UNIT 8 NURSING ASSESSMENT OF DIGESTIVE SYSTEM
Key unit competence
Take appropriate action based on findings of nursing assessment of digestive
systemIntroductory activity 8
What do you think is illustrated on image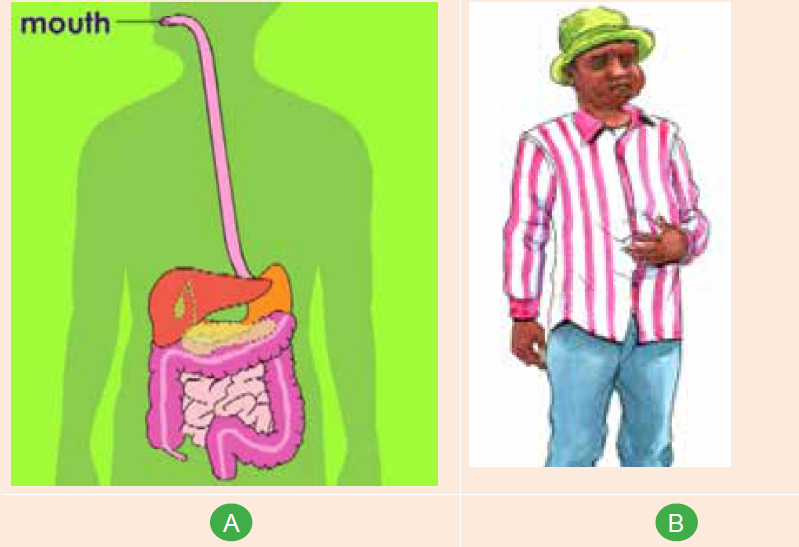
a, b and c ?
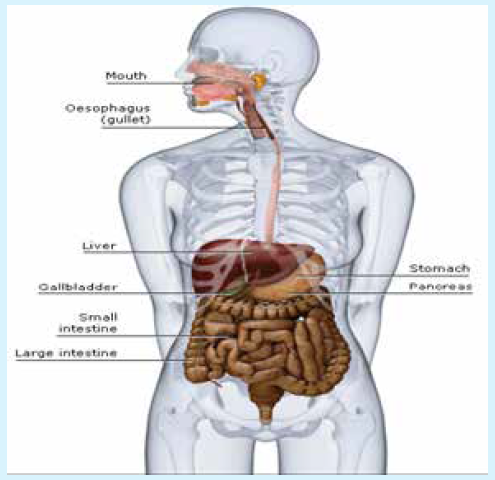
The functions of the gastrointestinal (GI) tract and its accessory organs are essential
for life. The process of digestion supplies nutrients to each and every cell in our
body, therefore, if there is a disruption in any of these mechanisms, the whole body
suffers.
8.1. Overview of the digestive system and terminologiesused
Learning activity 8.1.
Mr. Z. underwent a surgical intervention called appendectomy.
1. Locate the appendix on the anatomic model2. Explain the meaning of the word appendicectomy.
8.1.1. Overview of digestive system
The Digestive Tract Also called the gastrointestinal (GI) tract or alimentary canal
Is a muscular tube which Extends from the mouth to the anus. It Passes through
the pharynx, esophagus, stomach, and small and large intestines. It is composed
of the upper GI tract (oral cavity, esophagus, and duodenum), lower GI tract (small
intestine, cecum, colon, rectum, and anus), and associated glandular organs
(gallbladder, pancreas, and liver). The digestive system is responsible for ingestion,
mechanical processing, digestion, secretion, absorption, immunity and waste
excretion.The picture 8.1 illustrates the alimentary canal and the duration that each step take
8.1.2. Some of medical terminologies related to digestive system
A. PREFIXES
This section contains prefixes that are used for the medical terminology. Prefixesare used at the beginning of a word to modify or vary the meaning of the word.
B. SUFFIXES
Suffixes are placed at the end of a word root or word part to modify or vary themeaning. Suffixes can indicate a condition, disease or a procedure.
