Topic outline
UNIT 1 NORMAL PREGNANCY
Key Unit competence: Identify the characteristics of a normal pregnancy.Introductory activity 1.0
A 21 years old woman was admitted in consultation room at the health center
complaining of nausea and vomiting in early hours of the morning, frequent
urination, fatigue, loss of appetite, abdominal pain and not able to carry out
normal daily activities. During interview, she reported to be married 4 months
ago, living with a husband and missed her periods 6 weeks ago. On head-to-toe
examination, breasts were tender and full.
After reading and understanding the above scenario, based on your experiencesinterpret the above case.
1.1 Key concepts used in pregnancyLearning Activity 1.1
Pregnancy begins from the conception when the egg and sperm fuse together
and fertilization takes place. The fertilized egg becomes a zygote. Then, it
initiates organized development of a biological entity known as embryo, with a
human nuclear genome or altered human nuclear genome that has the potential
to develop up to, or beyond, the stage at which the primitive vein appears, and
has not yet reached 8 weeks of development since the first mitotic division to
become a fetus. The zygote that was formed after fertilization travels through the
oviduct to the uterus, which is a hollow muscular organ that plays a remarkable
role in pregnancy by stretching and expanding. The outer layer of the embryo
begins to merge with the endometrium (inner membrane of the uterus), and
thereafter (after getting pregnant) there is a formation of an organ which attaches
to the uterus called placenta that provides oxygen and nutrients to the growing
baby and remove waste products from the baby’s blood.
Based on the above passage, explain the following terms:
a. Pregnancy
b. Fertilization
c. Uterus
d. Placenta
e. Embryo
f. Fetus
The normal pregnancy starts from the conception, formation of the embryo and
fetus, progressive growth of uterus from the pelvic organ to become an abdominal
organ under the influence of hormones.
a. Pregnancy
Pregnancy is the time during which one or more fetus develop inside a woman.
It usually last about 40 weeks or nine months from the Last Menstrual Period.
Pregnancy can occur by sexual intercourse or assisted reproductive technology.
It always happens when a sperm fertilizes an egg after it’s released from the
ovary during ovulation. The fertilized egg then travels down into the uterus, where
implantation occurs. A successful implantation results in pregnancy.
b. Fertilization
Human fertilization also known as conception is the fusion of the genetic material of
the haploid sperm cell and the secondary oocyte to form the zygote. This process
takes approximately 12 to 24 hours and normally occurs in the ampulla of the
uterine tube.
c. Uterus
The uterus is a hollow muscular organ located in the female pelvis between the
bladder and rectum. It has three muscular layers, the internal layer (endometrium),
the middle muscular layer of the uterine wall (myometrium) and the outer layer
(perimetrium). Once the egg has left the ovary it can be fertilized and implant itself in
the lining of the uterus. The main function of the uterus is to nourish the developing
fetus prior to birth.
d. Placenta
The placenta is an organ that develops from throphoblasts in uterus during
pregnancy. This structure provides oxygen and nutrients to the growing baby and
removes wastes products from the baby’s blood. The placenta attaches to the wall
of the uterus and the baby’s umbilical cord arises from it.
e. Embryo
The embryo in human is defined as the developing organism from the fourth day
after fertilization to the end of the eighth week and undergoes early stages of growth
and differentiation.
f. Fetus
The fetus is an unborn baby that develops and grows inside the uterus (womb).The baby is referred to as a fetus from 8 weeks of gestation (pregnancy) until birth.
Self-assessment 1.1
1) Differentiate the embryo from fetus as human development stages.
2) Describe the Characteristics of Embryo & Fetus3) Where does the placenta develop from during the embryonic stage?
1.2 GametogenesisLearning Activity 1.2
A couple who has been married for over 2 years but have failed to reproduce
offspring was received in consultation. The woman is 40 years old and the
husband 52 years old. They both weigh 96kg. The husband is a tanker driver
and always exposed to the heat from the engine of the truck... He smokes 2
packets of cigarettes per day, at home, they reside near to an industrial plant
that produces pesticides, which pollute the nearby water source and their small
vegetable farm. The wife complained of irregular cycles for the past 3 years.
The wife states that before marriage, she has been using contraceptives pills
but stopped after her marriage. They came in consultation to seek solutions for
their problem.
1) With your knowledge and understanding of S3 biology, what do you think
are the possible causes for the delay in conception?
2) What advice can you give to them based on your knowledge andunderstanding of S3 biology.
In preparation for fertilization, germ cells undergo gametogenesis, which includes
meiosis, to reduce the number of chromosomes and differentiation to complete
their maturation.
The process of differentiation of a spermatogonium into a spermatid is known as
spermatogenesis. It is a complex, temporal event whereby primitive, totipotent
stem cells divide to either renew themselves or produce daughter cells that become
specialized testicular spermatozoa over a span of weeks. Spermatogenesis involves
both mitotic and meiotic proliferation. as well as extensive cell remodeling.
Spermatogenesis can be divided into three major phases: (1) proliferation and
differentiation of spermatogonia, (2) meiosis, and (3) spermiogenesis, a complex
metamorphosis that transforms round spermatids arising from the final division
of meiosis into a complex structure called the spermatozoon. In humans, the
process of spermatogenesis starts at puberty and continues throughout the entire
lifespan of the individual. It takes place in the lumen of the seminiferous tubules.
In fact, 90% of the testis volume is determined by the seminiferous tubules and
their constituent germ cells at various stages of development. Once the gonocytes
have differentiated into fetal spermatogonia, an active process of mitotic replication
is initiated very early in embryonic development. This appears to be under FSH
control and develops the baseline number of precursor cells of the testicle.
Proliferation and Differentiation of Spermatogonia
Within the seminiferous tubule, germ cells are arranged in a highly ordered
sequence from the basement membrane to the lumen. Spermatogonia lie directly
on the basement membrane, followed by primary spermatocytes, secondary
spermatocytes, and spermatids as they progress toward the tubule lumen. The
tight junction barrier supports spermatogonia and early spermatocytes within the
basal compartment and all subsequent germ cells within the luminal compartment.
Spermatocytogenesis
The purpose of spermatogenesis is to produce genetic material necessary for the
replication of the species through mitosis and meiosis. Spermatocytogenesis takes
place in the basal compartment. Primary spermatocytes enter the first meiotic
division to form secondary spermatocytes. Prophase of the first meiotic division
is very long, and the primary spermatocyte has the longest lifespan. Secondary
spermatocytes undergo the second meiotic division to produce spermatids.Secondary spermatocytes are short-lived (1.1 to 1.7 days).
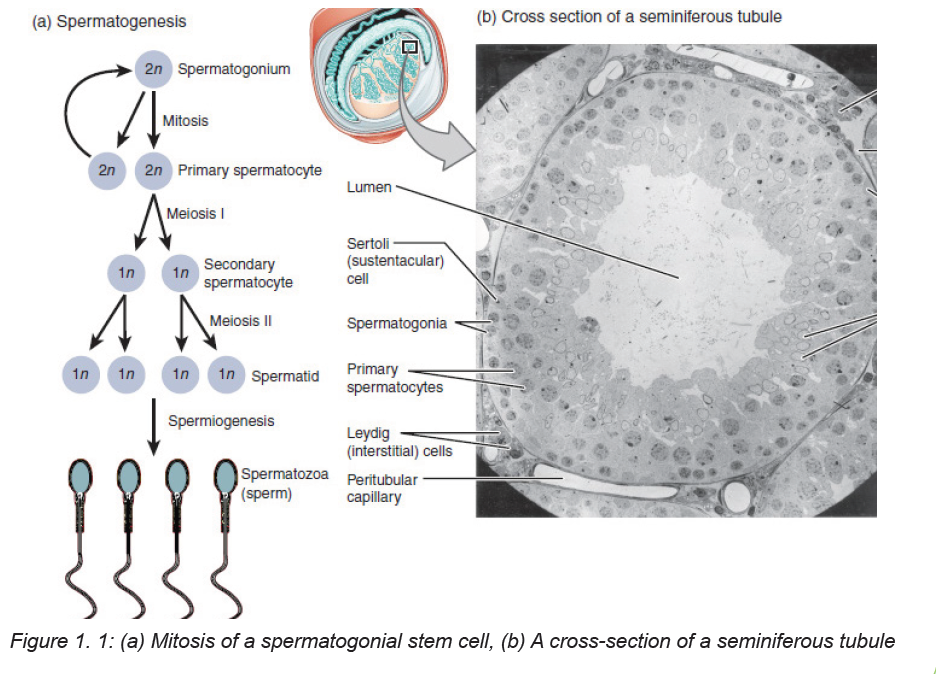
Mitosis
Mitosis involves proliferation and maintenance of spermatogonia. It is a precise,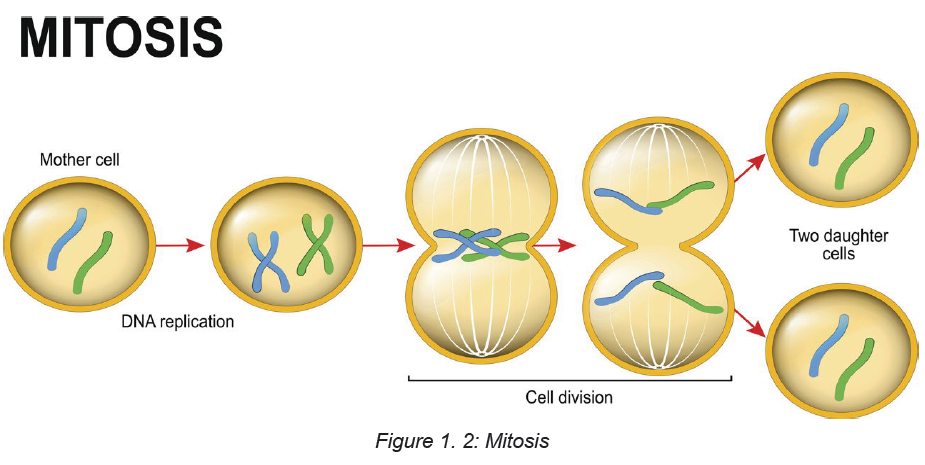
well-orchestrated sequence of events involving duplication of the genetic material
(chromosomes), breakdown of the nuclear envelope, and equal division of
the chromosomes and cytoplasm into two daughter cells. DNA is also spatially
organized into loop domains on which specific regulatory proteins interact during
cellular replication. The mitotic phase involves spermatogonia (types A and B) and
primary spermatocytes (spermatocytes I). Developing germ cells interconnected by
intracellular bridges produce the primary spermatocyte through a series of mitotic
divisions. Once the baseline number of spermatogonia is established after puberty,
the mitotic component will proceed in order to continue to provide precursor cellsand to start the process of differentiation and maturation.
Meiosis
Meiosis is a complex process with specific regulatory mechanisms of its own.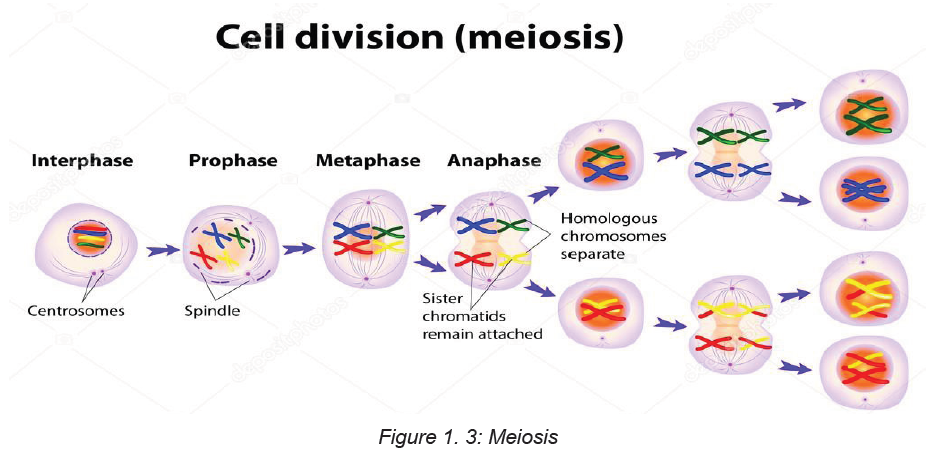
The process commences when type B spermatogonia lose their contact with the
basement membrane to form preleptotene primary spermatocytes. Thus, each
primary spermatocyte can theoretically yield four spermatids, although fewer
actually result, because some germ cells are lost due to the complexity of meiosis.
The primary spermatocytes are the largest germ cells of the germinal epithelium.
Meiosis is characterized by prophase, metaphase, anaphase, and telophase. In
this, two successive cell divisions yield four haploid spermatids from one diploid
primary spermatocyte. As a consequence, the daughter cells contain only half of
the chromosome content of the parent cell. After the first meiotic division (reduction
division), each daughter cell contains one partner of the homologous chromosome
pair, and they are called secondary spermatocytes. These cells rapidly enter the
second meiotic division (equational division), in which the chromatids then separate
at the centromere to yield haploid early round spermatids. Meiosis assures genetic
diversity and involves primary and secondary spermatocytes, which give rise tospermatids.
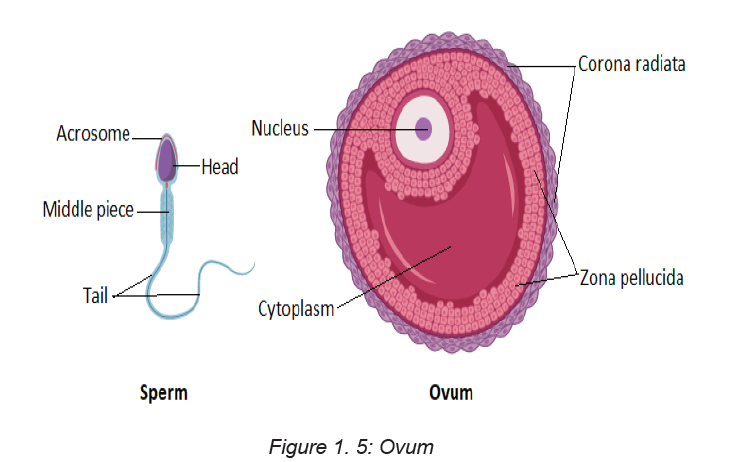
Ovum
The unequal cell division of oogenesis produces one to three polar bodies that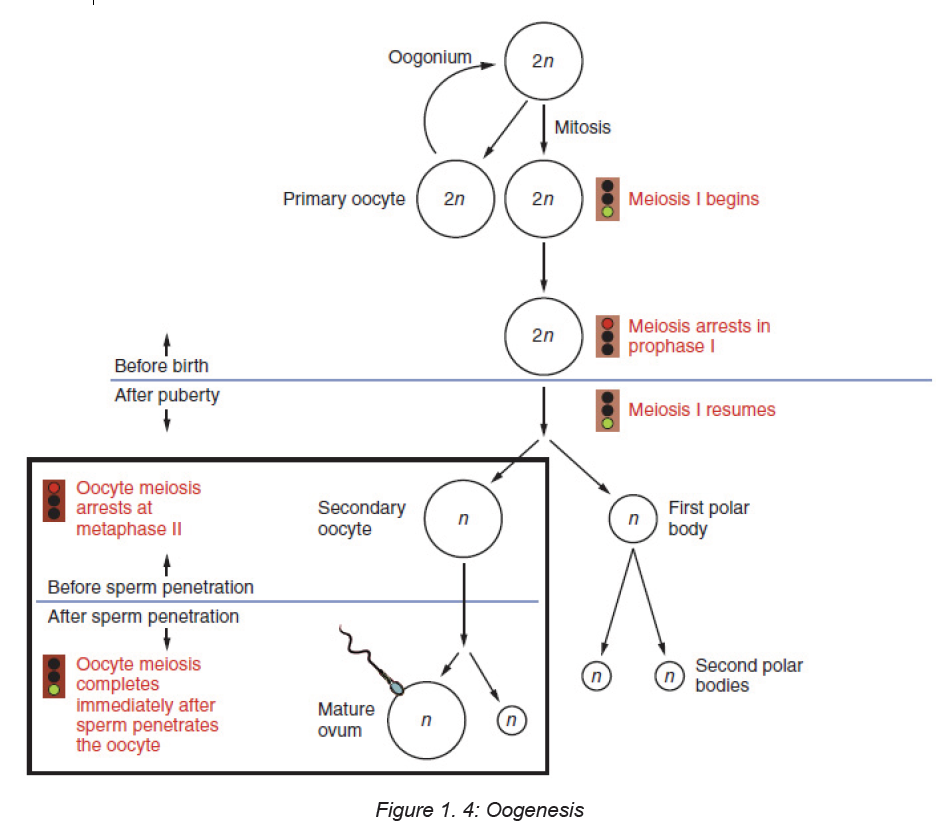
later degrade, as well as a single haploid ovum, which is produced only if there is
penetration of the secondary oocyte by a sperm cell.
Meiosis occurs in the female in the ovarian follicles and produces an egg, or ovum.
Each month one ovum matures with a host of surrounding supportive cells. At
ovulation the ovum is released from the ruptured ovarian follicle. High estrogen
levels increase the motility of the uterine tubes so their cilia are able to capture
the ovum and propel it through the tube toward the uterine cavity. An ovum cannot
move by itself. Two protective layers surround the ovum. The inner layer is a thick,
acellular layer, the zona pellucida. The outer layer, the corona radiata, is composed
of elongated cells.
Ova are considered fertile for about 24 hours after ovulation. If not fertilized by asperm, the ovum degenerates and is resorbed.
Ejaculation during sexual intercourse normally propels about a teaspoon of semen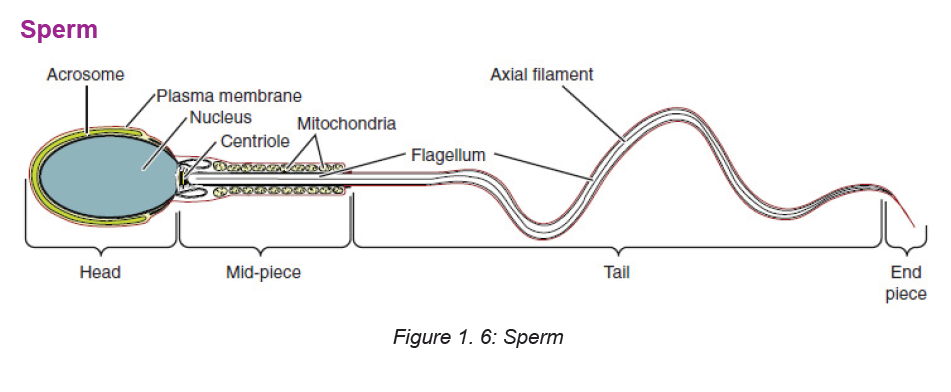
containing as many as 200 to 500 million sperm, into the vagina. The sperm swim
propelled by the flagellar movement of their tails. Some sperm can reach the site of
fertilization within 5 minutes, but average transit time is 4 to 6 hours. Sperm remain
viable within the woman’s reproductive system for an average of 2 to 3 days. Most
sperm are lost in the vagina, within the cervical mucus, or in the endometrium, or
they enter the uterine tube that contains no ovum. As the sperm travel through
the female reproductive tract, enzymes are produced to aid in their capacitation.
Capacitation is a physiologic change that removes the protective coating from
the heads of the sperm. Small perforations then form in the acrosome (a cap on
the sperm) and allow enzymes (e.g., hyaluronidase) to escape. These enzymes
are necessary for the sperm to penetrate the protective layers of the ovum beforefertilization.
Self-assessment 1.2
1) Describe the process of gametogenesis
2) Differentiate between spermatogenesis and oogenesis3) What are the differences between meiosis and mitosis?
1.3 Fertilization
Learning Activity 1.3
Using the diagram above:
a. Explain the process and stages of fertilization.b. What is capacitation?
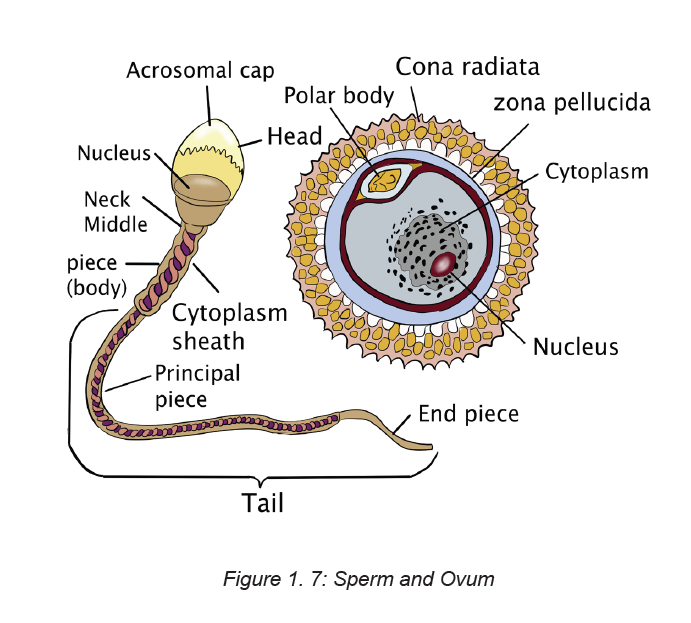
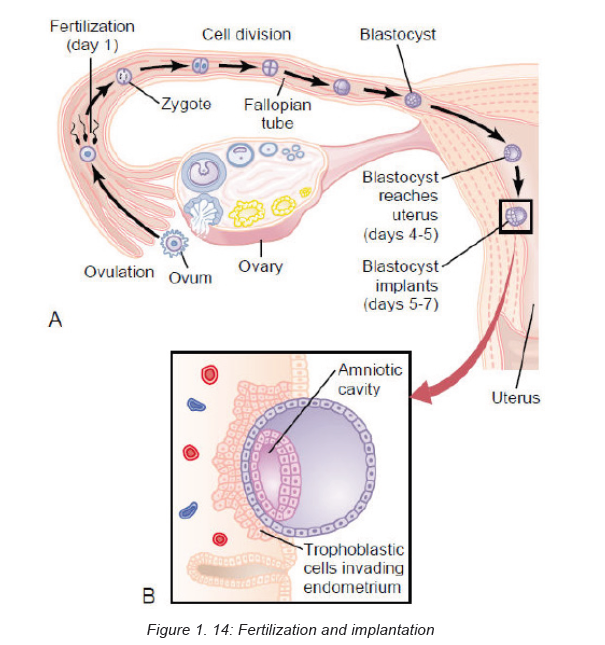
Fertilization occurs as a result of the female gamete, or oocyte, merging with the
male gamete, or spermatozoon. It is more commonly known as conception.
After the point of fertilization, the fused product of the female and male gamete is
referred to as a zygote or fertilized egg. For species that undergo internal fertilization,
such as humans, the fusion of male and female gametes usually occurs following
the act of sexual intercourse. However, the advent of artificial insemination and
in vitro fertilization have made achieving pregnancy possible without engaging in
sexual intercourse. This approach may be undertaken as a voluntary choice or dueto infertility.
The process of fertilization occurs in several steps and the interruption of any of
them can lead to failure. At the beginning of the process, the sperm undergoes a
series of changes, as freshly ejaculated sperm is unable or poorly able to fertilize.
The sperm must undergo capacitation (process where sperm undergoes changes
to the plasma membrane, resulting in the removal of the glycoprotein coat and
increased flagellation), in the female’s reproductive tract over several hours, which
increases its motility and destabilizes its membrane. By destabilizing the membrane,
the sperm prepares for the acrosome reaction, the enzymatic penetration of the
egg’s tough membrane, the zona pellucida. The sperm and the egg cell (which has
been released from one of the female’s two ovaries) unite in one of the two fallopian
tubes.
The fertilized egg, known as a zygote, then moves toward the uterus, a journey that
can take up to a week to complete until implantation occurs. Through fertilization,
the egg is activated to begin its developmental process (progressing through
meiosis II), and the haploid nuclei of the two gametes come together to form the
genome of a new diploid organism.
Nondisjunction during the completion of meiosis or problems with early cell
division in the zygote to blastula stages can lead to problems with implantation and
pregnancy failure.
Fertilization takes place in the ampulla (outer third) of the uterine tube. When a
sperm successfully penetrates the membrane surrounding the ovum, both sperm
and ovum are enclosed within the membrane, and the membrane becomes
impenetrable to other sperm; this process is termed the zona reaction. The second
meiotic division of the secondary oocyte is then completed, and the nucleus of
the ovum becomes the female pronucleus. The head of the sperm enlarges to
become the male pronucleus, and the tail degenerates. The nuclei fuse, and the
chromosomes combine, restoring the diploid number (46). Conception is said tohave taken place.
A, Ovum fertilized by X-bearing sperm to form female zygote.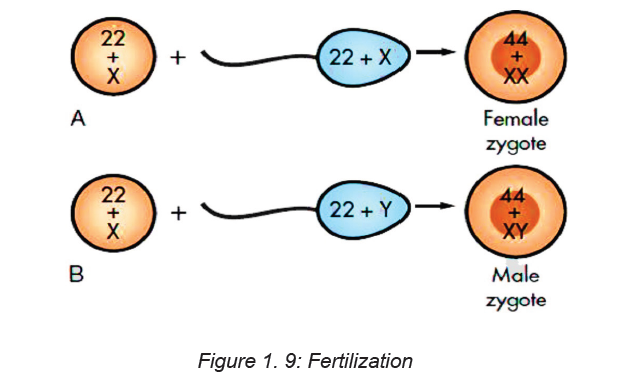
B, Ovum fertilized by Y-bearing sperm to form male zygote.
Mitotic cellular replication, called cleavage, begins as the zygote travels the length
of the uterine tube into the uterus. This transit takes 3 to 4 days. Because the
fertilized egg divides rapidly with no increase in size, successively smaller cells,
blastomeres, are formed with each division. A 16-cell morula, a solid ball of cells,is produced within 3 days and is still surrounded by the protective zona pellucida.
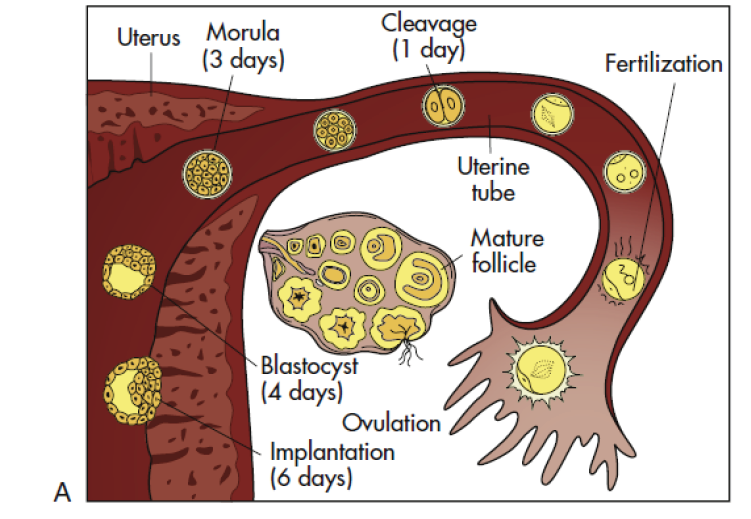
A, Follicular development in the ovary, ovulation, fertilization, and transport of the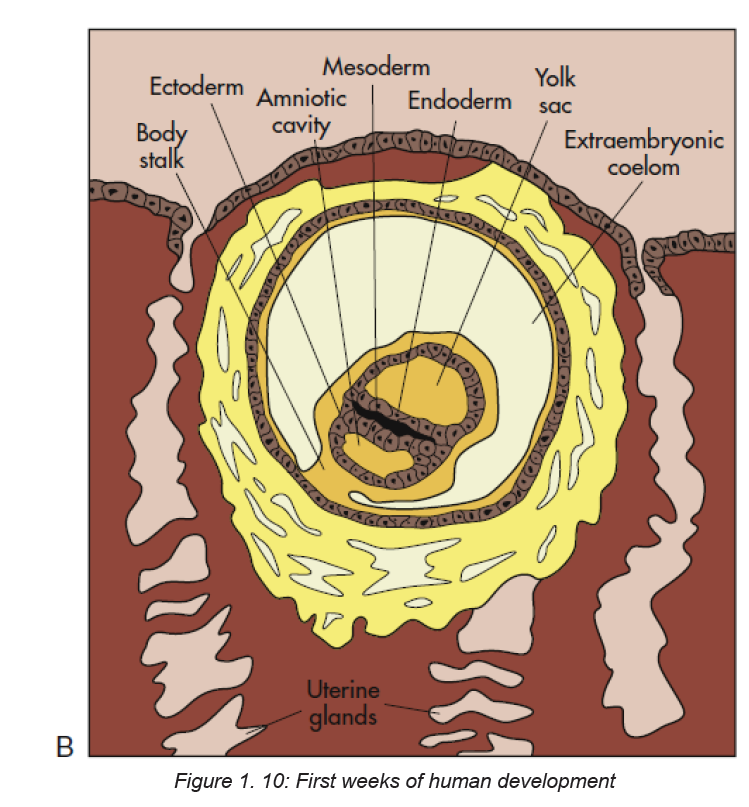
early embryo down the uterine tube and into the uterus, where implantation occurs.
