) Procedure of urine test (Glucose and Albumin)

Self-assessment 3.2.2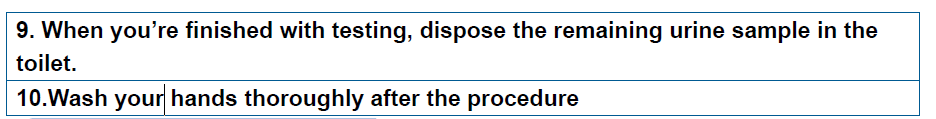
The following picture illustrate a urine test done using dipsticks on two different
patients (Case A and B). compare the test results in case A and case B to the
reference scale and explain whether the patient’s glucose and albumin level arein normal range or not
3.2.3 Techniques of performing Glycemia test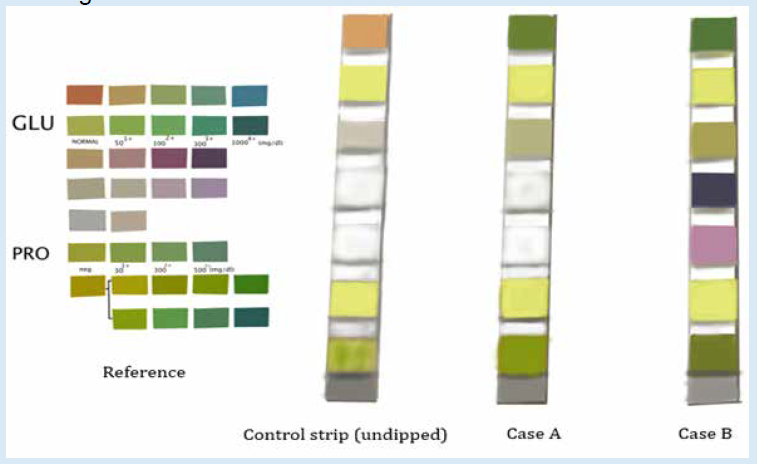
Learning activity 3.2.3
A blood glucose test is a blood test that check if patient have high glucose
level in the blood. The following materials are used in performing glycemia test:
glucometer, test strips, alcohol swab, lancet, gloves, cotton wool/gauze, sharpsbox or safety box
1) Modeling from the illustrate above perform the technique of glycemia test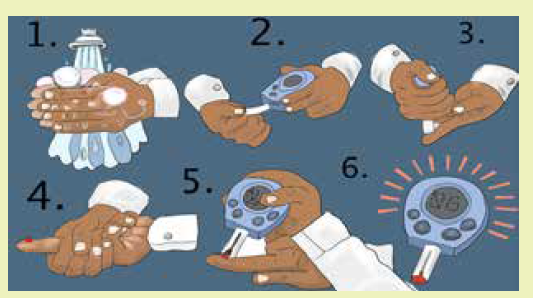
on the mannequin in the skills lab
2) The normal threshold of fasting glucose level and random glucose level
are different. Discuss and differentiate the fasting glucose level from therandom glucose level.
The technique of glycemia test using strips
a) Materials for glycemia test
Blood glucose monitor
1) Test strips (check that they are in
date and have not been exposed
to the air)
2) Alcohol swab
3) Single-use safety lancets or
lancing device,
4) Gloves,
5) Cotton wool/gauze,
6) Sharps box or safety box,
7) Control solution for calibration
b) Steps for Glycemia check
1) Ask the patient to sit down and explain what you are going to do.2) Wash the hands and put on gloves.
3) Choose the site for the blood sample: usually the side of a finger, but the
arm or thigh may be used (change the site used if frequent measurements
are needed).
4) Use an alcohol swab to clean the site and let the alcohol dry.
5) Insert the test strip into the monitor, following the instructions
6) Use a single-use lancet or a lancing device to draw blood and dispose of
it in a sharps container.
7) Don’t go deeper than necessary
8) Apply the blood to the testing strip in the correct way: some strips need
the blood drop to be over the whole of the test pad and some suck up the
blood directly from the site of the bleeding.
9) Place the gauze over the site and hold it there, or let the patient hold it
there until the bleeding stops.
10) Read and record the result, reporting and/or responding to abnormal
readings.
11) Tell the patient what the result is, explain it
12) Thank the patient
13) Dispose of all used equipment safely
14) Wash the handsGraphical illustration of the technique of glycemia test
Self-assessment 3.2.3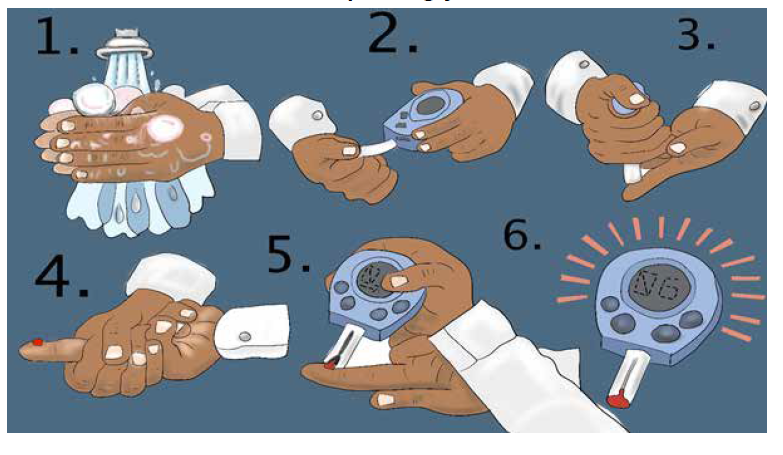
After learning the technique of screening glycemia group yourself in pair. go in
the skills lab, prepare materials for glycemia test and test each other by followingthe checklist of the technique.
End unit assessment 3
1) Is it recommended to use one RDT devise on more than one person?
a) Yes
b) No
2) Abnormally increased glycosuria, results from elevated plasma glucose,
or from impaired renal glucose absorptive capacity.
a) Yes
b) No
3) Which of the following confirmed values meet the diagnostic threshold for
diabetes?
a) Random glucose > 160 md/dl
b) Fasting blood glucose equal to 140 md/dl
c) 2 hrs post prandial glucose ≥ to 126 mg/dl
d) Fasting blood glucose ≥ 126 md/dl
4) Why is it advised to write down the time after adding the buffer in the RDT
and not after adding the blood?
5) The following 4 pictures illustrate real malaria rapid diagnostic results
tested from 4 different patients, observe them carefully and explain which
one reflect a positive malaria result, a negative malaria result and amalaria invalid results.
6) Mr. WS comes at the health center where you work as an associated
nurse. In consultation room he tells you that he is urinating a lot often at
night, is very thirsty, and very hungry. He tells you that before he enters in
your consultation room he took 2 bottle of Fanta. You decided immediately
to rule out if his blood glucose level is within normal range or not.
a) In a stepwise approach describe how you would perform the technique of
glycemia test
b) After the test you found that his glycemia is 198 md/dl. Interpret such
finding and explain whether it is normal or not
7) Albumin is a protein found in the bloodstream of mammalians, explainwhat you think as the main cause for it to be found in urine?
UNIT 4 FIRST AID CARE IN EMERGENCY SITUATIONS
Key unit competence
Provide first aid in case of emergencies
Introductory activity 4
1) What are similarities in these pictures?
2) Each picture represents an emergency situation. Attempt to describe the
situation and what is being done
3) What should be expected from a first aider?
4.1. First aid
4.1.1 Concepts of first aid, triage in emergency care
Learning activity 4.1.1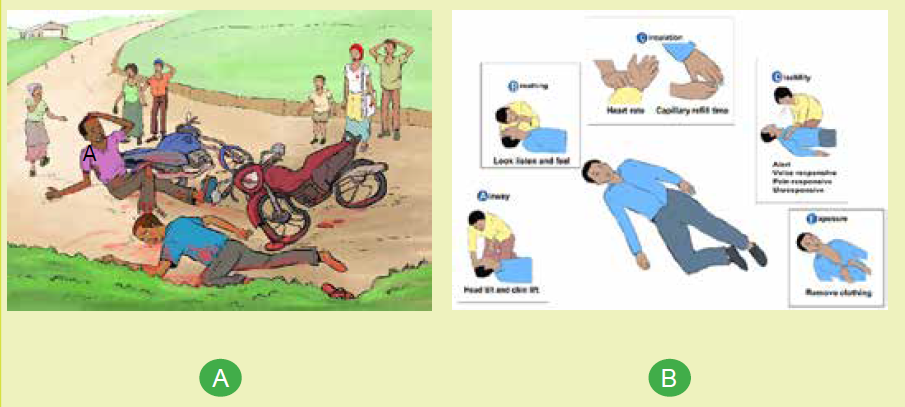
1) What do you observe on picture A and B
2) Assume that you are the first bystander at car accident, how can you
behave
a) Concepts of first aid
First aid referred as “Emergency aid” or immediate care is the first skilled
[acceptable] assistance given to a victim (sick or injured) on the occurrence of
accident or sudden illness in order to preserve life, prevent further injury and relive
suffering until qualified medical care is available. For minor conditions, first aid care
may be enough while for serious or complex problems, first aid care should be
continued until more advanced care becomes available. The person who provide
this emergency aid is called a first aider and has a responsibility to keep everyone
involved safe while taking care of the victim.
An emergency is a situation that poses an immediate risk to health, life, property
or environment and requires immediate action.
A Casualty or a Victim is a person who is injured or killed in an accident or in a war.
Bystander is a person/witness who is present at an event or incident but does not
take part.
Triage is a sorting process used to identify the sickest patients or those at greatest
risk of demise so immediate medical needs can be rapidly addressed. It is important
to obtain a verbal consent before attempting first aid as most first aid activities
involve touching to avoid causing offence or distress. A consent is an approval
of what is done or proposed by another or an agreement as to action or opinion.
However, if you encounter a confused casualty who is critically injured or ill, you can
assume that they would want you to help them.
b) Triage in emergency care
Triage is an effective system that classifies patients into groups according to acuity
of illness or injury and aims to ensure that the patients with life threatening illness
or injury, receive immediate intervention and resource allocation. It can be a difficult
decision to make as to who to treat first, however, you should work under the
principle of acting in a way that gives the greatest number of people the greatest
chance of survival.
To meet its goals, the process of triaging considers the following questions and use
START triage system to categorize casualties:
• How sick or injured is the victim?
• What is this victim’s potential for demise?
• How quickly do interventions, care and treatment need to be delivered?
• What is the evacuation plan after initial intervention?
The START triage system
“START” stand for Simple Triage And Rapid Treatment and is a simple way that
allows rapid assessment of victims within 15 seconds per casualty/victim. It is based
on respiratory, perfusion and mental status assessment.
Self-assessment 4.1.1
1) Why do we learn first aid?
2) Briefly explain the START triage flow char.
4.1.2 Principles of first aid care
Learning activity 4.1.2
1) Imagine you are a casualty in a road traffic accident. What would you
expect from the attending firs aider?
2) What qualities do you think should the first aider possess to be effective
in helping casualties?
Learning activity 4.1.2
It is important that when engaging in the application of first aid that you adhere to
the established first aid principles. Four basic principles and concepts underlying
the practice of first aid are:
a) Preserve life:
The first aim of first aid is to preserve life, which involves the key emergency
practices to ensure that the casualty isn’t in any mortal danger. Remember though,
this includes preserving your own life as you shouldn’t put yourself in danger in
order to apply first aid.
b) Prevent deterioration:
Once the first principle is met, as first aider your next priority is to prevent further
illness or injury and or worsening of illness or injury. This can be achieved through
keeping the victim still to avoid aggravating their injury, or from complicating any
unseen issues.
c) Promote recovery
This encompasses steps the first aider follow to lessen the time taken for a casualty
recover from an accident and aid in minimizing lasting damage and or scarring. For
example, applying cold water to a burn as soon as possible to lower the chance of
long-term scarring and helps speed up the healing process.
d) Protect the unconscious casualty
This involves placing an unconscious casualty into the recovery position to keep
their airway clear
4.1.3 Quality of First aid worker
Providing an effective require more than just technical skills. Therefore, a quality
first aider worker should possess several personal qualities and skills to be able to
work under pressure and use common sense.
a) Good communication skills
Communicating with sick and injured people can be challenging. Therefore, a first
aider should have excellent communication skills and a natural ability to talk to
people. Communication is key to good casualty care and is very important when
passing the casualty onto the next level of care. First-aiders should also take care
to listen to any remarks or requests a casualty makes.
b) Ability to work in a team
First aiders are often required to work alongside members of the emergency
services, especially the ambulance service; thus required to be good team player.
c) Ability to work under pressure
First aid situations can range from the mundane e.g. a small cut wound to incredibly
stressful and demanding situation such as cardiac arrest. A first aider must always
remain calm and assess the situation first before rushing to help the victim. This will
help reduce the overall stress levels of the injured person as well as bystanders who
may be concerned. Furthermore, it will help him/her manage tasks whilst having an
awareness of the overall situation. Panic is likely to make the situation much worse
and cause further distress and physical harm to the casualty as a result of wrong
decisions.
d) Good leadership skills
First-aiders must ensure the removal of any danger from the casualty, or remove
the casualty from dangers, and prevent the crowding of casualties by bystanders.
A first aider may therefore have to take command of a potentially volatile situation.
He or she may be looked upon by his/her colleges to provide leadership during an
emergency. A first aider may also have to organize bystanders to assist in various
tasks, such as moving the casualties.
e) Knowledge of their own limitations
A key skill of first aid is being able to recognize someone who needs quick
emergency help. However, a first aider should know the limits of their skills and
knowledge and be able to call for further appropriate help when required rather
than try to do it alone. Calling for help should be done as soon as possible by the
first aider him/her-self or by asking a bystander to do so if preoccupied by handing
the victim. This will ensure that a medical professional arrives quickly to handle the
situation in a more comprehensive manner and provide more specialist treatment.
First-aiders should also understand that first aid has its limitations and does not
take the place of professional medical treatment and that their responsibility ends
when the casualty is handed over to the care of a competent health provider.
Self-assessment 4.1.2
A first aider was attending a multiple causality at the scene below. Comments on
her intervention reflecting on what you have learnt regarding principles of first aid
and qualities of a good first aider.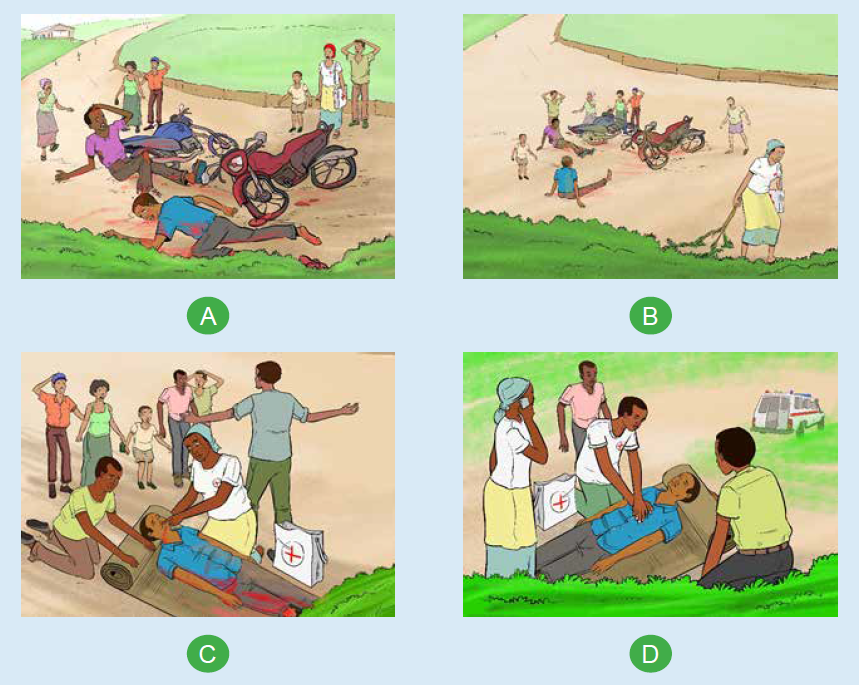
4.1.4 Emergency gestures
Learning activity 4.1.3
With reference to “picture B” illustrated in learning activity 4.1.1) figure out
what ABCDE approach involves for, for effective emergency care provision and
attempt to practice what you see on model mannequin in skills lab.
It is vital for a first aider to provide first aid in an organized and structured manner
for all casualties that is following DRSABCDE sequence. DRSABCDE involve
checking and addressing issues related to Dangers (for you as a first aider, the
victim and others involved people), Response (a quick assessment to find out
whether a casualty is conscious or unconscious), Shout or Send for help, Airway
maintenance with cervical spine protection, Breathing and ventilation, Circulation
with hemorrhage control, Disability and Exposure.
a) Airway maintenance with cervical spine protection
Check that a casualty’s airway is open and clear. If a casualty is alert and talking to
you, it follows that the airway is open and clear. If, however, a casualty is unconscious,
the airway may be obstructed. Obstructed airway dictates some lifesaving gestures
to open and clear the airway namely jaw thrust or chin lift/head tilt as appropriate.
Never move to next step until it is open and clear. for any known traumatic injuries,
the cervical spine immobilization is required.
b) Breathing and ventilation
Check whether the casualty is breathing. If he/she is alert and or talking to you, he
or she will be breathing, however you have to determine if the casualty is breathing
normally through noting the rate, depth, and ease with which he or she is breathing
which requires to look, listen, and feel for breaths. If an unconscious casualty is
not breathing, the heart will stop. Chest compressions and rescue breaths must
be started immediately. Note that a victim who is speaking full sentences is likely
breathing is sufficiently. If the casualty is unconscious and breathing normally, put
him/her in recovery position.
c) Circulation with hemorrhage control
Quickly estimate the patient’s heart rate and determine the quality of the pulse and
evaluate the patient’s skin temperature, color, capillary refill and moisture to assess
perfusion. Check for bleeding (absent or present, if present is it controlled or not).
Injuries that result in severe bleeding can cause blood loss from the circulatory
system, so they must be treated immediately to minimize the risk of a life-threatening
condition known as shock. If a pulse is present and capillary refill is < 2 seconds,
the patient’s circulation is likely sufficient.
d) Disability
Briefly evaluate the neurologic status and note any neurologic deficit. Any change
in mentation from baseline should be concerning.
e) Exposure
Expose the casualty both anterior and posterior body surfaces and look for injuries,
rash, etc., ask about recent exposure to infectious diseases note and address
environmental concerns (hypothermia/hyperthermia).
f) Recovery position
Putting a victim in a recovery position is a frequent emergency aid gesture used for
unresponsive victims who have open airway and are breathing. This position helps
keep the victim airway open and allows any vomit to drain onto the floor preventing
the victim from choking on it as well as from asphyxiation due to body position.
Following are the steps for putting the victim into the recovery position:
1) Put the person on the floor if he is not there already
2) Remove the person’s spectacles if necessary
3) Kneel down by the side of the casualty
4) Make sure both victim’s legs are outstretched
5) Place the nearest arm (the one on the side you are
kneeling next to) at right angles to the victim’s body
6) Bend the forearm upwards
with palm facing up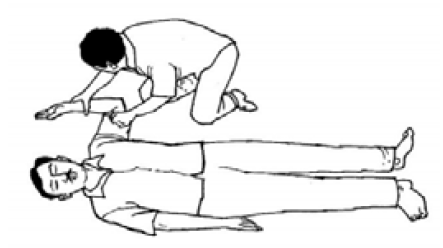
7) Lay the person’s other arm
across his chest.
8) Hold the back of this hand
against his cheek on the side
at which you are kneeling.
9) Keeping that hand in that
position, with your other free
hand, grasp the leg on the
other side of the victim’s body
under the knee.
10) Raise that leg, but leave the
person’s foot on the ground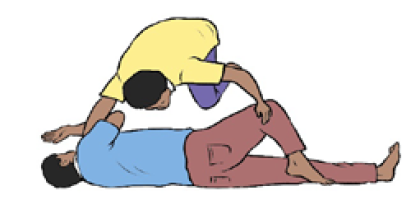
11) Pull the raised leg towards you.
12) In the meantime, keep the
back of the victim’s hand
held against his cheek. Roll
the person towards you so he
turns on his side.
13) Position the victim’s upper
leg in such a way that his hip
and knee are at right angles.
This will allow the victim to
maintain lateral position.
14) Tilt the head of the person
backwards to keep the airway open.
15) Make sure the mouth is
angled towards the ground.
This will prevent the risk of
choking on blood or vomit.
16) Adjust the hand under the cheek if necessary so that the head remains
tilted backwards and the mouth remains at a downward angle.
17) Do not leave a casualty alone and continue observing his condition and
monitoring his breathing. If the person stops breathing, start resuscitation.
Note:
An unconscious, breathing casualty who is heavily pregnant, should be placed on
their LEFT side so the weight of the baby does not put pressure on a major vein on
the right side of the abdomen.
Self-assessment 4.1.3
In your groups go in the simulation lab and perform the ABCDE used emergency
situation on model mannequin and attempt to put the mannequin in the recovery
position.
4.2.First aid in the selected common emergency situations
Introductory activity 4.2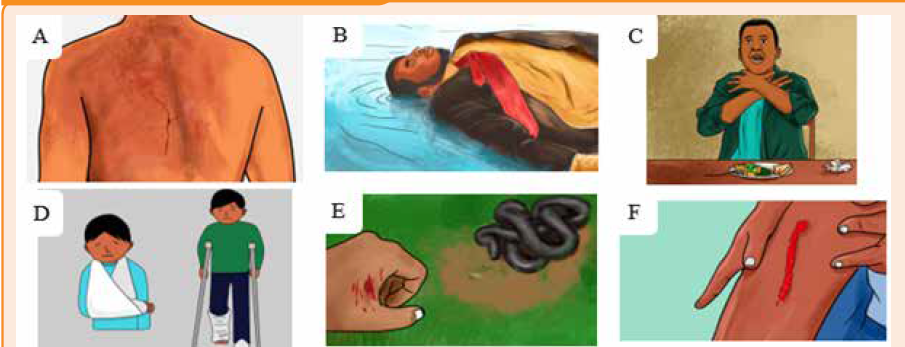
1) Observe and describe each of the above pictures?
2) Summarize the emergent interventions to a snake bite used in your
community
3) Which of the following are considered personal protective equipment?
a) Gloves
b) Mask
c) Eye shield
d) All of the above
4.2.1 Burns
Learning activity 4.2.1
Outline the causes of burn you known.
object, electrical current, radiations sources, certain chemicals and exposure to
extreme cold. The burn is characterized by its appearance, its location, its extend,
its degree and the presence of pain. Burns can vary from minor superficial burns to
very deep burns that damage muscles, tendons, nerves, and even bones.
First aid interventions in case of burn include:
• Assess the situation quickly and calmly to get an understanding of what
happened
• Calm and motivating the victim to collaborate.
• Ensure that the source of the burn has been dealt with, and the scene is safe.
• Wear personal protective equipment, and get the first aid kit if available.
• Gently remove any clothing and jewelry from the burned area. DO NOT try to
remove any clothing that is sticking to it
• Rinse the burn in cool or cold water for about 20 minutes. If the area cannot
be immersed such as the face, towel, sheets or wet clothes that have been
soaked in water can be applied. Change/rewet these regularly as they will
absorb heat from the burn.
• For small burn apply antibiotic / burn cream if available and the victim is not
allergic to it
• Cover the burn with a clean, dry non-stick dressing and loosely bandage in
place. If this is not available or the burn covers a large area use a dry, clean
sheet or other tissue material
• Have the person follow up with a health care provider.
• Do not apply ice to a burn. This technique will result in a cold injury on top of
a burn and cause further tissue damage
Note: Do not apply ice to a burn. This technique will result in a cold injury on top of
a burn and cause further tissue damage
Self-assessment 4.2.1
Your classmate, was using an iron that is in its maximum warming up accidently,
it /falls on his/her left foot cause a superficial burn. You are warned by a loud
scream of pain. You jump to see what happen. What will you do to help him/her?
4.2.2.Drowning
Learning activity 4.2.2
1) Observe and describe the picture
aside.
2) What can you do to help the drowned
victim?
Drowning is a type of suffocation induced by the submersion or immersion of the
mouth and nose in a liquid. Drowning can result in death from hypothermia due
to immersion in cold water, sudden cardiac arrest due to cold water, spasm of
the throat blocking the airway and/or inhalation of water and consequent airway
obstruction. You should not endanger your own life in trying to rescue the casualty
from water; if possible use an item that floats to rescue the victim from water. Once
the victim is out of water, turn him or her onto one side, open the airway and let any
water or vomit drain out and if no signs of life immediately start cardiorespiratory
resuscitation. It important to recognize early drowning victim’s distress signs.
The assistance to the drowning victim should be initiated as soon as possible. Note
that the chance for survival decreases as the time goes on. A drowned person
rescued within the first minute has a 95% survival chance, only 25% survival chance
if after 6 minutes, and these drop to only 3% survival chance if after 8 minutes.
The first thing to be done is to Assist the victim to get out of the water by giving
directions. However, as a first aider, you should not endanger your own life in trying
to rescue the casualty from water; if possible, use an item that floats to assist get
the victim to the dry land.
Once the victim is out of water:
• Turn him or her onto one side keeping the victim’s head lower than the rest of
the body to reduce the risk of inhaling water.
• Open the airway and let any water or vomit drain out and if no signs of life
immediately start cardiorespiratory resuscitation (CPR).
• Treat the victim for hypothermia that is remove wet clothes and cover him/her
with dry warm blanket. If the person regains full consciousness, give him/her
a warm drink.
When giving the emergency aid to a drowning casualty you should aim to restore
adequate breathing and keep the casualty warm while seek medical assistance and
or hospital care. Note that any casualty rescued from a drowning incident should
always receive medical attention even if he or she seems to have recovered as any
water entering the lungs causes them to become irritated, and the air passages
may begin to swell several hours later.
Self-assessment 4.2.2
Demonstrate how to position a drowning victim once out of water.
4.2.3 Choking
Learning activity 4.2.3
A group of teen in your village are celebrating their achieving with a steak dinner.
During the meal, one of them suddenly clutched his throat, with severe difficulty
breathing and he was unable to speak.
1) What do you think happened?
2) As a first Aider, attempt to rescue him
Choking is the result of either a totally or
partially obstructed airway caused by swollen
tissues or a foreign body. Food or other material
entering the windpipe instead of the esophagus.
Early recognition and intervention are the key
to successful outcome. Choking should be
distinguished from other conditions that may
cause sudden respiratory distress but require
different treatment such fainting, stroke, heart
attack, seizure, drug overdose, among others.
Signs of chocking range from mild to severe
airway obstruction and these along the age
of the casualty dictate steps emergency aid
interventions.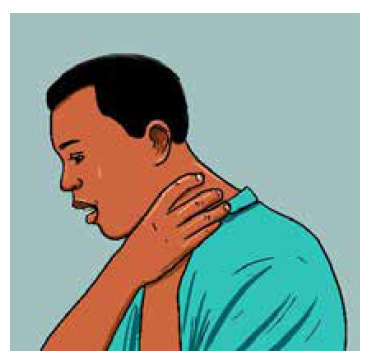
Universal choking sign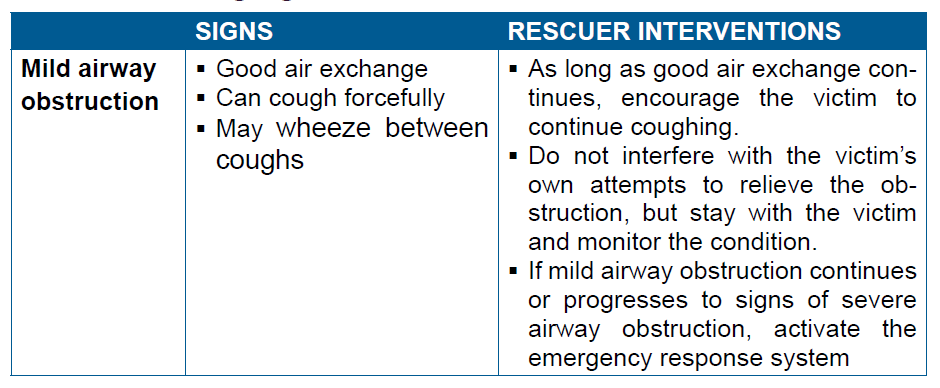

a) Choking relief in a responsive adult or child
Abdominal Thrusts also known as “Heimlich maneuver” is used to relieve choking
in a responsive adult or child. Individual thrust is given with the intention of relieving
the obstruction and it may be necessary to repeat the thrust several times to clear the
airway. This maneuver should not be used to relieve choking in an infant. Moreover,
this maneuver is avoided in pregnant or obese victims where chest thrusts are
performed instead of abdominal thrusts.
b) Choking relief in an unresponsive adult or child
In severe airway obstruction, the victim will be unable to speak, cough, or breathe,
and will eventually lose consciousness. If the rescuer is certain that that the victim’s
condition is caused by a foreign-body airway obstruction the following steps are
undertaken to help the victim.
1) Shout for help. If someone else is available, send that person to activate the
emergency response system.
2) Gently lower the victim to the ground if you see that he is becoming
unresponsive.
3) Begin CPR, starting with chest compressions. Do not check for a pulse.
4) Each time you open the airway to give breaths, open the victim’s mouth
wide. Look for the object.
• If you see an object that can be easily removed, remove it with your
fingers.
• If you do not see an object, continue CPR.
5) After about 5 cycles or 2 minutes of CPR, activate the emergency response
system if someone has not already done so.
Note:
• Sometimes the choking victim may already be unresponsive when you
first encounter him. In this situation you probably will not know that a
foreign-body airway obstruction exists. Activate the emergency response
system and start high-quality CPR.
• If the victim is pregnant or obese, perform chest thrusts instead of
abdominal thrusts
• You can tell if you have successfully removed
an airway obstruction in an unresponsive
victim if you feel air movement and see the chest rise when you give
breaths or see and remove a foreign body from the victim’s mouth
c) Choking relief in infants
Back slaps and chest thrusts are used to relieve choking in responsive infant rather
than abdominal thrusts through the following steps:
1) Kneel or sit with the infant in your lap.
2) If it is easy to do, remove clothing from the infant’s chest.
3) Hold the infant facedown with the head slightly lower than the chest,
resting on your forearm. Support the infant’s head and jaw with your
hand. Take care to avoid compressing the soft tissues of the infant’sthroat. Rest your forearm on your lap or thigh to support the infant.
4) Deliver up to 5 back slaps forcefully
between the infant’s shoulder blades,
using the heel of your hand. Deliver
each slap with sufficient force toattempt to dislodge the foreign body.
5) After delivering up to 5 back slaps, place your free hand on the infant’s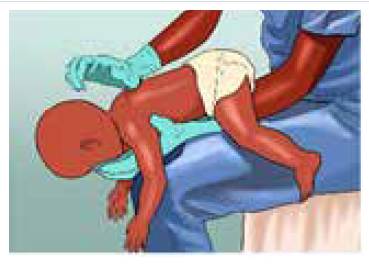
back, supporting the back of the infant’s head with the palm of your
hand. The infant will be adequately cradled between your 2 forearms,
with the palm of one hand supporting the face and jaw while the palm ofthe other hand supports the back of the infant’s head.
6) Turn the infant as a unit while carefully supporting the head and neck.
Hold the infant face-up, with your forearm resting on your thigh. Keep
the infant’s head lower than the trunk.
7) Provide up to 5 quick downward chest
thrusts in the middle of the chest,
over the lower half of the breastbone
(the same location as for chest
compressions during CPR). Deliver
chest thrusts at a rate of about 1 per
second, each with the intention of
creating enough force to dislodge theforeign body.
8) Repeat the sequence of up to 5 back slaps and up to 5 chest thrusts until
the object is removed or the infant becomes unresponsive.
d) Choking Relief in an Unresponsive Infant
If the infant victim becomes unresponsive, stop giving back slaps and begin CPR,
starting with chest compressions. To relieve choking in an unresponsive infant,
implement the following steps:
9) Shout for help. If someone responds, send that person to activate the
emergency response system.
10) Place the infant on a firm, flat surface and begin CPR starting with
compressions with 1 extra step: each time you open the airway, look for the
object in the back of the throat. If you see an object and can easily remove
it, remove it. You should never perform a blind finger sweep in attempt to
remove the foreign body as it may push the foreign body back into the
airway, causing further obstruction and or injury. Note that you do not check
for a pulse before beginning CPR.
11) After about 2 minutes of CPR, if no one has done so, activate the emergencyresponse system.
Self-assessment 4.2.3
1) A nine months old boy was playing with small block toys with his older
sister, and suddenly became unresponsive and his lips turned blue.
a) What do you think happened to the boy?
b) As a first aider on premises, what will you do step by step to help this
kid?
c) What type of choking is the kid suffering from?
2) What are specific considerations for relieving a choking 32 weekspregnant women?
4.2.4 Cardio respiratory distress
Learning activity 4.2.4
1) Observe and describe the pictures ABCD below2) If the victim is not breathing, how can you help him/her?
A distress is an urgent situation in which a person is suffering or is in danger
and therefore in urgent need of help. It requires urgent intervention to prevent
worsening of the situation.
The cardio respiratory distress is relating to the heart, the lungs and the airway
passages and breathing muscles. Severe cardio respiratory distress results in
cardiac arrest which can be witnessed or unwitnessed. Lack of quick interventions
to restart the heart can result in serious complications such as brain damage which
can be irreversible and the death follows in fact timing of intervention is crucial as
the brain may die within 4 to 6 minutes without oxygen.
Cardio Pulmonary Resuscitation (CPR) is the name given to the technique combining
chest compressions, airway management, and rescue breathing aiming to restart
the heart and is indicated when a casualty has no pulse, stops breathing or only
gasping for air and becomes unconscious. To deliver high-quality CPR, you must
begin high-quality chest compressions quickly, as these are considered the most
important factor in giving the person a chance to recover. Compressing the chest
circulates blood to the brain and the heart. High-quality chest compressions are
delivered at a rate between 100 to 120 beats per minute and at a depth between 2
to 2.4 inches (5 to 6 cm) in adult casualty.
Fundamental aspects of an effective CPR include:
• Immediate recognition of respiratory distress and cardiac arrest
• Activation of the emergency response system, getting help and equipment
• Early cardiopulmonary resuscitation (CPR)
• Rapid defibrillation with an automated external defibrillator (AED)a) Steps in CPR
• Place the victim on a hard surface,
often on the ground
• Check for responsivenessstimulate
patient: tap the victim
on the shoulder and ask if he or
she is okay
• Look for the chest to rise and fall,
listen for sounds of air movement
at the mouth and nose, feel for
the breath against your cheek• Shout for nearby help
• Check for pulse and breathing:
this should take no more than 10
seconds to assess for breathing
and check for a pulse. If rescuer
does not definitely feel a carotid
pulse in adults and brachial
pulse in children within that time
period, rescuer should start chestcompressions.
• Open the airway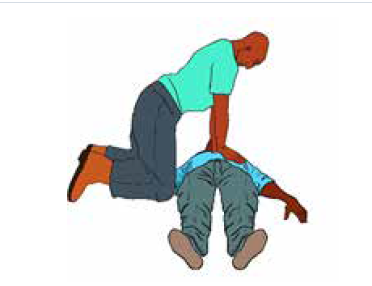
• If no breathing or only gasping
and no pulse, begin cycles of 30
compressions and 2 breaths until
AED is available
• Chest compressions:
• Kneel by the victim’s side
• Place the heel of one hand in the
centre of the victim’s chest.
• Place the heel of your other hand
on top of the first hand and ensure
that pressure is not applied overthe victim’s ribs.
• Do not apply any pressure over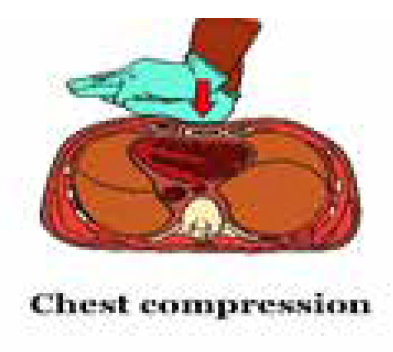
the upper abdomen or the bottom
end of the sternum
• With your arms straight, press
down on the sternum at least 5-6
cm at a rate of at least 100 per
minute (nearly 2 compressions
each second) but no more than120 per minute.
• After each compression, release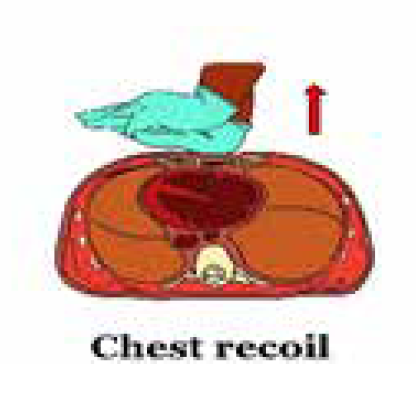
all the pressure on the chest
without losing contact between
your hands and the sternum
to allow chest recoil (chest
compression and chest recoil/
relaxation times should beapproximately equal)
• Minimize frequency and duration of interruptions in compressions.
• Once chest compressions have been started, a trained rescuer should deliver
breaths by bag-mask to provide oxygenation and ventilation at a ratio of 30
compressions: 2 breaths in adults and a rate of 15 compressions: 2 breaths if
2 or more rescuers involved (if 1 rescuer involved a rate of 30 compressions:
2 breaths)
• Managing the Airway:
• Use a head tilt–chin lift maneuver to open airway of a victim with NO
evidence of head or neck trauma.
• Use cervical spine injury is suspect, open airway using a jaw thrust without
neck extension.
• Give breaths using a mask;
however, mouth-to-mouth can also
be performed (Should not be done in
a hospital setting unless you have a
barrier but can be used at home with
family or people you know)
• Use ambubag-valve-mask attached
to oxygen once available:
• Choose the right mask size to
cover the mouth and nose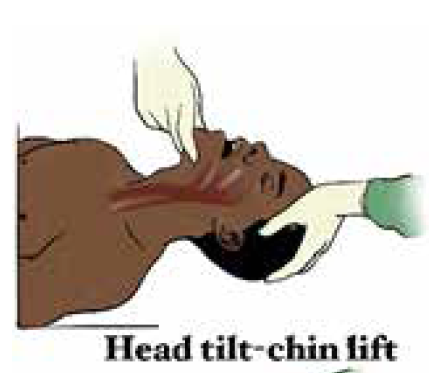
• Give breaths slowly (over one
second)
• Watch for chest rise. Don’t overinflate,
especially infants
• Reposition if no chest rise
• 5 cycles of compressions: breaths
should be done in about 2 minutes
• Check for pulse every 2 minutes
Note:
• Rescuer fatigue may lead to inadequate compression rates or depth. Therefore,
if 2 or more rescuers are available switch chest compressors approximately
every 2 minutes to prevent decreases in quality of compressions. Every effort
should be made to accomplish this switch in 5 seconds
• CPR should continue and can be stopped when rescuers are physically
exhausted or decision to stop is made by a doctor.
• If you can feel the pulse and the victim airways are open and can breathe,
put him/her in recovery position and continue monitoring the victim carefully,
checking regularly the pulse and watching for signs of reduced air passage such
as weak, ineffective cough, a high-pitched wheeze during inhalation, increased
strain during breathing, clutching at the throat slight cyanosis.b) The automated external defibrillator (AED)
An automated external defibrillator (AED) is a small,
lightweight, portable and easy to operate device used
to give an electric shock to restore when the casualty
is having a sudden cardiac arrest. This device once
attached to the victim analyzes the casualty’s heart
rhythm and advise you what action to take at each
stage. Starting CPR immediately and quickly using
an AED improves the chances of survival.
Following are universal steps for operating an AED:
1) Perform CPR until an AED arrives
2) Once AED obtained, turn the power on
3) Expose the victim chest and attach the
adhesive AED pads to the victim’s bare
chest
4) Clear the victim to make sure no one is
touching any part of the victim, let the AED
analyze the rhythm and wait until the AEDtells you what to do

