UNIT 6IMMEDIATE CARE OF A NEWBORN
Key Unit Competence: Provide immediate care to the newborn
a. What do you think about these images demonstrating the care given to the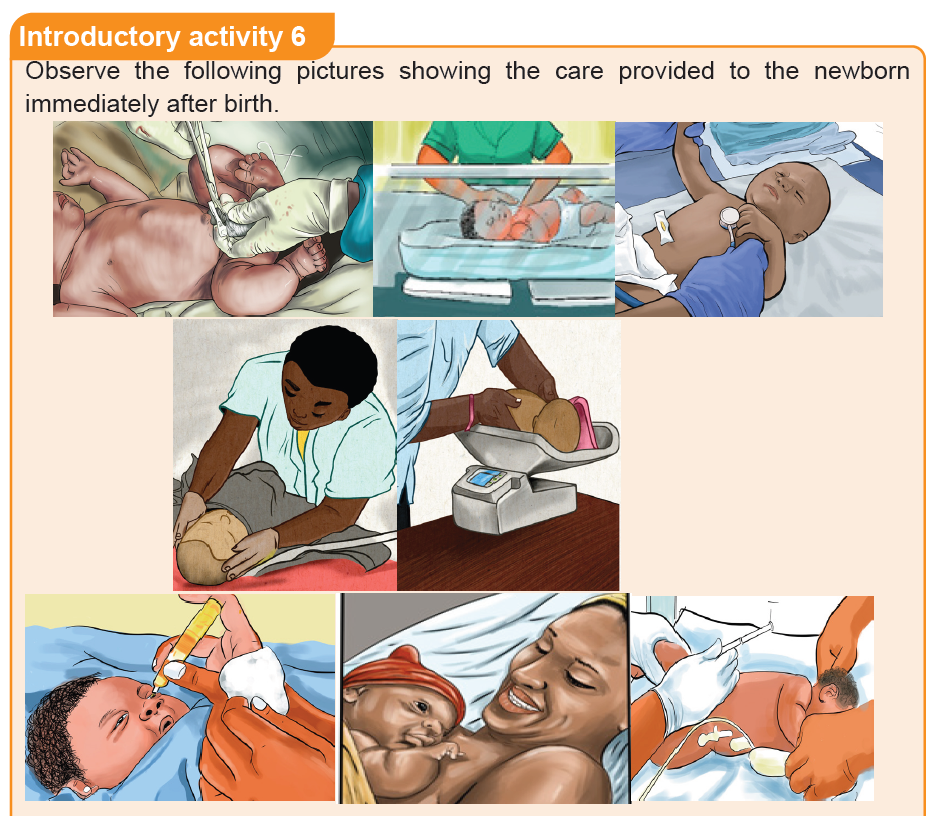
baby immediately after birth?
b. What do you think that it is necessary to have stethoscope and thermometer
while providing immediate newborn car?
c. What do you reflect to the image showing a health care provider injecting
the new-born baby?
d. What do you reflect about eye care to new born baby?
e. What do you think about the advantages of putting the baby on the mother’s
chest immediately after birth?
6.1. Concept of immediate care and components of essential
newborn care.Learning Activity 6.1
As associate nurse, you are called to care and provide essential newborn care
for a baby who was born just 3 minutes ago. While caring for that baby what can
be done to prevent hypothermia from evaporation, conduction and convection?
Based on the case described above,
a) When do you think immediate newborn care start from?
b) What do you think could be done to prevent hypothermia?
c) What do you think about the terminology of early breastfeeding in the
immediate newborn care?
d) What do you think are essential newborn care?
Key components of the essential new born care at birth:
• Thermal care or maintenance of baby’s body temperature.
• Clearing of airways only when necessary not as routine.
• Eye care
• Cord care
• Breastfeeding with in the first hour of birth
• Administration of vitamin k
• Weighing the baby and record weight.
• Routine monitoring
• Additional care if the baby was exposed to HIV or HBV.
Newborn immediate care is the care given to the neonate after birth by qualified
personnel in the delivery room.
Essential newborn care refers to key routine practices in the care of the newborn,
particularly at the time of birth and over the first hours of life, whether in the health
facility or at home.
Essential newborn care includes:
• Thermal care (including prompt drying and maximizing skin-to-skin contact
and covering the baby at birth, delayed bathing, maintaining “warm chain”)
• Early initiation and exclusive breastfeeding
• Hygiene practices (including cord-care and caregiver hand washing).
There is good evidence that adherence to recommended essential newborn care
practices substantially reduce mortality risk, especially for very small newborns.
Health service contacts (notably associated with antenatal care and the hospital
admission for childbirth) are important opportunities to influence these practices. In
some settings, community health workers (CHWs) can serve as important channels
to influence adoption of these practices among pregnant women.
Thermal protection and care of newborns:
All measures used by healthcare providers to prevent or manage hypothermia to
the newborn baby. Hypothermia contributes to neonatal morbidity and mortality.
Thermal protection and care is recommended as it reduces hypothermia, a
condition in which the body temperature falls below 36 degree Celsius. The
recommended thermal care practices include immediately drying and wrapping of
the baby; bathing practices such as delaying for at least 6 hours and using warm
water; day to day care such as covering the baby’s head; and keeping the baby
skin-to-skin.
The newborn loses heat in four ways:
• Evaporation: when amniotic fluid evaporates from the skin.
• Conduction: when the baby is placed naked on a cooler surface, such as the
floor, table, weighing scales, cold bed.
• Convection: when the baby is exposed to cool surrounding air or to a draught
from open doors and windows or a fan.
• Radiation: when the baby is near cool objects, walls, tables, cabinets, withoutactually being in contact with them
Early initiation of breastfeeding: is referred as the provision of mother’s breast milk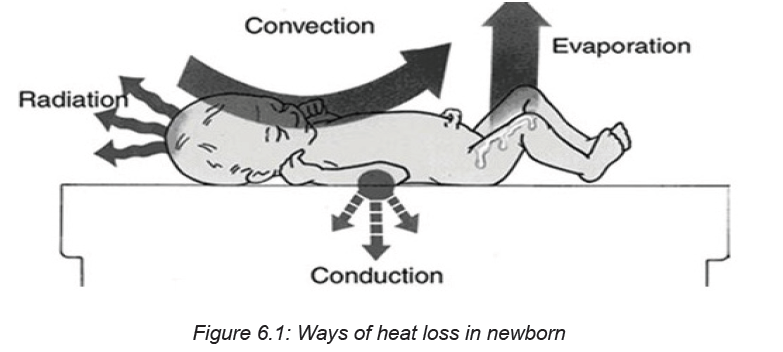
to infants within one hour of birth. This helps to ensure that the infant receives
the colostrum, or “first milk’, which is rich in protective factors. Early initiation of
breastfeeding, within one hour of birth, protects the newborn from acquiring infection
and reduces newborn mortality. It facilitates emotional bonding of the mother and
the baby and has a positive impact on duration of exclusive breastfeeding.
Newborn eye care
Newborn eye care is providing antibiotic eye drops or ointment in a newborn’s eyes
after birth. This is to protect babies from getting bacterial eye infections that can
be acquired during birth. Untreated, these infections can cause serious problems
including blindness. The antibiotic erythromycin and tetracycline are used most
often.
Umbilical Cord Care
The umbilical cord is the baby’s lifeline to the mother during pregnancy. However,
it’s no longer needed once the baby is born. Within a few minutes after birth, the
cord is clamped and cut close to the navel. The clamp helps stop bleeding from the
blood vessels in the umbilical cord.
Administration of vitamin K to newborn
Administering one intramuscular (IM) dose of vitamin K (0.5 mg for infants weighing
≤1,500 g or 1.0 mg for infants weighing >1,500 g) routinely to all newborns within the
first 6 hours post-birth and following initial stabilization and appropriate maternal/
newborn interaction, is now the recommended best practice. Vitamin K helps the
blood to clot and prevents serious bleeding. In newborns, vitamin K injections
can prevent a now rare, but potentially fatal, bleeding disorder called ‘vitamin K
deficiency bleeding’ (VKDB), also known as ‘hemorrhagic disease of the newborn’
(HDN).
Weighing the new born
According to the WHO, the average weight of a baby has born at 37–40 weeks
ranges from 2.5 to 4 kg. Newborns often lose around 226.8 g in the first 4 to 5 days
after birth but regain it by about 10 to 12 days of age. In the first month, the typical
newborn gains about 20 g a day, or about 110 g to 8 226.8 g a week.
Self-assessment 6.1
1. What are the key components of essential newborn care?
2. What is the importance of applying antibiotics drop/ ointments in the
newborn baby’s eyes immediately after birth?
3. What is done to protect the newborn baby against hypothermia?
4. Describe the 4 ways of loosing heat to the newborn baby after birth.6.2 APGAR score assessment
Learning Activity 6.2 APGAR SCOREObserve these images illustrating an associate nurse assessing APGAR SCORE
From the observation of above pictures,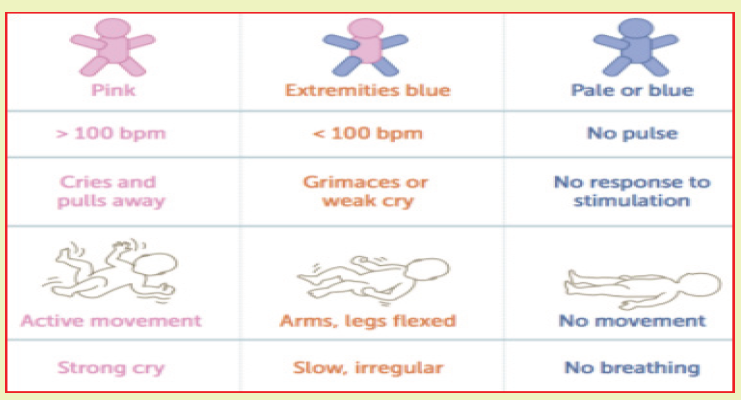
a. Have you come in contact with word APGAR SCORE previously? If yes
What is it?
b. What do you think about the importance of assessing APGAR score to the
newborn baby immediately after birth?
c. what do you think about APGAR at 5 minutes?