B, Blastocyst embedded in endometrium. Germ layers forming.
Further development occurs as the morula floats freely within the uterus. Fluid
passes through the zona pellucida into the intercellular spaces between the
blastomeres, separating them into two parts, the trophoblast (which gives rise to
the placenta) and the embryoblast (which gives rise to the embryo). A cavity forms
within the cell mass as the spaces come together, forming a structure called the
blastocyst cavity. When the cavity becomes recognizable, the whole structure of
the developing embryo is known as the blastocyst. Stem cells are derived from the
inner cell mass of the blastocyst. The outer layer of cells surrounding the blastocyst
cavity is the trophoblast. The trophoblast differentiates into villous and extravillous
trophoblast.
Simultaneous to implantation, the embryo continuous developing. the cell of
the embryoblast differentiates into two types of cells: the epiblast (closest to thetrophoblasts) and the hypoblast (closest to the blastocyst cavity). These two layers
of cells form a flat disc known as bilaminar embryonic disc through a process of
gastrulation (three layers). The first appearance of these layers collectively are
known as the primitive streak, around day 15.
ECTODERM: this is the start of tissue that covers most surfaces of the body. the
epidermis layer of the skin, hair and nails and the nervous system
MESODERM: The mesoderm forms the muscle, skeleton, dermis of the skin,
connective tissue, the urogenital glands, blood vessels, blood and lymph cells.
ENDODERM: They form the epithelial lining of the digestive, respiratory, urinarysystems and glandular cells of organs such as the liver and pancreas.
Figure 1. 11: Extravillous trophoblasts are found outside the villus and can be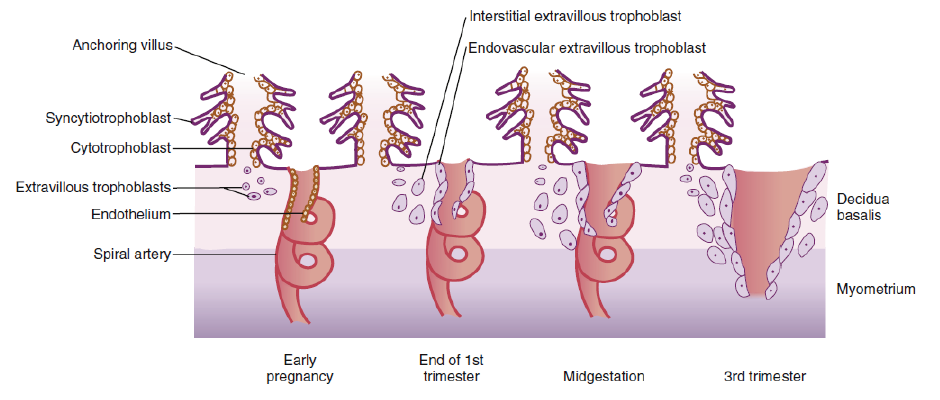
subdivided into endovascular and interstitial categories. Endovascular trophoblasts
invade and transform spiral arteries during pregnancy to create low-resistance
blood flow that is characteristic of the placenta. Interstitial trophoblasts invade thedecidua and surround spiral arteries.
Factors that may affect fertilization and implantation
Other factors include: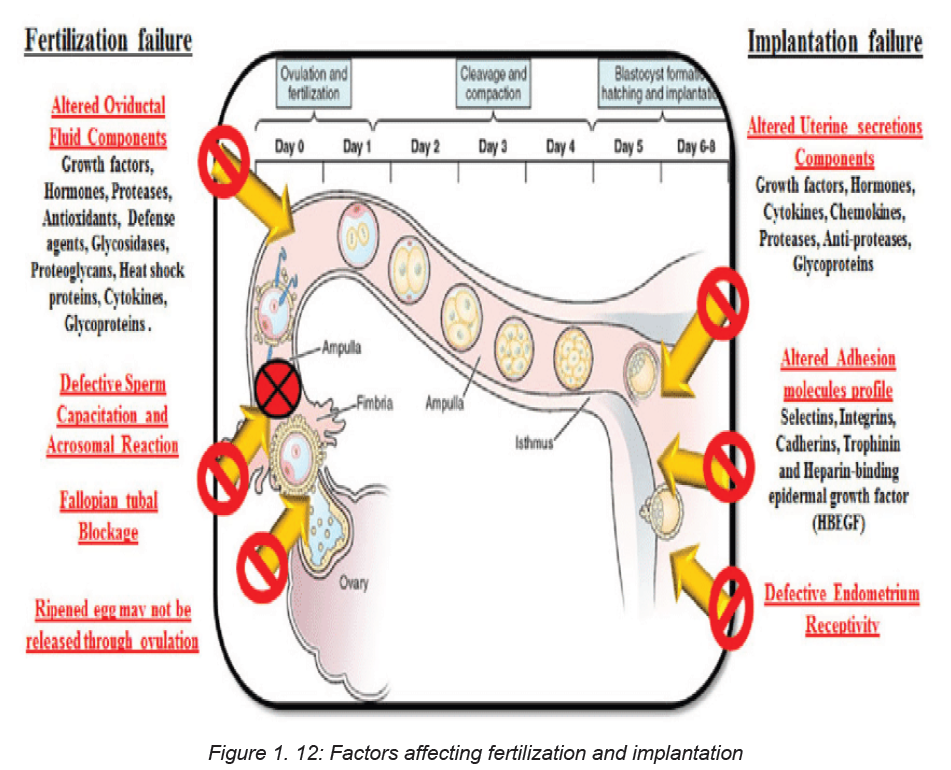
Age
Female age is the most important factor affecting fertility. Women are born with all
the eggs they will ever have and the number of eggs available decreases each day
from birth onwards. In young women the decline is fairly gradual (only a few eggs
are ‘lost’ each day), but as women approach their mid to late 30s, the decrease gets
much steeper (many more eggs are ‘lost’ each day). In addition to this decrease
in the number of eggs available, the quality of the eggs also declines as women
get older. This reduction in both the quantity and quality of available eggs means
that older women are less likely to get pregnant and, if they do get pregnant, they
are more likely to have a miscarriage. Male fertility may also decrease with age
although to a much lesser degree.
Previous Pregnancy
Couples are more likely to get pregnant if they have previously achieved a pregnancy
together (irrespective of whether or not that pregnancy resulted in the birth of a
baby) compared to couples that have never been pregnant.
Duration of subfertility
The longer couples have been trying to get pregnant, the less likely they are to be
successful. If a couple have been trying to get pregnant for less than 3 years they
are almost twice as likely to get pregnant than couples who have been trying for
more than 3 years.
Timing and Frequency of Sexual Intercourse
Most women have a 28-day menstrual cycle: this means there are 28 days between
the start of one period and the start of the next period. Ovulation (when an egg
is released from the ovary) occurs on day 14 of a 28-day cycle. Whether or not
that egg gets fertilised by a sperm depends on the day(s) in the cycle in which
intercourse occurs. The chance of getting pregnant is low at the beginning of the
cycle and starts to increase from about day 8 onwards. Women are most likely to
get pregnant if they have sex 2 days before they ovulate (i.e. on day 12 of 28-day
cycle).
Once ovulation has occurred, the chance of getting pregnant decreases dramatically:
sperm need to be present in the female genital tract prior to ovulation to maximise
the chances of getting pregnant. The reason for this is that once ovulation has
occurred, levels of the hormone progesterone increase and this causes cervical
mucus to become thick and sticky which prevents sperm from being able to swim
through it to get to the egg to fertilise.
Couples that have regular sex a week are most likely to get pregnant because this
frequency ensures that a good volume of fresh sperm will be present in the female
reproductive tract at the time of ovulation. If couples are only having sex once a
week, the chance of getting pregnant is less because there will be less fresh sperm
present in the female genital tract at the time of ovulation.
Lifestyle Factors
Weight
Overweight women who have irregular periods are less likely to release an egg
each month (ovulate) than women with regular periods. This means the chances
of getting pregnant are reduced. Losing weight, even as little as 5-10% of the total
body weight, may restore a regular menstrual cycle thereby increasing the chance
of getting pregnant.
Women who are overweight take longer to get pregnant than women who are
not, even if their periods are regular. Being overweight is also associated with
an increased risk of miscarriage and of problems during pregnancy and delivery.
Losing weight has been shown to improve fertility and increase the chance of
getting pregnant. No one diet has been shown to be better than any other but
group exercise programmes that involve both exercise and dietary advice leads to
more pregnancies than weight loss advice alone.
Men who are overweight may have suboptimal sperm and therefore reduced fertility.
Being underweight can also affect female fertility as it may mean that an egg is not
released each month. Being underweight is also associated with problems during
pregnancy. Gaining weight is likely to improve fertility.
Smoking
Women who smoke are 3 times more likely to experience a delay in getting pregnant
than non-smokers. Even passive smoking can be harmful. Smoking reduces
a woman’s ovarian reserve (so her ovaries will have fewer eggs in them than a
woman of the same age who does not smoke) and damages the cilia inside the
fallopian tube (which are important for transporting the egg and/or embryo along
the fallopian tube into the uterus). In men, smoking may reduce sperm quantity
and quality.
Caffeine
There is no clear association between caffeine consumption and infertility
Alcohol
Some studies report that drinking more than 5 units of alcohol a week may reduce
female fertility but others state that low to moderate alcohol consumption may
be associated with higher pregnancy rates than non-drinkers. Once pregnant,
excessive alcohol consumption may lead to birth defects and developmental delay.
The Royal College of Obstetricians and Gynaecologists and the Department of
Health recommend that women trying to get pregnant should avoid alcohol because
there is no ‘safe’ limit.
In men, excessive alcohol may lead to difficulties maintaining an erection, impaired
ejaculation and reduced sperm quality.
Over-the-counter and recreational drugs
Non-steroidal anti-inflammatory drugs such as ibuprofen can interfere with ovulation.
Aspirin may interfere with implantation. Recreational drugs such as marijuana
and cocaine may interfere with ovulation and/or the function of the fallopian tube.
The fallopian tube is important for transporting the egg from the ovary where it is
released, to the womb (uterus) where an embryo will hopefully implant. Fertilisation
occurs in the fallopian tube. Anabolic steroids, which are abused by some bodybuilders,
inhibit the production of sperm and this may be permanent even if the drug
is stopped.
Medical Conditions
Some women may have medical conditions that can affect their fertility. These
may or may not be known about when starting to try for a family. Some of these
conditions may be more general, for example thyroid disease and vitamin D
deficiency whilst others may be more specific, for example, polycystic ovarysyndrome and endometriosis.
Self-assessment 1.3
1. Where precisely does the fertilization normally take place?2. List the sequence of development of a fertilized egg from zygote to embryo.
1.4. ImplantationLearning Activity 1.4
Based on your knowledge and understanding of biology what is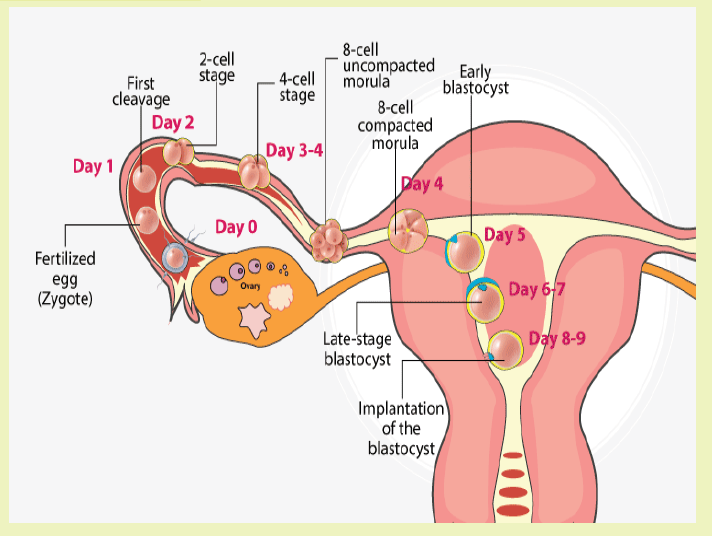
implantation?
At the end of the first week, the blastocyst comes in contact with the uterine wall and
adheres to it, embedding itself in the uterine lining via the trophoblast cells. Thus
begins the process of implantation, which signals the end of the pre-embryonic
stage of development. Implantation can be accompanied by minor bleeding.
The blastocyst typically implants in the fundus of the uterus or on the posterior
wall. However, if the endometrium is not fully developed and ready to receive the
blastocyst, the blastocyst will detach and find a better spot. A significant percentage
(50–75 percent) of blastocysts fail to implant; when this occurs, the blastocyst is
shed with the endometrium during menses. The high rate of implantation failure is
one reason why pregnancy typically requires several ovulation cycles to achieve.
When implantation succeeds and the blastocyst adheres to the endometrium,
the superficial cells of the trophoblast fuse with each other, forming the
syncytiotrophoblast, a multinucleated body that digests endometrial cells to firmly
secure the blastocyst to the uterine wall. In response, the uterine mucosa rebuilds
itself and envelops the blastocyst. The trophoblast secretes human chorionic
gonadotropin (hCG), a hormone that directs the corpus luteum to survive, enlarge,
and continue producing progesterone and estrogen to suppress menses. These
functions of hCG are necessary for creating an environment suitable for the
developing embryo. As a result of this increased production, hCG accumulates in
the maternal bloodstream and is excreted in the urine. Implantation is complete by
the middle of the second week. Just a few days after implantation, the trophoblast
has secreted enough hCG for an at-home urine pregnancy test to give a positiveresult.
Most of the time an embryo implants within the body of the uterus in a location that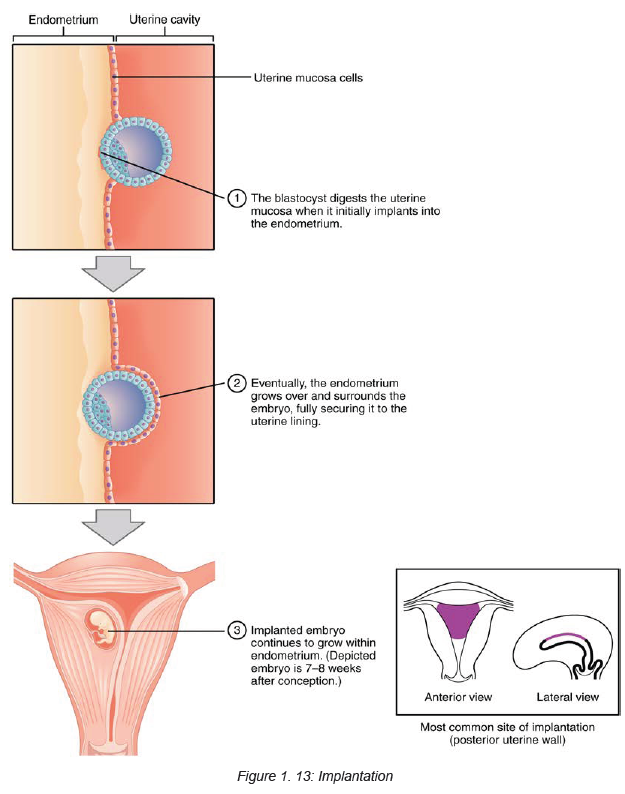
can support growth and development. However, in one to two percent of cases, the
embryo implants either outside the uterus (an ectopic pregnancy) or in a region of
uterus that can create complications for the pregnancy. If the embryo implants in
the inferior portion of the uterus, the placenta can potentially grow over the openingof the cervix, a condition call placenta previa.
Self-assessment 1.4
1. How do you know that an embryo has been successfully implanted?2. Differentiate implantation bleeding and normal menstrual bleeding.
1.5 Embryological and fetal development.Learning Activity 1.5
1. From the knowledge and understanding gained in biology Describe the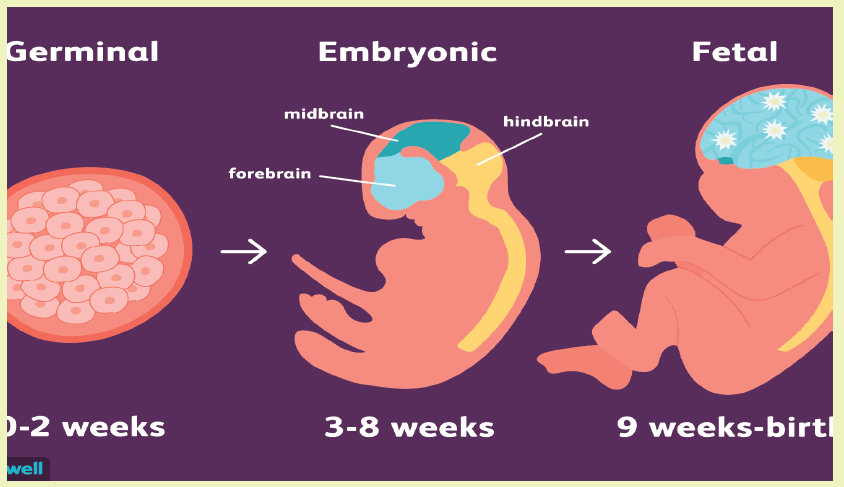
embryological stages of development.2. What is amniotic fluid? Discuss its functions in pregnancy.
Embryological and fetal periods of development.
a. Development of the embryo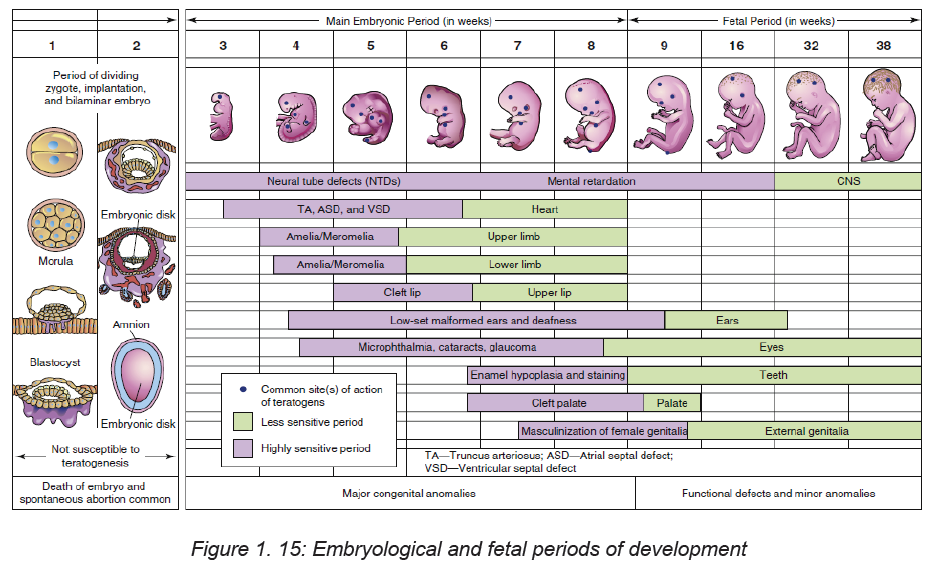
The stage of the embryo lasts from day 15 until approximately 8 weeks after
conception, when the embryo measures 3 cm from crown to rump. This
embryonic stage is the most critical time in the development of the organ
systems and the main external features. Developing areas with rapid cell
division are the most vulnerable to malformation caused by environmental
teratogens (substances or exposure that causes abnormal development).
At the end of the eighth week, all organ systems and external structures are
present, and the embryo is unmistakably human.
b. Membranes
At the time of implantation, two fetal membranes that will surround the
developing embryo begin to form. The chorion develops from the trophoblast
and contains the chorionic villi on its surface. The villi burrow into the decidua
basalis and increase in size and complexity as the vascular processes
develop into the placenta. The chorion becomes the covering of the fetal side
of the placenta.
The inner cell membrane, the amnion, develops from the interior cells of the
blastocyst. The cavity that develops between this inner cell mass and theouter layer of cells (trophoblast) is the amniotic cavity.
c. Amniotic fluid
Amniotic fluid is present at the formation of the amniotic sac. This is a thin-walled
sac that contains the fetus during pregnancy. Amniotic fluid is a clear alkaline
and slightly yellowish liquid contained within the amniotic sac.it is derived
from maternal circulation across placental membranes and exuded from the
fetal surface. The fetus contributes to the amniotic fluid through metabolism
in small quantities of urine and fluids from its lung. Amniotic fluid is made
up of 98% water and electrolytes, along with peptides, carbohydrates, and
signaling molecules. The remaining 2% is made up of lipids and hormones.
Function
Amniotic fluid serves a number of purposes during pregnancy, primarily to protect
the fetus from harm. The functions of the amniotic fluid include:
• Acting as a cushion: This protects the fetus from injury should the mother’s
abdomen be the subject of trauma or a sudden impact.
• Protecting the umbilical cord: Amniotic fluid flows between the umbilical
cord and fetus.
• Protecting from infection: Amniotic fluid has antibacterial properties.
• Containing essential nutrients: These include proteins, electrolytes,
immunoglobulins, and vitamins that assist in the development of the fetus.
• Allowing for the fetus to move: Amniotic fluid also allows the developing
fetus to move around in the womb, which in turn allows for proper development
and growth of the musculoskeletal system, gastrointestinal system, and
pulmonary system.
• Maintaining temperature: Amniotic fluid assists in keeping a constant steady
temperature around the fetus throughout pregnancy, protecting the baby from
heat loss.
d. Umbilical cord
By day 14 after conception, the embryonic disk, the amniotic sac, and the
yolk sac are attached to the chorionic villi by the connecting stalk. During the third
week the blood vessels develop to supply the embryo with maternal nutrients and
oxygen. During the fifth week the embryo has curved inward on itself from both
ends, bringing the connecting stalk to the ventral side of the embryo. The connecting
stalk becomes compressed from both sides by the amnion and forms the narrower
umbilical cord.
Two arteries carry blood from the embryo to the chorionic villi, and one veinreturns blood to the embryo.
e. York sac
When the amniotic cavity and amnion are forming, another blastocyst cavity forms
on the other side of the developing embryonic disk. This cavity becomes surrounded
by a membrane, forming the yolk sac. The yolk sac aids in transferring maternal
nutrients and oxygen, which have diffused through the chorion, to the embryo.
Summary of embryological and fetal development
Embryo
0–4 weeks
• Blastocyst implants
• Primitive streak appears
• Conversion of bilaminar disc into trilaminar disc
• Some body systems laid down in primitive form
• Primitive central nervous system forms (neurulation)
• Primitive heart develops and begins to beat
• Covered with a layer of skin
• Limb buds form
• Optic vessels develop
• Gender determined
4–8 weeks
• Very rapid cell division
• More body systems laid down in primitive form and continue to develop
• Spinal nerves begin to develop
• Blood is pumped around the vessels
• Lower respiratory system begins to develop
• Kidneys begin to develop
• Skeletal ossification begins developing
• Head and facial features develop
• Early movements
• Embryo visible on ultrasound from 6 weeks
Fetus
8–12 weeks
• Rapid weight gain
• Eyelids meet and fuse
• Urine passed
• Swallowing begins
• Distinguishing features of external genitalia appear
• Fingernails develop
• Some primitive reflexes present 12–16 weeks
• Rapid skeletal development – visible on X-ray
• Lanugo appears
• Meconium present in gut
• Nasal septum and palate fuse
• Eternal genitalia fully differentiate into male or female by week 12
• Fetus capable of sucking thumb
16–20 weeks
• Constant weight gain
• ‘Quickening’ – mother feels fetal movements
• Fetal heart heard on auscultation
• Vernix caseosa appears
• Skin cells begin to be renewed
• Brown adipose tissue (BAT) forms
20–24 weeks
• Most organs functioning well
• Eyes complete
• Periods of sleep and activity
• Ear apparatus developing
• Responds to sound
• Skin red and wrinkled
• Surfactant secreted in the lungs from week 20
24–28 weeks
• Legally viable and survival may be expected if born
• Eyelids open
• Respiratory movements
28–32 weeks
• Begins to store fat and iron
• Testes descend into scrotum
• Lanugo disappears from face
• Skin becomes paler and less wrinkled 32–36 weeks
• Weight gain 25 g/day
• Increased fat makes the body more rounded
• Lanugo disappears from body
• Hair on fetal head lengthens
• Nails reach tips of fingers and toes
• Ear cartilage soft
• Plantar creases visible.
36 weeks to birth
• Birth is expected
• Body round and plump
• Skull formed but soft and pliable
Self-assessment 1.5
a. Describe the Amnion and chorion and their specific characteristics.b. How many arteries and vein does the umbilical cord contain.
1.6 Development of Placenta and functionsLearning Activity 1.6
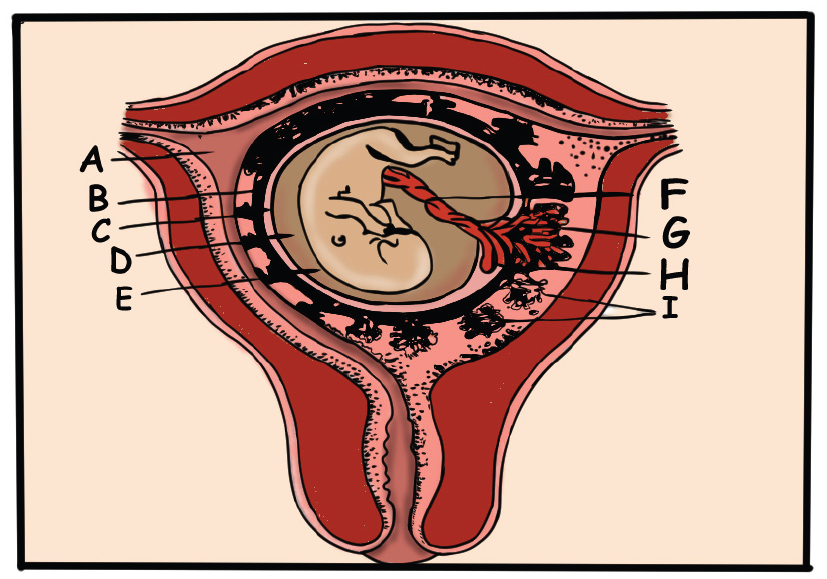
On the above diagram, show the structure of foetal membranes and the placenta
Development of placenta:
The human placenta develops from the trophectoderm (TE), the outer layer of the
pre-implantation embryo, which forms at 5 days’ post fertilization. At this stage, the
pre-implantation embryo (termed a blastocyst) is segregated into two lineages: theinner cell mass (ICM) and the trophectoderm.
Structure
The placenta begins to form at implantation. During the third week after conception
the trophoblast cells of the chorionic villi continue to invade the decidua basalis. As
the uterine capillaries are tapped, the endometrial spiral arteries fill with maternal
blood.
The placenta functions as a means of metabolic exchange. Exchange is minimal
at this time because the two cell layers of the villous membrane are too thick.
Permeability increases as the cytotrophoblast thins and disappears; by the fifth
month, only the single layer of syncytium is left between the maternal blood and thefetal capillaries.
Placenta at term
At term the placenta is discoid in shape, about 20 cm in diameter and 2.5 cm thick
at its centre and weighing approximately 470 g, which is directly proportional to the
weight of the fetus. The weight of the placenta may be affected by physiological
or active management of the third stage of labour owing to the varying amounts of
fetal blood retained in the vessels. The placenta is no longer routinely weighed in
clinical practice; however, some maternity units may do so as part of clinical trialsand research activities.
The maternal surface of the placenta (i.e. the basal plate) is dark red in colour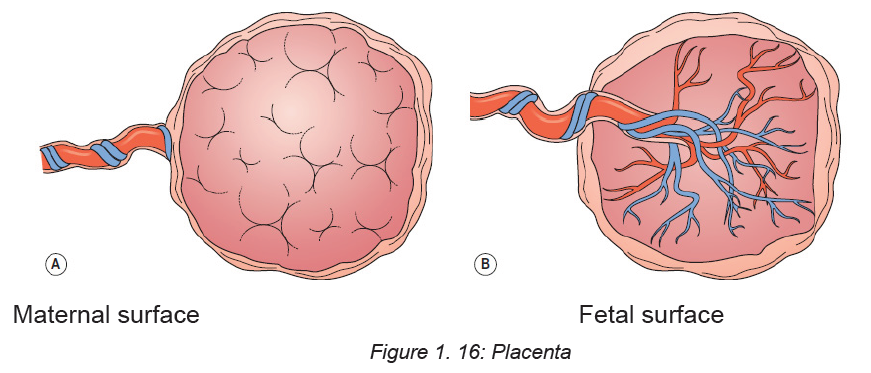
due to maternal blood and partial separation of the basal decidua. The surface is
arranged in up to 40 cotyledons (lobes), which are separated by sulci (furrows),
into which the decidua dips down to form septa (walls). The cotyledons are made
up of lobules, each of which contains a single villus with its branches. Sometimes
deposits of lime salts may be present on the surface, making it slightly gritty. This
has no clinical Significance.
