UNIT 5 FIRST AID CARE OF THE SELECTED EMERGENCY CONDITIONS OF SELECTED BODY SYSTEMS
Key unit competence
Apply correctly the techniques of victim’s evacuation and intervention during
emergenciesIntroductory activity 5.0
The above images represent health conditions that require emergency attention.
Observe them carefully and attempt the following questions:
1. Which health conditions do you thinks are portrayed in picture A, B, C and D?
2. Apart health condition adressed in question 1, What would you think more
of picture A and picture D? associate nurse, what could you do to care forpatient in picture D
5.1 Respiratory system pathologies
5.1.1 Brief anatomy and physiology of the respiratory system
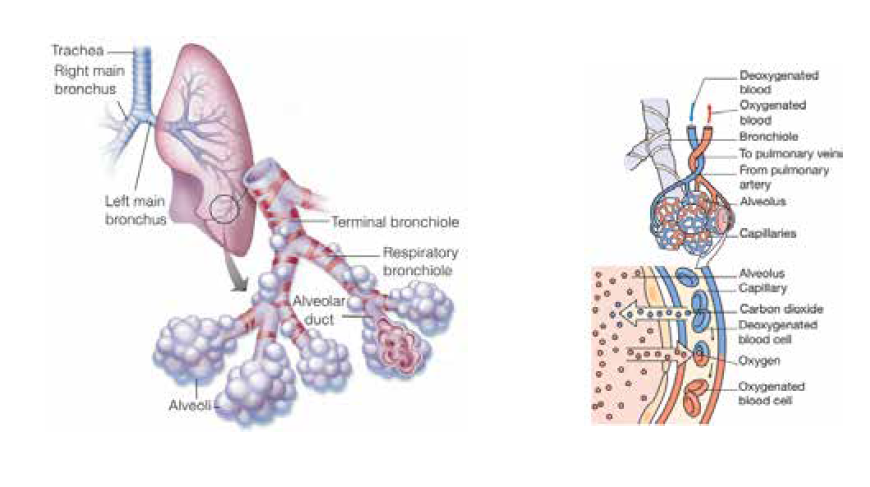
The respiratory system is one of the major systems of the body and primarily
consists of two lungs. its main function is to facilitate gas exchange trough ventilation
(the process of breathing) and respiration. Respiration can be expressed in two
ways: internal respiration and external respiration. External respiration refers to
exchange of gases at alveolar/ capillary level, whereby oxygen enters the blood
and carbon dioxide leaves to be excreted through exhalation. Internal respiration
refers to metabolism at cell level where oxygen is combined with carbohydrates to
produce energy; carbon dioxide is a waste product of this metabolic process. Below
is the representation of some respiratory system structures and external respirationphysiology:
Observe carefully the above pictures and answer the following questions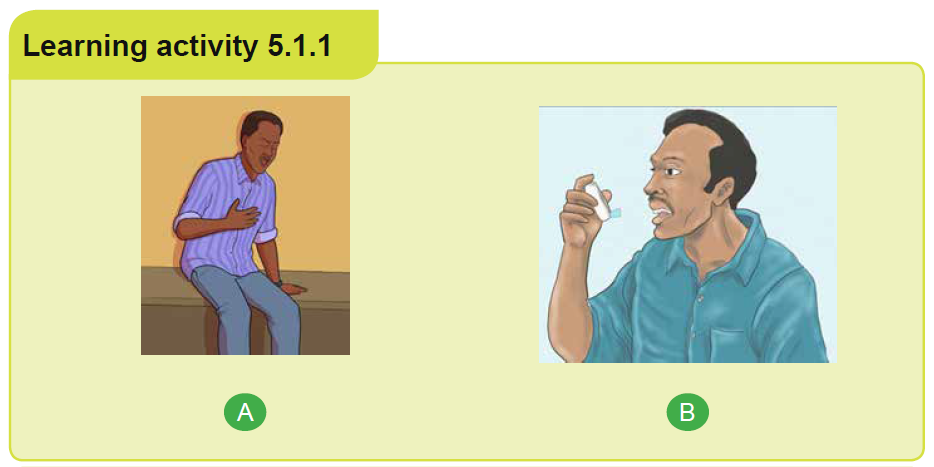
1) What do you think of piture A
2) What do you think the person in picture B is doing?
Asthma is a chronic inflammatory lung disease that causes airway hyperresponsiveness,
mucus production, and mucosal edema resulting in reversible
airflow obstruction triggering coughing, wheezing and shortness of breath. In fact,
“Asthma” is an ancient Greek word meaning “short breath,” and as the name
implies, it can leave the sufferer gasping for air.
Though, asthma is a common chronic inflammatory condition of the airways, its
course is not completely understood. As a result of inflammation, the airways are
hyper-responsive and they narrow easily in a response to a wide range of stimuli
regarded as precipitating or triggering factors. Allergens, irritants, air pollutants,
pollen, pollution, tobacco smoke, cold weather, physical exertion, strong odors, and
medications are common predisposing factors for asthma. Exercise and stress can
also be an asthma trigger for some.
Pathophysiologically, when a susceptible individual is exposed to a trigger, an
immediate inflammatory response with bronchospasm happens. This inflammation
causes increased responsiveness of the airways to multiple stimuli leading to
recurrent episodes of asthmatic symptoms. The response to an irritant in the
airways causes muscle tightening and narrowing of the lumen and with inflamed
airway lining mucus production increases. This leads to the clinically recognized
symptoms of shortness of breath, wheezing (high pitched whistling) chest tightness,coughing with sputum occasionally.
For some people, asthma is a minor nuisance while for others, it can be a major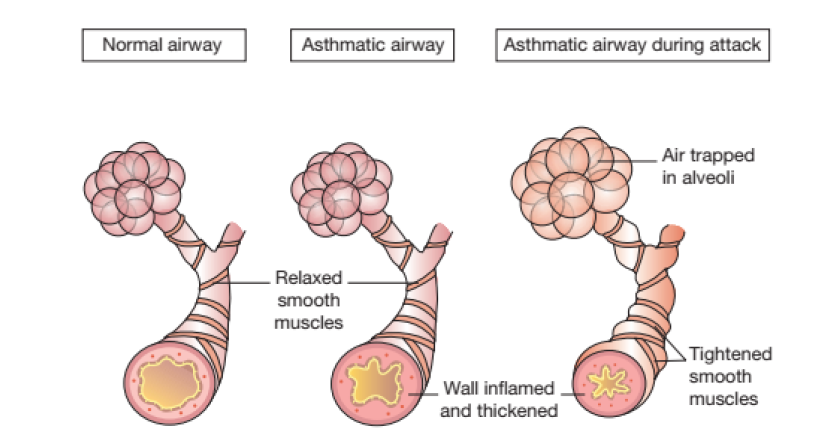
problem that interferes with their daily activities and may lead to a life-threatening
asthma attack. Simply classified, exist mild asthma, moderate asthma and severe
asthma. The below figure illustrates asthmatic events experienced in each severityclass:
Accurate history taking is possibly the most important aspect of patient assessment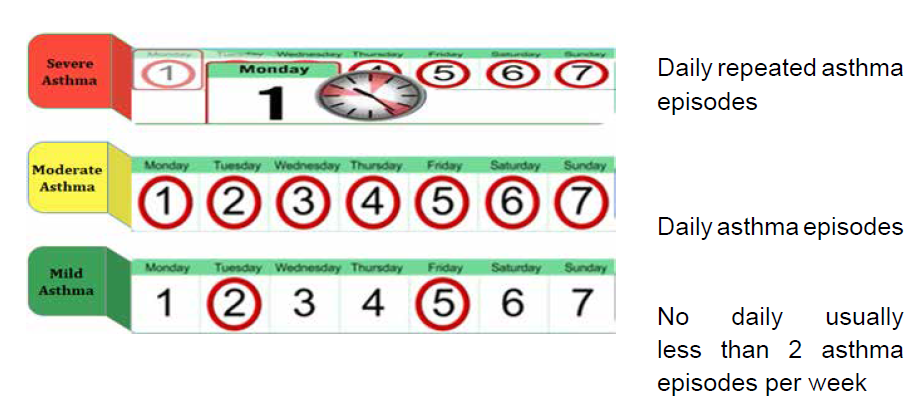
and can provide a great deal of the information required for a diagnosis. Clinical
diagnosis is based on the recognition of a characteristic pattern of symptoms and
signs and the absence of an alternative explanation for them.
The management of asthma consist of both symptoms management and avoiding
triggering factors. The goal of management is for people to be free from symptoms
and able to lead a normal active life. This is achieved partly through treatment,
tailored to the person, and partly by people getting to know what provokes their
symptoms and avoiding these triggers as much as possible. Since asthma is a
chronic condition, people with asthma may require daily medication to keep it
under control. These medications are prescribed and used in a step-wise approach
to prevent and control asthma symptoms, reduce the frequency and severity of
exacerbations, and reverse airway obstruction. However, for all patients, an
inhaled short-acting beta2 agonist (SABA) is recommended for quick relief of acute
symptoms. Strategies for long-term control vary and may need to be modified if a
short-acting bronchodilator is needed more than twice a week.
Inhaled therapy is the mainstay of treatment for people with asthma. Thus, drugs
are delivered directly to the airways where they are needed, work quickly and
effectively. Inhalers allow use of lower doses which is associated with fewer side
effects than with oral drugs. Inhaled therapy requires a delivery device to be able
to hold the drug, and to deliver it to the airway at the required moment. Health care
professionals should be well versed with the correct inhaler technique to effectively
support patient in need.
