UNIT 3 BASIC LABORATORY INVESTIGATIONS FOR COMMON CONDITIONS
Key unit competence
Perform basic Laboratory investigations for common conditions
Introductory activity 3
The following pictures illustrate different procedures. Critically analyze them andrespond to the following questions
1. Describe the procedure you think is being done in picture A and picture B
2. Which procedure do you think is invasive and why do you think so.
3. With clear rationale explain the procedure you think can produce results
as quick as possible between A and B
4. What do you think the technique performed will help the casualty
3.1. BASIC LABORATORY INVESTIGATIONS FOR
COMMON CONDITIONS
Learning activity 3.1
Search the book of nursing laboratory and diagnostic investigations then
define and explain the rationale for each of the following test.
a) Rapid disgnostic test
b) Glycemia test
c) Glucosuria test
d) Albuminuria test
3.1.1. Rapid Diagnostic Test for Malaria (RDT)
Malaria is among serious threat killing many people worldwide. Since infection
with Plasmodium parasites causes clinical presentation indistinguishable from
other fever-causing pathogens, rapid, accurate diagnosis is a crucial component of
effective case management.
Malaria rapid diagnostic tests (RDTs) assist in the diagnosis of malaria by detecting
evidence of malaria parasites (antigens) in human blood. These tests require a
drop of peripheral blood, normally collected from a finger or heel prick. Visual readouts
are available typically within 20 minutes or less.
Malaria rapid diagnostic test are frequently used in high malaria endemic area
such as sub-Saharan Africa and in low to moderate transmission area such as Asia
and South America, where maintenance of capacity for malaria microscopy and its
quality control are obvious burdens for malaria control programs.a) Parts of a malaria rapid diagnostic devices
b) Interpretation of RDT for Malaria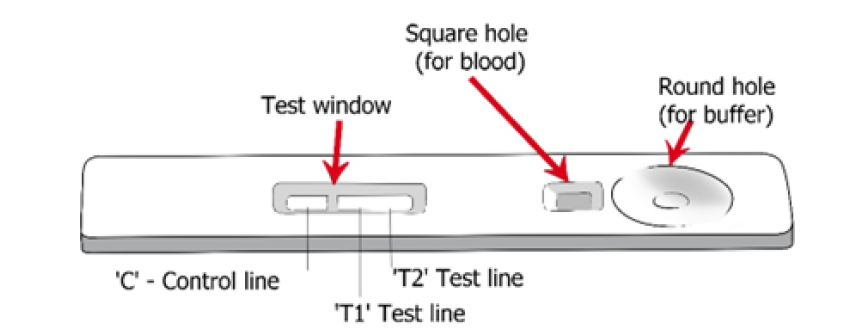
In interpreting rapid diagnostic test for malaria, one of the three possible outcome
should be revealed.
When the device shows the appearance of a line near T and C means that there
evidence of plasmodium parasites (Positive). Line near C and no line near T
means that there is no evidence of parasites (Negative). Line near T and or no line
means that the results is invalid. A studies assessing the sensitivity and specificity
of two different brand of RDT for malaria used Rwanda has demonstrated that the
sensitivity of RDT for malaria were around (80.2%-89.5%) while the specificity was
(86.2 %-94.3).
Such interpretation can be challenging, especially when compared with microscopy
exam. There are instances where RDT will be positive but no parasites will be seen
on microscopy, conversely, there are instances where RDT will be negative but
microscopy will detect parasites in the blood. There are instances too, when RDT
will be positive but there is no clinical malaria or, the fever is not caused by malaria.
Despite the fact that RDTs are recommended as a means of laboratory confirmation
of malaria before the prescription of antimalarial, the interpretation of test results
should be done with caution to ensure better malaria case management.Table illustrating possible Malaria Rapid diagnostic results
3.1.2 Glycemia test
Glycemia test also referred to as blood glucose test is a test used to measure the
level of glucose within the blood, again it is used to find out if the blood sugar levels
are in the healthy range.
The highlighted materials will be used in measuring glycaemia: Glucose meter
or glucometer measures how much sugar is in the blood sample. Test Strips,
Lancets, and Lancet Device: each small plastic strip contains chemicals that
convert the sugar in the blood into an electric current that the meter can read. It is
used by putting a test strip into the meter. Prick the side of the fingertip with a small
needle called a lancet. The results will be visible on glucometer machine within 1
minute.