Pads attached
5) Follow the AED advice such as shock
advised, no shock advised, continue CPR,
check connection, etc.
6) If a shock is indicated and other people are
present, warn them to keep clear and ensure
your body is not touching the person:
7) Say, “I’m going to shock on
three. One, I’m clear. Two,you’re clear. Three, everybody’s clear.”
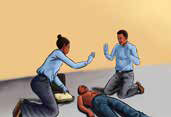
Clear the victim
8) Check to make sure no one is touching the
person or the AED then press the “Shock”
button to give a chock
9) Resume CPR with compressions for 2 min
10) After 2 min of CPR, the AED will prompt you
with further verbal and visual cues
Pads attached
Clear the victim
Note:
• The pads should be placed in a position that maximize current flow through heart(Sternum/apex or Anterior/posterior)
• When no pediatric pads available adult can be used for children > 8 years old or
weighing > 25 Kg
• Ensure that victim is not lying in water and wet areas on victim are dried beforeusing AED
Self-assessment 4.2.4
1) What should be done immediately when you find a person with apnea
before performing a CPR?2) Perform a CPR on model mannequin
4.2.5 Fractures
Learning activity 4.2.5
Observe carefully the figure above and attempt to answer the following questions:
1) What do you understand by fracture?2) Contrast and compare image A and image B
Observe carefully the figure above and attempt to answer the following questions:
1) What do you understand by fracture?
2) Contrast and compare image A and image B
Musculoskeletal injuries are common occurrences and these results into bone
fractures (break or crack in the continuity of the bone), joint dislocation (the bones
are partially or completely pulled out of their normal position), strains and sprains
(injuries to soft structures surrounding bones). All of these injuries results in almost
similar complaints. Use of x-ray is paramount to rule out fractures. Fractures arebroadly classified as either open or closed fractures.
Open fractures – also called “compound fractures”,
are fracture in which there is an open wound or break in
the skin near the site of the broken bone. Involved bone
is exposed at the surface where it breaks the skin but
both sides of the fracture do not need to be visible.
Closed fractures – are fractures in which the skin is
unbroken although the bone ends may damage nearbytissues and blood vessels.
Fractures can become life-threatening if there is severe internal or external bleeding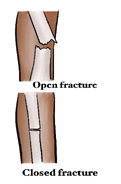
and due to the risk of shock. If organs or major nerves or other structures/systems
are also injured.
Common signs and symptoms of fracture include:
• Deformity, swelling, and bruising at the fracture site
• Pain and or difficulty in moving the area
• Shortening, bending, or twisting of a limb
• Coarse grating (crepitus) of the bone ends that can be heard or felt (by
casualty). Do not try to seek this.
• Signs of shock, especially if femur or pelvis are fractured
• Difficulty in moving a limb normally or at all (for example, inability to walk)
• A wound, possibly with bone ends protruding
First aid interventions in case of fracture should aim at preventing movement at
the injury site (immobilization) and at arranging transportation to the hospital, with
comfortable support during transit.
First aid care for broken bones includes the following:
1) Ensure the scene is safe and wear personal protective equipment.
2) Apply gauze to any open wounds.
3) Do not attempt to push the bone back in (if open fracture) and/or straighten
the extremity
4) Splint the bones in the position you find them in, never attempt to manipulate
or correct an abnormally positioned bone or joint. Splints can be made by
using magazines, wood, or rolled-up towels. Splint material are placed on
either side of the injured extremity, supporting the joints above and below
the injury and secure in place using tape or gauze ensuring they are not
compromising blood circulation. The fingertips or toes in a splinted extremityshould remain warm and pink.
5) Use a triangular arm sling to secure arm and shoulder injuries
6) Move the fractured body part as little as possible or handle gently to prevent
making the fracture worse (e.g. a closed fracture may become an open
fracture) and to lessen the person’s pain.
7) Encourage further evaluation by a health care provider and avoid use of theinjured part
Self-assessment 4.2.5
Referring to Images of learning activity 4.2.5, attempts the following questions:
1.What do you think is the right course of action by the first aider? (Multiple
answers are possible):
a) Try to straighten the limb in image B
b) Avoiding moving the victim
c) Immobilizing the limb in the position he/she found it in by use of tree
branches and clothes holding
d) Pushing back the protruding bone in picture A and apply pressure
dressing to control bleeding
2.Using the knowledge and skills leant previously on bandaging, attempt to
immobilize these fractures
4.2.6 HemorrhagesLearning activity 4.2.6
The body must have enough circulating blood volume to keep the body functioning
and keep the organs supplied with oxygen. Blood is moved around the body under
pressure by the heart and blood vessels. Without adequate blood volume and
pressure, the human body soon collapses. When blood vessels rupture due to a
severe injury, bleeding or hemorrhage, poses a threat. Note that hemorrhage is
a feature of many presentations particularly, but not exclusively, those involving
trauma. It is a loss of blood from damaged blood vessels and it may be internal or
external. The aim of the first aider is to reduce loss of blood from the casualty.
a) External bleeding
External bleeding is usually associated with wounds (cuts, abrasions, amputations,
incisions, lacerations and punctures). Serious wounds involve damage to blood
vessels. External Bleeds can be categorized into three main types with regard totheir origin:
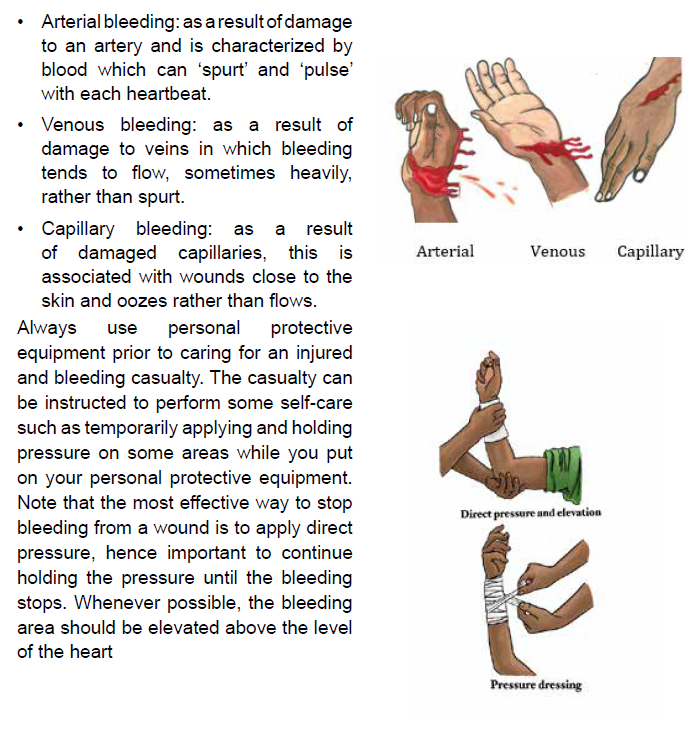
Record the time the tourniquet was applied and stay with the casualty and do not
release tourniquet. Only a medical professional should remove a tourniquet. Help
casualty into a comfortable position, if possible have him/her lying down. If the
casualty becomes unresponsive and not breathing normally follow ABCDE.
Note that blood loss often gets the most attention and many times the amount
of bleeding is overestimated and draws attention to wounds when more serious
injuries should be dealt with first. Therefore, whenever confronted with bleeding,
perform a quick overview of the person to make sure something more serious is notbeing overlooked, the rescuer should be calm and reassuring.
b) Internal bleeding
Always consider internal bleeding after injury, understanding it cannot be controlled
by the first aider. Internal bleeding is classified as either visible (where the bleeding
can be seen) or concealed, (where no direct evidence of bleeding is obvious).
Obtaining an adequate history of the incident or illness will, in most instances,
give the first aid provider the necessary clue as to whether internal bleeding may
be present. You should remember that current signs and symptoms or the lack
of them, do not necessarily indicate the casualty’s condition. Due to the stealth
of bleed, certain critical signs and symptoms may not appear until well after the
incident, becoming apparent despite there being no visible cause, only when the
casualty worsens.
Visible internal bleeding is referred to in this way because the bleeding can be seen
from:
• Ears: Blood or blood mixed with clear fluid.
• Lungs: Frothy, bright red blood coughed up by the casualty.
• Stomach, bowel or intestines: Bright, dark or tarry blood coughed up by the
casualty.
• Under the skin (bruising): The tissues appear dark due to blood under the
skin.
In concealed internal bleeding, detecting internal bleeding relies on good observation
and an appreciation of the physical forces that have affected the casualty. In these
cases, the first aid provider considers the history, signs and symptoms. If you
are unsure, assume the worst and treat for internal bleeding. Consider important
observations that may indicate internal bleeding, which include:
• Rapid, shallow, or irregular breathing
• ‘Guarding’ of the abdomen, with foetal position if lying down
• Pain or discomfort and/or swelling of the abdomen
• Nausea and/or vomiting
• Altered consciousness
• Pale, clammy skin
To help a casualty with an internal bleeding:
• Call emergent help/ambulance
• Wear personnel protective equipment
• If conscious, lie the casualty down on their back with both legs bent at the
knees and if unconscious, in recovery position with both legs bent at the
knees
c) Nosebleeds
Nosebleeds are not usually serious though sometimes they can be quite dramatic
and are often messy. They commonly occur because of dry air or high altitude, an
injury to the nose, or a medication (especially a blood thinner such as warfarin).
Blowing or picking the nose can also cause a nosebleed. People with nosebleeds
often swallow a fair amount of blood, which may result in vomiting. Therefore, be
sure to wear personal protective equipment and eye protection when attending tonosebleeds.
Note: If a severe bleeding is not managed promptly and correctly, it results into a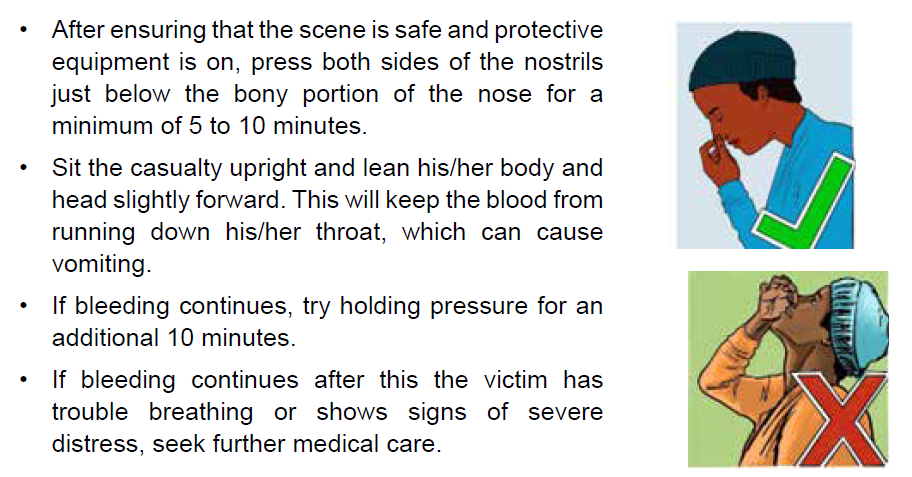
life-threatening condition called “Chock”. Hemorrhagic chock can result either from
severe external bleeding, internal bleeding or both
4.2.7 Loss of consciousnessLearning activity 4.2.7
Loss of consciousness we are referring to is synonymous to “fainting” which is a
common reaction to a variety of conditions. It is the body’s reaction to the decreased
blood flow to the brain that causes the person to pass out. Individuals may faint at
the sight of blood, reaction to pain, exhaustion, hunger or during periods of intense
emotional stress. Fainting also may result from long periods of physical inactivity,
such as standing or sitting still, especially in a warm atmosphere. More serious
conditions, such as an abnormal or erratic heart rhythm, can also cause fainting.
Moreover, severely dehydrated persons may faint when standing up suddenly.
Fainting is characterized by a brief loss of consciousness that causes the casualty
to fall to the ground, a slow pulse and the victim become pale, cold skin and he or
she is sweating.
The rescue a fainted victim aims at improving blood flow to the brain and at
reassuring the casualty and making him or her comfortable. When a casualty feels
faint, advise him/her to lie down. Approach the victim and kneel down, raise his/her
legs, supporting his ankles on your shoulders to improve blood flow to the brain.
Ensure that the casualty has plenty of fresh air; ask someone to open a window
if you are indoors. In addition, ask any bystanders to stand clear. As the casualty
recovers, reassure him/her and help him/her sit up gradually. If he/she starts to feel
faint again, advise him to lie down once again, and raise and support his legs until
he recovers fully.
Self-assessment 4.2.7
1) Enumerate signs and symptoms of fainting
2) Arrange the follow activities done to support a fainting uninjured causality
in a sequential manner using the table below
a) Continue CPR until help arrives or the person begins to breathe
b) To reduce the chance of fainting again, don’t get the person up too quickly.
c) Call our local emergency on 912.
d) Position the person on his or her back.
e) begin CPR,
f) If the person isn’t breathing,
g) Raise the person’s legs above heart level,
h) Check for breathing.
i) If the person doesn’t regain consciousness within one minute,j) Loosen belts, collars or other constrictive clothing.
4.2.8 Snake bites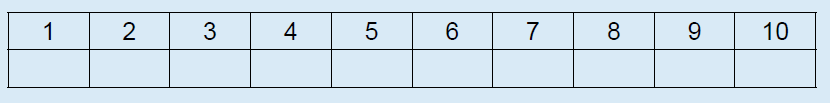
Learning activity 4.2.8
You were camping with your friends and suddenly one of them screamed “I
am pricked by something on my left leg”. Looking around, you saw multicolor
snake leaving your tent. Your friend leg present two puncture marks with parallel
scratches on skin area he felt pricks.
1) What do you think of this situation?
2) What first aid care do think is need to help him?
Many animals can bite or sting. Whereas most such bites and stings are painful,
only a few types can cause sickness, allergic reactions, or death. Poisonous snakes
inject a toxic venom when they strike their victim. It’s difficult to accurately identify
a snake once it has bitten someone, as snakes are similar in shape and have
many different colours, even within the same species. The effects of snake venom
can take up to 2 hours to become apparent, so symptoms are not always obvious
straight away. All snake bites are emergency and must be treated as venomous
until proven otherwise and the bite may be painless and without visible marks.
Do not attempt to kill or capture the snake that bit the casualty. But, if possible, make
a note of the snake’s appearance to help doctors identify the correct antivenom.Take precautions to prevent other people from being bitten.
b) Care and treatment
The first aid principles for treating any kind of snake bite are the same. The main
treatment for snake bite is the application of “Pressure Immobilization Technique”
(PIT).
• Follow DRABCDE and be prepared to perform cardio pulmonary resuscitation
• Ensure the casualty remain as still as possible to slow venom travelling through
the body
• Keep casualty under constant observation and at rest and provide reassurance.
• Apply the pressure immobilization technique (PIT):
1) Have the victim lie down Stay quiet; do not move the bitten part. The more
it is moved, the faster the poison will spread through the body. If the bite is
on the foot, the person should not walk at all.
2) Remove any rings, watches, or bracelets because swelling can spreadrapidly.
Note:
• Keep the limb immobilized until medical assistance arrives
• If only one bandage is available, start just below the bite site and wind as far up
the limb as possible, ensuring to cover the bite site.
• If no bandages, or splints available, improvise with clothing or whatever youcan from the surrounding environment.
• Do not wash the bitten area, as a venom sample may be obtained.
• Do not elevate the limb.
• Do not use an arterial tourniquet.
• Do not remove the bandage once it has been applied, even if casualty is feeling
well as long as there is no compromised blood circulation.
• Do not try to capture or kill the snake.• Do not cut the bite and suck the venom out.
Self-assessment 4.2.8
A 12 years’ kid was passing through a forest to fetch water and sustained snake
bite on the right leg about 2 cm above lateral malleolus
1) Critic and comment on the following bystander emergency aid to this
victim:
a) Used a vascular tourniquet to stop the venom to spread
b) Advised the victim to run fast and leave the forest
c) Took a short clip of the snake that was leaving the scene of incident
d) Reassured the victim
e) Once out the forest, he widened that wound to wash out the venom
2) What would do have done differently?
4.2.9 Epilepsy
Learning activity 4.2.9
You live in place where a family has a kid who experiences seizures several time.
1) The parents of that kid cognizant that you are an associate nurse ask you
this question “what do you think to be the cause of that condition?
2) What would you do when you find this kid in crisis?
Epilepsy is a common cause of seizures. Seizures are a disruption of brain function
that interrupts normal electrical activity of the brain. They consist of involuntary
contractions of many of the muscles in the body. It is only when there’s a tendency
for recurrent and major disturbances of brain activity seizures that epilepsy is
diagnosed.
No matter what the cause of the seizure, care must always include maintaining an
open, clear airway and a monitoring of the casualty’s level of response, breathing,
and pulse. You will also need to protect the casualty from further harm during a
seizure and arrange appropriate aftercare once he or she has recovered.
First aid management DOs in epilepsy include:
• Stay calm and remain with the casualty
• Note the start time and length of the seizure
• Protect the head from impacts
• Remove nearby objects and/or bystanders to protect from harm as cuts,
abrasion, suffocation, burns, and broken bones or teethes…
• Loosen tight clothing
• Follow the casualty’s seizure management plan (if there is one in place)
• When convulsions stop, or if vomiting starts, roll into recovery position and
maintain airway
• Observe and monitor breathing
• Call for an ambulance
• Reassure and let the person rest until fully recovered
First aid management DO NOTs include:
• Do not put anything in the casualty’s mouth
• Do not restrain the casualty
• Do not move the casualty unless they are in danger
Self-assessment 4.2.9
Witnessing a seizure in the street is impressive. How do you react as a first
aider?
End unit assessment 4
1) What does ABCDE stand for?
2) How should you open the airway of an unconscious casualty?
a) Head tilt and chin lift.
b) Jaw thrust.
c) Head tilt and jaw thrust.
d) Lift the chin.
3. What should your first action be when treating an electrical burn?
a) Ensure that the casualty is still breathing.
b) Wash the burn with cold water.
c) Check for danger and ensure that contact with the electrical source is
broken.
d) Check for level of response.
4. What is an open fracture?
a) A fracture in which the bone ends can move around.
b) A fracture in which the bone is exposed as the skin is broken.
c) A fracture which causes complications such as a punctured lung.
d) A fracture in which the bone has bent and split.
5. Which of the first aid duties below has the highest priority for you as a first
aider?
a) Re-assure the victim
b) Arrange medical attention
c) Be aware of the danger
d) Begin CPR
6. You are attending a party in your family and suddenly your 3 years old
nice become unresponsive after brief episode of coughing and crunching
of her throat.
a) What might be the cause of this unresponsiveness status?
b) As a first aider at the premises what steps would you undertake to help
her?
7. On your way while jogging, you find 2 victims involved in road traffic
accident. One of the victim is bleeding a lot on his left leg and his right
arm is broken and you can see forearm bones piercing through the skin.
The second victim, is unresponsive and has contusion on his forehead.
a) What would you do first to rescue these victims?
b) Who among the two victims should be attended to first and why?
c) Stepwise execute steps appropriate for bleeding control
d) Immobilize these fractures
8. What is the first question you must ask before you respond to any first aid
situation?
a) What is the age of the victim?
b) Is the scene safe?
c) What happened?
d) What time did you get hurt?
9. After observing picture B, what do u think is the first action when examining
the condition of a patient?
a) check for breathing
b) Check for airway and c-spine immobilization (if appropriate)
c) Check for insurance
d) Speak to Victim and shake his shoulders
e) Check for external injuries
10. How do you check for breathing referring to picture B?
a) Listen
b) Look for rising chest
c) Feel with the cheekd) Look, Listen and feel
UNIT 5 FIRST AID CARE OF THE SELECTED EMERGENCY CONDITIONS OF SELECTED BODY SYSTEMS
Key unit competence
Apply correctly the techniques of victim’s evacuation and intervention during
emergenciesIntroductory activity 5.0
The above images represent health conditions that require emergency attention.
Observe them carefully and attempt the following questions:
1. Which health conditions do you thinks are portrayed in picture A, B, C and D?
2. Apart health condition adressed in question 1, What would you think more
of picture A and picture D? associate nurse, what could you do to care forpatient in picture D
5.1 Respiratory system pathologies
5.1.1 Brief anatomy and physiology of the respiratory system
The respiratory system is one of the major systems of the body and primarily
consists of two lungs. its main function is to facilitate gas exchange trough ventilation
(the process of breathing) and respiration. Respiration can be expressed in two
ways: internal respiration and external respiration. External respiration refers to
exchange of gases at alveolar/ capillary level, whereby oxygen enters the blood
and carbon dioxide leaves to be excreted through exhalation. Internal respiration
refers to metabolism at cell level where oxygen is combined with carbohydrates to
produce energy; carbon dioxide is a waste product of this metabolic process. Below
is the representation of some respiratory system structures and external respirationphysiology:
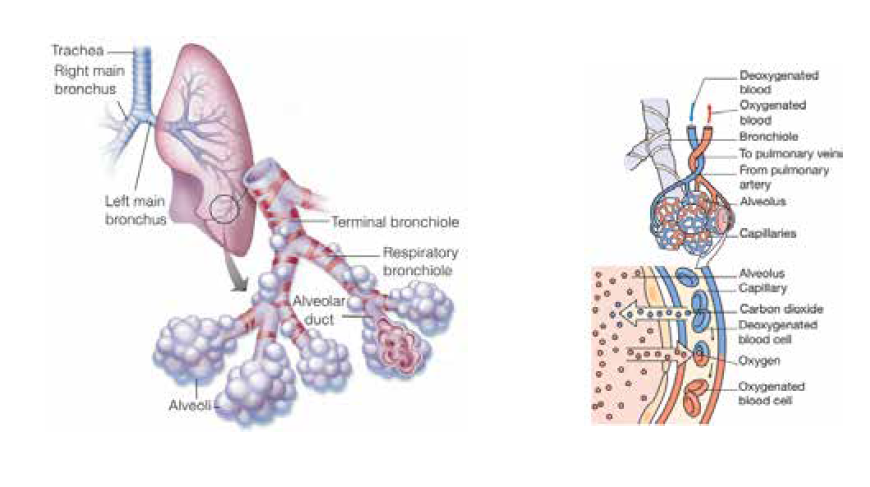
Observe carefully the above pictures and answer the following questions
1) What do you think of piture A
2) What do you think the person in picture B is doing?
Asthma is a chronic inflammatory lung disease that causes airway hyperresponsiveness,
mucus production, and mucosal edema resulting in reversible
airflow obstruction triggering coughing, wheezing and shortness of breath. In fact,
“Asthma” is an ancient Greek word meaning “short breath,” and as the name
implies, it can leave the sufferer gasping for air.
Though, asthma is a common chronic inflammatory condition of the airways, its
course is not completely understood. As a result of inflammation, the airways are
hyper-responsive and they narrow easily in a response to a wide range of stimuli
regarded as precipitating or triggering factors. Allergens, irritants, air pollutants,
pollen, pollution, tobacco smoke, cold weather, physical exertion, strong odors, and
medications are common predisposing factors for asthma. Exercise and stress can
also be an asthma trigger for some.
Pathophysiologically, when a susceptible individual is exposed to a trigger, an
immediate inflammatory response with bronchospasm happens. This inflammation
causes increased responsiveness of the airways to multiple stimuli leading to
recurrent episodes of asthmatic symptoms. The response to an irritant in the
airways causes muscle tightening and narrowing of the lumen and with inflamed
airway lining mucus production increases. This leads to the clinically recognized
symptoms of shortness of breath, wheezing (high pitched whistling) chest tightness,coughing with sputum occasionally.
For some people, asthma is a minor nuisance while for others, it can be a major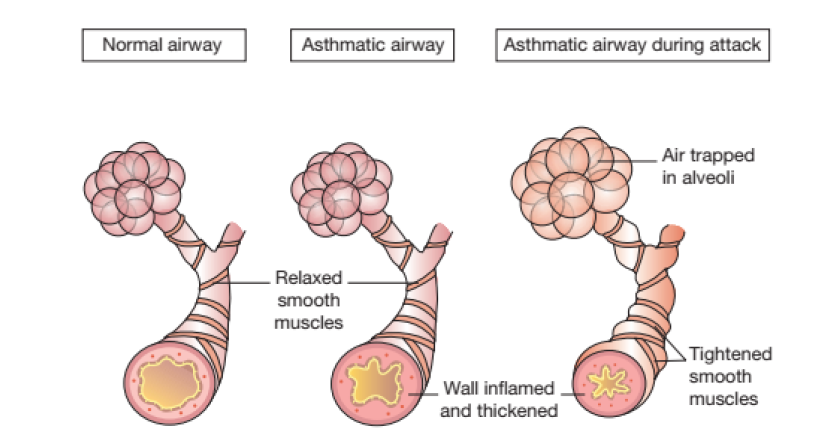
problem that interferes with their daily activities and may lead to a life-threatening
asthma attack. Simply classified, exist mild asthma, moderate asthma and severe
asthma. The below figure illustrates asthmatic events experienced in each severityclass:
Accurate history taking is possibly the most important aspect of patient assessment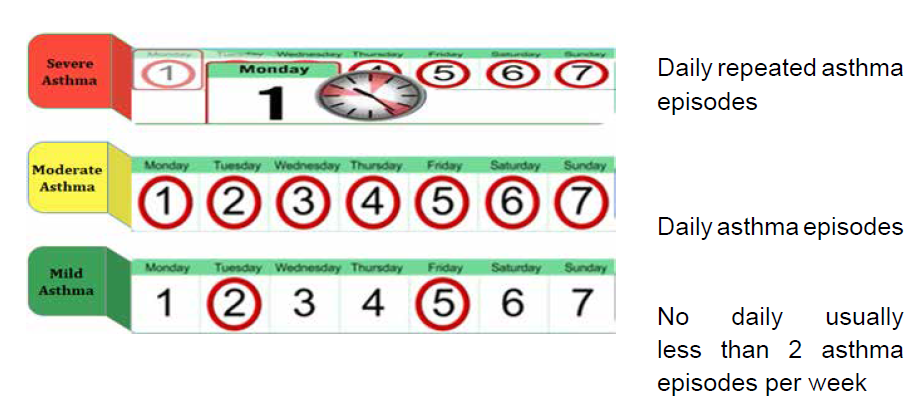
and can provide a great deal of the information required for a diagnosis. Clinical
diagnosis is based on the recognition of a characteristic pattern of symptoms and
signs and the absence of an alternative explanation for them.
The management of asthma consist of both symptoms management and avoiding
triggering factors. The goal of management is for people to be free from symptoms
and able to lead a normal active life. This is achieved partly through treatment,
tailored to the person, and partly by people getting to know what provokes their
symptoms and avoiding these triggers as much as possible. Since asthma is a
chronic condition, people with asthma may require daily medication to keep it
under control. These medications are prescribed and used in a step-wise approach
to prevent and control asthma symptoms, reduce the frequency and severity of
exacerbations, and reverse airway obstruction. However, for all patients, an
inhaled short-acting beta2 agonist (SABA) is recommended for quick relief of acute
symptoms. Strategies for long-term control vary and may need to be modified if a
short-acting bronchodilator is needed more than twice a week.
Inhaled therapy is the mainstay of treatment for people with asthma. Thus, drugs
are delivered directly to the airways where they are needed, work quickly and
effectively. Inhalers allow use of lower doses which is associated with fewer side
effects than with oral drugs. Inhaled therapy requires a delivery device to be able
to hold the drug, and to deliver it to the airway at the required moment. Health care
professionals should be well versed with the correct inhaler technique to effectively
support patient in need.
Three major types of inhalers are used to deliver asthma and chronic obstructive
pulmonary disease (COPD) medications: metered dose inhalers (MDIs), dry
powder inhalers (DPIs), and soft mist inhalers (SMIs). Each type has advantages
and disadvantages. Nevertheless, the two first types of inhalers i.e. metered dose
inhaler (MDI) and dry powder inhaler (DPI) are most common. In an MDI, a chemical
propellant is used to deliver the medication when the canister is depressed. In
contrast, a DPI contains no propellant. Instead, the medication is released by
inhaling rapidly through the mouthpiece. Manufacturers’ instruction leaflets, which
accompany each device, contain useful information about breath-hold, cleaning,
storing and problem solving; and should be read carefully before use and kept forfuture reference if needed.

Observe carefully the above pictures and answer the following questions:
1. What do you think picture A represent?
2. What do you think is happening in picture B
3. What do you think of picture C
5.1.2 First aid interventions in case of asthma attack
An asthma attack also known as an asthma exacerbation is a sudden worsening of
asthma symptoms and lung function caused by the tightening of muscle around your
airways (bronchospasm) leading to distress. This distress can be the presenting
manifestation of asthma or occur in patients with known asthma diagnosis in
response to environmental triggers, to viral upper respiratory infection, lack of
adherence to controller medication or an unknown stimulus.
A distress is an urgent situation in which a person is suffering or in danger and
therefore in urgent need of help to prevent a worsening of the situation. The best
strategy for management of asthma attack is early recognition and intervention
before attacks become severe and potentially life-threatening. Patients with long
standing asthma are generally able to determine when they have an exacerbation.
The assessment should include the onset of symptoms, the likely cause of severity
of symptoms, current medication and response to treatment of previous and riskfactors for asthma related death.
Risk factors for fatal asthma attack include: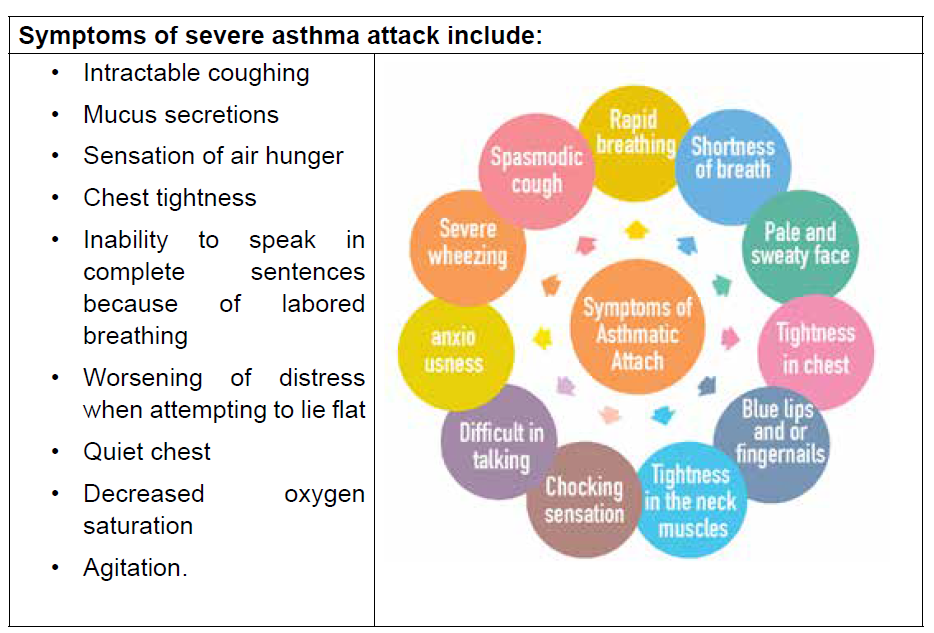
• Previous life-threatening attack requiring intubation or intensive care
admission
• Asthma attack despite current course of oral glucocorticoids
• More than one hospitalization for asthma in the last 12 months
• Use of more than one canister of SABA per month
• Comorbidities such as cardiovascular or chronic lung disease
• Not currently using inhaled glucocorticoids
• Food allergy in patient with asthma
• Three or more visits to emergency department for asthma in the past 12
months
• History of poor adherence to asthma medications and or written asthma plan
• Illicit drug use and major psychosocial problems including depression
• Difficulty perceiving asthma symptoms or severity of attack
First aid
• Sit the person comfortably upright, remain calm and speak calmly to patient
and do not the person alone
• Remove any obvious triggers in immediate patient environment area • Give 4 puffs of reliever inhaler (e.g., Ventolin) and use a spacer if available.
Give 1 puff at a time with 4 breaths after each puff. Use the person’s own
inhaler if possible, otherwise use the one in a first aid kit or borrow one
• Wait for 4 minutes, if the person still cannot breathe normally give more 4
puffs
• If the person still cannot breathe normally Call an ambulance (SAMU – 912)
and say that the person is having an asthma attack. And keep giving reliever
every 4 minutes till the ambulance arrives (4 puffs each time are safe dose for
children; in adults with a severe attack, you can give up to 6 – 8 puffs every
4 minutes)
• Keep monitoring the person and never leave him or her alone
In a healthcare facility setting:
• Start treatment immediately
• Semi-sitting position
• Give O2 to keep saturation above 90%
• Start short acting Beta 2 agonist nebulization (e.g., Salbutamol 5 mg in 5 ml
of normal saline over 10 minutes repeated ½ hour later)
• Hydrocortisone 100 mg IV every 6 hours
• Assess the need of ventilation according to the response to therapy
• Avoidance of the triggering agent if known
Note:
Close friends and family members of an asthmatic person should be aware of
how to manage an individual who is having an asthma attack, thus, paramount toeducate them on this.
6) Secure a good seal with the lips around the mouthpiece of the spacer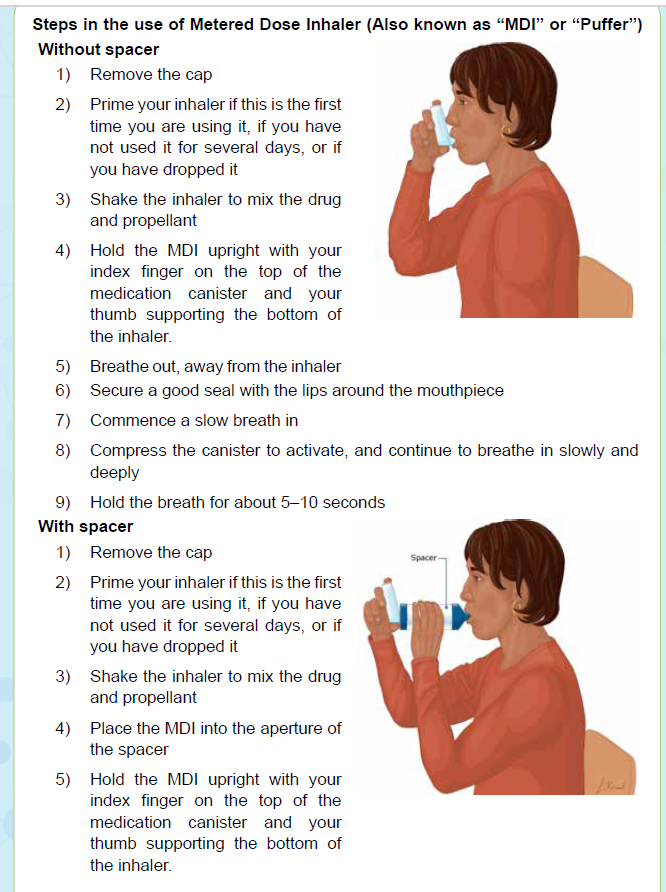
7) Compress the canister to activate, and continue to breathe in slowly and
deeply
8) Take four or five deep breaths
Note:
• The use of a spacer with an MDI is recommended to increase lung deposition
and reduce risks of failing to synchronize inhalation and activation of the
MDI. In fact, large volume spacers have been shown to be comparable to a
nebulizer in an emergency
• If your inhaler contains a steroid medicine, rinse the mouth (gargle with water
after you use and then spit out the water)Steps in use of capsule dry powder
1) Remove a capsule from the foil blister packaging, observing the
manufacturer’s instructions
2) Open the inhaler, and place the capsule inside the chamber
3) Close the inhaler
4) Pierce the capsule by squeezing the button on the side of the inhaler
5) Secure a good seal with the lips around the mouthpiece
6) Inhale as hard as possible
7) Hold the breath for 5–10 seconds
8) If any powder is left, repeat steps 5–6.
Self-assessment 5.1.2
1) Which of the following best describes asthma?
a. Intermittent airway inflammation with occasional bronchospasm
b. A disease of bronchospasm that leads to airway inflammation
c. Chronic airway inflammation with superimposed bronchospasm
d. Relatively fixed airway constriction
2. What first aid interventions should be done for a person with asthma
attack?5.1.3 Acute Respiratory distress (ARD)
Observe the above picture and answer the following question:
1. To you, what image A represent?
2. What do you think image B tries to portray?
3. What do you think is being done in image C?4. Attempt to establish, if any, relationships across the above images
5.1.3.1 Overview of acute respiratory distress (ASD)
a) Definition
Acute respiratory distress (ARD) is a severe lung condition that occurs when fluid
builds up in the tiny, elastic air sacs (alveoli) in the lungs. This fluid keeps the lungs
from filling with enough air, which means less oxygen reaches to the bloodstream.
Too much fluid in the lungs can lower the amount of oxygen or increase the amount
of carbon dioxide in the bloodstream. ARD can prevent the organs from getting the
oxygen they need to function, and it can eventually cause organ failure.
b) Etiology and pathophysiology
Although the exact cause of ARDS is unclear, it is known that ARDS does not occur as a
primary process but may follow a number of diverse conditions producing direct or indirect
lung injury. Direct injuries are those in which the lung epithelium sustains a direct
insult. Indirect injuries are those in which the insult occurs elsewhere in the body
and mediators are transmitted via the bloodstream to the lungs.
• Direct injuries include: aspiration, pneumonia, fat embolism, near drowning,
oxygen toxicity, pulmonary contusion, and toxic inhalation.
• Indirect injuries include: severe and widespread bacterial infection in the
body (sepsis), severe injury to the body that causes low blood pressure (shock),
excessive blood transfusions, anaphylaxis, disseminated intravascular
coagulation, and acute pancreatitis, drug overdose, embolism and long bone
or pelvic fractures.
The injuries result in an inflammatory reaction. This releases body chemicals into the
bloodstream. Typically, this reaction would protect the body and help fight infection
or heal from an injury. However, in some people these inflammatory chemicals will
cause the smallest blood vessels in the lungs to leak fluid. Fluid leaves these small
vessels and goes into the tiny air sacs in our lungs, called alveoli causing a noncardiogenic
pulmonary edema. Pulmonary edema interferes with allowing carbon
dioxide to be excreted (hypercarbia) and oxygen to be absorbed (hypoxemia).
Increased capillary pressure can cause pulmonary hypertension leading toatelectasis and a reduction in functioning lung volumes.
c) Signs and symptoms
Initial manifestations of ARDS typically develop 24 to 48 hours after the initial insult
and they vary depending on its cause and severity, as well as the presence of
underlying cardiorespiratory comorbidity. Dyspnea, tachypnea and anxiety are
early manifestations.
Common clinical manifestation of ARDS include:
• Acute onset of severe dyspnea, tachypnea, tachycardia, intercostal retractions
and use of accessory muscles, cyanosis.
• Increasing requirements of oxygen therapy. Hypoxemia refractory to
supplemental oxygen therapy.
• Scattered crackles and rhonchi heard on auscultation.
• Decreased pulmonary compliance, evidenced by increasing pressure required
to ventilate patient on mechanical ventilator
• As respiratory failure progresses, mental status changes such as agitation,
confusion and lethargy occur.
The diagnosis of ARDS is based on clinical, hemodynamic, and oxygen criteria.
The hallmark signs for ARDS include acute-onset, severe hypoxemia, despite
increasing oxygen therapy, and chest x-ray exhibiting bilateral infiltrates.
d) Treatment
Recognizing and promptly treating ARDS is critical to reduce the associated high
mortality. The treatment aims at maximizing clinical stability and managing symptoms
while treating the underlying cause as if this is not treated the ARDS will not resolve.
Thus, Current ARDS treatment is primarily supportive. Supportive measures assist
the patient while the underlying cause is being treated. Mechanical ventilation is
nearly always required to decrease work of breathing and improve oxygenation.
Fluid management must be maintained. The patient may be hypovolemic because
of the movement of fluid into the interstitium of the lung. Along medications to treatthe underlying cause, adequate nutrition should be initiated early and maintained.
Self-assessment 5.1.3
1) Acute respiratory distress (ARD) is defined as:
a) Acute respiratory distress syndrome occurs due to the collapsing of a
lung because air has accumulated in the pleural space
b) A conditions which causes the alveolar capillary membrane to leaks fluid
into the alveolar Sac
c) ARDS is a pulmonary disease that gradually causes chronic obstruction
of airflow from the lungs
2) Which patient below is at most risk for developing ARD:
a) A 50 years old patient with pneumothorax
b) A 49 years old patient with diabetes
c) A 70 female patient with sepsis caused by bacterial infection
3) As an associate nurse you know that ARD can be caused by direct or
indirect lung injury. Choose below all indirect causes of ARD
a) Drowning
b) Aspiration
c) Sepsis
d) Blood transfusion
e) Pneumoniaf) Pancreatitis
5.1.3.2 First aid in difficult breathing due to ARD
Learning activity 5.1.3.2
While you are traveling in the village you meet with a male person with breathing
faster a fast heartbeat, extreme tiredness, coughing that produces phlegm
and fainting. As first aider. Which position are you going to give him, make him
comfortable?
The primary goal of first aid is to ensure that a person has enough oxygen to
prevent organ failure. If person is having breathing difficulty, immediately call for
help (SAMU – 912) then:
• Position the patient in prone position - Prone positioning is widely used to
improve oxygenation of patients with acute respiratory distress syndrome
(ARDS)
• Check the person’s airway, breathing, and pulse. If necessary, begin CPR.
• Loosen any tight clothing.
• Help the person to use any prescribed medication (such as an asthma inhaler
or home oxygen) if he/she has
• Continue to monitor the persons breathing and pulse until medical help
arrives.
• Do NOT assume that the person’s condition is improving; if you can no longer
hear abnormal breath sounds, such as wheezing.
• If there are open wounds in the neck or chest, they must be closed immediately,
especially if air bubbles appear in the wound. Bandage should be performed
on such wounds at once. A “sucking” chest wound allows air to enter the
person’s chest cavity with each breath. This can cause a lung collapse.
Bandaging the wound with gauze pads allows trapped air to escape from the
chest, but it prevents air from entering the chest through the wound.
• Do NOT give the person food or drink.
• Do NOT move the person if there has been a chest or airway injury, unless it
is absolutely necessary.
• Do NOT place a pillow under the person’s head as this can close the airway.
• Do NOT wait to see if the person’s condition improves before getting medicalhelp. Call for help immediately
Self-assessment 5.1.3
1) You are caring a patient with ARD, as an associate nurse which position
is beneficial for this patient
a) Lateral position
b) Prone position
c) Spine position
2) How can you help someone with ARD out of health facility?
5.2 Cardiovascular system pathologies
5.2.1 Brief review on blood pressure physiology and bloodpressure measuring
a) Definition and classification of blood pressure (BP)
Blood pressure (BP) is the force exerted by the blood against the walls of the
blood vessel and must be adequate for tissue perfusion to be maintained during
activity and rest. It is traditionally measured by use of auscultation with a mercurytube
sphygmomanometer, measured in millimeters of mercury and expressed in
terms of systolic pressure (SBP) over diastolic pressure (DBP). SBP is the highest
arterial pressure when the heart contracts and empties. DBP is the lowest arterial
pressure when the heart relaxes to fill with blood. BP is one of the most commonly
measured clinical parameters and blood pressure values are major determinants of
therapeutic decisions.
In healthy adults the average systolic pressure is less than 120 mmHg and the
average diastolic pressure is less than 80 mmHg. The difference between the
systolic and diastolic pressure, known as the pulse pressure and reflects stroke
volume, ejection velocity, and systemic resistance and is a noninvasive indicator
of CO (normally ranging between 30 to 40 mm Hg, if less than 30 mm Hg indicate
decreased CO). The mean arterial pressure (MAP) is the average pressure in the
arterial circulation throughout the cardiac cycle, and it can be calculated using the
formula (systolic BP + diastolic BP + diastolic BP)/3. Diastole counts twice as much
as the systole because two-thirds of the cardiac cycle is spent in diastole. The tablebelow attempt to classify BP measurements with emphasis on hypertension.
b) Factors affecting the blood pressure
The BP is primarily a function of cardiac output (CO) which is the volume of blood
ejected from the heart per minute and systemic vascular resistance (SVR) that is
the force opposing the movement of blood within the blood vessels. Thus, factors
that influence any of these influence the BP. Factors that influence the BP arerepresented in the following figure:
A certain amount of pressure within the circulatory system is necessary to maintain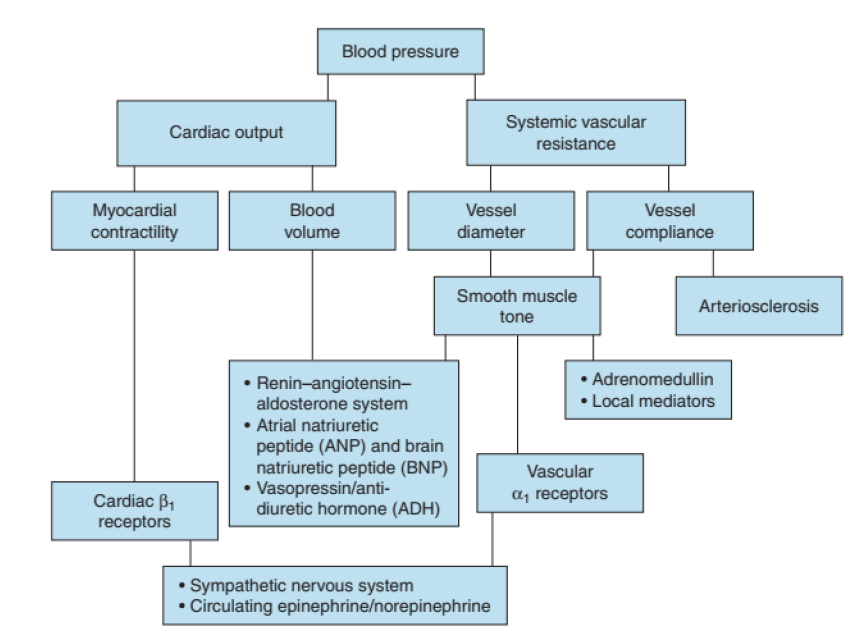
open vessels, capillary perfusion and oxygenation of all body tissues. The
predominant mechanisms of blood pressure control are the central nervous system
(CNS), the renin-angiotensin-aldosterone system, and extracellular fluid volume.c) Blood pressure measurement
Note: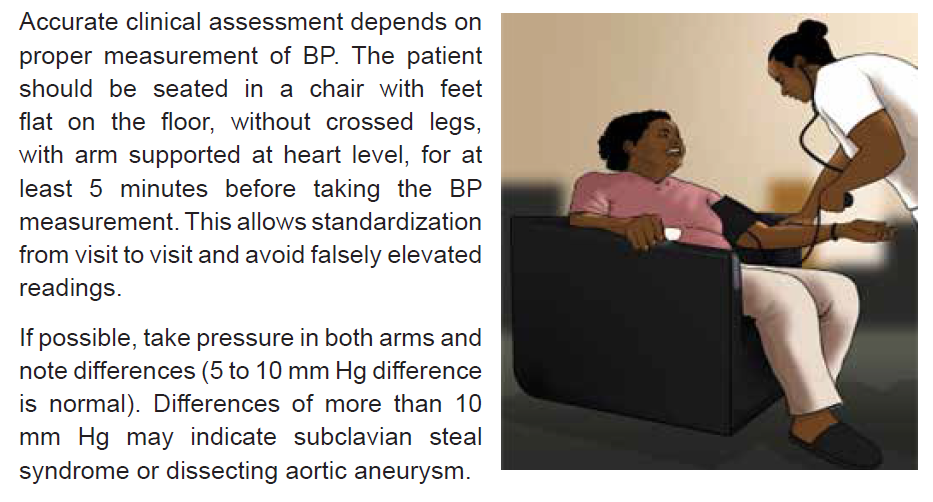
• Some patients may have elevated BP readings in a clinical setting and normal
readings when BP is measured elsewhere. This phenomenon is referred to
us, as “white coat” hypertension”.
• Some other patients have normal BP when in clinical setting and elevated BP
at home. This phenomenon is referred us, as “masked hypertension”.
• Naturally, both systolic and diastolic BP tend to move together (i.e. climb of
fall together). However, that is not always the case as isolated rise or fall of
systolic or diastolic readings exist; e.g. isolated systolic hypertension, isolateddiastolic hypertension.

5.2.2.Hypertensive Crisis

5.2.3.1 Brief review of hypertension
Hypertension is a disease of vascular regulation in which the mechanisms that
control arterial pressure within the normal range are altered characterized by a
persistently elevated systemic blood pressure. Thus, hypertension is consistent
blood pressure readings of ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic, based
on the average of three or more readings taken on separate occasions. While it
rarely causes symptoms or noticeably limits the person’s functional health patterns,
hypertension is a major risk factor for coronary heart disease, heart failure, stroke
and kidney failure.
Its cause is not identifiable in 90% of all of hypertension; this types of hypertension
is referred to us as “Essential or Primary Hypertension” while in the remaining 10%
exist an identifiable cause referred to us as “Secondary of hypertension”. A number
of risk factors have been identified for primary hypertension. Both genetics and
environmental factors play a role in the development of hypertension. Family history,
age, Genetic factors and race are non-modifiable factors linked to hypertension.
More others factors such as high sodium intake; low potassium, calcium and
magnesium intake; obesity; excess alcohol consumption and insulin resistance are
regarded to be modifiable factors linked to hypertension.
5.2.3.2 Definition and classification of hypertensive crisis
Hypertensive crisis is a severe and potentially life-threatening increase in blood
pressure therefore a medical emergency, defined as systolic blood pressure ≥
180mmHg and or diastolic blood pressure ≥ 120mmHg.
As a result of this severe increase in BP, the blood vessels and organs may
become damaged. Therefore, hypertensive crises can be divided into hypertensive
emergencies or hypertensive urgencies according to the presence or absence
of acute target organ damage, respectively. Hypertensive emergencies include
hypertensive encephalopathy, intracranial or subarachnoid hemorrhage, acute left
ventricular failure with pulmonary edema, heart attack, renal failure, dissecting
aortic aneurysm and eclampsia (during pregnancy).
This differentiation is an extremely useful classification in clinical practice since
a different management is needed, which in turn has a significant effect on the
morbidity and mortality of these patients.
5.2.3.3 Signs and symptoms
Hypertensive crisis is characterized by rapid onset of systolic pressure higher than
180 mmHg and or diastolic pressure higher than 120 mmHg often associated with
headache, blurred vision, papilloedema, nausea, vomiting, seizures, stupor and
altered mental status. Moreover, there may be typical signs and symptoms related
to resultant target organ damage.
• Brain effects:
• Signs and symptoms of encephalopathy (probably as a result of cerebral
edema and spasms of cerebral vessels)
• Signs and symptoms of stroke
• Progressive headache, stupor and seizures
• Kidney effects:
• Signs and symptoms of decreased blood flow and vasoconstriction
• Signs and symptoms of elevated blood urea nitrogen (BUN)
• Signs and symptoms of increased plasma renin activity
• Lowered urine-specific gravity
• Proteinuria
• Signs and symptoms of renal failure
• Cardiac effects:
• Signs and symptoms of left-sided heart failure
• Signs and symptoms of acute myocardial infarction (MI)
• Signs and symptoms of right-sided heart failure.
5.2.3.4 Management of hypertensive crisis
Hypertensive crisis requires an immediate medical attention and its treatment may
involve hospitalization and the use of oral and/or intravenous medications after
thorough assessment and classification. The goal of care is to reduce the blood
pressure by no more than 25% within minutes to 1 hour, then towards 160/100 within
2 to 6 hours. It is important to avoid rapid or excessive blood pressure decreases
that may lead to renal, cerebral or cardiac ischaemia. Blood pressure is monitored
frequently (every 5 to 30 minutes) during a hypertensive emergency. The serum
urea, creatinine, calcium and total protein levels are carefully.
Immediate interventions to be implemented when hypertensive crisis is suspected
include
• Assess BP in both arms
• Elevate the head of the bed to approximately 30 - 450
• Administer supplemental O2
• Notify the physician
• Perform a focus assessment to assess and document level of conscience,
respiratory status, neurological deficits, baseline vital signs including oxygen
saturation (if possible), note any visual disturbance, chest pain, peripheral
edema and hematuria
• Keep close monitoring including assessing changes in cardiac rhythm if
patient is on a monitor and in and out
• Anticipate and prepare to get ready to implement physician orders such as
obtain an IV access, order laboratory tests (BUN, creatinine, electrolytes,administering medications and transferring the patient to intensive care unit.
Self-assessment 5.2.2
1) What is an essential hypertension?
2) Define and classify hypertensive crisis events
3) Should we aim at obtaining normal BP reading values when treatinghypertensive crisis? Explain your answer
5.2.3.First aid for acute hypotension
Observe the images and attempt to figure-out what is happening:
1) What do you think of picture A?2) What does image B represent and shows?
5.2.3.1 Overview of hypotension
a) Definition
Hypotension is a decrease in systemic blood pressure below normal value i.e.,
a systolic pressure below 90mmHg and a diastolic below 60mmHg. It is a
relatively benign condition that is under-recognized mainly because it is typically
asymptomatic. However, it can be a sign of underlying condition especially in
elderly. Hypotension a concern once pumping pressure is so low to perfuse key
organs with oxygenated blood.
b) Types of hypotension
There are several types of hypotension. Low blood pressure is categorized
according to when it happens and what’s causing it.
• Orthostatic or postural hypotension – is the drop in blood pressure that
occurs when you move from sitting or lying down to standing. As the body
adjusts to the position change, someone may feel dizzy or lightheaded. This
is what some people refer to as “seeing stars” when they get up. Being the
most common form of hypotension, it can affect people of all ages, but it’s
especially common in older adults. Other reasons associated to hypotension
include pregnancy, dehydration, exhaustion, strong emotions and medication
(e.g., taking anti-hypertensive drugs or drugs that have hypotension as a side
effect. Conditions affecting the autonomic nervous system, such as Parkinson’s
disease and diabetes, can often lead to orthostatic hypotension.
• Postprandial hypotension - is a drop in blood pressure that occurs after
eating. It is more common in older adults and people with autonomic
dysfunction.
• Neutrally mediated hypotension - happens when there is an abnormal
reflex interaction between the heart and the brain. People with this disorder
feel faint, dizzy, and nauseous after exercising or standing for a long time.
Children experience this form of hypotension more often than adults as
result of standing in one position for a long time. Having a strong emotional
response, such as feeling shocked or scared also can result into this type of
hypotension in some people
• Severe hypotension - this type of hypotension is linked to shock. During
shock the BP drops to dangerously low levels, and the brain and organs can’t
get enough blood to function properly therefore life threatening if not treated
quickly. Shock can happen as a result of:
• Decreased effective circulating volume (hypovolemic shock)
• Impaired cardiac output due to heart pump dysfunction or obstruction to
cardiac filling (cardiogenic shock)
• Impaired peripheral i.e., loss of vascular tone (distributive shock)
c) Signs and symptoms of hypotension
The patient present with systolic pressure that is below 90mmHg or systolic BP 40
mm Hg less than baseline. Depending on how low the blood pressure is the patient
may have an altered level of consciousness; cool, pale, cyanotic, diaphoretic skin;
nausea and vomiting; shortness of breath; dizziness, blurry vision, weakness and
decreased urine output.
Immediate interventions
Using DRSABCD approach:
• Place patient in a supine position with head of the bed slightly elevated if
compromised airway
• Assess level of conscious, orientation, baseline vital signs with emphasis
on pulse quality and rhythm. Assess skin for color, temperature, moistness,
turgor, and capillary refill
• Call for medical assistance indicating patient’s status,
• Administer oxygen if inadequate respiratory effort
• Control any bleeding with direct pressure
• Obtain an IV access and give IV fluids if appropriate (hypotension may be due to
cardiac compromise, in which case fluids might be contraindicated
• Definitive management is established once the cause is identified (use
of clinical and para-clinical data). Depending of severity, this may include
administration of vasoactive medications and transfer of patient to a criticalcare unit.
Self-assessment 5.2.3
Which of the following statements concerning postural hypotension in the elderly
is false?
1) It increases the risk of falls and syncope
a) It is characterized by a drop in blood pressure when going from a standing
to a sitting position
b) It increases the risk of cardiovascular events
c) It is associated with the use of vasodilating medications
2) List four types of hypotension
3) What are the main mechanisms behind severe hypotension also knownas shock?
5.2.4 Heart Attack
Observe the above pictures and attempr to describe what you see and establish
any association or similarity if any
A. Overview of coronary artery disease
a) Introduction
The heart as a muscular pump responsible for moving blood throughout the body.
It needs an excellent blood supply to provide enough blood, oxygen and nutrients
to keep its pumping function effective. This is accomplished through coronary
circulation. With diseased coronary arteries, the supply of blood, oxygen and
nutrients to the heart is compromised which may lead to reversible or irreversible
injury to heart structures.
b) Review of vascularization anatomy of the heart
The heart structures are supply with oxygen rich blood by coronary arteries and
then the deoxygenated blood return into the general circulation through coronary
veins. The right and left coronary arteries arise at the base of the aorta, immediatelyabove the aortic valve.
They supply a discrete area of the myocardium and have limited collateral circulation
and are susceptible to obstruction by atherosclerotic plaque or thrombus that can
result in loss of blood flow to the myocardial muscle normally supplied by that
artery. This can be fatal, depending on the location of the obstruction. Blockage
of coronary arterial blood flow, especially in the left main coronary artery, usually
results in death from massive infarction of the left ventricle. However, if the blocked
artery supplies a smaller section of myocardium this may result not death.
c) Pathophysiology and classification of coronary artery diseases
The term of coronary artery disease (CAD) is a broad term used to refer to the
narrowing or occlusion of the coronary arteries. Pathophysiologically coronary
atherosclerosis (plaque buildup within the layers of the coronary arteries) is the
most common cause of CAD. The plaques progressively enlarge, thicken, and
calcify, causing a critical of the coronary artery lumen, resulting in a decrease in
coronary blood flow and an inadequate supply of oxygen to the heart muscle. The
term of “ischemic heart disease (IHD)” is used to indicate a condition in which there
is an inadequate supply of blood and oxygen to a portion of the myocardium.
Coronary heart diseases may be asymptomatic or symptomatic and are generally
divided into two categories:
• Chronic ischemic heart disease – this category includes stable and unstable
angina and silent myocardial ischemia.
• Acute coronary syndromes – this category ranges from unstable angina tomyocardial infarction (MI).