Three major types of inhalers are used to deliver asthma and chronic obstructive
pulmonary disease (COPD) medications: metered dose inhalers (MDIs), dry
powder inhalers (DPIs), and soft mist inhalers (SMIs). Each type has advantages
and disadvantages. Nevertheless, the two first types of inhalers i.e. metered dose
inhaler (MDI) and dry powder inhaler (DPI) are most common. In an MDI, a chemical
propellant is used to deliver the medication when the canister is depressed. In
contrast, a DPI contains no propellant. Instead, the medication is released by
inhaling rapidly through the mouthpiece. Manufacturers’ instruction leaflets, which
accompany each device, contain useful information about breath-hold, cleaning,
storing and problem solving; and should be read carefully before use and kept forfuture reference if needed.

Observe carefully the above pictures and answer the following questions:
1. What do you think picture A represent?
2. What do you think is happening in picture B
3. What do you think of picture C
5.1.2 First aid interventions in case of asthma attack
An asthma attack also known as an asthma exacerbation is a sudden worsening of
asthma symptoms and lung function caused by the tightening of muscle around your
airways (bronchospasm) leading to distress. This distress can be the presenting
manifestation of asthma or occur in patients with known asthma diagnosis in
response to environmental triggers, to viral upper respiratory infection, lack of
adherence to controller medication or an unknown stimulus.
A distress is an urgent situation in which a person is suffering or in danger and
therefore in urgent need of help to prevent a worsening of the situation. The best
strategy for management of asthma attack is early recognition and intervention
before attacks become severe and potentially life-threatening. Patients with long
standing asthma are generally able to determine when they have an exacerbation.
The assessment should include the onset of symptoms, the likely cause of severity
of symptoms, current medication and response to treatment of previous and riskfactors for asthma related death.
Risk factors for fatal asthma attack include: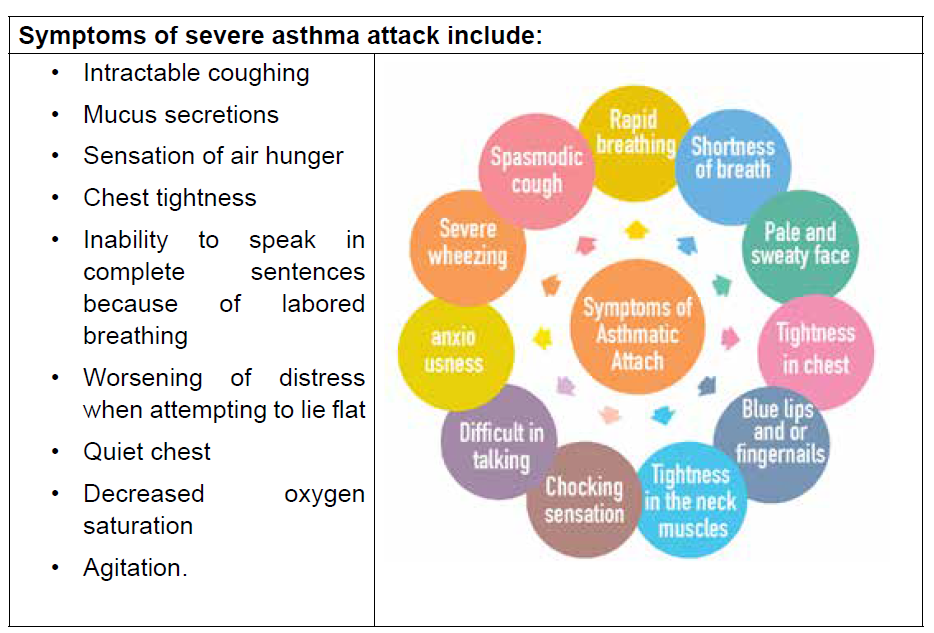
• Previous life-threatening attack requiring intubation or intensive care
admission
• Asthma attack despite current course of oral glucocorticoids
• More than one hospitalization for asthma in the last 12 months
• Use of more than one canister of SABA per month
• Comorbidities such as cardiovascular or chronic lung disease
• Not currently using inhaled glucocorticoids
• Food allergy in patient with asthma
• Three or more visits to emergency department for asthma in the past 12
months
• History of poor adherence to asthma medications and or written asthma plan
• Illicit drug use and major psychosocial problems including depression
• Difficulty perceiving asthma symptoms or severity of attack
First aid
• Sit the person comfortably upright, remain calm and speak calmly to patient
and do not the person alone
• Remove any obvious triggers in immediate patient environment area • Give 4 puffs of reliever inhaler (e.g., Ventolin) and use a spacer if available.
Give 1 puff at a time with 4 breaths after each puff. Use the person’s own
inhaler if possible, otherwise use the one in a first aid kit or borrow one
• Wait for 4 minutes, if the person still cannot breathe normally give more 4
puffs
• If the person still cannot breathe normally Call an ambulance (SAMU – 912)
and say that the person is having an asthma attack. And keep giving reliever
every 4 minutes till the ambulance arrives (4 puffs each time are safe dose for
children; in adults with a severe attack, you can give up to 6 – 8 puffs every
4 minutes)
• Keep monitoring the person and never leave him or her alone
In a healthcare facility setting:
• Start treatment immediately
• Semi-sitting position
• Give O2 to keep saturation above 90%
• Start short acting Beta 2 agonist nebulization (e.g., Salbutamol 5 mg in 5 ml
of normal saline over 10 minutes repeated ½ hour later)
• Hydrocortisone 100 mg IV every 6 hours
• Assess the need of ventilation according to the response to therapy
• Avoidance of the triggering agent if known
Note:
Close friends and family members of an asthmatic person should be aware of
how to manage an individual who is having an asthma attack, thus, paramount toeducate them on this.
6) Secure a good seal with the lips around the mouthpiece of the spacer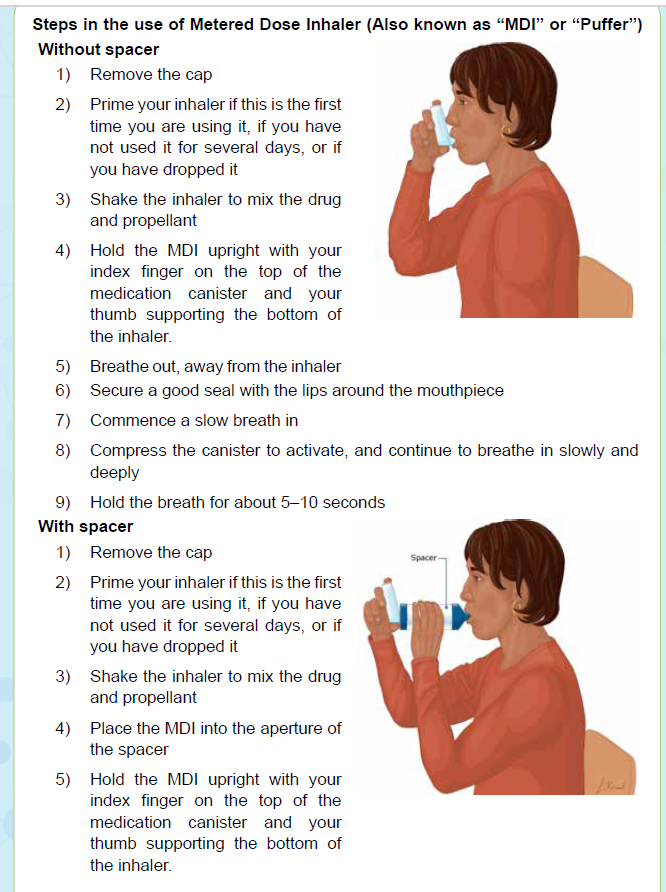
7) Compress the canister to activate, and continue to breathe in slowly and
deeply
8) Take four or five deep breaths
Note:
• The use of a spacer with an MDI is recommended to increase lung deposition
and reduce risks of failing to synchronize inhalation and activation of the
MDI. In fact, large volume spacers have been shown to be comparable to a
nebulizer in an emergency
• If your inhaler contains a steroid medicine, rinse the mouth (gargle with water
after you use and then spit out the water)Steps in use of capsule dry powder
1) Remove a capsule from the foil blister packaging, observing the
manufacturer’s instructions
2) Open the inhaler, and place the capsule inside the chamber
3) Close the inhaler
4) Pierce the capsule by squeezing the button on the side of the inhaler
5) Secure a good seal with the lips around the mouthpiece
6) Inhale as hard as possible
7) Hold the breath for 5–10 seconds
8) If any powder is left, repeat steps 5–6.