C. WORD ROOT AND COMBINING VOWEL FOR THE GASTROINTESTINAL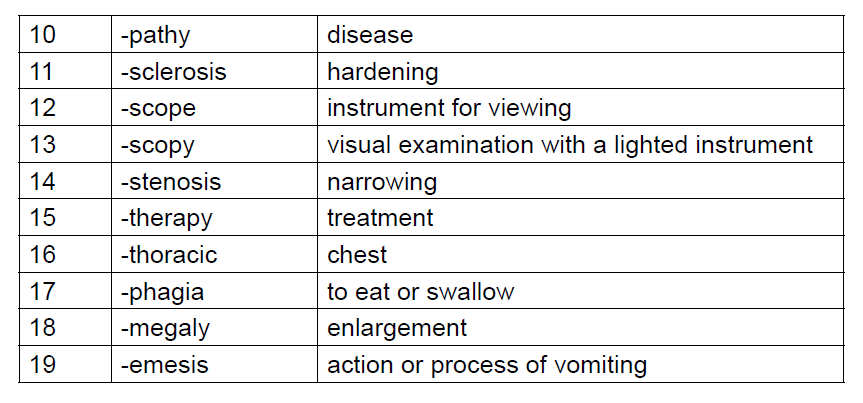
SYSTEM
This is a list of some word roots with their combining vowel used for the gastrointestinalsystem.
Self-assessment 8.1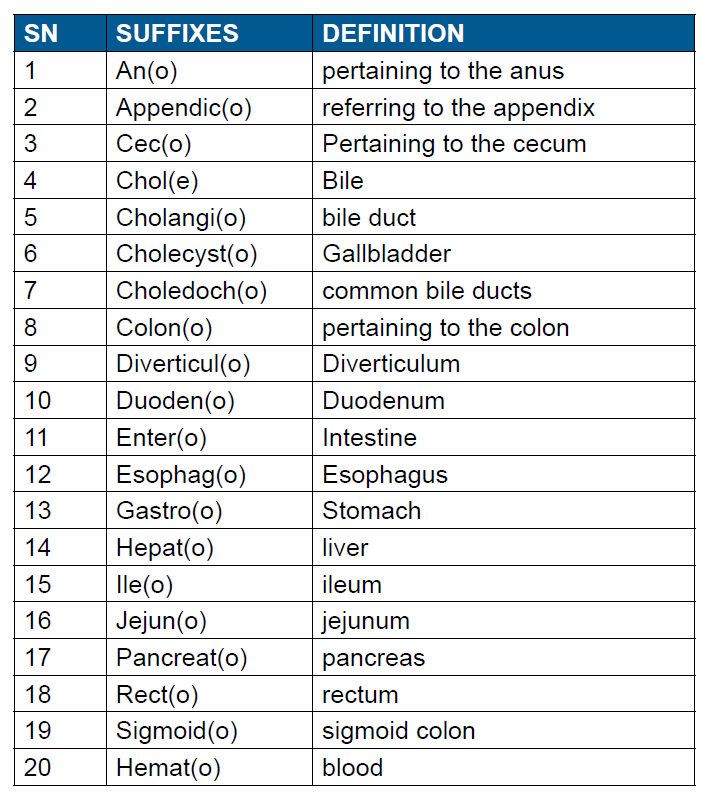
1. Show the main three components of the digestive system on the followingimage
2. Relate the terminologies with their meaning
8.2. History taking on digestive system
Learning activity 8.2.Observe careful the image below and respond to the following question
1. Predict what is happening in Image A
2. Outline the commonly reported symptoms of the gastrointestinal tract
The patient history is key to evaluating gastrointestinal (GI) tract disorders and should
include the problem onset, the setting in which it developed, and its presentation.
Patient warning signs and alarm symptoms should be identified quickly and when
referral is needed for further evaluation and intervention, it should be obtained in a
prompt manner.
The gastro intestinal tract starts from the mouth to the anus and any part of it can
be affected by a pathology. The purpose of history taking is to obtain a clear and
detailed picture of the patient’s complaints. Therefore, it is used to narrow the focus
of the diagnostic and therapeutic plan for the patient.
8.2.1. History of presenting complaint
The Healthcare provider who is going to take the patient history will wash the hands,
introduce him/her(self) to the client, have the client’s names and date of birth, have
the consent and ensures that the client is in a comfortable seating.
Every sick person presents at the consultation room for a certain reason; that
reason for looking care is the presenting complaint (s).
In order to elicit the client’s presenting complaint, it is recommended to allow the
client time to answer, try not to interrupt or direct the conversation, and help the
client expand on their PC (Presenting complaint).
There are a many GI (Gastro intestinal) symptoms and some can be specific to
the upper GI tract, some to the lower GI tract and others can be specific to the
hepatobiliary system.
a. Common symptoms of the gastro intestinal tractA variety of symptoms can arise from Gastro intestinal tract (GIT) dysfunction.