Pathophysiologic representation of ischemic heart diseases
Both modifiable and non-modifiable factors promote the occurrence of the disease
in genetically susceptible persons. Non-modifiable factors include age, gender,
race and family history. Modifiable factors include high level serum cholesterol,
smoking habits, obesity, diabetes, sedentary lifestyle and hypertension.
d) General manifestation of coronary artery disease
The cardinal manifestation is chest pain, characterized as either pressure,
heaviness, squeezing, choking, strangling, and/or cramping pain or discomfort.
This pain is usually localized behind middle or upper third of the sternum and the
patient will generally make a fist over the site of the pain rather than point to it with
his or her finger. It usually radiates to the neck, jaw, shoulders, arms, hands, and
posterior intrascapular area. Its duration depends on how severe the myocardium
is affected.
The OLDCART acronym can be used to adequately assess this chest pain. That
is Onset, Location, Duration, Characteristics, Aggravating symptoms, methods to
Relieve the pain, current Treatment. For instance, in chronic stable angina such
pain is associated with a specific level of physical or emotional stress and reliably
resolves with rest, relief of the stress, or nitroglycerin therapy and this last for less
than 10 minutes while for unstable one, this last usually for 10 – 20 minutes.
Associated symptoms may include diaphoresis, nausea, indigestion, dyspnea,
tachycardia, and increase in blood pressure.
e) Diagnosis and management of coronary artery disease
Laboratory tests may confirm the presence of risk factors, such as an abnormal blood
lipid profile and elevated blood glucose. Other common diagnostic tests to assess
for coronary heart disease include electrocardiography, stress testing, nuclear
medicine studies, echocardiography (ultrasound) and coronary angiography.
Drugs may be used for both acute and long-term relief CAD. The goal of drug
treatment is to reduce oxygen demand and increase oxygen supply to the
myocardium. Three main classes of drugs are used to treat angina: nitrates, betablockersand calcium channel blockers.
Self-assessment 5.2.4
1) What causes the pain that occurs with myocardial ischemia?
a) Death of myocardial tissue
b) Dysrhythmias caused by cellular irritability
c) Lactic acid accumulation during anaerobic metabolism
d) Increased pressure in the ventricles and pulmonary vessels
2) What are modifiable risk factor for CAD?3) How would you ascertain the chest pain is of CAD origin?
5.2.5. First aid intervention for heart attack
Observe the above images and attempt to answer the following questions: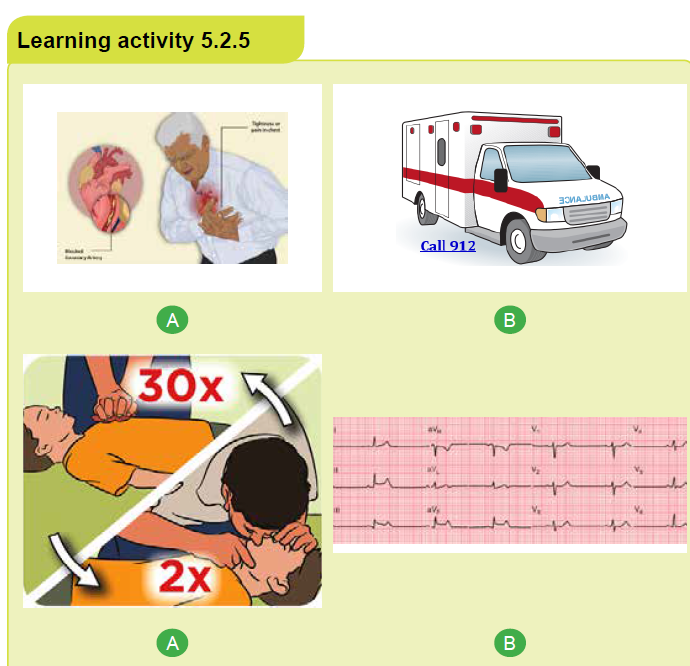
1) What do you think of image A?
2) What image B represent according to you?
3) What do you think is happening in image C?4) What do you think image D represent?
a) Introduction
Heart attack also known as Myocardial Infarction (MI) is one of the manifestations
of acute coronary syndrome (ACS) and is a life-threatening event. It refers to a
dynamic process by which one or more regions of the heart experience a prolonged
decrease or cessation in oxygen supply because of insufficient coronary blood flow
with subsequent necrosis or “death” to the affected myocardial tissue. If circulation
to the affected myocardium is not promptly restored, loss of functional myocardium
affects the heart’s ability to maintain an effective cardiac output. This may ultimately
lead to cardiogenic shock and death.
b) Brief heart attack pathophysiology
Most MIs occur as a result of coronary artery atherosclerosis, followed by rupture
of an unstable atheromatous plaque, platelet activation, and fibrin clot formation.
The resultant thrombosis interrupts blood flow and leads to an imbalance betweenmyocardial oxygen supply and demand and eventually myocardial tissue necrosis.

A: Damaged endothelium B: Fatty streak and lipid core formation C: Fibrous
plaque D: Complicated lesion
Non-atherosclerotic causes of MI include coronary artery spasm, congenital
abnormalities, coronary artery embolus, and connective tissue disorders.
c) Manifestations of Myocardial Infarction(MI)
Chest pain is the cardinal feature of MI, even though it is not universally present.
It is of the same character as angina pectoris; described as heavy, squeezing, or
crushing and is localized to the retrosternal area or epigastrium, sometimes with
radiation to the shoulder, arm, lower jaw, or neck. However, in contrast to stable
angina, however, it is more severe and persists for more than 20 minutes and is not
relieved by rest or Nitroglycerine.
Its onset is sudden and usually is not associated with activity. In fact, most MIs
occur in the early morning. The pain often is accompanied by sweating, nausea,
vomiting, and/or the sense of impending doom. People with a history of angina may
have more frequent anginal attacks in the days or weeks prior to an MI.
d) Immediate interventions
Early recognition and intervention is key for patient survival.
d.1. Prehospital first aid
Any heart attack might lead to cardiac arrest, but prompt action may prevent further
damage to the heart. A person suffering from a heart attack has a far better chance
of living than does a person whose heart has stopped. Therefore, the most important
first aid measure is to be able to recognize the signals of a heart attack and take
appropriate action promptly.
A person having a heart attack may deny the seriousness of the signals he or
she is experiencing, or believe the signals are just muscle soreness, indigestion
or heartburn. Therefore, do not let this denial influence you. If you think that the
person might be having a heart attack, you must act.
Though CPR is often what comes to mind when people think of first aid for a heart
attack or cardiac arrest, this is only part of a broader picture of what is needed for
the victim survival. There are five steps that are important when helping someone
with heart problems.
1) Early recognition and activation of emergency medical services system
such as SAMU Call 912).
2) Early CPR with an emphasis on chest compressions.
3) Early defibrillation.
4) Effective advanced life support.
5) Integrated post-cardiac arrest care.
Note: Each of these steps is as important as the others and time is a vital ingredient.
The following are important intervention steps for first aid:
a) Perform a scene survey, then do a primary survey to ascertain the acute
coronary syndrome (consider signs and symptom above by use of OLDCART
acronym).
b) Call for medical help (e.g., Call SAMU - 912) and get a defibrillator and
importantly ensure the emergency department is informed of heart attack.
c) Have the person stop what he or she is doing and rest comfortably. This will
ease the heart’s need for oxygen and many people find it easier to breathe
while sitting.
d) Loosen any restrictive or uncomfortable clothing
e) Ask the person if he or she has a history of heart disease. Some people who
have heart disease take prescribed medications for chest pain and you can
assist them taking them (e.g., sublingual Nitroglycerin)
f) Offer aspirin, if not contraindicated to lessen heart attack damage as Aspirin
acts to thin the blood and prevent further clot formation. A dose of 165 - 300
mg dose of Aspirin to be chewed by the victim
g) I feasible:
• Give oxygen if oxygen saturation is <90% or if the patient is short of breath
• Start IV fluids
• Give morphine as indicated e.g., 2 – 5mg if the pain not relieved by
Nitroglycerin
h) Monitor the person closely until emergency medical services personnel arrive.
Note any changes in the person’s appearance (i.e., loss of consciousness) or
behavior and record as well interventions undertaken.
i) Be prepared to perform CPR and use an AED if the person loses consciousness
and stops breathing.
j) Keep a calm and reassuring manner as comforting the person helps reduce
anxiety and ease some of the discomfort
d.2. Intra-hospital care at emergency department (ED)
Once arrived to the hospital, an immediate ED assessment and treatment should
be initiated.
• The assessment should include a brief targeted history and physical
examination; fibrinolytic checklist, especially contraindications
• Keep vital signs and O2 saturation monitoring
• Obtain IV access if not done
• Continue MONA (morphine, oxygen, nitroglycerin, aspirin)
• Obtain and analyze a 12-lead electrocardiograph (ECG)
• Obtain blood sample to get initial serum cardiac marker levels and evaluate
initial electrolyte and coagulation studies
• Obtain chest radiograph
• The definitive management is initiated depending of the outcome of theinvestigation
Self-assessment 5.2.5
1) You suspect a stable angina rather than MI pain in the patient who reports
that his chest pain
a) Is relieved by NTG.
b) Is a sensation of tightness or squeezing.
c) Does not radiate to the neck, back, or arms.
d) Is precipitated by physical or emotional exertion.
2) A patient hospitalized for evaluation of unstable angina has severe
chest pain and calls the nurse. Prioritize the subsequent interventions
from 1 (highest priority) to 6 (lowest priority). The appropriate medical
prescriptions and protocols are available to the nurse.
a) Notify the provider.
b) Obtain a 12-lead ECG.
c) Check the patient’s vital signs.
d) Apply oxygen per nasal cannula.
e) Perform a focused assessment of the chest.
f) Assess pain (OLDCART) and medicate as ordered.
3) Is CPR is the first intervention that should be undertaken in case of heart
attack? Explain your answer.
5.3 Neurological system pathologies
5.3.1 Stroke5.3.1.1 Overview of Stroke
1) Carefully observe the above the above three categories of images and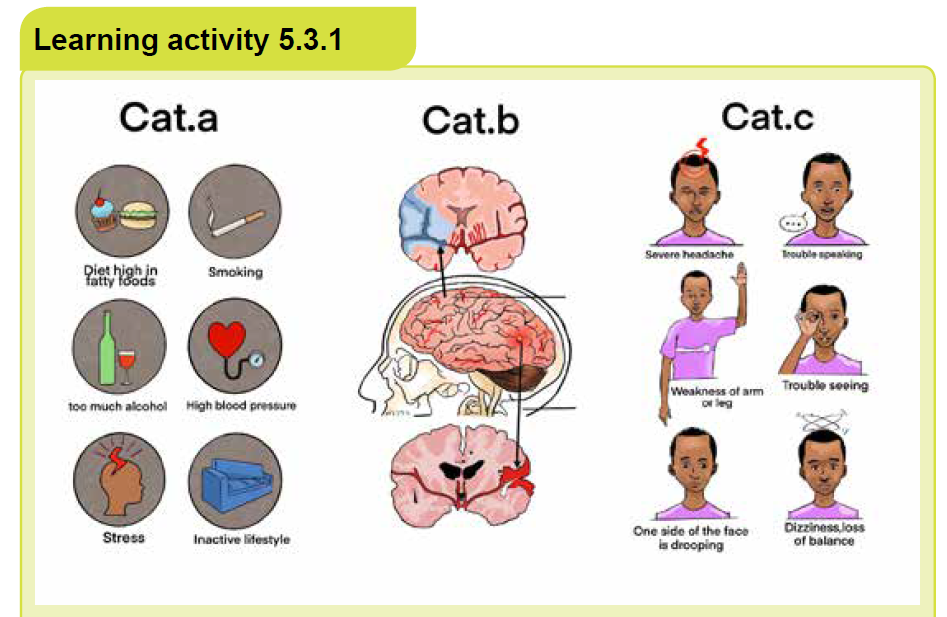
attempt give a general name to each category
2) Try to establish a coherent relationship across these group categories
3) What do you think differenciate the top image from the bottom image ofcategory B in relation to the middle one?
a) Definition of stroke
Stroke also known as Cerebro-Vascular Accident (CVA) or Brain Attack is an
interruption of the blood supply to any part of the brain. is a vascular insult producing
rapid onset of neurological deficit lasting for more than 24 hours, as a result of
inadequate blood flow to a part of the brain or hemorrhage into the brain. Thus, an
insult that results into neurological deficit that resolve within 24 hours is referred to
us as “Transient Ischemic Attack (TIA)”. The severity of the loss of functions varies
according to the location and extent of the brain involved and may involve loss or
impairment of functions such as movement, sensation or emotions.
b) Etiology and pathophysiology of stroke
Two important mechanisms are involved into occurrence of stroke. The blood flow
to a part of the brain is interrupted either by a blocked artery (Ischemic Stroke) orby a ruptured blood vessel in the brain (Hemorrhagic Stroke).
Note that ischemic stroke is the most common and is linked to some risk factors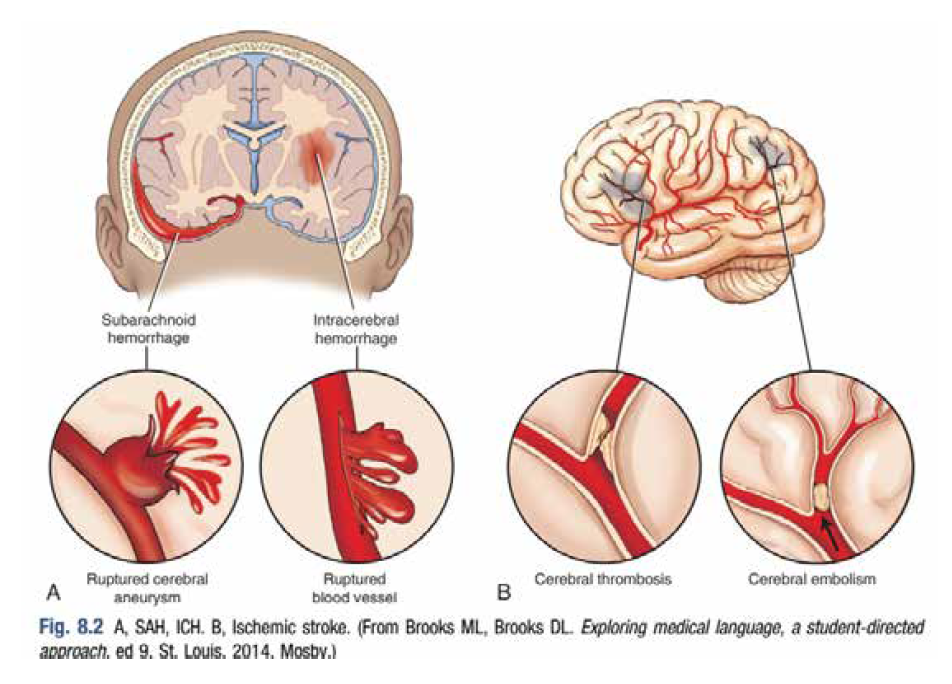
such as increasing age, male sex, family history of vascular disease, hypertension,
smoking, excess alcohol, high cholesterol, diabetes and structural heart (especially
recent myocardial or atrial fibrillation).
c) Sign and symptoms of stroke
Manifestations of a stroke vary depending on the vessel affected and the cerebral
territories it perfuses. They are always sudden in onset and usually multifocal one
sided. Headache may be a sign of impending cerebral hemorrhage or infarction;
however, it is not always present. The most common clinical manifestations include:
• Numbness (paresthesia), weakness (paresis), or loss of motor ability (plegia)
on one side of the body
• Difficulty in swallowing (dysphagia)
• Speech difficulties
• Visual difficulties of inattention or neglect (lack of acknowledgment of one
side of the sensory field), loss of half of a visual field (hemianopsia), double
vision, photophobia
• Altered cognitive abilities and psychological affect
• Dizziness, loss of balance• Self-care deficits.

Self-assessment 5.3
1) You suspect a stable angina rather than MI pain in the patient who reports
that his chest pain
a) Is relieved by NTG.
b) Is a sensation of tightness or squeezing.
c) Does not radiate to the neck, back, or arms.
d) Is precipitated by physical or emotional exertion.
2. A patient hospitalized for evaluation of unstable angina has severe
chest pain and calls the nurse. Prioritize the subsequent interventions
from 1 (highest priority) to 6 (lowest priority). The appropriate medical
prescriptions and protocols are available to the nurse.Perform a focusedassessment of the chest.
a) Notify the provider.
b) Obtain a 12-lead ECG.
c) Check the patient’s vital signs.
d) Apply oxygen per nasal cannula.
e) Perform a focused assessment of the chest.
f) Assess pain (OLDCART) and medicate as ordered.
3. Is CPR is the first intervention that should be undertaken in case of heartattack? Explain your answer.
5.3.2 First Aid in Stroke
The overall goal of stroke care is to minimize brain injury and optimize the individual’s
recovery. The emphases on:
• Rapid recognition of stroke symptoms,
• Early activation and dispatch of Emergency Medical service (EMS)
• Rapid EMS identification, management, and transport (preferably to stroke
center),
• Rapid triage, evaluation, and management in Emergency department (ED)
• Rapid stroke expert decision and therapy selection
• Fibrinolytic therapy• Rapid admission to the stroke unit or critical care unit
i.Pre-hospital
Prehospital providers should take quick and rapid action. The following steps should
be undertaken following DRSABCD approach bearing in mind FAST acronym as
vital to ensuring rapid treatment of a person suffering a stroke. FAST is about:
• FACE – check for facial droop by ask the victim to smile; one side of the face
may not move as well as the other side.
• ARMS – check for arm drift by ask the casualty to hold both arms out with
the palms up, and close their eyes. One arm may not move or drifts down
compared to the other arm.
• SPEECH – check for speech slurred by ask the victim to repeat a phrase
you say. The casualty may slur words, use the incorrect words or is not able
to speak. Also check whether the victim understand you.
• TIME – the time is critical. If you see any of these signs call 912 immediately
(alert the hospital “possible stroke patient”. Ensure as well you have
information regarding the onset of symptoms by asking the casualty, or their
family, friends or bystander.
• Undertake the following as part of initial assessment and stabilization:
• Check and support ABCs vital signs; give oxygen if hypoxemic
• Place the casualty at rest in the semi-sitting position
• Check blood glucose level as hypoglycemia can mimic stroke symptoms
• Obtain iv access and start IV fluid if possible (avoid excess fluids)
• Keep victim close monitoring and be calm and comforting while waiting
victim medical evacuation
• If the casualty becomes unconscious, follow first aid steps for
unconscious victim
• If there is paralysis, position the casualty with the paralyzed side up.
• Keep the victim nil per oral (NPO)
ii.Intra-hospital care at emergency department (ED)
Once arrived to the hospital, an immediate ED assessment and treatment should
be initiated.
• Check ABCs, vital signs; give O2 if hypoxemic
• Start IV fluids if not done in prehospital
• Obtain blood samples and a 12-lead ECG
• Check blood glucose level and correct any hypoglycemia or hyperglycemia
• Perform general neurologic screening assessment including use of specific
stroke assessment scale
• Initiate emergency CT scan or MRI of brain
• Based on assessment and results of investigations the decision is made and
appropriate therapeutic strategies implemented
• Admission to the stroke unit or critical care unit
Self-assessment 5.3.2
1) What does FAST entails with regard to stroke management?2) Why should you keep a stroke victim NPO?
5.3.3 EpilepsyOverview of epilepsy
Observe the above picture and try to figureout what each of them represent then
after attempt to establish any existing relationship.
a) Definition
Epilepsy also known as “Seizure Disorder” is a chronic disorder of the brain
in which there is abnormal, recurring, excessive and self-terminating electrical
discharge from neurons leading to seizures. Epilepsy is characterized by recurring
and unprovoked seizures, thus, a single seizure not sufficient to make a diagnosis
of epilepsy. Seizures occurring solely in association with precipitants (e.g. fever in
young children, metabolic disturbance, alcohol or drug abuse, acute head injury)
are termed acute symptomatic or situation related seizures.
A seizure sometimes called a “convulsion” is a single event of paroxysmal,
synchronous and excessive discharge of neurons in the cerebral cortex manifesting
as a stereotyped disturbance of consciousness, behavior, emotion, motor function
or sensation. An epileptic seizure typically has a sudden onset, lasts seconds to
minutes and usually ceases spontaneously. However, in case of Status epilepticus
there is sustained or recurrent seizures, with failure to regain consciousness between
seizures over 30 minutes. Status epilepticus constitute a medical emergency and
has a mortality rate of 10–15%.
b) Etiology and pathophysiology
Epilepsy is a symptom of numerous disorders but in more than 50% of patients
with epilepsy, no apparent cause is found, in spite of full investigation. It can affect
any person though most common in children and elderly. Seizures are thought
to results from imbalances of excitatory and inhibitory neurotransmitters such
as acetylcholine (ACh) or gamma aminobutyric acid (GABA). Vascular disease
(especially stroke), alcohol abuse, cerebral tumors and head injury are the most
common factors associated with seizures. Other factors associated with seizures
include family history (especially for absence seizure), antenatal and perinatal,
metabolic disorders, sleep deprivation, hypoxia, etc…
c) Signs and symptoms
Since seizures can affect any process your brain coordinates, signs and symptoms
of epilepsy vary across patients and depending of type of seizure. They may include
temporarily confusion, staring spell, jerking, altered mental status, psychological
symptoms such as fear, anxiety. Seizures may cause a person to have convulsions
(general term that people use to describe uncontrollable muscle contractions), but
this is not always the case.
Seizures are either classified as generalized or focalized. Generalized seizures
result from abnormal electrical activity affecting the entire cerebral cortex while
focal or partial seizures affect specific region of the brain. These seizures can
also be categorized as simple or complex depending on how they affect the level
of consciousness. In Simple focal seizures consciousness is retained whereas
consciousness is impaired in complex focal seizures Below is represented signsand symptoms of typical epileptic seizure.
d) Management of epilepsy
The aim of management is preventing or at least reducing the frequency of
seizures through medication and lifestyle modification; and is dependent on the
seizure type and patient. Anticonvulsant drug therapy is usually initiated after a
patient suffers a second unprovoked seizure and the dose is titrated to control
seizures while minimizing side effects. Non-pharmacological management of
epileptic patient involves avoiding activities that would be hazardous if a seizure
were to occur e.g. swimming, operating heavy machinery and driving.
d) Management of epilepsy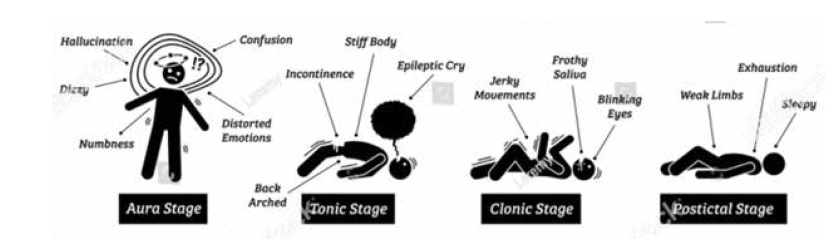
The aim of management is preventing or at least reducing the frequency of
seizures through medication and lifestyle modification; and is dependent on the
seizure type and patient. Anticonvulsant drug therapy is usually initiated after a
patient suffers a second unprovoked seizure and the dose is titrated to control
seizures while minimizing side effects. Non-pharmacological management of
epileptic patient involves avoiding activities that would be hazardous if a seizure
were to occur e.g. swimming, operating heavy machinery and driving.
Self-assessment 5.3.3.
1) Differentiate seizures from convulsions.
2) Who can get epilepsy?3) Enumerate at least one symptom of epileptic seizure on different stage
5.3.2.2 First aid for epilepsyLearning activity 5.3.4

With reference to image above
1. What type of seizure do you think is illustrated there?
2. What would you do to help through?
First aid interventions should include the following:
• Protect the patient from injury
• Manage the seizure or convulsion
• Manage the “After the seizure”
• Advise for Aftercare follow-up
Use the DRSABCD approach and:
• Keep other people out of the way.
• Check the immediate area for hazards, clear hard or sharp objects away
from the person.
• Look at the watch at the start of the seizure, to time its length
• Don’t try to hold the victim down or stop the movements.
• Place the victim on the floor so he/she do not fall and hurt him/herself
• Place the person on the side, if they have food or fluid in the mouth, roll him/
her onto the side immediately to help keep the airway clear so he/she can
breathe easier.
• Keep bystanders clear and reassure them that the seizure will end soon.
• Place something soft and flat under the head such a good soft pillow
• Loose or remove anything around the patient neck, such as a tie or a
necklace
• Remove glasses
• Protect the person from injuries.
• Keep the person safe until the seizure stops out at its self
• As soon as the seizure ends, quickly put the patient in safety recovery
position
• Cover the patient lightly with a coat or blanket.
• Check that normal breathing has resumed.
• Allow the patient to sleep until fully recovered, but check for a response
every few minutes.
• Stay with the person after the seizure stops
• If the patient does not wake up within 10 minutes, is not breathing well, or it
is the first seizure – call for an ambulance (SAMU – 912)
• Stay calm all the time.
• Do not restrain or put anything in the mouth
• Clear area around
• Reassure the person until he/she totally recovers
• After seizure ends, help the person sit in a safe place.
• If the patient has limited walking or standing ability, or is pregnant, has
cardio-respiratory conditions…. ask for help and put him in a rest position.
• If the seizure last more than five minutes, Breathing or consciousness doesn’t
return after the seizure stops, a second seizure follows immediately, if the
patient has high fever, the patient is pregnant, diabetic, the patient injured
her/himself during the seizure don’t wake up the person, call for help
• The medications for epilepsy are incredibly effective. More than half of the
cases are seizure-free after their first medication. check that any prescribed
medication is adequate Give the prescribed medication.
• Advise the patient not to drive. Try to arrange for someone to be with the
patient until he is safely home or in the ward.
• Advise the patient to report the seizure
• Advise the patient to continue taking anti-seizure medication.
• If the patient is known to have epilepsy, there is no need for medical aid or
an ambulance unless the seizure lasted more than 5 minutes or a second
seizure followed
• Check for any injuries and apply necessary first aid
• Reassure the patient as full consciousness is restored.
• Advise the patient not to drive. Try to arrange for someone to be with the
patient until he is safely home or in the ward.
Be aware about possible complications:
• Having a seizure at certain times can lead to circumstances that are
dangerous to the patient or others.
• Falling: fall during a seizure can injure the head or break a bone.
• Drowning. An epileptic person 13-19 times more likely to drown while
swimming or bathing.
• Car accidents. A seizure that causes either loss of awareness or control
can be dangerous if the patient is driving a car or operating other equipment.
• Pregnancy complications. Seizures during pregnancy pose dangers to
both mother and baby, and certain anti-epileptic medications increase the
risk of birth defects.
• Emotional health issues. People with epilepsy are more likely to have
psychological problems, especially depression, anxiety, and suicidal
thoughts and behaviors. Problems may be a result of difficulties dealing with
the condition itself as well as medication side effects, but even people with
well-controlled epilepsy are at increased risk.
Uncommon, complications but may happen, such as:
• Status epilepticus. This condition occurs if frequent recurrent seizures
without regaining full consciousness in between them. People with status
epilepticus have an increased risk of permanent brain damage and death.
• Sudden unexpected death in epilepsy (SUDEP). People with epilepsy
also have a small risk of sudden unexpected death. The cause is unknown.
This occurs to People with frequent tonic-clonic seizures or whose seizures
aren’t controlled by medications.
Nursing care in this situation should focus on:
• Accurate assessments and regular monitoring (immediate attention to
ABCDE and blood glucose monitoring: ongoing monitoring of neurological
status, vital signs and seizures)
• Symptom control and management (IV line and medications)
• Communication with the healthcare team, patient and family
• Risk assessment and management (safety, e.g. padded bed rails;maintenance of secure IV line if continual seizures)
Self-assessment 5.3.4
1) What is the main role of a first aider in case of epilepsy seizure?
2) What can you do if the seizures last more than five minutes?
3) Epilepsy seizure can lead to some complications. Enumerate at least four
of them
4) What is the meaning of Status epilepticus?
5) In skill lab perform first aid interventions for:
a) A client with focal seizuresb) A client in tonic-clonic seizures
a. A noise a person makes while breathing.
b. The way a person breathes when they are scared.
c. An illness that causes the airways to swell and get tight.
d. Something that a person gets from running too much.
6) What can trigger an asthma attack?
a) Being allergic to your cat.
b) Bing near someone who is smoking.
c) Being inside a room that is dusty.
d) All of the above.
7) What is the primary concern when assisting a person having a seizure?
a) Holding them still
b) Keeping them safe from harm
c) Placing them flat on their back
d) Stopping seizure
8) A 20-year-old person is having suddenly a seizure and make movements
and have froth around the mouth. The first best action to do by the first
aider is:
a) Keep other people out of the way
b) Stopping seizure
c) Wakeup the patient
d) Give medication
9) Stroke is a vascular insult producing rapid onset of neurological deficit
lasting for more than 24 hours; manifestations of a stroke vary depending
on:
a) Personality of patient
b) The etiology of stroke
c) The affected body system
d) The vessel affected and the cerebral territories it perfuses
0) Acute Respiratory Distress Syndrome does not occur as a primary
process but may follow a number of diverse conditions producing direct
or indirect lung injury; the direct injuries leading to ARDS are the following
except one:
a) Aspiration, pneumonia
b) Fat embolism
c) Excessive blood transfusion
d) Pulmonary contusion
11) In healthy adults the average systolic pressure is less than 120 mmHg
and the average diastolic pressure is less than 80 mmHg. The difference
between the systolic and diastolic pressure, known as the pulse pressure
is normally ranging:
a) Between 30 and 40 mmHg
b) Between 20 and 40 mmHg
c) Between 30 and 50 mmHg
d) Between 20 and 30 mmHg
12) Rank the following causes of stroke from the most common (1) to least
common (3):
a) Cerebral hemorrhage
b) Cerebral ischemia
c) Subarachnoid hemorrhage
13) Order the following immediate interventions to be implemented when
hypertensive crisis is suspected?
a) Elevate the head of the bed to approximately 30 – 450
b) Notify the physician
c) Administer supplemental O2
d) Assess BP in both arms
e) Perform a focus assessment
f) Keep close monitoring including assessing changes in cardiac rhythm
g) Anticipate and prepare to get ready to implement physician orders
14) Enumerate at least three advises to give to the patient/family after a crisis
of seizure.
15) How can you help if someone is having an asthma attack?
16) Both transient ischemic attack (TIA) and cerebral vascular accidents
(CVA) are vascular insult to brain tissue. Contrast these two conditions?
17) Through which mechanism does stroke occur?
18) List five steps that are important when helping someone with heart
problems.
19) A 67 years old is suffering from ischemic stroke that affects his lefttemporal area; what functions are likely to be affected?
UNIT 6 VICTIM’S EVACUATION TECHNIQUES
Key unit competence
Apply correctly the technique of victim’s evacuation during emergencies
Introductory activity 6Observe the image below and respond to the asked questions
1. What does the illustrates A, B, C and D above show?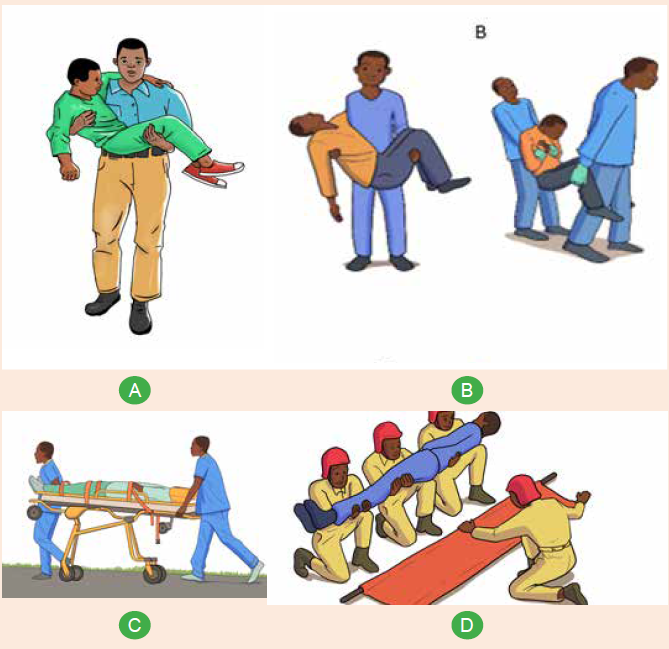
2. What are the materials do you see in use in the mentioned illustrate?
3. Differentiate different technique for victim evacuation observed on the
illustrate above.
6.1.Basic concepts of emergency response and management(ERM)
1) Observe the image above and mention what they all have in common.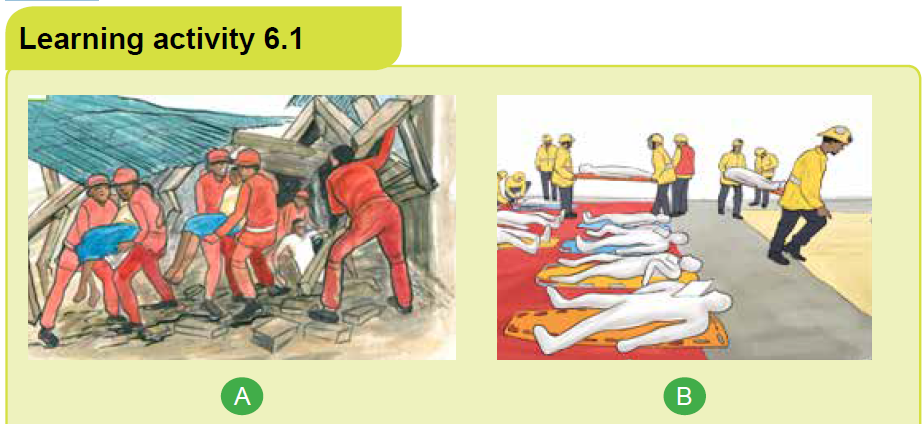
2) Referring to the above image explain the term emergency and emergency
response
a) Emergency /Disaster
An emergency is a situation that poses an immediate risk to health, life, property,
or environment. Most emergencies require urgent intervention to prevent a
worsening of the situation. While some emergencies are self-evident (such as
a natural disaster that threatens many lives), many smaller incidents require that
an observer (or affected party) decide whether it qualifies as an emergency.
b) Emergency Response
Response is a reaction to an emergency situation or event. Response can range
from individual to national level. The response phase of an emergency may
commence with search and rescue but in all cases the focus will quickly turn to
fulfilling the basic lifesaving and humanitarian needs of the affected population.
For the disaster, emergency response is the phase of the disaster-management
cycle that often attracts the most attention and resources. It should therefore be
seen as a critical part of the disaster management cycle. Emergency response is
a cyclical process, involving repeated assessment, planning, action and review, to
respond appropriately to needs and capacities as they evolve. It starts with an initial
assessment and may be triggered spontaneously by the disaster event, or officials
may authorize the mobilization of people and resources. Rapid and effective
mobilization is facilitated by proper disaster preparednes
-Aim of the Emergency Response Management
To reduce mortality rate and damage to property thereby reducing the impacts of
disaster and to ensure successful recovery of maximum number of people
-Importance of a Timely and Coordinated Response
Depending on injuries sustained by the victim, outside temperature, and victim’s
access to air and water, the vast majority of those affected by a disaster will die
within 72 hours after impact
-Activities included in emergency response management
• Search & Rescue
• Fire Fighting
• Emergency Medical Assistance including first aid, mass casualty
management and physiological first aid etc.
• Transportation of victims
• Need Assessment Survey
• Hospital Preparedness
• Evacuation
• Provision of food and non-food items
• Temporary shelter
• Emergency repair of critical facilities
• Security measures/tracing/family reunification
c) Emergency management
Emergency management is the organization and management of the resources
and responsibilities for dealing with all humanitarian aspects of emergencies. The
aim is to reduce the harmful effects of all hazards, including disasters.
The emergency management has 4 phases. preparedness, response, mitigation,
and recovery
Emergency Preparedness is a research-based set of actions that are taken as
precautionary measures in the face of potential disasters. These actions can include
both physical preparations (such as emergency supplies depots, or adapting
buildings to survive earthquakes) and trainings for emergency action. Preparedness
is an important quality in achieving goals and in avoiding and mitigating negative
outcomes.
Disaster Mitigation is the ongoing effort to lessen the impact disasters have on
people and property. Mitigation involves keeping homes away from floodplains,
engineering bridges to withstand earthquakes, creating and enforcing effectives.
building to protect property from sliding etc. Mitigation describes the ongoing effort
at the federal, state, local and individual levels to lessen the impact of disasters
upon families, homes, communities and economy.
Recovery is those activities that continue beyond the emergency period to restore
lifelines. Examples include providing temporary shelter, restoring power, critical
stress debriefing for emergency responders and victims, job assistance, smallbusiness loans, and debris clearance
Self-assessment 6.1.
1) Mitigation in the disaster management cycle involves what activity?
a) Prevention of disasters if possible
b) Caring for the birds injured
c) Responding to the disaster
d) Preparing for litigation after the event
2) Disasters can happen at any time. What is the first part of the disaster
management cycle to consider?
a) Response
b) Litigation
c) Recovery
d) Preparation
3) Most emergencies require urgent intervention to prevent a worsening of
the situation
a) Yes
b) Not
4) installing electricity destroyed after an earthquake strike is considered an
activity of:
a) Emergency Recovery
b) Emergency preparedness
c) Emergency mitigation
d) Emergency litigation6.2. Local level search and rescue technique
Analyze carefully the following images above and respond to the question aside.
1) Explain the common features observed among people on this picture?
2) What are different tasks are they doing?
3) How do you find the place where they are performing their duties?
4) What might be the cause of the situation observed on these pictures?
Search and rescue is a technical activity rendered by a group of specially trained
personnel, who rescue and attend to the casualties under adverse conditions,
where life is at threat. Search and rescue is organized in close cooperation with
the community and in a team approach. The search and rescue activities are
undertaken in two ways such as community local rescuers and outside community
rescuers.
6.2.1 Community Local Rescuers
With adequate safety measures, rescue immediately after any natural calamities
such as cyclone, flood, earthquake and fire in a community.
6.2.2 Outside Community Resources
Circumstances where the situation is grave and the local rescuers do not have
required efficiency and equipment, then specialist assistance from outside the
community is required. The role of public health providers is to promote, protect,
and improve the health of individuals and communities. The community rescuers
shall have to be in readiness to respond quickly, when a cyclone, flood, earthquake
and fire occur. The rescuers efficiency level has to be maintained thorough practice
nd demonstrations /mock-drills during the non-disaster period. The rescue team
should undergo standard training from time to time.
6.2.3 Rescue workers
An event requiring rescue operations will usually create three categories of rescue
workers survivors, untrained personnel and trained personnel.
a) Survivors
The immediate reaction of survivors in a major incident, once discovered that they
are not injured, is to help their neighbors and families. They often do not know
what to do, but obviously it is a serious situation and thus they feel they must do
something.
b) untrained personnel
The second ‘wave’ of rescue workers is drawn from people either witnessing the
event from the immediate vicinity, or are drawn to the site by curiosity and a desire
to assist the victims. Although not quite as emotionally involved as the survivors,
the danger inherent in utilizing untrained personnel is still a factor which must be
considered. On the positive side, they often bring necessary resources with them
and can be effective if brought under control and properly supervised.
c) Trained personnel
The last group to arrive at the scene is the trained rescuers: Police, Fire, Civil
Defense, etc. It takes some time for various emergency services to mobilize and
arrive at the scene. The quicker they can arrive, the less time there will have
been for the first two groups to aggravate the situation and create more dangers
to surviving victims and themselves. The well-trained team will know what to do,
and how to utilize the available resources and untrained personnel in efficiently
carrying out the necessary tasks in a manner that will not further endanger
anyone.
6.2.4 Team composition
Team composition will be determined by the various organizations within each
area on the basis of safe accomplishment of set tasks. Regardless of the team
composition, a team leader must be appointed. A team of 6 – 8 members is
required for effective general rescue teamwork. It is essential that each safe
shelter form a rescue group, comprising of 8 members; Team leader: 1, Skilled
persons: 2 Members: 5
-Activation
Each team should have a call out system established, and have determined the
time necessary to ensure a full team response. This system should include such
details as:
• Who calls out the team
• Who will be responsible for them
• Where to report
• What functions the team will perform
• What equipment to take
• Likely duration of task or event.
-Deployment
On call-out, teams should state clearly to the organization requesting their support,
details of accommodation and any feeding assistance that may be required.
If practicable, each team should be self-sufficient in the provision of food for the
first 24 hours.
-Coordinated incident management system (CIMS)
The Coordinated Incident Management System) provides the model for command,
control, and coordination of an emergency response. It provides a means of
coordinating the efforts of agencies as they work towards the common goal ofstabilizing an incident and protecting life, property, and the environment.
Self-assessment 6.2
1) Mention the two ways/levels search and rescue activities are undertaken.
2) Explain role of the three types of rescue workers.
3) How is the rescue team composed?
4) How does a rescue team coordinated.
6.3. Introduction to basic rescue victim’s techniques
Learning activity 6.3
Analyze careful the following image below and respond to the questions thatfollow
1) What is the purpose of the different activities depicted on the image above
2) Distinguish different technique observed on the image above.
6.3.1. The aim of rescue
The aim of rescue is to save the greatest number of lives in the shortest possible
time and to minimize further injury to people and damage to property.
-Basic rescue evacuation techniques: Evacuation and safe rescuing of victim by
applying simple manual techniques can save the life of the victim. Regular hands
on practice and drills will help the rescuer to safe lives in quicker and safer manners
Rescue drag and victim evacuation techniques,
• Required to evacuate an injured person from an emergency scene to a
location of safety.
• Manual carries are tiring for the rescuer and involve the risk of increasing the
severity of the casualty’s injury.
• Choose the evacuation techniques that will be least harmful, both to rescuer
and the victim.
• Causalities carried carefully and correctly handled, otherwise their injuries
may become more serious or possibly fatal.
• Situation permitting, evacuation of a causality should be organized and unhurried.
• Each movement should be performed as deliberately and gently as possible.
All rescuers must be aware that the safety of the casualty is paramount even
when immediate evacuation from a hazardous environment is necessary. A careful
assessment must be made of the casualties’ injuries, condition, and possible
entrapment, and a final check must be made to ensure that the casualty is actually
ready to move and is not caught or entangled in some unseen object. Selection or
sorting of casualties before evacuation of casualties where multiple casualties need
attention, the rescuer will be required to select casualties for treatment and rescue
by order of priority. This selection or sorting of casualties is known as triage.
Rescuers may be called upon to perform the triage role at a rescue site as a specific
task, or this may be a part of the overall reconnaissance element of a rescue. While
moving fairly quickly from casualty to casualty, the rescuer performing triage must:
• Quickly assess the condition of casualties and label them.
• Place any unconscious person in a lateral recovery position – care for airway,
breathing, and circulation.
• Temporarily control any serious bleeding by the use of bystanders or other
rescuers as necessary.
• Choose the casualties with the greatest chance of survival.
It must be noted that it will sometimes be necessary to treat and rescue casualties
of relatively low priority in order to access and clear the way for treatment of high
priority casualties. Additionally, the principle of ‘remove the casualty from the risk or
remove the risk from the casualty’ should be adopted where a site hazard presents
a risk to casualties being treated prior to rescue.
-casualty sorting
Before transporting the causalities, it is important to start by sorting them, in other
of priority.
Red: Priorities are displayed using a color code system.
• Those victims who need immediate advanced medical treatment (within 1
hour) to survive.
• These victims would have first priority for transport to a medical facility, if
available.
Yellow: These victims have serious injuries, but are not life threatening. They will
survive without advanced medical treatment and their situation can be maintained
through proper basic emergency care.
Green: Minor injuries that can be dealt with by first aid, or can wait for some time
without treatment
Black: Deceased, or who are unlikely to survive given the situation.
NOTE: These colour codes may constantly change, as the assessment of the
casualties and their injuries is an ongoing process. The victim’s colour code may
change as the situation changes (e.g., the availability of transport, medical supplies,
etc). In a major incident, be prepared to wait some time without either advanced
care on-site, or transport to an appropriate facility. After removal, many casualties
will have to be carried over piles of debris and uneven ground before being handed
over to the ambulance service or first aid station. Whilst speed of removal is
important, it must be consistent with safety and proper handling to prevent further
injury.
The technique used will depend on the immediate situation, the condition of
casualties, types of injuries, and available equipment. Rescue leaders should
conduct frequent exercises in the removal of casualties, using live people as
casualties to give team members understanding and confidence in the various
methods, enabling them to make decisions promptly in times of emergency. As
important as learning methods; rescuers should experience the physical effort
required in transporting casualties, either by stretchers or by some improvised
method. The transportation of casualties over long distances is a very tiring task
and requires fit personnel.
There are many types of victim evacuation techniques but in our context, we shall
focus on:
• Ankle pull
• Shoulder pull
• One-person lift
• Pack-strap car
• Two-person arm carry
• Two person carry by arms and legs
• Chair carry
• Improvised stretcher
• Fireman’s carry and• Blanket drag
Rescue tools

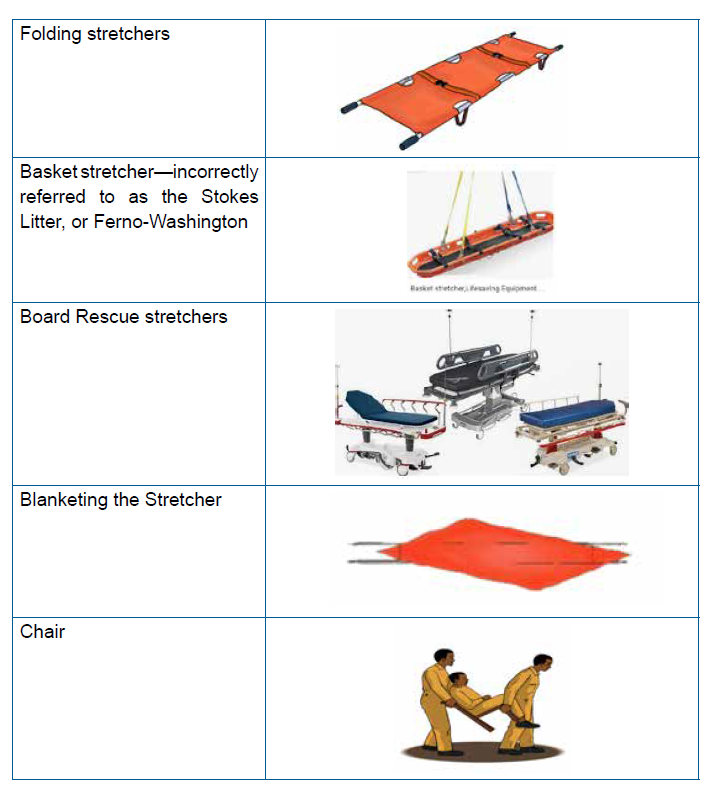
Self-assessment 6.3
1) Explain the methods used to sort or selecting the victim evacuation in
other of priority
2) Outline the Rescue drag and victim evacuation techniques3) Mention and differentiate at least 2 different victim evacuation techniques
6.4. Ankle pull

a) Description
Ankle pull evacuation technique is also known as ankle drag evacuation technique
and is used to move a victim who is too large to carry or move in any or other way.
Generally, the movement of a victim by lifting part of their body as the other part
drags is often used when a carry isn’t possible or practical. Regardless of whether
you carry or drag a victim to safety, you must remember to keep your own safety
a high priority. It doesn’t sound heroic to say, but it does no good for anyone if you
injure yourself and become part of the problem rather than the solution.
Things to consider before deciding to use ankle pull technique.
• How many victims are in need of rescue?
• How many rescuers are available?
• What are the capabilities and conditions of the rescuers?
• What is the size and condition of the victim(s)?
• What is the safety and stability of the environment?
The feet drag is a last resort. Moving a victim in this manner will most certainly be
uncomfortable for the victim and will likely cause greater injury. It’s a “life over limb”
technique. This can really be accomplished only if the victim is unconscious because
of the pain of dragging their torso and head along the ground. To perform ankle pull
evacuation technique, the rescuer has to grasp firmly the ankles of victim and move
backward, victim’s arms should be crossed aver his/her chest, the rescuer pulls the
victim to safety in a straight line. The technique should not be used if the victim issuspected to have a spinal cord injury, head or neck injuries.
Self-assessment 6.4
In simulation lab or in classroom make pairs and perform the ankle pull victim’s
evacuation technique.6.5. Shoulder pull
a) Description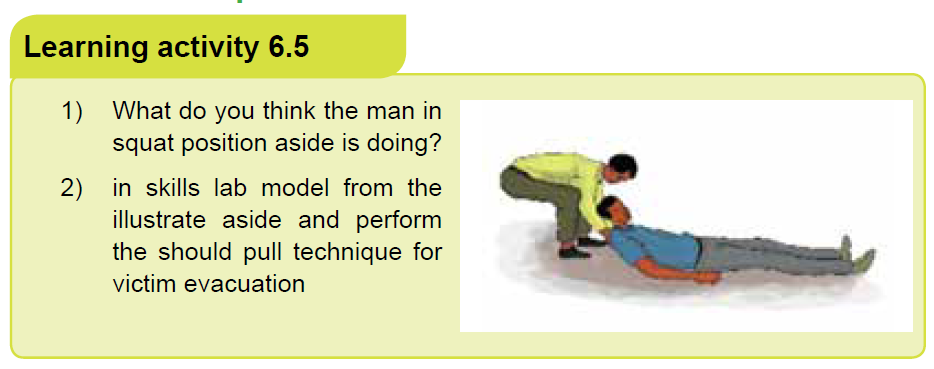
The shoulder pull technique is a one-man rescue technique used to evacuate the
causality from the danger area to the safe area or from the incident area to the
hospital. Because in this procedure the rescuers use his own hand, therefore it
does not require equipments. However, for trauma patients, it is always advised to
evacuate them using equipment that allows stabilization of the whole body and safe
handling of the injured in vertical and horizontal planes because maximum care
must be taken to avoid to worsen an unstable trauma. The head-neck-chest axis
must be kept straight to protect the spine, and the first responders must keep the
patient’s body stable (no movement of the feet) before the pull.
The shoulder pull is preferred to the ankle pull. It supports the head of the victim.
The negative is that it requires the rescuer to bend over at the waist while pulling.
b) Procedure
• Grasp the victim by the clothing under the shoulders.
• Keep your arms on both sides of the head.
• Support the head.
• Try to keep the pull as straight and in-line as possible
• Pull the victim
Self-assessment 6.5
In group of 2 go in the skills lab and perform the technique of shoulder pull oneach other
6.6. One-person lifting
One-person transport methods
• Fireman’s Carry- the easiest way to transport a light and smaller victim.
• Piggy Back- when the victim is conscious.
• Pack Strap Carry- when the victim is smaller than the first aider.
• Shoulder Drag- used when the floor is smooth, short distance transport.
• Fireman’s Drag or Tied-hands Crawl- used when the first aider and the victim
must crawl underneath a low structure.
• Blanket Drag- used when the victim is seriously injured and should not be
lifted.
Factors to Consider before lifting the causality by one-person lift:
• Weight and height of the victim
• Status of the victim (conscious or unconscious)
• Environment (safe, floor is smooth, narrow or wide)
• Special need considerations (injuries of the victims)
A single person who cannot walk but who does not need to be on a litter (one with,
for example, a broken ankle, mild exhaustion, or acute mountain sickness) may
be carried on the back of a strong rescuer using a rope seat. This is fashioned by
passing a long 1 inch (2.5 cm) rope or strap across the victim’s back and under his
arms, then crossing the rope in front of his chest.
The victim is loaded piggyback onto the rescuer’s back, and the rope ends are
passed forward over the shoulders of the rescuer, under his arms, and around to
the rescuer’s back, then between and through the victim’s legs from the front, and
around the outside of the victim’s legs just under the buttocks, to be tied snugly
in front of the rescuer’s waist. Such a rope seat is far preferable to a standard
fireman’s carry, which is very fatiguing. A blanket drag is only good for very short
distances, such as to pull a person quickly away from an immediate hazard.One rescuer handling technique