The fetal surface of the placenta (i.e. the chorionic plate) has a shiny appearance
due to the amnion covering it.
Branches of the umbilical vein and arteries are visible, spreading out from the
insertion of the umbilical cord, which is normally in the centre. The amnion can be
peeled off the surface of the chorion as far back as the umbilical cord, whereas the
chorion, being derived from the same trophoblastic layer as the placenta, cannot
be separated from it.
Functions
The placenta performs a variety of functions for the developing fetus which can bedetermined by the mneumonic SERPENT
Storage
The placenta metabolizes glucose, stores it in the form of glycogen and reconverts
it to glucose as required. It can also store iron and the fat-soluble vitamins.
Endocrine
The many and varied endocrine functions of the placenta are complex, requiring
maternal and fetal input. Both types of trophoblasts produce steroidal hormones
(oestrogens and progesterone) in addition to many placental protein hormones
necessary for pregnancy.
Steroid hormones
There are three important oestrogens: oestrone, oestradiol and oestriol. Both
maternal and fetal adrenal production provide precursors for oestrogen production
by the placenta.
Protein hormones
Human chorionic gonadotrophin (hCG) is produced under the influence of placental
gonadotrophic releasing hormone (GnRH) by the trophoblasts.
Respiration
Gaseous exchange to and from the fetus occurs as a result of diffusion. Transfer
of gases is assisted by a slight maternal respiratory alkalosis in pregnancy. The
fetal hemoglobin level is high in utero to facilitate transport of gases. The fetal
hemoglobin also has a high affinity for oxygen.
Protection
The placenta provides a limited barrier to infection. Few bacteria can penetrate with
the exception of the treponema of syphilis and the tubercle bacillus. However, many
types of virus can penetrate the placental barrier, such as human immunodeficiency
virus (HIV), hepatitis strains, human cytomegalovirus (CMV) and rubella. In addition
to this, some parasitic and protozoal diseases, such as malaria and toxoplasmosis,
will cross the placenta.
The placenta filters substances of a high molecular weight therefore some drugs
and medicines may transfer to the fetus.
Immunoglobulins will be passed from mother to fetus transplacentally in late
pregnancy, providing about 6–12 weeks’ naturally acquired passive immunity to the
baby. In the case of Rhesus disease, if sensitization occurs and fetal blood cells
enter the maternal circulation, responding antibodies produced by the mother may
cross the placenta and destroy fetal surface antigens and consequently fetal cells,
causing haemolysis, hydrops fetalis and potential fetal demise.
Excretion
The main substance excreted from the fetus is carbon dioxide. Bilirubin will also
be excreted as red blood cells are replaced relatively frequently. There is very little
tissue breakdown apart from this and the amounts of urea and uric acid excreted
are very small.
Nutrition
The fetus requires nutrients for its ongoing development, such as amino acids and
glucose which are required for growth and energy, calcium and phosphorus for
bones and teeth, and iron and other minerals for blood formation. These nutrients
are actively transferred from the maternal to the fetal blood through the walls of the
villi.
The placenta is able to select those substances required by the fetus, even depleting
the mother’s own supply in some instances. Water, vitamins and minerals also pass
to the fetus. Fats and fat-soluble vitamins (A, D and E) cross the placenta only with
difficulty and mainly in the later stages of pregnancy. Some substances, including
amino acids, are found at higher levels in the fetal blood than in the maternal blood.
Transfer of substances
Substances transfer to and from the fetus by a variety of transport mechanisms, as
stated below:
♦ Simple diffusion of gases and lipid soluble substances.
♦ Water pores transfer water-soluble substances as a result of osmotic and
potentially hydrostatic forces.
♦ Facilitated diffusion of glucose using carrier proteins.
♦ Active transport against concentration gradients of ions, calcium (Ca) and
phosphorus (P).♦ Endocytosis (pinocytosis) of macromolecules
Self-assessment 1.6
1. A natural cleavage plane between the placenta and the uterine wall is formed
when the cotyledons of the maternal surface of the placenta extend into the:
a. Myometrium
b. Uterine wall
c. Decidua’s basalis
d. Amniotic membrane
2. Which of the following is the portion of the placenta that is contributed by the
embryo?
a. Chorion
b. Yolk sac
c. Amnion
d. Allantois
3. Which of the following blood vessels transports blood rich in oxygen and
nutrients to the fetus?
e. Ductus arteriosus
f. Ductus venosus
g. Umbilical vein
h. Umbilical artery4. What are the nutritive and protective functions of the placenta?
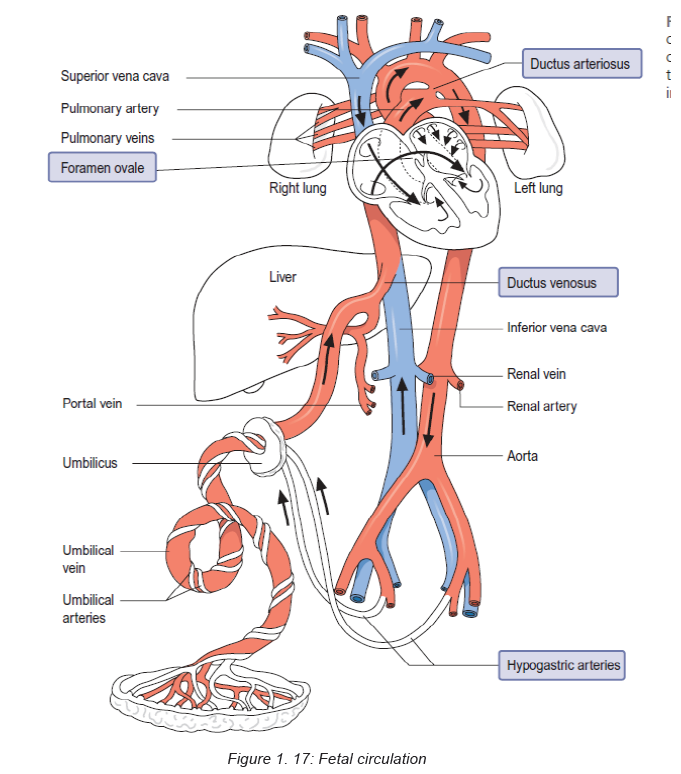
1.7 Fetal circulationLearning Activity 1.7
Blood circulation in fetuses is done to avail oxygen and nutrients for body use
and remove waste products. Based on the competences developed in senior 3,
please brainstorm on how fetal circulation is done.
The placenta is the source of oxygenation, nutrition and elimination of waste for the
fetus. There are several temporary structures in addition to the placenta and the
umbilical cord that enable the fetal circulation to occur. These include:
♦ The ductus venosus, which connects the umbilical vein to the inferior vena
cava.
♦ The foramen ovale, which is an opening between the right and left atria.
♦ The ductus arteriosus, which leads from the bifurcation of the pulmonary
artery to the descending aorta.
♦ The hypogastric arteries, which branch off from the internal iliac arteries and
become the umbilical arteries when they enter the umbilical cord. The fetal
circulation takes the following course:
Oxygenated blood from the placenta travels to the fetus in the umbilical vein. The
umbilical vein divides into two branches – one that supplies the portal vein in the
liver, the other anastomosing with the ductus venosus and joining the inferior vena
cava. Most of the oxygenated blood that enters the right atrium passes across the
foramen ovale to the left atrium, which mixes with a very small amount of blood
returning from the lungs from where it passes into the left ventricle via the bicuspid
valve, and then the aorta. The head and upper extremities receive approximately
50% of this blood via the coronary and carotid arteries, and the subclavian arteries
respectively. The rest of the blood travels down the descending aorta, mixing with
deoxygenated blood from the right ventricle via the ductus arteriosus.
Deoxygenated blood collected from the head and upper parts of the body returns to
the right atrium via the superior vena cava. Blood that has entered the right atrium
from the superior vena cava enters at a different angle to the blood that enters from
the inferior vena cava and heads towards the foramen ovale. Hence there are two
distinct blood flows entering the right atrium. Most of the lesser oxygenated blood
entering the right atrium from the superior vena cava passes behind the flow of
highly oxygenated blood going to the left atrium and enters the right ventricle via
the tricuspid valve. There is a small amount of blood mixing where the two blood
flows meet in the atrium. From the right ventricle a little blood travels to the lungs
in the pulmonary artery, for their development. Most blood, however, passes from
the pulmonary artery through the ductus arteriosus into the descending aorta. This
blood, although low in oxygen and nutrients, is sufficient to supply the lower body
of the fetus. It is also by this means that deoxygenated blood travels back to the
placenta via the internal iliac arteries, which lead into the hypogastric arteries, and
ultimately into the umbilical arteries. This circulation means that the fetus has a
well oxygenated and perfused head, brain and upper body compared to its lowerextremities.
Self-assessment activity 1.7
a. Differentiate ductus venosus from ductus arteriosusb. What are temporary structures formed during intra-uterine life?
1.8 Characteristics of a normal pregnancyLearning Activity 1.8
A 27 years old married lady is accompanied by her husband to the health center
to get medical care. She presents the signs and symptoms of nausea and
vomiting every morning in the last 4 days, pain in lower abdomen and nausea,
mood changes and selection of food. She also reported to have missed her
periods for the last two months. She states that she treated herself for malaria
last three months
Use the knowledge of S3 biology on the topic of pregnancy to recall the signs ofpregnancy in woman who is pregnant.
Pregnancy is a time of profound physical, physiological and psychological change.
In addition to the reproductive organs, all maternal physiologic systems make
adaptions needed to support the developing fetus and, at the same time, maintain
maternal homeostasis.
1.8.1 Physical and physiological characteristics of a normal
pregnancy
Some pregnant women experience a lot of physical changes and others
only a few.
♦ Aches and pain (possibly in your lower abdomen and in your joints)
♦ Morning sickness which may be nausea or actual vomiting, and does not just
happen in the morning
♦ Food cravings and aversions
♦ Heartburn and indigestion
♦ Constipation
♦ A need to urinate more often
♦ Skin change and itching and possibly skin tags.
♦ Larger and tender breasts.
1.8.2 Psychological characteristics of a normal pregnancy
Pregnancy is always associated with changes in the psychological functioning of
pregnant women. It is usually associated with ambivalence, frequent mood changes,
varying from anxiety, fatigue, exhaustion, sleepiness, depressive reactions to
excitement. During pregnancy, changes include body appearance, affectivity and
sexuality, whereas the position and role of women attains a new quality. Even
thoughts of pregnancy can bring about numerous worries about its course and
outcome, and especially of the delivery itself, which may be so intense that they
acquire a feature of phobia (which may be the reason for avoiding pregnancy).
Pregnancy as a stressful event: Pregnancy is identified as a potent stressor
that can seriously affect the psychic status of pregnant women, perinatal outcome,
but also psychic functioning of the new-born individual. Appropriate relationship
of partners and support of the society play an important role in overcoming stress
during pregnancy.
Conclusion: Pregnancy is an event that involves numerous somatic and
psychological changes. However, pregnancy can also be a potent stressor.
Existence of prenatal maternal stress may lead to different perinatal complications
that may have long-term consequences on the newborn. In prevention of maternal
stress emphasis has to be put on partner’s emotional support, as well as empathy of
the social environment. However, in certain cases, professional psychotherapeutic
support is necessary, in form of short supportive treatment. Preventive measures
should include adequate psychological support during pregnancy, especially the
first one, provided for all pregnant women, but also for those women that plan toget pregnant in the near future.
Self-assessment 1.8
Discuss the psychological characteristics of pregnancy
Learning Activity 1.9
A 16 years old boy who study science subjects including biology in S3 comes
home for holiday and realizes that his mother who is 30 weeks pregnant had an
accident which affected her pelvic bone thereby leading to unsteady gait when
walking as the pregnancy progresses. During interview with the mother states
that she feels more pain on her back as the pregnancy progress and difficulty
to stand straight. The child is concerned with the long-term effects that this gait
deviation will have on his mother’s vertebra column especially now that the
mother is pregnant.
a. Based on your knowledge and understanding of biology in S3
What is pelvis?
b. Which body part do you think might be an underlying cause of this gaitpattern?
Pregnancy and its changes is a normal physiological process that happens in all
mammalian in response to the development of the fetus. These changes happen in
response to many factors; hormonal changes, increase in the total blood volume,
weight gain, and increase in fetus size. All these factors have a physiological impact
on all systems of the pregnant woman; musculoskeletal, endocrine, reproductive
system, cardiovascular, respiratory, gastrointestinal system, and renal changes.1.9.1 Anatomy background of pelvis
♦ The pelvis is the region found between the trunk and lower limbs.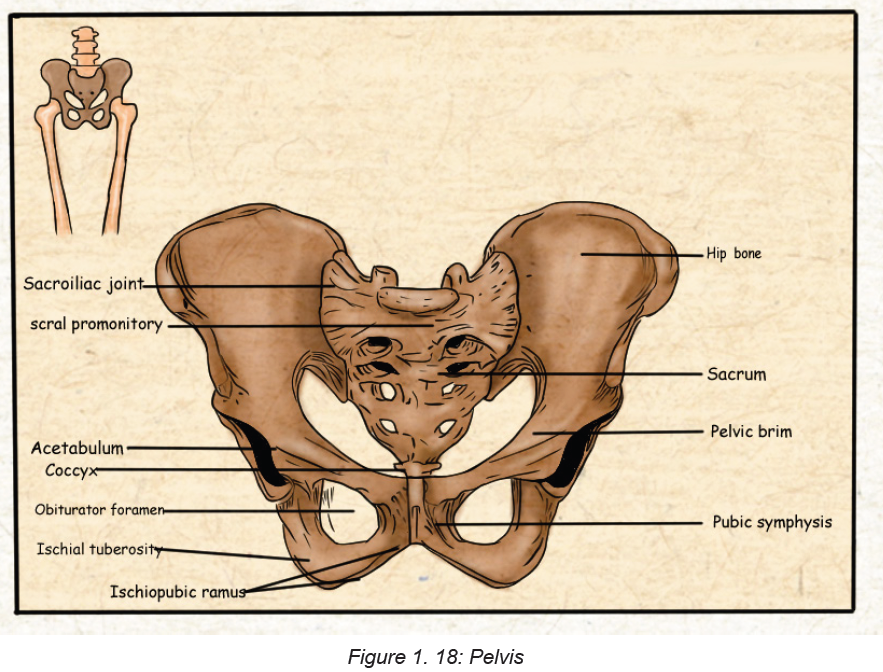
♦ In females, the pelvis is wider and lower than that of their male counterpart,
making it more suited to accommodate a fetus during both pregnancy and
delivery.
♦ It protects and supports the pelvic contents, provides muscle attachment and
facilitates the transfer of weight from trunk to legs in standing, and to the
ischial tuberosities in sitting.
♦ The cross-sectional anatomy of the female pelvis shows five bones: two hip
bones, sacrum, coccyx, and two femurs The joints are supported by some of
the strongest ligaments in the body which become laxer during pregnancy
leading to increased joint mobility and less efficient load transfer through the
pelvis.
♦ The pelvic outlet at the base of the pelvis is narrower in its transverse
diameter when compared with the pelvic inlet; it comprises the pubic arch,
ischial spines, sacrotuberous ligaments, and coccyx.
♦ Four pairs of abdominal muscles combine to form the anterior and lateral
abdominal wall and may be termed the abdominal corset.
♦ Transversus abdominis lies deep to the internal abdominal oblique and
external abdominal oblique with the rectus abdominis central, anterior and
superficial abdominal oblique, external oblique and transversus abdominis
insert into an aponeurosis joining in the midline at the linea alba. The deep
abdominal muscles, together with the pelvic floor muscles, multifidus, and
diaphragm, can be considered as a complete unit and may be termed the
lumbopelvic cylinder. This provides support for the abdominal contents and
maintains intraabdominal
pressure.
♦ Organs of the female reproductive system present in the pelvis are subdivided
into internal and external genitalia.
1.9.2 Types of pelvis
The pelvis is a group of bones located in the lower part of torso, between the lower
back and thighs. The shape of the pelvis often differs between males and females.
There are four main types of pelvis:
a. Gynecoid. This is the most common type of pelvis in females and is generally
considered to be the typical female pelvis. Its overall shape is round, shallow,
and open.
b. Android. This type of pelvis bears more resemblance to the male pelvis. It’s
narrower than the gynecoid pelvis and is shaped more like a heart or a wedge.
c. Anthropoid. An anthropoid pelvis is narrow and deep. Its shape is similar to
an upright egg or oval.
d. Platypelloid. The platypelloid pelvis is also called a flat pelvis. This is the least
common type. It’s wide but shallow, and it resembles an egg or oval lying onits side.
Table 1. 1: Types of pelvis
Pelvis shape can vary greatly among females around the world.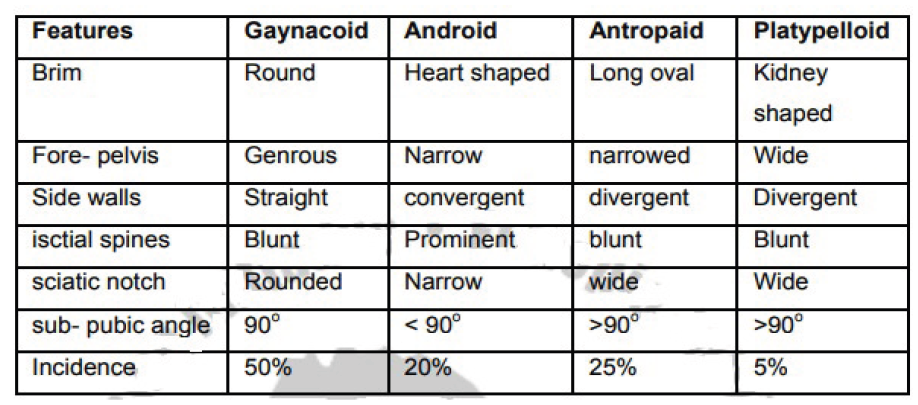
1.9.3 Pelvis in relation to pregnancy and child birth
The term pelvis is applied to the skeletal ring formed by the innominate bones and
the sacrum, the cavity within and even the entire region where the trunk and the
lower limb meet. The pelvis is divided by an oblique plane which passes through
the prominence of the sacrum, the arcuate line (the smooth rounded border on the
internal surface of the ilium), the pectineal line (a ridge on the superior ramus of
the pubic bone) and the upper margin of the symphysis pubis, into the true and the
false pelvis.
a. THE TRUE PELVIS: The true pelvis is the bony canal through which the fetus
must pass during birth. It is divided into a brim, a cavity and an outlet.
i. The pelvic brim:
The superior circumference forms the brim of the true pelvis; the included
space being called the inlet. The brim is round except where the sacralpromontory projects into it.
There are fixed points on the pelvic brim that are known as its landmarks.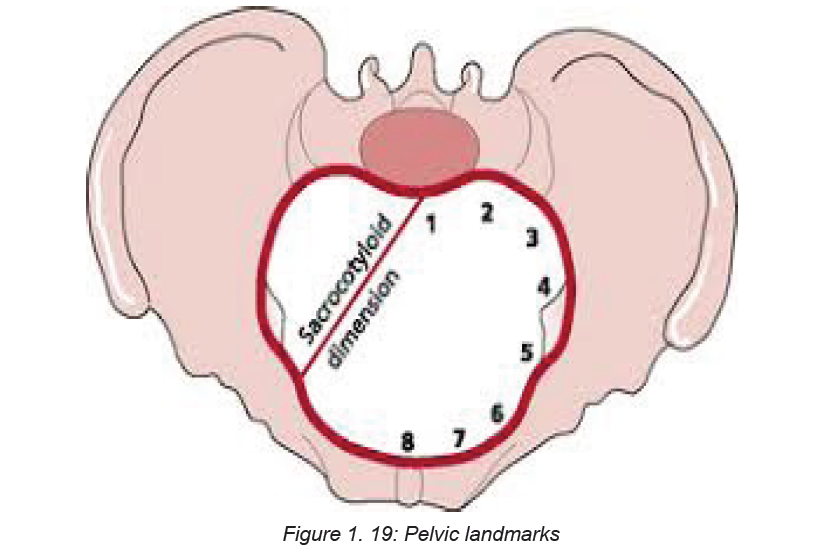
Commencing posteriorly, there are:
♦ Sacral promontory (1)
♦ Sacral ala or wing (2)
♦ Sacroiliac joint (3)
♦ Iliopectineal line, which is the edge formed at the inward aspect of the ilium(4)
♦ Iliopectineal eminence, which is a roughened area formed where the superior
ramus of the pubic bone meets the ilium (5).
♦ Superior ramus of the pubic bone (6)
♦ Upper inner border of the body of the pubic bone (7)
♦ Upper inner border of the symphysis pubis (8)
ii. The pelvic cavity:
The cavity of the true pelvis extends from the brim superiorly to the outlet inferiorly.
The anterior wall is formed by the pubic bones and symphysis pubis and its depth
is 4 cm. The posterior wall is formed by the curve of the sacrum which is 12 cm in
length. Because there is such a difference in these measurement, the cavity forms
a curved canal.
The cavity contains the pelvic colon, rectum, bladder and some of the reproductive
organs. The rectum is placed posteriorly, in the curve of the sacrum and coccyx, the
bladder is anterior behind the symphysis pubis.
iii. The pelvic outlet:
The lower circumference of the true pelvis is very irregular, the space enclosed by
it is called the outlet. Two outlets are described: the anatomical and the obstetrical.
The anatomical outlet is formed by the lower borders of each of the bones together
with the sacrotuberous ligament. The obstetrical outlet is of greater practical
significance because it includes the narrow pelvic strait through which the fetus
must pass. The obstetrical outlet is the space between the narrow pelvic strait and
the anatomical outlet. This outlet is diamond-shaped.
b.THE FALSE PELVIS: It is bounded posteriorly by the lumbar vertebrae and
laterally by the iliac fossae, and in front by the lower portion of the anterior abdominal
wall. The false pelvis varies considerably in size according to the flare of the iliacbones. However, the false pelvis has no significance in midwifery.
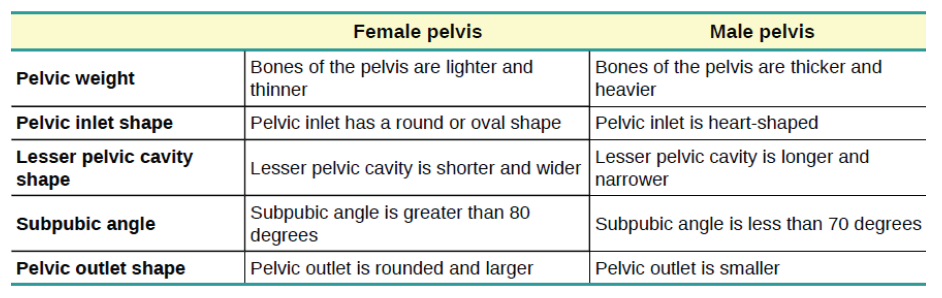
Table 1. 2: Differences between the Female and Male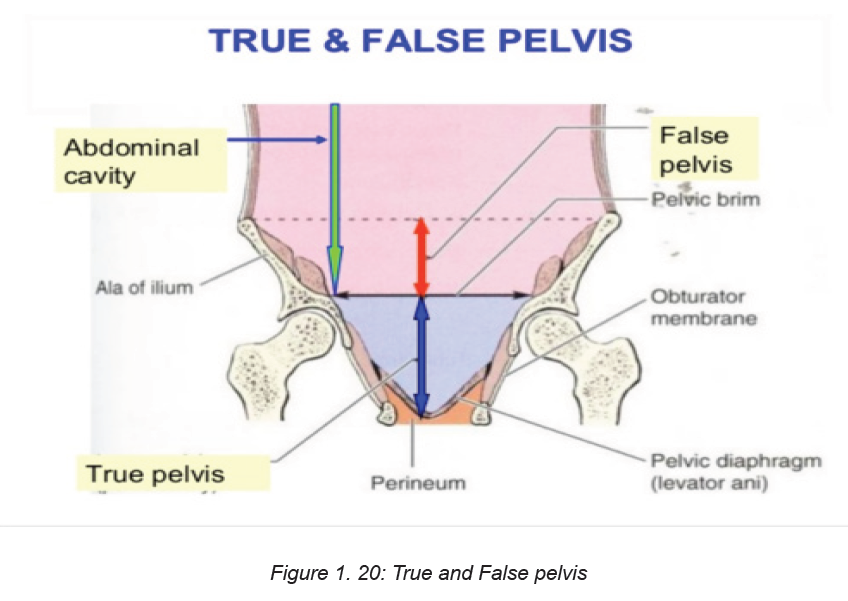
Pelvis
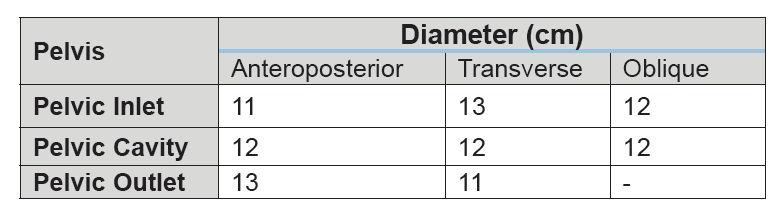
1.9.4 Pelvic diameters
Knowledge of the diameters of the normal female pelvis is essential in the practice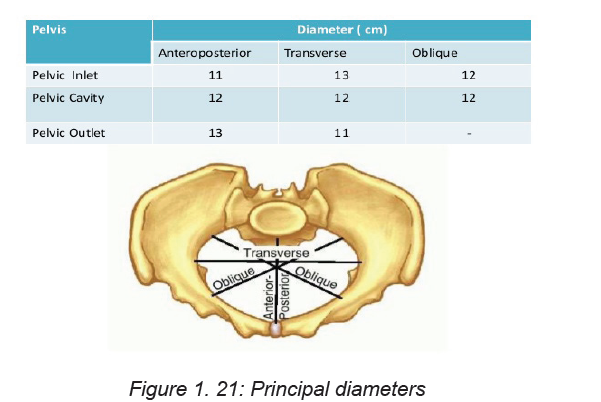
of midwifery because contraction of any of them can result in malposition or
malpresentation of the presenting part of the fetus.
Diameters of the pelvic inlet
The brim has four principal diameters: the anteroposterior diameter, the
transverse diameter and the two oblique diameters. The anteroposterior or
conjugate diameter extends from the midpoint of the sacral promontory to the upper
border of the symphysis pubis. Three conjugate diameters can be measured: the
anatomical (true) conjugate, the obstetrical conjugate and the internal or diagonal
conjugate The anatomical conjugate, which averages 12 cm, is measured from the
sacral promontory to the uppermost point of the symphysis pubis. The obstetrical
conjugate which averages 11 cm, is measured from the sacral promontory to the
posterior border of the upper surface of the symphysis pubis. This represents the
shortest anteroposterior diameter through which the fetus must pass and is hence
of clinical significance to midwives. The obstetrical conjugate cannot be measured
with the examining fingers or any other technique.
The diagonal conjugate is measured anteroposteriorly from the lower border of the
symphysis to the sacral promontory.
The transverse diameter is constructed at right-angles to the obstetric conjugate
and extends across the greatest width of the brim; its average measurement is
about 13 cm. Each oblique diameter extends from the iliopectineal eminence of one
side to the sacroiliac articulation of the opposite side; its average measurement is
about 12 cm.
Each takes its name from the sacroiliac joint from which it arises, so the left oblique
diameter arises from the left sacroiliac joint and the right oblique from the right
sacroiliac
joint. Another dimension, the sacrocotyloid, passes from the sacral promontory to
the iliopectineal eminence on each side and measures 9–9.5 cm. Its importance is
concerned with posterior positions of the occiput when the parietal eminences of
the fetal head may become caught.
Diameters of the cavity
The cavity is circular in shape and although it is not possible to measure its diameters
exactly, they are all considered to be 12 cm.
Diameters of the outlet
The outlet, which is diamond-shaped, has three diameters: the anteroposterior
diameter, the oblique diameter and the transverse diameter. The anteroposterior
diameter extends from the lower border of the symphysis pubis to the sacrococcygeal
joint. It measures 13 cm; as the coccyx may be deflected backwards during labour,
this diameter indicates the space available during birth. The oblique diameter,
although there are no fixed points, is said to be between the obturator foramen
and the sacrospinous ligament. The measurement is taken as being 12 cm. The
transverse diameter extends between the two ischial spines and measures 10–11
cm. It is the narrowest diameter in the pelvis. The plane of least pelvic dimensions
is said to be at the level of the ischial spines.
