Unit 12 Regulation of Glucose
Key Unit Competence
To be able to explain the mechanism of the regulation of blood glucose level.
LEARNING OBJECTIVES
At the end of this unit, the learner will be able to:
• Describe the role of hormones in sugar regulation.
• Describe the detailed structure of a liver lobule and the Islet of Langerhans.
• Explain the negative feedback mechanism in the process of blood glucose control.
• Discuss the causes and effects of blood sugar imbalances in the body.
• Appreciate the importance of a controlled diet for diabetics.
• Assist diabetics and people having hypertension in coping with their situation.
• Relate the structure of the liver and the pancreas to their functions.
• Relate the microstructure of the liver and the pancreas to sugar regulation.
• Describe the functions of the liver and pancreas in the regulation of glucose in the body.
• Describe the three main stages of cell signalling in control of blood glucose by adrenaline
as follows:
♦ Hormone-receptor interaction at the cell surface.
♦ Formation of cyclic AMP that binds to kinase protein.
♦ An enzyme cascade involving activation of enzymes by phosphorylation to amplify the
signal.
• Make research using internet or articles on the role of adrenaline in the control of blood
sugar.
• Explain the principles of the operation of dip sticks and biosensors for quantitative
measurements of glucose in the blood and urine.• Explain how urine analysis is used in diagnosis with reference to glucose, protein and ketones.
INTRODUCTORY ACTIVITY
The human body maintains constant different substances in the blood, a process called
homeostasis. The figures below show different organs involved in the regulation of bloodglucose level in the body
Observe the illustations X and Y above and answer to the questions that follow
a)What are the parts represented by letters A,B and C on the illustration X ?
b) All the organs shown in the illustration X are involved in the digestion of food.
What are the functions of A and B in the digestion
c) What are the organs involved in the regulation of blood level on the illustration X?
In which way does each organ state help in this regulation
d) The illustration Y shows the regulation of blood glucose level. What does the letters
A,,B and C show in this regulation
e) Alpha and beta cells are responsible for producing the hormones that are involved in
the regulation of blood glucose level. Which organ on the illustration Y produces these
hormones
f) Compare the mechanism of working of organs A and B in the regulation of bloodglucose level
12.1 IMPORTANCE OF GLUCOSE
ACTIVITY 1
Visit a nearby hospital to see the patients.
You will notice many patients lying on the bed with a bottle
hanging from a stand by the side of their bed as shown in the
picture.
Ask the doctor, what is inside the bottle and why is it given to the
patients?
Record the answer.
Note: In the hospital, patients are generally given glucose by
drip instead of food because, the drip directly deposits the
glucose into the blood stream and hence the body cells get it in matter of minutes, but if it is
given through food, the glucose’s energy would reach the body parts only after the digestionprocess and this will take a longer time.
Glucose is one of the most important carbohydrates molecules in our body. Body requires
glucose to carry out some of its most important functions. Glucose is synthesized in green
plants, from carbon dioxide, CO2 and water, H2O with the help of energy from sunlight. This
process is known as photosynthesis. The reverse of the photosynthesis reaction i.e., breakdown
of glucose in the presence of oxygen to form carbon dioxide and water releasing the energy, is
the main source of power for all the living organisms. The excess glucose in plants is stored inthe form of starch which serves as foods for various animals.
12.1.1 Glucose as Energy Source
Almost 80 per cent of carbohydrates in our food are converted to glucose during digestion in the
alimentary canal. Fructose and galactose is the other main product of carbohydrates digestion.
After absorption from the alimentary tract, fructose and galactose are converted into glucose
in the liver. And therefore, glucose constitutes more than 95 per cent of all the carbohydrates
circulating in the blood.
Body cells require glucose continuously for its various metabolic activities. These cells directly
absorbed glucose from the blood. Once inside the cells, glucose combines with a phosphate moiety
to form Glucose-6-phosphate with the help of enzyme glucokinase in liver and hexokinase in
most other cells. This phosphorylation reaction is irreversible and helps to retain the glucose
inside the cells. However, in liver cells, renal tubular epithelial cells and intestinal epithelialcells, an enzyme glucose phosphatase converts the glucose-6-phosphate back to glucose.
Complete oxidation of one molecule of glucose into carbon dioxide and water inside the cells
produce as many as 38 molecules of ATP (2 from glycolysis, 2 from Krebs cycle and 34 fromoxidative phosphorylation).
12.1.2 Glucose as Structural Component
As we discussed above, glucose is the main source of energy in all the living cells. Besides
being regarded as the universal fuel, glucose also acts as the source of carbon for all the
carbon containing compounds of the body. For example, ribose, a pentose monosaccharides
used in the synthesis of nucleotides and nucleic acids is synthesized from glucose through
Pentose Phosphate Pathway (PPP). Other important compounds include, glycoprotein, a
protein with oligosaccharide chains (glycans) covalently attached to their polypeptide side
chain; proteoglycans, a special class of glycoproteins which contain about 95% polysaccharide
(glycosaminoglycans) and 5% protein and various other polysaccharides like cellulose, chitin,
glycogen etc.
Glycoproteins are integral membrane proteins which play an important role in the cell-cell
interactions. For example, antigen-antibody interaction in blood-type compatibility is mediated
by glycoproteins which determine the blood type of the individual. Proteoglycans, on the otherhand are major components of extracellular matrices.
12.1.3 Glycogen
Glycogen is a homopolymer of glucose in which each molecule is linked to each other by
1 → 4 glycosidic bond and branching through 1 → 6 linkages. It is synthesized in the liver
cells. The process of biosynthesis of glycogen from glucose with the help of enzyme glycogen
synthase is known as glycogenesis. In response to decrease in blood glucose concentration,
glycogen breaks down to glucose-1-phosphate and glucose in the liver and muscle. This
process is known as glycogenolysis. The enzyme glycogen phosphorylase removes the
glucose residue sequentially from the glycogen to yield glucose-6-phosphate. Other enzymes,
glucan transferase and glucosidase help in breaking the branch forming α (1→ 6) glycosidic
bonds of the glycogen molecule. The overall final product of the glycogenolysis is glucose-
6-phosphate which is converted back to glucose by glucose phosphatase and release intothe blood stream.
12.2 ROLE OF LIVER AND PANCREAS IN GLUCOSE REGULATION
ACTIVITY 2
Discuss functions of various organs of our body.
Note down the organ and its functions which helps in the regulation of blood glucose level.Find the particular organ(s) which has/have the major role in glucose metabolism.
Our body maintains a narrow range of glucose concentration in the blood between
70 mg/dL to 130 mg/dL which may increase upto 180 mg/dL after a meal containing high
amount of carbohydrates. The hormones responsible for the regulation of blood sugar level—
insulin and glucagon are secreted by the pancreas. The excess glucose in our blood is converted
into glycogen in the liver. Therefore, pancreas and liver play a vital role in the regulation ofblood sugar concentration.