Application activity 6.6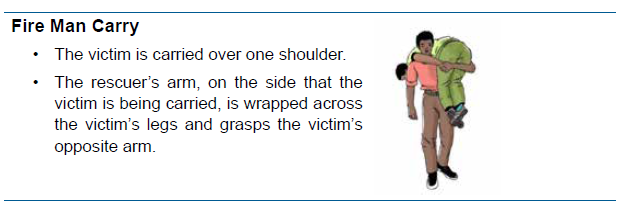
1) What are the factors to Consider before lifting the causality by one-person
lift?
2) In Fire Fighters Carry, the victim is carried over one _________.
a) knee
b) arm
c) shoulder
d) leg
3) Go in the simulation lab, pair yourself and perform the one-person liftarms carry technique for victim evacuation.
6.7. Pack- strap car victim evacuation technique
Learning activity 6.7Analyze carefully the following images and respond to the questions below:
1) The victim evacuation technique illustrated above is appropriate to a)
unconscious patient, b) conscious patient, c) adult causality.
2) describe in a stepwise approach the technique of pack-strap as observedon the illustrate A, B and C above.
a) Description
The pack-strap car is a rescue technique using no equipment for appropriate
victim evacuation; the pack-strap car technique involves only one rescuer handling
maneuvers to evacuate the causality from one area to another for appropriate care.
This technique is used on the conscious casualty with no fractures of the extremities.
b) Procedure
• The rescuer turns his/her back to the standing casualty.
• The rescuer after turning the back to the causality brings the causality’s arms
over his/her shoulders to cross his/her chest.
• The arms of causality must be kept straight as possible, the armpits over the
shoulders of rescuer.
• The rescuer holds casualty’s wrists, bends, and pulls the person onto his/herback.
Self-assessment 6.7
In your class make groups of two students one student will play the role of
casualty while the second one will play the role of rescuer then perform the
“pack- strap car” victim’ evacuation technique modeling on the illustrate above.
After performing the first round exchange the role and reperform the “pack-strapcar” victim’s evacuation technique
6.8. Two person arms carry
Two-person arms carry is a technique for victim evacuation which involve two
rescuers to drag the victim in a safe place using their hands. Both conscious and
unconscious victims can be carried with this technique. Two person carry involve
human crutch/two person drag technique, two handed seat technique and fourhanded
seat technique.
6.8.1. Human crutch/two-person drag
a) Description
For the conscious victim, this carry allows the victim to swing their leg using the
rescuers as a pair of crutches. For the unconscious victim, it is a quick and easy
way to move a victim out of immediate dangerb) Procedure
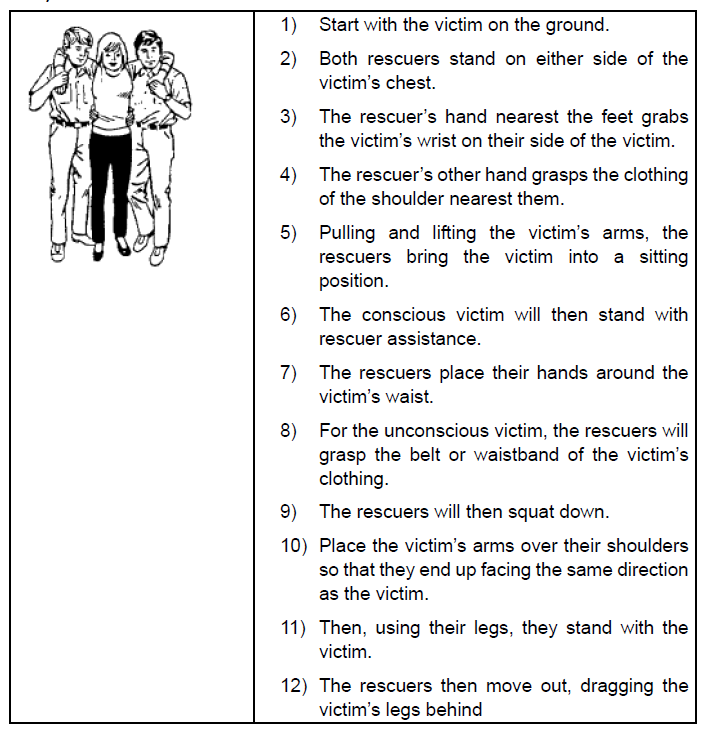
Self-assessment 6.8.1
In your groups model from the illustrate above and perform the technique of
human crutch /two-person drag
6.8.2. Two Handed- seat technique
a) Description
This technique is for carrying a victim for longer distances. This technique can
support an unconscious victim.b) Procedure

Self-assessment 6.8.2
Pair yourself in groups of two and perform the technique of two handed- seat for
victim evacuation modeling from the illustrate above
6.8.3 Four handed- seat
a) Description
This technique is for carrying conscious and alert victims in a moderate distance.
The victim must be able to stand unsupported and hold themselves upright during
transport.b) Procedure
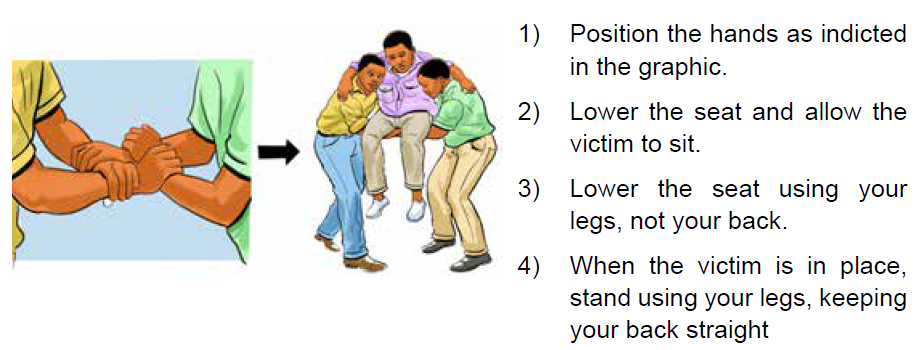
Self-assessment 6.8.3
Pair yourself in groups of 3 then model from the image above and perform the
technique of four handed seat for victim evacuation.6.9. Two person carry by arms and legs
Two persons carry by arms and legs technique is a method of victim evacuation
where one rescue holds the victim legs and the other one hold the arms to drag the
victims out of danger.
a) Things to consider before attempting the two arms and legs carry
technique
• Explain the Procedure to the casualty. If the casualty is conscious, tell him
what you are going to do. The explanation will help to calm his fears and will
help you to get his cooperation.
• Perform necessary measures before transporting. Make sure the casualty
is breathing properly, open wounds have been dressed and bandaged, and
fractures have been splinted before transporting the casualty.
• Have one person in charge. One person must give the instructions to the
remainder of the team so actions will be performed in union.
b) Precautions:
• Do not transport a casualty with a suspected fracture of the neck or back
unless a life-threatening hazard is in the immediate area. Wait until medical
personnel arrive.
• Go slowly to avoid further injury. If the injured person is able to talk, check in
frequently to make sure they are comfortable throughout the process.
• In the event the injured person is unconscious, you may want to tie their
hands loosely together at the wrists. This can make the carrying process
easier.
• Do not use anything thin or sharp to tie the person’s hands this could cut their
wrists.c) Procedure
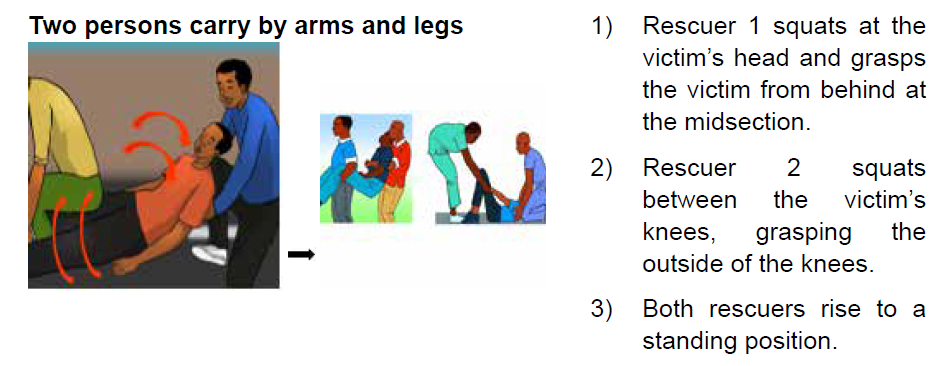

Self-assessment 6.9
1) What do you need to consider before evacuating a victim with arms and
legs.
2) Describe what the Fore and Aft method involves in two person carry by
arms and legs evacuation technique.6.10. Chair carry technique
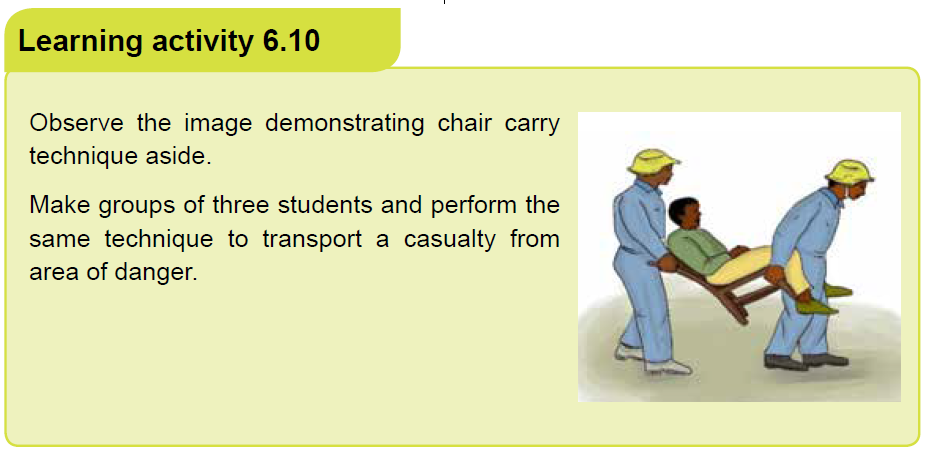
a) Description
A chair carry technique is a method often used to move a sick or injured person
away from a position of danger. The casualty is seated on a chair and a chair is
carried by two rescuers. The two-person seat carry requires a second responder.
This carry can be used by any person who is conscious and not seriously injured.
This method is prohibited if the casualty is suspected to have head, neck or spinal
injuries.
A chair carry method is a victim’s evacuation methods which doesn’t require
equipments; only an appropriate chair is used.
This is a good method for carrying victims up and down stairs or through narrow oruneven areas.
b) Procedure

Self-assessment 6.10
In your class make groups of three students. One student will play the role of
causality while the two others will play the role of rescuers then perform the “chair
carry” victim’ evacuation technique. After performing the first round exchange
the role and reperform the “chair carry” victim’s evacuation technique. Everystudent should play the role of rescuer.
6.11. Improvised stretchers
A stretcher is a light frame made from two long poles with a cover of soft materials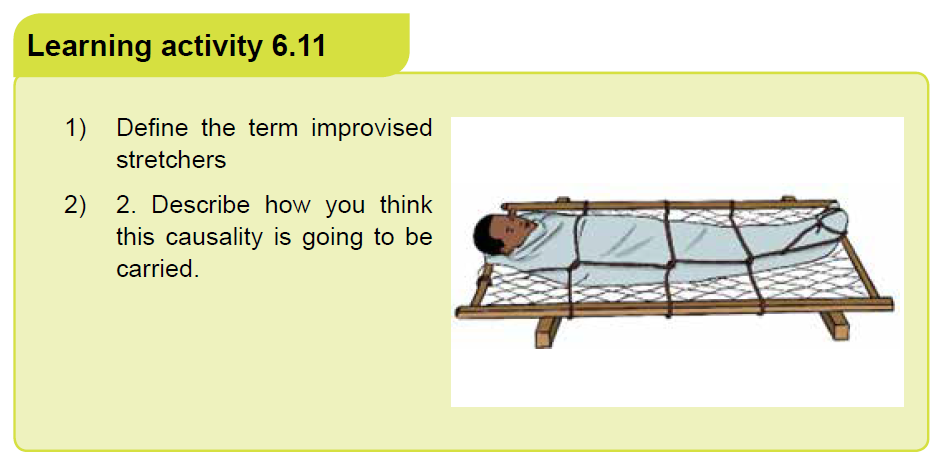
stretched between them, used for carrying people who are ill, injured, or dead.
Causality evacuation from the danger area to the safe area or from the incident
area to the hospital is crucial to save life. However, in some situation there may be
insufficient stretchers for the number of casualties involved. Therefore, improvised
stretchers have to be used to carry victims.There are many methods of improvisation

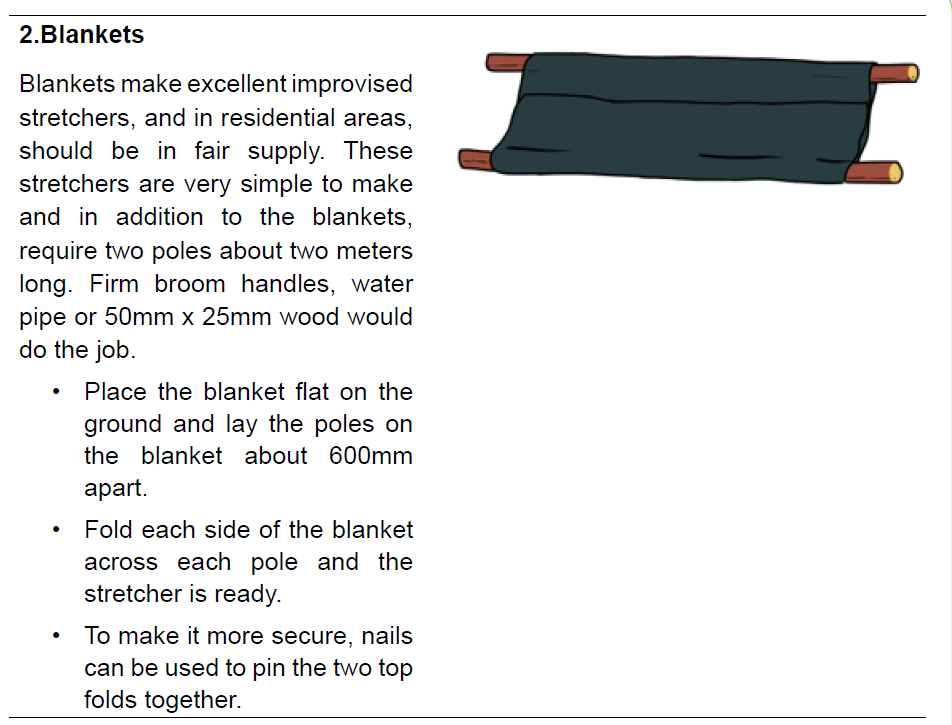
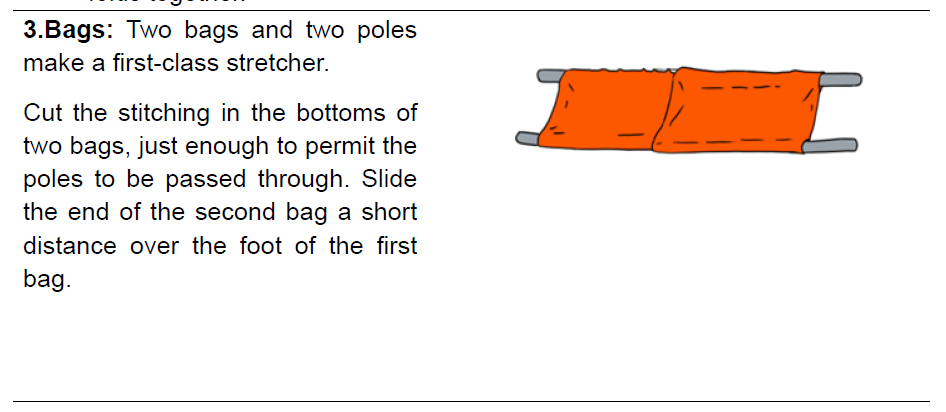
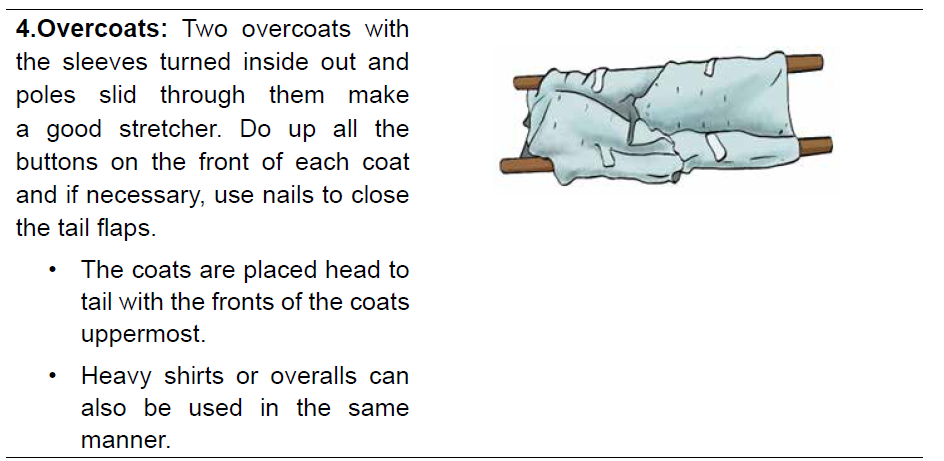
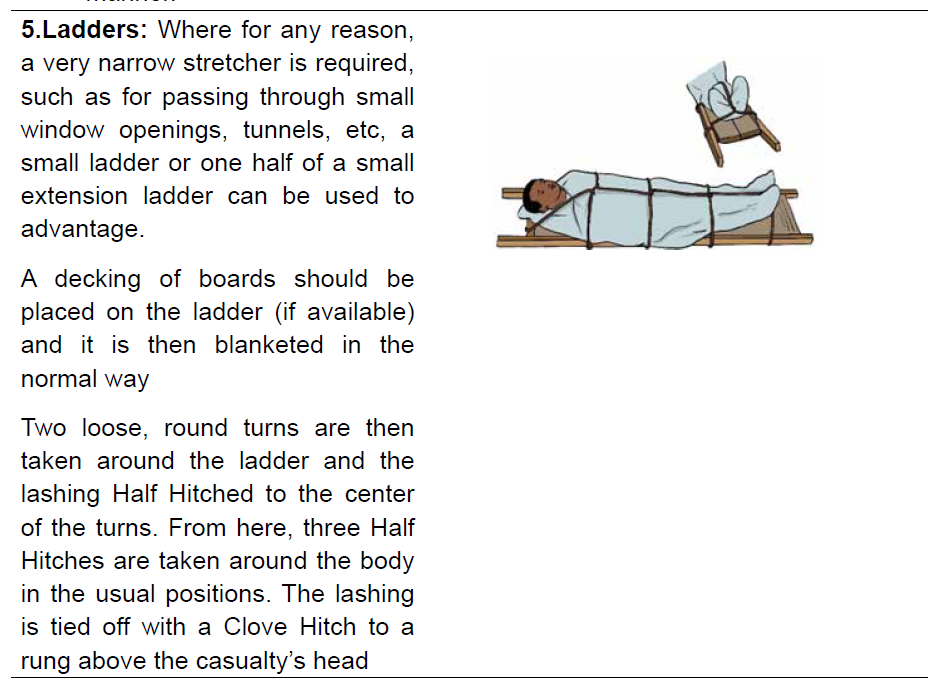

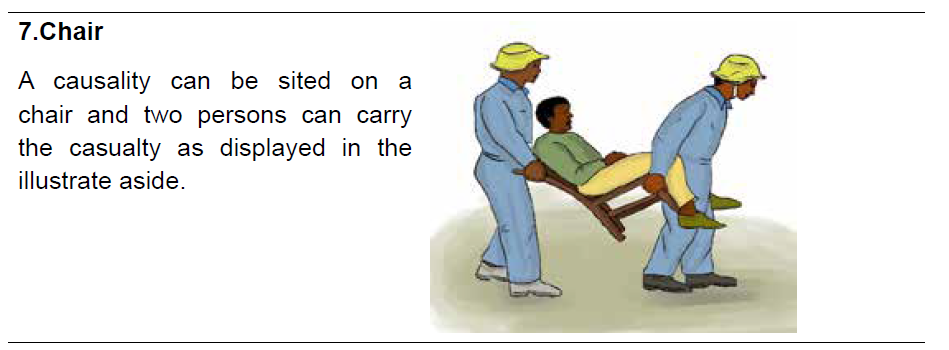
Self-assessment 6.11
1) What are the materials needed to make a blanket stretcher2) Describe the process of making a stretcher with a door.
6.12. Fire man’s carry technique
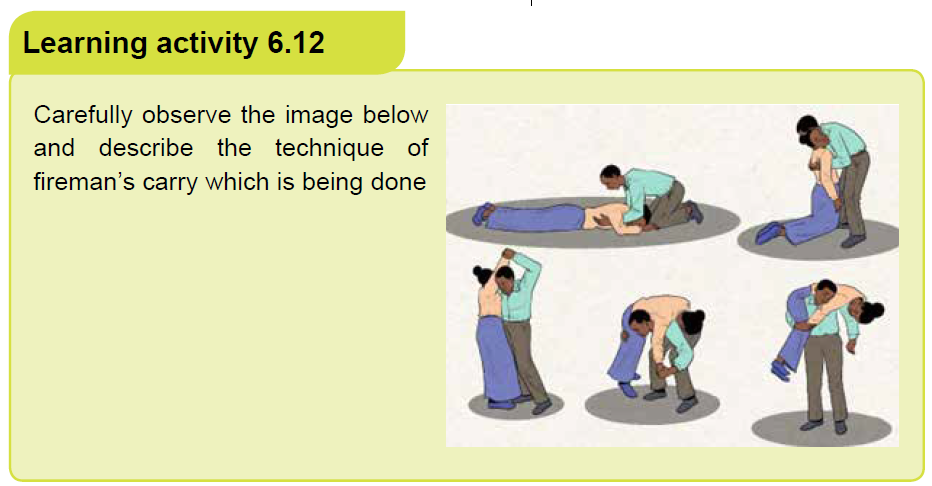
a) Description
A fireman’s carry or fireman’s lift is a technique allowing one person to carry
another person without assistance. It requires placing the carried person across the
shoulders of the carrier. This technique is for carrying a victim in longer distances.
It is very difficult to get the person up to this position from the ground. Getting the
victim into position requires a very strong rescuer or an assistant.
Fireman’s carry technique was commonly used by firefighters to carry injured
or unconscious people away from danger, but has been replaced in firefighting due
to the drawback that smoke and heat are greater higher up, and may be fatal to the
person being carried. The «fireman›s carry» technique is still taught for use outside
firefighting. Soldiers use this technique to carry the wounded. Lifeguards are
sometimes trained to use the fireman›s carry.
b) Advantage
Carrying someone in this manner has several advantages over other methods
of moving another person. The subject’s torso is fairly level, which helps prevent
further injuries. When the subject’s weight is evenly distributed over both shoulders,
it is easier to carry them for a longer distance mainly 15 meters or more.
The fireman’s carry is preferred over a single-shoulder carry if someone is seriously
hurt or if the person must be carried for a considerable amount of time. A person
being carried over one shoulder would experience more shaking as his or her body
is hanging more freely over the carrier’s shoulder. Also, blood would be unevenly
distributed if someone was hanging upside-down over the carrier›s shoulder for an
extended period of time. This could also be a very uncomfortable position for the
carried person if he or she is still conscious.
The fireman’s carry allows a soldier to carry an injured comrade securely using only
one hand, leaving their other hand free to carry and fire their weapon if required
c) Disadvantages
In firefighting, smoke and heat are greater higher up, and may be fatal to the person
being carried. The person carried is largely outside the rescuer’s field of vision,
and almost all vital areas are out of the rescuer’s view. Thus, dangerous changes
in their condition can be missed, and an inexperienced rescuer can inadvertently
create or further compound injuries via collision with obstacles. Furthermore, the
rescuer’s obstructed peripheral vision puts both persons at risk if the incident that
caused the injury is still ongoing (fire, combat, public disturbances, etc.). It is also
harder to get a patient onto a rescuers shoulders than it is to drag a patient by their
shoulders.
The fireman’s carry presents severe hazards if the person being carried has or mayhave a spinal injury, and should be avoided.

Self assessment 6.12
Go to the playground, pair yourself in groups of two of the same weight theperform the technique of fireman’s carry.
6.13 Blanket drag technique
1) Explain the material observed on the first above image.
2) Outline the advantages of victim evacuation technique observed on the
above image?
a) Description
The blanket drag technique also known as “blanket lift or blanket carry” technique
is an effective method for loading or moving a casualty in a confined space. This
technique can be used to transport suspected spinal injured casualties with correct
immobilization of the spine and with particular attention paid to the head and neck.
This ‘blanket carry’ can also be used as an improvised stretcher for carries over
moderate distances. This technique involves four or six rescuers.
b) Procedure
• Make a stretcher ready using one blanket.
• Roll a blanket lengthways for half of its width and lay the rolled section along
the side of the casualty (casualty flat on back).
• The leader then directs two (or three) rescuers to kneel down on each side
of the casualty.
• The rescuers on one side ease the casualty over on one side and the rolled
section of the blanket is pushed well underneath the casualty.
• With the rolled up section of the blanket now under the center of the casualty,
the casualty is eased over in the opposite direction and the blanket is unrolled.
The casualty should now be lying flat on their back.
• The sides of the blanket are rolled up close to the casualty’s body to provide
handgrips for the bearers.
• On the order from the leader, the casualty is lifted waist high, and carried to
the stretcher.
• On the order from the leader, the casualty is lowered onto the stretcher.
• The blanketing is then completed with one blanket, leaving the lifting blanketin position.
Self assessment 6.13
In your class, make groups of seven students. One student will play the role of
casualty while other students will be rescuers; then perform the “Blanket drag”evacuation technique
End unit assessment 6
From question 1-9; Select the bests answer, only one option is accepted:
1) It is critical to know background information about the patient you are
transporting because:
a) It helps you remain proactive in the prevention of injury
b) It can help you do your job better
c) Such information can help to diagnose the patient
d) You might have to relay the information to someone else
2) A technique/method where rescuer 1 grasps the victim from behind at the
midsection while the other rescuer grasping the outside of the knees is.
a) Two-Person Carry by arms and legs
b) Ankle Pull
c) Blanket Drag
d) Two Handed Seat
3) The following are the methods in carrying and transporting a victim
EXCEPT?
a) fighters carry
b) shoulder pull
c) ankle pull
d) chair carry
4) In Fire Fighters Carry, the victim is carried over one _________
a) knee
b) arm
c) shoulderd) leg
5) What technique/method is shown in the image below?
a) Four handed seat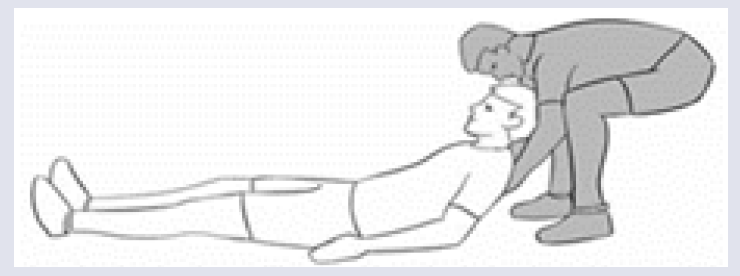
b) One-person carry
c) Ankle pull
d) Shoulder pull
6) Which of the following technique is the best in moving downstairs a
causality who has head or spinal injuries.
a) Blanket drag
b) Chair carry
c) Rope carry
d) Crutch carry
7) A technique/method of carrying where in rescuers get on both sides of the
victim is.
a) Hammock Carry
b) Chair Carry
c) Three Person Carry
d) Two Handed Seat
8) This carry allows the victim to swing their leg using the rescuers as a pair
of crutches.
a) Blanket Drag
b) Human Crutch
c) Hammock Carry
d) Crawling Technique
9) What type of carry is desirable for picking up persons and carrying abreast
in a straight for passing through a narrow place?
a) Four-man carry
b) Three-man hammock carry
c) six-man carry
d) Three man carry from one side
Open questions
1) What are the precautions to consider before carrying the causalities with
two arms?
2) Explain the method of two-handed seat:
3) Describe the steps to follow when performing the technique of human
crutch Carry?
Clarify things to consider before attempting carrying the victim with two arms
and legs. 5) List and explain the methods used to sort or selecting the
victim evacuation in other of priority
6) Explain with description the technique of fireman’s carry.7) Describe the method of blanket drag technique for victim evacuation
UNIT 7 NURSING ASSESSMENT OF CARDIO VASCULAR SYSTEM
Key unit competence
Take appropriate action based on findings of nursing assessment of cardio vascular
system
Introductory activity 7.0Observe the image below and respond to the asked questions;
1. Look on the image A and interpret the status of the client?
2. Look on image B:
Where are these two people?
What is the person with white coat doing?3. What is the relationship between B and C
7.1. Specific history taking on cardiovascular system
Learning activity 7.1
1. The images above show the nurse and the client who is complaining for
heart problems.
a) What are the chief complaints the client may present while consulting the
nurse?
b) Outline the questions a nurse will ask to the client for more understanding
the client’s heart’s problems?2. Explain why the history taking is important for cardiovascular assessment?
7.1.1. Specific history taking on cardio vascular system
Among the assessment techniques essential to valid diagnosis, performing a factfinding
history is a key. To obtain adequate history, providers must be well organized
attentive to the patient’s verbal and nonverbal language and able to accurately
interpret the patent’s responses to questions.
In many instances, the history may be more telling than the physical examination.
It is important to take a deep history for signs and symptoms of heart diseases but
also to alert the patient to the need for lifestyle education. The evaluation regarding
smoking, hypertension, exercise habits, diet, profession and personal life behavior
should be conducted. Many complaints are to be investigated like chest pain,
pressure or heaviness, left arm or jaw pain or numbness, dyspnea on exertion,
cough, paroxysmal dyspnea, hemoptysis, syncope, palpitations, fatigue and
edema. Complaints indicating peripheral ventricular diseases such as claudication,
skin changes especially in the lower extremities, dependent edema, or pain, also
should be investigated.
Determine the date of the last chest x-ray and electrocardiogram (EKG). Inquire
about comorbid conditions or other factors that may increase the patient’s risk forheart disease and peripheral vascular diseases.
c. Past Medical History
History of heart disease includes any previous diagnoses of congenital heart disease,
murmurs, palpitations, arrhythmias, abnormal EKGs, acute coronary syndrome,
angiography (Angiography or arteriography is a medical imaging technique used
to visualize the inside, or lumen, of blood vessels and organs of the body, with
particular interest in the arteries, veins, and the heart chambers), angioplasty(is a
minimally invasive endovascular procedure used to widen narrowed or obstructed
arteries or veins, typically to treat arterial atherosclerosis), stent placement (A
stent is a tiny, expandable metal mesh coil put into the newly opened area of the
artery to help keep the artery from narrowing or closing again), or coronary artery
bypass graft (is a surgical procedure to restore normal blood flow to an obstructed
coronary artery).
In summary: Note whether there have been any heart attacks, any history of
angina and any cardiac procedures or operations (type and date of intervention
and outcome). Previous levels of lipids if ever checked or known. Ask whether there
is any history of rheumatic fever or heart problems as a child.
d. Family History
Family history is particularly important for cardiac assessment because hypertension,
hyperlipidemia, and other vascular diseases often have a familial association that
is not easily ameliorated by lifestyle changes. If there are deaths in the family
related to cardiovascular, determine the age and exact cause of death, because
cardiovascular disease at a young age in the immediate family carries an increased
risk compared with cardiovascular disease in an elderly family member.
Ask about sudden death, which might indicate a congenital disease such as
“Marfan’s syndrome” which is an inherited disorder that affects connective tissue.
This is especially important to ask during pre-sports physicals because sudden
death in athletes is often related to congenital or familial heart disease.
7.1.2. Cardiovascular review of symptoms
The review of cardiovascular symptoms is a list of questions, arranged by
cardiovascular system, designed to uncover dysfunction and disease within that
system. A thorough history is vital for the diagnosis of patients with issues such as
chest pain, heart failure symptoms, palpitations or syncope. The most essential
questions for cardiovascular system review include the following:
• Have you had any shortness of breath? Describe features.
• Do you have chest pain or discomfort?
• Do you notice that your heart is beating faster? Are you having skipped
or extra beats?
• Have you had a loss of consciousness?
• Have you noticed any swelling in your feet, legs, or hands?
• Have you been especially fatigued or tired?
• Do you have blood in your expectoration?
• Have you had difficulty sleeping? How many pillows do you use? Do you
awaken short of breath?• Have you noticed any excessive sweating? Describe features?


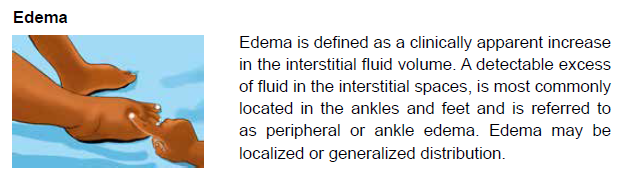
Self-assessment 7.1
1. In case the client consults the health care provider for cardiovascular
problems, the health care provider should take a family history for the
following reason:
a) Family history taking concludes the cardiovascular diagnosis
b) Cardiovascular diseases often have a familial association that is not
easily ameliorated by lifestyle changes Exposure to outdoor allergens.
c) The families who have cardiovascular diseases history have the risks
to have also respiratory diseases
2. Cardiovascular past medical history involves the following except:
a) The history of congenital heart diseases
b) Cardiovascular exams taken (angiogram and electrocardiogram)
c) The habit of physical exercises
3. A clinically apparent increase in the interstitial fluid volume and detectable
excess of fluid in the interstitial spaces is most commonly located in the
ankles and feet and is referred to as:
a) General distributed edema
b) Central edema
c) Peripheral edema
4. The following are attitudes of health care provider to obtain adequate
history:
a) The provider must be well organized
b) The provider must be attentive to the patient’s verbal and non verbal
response
c) The provider must be able to interpret patient’s response to asked
questions
d) All the above
5.During cardiovascular specific history taking the questions should include
the following:
a) Smoking and diet
b) Exercise habit
c) History of intestine disorders
d) Profession and personal life behaviore) A, B, D are true
7.2.General physical examination of cardiovascularsystem
Learning activity 7.1
Analyze carefully the following images and respond to the questions below;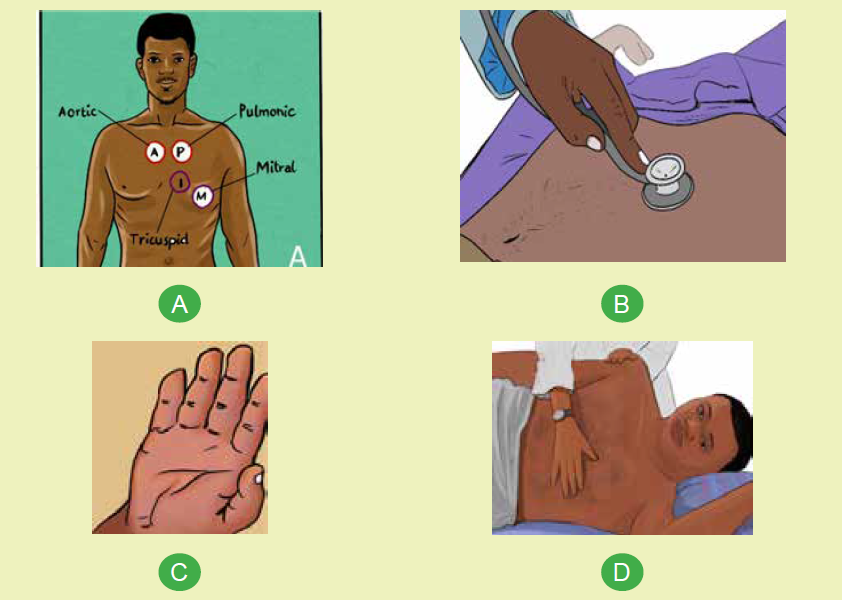
The above images show the physical examination of cardiovascular system;
a) How many heart auscultation locations shown on image A
b) The image B is showing the nurse who is auscultating the client’s heart
beat; name the equipment/material being used?
c) The image C is showing the cyanosis sign which is a bluish discoloration
of the skin due to poor circulation or inadequate oxygenation of the blood;
recall the causes of inadequate oxygenation in blood?
d) The nurse is touching on client’s chest on image D; identify what he/she
can feel on that left side of client’s chest?
The patients with impaired blood circulation may become irritable, somnolent,
restless, confused, or aggressive; the first step for a nurse is to conduct an
initial survey to determine the degree of consciousness if the patient is attentive,
cooperative, and normally oriented.
General signs of heart or circulatory disease include pallor, cyanosis, diaphoresis,
edema, restlessness, and confusion. Diminished or accentuated peripheral pulses
are indicative of Valvular Heart Diseases or tamponade. Jugular venous distention
and hepatojugular reflux suggest an increase in right ventricular pressure.The color and temperature of extremities
During general assessment, nurse may check the person’s. Color of Skin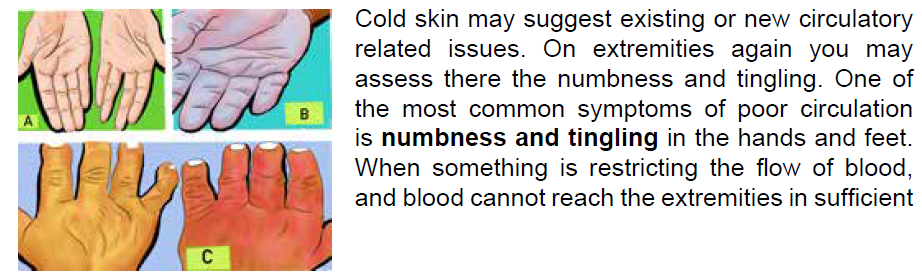
& Mucous Membrane; this may show Cyanosis (a bluish discoloration of the
skin due to poor circulation or inadequate oxygenation of the blood.) which may
suggest inadequate oxygenation and CV compromiseBlood pressure
Usually hypertension is defined as blood pressure above 140/90, and is
considered severe if the pressure is above 180/120.
High blood pressure often has no symptoms. Over time, if untreated, it can causehealth conditions, such as heart disease and stroke.
and count how many seconds until the patient’s full color returns.
• Brisk capillary refill: < (less than) 2 seconds• Delayed capillary refill: > (greater than) 2 seconds
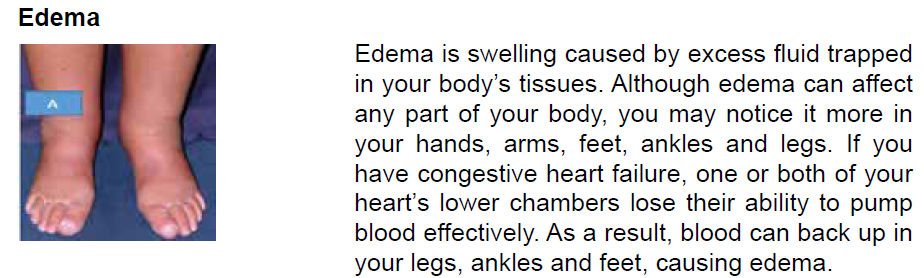
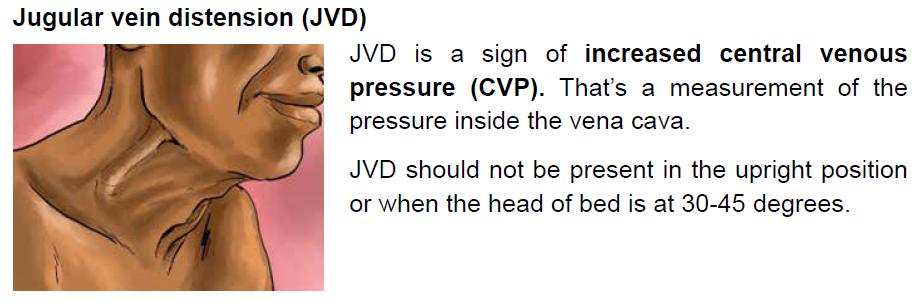
Self-assessment 7.2
1. Explain why it is crucial to assess the level of consciousness to the client
with cardiovascular problem firstly
2. Why Capillary Refill is performed to the patient with poor blood circulation?
3. Why it is necessary to assess the skin of patient with cardiovascular
problems?
4. When you are caring the patient, you observe that he have jugular veindistension(JVD) what is the cause of this JVD ?
7.3. Focused Physical examination of cardiovascularsystem and laboratory test
Learning activity 7.3
The images below illustrate the focused cardiovascular physical exam
1. Describe what you are observing on above images A, B and C?
2. What is common between images A and B?
I. Approach to physical examination of the cardiovascular system
While the patient is in a supine or lateral position, a focused physical examination
can be used to examine the patient’s chest. Inspection, palpation, percussion, and
auscultation are the four steps or procedures used in the process.
A. Inspection
This phase/technique of assessment requires the use of the eye of health care
provider to observe the client for pallor and extremities for cyanosis. A nurse should
observe the neck for jugular vein. A thorough examination of the patient is required,
with special attention paid to short or tall stature, which could indicate Turner’s orMarfan’s syndromes, both of which are connected to congenital cardiac problems.