In addition to collecting information on current complaints, a thorough patient history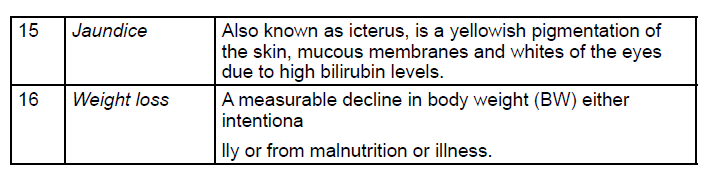
should gather information concerning medical history, social and family history,
and current medications. The healthcare professional should ask guided question
focused on determining the symptom’s onset, location, severity, and duration,
setting in which symptoms developed, aggravating and alleviating factors, and
associated symptoms of the complaint.
The symptom onset often provides important information that helps formulate a
differential diagnosis. For example, biliary colic or pain, such as that encountered
with symptomatic gallstone disease, typically evolves over minutes and is present
for hours, but pain caused by pancreatitis evolves over hours and lasts for days.
Also, the setting is always relevant as it provides clues to the possible origin of
the disorder. For example, in the patient with complaints of reflux or ulcer disease,
obtaining information as to whether the pain is alleviated or worsened by food or
diminished when administered acid-suppressive therapy can help guide diagnostic
and therapeutic interventions. For instance, ingesting a meal often relieves the pain
of duodenal ulcer, but worsens pain due to a gastric ulcer.
During History taking, the healthcare professional should ask questions that
address potential etiologic possibilities, including motility disorders, structural
diseases, malignancies, infections, psychosocial factors, dietary factors, and travelassociated
diseases.
Furthermore, a good cardiopulmonary history is also extremely relevant and should
be performed during the overall history. Questions concerning medical and family
history detailing illnesses, surgical interventions, injuries, foreign travel, living
conditions, and habits are valuable.
Always end by discussing the patient’s ideas, concerns & expectations(ICE). The
following questions may be asked:
1. Do you have an idea about what could be going on?
2. Is there anything that is worrying/concerning you at the moment?
3. Is there anything you were hoping for from this consultation?4. Do you have any further questions today?
Self-assessment 8.1
Watch a video of history taking and do a role play in pairs of history taking ondigestive system
8.3. Physical examination of digestive system
Learning activity 8.3.
The image illustrates the four quadrants of the abdomen that guide duringphysical assessment
1. List the materials that might be needed for abdominal physical assessment
2. Indicate the techniques which can be used for abdominal physicalassessment.
A comprehensive evaluation of the patient should be performed with notable
attention to physical appearances and vital signs as they may suggest signs of
systemic conditions eliciting gastro intestinal (GI) symptoms.
Communication during physical examination must be respectful and performed
in a culturally-sensitive manner. Privacy should be ensured, and the healthcare
professional needs to be aware that postures, body language, and tone of voice are
transmitting a message.
When performing a focused assessment, you will use at least one or all of the
following four basic techniques during your physical exam: inspection, auscultation,
percussion, and palpation. These techniques should be used in an organized
manner from least disturbing or invasive to most invasive to the patient.
Inspection is first, as it is non-invasive. Auscultation is performed following
inspection; the abdomen should be auscultated before percussion or palpation to
prevent production of false bowel sounds. For accurate assessment of the abdomen,
patient relaxation is essential. The patient should be comfortable and should have
an empty bladder. The environment should include a comfortable temperature, with
good light.8.3.1. Inspection of the abdomen
For the purpose of assessment, the abdomen can be divided into four quadrants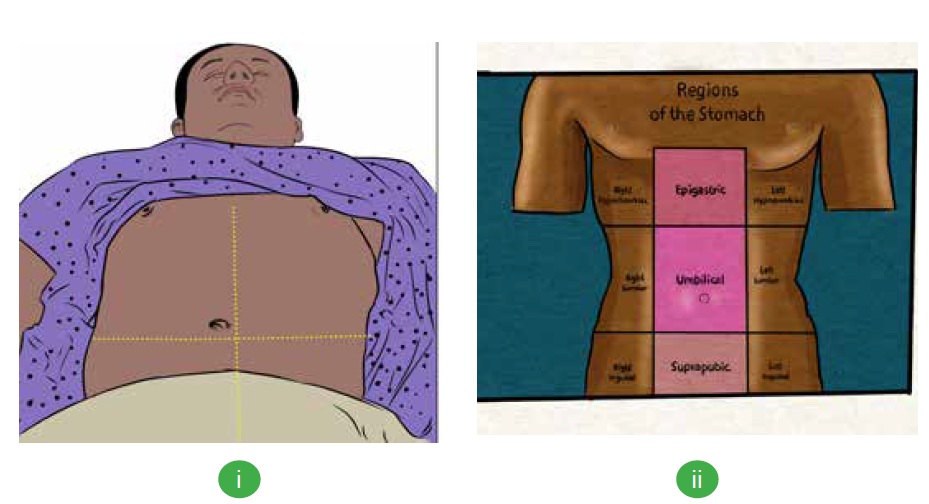
(see image i above) or nine quadrants for descriptive purposes (see image ii above).
