- This topic
UNIT 3 : PRINCIPLES OF DRUG ADMINISTRATION
Key Unit Competence
Administer safely medications to the patients
3.1 The rights of drug administration
Learning activity 3.1
You are carrying out a clinical attachment in the health centre. The patient is
prescribed the injectable medication for pain that will be injected intramuscularly.
Your colleague carrying out the clinical attachment in the same health centre
says there are key elements an associate nurse needs to consider before
administering the medication.
1. List the main 10 RIGHTs of drug administration that need to be considered
before medication administration.2. In which category of RIGHTs of drug administration would checking the
expiry date belong?CONTENT SUMMARY
It is a standard during nursing education to receive instructions on a guide to clinical
medication administration and upholding patient safety known as the ‘Ten rights’ or
‘Ten R’s’ of medication administration (Right Patient, Right Reason or Indication,
Right drug, Right dose, Right Route and form, Right Time, Right Documentation,
Right Response, Right to Refuse, and Right evaluation). These ‘rights’ came into
being during an era in medicine in which the precedent was that an error committed
by a provider was that provider’s sole responsibility and patients did not have as
much involvement in their own care.Right Patient: When administering a drug, it is important to use two methods
(visual as well as verbal methods) to identify the patient before administering the
medication. Nurse must be certain that the patient receiving the drug is the patient
for whom the drug has been ordered by reading properly the physician’s order. Call
the patient by name and ask him to repeat his name aloud. Be very careful if the
patient is deaf or otherwise does not understand the language.A visual identifier may include checking the patient’s name on his or her wristband,
on the patient’s card and on the medicine card for matching name and ID number
as on a chart. It is advisable not to address patients by first name or surname
alone, in the event, there are two or more patients with identical or similar names
in a unit. Depending on the unit that a patient may be in, some patients, such as
psychiatric patients, may not wear wristbands or may have altered mentation to the
point where they are unable to identify themselves correctly. In these instances,
nurses are advised to confirm a patient’s identity through alternative means with
appropriate due diligence.If there is no written identification verifying the patient’s name, nurse should obtain
a wristband or other form of identification before administering the drug. Nurse
may also ask the patient to identify him- or herself and request another unique
identifier such as date of birth. However, do not ask, “Are you Mr or Mrs A?” Some
patients, particularly those who are confused or have difficulty hearing, may respond
by answering “yes” even though that is not their name. Some long-term care or
rehabilitation care facilities have pictures of the patient available, which allow the
nurse to verify the correct patient. If pictures are used to identify patients, it is critical
that they are recent and bear a good likeness of the individual.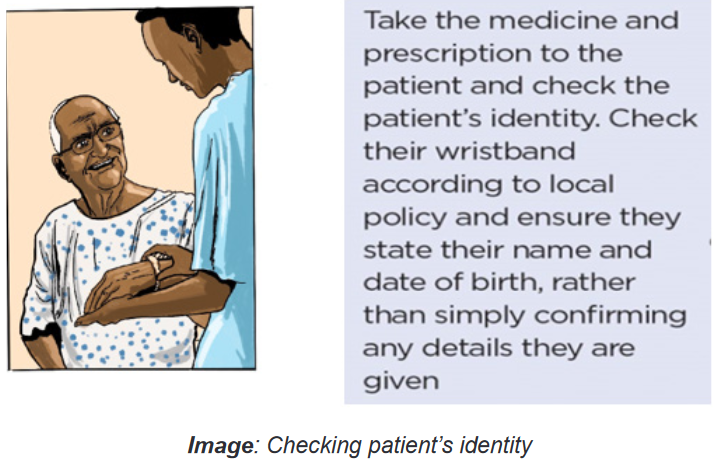
Right Reason or Indication addresses the appropriateness in use of the
medication to the patient. Confirm the rationale for use through researching the
patient’s history while also asking the patient the reason he or she is taking the
drug. Always revisit the rationale for long-term medication use. Knowledge of the
drug’s indication allows the nurse, prescriber, members of the health care team,
patient and/or family members to understand what is being treated. Understanding
the indication helps pharmacists and nurses to catch potential errors, provide
thorough explanations to the patient/family, and decrease challenges to medication
reconciliation.The nurse has the responsibility to verify the reason that the patient is receiving
the medication. It is important to understand the indication, which is related to the
medical diagnosis. If in doubt about the reason for the order, the nurse must verify
the medication order with the prescriber before administration.Right medication or drug: Some brand names or generic names may have very
similar spelling or sound very similar due to prefix, suffix, or starting with the same
first letter. Poor handwriting and abbreviations account for many medical errors
due to misreading letters or numerals that appear differently to different individuals.
Right Drug names can be confused, especially when the names sound similar, or
the spellings are similar.Quickly preparing a drug for administration or failing to look up questionable drugs
can put you at increased risk for administering the wrong drug. An error in drug
name or amount can be found when nurse compares the medication administration
record: with the container label, as the item is removed from the card, and before
the actual administration of the drug.The nurse must be careful of drugs whose names sound alike. When administering
medications, the nurse compares the label of the medication container with the
medication form three times: before removing the container from the drawer or
shelf, as the amount of medication ordered is removed from the container and
before returning the container to storage.The nurse must look for colour, odour, and consistency of the drug. Unusual
characteristics of the drugs should be questioned. The nurse must also administer
medicine only from clearly labelled container and remember to check other critical
information on packaging such as the expiration date. The nursing providers should
also develop a routine habit of explicitly asking patients about known allergies or
history of an allergic. The conversation or anything that distracts the mind not
recommended during drug administration. The nurse must be familiar with the trade
names.If there is doubt consult the physician or at least seniors or other reliable sources.
Avoid accepting the verbal orders, only in emergencies are accepted. Always
identify the patient before giving medication. The nurse must make sure that the
drug has not been discontinued by the prescriber.The nurses administer only the medications they prepare. If an error occurs, the
nurse who administers the medication is responsible for the error. Clients who
self-administer medications should keep them in their original labelled containers,
separate from other medications, to avoid confusion.Right Route and form: A nurse must know the particulars about each medication
before administering it to ensure that the right drug, dose, route, and dosage form
are being used. A complete medication order includes the route of administration.
Confirm the appropriateness of the prescribed route while also making sure the
patient can take/receive the medication by the prescribed route. If a medication
order does not include the route, be sure to ask the prescriber to clarify it. Never
assume the route of administration.In addition, it is critical to patient safety to be aware of the right form of medication.
For example, there are various dosage forms of a commonly used medication,
acetaminophen.It is available in oral suspension, tablet, capsule, gel cap, and paediatric drops, as
well as rectal suppository dosage forms. Nurses need to give the right drug via the
right route with use of the correct dosage form.Medications can be given to patients in different many ways, all of which vary in the
time it takes to absorb the chemical, time it takes for the drug to act, and potential
side-effects based on the mode of administrations, include oral, intramuscular,
intravenous, topical, or subcutaneous injection and others. It is crucial thatnurses remain educated and up to date on newer medications or less commonly
administered medications to learn how they are safely delivered to patients before
being asked to do so in clinical practice.If a prescriber’s order does not designate a route of administration, the nurse
consults the prescriber. The nurse should alert the prescriber immediately if the
specified route is not the recommended route and he/she must report immediately
if an error occurs in the medication. The nurse must know and must be familiar with
the abbreviations used to designate the route of administration.Right time: Medications can be given to patients in different many ways, all of
which vary in the time it takes to absorb the chemical, time it takes for the drug
to act, and potential side-effects. Certain drugs have specific intervals or window-
periods during which another dose should be given to maintain a therapeutic effect
or level.Often, a guiding principle of this ‘right’ is that medications should be prescribed as
closely to the time as possible, and nurses should not deviate from this time by
more than half an hour to avoid consequences such as altering bioavailability or
other chemical mechanisms. Similarly, it is crucial that medications that are given
by an infusion, such as intravenous medications, are administered at the correct
rate.Failure to deliver a drug at the correct rate may lead to devastating consequences
for a patient. For example, vancomycin requires administration by slow intravenous
infusion to avoid a complication known as “red man syndrome,” a hypersensitivity
reaction that is managed by further slowing the infusion rate of vancomycin or
discontinuing the agent altogether.The administering medications at a time that was intended by the prescriber. The
nurse must Read the physician’s orders, know the hospital routines for the interval,
know the abbreviations for the time, give the medicine near the time ordered,
give the medicine as ordered in relation to the food intake and give the medicines
according to the actions expected. E.g., sleeping pills are given at bedtime.Right dose: Incorrect dosage, conversion of units, and incorrect substance
concentration are a prevalent modality of medication administration error. This error
type stems from nurses giving a patient an incorrect dose of medications, even if it
is the correct medication and the patient’s identity is verified, without first checking
to ensure it is the correct strength for the patient. This error type may be due to
misplaced decimals, errors in arithmetic, or incorrect conversion between two units.The nurse must have adapted observing positive behaviors to reduce medical
errors include consulting with pharmacy personnel, read physician orders to know
the correct dose, consider the age and weight of the patient, know the minimumand maximum dose of the medicine administered, using calculators to assist in
arithmetic, or in some cases, cross-consulting with patients or their families about
usual doses they administer at home. Use ounce glasses instead of teaspoons to
measure ounces accurately, have written order before you prepare the drug, avoid
conversation or anything that distracts the mind.Right Documentation: Medication error can result from inaccurate documentation.
Nurse should ensure appropriate documentations clearly reflect the client’s name,
the name of the ordered medications, the time the medication was administered, the
medication’s dosage, route, the date or the method of administration, frequency, the
signature of the physician, and Standing orders or routine medication orders. If any
of this information is missing the nurse should verify the order with the prescriber.After the administration of any drug, record the process immediately. Immediate
documentation is particularly important when drugs are given on an as-needed
(PRN) basis. For example, most analgesics require 20 to 30 minutes before the
drug begins to relieve pain.A patient may forget that he or she received a drug for pain, may not understand
that the administered drug was for pain, or may not know that pain relief is not
immediate, and may ask another nurse for the drug again. If the administration
of the analgesic was not recorded, the patient might receive a second dose of
the analgesic shortly after the first dose. This type of situation can be extremely
serious, especially when opioids or other central nervous system depressants are
administered. Immediate documentation prevents accidental administration of a
drug by another individual and it is essential to the process of administering drugs
correctly.Right Response refers to the drug and its desired response in the patient.
Continually assess and evaluate the achievement of the desired response, as
well as any undesired response. Examples of data gathering include, but are not
limited to, monitoring vital signs, weight, oedema, intake and output, nutritional
intake, laboratory values, results of diagnostic testing, and auscultating heart and
lung sounds. Document any assessment, intervention, and monitoring as deemed
appropriate.Right to Refuse: The ninth right is that of the right of the patient to refuse. Patients
refuse medications for a variety of reasons. If refusal of a medication occurs,
always respect the patient’s right (to refuse), determine the reason, and take
appropriate action, including notifying the prescriber. Do not force! Document the
refusal and a concise description of the reason for refusal. Document any further
actions you take at this time, such as vital signs and/or system assessment. If
a consequence to the patient’s condition and/or as hospital policy dictates, the
prescriber is to be contacted immediately. Never return unwrapped medication to acontainer, and discard medication dose according to agency policy. If the wrapper
remains intact, return the medication to the automated medication-dispensing
system. Revise the nursing care plan as needed.Right evaluation: The health professional after administrating the medications to
the client must ensure the medication is working the way it should, ensure that the
medications are reviewed regularly and the ongoing observations if required to
detect early any sides’ effect or adverse effect associated with the taken medication.Self- assessment 3.1
1. What are the two methods a nurse can use to identify the right patient
before the drug administration?2. What does the nurse have to do if the patient refuses to take the prescribed
medications?3. Which of the following options addresses the appropriateness in use of
the medication to the patient?
A. Right indication
B. Right evaluation
C. Right documentation
D. Right to refuse4. You have been instructed to administer an oral medication (Ranitidine
150mg) to a patient. What is the minimum of times the nurse should
check the medication label before administering this drug?