History and description of APGAR SCORE
One of the first assessments is a baby’s Apgar score. At one minute and five
minutes after birth, infants are checked for heart and respiratory rates, muscle tone,
reflexes, and color. This helps identify babies that have difficulty breathing or have
other problems that need further care.
Apgar is a quick test performed on a baby at 1 and 5 minutes’ score after birth, the
1 minute score determines how well the baby tolerated the birth process. The 5
minutes’ score tells the healthcare provider how well the baby is doing outside the
mother’s womb.
Dr. Virginia Apgar was an obstetrical anesthesiologist designed and introduced the
APGAR Score, the first standardized method for evaluating a new-born’s transition
to life outside the womb. She created a system in 1952 and used her name as
MNEMONIC for each of the 5 elements that a person will score.
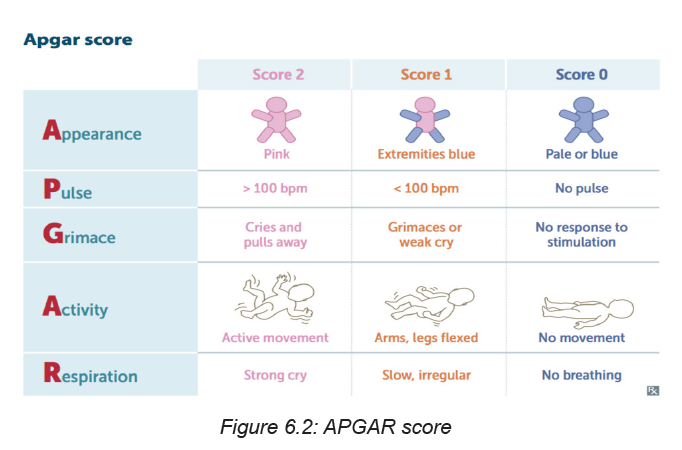
A = APPEARANCE
0 Points = Bluish-gray or pale all over
1 Point = Normal color (but hands and feet are bluish)
2 Points = Normal color all over (hands and feet are pink)
P = PULSE
0 Points = Absent (no pulse)
1 Point = Pulse below 100 beats per minute (bpm)
2 Points = Pulse over 100 beats per minute (bpm)
G = GRIMACE
0 Points = Absent, no response to stimulation
1 Point = Facial movement only, grimacing with stimulation
2 Points = Pulls away, sneezes, coughs, or cries with stimulation
A = ACTIVITY
0 Points = No movement, or “floppy” tone
1 Point = Flexed arms and legs with little movement
2 Points = Active, spontaneous movement
R = RESPIRATION
0 Points = Absent, no breathing
1 Point = Slow or irregular breathing, weak crying2 Points = Normal rate of breathing and effort, good crying
Self-assessment 6.2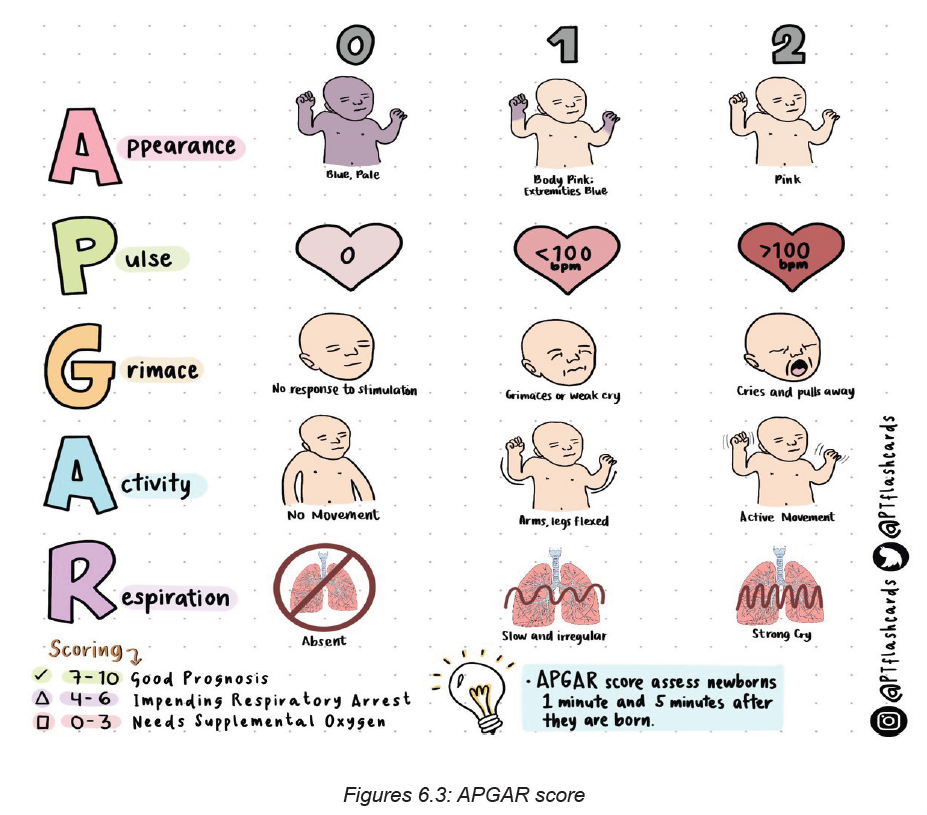
1. What is APGAR score?
2. What does mean the mnemonic APGAR in full words?
3. Who discovered APGAR?
4. In which year DR Virginia Apgar created the system?
6.3. Requirements, aims and importance of the assessment of the
newborn immediately after birth.
Learning Activity 6.3
As an associate nurse, you are called to perform assessment for a newborn
baby boy who was born in past 10 minutes. In that call, you are told to examine
the baby from head to toes
From the above call,
a. What do you think will be the materials that you will use to assess that
newborn baby?
b. What do you think about the aim and importance of assessing that newborn
baby immediately after birth?
c. What do you think about the role of health care provider in examination of
newborn?
Roles of the associate nurse in assessing/examining the newborn baby
immediately after birth.
The role of the nurse/midwife is:
• To carry out good interpersonal communication.
• To take complete history about the mother and neonate.
• To be sure that the neonate has identification band.
• To perform complete physical assessment (General appearance, vital signs,
growth measurements, gestational age assessment).
• Prevention of hemorrhage (administer vitamin K if not given in the delivery
room).
• Documentation.
Aims of assessing/examining the newborn baby immediately afterbirth
The aim of assessing/examining the newborn baby immediately afterbirth is to:
• To describe and carry out an examination of a baby soon after birth
• To screen for malformations
• To observe smooth transition to extra uterine life
• An ass overall of baby’s condition
Principles of examination of the newborn baby immediately afterbirth
The Principles of examination of the newborn baby immediately afterbirth include:
♦ Assess
♦ Ask, Check, Record
♦ Look, Listen, Feel
♦ Classify
♦ Treat/refer or advise
Types and stages of newborn assessment
The following are types and stages of newborn assessment:
1. The initial assessment: done in the 1st 10 minutes
APGAR scoring system
Purpose: is to assess the newborn’s immediate adjustment to extra-uterine life.
2. Transitional assessment (Periods of reactivity):
I) First period of reactivity:
Stage 1: During the first 30 minute through which the baby is characterized as
physiologically unstable, very alert, cries vigorously, may suck a fist greedily, &
appears very interested in the environment.
Stage 2: It lasts for about 2-4 hours, through this period; all V.S & mucus production
are decreased. The newborn is in state of sleep and relative calm.
II) Second period of reactivity: It lasts for about 2-5 hours,
In Second period of reactivity the newborn is alert and responsive, heart &
respiratory rate, gastric & respiratory secretions are increased & passage of
meconium commonly occurs.
Following this stage is a period of stabilization through which the baby becomes
physiologically stable & a vacillating pattern of sleep and activity
Minimum prerequisites of examination of the newborn baby immediately
afterbirth:
The Minimum Requirements of examination of the newborn baby immediately
afterbirth includes:
• Mother & baby together
• Warm room, fresh clean sheet/clothes
• Thermometer
• Weighing scale
• Watch with seconds• Stethoscope
Self-assessment 6.3
1. Outline 3 roles of the associate nurse in assessing/examining the newborn
baby immediately after birth?
2. What is the Aim of assessing/examining the newborn baby immediately
after birth?
3. What are the minimum requirements of examination of the newborn baby
immediately afterbirth?
4. What includes the first period of reactivity?
6.4 Anthropometric measurements
Learning Activity 6.4
Observe these images illustrating an associate nurse taking measurements tothe newborn baby.
From the observation of above pictures,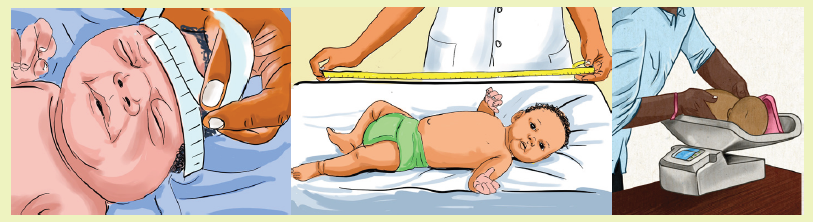
a. What measurements do you think the nurse is taking to that baby?
b. What do you think about the importance of weighing baby after birth?
c. What do think about about normal head circumference?
Weight measurement
Birth weight is an important marker of health. Full-term babies are born between
37 and 41 weeks of pregnancy. The normal birth weight ranges between
2500-4000grams. In general, very small babies and very large babies are at greater
risk for problems. Babies are weighed every day in order to look for growth. If the
baby weighs less than 1,500 gm or more than 4000grams, the associate nurse
must quickly refer the baby for further advanced care.
While taking the baby’s weight, the associate nurse must keep in mind that the new
born baby loses 10% of their birth weight in the first 10 days. Thereafter, the babies
gain about 25-30gms/day. Babies will usually gain this weight back within the first
2 weeks after birth. Premature and sick babies may not begin to gain weight right
away.
Length measurement
This is the measurement taken from crown of head to the heel. The normal range
is 45 to 50 cm.