Inspection of the abdomen may reveal scars, hernias, masses, ascites or peristalsis.
The four quadrants include the right upper quadrant, left upper quadrant, right
lower quadrant, and left lower quadrant.
When assessing the abdomen, it is important to make the patient as comfortable as
possible. Following are the steps for inspection of the digestive system:
1. Position the patient in a lying (supine) position with their head and knees
supported by a pillow. Alternative positions are lying with knees bent or
a side-lying position. Always make sure the client is in as comfortable
position as possible
2. Be sure and remove the clothing or lift the gown.
3. Check the skin for any rashes, scars, lesions, masses or bulges, surgical
incision….
4. Inspect the contour of the abdomen, is the abdomen flat, rounded, scaphoid,or protuberant?
5. Inspect the abdomen for symmetry. The abdomen should be symmetrical
bilaterally. Inspect the umbilicus.
6. Check for any types of equipment such as G-tube, drains, ….8.3.2. Auscultation of the abdomen
Auscultation of the abdomen should
always be done after inspection and
before percussion and palpation as
they can alter the bowel sounds.
Auscultation should begin in the right
lower quadrant. If bowel sounds are not
heard, in order to determine if bowel
sounds are truly absent, listen for a total
of five minutes. It is suggested that you
listen to bowel sounds for a full minute before determining if they are normal,
hypoactive, or hyperactive. An example of a video demonstrating abdominal
auscultation can be viewed at:
Following are the steps for auscultation of the digestive system:
1. Use the diaphragm of the stethoscope and apply light pressure.
2. Auscultate the abdomen in all four quadrants.
3. Listen for bowel sounds, noting the characteristic and frequency.
4. Listen for bruits or any vascular sounds.8.3.3. Percussion of the abdomen
Percussion of the abdomen is used
to assess for the amount of gas in the
abdomen. Also, it can be used to identify
organs, masses or to elicit tenderness
and sounds that give clues to underlying
problems.
Percussion can help estimate the
size of the liver or spleen. Percussion
of the abdomen allows for detection of
tympany, measurement of visceral
size, and detection of ascites. It is may be difficult to percuss the liver as most
of it is covered by the ribcage. Dullness is heard when percussing the liver
through intercostal space. The spleen’s percussion is easier when it enlarges.
It usually extends forward, downward and to the sides. The abdomen is
percussed in all four quadrants to assess areas of tympany and dullness.
Tympany is usually heard over a gas-filled area while dullness is heard over
solid masses or organs.
Following are the steps for auscultation of the digestive system:
1. Press the distal part of the middle finger of your non-dominant hand firmly
on the body part.
2. Keep the rest of your hand off the body surface.
3. Flex the wrist, but not the forearm, of your dominant hand.
4. Using the middle finger of your dominant hand, tap quickly and directly over
the point where your other middle finger contacts the patient’s skin, keeping
the fingers perpendicular.
5. Listen to the sounds produced. When examining the abdomen, percuss for
general tympany, liver span, and splenic dullness. Tympany should be the
predominant sound when percussing the abdomen while Dullness is usually
heard over solid organs or masses such as the liver, spleen, or a full bladder.
An example of a video demonstrating abdominal percussion can be viewed at:
Percussion is contraindicated in patients with suspected aortic aneurysm,
appendicitis, or those who have received abdominal organ transplants
8.3.4. Palpation of the abdomen
Palpation is another commonly used physical exam technique that requires the
examiner to touch the client with his/her hand(s). Palpation may allow to identify
tenderness, rigidity, masses, and hernias. The client will be always asked if they
have any areas of pain before beginning palpation. The painful areas are palpated
last.
Palpation allows you to assess for texture, tenderness, temperature, moisture,
pulsations, masses, and internal organs. Normally, there should be no tenderness
on either light or deep palpation of the abdomen.
Following are the steps for auscultation of the digestive system:a. To lightly palpate the abdom

Light palpation
1. With the fingers together, place
the hand flat on the abdomen.