A. One
B. Two
C. Three
D. Four3.2 Compliance/adherence to drug regimen
Learning activity 3.2
You are at the healthcare facility where you are carrying out a clinical attachment
as a requirement to complete your associate nursing program. A 41-year-old
female patient comes 10 days after interrupting his antiretroviral treatment.
While discussing with the patient, she reveals that she delayed to come to get
antiretroviral medications because the time of appointment coincided with the
time she had no money, and as she lives far, she could not travel to the health
facility. In your understanding, you realize that the patient was limited by the
financial constraints.
1. How can you define the word “drug adherence?”
2. What are the 5 factors (dimensions) that can lead to poor drug adherence
and compliance as stated by the World Health Organization?CONTENT SUMMARY
Adherence describes how a patient follows a medical regime recommended by
a healthcare provider. Poor treatment adherence represents a complex and
challenging problem of international healthcare systems, as it has a substantial
impact on clinical outcomes and patient safety and constitutes an important
financial burden. Since it is one of the most common causes of treatment failure, it
is extremely important for physicians to reliably distinguish between non-adherence
and non-response.Three different terms are used in the literature to describe to which extent a patient’s
behaviour corresponds with the advice given by a healthcare provider: Compliance,
adherence and concordance. These three terms are often used interchangeably,
but they reflect different philosophies of the physician-patient relationship. It can
be difficult to accurately compare studies on this topic, since the terminology used
differs amongst authors. Until around 2003, the term compliance was most widely
used in the literature. Compliance implies an authoritarian, asymmetric physician-
patient relationship, in which the doctor has the exclusive decisional power.
Physicians give instructions and patients are passive recipients and should follow
the prescribed regime without deviation.The word compliance may have negative connotations as it requests a submissive
and obedient patient. The concept of an appropriate physician-patient relationship
has substantially changed in the last years, since patients have gained more
autonomy. This paradigmatic shift is reflected by the new term adherence, which
is nowadays preferably used. The concept of adherence is based on a partnership
between physician and patient, where both parties are actively involved in findinga mutual treatment agreement. The word concordance, which originated in British
literature, goes even further and places the patient in the centre of the decision-
making process. It focuses less on compliance and more on overall success of
treatment as a shared goal.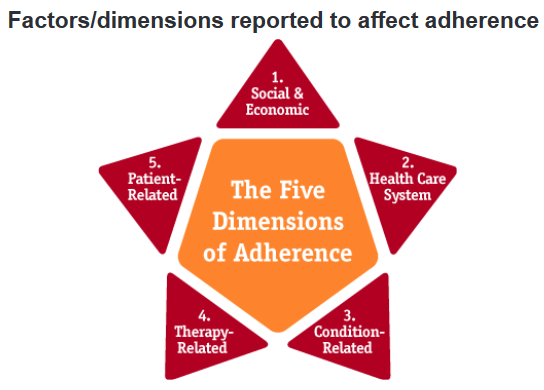
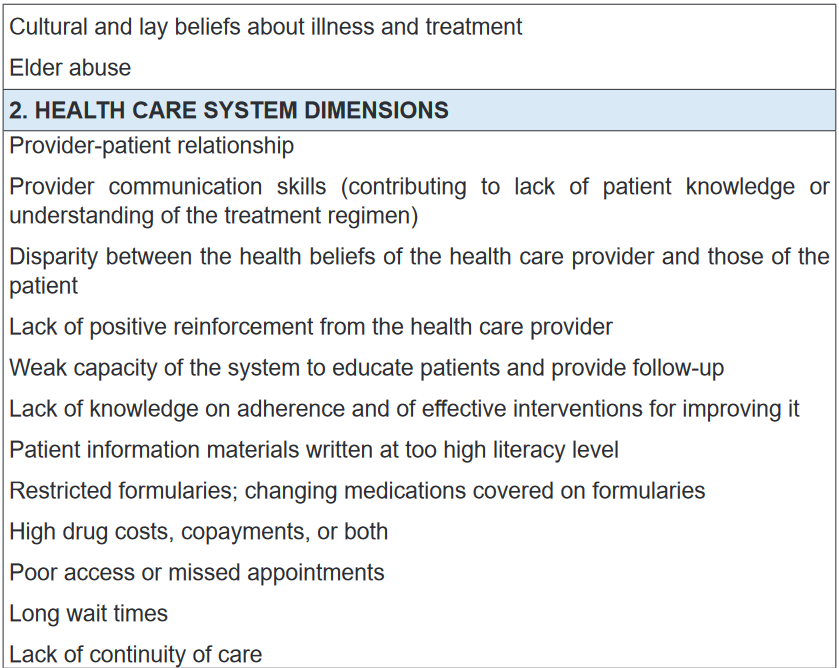
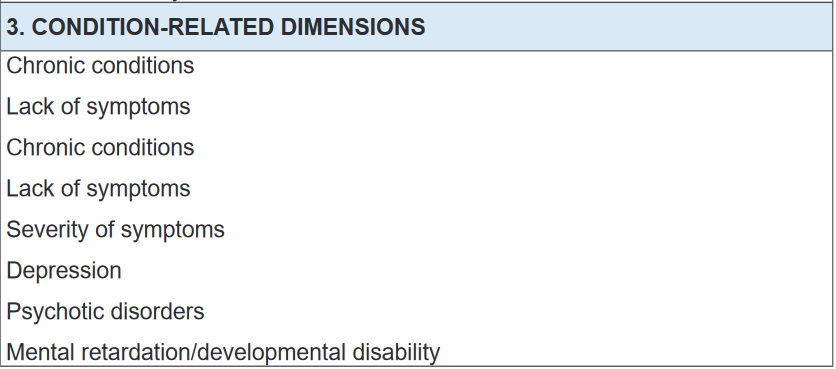
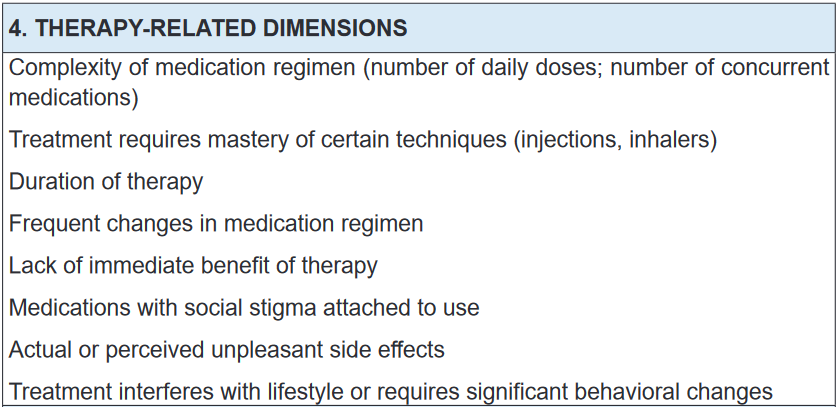
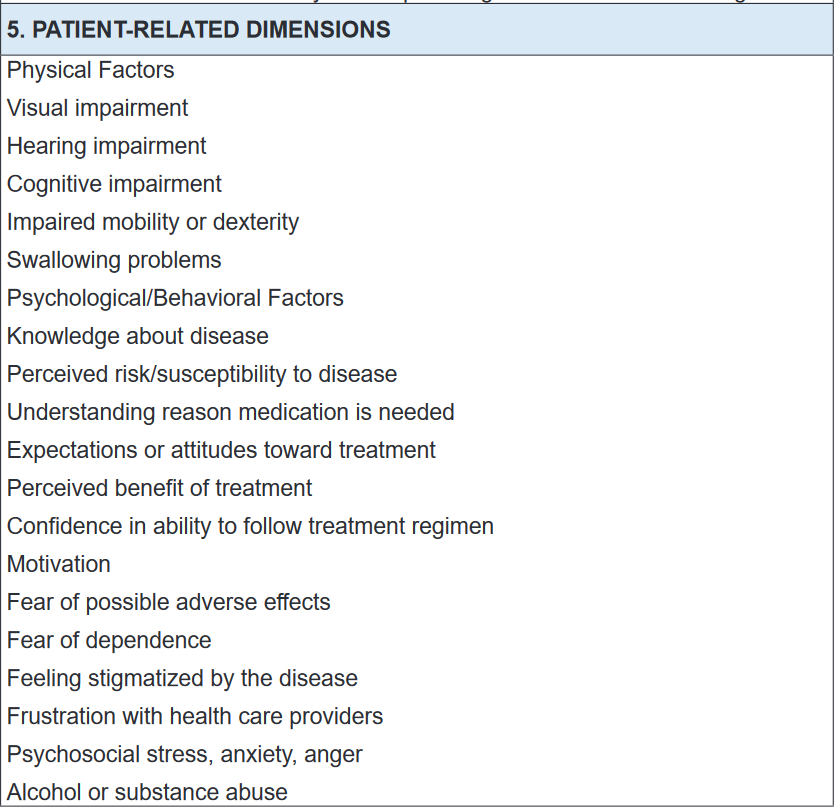
Adherence is a multidimensional phenomenon determined by the interplay of five
sets of factors, termed “dimensions” by the World Health Organization:
1. Social/economic factors
2. Provider-patient/health care system factors
3. Condition-related factors
4. Therapy-related factors
5. Patient-related factors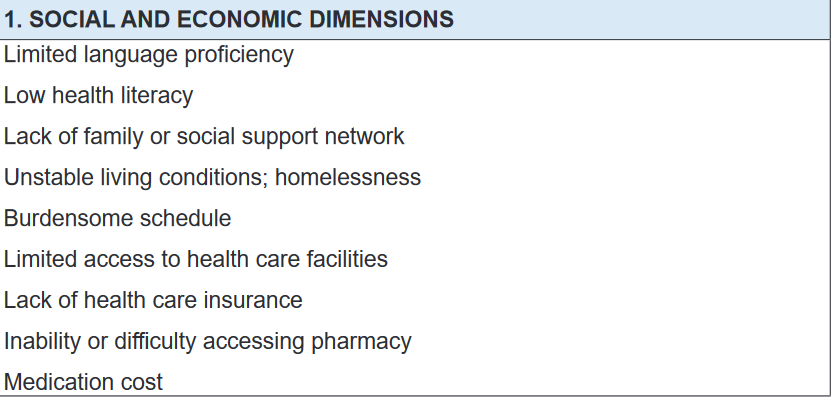
Self- assessment 3.2
1. Enumerate patient-related factors affecting adherence to medications.
2. The term “Adherence to drug regimen” has negative connotations
as it requests a submissive and obedient patient. It is nowadays less
preferable, and was replace by the term “Compliance.” TRUE or FALSE3. In patient adherence to drug regimen, concordance implies an
authoritarian, asymmetric physician-patient relationship, in which the
doctor has the exclusive decisional power. TRUE or FALSE3.3 Drug storage
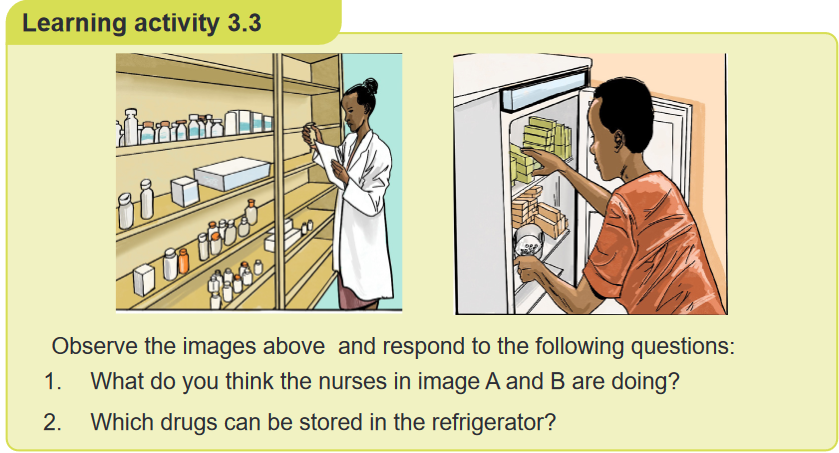
CONTENT SUMMARY
Drugs and biologicals are to be stored in a secure and orderly manner under proper
temperatures and are to be accessible only to licensed nursing and pharmacy
personnel. All medications are to be stored in the containers in which they are
received, internals separately from externals and both separately from poisons.Medications received from the Pharmacy should be stored in a secure location
that is out of reach from children. Medications that are dispensed in vials, such
as tablets and capsules, should not be placed in bathroom or kitchen cabinets
where it may be subjected to high humidity. Most medications can only be stored at
room temperature, but some medications may require refrigeration or other storage
requirements. Please consult with your pharmacist if you are unsure.The drugs which are supplied to ward are stored in drug cupboards to provide a
uniform supply of drugs to the patients. The drugs are stocked in containers, such
as boxes and on flexible racks and shelves etc. It must be ensured that drugs which
are stored remain preserved during their storage. There should not be any damage
due to high temperature or exposure to sunlight. The drugs are to be stored as per
the prescribed conditions of their storage. The drugs stored in a drug store should
be arranged in such a way that they are easily traceable when required.Drugs can be stored:
1. According to pharmacological action or
2. AlphabeticallyFactors that govern storage of drugs
Proper drug storage
Storage Environment
Arrangement of drugs on shelves
The storeroom
The dispensaryA. Proper drug storage
Drugs are stored in a specially designed secure area or space of a building in order
to:
• Avoid contamination or deterioration,
• Avoid disfiguration of labels,
• Maintain integrity of packaging and so guarantee quality and potency of drugs
during shelf life,
• Prevent or reduce pilferage (stealing things of small value), theft or losses
• Prevent infestation of pests and vermin.The storage should not hinder the cleaning and should have sufficient space for
movement of stocks and handling. Products are to be stored in a manner that
prevents damage due to excessive vertical stacking heights and not to exceed
eight stacks.Store the products as per product storage condition (As per label) to prevent
deterioration of finished product on storage. Monitor and record the temperature of
storage area on daily basis.B. The storage environment
The storage environment should possess the following:
• Adequate temperature,
• Sufficient lighting,
• Clean conditions,
• Humidity control,
• Cold storage facilities, and
• Adequate shelving to ensure integrity of the stored drugs.Drugs to be stored under condition that prevents contamination & as far as possible,
deterioration. They must be “Well closed container” precautions to be taken in
relation to the effects of the atmosphere, moisture, heat & light. “Protected from
moisture” means that the product is to be “stored in air tight container”. “Protected
from light” the product is to be stored either in a container made of material that
absorbs actinic light sufficiently to protect the contents from change induced by
such light. Temperature: In a deep freeze (-15°C), in a refrigerator 2°C-8°C, Cold
or cool 8°C-15°C and Room temperature15°C-25°C.Drugs stored in the medicines refrigerator include: vaccines; insulin; chemotherapy
drugs; topical preparations, such as some types of eye drops; and other treatments
such as glucagon, which is used to manage severe hypoglycaemia.Storage premises: The Storage area must be free from unsanitary conditions (Ex
Rodents, insects, Birds). The floor of the warehouse should be made of hard floor
(Concrete /Kota/Epoxy) and must be in a good state of repair and appearance at
all times. The floors are kept clean and free of trash, dirt, spillage water, drain water
etc. The area must be kept clean. The area used for storage of IV fluids should
have adequate space and to prevent exposure to direct sunlight. Secured area
availability for damaged, rejected and expired goods. Ensure adequate pest control
program in place and shall be carried out at a minimum frequency of a year. The
Pest control shall cover treatment for Termite and Rodents.C. Arrangement of drugs on shelves
Shelves should be made of steel or treated wood. Shelves should be strong. Drugs
are arranged in alphabetical order of generic names. Each dosage form of drug is
arranged in separate and distinct areas. Most recently received drugs are placed
behind old stock on the shelf except where new drugs have shorter expiration dates.
Always put lids properly on tins always and at the close of the day. Put drugs in a
dry place protected from light and heat. Store liquids on a pallet on the floor or on
the lowest shelf. The store must be cleaned daily and mopped at least once a week.D. The store room
A well-arranged store enables easy identification of drugs and saves time when
picking a drug from the shelves. This helps remove drugs quickly and makes for
easy inventory control. The rule of FIRST IN FIRST OUT (FIFO) should be applied
always. So, drugs that were received first should be used first, because the old
stock has shorter expiration dates than the new stock.In this regard, the principle of FIRST TO EXPIRE FIRST OUT (FEFO) should apply.
To have access to drugs with shorter expiration dates, put these in front of the
shelves. Those with longer expiration dates should be placed behind those with
shorter dates.E. The dispensaries
Clean after each use tablet counters and place within easy reach on the table.
Avoid dispensing wrong drugs by arranging drugs on the table in alphabetical
order so that the drug being dispensed is not confused with another. Always close
drug containers from which drugs are not being dispensed to prevent spillage or
dispensing the wrong drug. Medications must not be administered, and products
and equipment must not be used beyond their expiry dates. All medical equipment,
dressings and solutions used during invasive procedures must be sterile. Single-
use devices are meant for single use only and must not be re-used.Storage, maintenance and security: All drugs, including samples, should be
maintained separate from non-medications in a locked cabinet which is sufficiently
secure to deny access to unauthorized persons. Key should be available only to
authorized personnel who are assigned medication-related responsibilities. Store
medications that are “for external use only” separate from medications intended for
internal use. Store look-alike and sound-alike drugs (LASA) separately. Maintain
temperature between 59 degrees and 86 degrees Fahrenheit for non-refrigerated
medications. Where refrigeration is necessary use a “Medications Only” refrigerator
and maintain temperature between 36 degrees and 46 degrees Fahrenheit.On daily basis check, verify and document the proper temperature. All multiple-
dose injectable medications should be initialled and have the date of first entry
recorded on the label. Rotate medication stock monthly employing a “FIFO” (first
in/first out) process.Controlled drug regulation.
• Double locked container, and 2 licensed personnel count (or verify any
discrepancies) every shift (8 hours)• Witness to all discards
• Record on Control Substance Sheet all administrations and wastes
All details must be completed in the doctors own handwriting, like: Name of drug,
Dose of drug, Number of doses or length of course, Signature of prescribing doctor
and date.Storage of controlled drugs
They must be kept in a locked cabinet or cupboard. The keys to the cabinet must
be in the possession of an authorised person. Authorised person refers to ward
manager or deputy who must be a trained nurse or midwife. Students should not be
responsible for the controlled drug cupboard keys.Recording of controlled drug use: Records in the form of CONTROLLED DRUG
REGISTERS must be kept. Each drug must have its own specified page which is
headed with the drugs name and strength. The number of ampoules of a drug must
be entered and updated with every use.Must record: ü Date ü Time ü Dose of every administration ü Name of receiving
patient/client ü Number of ampoules at start and finish of administration Entry
must be signed by 2 people one of who must be registered.Self- assessment 3.3
1. What are the 5 factors that govern the storage of drugs?
2. In order to prevent damage of stored drugs, what is the number of stacks
that should not be exceeded in case of vertical stacking?
A. Two stacks
B. Twenty stacks
C. Eight stacks
D. Fifteen stacks3. How should the nurse arrange medications in the store room to ensure
the FIRST TO EXPIRE FIRST OUT (FEFO) principle?4. What are the characteristics of drug storage environment?
3.4 Enteral routes of drug administration
Learning activity 3.4
A 50-yaer-old female patient consults the health facility where you are carrying
out the clinical placement, for the follow up of her chronic disease. She used
to be taking insulin for type 2 diabetes mellitus, and her glycemia has become
stable so that she can shift to non-injectable forms. Your colleague in associate
nursing program carrying out the clinical placement at the same health facilty
wants to shift from injectable from to enteral routes, but she does not remember
what an enteral route is.A. How can you define an enteral route of drug administration to your
colleague?B. What are different types of enteral routes of drug administration would
you tell your colleague?C. Which enteral route poses a greater risk of first-pass effect (first
metabolism)?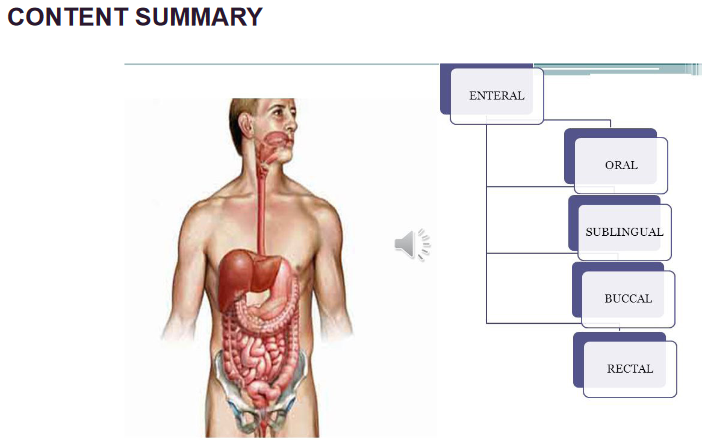
Routes of drug administration are the medium through which the drug is introduced
into the body to show its pharmacological action or for diagnosis. They are generally
classified by the location at which the substance is applied or based on the target
of action is. Route of administration and dosage form are the main aspects of drug
delivery. Enteral administration is the involvement of the gastrointestinal tract
and is further classified as follows: Oral Administration, Buccal or Sublingual
Administration, and Rectal route.i) Oral Administration
It is the first choice for the administration of drugs. It is designated as Per Os (PO),
which means to administer by mouth. The absorption of drugs administered by
this route is determined by the physiological state of the GI tract. Types of dosage
forms administered through this route include pills, tablets, capsules, solutions,
suspensions, emulsions, syrups, elixir, etc.Advantages: Most Convenient and cost-effective. Safest and painless. Self-
administered. No sterilisation required.Disadvantages: Not suitable for an emergency as the onset of action is slow. Not
suitable for unconscious patients, uncooperative and unreliable patients. For drugs
with extensive first-pass metabolism, this route is not used. Unpalatable and highly
irritant drugs are not suitable.ii) Buccal or Sublingual Administration
Sublingual administration involves placing the drug under the tongue. Buccal
administration involves placing the pill between the gums and cheek wherein both
the cases, the drug is absorbed into the blood. The types of dosage forms for this
route include tablets, troches and lozenges. Examples- Nitroglycerin.
Advantages: Economic & Quick drug absorption. Bypassing the first-pass
metabolism. Quick termination-spit off. Self-administered. Increased bioavailability.Disadvantages:
Not suitable for bitter and irritating drugs. High doses can’t be taken.
Less patient compliance. Highly ionic drugs cannot be administered.iii) Rectal route
Rectal medicines are administered through the anus, into the rectum. The types
of dosage forms for this route include suppositories and enemas Ex: prednisolone
enema, indomethacin, diazepam.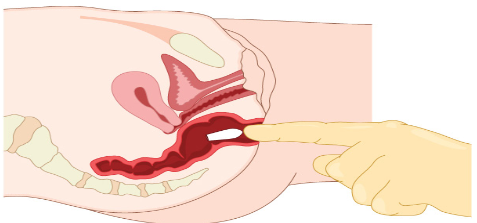
Advantages: It avoids the first-pass metabolism. Suitable for children and old age.
It is used for unconscious and vomiting patients. Irritating drugs are contraindicated.Disadvantages: Absorption is slow and erratic. Not well accepted by patients.
Inconvenient.Self- assessment 3.4
1. Which of the following is an advantage of the oral route of drug
administration?
A. It is easily self-administered method;
B. Toxicity may be overcome with antidotes;
C. Drugs avoid first-pass metabolism;
D. Drugs go directly into the systemic circulation.3. All of the following are advantages of the rectal route of drug administration,
EXCEPT:
A. Suitable for patients with nausea or vomiting
B. Suitable for the young population (children)
C. Suitable for patients with unconscious state
D. Drugs are subject to first-pass metabolism.3. Pick out the appropriate alimentary route of administration when passage
of drugs through liver is minimized:
A. Rectal
B. Sublingual
C. Oral
D. Intraduodenal4. The oral route of drug administration is suitable for an emergency situation
as the onset of action is rapid. TRUE or FALSE3.5 Parenteral routes of drug administration
Learning activity 3.5
A 20-year-old male patient is admitted in the healthcare facility for an infectious
bacterial disease. The assessment reveals that the patient must be given
the tablets to swallow twice a day with plenty of water. After 2 days of
the treatment, the nurse realizes that the patient vomits all the drugs he
takes, and the nurse needs to shift to another route that would help to
ensure that all the drug is taken into the patient’s body. The nurse then
asks you a question regarding the alternative routes she should use to
ensure that the drug is not vomited.