Head circumference
This is the distance around the baby’s head. Immediately after birth, molding of the
skull may give inaccurate measurement of the head circumference. So it should
be measured after 48 hours after birth. The normal range of head circumference is
33 to 37 cm and it may be larger in case of hydrocephalus and smaller in case of
microcephaly.
Chest circumference
This is the distance around the baby’s chest and it is about 2-3cm less than head
circumference. Head and chest circumference may be equal for the first 24 to 48hours of life.
Self-assessment 6.4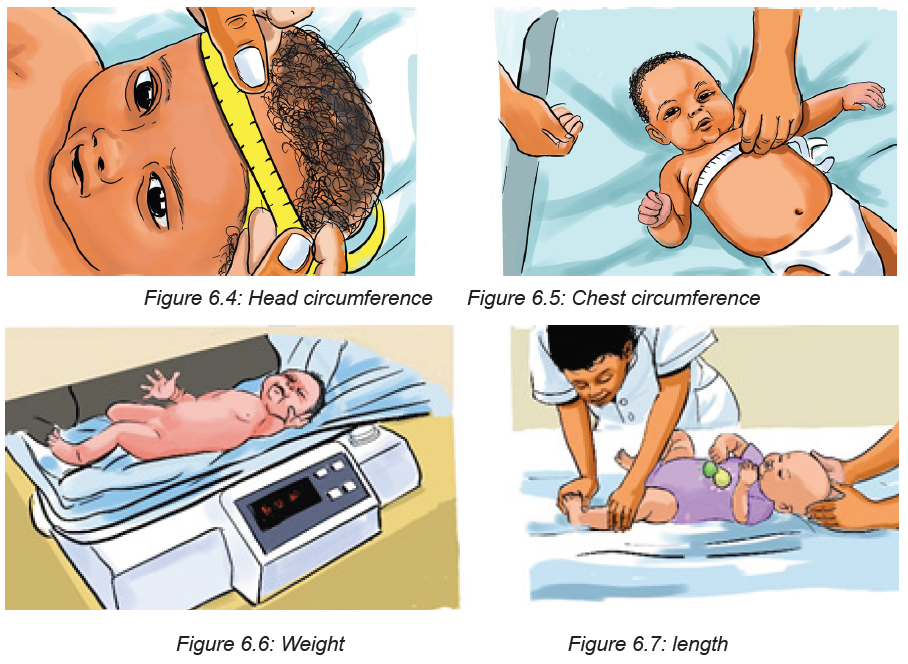
1. a. What are the essential measurements that are taken when the baby is
born?
b. What are the normal range findings for those measurements?
2. How molding can affect results of head circumference measurement?
3. What will the associate nurse do if the baby weighs less than 1,500 gm or
more than 4000grams?
4. The newborn loses weight during the first week of life at which percentage
in the following
a. 5%
b. 15%
c. 10%
d. 20%e. None of the above
6.5 Vital signs measurements of the newborn
Learning Activity 6.5
Observe these images illustrating an associate nurse taking vital signs to thenewborn baby.
From the observation of above pictures,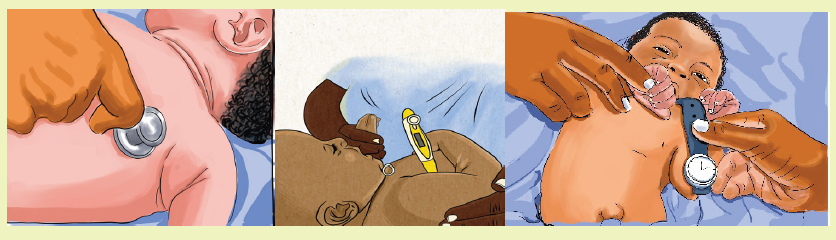
a. What vital signs do you think the nurse is taking to that baby?
b. What do you think can be normal regarding body temperature of newborn?c. What do you think to be normal range of respiratory rate in new born?
Vital Signs and Measurements
Temperature: Normal range 36.5 to 37.5 axillary
Common variations:
Crying may elevate temperature
Stabilizes in 8 to 10 hours after delivery
Signs of potential distress or deviations from expected findings:
Temperature is not reliable indicator of infection
A temperature less than 36.5 oc
Heart rate: Normal range: 120 to 160 beats per minute
Common variations:
Heart rate range to 100 when sleeping to 180 when crying
Color pink with acrocyanosis
Heart rate may be irregular with crying
Signs of potential distress or deviations from expected findings:
• Although murmurs may be due to transitional circulation-all murmurs
• should be followed-up and referred for medical evaluation
• Deviation from range
• Faint sound
Respiration rate: Normal range 30 to 60 breaths per minute
Common variations:
• Bilateral bronchial breath sounds
• Moist breath sounds may be present shortly after birth
Signs of potential distress or deviations from expected findings:
• Asymmetrical chest movements
• Apnea >15 seconds
• Diminished breath sounds
• Seesaw respirations
• Grunting
• Nasal flaring
• Retractions
• Deep sighing
• Tachypnea - respirations > 60
• Persistent irregular breathing
• Excessive mucus
• Persistent fine crackles
• Stridor (Crowing respiratory sound)Blood Pressure - not done routinely
Self-assessment 6.5
1. When does the temperature stabilize after birth?
2. What is the heart rate of the crying baby?
3. What changes may occur regarding the baby’s body temperature when the
baby is crying
4. Enumerate signs of potential distress.
6.6 Head and neck assessment
Learning Activity 6.6
Observe these images illustrating an associate nurse that is assessing thenewborn’s head and neck.
From the observation of above pictures,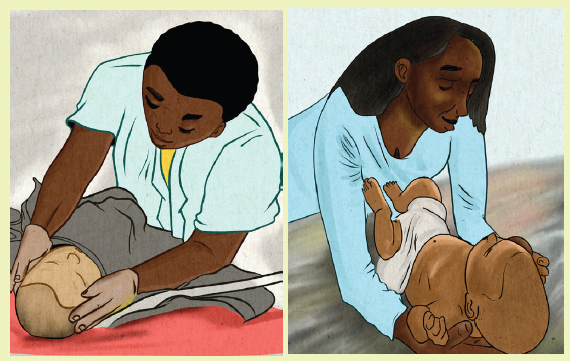
a. What elements do you think the nurse will assess to that baby’s head and
neck?
b. Have you heard a word fontanel? If yes, when do you think anterior fontanel
closes?
c. What do you understand by the word fontanel?
Head: It consists of skulls bones that are not closed completely, due to this, the
skull is easily molded during the passage through the birth canal at the time of birth
where the suture lines are joined and form the fontanelles.
Fontanel is a space between the bones of the skull in an infant, where ossification
is not complete and the sutures not fully formed.Sutures are fibrous bands of tissue that connects the borns of the skull.
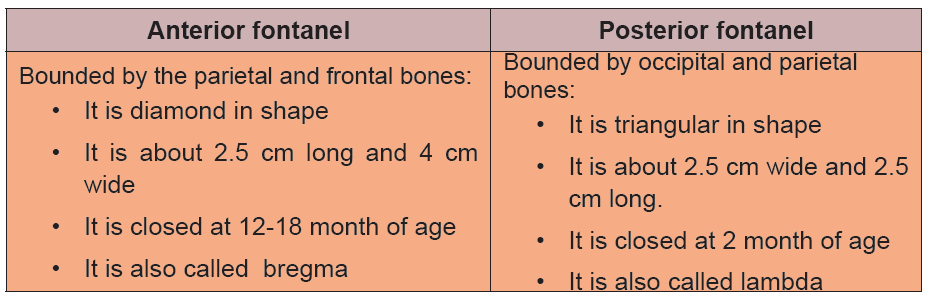
Table 6.1 Difference between fontanelles
If the sutures are wide and fontanels are bulged, this indicates the increased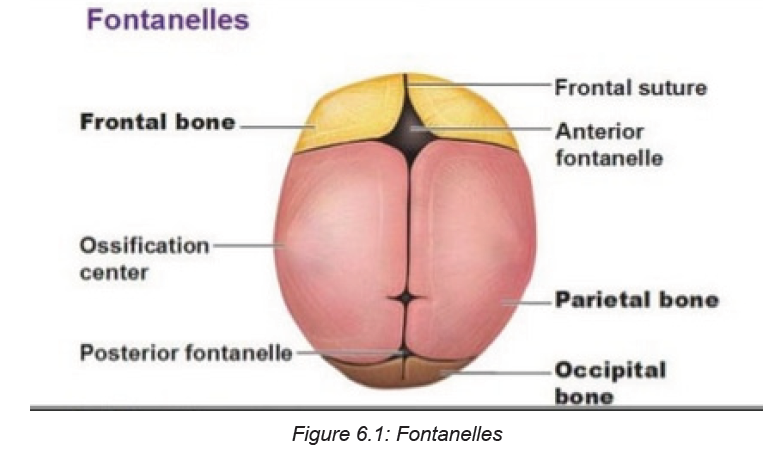
intracranial pressure which is commonly seen in hydrocephalus condition. When
fontanel depressed, it indicates dehydration. The associate nurse should also
observe the caput succedaneum and cephalohematoma.
Face
The associate nurse looks at the eyes, ears, nose, and cheeks. He/ She he also
examines the face for any asymmetry or obvious malformations.
Eyes
On the eyes of the newborn, the associate nurse will check for any asymmetry,
spacing, and movement. He/ She he also checks for oedema, discharge, colour of
sclera. Yellow color indicates jaundice. Position of the eyes and distance between
inner canthus of both eyes should be checked, it should be 2 cm in diameter. If it is
more than 2 cm; it is known as hypertelorism and if it is less than 2 cm; it is known
as hypotelorism. Neonate’s pupils are round in shape and react to the light.
Ear
On the ear, the associate nurse will check for symmetry and to make sure ears
are parallel to the eyes and not low set, which can indicate a problem. Also the size
and shape will be assessed. The ear cartilage is full in term infants and it is fully
developed and returns its shape. Observe the startle reflex by the loud noise which
indicates audibility of the neonates.
Nose
The associate nurse will check for patency, depression or low nasal bridge. He/
she will also assess for nasal discharge, deviated nasal septum, and nasal flaring.