2. Lightly palpate the abdomen
using a dipping motion.
3. Raise the hand off the skin
while moving from one place toanother.
2. Palpate all four quadrants.
3. Check for tenderness.
4. Palpate for any superficial organs or masses.
5. Notice if the patient is guarding while palpating.b. To deeply palpate the abdomen:

Deep palpation
1. Use the palmer side of the hand.
2. Palpate all four quadrants.
3. Assess for masses noting the
location, size, and shape.4. Check for tenderness.
c. To palpate the liver:

Liver palpation
1. Stand on the right side of the
client.
2. Place your left hand behind the
client around the 11th or 12th rib.
3. Have the patient relax their back
onto your hand?
4. Press your left hand forward as the client relaxes into it. This pushes the liver
forward and makes it easier to palpate with your right hand.
5. Place your right hand on the right side of the client’s abdomen.
6. Place your fingertips at the lower border of the costal margin.
7. Press gently inward and upward on the abdomen.
8. Ask the patient to take a deep breath so you can feel the borders of the liver
as it moves under your fingers.
9. Ask the patient if they have any tenderness.
While assessing the abdomen, remember that palpation and percussion are
contraindicated in patients that are suspected for having a diagnosis of an
abdominal aortic aneurysm, appendicitis and other conditions. Always check forcontraindications before beginning an abdominal assessment.
Self-assessment 8.3.
Answer whether the statement is true or false
1. During physical examination communication have be respectful and the
procedure is performed in a culturally-sensitive manner.
2. For the purpose of assessment, the abdomen is divided into four
quadrants.
3. Palpation is always done before auscultation for physical assessment of
the digestive system
4. The client is asked if he/she has any areas of pain before beginning
palpation and the painful areas are palpated first to identify any emergency
situation.
5. Tympany sound is heard when percussing the liver.6. Dullness is usually predominant while percussing the abdomen.
8.4. Interpretation of specific findings on digestive
system
Learning activity 8.4.
The image shows some of the problems occurring to the digestive system
1. Describe the symptoms that you think may occur to a client presenting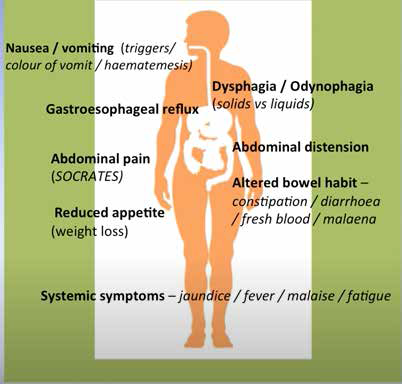
with digestive system disease conditions
8.4.1. Interpretation of some findings from physical assessment
A. Some definitions
• Ascites is an abnormal accumulation of serous fluid in the abdominal cavity
containing large amounts of protein and electrolytes.
• Bulge is a protruding part; an outward curve or swelling.
• Cirrhosis is a chronic disease of the liver characterized by the replacement
of normal tissue with fibrous tissue and the loss of functional liver cells.
• Hernia is the protrusion of an organ or other bodily structure through the
wall that normally contains it.
• Food intolerance is inability to completely digest a type of food, usually due
to an enzyme deficiency
• Referred pain is a pain sensation experienced in one part of the body that
is different to the actual area of pathology.
• Visceral pain is a pain related to the internal organs.
• Esophageal varices are abnormally dilated or swollen vessels in the
esophagus, which can lead to bleeding.
B. Abdominal shape
• A flat abdomen is commonly seen in a person of normal weight. There is
a straight line from the costal margin to the symphysis pubis.
• A rounded abdomen has a convex shape. This usually indicates additional
fat around the abdominal area however a rounded abdomen is normal in
pregnant women and toddlers.
• A scaphoid abdomen has a concave shape. From the side, the abdomen
looks sunken. This shape is usually seen in patients who are extremely
thin.
• A protuberant abdomen is seen in people who are obese or have ascites.
The abdomen is extremely rounded. This shape is seen in women who are
pregnant but is also seen in men with ascites.
C. On inspection
• If a protrusion is noticed around the umbilicus or any incisions, a hernia may
be present.
• Peristalsis is not normally visible but, can be visible with an intestinal
obstruction.
• Pulsations can sometimes be visualized with an abdominal aneurysm.
• Jaundice is the yellow color of skin and mucous membranes due to
accumulation of bile pigments in blood and their deposition in body tissues.