If the level of sugar in the blood is high it will be referred as hyperglycemia, and
hypoglycemia for low level. Blood glucose test is often used to help diagnose and
monitor diabetes. People with diabetes require regular monitoring of their blood
glucose to help them achieve as close to normal blood glucose levels as possible for
as much of the time as possible. The benefits of maintaining a blood glucose level
that is consistently within the normal range will reduce the short-term, potentially
life-threatening complications of hypoglycemia as well as the occurrence rate and
severity of the long-term complications of hyperglycemia.
a) Fasting glucose Level
We say fasting glucose when the blood sample is obtained after 8 hours of fasting.
In non-diabetic patient, glucose levels vary between 70 mg/dl to 110mg/dl (4.0
to 5.4 mmol/L). In diabetic patient glucose level is more above110mg/dl but less
126mg/dl or 7.0 mmol/L.
b) Random glucose level
Random glucose level refers to the glucose level checked without regard to the last
meal. It is useful for people who need a speedy diagnosis, such as those with type 1
diabetes who require medication as a matter of emergency. Diabetes is diagnosed
if random glucose level is above 200 mg/ dl or above 11.1 mmol/l with symptoms
of diabetes.
c) Principles of measuring glycemia
The measurement of glucose is one of the longest established and most frequently
performed tests in the clinical biochemistry laboratory. Although conventional
laboratory techniques measure blood glucose as concentration in plasma or whole
blood, not that direct-reading electrode systems measure it as molality in mmol/kg
water, which is numerically greater, but results are often factorized and expressed,
e.g. as plasma glucose concentration.
In measuring glycemia as an associate nurse, you need to know that glycemia can
measured by two main methods. A blood drop sample is usually collected from a
fingertip prick. Alternatively, the glycaemia may be measured by taking the blood
from the vein.
Ensure that the patient has fasted for at least 8 hours in case of fasting blood
glucose. The patient should not eat or drink anything other than water for at least 8
hours before the blood sample is taken.
If random blood glucose, the glycemia is taken regardless of when the patient
last ate. In this case, several random measurements may be taken throughout
the day to allow for identification of fluctuations in blood glucose levels. When the
fluctuations vary widely, this may mean a problem.
A 2-hour postprandial blood sugar test measures blood sugar exactly 2 hours
after the patient starts eating a meal. This is useful for diabetic patients who may
need to inquire about the efficacy of insulin being taken, and if the right amount of
insulin is being taken with meals.
Sites for rapid blood glucose checking may be alternated and apart from pricking
the fingers, there is a way to prick the earlobe, heel, forearm or palm. Alternate
site testing provides similar results to finger-prick testing, especially in the fasting
and two-hour post meal times. Using alternate sites may be less painful but may
need a deeper lance. Ensure that the blood glucose machine and its equipment
allow the alternate sites. It is recommended to respect principles of asepsis in
measuring blood sugar level.
3.1.3. Urine test
Urine tests sometime referred to as urinalysis are laboratory investigation done
to examine the physical and chemical properties of urine and its microscopic
appearance to aid in medical diagnosis of different health conditions. Urine test is a
simple and noninvasive test that provides valuable information. An associate nurse
should be able to perform urine test using urine strips and analyses glucose and
albumin in it. After doing the technique of urine collection, Results are obtained by
direct comparison of the color blocks printed on the bottle label. The color blocks
represent nominal values; actual values will vary around the nominal values.
a) Albuminuria
Albumin is a protein found in human blood. Albumin help to maintain blood volume
and pressure. The action of the kidney is to filter the blood to remove waste products
and these filters (known as glomeruli) prevent large molecules, such as albumin,
from passing through. If these filters are damaged, albumin passes from the blood
in to the urine. If kidneys are damaged and albumin leaks into the urine in very
small amounts it will be referred as microalbuminuria. As kidney function declines
the amount of albumin in the urine increases, and larger or ‘macro’ amounts of
albumin may be present. This is known as macroalbuminuria.