1. Which routes would you advise to the nurse to use?
2. Which angles of the needle would you respect while administering drugs
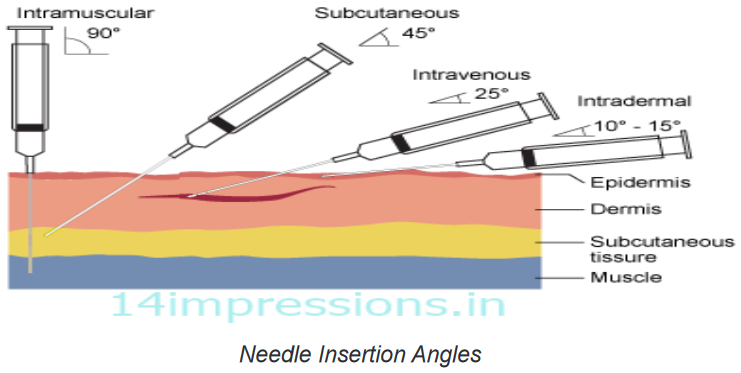
via the 4 main routes?CONTENT SUMMARY
During patient care, some medications can be administered by parenteral routes.
The word parenteral is derived from Greek word “para” which means outside and
“enter one” which means the intestine. These are the injection or infusion through
a needle or catheter into the body. This route helps bypass the alimentary canal.
The injection is the act of putting a liquid, especially a drug, into a person’s body
using a needle and a syringe. Injections are classified as follows:a. Subcutaneous route/injection
The drug is deposited just beneath the skin in the loose subcutaneous tissue. As
it is less vascular, absorption is slow, so prolonged action is produced. Only small
volumes can be injected. The needle is injected into the pinched skin at 90-degree
angle and do this quickly without force. If you have very little fat, then inject at a
45-degree angle. In addition to injection, it is also possible to slowly infuse fluids
subcutaneously in the form of hypodermoclysis. A subcutaneous route is used for
protein drugs because such drugs would be destroyed in the digestive tract if they
were taken orally. Certain drugs (progestins for hormonal birth control) may be
given by inserting capsules under the skin.Advantages: Onset of action is faster than oral route.
Disadvantages: Sterile technique is needed. More expensive. Some drugs can
irritate tissue and cause pain. Only small volumes must be administered.
Various forms of subcutaneous (SC) route are: Dermojet, Pellet and Sialistic (non-
biodegradable and biodegradable implants).Dermojet: It is a needleless injection system with a high-pressure jet injector. A
high velocity of drug solution is projected from a fine micro orifice using a GUN like
an implant; the solution passes through the superficial layers and gets deposited
in the subcutaneous tissue. It is nearly painless and suitable for mass inoculations.
E.g. Insulin.Pellet: Drug in the form of solid pellet is introduced with TROCHAR and CANNULA
which provides sustained release of drug for weeks and months without repeated
administration.E.g. DOCA, TESTOSTERONE.
Sialistic (non-biodegradable or biodegradable): Crystalline drug is packed in tubes
or capsules and implanted under the skin. Slow and uniform release of drug for
months with constant blood levels (non-biodegradable drug have to be removed
later). E.g. hormones and contraceptives like “NoRPLANT”.b. Intravenous route/injection
Method of administering medications directly into the vein using a needle. It is
the best way to deliver a precise dose quickly and in a well-controlled manner
throughout the body. Drugs are delivered immediately into the bloodstream and
tend to take effect more quickly than any other route. Hence it is of great value in an
emergency. A 25-gauge needle 2 cm long with 25-degree angle is inserted into the
skin. It is also used for irritable solutions which cause pain and damage to tissues if
given by subcutaneous or intramuscular injection. A solution containing a drug may
be given in a single dose, or continuous infusion from a collapsible plastic bag or
infusion pump through thin, flexible tubing inserted to the vein, usually a forearm.
Vital organs like heart, brain etc. get exposed to high concentrations of the drug.Advantages: Rapid onset of action. It bypasses the GI and first-pass metabolism.
Useful for drugs which are irritant to intramuscular route.Disadvantages: Administered by trained person. Accidental overdose can have
serious consequences. Limited to highly soluble drugs. Break of
skin barrier.c. Intramuscular route/injection
The drug is injected into one of a large skeletal muscle such as triceps and rectus
femoris among others. It is a preferred route when larger volumes of a drug product
are needed. It is more vascular; hence absorption is faster and less painful. The
angle for IM is 90 degrees. DEPOT preparations (oily solutions and aqueous
suspensions) can be injected by this route. Muscle permits the tissue to receive a
larger volume of medication (deltoid and biceps maximum of 3ml).NOTE: IM injections should be avoided in anticoagulant treatment patients as it can
produce Local haematoma.Advantages: Can administer larger volumes. Technically easier than IV. GI and
first-pass metabolism are involved.Disadvantages: Break the skin barrier, produce anxiety and painful.
d. Intradermal route/injection
The drug is delivered in the upper layer of the skin to the dermis, where the
absorption is low. The angle for ID is 5 to 15 degrees with a needle placed almost
flat to the skin. It is the common method used for allergy testing. Injections are
made with fine short needles (26 gauge) and a small barrel syringe.Advantages: Absorption is low, advantage for allergy testing.
Disadvantages: Amount of drug administered must be small.
The above are the 4 main routes. The following are other parenteral routes,
less commonly used.e. Intra Arterial route/injection
Intra Arterial injection or infusion is a method of delivering a drug directly into arteries
to localise its effect to a particular organ/region while minimising the exposure of the
body to potentially toxic effects of the agent.Advantages: Used in chemotherapy to target drug organs.
Disadvantages: Drugs may be distributed to other tissues or organs.
f. Intra Articular route/injection
It is the injection which is directly delivered into the joints to relieve pain and swelling.
Most of the anti-inflammatory drugs for arthritis treatment are given by this route.Advantages: High concentration is obtained in localized areas. Rapid onset of
action.Disadvantages: Sepsis and joint damage may occur on repeated drug
administration.g. Intrathecal route/injection
Intrathecal administration is a route for drugs via an injection into the spinal canal,
or into the subarachnoid space so that it reaches the cerebrospinal fluid (CSF) and
is useful in spinal anaesthesia, chemotherapy & pain management applications.Advantages: Drugs act directly on meninges and CNS. Bypass BBB & Blood-CSF
barrier.
Disadvantages: Painful procedure. Expertise neededSelf- assessment 3.5
1. Parenteral routes of drug administration are:
A. Intravenous, intramuscular, subcutaneous
B. Intravenous, intramuscular, intranasal
C. Intravenous, sublingual, transdermal
D. Transdermal, subcutaneous, by inhalation2. All of the following are the disadvantages of intravenous drug
administration, EXCEPT:
A. A trained staff is required to administer the drug
B. Its use is limited to highly soluble drugs.
C. Accidental overdose can have serious consequences
D. Drugs undergo first-pass metabolism in the liver3. Which of the following is the correct angle to use while administering the
drugs intramuscularly?
A. 75%
B. 50%
C. 90%
D. 45%4. Which of the following statements best defines the intradermal injection?
A. The drug is delivered in the upper layer of the skin to the dermis, where
the absorption is low
B. The drug is injected into one of a large skeletal muscle such as triceps
and rectus femoris
C. Intrathecal administration is a route for drugs via an injection into the
spinal canal, or into the subarachnoid space
D. Method of administering medications directly into the vein using a
needle and a syringe3.6 Topical routes of drug administration
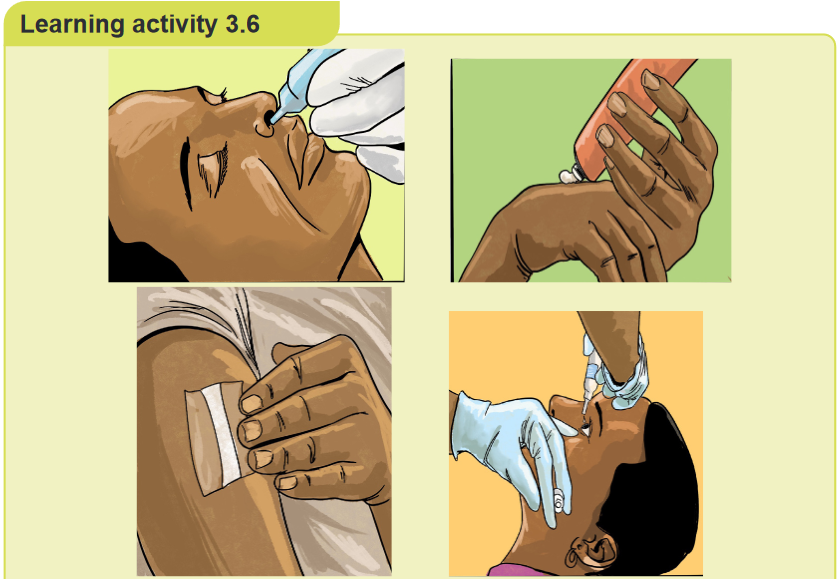
Observe the images above (A, B, C, D), and answer the questions below
pertaining to them:
1. What do you observe on these images (ABCD)?
2. What are the benefits of using the route of drug administration in the
images above?CONTENT SUMMARY
The topical route includes: skin, eyes, or other specific membranes, the intranasal,
inhalation, intra-vaginal. The medication is applied directly to the body surfaces,
including the skin and mucous membranes of eyes, ears, nose, vagina and rectum.
Ex: Antibiotics, hormones, narcotics and chemotherapeutics.The definition of the topical route of administration sometimes states that both the
application location and the pharmacodynamic effect thereof is local.In other cases, topical is defined as applied to a localized area of the body or to
the surface of a body part regardless of the location of the effect. By this definition,
topical administration also includes transdermal application, where the substance
is administered onto the skin but is absorbed into the body to attain systemic
distribution.BENEFITS OF THE TOPICAL ROUTE OF DRUG ADMINISTRATION
Medications delivered via the topical route offer a whole host of benefits. Here are
five benefits of using a topical drug delivery system.1. Alternative to oral administration
Many patients struggle with oral drug administration. Some risk vomiting, while
others find swallowing pills a near-impossible task. Consequently, if an orally
administered drug is rejected, this reduces a drug’s effectiveness, prolonging the
ailment. This problem is most common in infants or young children who are not
used to swallowing tablets. Parents often find it difficult to get their children to take
medication. Commonly, this results in wasted doses and slower recovery times. By
using a topical medication, parents may be able to avoid these problems and help
their children feel better more quickly.2. Fewer risks of gastrointestinal difficulties
Different individuals absorb medication at different rates. Oral medications can
cause a variety of digestive side effects. Patients who experience these often
painful side effects may opt to terminate their medication. A topical drug delivery
system overcomes this limitation, improving the patient’s recovery process.3. Fewer risks of abuse
Medication administered through tablets or injections can easily be abused. Drug
abuse by patients is far too common, especially with pain medications. Such
abuse can lead to addiction. On the other hand, administering medication through
ointments or creams greatly lowers the risk of abuse. Topical medications not only
help doctors and patients manage ailments, but also help to prevent the problem
of drug abuse.4. Easy to administer
Almost everyone has a fear of something. Some people are afraid of injections or of
swallowing tablets, but few are fearful of rubbing an ointment on their skin. For this
reason, doctors find it easier to encourage their patients to take their medication
when using a topical drug delivery system. The patient can easily manage the
medication at home.5. Reduced hospital congestion
Previously, hospitals administered many medications by injection, filling their beds
to capacity. Today, if the patient condition isn’t serious, the patient can walk into a
hospital and walk out again a short time later with topical medication. This leaves
hospital beds free to cater to more serious cases and reduces both hospital and
patient medical costs.Innovating with topical drug delivery
The increased adoption of topical medication in recent years has been impressive.