• Cholestasis refers to a decreased rate of bile flow.
Depending on the clinical situation, jaundice and cholestasis may coexist or each
may exist without the other. Although many sources confidently say that jaundice
can be recognized when the serum bilirubin rises to 2 to 2.5 mg/dl, experienced
clinicians often cannot see a yellow skin coloration until the serum bilirubin is at
least 7 to 8 mg/dl.
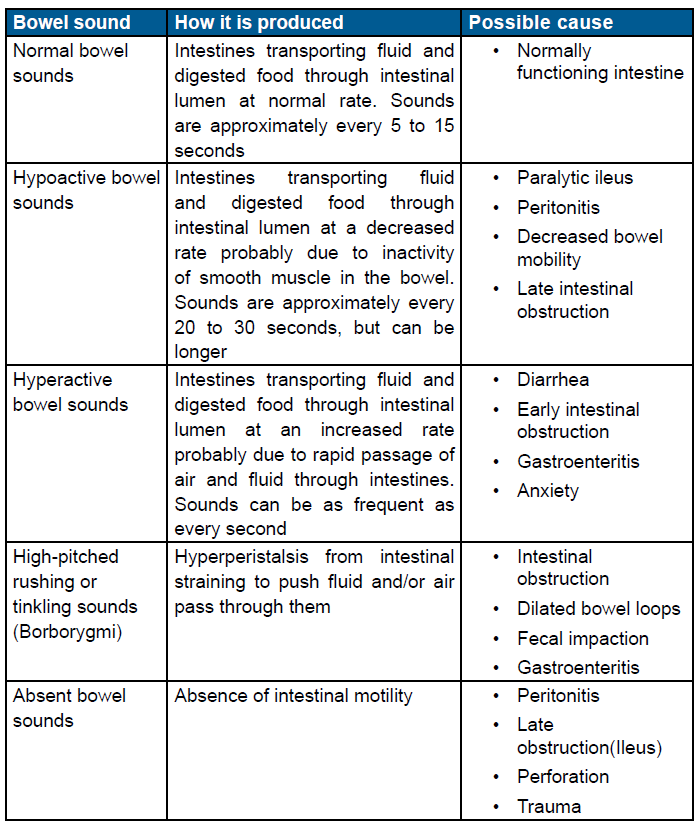
C. On auscultation
The table describes how different bowel sounds are produced and what they mayindicate.

D. Pain scale
The pain is rated on a scale of 10 in order to have an idea of its intensity and
plan the intervention accordingly. The following facies indicate the level atwhich a patient is suffering and the score related to it.

8.4.2. Interpretation of some findings from laboratory findings
There are many common laboratory exams that help in the assessment of client’s
gastrointestinal system and accessory organs. Lab values should be looked
at collectively in the context of a complete abdominal history and examination.
The following table illustrates examples of lab values and the possible relatedgastrointestinal disturbances.

N.B: Normal lab value reference ranges may differ from institutions. Always check
with the facility’s protocol.
Self-assessment 8.4.
CHIEF COMPLAINT: My eyes are yellow for two days.
HISTORY OF PRESENT ILLNESS: Mrs. S is a 36 year old unemployed woman
who presents with yellow discoloration of her eyes which she noticed two days
ago while washing her face. At first she thought the color was due to the lighting
in her bathroom, but this morning, when going outside, she noticed that her
hands “looked yellow.”
Mrs. Salco further admits to feeling “sick and tired” for the past 2 -3 weeks. She
has lost her appetite and feels weak. During this time, she has been frequently
nauseated and ate very little food. Last night she developed a fever and “shook
all over with a chill.” This morning she awoke after a restless night with pain and
a sensation of fullness in the right upper abdomen. She also vomited twice. The
emesis was non -bloody. She has not had diarrhea. She has no back or shoulder
pain. She thinks she lost 7kg during the last 3 months. She has no joint pain or
skin rash.
Mrs. Salco is a chronic alcoholic who has been hospitalized on several occasions
for alcohol related problems, including a psychiatric admission at Ndera Neuro –
psychiatric hospital. Although she was considered as a gifted, young accountant
with a bright future. Since graduation from business and Management school
she has had many alcohol related work problems and lost her position at
a prestigious company three weeks ago. Since that time she has consumedapproximately 3 bottles of Red Waragi (alcohol spirits) every day.
The relationship with her husband is not good these days and she is taking
Paracetamol regulary to calm her headache. She smokes one pack of cigarettes
per day. She is having an affair with a man who uses IV drugs and has history
of hepatitis.