12.2.1 Role of Liver in Glucose Regulation
The liver is the largest internal solid organ in the body second to the skin as the largest organ
overall. It performs various functions in our body, including synthesis and storage of proteins
and fats, carbohydrates metabolism, formation and secretion of bile, detoxification and excretion
of potentially harmful compounds. Liver contains two main cell types: Kupffer cells andHepatocytes.
1. Kupffer cells are a type of macrophage that capture and break down old, worn out red
blood cells passing through liver sinusoids.
2. Hepatocytes are cuboidal epithelial cells that line the sinusoids and make up the majority
of cells in the liver. Hepatocytes perform most of the liver’s functions—metabolism,
storage, digestion, and bile production.
Hepatocytes cells contain various enzymes which help in the regulation of blood glucose.These are:
1. Glycogen synthase; responsible for glycogen biosynthesis (Glycogenesis). When the
concentration of glucose in the blood increases beyond the normal value, the excessglucose is converted to glycogen in the liver with the help of enzyme glycogen synthase.
2. Glycogen phosphorylase; responsible for breaking down of glycogen (Glycogenolysis).
When the blood glucose level drops, the enzyme glycogen phosphorylase convert glycogen
to glucose-6-phosphate. Other two enzymes, glucan transferase and glucosidase also helpin glycogenolysis.
3. Glucose phosphatase; responsible for conversion of glucose-6-phosphate to glucose in
the liver. Glucose is then released into the blood stream, thereby increasing the bloodglucose level
12.2.2 Role of Pancreas in Glucose Regulation
Pancreas is the most important endocrine organ for the regulation of blood glucose. It
secretes insulin and glucagon, the two main hormones responsible for the regulation of
blood glucose.
1. Insulin: When the blood glucose concentration increases rapidly, for example after a
meal with high carbohydrates content, pancreas secretes insulin hormone into the blood
stream. Insulin binds to its receptors and increases the rate of glucose uptake, storage
and utilization by almost all tissues of the body resulting in lowering of blood glucose
level. Besides, insulin also stimulates glycogenesis, lipid and proteins biosynthesis which
helps in decreasing blood glucose concentration.
2. Glucagon: In response to decrease in blood glucose concentration, pancreas secretes
glucagon which activates the enzyme glycogen phosphorylase responsible for degradation
of glycogen to glucose-6-phosphate. Glucose-6-phosphate is then dephosphorylated to
form glucose and finally released into the blood stream thereby increasing the blood
glucose level. Glucagon also stimulates gluconeogenesis i.e., biosynthesis of glucosefrom non-carbohydrate compounds like pyruvate and amino acids.
12.3 DETAILED STRUCTURE OF LIVER LOBULE AND ISLET OFLANGERHANS
ACTIVITY 3
Observe permanent slides of transverse section of liver and pancreas under the light microscope
in low magnification followed by higher magnification.
Observe the liver lobules and islet of Langerhans and draw your observation on your record.
Discuss the structure and relate the observed structure with the function of liver and
pancreas.
Note: Care should be taken while focussing the slide under the microscope. Focussing shouldbe done starting from the lower magnification to avoid any unwanted damage to the lens.
12.3.1 Liver and Liver Lobules
The liver is a roughly triangular in shape and extends across the entire abdominal cavity under
the diaphragm. Most of the liver’s mass is located on the right hypochondrium (i.e., upper
part of the abdomen) as well as part of the abdomen (Figure 12.3). The liver is made of very
soft, pinkish-brown tissues encapsulated by a connective tissue capsule. This capsule is further
covered and reinforced by the peritoneum of the abdominal cavity, which protects and holds
the liver.
The liver consists of 4 distinct lobes—the left, right, caudate, and quadrate lobes. The
Falciform ligament divides the liver into two main lobes, right and left. The larger right lobe
is again sub-divided into three lobes, the right lobe proper, the caudate lobe and the quadrate
lobe (Figure 12.1). Each liver lobe is made up of about 100,000 small hexagonal functional
units known as lobules. A typical liver lobule comprises rows of liver cells, hepatocytes,
radiating out from a central vein. The six angles of the hexagon are occupied by a portal
triad comprising a hepatic portal vein, a hepatic artery and a bile duct. The portal veins
and arteries are connected to the central vein through a network of capillary-like tubes
called sinusoids (Figure 12.2). Blood flows out of the sinusoids into the central vein and istransported out of the liver.
Figure 12.1: Anatomy of Liver—(A) Anterior view (B) Posterior view
Figure 12.2: Transverse section of Liver showing liver lobules anddiagrammatic representation of a typical liver lobule
12.3.2 Pancreas
The pancreas is an elongated, tapered organ, located in the abdominal region, behind the
stomach and next to the duodenum—the first part of the small intestine (Figure 12.3). The
right side of the organ, called the head, is the widest part of the organ and lies in the curve of
the duodenum. The tapered left side which extends slightly upward is the body of the pancreas.The tail of the pancreas ends near the spleen.
Figure 12.3: Diagrammatic representation of the location of pancreas and liver in the body
Structure and Function of Pancreas
Pancreas has two main functional components:
1. The Exocrine cells, the acini—Cells that release digestive enzymes into the gut via the
pancreatic duct. These enzymes include trypsin and chymotrypsin to digest proteins;amylase for the digestion of carbohydrates; and lipase to break down fats. The pancreatic
duct joins the common bile duct to form the ampulla of Vater in the duodenum. The
pancreatic juices and bile (from gallbladder) released into the duodenum help the bodyto digest fats, carbohydrates as well as proteins.
2. The Endocrine pancreas—Highly vascularized groups of cells known as the Islets of
Langerhans within the exocrine tissue constitute the endocrine pancreas (Figure 12.4).
The human pancreas has 1–2 millions islets of Langerhans. It contains four different
types of cells which are distinguished from one another by their morphology and stainingcharacteristics;
(i) Alpha cells: Which secrete glucagon, constitute about 25 per cent of all the cells of
islet of langerhans.
(ii) Beta cells: The most abundant of the islet cells constitute about 60% of the cells.
They release insulin and amylin hormones with unknown function, secreted in
parallel to the insulin.
(iii) Delta cells: Constitute about 10 per cent of total cells and secrete somatostatin which
regulates both the alpha and beta cells.
(iv) F cells or PP cells: Are present in small number and secrete a polypeptide known
as pancreatic polypeptide which inhibits the digestive enzymes produced by theexocrine pancreas.
Figure 12.4: Transverse section of Pancreas showing the acini and Islet of Langerhans andDiagrammatic representation of an Islet of Langerhans
APPLICATION 12.1
1.Complete the sentence with appropriate terms:
(i)................... is a homopolymer of glucose synthesized in liver cells.