This is largely due to the fact that the medication has proven to have more
advantages than drawbacks. After all, the skin is ideal for drug administration, as it
produces both systematic and local effects.Call it a life-changing medical innovation. Topical drug delivery systems have
surely changed the way we look at medication. More and more medical institutions
and health practitioners are adopting this form of medication in an attempt to improve
their services to patients. This medical breakthrough offers a future of health care
that is definitely more effective and agreeable for patients.Some types of topical routes of drug administration
Inhalational route
Inhaled medications can be absorbed rapidly and act both systemically and locally.
A proper technique with inhaler devices is necessary to achieve the correct dose.
Total size absorbed is variable. Nasal Inhalations, Inhalation by smoking a substance
is likely the most rapid way to deliver drugs to the brain, as the substance travels
directly to the brain without being diluted in the systemic circulation. The severity of
dependence on psychoactive may increase with more rapid drug delivery.Advantages: May be used for local or systemic effects.
Disadvantages: Particle size of drugs determines anatomic placement in
the respiratory tract. May stimulate cough reflex. Some drugs may be swallowed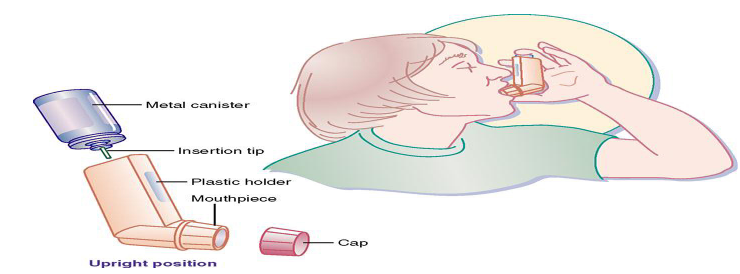
Transdermal route
Transdermal administration is a route wherein active ingredients are delivered
across the skin for systemic distribution of the drug. E.g. Transdermal patches. The
drug is administered in the form of a patch or an ointment that delivers the drug into
the circulation for systemic effect. The absorption rate may vary. It is slow. Increased
absorption with occlusive dressings. Formulations and devices for transdermally
administered substances include: Transdermal pathways are those by which drugs
can cross the skin and reach the systemic circulation. Ex: Transcellular pathway,
Intercellular pathway, Microneedles. The more direct route used is known as the
transcellular pathway.Advantages: The transdermal delivery system (patch) is easy to use and withdraw.
Continuous release of the drug is observed for a specified period of time. It is used
for lipid-soluble drugs with a low dose and low molecular weight. Low pre-systemic
metabolism.Disadvantages: Some irritation by patch or drug. Permeability of skin is variable
with the condition, anatomic site, age and gender. Type of cream or ointment base
effects the drug release and absorption.Self- assessment 3.6
1. What are the advantages of administering the drugs by the inhalational
route?2. What are the disadvantages of administering the drugs by the inhalational
route?3. Transdermal administration is a route wherein active ingredients are
delivered to the body through an injection in the upper layer of the skin.
TRUE or FALSE4. What are the advantages of administering the drugs by the transdermal
route?3.7 Introduction to medications errors and classification
of medication errorsLearning activity 3.7
A 33-year-old male patient is admitted to the hospital where he is being treated
with injectable antibiotics. In addition, the patient is receiving two tablets of pain
medication every 6 houurs. The nurse on the night shift realizes that the patient
received 2 tablets at the latest as indicated. The nurse on the night shift finally
realizes that it is the dose that was prescribed for the patient as it appears in the
treatment sheet, but after keen search, he realizes that the patient should be
taking only 1 tablet for pain medication every 12 hours, instead of 2 tablets every
6 hours. The nurse then withholds the dose, documents it and gets the view from
the working team.1. What type of medication error was committed for this patient?
2. What are other types of medication errors according to their categories
or classification?3. What is the definition of a medication error?
CONTENT SUMMARY
Medicine errors cause considerable patient morbidity, mortality and increased
healthcare cost. The most common used definition is that given by the National
Coordinating Council for Medication Error Reporting and Prevention (NCCMERP)
in the USA, which defines medication errors as: “Any preventable event that may
cause or lead to inappropriate medication use or patient harm while the medication
is in the control of the healthcare professional, patient, or consumer.” The published
studies estimated that about 5—10% of hospital admissions were due to the
medication errors. It is suspected that approximately 3% of deaths in the Swedish
population are because of the medication errors. In Canada, up to 50% of the
patient safety incidents in primary care are related to medication errors. Reporting
the medication error is one most effective strategy to improve patient safety. While,
these reports help to understand the medication errors contributing factors.Causes of Medication Errors
1. Expired Product: Usually occurs due to improper storage of preparations
resulting in deterioration or use of expired products.2. Incorrect Duration: Duration errors occur when medication is received for
a longer or shorter period of time than prescribed.3. Incorrect Preparation: This error usually occurs with compounding or
some other type of preparation before the final administration. An example
is choosing the incorrect diluent to reconstitute.4. Incorrect Strength: It may potentially occur at many points in the medication
process. It usually occurs due to human error when similar bottles or syringes
with the incorrect strength is selected.5. Incorrect Rate: Most often occurs with medications that are given as IV push
or infusions. This is particularly dangerous with many drugs and may result
in significant adverse drug reactions. Examples include tachycardia due to
rapid IV epinephrine or red man syndrome due to the rapid administration
of vancomycin.6. Incorrect Timing: In both home and institutional settings, it is challenging
to be completely accurate with scheduled doses. The concern is that some
medications absorption is significantly altered if taken with or without food.
As such, it is important to adhere to scheduled times as commonly; this may
lead to under or overdosing.7. Incorrect Dose: This error includes overdose, underdose, and an extra dose.
An incorrect dose occurs when an inappropriate or different medication dose
is given other than what was ordered, errors of omission when a scheduled
dose of medication is not given, and when a drug is given via an incorrect
route. Errors due to incorrect routes usually occur due to unclear labelling
or tubing that is adaptive to multiple connectors/lines of access. Incorrect
routes often result in result in significant morbidity and mortality.8. Incorrect Dosage Form: This occurs when a patient receives a dosage form
different than prescribed, such as immediate-release instead of extended-
release.9. Incorrect Patient Action: This occurs when a patient takes a medication
inappropriately. Patient education is the only way to prevent this type of
error.10. Known Allergen: Dispensing a drug that the patient has an allergy often
due to failure to communicate with the patient, inappropriate chart review,
inaccurate charting, or lack of technologic interface.11. Known Contraindication: This occurs when medications are not vigilantly
reviewed for drug-drug, drug-disease, or drug-nutrient interactions.Medication Errors Classification
Errors can be classified according to contextual categories; such as stage of
occurrence. So, in accordance with the medication use process, medication errors
can be classified as prescribing errors, transcription errors, dispensing errors,
administration errors or monitoring errors.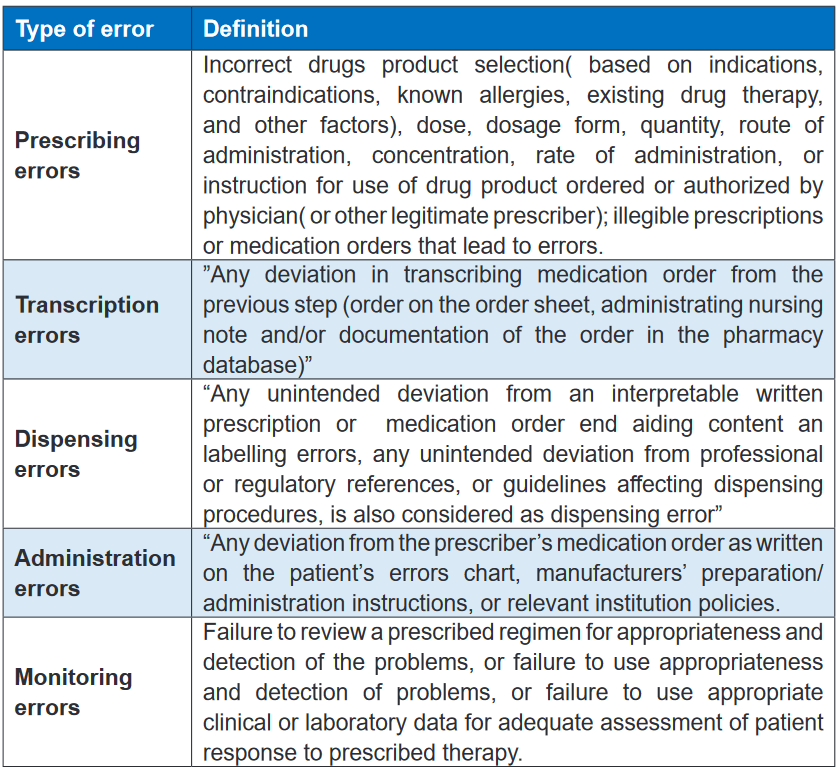
Self- assessment 3.7
1. What are the causes of medication errors?
2. In which of the following types of medication errors would a medication
error which involves incorrect drug product selection based on indications
be classified?
A. Prescribing errors
B. Transcription errors
C. Dispensing errors
D. Monitoring errors3. In which of the following types of medication errors would a medication
error which involves a failure to review a prescribed regimen for
appropriateness and detection of problems be classified?
A. Prescribing errors
B. Transcription errors
C. Dispensing errors
D. Monitoring errors3.8 Actions to take in case of medication errors, and use
of high alert medicationsLearning activity 3.8
A nurse is preparing to administer an injectable dug to patient. His colleague who
is an associate nurse says it is a high alert medication, and advises to check well
the prescription in order to avoid any risk of committing a medication error.
1. As a nurse student, how can you define a high alert medication?
2. What are the strategies to reduce errors involving High Alert Medications
on the aspect of their storage?CONTENT SUMMARY
Medication errors are a common finding in healthcare settings. The healthcare
providers need to take necessary measures in order to avoid or minimize the
medication errors. They do however often occur due to different circumstances.
When they do occur, the nurses as well as other healthcare providers must take
quick actions, and make sure they report that incident.Steps of Reporting Medication Errors
1. Any staff member who discovers a medication error whether it’s a physician,
pharmacist, or a nurse must be immediately complete the Medication Error
Report. The details include; patient name, hospital number, prescription
details, details of errors and any incorrect medicine or dose administered to
the patient2. When these details of errors are recorded on the form, the manager or
deputy need to identify those staff involved and explain the error to get them
and them write about the error causes any comments about the error. The
manager or deputy need to mention the immediate the action taken.3. Send the completed form to Pharmacy department in the hospital within
24 hours4. The Medication Safety Officer needs to complete the medication error
from such as assesses the incident severity, conduct Root Cause Analysis
if need (for all significant or potentially significant medication errors) and
suggest recommendation to reduce reoccurrence the error.5. The Medication Safety Officer needs to inform the Medication Safety
6. Medication Safety officer in the hospital needs to review all the medication
errors and to take the required action to avoid occurring similar errors in the
future.7. Forwarded to Total Quality Management (TQM) Department in the hospital.
GUIDELINES ON SAFE USE OF HIGH ALERT MEDICATIONS
High-Alert Medications are medicines that have high potential risk to the patient
when they are utilized in error. Although mistakes may or may not be common
with these medicines, the significances of an error are dearly more devastating to
patients.Examples: Adrenergic agonists. IV (E.g: Epinephrine, Norepinephrine,
Phenylephrine); Anaesthetic agents, general, inhaled and IV (e.g., Propofol,
Ketamine)• Hospitals and healthcare providers aim to provide high quality and safe medical
care to their patients, including the safe and effective use of medications.• These medications, however, can be compared to a two-edged sword: while
useful, they can also be harmful as a result of errors associated with their
use as well as from adverse events/effects especially with these medications
that have a very narrow margin of safety and can cause severe harm to the
patient.• These medications are recognized as High Alert Medications.