PHYSICAL EXAMINATION:
–– The patient is alert but haggard looking. She is skinny and shows prominent
cheek bones. Her clothing is disheveled and her hair is uncombed. She
appears much older than her stated age. Bilateral, deep conjunctival
icterus
–– Vital signs: Blood pressure in right arm 104/60 mmHg, Heart Rate 110/
minute and regular, Respiratory Rate 18/minute, Temperature 38.90 C.
ABDOMEN: The abdomen is round and slightly tympanitic. The liver is palpable
beneath the costal margin (9 cm.) and tender. The liver span is 20 cm. There is no
rebound tenderness, shifting dullness or splenomegaly. Normal bowel sounds.
SKIN: Icteric
LABORATORY DATA:
Aspartate arninotransferase (AST) 150 U/L
Alanine aminotransferase (ALT) 60 U/L
Total Bilirubin 22 mg/dL
During, hospitalization WBC rose to 42,000/mm3; total bilirubin rose to 32 mg/dL
1. Cite the main clinical reason for consultation of Mrs S.
2. Elicit other significant clinical problems that Mrs S. has.3. Recommend the possible differential diagnoses for Mrs S.
8.5. Identification of client problems
Learning activity 8.5.Observe the pictures carefully and answer the asked questions
1. Describe what Picture A, B, C and D are showing?
2. What does picture A and B have in common?
8.5.1. Abdominal pain
Pain can be subjective or objective. The patient will point to the location of the
pain, the nature of the pain and any aggravating or relieving factors, how often
the pain felt and how long it lasts and if there is radiation elsewhere (SOCRATES
Site, Onset, Character, Radiation, Associated symptoms, Time, Exacerbating/
relieving, Severity). Abdominal pain related to gynecological matters have to bedifferentiated from the one originating from the digestive system.:
8.5.2. Appetite and eating disorders
Appetite and eating can be influenced by many factors that may indicate
gastrointestinal disease or that can be attributed to socioeconomic considerations
such as food availability, family norms, peers, and cultural practices.
• A loss of taste sensation can contribute to loss of appetite and potentially result
in poor nutrition, especially in older individuals. Attempts at voluntary control
can be a factors, such as dieting or eating disorders. Appetite disorders may
result in weight loss which can also be associated with illness, while weight
gain may be attributed to fluid retention or a mass.
• On the other hand, dysphagia which is difficulty swallowing may occur. Some
people may be completely unable to swallow or may have trouble swallowing
liquids, foods, or saliva. Eating becomes a challenge, making it difficult to take
in enough calories and fluids to nourish the body. The patient will be asked
if they have any difficulty swallowing and when the difficulty first occurred.
People with diseases of the nervous system, such as cerebral palsy or
Parkinson’s disease, often have swallowing problems. Additionally, stroke or
head injury may affect the coordination of the swallowing muscles or limitsensation in the mouth and throat.
• Moreover, nausea and vomiting may indicate food poisoning. Questions
about types of food eaten in the past 24 hours should be asked to rule out
potential poisoning. If vomiting is present, you will want to ask about the
amount, frequency, color, and odor of the vomitus.
• Hematemesis, or blood in the vomitus, is a common symptom of gastric or
duodenal ulcers and may also indicate esophageal varices. Coffee ground
emesis indicates an “old” gastrointestinal bleed. The old, partially digested
blood appears to look like coffee grounds.
• Changes in Bowel Habits is a common manifestation of gastrointestinal
disease. The frequency, color, and consistency of bowel movements, use of
laxatives.
8.5.3. Ascites
Usually seen in patients with cirrhosis of the liver. The patient will have a protuberant
abdomen. It is caused by increased hydrostatic pressure in patients with cirrhosis
of the liver. Percussion is normally used for the assessment of ascites, however,
there are other methods. An abdomen with ascites will have both tympanic and dull
sounds.
You will hear tympany at the top of the abdomen around the epigastric area and
dullness will be heard lower around the umbilicus or any dependent areas of the
abdomen.
8.5.4. Nursing diagnoses
According to different domains of diagnosis by NANDA, examples of nursing
diagnosis can be set down; Imbalanced nutrition, Impaired swallowing, Obesity,
Overweight, Abnormal distention, Pain, Diarrhea, Constipation, Bowel incontinence,
Excess fluid volume, Fluid volume deficit, Fatigue, Risk for infection, Lack of
knowledge, Anxiety, and Disturbed body image.