Orientation of the pelvis
In the standing position, the pelvis is placed such that the anterior superior iliac
spine and the front edge of the symphysis pubis are in the same vertical plane,
perpendicular to the floor. If the line joining the sacral promontory and the top of
the symphysis pubis were to be extended, it would form an angle of 60° with the
horizontal floor. Similarly, if a line joining the centre of the sacrum and the Centre of
the symphysis pubis were to be extended, the resultant angle with the floor would
be 30°. The angle of inclination of the outlet is 15°. When in the recumbent position,
the same angles are made as in the vertical position; this fact should be kept in
mind when carrying out an abdominal examination.
Pelvic planes
Pelvic planes are imaginary flat surfaces at the brim, cavity and outlet of the pelvic
canal at the levels of the lines described above.
Axis of the pelvic canal
A line drawn exactly half-way between the anterior wall and the posterior wall of the
pelvic canal would trace a curve known as the curve of Carus. The midwife needs
to become familiar with this concept in order to make accurate observations on
vaginal examination and to facilitate the birth of the baby.Table 1. 3: Summary of pelvic diameters
Self-assessment activity 1.9
1. What is the narrowest diameter for the fetus to pass through?
2. Which of the following statements is false? In each case, say why it is
incorrect.
a. The female bony pelvis is broader and flatter than the male pelvis.
b. The pelvic inlet is narrower than the pelvic outlet.
c. The iliac crest is an important landmark in measuring the progress of the
fetus down the birth canal.
d. The sutures in the fetal skull are strong hard joints that hold the skull bones
rigidly in place.e. A newborn baby’s pulse can be seen beating in the anterior fontanel.
Match the terms with the appropriate explanation
1.10 The fetal skull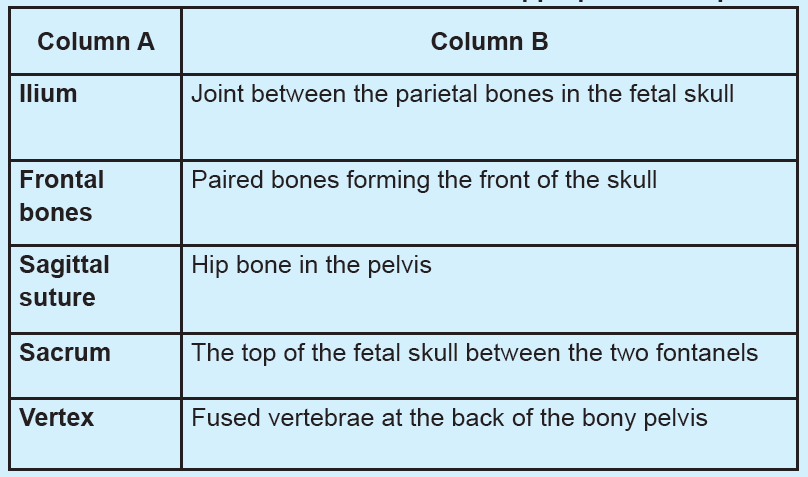
Learning Activity 1.10
Study the following structure of the fetal skull, a bony structure that protects thebrain:
1. Describe the above structure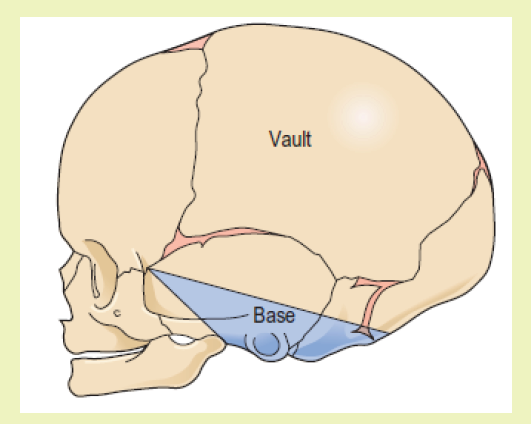
2. Predict how the fetal skull protects the brain in fetuses.
The fetal head is large in relation to the fetal body compared with the adult.
Additionally, it is large in comparison with the maternal pelvis and is the largest part
of the fetal body to be born. Adaptation between the skull and the pelvis is necessary
to allow the head to pass through the pelvis during labour without complications.
The bones of the vault are thin and pliable, and if subjected to great pressure
damage to the underlying delicate brain may occur.
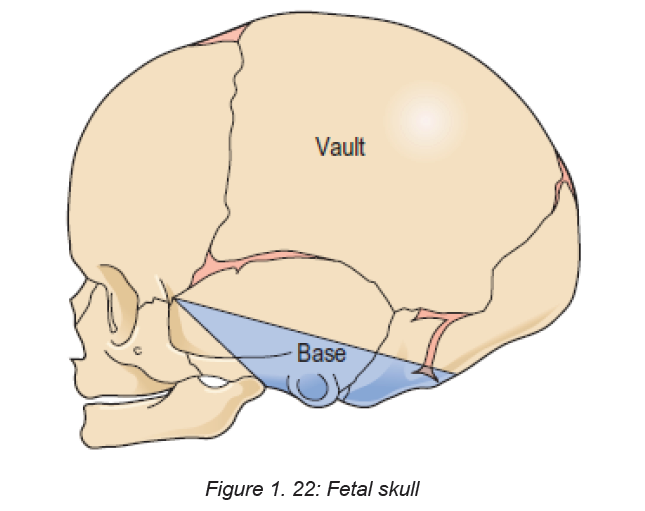
1.10.1 Divisions of the fetal skull
The skull is divided into the vault, the base and the face. The vault is the large,
dome-shaped part above an imaginary line drawn between the orbital ridges and
the nape of the neck. The base comprises bones that are firmly united to protect
the vital centres in the medulla oblongata. The face is composed of 14 small bonesthat are also firmly united and non-compressible.
1.10.2 Bones of the vault
The bones of the vault are laid down in membrane. They harden from the centre
outwards in a process known as ossification. Ossification is incomplete at birth,
leaving small gaps between the bones, known as the sutures and fontanelles. The
ossification centre on each bone appears as a protuberance. Ossification of the
skull is not complete until early adulthood. The bones of the vault consist of:
The occipital bone, which lies at the back of the head. Part of it contributes to the
base of the skull as it contains the foramen magnum, which protects the spinal cord
as it leaves the skull. The ossification centre is the occipital protuberance.
♦ The two parietal bones, which lie on either side of the skull. The ossification
centre of each of these bones is called the parietal eminence.
♦ The two frontal bones, which form the forehead or sinciput. The ossification
centre of each bone is the frontal eminence. The frontal bones fuse into a
single bone by eight years of age.
♦ The upper part of the temporal bone on both sides of the head forms part ofthe vault.
1.10.3 Regions of landmarks’ diameters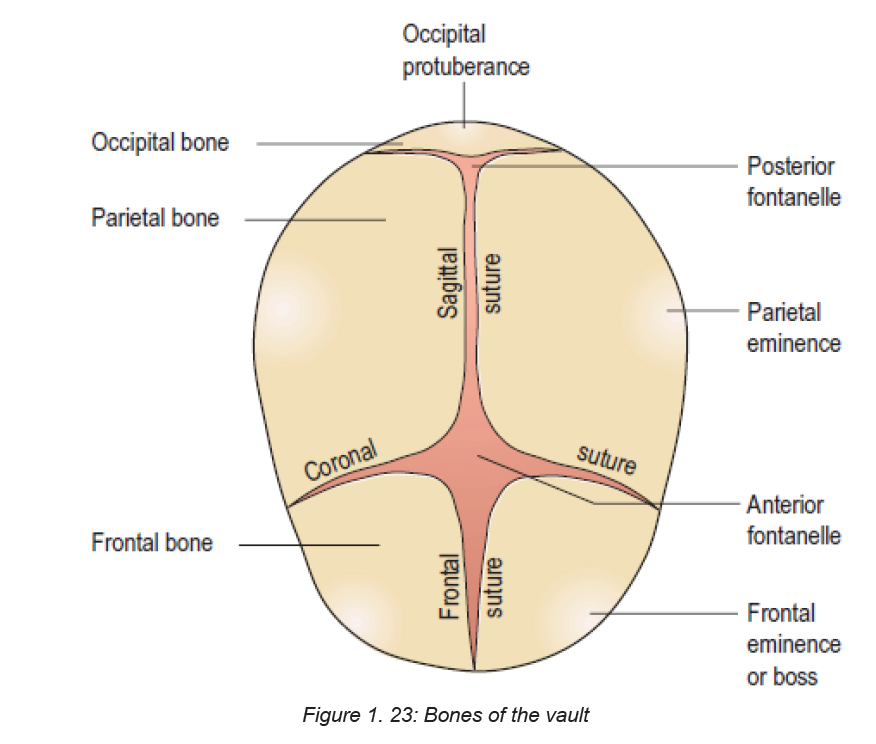
The skull is further separated into regions, and within these there are important
landmarks. These landmarks are useful to the midwife when undertaking a vaginal
examination as they help ascertain the position of the fetal head. The occiput region
lies between the foramen magnum and the posterior fontanelle. The part below the
occipital protuberance (landmark) is known as the sub-occipital region.
The vertex region is bounded by the posterior fontanelle, the two parietal eminencesand the anterior fontanelle.
The forehead /sinciput region extends from the anterior fontanelle and the coronal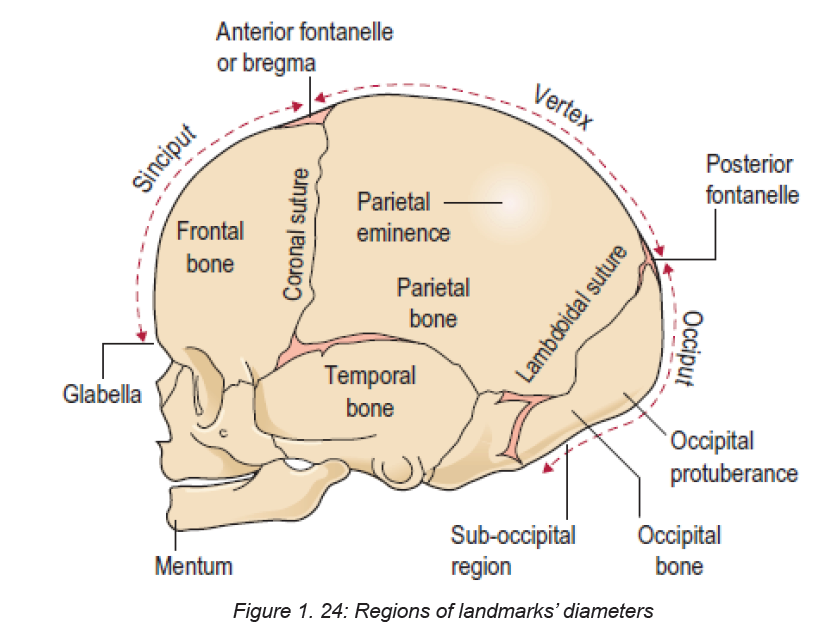
suture to the orbital ridges.
The face extends from the orbital ridges and the root of the nose to the junction of
the chin or mentum (landmark) and the neck. The point between the eyebrows is
known as the glabella.
1.10.4 Sutures and fontanels
The sutures are the cranial joints formed where two bones meet. Where two or
more sutures meet, a fontanelle is formed. The sutures and fontanelles described
below permit a degree of overlapping of the skull bones during labour, which is
known as moulding.
♦ The lambdoidal suture separates the occipital bone from the two parietal
bones.
♦ The sagittal suture lies between the two parietal bones.
♦ The coronal suture separates the frontal bones from the parietal bones,passing from one temple to the other.
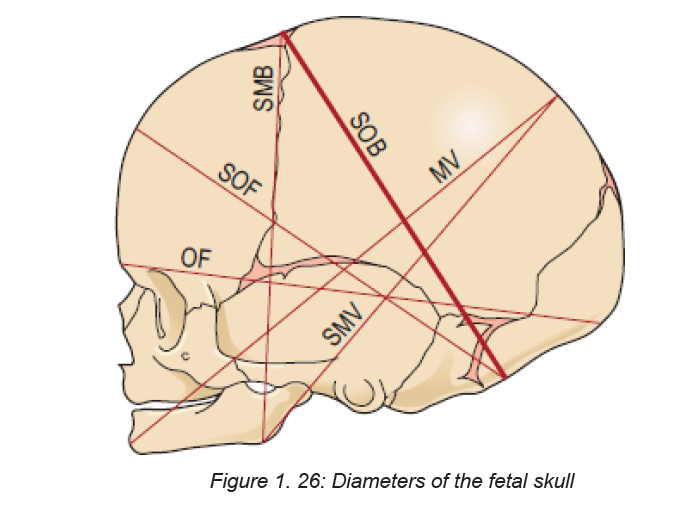
1.10.5 Diameters of the fetal skull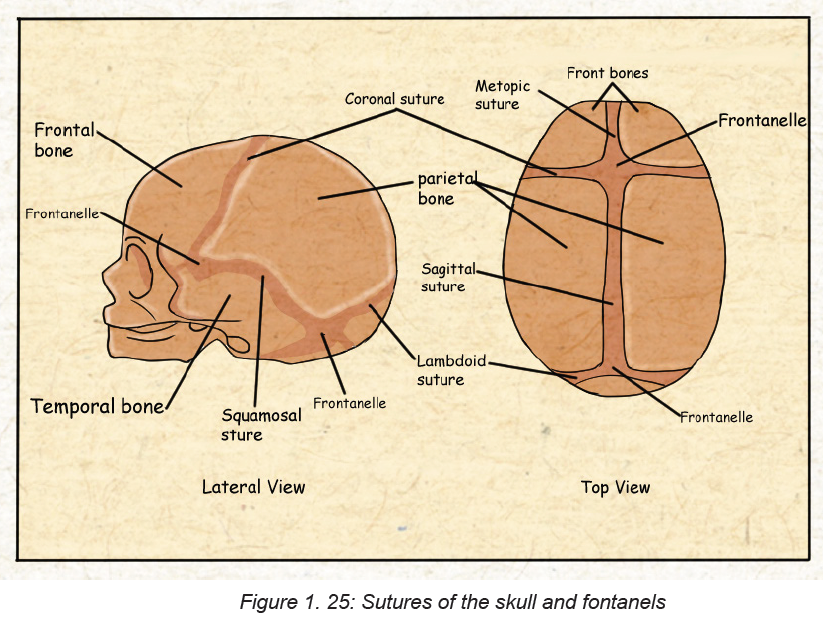
Knowledge of the diameters of the skull alongside the diameters of the pelvis allows
the midwife to determine the relationship between the fetal head and the mother’s
pelvis. There are six longitudinal diameters.
The longitudinal diameters are:
♦ The sub-occipito bregmatic (SOB) diameter (9.5 cm) measured from below
the occipital protuberance to the centre of the anterior fontanelle or bregma.
♦ The sub-occipitofrontal (SOF) diameter (10 cm) measured from below the
occipital protuberance to the centre of the frontal suture.
♦ The occipitofrontal (OF) diameter (11.5 cm) measured from the occipital
protuberance to them glabella.
♦ The mentovertical (MV) diameter (13.5 cm) measured from the point of the
chin to the highest point on the vertex.
♦ The sub-mentovertical (SMV) diameter (11.5 cm) measured from the point
where the chin joins the neck to the highest point on the vertex
♦ The sub-mentobregmatic (SMB) diameter (9.5 cm) measured from the pointwhere the chin joins the neck to the centre of the bregma (anterior fontanelle).
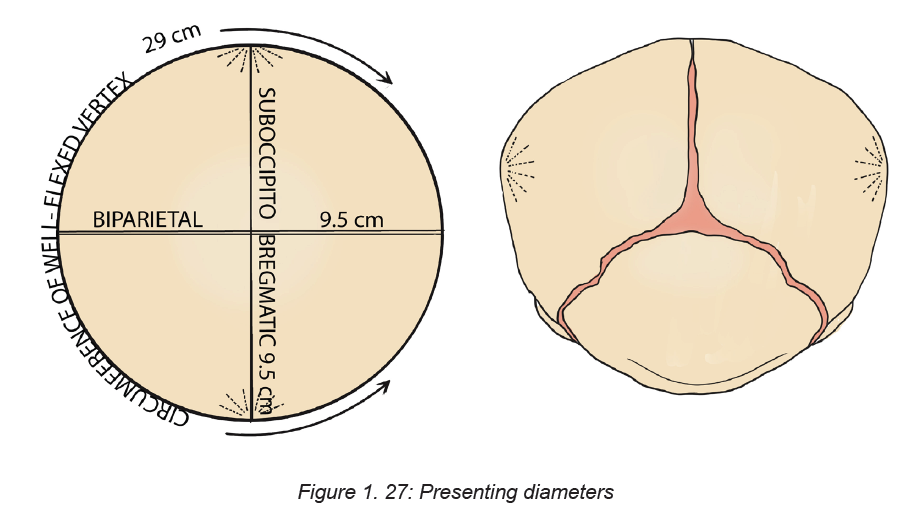
Presenting diameters
Some presenting diameters are more favourable than others for easy passage
through the maternal pelvis and this will depend on the attitude of the fetal head.
This term attitude is used to describe the degree of flexion or extension of the
fetal head on the neck. The attitude of the head determines which diameters will
present in labour and therefore influences the outcome. The presenting diameters
of the head are those that are at right-angles to the curve of Carus of the maternal
pelvis. There are always two: a longitudinal diameter and a transverse diameter.
The presenting diameters determine the presentation of the fetal head, for which
there are three:
1. Vertex presentation. When the head is well flexed the sub-occipitobregmatic
diameter (9.5 cm) and the biparietal diameter (9.5 cm) present.
As these two diameters are the same length the presenting area is circular, which is
the most favourable shape for dilating the cervix and birth of the head. The diameter
that distends the vaginal orifice is the sub-occipitofrontal diameter (10 cm). When
the head is deflexed, the presenting diameters are the occipitofrontal (11.5 cm) and
the biparietal (9.5 cm). This situation often arises when the occiput is in a posterior
position. If it remains so, the diameter distending the vaginal orifice will be the
occipitofrontal (11.5 cm).
2. Face presentation. When the head is completely extended the presenting
diameters are the submentobregmatic (9.5 cm) and the bitemporal (8.2 cm). The
sub-mentovertical diameter (11.5 cm) will distend the vaginal orifice.
3. Brow presentation. When the head is partially extended, the mentovertical
diameter (13.5 cm) and the bitemporal diameter (8.2 cm) present. If this presentationpersists, vaginal birth is unlikely.
Self-assessment activity 1.10
– Explain the role of the sutures and fontanelles during child birth
– State the six longitudinal diameters of the fetal skull.
Identify the three major types of head presentation of the fetus?– Identify the three major types of head presentation of the fetus?
End unit assessment
1. What is fertilization?
2. How long does the process of fertilization take? And at which portion of the
fallopian tube does fertilization take place.
3. What is the main function of the uterus during pregnancy?
4. Describe the major phases of spermatogenesis?
5. Describe the process of capacitation
6. Give the differences between spermatogenesis and oogenesis
7. Give the differences between spermatogenesis and oogenesis
8. Define the following terms:
– Trophoblast
– Embryoblast
– Blastocyst
9. Zygote Describe the factors that can affect fertilization
10. Explain the term “implantation”, what condition favors successful
implantation
11. What are the functions of the amniotic fluid during pregnancy?
12. In relation to embryology and fetal development, explain which organs
forms at 4-8 weeks of pregnancy
13. What is a placenta? And how does it form in embryological stage
14. Describe the functions of the placenta
15. What are the differences between the female and male pelvis.
16. List eight fixed points on the pelvic brim?
17. What is the primary role of the female pelvis?
18. Which type of pelvis is adequate for a normal child birth and why?
19. What is the largest part of the fetal fetus?
20. Explain the sutures and bones of the fetal head and the role they play in
childbirth.
21. What are the temporary structures in addition to the placenta and umbilical
cord that enables fetal circulation?
22. Describe the physical and physiological characteristics of a normal
pregnancy
23. In a table format, show the different types of pelvis and their characteristics
24. Among the four types of pelvis which is more adaptable to child birth and
why?
25. What are the divisions of the pelvis?
26. What are the functions of the female pelvis?
27. List the land marks of the pelvic brim, cavity and outlet and relate their
relevance to child birth28. List the bones and sutures that make up the fetal head.
UNIT 2 ANTENATAL CARE
Key Unit competence: Demonstrate the ability to manage a pregnant woman
during antenatal periodIntroductory activity 2.0
A 34 years old married housewife visited the health center complaining to be
pregnant. Since her pregnancy, it is her first time to visit the health center. During
interview with the nurse, the woman reported to have missed her periods 7
months ago, has increased appetite for cassava and rice only. She did not attend
earlier because of the fear of witchcraft to take her pregnancy away. She has
been using traditional medicines given by her mother in law from the beginning
of the pregnancy. She is experiencing, chills, headache, inability to carry out
daily living activities and she does not know her HIV status.
After reading and understanding the above case:
1. How can you interpret the case?2. What advice can you offer to women in this case?
Antenatal care (ANC) is an umbrella term used to describe the medical and nursing/
midwfery procedures and care that are carried out during pregnancy. It is the care
a woman receives throughout her pregnancy and is important in helping to ensure
a healthy pregnancy state and safe childbirth.
During the prenatal period, health care providers play important role in educating
women about healthy pregnancy behaviors, danger signs of complications,
breastfeeding and family planning; identify and treat pregnancy-related conditions;
refer mothers to specialized care when necessary; encourage the use of a skilled
birth attendant; and minimize the risk of mother-to-child transmission of HIV. In
addition, the ANC provides an opportunity to screen for and treat other chronicconditions and non-communicable diseases.
2.1 Key Concepts used in antenatal careLearning Activity 2.1
Using the school book of Maternal and Child Health, read the information related
to the antenatal care and take short notes on the difference between:
1. Antenatal care and focused antenatal care,
2. Health promotion, health education, health screening and diseasescreening
2.1.1 Antenatal Care
Antenatal care (prenatal care) is the care given to pregnant women from the time
conception is confirmed until the beginning of labour. The nurse provides her with
accessible and relevant information to help her make informed choices throughout
the pregnancy.
2.1.2 Focused Antenatal Care (FANC)
FANC is personalized care provided to a pregnant woman which emphasis on
the woman overall health status, her preparation for childbirth, and readiness for
complications.
2.1.3 Health Promotion
Health promotion refers to any activity that aims to achieve better health in a
community or a country.
2.1.4 Health education
It is the effective transmission of accurate, useful, health-related information to
community members; it enables individuals and groups to develop their knowledge
of health issues, and increase their self-reliance and competence to solve their
own health problems through their own initiatives. A major determinant of good or
ill health is the knowledge people have about health issues, their beliefs, attitudes
and behaviour, and their desire to bring about positive behaviour change in their
lives.
2.1.5 Health screening
Health screening is the routine testing of individuals to see if they are at risk of
developing a health problem. Health screening is an important health promotion
activity that you will conduct as part of your antenatal care service. For example,
you will take the temperature, blood pressure and pulse of every pregnant woman
at every antenatal visit to see if she may be developing a health problem that could
harm her or her baby.
2.1.6 Disease Prevention
It is any action taken to prevent a disease from developing. For example, giving
pregnant women iron supplements as a routine part of antenatal care is an action to
prevent the development of anaemia, a condition in which the body makes too fewred blood cells because the woman’s diet does not contain enough iron.
2.1.7 Booking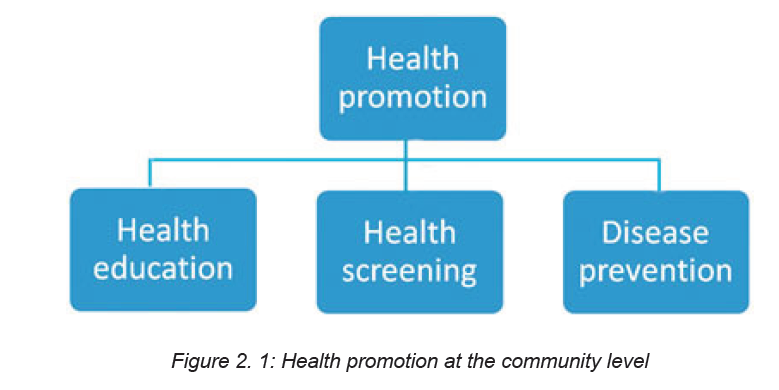
An Antenatal Booking Appointment is the APPOINTMENT where the woman enters
the maternity care pathway, characterized by information giving and detailed history
taking to help the woman choose the most appropriate Antenatal care pathway.
2.1.8 History taking
History taking is the process of collecting information to assess the past and present
obstetrical, medical and surgical problems in order to detect risk factors for thepatient and her fetus.
Self-assessment 2.1
1. Discuss the objectives of the initial assessment (booking)2. What is history taking and state the purpose for taking history.
2.2 Principles, objectives and components of Focused Antenatal
CareLearning Activity 2.2
1. On the above chart, describe the person A and B, and what you think, they
are doing
2. From the above chart, identify the importance of communication
Focused antenatal care (FANC) is a personalized care provided to a pregnant
woman which emphasizes on the women’s overall health status, her preparation
for child birth and readiness for complications or it is timely, friendly, simple safe
services to pregnant women.
Principles of FANC are as follow:
a. Developing a trusting relationship with the woman
b. Providing a holistic approach to the woman’s care that meets her individual
needs
c. Making a comprehensive assessment of the woman’s health and social status
d. Promoting an awareness of the public health issues for the woman and her
family
e. Exchange the information with the woman and her family
f. Enabling them to make informed choices about pregnancy and birth
g. Be an advocate for the woman and her family during her pregnancy
h. Supporting her to choose care appropriate for her own needs and those of
her family
i. Identifying potential risk factors and taking appropriate measures to minimize
them
j. Timely share information with relevant agencies and professionals
k. Accurate documentation of assessment, plans, care and evaluation
l. Recognizing complications of pregnancy and appropriately referring women
to the obstetric team or relevant health professionals
m. Preparing the woman and her family to meet the challenges of labour and
birth, and facilitating the development of birth plan
n. Facilitating the woman to make an informed choice about methods of infant
feeding and giving appropriate and sensitive advice to support her decision
o. Offering parenthood education within a planned programme or on individual
basis
Major goals/objectives of the FANC are as follow:
a. Promote and maintain the physical, mental, and social health of mother and
baby by providing education on nutrition, personal hygiene, and birthing
process;
b. Detect and manage complications during pregnancy, whether medical,
surgical, or obstetrical;
c. Develop birth preparedness and complication readiness plan;
d. Help prepare mother to breastfeed successfully, experience normal
puerperium, and take good care of the child physically, psychologically, and
socially.
Components of FANC are as follow:
a. Blood pressure measurement,
b. Provision of a blood sample,
c. Provision of a urine sample,
d. Tetanus vaccination,
e. Intermittent preventive treatment of malaria during pregnancy (IPTp) including
number of times,
f. Deworming treatment,
g. Iron-folic acid supplements
COMMUNICATION IN MATERNITY
The nurse requires many skills to provide optimal antenatal care. Fundamentally the
ability to communicate effectively and sensitively. Listening skills involve focusing
on what the woman is saying and how she is saying it, considering the content and
tone.in addition non-verbal communication.
Importance of communication in antenatal care
Communication skills are critical to the delivery of high-quality maternity services.
It is impossible to ensure the provision of the best possible care, using available
resources to their fullest, without accurate and complete communication with
women, their families and multi-professionals.
Table 2. 1: ANC schedule for the new model of eightcontacts
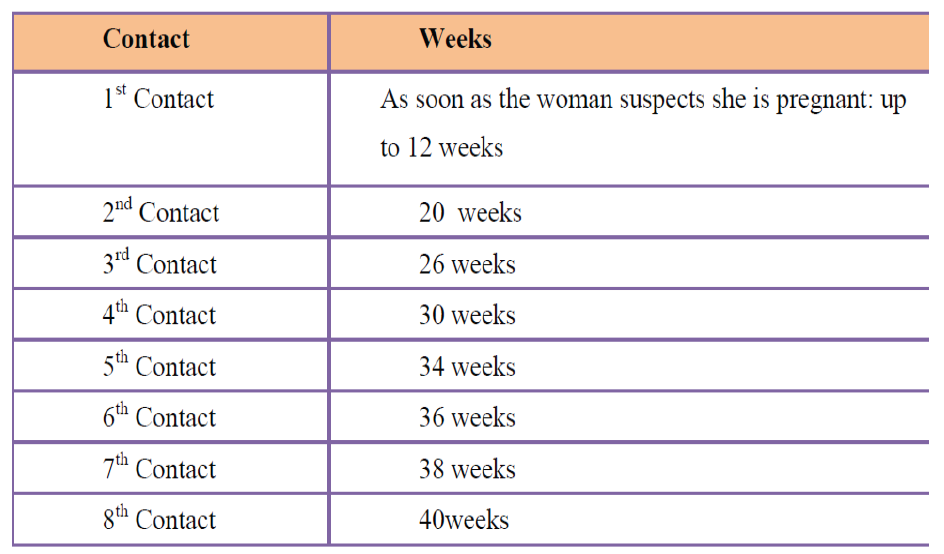
Self-assessment 2.2
– Discuss the principles of FANC– What are the components of antenatal care?