In normal person, albumin is not excreted in the urine. Increase level of albumin
may cause major health risk therefore detection of albumin in urine is essential for
diagnosis albuminuria related diseases. Several methods to detect albumin in the
urine have been identified including calorimetry, radioimmunoassay, immuno enzymatic
assay, turbidimetry, and dipsticks tests. Our focus here will be dipsticks test
only. The strips technique is simple, cost effective and can give quicker results.
The albumin strip technique can be used even in rural areas where sophisticatedlaboratory testing facilities are not available.
Interpreting albumin results test is not
difficult. Results are obtained by direct
comparison of the color blocks printed on
the bottle label. The color blocks represent
nominal values; actual values will vary
around the nominal values.
False positive results may be obtained
with highly alkaline urine. Contamination
of the urine specimen with quarternary
ammonium compounds may also produce
false positive results.
In 24-hour urine, 1.0-14.0 mg/dl of protein may be excreted by the normal kidney.
A color matching any color block greater than trace indicates significant proteinuria.
For urine with high specific gravity, the test area may most closely match the trace
color block even though only normal concentrations of protein are present. Clinical
judgment is needed to evaluate the significance of trace results.
a) Glycosuria
Glycosuria meaning glucose in the urine, results from the glomerular filtration of
more glucose than the renal tubule can absorb. It occurs in all normal individuals
in amounts up to 25 mg/dl in random flesh urine. Abnormally increased glycosuria,
results from either an elevated plasma glucose, an impaired renal glucose absorptive
capacity, or both.
The plasma glucose concentration of 25mg/dl indicating glucosuria is called
the renal threshold for glucose. Its value is variable, and deviations occur both above