(ii) Complete oxidation of one molecule of glucose yields ..................... molecules of ATP.
(iii) The liver consists of four distinct lobes ....................., ......................, ................., and
...................... .
(iv) The endocrine pancreas consists of highly vascularized groups of cells called
.......................... .
2.What is the main cause of type I diabetes?
3.What is the main treatment for type I diabetes4 What type of diet is most closely associated with the development of type II diabetes?
12.4 HOMEOSTATIC CONTROL OF BLOOD GLUCOSE CONCENTRATION BYINSULIN AND GLUCAGON
ACTIVITY 4
Discuss the mechanism of glucose regulation. Prepare a PowerPoint presentation usinginternet available resources. Show your presentation to the class.
Insulin and glucagon are the major hormones responsible for the regulation of blood glucose.
Both insulin and glucagon are secreted by the pancreas, and are referred to as pancreaticendocrine hormones.
12.4.1 Insulin
Insulin was first discovered in 1922 by Banting and Best. Although there is always a low level
of insulin secreted by beta cells of pancreas, the amount secreted into the blood increases as the
blood glucose level rises. In the blood, it circulates entirely in an unbound form with plasma
half-life of about 6 minutes. Only a small portion of the insulin binds with the insulin receptors
of the target cells while the rest is degraded by the enzyme insulinase, mainly in liver and to alesser extends in kidney and muscles.
Function of Insulin
Binding of insulin to the receptors stimulates the rate of glucose uptake, storage and utilization
by almost all tissues of the body mainly in muscles, adipose tissue and liver. Other important
functions of insulin include:
1. Insulin promotes glycogenesis by activating enzyme glycogen synthase.
2. Insulin inactivates liver phosphorylase, the key enzyme of glycogenolysis.
3. Insulin promotes lipid synthesis by increasing the conversion of excess glucose into fatty
acids in the liver. These fatty acids are transported as triglycerides to the adipose tissue
where it is deposited as fat.
4. Insulin inhibits the enzymes responsible for gluconeogenesis in liver.
5. Insulin promotes protein synthesis by increasing the rate of transcription and translation.
It also stimulates transport of many amino acids into the cells.6. Insulin inhibits breakdown of lipids and proteins.
Regulation of Insulin Secretion
The secretion of insulin by beta cells of islet of Langerhans depends on the following factors:
1. Blood glucose level: Increased in the blood glucose level stimulates the insulin secretion
while decreased in the blood glucose concentration inhibits the secretion.
2. Blood fatty acids and amino acids concentration: Insulin secretion is also stimulated
by increased in the concentration of blood’s fatty acids and amino acids concentration
and inhibited when its concentration decreased.
3. Gastrointestinal hormones: Insulin secretion increases moderately in response to several
gastrointestinal hormones—gastrin, secretin, cholecystokinin and gastric inhibitory peptide.
These hormones are released after the person takes meal and the increased in insulin secretion
can be regarded as preparation for the glucose and amino acids uptake by cells.
4. Other hormones: Other hormones that are associated with the increase in the insulinsecretion are glucagon, growth hormone, cortisol, progesterone and estrogen.
12.4.2 Glucagon
Glucagon is secreted by the alpha cells of the pancreatic islets in response to low blood glucose
levels and to events whereby the body needs additional glucose, such as in response to vigorousexercise.
Functions of Glucagon
The effect of glucagon in regulating blood glucose level is exactly opposite to insulin.
1. The most important function of glucagon is activation of glycogen phosphorylase enzyme
responsible for degradation of glycogen to glucose-6-phosphates. The glucose-6-phosphate
is then dephosphorylated to glucose and finally released into the blood stream resulting
in increase in blood glucose concentration.
2. Glucagon also stimulates the increase in rate of amino acid uptake and its conversion
into glucose, i.e., gluconeogenesis.
3. Glucagon activates adipose cell lipase enzyme which stimulates lipids metabolism.
4. Glucagon also inhibits the storage of triglycerides in the liver by preventing the liver from
removing fatty acids from the blood.
5. Glucagon also enhances the strength of the heart; increases blood flow in some tissues,especially the kidneys; enhances bile secretion; and inhibits gastric acid secretion.
Regulation of Glucagon Secretion
Glucagon secretion increases with the decrease in the concentration of blood glucose level while
the increasing concentration of glucose inhibits its secretion. Other factors which stimulate
glucagon secretion are, increase in the concentration of amino acids in blood and vigorousphysical exercise
12.4.3 Negative Feedback Mechanism
Negative feedback is an important regulatory mechanism for physiological function in all
living cells. It occurs when a reaction is inhibited by increased concentration of the product.
Regulation of blood glucose level is an excellent example of homeostatic control throughnegative feedback mechanism (Figure 12.5).
Figure 12.5: Negative feedback regulation of blood glucose level by insulin and glucagon
Response to an Increase in Blood Glucose
When there is increase in blood glucose level, the beta cells of the pancreatic islets of langerhans
increase the release of insulin into the blood. Insulin binds to receptors on the cell membrane
and stimulates the cells to increase glucose absorption. This led to a decrease in blood glucose
level. Besides, insulin also stimulates glycogenesis and glycolysis while inhibiting glycogenolysis,gluconeogenesis, lipolysis etc. which all contributes in reducing blood glucose levels.
Response to a Decrease in Blood Glucose
Decreased in blood glucose level stimulates the alpha cells of pancreas islets to increase the
secretion of glucagon. Glucagon activates enzyme glycogen phosphorylase in the liver and
muscle cells which start glycogenolysis. It also promotes gluconeogenesis, lipid metabolism etc.The overall effect of glucagon is an increase in the concentration of blood glucose.
12.5 INTERACTION OF GLUCOSE CONTROL MECHANISMS BYOTHER HORMONES
ACTIVITY 5
Using the internet, find research papers on the role of adrenaline in regulating blood glucose
level.
Make a PowerPoint presentation of the research paper.Show the presentation to the class.
12.5.1 Hormones Involved in Glucose Regulation
Other than insulin and glucagon, there are many hormones which contribute to the regulation
of blood glucose level (Figure 12.6). They are:
1. Somatostatin: It is secreted by delta cells of pancreatic islet of langerhans in response
to many factors related to ingestion of food like increased concentration of glucose,
amino acids, fatty acids and several gastrointestinal hormones released from the upper
gastrointestinal tract. Somatostatin acts locally within the islets of Langerhans and
inhibits the secretion of both insulin and glucagon. It also reduces the motility of the
stomach, duodenum, and gallbladder and decreases the secretion and absorption in the
gastrointestinal tract. Hence, lowers overall blood glucose level.