Self-assessment 5.1.2
1) Which of the following best describes asthma?
a. Intermittent airway inflammation with occasional bronchospasm
b. A disease of bronchospasm that leads to airway inflammation
c. Chronic airway inflammation with superimposed bronchospasm
d. Relatively fixed airway constriction
2. What first aid interventions should be done for a person with asthma
attack?5.1.3 Acute Respiratory distress (ARD)
Observe the above picture and answer the following question: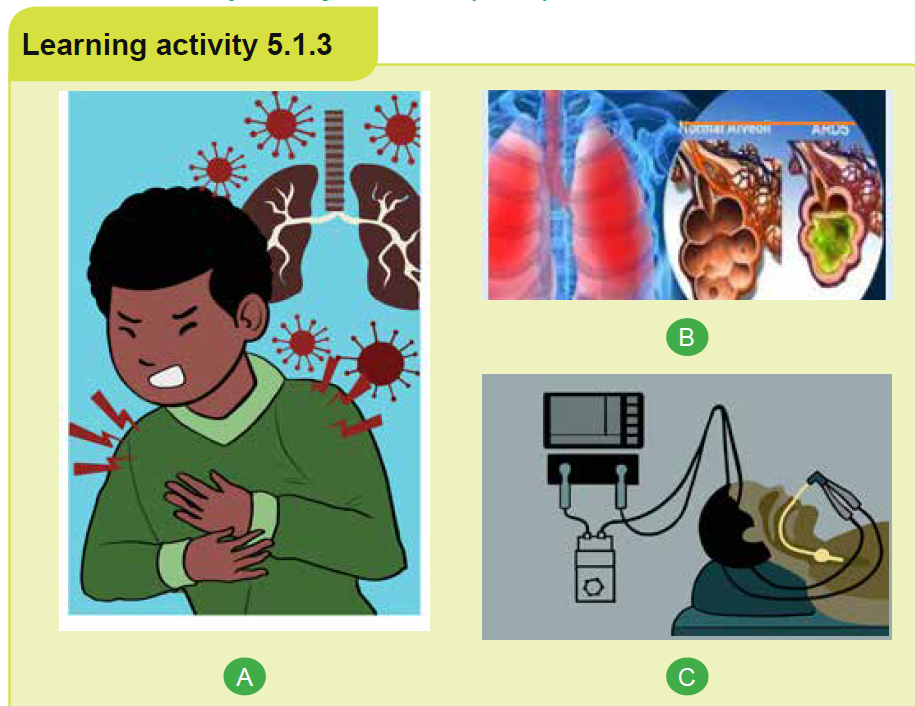
1. To you, what image A represent?
2. What do you think image B tries to portray?
3. What do you think is being done in image C?4. Attempt to establish, if any, relationships across the above images
5.1.3.1 Overview of acute respiratory distress (ASD)
a) Definition
Acute respiratory distress (ARD) is a severe lung condition that occurs when fluid
builds up in the tiny, elastic air sacs (alveoli) in the lungs. This fluid keeps the lungs
from filling with enough air, which means less oxygen reaches to the bloodstream.
Too much fluid in the lungs can lower the amount of oxygen or increase the amount
of carbon dioxide in the bloodstream. ARD can prevent the organs from getting the
oxygen they need to function, and it can eventually cause organ failure.
b) Etiology and pathophysiology
Although the exact cause of ARDS is unclear, it is known that ARDS does not occur as a
primary process but may follow a number of diverse conditions producing direct or indirect
lung injury. Direct injuries are those in which the lung epithelium sustains a direct
insult. Indirect injuries are those in which the insult occurs elsewhere in the body
and mediators are transmitted via the bloodstream to the lungs.
• Direct injuries include: aspiration, pneumonia, fat embolism, near drowning,
oxygen toxicity, pulmonary contusion, and toxic inhalation.
• Indirect injuries include: severe and widespread bacterial infection in the
body (sepsis), severe injury to the body that causes low blood pressure (shock),
excessive blood transfusions, anaphylaxis, disseminated intravascular
coagulation, and acute pancreatitis, drug overdose, embolism and long bone
or pelvic fractures.
The injuries result in an inflammatory reaction. This releases body chemicals into the
bloodstream. Typically, this reaction would protect the body and help fight infection
or heal from an injury. However, in some people these inflammatory chemicals will
cause the smallest blood vessels in the lungs to leak fluid. Fluid leaves these small
vessels and goes into the tiny air sacs in our lungs, called alveoli causing a noncardiogenic
pulmonary edema. Pulmonary edema interferes with allowing carbon
dioxide to be excreted (hypercarbia) and oxygen to be absorbed (hypoxemia).
Increased capillary pressure can cause pulmonary hypertension leading toatelectasis and a reduction in functioning lung volumes.
c) Signs and symptoms
Initial manifestations of ARDS typically develop 24 to 48 hours after the initial insult
and they vary depending on its cause and severity, as well as the presence of
underlying cardiorespiratory comorbidity. Dyspnea, tachypnea and anxiety are
early manifestations.
Common clinical manifestation of ARDS include:
• Acute onset of severe dyspnea, tachypnea, tachycardia, intercostal retractions
and use of accessory muscles, cyanosis.
• Increasing requirements of oxygen therapy. Hypoxemia refractory to
supplemental oxygen therapy.
• Scattered crackles and rhonchi heard on auscultation.
• Decreased pulmonary compliance, evidenced by increasing pressure required
to ventilate patient on mechanical ventilator
• As respiratory failure progresses, mental status changes such as agitation,
confusion and lethargy occur.
The diagnosis of ARDS is based on clinical, hemodynamic, and oxygen criteria.
The hallmark signs for ARDS include acute-onset, severe hypoxemia, despite
increasing oxygen therapy, and chest x-ray exhibiting bilateral infiltrates.
d) Treatment
Recognizing and promptly treating ARDS is critical to reduce the associated high
mortality. The treatment aims at maximizing clinical stability and managing symptoms
while treating the underlying cause as if this is not treated the ARDS will not resolve.
Thus, Current ARDS treatment is primarily supportive. Supportive measures assist
the patient while the underlying cause is being treated. Mechanical ventilation is
nearly always required to decrease work of breathing and improve oxygenation.
Fluid management must be maintained. The patient may be hypovolemic because
of the movement of fluid into the interstitium of the lung. Along medications to treatthe underlying cause, adequate nutrition should be initiated early and maintained.
Self-assessment 5.1.3
1) Acute respiratory distress (ARD) is defined as:
a) Acute respiratory distress syndrome occurs due to the collapsing of a
lung because air has accumulated in the pleural space
b) A conditions which causes the alveolar capillary membrane to leaks fluid
into the alveolar Sac
c) ARDS is a pulmonary disease that gradually causes chronic obstruction
of airflow from the lungs
2) Which patient below is at most risk for developing ARD:
a) A 50 years old patient with pneumothorax
b) A 49 years old patient with diabetes
c) A 70 female patient with sepsis caused by bacterial infection
3) As an associate nurse you know that ARD can be caused by direct or
indirect lung injury. Choose below all indirect causes of ARD
a) Drowning
b) Aspiration
c) Sepsis
d) Blood transfusion
e) Pneumoniaf) Pancreatitis
5.1.3.2 First aid in difficult breathing due to ARD
Learning activity 5.1.3.2
While you are traveling in the village you meet with a male person with breathing
faster a fast heartbeat, extreme tiredness, coughing that produces phlegm
and fainting. As first aider. Which position are you going to give him, make him
comfortable?
The primary goal of first aid is to ensure that a person has enough oxygen to
prevent organ failure. If person is having breathing difficulty, immediately call for
help (SAMU – 912) then:
• Position the patient in prone position - Prone positioning is widely used to
improve oxygenation of patients with acute respiratory distress syndrome
(ARDS)
• Check the person’s airway, breathing, and pulse. If necessary, begin CPR.
• Loosen any tight clothing.
• Help the person to use any prescribed medication (such as an asthma inhaler
or home oxygen) if he/she has
• Continue to monitor the persons breathing and pulse until medical help
arrives.
• Do NOT assume that the person’s condition is improving; if you can no longer
hear abnormal breath sounds, such as wheezing.
• If there are open wounds in the neck or chest, they must be closed immediately,
especially if air bubbles appear in the wound. Bandage should be performed
on such wounds at once. A “sucking” chest wound allows air to enter the
person’s chest cavity with each breath. This can cause a lung collapse.
Bandaging the wound with gauze pads allows trapped air to escape from the
chest, but it prevents air from entering the chest through the wound.
• Do NOT give the person food or drink.
• Do NOT move the person if there has been a chest or airway injury, unless it
is absolutely necessary.
• Do NOT place a pillow under the person’s head as this can close the airway.
• Do NOT wait to see if the person’s condition improves before getting medicalhelp. Call for help immediately
Self-assessment 5.1.3
1) You are caring a patient with ARD, as an associate nurse which position
is beneficial for this patient
a) Lateral position
b) Prone position
c) Spine position
2) How can you help someone with ARD out of health facility?
5.2 Cardiovascular system pathologies
5.2.1 Brief review on blood pressure physiology and bloodpressure measuring
a) Definition and classification of blood pressure (BP)
Blood pressure (BP) is the force exerted by the blood against the walls of the
blood vessel and must be adequate for tissue perfusion to be maintained during
activity and rest. It is traditionally measured by use of auscultation with a mercurytube
sphygmomanometer, measured in millimeters of mercury and expressed in
terms of systolic pressure (SBP) over diastolic pressure (DBP). SBP is the highest
arterial pressure when the heart contracts and empties. DBP is the lowest arterial
pressure when the heart relaxes to fill with blood. BP is one of the most commonly
measured clinical parameters and blood pressure values are major determinants of
therapeutic decisions.