2.3 The diagnosis of pregnancyLearning Activity 2.3
A 22 years’ young lady, visited health care facility complaining of nausea,
tiredness, loss of appetite, she vomited two time in morning, and she stated not
having her menstrual period last month.
– What do you think would be the problem and which advice can you give
to her?
Most women are diagnosed with pregnancy after a missed menstrual cycle and a
positive urine or serum HCG. The pregnancy is diagnosed as viable with serial
exams and normal pregnancy development, a normal dating ultrasound, or positivefetal heart tones by Doppler.
Women who are aware of their bodies must begin to suspect that they are pregnant
within the first few days of pregnancy. But for most, the first sign is missing a period.
Other symptoms include nausea and vomiting, breast tenderness and fullness,
urinary frequency, and fatigue.
Traditionally, diagnosis has been based on history, and physical examination.
Issues that may confuse the diagnosis of an early pregnancy are an atypical last
menstrual period, contraceptive use, and history of irregular periods. Spotting or
light bleeding is common in early pregnancy between six and seven weeks which
may further complicate the assessment.
SIGNS AND SYMPTOMS OF PREGNANCY
PRESUMPTIVE SIGNS
Presumptive signs and symptoms of pregnancy are those signs and symptoms
that are usually noted by the client, which impel her to seek care. These signs and
symptoms are not proof of pregnancy but they will make the health provider and
woman suspicious of pregnancy.
Amenorrhea (Cessation of Menstruation)
Amenorrhea is one of the earliest clues of pregnancy. The majority of clients have
no periodic bleeding after the onset of pregnancy
Other causes for amenorrhea must be ruled out, such as:
♦ Menopause.
♦ Stress (severe emotional shock, tension, fear …)
♦ Chronic illness (tuberculosis, endocrine disorders, or central nervous system
abnormality).
♦ Anemia.
Nausea and Vomiting (Morning Sickness)
Usually occurs in early morning during the first weeks of pregnancy. It is usually
spontaneous and subsides in 6 to 8 weeks or by the twelfth to sixteenth week of
pregnancy. Nausea and vomiting are unreliable signs of pregnancy since they may
result from other conditions.
Frequent Urination:
Frequent urination is caused by pressure of the expanding uterus on the bladder.
It subsides as pregnancy progresses and the uterus rises out of the pelvic cavity. The
uterus returns during the last weeks of pregnancy as the head of the fetus presses
against the bladder. Frequent urination is not a definite sign since other factors can
be apparent (such as tension, diabetes, urinary tract infection, or tumors).
Breast changes
In early pregnancy, changes start with a slight, temporary enlargement of the
breasts causing a sensation of weight, fullness, and mild tingling. As pregnancy
continues the patient may notice Darkening of the areola--the brown part around the
nipple. Enlargement of Montgomery glands--the tiny nodules or sebaceous gland
within the areola. Increased firmness or tenderness of the breasts More prominent
and visible veins due to the increased blood supply. Presence of colostrum (thin
yellowish fluid that is the precursor of breast milk). This can be expressed during
the second trimester and may even leak out in the latter part of the pregnancy.
Vaginal changes
CHADWICK’S SIGN: The vaginal walls have taken on a deeper colour caused by
the increased vascularity because of increased hormones. It is noted at the sixth
week when associated with pregnancy. It may also be noted with a rapidly growing
uterine tumor or any cause of pelvic congestion.
Quickening (FIRST FETAL MOVEMENT FELT BY THE MOTHER)
This is the first perception of fetal movement within the uterus. It usually occurs
toward the end the fifth month because of spasmodic flutter.
♦ A multigravida can feel quickening as early as 16 weeks.
♦ A primigravida usually cannot feel quickening until after 18 weeks.
Skin changes
Striae gravidarum (stretch marks). These are marks noted on the abdomen and/or
buttocks.
These marks may be seen on a patient with Cushing’s disease or a patient with
sudden weight gain.
Linea nigra
his is a black line in the midline of the abdomen that may run from the sternum orumbilicus to the symphysis pubis.
This appears on the primigravida by the third month and keeps pace with the rising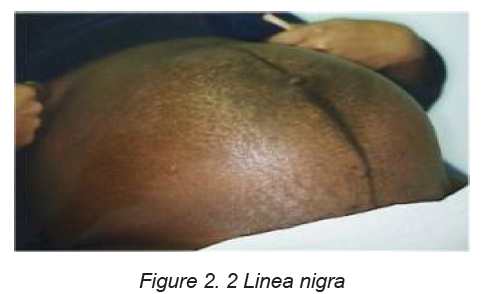
height of the fundus. The entire line may appear on the multigravida before the third
month.
Chloasma
This is called the “Mask of Pregnancy.” It is a bronze type of facial coloration seen
more on dark-haired women. It is seen after the sixteenth week of pregnancy.
PROBABLE SIGNS OF PREGNANCY
Probable signs of pregnancy are those signs commonly noted by the health providers
upon examination of the client. These signs include: uterine changes; abdominal
changes; cervical changes; basal body temperature; a positive pregnancy test and
fetal palpation.
Uterus grows - the abdomen gets larger
Position: By the twelfth week, the uterus rises above the symphysis pubis and it
should reach the xiphoid process by the 36th week of pregnancy.
Size: The uterine increases in width and length approximately five times its normal
size. Its weight increases from 50 grams to 1,000 grams.
Hegar’s Sign: This is softening of the lower uterine segment just above the cervix.
When the uterus is compressed between examining fingers
Ballottement: Ballottement is when the lower uterine segment or the cervix is
tapped by the examiner’s finger which is left in place during the procedure. The
fetus floats upwards, then sinks back and a gentle tap is felt on the finger .it is done
at 16th to 20th weeks
Abdominal Changes
This corresponds to changes that occur in the uterus. As the uterus grows, the
abdomen gets larger. Abdominal enlargement alone is not a sign of pregnancy.
Enlargement may be due to uterine or ovarian tumors, or edema.
Cervical changes
Goodell’s sign: The cervix is normally firm, like the cartilage at the end of the nose.
Goodell’s sign occurs when there is marked softening of the cervix. This is present
at the 6th week of pregnancy.
Formation of a mucous plug: This is due to hyperplasia of the cervical glands
as a result of increased hormones. It serves to seal the cervix of the pregnant
uterus and to protect it from contamination by bacteria in the vagina. The mucous
is expelled at the end of pregnancy near or at the onset of labour.
Braxton-Hick’s contractions: This involves painless uterine contractions occurring
throughout pregnancy. It usually begins at about the 12th week of pregnancy and
becomes progressively stronger. These contractions will, generally, cease with
walking or other forms of exercise.
POSITIVE SIGNS OF PREGNANCY
Positive signs of pregnancy are those signs that are definitely confirmed as a
pregnancy. They include fetal heart sounds, ultrasound scanning of the fetus,
palpation of the entire fetus, palpation of fetal movements, x-ray, and actual deliveryof an infant.
Self-assessment 2.3
– List positive signs of pregnancy– Describe the chloasma of pregnancy
2.4 Comprehensive assessment of a pregnant womanLearning Activity 2.4
A 30 years’ pregnant woman for the first time visited the health center for focused
antenatal consultation (FANC) at 12 weeks, during interview, you realized it was
her first antenatal contact, she stated that she does not have problem but she
wants to know the condition of her baby and pregnancy.
-In your opinion, suggest reasons why it is important to check the wellbeing of
mother and baby during pregnancy.
2.4.1 Introduction to Booking and history taking
The booking assessment shapes the direction of a woman ‘antenatal pathway.it is
where her risk status is determined and appropriate referral made. The information
gathered regarding the woman’s obstetric, medical and social history and current
pregnancy enables the nurse to assess her status. If a risk factor is identified, the
woman should be referred to the doctor who will discuss a plan of care for her
based on identified problem.
A comprehensive assessment is done from head to toe with the woman’s consent.
The initial assessment (Booking visit)
The purpose of this unit is to initiate the development of a trusting relationship that
facilitates positive engagement of the woman with the maternity service. This is
the most important element of ANC care. Whilst, it is crucial that risk assessment
and identification of clinical relevant information is obtained, none of these can be
undertaken if the woman does not feel able to communicate with the nurse.
Objectives for the initial assessment
♦ To assess levels of health by taking a detailed history and to offer appropriate
screening tests.
♦ To ascertain baseline recordings of blood pressure, urinalysis, blood values,
uterine growth and fetal development to be used as a standard for comparison
as the pregnancy progresses.
♦ To identify risk factors by taking accurate details of past and present history,
obstetrics, medical, family and personal history.
♦ To provide an opportunity for the woman and her family to express and discuss
any concerns they might have about the current pregnancy and previous
pregnancy loss, labour, birth or puerperium.
♦ To give public health advice and that pertaining to pregnancy in order to
maintain the health of the mother and the healthy development of the fetus.
♦ To build the foundation for a trusting relationship in which the woman and
midwife are partners in care.
♦ To make appropriate referral where additional healthcare or support needs
have been identified
First impressions
The initial observation and assessment of a woman at the start of first meeting is
very important. The observation should be carried sensitively enhancing the woman
to experiences of pregnancy birth.
Observation of physical characteristics is also important. Posture and gait can
indicate back problems or previous trauma to the pelvis; the woman may be
lethargic, which could be an indication of extreme tiredness, anemia, malnutritionor depression.
2.4.2 History taking:
This is the process of collecting all relevant information from a pregnant woman
which will build the bases for monitoring her pregnancy.
Points to consider while taking history
• Ensure privacy (respectful maternity care)
• Ensure quiet and calm atmosphere
• Make the woman comfortable and relaxed
• Maintain confidentiality
• Establish rapport
• Record all information on the patient’s file
• High light abnormal findings
History to be taken include:
A. Personal and preliminary data
♦ Woman full names
♦ Age
♦ Date and place of birth
♦ Address and phone number
♦ Ethnic or racial appartenance
♦ Profession and that of the partner or employment history
♦ Religion
♦ Marital status and number of years married
B. Chief complains: the major health problem or concern, and its time course
(e.g. abdominal pain for past 4 hours).
C. History of present illness
After determining the chief concern for a visit, the next step is to inquire about the
history of the present illness (HPI). This is often a misnomer—for example, the
reason for a visit of “I need my Pap test and birth control pills” leads to an HPI that
addresses how the woman is managing her contraception and her satisfaction with
her current method (and possibly to a discussion of screening recommendations). A
chief concern that begins with abnormal uterine bleeding leads to the more traditional
assessment of the history of the woman’s current symptoms. A common mnemonic
for the questions asked about a health problem is OLD CARTS (Onset, Location/
radiation, Duration, Character, Aggravating factors, Relieving factors, Timing, and
Severity). These questions can be followed by “What has changed now that made
you come in?” or “How did you decide it was time to come in?”
D. Social history
The social history, like the sexual history, brings up topics that may be embarrassing
or even threatening to some women. Ask these questions in a quiet, professional
tone, and respect the woman’s need to avoid certain answers. Providing information
“why” the information is needed often reassures the woman and may help the
midwife feel comfortable asking for it. Obviously if there is no reason for eliciting
sensitive information, asking it should be omitted. Relationship questions should
be asked in a pattern that allows women to reveal relationships that are more
complicated than “single” or “married with children.”Table 2. 2 Elements assessed in social history
E. General health status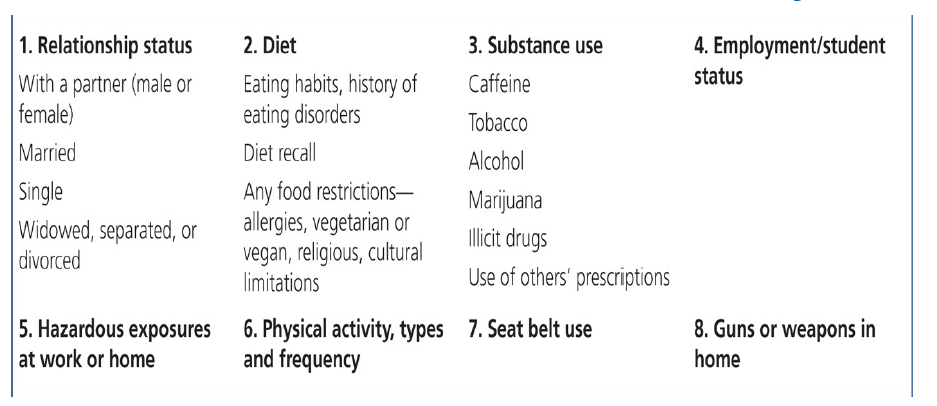
General health should be discussed and good habits reinforced, giving further
advice when required e.g exercise puts added demands on the cardiovascular and
respiratory systems, however mild exercise should be continued.
Smoking: women may be ready to cut down or give up smoking. The midwife has a
role or duty to help women to set goals throughout their pregnancy and help them
to cut down their smoking, strategies to help them cut down includes:
• Doing something else;
• Delaying having a cigarette or drinking water can help them cut down on
smoking.
Babies born to women who smoke are frequently smaller, have respiratory tract
problems at birth and in their first year, have higher rates of prematurity, still birth
and low birth weight. There is also increased risk of asthma and otitis media in
these babies for women who are more addicted should stick smoking earlier in the
day, stop last thing at night, they should be referred to appropriate organizations
for help.
• Alcohol: alcohol is less common but can affect the baby. There is no
conclusive evidence of adverse effects on the fetus at a consumption level
below 10 units per week, but it is recommended that women do not exceed
one to two unites once a week.
F. Menstrual history
An accurate menstrual history is taken to determine the expected date of delivery
(EDD). This will enable the midwife to predict a birth date and subsequently calculate
gestational age at any point in the pregnancy abdominal assessment of uterine size
can be during ANC consultation.
The duration of pregnancy could also be based on the Naegle’s rule which is
based on the mythical normal woman who has a 28 days cycle and ovulates two
weeks before the start of her next menstrual period i.e. on day 14. The rule is to add
seven days to the first day of the last menstrual period and count back three months
to reach the expected date of delivery or confinement or EDC.
The EDD is calculated by adding 9 calendar months if the last month of
menstruation is ≤ to 3 or moins 3 if month ≥ to 4 and adding 7 days to the date of
the 1st day of the woman’s last menstrual period (LMP) this method assumes that:
• The woman takes regular note of regularity and length of time between periods
• Conception occurred 14 days after the 1st day of the last period; this is true
only if the woman has a regular 28 days’ cycle.
• The last period of bleeding was true menstruation but implantation of the
ovum may cause slight bleeding.
Example on calculation of EDD
Calculating from “sure” dates by Naegele’s Rule
Cycle of 28days=LMP: 9 June 2014
EDD = 9+7days/6- 3/
EDD: 16 March 2015
NB: Gestational age in weeks of pregnancy can be calculated by using Mac Donald
formula which use the fundus height
The formula is Fundus height in cm *8 divides by 7. For example, if the fundus
height is 24 cm, gestational age is 24cm*8=192 = 27 week’s gestation.
The features to note are:
• Normality of last menstrual period; an implantation bleed may occur at about
the time of the expected period (i.e. 10-14 days after ovulation). This is almost
always much lighter and shorter than a normal period. If an implantation bleed
is mistaken for a time period, the gestational age calculation would be behind
by about four weeks.
• Cycle interruption: a calculation adjustment is needed in those women who
have not re-established regular cycles after pregnancy, lactation or the
contraceptive pills. However, as the differences in gestational age between
the two methods increase, ultrasound becomes the more accurate method
for predicting the EDD.
• The calculation is difficult if the woman does not know the date of her last
mentraual period, where cycles are irregular,or a normal cycle has not
resumed since taking the oral contraceptives pill.if the woman has a good
idea of when conception occurred ,the EDD can be calculated by adding 38
weeks to this date ,or subtracting 7 days from 9 months.
• Women should be asked to note the date when fetal movement are first felt.
Primigradae normally become aware of fetal movement between 18-20weeks
while multigradae recognize the sensation a little earlier, between 16-18weeks.
This may be used to estimate the expected date of delivery.
G. Family history
Certain conditions are genetic in origin others are familial or related to ethnicity and
some are associated with the physical or social environment in which the family
lives. The family history may reveal factors that increase the risk of blood disorder,
maternal medical complications or fetal abnormalities; e.g. Twins, Diabetes mellitus,
Hypertension, hereditary diseases like asthma.Table 2. 3 Family History (Three Generations)
H. Past medical history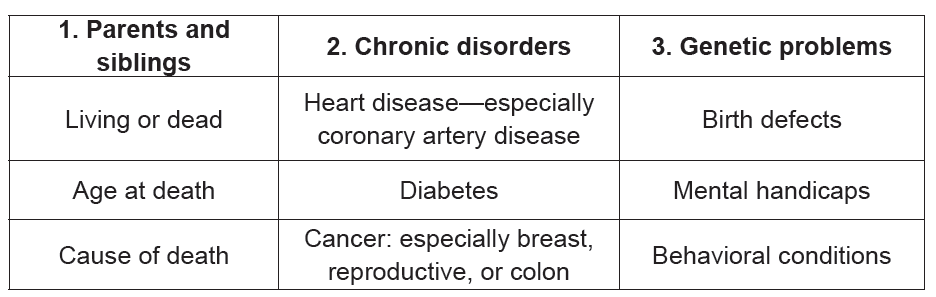
Past current medical disorders and associated medications may threaten the mother
and fetus e.g. Diabetes mellitus, Epilepsy, Rheumatics fever, Renal diseases.
During pregnancy both the mother and fetus may be affected by a medical condition
or a medical condition may be altered by the pregnancy, if untreated there may be
serious consequences for the woman’s health. Other conditions including asthma,
epilepsy, infections, and psychiatric disorders may require treatment, which may
adversely affect fetal development. Major medical complications such as diabetes
and cardiac conditions require the involvement and support of a medical specialist
♦ Urinary stasis and reflex occur during pregnancy. A urinary tract infection
(UTI) can easily develop into pyelonephritis, which, untreated may lead to
kidney damage and cause preterm labour, between 30 and 50% of women
will be asymptomatic if it is untreated;
♦ Pregnancy predisposes to deep vein thrombosis and thus pulmonary
embolism, women of increasing weight and maternal age, those who are
obese and those with a history of thromboembolic disorders are most at risk;
♦ Essential hypertension predisposes to pregnancy induced hypertension,
which can result in reduced placental function, intrauterine growth retardation,
abruption placenta, fetal compromise or death. Effect on the mother includes
congestive heart failure, intracerebral hemorrhage, acute renal failure,
disseminated intravascular coagulation (DIC) or death as a result of any of
above (Hallak 1999).
♦ Pregnancy and concomitant disease (Can be exacerbated by the pregnancy
or complicate it) especially Diabetes, Heart disease, Hypertension,
Neuromuscular disorders
♦ Medications and allergies to medications Should be identified and recorded
♦ Any current ongoing illness, e.g. diabetes, malaria
♦ Past history containing physiological and pathological data
Example: Past medical/surgical history including major illnesses, any previous
surgery/operations
I. Past surgical history
♦ General surgical procedures;
♦ Gynecological surgical procedures;
♦ Myomectomy scar may increase risk of uterine rupture;
♦ Conisation or cervical cerclage of the cervix and therapeutic abortion may
increase the risk of cervical incompetence and premature labour.
J. Past obstetric history/ General OB/GYN Assessment
Like histories in general, many complications of pregnancy have a tendency to
recur; it is for this reason that the previous obstetric history holds a wealth of
valuable relevant information:
Collect Subjective data
♦ Prenatal history
♦ Past pregnancies
♦ Gynecologic history including LPM
Obstetric History Concerns
♦ Gravida/para (G/P) status
• Number of living children?
• Number of dead children, when, how and on which pregnancy
• Complications with previous pregnancies or deliveries?
• History of preterm delivery?
• Gestational age?
• History of elective or spontaneous abortion?
• Has patient delivered vaginally after a cesarean section?
• When was, and what was length of last labor?
• With regard to current pregnancy, what is estimated date of confinement
(EDC)?
• Has patient received adequate, limited (three or fewer visits), or no prenatal
care?
• Any problem with pregnancy identified? If so, what?
• Diagnostic tests like ultrasound done? If so, what were results?
• Is patient taking any medications for obstetric or non-obstetric reasons?
• If so, which medication(s), what dose(s), and compliant schedule(s)?
• Drug or alcohol abuse suspected? If so, which substance(s), frequency of
use, date of last use? Patient smoking?
• Pregnancy weight gain normal, or patient malnourished or obese?
• Is patient having contractions? If so, when did they begin, and what are their
frequency and duration?
• Antenatal complications e.g. pre-eclampsia, premature labour, isoimmunisation;
• Induction of labour and indication; Assisted vaginal delivery;
• Caesarean section- indications, type of section and complication if any;
• Third stage complications: post-partum hemorrhage and/or manual removal
of placenta;
• Neonatal outcome, e.g. intrauterine growth restriction, macrosomia, congenital
anomaly, perinatal death or morbidity. On the other hand, one or more totally
normal pregnancies is the best prognostic factors for a successful outcome insubsequent pregnancies.
The final question in the history taking should be some variant of “Is there anything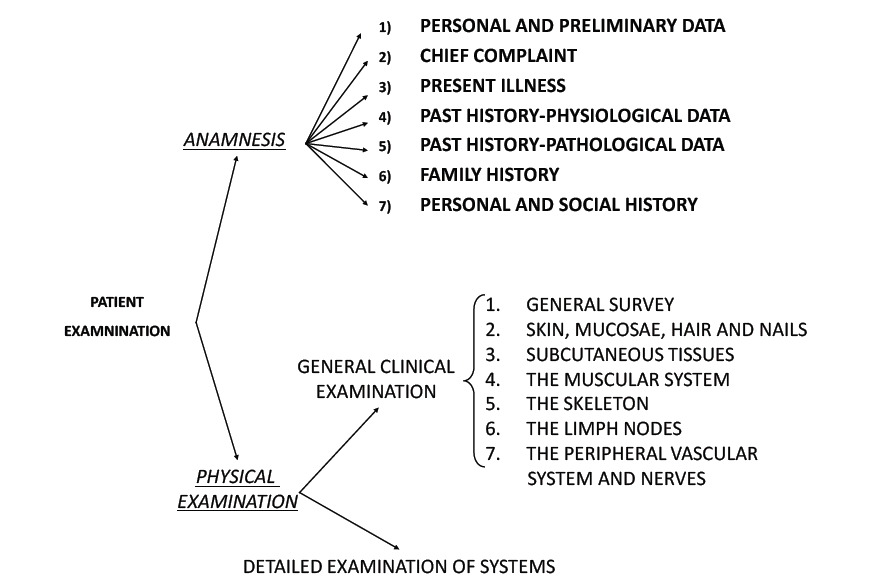
else I should have asked you today?” or, alternatively, “Is there anything else I
should know or that you want to share with me?”
Table 2.4: Factors that may require additional
antenatal support or referral to an obstetrician/physician or other health professional
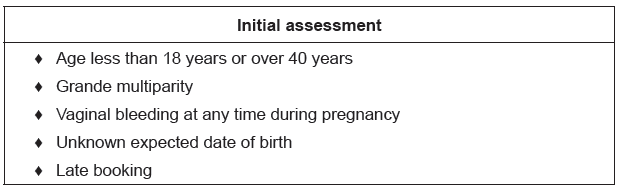
Self-assessment 2.4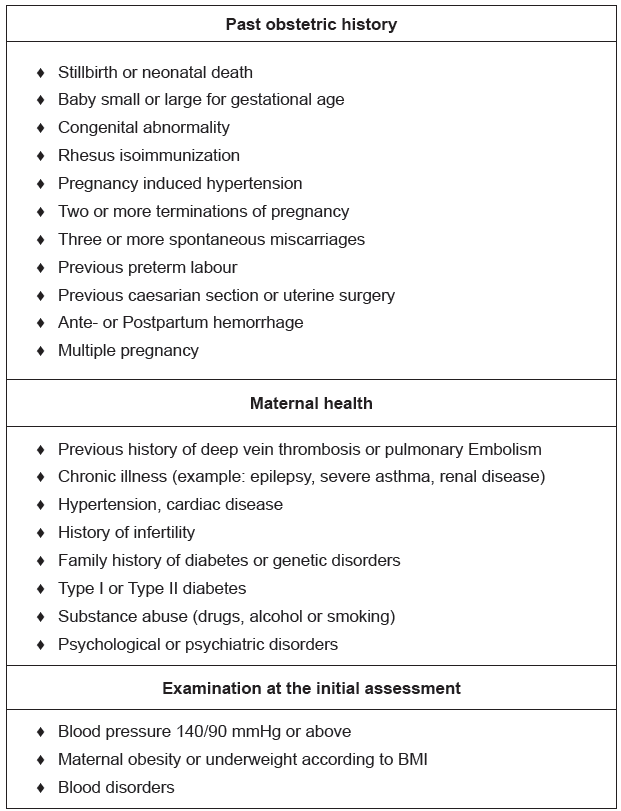
1. What are the important points to note before taking history?2.5 Physical examination
2.5 Physical examination
Learning Activity 2.5
Watch the Video on physical examination of a pregnant woman and discuss
what you have seen in your groups.https://www.youtube.com/watch?v=kSRR1HT1ENA
This is a systematic assessment of the pregnant woman from head to toe. Prior to
conducting the physical examination of a pregnant, her consent and comfort are
primary considerations. Observation of physical characteristics is important.
A thorough examination is made at the first visit. This is divided into a general
examination and an obstetric examination.
The general examination should include:
a. General appearance: Namely, the nutritional status, whether weak or sick
looking. Note the gait and if she walks with a limp.
b. Height: You may note that any woman below 150 cm in height is likely to have
cephalo-pelvic disproportion (CPD).
c. Weight: That is, a pregnant woman on average gains 2kg every month. The
total weight gain by the end of pregnancy is about 10-20 kg. Excessive weight gain
indicates accumulation of fluid in the tissues (Oedema). Lack of increase in weight
or loss may mean malnutrition. Obesity may lead to an increased risk of gestational
diabetes.
d. Blood pressure: Blood pressure is taken in order to ascertain normality and
provide a baseline reading for comparison throughout pregnancy. Systolic blood
pressure does not alter significantly in pregnancy, but diastolic falls in mid pregnancy
and rises to near non-pregnant levels at term. The systolic recording may be falsely
elevated if a woman is nervous or anxious, if a small cough is used on a large arm,
the arm is unsupported or if the bladder is full. The woman should be comfortably
seated or resting in lateral position on the couch for the measurement. Brachial
artery pressure is highest when the subject is sitting and lower when in recumbent
position.e. Other vital signs (temperature, pulse and respiration).
HEAD TO TOE ASSESSMENT
1.HEAD (HEENT):
- Hair: check for malnutrition, hygiene, any injury
- Face: the face will indicate:
♦ The general health of the woman nourished and content, or malnourished,
♦ Pallor of the conjunctiva indicates anemia,
♦ Jaundice is early recognized by the yellow conjunctiva.
♦ Edema of the face is a serious sign of pre-eclampsia. Also check for symmetry.
- Mouth:
♦ Stomatitis indicates vitamin B deficiency,
♦ Check tongue pallor.
♦ The gums are sensitive during pregnancy because of hormonal changes,
♦ Dental caries are a potential source of infection
- Ears: check for any symmetry, discharge or other abnormality
- Nose: symmetry, discharges, tumors
2. NECK:
– Swollen glands, stiffness, and thyroid enlargement.
– Veins turgescence
3. CHEST:
– Symmetry of the breasts
– Breathing movement (inspection and auscultation) or abnormalities
– Breast examination: the breasts may be examined to note pregnancy changes,
a useful aid in diagnosis of pregnancy and to note any features such as the
presence of lumps or abnormal discharges from the nipples. The breasts are
likely to feel tender in the first trimester; palpate gently with the flat of the hand
to feel for any lumps. Check if the nipple is protractile. Educate the woman on
how to examine the breasts by herself
– The heart and the lungs will be checked and any deviations noted (auscultation
for rate and rhythm).
– The back is examined for spinal deformities, back tenderness and costal
vertebral angle tenderness (CVAT) for kidney infection
4.UPPER LIMBS:
check for symmetry, pallor of the palm of hands and nails, edema
5. ABDOMEN:
– The abdomen is examined to ascertain whether the uterus is palpable and, if
so, if its size is compatible with the estimated period of gestation
– Assess the shape, the size, previous scar, fetal movements, strae gravidarum,
linea negra.