2. Epinephrine: Commonly known as Adrenaline, it is secreted by the medulla of the
adrenal glands in response to strong emotions such as fear or anger. It causes increases
in the heart rate, muscle strength, blood pressure and sugar metabolism. In response, it
enhances the process of glycogenolysis, increasing the overall blood glucose concentration.
3. Cortisol: It is also known as stress hormone and is secreted by the adrenal cortex of the
adrenal gland in response to stress. Cortisol enhances gluconeogenesis and increases the
concentration of glucose in the blood.
4. Adrenocorticotropic Hormone (ACTH): In response to various stresses, hypothalamus
secretes corticotropin-releasing hormone which stimulates anterior pituitary to secreteACTH. It stimulates the the adrenal cortex to release the cortisol hormones.
Figure 12.6: Hormonal regulation of blood glucose level
5. Growth hormone (GH): It is another anterior pituitary hormone which antagonizes
the action of insulin by inhibiting the glucose uptake by cells and increasing the blood
glucose level.
6. Gastrointestinal hormones: The hormones released by gastrointestinal tract such as
gastrin, secretin, cholecystokinin and gastric inhibitory peptide etc. increase the digestion
and absorption of nutrients in the gastrointestinal tracts. These hormones stimulate thepancreas to secrete insulin in anticipation of the increase in blood glucose level.
12.5.2 Mechanism of Hormonal Regulation
Our body maintains certain variables like temperature, pH etc. within a safe range so that it
does not cause any harm to the body and the internal environment remains stable and relatively
constant. This is known as homeostasis. Hormones are chemical messenger that are directlyreleased into the blood stream. They play a very important role in maintaining the homeostasis.
Steps of Hormonal Signalling
Hormonal signal transduction is a complex process which involves the following steps:
1. Hormones are the first synthesis in particular cells of an organ and stored for secretion
in response to certain stimulus.
2. When the organ receives the stimulus; hormones are secreted directly into the blood
stream.
3. Blood carries the hormone to the target cell(s).
4. The hormone is recognized by the specific receptor in the cell membrane or by the
intracellular receptor protein.
5. The hormonal signal is relayed and amplified through a series of signal transductionprocess in the target cells which lead to cellular response.
Cell Signalling Mechanism Involves in Glucose Regulation—Glycogenolysis
As mentioned earlier, several hormones affect glycogenolysis. Among these, glucagon and
epinephrine are the most important hormones which trigger the breakdown of glycogen.
Epinephrine is released in response to rigorous muscular activity from the adrenal medulla
and stimulates the breakdown of glycogen in muscle to a larger extent than in the liver. The
liver cells are more responsive towards glucagon. Both epinephrine and glucagon can bind
to common receptor and through a series of other enzymes; activate the enzyme glycogen
phosphorylase necessary to initiate glycogenolysis.
The whole process of signal transduction epinephrine and glucagon can be divided into threemain steps (Figure 12.7).
1. Hormone-receptor interaction at the cell surface
The hormone epinephrine and glucagon act as a ligand and bind to specific receptors
known as 7TM, found in the plasma membranes of muscle and liver cells. The bindingactivate the alpha-subunit of the Gs protein.
Figure 12.7: Hormonal signal transduction pathway in the activation ofglycogen phosphorylase enzyme during glycogenolysis
2. Formation of cyclic AMP that binds to kinase protein
The activated alpha-subunits of Gs protein activate the adenylate cyclase, a transmembrane
protein. Adenylate cyclase catalyzes the formation cyclic AMP (cAMP) which acts as
the second messenger in the signal transduction pathways.
3. Activation of an enzyme cascade by phosphorylation and amplification of the signal
As level of cyclic AMP increases in the cytoplasm, it binds to the regulatory subunits
of protein kinase A and activates protein kinase A. The activated protein kinase A
phosphorylates and activates another enzyme phosphorylase kinase which finally activates
glycogen phosphorylase and initiates the glycogenolysis.
Once activated, cyclic AMP cascade can highly amplify the effects of hormones through the
number of enzymes. Therefore, binding of a small number of hormone to cell-surface receptorscan lead to the release of a very large number of sugar molecules.
APPLICATION 12.2
1. Complete with appropriate terms:
(i) Insulin was first discovered in 1922 by ...................... .
(ii) Glucagen is secreted by ....................... cells of pancreatic islets.
(iii) Epinephrine commonly known as ....................... .
(iv) Hormone .................... enhances glycogenolysis and increases concentration of glucose
in the blood.
(v) ............................. catalyzes the formation of cycle AMP.
(vi) ............................ activates glucagon phosphorylase and initiates the glycogenolysis.
2. An investigation was carried out to determine the response of pancreatic cells to an increase
in the glucose concentration of the blood. A person who had been told not to eat or drink
anything other than water for 12 hours then took a drink of a glucose solution. Blood samples
were taken from the person at one hour intervals for five hours, and the concentration of
glucose, insulin and glucagon in the blood were determined. The results are shown in thegraph below:
a) Explain why the person was told not to eat or drink anything other than water for
12 hours before having the glucose drink.
b) Use the information in the figure to describe the response of the pancreatic cells to
an increase in the glucose concentration.
c) Outline the role of insulin when the glucose concentration in the blood increases.
d) Suggest how the results will change if the investigation continued longer than fivehours without the person taking any food.
12.6 CAUSE OF BLOOD SUGAR IMBALANCES IN THE BODY
ACTIVITY 6
Draw the diagram of the negative feedback mechanism of glucose regulation on the chart
paper.
Illustrate the effect of various hormones on each step.Highlight the important steps which can cause or affect the blood sugar balance.
Our body obtains glucose from various food sources or synthesis in the liver and muscles from
other compounds like pyruvate, lactate, glycerol, and glucogenic amino acids. The blood carriesglucose to all the cells in the body where it is metabolized to produce energy.
Blood sugar levels keep on fluctuating throughout the day increasing after meals and decreasing
in between the meals. When the blood glucose level rises beyond the normal value, the condition
is known as hyperglycaemia. On the other hand, hypoglycaemia or low blood sugar is thecondition in which the blood glucose level is below normal (~70 mg/dL).
12.6.1 Hyperglycaemia
High blood glucose level can be caused due to various reasons like:
1. Carbohydrates: Eating food containing too much carbohydrates. The body of a person
cannot process high levels of carbohydrates fast enough to convert it into energy.
2. Insulin control: The pancreas of the individual are unable to produce enough insulin.
3. Stress: Stress stimulates the secretion of certain hormones like cortisol and epinephrine
etc., which increases the blood glucose level.
4. Low levels of exercise: Daily exercise is a critical contributor to regulating blood sugar
levels.
5. Infection, illness, or surgery: With illness, blood sugar levels tend to rise quickly over
several hours.