In healthy adults the average systolic pressure is less than 120 mmHg and the
average diastolic pressure is less than 80 mmHg. The difference between the
systolic and diastolic pressure, known as the pulse pressure and reflects stroke
volume, ejection velocity, and systemic resistance and is a noninvasive indicator
of CO (normally ranging between 30 to 40 mm Hg, if less than 30 mm Hg indicate
decreased CO). The mean arterial pressure (MAP) is the average pressure in the
arterial circulation throughout the cardiac cycle, and it can be calculated using the
formula (systolic BP + diastolic BP + diastolic BP)/3. Diastole counts twice as much
as the systole because two-thirds of the cardiac cycle is spent in diastole. The tablebelow attempt to classify BP measurements with emphasis on hypertension.
b) Factors affecting the blood pressure
The BP is primarily a function of cardiac output (CO) which is the volume of blood
ejected from the heart per minute and systemic vascular resistance (SVR) that is
the force opposing the movement of blood within the blood vessels. Thus, factors
that influence any of these influence the BP. Factors that influence the BP arerepresented in the following figure:
A certain amount of pressure within the circulatory system is necessary to maintain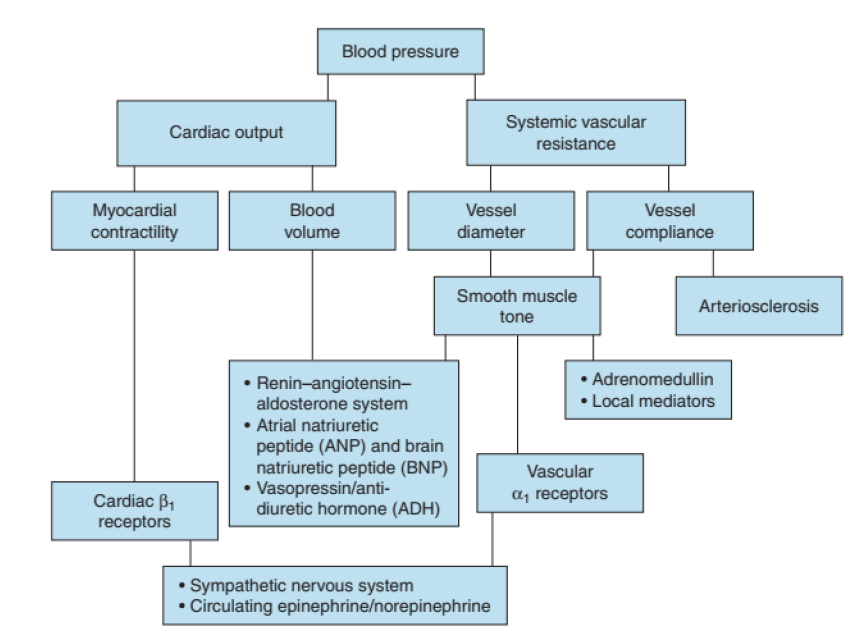
open vessels, capillary perfusion and oxygenation of all body tissues. The
predominant mechanisms of blood pressure control are the central nervous system
(CNS), the renin-angiotensin-aldosterone system, and extracellular fluid volume.c) Blood pressure measurement
Note: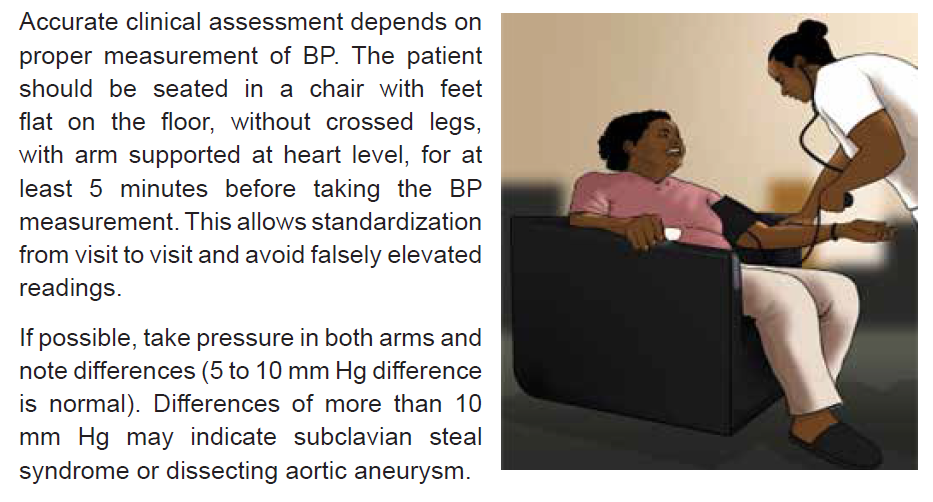
• Some patients may have elevated BP readings in a clinical setting and normal
readings when BP is measured elsewhere. This phenomenon is referred to
us, as “white coat” hypertension”.
• Some other patients have normal BP when in clinical setting and elevated BP
at home. This phenomenon is referred us, as “masked hypertension”.
• Naturally, both systolic and diastolic BP tend to move together (i.e. climb of
fall together). However, that is not always the case as isolated rise or fall of
systolic or diastolic readings exist; e.g. isolated systolic hypertension, isolateddiastolic hypertension.

5.2.2.Hypertensive Crisis

5.2.3.1 Brief review of hypertension
Hypertension is a disease of vascular regulation in which the mechanisms that
control arterial pressure within the normal range are altered characterized by a
persistently elevated systemic blood pressure. Thus, hypertension is consistent
blood pressure readings of ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic, based
on the average of three or more readings taken on separate occasions. While it
rarely causes symptoms or noticeably limits the person’s functional health patterns,
hypertension is a major risk factor for coronary heart disease, heart failure, stroke
and kidney failure.
Its cause is not identifiable in 90% of all of hypertension; this types of hypertension
is referred to us as “Essential or Primary Hypertension” while in the remaining 10%
exist an identifiable cause referred to us as “Secondary of hypertension”. A number
of risk factors have been identified for primary hypertension. Both genetics and
environmental factors play a role in the development of hypertension. Family history,
age, Genetic factors and race are non-modifiable factors linked to hypertension.
More others factors such as high sodium intake; low potassium, calcium and
magnesium intake; obesity; excess alcohol consumption and insulin resistance are
regarded to be modifiable factors linked to hypertension.
5.2.3.2 Definition and classification of hypertensive crisis
Hypertensive crisis is a severe and potentially life-threatening increase in blood
pressure therefore a medical emergency, defined as systolic blood pressure ≥
180mmHg and or diastolic blood pressure ≥ 120mmHg.
As a result of this severe increase in BP, the blood vessels and organs may
become damaged. Therefore, hypertensive crises can be divided into hypertensive
emergencies or hypertensive urgencies according to the presence or absence
of acute target organ damage, respectively. Hypertensive emergencies include
hypertensive encephalopathy, intracranial or subarachnoid hemorrhage, acute left
ventricular failure with pulmonary edema, heart attack, renal failure, dissecting
aortic aneurysm and eclampsia (during pregnancy).
This differentiation is an extremely useful classification in clinical practice since
a different management is needed, which in turn has a significant effect on the
morbidity and mortality of these patients.
5.2.3.3 Signs and symptoms
Hypertensive crisis is characterized by rapid onset of systolic pressure higher than
180 mmHg and or diastolic pressure higher than 120 mmHg often associated with
headache, blurred vision, papilloedema, nausea, vomiting, seizures, stupor and
altered mental status. Moreover, there may be typical signs and symptoms related
to resultant target organ damage.
• Brain effects:
• Signs and symptoms of encephalopathy (probably as a result of cerebral
edema and spasms of cerebral vessels)
• Signs and symptoms of stroke
• Progressive headache, stupor and seizures
• Kidney effects:
• Signs and symptoms of decreased blood flow and vasoconstriction
• Signs and symptoms of elevated blood urea nitrogen (BUN)
• Signs and symptoms of increased plasma renin activity
• Lowered urine-specific gravity
• Proteinuria
• Signs and symptoms of renal failure
• Cardiac effects:
• Signs and symptoms of left-sided heart failure
• Signs and symptoms of acute myocardial infarction (MI)
• Signs and symptoms of right-sided heart failure.
5.2.3.4 Management of hypertensive crisis
Hypertensive crisis requires an immediate medical attention and its treatment may
involve hospitalization and the use of oral and/or intravenous medications after
thorough assessment and classification. The goal of care is to reduce the blood
pressure by no more than 25% within minutes to 1 hour, then towards 160/100 within
2 to 6 hours. It is important to avoid rapid or excessive blood pressure decreases
that may lead to renal, cerebral or cardiac ischaemia. Blood pressure is monitored
frequently (every 5 to 30 minutes) during a hypertensive emergency. The serum
urea, creatinine, calcium and total protein levels are carefully.
Immediate interventions to be implemented when hypertensive crisis is suspected
include
• Assess BP in both arms
• Elevate the head of the bed to approximately 30 - 450
• Administer supplemental O2
• Notify the physician
• Perform a focus assessment to assess and document level of conscience,
respiratory status, neurological deficits, baseline vital signs including oxygen
saturation (if possible), note any visual disturbance, chest pain, peripheral
edema and hematuria
• Keep close monitoring including assessing changes in cardiac rhythm if
patient is on a monitor and in and out
• Anticipate and prepare to get ready to implement physician orders such as
obtain an IV access, order laboratory tests (BUN, creatinine, electrolytes,administering medications and transferring the patient to intensive care unit.
Self-assessment 5.2.2
1) What is an essential hypertension?