6. LOWER LIMBS:
The lower limbs are examined for:
♦ Feet and knee reflexes. If BP is high, protein in urine or woman has headache,
visual changes or epigastric pain (patellar reflex)
♦ Checking for symmetry
♦ Physiological oedema occurs after rising in the morning and worsens during
the day; it is often associated with daily activities or hot weather. At visits later
in pregnancy the midwife should observe for oedema and ask the woman
about symptoms. Often the woman may notice that her rings feel tighter and
her ankles are swollen. Pitting oedema in the lower limbs can be identified
by applying gentle fingertip pressure over the tibial bone: a depression will
remain when the finger is removed. If oedema reaches the knees, affects
the face or is increasing in the fingers it may be indicative of hypertension of
pregnancy if other markers are also present.
♦ Homan’s signs are checked in order to diagnose any thrombophlebitis (more
specific in post-partum period)
♦ Checking varicose veins. These are more likely to occur during pregnancy
and are a predisposing cause of deep vein thrombosis. The woman should
be asked if she has any pain in her legs. Reddened areas on the calf may be
due to varicosities, phlebitis or deep vein thrombosis. Areas that appear white
as if deprived of blood could be caused by deep vein thrombosis. The woman
should be asked to report any tenderness that she feels either during the
examination or at any time during the pregnancy. Referral should be made
to medical colleagues as appropriate. Support stockings will help alleviatesymptoms although not prevent varicose veins occurring.
Self-assessment 2.5
Using mannequin in simulation lab, demonstrate steps of physical examinationof pregnant woman.
2.6 Leopold’s manoeuver
The Leopold maneuvers are used to palpate the gravid uterus systematically. This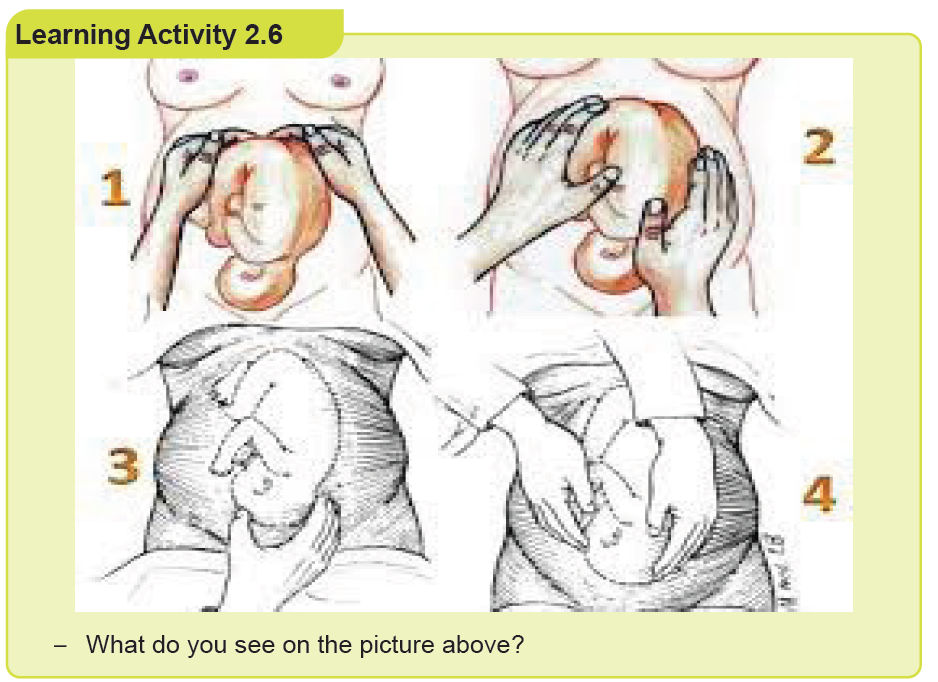
method of abdominal palpation is of low cost, easy to perform, and non-invasive.
It is used to determine the position, presentation, and engagement of the fetus in
utero.
Abdominal examination
Abdominal examination is carried out from 24 weeks’ gestation to establish and
affirm that fetal growth is consistent with gestational age during the pregnancy. The
specific aims are to:
• Observe the signs of pregnancy
• Assess fetal size and growth
• Auscultate the fetal heart when indicated
• Locate fetal parts
• Detect any deviation from normal.
Preparation
The woman should be asked to empty her bladder before making herself
comfortable on the couch. A full bladder will make the examination uncomfortable;
this can also make the measurement of fundal height less accurate. The midwife
washes her hands and exposes only that area of the abdomen she needs to
palpate, and covers the remainder of the woman to promote privacy and protect
her dignity. The woman should be lying comfortably with her arms by her sides to
relax the abdominal muscles. The midwife should discuss her findings throughout
the abdominal examination with the woman.
Inspection
The uterus is first assessed by observation. A full bladder, distended colon or obesity
may give a false impression of fetal size. The shape of the uterus is longer than it
is broad when the lie of the fetus is longitudinal, as occurs in the majority of cases.
If the lie of the fetus is transverse, the uterus is low and broad.
The multiparous uterus may lack the snug ovoid shape of the primigravid uterus.
Often it is possible to see the shape of the fetal back or limbs. If the fetus is in
an occipitoposterior position a saucer-like depression may be seen at or below
the umbilicus. The midwife may observe fetal movements, or the mother may feel
them; this can help the midwife determine the position of the fetus. The woman’s
umbilicus becomes less dimpled as pregnancy advances and may protrude slightly
in later weeks.
Lax abdominal muscles in the parous woman may cause the uterus to sag forwards;
this is known as pendulous abdomen or anterior obliquity of the uterus. In the
primigravida it is a significant sign as it may be due to pelvic contraction.
Skin changes
Stretch marks from previous pregnancies appear silvery and recent ones appear
pink. A linea nigra may be seen; this is a normal dark line of pigmentation running
longitudinally in the centre of the abdomen below and sometimes above the
umbilicus. Scars may indicate previous obstetric or abdominal surgery or self-harm.
Measuring fundal height
In order to determine the height of the fundus the midwife places her hand just at
the upper border of the symphysis pubis. Pressing gently, she moves her hand
to the abdomen up to the level below the sternum where she feels the fundus.
Clinically assessing the uterine size to compare it with gestation does not always
produce an accurate result, although there are landmarks that can be used as an
approximate guide. From 25 weeks of pregnancy, the midwife should commence
serial symphysis fundal height (SFH) measurements. She uses a tape measure
(with the centimetres facing the mother’s abdomen) held at the symphysis pubis
and extended up to the fundus, to take a single measurement. This should be
recorded in the pregnancy record and plotted on a customized chart rather than apopulation-based chart.
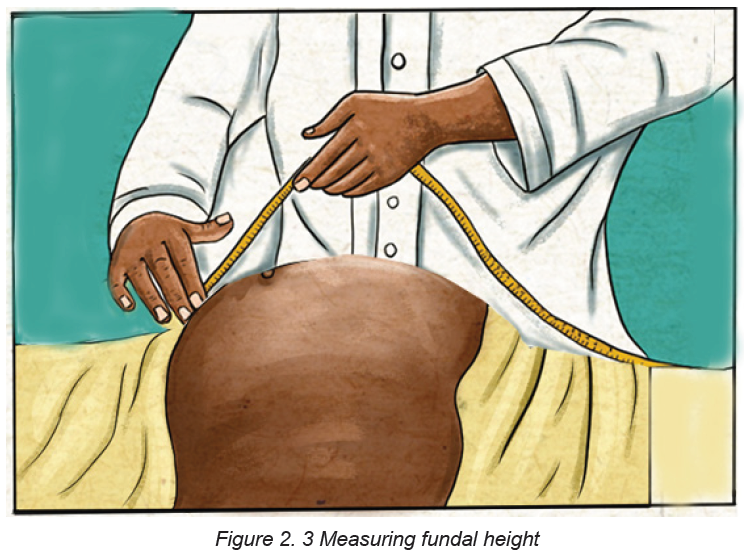
Leopold’s manoeuvers: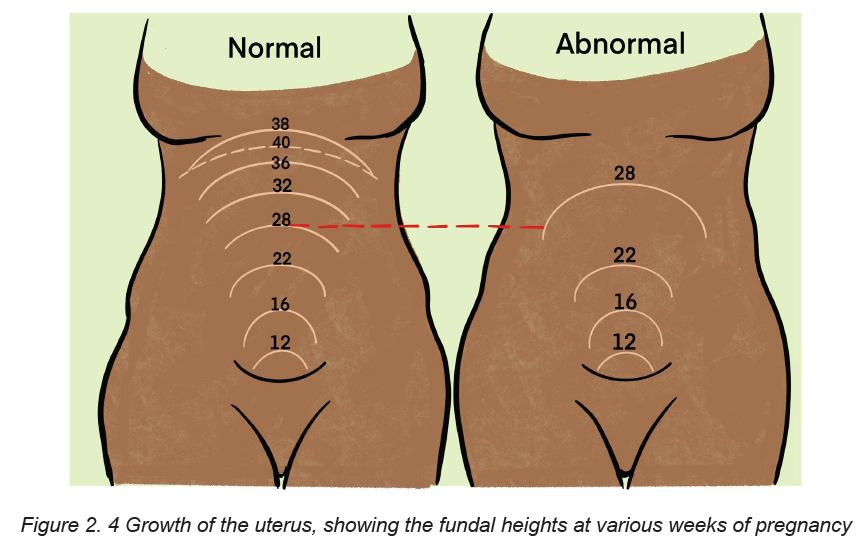
Fundal palpation
This determines the presence of the breech or the head in the fundus. This
information will help to diagnose the lie and presentation of the fetus. Talking through
the palpation with the woman, making eye contact with her during the procedure,
the midwife lays both hands on the sides of the fundus, fingers held close together
and curving round the upper border of the uterus. Gentle yet deliberate pressure is
applied using the palmar surfaces of the fingers to determine the soft consistency
and indefinite outline that denotes the breech. Palms of hands on either side of thefundus, fingers held close together palpate the upper pole of the uterus.
Lateral palpation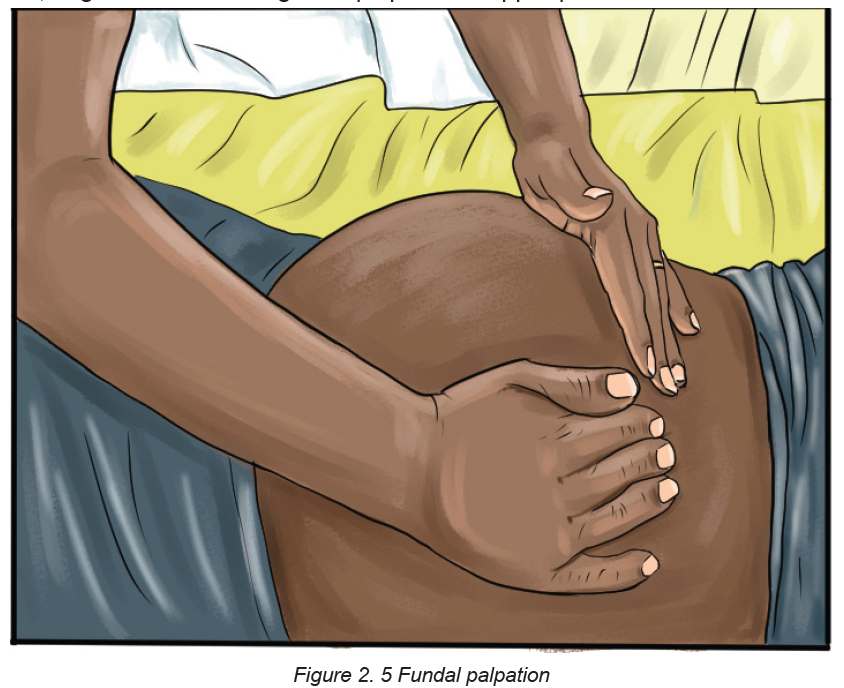
This is used to locate the fetal back in order to determine position. The hands are
placed on either side of the uterus at the level of the umbilicus. Gentle pressure
is applied with alternate hands in order to detect which side of the uterus offers
the greater resistance. More detailed information is obtained by feeling along the
length of each side with the fingers. This can be done by sliding the hands down
the abdomen while feeling the sides of the uterus alternately. Some midwives prefer
to steady the uterus with one hand, and using a rotary movement of the opposite
hand, to map out the back as a continuous smooth resistant mass from the breech
down to the neck; on the other side the same movement reveals the limbs as small
parts that slip about under the examining fingers.
‘Walking’ the fingertips of both hands over the abdomen from one side to the other
is another method of locating the fetal back. Hands placed at umbilical level oneither side of the uterus. Pressure is applied alternately with each hand.
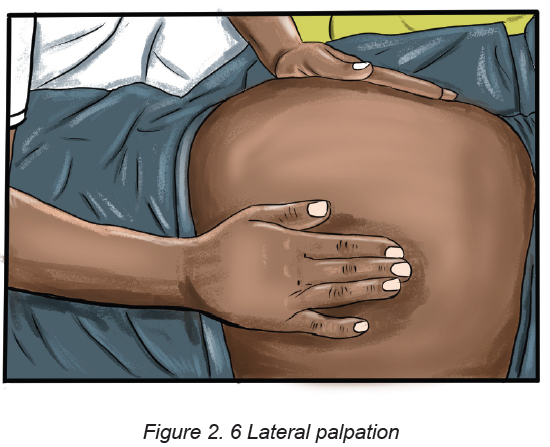
Pelvic palpation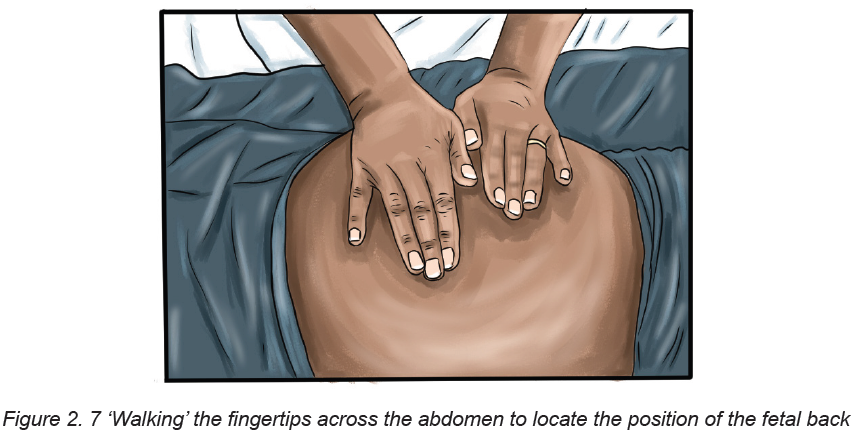
Pelvic palpation will identify the pole of the fetus in the pelvis; it should not cause
discomfort to the woman. This is done only from 36 weeks onwards.
The midwife should ask the woman to bend her knees slightly in order to relax the
abdominal muscles and also suggest that she breathe steadily; relaxation may be
helped if she sighs out slowly. The sides of the uterus just below umbilical level
are grasped snugly between the palms of the hands with the fingers held close
together, and pointing downwards and inwards.
If the head is presenting (towards the lower part of the uterus), a hard mass with a
distinctive round smooth surface will be felt. The midwife should also estimate how
much of the fetal head is palpable above the pelvic brim to determine engagement.
This two-handed technique appears to be the most comfortable for the woman and
gives the most information.
Pawlik’s manoeuvre, where the practitioner grasps the lower pole of the uterus
between her fingers and thumb, which should be spread wide enough apart to
accommodate the fetal head, is sometimes used to judge the size, flexion and
mobility of the head, but undue pressure must not be applied. It should be used only
if absolutely necessary as it can be very uncomfortable for the woman: There is noresearch evidence to support one method over the other.
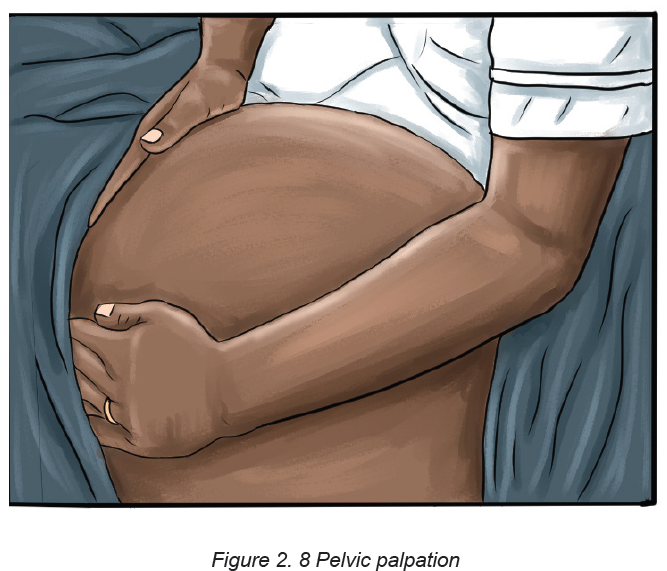
On the figure above, the fingers are directed inwards and downwards.
On the figure above, the lower pole of the uterus is grasped with the right hand, the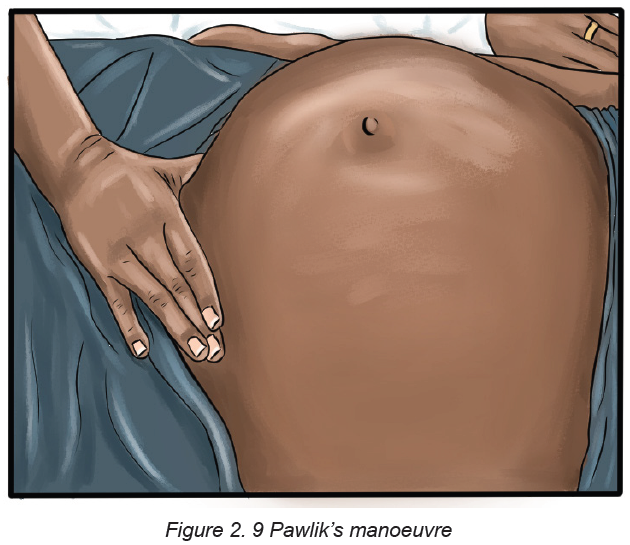
midwife facing the woman’s head.
Engagement
Engagement is said to have occurred when the widest presenting transverse
diameter of the fetal head has passed through the brim of the pelvis. In cephalic
presentations this is the biparietal diameter and in breech presentations the
bitrochanteric diameter. In a primigravid woman, the head normally engages at any
time from about 36 weeks of pregnancy, but in a multipara this may not occur until
after the onset of labour. Engagement of the fetal head is usually measured in fifths
palpable above the pelvic brim.
When the vertex presents and the head is engaged the following will be evident on
clinical examination:
• Only two- to three-fifths of the fetal head is palpable above the pelvic brim
• The head will not be mobile.
On rare occasions, the head is not palpable abdominally because it has descended
deeply into the pelvis. If the head is not engaged, the findings are as follows:
• More than half of the head is palpable above the brim
• The head may be high and freely movable (ballotable) or partly settled in the
pelvic brim and consequently immobile.
In a primigravid woman, it is usual for the head to engage by 37 weeks’ gestation;
however, this is not always the case. When labour starts, the force of labour
contractions encourages flexion and moulding of the fetal head and the relaxed
ligaments of the pelvis allow the joints to give. This is usually sufficient to allow
engagement and descent. Other causes of a non-engaged head at term include:
• Occipitoposterior position
• Full bladder
• Wrongly calculated gestational age
• Polyhydramnios
• Placenta praevia or other space-occupying lesion
• Multiple pregnancy
• Pelvic abnormalities
• Fetal abnormality
Checklist to be used when performing Leopold maneuver
a) Equipment
♦ Tray
♦ Vital signs materials
♦ Weighing and height scale
♦ Table of examination
♦ Pinard fetoscope
♦ Pregnancy wheel
♦ Preventive medication
♦ IEC materials
♦ ANC and Client records
♦ Screening materials (HIV, Syphilis, Albuminuria, Urinalysis, Full blood counts
(FBC)
♦ Gloves (examination gloves and sterile gloves)
♦ Trash can
♦ Dust bin
b) Implementation
♦ Wash and dry hands
♦ Put on examination gloves.
♦ Systematic assessment from head to toe for pregnant woman (inspection,
palpation, auscultation and percussion)
♦ Explain to the woman/client/ couple/ family each step of procedure and
provide feedback
♦ Ask the woman to lie on her back, feet posed on the bed and knees bending
(LEOPOLD MANEUVER)
♦ Assess fundal /uterine height: Use two hands to palpate the top of the uterus,
and then the measurement is taken from the upper border of the symphysis
pubis to the highest point of the fundus of the uterus by using a tape measure.
♦ First Maneuver: Feel the consistency and the mobility of the fetal part lying
in the fundus of the uterus. The fetal head is firm, hard and round, it moves
independently from the fetal body. The breech/buttock is softer and moves at
the same time as the whole fetal body. If fundus is empty suspect transverse
lie (presentation transverse)
♦ Second Maneuver: Determine the lie (presentation): the position of the fetal
back and other small parts of the fetal body). By moving the hands to half
way down the uterus, palpate the abdomen, apply gentle pressure. One hand
palpates, the other hand supports the abdomen. The fetal back, which is
on the side of the abdomen, is a continuous smooth resistant mass during
palpation. The other side of the abdomen, where limbs are felt as small parts,
is embossed or irregular.
♦ Third Maneuver: Place one hand just above the symphysis. Determine which
part of the fetus occupies the lower uterine pole: if the palpated part is the
head or the buttock of the fetus or other, and check/verify if the presentation
is engaged
♦ Change position by turning your back towards the client.
♦ Fourth Maneuver: Two hands are placed to the lower uterine pole and slide
them on the sides of the uterus towards the pubis. Identify a cephalic, a
breech or another presentation. Determine the degree of the engagement of
the presentation
♦ Auscultation of the FHR (see checklist FHR)
♦ This is a separate procedure but it should be done after this procedure
c) COMPLETION
♦ Thank the client for her collaboration and request the client if she has any
concern
♦ Assist the client to maintain a comfortable position.
♦ Clean and dispose used materials and clean the work area.
♦ Wash hand
♦ Provide preventive medications if indicated♦ Document the results of the examination and give appointment.
Presentation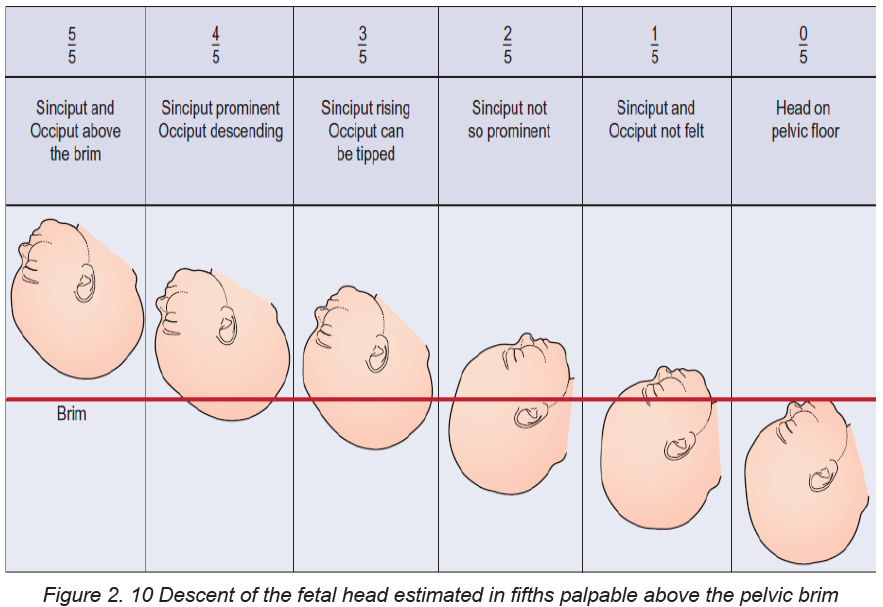
Presentation refers to the part of the fetus that lies at the pelvic brim or in the lower
pole of the uterus. Presentations can be vertex, breech, shoulder, face or brow.
Vertex, face and brow are all head or cephalic presentations. When the head is
flexed the vertex presents; when it is fully extended the face presents; and when it
is partially extended the brow presents.
Auscultation
A Pinard’s fetal stethoscope will enable the midwife to hear the fetal heart directly
and determine that it is fetal and not maternal. The stethoscope is placed on the
mother’s abdomen, at right-angles to it over the fetal back. The ear must be in close,
firm contact with the stethoscope but the hand should not touch it while listening
because then extraneous sounds are produced. The stethoscope should be moved
about until the point of maximum intensity is located where the fetal heart is heard
most clearly. The midwife should count the beats per minute, which should be in the
range of 110–160. The midwife should take the woman’s pulse at the same time aslistening to the fetal heart to enable her to distinguish between the two.
Lie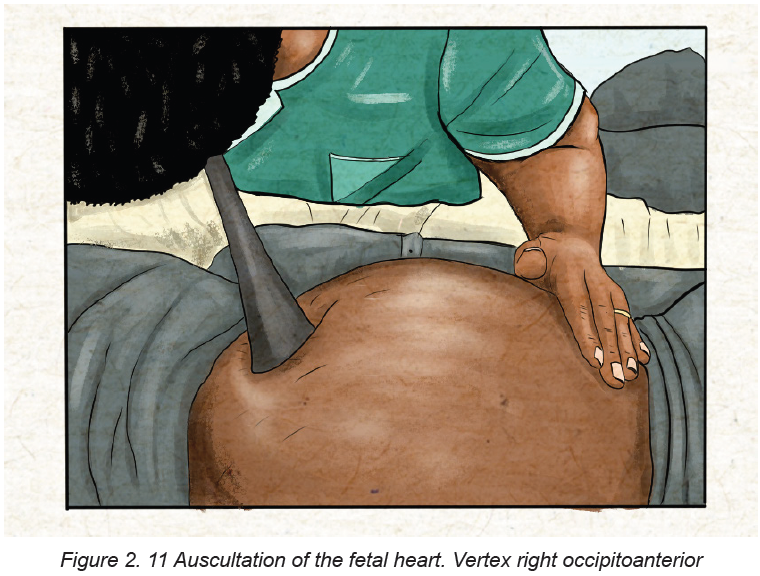
The lie of the fetus is the relationship between the long axis of the fetus and the long
axis of the uterus. In the majority of cases the lie is longitudinal due to the ovoid
shape of the uterus; the remainder are oblique or transverse.
Attitude
Attitude is the relationship of the fetal head and limbs to its trunk. The attitude
should be one of flexion. The fetus is curled up with chin on chest, arms and legs
flexed, forming a snug, compact mass, which utilizes the space in the uterine cavity
most effectively. If the fetal head is flexed the smallest diameters will present and,
with efficient uterine action, labour will be most effective.
Denominator
‘Denominate’ means ‘to give a name to’; the denominator is the name of the part of
the presentation, which is used when referring to fetal position. Each presentation
has a different denominator and these are as follows:
• In the vertex presentation it is the occiput
• In the breech presentation it is the sacrum
• In the face presentation it is the mentum.
Position
The position is the relationship between the denominator of the presentation andsix points on the pelvic brim.