and below the commonly accepted «normal» threshold of 180 mg/dl. In diabetic
patients, the value is reported to vary from 54 to 300 mg/dl. Although glucosuria
greater than 25 mg/dl is considered pathologic, many commercial urine tests for
glucosuria that are available to patients fail to detect glucosuria until it reaches a
level of 50–250 mg/dl.
Techniques for measuring glucosuria are based upon either glucose oxidase
(specific for glucose) or copper sulfate reduction. Strip test are oxidase base and is
our focus in this unit. The sensitivity of commercial clinical “strip” methods can be10–15 mg/dl, although 50 mg/dl is usually detected.
The test of glucosuria using strips is based
on a double sequential enzyme reaction.
One enzyme, glucose oxidase, catalyzes
the formation of gluconic acid and hydrogen
peroxide from the oxidation of glucose. A
second enzyme, peroxidase, catalyzes the
reaction of hydrogen peroxide with potassium
iodide chromogen to oxidize the chromogen
to colors ranging from blue-green to greenishbrownthrough brown and dark brown.
Self-assessment 3.1
1) Explain how does rapid diagnostic test for malaria work?
2) How accurate are malaria rapid test?
3) In human body glucose level can be tested from the peripheral capillaries
or from the urine. Discuss on normal ranges from each method and onthe main causes of deviation from normal ranges in each method?
3.2. Techniques of performing basic laboratory investigations
for common conditions
3.2.1.The technique of performing Rapid Diagnostic Test for
malaria
Learning activity 3.2.1
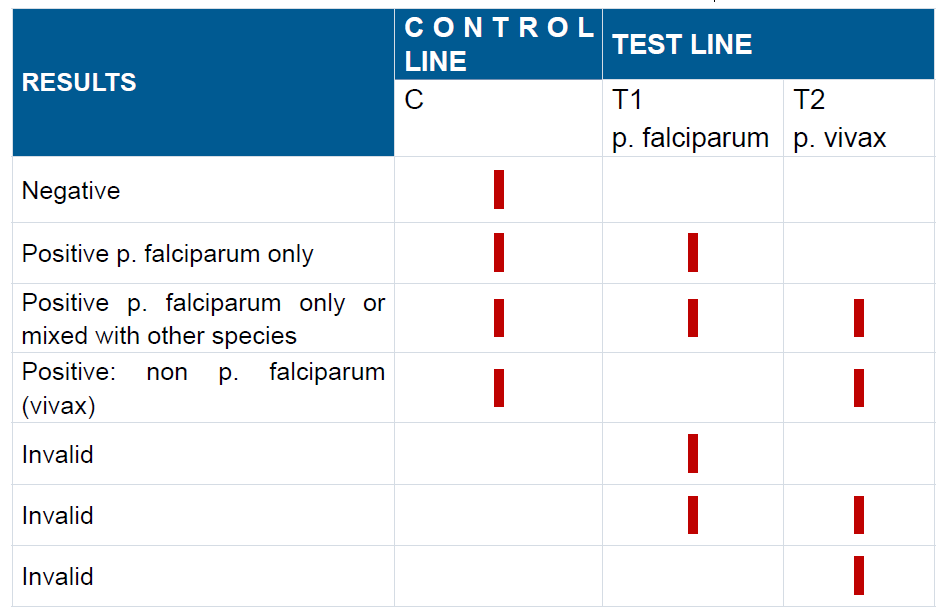
The following picture illustrate the steps of rapid diagnostic test for malaria. Byfollowing the steps as illustrated in the image:
1) Perform the technique of rapid diagnostic test on the mannequin in the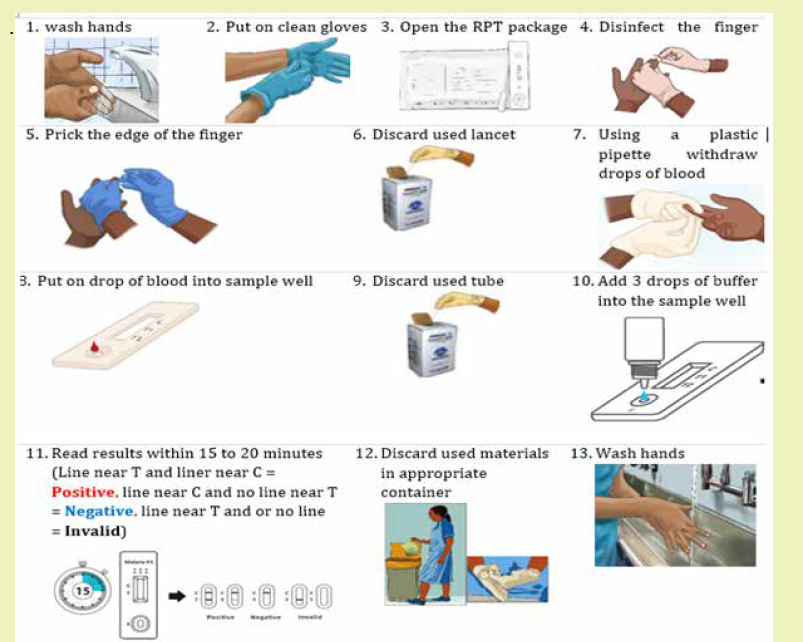
skills lab
2) What do you think would happen if you start the technique without washing
your hands?
3) After pricking the finger with a lancet it should be thrown in shaft box.