2) Define and classify hypertensive crisis events
3) Should we aim at obtaining normal BP reading values when treatinghypertensive crisis? Explain your answer
5.2.3.First aid for acute hypotension
Observe the images and attempt to figure-out what is happening:
1) What do you think of picture A?2) What does image B represent and shows?
5.2.3.1 Overview of hypotension
a) Definition
Hypotension is a decrease in systemic blood pressure below normal value i.e.,
a systolic pressure below 90mmHg and a diastolic below 60mmHg. It is a
relatively benign condition that is under-recognized mainly because it is typically
asymptomatic. However, it can be a sign of underlying condition especially in
elderly. Hypotension a concern once pumping pressure is so low to perfuse key
organs with oxygenated blood.
b) Types of hypotension
There are several types of hypotension. Low blood pressure is categorized
according to when it happens and what’s causing it.
• Orthostatic or postural hypotension – is the drop in blood pressure that
occurs when you move from sitting or lying down to standing. As the body
adjusts to the position change, someone may feel dizzy or lightheaded. This
is what some people refer to as “seeing stars” when they get up. Being the
most common form of hypotension, it can affect people of all ages, but it’s
especially common in older adults. Other reasons associated to hypotension
include pregnancy, dehydration, exhaustion, strong emotions and medication
(e.g., taking anti-hypertensive drugs or drugs that have hypotension as a side
effect. Conditions affecting the autonomic nervous system, such as Parkinson’s
disease and diabetes, can often lead to orthostatic hypotension.
• Postprandial hypotension - is a drop in blood pressure that occurs after
eating. It is more common in older adults and people with autonomic
dysfunction.
• Neutrally mediated hypotension - happens when there is an abnormal
reflex interaction between the heart and the brain. People with this disorder
feel faint, dizzy, and nauseous after exercising or standing for a long time.
Children experience this form of hypotension more often than adults as
result of standing in one position for a long time. Having a strong emotional
response, such as feeling shocked or scared also can result into this type of
hypotension in some people
• Severe hypotension - this type of hypotension is linked to shock. During
shock the BP drops to dangerously low levels, and the brain and organs can’t
get enough blood to function properly therefore life threatening if not treated
quickly. Shock can happen as a result of:
• Decreased effective circulating volume (hypovolemic shock)
• Impaired cardiac output due to heart pump dysfunction or obstruction to
cardiac filling (cardiogenic shock)
• Impaired peripheral i.e., loss of vascular tone (distributive shock)
c) Signs and symptoms of hypotension
The patient present with systolic pressure that is below 90mmHg or systolic BP 40
mm Hg less than baseline. Depending on how low the blood pressure is the patient
may have an altered level of consciousness; cool, pale, cyanotic, diaphoretic skin;
nausea and vomiting; shortness of breath; dizziness, blurry vision, weakness and
decreased urine output.
Immediate interventions
Using DRSABCD approach:
• Place patient in a supine position with head of the bed slightly elevated if
compromised airway
• Assess level of conscious, orientation, baseline vital signs with emphasis
on pulse quality and rhythm. Assess skin for color, temperature, moistness,
turgor, and capillary refill
• Call for medical assistance indicating patient’s status,
• Administer oxygen if inadequate respiratory effort
• Control any bleeding with direct pressure
• Obtain an IV access and give IV fluids if appropriate (hypotension may be due to
cardiac compromise, in which case fluids might be contraindicated
• Definitive management is established once the cause is identified (use
of clinical and para-clinical data). Depending of severity, this may include
administration of vasoactive medications and transfer of patient to a criticalcare unit.
Self-assessment 5.2.3
Which of the following statements concerning postural hypotension in the elderly
is false?
1) It increases the risk of falls and syncope
a) It is characterized by a drop in blood pressure when going from a standing
to a sitting position
b) It increases the risk of cardiovascular events
c) It is associated with the use of vasodilating medications
2) List four types of hypotension
3) What are the main mechanisms behind severe hypotension also knownas shock?
5.2.4 Heart Attack
Observe the above pictures and attempr to describe what you see and establish
any association or similarity if any
A. Overview of coronary artery disease
a) Introduction
The heart as a muscular pump responsible for moving blood throughout the body.
It needs an excellent blood supply to provide enough blood, oxygen and nutrients
to keep its pumping function effective. This is accomplished through coronary
circulation. With diseased coronary arteries, the supply of blood, oxygen and
nutrients to the heart is compromised which may lead to reversible or irreversible
injury to heart structures.
b) Review of vascularization anatomy of the heart
The heart structures are supply with oxygen rich blood by coronary arteries and
then the deoxygenated blood return into the general circulation through coronary
veins. The right and left coronary arteries arise at the base of the aorta, immediatelyabove the aortic valve.
They supply a discrete area of the myocardium and have limited collateral circulation
and are susceptible to obstruction by atherosclerotic plaque or thrombus that can
result in loss of blood flow to the myocardial muscle normally supplied by that
artery. This can be fatal, depending on the location of the obstruction. Blockage
of coronary arterial blood flow, especially in the left main coronary artery, usually
results in death from massive infarction of the left ventricle. However, if the blocked
artery supplies a smaller section of myocardium this may result not death.
c) Pathophysiology and classification of coronary artery diseases
The term of coronary artery disease (CAD) is a broad term used to refer to the
narrowing or occlusion of the coronary arteries. Pathophysiologically coronary
atherosclerosis (plaque buildup within the layers of the coronary arteries) is the
most common cause of CAD. The plaques progressively enlarge, thicken, and
calcify, causing a critical of the coronary artery lumen, resulting in a decrease in
coronary blood flow and an inadequate supply of oxygen to the heart muscle. The
term of “ischemic heart disease (IHD)” is used to indicate a condition in which there
is an inadequate supply of blood and oxygen to a portion of the myocardium.
Coronary heart diseases may be asymptomatic or symptomatic and are generally
divided into two categories:
• Chronic ischemic heart disease – this category includes stable and unstable
angina and silent myocardial ischemia.
• Acute coronary syndromes – this category ranges from unstable angina tomyocardial infarction (MI).

Pathophysiologic representation of ischemic heart diseases
Both modifiable and non-modifiable factors promote the occurrence of the disease
in genetically susceptible persons. Non-modifiable factors include age, gender,
race and family history. Modifiable factors include high level serum cholesterol,
smoking habits, obesity, diabetes, sedentary lifestyle and hypertension.
d) General manifestation of coronary artery disease
The cardinal manifestation is chest pain, characterized as either pressure,
heaviness, squeezing, choking, strangling, and/or cramping pain or discomfort.
This pain is usually localized behind middle or upper third of the sternum and the
patient will generally make a fist over the site of the pain rather than point to it with
his or her finger. It usually radiates to the neck, jaw, shoulders, arms, hands, and
posterior intrascapular area. Its duration depends on how severe the myocardium
is affected.
The OLDCART acronym can be used to adequately assess this chest pain. That
is Onset, Location, Duration, Characteristics, Aggravating symptoms, methods to
Relieve the pain, current Treatment. For instance, in chronic stable angina such
pain is associated with a specific level of physical or emotional stress and reliably
resolves with rest, relief of the stress, or nitroglycerin therapy and this last for less
than 10 minutes while for unstable one, this last usually for 10 – 20 minutes.
Associated symptoms may include diaphoresis, nausea, indigestion, dyspnea,
tachycardia, and increase in blood pressure.
e) Diagnosis and management of coronary artery disease
Laboratory tests may confirm the presence of risk factors, such as an abnormal blood
lipid profile and elevated blood glucose. Other common diagnostic tests to assess
for coronary heart disease include electrocardiography, stress testing, nuclear
medicine studies, echocardiography (ultrasound) and coronary angiography.
Drugs may be used for both acute and long-term relief CAD. The goal of drug
treatment is to reduce oxygen demand and increase oxygen supply to the
myocardium. Three main classes of drugs are used to treat angina: nitrates, betablockersand calcium channel blockers.
Self-assessment 5.2.4
1) What causes the pain that occurs with myocardial ischemia?
a) Death of myocardial tissue
b) Dysrhythmias caused by cellular irritability
c) Lactic acid accumulation during anaerobic metabolism
d) Increased pressure in the ventricles and pulmonary vessels
2) What are modifiable risk factor for CAD?3) How would you ascertain the chest pain is of CAD origin?
5.2.5. First aid intervention for heart attack
Observe the above images and attempt to answer the following questions: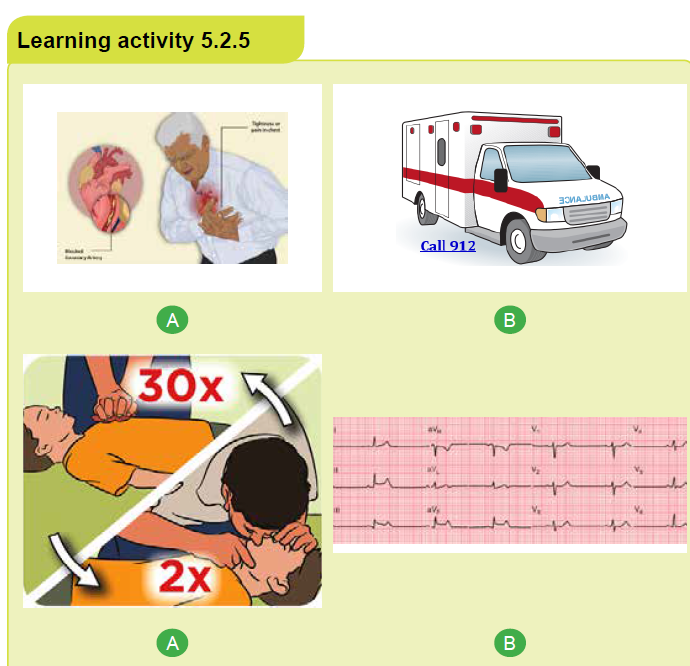
1) What do you think of image A?