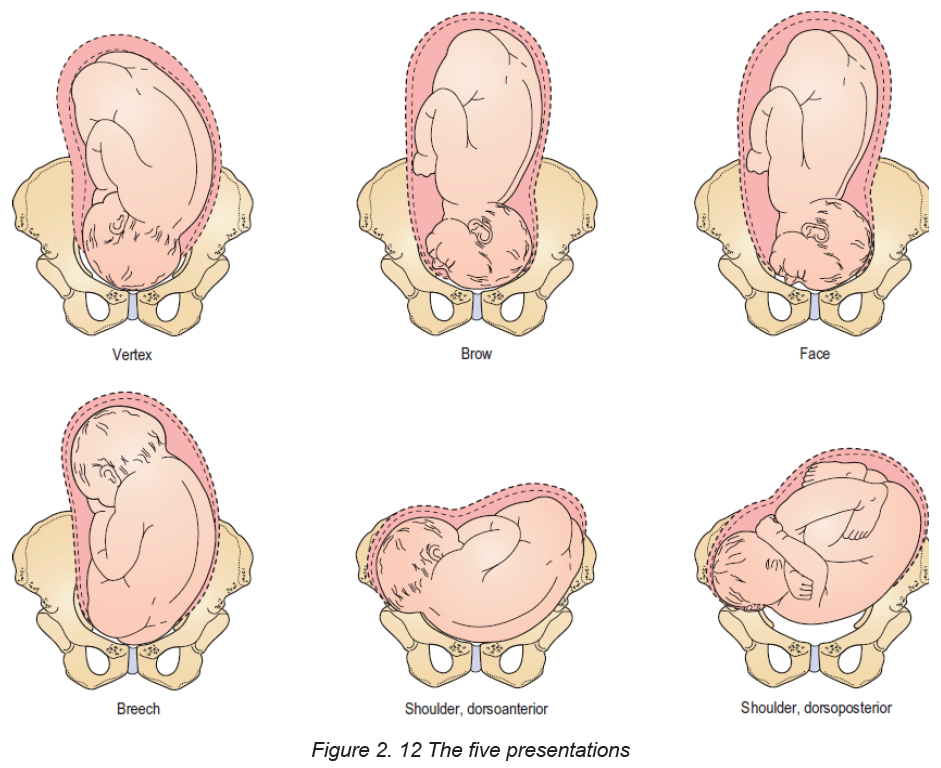
Indicators of maternal wellbeing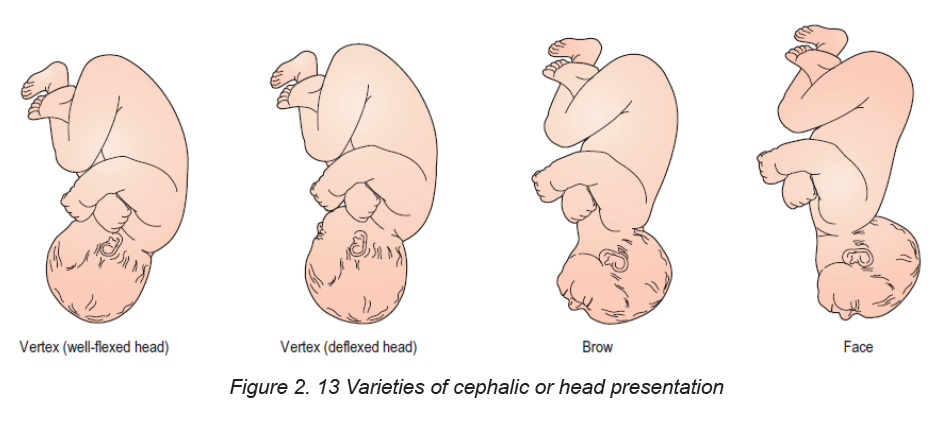
The woman’s general health and wellbeing is observed throughout and the midwife
must remain vigilant for signs of domestic abuse, emotional fragility and social
instability. Endeavouring to maintain continuity of carer will be a key process for
identifying impending problems and for encouraging free exchange of information
between the woman and her midwife.
Indicators of fetal wellbeing
These include:
• Increasing uterine size compatible with the gestational age of the fetus;
• Fetal movements that follow a regular pattern from the time when they are
first felt;
• Fetal heart rate that is regular and variable with a rate between 110 and 160
beats/minute.
Self-assessment 2.6
– Using checklist in the simulation lab, perform Leopold’s manoeuvers on
mannequin
– Practice in simulation lab, on listening to the fetal heart beat using the
pinard’s stethoscope
2.7 Calculation of gestational age based on the last menstruation
period and pregnancy wheel
Learning Activity 2.7
Madam X, aged 28 years, attend the health center for her ANC first contact; she
wanted to know how her baby is and when she will deliver.
– How will you determine the time the woman will deliver her baby?
An accurate menstrual history helps determine the expected date of birth (EDB),
enables the nurse to predict a birth date and subsequently calculate the gestational
age at any point in the pregnancy. This is particularly important for the timing of fetal
anomaly screening and measuring fetal growth. The EDB is calculated by adding
9 calendar months and seven days to the date of the first day of the woman’s last
menstrual period (known as Naegele’s Rule). This method assumes that:
a. The woman takes regular notes of regularity and length of times between
periods
b. Conception occurred 14 days after the first day of the last period, this is true
only if the woman has 28-day cycle
c. The last period of bleeding was true menstruation; implantation of the ovum
may cause slight bleeding
d. Breakthrough bleeding and anovulation can be affected by the contraceptive
pill thus impacting on the accuracy of a Last Menstrual Period (LMP)
The duration of pregnancy based on Naegele’s Rule is 280 days. However, if the
woman has 35-day cycle, then, 7 days should be added; if her cycle is less than 28
days, then the appropriate number of days is subtracted. A definitive EDB will be
given when the woman attends for her dating ultrasound scan at around 12 weeks
of pregnancy.
The EDD is calculated by adding 9 calendar months if the last month of
menstruation is≤ to 3 or moins 3 if month ≥ to 4 and adding 7 days to the date of
the 1st day of the woman’s last menstrual period (LMP) this method assumes that:
• The woman takes regular note of regularity and length of time between periods
• Conception occurred 14 days after the 1st day of the last period; this is true
only if the woman has a regular 28 days cycle.
• The last period of bleeding was true menstruation but implantation of the
ovum may cause slight bleeding.
Example on calculation of EDD
Calculating from “sure” dates by Naegele”s Rule
Cycle of 28days=LMP: 9 June 2014
EDD = 9+7days/6- 3/EDD: 16 March 2015
A pregnancy wheel is used to determine the due date of delivery. Also known as a
gestation calculator, it uses the first day of your last menstrual period to establish
your due date
It combines three things needed to derive all the dates necessary in pregnancy
care, and no other app has this combination. It contains a calendar calculator todetermine EDD (EDC) from LMP or from a sonogram report.
Self-assessment 2.7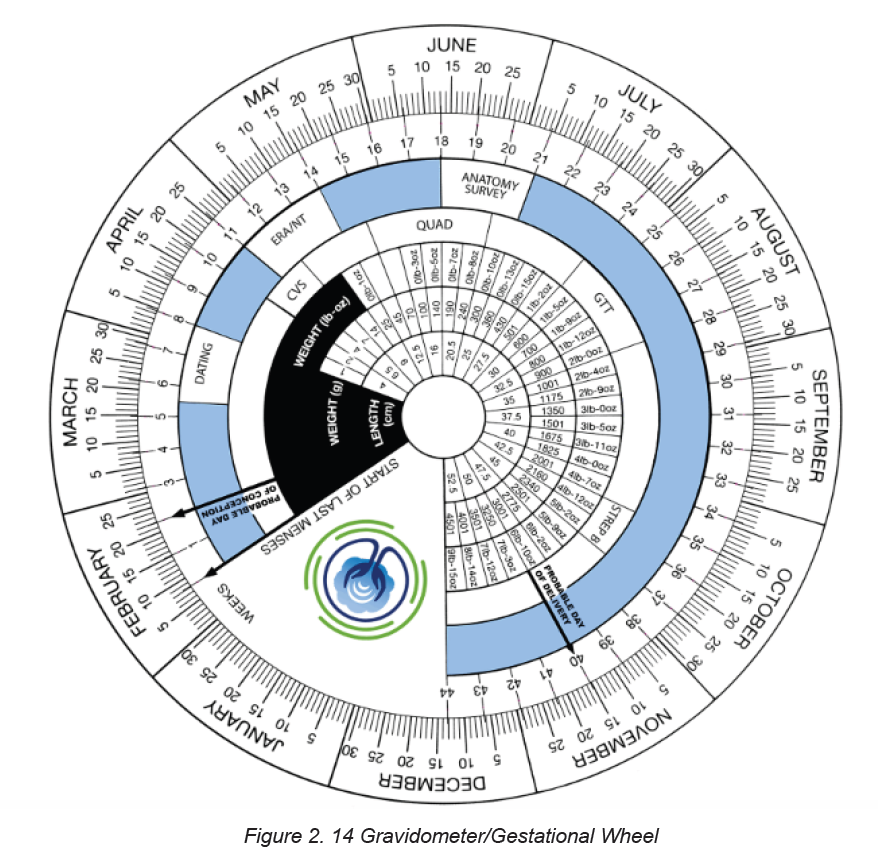
Calculate the EDD of a pregnant woman whose last menstrual period (LMP) was
on 14th December 2020.
2.8 Physiological changes during pregnancy: Changes in the
female reproductive system during pregnancy
Learning Activity 2.8
– What happens with menstruation to a pregnant woman?
Changes in the body during pregnancy are most obvious in the organs of the
reproductive system.
Uterus
When a woman becomes pregnant, the part of her body affected first and the part
that undergoes the most significant changes is the uterus. It increases to 20 times
its original weight, and 1,000 times its initial capacity. The amount of its muscle,
connective and elastic tissue, blood vessels, and nerves increases.
The cervix and vagina
Other parts of the reproductive system change along with the uterus. The cervix
and vagina have an increased blood supply, which causes a darkening in color
apparent by the sixth week.
Ovaries
The ovaries cease to ovulate. The follicle-stimulating hormone (FSH) ceases its
activity due to the increased levels of estrogen and progesterone secreted by the
ovaries and corpus luteum. The FSH prevents ovulation and menstruation.
Breasts
Breasts must undergo many changes during pregnancy to produce milk. In the first
two months of pregnancy, breasts may feel sore or full. They enlarge, and veins
may become visible. The nipples also increase in size and usually darken. By midpregnancy,
colostrum (a thick, yellowish fluid) can be expressed, but milk is not
produced until after delivery.
Self-assessment 2.8
What are the physiological changes on the breast during pregnancy?
2.9 Physiological changes in pregnancy on endocrine system
Learning Activity 2.9
– Describe 3 hormones involved in reproductive system based on your
knowledge from S3 biology?
The female endocrine system consists of the pituitary, the thyroid, the adrenal and
the thymus glands, along with the pancreas and the ovaries. All of them undergo
changes during pregnancy in order to prepare the mother’s body to effectively meet
the challenges associated with pregnancy, childbirth and breastfeeding. Some of
the most significant changes occur in the pituitary and thyroid glands to meet the
nutritional needs of the baby in the uterus, restricting reproductive organs andpassing on genetic information.
Main female reproductive hormones and their
functions in preparing the uterus for pregnancy.
Estrogens and progesterone are the chief hormones throughout pregnancy.
Oestrogens
A woman will produce more estrogens during one pregnancy than throughout her
entire life when not pregnant. During pregnancy, estrogen promotes maternal blood
flow within the uterus and the placenta.
Progesterone
A pregnant woman’s progesterone levels are also very high. Among other effects,
high levels of progesterone cause some internal structures to increase in size,
including the uterus, enabling it to accommodate a full-term baby. Levels of
progesterone and estrogens rise continually throughout pregnancy, suppressing
the hypothalamic axis and subsequently the menstrual cycle. Estrogen is mainly
produced by the placenta and is associated with fetal well–being.
HCG
Women also experience increased human chorionic gonadotropin (β-hCG); which
is produced by the placenta. This maintains progesterone production by the corpus
luteum. The increased progesterone production, first by corpus luteum and later by
the placenta, mainly functions to relax smooth muscle.
Prolactin
Prolactin levels increase due to maternal pituitary gland enlargement by 50%.
This mediates a change in the structure of the mammary gland from ductal to
lobular-alveolar.
Parathyroid hormone
Parathyroid hormone is increased which leads to increases of calcium uptake in
the gut and re-absorption by the kidney. Adrenal hormones such as cortisol and
aldosterone also increase.
HPL
Human placental lactogen (HPL) is produced by the placenta and stimulates
lipolysis and fatty acid metabolism by the woman, conserving blood glucose for
use by the fetus. It can also decrease maternal tissue sensitivity to insulin, resulting
in gestational diabetes.There are some experiences in life of a woman that cause
similar conditions like those in pregnancy, therefore correct diagnosis is very
important.
Self-assessment 2.9
– Describe two hormones that help to maintain pregnancy.
2.10 Changes in the cardiovascular and respiratory systems
Learning Activity 2.10– What is the role the heart in human being?
Changes in the cardiovascular system
During pregnancy profound but predominantly reversible changes occur in
maternal haemodynamics and cardiac function. These complex adaptations
are necessary to:
• Meet evolving maternal changes in physiological function
• Promote the growth and development of the uteroplacental–fetal unit
• Compensate for blood loss at the end of labour.
Table 2. 4 A summary of the key components of
the cardiovascular system and adaptations inpregnancy
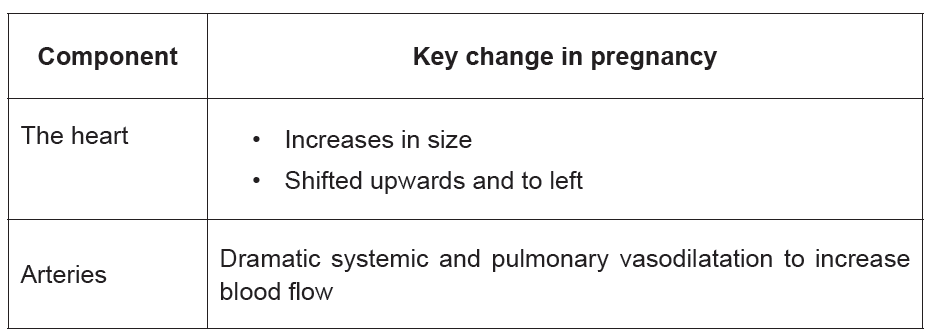
Changes in the respiratory system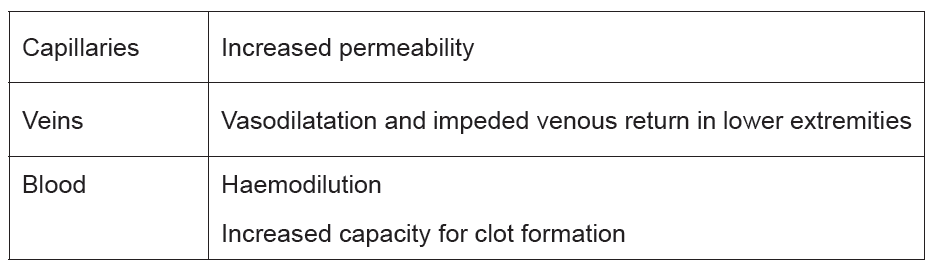
To accommodate increased oxygen requirements and the physical impact of the
enlarging uterus intricate changes occur in respiratory physiology.
•Breathlessness
The respiratory changes can be extremely uncomfortable and may lead to dyspnoea,
dizziness and altered exercise tolerance. Up to 75% of pregnant women with no
underlying pre-existing respiratory disease experience some dyspnoea, possibly
due to an increased awareness of the physiological hyperventilation.
Self-assessment 2.10
How does pregnancy affect the heart?
2.11 Changes in the urinary and Gastro-intestinal system
Learning Activity 2.11
A pregnant woman of 32 weeks visited your antenatal care facility complaining
of not sleeping at night and urinate all the time. She is worried and want you to
help her with this problem.
1. What advice can you give to her?
2. Describe the reason why you think she is having this problem.
The striking anatomical and physiological changes occurring in the urinary system
are critical for an optimal pregnancy outcome. Systemic vasodilatation in the first
trimester and an increase in blood volume and cardiac output results in a massivevasodilatation of the renal circulation that increases the renal plasma flow.
Gastrointestinal system changes:
Anatomical and physiological changes take place in each organ of the gastrointestinal
system. Influenced by oestrogen and progesterone.
Anatomical and physiological changes take place in each organ of the gastrointestinal
system. Influenced by oestrogen and progesterone.
♦ Ptyalism
Ptyalism is the excessive production of saliva throughout pregnancy. Ptyalism
causes a bad taste in the mouth and women complain that swallowing the excessive
or thickened saliva perpetuates a sense of nausea and that they need to spit it out.
♦ Nausea and vomiting
Nausea and vomiting (morning sickness) has varying levels of severity and has farreaching
effects for some women in terms of ability to carry out day-to-day tasks,
care for children and take part in full-time employment.
Symptoms usually begin in the 4th week of pregnancy with a marked increase
between 5 and 10 weeks when hCG levels are at their highest, followed by a steady
decline until 20 weeks.
♦ Pica
Pica is the persistent craving and compulsive consumption of substances such as
ice, clay, soap, coal or starch.
♦ Heartburn
Troublesome symptoms of retrosternal and epigastric pain, regurgitation and acid
taste in the mouth can all affect the woman’s quality of life. Increasing gestational
age, heartburn before pregnancy and multiparity may also predispose women to
gastrooesophageal reflux in pregnancy which usually resolves after the birth of the
baby.
Management
• Skip foods and drinks that can make it worse, such as citrus; spicy, fatty
(especially fried or greasy) foods; caffeine; and carbonated drinks.
• Eat several small meals throughout the day.
• Take your time when eating.
• Drink liquids between — not during — meals.
♦ Abdominal distension
Abdominal distension and a bloated feeling occur when nutrients and fluids remain
in the intestinal tract for longer, particularly in the third trimester due to the prolonged
transit time
♦ Constipation and hemorrhoids
Hemorrhoids are varicosities of the anal and perianal venous plexus. They are
caused by the rise in intra-abdominal pressure and restriction of venous return in
the lower extremities and pelvis.
♦ Maternal weight
A variety of components contribute to weight gain during pregnancy.
These includes:
Fetus 27%, the placenta, amniotic fluid and uterus 20%, Breasts 3%, blood volume
and extravascular fluid 23%, and maternal fat stores 27%. Most weight is gained in
the second and third trimesters at rates of 0.45 kg and 0.40 kg per week respectively.Table 2. 5 Distribution of average increase in weight
Self-assessment 2.11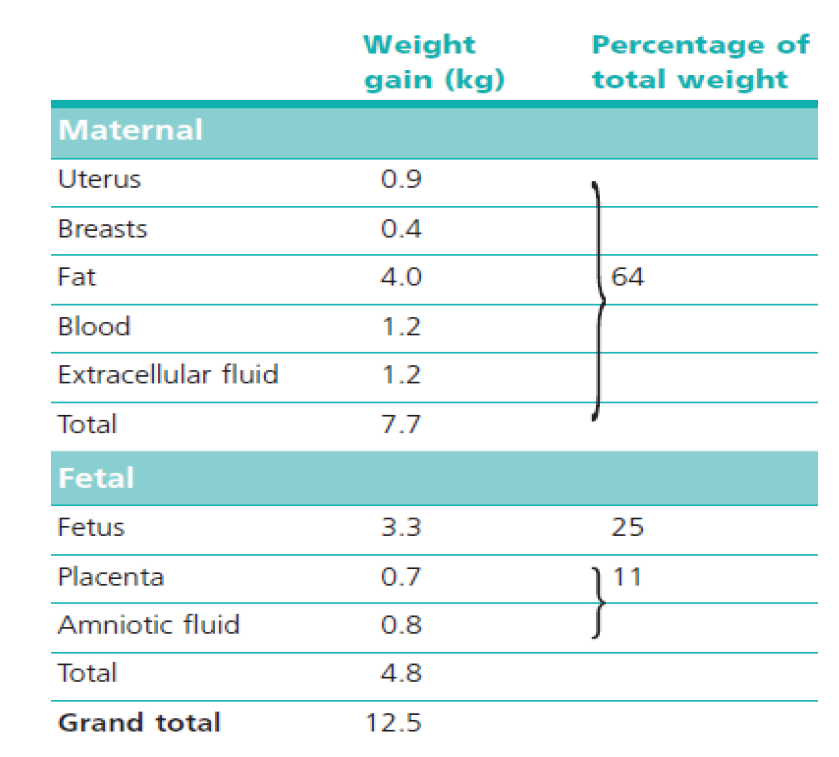
What contributes to weight gain during pregnancy?
Discuss Heart burns and how it can be managed.
2.12 The basic laboratory investigations during antenatal care
Learning Activity 2.12
– Which test can you request to a couple who visited the hospital and
complained that the wife has not seen her monthly period?
This is a process of identifying pregnant women who may be at an increased risk
of a disease or condition, they can then be offered information, further tests and
appropriate treatment to reduce their risk and/or any complications arising from the
pregnancy.
Screening of a mother and baby is now a major part of care for all pregnancies. The
underlying principles of screening are that the condition being screened for must be
important and well understood (i.e. something that makes a difference to health and
wellbeing and does more good than harm).
a) CLINICAL URINE TEST
Results of a clinical urine test can vary depending on the medical facility that you
visit. However, you can usually expect your results within a week of taking the test
b) BLOOD TEST
A laboratory tests of blood to detect human chorionic gonadotropin level (HCG).
There are two types of pregnancy blood tests:
Qualitative HCG blood test: This test checks to see whether any HCG is being
produced in the body. It gives a simple yes or no answer as to whether woman is
pregnant.
Quantitative HCG blood test: This test measures the specific level of HCG in the
blood. Quantitative HCG blood tests are very accurate because they measure the
exact amount of HCG in the blood. They can detect smaller amounts of the hormone
than a qualitative HCG blood test or a urine test.
Blood tests can detect HCG earlier than urine tests.
Progesterone test
♦ Progesterone is given to women with amenorrhea.
♦ If she is pregnant, no bleeding will follow, otherwise, bleeding should occur
within 7-10 days of progesterone administration.
♦ This is reliable in the non-pregnant patient only if there is adequate estrogenstimulation of the endometrium
Self-assessment activity 2.12
– Explain the most accurate test done to confirm pregnancy
2.13 Common laboratory investigations to rule out medical
conditions during antenatal care.
Learning Activity 2.13
– Why is it important to rule out sexual transmitted diseases in pregnant
women?
First antenatal screens usually include Complete blood count, Blood group and
antibody screen, rubella antibody status, syphilis serology, Hepatitis B serology and
HIV abs testing.
The most important test in the second antenatal testing screen is gestational
diabetes screening and protein detection in urine to rule out preeclampsia.
Complete blood count
Anemia is one of the commonest complications of pregnancy. The most common
reason for iron deficiency anemia in pregnancy is the increased demands of the
fetus for iron. Anemia in pregnancy is defined as Hb < 11 g/dL (severe anemia as
Hb < 7 g/dL) at any gestational age.
Anemia is generally defined as hemoglobin level less than 11g/dl or specifically:
♦ HB <11g/dL in 1st trimester
♦ HB <10.5g/dL in 2nd trimester
♦ HB <11g/dL in 3rd trimester
Blood group and antibody screen
Identifying ABO blood group, rhesus D status and red cell antibodies in pregnant
women is important to prevent “haemolytic disease of the new-born” in subsequent
pregnancies. If the foetus is rhesus D-positive (and the mother is negative),
the mother may form anti-D antibodies, which may affect a subsequent rhesusD-positive foetus. Haemolytic disease of the new-born in subsequent pregnancies.
Rubella antibody status
All pregnant women should be screened for rubella antibodies. Congenital Rubella
Syndrome occurs when the rubella virus infects the developing foetus, especially
during the first trimester when up to 90% of affected infants will be born with a birth
defect, e.g. deafness, eye defects, heart defects, mental retardation.
Syphilis serology
All pregnant women should be screened for syphilis, mothers infected with syphilis
can experience long-term morbidity and the complications for pregnancy are
significant. Treponema Elisa Screen assay is used to screen for syphilis as this can
detect primary or secondary infection.
Hepatitis B serology
Transmission of the hepatitis B virus from mother to infant can be prevented by
administration of the hepatitis B vaccine and immunoglobulin to the infant at birth,
therefore screening is important.
HIV screening
All pregnant women should be screened for HIV. Women who are HIV positive can
be given treatment to reduce the risk of HIV being transmitted to their infant (risk
reduced from 32% to less than 1%).
Screening for gestational diabetes
Gestational diabetes affects 5–8% of pregnant, it is recommended that testing for
gestational diabetes occurs for all women between 26 and 28 weeks of gestation.
Screening for Group B streptococcus
Group B streptococcal (GBS) infection is a significant cause of serious neonatal
infection. Women may have a vaginorectal culture collected at 35 to 37 weeks’
gestation to prevent this infection.
Malaria
All women with malaria symptoms will receive early detection and management of
malaria. During antenatal care, the health facility staff must do the following to the
pregnant woman:
• Give her a long-lasting insecticide treated mosquito net;
• Rapid Diagnostic Tests (RDT) in case of signs and symptoms.
Additional testing in pregnancy
Testing for chlamydia and gonorrhoea should be considered for those who may be
at increased risk based on age (e.g. less than 25 years) and sexual history.
Vitamin D
It is required for normal bone growth development in the fetus. Mothers with known
vitamin D deficiency or at risk for deficiency (e.g. dark-skinned women, women whowear a veil) should receive vitamin D supplementation.
Self-assessment 2.13
– Discuss some laboratory investigations you know that can be done in
pregnancy based on your knowledge and understanding from biology in
S3
2.14 Danger signs of pregnancy
Learning Activity 2.14
In a community work “umuganda”, they were discussing about maternal health,
and chief of village identifies you as a scientist and asked to explain to those
pregnant women the bad signs that may show on pregnancy.
Every woman needs to be aware of the danger signs that occur during pregnancy,
as complications can be unpredictable. These danger signs usually indicate the
presence of an obstetric complication that may arise during pregnancy, delivery or
post-delivery. Knowledge of these danger signs will help women and the nurse to
make the right decisions and take appropriate healthcare seeking actions
These danger signs include:
♦ Vaginal bleeding
♦ Sudden gush of fluid or leaking of fluid from vagina
♦ Severe headache not relieved by simple analgesics (e.g. paracetamol)
♦ Dizziness and blurring of vision
♦ Sustained vomiting
♦ Swelling (hands, face, etc.)
♦ Decrease or Loss of fetal movements
♦ Convulsions
♦ Premature onset of contractions (before 37 weeks)
♦ Severe or unusual abdominal pain,
♦ Chills or fever
If a patient should develop any of the above signs during pregnancy the nurse mustquickly refer the patient for expert management.
Self-assessment 2.14
– What will the knowledge of the danger signs of pregnancy help the nurse
to achieve in the care pathway for the woman?
2.15 Management of minor pregnancy complications
Learning Activity 2.15
Based on what you have learnt; what problems do you think a pregnant woman
can have?
Early morning sickness
Around half to two-thirds of all pregnant women will experience morning sickness.
Possible causes include high levels of hormones, blood pressure fluctuations and
changes in carbohydrate metabolism. Severe morning sickness, called hyperemesis
gravidarum, may require hospitalisation. Symptoms of morning sickness may be
relieved by eating a few dry crackers before you get up in the morning, avoiding
foods and smells that make you nauseous, drinking plenty of fluids and choosing
high-carbohydrate and high-protein foods.
Pregnant women should be informed that symptoms of nausea and vomiting
usually resolve in the second half of pregnancy. Ginger, chamomile, and vitamin B6
are recommended for the relief of nausea in early pregnancy, based on woman’s
preferences and available options.
Pregnant women with persistent vomiting or with severe symptoms and signs of
dehydration, reduced urine output, and dark-colored urine should be referred to
hospital level.
Tetanus
Tetanus is an acute disease caused by an exotoxin produced by Clostridium tetani.
Neonatal infection usually occurs through the exposure of the unhealed umbilical
cord stump to tetanus spores, which are universally present in soil, and newborns
need to have received maternal antibodies via the placenta to be protected at birth.
Neonatal disease usually presents within the first two weeks of life and involves
generalized rigidity and painful muscle spasms, which in the absence of medical
treatment leads to death in most cases. Global vaccination programs have reducedthe global burden of neonatal tetanus deaths and continue to do so.
In Rwanda, 34% of women who had a live birth received two or more doses of antitetanus
vaccine during their most recent pregnancy. This figure has not changed
since 2010. Considering mothers who had previous protection against tetanus, the
proportion protected against tetanus rises to 82 percent, an increase from 79 percent
in 2010. This means that 18 percent of pregnant women were not protected against
tetanus. Because tetanus spores are ubiquitous in the environment, eradication is
not biologically feasible and high immunization coverage remains essential.
Table 2. 6 Schedule for Tetanus Toxoidadministration
If Hb < 7 g/dL, especially if symptomatic, then blood transfusion. Transfuse rapidly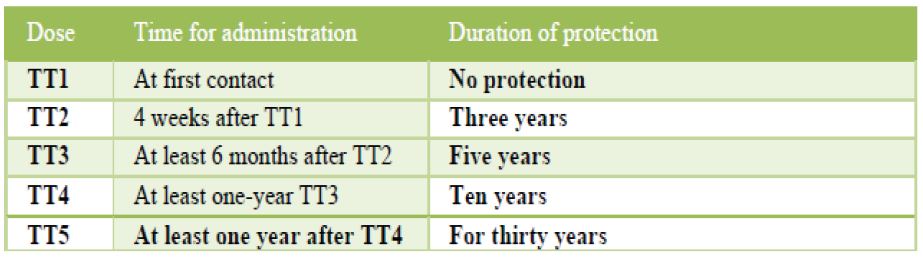
in anaemia due to acute blood loss.
Transfuse slowly if chronic anaemia (Consider use of diuretics like Lasix 20-
40mg stat as necessary to reduce risk of congestive cardiac failure due to sudden
circulatory overload).
♦ IF Hb is <7 and asymptomatic manage according to clinician judgement treat
the cause + Fe supplement
♦ If Hb < 8 g/dL, treat as per FBC results
• If MCV < 80, then send blood for iron studies (ferritin, TIBC and %
saturation (% sat) if available.