• The Institute for Safe Medication Practices has gathered a list of “high-alert”
medications. These medications require extra precaution because they have
highly potentially rich to the patient when used in error.Managing High Alert Medications
The pharmacy department in the hospital needs to provide general guidelines for
the proper handling of High Alert Medications including the medication list.Concentrated electrolytes (Potassium & Sodium Phosphate, Potassium Chloride,
and Sodium Chloride) are High-Alert Medications, so should not be stocked in the
patient care areas except as part of the crash cart medications. Limited quantities
of these concentrated electrolytes can be stocked in specific area such as ICU
(Intensive Care Unit) and ER (Emergency Room) and need to be kept in a separate
locker and away from the regular ward stock medications and should by monitored
frequently by nursing and pharmacy staff.Label all containers and shelves used for storing High Alert Medications as “HIGH
ALERT MEDICATIONS”High Alert Medications must be double checked before they are prepared, dispensed
and administered to the patientsThe Medication Safety officer in the hospital must be check if the staff commitment
to do the double check before they are prepared, dispensed and administered to
the patients.Strategies to reduce errors involving High Alert Medication
* Procurement
• Limit the drug strengths available in the hospital.
• Avoid frequent changes of brand or color and notify the other healthcare staff
if there are changes.
• Inform all relevant personnel regarding in the hospital about the new High
Alert Medications listed.* Storage
• Minimize High Alert Medications from clinical areas, where possible.
• High Alert Medication should be stored individually in separate labelled plastic
container.
• Label the shelves or containers used for storing Alert Medications as “HIGH
ALERT MEDICATIONS.”* Prescribing
• Avoid using abbreviations when prescribing High Alert Medications.
• Avoid ordering High Alert Medications verbally accept in case of emergency
orders.
• Prescribe oral liquid medications with the dose specified in milligrams.
• Avoid using trailing zero when prescribing (e.g. 5.0 mg can be mistaken as
50 mg)
• Reduce the total dose of High Alert Medications in continuous IV drip bags
(e.g., 12,500 Units of Heparin in 250 ml vs. 25,000 Units in 500 ml) to reduce
risk• Dispensing / Supply
All High Alert Medication containers, product packages, vials or ampoules issued
towards units need to have caution label “HIGH ALERT MEDICATIONS” except for
parenteral nutrition preparations.
Accuracy check performance must be applied for the High Alert Medications before
dispensing the medicines.GUIDE ON HANDLING LOOK-ALIKE & SOUND-ALIKE MEDICATIONS
The patient safety incidents are widely spread because the health services system
become more complex, due to new technologies, medicines and treatments
strategies.Currently, thousands of medications are available in the markets and in the hospitals.
Some of these medicines have similarity in the names or packaging. The evidences
show that Look-alike/sound-alike medicines names and packaging are one of the
most common contributed factors associated with medication errors.Look Alike Sound Alike (LASA) medications involve medicines that are visually
similar in physical appearance or packaging and names of medications that have
spelling similarities and/or similar phonetics.Contributing Factors
Several Contributing factors may lead to confusion with LASA medications,
these include:
• Illegible handwriting.
• Incomplete knowledge of drug names.
• Newly available products.
• Importantly, it has similar packaging or labelling.
• Similar strengths, dosage forms, frequency of administration.
• Finally, similar clinical useStrategies to avoid errors with LASA Medications
* Procurement
Minimize the availability of multiple medicines strengths
Whenever possible, avoid purchase of medicines with similar packaging and
appearance. As new products or packages are introduced, compare them with
existing packaging.* Storage
Use Tall Man lettering to emphasize differences in medications with sound-alike
names.Tall Man lettering (or Tallman lettering) is the practice of writing part of a medicines
name in upper case letters to help distinguish sound-alike/look-alike medications
from one another to avoid medication errors.Examples of Tall Man lettering are metFORMIN and metoPROLOL
Using caution red tag notes on shelves, in order to alert the dispenser that a
medicine has look-alike and sound-alike medicines.Using techniques such as boldface and differences to reduce the confusion
associated with the use of LASA names on labels in the medicine’s storage
containers and shelves.* Prescribing
Place LASA medications in locations separate from each other or in non- alphabetical
order.Write legibly, using both the brand and generic names for prescribing LASA
medications.Prescription should clearly specify name of medication, dosage form, dose and
complete direction for use.Write the diagnosis or medication’s indication for use. This information helps to
differentiate possible choices in illegible orders.In electronic prescribing system, using techniques such as Tall-man lettering,
boldface and color differences to reduce the confusion associated with the use of
LASA names on the computer screens and medication administration records.Communicate clearly. Take your time in pronouncing the drug name whenever an
oral order made.Ask that the recipient of the oral communication repeat the medication name and
dose.
Minimize the use of Verbal and Telephone orders.* Dispensing/Supply
Identify medicines based on its name and strength and not by its appearance or
location.Check the purpose of the medication and the dose for the medicines dispensed.
Read medication prescription and label carefully at all dispensing stages
Commitment to a final accuracy check by a qualified person, before handing over
the medicine to the patient or the patient’s representativeDouble check should be conducted at any stage during the dispensing and supply
process.Highlight changes in medication appearances to patients upon dispensing.
* Administration
Read carefully the medication labels each time during the administration process
Perform the double check to check actual medicine and compare it with the
prescription and label.
Check the purpose of the medication and the dose prior to administration.Self- assessment 3.8
1. How can you define Look Alike Sound Alike (LASA) medications?
2. How can you explain “Tall Man lettering” as a strategy to reduce the errors
associated with the use of LASA medications?
3. What are the strategies to avoid errors with LASA Medications during
their supply/dispensing?
4. What are the strategies to avoid errors with High Alert Medications during
their prescription?3.9 Systems of measurement used in pharmacology
Learning activity 3.9
You are carrying the clinical practice at a health centre. A mother brings her
24-month-old female child who has a lower respiratory infection. An oral liquid
antibiotic is prescribed, and the mother is instructed to give 5mL TDS. The
mother does not have a tool to accurately measure 5mL, and she admits to have
different materials meant for household measurement.
1. Which household measurement material equivalent to 5mL would you tell
the mother to use?
2. How many teaspoons are usually in one tablespoon?CONTENT SUMMARY
Introduction to measuring systems
One of the most essential functions of a health care professional is the ability to
perform accurate pharmaceutical measurements, calculations and conversions.
Without this ability, a health care professional is not able to apply their knowledge
of pharmacology in a practical manner during their everyday work functions. This
is important as one incorrect calculation, conversion or measurements will affect
a dosage, and can potentially harm a patient. Possessing a working knowledge
of the pharmaceutical systems of measurement will only benefit a pharmaceutical
professional.At least four different systems are currently used in drug preparation and delivery:
the metric system, the apothecary system, the household system, and the
avoirdupois system. With the growing number of drugs available and increasing
awareness of medication errors that occur in daily practice, efforts have been
made to decrease the dependence on so many different systems. In 1995, the U.S.
Pharmacopeia Convention established standards requiring that all prescriptions,
regardless of the system that was used in the drug dosing, include the metric
measure for the quantity and strength of drug. It was also established that drugs
may be dispensed only in the metric form. Prescribers are not totally converted
to this new standard, however, so the nurse must be able to convert the dose
ordered into the available dose form to ensure patient safety. It is important to be
able to perform conversions (finding the equivalent values between two types of
measure, within each system of measure, and between systems of measure).METRIC SYSTEM
The metric system is the most widely used system of measure. It is based on
the decimal system, so all units are determined as multiples of 10. This system
is used worldwide and makes the sharing of knowledge and research information
easier. The metric system uses the gram as the basic unit of solid measure and the
liter as the basic unit of liquid measure. When using the metric system to convert
from smaller to larger, a person would simply move the decimal to the appropriate
number of places to the left. When converting from larger to smaller, a person
would move the decimal the necessary number of places to the right.APOTHECARY SYSTEM
The apothecary system is a very old system of measurement that was specifically
developed for use by apothecaries or pharmacists. The apothecary system uses
the minim as the basic unit of liquid measure and the grain as the basic unit
of solid measure. It uses weight and volume as divisions of measurement, they
include measurements of ounces, gallons, pints and quarts. This system is much
harder to use than the metric system and is rarely seen in most clinical settings.
Occasionally, a prescriber will write an order in this system, and the dose will have
to be converted to an available form. An interesting feature of this system is that
it uses Roman numerals placed after the unit of measure to denote amount. For
example, 15 grains would be written “gr xv.”HOUSEHOLD SYSTEM
The household system is the measuring system that is found in recipe books. This
system uses the teaspoon as the basic unit of fluid measure and the pound
as the basic unit of solid measure. Although efforts have been made in recent
years to standardize these measuring devices, wide variations have been noted in
the capacity of some of them. Patients need to be advised that flatware teaspoonsand drinking cups vary tremendously in the volume that they contain. A flatware
teaspoon could hold up to two measuring teaspoons of quantity. When a patient
is using a liquid medication at home, it is important to clarify that the measures
indicated in the instructions refer to a standardized measuring device.AVOIRDUPOIS SYSTEM
The avoirdupois system is another older system that was very popular when
pharmacists routinely had to compound medications. This system uses ounces
and grains, but they measure differently than those of the apothecary and household
systems. The avoirdupois system is seldom used by prescribers but may be used
for bulk medications that come directly from the manufacturer. The avoirdupois
system exclusively measures weight based on 16-ounces equaling 1 lb. This
system of measurement is the everyday weight-measuring system most people
recognize. In pharmaceutical measurements, the avoirdupois system is useful
for measuring bulk quantities when buying or selling, including over-the-counter
pharmaceuticals and chemicals.OTHER SYSTEMS
Some drugs are measured in units other than those already discussed. These
measures may reflect chemical activity or biological equivalence. One of these
measures is the unit. A unit usually reflects the biological activity of the drug in
1 mL of solution. The unit is unique for the drug it measures; a unit of heparin is
not comparable to a unit of insulin. Milliequivalents (mEq) are used to measure
electrolytes (e.g., potassium, sodium, calcium, fluoride). The milliequivalent refers
to the ionic activity of the drug in question; the order is usually written for a number
of milliequivalents instead of a volume of drug. International units are sometimes
used to measure certain vitamins or enzymes. These are also unique to each drug
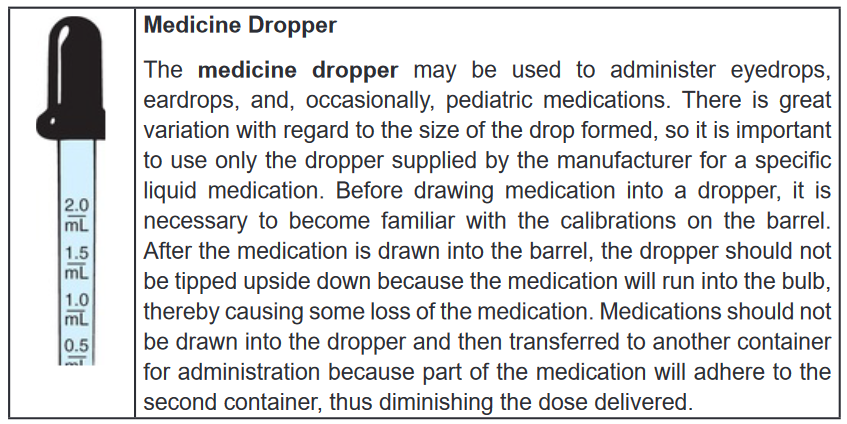
and cannot be converted to another measuring form.Material used for measuring liquid for metric and household
A medicine cup is a plastic container with scales (metric, household) for measuring
liquid medications. Examine the medicine cup carefully before pouring any
medication to ensure that the proper scale is being used for measurement. The
medicine cup should be placed on a hard surface when measuring liquid medication
and then read at eye level. The medicine cup is inaccurate for measuring doses
of less than 1 teaspoon, although it is reasonably accurate for larger volumes.