6. Other medications: Certain drugs, especially steroids, can affect blood sugar levels.
A high blood sugar level can be a symptom of diabetes. If hyperglycaemia persists for several
hours, it can lead to dehydration. Other symptoms of hyperglycaemia include dry mouth, thirst,
frequent urination, blurry vision, dry, itchy skin, fatigue or drowsiness, weight loss, increased
appetite, difficulty breathing, dizziness upon standing, rapid weight loss, increased drowsinessand confusion, unconsciousness or coma.
12.6.2 Hypoglycemia
Hypoglycaemia is generally defined as a serum glucose level below 70 mg/dL. Symptoms
typically appear when the blood glucose levels reaches below 60 mg/dL and levels below 50
mg/dL can be fatal.
Common causes of low blood sugar include the following:
1. Overmedication with insulin or antidiabetic pills
2. Use of alcohol
3. Skipped meals
4. Severe infection
5. Adrenal insufficiency
6. Kidney failure
7. Liver failure, etc.
Common symptoms of hypoglycemia include trembling, clammy skin, palpitations (pounding
or fast heart beats), anxiety, sweating, hunger, and irritability. If the brain remains deprived
of glucose for longer period, a later set of symptoms can follows like difficulty in thinking,
confusion, headache, seizures, and coma. And ultimately, after significant coma or loss ofconsciousness, death can occur.
12.7 DIABETES MELLITUS
ACTIVITY 7
Using the internet, study the different symptoms and causes of diabetes mellitus.Prepare a PowerPoint presentation and present to the class.
Diabetes mellitus (commonly referred to as diabetes) is a chronic condition associated with
abnormally high levels of sugar in the blood due to impaired carbohydrate, fat, and protein
metabolism. It can be due to absence or insufficient production of insulin by the pancreas, or
inability of the body to properly use insulin. Hence, there are two types of diabetes mellitus –
Type I causes by lack of insulin secretion and Type II, caused by reduced sensitivity of targetcells to insulin.
12.7.1 Type I Diabetes
It is known as insulin dependent diabetes mellitus (IDDM) and cause due to insufficient
insulin production by the beta cells of pancreatic islet of langerhans or due to absence of the
beta cells itself. Since the pancreas makes very little or no insulin at all, glucose cannot get
into the body’s cells and remain in the blood leading to hyperglycemia. The concentration of
blood glucose level can be as high as 300 – 1,200 mg/dL. The symptoms of Type I diabetesincludes:
1. Loss of glucose in urine; due to increase in blood glucose, concentration goes beyond
180 mg/dL.
2. Dehydration; due to osmotic loss of water from cells and inability to reabsorb water in
kidney.
3. Tissue injury; due to damages blood vessels in many tissues.
4. Metabolic acidosis; due to increased fat metabolism.5. Depletion of body’s protein; due to increase protein metabolism.
Treatment of Type I Diabetes
Persons with Type I diabetes require treatment to keep blood sugar levels within a target range
which includes:
1. Taking insulin from external source everyday either through injections or using an insulin
pump.
2. Monitoring blood sugar levels several times a day.
3. Eating a healthy diet that spreads carbohydrates throughout the day.
4. Regular physical activity or exercise. Exercise helps the body to use insulin more efficiently.
It may also lower your risk for heart and blood vessel disease.
5. Not smoking.6. Not drinking alcohol if you are at risk for periods of low blood sugar.
12.7.2 Type II Diabetes
Also known as non-insulin dependent diabetes mellitus (NIDDM), it is caused due to the
inability of cells to take up glucose from the blood. It can be either due to defective insulin
receptors over cell surfaces or abnormality of blood plasma protein, amylin. Due to decrease
sensitivity of cells to insulin, a condition known as insulin resistance, the beta cells secrete
large amount of insulin into the blood stream resulting in increase concentration of insulin in
blood. This condition is known as hyperinsulinemia. Type II diabetes are more common and
account for almost 80–90 per cent of the total diabetes mellitus cases.
The symptoms of type II diabetes include:
1. Obesity, especially accumulation of abdominal fat;
2. Fasting hyperglycemia;
3. Lipid abnormalities such as increased blood triglycerides and decreased blood highdensity
lipoprotein-cholesterol; and4. Hypertension.
Treatment of Type II Diabetes
There’s no cure for diabetes, so the treatment aims to keep the blood glucose levels as normal as
possible and to control the symptoms and prevent health problems developing later in life. In type II
diabetes, the pancreas is still working but our body develops insulin resistance and is unable to
effectively convert glucose into energy leaving too much glucose in the blood. Therefore, Type
II diabetes can be managed through lifestyle modification including:
1. Healthy diet as eating well helps manage our blood glucose levels and body weight.
2. Regular exercise helps the insulin work more effectively, lowers your blood pressure and
reduces the risk of heart disease.
3. Regular monitoring of blood glucose levels to test whether the treatment being followedis adequately controlling blood glucose levels or we need to adjust the treatment.
12.7.3 Importance of Controlled Diet in Diabetes
Controlled diet is very important for diabetic patients because blood sugar is mostly affected
by the food one eats. The glycaemic index of a food measures how the food affects the blood
glucose level. The higher the glycemic index of the food, the greater the potential of increasing
blood glucose. Therefore, in order to control glucose levels in the blood, it is important that
diabetic primarily chooses low glycaemic index carbohydrates like dried beans and legumes
such as lentils and pintos, non-starchy vegetables, fruits, whole grain bread and cereals, sweet
potatoes etc. Foods like white bread, white rice, cornflakes, white potatoes, popcorn, pineapple,
and melons are high glycaemic index foods and should be eaten moderately.
Because people with diabetes are at risk of high blood pressure, it makes sense to also choose
foods that are heart healthy (i.e., lean, low-fat) and the ones that are low in salt. Increasing
the amount of fibre in diet and reducing fat intake, particularly saturated fat, can help prevent
diabetes or manage the diabetic condition from developing any complications. Therefore, one
should:
1. Increase the consumption of high-fibre foods, such as wholegrain bread and cereals,
beans and lentils, and fruits and vegetables.
2. Choose foods that are low in fat for example, replace butter, ghee and coconut oil with
low-fat spreads and vegetable oil.
3. Choose skimmed and semi-skimmed milk, and low-fat yoghurts.
4. Eat fish and lean meat rather than fatty or processed meat, such as sausages and burgers.
5. Grill, bake, poach or steam food instead of frying or roasting it.
6. Avoid high-fat foods, such as mayonnaise, chips, crisps, pasties, poppadoms and samosas.
7. Eat fruit, unsalted nuts and low-fat yoghurts as snacks instead of cakes, biscuits, bombaymix or crisps etc.
12.7.4 Coping with Situation of Diabetics and Hypertension
Blood pressure is the measure of the force of blood pushing against blood vessel walls. The
heart pumps blood into the arteries, which carry the blood throughout the body. The normal
plod pressure is less than 120 (systolic) over 80 (diastolic). High blood pressure, also called
hypertension, is dangerous because it makes the heart work harder to pump blood out to the
body and contributes to hardening of the arteries, or atherosclerosis, to stroke, kidney disease,
and to the development of heart failure. Diabetics are more likely to develop high blood pressure
and other heart and circulation related problems, because diabetes damages arteries and makes
them targets for hardening (atherosclerosis). Obesity is another main factor which is responsible
for hypertension.