2) What image B represent according to you?
3) What do you think is happening in image C?4) What do you think image D represent?
a) Introduction
Heart attack also known as Myocardial Infarction (MI) is one of the manifestations
of acute coronary syndrome (ACS) and is a life-threatening event. It refers to a
dynamic process by which one or more regions of the heart experience a prolonged
decrease or cessation in oxygen supply because of insufficient coronary blood flow
with subsequent necrosis or “death” to the affected myocardial tissue. If circulation
to the affected myocardium is not promptly restored, loss of functional myocardium
affects the heart’s ability to maintain an effective cardiac output. This may ultimately
lead to cardiogenic shock and death.
b) Brief heart attack pathophysiology
Most MIs occur as a result of coronary artery atherosclerosis, followed by rupture
of an unstable atheromatous plaque, platelet activation, and fibrin clot formation.
The resultant thrombosis interrupts blood flow and leads to an imbalance betweenmyocardial oxygen supply and demand and eventually myocardial tissue necrosis.

A: Damaged endothelium B: Fatty streak and lipid core formation C: Fibrous
plaque D: Complicated lesion
Non-atherosclerotic causes of MI include coronary artery spasm, congenital
abnormalities, coronary artery embolus, and connective tissue disorders.
c) Manifestations of Myocardial Infarction(MI)
Chest pain is the cardinal feature of MI, even though it is not universally present.
It is of the same character as angina pectoris; described as heavy, squeezing, or
crushing and is localized to the retrosternal area or epigastrium, sometimes with
radiation to the shoulder, arm, lower jaw, or neck. However, in contrast to stable
angina, however, it is more severe and persists for more than 20 minutes and is not
relieved by rest or Nitroglycerine.
Its onset is sudden and usually is not associated with activity. In fact, most MIs
occur in the early morning. The pain often is accompanied by sweating, nausea,
vomiting, and/or the sense of impending doom. People with a history of angina may
have more frequent anginal attacks in the days or weeks prior to an MI.
d) Immediate interventions
Early recognition and intervention is key for patient survival.
d.1. Prehospital first aid
Any heart attack might lead to cardiac arrest, but prompt action may prevent further
damage to the heart. A person suffering from a heart attack has a far better chance
of living than does a person whose heart has stopped. Therefore, the most important
first aid measure is to be able to recognize the signals of a heart attack and take
appropriate action promptly.
A person having a heart attack may deny the seriousness of the signals he or
she is experiencing, or believe the signals are just muscle soreness, indigestion
or heartburn. Therefore, do not let this denial influence you. If you think that the
person might be having a heart attack, you must act.
Though CPR is often what comes to mind when people think of first aid for a heart
attack or cardiac arrest, this is only part of a broader picture of what is needed for
the victim survival. There are five steps that are important when helping someone
with heart problems.
1) Early recognition and activation of emergency medical services system
such as SAMU Call 912).
2) Early CPR with an emphasis on chest compressions.
3) Early defibrillation.
4) Effective advanced life support.
5) Integrated post-cardiac arrest care.
Note: Each of these steps is as important as the others and time is a vital ingredient.
The following are important intervention steps for first aid:
a) Perform a scene survey, then do a primary survey to ascertain the acute
coronary syndrome (consider signs and symptom above by use of OLDCART
acronym).
b) Call for medical help (e.g., Call SAMU - 912) and get a defibrillator and
importantly ensure the emergency department is informed of heart attack.
c) Have the person stop what he or she is doing and rest comfortably. This will
ease the heart’s need for oxygen and many people find it easier to breathe
while sitting.
d) Loosen any restrictive or uncomfortable clothing
e) Ask the person if he or she has a history of heart disease. Some people who
have heart disease take prescribed medications for chest pain and you can
assist them taking them (e.g., sublingual Nitroglycerin)
f) Offer aspirin, if not contraindicated to lessen heart attack damage as Aspirin
acts to thin the blood and prevent further clot formation. A dose of 165 - 300
mg dose of Aspirin to be chewed by the victim
g) I feasible:
• Give oxygen if oxygen saturation is <90% or if the patient is short of breath
• Start IV fluids
• Give morphine as indicated e.g., 2 – 5mg if the pain not relieved by
Nitroglycerin
h) Monitor the person closely until emergency medical services personnel arrive.
Note any changes in the person’s appearance (i.e., loss of consciousness) or
behavior and record as well interventions undertaken.
i) Be prepared to perform CPR and use an AED if the person loses consciousness
and stops breathing.
j) Keep a calm and reassuring manner as comforting the person helps reduce
anxiety and ease some of the discomfort
d.2. Intra-hospital care at emergency department (ED)
Once arrived to the hospital, an immediate ED assessment and treatment should
be initiated.
• The assessment should include a brief targeted history and physical
examination; fibrinolytic checklist, especially contraindications
• Keep vital signs and O2 saturation monitoring
• Obtain IV access if not done
• Continue MONA (morphine, oxygen, nitroglycerin, aspirin)
• Obtain and analyze a 12-lead electrocardiograph (ECG)
• Obtain blood sample to get initial serum cardiac marker levels and evaluate
initial electrolyte and coagulation studies
• Obtain chest radiograph
• The definitive management is initiated depending of the outcome of theinvestigation
Self-assessment 5.2.5
1) You suspect a stable angina rather than MI pain in the patient who reports
that his chest pain
a) Is relieved by NTG.
b) Is a sensation of tightness or squeezing.
c) Does not radiate to the neck, back, or arms.
d) Is precipitated by physical or emotional exertion.
2) A patient hospitalized for evaluation of unstable angina has severe
chest pain and calls the nurse. Prioritize the subsequent interventions
from 1 (highest priority) to 6 (lowest priority). The appropriate medical
prescriptions and protocols are available to the nurse.
a) Notify the provider.
b) Obtain a 12-lead ECG.
c) Check the patient’s vital signs.
d) Apply oxygen per nasal cannula.
e) Perform a focused assessment of the chest.
f) Assess pain (OLDCART) and medicate as ordered.
3) Is CPR is the first intervention that should be undertaken in case of heart
attack? Explain your answer.
5.3 Neurological system pathologies
5.3.1 Stroke5.3.1.1 Overview of Stroke
1) Carefully observe the above the above three categories of images and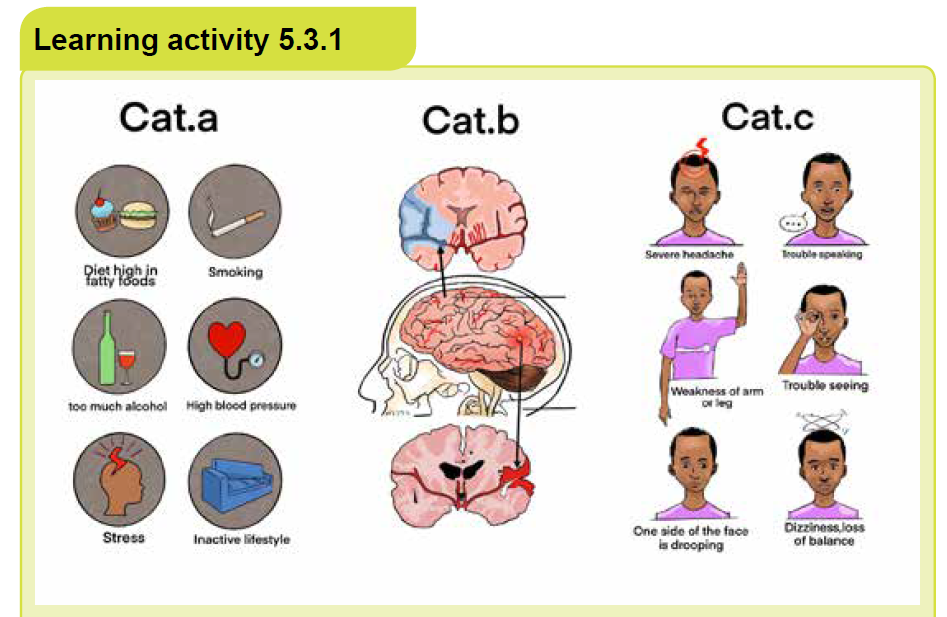
attempt give a general name to each category
2) Try to establish a coherent relationship across these group categories
3) What do you think differenciate the top image from the bottom image ofcategory B in relation to the middle one?
a) Definition of stroke
Stroke also known as Cerebro-Vascular Accident (CVA) or Brain Attack is an
interruption of the blood supply to any part of the brain. is a vascular insult producing
rapid onset of neurological deficit lasting for more than 24 hours, as a result of
inadequate blood flow to a part of the brain or hemorrhage into the brain. Thus, an
insult that results into neurological deficit that resolve within 24 hours is referred to
us as “Transient Ischemic Attack (TIA)”. The severity of the loss of functions varies
according to the location and extent of the brain involved and may involve loss or
impairment of functions such as movement, sensation or emotions.
b) Etiology and pathophysiology of stroke
Two important mechanisms are involved into occurrence of stroke. The blood flow
to a part of the brain is interrupted either by a blocked artery (Ischemic Stroke) orby a ruptured blood vessel in the brain (Hemorrhagic Stroke).