Note that alterations in gastrointestinal assessment findings could indicate
potential problems and being knowledgeable about the focused, gastrointestinal
assessment will allow the healthcare provider to intervene quickly and appropriatelyfor gastrointestinal disorders
Self-assessment 8.5.
1. Client X is admitted at the Hospital for an intensive pain of 7/10 located
in her hypogastric region. In your judgement, mention 2 health problems
that might be the underlying causes of this pain.
8.6. Nursing intervention based on patient’s problemLearning activity 8.6.
Mr. Z. is a 26 years old male suffering from peptic ulcer problem which is
worsening as the crises have increased considerably this last year.
1. Do you think you can help Mr. Z as an Associate Nurse?
Within the framework of his or her role, the nurse performs acts or provides care
aimed at identifying risks, ensuring comfort and safety of the person and his or her
environment, and informing the person and his or her family.
Basically for digestive system problems, the interventions will base on care
and procedures to ensure the hygiene of the person and his/her environment,
Supervision of hygiene and dietary balance, Supervision of food intake and
Monitoring of intestinal elimination.
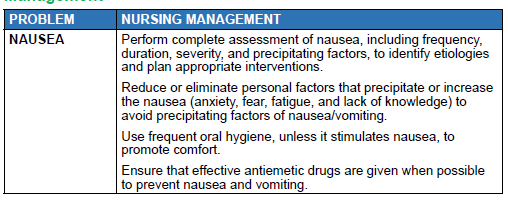
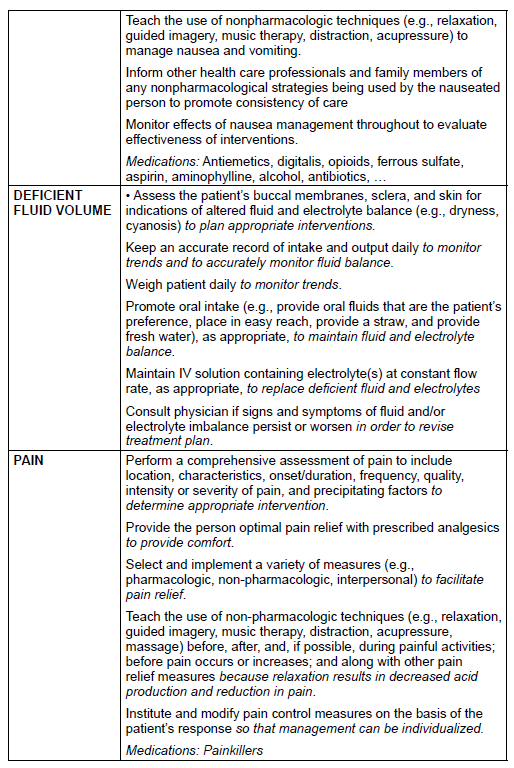
8.6.1. Samples of digestive system problems and theirManagement
In conclusion, for the digestive system intervention, Implement the appropriate
care for each type of transit disorder, Manage the pain as prescribed, Educate the
patient on foods and preventive dietary measures, Monitor vital parameters and
Reassure the patient
Self-assessment 8.6.
Mr. Z. is a 26 years old male suffering from peptic ulcer problem which is worsening
as the crises have increased considerably this last year. When the nurse asked him
about willingness to modify lifestyle he was doubting and delayed to reply to the Nurse.What would be the nursing interventions to Mr. Z?
End unit 8 assessment
1. Appendicitis means ……………………………………………………………
…………………………….
2. Hepatitis means ………………………………………………………………
……………………………….
3. Dysphagia means ……………………………………………………………
…………………………………
4. Melena means …………………………………………………………………
……………………………….
5. Outline 10 commonly presenting complaints of the gastro intestinal
system at the hospital
6. Explain how, the setting is relevant and can provide clues to the possible
origin of a disorder
7. In conclusion of a history taking session, we should always end by ICE.
Write ICE in full.
8. What can occur as a result of the aging process?
A. Dysphagia
B. Blood in the stools
C. Increase in food intolerance
9. Alcohol can cause liver cirrhosis and ________.
10. Age affect digestion by:
a. Slowing swallowing
b. Overgrowth of bacteria which reduces the amount of nutrients the
intestines absorb
c. Reducing stomach secretions
d. All of the above
11. Most of the digestive process take place in:
a. Small intestine
b. Large intestine
c. Stomach
d. All of the above
12. The liver helps digestion by:
a. Making important enzymes
b. Neutralizing stomach acid
c. Producing biled. Regulating insulin