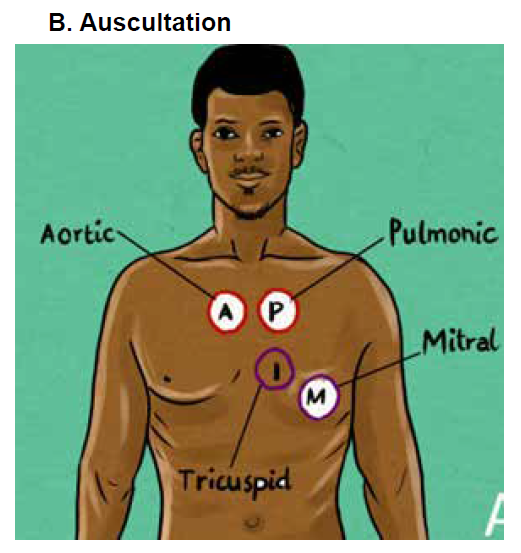
This picture is showing the Cardiac auscultation locations
The most useful element of the heart examination is usually auscultation. A
stethoscope is used to auscultation for heart sounds. Determine the heart’s rate
and rhythm first. Identify S1 (louder at the apex) and S2 (louder at the base) (heard
louder at the base). The diaphragm of the stethoscope is used to identify high-pitched
sounds, while the bell is used to identify low-pitched sounds. There are two normal
heart sounds that should be elicited in auscultation: S1 (lub) and S2 (dub).
Auscultation of Carotid artery: A carotid bruit is a vascular sound caused by
turbulent, non-laminar blood flow through a stenotic region that can be heard with a
stethoscope over the carotid artery. A carotid bruit could indicate underlying artery
occlusive disease, which could result in a stroke. Ask the patient temporarily to stop
breathing. Look for a rushing or blowing sound a bruit. Heart sounds or murmurs
coming from the chest should not be misinterpreted.
Auscultation of the heart: Listen over each of the four main heart valve areas: the
aortic, pulmonary, tricuspid and mitral valve areas. They should also listen for any
additional sounds such as clicks, and heart murmurs which are not normal.
Murmurs are produced by blood flow turbulence and are more prolonged than
heart sounds; they may be systolic
Rubs are high-pitched, scratchy sounds often with 2 or 3 separate components,
which may vary according to body position; during tachycardia, the sound may bealmost continuous.
Location of heart auscultation points

C. Palpation
Palpation of carotid artery is performed by placing the fingers just medial to the
trachea and below the angle of the jaw. The pulse should be regular in rhythm and
have equal strength in the right and left carotid arteries. Don’t palpate both carotid
arteries at the same time or press too firmly. If you do, the patient may faint or
become bradycardia.
Palpation of a sustained apical or ventricular impulse can provide information on
heart size.
• The apex beat, also known as the point of maximal impulse (PMI), corresponds
to the lower left heart border. It is the most inferior and lateral position that the
cardiac impulse can be felt.
• Locate the PMI in the fifth intercostal space in the mid-clavicular line by
counting down from the second intercostal space adjacent to the angle of
Louis.
• Palpate with the first two fingers.
• If this cannot be palpated, ask the patient to lie on his/her left side.
• The apex beat will be displaced laterally if the heart is enlarged (cardiomegaly).
• Next, palpate for heaves and thrills (a thrill is a palpable murmur).
• Place the palm of the hand in each of the four heart zones in the pre-cordium
and then on the upper left and right chest wall. A thrill feels like a vibration or
buzzing underneath your hand.
• Place the hand at the left sternal edge. A parasternal heave is a sign of right
ventricular enlargement and feels like a “lifting feeling” under the hand.
• Assess for jugular venous distention by palpating the liver while breathing
deeply because this may cause hepatojugular which is the distension of the
neck veins caused by applying forceful pressure to the liver.
• Feel the peripheral pulses at the femoral, popliteal, anterior tibial, and dorsalis
pedis locations.
D.Percussion:
Involves tapping on the surface of the body in order to determine the underlying
structure. Because of its limited sensitivity, percussion of the heart borders is rarely
used; it is replaced by x ray
II.Laboratory tests and Interpretations
Cardiovascular screenings can detect issues in major arteries before symptoms
develop, lowering the risk of heart attack, stroke, aneurysm, heart disease, and other
dangerous diseases. These laboratory tests are helpful in diagnosing, monitoring,
and treating a variety of health conditions, including heart disease.
1. Lactate dehydrogenase (LDH), normal value: 45–90 u/L
the significance is that is damaged, an enzyme is released. Hemolytic conditions,
hyperthyroidism, kidney illness, stomach cancer, and megaloblastic anemia can all
cause an increase.
2. Creatine phosphokinase (CPK), Normal value: 55–170 u/L for men; 30–
135 u/L for women
CPK is elevated in MI but not specific to myocardial damage. Also seen with skeletal
muscle damage owing to excessive exercise or rhabdomyolysis.
3. Creatine kinase-myocardial band (CK-MB), normal value: 0–3 ng/mL
the significance is This cardiac is enzyme is most sensitive in detecting myocardial
injury within the first 3 to 8 hours after onset of ischemia symptoms.
4. Troponin I (cTnI)
The normal value is < 0.35 ng/mL. This index is useful in the diagnosis of acute
myocardial injury. After 4 hours, it is equally as sensitive as CK-MB for up to 48
hours. Troponin I remains elevated longer than CK-MB and is more cardiac specific.
5. Troponin T (cTnT), normal value: <0.2 mg/L
The sensitivity of cTnT for detecting acute MI is 100% from 10 hours to 7 days after
onset. The sensitivity begins to decrease after 7 days.
6. Potassium (K+), normal value:
3.5–5 mEq/L. Above all, high K+ levels can lead to ventricular fibrillation. Wider
P waves, peaked T waves, expanded QRS complex, depressed ST-segment,
and heart block are further EKG alterations. Inverted T waves, U waves, and a
depressed ST segment are all symptoms of low K+. Patients with low K+ levels are
at risk of digitalis toxicity.
7. Sodium (Na+), Normal value:135–145 mEq.
Na+ is important for fluid balance particularly when dehydration may be an issue or
in heart failure, where Na+ less than 130 indicates a poor prognosis.
8. Calcium (Ca+), normal value: 8.5–10.6 mg/dL
The hypercalcemic effects on the heart include shortening of the QT interval and
atrioventricular block. The effect of hypocalcemia is prolongation of the ST-segment.
9. Glucose, normal value: 70–100 mg/dL
Changes in blood glucose can have indirect effects on the heart. Diabetes
significantly increases the risk for MI and hyperlipidemia.
10. Creatinine, normal value: 0.6–1.2 mg/dL
Chronic renal illness can raise blood pressure, increasing the risk of cardiovascular
and cerebrovascular disease over time. When prescribing certain drugs for
hypertension and heart failure, such as ACE inhibitors and diuretics, the level of
creatinine is also significant. If the creatinine level is higher than 1.5, a loop diuretic
should be used instead of a thiazide diuretic.
11. Cholesterol, normal value: Total, < 200 mg/dl, LDL, < 130 mg/dL HDL,
> 40 mg/dL
Increased total and LDL cholesterol, as well as lower HDL, raise the risk of coronary
artery disease. Obesity, thyroid problems, or a high-fat diet may be the cause, which
can be hereditary or acquired.
12. Triglycerides, normal value: < 150 mg/dL
Elevated levels increase the risk for heart disease.
13. Thyroid-stimulating hormone (TSH), normal value: 0.4–4.2 mIU/L
Hypothyroidism in the elderly may lead to the development of HF. In adults over the
age of 50, hyperthyroidism can manifest as atrial fibrillation or other arrhythmias.
14. Hemoglobin (Hgb), normal value: 11.5–15 g/dL
Many types of cardiac disease can cause or be caused by anemia.
15. Hematocrit (Hct), normal value: 34%–44%
Anemia may be a cause or a result of many forms of heart disease.
16. Oxygen saturation, normal value: 95%–97%
Pulse oximetry can be used to assess clinical state in individuals with severemyocardial injury and HF.
Self-assessment 7.3
1. Explain element which is most useful during cardiovascular physical
examination
2. Patient with cardiovascular problem may have hypoxia, what will you
focus on the skin during inspection
3. Explain why it is important to know Hemoglobin to the patient who have
cardiovascular problems4. What do you understand with the term hepatojugular
7.4. Interpretation of specific findings on cardiovascularsystem
Learning activity 7.4
The above images B and C show the abnormal hearts and a nurse who is
interpreting heart sounds with stethoscope;
1) Recall the heart normal findings from auscultation
2) Recall the heart normal findings from inspection
3) List the cardiovascular abnormal findings from palpation
The image A is showing a nurse taking hematologic sample;
1) What is normal value of hemoglobin?2) What is the condition which can cause a decreased level of hemoglobin?
7.4.1. The normal findings and abnormal findings fromcardiovascular physical examination

7.4.2. Normal heart sounds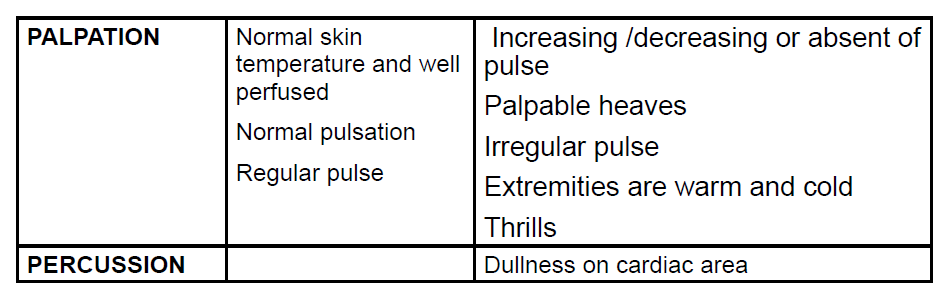
Normal heart sounds are S1 and S2. Identify S1 as lub and S2 as dub. S1 is heard
in the tricuspid area. S2 signals the end of systole and beginning of diastole as the
aortic and pulmonic valves close.
S1 is generated by vibrations created by the closing of the mitral and tricuspid
valves in the heart. When the two ventricles contract and pump out blood into the
aorta and pulmonary artery, these valves close to prevent the blood flowing back
into the atria.
The ventricles relax to receive blood from the atria after pumping blood, and the
diastole phase begins. The second heart sound, S2, is produced when the aortic
and pulmonic valves close and induce vibrations. The increase in volume of this
sound could suggest a number of things.
7.4.3. Abnormal heart sounds
A heart murmur is an unusual sound heard between heartbeats.
A murmur is a blowing, whooshing, or rasping sound that occurs during your
heartbeat.
S4 in late diastole, right before S1, sounds like “lub-lub dub.” It is usually abnormal.
The third heart sound is a low-pitched sound audible with the rapid rush of blood
from the atrium into the ventricle as it starts relaxing. This may be a normal sound
in some people but in people with heart conditions, S3 may indicate heart failure
A low intensity sound heard right before S1 in the cardiac cycle is the fourth. This
sound is caused by the ventricle’s rapid slowing of blood flow as the atrial contracts,
which could be a sign of heart disease.
7.4.4. Abnormal percussion sounds
Dullness: Indicates a solid structure on the heart with a fluid-filled area occur due to
dilation of the heart chambers and to a lesser extent due to thickening (hypertrophy)
of myocardial wall. Also, it can occur to patient with pericardial effusion.
7.4.5. Abnormal findings from inspection
Chest deformity (in case of marfan syndrome) With Marfan syndrome, the heart
muscle may enlarge and weaken over time, causing cardiomyopathy, even if the
heart valves are not leaking.
Jugular vein distension: due to the increased pressure of the superior vena
cava causes the jugular vein to bulge, making it most visible on the right side of a
person’s neck.
Clubbing of Nails: This is due to chronic low blood-oxygen levels.
Edema: When the heart’s diseased or overworked left ventricle (heart’s lower
chamber) isn’t able to pump out enough of the blood it receives from the lung
Pallor: This is due to the decreased blood supply to the skin.
7.4.6. Abnormal findings from palpation
Bruits: While you are palpating each carotid artery medial to the sternomastoid
muscle in the neck. Those bruit are (swooshing sounds similar to the sound of
blood pressure) result from turbulent blood flow related to atherosclerosis.
A thrill: a vibratory sensation felt on the skin overlying an area of turbulence and
indicates a loud heart murmur usually caused by an incompetent heart valve.
Irregular pulse: This can be due to current heart attack or scarring from a previous
heart attack, locked arteries in the heart (coronary artery disease), and Changes to
the heart’s structure, such as from cardiomyopathy, diabetes, high blood pressure.
Bounding pulse: The pulse will probably feel strong and powerful if you have
a bounding pulse. You may feel the pulse in the arteries of the neck or throat.
Sometimes it can be seen as it moves the skin in a more forceful way.
Warm or cold extremities: due to the plaque buildup, blood clots or narrowed
blood vessels which lead to poor circulation. When obstacles or narrow paths slow
down blood flow, it›s difficult for the body to send blood to every part of your body
in an efficient way.
7.4.7. Abnormal cardiovascular pattern
Tachycardia: Excessive cardiac frequency, high to the normal, more than 100beatings per minutes for adult
Tachyarrhythmia: when heart beat is fast and irregular.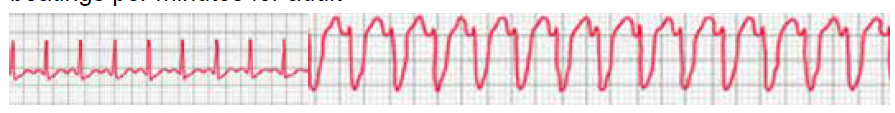
Bradycardia: Low heartbeat rate, less than 60 beatings per minute for an adultperson
Bradyarrhythmia: when heart beat is slow and irregular.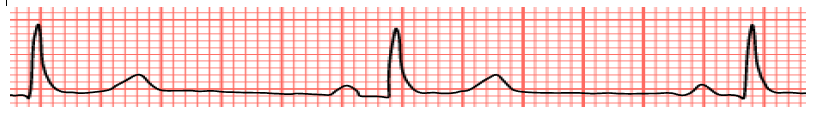
Dysrhythmia or arrhythmia: a pulse with an irregular rhythm
Bounding pulse or dense pulse: When the power of beating is exaggerated, that
means strong contractions, blood volume increases strongly, strong beatings as”
knock”
Falling, weak, depressed or thready pulse: When the pulse becomes difficult to
feel, that it is hardly audible, that means that the power of the beating is lower than
normal.
Self-assessment 7.4
1. Examination of a patient in spine position reveals distended jugular vein
from the base of neck to the angle of jaw. This finding indicates:
a) Increased pulmonary pressure
b) Muddle site heart failure
c) Increased central venous pressure
d) Decreased venous return
2. When you are auscultating the patient heart rate and rhythm you detect
twice an irregular heart beat. You should :
a) Document this normal findings
b) Schedule the patient for another appointment
c) Assess the patient for sign and symptoms of lung diseases
d) Refer the client to a physician
3. The sound generated by the turbulent flow of blood within the heart is:
a) S1
b) Murmur
c) S2
d) Diastole
7.5. Identification of client’s problems and nursing
interventions based on client’s problems
Learning activity 7.5Analyze carefully the following images and respond to the questions below;
Question 1: Describe the image A about different observations hosted in it?
Question 2: Relate the observations of image A with cardiovascular problems
identification?
Question 3: What are different nursing interventions are observed on image B
and their relation with cardiovascular system ?
7.5.1 Cardiovascular client’s problems
Cardiovascular diseases are conditions that affect the structures or functions of
heart; cardio cardiovascular diseases are the leading cause of death. It is important
for a nurse to know about hearts’ problems in order to prevent, assess or provide
nursing interventions to patients who have different heart’s problems.
Types of cardiovascular diseases can have various causes; it is better to know their
difference;
a. Abnormal heart rhythms or arrhythmias
The heart is an amazing organ. It beats in a steady, even rhythm, about 60 to
100 times each minute. That’s about 100,000 times each day. Sometimes your
heart gets out of rhythm. Your doctor calls an irregular or abnormal heartbeat an
arrhythmia. An arrhythmia (also called a dysrhythmia) can bring on an uneven
heartbeat or a heartbeat that is either too slow or too fast.
b. Aorta disease and Marfan syndrome
The aorta is the large artery that leaves your heart and brings oxygen-rich blood
to the rest of your body. The number of conditions can cause the aorta to widen or
tear. This raises the chance of things like: Atherosclerosis (hardened arteries), High
blood pressure and Connective tissue disorders.
c. Congenital heart disease
This is a problem in one or more parts of the heart or blood vessels. It happens
before birth. Genes may play a role, or it can happen if a baby is exposed to viral
infections, alcohol, or drugs before it’s born.
d. Coronary artery disease (narrowing of the arteries)
It’s when plaque builds up and hardens the arteries that give your heart vital oxygen
and nutrients. That hardening is also called atherosclerosis.
e. Deep vein thrombosis and pulmonary embolism
Blood clots can form in your deep veins, usually in your legs. This is deep vein
thrombosis (DVT). They can break loose and travel through your bloodstream to
your lungs, where they can block blood flow. This condition is called pulmonary
embolism. It’s life threatening and needs immediate medical attention.
You might be at higher risk of DVT because of your genes or family history. Other
things that can increase risk include sitting for a long time, like in a car or on a
plane; long-term bed rest; pregnancy; and using birth control pills or hormone
replacement.
f. Heart attack
A heart attack, also called a myocardial infarction, happens when a part of the heart
muscle doesn’t get enough blood.
g. Heart failure
It means your heart doesn’t pump as strongly as it should. This will cause your body
to hold in salt and water, which will give you swelling and shortness of breath.
h. Heart muscle disease (cardiomyopathy)
This is the term for diseases of the heart muscle. They’re sometimes simply called
enlarged heart. People with these conditions have hearts that are unusually big,
thick, or stiff. Their hearts can’t pump blood as well as they should. They can lead
to heart failure and abnormal heart rhythms. Cardiomyopathy may sometimes run
in families, but it can also be caused by high blood pressure, diabetes, obesity,
metabolic diseases, or infections.
i. Heart valve disease
Your valves sit at the exit of each of your four heart chambers. They keep blood
flowing through your heart. Sometimes, there are problems with these valves
j. Pericardial disease
This condition is rare and means the lining surrounding your heart is inflamed. An
infection often causes this cardiac condition.
k. Rheumatic Heart Disease
This happens when rheumatic fever, an inflammatory disease that’s most common
in children, damages your heart valves. Rheumatic fever starts with untreated strep
throat and can affect many parts of your child’s body.
l. Stroke
Strokes happen when something slows or blocks blood flow to your brain. Your
brain can’t get the oxygen and nutrients it needs, and brain cells start to die. When
blood can’t get to the part of your brain that controls a certain function, your body
doesn’t work like it should. A stroke can happen because of a blocked artery or a
leaking or burst blood vessel. It needs immediate treatment to limit brain damage
and other complications.
m. Peripheral vascular disease
Your circulatory system is made up of the vessels that carry blood to every part
of your body. Vascular disease includes any condition that affects your circulatory
system. These include diseases of the arteries that go to your legs (peripheral
vascular disease) and slow blood flow to your brain, causing strokes.
7.5.2 Nursing interventions for a client with cardiovascular
problems
Nursing Interventions
• Monitor for symptoms of heart failure. *Observe for chest pain or discomfort.
• Place patient on cardiac monitor.
• Assess blood pressure carefully
• Administer nitroglycerin with Medical Doctor order.
• Place oxygen.
• Ensure that the IV is in place for emergency use.
• Notify physician.
• Monitor edema, intake, and output.
• Weigh patient daily.
• Auscultate lung and heart sounds. *Administer diuretic with order.
• Elevate head of bed for dyspnea
• Collaborative interventions.
Self-assessment 7.5
1) Cardiomyopathy is the term for diseases of the heart muscle;
A) How is the structure of heart muscle in this condition?
B) List at least causes of cardiomyopathy?
2) Explain how does stroke happen and what can a nurse observe on
client in case of this condition?3) List the nursing interventions toward a client with cardiovascular problems?
End unit 7 assessment
Multiple choices questions
Select the bests answer, only one option is accepted:
1. Rheumatic heart disease happens when rheumatic fever, an inflammatory
disease that’s most common in children, damages your:
a) Heart valves
b) Heart ventricles
c) Heart coronary arteries
d) Heart coronary veins
2. This condition is rare and means that the lining surrounding your heart is
inflamed. An infection often causes this cardiac condition which is called:
a) Heart valves disease
b) Heart muscle disease
c) Pericardial disease
d) Myocardiopathy
3. It is important to take a deep history for signs and symptoms of heart
diseases but also to alert the patient to the need for lifestyle education.
The elements of lifestyle education include the following except:
a) Diet,
b) Smoking,
c) Exercise habits,d) Number of hospitalization
4. If there are deaths in the family related to cardiovascular, the history
taking should determine the age and exact cause of death because:
a) Cardiovascular disease at a young age have low impact in family
b) Cardiovascular disease at a young age has a chance to be cured
c) Cardiovascular disease at a young age carries an increased risk in
family
d) Cardiovascular disease in an elderly family member carries an increased
risk in family
5. Which instrument is used to listen to the heart sounds of the human body?
a) Sphygmomanometer
b) Reflex hammer
c) Stethoscope
d) Heart scope
6. While palpating the apex, left sternal border, the base in an adult client,
you detect a thrill. You should further assess the client for”
a) Pericarditis
b) Cardiac murmurs
c) Congestive heart
d) Left side heart failure
7. While assessing an older adult client, you detect a bruit over the carotid
artery. You should explain to the client that a bruit is
a) A normal sound heard in adult’s patient
b) Wheezing sound
c) Heard when the artery is almost totally occluded
d) Associated with occlusive arterial disease
8. You are planning to auscultate a female patient for carotid arteries. You
should plan to:
a) Ask the patient to hold the breath
b) Palpate the arteries before auscultation
c) Place the stethoscope over the artery
d) Ask the patient to breath as usual
9. The nurse is preparing to assess the patient with cardiovascular problem.
Which phase is most used in physical assessment:
a) Inspection
b) Palpation
c) Auscultation
d) Percussion
10. Bradycardia is a condition in which the pulse rate becomes greater than:
a) 50 beats per minute
b) 60 beats per minute
c) 90 beats per minutes
d) None of the above
Matching questions:A. Relate the heart symptom with its meaning
Short answer questions: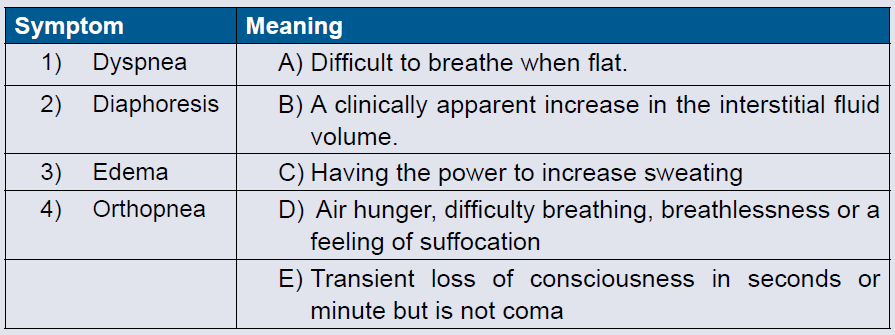
1. List four symptoms of cardiovascular problems the client can present
when is visiting clinic?
2. Label the subjective sensation of conscious perception of heart beats?
3. Recall the elements of family history a nurse should assess forcardiovascular problems?
UNIT 8 NURSING ASSESSMENT OF DIGESTIVE SYSTEM
Key unit competence
Take appropriate action based on findings of nursing assessment of digestive
systemIntroductory activity 8
What do you think is illustrated on image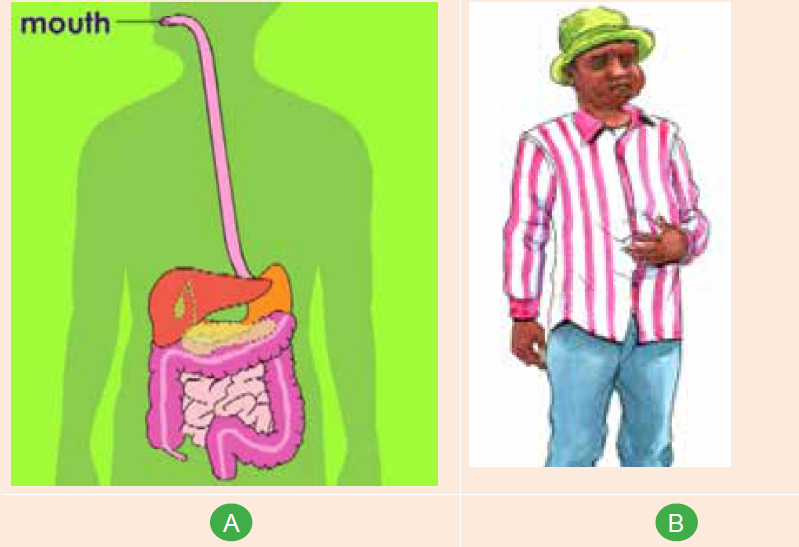
a, b and c ?
The functions of the gastrointestinal (GI) tract and its accessory organs are essential
for life. The process of digestion supplies nutrients to each and every cell in our
body, therefore, if there is a disruption in any of these mechanisms, the whole body
suffers.
8.1. Overview of the digestive system and terminologiesused
Learning activity 8.1.
Mr. Z. underwent a surgical intervention called appendectomy.
1. Locate the appendix on the anatomic model2. Explain the meaning of the word appendicectomy.
8.1.1. Overview of digestive system
The Digestive Tract Also called the gastrointestinal (GI) tract or alimentary canal
Is a muscular tube which Extends from the mouth to the anus. It Passes through
the pharynx, esophagus, stomach, and small and large intestines. It is composed
of the upper GI tract (oral cavity, esophagus, and duodenum), lower GI tract (small
intestine, cecum, colon, rectum, and anus), and associated glandular organs
(gallbladder, pancreas, and liver). The digestive system is responsible for ingestion,
mechanical processing, digestion, secretion, absorption, immunity and waste
excretion.The picture 8.1 illustrates the alimentary canal and the duration that each step take
8.1.2. Some of medical terminologies related to digestive system
A. PREFIXES
This section contains prefixes that are used for the medical terminology. Prefixesare used at the beginning of a word to modify or vary the meaning of the word.
B. SUFFIXES
Suffixes are placed at the end of a word root or word part to modify or vary themeaning. Suffixes can indicate a condition, disease or a procedure.
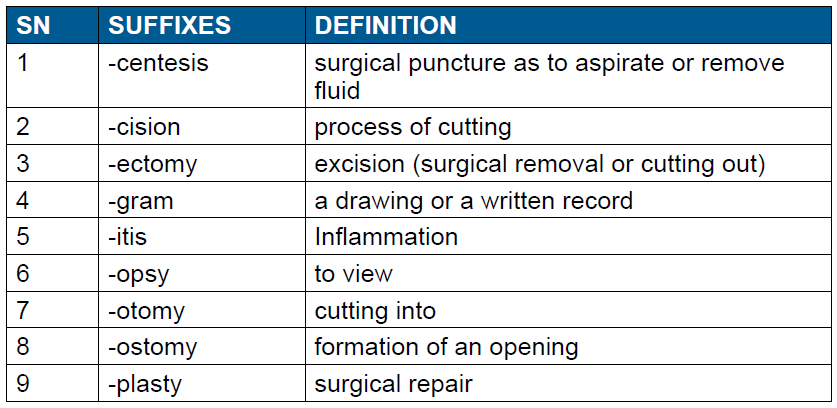
C. WORD ROOT AND COMBINING VOWEL FOR THE GASTROINTESTINAL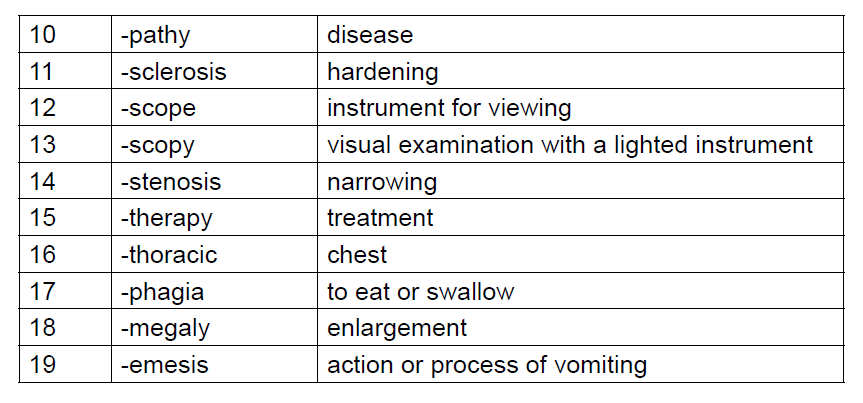
SYSTEM
This is a list of some word roots with their combining vowel used for the gastrointestinalsystem.
Self-assessment 8.1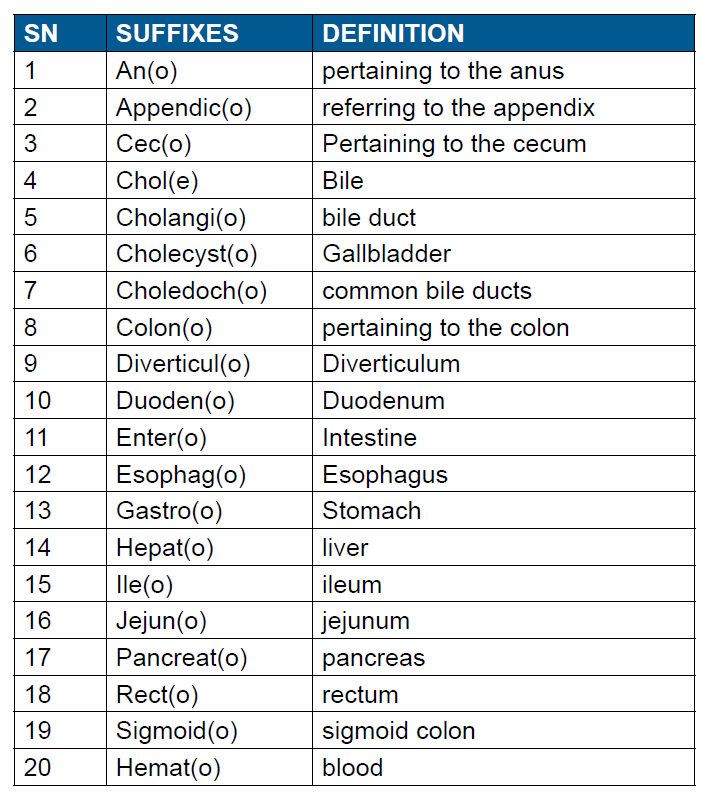
1. Show the main three components of the digestive system on the followingimage
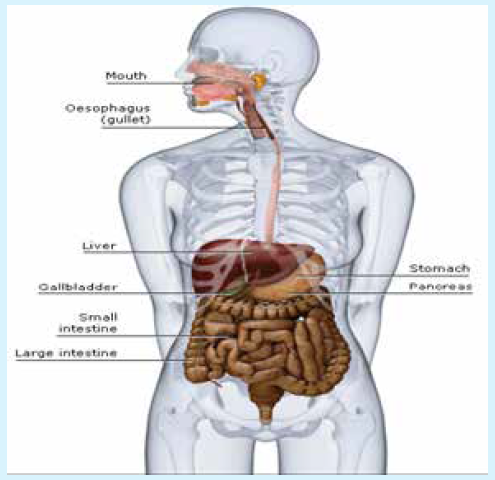
2. Relate the terminologies with their meaning
8.2. History taking on digestive system
Learning activity 8.2.Observe careful the image below and respond to the following question
1. Predict what is happening in Image A
2. Outline the commonly reported symptoms of the gastrointestinal tract
The patient history is key to evaluating gastrointestinal (GI) tract disorders and should
include the problem onset, the setting in which it developed, and its presentation.
Patient warning signs and alarm symptoms should be identified quickly and when
referral is needed for further evaluation and intervention, it should be obtained in a
prompt manner.
The gastro intestinal tract starts from the mouth to the anus and any part of it can
be affected by a pathology. The purpose of history taking is to obtain a clear and
detailed picture of the patient’s complaints. Therefore, it is used to narrow the focus
of the diagnostic and therapeutic plan for the patient.
8.2.1. History of presenting complaint
The Healthcare provider who is going to take the patient history will wash the hands,
introduce him/her(self) to the client, have the client’s names and date of birth, have
the consent and ensures that the client is in a comfortable seating.
Every sick person presents at the consultation room for a certain reason; that
reason for looking care is the presenting complaint (s).
In order to elicit the client’s presenting complaint, it is recommended to allow the
client time to answer, try not to interrupt or direct the conversation, and help the
client expand on their PC (Presenting complaint).
There are a many GI (Gastro intestinal) symptoms and some can be specific to
the upper GI tract, some to the lower GI tract and others can be specific to the
hepatobiliary system.
a. Common symptoms of the gastro intestinal tractA variety of symptoms can arise from Gastro intestinal tract (GIT) dysfunction.

In addition to collecting information on current complaints, a thorough patient history
should gather information concerning medical history, social and family history,
and current medications. The healthcare professional should ask guided question
focused on determining the symptom’s onset, location, severity, and duration,
setting in which symptoms developed, aggravating and alleviating factors, and
associated symptoms of the complaint.
The symptom onset often provides important information that helps formulate a
differential diagnosis. For example, biliary colic or pain, such as that encountered
with symptomatic gallstone disease, typically evolves over minutes and is present
for hours, but pain caused by pancreatitis evolves over hours and lasts for days.
Also, the setting is always relevant as it provides clues to the possible origin of
the disorder. For example, in the patient with complaints of reflux or ulcer disease,
obtaining information as to whether the pain is alleviated or worsened by food or
diminished when administered acid-suppressive therapy can help guide diagnostic
and therapeutic interventions. For instance, ingesting a meal often relieves the pain
of duodenal ulcer, but worsens pain due to a gastric ulcer.
During History taking, the healthcare professional should ask questions that
address potential etiologic possibilities, including motility disorders, structural
diseases, malignancies, infections, psychosocial factors, dietary factors, and travelassociated
diseases.
Furthermore, a good cardiopulmonary history is also extremely relevant and should
be performed during the overall history. Questions concerning medical and family
history detailing illnesses, surgical interventions, injuries, foreign travel, living
conditions, and habits are valuable.
Always end by discussing the patient’s ideas, concerns & expectations(ICE). The
following questions may be asked:
1. Do you have an idea about what could be going on?
2. Is there anything that is worrying/concerning you at the moment?
3. Is there anything you were hoping for from this consultation?4. Do you have any further questions today?
Self-assessment 8.1
Watch a video of history taking and do a role play in pairs of history taking ondigestive system
8.3. Physical examination of digestive system
Learning activity 8.3.
The image illustrates the four quadrants of the abdomen that guide duringphysical assessment
1. List the materials that might be needed for abdominal physical assessment
2. Indicate the techniques which can be used for abdominal physicalassessment.
A comprehensive evaluation of the patient should be performed with notable
attention to physical appearances and vital signs as they may suggest signs of
systemic conditions eliciting gastro intestinal (GI) symptoms.
Communication during physical examination must be respectful and performed
in a culturally-sensitive manner. Privacy should be ensured, and the healthcare
professional needs to be aware that postures, body language, and tone of voice are
transmitting a message.
When performing a focused assessment, you will use at least one or all of the
following four basic techniques during your physical exam: inspection, auscultation,
percussion, and palpation. These techniques should be used in an organized
manner from least disturbing or invasive to most invasive to the patient.
Inspection is first, as it is non-invasive. Auscultation is performed following
inspection; the abdomen should be auscultated before percussion or palpation to
prevent production of false bowel sounds. For accurate assessment of the abdomen,
patient relaxation is essential. The patient should be comfortable and should have
an empty bladder. The environment should include a comfortable temperature, with
good light.8.3.1. Inspection of the abdomen
For the purpose of assessment, the abdomen can be divided into four quadrants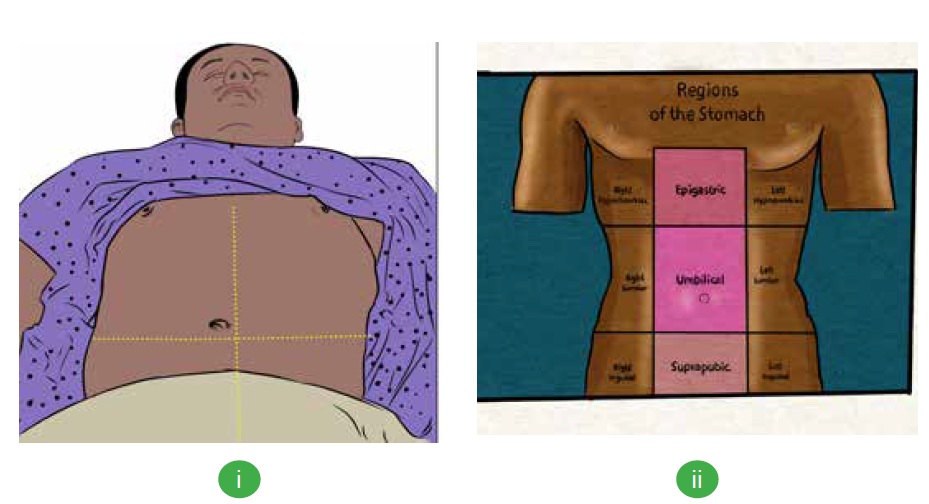
(see image i above) or nine quadrants for descriptive purposes (see image ii above).
Inspection of the abdomen may reveal scars, hernias, masses, ascites or peristalsis.
The four quadrants include the right upper quadrant, left upper quadrant, right
lower quadrant, and left lower quadrant.
When assessing the abdomen, it is important to make the patient as comfortable as
possible. Following are the steps for inspection of the digestive system:
1. Position the patient in a lying (supine) position with their head and knees
supported by a pillow. Alternative positions are lying with knees bent or
a side-lying position. Always make sure the client is in as comfortable
position as possible
2. Be sure and remove the clothing or lift the gown.
3. Check the skin for any rashes, scars, lesions, masses or bulges, surgical
incision….
4. Inspect the contour of the abdomen, is the abdomen flat, rounded, scaphoid,or protuberant?
5. Inspect the abdomen for symmetry. The abdomen should be symmetrical
bilaterally. Inspect the umbilicus.
6. Check for any types of equipment such as G-tube, drains, ….8.3.2. Auscultation of the abdomen
Auscultation of the abdomen should
always be done after inspection and
before percussion and palpation as
they can alter the bowel sounds.
Auscultation should begin in the right
lower quadrant. If bowel sounds are not
heard, in order to determine if bowel
sounds are truly absent, listen for a total
of five minutes. It is suggested that you
listen to bowel sounds for a full minute before determining if they are normal,
hypoactive, or hyperactive. An example of a video demonstrating abdominal
auscultation can be viewed at:
Following are the steps for auscultation of the digestive system:
1. Use the diaphragm of the stethoscope and apply light pressure.
2. Auscultate the abdomen in all four quadrants.
3. Listen for bowel sounds, noting the characteristic and frequency.
4. Listen for bruits or any vascular sounds.8.3.3. Percussion of the abdomen
Percussion of the abdomen is used
to assess for the amount of gas in the
abdomen. Also, it can be used to identify
organs, masses or to elicit tenderness
and sounds that give clues to underlying
problems.
Percussion can help estimate the
size of the liver or spleen. Percussion
of the abdomen allows for detection of
tympany, measurement of visceral
size, and detection of ascites. It is may be difficult to percuss the liver as most
of it is covered by the ribcage. Dullness is heard when percussing the liver
through intercostal space. The spleen’s percussion is easier when it enlarges.
It usually extends forward, downward and to the sides. The abdomen is
percussed in all four quadrants to assess areas of tympany and dullness.
Tympany is usually heard over a gas-filled area while dullness is heard over
solid masses or organs.
Following are the steps for auscultation of the digestive system:
1. Press the distal part of the middle finger of your non-dominant hand firmly
on the body part.
2. Keep the rest of your hand off the body surface.
3. Flex the wrist, but not the forearm, of your dominant hand.
4. Using the middle finger of your dominant hand, tap quickly and directly over
the point where your other middle finger contacts the patient’s skin, keeping
the fingers perpendicular.
5. Listen to the sounds produced. When examining the abdomen, percuss for
general tympany, liver span, and splenic dullness. Tympany should be the
predominant sound when percussing the abdomen while Dullness is usually
heard over solid organs or masses such as the liver, spleen, or a full bladder.
An example of a video demonstrating abdominal percussion can be viewed at:
Percussion is contraindicated in patients with suspected aortic aneurysm,
appendicitis, or those who have received abdominal organ transplants
8.3.4. Palpation of the abdomen
Palpation is another commonly used physical exam technique that requires the
examiner to touch the client with his/her hand(s). Palpation may allow to identify
tenderness, rigidity, masses, and hernias. The client will be always asked if they
have any areas of pain before beginning palpation. The painful areas are palpated
last.
Palpation allows you to assess for texture, tenderness, temperature, moisture,
pulsations, masses, and internal organs. Normally, there should be no tenderness
on either light or deep palpation of the abdomen.
Following are the steps for auscultation of the digestive system:a. To lightly palpate the abdom

Light palpation
1. With the fingers together, place
the hand flat on the abdomen.
2. Lightly palpate the abdomen
using a dipping motion.
3. Raise the hand off the skin
while moving from one place toanother.
2. Palpate all four quadrants.
3. Check for tenderness.
4. Palpate for any superficial organs or masses.
5. Notice if the patient is guarding while palpating.b. To deeply palpate the abdomen:

Deep palpation
1. Use the palmer side of the hand.
2. Palpate all four quadrants.
3. Assess for masses noting the
location, size, and shape.4. Check for tenderness.
c. To palpate the liver:

Liver palpation
1. Stand on the right side of the
client.
2. Place your left hand behind the
client around the 11th or 12th rib.
3. Have the patient relax their back
onto your hand?
4. Press your left hand forward as the client relaxes into it. This pushes the liver
forward and makes it easier to palpate with your right hand.
5. Place your right hand on the right side of the client’s abdomen.
6. Place your fingertips at the lower border of the costal margin.
7. Press gently inward and upward on the abdomen.
8. Ask the patient to take a deep breath so you can feel the borders of the liver
as it moves under your fingers.
9. Ask the patient if they have any tenderness.
While assessing the abdomen, remember that palpation and percussion are
contraindicated in patients that are suspected for having a diagnosis of an
abdominal aortic aneurysm, appendicitis and other conditions. Always check forcontraindications before beginning an abdominal assessment.
Self-assessment 8.3.
Answer whether the statement is true or false
1. During physical examination communication have be respectful and the
procedure is performed in a culturally-sensitive manner.
2. For the purpose of assessment, the abdomen is divided into four
quadrants.
3. Palpation is always done before auscultation for physical assessment of
the digestive system
4. The client is asked if he/she has any areas of pain before beginning
palpation and the painful areas are palpated first to identify any emergency
situation.
5. Tympany sound is heard when percussing the liver.6. Dullness is usually predominant while percussing the abdomen.
8.4. Interpretation of specific findings on digestive
system
Learning activity 8.4.
The image shows some of the problems occurring to the digestive system
1. Describe the symptoms that you think may occur to a client presenting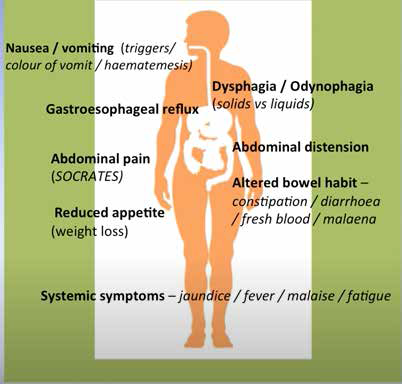
with digestive system disease conditions
8.4.1. Interpretation of some findings from physical assessment
A. Some definitions
• Ascites is an abnormal accumulation of serous fluid in the abdominal cavity
containing large amounts of protein and electrolytes.
• Bulge is a protruding part; an outward curve or swelling.
• Cirrhosis is a chronic disease of the liver characterized by the replacement
of normal tissue with fibrous tissue and the loss of functional liver cells.
• Hernia is the protrusion of an organ or other bodily structure through the
wall that normally contains it.
• Food intolerance is inability to completely digest a type of food, usually due
to an enzyme deficiency
• Referred pain is a pain sensation experienced in one part of the body that
is different to the actual area of pathology.
• Visceral pain is a pain related to the internal organs.
• Esophageal varices are abnormally dilated or swollen vessels in the
esophagus, which can lead to bleeding.
B. Abdominal shape
• A flat abdomen is commonly seen in a person of normal weight. There is
a straight line from the costal margin to the symphysis pubis.
• A rounded abdomen has a convex shape. This usually indicates additional
fat around the abdominal area however a rounded abdomen is normal in
pregnant women and toddlers.
• A scaphoid abdomen has a concave shape. From the side, the abdomen
looks sunken. This shape is usually seen in patients who are extremely
thin.
• A protuberant abdomen is seen in people who are obese or have ascites.
The abdomen is extremely rounded. This shape is seen in women who are
pregnant but is also seen in men with ascites.
C. On inspection
• If a protrusion is noticed around the umbilicus or any incisions, a hernia may
be present.
• Peristalsis is not normally visible but, can be visible with an intestinal
obstruction.
• Pulsations can sometimes be visualized with an abdominal aneurysm.
• Jaundice is the yellow color of skin and mucous membranes due to
accumulation of bile pigments in blood and their deposition in body tissues.
• Cholestasis refers to a decreased rate of bile flow.
Depending on the clinical situation, jaundice and cholestasis may coexist or each
may exist without the other. Although many sources confidently say that jaundice
can be recognized when the serum bilirubin rises to 2 to 2.5 mg/dl, experienced
clinicians often cannot see a yellow skin coloration until the serum bilirubin is at
least 7 to 8 mg/dl.
C. On auscultation
The table describes how different bowel sounds are produced and what they mayindicate.
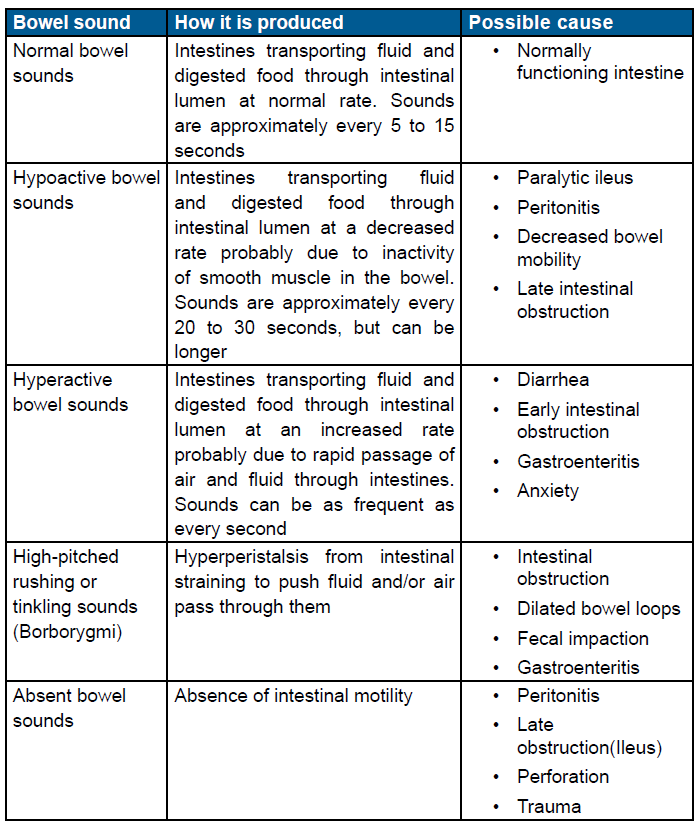

D. Pain scale
The pain is rated on a scale of 10 in order to have an idea of its intensity and
plan the intervention accordingly. The following facies indicate the level atwhich a patient is suffering and the score related to it.

8.4.2. Interpretation of some findings from laboratory findings
There are many common laboratory exams that help in the assessment of client’s
gastrointestinal system and accessory organs. Lab values should be looked
at collectively in the context of a complete abdominal history and examination.
The following table illustrates examples of lab values and the possible relatedgastrointestinal disturbances.