Note that ischemic stroke is the most common and is linked to some risk factors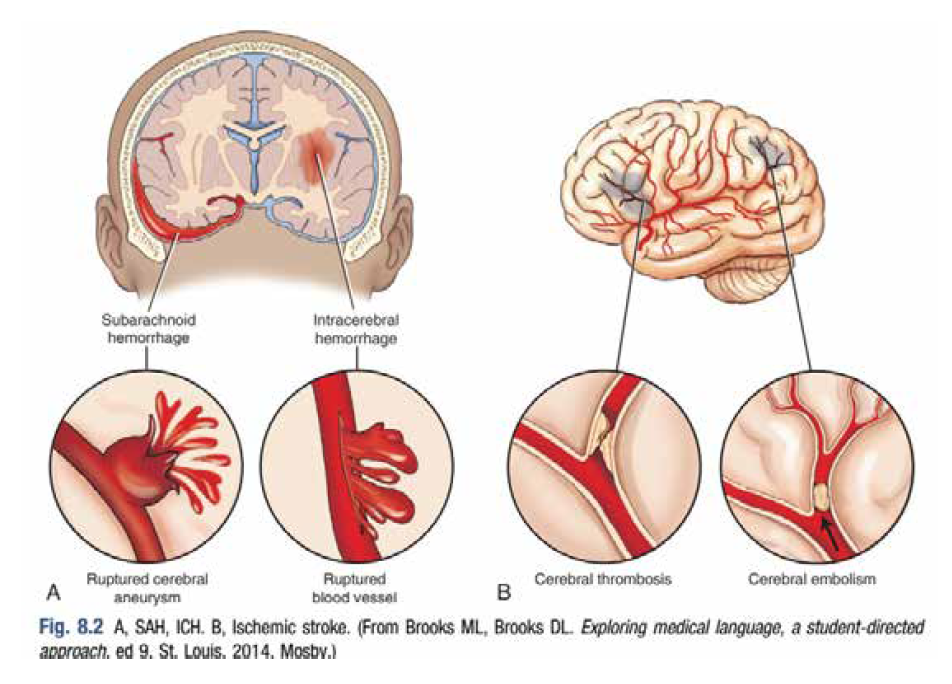
such as increasing age, male sex, family history of vascular disease, hypertension,
smoking, excess alcohol, high cholesterol, diabetes and structural heart (especially
recent myocardial or atrial fibrillation).
c) Sign and symptoms of stroke
Manifestations of a stroke vary depending on the vessel affected and the cerebral
territories it perfuses. They are always sudden in onset and usually multifocal one
sided. Headache may be a sign of impending cerebral hemorrhage or infarction;
however, it is not always present. The most common clinical manifestations include:
• Numbness (paresthesia), weakness (paresis), or loss of motor ability (plegia)
on one side of the body
• Difficulty in swallowing (dysphagia)
• Speech difficulties
• Visual difficulties of inattention or neglect (lack of acknowledgment of one
side of the sensory field), loss of half of a visual field (hemianopsia), double
vision, photophobia
• Altered cognitive abilities and psychological affect
• Dizziness, loss of balance• Self-care deficits.

Self-assessment 5.3
1) You suspect a stable angina rather than MI pain in the patient who reports
that his chest pain
a) Is relieved by NTG.
b) Is a sensation of tightness or squeezing.
c) Does not radiate to the neck, back, or arms.
d) Is precipitated by physical or emotional exertion.
2. A patient hospitalized for evaluation of unstable angina has severe
chest pain and calls the nurse. Prioritize the subsequent interventions
from 1 (highest priority) to 6 (lowest priority). The appropriate medical
prescriptions and protocols are available to the nurse.Perform a focusedassessment of the chest.
a) Notify the provider.
b) Obtain a 12-lead ECG.
c) Check the patient’s vital signs.
d) Apply oxygen per nasal cannula.
e) Perform a focused assessment of the chest.
f) Assess pain (OLDCART) and medicate as ordered.
3. Is CPR is the first intervention that should be undertaken in case of heartattack? Explain your answer.
5.3.2 First Aid in Stroke
The overall goal of stroke care is to minimize brain injury and optimize the individual’s
recovery. The emphases on:
• Rapid recognition of stroke symptoms,
• Early activation and dispatch of Emergency Medical service (EMS)
• Rapid EMS identification, management, and transport (preferably to stroke
center),
• Rapid triage, evaluation, and management in Emergency department (ED)
• Rapid stroke expert decision and therapy selection
• Fibrinolytic therapy• Rapid admission to the stroke unit or critical care unit
i.Pre-hospital
Prehospital providers should take quick and rapid action. The following steps should
be undertaken following DRSABCD approach bearing in mind FAST acronym as
vital to ensuring rapid treatment of a person suffering a stroke. FAST is about:
• FACE – check for facial droop by ask the victim to smile; one side of the face
may not move as well as the other side.
• ARMS – check for arm drift by ask the casualty to hold both arms out with
the palms up, and close their eyes. One arm may not move or drifts down
compared to the other arm.
• SPEECH – check for speech slurred by ask the victim to repeat a phrase
you say. The casualty may slur words, use the incorrect words or is not able
to speak. Also check whether the victim understand you.
• TIME – the time is critical. If you see any of these signs call 912 immediately
(alert the hospital “possible stroke patient”. Ensure as well you have
information regarding the onset of symptoms by asking the casualty, or their
family, friends or bystander.
• Undertake the following as part of initial assessment and stabilization:
• Check and support ABCs vital signs; give oxygen if hypoxemic
• Place the casualty at rest in the semi-sitting position
• Check blood glucose level as hypoglycemia can mimic stroke symptoms
• Obtain iv access and start IV fluid if possible (avoid excess fluids)
• Keep victim close monitoring and be calm and comforting while waiting
victim medical evacuation
• If the casualty becomes unconscious, follow first aid steps for
unconscious victim
• If there is paralysis, position the casualty with the paralyzed side up.
• Keep the victim nil per oral (NPO)
ii.Intra-hospital care at emergency department (ED)
Once arrived to the hospital, an immediate ED assessment and treatment should
be initiated.
• Check ABCs, vital signs; give O2 if hypoxemic
• Start IV fluids if not done in prehospital
• Obtain blood samples and a 12-lead ECG
• Check blood glucose level and correct any hypoglycemia or hyperglycemia
• Perform general neurologic screening assessment including use of specific
stroke assessment scale
• Initiate emergency CT scan or MRI of brain
• Based on assessment and results of investigations the decision is made and
appropriate therapeutic strategies implemented
• Admission to the stroke unit or critical care unit
Self-assessment 5.3.2
1) What does FAST entails with regard to stroke management?2) Why should you keep a stroke victim NPO?
5.3.3 EpilepsyOverview of epilepsy
Observe the above picture and try to figureout what each of them represent then
after attempt to establish any existing relationship.
a) Definition
Epilepsy also known as “Seizure Disorder” is a chronic disorder of the brain
in which there is abnormal, recurring, excessive and self-terminating electrical
discharge from neurons leading to seizures. Epilepsy is characterized by recurring
and unprovoked seizures, thus, a single seizure not sufficient to make a diagnosis
of epilepsy. Seizures occurring solely in association with precipitants (e.g. fever in
young children, metabolic disturbance, alcohol or drug abuse, acute head injury)
are termed acute symptomatic or situation related seizures.
A seizure sometimes called a “convulsion” is a single event of paroxysmal,
synchronous and excessive discharge of neurons in the cerebral cortex manifesting
as a stereotyped disturbance of consciousness, behavior, emotion, motor function
or sensation. An epileptic seizure typically has a sudden onset, lasts seconds to
minutes and usually ceases spontaneously. However, in case of Status epilepticus
there is sustained or recurrent seizures, with failure to regain consciousness between
seizures over 30 minutes. Status epilepticus constitute a medical emergency and
has a mortality rate of 10–15%.
b) Etiology and pathophysiology
Epilepsy is a symptom of numerous disorders but in more than 50% of patients
with epilepsy, no apparent cause is found, in spite of full investigation. It can affect
any person though most common in children and elderly. Seizures are thought
to results from imbalances of excitatory and inhibitory neurotransmitters such
as acetylcholine (ACh) or gamma aminobutyric acid (GABA). Vascular disease
(especially stroke), alcohol abuse, cerebral tumors and head injury are the most
common factors associated with seizures. Other factors associated with seizures
include family history (especially for absence seizure), antenatal and perinatal,
metabolic disorders, sleep deprivation, hypoxia, etc…
c) Signs and symptoms
Since seizures can affect any process your brain coordinates, signs and symptoms
of epilepsy vary across patients and depending of type of seizure. They may include
temporarily confusion, staring spell, jerking, altered mental status, psychological
symptoms such as fear, anxiety. Seizures may cause a person to have convulsions
(general term that people use to describe uncontrollable muscle contractions), but
this is not always the case.