Mouth and throat
The associate nurse will check for cleft palate and cleft lips. He/she will observe the
natal teeth. To assess for cleft palate or abnormality, the palpation of the palette willbe done. A small jaw could also indicate a problem.
Neck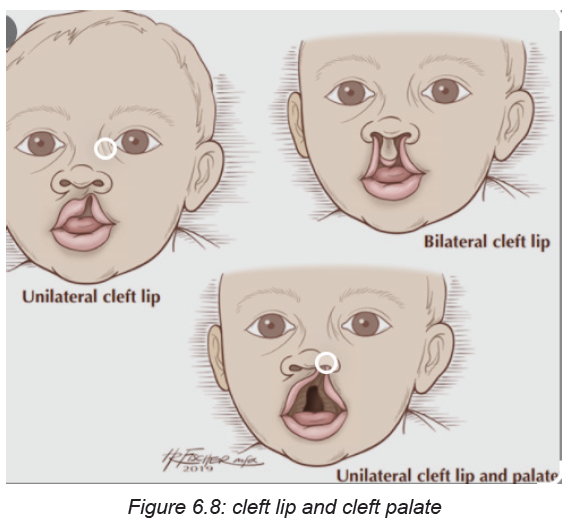
For the neck, the associate nurse will palpate for masses and the clavicles are
palpated for crepitus, which could indicate an injury. Neck of the new born is short
and has various folds and it should be checked for mobility, and webbing of theneck.
Self-assessment 6.6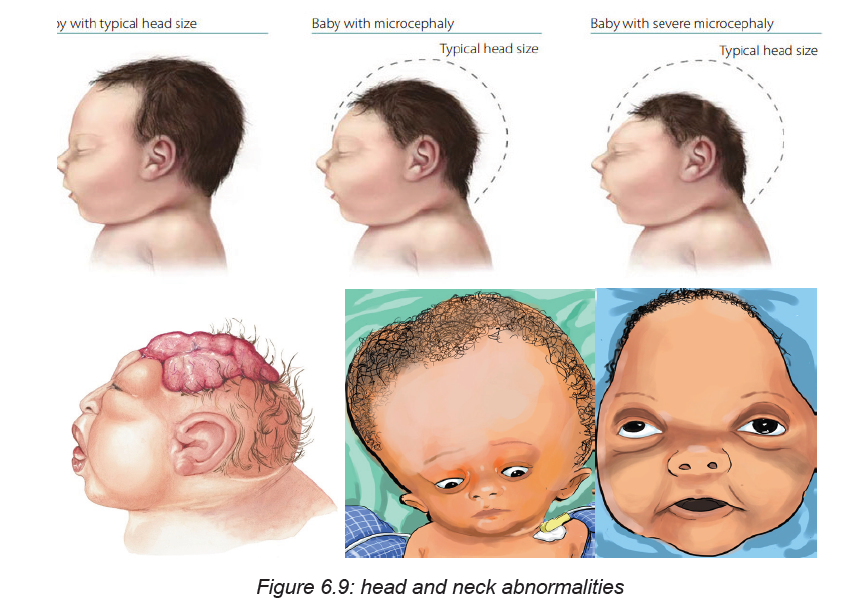
1. When the anterior fontanel closes?
2. When the posterior fontanel closes?
3. What will the associate nurse check on newborn’s eyes?
4. What will the associate nurse observe on newborn’s face5. Define the word sutures?
6.7 Chest and lungs assessment
Learning Activity 6.7
Observe these images illustrating an associate nurse assessing the newborn’schest.
From the observation of above pictures,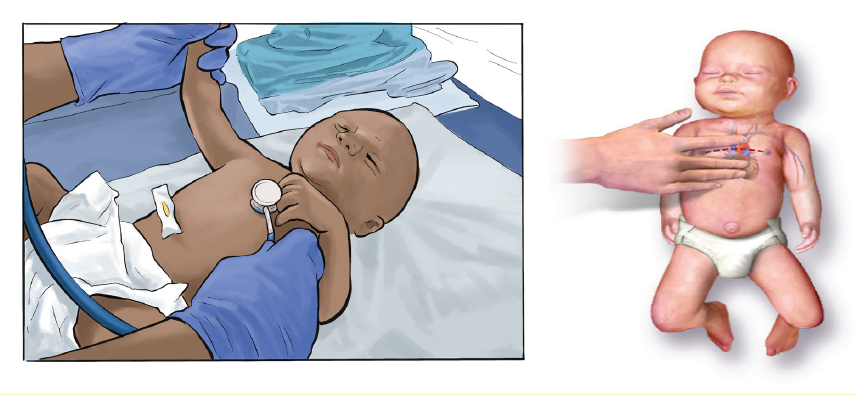
a. What elements do you think the nurse will assess newborn ‘chest?b. What do you think about inter costal retractions during breathing?
Normally, the chest is barrel shaped. A malformed chest could indicate a problem.
Retractions may be observed with respiratory difficulty.
The associate nurse observes the nipple and breast tissue. Breast size and location
should be assessed. He/she observes witch’s milk (milky discharge due to effect
of maternal hormones). Parents of the baby should not be worry because it will be
resolved slowly and there is no treatment for it.
Check the rate and rhythm of the respiration, neonate’s abdomen rises and falls
during each breathe. The lungs should be auscultated while the infant is quiet.
Respirations should be observed and counted for a full minute. Heart rate should
be assessed with a stethoscope while listening for murmurs.
Clinical evaluation of breath sounds is the first and most common method of
assessing lung health. The stethoscope placed on the back and chest lets the
physician listen to the breath sounds. This process is called auscultation.
Intercostal retractions: One of the most important physical findings to be able to
recognize in a new-born is the presence of retractions. Sepsis, pulmonary pathology,
cardiac disease, metabolic disorders, polycythaemia, cold stress, and others can
all cause retractions -- it is a sign of a new-born in distress. In the photo, taken
during inspiration, the shadows between the ribs can be clearly seen. Retractions
may or may not occur in combination with other signs of distress: nasal flaring,grunting, and tachypnea.
Self-assessment activity 6.7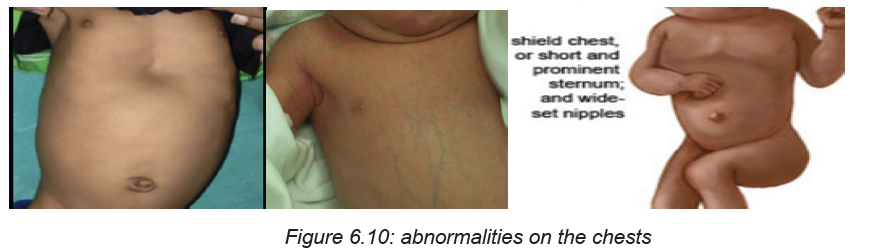
1. What the associate nurse assesses on the newborn’s chest?
2. What the associate nurse tells and explains to the mother is worried about
the witch’s milk found on his baby?
3. What is normal shape of the chest?4. When to auscultate the lungs of the newborn?
6.8 Abdomen, back and genitalia assessment
Learning Activity 6.8
Observe these images illustrating an associate nurse assessing the newborn‘abdomen, back and genitalia.
From the observation of above pictures,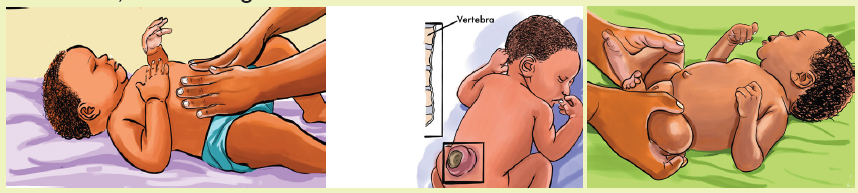
a. What elements do you think the nurse will assess to the back, abdomen,
spine and genitalia of the newborn?b. What do you think to be observed on umbilical cord after birth?
Abdomen
On abdomen, the associate nurse will check for the shape and distension. He/
she will also check for bowel sounds, and observe the umbilical cord for infection
and any discharge, redness and observe two arteries and one vein. Check for anyhernia or any abnormalities. Abdomen should feel soft during palpation.
Back and spine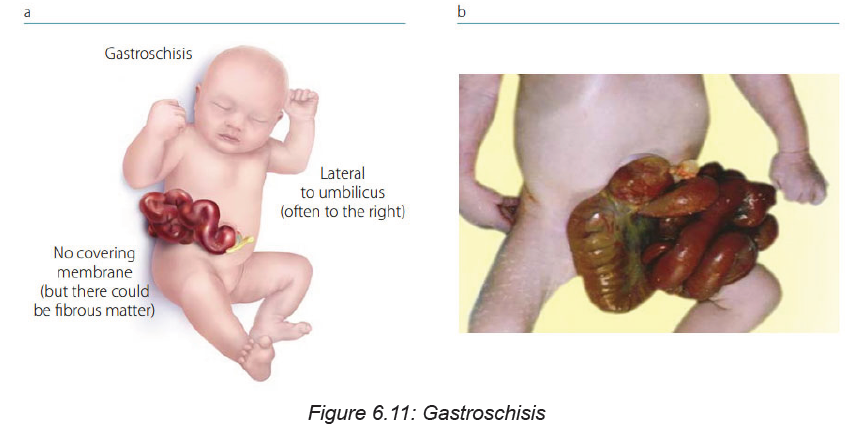
On the back, the associate nurse will check for any abnormal spinal curvature, hair
on the skin, depression in the spine, spina bifida, meningocele, meningomyelocele
Buttocks: Buttocks should be observed for any mass. Perineal area should bechecked for anal opening, anal fissure or any other abnormalities.
Genitalia
On female genitalia the associate nurse will check if the labia major cover the labia
minor (sign of maturity) and if the clitoris is visible on separating the labia. Urethral
opening should be below the clitoris. Pink red mucous vaginal discharge may be
found during the first week due to sudden decrease of maternal hormones, which
is known as pseudomenstruation.
On male neonates, testes should be inspected and palpated for descend; scrotum
appears pigmented and wrinkled with rugae. Penis should be inspected for urethralopening. Check for hydrocele and inguinal hernia.