When it comes to preventing diabetes complications, normal blood pressure is as important as
good control of blood glucose levels. Therefore, to treat and help prevent high blood pressure,
one should control their blood glucose, stop smoking, eat healthy, maintain a healthy bodyweight, limit alcohol and salt consumption and exercise regularly.
Assisting Hypertension Patients
The following first aid tips are recommended when a person experiences hypertension:
1. Make the patient to lie on the bed and rest adequately. Tell the patient to take deep breaths
and reassure them.
2. Do not allow them to walk about, accompany the patient if it is really needed.
3. If the patient is in a stressful situation, try to comfort and reduce anxiety, as anxiety
alone can increase blood pressure.
4. If the patient is vomiting or having seizures, turn to lateral side to prevent aspiration.
5. Keep monitoring breathing, pulse rate, blood pressure, level of consciousness and for
any other dangerous signs ( e.g., paralysis of body in stroke, convulsions, etc.)
6. Do not give anything by mouth to eat/drink if there is suspicion of stroke.
7. If the patient’s nose is bleeding, administer appropriate first aid.
8. Give drinks that are high in potassium to help balance the amount of sodium (salt) inthe body to lower blood pressure levels.
12.8 MONITORING OF BLOOD GLUCOSE LEVELS
ACTIVITY 8
Aim: To perform blood glucose quantification test.
Materials Required:
1. Glucose meter
2. Test strips
3. Lancets (small needles used to prick the skin) and lancet device
that
holds the lancet.
Procedure:
1. Wash your hands with soap and water and dry them properly.
2. Prepare the blood glucose meter with the test strip according to the manufacturer’s instructions.
3. Use the lancet device to prick the side of your fingertip with a lancet.
4. Place a drop of blood onto the correct part of the test strip.
5. The strip will draw up the blood into the meter and show a digital reading of the blood
glucose level within seconds.
6. Note the reading.
7. Use a clean cotton ball to apply pressure to the fingertip for a few moments until the bleeding
stops.
8. Similarly, measure the blood glucose level of your friends.
9. Compare your blood glucose level with that of your friends.
Discussion:
In general, a fasting blood glucose reading (taken before a meal) should be between 72 mg/dL
to 126 mg/dL. And a blood glucose reading 2 hours after a meal should be between 90 mg/dL
to 180 mg/dL.
Precautions:
1. Make sure the lancelet is properly sterilized.2. Insert the test strip properly.
Blood glucose monitoring is a way of testing the concentration of glucose in the blood (glycaemia).
As mentioned earlier, the concentration of blood glucose kept on fluctuating throughout the
day. Under certain physiological disorders, especially when the person is suffering from diabetesmellitus, the blood glucose concentration can increase well above the normal concentration.
Most people with type II diabetes need to monitor their blood sugar levels at home. A blood
glucose test is generally performed by piercing the skin (typically, on the finger) to draw blood,
then applying the blood to a chemically active disposable ‘test-strip’ as described (see activity 8)or to a biosensor.
Dipstick Test
A dipstick or the reagent strips is a narrow strip of plastic with small pads attached to it.
Each pad contains specific reagents for a different reaction, thus allowing for the simultaneous
determination of several compounds. The blood glucose test use enzymes glucose oxidase and
hexokinase which are specific to glucose, embedded on a test strip or a dipstick. When the
blood sample is applied onto the strip, the enzymes catalyzed glucose specific reaction whichchanges the colour. The chemical reaction involves in the glucose oxidase test is as follows:
Numbers of chromogen like potassium iodide, tetramethylbenzine, O-tolidinehydrochloride,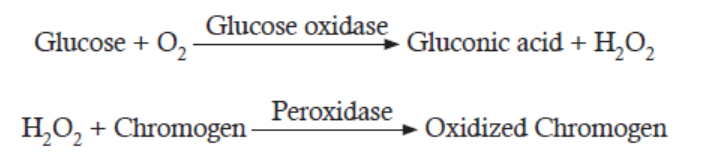
4-aminoantipyrine etc. are used in the dipstick. The colour reaction of the dipsticks is kinetic
and will continue to react after the prescribed time. Therefore, reading taken after the prescribedtime can give false result.
Biosensors
A biosensor is a device which is composed of two elements; a bio-receptor that is an immobilized
sensitive biological element (e.g. enzyme, DNA probe, antibody) recognizing the analyte (e.g.
enzyme substrate, complementary DNA, antigen) and a transducer, used to convert biochemical
signal resulting from the interaction of the analyte with the bioreceptor into an electronic
signal. The intensity of generated signal is directly or inversely proportional to the analyte
concentration. For example, the glucose biosensor is based on the fact that the immobilized
Glucose oxidase enzyme which catalyzes the oxidation of β-D-glucose by molecular oxygen
producing gluconic acid and hydrogen peroxide. An electrochemical transducer converts thisreaction into electronic signal which appears on the screen of the glucose meter.
Continuous Glucose Monitoring
Continuous glucose monitoring systems (CGMS) use a glucose sensor inserted under the
skin in the form of a small needle. The signal from the sensor is transmitted wirelessly and the
result is recorded in a small recording device. The monitor of the device updates and displays
the blood sugar level every few minutes. The glucose sensor needs to be removed and replaced
at least once per week.
Advantages of continuous glucose monitoring:
1. The monitor displays blood sugar level every few minutes, allowing one to see whether
the level is increasing, decreasing, or is stable.
2. The receiver can also be set to alarm if the blood sugar level is above or below a pre-set
level.
3. The blood sugar results from the continuous monitor can be downloaded to a computer,
allowing you to check blood sugar trends over time.
The only disadvantage of continuous monitor other than the cost is its inaccuracy compared
to more traditional accurate dipstick method. Therefore, most experts recommend continuous
glucose monitoring along with several finger sticks daily to calibrate the CGMS device and toverify that the sensor readings are accurate.
Roles of Adrenaline in the Control of Blood Sugar Level
Adrenaline, a natural stimulant created in the kidney’s adrenal gland, travels through the
bloodstream and controls functions of the autonomous nervous system, including the secretion
of saliva and sweat, heart rate and pupil dilation. The substance also plays a key role in the
human flight-or-flight response.