Discuss why it should not be thrown in the dustbin
4) In step 4, it is stated that the finger should be dried. What do you think as
the main reason?
a) Materials
1) Gloves
2) RDT kit
3) Safety box
4) Dustbin
5) Timerb) Procedure of Rapid diagnostic test for malaria
Self-assessment 3.2.1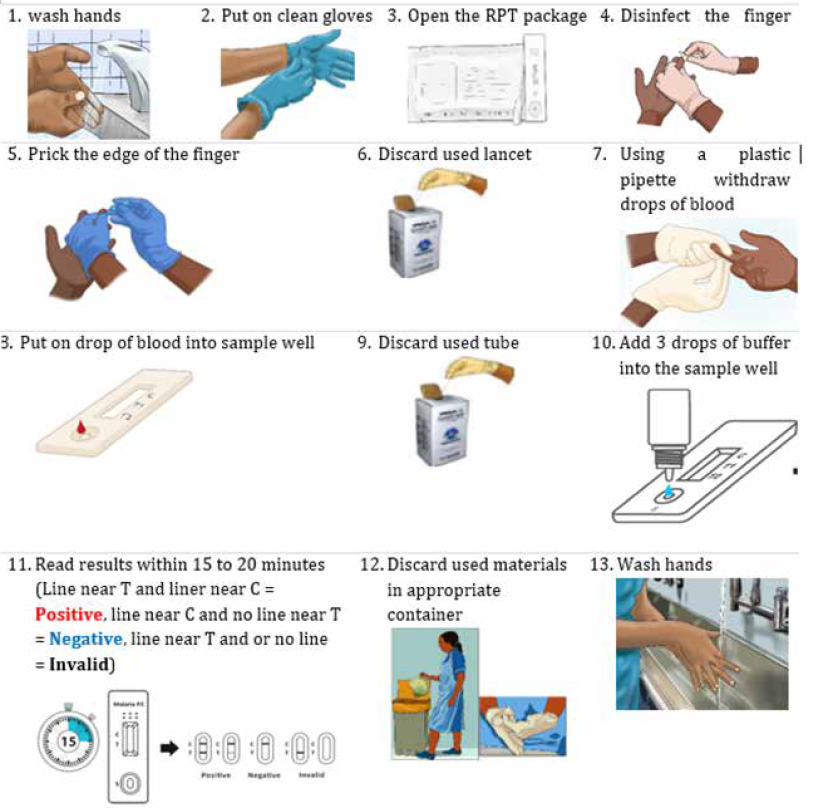
After learning the technique of rapid diagnostic test for malaria make groups of
two then go in the skills lab then screen malaria on each other using RDT. Make
sure to follow steps as you learnt them.
3.2.2.The technique of performing urine test (Albumin, Glucose)
In pairs of two and perform urine test for albumin and glucose on each other
using urine dipstrip available in the simulation lab.
The Urine must be tested within a few hours of voiding as urinary constituents can
become unstable and may affect test results.
a) Materials
1) Package insert
2) Strips
3) Specimen container
4) Glovers
5) Timeb) Procedure of urine test (Glucose and Albumin)

Self-assessment 3.2.2
The following picture illustrate a urine test done using dipsticks on two different
patients (Case A and B). compare the test results in case A and case B to the
reference scale and explain whether the patient’s glucose and albumin level arein normal range or not
3.2.3 Techniques of performing Glycemia test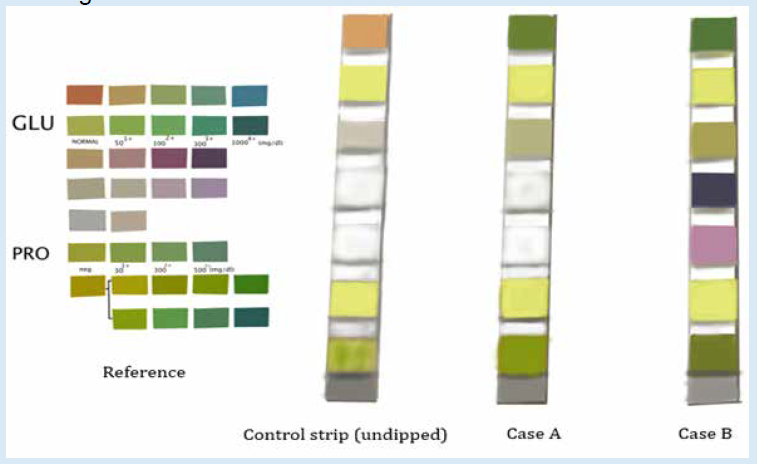
Learning activity 3.2.3
A blood glucose test is a blood test that check if patient have high glucose
level in the blood. The following materials are used in performing glycemia test:
glucometer, test strips, alcohol swab, lancet, gloves, cotton wool/gauze, sharpsbox or safety box
1) Modeling from the illustrate above perform the technique of glycemia test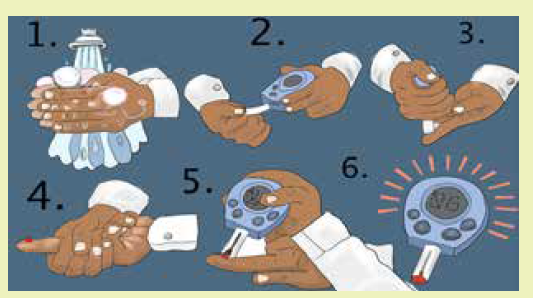
on the mannequin in the skills lab
2) The normal threshold of fasting glucose level and random glucose level
are different. Discuss and differentiate the fasting glucose level from therandom glucose level.