Seizures are either classified as generalized or focalized. Generalized seizures
result from abnormal electrical activity affecting the entire cerebral cortex while
focal or partial seizures affect specific region of the brain. These seizures can
also be categorized as simple or complex depending on how they affect the level
of consciousness. In Simple focal seizures consciousness is retained whereas
consciousness is impaired in complex focal seizures Below is represented signsand symptoms of typical epileptic seizure.
d) Management of epilepsy
The aim of management is preventing or at least reducing the frequency of
seizures through medication and lifestyle modification; and is dependent on the
seizure type and patient. Anticonvulsant drug therapy is usually initiated after a
patient suffers a second unprovoked seizure and the dose is titrated to control
seizures while minimizing side effects. Non-pharmacological management of
epileptic patient involves avoiding activities that would be hazardous if a seizure
were to occur e.g. swimming, operating heavy machinery and driving.
d) Management of epilepsy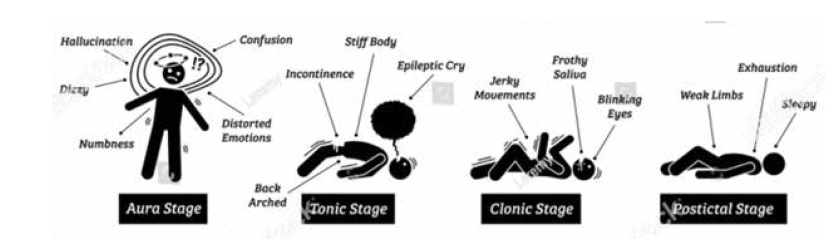
The aim of management is preventing or at least reducing the frequency of
seizures through medication and lifestyle modification; and is dependent on the
seizure type and patient. Anticonvulsant drug therapy is usually initiated after a
patient suffers a second unprovoked seizure and the dose is titrated to control
seizures while minimizing side effects. Non-pharmacological management of
epileptic patient involves avoiding activities that would be hazardous if a seizure
were to occur e.g. swimming, operating heavy machinery and driving.
Self-assessment 5.3.3.
1) Differentiate seizures from convulsions.
2) Who can get epilepsy?3) Enumerate at least one symptom of epileptic seizure on different stage
5.3.2.2 First aid for epilepsyLearning activity 5.3.4

With reference to image above
1. What type of seizure do you think is illustrated there?
2. What would you do to help through?
First aid interventions should include the following:
• Protect the patient from injury
• Manage the seizure or convulsion
• Manage the “After the seizure”
• Advise for Aftercare follow-up
Use the DRSABCD approach and:
• Keep other people out of the way.
• Check the immediate area for hazards, clear hard or sharp objects away
from the person.
• Look at the watch at the start of the seizure, to time its length
• Don’t try to hold the victim down or stop the movements.
• Place the victim on the floor so he/she do not fall and hurt him/herself
• Place the person on the side, if they have food or fluid in the mouth, roll him/
her onto the side immediately to help keep the airway clear so he/she can
breathe easier.
• Keep bystanders clear and reassure them that the seizure will end soon.
• Place something soft and flat under the head such a good soft pillow
• Loose or remove anything around the patient neck, such as a tie or a
necklace
• Remove glasses
• Protect the person from injuries.
• Keep the person safe until the seizure stops out at its self
• As soon as the seizure ends, quickly put the patient in safety recovery
position
• Cover the patient lightly with a coat or blanket.
• Check that normal breathing has resumed.
• Allow the patient to sleep until fully recovered, but check for a response
every few minutes.
• Stay with the person after the seizure stops
• If the patient does not wake up within 10 minutes, is not breathing well, or it
is the first seizure – call for an ambulance (SAMU – 912)
• Stay calm all the time.
• Do not restrain or put anything in the mouth
• Clear area around
• Reassure the person until he/she totally recovers
• After seizure ends, help the person sit in a safe place.
• If the patient has limited walking or standing ability, or is pregnant, has
cardio-respiratory conditions…. ask for help and put him in a rest position.
• If the seizure last more than five minutes, Breathing or consciousness doesn’t
return after the seizure stops, a second seizure follows immediately, if the
patient has high fever, the patient is pregnant, diabetic, the patient injured
her/himself during the seizure don’t wake up the person, call for help
• The medications for epilepsy are incredibly effective. More than half of the
cases are seizure-free after their first medication. check that any prescribed
medication is adequate Give the prescribed medication.
• Advise the patient not to drive. Try to arrange for someone to be with the
patient until he is safely home or in the ward.
• Advise the patient to report the seizure
• Advise the patient to continue taking anti-seizure medication.
• If the patient is known to have epilepsy, there is no need for medical aid or
an ambulance unless the seizure lasted more than 5 minutes or a second
seizure followed
• Check for any injuries and apply necessary first aid
• Reassure the patient as full consciousness is restored.
• Advise the patient not to drive. Try to arrange for someone to be with the
patient until he is safely home or in the ward.
Be aware about possible complications:
• Having a seizure at certain times can lead to circumstances that are
dangerous to the patient or others.
• Falling: fall during a seizure can injure the head or break a bone.
• Drowning. An epileptic person 13-19 times more likely to drown while
swimming or bathing.
• Car accidents. A seizure that causes either loss of awareness or control
can be dangerous if the patient is driving a car or operating other equipment.
• Pregnancy complications. Seizures during pregnancy pose dangers to
both mother and baby, and certain anti-epileptic medications increase the
risk of birth defects.
• Emotional health issues. People with epilepsy are more likely to have
psychological problems, especially depression, anxiety, and suicidal
thoughts and behaviors. Problems may be a result of difficulties dealing with
the condition itself as well as medication side effects, but even people with
well-controlled epilepsy are at increased risk.
Uncommon, complications but may happen, such as:
• Status epilepticus. This condition occurs if frequent recurrent seizures
without regaining full consciousness in between them. People with status
epilepticus have an increased risk of permanent brain damage and death.
• Sudden unexpected death in epilepsy (SUDEP). People with epilepsy
also have a small risk of sudden unexpected death. The cause is unknown.
This occurs to People with frequent tonic-clonic seizures or whose seizures
aren’t controlled by medications.
Nursing care in this situation should focus on:
• Accurate assessments and regular monitoring (immediate attention to
ABCDE and blood glucose monitoring: ongoing monitoring of neurological
status, vital signs and seizures)
• Symptom control and management (IV line and medications)
• Communication with the healthcare team, patient and family
• Risk assessment and management (safety, e.g. padded bed rails;maintenance of secure IV line if continual seizures)
Self-assessment 5.3.4
1) What is the main role of a first aider in case of epilepsy seizure?
2) What can you do if the seizures last more than five minutes?
3) Epilepsy seizure can lead to some complications. Enumerate at least four
of them
4) What is the meaning of Status epilepticus?
5) In skill lab perform first aid interventions for:
a) A client with focal seizuresb) A client in tonic-clonic seizures
a. A noise a person makes while breathing.
b. The way a person breathes when they are scared.
c. An illness that causes the airways to swell and get tight.
d. Something that a person gets from running too much.
6) What can trigger an asthma attack?
a) Being allergic to your cat.
b) Bing near someone who is smoking.
c) Being inside a room that is dusty.
d) All of the above.
7) What is the primary concern when assisting a person having a seizure?
a) Holding them still
b) Keeping them safe from harm
c) Placing them flat on their back
d) Stopping seizure
8) A 20-year-old person is having suddenly a seizure and make movements
and have froth around the mouth. The first best action to do by the first
aider is:
a) Keep other people out of the way
b) Stopping seizure
c) Wakeup the patient
d) Give medication
9) Stroke is a vascular insult producing rapid onset of neurological deficit
lasting for more than 24 hours; manifestations of a stroke vary depending
on:
a) Personality of patient
b) The etiology of stroke
c) The affected body system
d) The vessel affected and the cerebral territories it perfuses
0) Acute Respiratory Distress Syndrome does not occur as a primary
process but may follow a number of diverse conditions producing direct
or indirect lung injury; the direct injuries leading to ARDS are the following
except one:
a) Aspiration, pneumonia
b) Fat embolism
c) Excessive blood transfusion
d) Pulmonary contusion
11) In healthy adults the average systolic pressure is less than 120 mmHg
and the average diastolic pressure is less than 80 mmHg. The difference
between the systolic and diastolic pressure, known as the pulse pressure
is normally ranging:
a) Between 30 and 40 mmHg
b) Between 20 and 40 mmHg
c) Between 30 and 50 mmHg
d) Between 20 and 30 mmHg
12) Rank the following causes of stroke from the most common (1) to least
common (3):
a) Cerebral hemorrhage
b) Cerebral ischemia
c) Subarachnoid hemorrhage
13) Order the following immediate interventions to be implemented when
hypertensive crisis is suspected?
a) Elevate the head of the bed to approximately 30 – 450
b) Notify the physician
c) Administer supplemental O2
d) Assess BP in both arms
e) Perform a focus assessment
f) Keep close monitoring including assessing changes in cardiac rhythm
g) Anticipate and prepare to get ready to implement physician orders
14) Enumerate at least three advises to give to the patient/family after a crisis
of seizure.
15) How can you help if someone is having an asthma attack?
16) Both transient ischemic attack (TIA) and cerebral vascular accidents
(CVA) are vascular insult to brain tissue. Contrast these two conditions?
17) Through which mechanism does stroke occur?
18) List five steps that are important when helping someone with heart
problems.
19) A 67 years old is suffering from ischemic stroke that affects his lefttemporal area; what functions are likely to be affected?