The “fight or flight” hormone that gives us a quick boost of extra energy to cope with danger
— including the danger of low blood glucose. When blood glucose levels drop too low, the
adrenal glands secrete epinephrine (also called adrenaline), causing the liver to convert stored
glycogen to glucose and release it, raising blood glucose levels. Epinephrine also causes many
of the symptoms associated with low blood glucose, including rapid heart rate, sweating, and
shakiness. The epinephrine response spurs the liver to correct low blood glucose or at least raiseblood glucose levels long enough for a person to consume carbohydrate.
12.9 DETECTION OF GLUCOSE IN URINE
ACTIVITY 9
Aim: To test the presence of glucose in the urine sample using Benedict’s test.
Materials Required:
1. Benedict’s solution (100 g of anhydrous sodium carbonate, 173 g of sodium citrate and
17.3 g of copper (II) sulfate pentahydrate in 1L dH2O prepared freshly; not more than 3
months old),
2. Urine sample
3. Dropper,
4. Test-tube,
5. Test-tube holder.
Procedure:
1. Take 5 ml (one teaspoon) of Benedict’s solution in the test-tube.
2. Holding the test-tube with the holder, heat it over a spirit lamp till the Benedict’s Solution
boils without overflowing.
3. Drop 8 to 10 drops of urine into the boiling Benedict’s solution.
4. After again boiling the mixture, let it cool down.
• Do you see any change in the colour of the mixture?
• Why does it happen?
Discussion:
1. Note down the colour of the mixture after cooling.
2. The colour of the mixture serves as a guide to the amount of sugar in the urine:
• Blue: sugar absent;
• Green: 0.5% sugar;
• Yellow: 1% sugar;
• Orange: 1.5% sugar;
• Red brown/Red ppt.: 2 % or more sugar.
Precautions:
1. Care should be taken while heating the Benedict’s solution.
2. Use disposable gloves while handling the urine sample.
3. Result should be noted only when the solution cold to the room temperature.Note: Coloured water sample can be used instead of the urine sample to avoid the cases of infection.
ACTIVITY 10
Aim: To determine the urine glucose concentration using coloured water (simulated urine).
Materials Required:
1. Coloured water (Blue, Green, Yellow, Orange, Red Brown)
2. Test tubes
Procedure:
1. Take a test tube containing coloured water.
2. Write down approximate concentration of glucose depending on the colour of the water.
3. Explain your result.
Discussion:
1. The colour of the water serves as a guide to the amount of sugar in the simulated urine:
• Blue: sugar absent;
• Green: 0.5% sugar;
• Yellow: 1% sugar;
• Orange: 1.5% sugar;• Red brown/Red ppt.: 2% or more sugar.
Urine analysis can be used to test pH, protein, glucose, ketones, occult blood, bilirubin,
urobilinogen, nitrite, leukocyte esterase etc. in the urine sample. Simple test for glucose in
urine can be used to diagnose diabetes mellitus. Generally, healthy person do not loss glucose
in their urine whereas a person with diabetes mellitus loses small to large quantities of glucosein their urine.
Detection of Glucose in Urine
The presence of glucose in the urine is called glycosuria (or glucosuria). The urine analysis
of glucose is based on enzyme glucose oxidase which is impregnated in a dipstick (reactiondescribed in previous section).
Detection of Protein in Urine
The glomerular filtrate of a normal kidney contains little amount of low–molecular weight
protein. Most of these proteins get reabsorbed in the tubules with less than 150 mg being
excreted through urine per day. Therefore, the abnormal increase in the amounts of proteinin the urine, Proteinuria, can be an important indicator of renal diseases. There are certain
physiologic conditions such as exercise and fever that can lead to increased protein excretionin the urine in the absence of renal disease.
Proteinuria is a symptom of chronic kidney disease (CKD), which can be due to diabetes, high
blood pressure, and diseases that cause inflammation in the kidneys. Therefore, urine analysis
for protein is part of a routine medical assessment for everyone. If CKD is not checked in time,
it can lead to end-stage renal disease (ESRD), when the kidneys completely stop functioning.
A person with ESRD requires a kidney transplant or regular blood-cleansing treatments calleddialysis to further sustain.
The tests for proteinuria are based either on the “protein error of indicators” principle (ability
of protein to alter the colour of some acid-base indicators without altering the pH) or on the
ability of protein to be precipitated by acid or heat. According to “protein error of indicators”
principle, a protein-free solution of tetra bromophenol blue at pH 3 is yellow in colour and
its colour changes from yellow to blue (or green) when the pH increases from pH 3 to pH 4.
However, in the presence of protein (albumin), the colour changes occur between pH 2 and 3
i.e., an “error” occurs in the behaviour of the indicator. The method is more sensitive to albuminthan to other proteins, whereas the heat and acid tests are sensitive to all proteins.
The test result may show false-positive results in a highly buffered alkaline urine, which may
result from alkaline medication or stale urine. Also, if the dipstick is left in the urine for too
long, the buffer could be washed out of the reagent resulting in increase pH and the strip may
turn blue or green even if protein is not present. On the other hand, false-negative results
can occur in dilute urines or when the urine contains proteins other than albumin in higherconcentrations.
Detection of Ketones in Urine
As discussed earlier, ketones, or ketone bodies are formed during lipid metabolism. One of
the intermediate products of fatty acid breakdown is acetyl CoA. If the lipid metabolism and
carbohydrate metabolism are in balanced, Acetyl-CoA enters the citric acid cycle (Krebs cycle)
where it reacts with oxaloacetate to form citrate. When carbohydrate is not available in the cells,
all available oxaloacetate get converted to glucose and so none is available for condensation
with Acetyl- CoA. As such, Acetyl-CoA cannot enter the Krebs cycle and is diverted to form
ketone bodies.
The ketone bodies are acetoacetic acid (diacetic acid), hydroxybutyric acid and acetone.
Acetyl-CoA is first converted to acetoacetic acid which later gets converted to other two ketonesthrough the following reaction:
Hydroxybutyric acid is formed by reversible reduction, and acetone is formed by a slow
spontaneous decarboxylation. Acetoacetic acid and hydroxybutyric acid are normal fuels of
respiration and are important sources of energy. In fact, the heart muscle and the renal cortex
prefer to use acetoacetate instead of glucose. The odour of acetone may be detected in the breath
of an individual who has a high level of ketones in the blood because acetone is eliminatedthrough lungs.
Laboratory tests for ketones include reagent test-strip methods and tablet-based tests such as
Acetest. The test strip or dipstick contains the reagents sodium nitroprusside and an alkaline
buffer, which react with diacetic acid in urine to form a maroon colour, as in the followingreaction:
False-positive results may occur when the urine sample is highly pigmented, contains large
amounts of levodopa metabolites, have high specific gravity and a low pH or contain sulfhydrylgroups
APPLICATION 12.3
1.Complete with appropriate terms:
(i) Hyperglycaemia is the condition when the blood glucose level is below ....................... .