The technique of glycemia test using strips
a) Materials for glycemia test
Blood glucose monitor
1) Test strips (check that they are in
date and have not been exposed
to the air)
2) Alcohol swab
3) Single-use safety lancets or
lancing device,
4) Gloves,
5) Cotton wool/gauze,
6) Sharps box or safety box,
7) Control solution for calibration
b) Steps for Glycemia check
1) Ask the patient to sit down and explain what you are going to do.2) Wash the hands and put on gloves.
3) Choose the site for the blood sample: usually the side of a finger, but the
arm or thigh may be used (change the site used if frequent measurements
are needed).
4) Use an alcohol swab to clean the site and let the alcohol dry.
5) Insert the test strip into the monitor, following the instructions
6) Use a single-use lancet or a lancing device to draw blood and dispose of
it in a sharps container.
7) Don’t go deeper than necessary
8) Apply the blood to the testing strip in the correct way: some strips need
the blood drop to be over the whole of the test pad and some suck up the
blood directly from the site of the bleeding.
9) Place the gauze over the site and hold it there, or let the patient hold it
there until the bleeding stops.
10) Read and record the result, reporting and/or responding to abnormal
readings.
11) Tell the patient what the result is, explain it
12) Thank the patient
13) Dispose of all used equipment safely
14) Wash the handsGraphical illustration of the technique of glycemia test
Self-assessment 3.2.3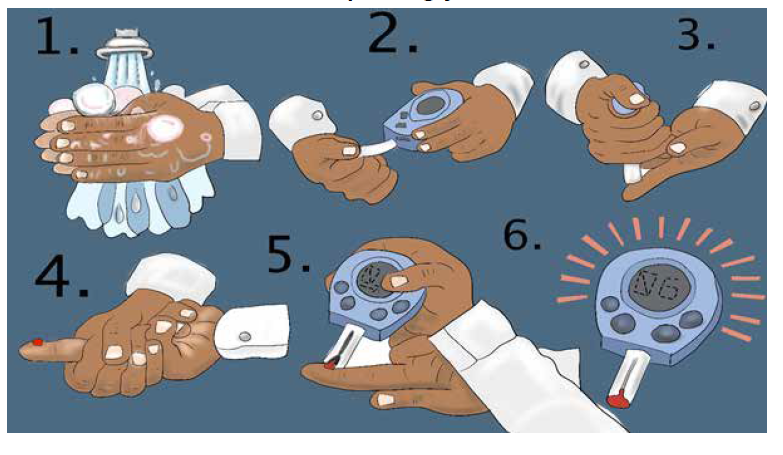
After learning the technique of screening glycemia group yourself in pair. go in
the skills lab, prepare materials for glycemia test and test each other by followingthe checklist of the technique.
End unit assessment 3
1) Is it recommended to use one RDT devise on more than one person?
a) Yes
b) No
2) Abnormally increased glycosuria, results from elevated plasma glucose,
or from impaired renal glucose absorptive capacity.
a) Yes
b) No
3) Which of the following confirmed values meet the diagnostic threshold for
diabetes?
a) Random glucose > 160 md/dl
b) Fasting blood glucose equal to 140 md/dl
c) 2 hrs post prandial glucose ≥ to 126 mg/dl
d) Fasting blood glucose ≥ 126 md/dl
4) Why is it advised to write down the time after adding the buffer in the RDT
and not after adding the blood?
5) The following 4 pictures illustrate real malaria rapid diagnostic results
tested from 4 different patients, observe them carefully and explain which
one reflect a positive malaria result, a negative malaria result and amalaria invalid results.
6) Mr. WS comes at the health center where you work as an associated
nurse. In consultation room he tells you that he is urinating a lot often at
night, is very thirsty, and very hungry. He tells you that before he enters in
your consultation room he took 2 bottle of Fanta. You decided immediately
to rule out if his blood glucose level is within normal range or not.
a) In a stepwise approach describe how you would perform the technique of
glycemia test
b) After the test you found that his glycemia is 198 md/dl. Interpret such
finding and explain whether it is normal or not
7) Albumin is a protein found in the bloodstream of mammalians, explainwhat you think as the main cause for it to be found in urine?