N.B: Normal lab value reference ranges may differ from institutions. Always check
with the facility’s protocol.
Self-assessment 8.4.
CHIEF COMPLAINT: My eyes are yellow for two days.
HISTORY OF PRESENT ILLNESS: Mrs. S is a 36 year old unemployed woman
who presents with yellow discoloration of her eyes which she noticed two days
ago while washing her face. At first she thought the color was due to the lighting
in her bathroom, but this morning, when going outside, she noticed that her
hands “looked yellow.”
Mrs. Salco further admits to feeling “sick and tired” for the past 2 -3 weeks. She
has lost her appetite and feels weak. During this time, she has been frequently
nauseated and ate very little food. Last night she developed a fever and “shook
all over with a chill.” This morning she awoke after a restless night with pain and
a sensation of fullness in the right upper abdomen. She also vomited twice. The
emesis was non -bloody. She has not had diarrhea. She has no back or shoulder
pain. She thinks she lost 7kg during the last 3 months. She has no joint pain or
skin rash.
Mrs. Salco is a chronic alcoholic who has been hospitalized on several occasions
for alcohol related problems, including a psychiatric admission at Ndera Neuro –
psychiatric hospital. Although she was considered as a gifted, young accountant
with a bright future. Since graduation from business and Management school
she has had many alcohol related work problems and lost her position at
a prestigious company three weeks ago. Since that time she has consumedapproximately 3 bottles of Red Waragi (alcohol spirits) every day.
The relationship with her husband is not good these days and she is taking
Paracetamol regulary to calm her headache. She smokes one pack of cigarettes
per day. She is having an affair with a man who uses IV drugs and has history
of hepatitis.
PHYSICAL EXAMINATION:
–– The patient is alert but haggard looking. She is skinny and shows prominent
cheek bones. Her clothing is disheveled and her hair is uncombed. She
appears much older than her stated age. Bilateral, deep conjunctival
icterus
–– Vital signs: Blood pressure in right arm 104/60 mmHg, Heart Rate 110/
minute and regular, Respiratory Rate 18/minute, Temperature 38.90 C.
ABDOMEN: The abdomen is round and slightly tympanitic. The liver is palpable
beneath the costal margin (9 cm.) and tender. The liver span is 20 cm. There is no
rebound tenderness, shifting dullness or splenomegaly. Normal bowel sounds.
SKIN: Icteric
LABORATORY DATA:
Aspartate arninotransferase (AST) 150 U/L
Alanine aminotransferase (ALT) 60 U/L
Total Bilirubin 22 mg/dL
During, hospitalization WBC rose to 42,000/mm3; total bilirubin rose to 32 mg/dL
1. Cite the main clinical reason for consultation of Mrs S.
2. Elicit other significant clinical problems that Mrs S. has.3. Recommend the possible differential diagnoses for Mrs S.
8.5. Identification of client problems
Learning activity 8.5.Observe the pictures carefully and answer the asked questions
1. Describe what Picture A, B, C and D are showing?
2. What does picture A and B have in common?
8.5.1. Abdominal pain
Pain can be subjective or objective. The patient will point to the location of the
pain, the nature of the pain and any aggravating or relieving factors, how often
the pain felt and how long it lasts and if there is radiation elsewhere (SOCRATES
Site, Onset, Character, Radiation, Associated symptoms, Time, Exacerbating/
relieving, Severity). Abdominal pain related to gynecological matters have to bedifferentiated from the one originating from the digestive system.:
8.5.2. Appetite and eating disorders
Appetite and eating can be influenced by many factors that may indicate
gastrointestinal disease or that can be attributed to socioeconomic considerations
such as food availability, family norms, peers, and cultural practices.
• A loss of taste sensation can contribute to loss of appetite and potentially result
in poor nutrition, especially in older individuals. Attempts at voluntary control
can be a factors, such as dieting or eating disorders. Appetite disorders may
result in weight loss which can also be associated with illness, while weight
gain may be attributed to fluid retention or a mass.
• On the other hand, dysphagia which is difficulty swallowing may occur. Some
people may be completely unable to swallow or may have trouble swallowing
liquids, foods, or saliva. Eating becomes a challenge, making it difficult to take
in enough calories and fluids to nourish the body. The patient will be asked
if they have any difficulty swallowing and when the difficulty first occurred.
People with diseases of the nervous system, such as cerebral palsy or
Parkinson’s disease, often have swallowing problems. Additionally, stroke or
head injury may affect the coordination of the swallowing muscles or limitsensation in the mouth and throat.
• Moreover, nausea and vomiting may indicate food poisoning. Questions
about types of food eaten in the past 24 hours should be asked to rule out
potential poisoning. If vomiting is present, you will want to ask about the
amount, frequency, color, and odor of the vomitus.
• Hematemesis, or blood in the vomitus, is a common symptom of gastric or
duodenal ulcers and may also indicate esophageal varices. Coffee ground
emesis indicates an “old” gastrointestinal bleed. The old, partially digested
blood appears to look like coffee grounds.
• Changes in Bowel Habits is a common manifestation of gastrointestinal
disease. The frequency, color, and consistency of bowel movements, use of
laxatives.
8.5.3. Ascites
Usually seen in patients with cirrhosis of the liver. The patient will have a protuberant
abdomen. It is caused by increased hydrostatic pressure in patients with cirrhosis
of the liver. Percussion is normally used for the assessment of ascites, however,
there are other methods. An abdomen with ascites will have both tympanic and dull
sounds.
You will hear tympany at the top of the abdomen around the epigastric area and
dullness will be heard lower around the umbilicus or any dependent areas of the
abdomen.
8.5.4. Nursing diagnoses
According to different domains of diagnosis by NANDA, examples of nursing
diagnosis can be set down; Imbalanced nutrition, Impaired swallowing, Obesity,
Overweight, Abnormal distention, Pain, Diarrhea, Constipation, Bowel incontinence,
Excess fluid volume, Fluid volume deficit, Fatigue, Risk for infection, Lack of
knowledge, Anxiety, and Disturbed body image.
Note that alterations in gastrointestinal assessment findings could indicate
potential problems and being knowledgeable about the focused, gastrointestinal
assessment will allow the healthcare provider to intervene quickly and appropriatelyfor gastrointestinal disorders
Self-assessment 8.5.
1. Client X is admitted at the Hospital for an intensive pain of 7/10 located
in her hypogastric region. In your judgement, mention 2 health problems
that might be the underlying causes of this pain.
8.6. Nursing intervention based on patient’s problemLearning activity 8.6.
Mr. Z. is a 26 years old male suffering from peptic ulcer problem which is
worsening as the crises have increased considerably this last year.
1. Do you think you can help Mr. Z as an Associate Nurse?
Within the framework of his or her role, the nurse performs acts or provides care
aimed at identifying risks, ensuring comfort and safety of the person and his or her
environment, and informing the person and his or her family.
Basically for digestive system problems, the interventions will base on care
and procedures to ensure the hygiene of the person and his/her environment,
Supervision of hygiene and dietary balance, Supervision of food intake and
Monitoring of intestinal elimination.
8.6.1. Samples of digestive system problems and theirManagement
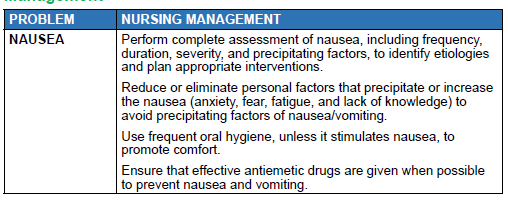
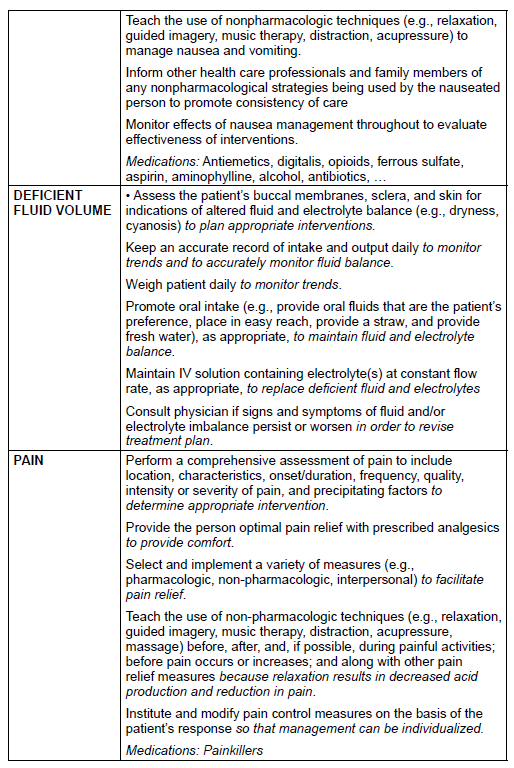
In conclusion, for the digestive system intervention, Implement the appropriate
care for each type of transit disorder, Manage the pain as prescribed, Educate the
patient on foods and preventive dietary measures, Monitor vital parameters and
Reassure the patient
Self-assessment 8.6.
Mr. Z. is a 26 years old male suffering from peptic ulcer problem which is worsening
as the crises have increased considerably this last year. When the nurse asked him
about willingness to modify lifestyle he was doubting and delayed to reply to the Nurse.What would be the nursing interventions to Mr. Z?
End unit 8 assessment
1. Appendicitis means ……………………………………………………………
…………………………….
2. Hepatitis means ………………………………………………………………
……………………………….
3. Dysphagia means ……………………………………………………………
…………………………………
4. Melena means …………………………………………………………………
……………………………….
5. Outline 10 commonly presenting complaints of the gastro intestinal
system at the hospital
6. Explain how, the setting is relevant and can provide clues to the possible
origin of a disorder
7. In conclusion of a history taking session, we should always end by ICE.
Write ICE in full.
8. What can occur as a result of the aging process?
A. Dysphagia
B. Blood in the stools
C. Increase in food intolerance
9. Alcohol can cause liver cirrhosis and ________.
10. Age affect digestion by:
a. Slowing swallowing
b. Overgrowth of bacteria which reduces the amount of nutrients the
intestines absorb
c. Reducing stomach secretions
d. All of the above
11. Most of the digestive process take place in:
a. Small intestine
b. Large intestine
c. Stomach
d. All of the above
12. The liver helps digestion by:
a. Making important enzymes
b. Neutralizing stomach acid
c. Producing biled. Regulating insulin
UNIT 9 NURSING ASSESSMENT OF GENITO-URINARY SYSTEM
Key Unit Competence:
Take appropriate action based on findings of nursing assessment of genito-urinary
system.Introductory activity 9.0
Observe the images above and answer the following questions:
a. What do images above means to you?
b. Guess the lesson we are going to study.
c. List the anatomical parts illustrated on image B and D
Genito-urinary system combines both reproductive and urinary system. The
reproductive system serves to ensure the survival of species. To do so, it produces
ovum and sperm cells, transport and sustain these cells, nurture the growing offspring
and produce hormones. Gonads are the primary organs of the reproductive system;
it consists of ovaries and testes in female and male respectively. These organs
are responsible for producing the ovum and sperm cells and hormones. These
hormones function in the maturation of the reproductive system, the development of
sexual characteristics, and regulation of the normal physiology of the reproductive
system. The remaining organs, ducts, and glands in the reproductive system
are considered secondary, or accessory, reproductive organs. These structures
transport and sustain the gametes and nurture the developing offspring.
The urinary system has its upper part composed of two kidneys and two ureters
while its lower part consists of a urinary bladder and a urethra. The kidneys serve
as principal organs of the urinary system. The main functions of the kidneys are
to (1) regulate the volume and composition of the blood and (2) excrete waste
products from the body in the form of urine. The kidneys also function to control
blood pressure, produce erythropoietin, activate vitamin D, and regulate acid-base
balance. Urine is formed in the kidneys, drains through the ureters to be stored in
the bladder, and then passes from the body through the urethra.9.1. History taking of genitourinary system
Learning activity 9.1
Observe the image above and respond to the following question
a. What does the image A illustrate?b. What can be the reason behind the posture on image B
9.1.1. History taking of the genitourinary system
After greeting, introduction and listening the chief complaint of the patient,
the examiner will decide to ask specific questions to know the health status of
genitourinary system. The patient may report frequency, urgency, nocturia, dysuria,
hesitancy, straining, urine color change, penis pain, lesion and discharge, scrotal pain
and swelling, reduced sexual activity and sexual desire, contraception measures
and past genitourinary history. Menstrual history, obstetric history, menopause,
lower abdominal pain, vaginal discharge, and painful sexual intercourse are usually
female specific.
Here are questions to be used for appropriate history taking of the genitourinary
system:
1. Are you urinating more often than usual? Frequency said when an adult
patient reports to urinate more than 5-6 times per a day. Polyuria is the
excessive quantity of the urine, oliguria is a diminished quantity of the urine
< 400ml/24 hours, whereas anuria is the absence of urine or quantity <
100ml/24 hours. Urgency is when a patient can’t wait to urinate. Awakening
desire to urinate during the night is known as nocturia. The examiner will
go in deep and ask how many times per a night and if it is a recent change.
Frequency, urgency and nocturia mostly happen in urinary tract conditions
2. Do you feel pain or burning sensation during urination? Dysuria is common
in acute cystitis, prostatitis and urethritis.
3. Do you have difficult starting urine stream? Or do you need to strain to start
or maintain urine stream? Hesitancy and straining respectively indicate that
the patient has outlet obstruction due to benign prostatic hyperplasia.
4. What is the color, smell and consistency of the urine? The intensive
yellow to dark color of the urine indicates dehydration, cloudy in urinary
tract infection. Hematuria: presence of blood in the urine is a danger sign
that warrants further investigations. Some color changes are temporary or
harmless. However, for blood in urine or for a color change lasting longer
than a day, seek health care. Hematuria may signal glomerulonephritis,
cancers of prostate or bladder.
5. Do you have difficulty controlling urine? Urge incontinence is when the
detrusor muscle of the bladder is overactive and cause involuntary urine
loss. Stress incontinence is when physical effort, sneezing or coughing
causes involuntary urine falls due to weakness in pelvic floor.
6. Any problem with the penis? These problem can be pain, lesion or discharge.
Urethral discharge is more frequent in urinary tract infection and sexually
transmitted infections.
7. Do you have any problem on the scrotum or testicles? Problems can be
lumps or swelling. A list of complains may be reported by the clients such as
spermatocele, hydrocele, varicocele and rarely testicular cancer.
8. Are you in relationship that involves sexual intercourse? This question is
relevant when assessing genitourinary system and should be gender neutral
to avoid embracing people with different sexual orientation. Ensure that thepatient accept individual’s sexual activity and believe that it is important.
Self-assessment 9.1
1. M.R. is a 19-year-old male student who 2 days noted acute onset of painful
urination, frequency, and urgency. Noted some thick penile discharge. He
is worried because of unprotected sexual intercourse he had last week
with one of his girlfriend.
a. Ask this patient 5 additional questions to ruler out complete subjective
information?
b. What medical condition will you think first to fit the patient’s complaints?
2. I.C. urinates 4 or 5 times/day, clear, straw-colored. No nocturia, dysuria,
or hesitancy. No pain, lesions, or discharge from penis. Does not do
testicular self-examination. No history of genitourinary disease. Sexually
active in a monogamous relationship. Sexual life satisfactory to self and
partner. Uses birth control via barrier method (partner uses diaphragm).
No known STI contact. Objective no lesions, inflammation, or discharge
from penis. Testes descended, symmetric, no masses. No inguinal hernia.
3. What is your conclusion as an associate nurse after getting the aboveinformation from your patient.
9.2. Physical assessment of genitourinary systemLearning activity 9.2
Observe the image above and respond to the following questions
a. What does this image A represent?
b. What is being done by gloved hangs on image B
c. In your own word, comment on abnormalities seen on image C, D, E, Fd. Enumerate the organs sees on image A and B.
The assessment of urinary system will start with inspection then percussion and
palpation of the abdomen. The abdomen must the soft, flat, concave and symmetric.
Observe the color of the costo-vertebral angle and hypogastric region where the
kidneys and urinary bladder are located respectively.
The examiner will make sure that the room is prepared with availability of necessary
materials such as gynecological table, sheets, pillow, gloves, and sample collection
items as needed. The temperature of the room should be warm and privacy is
mandatory to stop any movement in and out of the room during examination.
Clean your hands and don examination gloves. Women may feel apprehensive
about having their genitalia examined, especially if the nurse is male. If necessary,
arrange for a female assistant. Before bringing the woman to the examination room,
ask her to empty her bladder. She should be instructed to undress completely and
put on a gown. Most of the time, the woman will be in the lithotomy position and
asked to remove clothes. The lithotomy position may make her feel embarrassed
and vulnerable. If she seems uncomfortable or embarrassed, you may ask her if
she would like her head elevated so she can see you better. Position her with her
buttocks at the edge of the examination table. Ask her to place her arms at her sides
or across her chest but not over her head (this tightens the abdominal muscles).
Position the sheet completely over the patient’s lower abdomen and upper legs,
exposing only the vulva for your examination. Push the sheet down so you can see
the woman’s face as you proceed. As you start the examination, reassure her that
you will tell her everything that you are going to do before you actually do it. Help
the woman relax and assure her that, if she becomes too uncomfortable, you will
stop what you are doing and reassess what is happening. Please, every step here
must be objective and matter of facts; don’t be tentative with your touch; once you
make physical contact, maintain it for assessment purpose. Be sure to talk to the
woman throughout the examination to tell her what you are doing, what you are
seeing or feeling, and how long it will be until you are finished.
The assessment of GU in both male and female starts by external genitalia. Pubic
area is inspected for normal characteristic and distribution hair per age category.
The skin should be intact, inguinal regions with no erythema fissure or enlarged
lymph nodes. For female, each type of labia is symmetric and equal size to its
homologous. The clitoris allocated above urinary meatus measures about 1 to
1.5cm. The vaginal opening should not show swelling, redness or any protrusion.
Inspect the urethra through its meatus for patency and position. Inspect the
perineum, skin must be intact with no lesion or tears. Note that female who had
episiotomy manifests healed scars. The available findings will direct the examiner
to the advanced assessment cervix and vaginal wall by using the speculum.
Physical assessment of the penis need both inspection and palpation of the its
surface to look at and feel its consistence. It has a visible vein on the dorsal part
identified when inspecting the posterior part. Penis has no edema, discharge, pain,
lesions or nodules. For uncircumcised male the foreskin covers the gland, it is
easily retracted by the patient, some smegma are present. For circumcised male,
the gland is visible, lighter than the shaft and free of smegma.
The external urinary meatus is located centrally on the glands on the tip of the
penis. The external urethral meatus has no discharge, stenosis, or warts. The
glands can be opened by pressing it between thumb and forefinger. The patient can
be instructed to do this. Then request him to milk the penis from the base toward
the glands or head. Note color, consistency, or odor of any discharge. The glands
is smooth and pink with no discharge. Inspect and palpate the scrotum on both its
sides. It is divided into two sacs. The scrotum is hanged asymmetrically, with the
left side lower than the right. The anterior and posterior skin appears darker with
a rugous or wrinkled surface. Palpate each testicle separately. Note the smooth,
rubbery consistency of each testicle; no nodules should be felt. Irregularities in
texture or size may indicate an infection, tumor, or cyst. Palpate the epididymis on
the posterolateral surface of each testicle. It feels smooth and non tender.
In this unit, we are going to learn GU findings that need clinical attention. Starting on
the pubic area, there may be no hair, presence of patchy growth, skin inflammation,
lesions, dermatitis, or infestations. Candidiasis (infection due to candida albicans)
causes crusty, multiple, red, round erosions and pustules. Whereas, Tinea curis, a
fungal infection with large red, scaly, and extremely itchy patches. Bulges or masses
in inguinal areas for male suggest a hernia. Hernias occur when a loop of intestine
prolapses through the inguinal wall or canal or abdominal musculature. The patient
will report pain on exertion or lifting. On examination, pain increases when position
increases intra-abdominal pressure. Testicular irregularities in texture or size may
indicate an infection, tumor, or cyst. The foreskin or prepuce can develop either
phimosis or paraphimosis. Phimosis is when the foreskin can’t be retracted from
the tip of the penis. Paraphimosis is when the foreskin is retracted but can’t move
back up to the tip of the penis. Both phimosis and paraphimosis affect blood flow
in the penis and cause inflammation. Management of these conditions involves
non-steroid anti inflammatory to control pain and inflammation and allow chance
circumcision. Urinary meatus can be allocated upper or lower than the normal
location, these conditions are epispadias and hypospadias respectively. Contact
dermatitis is common in childhood and manifests red, itchy rash caused by direct
contact with a substance or an allergic reaction to it. The rash isn’t contagious or
life-threatening, but it can be very uncomfortable. Various substances can cause
such reactions, including soaps, cosmetics, fragrances, jewelry and plants. The
management of contact dermatitis involves identification and avoidance of thecause, apply skin soothing product or anti histaminic medications.
Self-assessment 9.2
1. Mr. N.S. is entering consultation room in a bent over position, anxious
and guarding genital area. Physical examination revealed redness that
urethral meatus has mild edema with purulent urethral discharge. No pain
on palpation of genitalia. Testes symmetric with no masses.
a. What will you record from the above physical assessment?
b. What will be your nursing intervention to this patient?
2. D.C. 27-year-old married woman with Parity 1. Presents at clinic with
urinary burning, vaginal itching, and whitish curdy discharge since 4
days ago. After physical examination, vaginal sample showed spores of
Candida Albicans.
a. Which medical condition would you pose for this woman?
3. B.L., 17-year-old female high school student, comes to clinic for oral
contraceptives. She had menarche at 12 years, cycle every 30 days,
duration 4 days, mild cramps relieved by Ibuprofen. LMP 7 days ago.
No dysuria, vaginal discharge, vaginal itching. Relationship involving
vaginal intercourse with one boyfriend for since 6 months. She thinks
that her boyfriend is involved in other heterosexual contacts. For birth
control boyfriend uses condoms sometimes. Wants to start birth control
pills. Never had pelvic examination. Never had teaching about breast
self-examination or STIs except AIDS. Smokes cigarettes, PPD; started
age 11 years. Has not had HPV vaccines.
a. Depending on the information and suggestions of this girl, what is the best
family planning method would you advise her?
b. After physical assessment, what is your clinical decision or diagnosis?c. Which interventions do you think to be important in this case?
9.3.Interpretation of specific findings on Urogenital
system.
Learning activity 9.3
1. After history taking and physical examination, the nurse decides to take
urine sample. The patient reported dysuria and genital itching. The urine
looks bloody and has a very bad odor.
a. Is it normal to have blood in the urine?b. What does dysuria means?
Following the history taking and physical examination of GU, we are going to attach
the meaning on some special findings. Urinary frequency (increased number
of urination) can originate from urinary tract infection, bladder calculi and urethra
stricture. In older male, urinary frequency is the sign of benign prostatic hyperplasia
or prostate cancer which compress the bladder. Urgency known as strong need
to urinate is an indicator to urinary tract infection, chronic prostatitis, urethritis,
obstruction of lower urinary tract leading to residual urine and overflow, anxiety, use
of diuretics, benign prostatic hyperplasia, urethral stricture, and diabetic neuropathy.
Hesitancy is the delayed or difficult starting urination. The main causes are benign
prostatic hyperplasia, compression of urethra, outlet obstruction, and neurogenic
bladder. Enuresis is the involuntary urination when someone is sleeping sleep.
Enuresis is said when bladder control can’t achieved by 5 years of age due to
delayed functional maturation of the central nervous system. Other causes of
enuresis are obstructive disease of lower urinary tract, genetic factors, failure to
concentrate urine, urinary tract infection and psychological stress.
Nocturia or excessive urination during the night indicates renal or lower urinary
tract. It can also indicate metabolic disorders as well as side effects of diuretic
medications. Urinary incontinence as the inability to voluntarily control urine
is linked to stress incontinence, tumor, bladder cancer, calculi and neurological
conditions such as spinal cord injury and Guillain-Barré syndrome. Normal urine
output in a healthy individual must be between 0.5-1.5 mL/kg/hour, and patients
should generally be urinating at least every 6 hours. On the other side oliguria is
defined as the production of inadequate volumes of urine (<500 ml/day in adults,
<0.5 mL/kg/hour in children, and <1.0 mL/kg/hour in infants. Oliguria is caused by
acute or chronic kidney failure and inadequate fluid intake. Polyuria is the increased
volume of urine. The main causes of are diabetes mellitus, diabetes insipidus, use
of diuretics, excess fluid intake. Anuria is the absence of urine or urine output of
less than 100ml per 24 hours. Anuria is due to acute or chronic kidney failure and
complete obstruction. Hematuria is the presence of red blood cells in the urine. The
causes of hematuria are cancer of genitourinary tract, acute glomerulonephritis,
renal stones, renal tuberculosis, trauma and extreme exercise. Proteinuria is the
presence proteins in the urine. Proteinuria may the sign of acute and chronic renal
disease, nephrotic syndrome, vigorous exercise, severe heart failure and diabetic
nephropathy. Kidney enlargement is palpable in the costo-vertebral angle in case
of cyst, hydronephrosis or tumor.
Syphilitic chancre is an initial sign of the infestation of Treponema Pallidum. The
chancre appears in red, painless, eroding lesion with raised boarder. It is located
inside the vagina in female or to the other parts of external genitalia in both sexes.
Vaginitis is the inflammation of the vagina resulting from overgrowth infectious microorganisms.
Vaginitis is categorized under bacterial vaginosis, Candida albicans
infection, trichomoniasis, and mucopurulent cervicitis depending on infecting agent.
Bacterial vaginosis is identified as thin grayish white discharge. Vaginal candidiasis
appears as thick, white, curdlike discharge and appears in patches on the cervix
and vaginal walls. Another form is mucopurulent cervitis originating from gonorrhea
or Chlamydia. They both produce purulent yellow discharge from the cervix.
Trichomoniasis may generate a malodorous yellow or green, foamy or watery, foulsmelling
discharge. It can also create red papules on the cervix and vaginal walls,
giving the tissue a strawberry appearance.
Genital warts, a sexually transmitted disease caused by human papilloma virus.
They produce painless warts on the penis, vulva, vagina, cervix, or anus. Warts
start as tiny red or pink swellings that grow. They become multiple swellings with a
cauliflower appearance.
Genital herpes is due to herpes simplex virus type 2. It produces multiple,
superficial vesicles, lesions, or crusts inside the vagina, on the external genitalia in
both sexes, on the buttocks and, sometimes, on the thighs. Symptoms of genital
warts are dysuria, regional lymph node inflammation, pain, edema, and sometimes
with fever.
Vaginal prolapse occurs when the anterior vaginal wall and bladder prolapse into
the vagina. The uterus may prolapse into the vagina and can even be seen outside
the body.
The testicular tumor is identified as painless lump in the testicles which causes
weight in the scrotum. Prostate gland enlargement is identified using digital rectal
examination. It can be categorized as benign prostatic hyperplasia (BPH) or acute
prostatitis. The BPH usually starts after age 50 with signs and symptoms of nocturia,
urinary hesitancy, frequency and recurring urinary tract infections. In the acute
prostatitis, the prostate gland is firm, warm, and extremely tender and swollen withfever as the condition originate from infection.
Self-assessment 9.3
1. How can you differentiate vulvovaginal candidiasis to contact dermatitis
by using inspection?
2. What is the causative agent of genital warts?
3. State the characteristics of paraphimosis
4. Differentiate inguinal hernia to testicular torsion
9.4. Identification of client problemsLearning activity 9.4
a. Mention possible patient problems being identified by the nurse after the
assessment of the patient’s abdomen.
b. Which anatomical organs of the internal female reproductive herementioned?
The problems of genitourinary system can be allocated under structural, functional,
infectious and tumor based origin. One of the common infection of GU is candidiasis
identified as vulvovaginal edema, erythema, and excoriation; thick white secretions.
The microscopy will show pseudohyphae, occasional budding yeast. Bacterial
vaginosis is another infection with whitish to grayish creamy secretions that coat
the vaginal walls with a strong fishy odor and vaginal itching or burning.
Laboratory investigation will show clue cells on microscopy and possibly WBCs are
present. Gonnorhea, one of the STIs, clinically present yellow purulent discharge
from the cervix; tenderness or pain with the pelvic examination. Diagnostic test
using Gram stain shows intracellular diplococcic.
Syphilis, an infection resulting from Treponema Pallidum inoculation which
penetrates intact skin or mucous membrane during sexual contact. In its early
stage it demonstrates a chancre: a painless ulceration at the point of entry which
can be on the penis or vulva.
Pediculosis pubis presents with mild to severe itching, especially in the mons pubis
and perineum. The external genitalia are excoriated. Tiny spots of blood and lice
may be seen on the underwear. Eggs normally adhere to the pubic hair and can
appear as small dark spot. The risk factors for pediculosis pubic are direct contact
with the infected person especially during sexual contact, sharing personal items
such as bed linen and living in institutionalized condition.
Uterine prolapsed is when the uterus fall into the vagina due to gradual weakening
of uterine ligaments. It may be a consequence of multiple vaginal births or an
enlarging uterus. The patient presents with low pressure, fecal impaction, and
vaginal and uterine irritation.
Ectopic Pregnancy happens when a fertilized ovum implants outside uterine
endometrium mostly in the fallopian tubes and cervix. Risk factors include previous
ectopic pregnancy, past pelvic infection, endometriosis, or tube abnormalities. The
patient presents with symptoms of a normal pregnancy initially. As the ectopic
pregnancy grows larger, there is internal hemorrhage and subsequent lower
quadrant pain.
Testicular torsion is another male related condition manifested as a sudden twisting
of the spermatic cord, usually on the left side, is rare after 20 years. It results
from poor attachment of the testis on the scrotal wall. Signs and symptoms involve
impaired blood supply which leads to ischemia and venous engorgement. Because
the testis can become gangrenous within a few hours, this is a surgical emergency.
Hydrocele is the collection of serous fluid develops in the tunica vaginalis
surrounding the testis. The patient presents with unilateral and intermittent edemaof the scrotum but no pain.
Self-assessment 9.4
1. Why is testicular torsion considered as a surgical emergency?
2. A patient is presenting lice like insects in his pubic area and perineum.
They cause itching at a level of skin laceration.
a. What is the medical diagnosis for this patient?b. What are the preventive measures for this condition?
9.5.Nursing intervention based on patient’s problem.Learning activity 9.5
a. Describe the above images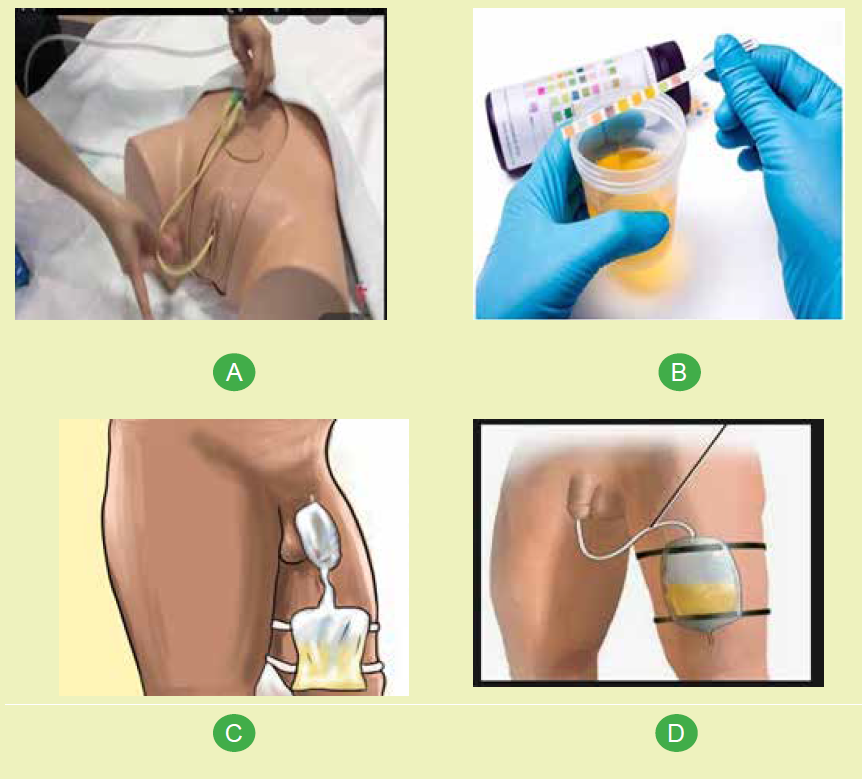
b. What are the indications of urinary catheterization?
Nurse’s activities in relations to genitourinary system are individualized and depend
on patient’s problem. After the assessment, a nurse will make priority actions which
can extend from education, advocacy or provision of nursing intervention. The
education can be safe sex practices to prevent STIs and adequate water intake to
keep urinary track flushed to prevent UTIs and renal stones. Female are advised
to clean anus after defecation from front to back to avoid contamination of feces in
the genitals which can originate from unnecessary contamination which results in
infections.
Depending on data collected from the patient, some may be alarming and require
immediate interventions such as paraphimosis and testicular torsion. The nurse
will immediately inform the physician for advanced assessment and preparation for
emergency surgery. Other nursing intervention can be urine or secretion specimen
collection, measuring urine output, provide bedpan, urinary catheter insertion and
removal as needed. The nurse also will administer prescribed orders to treat GUconditions.
Self-assessment 9.5
1. Which health education topics will you initiate after consulting a 18 year
boy used to have unprotected sex with girls of his age?
2. List the intervention a nurse can provide to manage the GU problems.3. Why is it important to drink enough water on the GU health status?
End unit 9 assessment
1. List 5 nursing interventions specific to the GU
2. Write and describe abnormalities in urination
3. List 10 clinical conditions common on GU system.4. Match the following terms to their description

UNIT 10 SOCIETY AND HEALTH
Key Unit Competence
Relate society, family, and special group to health and illnessIntroductory activity 10
1. What does the image A display?
2. Describe the interconnectedness showed in image B in terms of societyand health.
10.1. Definition of society and FamilyLearning activity 10.1
Referring to the image aside define the
following terms
a) Societyb) Family
a. Society
A society is a group of individuals involved in persistent social interaction, or a
large social group sharing the same spatial or social territory, typically subject
to the same political authority and dominant cultural expectations. Societies are
characterized by patterns of relationships (social relations) between individuals
who share a distinctive culture and institutions; a given society may be described
as the sum total of such relationships among its constituent of members. In the
social sciences, a larger society often exhibits stratification or dominance patterns
in subgroups.
Societies construct patterns of behavior by deeming certain actions or concepts
as acceptable or unacceptable. These patterns of behavior within a given society
are known as societal norms. Societies, and their norms, undergo gradual and
perpetual changes.
• Society can enable its members to benefit in ways that would otherwise be
difficult on an individual basis; both individual and social (common) benefits
can thus be distinguished, or in many cases found to overlap.
• A society can also consist of like-minded people governed by their own norms
and values within a dominant, larger society. This is sometimes referred to as
a subculture, a term used extensively within criminology, and also applied to
distinctive subsections of a larger society.
b. Family
The family is an intimate domestic group made up of people related to one another
by bonds of blood, sexual mating or legal ties. It is the smallest and most basic
social unit, which is also the most important primary group found in any society.
It is the simplest and most elementary group found in a society. It is a social group
consisting of a father, mother and one or more children. It is the most immediate
group a child is exposed to. In fact, it is the most enduring group, which has
tremendous influence on the life of an individual, from birth until death. It also
accounts for the most enduring social relation¬ship found in society. Every family
provides an individual with a name, and hence, it is a source of nomenclature. Each
member of family shares duties and responsibilities.
The family is the central and important social institution for health development in
which individuals are born and receive resources for their growth and development.
It has the primary influence on the health and development of children. The family
influences healthy behaviors, and provides care and facilitates recovery from the
illnesses.
The family is commonly linked to positive health outcomes. Two parent biological
families are particularly shown to be more protective for mental health of children
and adolescents.
Marriage has a protective role on health since married individuals report healthier
lifestyle, less risky behaviour, early screening and testing for disease, more health
checkups and timely treatment-seeking. But the benefits of marriage for health are
strongly dependent on the quality of the marital relationship and conjugal harmony
Intra-family dynamics and relationship has a key role in health outcomes of the
family. Supportive family/kinship relationships have reportedly decreased the
likelihood of the onset of chronic diseases and mental illness and delayed mortality.
Families provide the support and conditions needed for healthy living, prevention
of disease and opportunities for early diagnosis and treatment to avert or delay
complications. Interventions for health to be effective, must necessarily take intoaccount the social determinants of health.
Self-assessment 10.1
Select the best response
1. Social dispute contributes to good health
a) True
b) False
2. A society consist of
a) People
b) Institution
c) A and b
d) None of the above
3. The definition of family
a) Is consistent across communities
b) Is defined by our government to include all current family structures
c) Can include only biological family members
d) Varies from community to community and from state to state
4. A homeless woman is more likely than other women to have all of the
following characteristics except:
a) To have less than a high school education
b) To have grown up in foster care
c) To be employed
d) To have had an abortion by age 16
10.2.Family Structure
Learning activity 10.2
Relating to family structure, describethe image aside
The following types of families exist today, with some families naturally falling into
multiple categories.
a. Nuclear Family
The nuclear family is the traditional type of family structure. This family type
consists of two parents and children. Children in nuclear families receive strength
and stability from the two-parent structure and generally have more opportunities
due to the financial ease of two adults.
b. Single Parent Family
The single parent family consists of one parent raising one or more children on his
own. This family may include a single mother with her children, a single dad with his
kids, or a single person with their kids.
c. Extended Family
The extended family structure consists of two or more adults who are related, either
by blood or marriage, living in the same home. This family includes many relatives
living together and working toward common goals, such as raising the children and
keeping up with the household duties. Many extended families include cousins,
aunts or uncles and grandparents living together.
d. Childless Family
While most people think of family as including children, there are couples who
either cannot or choose not to have children. The childless family is sometimes the
“forgotten family,” as it does not meet the traditional standards set by society.
e. Stepfamily
For the divorced individuals, many choose to get remarried. This creates the step
or blended family which involves two separate families merging into one new unit.
It consists of a new husband, wife, or spouse and their children from previous
marriages or relationships. Stepfamilies are about as common as the nuclear
family, although they tend to have unique challenges, such as adjustment periods
and discipline issues. Stepfamilies need to learn to work together and also work
with their exes to ensure these family units run smoothly.
f. Grandparent Family
Many grandparents nowadays are raising their grandchildren for a variety of
reasons. One in fourteen children is raised by their grandparents, and the parents
are not present in the child’s life. This could be due to parents’ death, addiction,
abandonment or being unfit parents. Many grandparents need to go back to workor find additional sources of income to help raise their grandchildren.
Self-assessment 10.2
Compare and contrast stepfamily from nuclear family
10.3.Special groups in the society
Learning activity 10.3What does the following images indicate?