(ii) .................... is caused due to insufficient insulin production by beta cells.
(iii) A ........................... diet is important to regulate glucose level in body.
(iv) The test strip or dipstick contains the reagents ..................... and .......................... .
(v) The presence of glucose in urine is called ......................... .
2.a) Name the process by which glucose enters and leaves cells.
b) Explain why:
i. Muscle cells do not have receptors for insulin.
ii. There are second messengers for insulin and glucagon.
iii. Insulin and glucagon have different second messengers.
3.a. Explain why insulin cannot be taken by mouth.
b. Suggest how people with type 1 diabetes can monitor the effectiveness of the insulin
that they take.c. Suggest how people with type 2 diabetes can control their blood glucose
12.10 SUMMARY
• Glucose is the universal fuel which provides energy to all the living cells.
• Glucose is converted to glucose-6-phosphate with the help of enzyme glucokinase in
liver and hexokinase in most cells, which help the cells to retain glucose.
• One molecule of glucose yields 38 molecules of ATP.
• Polysaccharides of glucose viz. cellulose, chitin are important structural components of
plants and animal cells.
• Excess glucose in the body is stored in the form of glycogen through glycogenesis.
• When the blood glucose level falls, glycogen breaks down into glucose through glycogenolysis.
• Pancreas and liver are the main organs responsible for regulation of blood glucose level.
• Pancreas secretes insulin and glucagon hormones responsible for glucose regulation.
• Exocrine pancreas release digestive enzymes including trypsin, chymotrypsin, amylase
and lipase.
• The islet of langerhans is the endocrine component of pancreas and secretes insulin
(by beta cells), glucagon (by alpha cells), somatostatin (by delta cells) and pancreatic
polypeptide (by F cells).
• Liver is a vital organ of our body which performs various functions ranging from protein
synthesis to detoxification of drugs.
• Liver lobes are compost of small units, known as liver lobules.
• Insulin stimulates rapid glucose uptake by cells, promote glycogenesis while inhibiting
glycogenolysis and gluconeogenesis resulting in decreasing blood glucose level.
• Glucagon activates enzyme glycogen phosphorylase and initiates glycogenolysis in the
liver and muscle cells.
• In liver cells, glucagon increases the rate of amino acid uptake and converts it into glucose.
• Blood glucose level regulation by insulin and glucagon is an excellent example of negative
feedback mechanism where the effect of one hormone stimulates the other hormone
and vice versa.
• Hormonal regulation of glucose is a three step process which involves hormone-receptor
interaction followed by activation of second messenger, cAMP and a series of enzyme
cascade.
• Hyperglycemia is a condition when the blood glucose level rises higher than the normal
level.
• Hypoglycaemia is the condition when the serum glucose level is below 70 mg/dL.
• Diabetes mellitus is a chronic condition associated with abnormally high levels of glucose
in the blood.
• The concentration of insulin increase in the blood (hyperinsulinemia) as more and more
insulin is secreted by beta cells in response to decrease sensitivity by cells. This condition
is known as insulin resistance.
• Blood glucose monitoring is a very important exercise to keep the glucose level checked
and avoids various harmful consequences of high blood sugar due to diabetes mellitus.
• Urine analysis of glucose, ketone bodies and protein, blood glucose test, glucose tolerancetest and acetone breath test.
12.11 GLOSSARY
• Glycosuria: Presence of glucose in urine.
• Glycolysis: Splitting of glucose molecule into two molecules of pyruvic acid.
• Glycogenesis: Biosynthesis of glycogen.
• Glycogenolysis: Breaking down of glycogen.
• Gluconeogenesis: Formation of glucose from non-carbohydrate compounds.
• Hyperglycemia: Condition of high blood glucose concentration.
• Hypoglycemia: Condition of low blood glucose concentration below 70 mg/dL.• Hyperinsulinemia: High concentration of insulin in blood.
END UNIT ASSESSMENT 12
I. State whether the following statements are True (T) or False (F)
1. Excess glucose in the body is stored in the form of glycogen.
2. Trypsin is an enzyme used for carbohydrate digestion.
3. Bile salt is secreted by exocrine liver.
4. Glucagon is secreted by pancreas in response to high blood glucose concentration.
5. Insulin administration is recommended for people with type II diabetes mellitus.
6. Type I diabetes mellitus is due to insufficient secretion of insulin by beta cells.
7. Ketone bodies are formed when our body have excessive fat metabolism.
8. Hyperinsulinaemia is associated with type II diabetes mellitus.
9. Glycogenolysis is the breakdown of glucose to form pyruvate.10. The binding of hormones to receptors activates cAMP.
II. Multiple Choice Questions
1. Which of the following monosaccharides is not a product of carbohydrate metabolism
in our body?
(a) Glucose (b) Fructose
(c) Ribose (d) Galactose
2. One molecule of glucose yield …………………… molecules of ATP.
(a) 34 (b) 36
(c) 38 (d) 40
3. Which of the following is not a part of the portal triad?
(a) Central vein (b) Hepatic artery
(c) Hepatic portal vein (d) Bile duct.
4. Somatostatin is secreted by
(a) Alpha cells (b) Beta cells
(c) Delta cells (d) F cells
5. The process of formation of glucose from non-carbohydrates source in the body is
known as
(a) Glycogenesis (b) Gluconeogenesis
(c) Glycolysis (d) Glycogenolysis
6. Which of the following hormones is responsible for decreasing blood glucose level?
(a) Glucagon (b) Insulin
(c) Somatostatin (d) Adrenaline
7. Which of the following compounds is not a ketone body?
(a) Acetoacetic acid (b) Hydroxybutyric acid
(c) Acetone (d) Citric acid
8. In the digestive tract, fructose is absorbed inside the epithelial cells of intestine through
(a) GLUT1 (b) GLUT3
(c) GLUT5 (d) SGLUT2
9. The enzyme used in the dipstick for testing concentration of glucose is
(a) Glucose oxidase (b) Glycogen phosphorylase
(c) Glucose phosphatase (d) Glucosidase
10. Hypoglycemia is the condition when the blood glucose level reach
(a) Above 140 mg/dL (b) Below 140 mg/dL(c) Above 70 mg/dL (d) Below 70 mg/dL
III. Long Answer Type Questions
1. Glucose is the most important carbohydrate in our body. Justify the statement.
2. Describe the negative feedback mechanism with an example.
3. Describe the functions of liver and pancreas in regulating blood glucose level.
4. What are the causes of sugar imbalance in our body?
5. What is diabetes mellitus? Discuss its cause and effect.
6. Discuss in brief the importance of analysing urine in diagnosis diabetes mellitus.
7. How does glucose regulation effect aging? What possible effects can regulation of
glucose have on health of an organism?
8. In your own words, describe three main stages of cell signalling in control of bloodglucose by adrenaline.