Self-assessment activity 6.8
1. What will the associate nurse assess on umbilical cord of the newborn?
2. What will the associate nurse assess on back and spine of the newborn?
3. What will the associate nurse assess on male neonate’s genitalia?4. Define the term pseudo menstruation?
6.9 Assessment of the limbs
Learning Activity 6.9
Observe these images illustrating an associate nurse assessing the newborn‘upper and lower limbs.
From the observation of above pictures,
a. What elements do you think the nurse will assess newborn ‘limbs?b. Define the term polydactyl?
Each newborn baby is carefully checked at birth for signs of problems or
complications. The healthcare provider will do a complete physical exam, on limbs,
the associate nurse assesses arms, Legs, Hands, and Feet. He/she checks for any
symmetricity, abnormal length and deviations, fractures, paralysis, and weakness.
He/she also assesses if there is polydactyly, syndactyly and abnormal skin creases.
Polydactyl condition of having more than the normal number of fingers or toes.
Hips: On hips, the associate nurse assesses the range of motion adequate and click.
If any deviation, it indicates congenital hip dislocation through these maneuvers;
The Barlow manoeuvre involves flexing the new-born’s hips and knees at 90
degrees and applying gentle pressure downwards. The Barlow test is considered
to be positive if the examiner feels the head of the femur slip out of the hip socket.
The Ortolani manoeuvre is performed after the Barlow manoeuvre. It confirms hip
displacement and returns the displaced bone back into the hip socket. The Ortolani
manoeuvre involves abducting (moving apart) the flexed legs while applying a
gentle forward pressure with the middle finger against the head of the femur. An
audible ‘clunk’ can be heard when the femoral head returns to the hip socket.
Plantar creases: These are creases on the soles of the feet. They can range from
absent to covering the entire foot, depending on the maturity.
Various Congenital malformations that can be detected while doing limbsassessment.
Self-assessment 6.9
1. What the associate nurse assesses on the newborn’s hands?
2. What the associate nurse assesses on the newborn’s legs and feet?
3. What will the associate assess on the newborn’s hips?4. Define the term plantar creases?
6.10 Assessment of the skin
Learning Activity 6.10Observe these images illustrating the newborn ‘skin
From the observation of above pictures,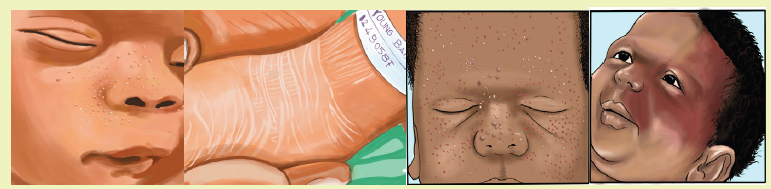
a. What elements do you think the nurse will assess for the newborn ‘skin?b. What do you think about lanugo hair?
The skin of a healthy newborn at birth has:
• Deep red or purple skin and bluish hands and feet. The skin darkens before
the infant takes their first breath (when they make that first vigorous cry).
• A thick, waxy substance called vernix covering the skin. This substance
protects the foetus’s skin from the amniotic fluid in the womb. Vernix should
wash off during the baby’s first bath.
• Fine, soft hair (lanugo) that may cover the scalp, forehead, cheeks, shoulders,
and back. This is more common when an infant is born before the due date.
The hair should disappear within the first few weeks of the baby’s life.
• New-born skin will vary, depending on the length of the pregnancy. Premature
infants have thin, transparent skin. The skin of a full-term infant is thicker.
• By the baby’s second or third day, the skin lightens and may become dry and
flaky. The skin still often turns red when the infant cries. The lips, hands, and
feet may turn bluish or spotted (mottled) when the baby is cold.
The associate nurse assesses the following on the newborn’s skin:
Normal - Short-term (resolves in days to months)
For normal short-term skin conditions, the associate nurse checks for
• Miliaria (Heat Rash)
• Petechiae on scalp and face after vertex delivery
• Vernix Caseosa (Cheesy white skin covering present at birth)
• Transient vascular phenomena like skin mottling related to cold exposure and
positional erythema on the dependent side of the body)
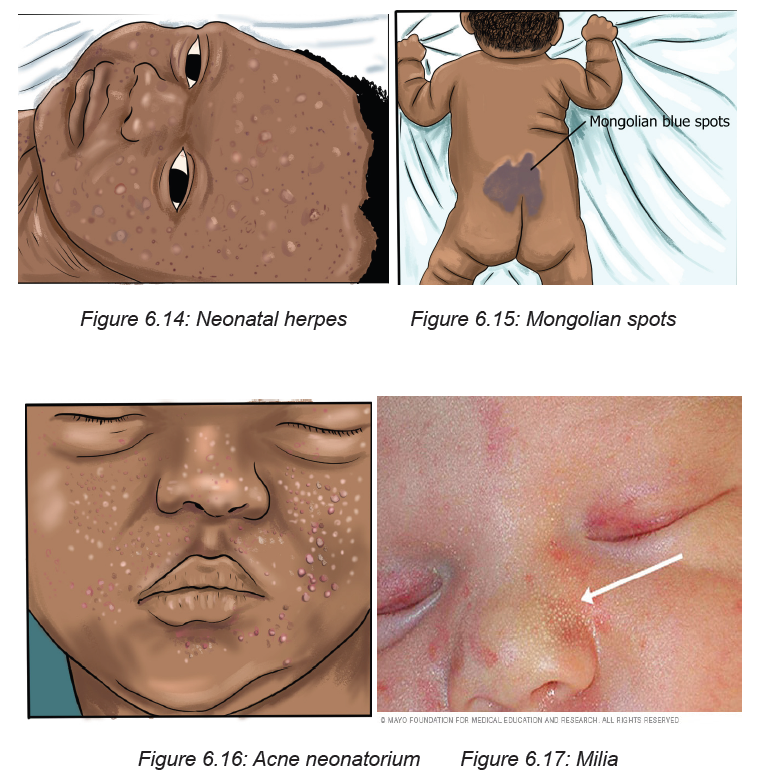
Normal - Short-term (resolves in days to months):
The associate nurse checks for:
• Erythema toxicum neonatorum (Yellow papules on red base affected face
and trunk, disappearing within days to a week
• Neonatal Pustular Melanosis(Milky fluid filled Vesicles without erythema, <5
mm on torso, buttock, forehead, chin
• Milia (Pinpoint white, keratin-filled Papules (blocked sebaceous glands) on
nose and cheeks
• Lanugo (Fine hair on Shoulders and back). If too much, it can indicate
prematurity
• Spontaneous Fat Necrosis
• Acne Neonatorum
Normal - Birthmarks, Long-term (Persists for months to years - some do not
resolve)
• See abnormal or risk-associated Birthmarks below (e.g. Congenital
Melanocytic Nevi)
• Mongolian Spots (Large up to 10 cm bluish-gray pigment patches on
extremities as well as lumbar, sacral and buttock region
• Nevus Simplex (Macular pink to red capillary dilations that fade with time,
occurring on upper Eyelids, forehead, nape of neck
• Hemangioma (Benign vascular lesions)
Important skin infection related lesions
• Neonatal Herpes Simplex Virus (Vesicular Lesions in infant born to mother
with HSV
• Congenital Syphilis (Lesions on palms and soles)
• Staphylococcal Scalded Skin
• Impetigo
Abnormal or lesions that require evaluation, specific management or
observation
• Pallor (indicates bleeding or Anemia)
• Jaundice onset within first day of life(indicates Hemolytic Disease of the
Newborn and Neonatal Jaundice)
• Cyanosis(can indicate respiratory distress, cardiovascular
disorders,hypoxia,etc)
• Mottling( can indicate Sepsis,or Hypothermia)
• Gray Skin Coloration( is a sign of metabolic Acidosis)
• Vesicles( can indicate Neonatal HSV)
• Bullae
• Nevus Sebaceus.It is a yellow hairless Plaque on scalp or face. It may be
associated with epidermal nevus syndrome and carries risk of future skin
cancer in 10-15% of cases
• Hyperpigmentation
• Cafe-Au-Lait Macule”Coffee with milk” (tan to brown) colored flat• Macule, <4 cm located on trunk
Self-assessment 6.10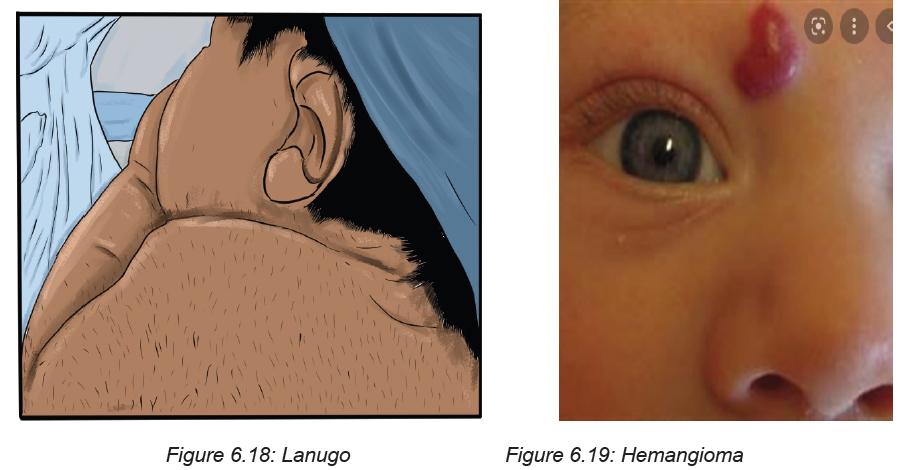
1. What are the normal short-term skin conditions that the associate nurse
checks on the newborn?
2. What are the Normal Birthmarks that the associate nurse checks on thenewborn?
6.11 Reflexes assessment
Learning Activity 6.11
Observe these images illustrating an associate nurse taking measurements tothe newborn baby.