Though the concepts of society and family were well described, it is very important
to pay attention on the health of special peoples within the society which include:
a. Sex workers
Sex workers are a diverse group of people. They are men, women, and transgender
people. Some are parents, members of religious groups, and members of the society.
Some sex workers enjoy their work and see it as a way to express their sexuality.
Others like the income and flexibility. Yet, whoever sex workers are and whatever
they do, they deserve the same protections as everyone else. This includes the
right to health care, and to safety. Stigma against sex workers leads to extreme
barriers to health care. A UNFPA report found that nearly 1 in 4 sex workers have
been denied health care because of their occupation. And, not surprisingly, more
than 60% of sex workers fear and distrust health care workers.
Different report highlight that sex workers are more likely to be HIV+ than the general
population because they are less able to access health care service. Many sex
workers face rejection from the family and that lead to lot of psychological problem
among them. Sex workers have reported facing daily harassments and stigma and
many have even attempted suicide as a consequence to such maltreatment from
the society. It is therefore very important for health care workers to understand the
complexity and health challenges of sex workers and consider them in the planning
of preventive and curative interventions to them.
b. Prisoners
A prisoner is a person legally committed to prison as a punishment for a crime or
while awaiting trial. Hundreds of men and women are imprisoned in different prison
around the world. Most of these prisoners are from poor and vulnerable communities.
Prisons are not healthy places. Communicable diseases are frequently transmitted
among prisoners, and the rates of HIV, hepatitis and tuberculosis are much higher
among them than in the general population.
There is also a high prevalence of mental health problems, including substance
abuse disorders, and a higher prevalence of non-communicable diseases.
Unhealthy conditions such as overcrowding and poor hygiene are common in many
prisons. Prison health is part of public health and prisons are part of our society.
One third of prisoners leave prison every year and the interaction between prisons
and society is huge. Health care workers must contribute to initiative designed to
ensure that prisons are not becoming breeding places for communicable and noncommunicable
diseases, and must also seek to use the experience of imprisonment
for the benefit of prisoners and society.
c. Disabled persons
Disability refers to the interaction between individuals with a health condition. Over
1 billion people are estimated to experience disability. This corresponds to about
15% of the world’s population. disabled persons are then part of the society. The
number of people experiencing disability will continue to increase due to a rise
in chronic health conditions and population ageing. WHO report that people with
disability face barriers, stigmatization and discrimination when accessing health
and health-related services and strategies.
There are attitude, physical, financial and communication related barriers to
healthcare among disabled persons which include:
Attitudinal barriers
• People with disability commonly report experiences of prejudice, stigma and
discrimination by health service providers and other staff at health facilities.
• Many service providers have limited knowledge and understanding of the
rights of people with disability and their health needs and have inadequate
training and professional development about disability.
• Many health services do not have policies in place to accommodate the
needs of people with disability. Such policies could include allowing longer
and flexible appointment times, providing outreach services and reducing
costs for people with disability.
• Women with disability face particular barriers to sexual and reproductive
health services and information. Health workers often make the inaccurate
assumption that women with disability are asexual or are unfit to be mothers.
• People with disability are rarely asked for their opinion or involved in decisionmaking
about the provision of health services to people with disability.
Physical barriers
• Health services and activities are often located far away from where most
people live or in an area not serviced by accessible transport options.
• Stairs at the entrance to buildings or services and activities located on floors
which do not elevator access are inaccessible.
• Inaccessible toilets, passages, doorways and rooms that do not accommodate
wheelchair users, or are difficult to navigate for people with mobility
impairments, are common.
• Fixed-height furniture, including examination beds and chairs, can be difficult
for people with disability to use.
• Health facilities and other venues for activities are often poorly lit, do not have
clear signage, or are laid out in a confusing way that makes it hard for people
to find their way around.
Communication barriers
• A key barrier to health services for people who have a hearing impairment
is the limited availability of written material or sign language interpreters at
health services.
• Health information or prescriptions may not be provided in accessible formats,
including Braille or large print, which presents a barrier for people with vision
impairment.
• Health information may be presented in complicated ways or use a lot of
jargon. Making health information available in easy to follow formats including
plain language and pictures or other visual cues can make it easier for people
with cognitive impairments to follow.
Financial barriers
• Over half of all people with disability in low-income countries cannot afford
proper health care.
• Many people with disability also report being unable to afford the costs
associated with travelling to a health service and paying for medicine, let
alone the cost of paying to see a health service provider.
Disability inclusion in health care is critical to achieving universal health coverage
without financial hardship, because persons with disabilities are: Three times more
likely to be denied health care, four times more likely to be treated badly in the
health care system and 50% more likely to suffer catastrophic health expenditure.
d. Elders persons
People worldwide are living longer. Today most people can expect to live into their
sixties and beyond. Every country in the world is experiencing growth in both the
size and the proportion of older persons in the population. ageing is associated to
lot of conditions. Common conditions in older age include hearing loss, cataracts
and refractive errors, back and neck pain and osteoarthritis, chronic obstructive
pulmonary disease, diabetes, depression and dementia. As people age, they are
more likely to experience several conditions at the same time.
Older age is also characterized by the emergence of several complex health states
commonly called geriatric syndromes. They are often the consequence of multiple
underlying factors and include frailty, urinary incontinence, falls, delirium and
pressure ulcers.
A longer life brings with it opportunities, not only for older people and their families,
but also for societies as a whole. Additional years provide the chance to pursue
new activities such as further education, a new career or a long-neglected passion.
Older people also contribute in many ways to their families and communities.
Yet the extent of these opportunities and contributions depends heavily on one
factor: health. Maintaining healthy behaviours throughout life, particularly eating
a balanced diet, engaging in regular physical activity and refraining from tobacco
use, all contribute to reducing the risk of non-communicable diseases, improving
physical and mental capacity and delaying care dependency. All countries face
major challenges to ensure that their health and social systems are ready to make
the most of this demographic shift. Therefore, health care workers must also be
ready to contribute in preserving health of this special group.
f. Homosexual person
Homosexual persons are also part of special people within the society. in health
care, the relationship between users and health services is considered essential
to strengthen the quality of care. However, the Lesbian, Gay, Bisexual, and
Transgender population suffer from prejudice and discrimination in access and
use of these services. A sympathetic study reveal that the homosexual population
have difficulties of access to health services as a result of heteronormative attitudes
imposed by health professionals. The discriminatory attendance implies in human
rights violations in access to health services. though there is what done, a lot must
still be achieved to ensure access to health services for sexual minorities, through
the adoption of holistic and welcoming attitudes.
Self-assessment 10.3
1. Is being lesbian, gay, or bisexual a mental disorder?
2. Mention 3 most common medical conditions elders people tend toexperience.
10.4. Social distribution of diseasesLearning activity 10.4
Describe image A and B below in terms of social distribution of diseases
Epidemiology is the discipline that studies the distribution and cause of disease.
Social epidemiology is a branch of epidemiology that studies the distribution and
determinants of health and disease in populations. Social epidemiology focuses
particularly on the effects of socio-structural factors on states of health.
In the society people interact each other and this allow easy transmission of
diseases especially communicable diseases. The distribution of the disease may
either start in utero, get developed in families and then in general community. Due to
interconnectedness of societies and regular travel of people in the society disease
vector may propagate in the whole country or even worldwide causing disease as
for the recent case of Covid-19 pandemic.
Parents can transmit some diseases to their children during pregnancy, birth or
during breastfeeding. At home where family members share beddings, bathrooms
etc; there is high risk of sharing some communicable diseases especially when the
hygiene is poor. In the community children, pregnant women and elderly people
are more at risk of getting ill because of their low immunity. In Rwanda, Children
are mostly contaminated by communicable diseases like worms (eg. ascariasis),
amoebiasis, malaria, diarrhea, pneumonia among others and also children are
exposed to malnutrition conditions like anemia, kwashiorkor and marasmus.
Pregnant women are most likely to have anemia, malaria and other pregnant related
diseases. Elderly people are mostly exposed to non-communicable diseases like
hypertension, diabetes, stroke among others. Diseases are different from towns
comparing to rural areas.
Self-assessment 10.4
Select the best response
1. A disease vector is a
a. organism that transmits a disease
b. symptom of a disease
c. environmental condition associated with a disease
2. An epidemic that becomes unusually widespread and even global in its
reach is referred to as a
a. Pandemic
b. Hyperendemic
c. Covid-19
3. Social epidemiologists are interested in learning about
a. Social distribution of disease in population
b. the frequency and geographic distribution of diseases
c. the causal relationships between diseasesd. All the above
10.5. Implication of society in healthcareLearning activity 10.5
The central purpose of governments is the promotion of health and social
development for their people. However, we ought to take into account that the
health of every human being largely depends, besides their genetic endowment
and personal behaviors, on social determinants that are only very partially within
their control. Lifestyle plays a major role in the development of most illness globally.
Six of the 10 leading factors contributing to the global burden of disease are
lifestyle related: unsafe sex, high blood pressure, tobacco use, alcohol use, high
cholesterol and obesity. Lifestyle-related illnesses also contribute to the rising costs
of healthcare. Given the well-documented relationship between lifestyle, disease
burden and healthcare costs, it makes economic and medical sense to hold
individuals morally responsible for their health-related choices. Although individuals
should play an important role in maintaining their own health, they should not be
held entirely responsible for it. Assuming that responsibility for health rests either
with individuals or with society, it follows that society should also help to promote
health and prevent disease.
Undoubtedly, ensuring access to healthcare is an important social responsibility,
but societies can also participate in promotion of health, such as through sanitation,
pollution control, food and drug safety, sport activities, health education, diseasesurveillance, urban planning and occupational health as well as in health research.
Self-assessment 10.5
1. Mention at least 4 lifestyle related behaviors which contribute to global
burden of disease globally
2. Mention 2 health promotion activities that your society regularly beinvolved in.
10.6. Approach to Family Health NursingLearning activity 10.6
1. Describe image aside
2. Relate to the image aside
and define the term Familynursing.
Family health: A condition including the promotion and maintenance of physical,
mental, spiritual, and social health for the family unit and for individual family
members.
In health care, there are many different approaches throughout the field of nursing.
When considering the field of family nursing, there are four different approaches
to caring for patients. The approaches that will be discussed include family as a
context, family as a client, family as a system, and family as a component to society.
The approach that nurses use is determined by many factors including the health
care setting, family circumstances and nurse resources.
a. Family as a context of care
Family as a context is an approach that focuses on care of an individual client in
which the family is the context. Although the nurse focuses the nursing process
on the individual’s health status, the nurse also assesses the extent to which the
family provides the individual’s basic needs. These needs vary, depending on the
individual’s development level and situation. Because families provide more than
just material essentials, their ability to help the client meet psychological needs must
also be considered. Family members may need direct interventions themselves.
b. Family as a client
In this approach, the family nursing care centers on the assessment of all family
members. the family nurse is interested in the way all family members are individually
affected by the health event of one family member. The family is the foreground and
individuals are in the background. In this approach, the family is seen as the sum
of individual’s family members. The nurse focus is concentrated on each and every
individual as they affect the whole family. From this perspective, a nurse might
ask a family member who has just become ill. Example, “tell me about what has
been going on with your own health and how you perceive each family member
responding to your mother’s recent diagnosis of liver cancer”.
c. Family as a system
In this approach the family is viewed as an international system in which the whole
is more than the sum of its parts. This approach focuses on the individual and family
members become the target for nursing interventions. Eg: the direct interaction
between the parent and the child. The system approach to the family always implies
that when something happens to one affected. It is important to understand that
although theoretical and practical distinctions can be made between the family as
context and the family as client, they are not necessarily mutually exclusive, and
both are often used simultaneously, such as with the perspective of the family as
system.
d. Family as a component of society
In this approach, the family is seen as one of many institutions in society, along
with health, educational, religious, or economic institution. The family is a basic or
primary unit of society, as are all the other units and they are all a part of the larger
system of society. The family as a whole interacts with other institutions to receive
exchange or give communications and services. Community health nursing has
drawn many of its clients from this perspective as it focuses on the interface between
families and communities. Family health nursing practice like any nursing practice
begins with the nursing process. By using this process, the nurse practicing with
family perspectives is potentially able to effectively intervene at any of the levels.
After an assessment of the individuals, family unit, and supra system, the nurse isready to begin to identify areas of concern or need.
Self-assessment 10.6
Match approach to family nursing in column A with specific examples providedin column B
10.7 Theories related to family health nursing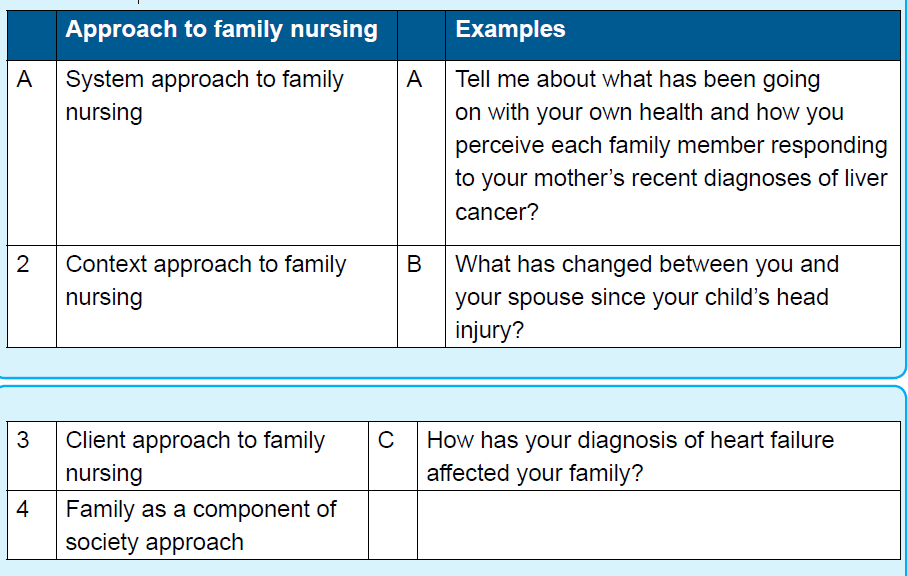
Learning activity 10.7
Describe the figure aside by showing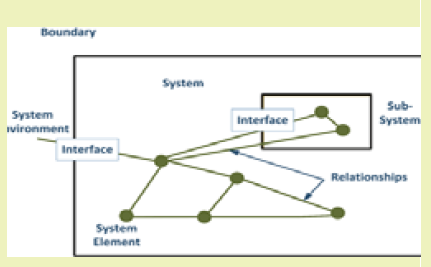
how these areas are connected to thefamily as well as to the society.
a. Functional theory
Also called structural theory. Functional was written in 1898 by an English
Philosopher and biologist Herbert Spencer (1820-1903). This theory sees society
as a structure with interrelated parts designed to meet the biological and social
needs of the individuals in that society. Spencer saw similarities between society
and the human body; he argued that just as the various organs of the body work
together to keep the body functioning that how the various parts of society work
together to keep society functioning. The parts of society that Spencer referred
to were the social institutions, or patterns of beliefs and behaviors focused on
meeting social needs, such as government, education, family, healthcare, religion,
and the economy.
According to this theory, the society is held together by shared values, languages,
and symbols. He believed that to study society, a sociologist must look beyond
individuals to social facts such as laws, morals, values, religious beliefs, customs,
fashion, and rituals, which all serve to govern social life.
b. Family interaction theory
Family interaction theory (FIT) stems from symbolic interactions that are applied to
the family. This approach focuses on the way by which family members relate to
one another. The family is viewed as a set of interacting personalities. The family
dynamics and the relationships of the child to the family significantly affects the
emotional development. According to FIT, the parent-child relationship is perceived
to influence the important aspects of the child’s personality. The child’s attachment
to the family of origin and social institutions such their experiences in school are
believed to be central to the child and also parenteral satisfaction and low parentchild
conflict are also perceived to influence the well-being of the child. The parentchild
interactions can significantly impact the development of the child’s emotional
competence, which specifically includes self-esteem.
c. General system theory
General system theory was written by Von Bertalanffy in 1950’s. Von Bertalanffy
introduced General systems theory as a universal theory applicable to many fields
of study which provides a way of examining interrelationship and deriving principles.
The author started by defining a system as a set consisting of integrated, interesting
parts or components that function as a whole. Each part is necessary to make a
complete and meaningful whole.
General system theory describes how to break the whole apart and then learn how
the parts work together.
• Emphasizes the relationships between parts.
• Describes how parts function and behave.
Principles of General system theory and its application in Nursing
1. The principle of wholeness: It is the core of General system theory; this
principle provides the guidance or methodology to us in order that we can
study all kinds of objects effectively.
2. The principle of optimization: The principle of optimization of a system
is to achieve an optimal state in certain condition and to perform its best
function by organization and coordination. With the principle of optimization
3. The principle of modeling. Modeling is to design a model similar to a real
system first, then to describe and understand the characterization and level
of real system by studying the model.
d. Developmental theories
Child development theories focus on explaining how children change and grow over
the course of childhood. Such theories center on various aspects of development
including social, emotional, and cognitive growth. The study of human development
is a rich and varied subject. We all have personal experience with development, but
it is sometimes difficult to understand how and why people grow, learn, and act as
they do.
Some of the development theories are: Freud’s Psychosexual Developmental Theory,
Erikson’s Psychosocial Developmental Theory, Behavioral Child Development
Theories, Piaget’s Cognitive Developmental Theory, Bowlby’s Attachment Theory,
Bandura’s Social Learning Theory, Vygotsky’s Sociocultural Theory.
Example, Attachment theory written by John Bowlby who believed that early
relationships with caregivers play a major role in child development and continue to
influence social relationships throughout life. Bowlby’s attachment theory suggested
that children are born with an innate need to form attachments. Such attachments
aid in survival by ensuring that the child receives care and protection. Not only
that, but these attachments are characterized by clear behavioral and motivational
patterns.
In this theory, both children and caregivers engage in behaviors designed to ensure
proximity. Children strive to stay close and connected to their caregivers who in
turn provide a safe haven and a secure base for exploration. Children who receive
consistent support and care are more likely to develop a secure attachment style,
while those who receive less reliable care may develop an ambivalent, avoidant, ordisorganized style.
Self-assessment 10.7
Select the best response
1. Functional theory
a. Form a whole which is more than the sum of its parts
b. The family is viewed as a set of interacting personalities
c. The society is held together by shared values, languages, and symbols
d. All of them
e. None of them
2. The family dynamics and the relationships of the child to the family
significantly affects the emotional development. Which theory is this?
a. Attachment theory
b. Family interaction theory
c. General system theory
d. None of them
3. General system theory describes how to break the whole apart and then
learn how the parts work together. Which theory is this?
a. Functional theory
b. Family interaction theory
c. General system theory
d. All of them
4. Focus on explaining how children change and grow over the course of
childhood
a. Family interaction theory
b. Development theory
c. Attachment theory
d. None of them5. John Bowlby is the author of which theory?
10.8. Role of family in health promotion and diseases
preventionLearning activity 1.9
Describe image A and B in relation to the role of family in health promotion anddisease prevention.
The family is the central and important social institution for health development in
which individuals are born and receive resources for their growth and development.
It has the primary influence on the health and development of children. The family
influences healthy behaviors, and provides care and facilitates recovery from the
illnesses. The family is a source of nurture and emotional support as well.
Families provide the support and conditions needed for healthy living, prevention
of disease and opportunities for early diagnosis and treatment to avert or delay
complications. Social support for family’s needs to be responsive to the dynamics
of today’s family structure and the composition, condition, and challenges faced by
families. Family as the foundation for health development of individuals; changing
family structure, demography, roles, and responsibilities poses challenges in
nurturing healthy behaviors. Intersectoral interventions to empower families are
crucial to build adequate support systems for healthy family development; to strive
towards social inclusiveness increasing family access to public services; to enable
institutions to assess family at-risk before crisis; and, to design family centred
support systems. Active participation of families is crucial for family empowerment.
Empowering women to promote family health and well-being to gain control of their
own lives, income and fertility contributes directly to their family health and health
development.
In Rwanda, health promotion activities families get involved in regularly include:
ensuring the immunization of their children, designing kitchen garden to fight
against malnutrition, participating in umuganda, ensuring hygiene at home and in
the community, avoidance of water and air pollution etc.
To conclude; Important areas where families impact health includes healthy
behaviour, self-care, care during pregnancy and childbirth, child and adolescent
health, care of the aged, nursing and nurturing the sick, individuals with special needs(including those with stigmatizing health conditions) and disaster preparedness.
Self-assessment 10.8
What is the major role of the family in disease prevention?End unit assessment 10
Respond to all questions from both sections
SECTION A: Select the best response
1. A homeless woman is more likely than other women to have all of the
following characteristics except:
a) To have less than a high school education
b) To have grown up in foster care
c) To be employed
d) To have had an abortion by age 16
2. What is the definition for the nuclear family?
a) Individual living together
b) Two adults with their own biological children
c) Single person
d) All of the above
3. Maliko mom has just remarried and is expecting baby. Name the type of
his family
a) Blended family
b) Extended family
c) Lone family
d) Residential care family
4. Which is a developmental task for the family with teenagers?
a) Releasing young adults into the world
b) Adjusting to retirement
c) Helping children cope with independence
d) Promoting education
5. Which family function is providing a home (shelter), clothing and food to
the best of your ability?
a) Basic needs
b) Spiritual
c) Recreation
d) Adaption
6. There certain things in our society that have been happening before
civilization and still happening, such as prostitution, which people refer
to as sex worker?
a) someone that exchange sex for money
b) someone that engage sex for pleasure
c) someone hire for sexual activities
d) all of the above
7. Equity and inclusion for children with disabilities means equal…
a) Opportunities
b) Treatment
c) Rights
d) All of the Above
8. What does the disabled person require from the society?
a) Peer support
b) Housing
c) Transport
d) All the above
9. Most of the health problems in rural areas of Rwanda are due to:
a) Parasitic worms and microorganisms
b) Psychological tension resulting from work
c) Air pollution
d) HIV
10. In Rwanda children are most likely to suffer from
a) Hypertension
b) Diabetes
c) Kwashiorkor
d) HIV
SECTION B: Open ended questions
11. Differentiate system approach to family nursing and family as a component
of society approach to family nursing are.
12. Mention at least 3 reasons why sex workers are more likely to get HIV+and other STI than the general population.
UNIT 11 COMMUNICATION AND COUNSELING
Key Unit Competence
Provide an appropriate counseling for individual, groups, and familyIntroductory activity 11
1. What do you see on pictures above?
2. What are differences between pictures A, B and picture C?
3. On your point of view, how do you interpret the picture C?
11.1. Definition and Communication processLearning activity 11.1
Observe the picture aside and answer
following questions:
1. What do you see on pictures
above?
2. What are doing persons on the
picture?
3. On your point of view, what couldbe the topic of conversation?
11.1.1 Definition of communication
Communication can broadly be defined as exchange of ideas, messages and
information between two or more persons, through a medium, in a manner
that the sender and the receiver understand the message in the common
sense, that is, they develop common understanding of the message.
Berelson and Steiner define communication as the transmission of information,
ideas, and emotions, skills through the use of symbols, words, pictures, figures,
and graph
11.1.2 Communication process
The communication process has several components that enable the transmission
of a message. Here are the various parts
a. Sender: This is the person that is delivering a message to a recipient.
b. Message: This refers to the information that the sender is relaying to the
receiver.
c. Channel of communication: This is the transmission or method of delivering
the message.
d. Decoding: This is the interpretation of the message. Decoding is performed
by the receiver.
e. Receiver: The receiver is the person who is getting or receiving the message.
f. Feedback: In some instances, the receiver might have feedback or aresponse for the sender. This starts an interaction.
The Communication Process:
DIAGRAM
Counselling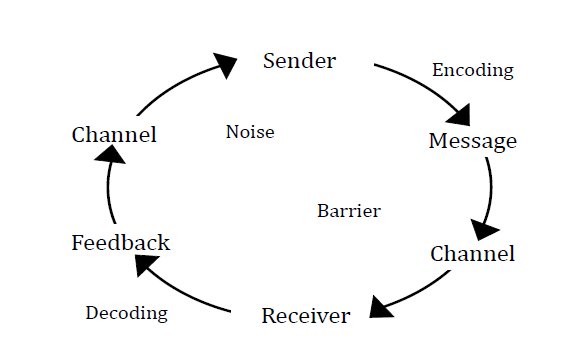
How does the communication process work?
In order to successfully communicate, it’s important to understand how the process
works.
Here are the seven steps in the communication process:
1. The sender develops an idea to be sent.
2. The sender encodes the message.
3. The sender selects the channel of communication that will be used.
4. The message travels over the channel of communication.
5. The message is received by the receiver.
6. The receiver decodes the message.7. The receiver provides feedback, if applicable.
Self-assessment 11.1
1. Explain what communication meant?
2. What is the importance of communication?3. Give seven steps in the communication process.
11.2. Types and techniques of communication
Learning activity 11.2
Observe the pictures above and answer following questions:
1. How can you interpret pictures A, B, C and D?
2. On your point of view, what is a difference between picture C and D
Type: a type means people, places or things that share traits which allow them to
belong to the same group
Technique: a way of carrying out a particular task, especially the execution or
performance of an artistic work or a scientific procedure
11.2.1. Types of Communications:
11.2.1.1. Verbal Communication
The most common form of communication is the spoken word. It can be used
to convey information, ask questions or request a response from others. Verbal
communication includes all forms of speech, such as talking, shouting, whispering,
and singing, chanting, and reading aloud.
11.2.1. 2. Non-verbal Communication
There are many other ways that people communicate with each other without using
words. Non-verbal communication includes nodding, shaking hands, pointing, eye
contact, smiling, frowning, touching, leaning forward, standing up straight, sitting
down, crossing arms, etc. These gestures help us understand what another person
means when they speak.
We also use non-verbal cues to express ourselves to others. For example, if
someone smiles at me while I’m speaking to him, he might be expressing interest
in what I have to say. Or if he leans back in his chair, it tells me that he doesn’t want
to hear what I am saying.
11.2.1.3. Written Communication
The written word has been an important means of communication since ancient
times. Written communication includes letters, e-mails, faxes, memos, reports, and
other written messages. Written messages include text on paper and computer
screens. Writing allows us to store large amounts of information quickly and easily.
11.2.1.4. Visual Communication
Another way that we communicate with each other is through pictures or images.
Visual communication includes photographs, paintings, diagrams, charts, maps,
graphs, drawings, sketches, animations, and videos.
11.2.2. Techniques of communication
Communicating effectively will benefit you in every aspect of your life. Good
communication skills impact your relationship with every person you interact with.
Following 5 techniques are used in communication
• Pay attention: Give the speaker your undivided attention.
• Show that you’re listening: It is important that you are ‘seen’ to be
• Give feedback: Our life experiences and beliefs can distort
• Keep an open mind: a willingness to listen to or accept different ideas or
opinions.• Respond appropriately: Active listening encourages respect
Self-assessment 11.2
1. Differentiate type and technique of communication
2. Explain different types of communication3. Give five techniques used in communication
11.3 Factors and characteristics of communication
Learning activity 11.3
After observing the pictures above, answer the following questions
1) What do you see on picture A?
2) What does every one from picture A means to you ?
3) Is the person sitting in picture B safe ? if no what do you think could bethe cause?
11.3.1. Factors, Barriers and Benefits of effective
communication
a. Factors that enhance effective communication
• Active listening
• Simplicity
• Straight forwardness
• Feedback
• Speaking clearly/articulation
• Knowledge of the receiver / audience
• Speed and sequence of speech
• Relationship between the sender and the receiver
• Command of subject (mastery of subjects matter)• Commanding attention
b. Barriers to effective communication
• Poor listening habits
• Inadequate knowledge of the subject
• Biases and stereotypes
• Lack of interest on the subject
• Personal opinions
• Interruptions
• Religious and cultural difference
• Language barrier
• Poor timing
• Guilt
• Status
c. Benefits of effective communication
• Right information is shared
• Minimizes conflicts
• Resources such as time and money are saved
• Helps in establishing rapport
• Intended results are achieved
• Sender is able to provide intended feedback
• Enhances harmonious co-existence and conflicts are resolved amicably
11.3.2.Collaborative professional communicationLearning activity 11.3.2
Observe the illustration aside and
answer the following questions :
1. In which domain can you classify
the people on the picture ?
2. Are they from the same area of
work ?
3. In which department would you
classify each of them ?
4. Advise them in one sentence
what they can do to achieve their
goals .
Collaboration
Collaboration is defined as a joint effort of multiple individuals or work groups to
accomplish a task or project
Collaborative Practice in health
The collaborative practice in health care can be defined as the provision of
services based on comprehensiveness, developed by health professionals
from different areas. It aims to achieve the highest quality of care in the service
network, involving patients, families, caregivers, and communities. Such practice
can be included in clinical and non-clinical work, such as diagnosis, treatment,
surveillance or communication in health, administration, and sanitary engineering.
Inter-professional collaboration, on the other hand, is characterized by the sharing
of health information, that is, communication between professionals in order to
favor the care of the singularities for those who are inserted in a service in search
for health care
Types of collaboration
• creative – where two or more people create something to achieve a specific
goal,
• connective – bringing together information from disparate sources, and
• compounding – where a team builds on previous achievements to reach
further.
Six Elements of Successful Collaboration
• Motivation. After the thrilling netball final at the recent Commonwealth
Games, the captain of the losing Australian team questioned whether the
lower-ranked English were hungrier for the win. They chased down every ball
relentlessly, making every goal matter. Their effort paid off. Motivating a team
to be first to market, or to create the best possible customer experience, is a
key element.
• Communication. It is important to recognise the difference between
communication – a one-way process where a single person is responsible
– and collaboration – where a group takes responsibility and agrees on how
to achieve the same thing. I like to say that you can communicate without
collaboration, but you can’t collaborate without communication. From setting
out specific objectives and roles, to keeping a team informed of progress and
challenges, strong communication is vital to team achievement.
• Diversity. Just as a soccer team would fail if it consisted of eleven centreforwards,
a business team will flounder if it consists of identical personality
types or roles. A variety of personalities and demographics brings a farbroader range of perspectives.
• Sharing. Making sure that everyone is recognised, and that findings are
shared across the team, leads to stronger bonding and deeper understanding.
Other shared information, such as calendars and scheduling, can also lead
to team efficiency. Apps like Calendar.help, based on Cortana Analytics,
can recognise the nature of an appointment by language from the initiating
email, check everyone’s availability, and suggest suitable times. When a
team member no longer spends time chasing dates, they can devote more
attention to the core objectives of a project.
• Support. When everybody supports each other, without finger-pointing, the
team dynamic is infinitely more powerful. Those able to express ideas in a
supportive environment are more likely to make breakthroughs, whereas
teams with a blame culture repress innovation. Mistakes can be some of the
most powerful learning opportunities in a supportive group.
• Problem-Solving. Any collaboration is about solving problems, so a group
that can’t solve problems can’t work. This often links back to team diversity –
including some problem-solving personalities in the group is essential. This
can mean looking beyond the obvious – sometimes it may be an engineer
who solves a marketing problem, and a customer service clerk who identifies
the flaw in a new app design. Diversity and problem-solving often go handin-
hand.
11.3.3. Caracteristics of goood communicator
Excellent communication skills can benefit most professionals. Being an effective
communicator can improve your work relationships, productivity and mutual
understanding. If you would like to strengthen your communication skills, it may
be helpful to consider the common characteristics of great communicators. In
this article, we list good communication traits to adopt and explain how these
characteristics improve communication.
a. Good listener: Communication usually requires two or more parties to be
active in the conversation. Listening to others can help build relationships
and ensure understanding. Actively listening when others are speaking or
otherwise communicating with you can show that you respect them and allow
you to learn more about the speaker or the subject of the conversation.
b. Concise: Being direct and clear with your communication can ensure that you
properly convey your intentions. For example, if you’re explaining a process
to a new employee, offering clear, straightforward steps can help them learn
quickly. It’s also important to consider your team member’s and client’s time
when conversing with them. If they appear busy, being concise shows you
respect their schedule.
c. Empathetic: Empathizing with others can help you build trust and relationships
in the workplace. Try to be understanding when a coworker or employee ishaving trouble and express your sympathy.
d. Confident: Being confident in your communication can grow your credibility
as a professional. It also can help you properly communicate your needs.
Consider expanding your vocabulary and pausing whenever you are unsure
of what to say. This can help you remember your thoughts and speak clearly.
e. Friendly: Speaking and writing in a friendly tone can encourage others to
communicate with you more often. Consider greeting people when you speak
to them both in verbal conversation and in messages such as emails. Use the
person’s name if you know it, and be positive and friendly when interacting
with others in person or on the phone.
f. Observant: Observing nonverbal communication, such as body language,
is a very important aspect of communication. Recognizing your coworkers’
and customers’ body language can give you insight into how they are feeling.
It can also help you determine how they feel about your own demeanor. For
example, if you’re having a casual conversation with someone who seems
relaxed, your demeanor is probably also relaxed. Being purposeful in your
own body language can help others understand your needs and intentions
as well.
g. Appreciative: Letting others know when you are thankful for their actions can
help motivate your team and improve their skills. Providing verbal positive
reinforcement also can help ensure that the person you are praising or
thanking continues their good practices.
h. Polite: Being polite in your written, verbal and nonverbal communication can
ensure that your intentions are clear. Consider kindly greeting others when
starting conversations, actively listen and use good manners when interacting
with others.
i. Organized: Try to organize your speaking points, emails and other forms of
communication so others understand your intended purpose of the interaction.
j. Sincere: Being genuine when you communicate with others can build a sense
of trust and respect. Speaking with sincerity involves sharing your feelings
and opinions, which can encourage clear and meaningful interactions with
others.
k. Good judgment: Being able to decide the appropriate method and time to
communicate with others can ensure peaceful and effective interactions..
l. Respectful: Showing respect during your communications involves being
polite and attentive. In order to convey your respect for someone you are
speaking with, allow them to finish speaking before replying.
m. Consistent: Consistent communicators interact with others on a regular basis.
Establishing a predictable and reliable channel of communication can help
keep others well informed and maintain work relationships. Consider creating
a time frame and method in which you respond to others or are available for
conversation.
n. Retentive: Being retentive means you can remember details of previous
conversations and interactions with others very well.
o. Inquisitive: Asking detailed and thoughtful questions can lead you to learn
new things and help clarify instructions. Skilled communicators often ask
questions to strengthen their understanding of other’s expectations, intentions
and feelings.
p. Honest: Great communicators are often dedicated to being honest. This
practice can earn you a positive reputation and ensure that all workplace
communication is accurate.
I. Reliable: Being a reliable communicator means that your coworkers and
employees can trust you to start a conversation when needed and respond
effectively to others. Try to craft timely responses when others contact you.
Consider reaching out to others quickly when you need help or clarification.
s. Proactive: Skill communicator address conflicts in a timely manner and starts
a conversation when needed.
t. Reflective: Self-reflection is an important aspect of communication. It allows
you to think thoroughly before speaking, which ensures that you are clearly
and intentionally communicating. Being reflective can also encourage you toconsider how your words and body language might make others feel
Self-assessment 11.3
1. Enumerate five factors that can enhance effective
2. Give seven barriers of effective communication.
3. What are 5 benefits of effective communication?
4. Give six elements of successful collaboration.
5. Define Collaborative professional communication6. What are 5 caracteristics of good communicator?
11.4. Principles and guidance of counsellingLearning activity 11.4
Picture A: Mr x and health care provider in medical specialized
conversation
Mr. x consulted hospital seeking for health care for alleviates distress related
to the death of his wife. Arriving at the hospital the customer care agent orients
him to one health care provider who uses a broad range of culturally –sensitive
practices to help people improve their well-being, prevent and alleviate distress
and maladjustment, resolve crises and increase their ability to function better in
their lives.
Picture B: Miss M and health care provider
Miss M was reading newspapers and found out an announcement about job
application of becoming a head of internal medicine in a hospital. Miss M passed
an exam and was selected for a job position. Now she is having a conversation
with the head of hospital.
Based on the scenario above, answer the following questions:
1) What is the relationship between Mr. X and health care provider?
2) Why Mr. X has been specifically oriented to that health care provider?
3) Can this medical process happen out of health care facility?
4) Based on the picture B and its interpretation what is the conversation
about?
5) Is it really necessary to have this type of conversation on picture B? If yes
why?
11.4.1 Definition of words:
a. Counseling
Counseling is the psychotherapeutic relationship in which an individual receives
direct help from an adviser or finds an opportunity to release negative feelings and
thus clear the way for positive growth in personality.”
b. Guidance
Guidance is a piece of active advice offered to individuals from a superior in the
respective field or a professional. It is the procedure of guiding, managing or leading
a person for a particular course of action.
11.4.2 Counseling process:
Counselors and clients attempt to define, address, and resolve problems of theclient in face-to-face interview
Role of a counselor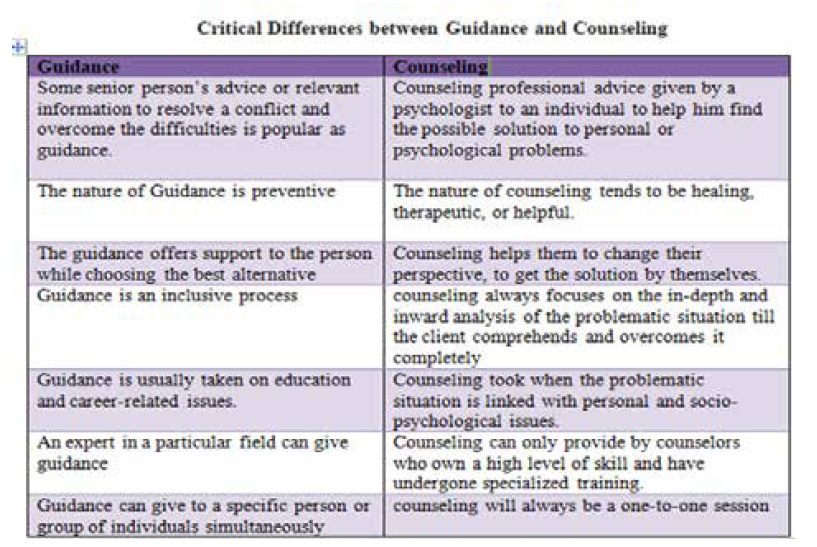
Counseling psychologists help people with physical, emotional and mental health
issues improve their sense by helping them see their situation and feelings from a
different viewpoint. A helping approach that highlights the emotional and intellectual
experience of a client is one of the ways that counseling works with clients from
childhood through to old age.
4 types of counseling
• Individual counseling. Individual counseling is a way to help people work
through difficulties in their lives.
• Couples counseling.
• Group counseling.
• Family counseling
Principles of Counseling:
a. Principle of acceptance
Accept the patient with his physical, psychological,
social, economic and cultural
conditions.
b. Principle of communication
Communication should be verbal as well as non-verbal and should be skillful.
c. Principle of empathy
Instead of showing sympathy put yourself in patient’s shoes and then give reflections
accordingly (Empathy is ability to identify with a person.)
d. Principle of non-judge
Mental attitude-do not criticizes or comments negatively regarding patient’s
complaints.
e. Principle of confidentiality
Always keep the patient’s name, and the problems strictly secrete and assure the
patient about the same.
f. Principle of individuality
Treat each and every patient as unique and respect his problem as well.
g. Principles of non-emotional involvement
Not getting emotionally involved
with the patient and avoid getting carried awaywith his feelings.
Self-assessment 11.4
1. Differentiate Counseling and guidance
2. State 5 types of counseling3. Explain at least 4 principles of counselling
11.5. Counseling skills and qualities of good counselor
Learning activity 11.5
Observe the pictures above and answer to the following questions:
1. What do you see on both picture A and picture B?
2. Why one of each picture is writing?
3. If they are in a health care facility, they are in which unit?
4. Discuss the behaviors of the people on the pictures above?
Qualities of a Good Counselor
There are six personal characteristics that are critical for good counselors and
should be improved upon continually.
These include having good interpersonal skills and being trustworthy, flexible,
hopeful/optimistic, culturally sensitive, and self-aware.
a. Interpersonal skills
Counselors must be able to express themselves clearly and effectively. It is important
not only to be able to educate clients about therapeutic topics, but also to gauge the
client’s understanding at any given time.
Being able to sense what clients are thinking and feeling and relate to them by
showing warmth, acceptance, and empathy are cornerstones of effective therapy.
You can learn about and improve interpersonal skills and empathy by downloading
our Emotional Intelligence Exercises.
b. Trust
According to Hill and Knox (2001), most people determine whether they can trust
someone within 50 milliseconds of meeting them. Counselors must be able to
communicate verbally and nonverbally that they are trustworthy.
Clients need to feel comfortable sharing private, confidential information and parts
of themselves that are often entirely unknown by others. Having faith in the quality
of the relationship and the confidentiality of what is disclosed leads to a deeper
connection with the therapist.
c. Flexibility
A good counselor will create a meaningful treatment plan that is individualized for
each client. This means the counselor shouldn’t follow a rigid schedule of treatment
or have a “one size fits all” approach.
Prochaska and Norcross (2001) found that some treatments are better than
others for specific types of disorders. Matching the treatment to the client’s stage
of readiness is the most effective way to implement therapeutic techniques.
Additionally, counselors need to be able to adapt and change course if treatment is
not working for the client.
d. Hope and optimism
Hope is a wonderful motivator. Effective counselors can find a balance between
realism and hope.
A good counselor will set realistic goals that engage the client and inspire a more
optimistic outlook.
As attainable goals are reached, clients will develop a sense of resilience and
confidence that can help in all areas of life. These traits are why positive psychology
is such an effective method of improving emotional health.
e. Multicultural sensitivity
The American Psychological Association recommends that therapists adapt
treatment to a client’s cultural values and show respect for differences, beliefs, and
attitudes.
When working with clients, it is important to be educated and sensitive to issues of
race, gender, ethnicity, sexual orientation, religion, and cultural background.
f. Self-awareness
An effective counselor can separate personal issues from those of the client.
Countertransference is a phenomenon described by Freud where issues expressed
by a client lead to an emotional reaction of the therapist
g. Counseling skills
Counseling skills are soft (interpersonal) and hard (technical) attributes that a
counselor puts to use in order to best help their clients work through personal
issues and overcome obstacles that are currently preventing them from living a full
and happy life.
h. Examples of counseling skills
There are a variety of skills that are beneficial to a counselor’s understanding of
their client, and to the client’s overall comfort and willingness to be vulnerable about
their personal hardships. Here is a list of useful skills that counselors should have:
i. Active listening
Active listening is an important skill for a counselor to have. It can be defined as the
use of eye contact, facial expressions and gestures to imply that you are engaged
and focused on the information the other person is saying. It can help a client feel
like they’ve been heard and validated in the information they chose to share.
j. Questioning
There are two types of questioning styles that a counselor should be able to utilize—
open questioning and closed questioning. Being skilled in questioning techniques
can help a counselor to better interpret what a client is saying and it can help them
think more deeply into their personal situation as well.
Open questioning includes all questioning that is directed toward gathering more
detailed and complex information. Closed questioning is directed toward more
short-ended questions with specific answers.
k. Note-taking
Counselors should be skilled in organized note-taking techniques in order to record
important points that were discussed during the session and information the client
provided. This can be used for further analysis later on.
l. Interpretation
Counselors should be able to interpret vague information that a client shares and
place it within the context of what they are going through. Phrases like “I’m just so
tired,” or “I’m on edge all the time,” constitute further information, and it is up to the
counselor to interpret this information.
m. Nonverbal communication competency
Similar to information interpretation, counselors should be able to identify current
attitudes or feelings based upon the body language that a client uses during the
session.
n. Self-awareness
Counselors need to be aware of how their body language, gestures and tone of
voice can affect their client and their willingness to talk about the situation. Having
good self-awareness can keep a counselor from accidentally exhibiting signs of
boredom, frustration or judgment.
o. Trustworthiness
An important skill for a counselor is to be able to build and maintain trust with their
clients. This can affect a client’s willingness to share information.
p. Empathy
A counselor needs to be able to see a client’s situation from their perspective in
order to best help them overcome their obstacles.
r. Emotional compartmentalization
Another skill that can be specific to counselors is the ability to emotionally
compartmentalize themselves from their clients and maintain professional
boundaries in order to continue healthy client relationships.
s. Information recall
Counselors should be able to remember information that was shared with them
earlier in the session or from a previous session in order to help guide their
questioning toward a particular client.
t. Confidentiality
Confidentiality can be seen as a valued skill for a counselor to have as they must
respect their clients and the information, they share with them.
u. Record keeping
Counselors should be able to keep detailed records of their clients, relevant
paperwork and session notes to make sure everything stays up-to-date.
Description of counseling process
The process begins with exploring the challenges a client faces. Helping clients with
physical, emotional, and mental health issues, the counselor helps them resolve
crises, reduce feelings of distress, and improve their sense of wellbeing. Treatment
can change how a client thinks, feels, and behaves in an upsetting situation.
Positive psychology includes strengths, values, and self-compassion, and these
science-based exercises will give you the tools to enhance the wellbeing of your
clients, students, or employees. We informally give advice to family, friends, and
colleagues.
A professional counselor is a highly trained individual who is able to use a different
range of counseling approaches.Self-assessment 11.5
1. State different qualities of a good councilor?
2. Enumerate different counseling skills?
3. Describe the process of counseling?
11.6. Counseling process and barriers to effective
counsellingLearning activity 11.6
Based on the picture beside:
1) Are the two people in good mood?
2) Can they communicate well?
3) If they cannot communicate well, what
is the main reason?
4) What does the man need?
5) Which factor can help the two people toeffective counseling?
5 stages of the counseling process
• Relationship building is stage one of the process.
• Stage two is problem assessment.
• Goal setting is the third stage.
• Stage four includes counseling intervention.
• Stage five includes evaluation, firing or referral.
• The client has some key steps.
Therapeutic communication skills during client-nurse relationship
Roger’s theory and practice supported the patient’s ability to foster self-knowledge
and control his impulses by empowering him to actively contribute to his own
healing.
Therapeutic Communication Skills are:
• Empathy
• Authenticity
• Unconditional Positive Regard
• Accepting others for who they are is the basis of therapeutic communication
and the foundation on which humanistic psychology lies.
a. Empathy
Sensing a client’s emotions and reacting to them as if they were your own
describes empathy within therapy. This concept of compassion reflects your
profound understanding of the client’s emotions and circumstances that exceeds
any calculated analysis of the client by the therapist. In his article on clientcentered
therapy, Rogers emphasizes the characteristics of successful therapeutic
communication by saying: “If the counselor can create a relationship permeated
by warmth, understanding, safety from any type of attack, no matter how trivial,
and basic acceptance of the person as he is, then the client will drop his natural
defensiveness and use the situation.
Sensing a client’s emotions and reacting to them as if they were your own
describes empathy within therapy. Feeling emotion with a patient can generate a
compassionate and therapeutic environment in which the patient can feel secure
and recognize that you’re listening to him rather than evaluating him.
b. Authenticity
Exhibiting genuine thoughts and emotions in the therapeutic approach and gaining
insight into your patient requires you to also be in touch with your own feelings.
Rogers called for the clinician to be “a real human being with real thoughts, real
feelings, and real problems.” In order for an effective therapeutic client-centered
relationship to form, you must be sensitive and honest in your communication.
Exhibiting genuine thoughts and emotions in the therapeutic approach and gaining
insight into your patient requires you to also be in touch with your own feelings.
Therapists must also posses an intuitive sense of self because it cultivates trust and
confirms that you aren’t projecting yourself as a superior force over your patient.
c. Unconditional Positive Regard
Displaying unconditional positive regard means that you show your patient that no
matter what he does, your respect for him remains the same. Yet, you continue
to reveal the desire for him to move towards healing. Rogers emphasized the
importance for the therapist to remove any concern for diagnostic tendencies
and be available to provide the patient with acceptance and consideration of the
emotions he’s exploring in the present.
English psychotherapist Greg Mulhauser of Mulhauser Consulting, Ltd., explains
that unconditional positive regard implies that you accept your client categorically
and without prejudice. This notion of therapy assures the client that he may examine
and express any of his thoughts or feelings without the threat of being criticized or
disregarded.
Displaying unconditional positive regard means that you show your patient that no
matter what he does, your respect for him remains the same.
This notion of therapy assures the client that he may examine and express any of
his thoughts or feelings without the threat of being criticized or disregarded.
Barriers to effective counseling
a. Counseling is too expensive.
Anyone who is considering counseling is making a choice about how to manage
the difficult circumstances in their life. By the time this choice is being made there’s
a good chance they’ve already tried any number of other alternatives that aren’t
working.
b. Counseling is too embarrassing.
It can be very difficult to find someone to trust. Almost everybody in your life has
a set of expectations for you, and your relationship with them usually depends on
how well you meet those expectations.
I’ve been to counseling and it didn’t work.
Counseling, like any other relationship, requires clear expectations, healthy
boundaries, and honesty. It is important that both the counselor and client are
able to admit when their personalities or perspectives don’t match. In some cases
a smooth ending to a counseling relationship, for whatever reason, may not be
possible.
I’m not the one who needs counseling.
All of us know somebody who needs therapy. After reading that you’re probably
thinking about them right now. To be honest, if you start asking around you’ll
probably find a few people who think that about you.
I don’t have time for counseling.
Anxiety is all around us. Technology has made everything easier to do, so instead
of relaxing we end up trying to do more than ever. The need to achieve can quicklyuse up our time, our energy, and our attention.
Self-assessment 11.6
1. What is counseling process?
2. What are the 5 types of counseling?3. Critically Differentiate Guidance and Counseling?
End unit 11 assessment
1. Referring on the communication process diagram, complete the chartbelow
2. Define the following words :
a. Communication
b. Collaboration
c. Counselling
d. Guidance
e. Empathy
3. What is the difference between verbal and non-verbal communication?
4. What are the Benefits of effective communication
5. Explain the role of a counsellor during a psychotherapy session
6. Give 5 stages of the counseling process?7. Enumerate barriers of counseling?
UNIT 12 GENDER BASED VIOLANCE (GBV)
Introductory activity 12
Observe the above images and attempt the following questions: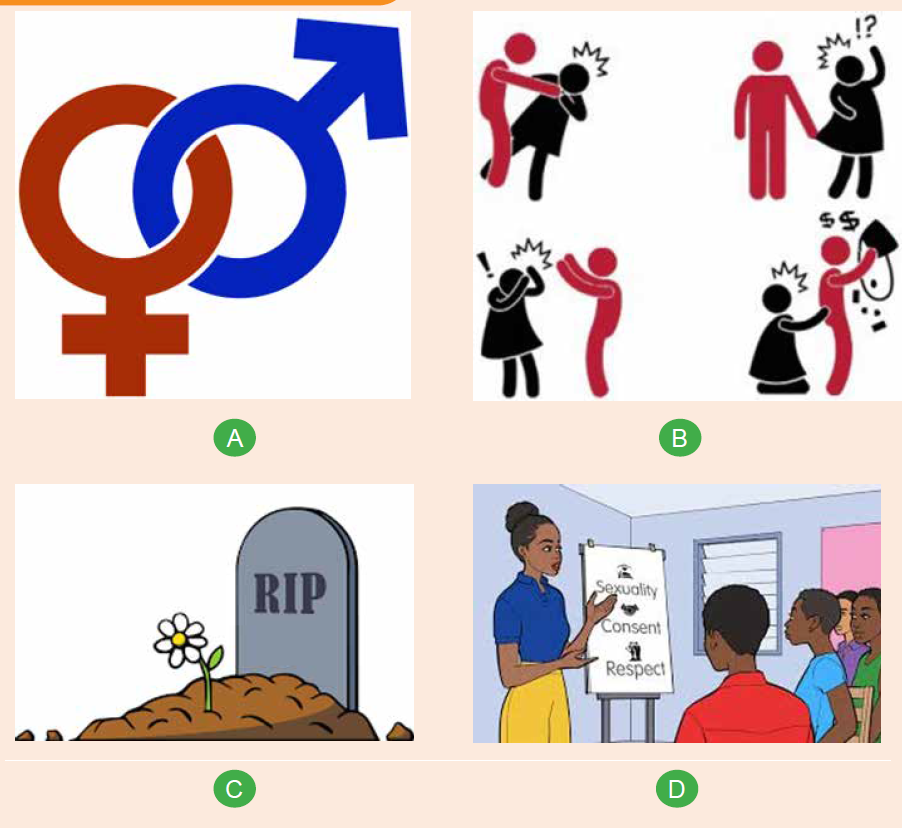
a. What do you think Image A represent?
b. What do you think picture B is trying to describe?
c. What do you think image C?d. What do you think is happening in image D?
12.1.Introduction to gender and gender-based violence
related conceptsLearning activity 12.1
Carefully observe the above images and attempt the following questions: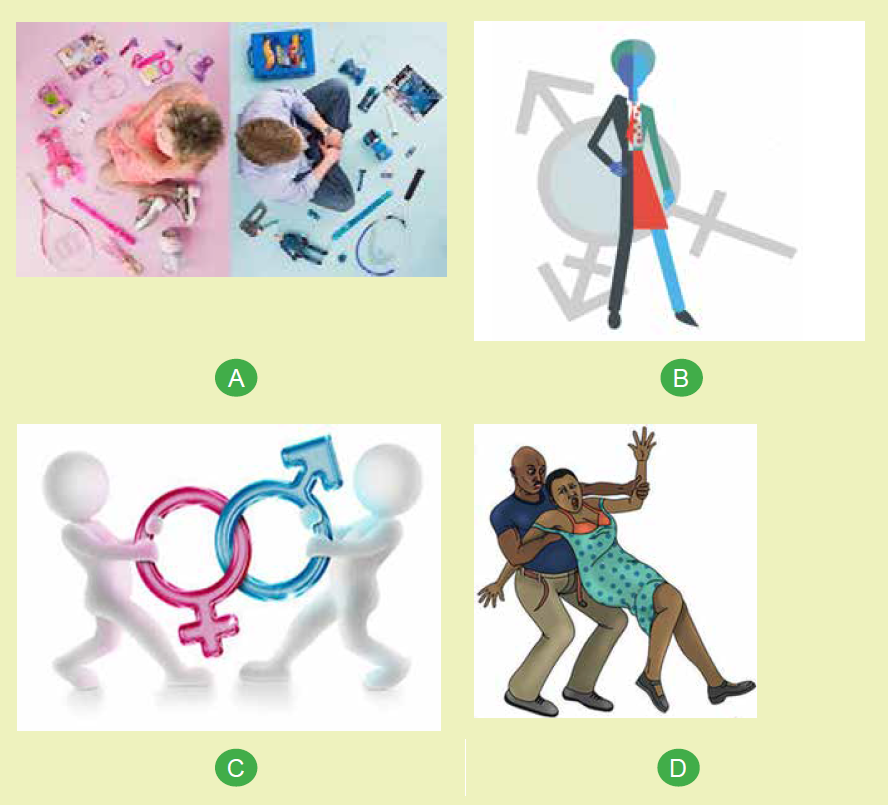
a. What does image A try to explain?
b. What do you think of image B?
c. What do you think of image C is about?d. What do you think is happening in image D?
12.1.1 Gender and sex
Gender refers to what it means to be a male or a female in a given society and
culture. Thus, gender is social construct that determines the roles, behaviour,
activities and attributes that a particular society at a given time considers appropriate
for men and women, girls and boys. It is shaped by the sociocultural environment
and experience in addition to biology and vary widely within and between cultures
and often evolve over time.
Gender is not synonymous to sex; which refers to biological classification of
people as male or female based on physical and physiological features including
chromosomes, gene expression, hormone level and function, and reproductive and
sexual anatomy. The term “intersex” is used as an umbrella term for individuals
born with natural variations in biological or physiological characteristics (including
sexual anatomy, reproductive organs and or chromosomal patterns that do not fit
traditional definitions of male or female. Infants are generally assigned the sex of
male or female at birth based on the appearance of their external genitalia.
12.1.2 Sexual orientation and gender identity
There is tremendous variability in the ways that individuals express their gender and
in the ways, they express their sexual orientation. Accordingly, various concepts exist
to accommodate these variations and healthcare providers should be conversant
with them to appropriately use them when working with diverse clients.
Sexual orientation is a function of sexual attraction, identity, and behavior. Sexual
attraction is about the type of person an individual desire sexually, romantically,
emotionally, and in other sexual ways; heterosexual individuals are attracted to
people of the opposite sex, homosexual individuals are attracted to people of the
same sex, and bisexual individuals are attracted to both people of the opposite
sex and the same sex. Sexual identity is about how people present their sexuality
to others, with some people very private about their sexual identity and others very
open. Sexual behavior is about the sexual actions in which a person engages.
Some people choose to be celibate.
Besides sexual orientation exists gender identity, which is an individual’s sense
of maleness or femaleness and gender expression which is how an individual
expresses their own gender to the world, i.e., through names, clothes, how they
walk, speak, communicate, their roles in society and general behaviour. These may
sometimes not match societally accepted norms for their biological sex at birth. A
cisgender person has a gender identity that aligns with the sex assigned to that
person at birth. A transgender person has a gender identity that does not match
the sex assigned at birth.
12.1.3 Gender equality and equity
Gender being an array of socially constructed characteristics and roles, makes it
hierarchical and is surrounded with inequalities and inequities. Gender inequality
refers to unequal treatment or perceptions of individuals based on their gender.
It emerges when one of the two sexes is considered more valuable, capable,
powerful, and has more access to information, resources and opportunities than
the other and is an important factor for gender-based violence. Opposed to this,
is gender equality that refers to a state where there is no discrimination on the
basis of a person’s sex in the allocation of resources and in the access to various
services in a society. With gender equality, individual’s rights, responsibilities and
opportunities are not determined by the sex they are assigned at birth nor gender
identity or sexual orientation.
To achieve gender equality, some strategies and processes “equity” come in.
Gender equity therefore refers to fairness and justice in the distribution of
resources, opportunities, and benefits to women/girls in relation to men/boys. It
implies objectivity of treatment for all genders with regards to their respective needs
and strives to bring all the genders to an equal playing field. It recognizes that certain
groups face disadvantages because of historical and structural reasons therefore
contextual measures required to ensure that their disadvantaging situations are not
perpetuated.
12.1.4 Gender-based violence
Gender-based violence (GBV) refers to any act of violence that results in, or is
likely to result in, physical, sexual or psychological harm or suffering to someone
on the basis of their gender or sex. Although, this definition is applicable to both
men and women, the phenomenon of GBV mostly affects women. It roots deeply
in discriminatory cultural beliefs and attitudes that perpetuate inequality andpowerlessness, in particular of women and girls.
Self-assessment 12.1
1. What is the difference between gender and sex?
2. What does intersex mean to you?
3. Define the following concepts:
a. Gender-based violence
b. Sexual behaviourc. Gender identity
12.2 Role of gender in health promotion and diseases
preventionLearning activity 12.2
Carefully observe the above images and attempt the following questions:
a. What do you think image A is attempting to explain?
b. What do you think image A is attempting to explain?
c. Through the lens gender and health, attempt to establish a relationship
between image A and B
It is usually wise to spent little on health promotion and disease prevention
interventions than to spend relatively large amounts of money for recovery from
serious health problems. Disease prevention involves determining preventive
health interventions that are effective in various population group as well as how
well successful interventions can be scaled up for widespread implementation.
Health promotion, on the other hand, encourages individuals and communities
to improve their health through healthy public policies, supportive environments,
skilled personnel, strong communities, and increased access to preventive health
services.
Biological differences between male and female along with socially constructed
masculine and feminine the roles and responsibilities affect both health promotion
and disease prevention strategies. Cognizant of this, any of these interventions
should carter for these differences to yield good results. For instance, these
differences affect the way different individual or groups of individuals take risk
beside risks they are exposed to; their attempts to improve their health, and how
the health system responds to their needs. Furthermore, gender-based principles
as well as discriminatory societal and cultural norms and prejudices, may translate
into activities that harm one’s health and well-being.
12.2.1 Gender and health promotion
Gender influences on health include access to health-promoting resources,
commonplace exposure to health-damaging and health-promoting factors, and
varied expectations of behavior such as consuming alcohol, taking risks, and using
healthcare. For instance men have more harmful smoking practices, unhealthier
dietary patterns, heavier alcoholic drinking habits and higher rates of injuries and
interpersonal violence than women. With traditional masculinities and femininities
expectations women are less likely to engage into physical activities than men.
Additionally, traditional masculinities frequently function as a barrier to men
seeking health treatment, engaging in preventive behaviors, and managing selfcare,
whereas women’s health is frequently relegated to sexual, reproductive, and
maternal health.
Effective health promotion program should be holistic and use gender analysis
and gender integration for healthy public policies can be developed for concrete
and effective individual and community actions relevant to promoting health and
wellness. Effective health promotion policies and programmes are those centred on
joint commitment and that use a multi-sectorial approach and which are based on
evidence gathered with gender dimensions in mind.
12.2.2 Gender and diseases prevention
Gender norms, roles and relations influence the development and course of risk
factors of various diseases and impact the way men and women use services and
respond to healthcare services therefore affect various level of disease prevention.
For instance, traditional masculinities will often act as a barrier to men seeking
health care including those required for primary (e.g., vaccination), secondary (e.g.
checking blood pressure routinely to detect the onset of hypertension) and tertiary
(e.g. Physical therapy to people who have been injured in a vehicle collision in
order to prevent long term disability) disease prevention. Furthermore, they may
also adopt risky behaviours heavy smoking, drug use, etc. which is associated
disastrous health affects couple with poor self-care management.
On the other hand, women play a vital role in health promotion as in most culture
and societies they are regarded to master the art of taking care of others. For
instance their involvement into children vaccination program cannot be overlooked
beside the role they play in nutrition of their family members. Additionally, health
education messages quite often target women as viewed as care guarantor of every
individual in the household. Nevertheless, following prevailing gender inequalities
that affect mostly women, implementation prevention strategies might face short
comings, thus not as effective. These inequalities also expose women to GBV with
associated health outcomes hence specific prevention strategies.
As for health promotion, disease prevention plans should address differences
between women and men, boys and girls in an equitable manner in order to beeffective.
Self-assessment 12.2
1. Contrast health promotion and disease prevention
2. What should be done gender-wise, for an effective health promotionprogram?
12.3. Types of gender based violenceLearning activity 1.8
Carefully observe the above images and attempt the following questions:
a. What is common across the above images?b. Describe what you see in each picture and attempt categorizing GBV
GBV is a complex phenomenon that affects both males and females differently,
women and girls being the most affected. Categorizing its different types varies;
and it can be categorized as Sexual violence i.e. rape, forced prostitution, incest,
sexual abuse, etc.; Physical violence i.e. trafficking, slavery, war, displacement etc.;
Emotional &psychological violence (abuse, humiliation, confinement, etc.);Harmful
traditional practices such as female genital mutilation, early marriage, honour
killing, etc.; and Socio-economic violence such as discrimination, social exclusion,
ostracism based on sexual orientation, etc.
a. Physical violence:
Physical violence is an act attempting to cause, or resulting in pain and or physical
injury through coercion. Physical violence in intimate relationships, often referred
to us as domestic violence, continues to be a widespread phenomenon in every
country. Acts of physical violence include beating, burning, kicking, punching, biting,
maiming or killing, or the use of objects or weapons.
Some classifications also include human trafficking and slavery in the category
of physical violence because initial coercion is often experienced, and the people
involved often end up becoming victims of further violence as a result of their
enslavement. Physical violence in the private sphere also affects young people. As
mentioned above, witnessing the abuse of one parent by another leads to serious
psychological harm in children. Often, children and young people who are present
during an act of a parent abuse like spouse abuse may also be injured, sometimes
by accident and sometimes because they try to intervene.
b. Verbal violence and hate speech
Verbal violence can include issues that are specific to a person, such as putdowns
(in private or in front of others), ridiculing, the use of swear-words that are
especially uncomfortable for the other, saying bad things about the other’s loved
ones, threatening with other forms of violence, either against the victim or against
somebody dear to them. At other times, the verbal abuse may be relevant to the
background of the victim, such as their religion, culture, language, (perceived)
sexual orientation or traditions. Depending on the most emotionally sensitive areas
of the victim, abusers often consciously target these issues in a way that is painful,
humiliating and threatening to the victim.
Most of the verbal violence that women experience because of being women is
sexualized, and counts as sexual violence. Verbal gender-based violence in the
public sphere is also largely related to gender roles and it may include comments
and jokes about women or may present women as sex objects (e.g. jokes about
sexual availability, prostitution, rape). A great deal of bullying is related to the
perceived sexuality of young people (especially boys).
The regular negative use of words such as “queer” or “fag” is often traumatizing for
those perceived as gays and lesbians. This is very likely one of the reasons why
many gays and lesbians only “come out” after secondary school.
Verbal violence may be classified as hate speech and can take many forms i.e.
words, videos, memes, or pictures that are posted on social networks, or it may
carry a violent message threatening a person or a group of people because of
certain characteristics.
Many cultures have sayings or expressions to the effect that words are harmless,
and there is a long tradition that teaches people to ignore verbal attacks. However,
when these attacks become regular and systematic and purposefully target
someone’s sensitive spots, the object of the attacks is right to consider themselves
victims of verbal abuse. Gender-based hate speech mainly targets women (in this
case, it is often called “sexist hate speech”).
Gender-based hate speech can take many different forms i.e. jokes, spreading
rumors, either using internet using online messaging, threats, slander, and
incitement of violence or hate. It aims at humiliating, dehumanizing and making a
person or group of people scared. As with any type of violence, gender-based hate
speech is usually very destructive for the person targeted. People who experience
hate speech often feel helpless, and do not know what to do.
c. Emotional & psychological violence:
All forms of violence have a psychological aspect, since the main aim of being
violent or abusive is to hurt the integrity and dignity of another person. Apart from
this, there are certain forms of violence which take place using methods which
cannot be placed in other categories, and which therefore can be said to achieve
psychological violence in a “pure” form. This includes isolation or confinement,
withholding information, disinformation, and threatening behavior. In the private
sphere, psychological violence includes threatening conduct which lacks physical
violence or verbal elements, for example, actions that refer to former acts of
violence, or purposeful ignorance and neglect of another person.
d. Sexual violence:
Includes actual, attempted or threatened (vaginal, anal or oral) rape, including
marital rape; sexual abuse and exploitation; forced prostitution; transactional or
survival sex; and sexual harassment, intimidation and humiliation. Furthermore,
sexual violence comprises engaging in non-consensual vaginal, anal or oral
penetration with another person, by the use of any body part or object; engaging in
other non-consensual acts of a sexual nature with a person; or causing someone
else to engage in non-consensual acts of a sexual nature with a third person. Marital
rape and attempted rape constitute sexual violence.
Examples of forced sexual activities include being forced to watch somebody
masturbate, forcing somebody to masturbate in front of others, forced unsafe sex,
sexual harassment, and abuse related to reproduction (e.g. forced pregnancy,
forced abortion, forced sterilization, female genital mutilation).
Certain forms of sexual violence are related to a victim’s personal limits, and are
more typical of the private sphere. The perpetrator deliberately violates these
limits: examples include date rape, forcing certain types of sexual activities. One
common example of such violence in the public sphere includes the isolation of
young women or men who do not act according to traditional gender roles. Isolation
in the public sphere is most often used by peer groups, but responsible adults such
as teachers and sports coaches can also be perpetrators. Most typically, isolation
means exclusion from certain group activities. It can also include intimidation, in a
similar fashion to psychological abuse in the private sphere withdrawal of sexual
attention as a form of punishment, or forcing other(s) to watch (and sometimes to
imitate) pornography.
e. Socio-economic violence
Socio-economic deprivation can make a victim more vulnerable to other forms of
violence and can even be the reason why other forms of violence are inflicted.
Typical forms of socio-economic violence include taking away the earnings of the
victim, not allowing them to have a separate income (giving them “housewife”
status, or making them work in a family business without a salary), or making the
victim unfit for work through targeted physical abuse.
Socio-economic violence in the public sphere is both a cause and an effect of
dominant gender power relations in societies. It may include denial of access to
education or(equally) paid work (mainly to women), denial of access to services,
exclusion from certain jobs, denial of pleasure and the enjoyment of civil, cultural,
social and political rights. Some public forms of socio economic gender-based
violence contribute to women becoming economically dependent on their partner
(lower wages, very low or no child-care benefits, or benefits being tied to the income
tax of the wage-earning male partner). Such a relation of dependency then offers
someone with a tendency to be abusive in their relationships the chance to act
without fear of losing their partner.
f. Domestic violence or violence in intimate relationships
Domestic violence includes acts of physical, sexual, psychological or economic
violence that occur within the family or domestic unit or between former or current
spouses or partners, whether or not the perpetrator shares or has shared the same
residence with the victim. Domestic violence, or intimate partnership violence, is
the most common type of GBV. It also requires special attention, because it is
a relational type of violence, and the dynamics are therefore very different from
violent incidents that occur among strangers.
The fact that domestic violence was long considered to be a private, domestic
issue has significantly hampered recognition of the phenomenon as a human rights
violation. The invisibility of the phenomenon was reinforced by an understanding
of international human rights law as applicable only to relations between individual
and the state (or states). However, it is now recognized that state responsibility
under international law can arise not only from state action, but also from state
inaction, where a state fails to protect citizens against violence or abuse (the “due
diligence” principle).
Although the vast majority of domestic violence is perpetrated against women by
men, it actually occurs in same sex relationships just as frequently as in heterosexual
relationships, and there are cases of women abusing their male partners. Domestic
violence such as rape, battering, sexual or psychological abuse leads to severe
physical and mental suffering, injuries, and often death.
g. Harmful traditional practices and sexual harassment
Include female genital mutilation/cutting (FGM/C); forced marriage; child marriage;
honour or dowry killings or maiming; infanticide, sex-selective abortion practices;
sex-selective neglect and abuse; and denial of education and economic opportunities
for women and girls.
Sexual harassment defined as any form of unwanted verbal, non-verbal or physical
conduct of a sexual nature with the purpose or effect of violating the dignity of a
person, in particular when creating an intimidating, hostile, degrading, humiliating or
offensive environment. Verbal examples of sexual harassment may include making
sexual comments about a person’s body, making sexual comments or innuendos,
asking about sexual fantasies, preferences, or history, asking personal questions
about someone’s social or sex life, making sexual comments about a person’s
clothing, anatomy, or looks, repeatedly trying to date a person who is not interested,
telling lies or spreading rumors about a person’s sex life or sexual preferences.
Examples of non-verbal harassment include looking a person up and down
“elevator eyes”, following or stalking someone, using sexually suggestive visuals,
making sexual gestures with the hands or through body movements, using facialexpressions such as winking, throwing kisses, or licking lips.
Self-assessment 12.3
1. Explain the different types of gender-based violence?
2. Which of the following types of violence can be defined as a form of
psychological violence? (Choose all that apply):
a. Making threats
b. Teasing
c. Intimidation
d. Insulting someone and Bullying
e. Humiliation and Ignoringf. All of the above
12.4. Common causes of Gender Based ViolenceLearning activity 12.4
Carefully observe the above images and attempt the following questions:
a. According to your understanding, what each of the above image represents?
b. Referring to what you see on the above images, what do you think are
causes of the GBV?
The root cause of GBV is the imbalance of power in relationships between men and
women.
GBV is deeply rooted in discriminatory cultural beliefs and attitudes that perpetuate
inequality and powerlessness, in particular of women and girls. Various other factors,
such as poverty, lack of education and livelihood opportunities, and impunity for
crime and abuse, also tend to contribute to and reinforce a culture of violence and
discrimination based on gender.
However, a variety of factors on the individual level, the family level, and at the
level of community and society, often combine to raise the likelihood of violence
occurring. There is no single factor that can explain gender-based violence in our
societies, but rather a myriad of factors contributes to it, and the interplay of these
factors lies at the root of the problem. Cultural, legal, economic and political factors
are the main 4 categories of GBV underlying factors.
a. Cultural factors
These include gender stereotypes and prejudice, normative expectations of
femininity and masculinity, the socialization of gender, an understanding of the
family sphere as private and under male authority, and a general acceptance of
violence as part of the public sphere (e.g. street sexual harassment of women), and
or as an acceptable means to solve conflict and assert oneself.
Religious and historical traditions have sanctioned the physical punishment of
women under the notion of entitlement and ownership of women. The concept of
ownership, in turn, legitimizes control over women’s sexuality, which, according to
many legal codes, has been deemed essential to ensure patrilineal inheritance.
Sexuality is also tied to the concept of so-called “family honour” in many societies.
With this regards, traditional norms in these societies allow the killing of women
suspected of defiling the “honour” of the family by indulging in forbidden sex or
marrying and divorcing without the consent of the family. The same norms around
sexuality can help to account for the mass rape of women.
b. Legal factors
Being a victim of GVB is perceived in many societies as shameful and weak, with
many women still being considered guilty of attracting violence against themselves
through their behaviour. This partly accounts for enduring low levels of reporting and
investigation. Until recently, the law in some countries still differentiated between
the public and private spaces, which left women particularly vulnerable to domestic
violence.
There are times even though most forms GVB are criminalized, the practices of law
enforcement may in many cases favor the perpetrators, which help to account for
low levels of trust in public authorities and for the fact that most of these crimes go
unreported. In many societies, the decriminalization of homosexuality is still relatively
new. While some countries have made progress by allowing equal marriage, this
has often resulted in a backlash, such as strengthening opinions that the traditional
family is a union between a man and a woman, or where governments have passed
laws prohibiting “gay propaganda.”
c. Economic factors
Scarcity of resources generally makes women more vulnerable to violence and
sometimes men as well. It creates patterns of violence and poverty that become
self-perpetuating, making it extremely difficult for the victims to extricate themselves.
When men face unemployment and hardship, they may react violently to assert
their masculinity.
d. Political factors
The under-representation of women in power and politics means that they have
fewer opportunities to shape the discussion and to affect changes in policy, or
to adopt measures to combat GBV and support equality. The topic of genderbased
violence is in some cases is deemed not to be important, with domestic
violence being given insufficient resources and attention. Though, women have
raised questions and increased public awareness around traditional gender norms,
highlighting aspects of inequality and its relationship to GBV, this status quo has not
changed much due to lack of enough political influence.
e. Harmful Gender Norms
Gender stereotypes are often used to justify violence against women. Cultural norms
often dictate that men are aggressive, controlling, and dominant, while women are
docile, subservient, and rely on men as providers. These norms can foster a culture
of abuse outright, such as early and forced marriage or female genital mutilation,the latter spurred by outdated and harmful notions of female sexuality and virginity.
Self-assessment 12.4
1. What are the deepest root causes of gender-based violence?
a. Poverty
b. Abuse of power, inequality between men and women and disrespect for
human rights
c. Lack of education
d. Abuse of power and poverty
e. War
2. What impacts do conflict and natural disaster have on GBV? (Choose all
that apply):
a. Women and girls have to travel further to get necessary resources and are
therefore exposed to violenceb. Militarization leads to more violence
c. There are more opportunities for sexual exploitation
d. Social and support structures breakdown which makes everyone morevulnerable
12.5. The primary victims and survivors of Gender Based
ViolenceLearning activity 12.5
Carefully observe the above images and attempt the following questions:
a. Describe what you see in picture A
b. Describe if any, relationship between picture A and picture B anddifferentiate primary victim from other ones
Both the terms of survivor and victim are used for a person who experienced
GBV and often used interchangeably. The term “victim” is often used in the legal
and medical sectors, recognizing that many forms of GBV are crimes. The term
“survivor” is generally preferred in the psychological and social support sectors
because it implies resiliency.
Gender-based violence is a widespread problem that affects males and females.
It disproportionately affects women and girls as a result of power imbalances
stemming from gendered power structural perceptions of masculinity and femininity
that create a rank order of gender.In case of domestic violence, children can be
affected by violence committed against their mothers, and they themselves can be
abused by the perpetrator, which can often be their fathers or stepfathers.
Persons who have been separated from their family or community, and or lack
access to shelter, education and livelihood opportunities, are among those most
at risk of GBV. This includes Children, especially unaccompanied minors, fostered
children, female and child heads-of-households, boys and girls in foster families or
other care arrangements, persons with mental and or physical disabilities, persons
in detention, house girls, single mothers, economically disempowered people, junior
staff, students, less privileged community members particularly those of minority
groups, asylum seekers, refugees and internally displaced people and girls and
boys born to rape victims/survivors. Women are the primary victim of GBV becausethey are usually second class, culturally considered inferior.
Self-assessment 12.5
1. True or false? GBV affect only women and girls as culturally considered
inferior
2. Children X and Y assist a domestic GVB. What kind of victim are they?3. Contrast the terms of victim and survivor with regard to GBV.
12.6 The main GBV perpetratorsLearning activity 12.6
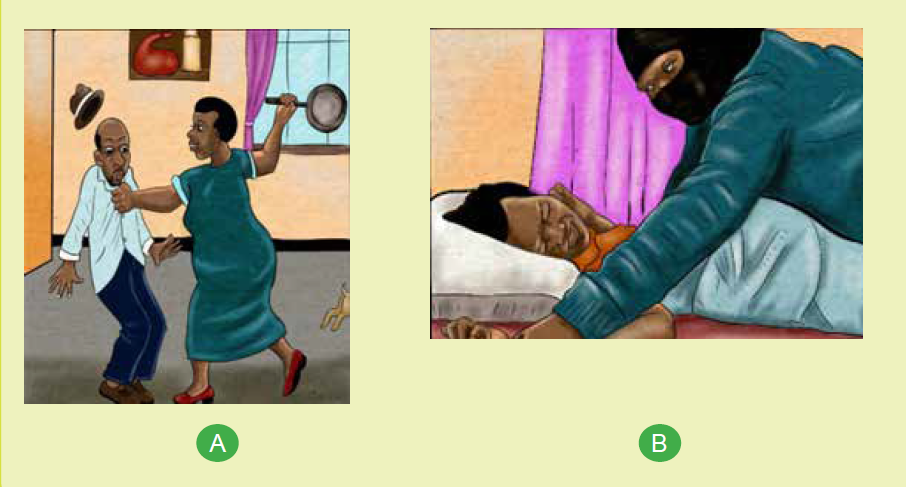
Carefully observe the above images and attempt the following questions: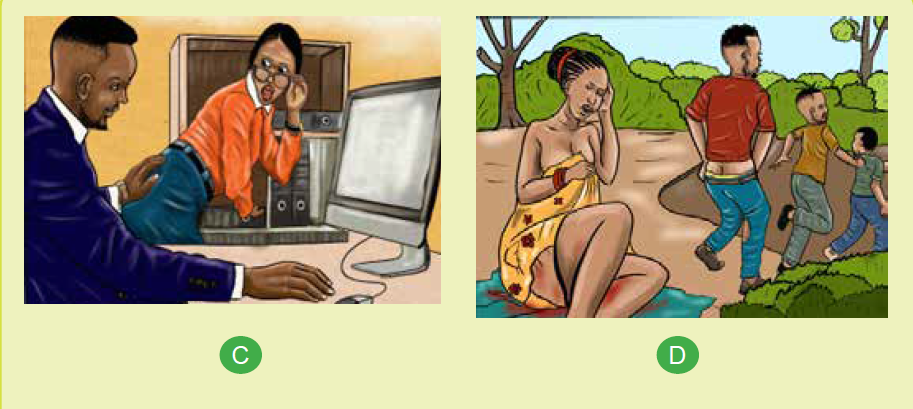
a. What is common to all the images above?
b. Describe what you see in each picture and attempt to establish therelationship between the individuals observed
A perpetrator is an individual, group, or institution that inflicts, supports, or
condones act of GBV or other types of abuse against a person or group of persons.
Generally, perpetrators include those individuals with real or perceived power,
persons in decision making positions or persons in authority. Anyone can be a GVB
perpetrator though primary GBV perpetrators are men and boys who often use
violence to assert or maintain their privileges, power and control over others.
GBV is usually perpetrated by persons who hold a position of power or control others,
whether in the private or public sphere. In most cases, those responsible are known
to the victim/survivor, such as intimate partners, family members, friends, domestic
staff and influential community members who are in positions of authority (teachers,
community or religious leaders, politicians). Others in positions of authority, such as
police or prison officials, and members of armed forces and groups, are frequently
responsible for such acts, in particular in times of armed conflict. In some cases,
this has also included humanitarian workers and peacekeepers. Furthermore, by
depicting women and girls negatively in their products, musicians, storytellers, and
other artists unconsciously promote GBV along with the role of mass media in
diffusing these.
• Intimate partners (husbands, wives, boyfriends, and girlfriends) may
perpetrate various murder, physical assault, marital rape, date rape, battery,
sexual violence, neglect, vandalism of property, confiscation of property,
forced sodomy, among, etc.
• Family member and friends; a category of perpetrators that is usually not
reported, may perpetrate incest, battery, trafficking, exposure to pornography,
neglect, denial of education, female genital mutilation, etc.
• Influential community members: This category of GBV perpetrator includes
people who enjoy positions of authority that they can easily abuse such
teachers, community leaders, politicians, religious leaders and business
owners. Examples of GBV perpetrated include sexual exploitation, sexual
harassment, forced prostitution, battery, and trafficking. Because of fear of
retaliation, loss of privileges, or pressure to protect the perpetrator’s honour;
survivors may find it difficult to report them.
• Security forces (soldiers, police officers, guards): This category holds the
authority to give and deny rights and privileges which they can eventually
abuse to perpetrate sexual extortion, arbitrary arrest, extrajudicial killing,
violating people who report to them, and concealing evidence.
• Institutions may perpetrate GBV by omission or commission. Institutions,
for example, might provide discriminatory social services that preserve and
expand gender inequalities, such as withholding information, delaying or
rejecting medical treatment, paying uneven wages for the same labor, and
obstructing justice. They may also fail to prevent or respond to GBV, and may
even institutionalize cultures that favor GBV.
• Humanitarian assistance workers: they hold positions of great authority and
command access to vast resources, including money, influence, food, and
basic services; unfortunately, some use this power to commit GBV, especially
sexual exploitation and abuse.Self-assessment 12.6
1. Explain the role of mass media in promoting acts of GBV
2. True or false?
• Religious leaders are respected man of God therefore clean from
perpetrating GBV
• Perpetrators are always unknown to their victims
• From fear of repercussion, survivor of GBV perpetrated by community
leaders are less likely to be reported
3. Which category of GBV perpetrators is associated with female genitalmutilation?
12.7. Interventions for GBVLearning activity 12.7
Carefully observe the above images and attempt the following questions:
a. According to you understanding, describe what you see image A, B, C
b. Establish if any, relationship across images A, B and C
c. With reference to observed images, explain what can be the interventionsfor GBV
Combating gender-based violence requires an understanding of its causes and
contributing factors, which often also serve as barriers to effective prevention and
response.
There is a growing awareness and evidence that men and boys, in partnership with
women and girls, can play a significant role. Engaging men and boys as part of the
solution, instead of approaching them as perpetrators, is most effective.
a. The responsibility of the country
The country has primary responsibility for preventing and responding to genderbased
violence. This includes taking all necessary legislative, administrative,
judicial and other measures to prevent, investigate and punish acts of gender-based
violence, whether in the home, the workplace, the community, while in custody, or
in situations of armed conflict, and provide adequate care, treatment and support
to victims/survivors.
To that effect country should, for ensure the following:
• Criminalize all acts of gender-based violence and ensure that national law,
policies and practices adequately respect and protect human rights without
discrimination of any kind, including on grounds of gender.
• Investigate allegations of GBV thoroughly and effectively, prosecute and
punish those responsible, and provide adequate protection, care, treatment
and support to victims/survivors, including access to legal counseling, health
care, psycho-social support, rehabilitation and compensation for the harm
suffered.
• Take measures to eliminate all beliefs and practices that discriminate against
women or sanction violence and abuse, including any cultural, social,
religious, economic and legal practices.
• Take action to empower women and strengthen their personal, legal, social
and economic independence
b. The role of human rights and humanitarian actors
While primary responsibility lies with the national authorities, human rights and
humanitarian actors also play an important role in preventing and responding to
GVB. In addition to ensuring an effective GBV response from the beginning of an
emergency, this entails ensuring that gender concerns are adequately integrated
into and mainstreamed at all levels of the humanitarian response. Human rights and
humanitarian actors, as well as peace-keepers, must not under any circumstances,
encourage or engage in any form of sexual exploitation or abuse.
c. Role of community
This is through community groups (especially existing women’s groups); trusted
individuals (people who have been champions to speak out about positive male
norms, and the unacceptability of GBV); religious leaders and community leaders.
These groups may involve relevant community members and deploy resources
depending to the context. Using male engagement approaches is also one of
important aspects community intervention focus on. Additionally, engage key
individuals and organizations who are already working in the community.
d. The health institutions
They should think of ways to include the tracking of GBV-related incidents or
related norms within their programs and consider including activities that have the
potential to prevent GBV. Partnering with organizations that have GBV expertise
to provide GBV-related trainings to various groups they work with e.g. producer
groups, mother’s groups, etc. and allocate resources to GBV-specific inquiries and
trainings.
Working with local organizations that have expertise in facilitating single-sex safe
spaces for critical reflection on men’s/women’s own experiences of gender norms
and expectations, followed by opportunities for mixed sex dialogue and reflection.
They can also engage men and boys in addressing harmful culture norms and
promoting gender equality, accessing health services and policy/program
development. Fully participation and involvement of men and boys in increasing
public awareness of the value of all children and strengthen self-image, self-esteem
for all children. This can also be a great opportunity to improving the welfare of all
children, especially in regard to health, nutrition, and education including gender
education at family level. By doing so, health institution may help eliminating all
root causes of son preference, which result in female infanticide and prenatal sexselection.
Self-assessment 12.7
1. Outline at least 3 measures to be taken by our country as a primary
responsibility for preventing and responding to gender-based violence?
2. The strategies to engage men and boys in addressing harmful culture
norms and promoting Gender equality include: (Select all that apply)
a. Involving men and boys in policy/program development
b. Mainstreaming men engage philosophy into existing programs
c. Fully participation and involvement of men and boys in increasing public
awareness of the value of all childrend. No educational the welfare of all children
12.8. National guidelines for GBV preventionLearning activity 12.8
Carefully observe the above images and attempt the following questions:
a. What do you see in the above images?b. Attempt to relate image A and image B
12.8.1 Introduction
Considering that GBV affects disproportionately women and causes harm not only
to the individuals experiencing violence, but also to their families, communities,
and the socio-economic wellbeing of the national as a whole, the government
of Rwanda has taken significant steps in addressing including the enactment of
laws and policies against GBV. With zero tolerance to any form of GBV, GBV is
criminalized in Rwanda since 2008 and is currently under Law No 68/2018 of
30/08/2018, which defines four types of GBV: bodily (physical), economic, sexual
and psychological.
Current national policy against GBV, introduce in 2011 and seeks to progressively
eliminate GBV through the development of a preventive, protective, supportive
and transformative environment. This policy acknowledges GBV as a cross-cutting
issue, thus a multi-sectoral approach is required to tackle it with the Ministry of
Gender and Family Promotion (MIGEPROF) holding primary responsibility for
policy implementation, dissemination, and coordination.
To address GBV, a strong partnership combining different ministries and other
government as well as private institutions, academic instructions, civil society
organisations, among others was established with each one having a key role to play.
For example the ministry of health is responsible of ensuring that the appropriate
policies and programmes are in place so that victims of GBV are able to access
appropriate services, ensuring an integrated human rights-based approach into
reproductive health services and scaling up ISANGE one stop centers; MIGEPROF
in collaboration with the Ministry of Local Government are responsible for facilitating
and coordinating gender mainstreaming initiatives at the district and sector levels;
etc.
Strategic areas addressed under this policy include: prevention strategies (i.e.
foster a prevention focused environment where GBV is not tolerated in society
and reduce vulnerability of most at risk groups to GBV); response strategies (i.e.
provide comprehensive services to victims of GBV and improve accountability
and eliminate impunity for GBV); and building coordination, monitoring systems
and expand the evidence available on GBV (i.e. build coordination and monitoring
systems and expand evidence available on GBV in Rwanda).
12.8.2. Implementation
Areas various actors intervene in include but not limited to:
a. Assessment, analysis and strategic planning related to the GBV – they
participate in identification of champions to catalyze processes of GBV
prevention, mitigation and effective immediate response across all clusters
and or sectors of humanitarian action. Make available any existing data on
affected populations, any risks of exposure to GBV for inclusion in response
strategies and to inform initial assessments.
b. Resources mobilization – they work with donors and express the importance
of providing resources for life-saving GBV interventions and for targeted
prevention and mitigation interventions programmes.
c. Coordination with others humanitarian sectors – to promote the guidelines
and related tools in inter-sectoral emergency preparedness meetings to
ensure all decision makers are aware of and have access to GBV prevention
guidance relevant to their clusters/sectors and geographic areas.
d. Monitoring and evaluation – identify at least one relevant indicator from
each area that require regular monitoring reports on actions and results taken
to prevent and mitigate GBV. They may include GBV as a standing agenda
item in government reporting meetings and integrate indicators from the
guidelines in assessments and evaluations while engaging the community
and partner organizations.
e. Involve relevant community members - this enables the community to learn
about how the program will operate and offer information on how the program
may positively and/or negatively impact community norms and existing gender
roles and inequalities in preventing GBV. Engage all members of affected
communities; this includes the leadership and meaningful participation of
women and girls alongside men and boys in all awareness.
f. Education, teaching and learning level – Some of the contemporary issues
that should be taught in the social studies programmes include law-related
education, family life education and peace education. This can enable the
existing social studies curriculum to equip students to have awareness of and
development of attitudes and values for combating gender-based violence.
Law-related education should aim at developing an understanding of the
basic legal concepts such as justice, authority, freedom, privacy, equality,
honesty and fairness.
g. Involvement of different sectors: Utilizing a multi-sectoral approach to
combating GBV is beneficial for establishing a comprehensive strategy i.e.
community anti-GBV committees, school-based anti-GBV clubs, community
policing, etc. However, many entities have reported a need for greater
effectiveness of local mechanisms that address GBV such as “Umugoroba
w’Ababyeyi” and “Inshuti z’Umuryango”, largely due to a need for capacity
building and adequate resources to implement their actions.
h. Communications and Information Sharing – they may appoint focal points
within relevant government bodies to drive and monitor awareness of how
the guidelines can be used to strengthen GBV prevention, mitigation andresponse throughout humanitarian action.
Self-assessment 12.8
1. Describe the national guiding elements for gender based violence
prevention?
2. Explain why it is important to involve relevant community members as a
guideline to prevent GBV?
3. List the 3 elements of the implementation guideline action for GBVprevention
12.9 Professional behavior in managing GBV casesLearning activity 12.9
Carefully observe the above images and attempt the following questions:
a. Describe what you see in image A, B and C
b. With reference to the above images, what do you think GBV interventionsinclude?
The health professional must always keep in mind that the safety and security of
the affected person is of primary importance. Four guiding principal for managing
the GBV cases include but not limited to (1) Right to dignity and self-determination,
(2) Right to confidentiality, (3) Non-discrimination, and (4) Right to safety.
The wishes, rights and dignity of GBV survivors must be respected at all times. All
information of the affected person and her/his family must be kept confidential and
will only be shared with those who need to know, with the explicit consent of the
survivor. Those with whom the information might be shared include Police, Medical
hospital staff, Officers of agencies with a protection mandate (e.g. UNHCR or
UNICEF) or otherwise involved in addressing needs of victims, among others. Along
with support and management of the cases, first line support requires that health
professionals are patient, do not pressure women to talk about their experiences,
and ensure that women are given information and access to resources.
Goals and guidelines elements for managing GBV cases with providingcentered
care Establish a relationship with the survivor, Promote the survivor’s
emotional and physical safety, Build trust, Helps the survivor restore some control
over her life. Be non-judgmental, supportive, and validating, provide practical care
and support that responds to her concerns, but does not intrude.
During history taking and examination: Informed consent is one of the most
important elements to obtain from a patient before beginning the examination and
documentation. Health professionals first need to obtain informed consent from the
patient on all aspects of the consultation. This means explaining all aspects of the
consultation to the patient, so that she understands all her options and is able to
make informed decisions about further management.
Ask about her history of violence, listen carefully, but do not pressure her to talk
(care should be taken when discussing sensitive topics while interpreters are
involved). Help her access information about resources, including legal and other
services that she might think helpful. Assist her to increase safety for herself and
her children, where needed. Ensure the consultation is conducted in private and
informing the limits of confidentiality.
In cases of sexual violence, the following information should be added: the
time since assault and type of assault, the risk of pregnancy, the risk of HIV and
other sexually transmitted infections, the woman’s/girl mental health status.
when interviewing the patient about GBV, health professionals should: ask
her to tell in her own words what happened, avoid unnecessary interruptions
and ask questions for clarification only after she has completed her account , be
thorough, bearing in mind that some patients may intentionally avoid particularly
embarrassing ,details of the assault, such as details of oral sexual contact or anal
penetration, use open-ended questions and avoid questions starting with “why”,
which tends to imply blame. Address patient questions and concerns in a nonjudgmental,
empathic manner, for instance, through using a very calm tone of
voice, maintaining eye contact as culturally appropriate and avoiding expressing
shock or disbelief. After taking the history, health professionals should only conduct
a complete physical examination (head-to-toe; for sexual violence also including
the patient’s genitalia) if appropriate.
When undertaking medical examination and providing medical or nursing care:
Following disclosure of GBV, health professionals should undertake a medical
examination, if appropriate, and provide medical or nursing care. Throughout the
entire process of medical examination and care, health providers need to take into
account that survivors of sexual violence are often in a heightened state of awareness
and very emotional after an assault. Throughout the physical examination inform
the patient what you plan do next and ask permission. Always let her know when
and where touching will occur; show and explain the instruments and collection
materials.
Documenting GBV cases: Health providers have a professional obligation to
record the details of any consultation It is not only a professional obligation to
record details, but is also important for medical records, since medical records can
be used in court as evidence. Documenting the health consequences may help
the court with its decision-making as well as provide information about past and
present violence. Recording injuries, documentation of violence protect the identity
and safety of a survivor. Do not write down, take pictures or verbally share any
personal/identifying information about a survivor or their experience, including with
your supervisor. Put phones and computers away to avoid concern that a survivor’s
voice is being recorded.The Do’s, Don’ts of professional management of GBV cases