A syringe comparable to the volume to be measured should be used for smaller
volumes. For volumes of less than 1 mL, a tuberculin syringe should be used.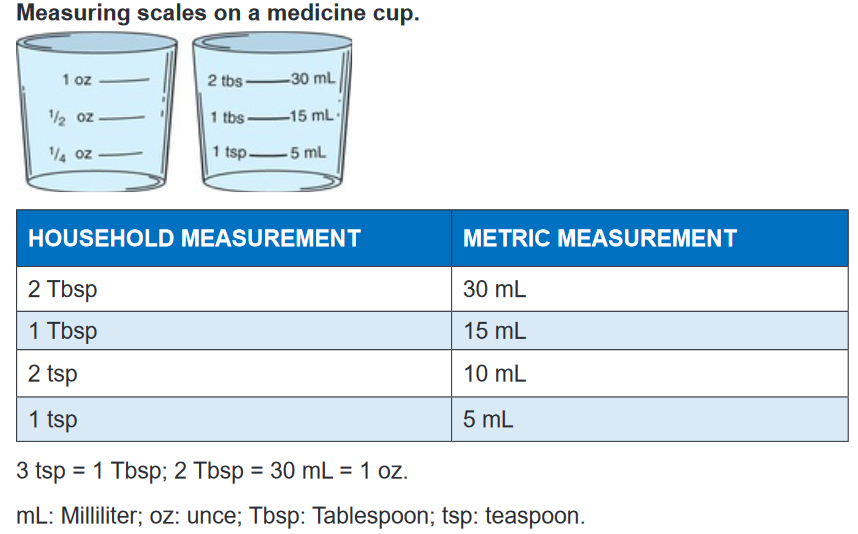
Teaspoon
Doses of most liquid medications are prescribed in terms using the teaspoon as the
unit of measure. However, there is great variation between the volumes measured
by various spoons in the home. In the hospital, 1 teaspoon is converted to 5
mL, and this is read on the metric scale of the medicine cup. For home use, an oral
syringe is recommended. If this is not available, a teaspoon that is used specifically
for baking may be used as an accurate measuring device.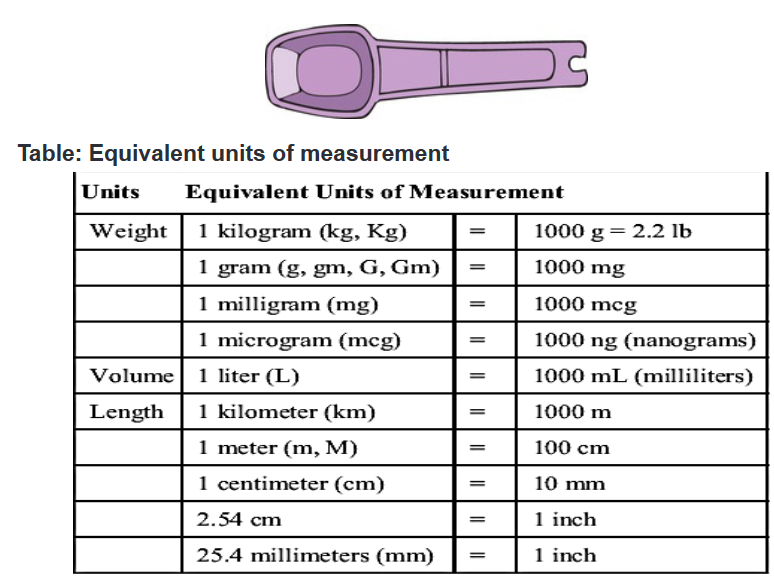
Self- assessment 3.9
1. What are the 4 main measuring systems used in pharmacology?
2. What is the equivalent metric measurement (in mL) for 2 tablespoons of
household measurement?
3. What is the basic unit of liquid measure in household system?
4. What is the equivalent metric measure of 2 teaspoons?3.10 Characteristics of a well written medical prescription
Learning activity 3.10
ou are carrying out clinical practice in a health center. You colleague finds a
prescription of paracetamol 500mg PRN for a patient who is being managed
for an intermittent fever. The colleague then gets confused with the meaning of
PRN.
1. How can you explain a PRN order to your colleague?
2. What are other types of medication orders?
3. In Rwanda, who have the broadest prescriptive authority of medications?CONTENT SUMMARY
Introduction
A prescription (℞) is a health-care program implemented by a physician or other
medical practitioner in the form of instructions that govern the plan of care for an
individual patient.Prescriptions may include orders to be performed by a patient, caretaker, nurse,
pharmacist or other therapist.Commonly, the term prescription is used to mean an order to take certain
medications.Prescriptions have legal implications, as they may indicate that the prescriber takes
responsibility for the clinical care of the patient and in particular for monitoring
efficacy and safety.However, as medications have increasingly become pre–packaged manufactured
products and medical practice has become more complex, the scope of meaning
of the term “prescription” has broadened to also include clinical assessments,
laboratory tests, and imaging studies relevant to optimizing the safety or efficacy.Both pharmacists and prescribers are regulated professionals in most jurisdictions.
A prescription as a communications mechanism between them is also regulated
and is a legal document.Regulations may define what constitutes a prescription, the contents and format of
the prescription (including the size of the piece of paper and how prescriptions are
handled and stored by the pharmacist).Many jurisdictions will now allow faxed or phone prescriptions containing the same
information.Many brand name drugs have less expensive generic drug substitutes that are
therapeutically and biochemically equivalent.Prescriptions will also contain instructions on whether the prescriber will allow
the pharmacist to substitute a generic version of the drug. This instruction is
communicated in a number of ways.In some jurisdictions, the preprinted prescription contains two signature lines: one
line has “dispense as written” printed underneath the other line has “substitution
permitted” underneath.Some have a preprinted box “dispense as written” for the prescriber to check off
(but this is easily checked off by anyone with access to the prescription).Other jurisdictions the protocol is for the prescriber to handwrite one of the following
phrases: “dispense as written”, “DAW”, “brand necessary”, “do not substitute”, “no
substitution”, “medically necessary”, “do not interchange”.In other jurisdictions may they use completely different languages, never mind a
different formula of words.In some jurisdictions, it may be a legal requirement to include the age of child on
the prescription.For pediatric prescriptions, some advise the inclusion of the age of the child if the
patient is less than twelve and the age and months if less than five. In general,
including the age on the prescription is helpful. Adding the weight of the child is
also helpful.Prescriptions often have a “label” box. When checked, the pharmacist is instructed
to label the medication. When not checked, the patient only receives instructions for
taking the medication and no information about the prescription itself.Some prescribers further inform the patient and pharmacist by providing the
indicator for the medication i.e. what is being treated.This assists the pharmacist in checking for errors as many common medications
can be used for multiple medical conditions.Some prescriptions will specify whether and how many “repeats” or “refills” are
allowed, that is whether the patient may obtain more of the same medication without
getting a new prescription from the medical practitioner.Regulations may restrict some types of drugs from being refilled.
In group practices, the preprinted portion of the prescription may contain multiple
prescribers’ names.Prescribers typically circle themselves to indicate who is prescribing or there may
be a checkbox next to their name.Types of Medication Orders
The health care practitioner prescribes medications in different ways, depending on
their purpose. Medications can be prescribed as stat, single-dose, standing, and as
needed (prn) orders.STAT ORDERS
A stat order is an order for a single dose of medication to be given immediately. Stat
drugs are often prescribed in emergency situations to modify a serious physiological
response; a stat dose of nitroglycerin may be ordered for a client experiencing
chest pain.The nurse should assess and document the client’s response to all stat medications.
SINGLE-DOSE ORDERS
Single-dose orders are one-time medications or may require the administration of
drops or tablets over a short period of time.The nurse should administer single-dose orders only once, either at a time specified
by the health care practitioner or at the earliest convenient time.These drugs are often prescribed in preparation for a diagnostic or therapeutic
procedure for example, radiopaque tablets may be administered in preparation for
a gallbladder test, or a one-time order may be given for a preoperative medication.STANDING ORDERS
Standing orders are also referred to as scheduled orders because they are
administered routinely as specified until the order is canceled by another order.The standing orders stay in effect until the health care practitioner discontinues or
modifies the dosage or frequency with another order or until a prescribed number
of days has elapsed as determined by agency policy.The purpose of a standing medication order is to maintain the desired blood level
of the medication.PRN ORDERS
A drug may be ordered on a prn (as needed) basis as circumstances indicate.
The drug is administered when, in the nurse’s judgment, the client’s condition
requires it.Before administering a prn medication, the nurse must thoroughly assess the client,
using both objective and subjective data in determining the appropriateness of
administering the medication.This type of order is commonly written for analgesics, antiemetic, and laxatives.
The order written by the health care practitioner indicates how frequently a prn
medication can be given.A nurse cannot administer a prn medication more frequently than the order indicates
without consulting with the health care practitioner for a change in that order.Examples of prn orders are meperidine (a narcotic analgesic) 75 mg IM q3–4 hours
prn incisional pain and Tylenol 650 mg q4 hours prn headache.When the prn medication has been administered, the nurse documents the
assessment and the time of administration.In addition, the nurse is responsible for monitoring the effectiveness of the medication
and documenting the effect in the client’s medical record.The nurse administers the pain medication on the basis of the assessment of the
client’s pain and as specified in the order.Who can write prescriptions (that may legally be filled with prescription-only
items)?Any jurisdiction that allows freedom of written communication generally must
therefore allow anybody to write a prescription to anybody, in as much as the
prescription itself is just written advice.Therefore “who can write prescriptions” will be explained below as shorthand for
“whose prescriptions may legally be filled with items restricted to dispensing via the
order of certain persons”.National or legislation governs who can write a prescription.
In Rwanda, physicians have the broadest prescriptive authority.
Many other healthcare professions also have some form of prescriptive authority
related to their area of practice. Veterinarians, dentists, and podiatrists have
prescribing power.All the country allows registered certified Nurse practitioners prescription power
with some limitations to controlled substances.Both pharmacists and prescribers are regulated professionals in most jurisdictions.
A prescription as a communications mechanism between them is also regulated
and is a legal document.Regulations may define what constitutes a prescription, the contents and format of
the prescription including the size of the piece of paper and how prescriptions are
handled and stored by the pharmacist.Many jurisdictions will now allow faxed or phone prescriptions containing the same
information.Parts of the drug order
All orders should be written clearly and legibly, and the drug order should contain
seven main parts:
1. Identification of the client (name, age, sex, etc)
2. The date and time when the order is written
3. The name of the drug to be administered
4. The dosage5. The route by which it is to be administered and special directives about its
administration6. The time of administration and frequency
7. The signature of the person writing the order, such as the physician or
advanced practice registered nurseConventions for avoiding ambiguity
Not only the drug order and medical prescription should have the above mentioned
parts, should they also have the full information in order to give all required details
about the order or prescription.Prescribers have developed many conventions for prescription-writing, with the
goal of avoiding ambiguities or misinterpretation.These include:
• Date medication dispensed
• Sequential number
• Client full identity
• Prescriber’s direction for usage including the frequency and route of
administration
• Prescriber’s name
• Name and address of the agency dispensing
• Name and strength of the drug dispensed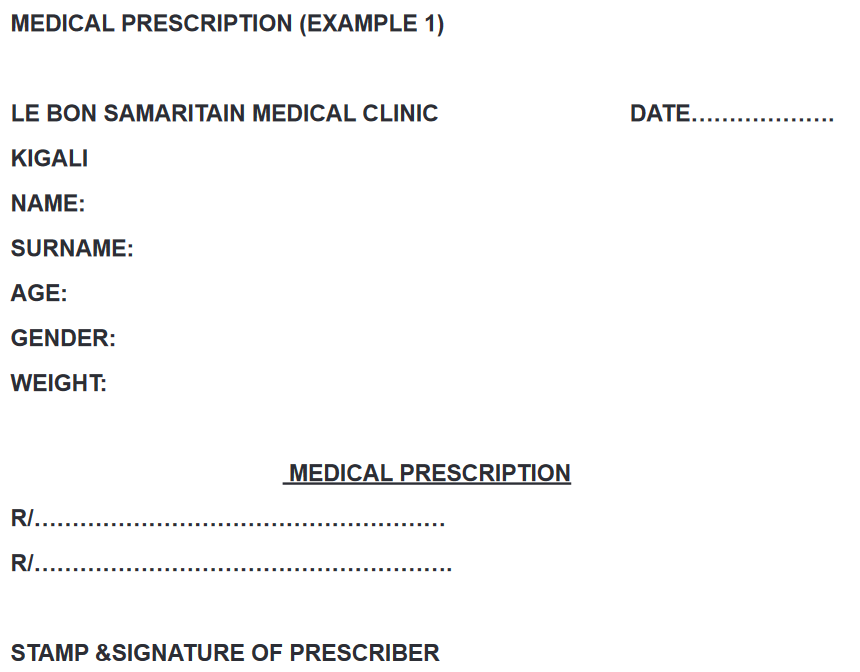
Self- assessment 3.10
1. Which of the following statements best describes a STAT order?
A. The drug is administered when, in the nurse’s judgment, the client’s
condition requires it such as in case of pain management.