From the observation of above pictures,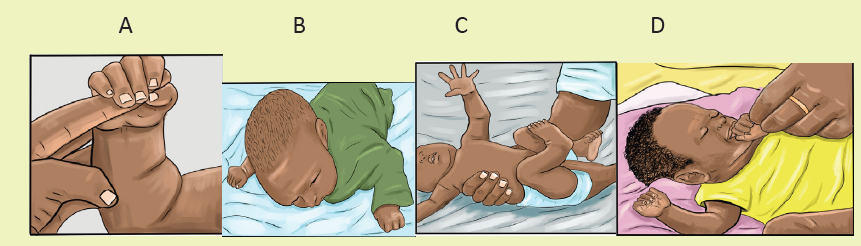
a. What reflex do you think the nurse is taking to that baby in the picture A,
B, C, D?b. What do you think about necessity of assessing reflexes on baby?
Reflexes are involuntary movements or actions. Some movements are spontaneous
and occur as part of the baby’s normal activity. Others are responses to certain
actions. Healthcare providers check reflexes to determine if the brain and nervous
system are working well. The presence and strength of a reflex is an important sign
of nervous system development and function. Many infant reflexes disappear as
the child grows older, although some remain through adulthood
Exam 1: Foot
a. Stroke Inner Sole: Toes curl around (“grasp”) examiner’s finger
b. Stroke Outer Sole (Babinski): Toes spread, great toe dorsiflexion
Exam 2: Doll’s Eyes and grasping reflexes
A. Give one forefinger to each hand - baby grasps both
1. Pull baby to sitting with each forefinger
B. Eyes open on coming to sitting (Like a Doll’s)
1.Head initially lags
2.Baby uses Shoulders to right head position
Exam 3: Primitive Stepping (Walking Reflex)
A. Hold baby up with one hand across chest
B. As feet touch ground, baby makes walking motion
Exam 4: Protective Reflex
a. Soft cloth is placed over the baby’s eyes and nose
b. Baby arches head and turns head side to side
c. Brings both hands to face to swipe cloth away
Exam 5: Rooting and sucking reflexes
a. Touch newborn on either side of cheek
b. Baby turns to find Breast
c. Sucking mechanism on finger is divided into 3 steps
1. Front of Tongue laps on finger
2. Back of Tongue Massages middle of the finger
3. Esophagus pulls on tip of finger
Exam 6: Tonic Neck (Fencing) Reflex
A. If the Babies’ head is rotated leftward
1. The left arm (face side) stretches into extension
2. The right arm flexes up above head
B. Opposite reaction if head is rotated rightward
Exam 7: Moro Reflex (Startle Reflex)
A. Hold supine infant by arms a few inches above bed
1.Gently drop infant back to elicit startle
B. Baby throws Arms out in extension and baby grimace
Exam 8: Hand-to-Mouth (Babkin) Reflex
A. Stroke newborns cheek or put finger in baby’s palm
B. Baby will bring his fist to mouth and suck a finger
Exam 9: Swimmer’s (Gallant) Response
A. Hold baby prone while supporting belly with hand
1. Stroke along one side of babies’ spine
B. Baby flexes whole body toward the stroked side
Exam 10: Crawling Reflex
A. Newborn placed on AbdomenB. Baby flexes legs under him and starts to crawl
Self-assessment 6.11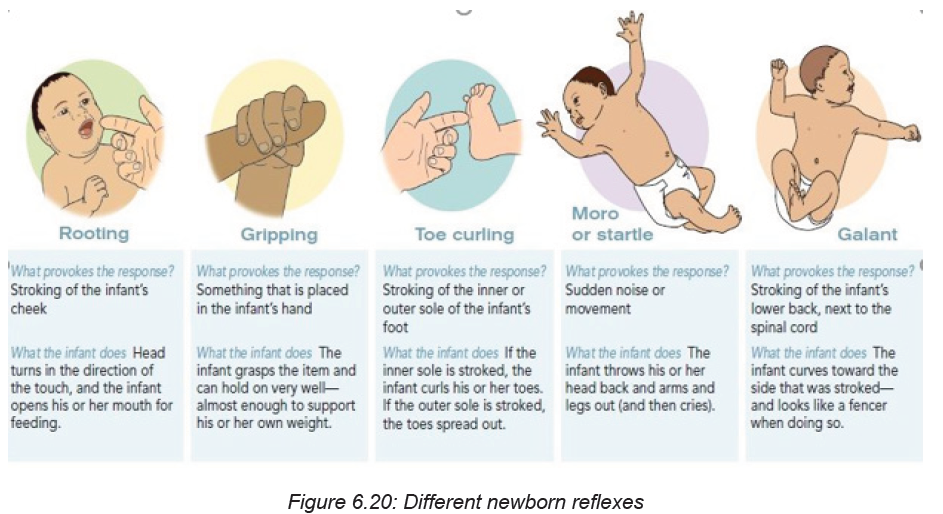
1. How will the associate nurse to check for Babinski reflex?
2. How the associate nurse checks for Moro Reflex (Startle Reflex)
3. Define the term reflex?4. What does it mean when reflexes are present?
6.12 Helping the Baby Breathe (HBB)
Learning Activity 6.12Observe these images illustrating steps of Helping the Baby Breathe (HBB)
1. What do you think about the Helping the Baby Breathe (HBB) program?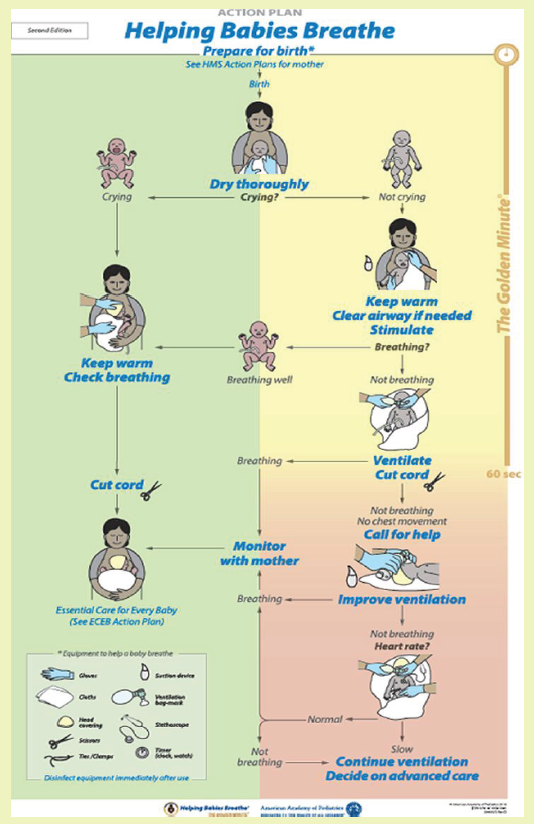
2. What do you think will be done to help the baby breathe in the first minute(Golden) of birth?
The first minutes after birth are critical to reducing neonatal mortality. Helping
Babies Breathe (HBB) is a simulation-based neonatal resuscitation program for low
resource settings.
The Golden Minute:
A key concept of HBB is The Golden Minute. Within one minute of birth, a baby
should be breathing well or should be ventilated with a bag and mask. The Golden
Minute identifies the steps that a birth attendant must take immediately after birth to
evaluate the baby and stimulate breathing.
HELPING BABY BREATHE INCLUDE:
Routine care
• Dry thoroughly
• Is the baby crying?
• Keep warm, check for breathing
• Clamp or tie the umbilical cord
Before delivery
• Identify a helper and review emergency plan
• Prepare the area for delivery
• Wash hands
• Prepare the area for ventilation
• Assemble disinfected equipment and supply
• Test the ventilation bag, mask
Materials
• Gloves
• Suction device
• Cloths
• Ventilation bag mask
• Head covering
• Stethoscope
• Scissors
• Ties or cord clamp
• Timer
Procedure
Dry the baby thoroughly at birth. Drying help keeping the baby to stay warm and
stimulates breathing. A newly born baby is wet and may become cold even in a
warm room.
• Dry the body, head, arms, and legs by rubbing gently with a cloth
• Drying the back provides important stimulation to breathe. Wipe the face,
clean of feces and blood.
• Drying can be done on the mother’s abdomen.
• Place a clean cloth on the mother’s abdomen before birth.
• Position the baby on the cloth and dry thoroughly.
• Remove the wet cloth and place the baby on skin to skin with the mother and
cover with a dry one. A baby who is crying is receiving routine care and kept
warm and check breathing.
• If the baby is not crying after drying he needs help to breathe in the golden
minute.
• Keep warm on mother abdomen or chest, or a warm area with dry blanket
beside the mother and cover the head
• Clear airway if needed
• Position the head. Position the neck slightly extended to keep airway open.
– The nose will be as far forward as possible.
– If the neck is flexed or extended too far, air may not enter freely.
– If secretions are not seen and there is no meconium, move directly to stimulate
breathing. Some babies will have a shallow, irregular, slow, or noisy breathing
immediately after birth. Other may have chest in-drawing or retractions. These
babies with abnormal breathing will require continued monitoring or their
breathing, heart rate, and color to decide if they need more help to breathe
• Decide what care the baby needs after clearing the airway and stimulation.
If the baby is breathing well, the baby can receive routine care. Continue to check
the breathing. Clamp or tie and cut the umbilical cord. Encourage breastfeeding in
the first hour.
If the baby is not breathing well (gasping or not breathing at all), begin ventilation
with bag and mask. Quickly move the baby to the area for ventilation. Delayingventilation may result in death or brain damage.
Self-assessment 6.12
1. What would happen within one minute of birth?
2. What are the routine cares provided in HBB?
3. Why is it important to dry thoroughly the baby in the golden minute?4. What are preparations of delivery area before delivery?
6.13 Breastfeeding
Breastfeeding is when baby is feed with breast milk, it is also called nursing. Breast
milk is the ideal food for infants. It is safe, clean and contains antibodies which
help protect against many common childhood illnesses. Breast milk provides all the
energy and nutrients that the infant needs for the first months of life, and it continues
to provide up to half or more of a child’s nutritional needs during the second half
of the first year, and up to one third during the second year of life. It’s best to try to
breastfeed the baby in the first hour after birth because by latching on and sucking
rhythmically, the breast begins switching on the cells to initiate the body’s breast
milk supply. is Exclusive breastfeeding recommended for 6 months. Even, after the
introduction of other foods, it recommends continuing to breastfeed through the
baby’s first year of life. Normally, newborns often want to feed every 2-3 hours.