Don’t assume that confidentiality is a given; take steps to ensure confidentiality.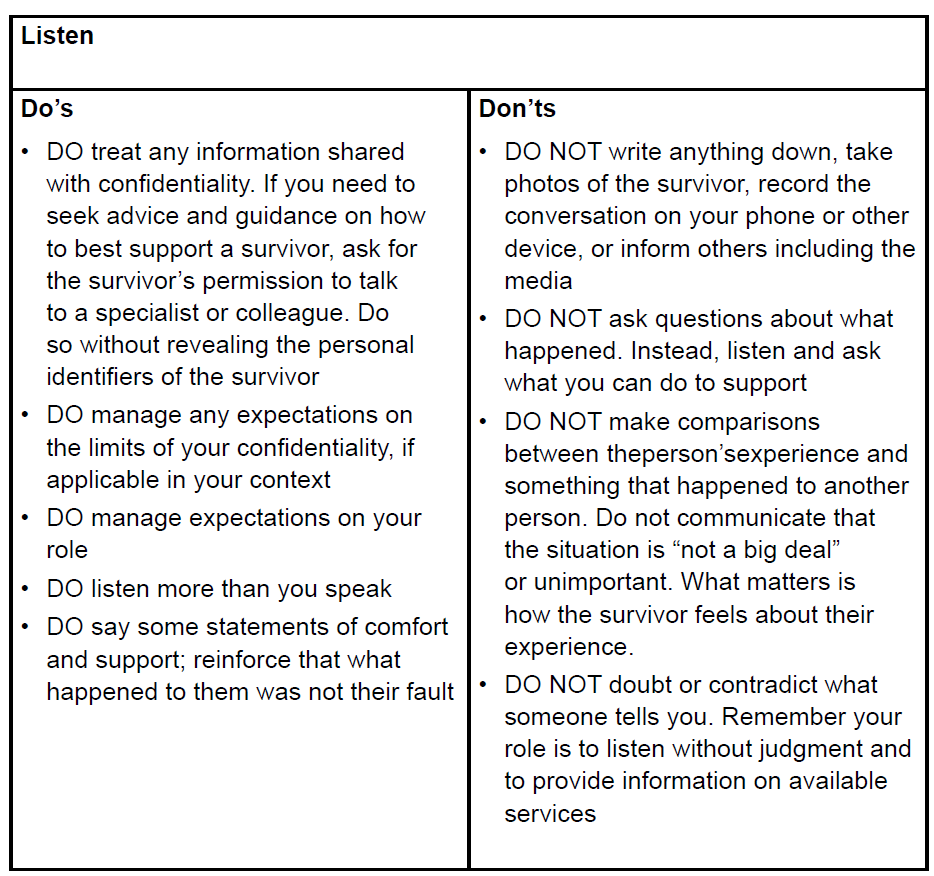
Don’t let staff give out personal phone numbers or become a case manager. Don’t
examine a person without her consent may result in criminal prosecution of healthcare professionals.
Self-assessment 12.9
1. What is the goal of survivor centered case management? (Choose one
answer):
a. Establish a relationship with the survivor
b. Promote the survivor’s emotional and physical safety
c. Build trust
d. Helps the survivor restore some control over her life
2. What are the 4 guiding principles of GBV case management? (choose 4
answers)
a. Right to be happy
b. Right to dignity and self-determination
c. Mandatory reporting
d. Right to confidentiality
e. Non-discrimination
f. f. Legal information
g. Right to safety3. What is the Non-discrimination mean?
12.10 The consequences of GBVLearning activity 12.10
Carefully observe the above images and describe and give sense what you
see.
GBV has significant and far-reaching consequences that affect not only GBV
survivors but also their families, communities, and society. For instance at societal
level, GBV can lead to social stigma, rejection, break-up of families, homelessness,
dispossession, and destitution. GBV survivors are at high risk of severe and longlasting
health problems and even loss of life. There are different categorizations of
GBV repercussions, with each variety of GBV having its own, even though there
are some overlaps.
a. Physical consequences – Physically, victims may suffer various injuries,
including bleeding, wounds, burns, fractures, permanent disfigurement,
physical disability, stunted physical growth (for children), fistula or even death.
b. Sexual and reproductive health consequences – GBV has grave sexual
and reproductive health consequences. It can deter survivors from seeking
reproductive health and family planning services. There is a strong between
GBV and HIV among persons living with HIV/AIDS. Consequences of GBV
under this category including:
• Unplanned pregnancies and children
• Induced, unsanitary, and dangerous abortions
• Sexually transmitted infections, including HIV
• Barrenness due to disease and injury
• Sexual dysfunction
• Injury to reproductive organs, leading to lifelong malfunctions
• Early pregnancy
• Destabilization of the menstrual cycle
• Deformed genitalia and related health complications
• Loss of sexual desire and painful sexual intercourse
• Infertility
c. Emotional/psychological consequences – these include but not limited
to anxiety, depression, anger or hostility, low self-esteem, suicide (attempts
and actual suicide), self-harm, post-traumatic stress disorder (PTSD), fear,
shame, Obsessive-compulsive disorder, dissociation and loss of memory,
inability to trust others, especially in cases of intimate partner violence, sleep
disturbance, emotional detachment, etc.
d. Social and cultural consequences – they include among others:
• Alienation and rejection
• Loss of respect and dignity among peers, family, and community
• Aggressive behaviours that may be accompanied by retaliatory attitudes
• Break of social networks of support
• Rejection, stigmatization, and neglect of children resulting from rape or incest
• Early marriage in a bid to reclaim family’s honour with associated loss of
children’s right to education as a result of early marriage
• Stigma and discrimination for life
• Repeat violation due to perceived vulnerability
• Breakdown in heterosexual relationships, including marriage
• Identity crisis for children born out of sexual violation
• Exclusion of victims from important communal events such as burial rites
• Poor performance and increased dropping out of school
• Slow rate of development due to withdrawal syndrome and limited interaction
with peers
e. Economic consequences – GBV costs survivors, their families, and society
at large both directly (such as treatment, visits to the hospital doctor and other
health services) and indirectly such as lost productivity, absenteeism, reduced
employability (as a result of reduced education/incapacity to focus at work),
disability, decreased quality of life and premature death. Other economic
repercussions include among others; reduced investments as savings are
diverted to medical treatment, costs incurred by the criminal justice system
in apprehending and prosecuting offenders and costs associated with casemanagement, counseling and psycho-social support, etc.
Self-assessment 12.10
1. List at least 4 sexual and health reproductive consequences of GBV
2. Contrast direct and indirect economic consequences of GVB
3. True or false? GBV consequences are always in line with the type or formof GBV
End unit 12 assessment
1. Contrast gender and sex
2. How gender identity differ from gender orientation
3. Explain how legal factor influence GBV
4. Among other consequences of GBV, there are economic repercussions.
Explain how these affect the survivors and their families and the society
at large.
5. True or false?
a. Domestic violence is common occurrence and might be the most under
reported form of GBV
b. In general, gender differences are permanent and universal
c. Gender refers to the natural differences that separate men and women
d. GBV survivors are at high risk of severe and long-lasting health problems
and even loss of life
e. Men access healthcare services more frequently than do women and
respond positively to received services
a. Health promotion and disease prevention messages target frequently
women
6. The following are social and cultural repercussions of GBV except:
a. Rejection, stigmatization, and neglect of children resulting from rape or
incest
b. Post-Traumatic Stress Disorder (PTSD)
c. Breakdown in heterosexual relationships, including marriage
d. Aggressive behaviours that may be accompanied by retaliatory attitudes
7. Give 3 examples of GBV forms that are likely to be perpetrated by
Influential community members
8. Why is human trafficking classified as physical GBV?
9. What is the country responsibility in GBV prevention?10. List four professional guiding principles for GBV case management
REFERENCES
A Jones, S. (2012). First Aid, Survival and CPR. F.A. Davis Company.
Aid, F., & Version, B. (2021). Australia Wide First Aid eBook (Version 6.1). Australia
Wide First Aid.
Amercan Heart Association. (2016). Basic life support: Provider Manual (First
Edition). American Heart Association.
Baranoski, S., & Ayello, E. A. (2012). Wound Care Essentials: Practice Principles
(3rd ed.). Wolters Kluwer health | Lippincott Williams & Wilkins.
BrainKart.com, 2018 guidelines and types of bandages retrieved online at:https://
www.brainkart.com/article/Uses Guidelines-and-Types-of-bandages-_2308/ on
09th Sept 2021
Cowart, S. L. and Stachura, M. A. X. E. (2000) ‘Laboratory’, in Clinical Methods:
The History, Physical, and Laboratory Examinations. 3rd edition, pp. 653–657.
Cunningham, J. et al. (2019) ‘A review of the WHO malaria rapid diagnostic test
product testing programme (2008-2018): Performance, procurement and policy’,
Malaria Journal. BioMed Central, 18(1). doi: 10.1186/s12936-019-3028-z.
Directorate of Forests Government of West Bengal. (2016). Manual for First Aid.
1–30.
Disque, K. (2021). CPR, AED & First Aid: Provider Handbook. 2020-2025 Guidelines
and Standards Satori Continuum Publishing.
Emmett, M. (2014) ‘Albuminuria’, Cleveland Clinic Journal of Medicine, 81(6), p.
345. doi: 10.3949/ccjm.81c.06006.
Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? Arch Dis
Child. 2016;101(6):569–74.
Indian Red Cross society. (2016). Indian first aid manual 2016. 7th editio, 1–346.
https://www.indianredcross.org/publications/FA-manual.pdf
Lao National First Aid Curriculum Development Technical Working Group. (2014).
Trainer’ s Manual First Aid for National Village Health Volunteers.
Lewis, S.L, Dirksen, T.R, Heitkemper, M. McLean and Bucher, L. (2014). Medical
Surgical Nursing: Assessment and Management of Clinical Problems. 9th Edition
Lojpur, M. (n.d.). First Aid to the Injured.
Loren Nell Melton Stein & Connie J. Hollen (2021) Concept-Based Clinical Nursing
Skills: Fundamental to Advanced. Elsevier Inc.
New Zeland Red Cross. (2021). Essential First Aid. ttps://doi.org/10.1136/
bmj.2.4318.456-a
Piazza, G. M. (2014). First Aid Manual: The Step by Step Guide for Everyone. (5th
ed.). DK Publishing.
Pickering D, Marsden J. How to measure blood glucose Understanding and caring
for a Schiotz tonometer. Community Eye Heal. 2014;27(87):56–7.
Razzak RA, Alshaiji AF, Qareeballa AA, Mohamed MW, Bagust J, Docherty S. Highnormal
blood glucose levels may be associated with decreased spatial perception
in young healthy adults. PLoS One. 2018;13(6):1–12.
Semanoff A. A Case Study - Diabetes Mellitus. Am J Nurs. 2018;37(9):1–4.
Slachta, P. A. (2012). Wound care made incredibly visual! (2nd ed.). Lippincott
Williams & Wilkins.
Steggall, M. J. (2007) ‘Urine samples and urinalysis.’, Nursing standard (Royal
College of Nursing (Great Britain) : 1987), 22(14–16), pp. 42–45. doi: 10.7748/
ns2007.12.22.14.42.c6303.
Stein, L. N. M., & Hollen, C. J. (2021). Concept-Based Clinical Nursing Skills:
Fundamental to Advanced (First). Elsevier Inc.
Visser, L. S., & Montejano, A. S. (2018). Guide for Triage and Emergency Nurses:
Chief Complaints with High Risk Presentations (1st ed., Vol. 148). Springer
Publishing Company, LLC.
Wound, Ostomy and Continence Society (2016). Core Curriculum: Wound
Management. Wolters Kluwer health | Lippincott Williams & Wilkins.
Yancey CC, O’Rourke MC. Emergency Department Triage. [Updated 2021 Jul 30].
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK557583/?report=classic
Erica Roth, C. (2021). Everything you need to know about Low blood pressure.
Healthline
Preston, W., & Kelly, C. (2017). Respiratory Nursing at a Glance. John Wiley and
Sons, Ltd.
Nettina, S. M. (2019). Lippincott manual of nursing practice (11th ed.). Wolters
Kluwer Health | Lippincott Williams & Wilkins.
Harding, M. M., Kwong, J., Roberts, D., Hagler, D., & Reinisch, C. (2020). Lewis’ s
Medical-Surgical Nursing Assessment and Management of Clinical Problems (11th
ed.). Elsevier, Inc.
Zealand N, Defence C, Management E. General Rescue Manual New Zealand Civil
Defence Emergency Management Table of Contents. 2020.
Spray A, Merry W, Sweeting G, Colwell D. Ground Search & Rescue (GSAR)
Participant Manual. Justice Inst. Br. Columbia. 2018.
Kentucky Emergency Management. SAR Field Search Methods: Search Techniques
Used by Trained Teams in the Field. 2019;8. Available from: https://kyem.ky.gov/
Who We Are/Documents/SAR Field Search Methods.pdf
Search S, Rescuers CL, Resources OC, Aid F, Composition T. Chapter 1: Search
and Rescue. 2021;1–16. Available from: http://www.sdmassam.nic.in/download/
searchandrescuemanual.pdf
Wong J, Robinson C. Urban search and rescue technology needs: identification of
needs. Fed Emerg Manag Agency Natl Inst Justice. 2016;73.
A Jones, S. (2012). First Aid, Survival and CPR. F.A. Davis Company.[1]
Aid, F., & Version, B. (2021). Australia Wide First Aid eBook (Version 6.1). Australia
Wide First Aid.
Directorate of Forests Government of West Bengal. (2016). Manual for First Aid.
1–30. Disque, K. (2021).
Lao National First Aid Curriculum Development Technical Working Group. (2014).
Trainer’s Manual First Aid for National Village Health Volunteers.
Erica Roth, C. (2021). Everything you need to know about Low blood pressure.
Healthline
Preston, W., & Kelly, C. (2017). Respiratory Nursing at a Glance. John Wiley and
Sons, Ltd.
Nettina, S. M. (2019). Lippincott manual of nursing practice (11th ed.). Wolters
Kluwer Health | Lippincott Williams & Wilkins.
Harding, M. M., Kwong, J., Roberts, D., Hagler, D., & Reinisch, C. (2020). Lewis’ s
Medical-Surgical Nursing Assessment and Management of Clinical Problems (11th
ed.). Elsevier, Inc.
Goolsby, M. J., & Grubbs, L. (2018). Advanced assessment interpreting findings
and formulating differential diagnoses. FA Davis
Forbes, H., & Watt, E. (2015). Jarvis’s physical examination and health assessment.
Elsevier Health Sciences.
Berman, A., Snyder, S. J., Kozier, B., Erb, G., Levett-Jones, T., Dwyer, T., & Stanley,
D. (2010). Kozier and Erb’s fundamentals of nursing (Vol. 1). Pearson Australia.
Hogan-Quigley, B., & Palm, M. L. (2021). Bates’ nursing guide to physical
examination and history taking. Lippincott Williams & Wilkins.
Wiliams, L. (2011). Wilkins. Health assessment made incredibly visual!
Honjo, K. (2004). Social epidemiology: Definition, history, and research examples.
Environmental health and preventive medicine, 9(5), 193-199.
Broom, D. H. (1984). The social distribution of illness: is Australia more equal?.
Social science & medicine, 18(11), 909-917.
Wikler D. Personal and social responsibility for health. Ethics Int Aff 20021647–55.
[PubMed] [Google Scholar]
Callahan D, Koenig B, Minkler M. Promoting health and preventing disease: ethical
demands and social challenges. In: Callahan D, ed. Promoting healthy behavior.
Washington, DC: Georgetown University Press, 2000153–170.
WHO. (2013). Family as Centre of Health Development Family as Centre of Health
Development. (March), 18–20.
Bauml, J., Frobose, T., Kraemer, S., Rentrop, M., &Pitschel-Walz, F. (2006).
Psychoeducation: A basic psychotherapeutic intervention for patients with
schizophrenia and their families. Schizophrenia Bulletin, 32, 11–19.
Farber, B., Berano, K., &Capobianco, J. (2004). Clients’ perceptions of the process
and consequences of self-disclosure in psychotherapy. Journal of Counseling
Psychology, 51, 340–346.
Guilbeault, L. (2020). What is the therapist’s role in non-directive therapy? Better
Help. Retrieved August 4, 2020 from https://www.betterhelp.com/advice/therapy/
what-is-the-therapists-role-in-nondirective-therapy/
Hill, C., & Knox, S. (2001). Self-disclosure. Psychotherapy: Theory, Research,
Practice, Training, 38, 413–417.
Horvath, A. (2001). The alliance. Psychotherapy: Theory, Research, Practice,
Training, 38, 365–372.
Lambert, M. J. (1991). Introduction to psychotherapy research. Psychotherapy
Research: An International Review of Programmatic Studies. Washington, DC:
American Psychological Association.
Meyers, L. (2014). Connecting with clients. Counseling Today, 18. Retrieved August
2020 from www.ct.counseling.org/2014/08/connecting-with-clients/#
Prochaska, J., & Norcross, J. (2001). Stages of change. Psychotherapy: Theory,
Research, Practice, Training, 38, 443–448.
Rennie, D. (1994). Clients’ accounts of resistance in counseling: A qualitative
analysis. Canadian Journal of Counseling, 28, 43–57.
Rogers, C. (1957). The necessary and sufficient conditions of therapeutic personality
change. Journal of Consulting Psychology, 21, 95–103.
Rogers, C. (1961). On becoming a person: A therapist’s view of psychotherapy.
New York, NY: Houghton Mifflin.
Schueller, S. M. (2009). Promoting wellness: Integrating community and positive
psychology. Journal of CommunityPsychology, 37, 922–937.
Sexton, T. L. (1996). The relevance of counseling outcome research: Current trends
and practical implications. Journal of Counseling and Development, 74, 590–600.
Detels, R., Gulliford, M., Karim, Q. A., & Tan, C. C. (2015). Oxford Textbook of
Global Public Health. In Global Public Health: A New Era (6th ed.). Oxford University
Press. https://doi.org/10.1093/acprof:oso/9780199236626.001.0001
GACA. (2018). Providing a safe and protective environment for the child: Additional
Training Module & Activity Facilitation Guide On Adolescence, Sexual And
Reproductive Health, Gender And Sexual And Gender Based Violence (SGBV).
UNICEF Ghana and Department of Community Development of the Ministry of
Local Government and Rural Development.
Inter-Agency Standing Committee. (2015). How to Support Survivors of Violence
when a GBV Actor is not available in your Area: A Step-By-Step Pocket Guide for
Humanitarian PractitionerS. September 2015, 2–3. https://gbvguidelines.org/wp/
wp-content/uploads/2018/03/GBV_Background_Note021718.pdf
Jacobsen, K. H. (2019). Introduction to global health (3rd ed.). Jones & Bartlett
Learning, LLC.
MIGEPROF. (2011). Gender Based Violence Training Module. Republic of Rwanda
MIGEPROF. (2011). National Policy against Gender-Based Violence.July. Republic
of Rwanda http://www.migeprof.gov.rw/fileadmin/_migrated/content_uploads/
GBV_Policy-2_1_.pdf
Ostlin, P., Eckermann, E., Mishra, U. S., Nkowane, M., &Wallstam, E. (2007).
Gender and health promotion: a multisectoral policy approach. Health Promotion
International, 21, 25–35. https://doi.org/10.1093/heapro/dal048
Skolnik, R. (2016). Global Health 101 (3rd ed.). Jones & Bartlett Learning, LLC.
UNHCR Global Protection Cluster Working Group.(2019). Handbook for the
Protection of Internally Displaced Persons Goals.UNHCR. https://doi.org/10.12968/
bjon.2019.28.10.607
UNHCR. (2016). SGBV Prevention and Response - Training Package. UNHCR.
http://siteresources.worldbank.org/INTEAPREGTOPENVIRONMENT/Resources/
Water_Pollution_Emergency_Final_EN.pdf
United Nations Country Team in Kenya. (2019). Gender Based Violence Training
Ressource Pack: A Standardized Bearers, Stakeholders, Training Tool for Duty and
Rights Holders. UN Women Kenya Country Office.
United Nations Country Team in Kenya. (2019). Gender Based Violence Training
Ressource Pack: A Standardized Bearers, Stakeholders, Training Tool for Duty and
Rights Holders. UN Women Kenya Country Office.
United Nations Country Team in Kenya. (2019). Gender Based Violence Training
Ressource Pack: A Standardized Bearers, Stakeholders, Training Tool for Duty and
Rights Holders. UN Women Kenya Country Office.
WHO Regional Office for Europe. (2020). Gender and non-communicable diseasesin Europe: Analysis of STEPS data. World Health Organization.