B. These are one-time medications or orders that require the administration
of drops or even tablets over a specified short period of time.
C. An order for a single dose of medication to be given immediately, often
in emergency situations to modify a serious physiological response
D. These are the orders for drugs that are administered routinely as
specified until the order is canceled by another order.2. What are the 7 main parts of a drug order?
3. Some prescriptions will specify whether and how many “repeats” or
“refills” are allowed for prescribed drugs. What do you understand by3.11 Drug dosage calculation
Learning activity 3.11
1. The nurse is preparing to give an oral dose of acetaminophen (Tylenol)
to a child who weighs 12 kg. The dose is 15 mg/kg. How many milligrams
will the nurse administer for this dose?2. The patient is to receive 60mg of gentamicin BID intramuscularly. The
available ampules are 80mg dissolved in 2 mL each. How many milliliters
will the associate nurse draw from the ampule at each drug administration
(dose)?3. A 20-year-old male patient is to be given tablets of erythromycin for his
respiratory infection. He has been prescribed 500mg TDS for 7 days. The
available erythromycin tablets strength is tablets of 250mg. How many
tablets will the patient receive per day?CONTENT SUMMARY
Drug Dosage Calculations
Drug dosage calculations are required when the amount of medication ordered (or
desired) is different from what is available on hand for the nurse to administer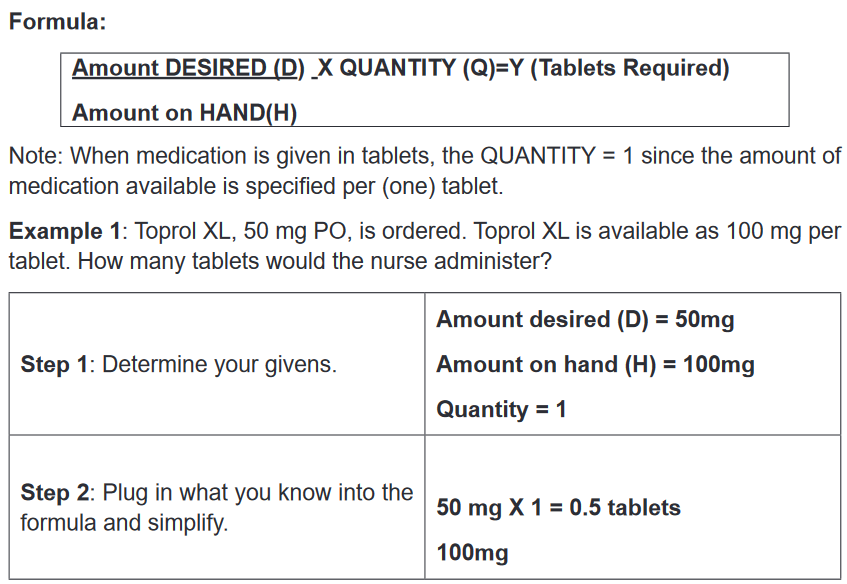
Therefore, the nurse would administer 0.5 of a tablet.
Example 2: 1200 mg of Klor-Con is ordered. This medication is only available as
600 mg per tablet. How many tablets should the nurse give?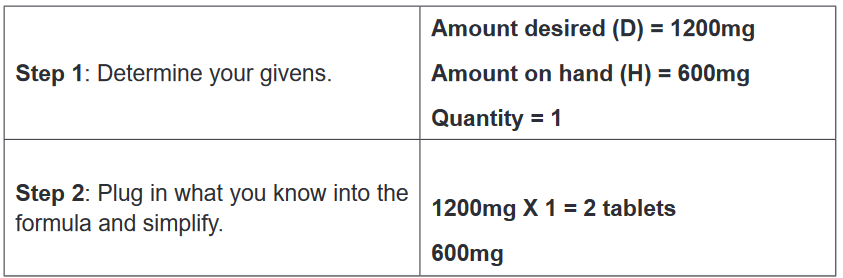
Therefore, the nurse should give 2 tablets.
The same formula can be used for dosage calculations where the medication is
available as amount per certain volume. In these types of calculations, the volume
available on hand is the QUANTITY.Example 3: Dilantin-125 is available as 125 mg/5 mL. Dilantin-125, 0.3 g PO, is
ordered. How much should the nurse administer to the patient?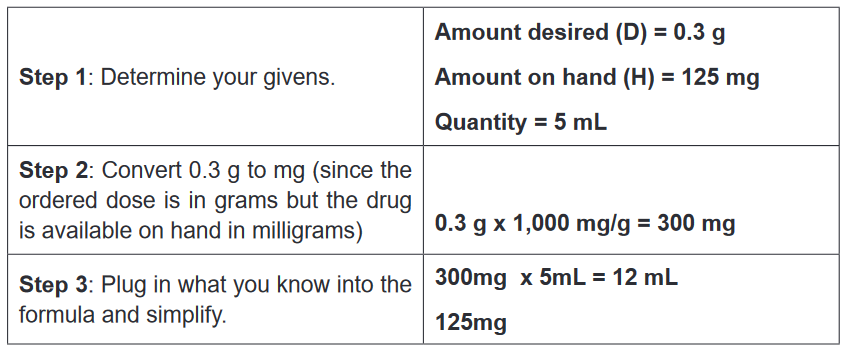
Therefore, the nurse would administer 12 mL.
Example 4: Furosemide is available as 40 mg in 1 mL. 10 mg is ordered to
be administered through an IV. What amount of furosemide should the nurse
administer?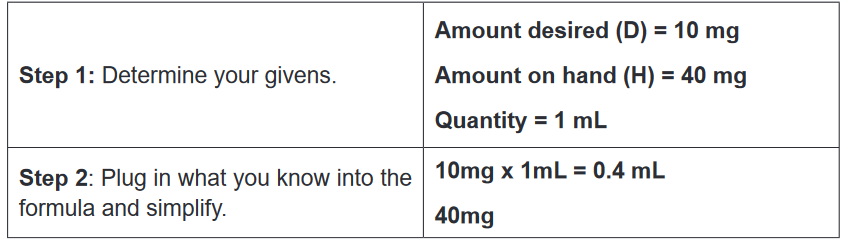
Therefore, the nurse should administer 0.4 mL of furosemide.
Dosage Calculations based on Body Weight
Dosage calculations based on body weight are required when the dosage ordered
and administered is dependent on the weight of the patient. For example, many
pediatric drugs are ordered and given per weight (usually in kg). Dosage calculations
based on body weight are calculated in two main stages.Stage 1: Using the formula below, calculate the total required dosage based on
given the body weight.
Weight (kg) x Dosage Ordered (per kg) = Y (Required Dosage)Stage 2: Apply the D/H x Q formula to calculate the actual amount of medication to
be administered.Example 1: Medrol 4 mg/kg is ordered for a child weighing 64.8 lb. Medrol is available
as 500 mg/4mL. How many milliliters of medication must the nurse administer?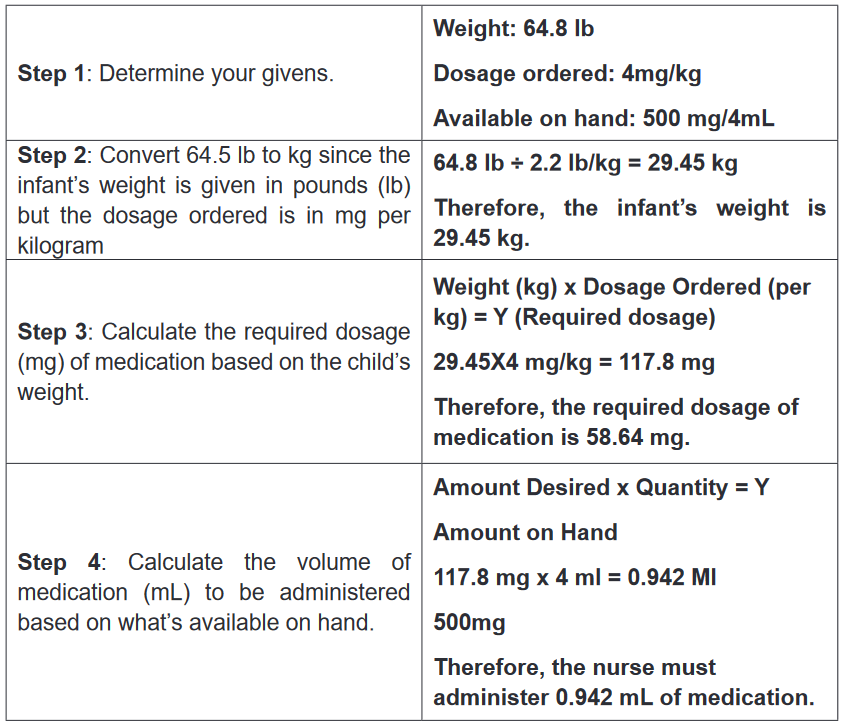
Self- assessment 3.11
1. 1000 mg of potassium chloride is ordered. This medication is only
available as 500 mg per tablet. How many tablets should the nurse give?2. Diclofenac injection is available as an ampule of 75mg/3 ml. This means
that the concentration is 25 mg/ml or 75 mg/ 3 ml. Question: How much
volume of liquid will the client receive when the prescription is to give only
50 mg?3. A syrup is available as 25mg/5ml and the patient must be given 50mg.
What volume in milliliters will be given?3.12 End unit assessment
End Unit assessment 3
1. During drug administration, the nurse needs to ensure that all the RIGHTs
of medication administration are respected. Therefore, while applying the
right time, medications should be prescribed as closely to the time as
possible, and nurses should not deviate from this time by:
A. More than two hours to avoid consequences
B. More than three hours to avoid consequences
C. More than half an hour to avoid consequences
D. More than one hour to avoid consequences2. Which of the following RIGHTs of medication administration seeks to
ensure the medication is working the way it should after its administration?
A. Right evaluation
B. Right documentation
C. Right route and form
D. Right patient3. Which of the following instructions are applied to controlled drug
regulation?
A. The controlled drugs should be in double locked container, and 1
licensed personnel counts (or verifies any discrepancies) every two
days.
B. The controlled drugs should be in double locked container, and 2
licensed personnel count (or verify any discrepancies) every shift.
C. The controlled drugs should be in double locked container, and 2
licensed personnel counts (or verifies any discrepancies) every two
days.
D. The controlled drugs should be in double locked container, and 1
licensed personnel counts (or verifies any discrepancies) four times a
day.4. Which of the following statements best defines the subcutaneous
injection?
A. The medication is deposited just beneath the skin in the loose
subcutaneous tissue.B. The drug is injected into one of a large skeletal muscle such as triceps
and rectus femoris
C. Intrathecal administration is a route for drugs via an injection into the
spinal canal, or into the subarachnoid space
D. Method of administering medications directly into the vein using a
needle and a syringe5. In which of the following types of medication errors would a medication
error which involves any deviation from the prescriber’s medication order
as written on the patient’s errors chart, manufacturers’ preparation, or
relevant institution policies be classified?
A. Prescribing errors
B. Administration errors
C. Dispensing errors
D. Monitoring errors6. How many millilitres are in one teaspoon used in the measurement of
drugs?
A. 7 millilitres
B. 10 millilitres
C. 15 millilitres
D. 5 millilitres7. Which of the following statements best describes a STANDING order?
A. The drug is administered when, in the nurse’s judgment, the client’s
condition requires it such as in case of pain management.
B. These are one-time medications or orders that require the administration
of drops or even tablets over a short period of time.
C. An order for a single dose of medication to be given immediately, often
in emergency situations to modify a serious physiological response
D. These are the orders for drugs that are administered routinely as
specified until the order is canceled by another order.8. Enumerate social and economic dimensions affecting adherence to
medications.9. Enumerate the advantages of rectal route of drug administration.
10. What are the disadvantages of administering the drugs by the transdermal
route?