Signs showing that the baby is hungry
One of the most common ways to know that the baby is hungry is ‘’cry’’. Other signs
showing that the baby wants to breastfeed include:
• Licking their lips or sticking out their tongue
• Rooting, which is moving their jaw, mouth, or head to look for your breast
• Putting their hand in their mouth
• Opening their mouth
• Fussiness
• Sucking on things.
Benefits of breastfeeding for the Baby
Breast milk provides the ideal nutrition for infants. It has a nearly perfect mix
of vitamins, protein, and fats it has everything that baby needs to grow. And it’s all
provided in a form more easily digested than infant formula.
• Breast milk contains antibodies that help your baby fight off viruses and
bacteria.
• Breastfeeding lowers your baby’s risk of having asthma or allergies. Plus,
babies who are breastfed exclusively for the first 6 months, without any formula,
have fewer ear infections, respiratory illnesses, and bouts of diarrhoea.
• They also have fewer hospitalizations and trips to the health care provider;
Breastfeeding has been linked to higher intellectual quatience (IQ) scores in
later childhood in some studies.
• What’s more, the physical closeness, skin-to-skin touching, and eye contact
all help your baby bond with you and feel secure. Breastfed infants are
more likely to gain the right amount of weight as they grow rather than
become overweight children.
Benefits of breastfeeding for the mother
• Breastfeeding burns extra calories, so it can help losing pregnancy
weight faster. It releases the hormone oxytocin, which helps uterus to
return to its pre-pregnancy size and may reduce uterine bleeding after birth.
Breastfeeding also lowers risk of breast and ovarian cancer.
• Breastfeeding is economic because no need to measure formula, sterilize
nipples, or warm bottles, it saves time and money.
• It also gives regular time to relax quietly to the mother with the newborn as
they bond.
The first few days after birth, breasts make ideal “first milk.” It’s called colostrum.
Colostrum is thick, yellowish, and there’s not a lot of it, but there’s plenty to meet
the baby’s nutritional needs. Colostrum helps a new-born’s digestive tract develop
and prepare itself to digest breast milk.
Colostrum is the first phase of breast milk, which changes over time the baby grows.
The second phase is called transitional milk. The colostrum is gradually replaced
with the third phase of breast milk, called mature milk.
The transitional milk starts few days after birth. By 10 to 15 days after birth, the
body make mature milk, which gives to the baby all the nutrition they need.
LATCHMENT
Position the baby facing the mother, so the baby is comfortable and doesn’t have to
twist the neck to feed. With one hand, the mother cups the breast and gently strokes
her baby’s lower lip with the nipple. The baby’s instinctive reflex will be to open
the mouth wide. With the mothers’ hand supporting the baby’s neck, brings the
mouth closer around her nipple, trying to centre the nipple in the mouth above the
baby’s tongue.
The mother will know the baby is “latched on” correctly when both lips are pursed
outward around the nipple. The baby should have all of nipple and most of the
areola in the mouth. While the mother feels a slight tingling or tugging, breastfeeding
should not be painful.
If the baby isn’t latched on correctly and nursing with a smooth, comfortable rhythm,
the mother gently nudges her pinky between the baby’s gums to break the suction,
remove the nipple, and try again. Good “latching on” helps prevent sore nipples.
Signs of a Good Latch
• The latch is comfortable and pain free.
• The baby’s chest and stomach rest against your body, so that baby’s head is
straight, not turned to the side, the chin touches your breast.
• The baby’s mouth opens wide around your breast, not just the nipple.
• The baby’s lips turn out.
Breast feeding positions
The associate nurse must teach and assist the mother to be in best, comfortable
and relaxed position and the mother must not strain to hold the position or keep
nursing. Here are some common positions for breastfeeding the baby:
Cradle position: The mother rests on the side of the baby’s head in the crook of
her elbow with the whole baby’s body facing the mother. The mother positions the
baby’s belly against her body so they feel fully supported. Other, “free” arm can
wrap around to support the baby’s head and neck or reach through the baby’s legsto support the lower back.
Football position: The mother lines the baby’s back along the mother’s forearm to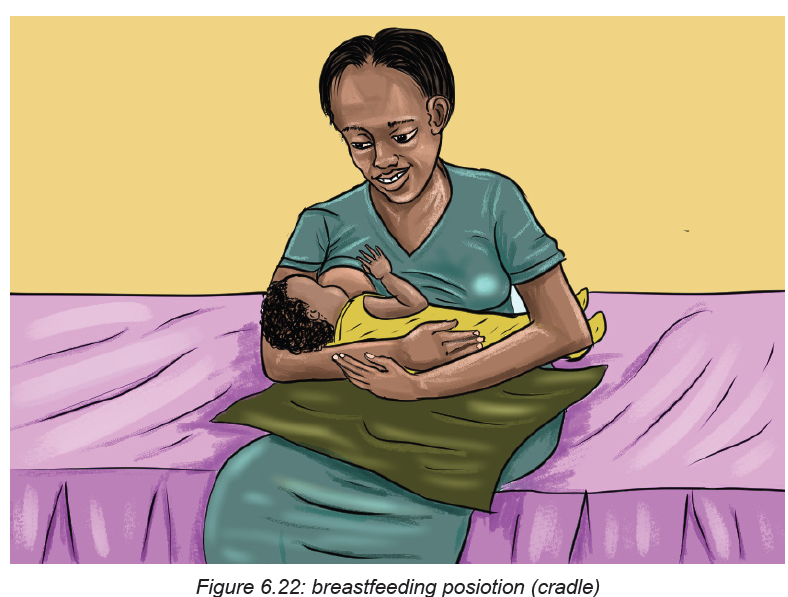
hold the baby like a football, supporting the head and neck in her palm.
This works best with new-borns and small babies. It’s also a good position for the
mother recovering from a cesarean birth and need to protect the belly from thepressure or weight of the baby.
Side-lying position: This position is great for night feedings in bed. Side-lying also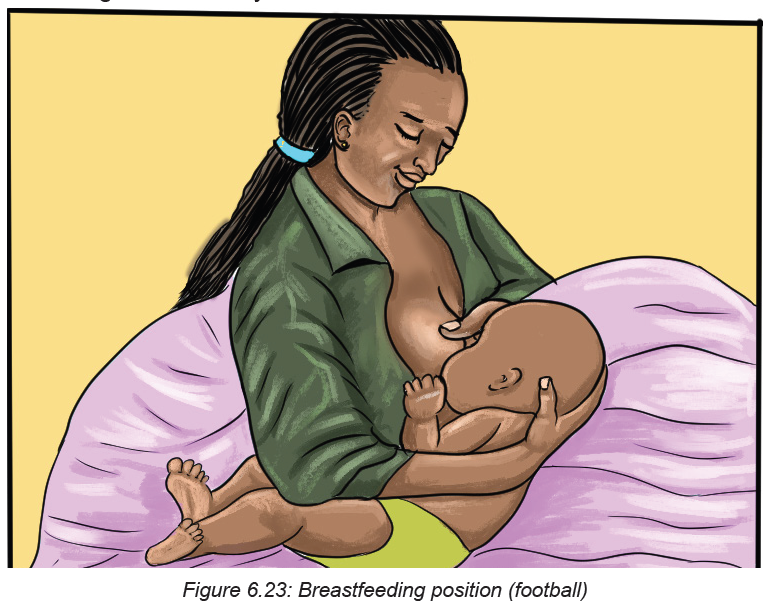
works well if the mother is recovering from an episiotomy, an incision to widen
the vaginal opening during delivery. The mother uses pillows under head to get
comfortable. Then snuggle close to the baby and the mother use her free hand to
lift the breast and nipple into the baby’s mouth. Once the baby is correctly “latched
on,” the mother supports the baby’s head and neck with her free hand so there’s notwisting or straining to keep nursing.
Cross-cradle hold: The mother sits straight in a comfortable chair that has armrests.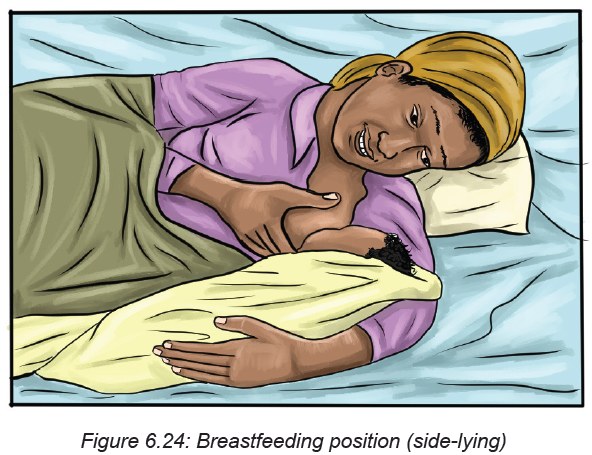
The mother holds her baby in the crook of her arm that’s opposite the breast she will
use to feed them. The mother supports the baby’s head with her hand. She brings
the baby across her body in a way that her tummies face each other. She uses her
other hand to cup the breast in a U-shaped hold. She brings the baby’s mouth toher breast and cradles them close, and does not lean forward.
Laid-back position: This position, also called biological nurturing, is a lot like it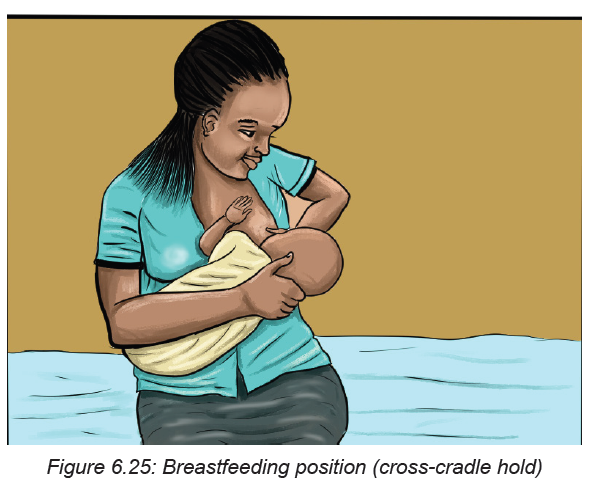
sounds. It’s meant to tap into the natural breastfeeding instincts the mother and
baby have. The mother leans back, but not flat, on a couch or bed. The mother
ensures good supports of her head and shoulders. She holds the baby in entire
fronts touch. She lets the baby take any position they’re comfortable in as long ascheek rests near her breast. The mother helps the baby latch on if he needs it.
Self-assessment 6.13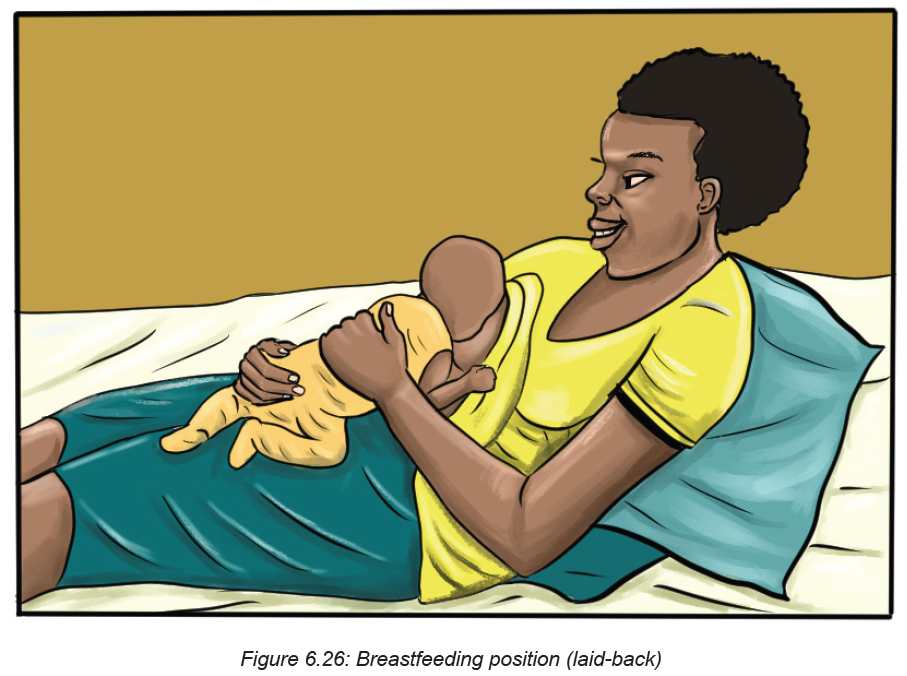
1. When the newborn has to start breastfeeding after birth
2. What are the advantages of breastfeeding to the mother?
3. Which period fit for exclusive breast feeding?
4. What is colostrum?
5. What are the advantages of breastfeeding to the baby?
6. Enumerate comfortable positions that the mother can take whilebreastfeeding.
End unit assessment 6
SECTION A. MULTIPLE CHOICE QUESTIONS
1. The associate nurse is assessing the one minute APGAR score of a newborn
baby. On assessment, the associate nurse notices the following complains on the
newborn patient: heart rate 130, pink body and hands with cyanotic feet, weak
cry, flexion of the arms and legs, active movements and crying when stimulated.
What is the newborn’s APGAR score?
g. APGAR 9
h. B. APGAR 10
i. APGAR 8
j. APGAR 5
2. The associate nurse is assessing the one minute APGAR score of the newborn
baby. On the assessment, he/ she notice the following problems on the newborn
patient: heart rate 101, cyanotic body and extremities, no response to stimulation,
no flexion of extremities, and weak cry. What is the newborn’s APGAR score?
a. APGAR 4
b. APGAR 6
c. APGAR 3
d. APGAR 2
3. A newborn’s fifth minute APGAR score is 5. Which of the following nursing
interventions will the associate nurse provide to this newborn?
e. Routine post-delivery care
f. Continue to monitor and reassess the APGAR score in 10 minutes
g. Some resuscitation assistance such as oxygen and rubbing baby’s back
and reassess APGAR score
h. Full resuscitation assistance is needed and reassess APGAR score.
4. The associate nurse in a delivery room is assisting for the delivery of a
newborn baby. After the delivery, which nursing intervention that the associate
nurse should perform in order s to prevent the heat loss in the newborn as the
result of result of evaporation:
a. Warming the crib pad
b. Turning on the overhead radiant warmer
c. Closing the doors to the room
d. Drying the infant in a warm towel
5. The associate nurse in a newborn nursery is performing an assessment
of a newborn baby. The associate nurse is preparing to measure the head
circumference of the baby and he/ she would most appropriately:
a. Wrap the tape measure around the infant’s head and measure just above
the eyebrows.
b. Place the tape measure under the infant’s head at the base of the skull and
wrap around to the front just above the eyes.
c. Place the tape measure under the infant’s head, wrap around the occiput,
and measure just above the eyes.
d. Place the tape measure at the back of the infant’s head, wrap around
across the ears, and measure across the infant’s mouth.
6. During an assessment of the new born, the associate nurse notes that when
the baby’s head is turned to the right side, the leg and arm on the right side will
extend, while the leg and arm on the left side will also flex. The associate nurse
documents this as what type of reflex?
a. Rooting Reflex
b. Sucking Reflex
c. Moro Reflex
d. Tonic Neck Reflex
7. The associate nurse notes that when a finger is placed under the toes of the
newborn, the toes will curl downward. This is known as the ……?
a. Babinski reflex
b. Plantar grasp reflex
c. Tonic neck reflex
d. Step reflex
8. When does the sucking reflex in an infant disappear and become voluntary?
a. 6 months
b. 2 months
c. 4 months
d. 12 months
9. Speeding of postpartum recovery is the one of the benefits of breastfeeding to
the mother. Respond by True or False.
a. True
b. False
10. True or False: To maintain a schedule, a breastfed baby should only be fed
every three hours.
a. True
b. False
c. SECTION B: SHORT ANSWERS
11. What is the difference between the baby’s chest and head circumferences?
12. When the head and chest circumference may be equal?
13. How to check for audibility while assessing the newborn baby?
14. How will the associate nurse know the clavicle injury to the newborn?
15. What will the associate nurse check on newborn’s nose?
16. What is hypotelorism and hypertelorism?
17. What is the pseudo menstruation?
18. What are the signs of potential distress or deviations from expected findings
the associate nurse will notice while assessing the respiration patterns for the
baby?
19. List 5 Abnormal findings or lesions on the newborn ‘skin that require
evaluation, specific management or observation
20. Why does the healthcare providers need to check for reflexes
21. In HBB, what is done by the health care provider before delivery?
22. What are the signs showing that the baby is hungry and needs to breastfeed?
REFERENCES
1. Annama, J. (2012). A COmprehensive Textbook Of Midwifery & Gynecological
Nursing
2. Breastfeeding. A Guide for the Medical Profession Book • Ninth Edition •
2021. By Ruth A. Lawrence & Robert M. Lawrence
3. Committee, F. S. M. and N. H. (SMNH) (2012) ‘Management of the second
stage of labor’, International Journal of Gynecology & Obstetrics, 119(2), pp.
111–116. doi: https://doi.org/10.1016/j.ijgo.2012.08.002.
4. Deitra, L., Shannon, E., Kitty, C. (2016). Maternity women’s health care. 11th
Edition
5. Durham, R. and Chapman, L. (2013) Maternal-newborn nursing: The critical
components of nursing care. FA Davis.
6. Early essential newborn care. Clinical practice pocket guide. First Embrace.
By World Health Organization
7. Edmonds, K. (2018) Dewhurst’s Textbook of Obstetrics & Gynaecology. John
Wiley & Sons.
8. Examination of the Newborn. A Practical Guide. By Helen Baston,Heather
Durward. 2017.
9. Fuwa, K. et al. (2021) ‘Umbilical cord milking versus delayed cord clamping in
term infants: a systematic review and meta-analysis’, Journal of Perinatology,
41(7), pp. 1549–1557.
10. Hadlow, N. (2017). Biochemical Changes in Pregnancy-What Should A
Clinician Know ?, 4(1), 8–11. https://doi.org/10.19080/JGWH.2017.04.555626
11. Jacob, A. (2018) A Comprehensive Textbook of Midwifery & Gynecological
Nursing. Jaypee Brothers Medical Publishers.
12. Kloser, N. jayn., & Hatfield, N. T. (2010). Introductory Maternity and Pediatric
Nursing. China. Edition 2
13. Macdonald, S., & Magill-Cuerden, J. (2010). Mayer’s Midwifery Fourteeth
Edition. Bailliere Tindall Elsevier.
14. Marshall, H. K., John, H. K., & Phyllis, H. K. (2012). THE DOULA BOOK :
How a trained Labor Companion can help you have a Shorter , Easier,
and Healthier Birth (Third Edit). MERLOYD LAWRENCE BOOK DA CAPO
PRESS.
15. Marshall, J., & Raynor, M. (2014). Myles TEXT BOOK FOR MIDWIVES
(sixteen ed). Elsevier.
16. PCEP Maternal and Fetal Evaluation and Immediate Newborn Care (Book
I) (3rd Edition). By Robert A. Sinkin, MD, MPH, FAAP;Christian A. Chisholm,
MD, FACOG
17. Perry, L., & Alden, C. (2016). Maternal &Women’s Health Care. (E. F.olshansky,
Ed.) (11th Editi). St. Louis, Missouri: Elsevier.
18. Physical Assessment of the Newborn: A Comprehensive Approach to the
Art of Physical Examination, Fifth Edition. By Ellen P. Tappero&Marry Ellen
Honeyfield.
19. Regan, J., VanPutte, C., & Russo, A. (2016). SEELEY’S ESSENTIALS OF
ANATOMY & PHYSIOLOGY (Ninth edit). MC Graw Hill Education.
20. The Student Guide to the Newborn Infant Physical Examination. By Tracey
Jones.2020.
21. Weeks, A. (2007) ‘Umbilical cord clamping after birth’, BMJ (Clinical research
ed.), 335(7615), pp. 312–313. doi: 10.1136/bmj.39282.440787.80.
22. WHO (2009) WHO guidelines for the management of postpartum haemorrhage
and retained placenta. World Health Organization.
23. WHO (2018) WHO recommendations on intrapartum care for a positivechildbirth experience. World Health Organization.