• If MCV 80-93, then send blood for peripheral smear and consult
hematologist
• If MCV ≥ 94, then treat for folate or vitamin B12 deficiency
♦ If Hb > 8 g/dL, then treat with folate and FeSO4 325 mg PO BD and recheck
Hb in 2-4 weeks
♦ Treat with Albendazole
♦ Treat for malaria or schistosomiasis if indicated
♦ Mixed anemia may occur and complicate laboratory findings
♦ If iron deficiency, then treat with elemental iron 200 mg PO OD. Titrate up to
reduce side effects and encourage compliance. Take iron on empty stomach
with vitamin C and without antacids.
♦ If folate deficiency, then treat with folate 1 mg PO OD.
♦ If vitamin B12 deficiency, then treat with vitamin B12 1000 mg IM monthly.
♦ If hemolytic anemia, then send blood for direct and indirect Coombs tests.
♦ Treat with corticosteroids. Of note, drug-induced (i.e. methyldopa, penicillin,
cephalosporin) hemolytic anemia is typically milder and is treated by stopping
the offending medication.
Leg cramps
Non-pharmacological treatment options like muscle stretching, dorsiflexion,
relaxation, heat therapy, massage can be used for the relief of leg cramps in
pregnancy, based on a woman’s preferences and available options.
In addition to multivitamin, Magnesium and calcium supplementation can also be
prescribed according to the woman preferences and options.
Low back and pelvic pain
Regular exercise throughout pregnancy is recommended to prevent low back and
pelvic pain. There are a several number of different treatment options, such as
physiotherapy and support belts based on a woman’s preferences and availability.
Refer to hospital level if exercise does not improve symptoms.
Varicose veins and edema
Non-pharmacological options, such as compression stockings and leg elevation
can be used for the management of varicose veins and edema in pregnancy, based
on a woman’s preferences and available options. Refer to hospital level if symptoms
are severe.
Self-assessment 2.15
A 22 years old pregnant woman at 34 weeks of pregnancy tells you that she
craves to eat clay soil. She also tells you that she has developed darker brown
patches on her face, and that her feet and ankles swell up during the day.
1. Identify the minor disorders of pregnancy this woman is displaying, using
their medical names.
2. What advices should you give her to manage her symptoms?
2.16 Anemia in pregnancy
Learning Activity 2.16
Mrs. A. aged 23 is a married pregnant female student who lives in the campus
as she is studying at the University.
She is not able to eat the food from the university restaurant and she is having a
lot of nausea and sometimes vomiting. Her gestational age is 28 weeks. Today
she comes for consultation and complaining of dizziness, tiredness and not able
to stand for long time.
What problem do you think she maybe having?
Anemia results from a lack of red blood cells or dysfunctional red blood cells in the
body. This leads to reduced oxygen flow to the body’s organs.
A serum ferritin concentration <30 μg/L together with an Hb concentration <11 g/dL
during the 1st trimester, <10.5 g/dL during the 2nd trimester, and <11 g/dL during
the 3rd trimester are diagnostic for anemia during pregnancy.
How does iron deficiency anemia during pregnancy affect the baby? Severe anemia
during pregnancy increases your risk of premature birth, having a low birth weight
baby and postpartum depression. Some studies also show an increased risk of
infant death immediately before or after birth.
Types of Anemia during Pregnancy
Iron-deficiency anemia. This type of anemia occurs when the body doesn’t have
enough iron to produce adequate amounts of hemoglobin. That’s a protein in red
blood cells. It carries oxygen from the lungs to the rest of the body.
Types of anemia during pregnancy:
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues
throughout the body.
♦ Iron deficiency is the most common cause of anemia in pregnancy.
♦ Folate-deficiency anemia. Folate deficiency can directly contribute to certain
types of birth defects, such as neural tube abnormalities (spina bifida) and
low birth weight.
♦ Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red
blood cells.
♦ Blood loss during and after delivery can also cause anemia.
RISK FACTORS
♦ Are pregnant with multiples (more than one child)
♦ Have had two pregnancies close together
♦ Vomit a lot because of morning sickness
♦ Are a pregnant teenager
♦ Don’t eat enough foods that are rich in iron
♦ Had anemia before you became pregnant
Symptoms of Anemia during Pregnancy
♦ Pale skin, lips, and nails
♦ Feeling tired or weak
♦ Dizziness
♦ Shortness of breath
♦ Rapid heartbeat
♦ Trouble concentrating
Preventing Anemia
To prevent anemia in pregnancy, encourage pregnant women to consume food like:
♦ lean red meat, poultry, and fish
♦ leafy, dark green vegetables (such as spinach, broccoli, and kale)
♦ iron-enriched cereals and grains
♦ beans, lentils, and tofu
♦ nuts and seeds
♦ eggs
Foods that are high in vitamin C and iron. These include:
♦ citrus fruits and juices
♦ strawberries
♦ kiwis
♦ tomatoes
♦ bell peppers
♦ leafy green vegetables
♦ citrus fruits and juices
♦ dried beans♦ breads and cereals fortified with folic acid
Self-assessment 2.16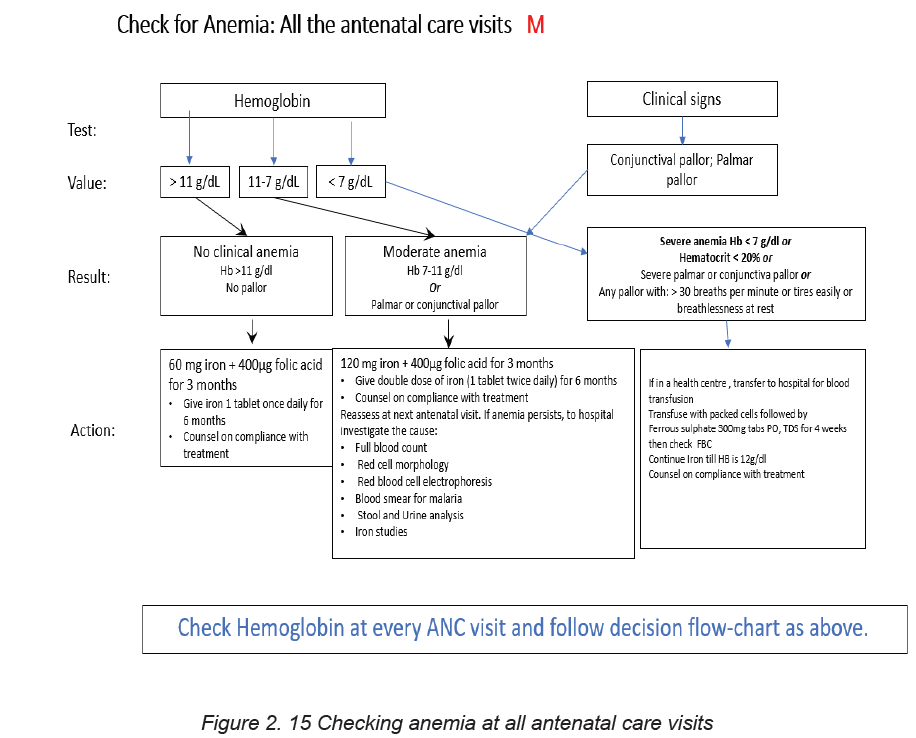
– How does iron deficiency anemia affect the fetus during pregnancy?
2.17 Nutrition during pregnancy
Learning Activity 2.17
In village, pregnant women and other families with under five years’ children
were being taught the importance of kitchen garden (“akarima k’igikoni”), and
you were asked to talk about what the pregnant need to eat to be healthy.
– Describe a balanced diet and its benefits to human body.
To maintain a healthy pregnancy, approximately 300 extra calories are needed each
day. These calories should come from a balanced diet of protein, fruits, vegetables
and whole grains. Sweets and fats should be kept to a minimum. A healthy, wellbalanced
diet can also help to reduce some pregnancy symptoms, such as nausea
and constipation.
Key messages on nutrition for a positive pregnancy:
♦ All pregnant women should be counseled on healthy eating for a positive
pregnancy at each ANC visit. These messages should be reinforced by the
CHWs during home visits;
♦ Pregnant women should receive 3 meals and at least one additional snack
using diverse food types to improve the quality and micronutrient intake;
♦ Pregnant women should avoid coffee, energy drinks, Coca-Cola, alcohol,
fatty foods, raw or undercooked meats in pregnancy;
♦ Pregnant women who are obviously malnourished need special attention,
counselling and advice from a trained nutritionist or a trained health care
provider;
♦ Adolescent girls who are pregnant have their own need for growth and
additional needs for fetus growth. Adolescent girls who become pregnant
needs very special care with at least 3 meals and 2 snacks daily, using a
variety of foods including animal source foods in every meal.
Education for appropriate infant feeding:
Health providers should discuss the importance and management of breastfeeding
with all pregnant women and their families. All pregnant women must have basic
information about breastfeeding, in order to make informed decisions.
Where facilities provide antenatal care, pregnant women and their families should
be counselled about the benefits and management of breastfeeding.
The health facility could organize classes with practical sessions on breastfeeding
and how to overcome breastfeeding difficulties.
The message given during antenatal discussion, group’s education and
communication materials should include at a minimum:
• Importance of breastfeeding;
• Exclusive breastfeeding for the first 6 months, the risks of giving formula or
other breast-milk
• Substitutes, and the fact that breastfeeding continues to be important after 6
months;
• Importance of immediate and sustained skin to-skin contact;
• Importance of early initiation of breastfeeding within one hour after birth;
• Importance of rooming-in;
• Basics of good positioning and attachment;
• Recognition of feeding cues;
• Importance of starting to give other foods at 6 months of age;
• Importance of gradually introducing a variety of foods from 6 months to one
year;
• Importance of continuing to breastfeed the child up to 24 months;
If the mother’s HIV test is positive, she should receive ARTs and be counselled and
supported for infant feeding; the mother can breastfeed like for other infants, except
that breastfeeding should gradually be interrupted at 18 months.
Micronutrient supplementation during pregnancy:
During pregnancy, women have additional needs in all nutrients and micronutrients.
For some micronutrients such as iron, folic acid and calcium, the needs are difficult
to be covered by food intake alone and micronutrients supplements are needed.
a. Iron and folic acid supplementation:
Pregnant women should be prescribed a daily dose of oral iron (60mg) and folic
acid supplementation (400μg =0.4 mg) during the whole course of pregnancy to
prevent maternal anemia, puerperal sepsis, low birth weight, and preterm birth.
b. Calcium supplementation:
Given the insufficient intake of calcium in women in Rwanda, pregnant women
should receive a daily calcium supplementation (1.5–2.0 g oral elemental calcium)
to reduce the risk of pre-eclampsia.
Dividing the dose of calcium may improve acceptability. The suggested scheme
for calcium supplementation is 1.5–2 g daily, with the total dose divided into three
doses, preferably taken at mealtimes.
Calcium supplementation is recommended to woman with high risks to develop
pre-eclampsia during pregnancy:
• Primigravidae, teenagers and elderly primigravidae.
• Women of age 35 years and above.
• Previous pregnancy complicated by pre-eclampsia.
• Previous abruptio placentae or intra-uterine death.
• Multiple pregnancies.
• Medical complications such as chronic hypertension, renal disorders,diabetes, connective tissue disorders or antiphospholipid syndrome
Self-assessment 2.17
– Differentiate micro nutrients from macro nutrients
End unit assessment 2
1. What is focused FANC?
2. Differentiate the terms: Health promotion and health education
3. Describe the components of focused ANC
4. Using a table, show the new model of eight contacts in FANC5. List the issue that may confuse the diagnosis of an early pregnancy
UNIT 3 LABOUR MONITORING
Key Unit competence: Monitor adequately a woman in labour
Introductory activity 3By looking at the following picture A and B, respond to the questions below:
1. Describe the situation on the above pictures.
2. What are the signs that characterize the mother’s situation on both pictures
A and B.
3. What should be the elements to assess on a pregnant woman?
4. According to the picture above explain how patient’s rights are respected.
3.1. Concepts of normal labour
Learning Activity 3.1
Using different source of information (internet, libraries) search for the meaning
of the following terms and be prepared for class presentation
1. Labour
2. Uterine contractions
3. Cervical effacement
4. Cervical dilatation
5. engagement
6. Descent
7. Stations
During the last weeks of pregnancy, a woman and her fetus prepares for the labour
process. This process is considered as normal at 40 weeks (- or + 2 weeks). The
pregnant woman undergoes the various physiological changes and adaptations
during pregnancy that prepares her for childbirth and later along motherhood. The
term labor refers to the process of moving the fetus, placenta, and membranes
out of the uterus and through the birth canal. The labour process occurs with the
presence of uterine contractions which are forceful and very painful motion of the
uterus resulting in tightening and shortening of the uterine muscles.
The presence of uterine contractions also facilitates the cervical effacement which
refers to the softening, thinning and shortening of the cervical canal. In primigravida,
the cervical effacement occurs before the cervical dilatation referring to the increase
in diameter of the cervical opening. Contrary to prim gravida, these two processesoccur simultaneously among multigravida women
The fetus begun to enter the maternal pelvis and when then largest transverse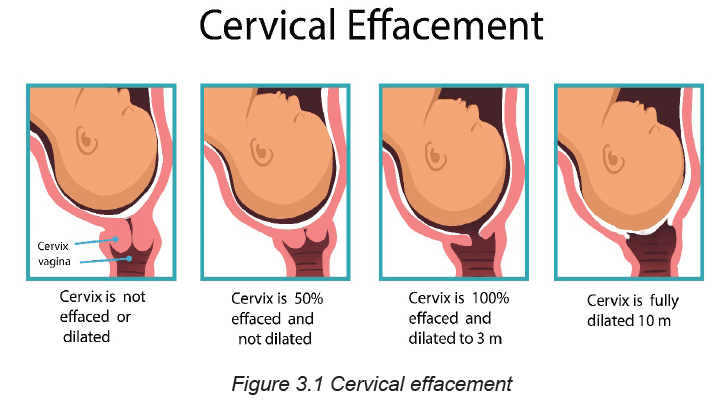
diameter of the presenting part (usually biparietal diameter in case of Cephalic
presentation or bitrochanteric diameter in breech presentation) has passed
though the maternal pelvic brim or inlet into the true pelvis this process is named
engagement. When the fetus is engaged, the presenting part continues to progress
through the pelvis (Descent). The descent of the fetus and its relationship to thelevel of ischial spines is evaluated and reported as stations.
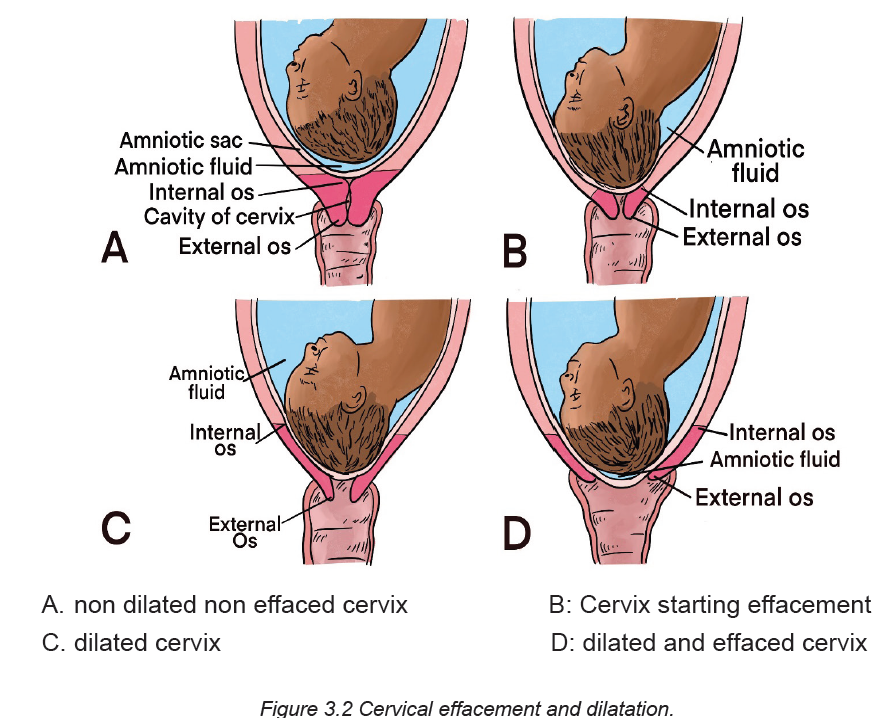
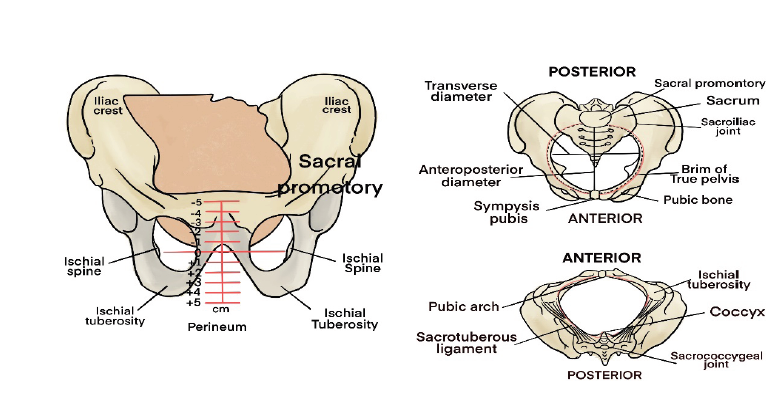
Self-assessment 3.1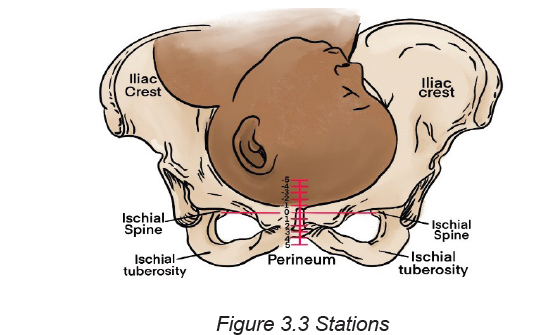
1. Define labour and uterine contractions.
2. Differentiate cervical dilatation from cervical effacement.
3.2. Signs preceding labor, types and onset of labour
Learning Activity 3.2
Use books or other sources of information to answer the following questions.
1. What are the common signs that may indicate that a woman will be soon
in labour?
2. What are the types of labour for a pregnant woman?
3. Describe the onset of labour for a pregnant woman.
3.2.1. Signs preceding labour
Before the onset of labor, a number of physiological changes occur that signal the
readiness for labor and birth. These changes are usually noted by the primigravid
woman at about 38 weeks of gestation. In multigravidas, they may not take place
until labor begins.
Labor itself can be discussed in terms of the mechanisms involved in the process
and the stages through which the woman moves.
3.2.2 Types of labour
False labour
Braxton-Hicks contractions As the pregnancy approaches term, most women
become more aware of irregular contractions called Braxton-Hicks contractions.
As the contractions increase in frequency (they may occur as often as every 10
to 20 minutes), they may be associated with increased discomfort. Braxton-Hicks
contractions are usually felt in the abdomen or groin region and patients may
mistake them for true labor. It is believed that these contractions contribute to the
preparation of the cervix and uterus for the advent of true labor. Braxton-Hicks
contractions do not lead to dilation or effacement of the cervix, and thus are often
termed “false labor.”
True labour
As time passes, the woman’s uterine contractions increase the intensity, regularity
and pain. A woman starting labour experiences cervical changes in preparation
for passage of the fetus. The cervix soften (cervical ripening), stretches, and thin,
and eventually is taken up into the lower segment of the uterus. This softening
and thinning is called cervical effacement. As the effacement progresses, there
may be rupture of the small cervical capillaries. The added pressure created by
engagement of the presenting part may lead to the expulsion of a brownish or
blood-tinged cervical mucus plug, called bloody show. This mucus acts as a
protective barrier for the uterus and its contents throughout the pregnancy. The
cervix becomes soft (ripens) and partially effaced and may begin to dilate.
Rupture of membranes
A few numbers of pregnant women experience spontaneous rupture of the amniotic
sac (“rupture of membranes” or “rupture of the bag of water” prior to onset of
labour. the rupture of membrane may be spontaneous or artificial. The rupture of
membrane is a critical event in pregnancy.
Table no 3.1 Differences between False and Truelabor
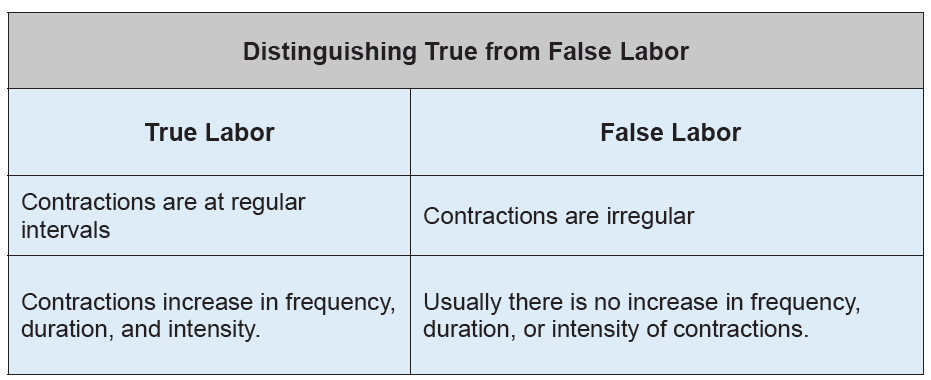
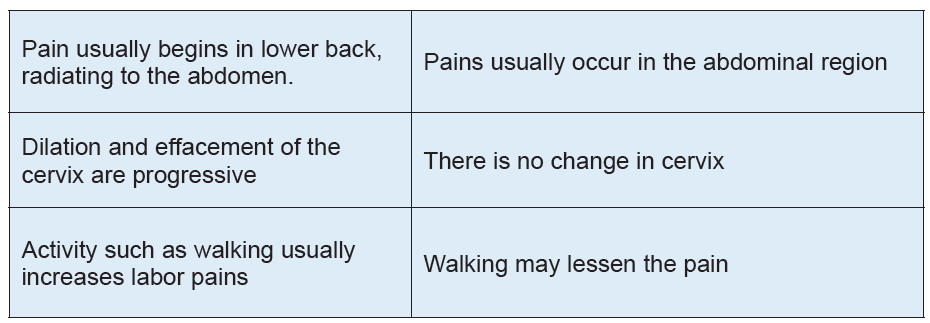
3.2.3. Onset of labor
At the onset of labor, the position of the fetus with respect to the birth canal is critical
to the route of delivery. The onset of labour is determined by a complex interaction
of maternal and fetal hormones and it is not yet well understood. Childbirth is theperiod from the onset of regular uterine contractions until expulsion of the placenta.
Self-assessment 3.2
1. List four signs that may signify impending of labour?
2. Distinguish the two types of labour for a pregnant woman
3. What determines the onset of labour of a pregnant woman?
4. Describe when a woman experiencing contractions at term should beinstructed to go to the hospital.
3.3. Factors affecting labour and Mechanism of labour
Learning Activity 3.3
When a pregnant woman is on labour there are factors that are affecting labour
process. Use books or other sources of information to answer the followings
questions:
1. List 2 factors affecting the labour process?
2. What are the 7 elements of the mechanism of labour?
The mechanisms of labor, also known as the cardinal movements, involve changes
in the position of the fetus’s head during its passage in labor. These are described
in relation to a vertex presentation.
The labour and birth process are affected by at least five factors. These factors are
known as:
A. Factors affecting labour
Five P’s : Passageway( Birth canal) , Passenger ( fetus and placenta ) ,Power
( Uterine contractions ) , Position of the mother , and psychologic response of
the mother. Based on the maternal needs and her childbearing rights, a sixth P is
added which is Partner. This partner may be her husband /life partner or a person
of her choice.
The first four factors are presented here as the basic for understanding the
physiologic process of labour. The firth and six Ps are the factors that may affect
labour indirectly but with positive impact.
• Passageway
The passageway, or birth canal, is composed of the mother’s rigid bony pelvis
and the soft tissues of the cervix, the pelvic floor, the vagina, and the introitus
(the external opening to the vagina). Even though the soft tissues, particularly
the muscular layers of the pelvic floor, contribute to vaginal birth of the fetus, the
maternal pelvis plays a far greater role in the labor process because the fetus must
successfully accommodate itself to this relatively rigid passageway.
• Passenger
During labour and birth process the fetus moves through the birth canal. These
fetal movements are affected by the following factors: The fetal presentation, lie,
attitude, position and size.
• Position of a labouring woman:
Position of the labouring woman affects the woman’s anatomic and physiologic
adaptations to labour. Frequent changes in position relieve fatigue, increase comfort,
and improve circulation. Therefore, a laboring woman should be encouraged to find
positions that are most comfortable to her. Positioning for labor may be determined
by the woman’s preference, but choices are limited by her condition or that of the
fetus, the environment, and the health care provider’s confidence in assisting in ina specific position.
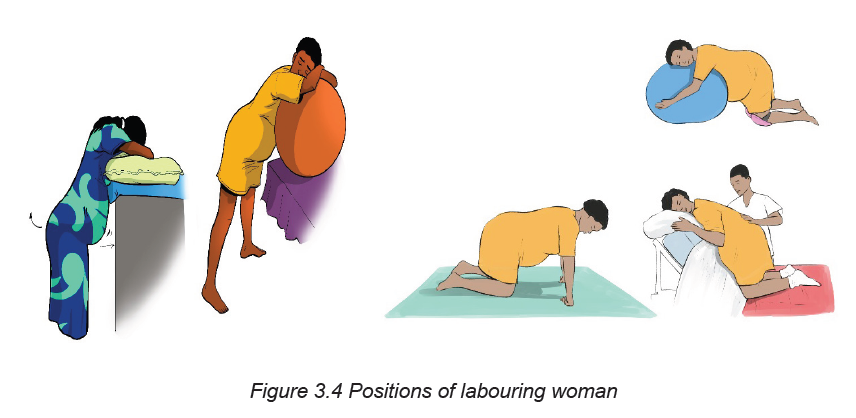
B. Mechanism of Labour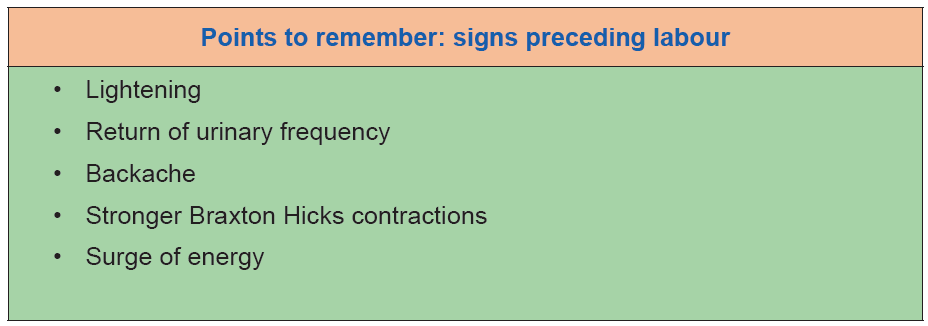
The most common fetal presentation is Occiput Anterior Presentation (Vertex
presentation). During labour process, the fetus adopts positional changes in the
presenting part required to navigate the pelvic canal. These positional changes
constitute the mechanism of labour
The cardinal movements of labour are engagement, descent, flexion, Internal
rotation, extension, external rotation, and expulsion
A. Engagement
The term engagement designates the mechanism by which the biparietal diameter
“the greatest transverse diameter in an occiput presentation” passes through the
pelvic inlet is designated engagement
B. Descent
Descent refers to the progress of the presenting part through the pelvis. Descent
depends on at least four forces: (1) pressure exerted by the amniotic fluid, (2) direct
pressure exerted by the contracting fundus on the fetus, (3) force of the contraction
of the maternal diaphragm and abdominal muscles in the second stage of labor,
and (4) extension and straightening of the fetal body. The effects of these forces
are modified by the size and shape of the maternal pelvic planes and the size of the
fetal head and its capacity to mold.
C. Flexion
As soon as the descending head meets resistance from the cervix, pelvic wall, or
pelvic floor, it normally flexes so that the chin is brought into closer contact with the
fetal chest (see Fig. 16-12, B). Flexion permits the smaller suboccipito-bregmatic
diameter (9.5 cm) rather than the larger diameters to present to the outlet.
D. Internal rotation
The maternal pelvic inlet is widest in the transverse diameter; therefore, the fetal
head passes the inlet into the true pelvis in the occipito-transverse position. The
outlet is widest in the anteroposterior diameter; for the fetus to exit, the head must
rotate. Internal rotation begins at the level of the ischial spines but is not completed
until the presenting part reaches the lower pelvis. As the occiput rotates anteriorly,
the face rotates posteriorly. With each contraction the fetal head is guided by the
bony pelvis and the muscles of the pelvic floor.
E. Extension
After internal rotation, the sharply flexed head reaches the vulva and undergoes
extension. When the fetal head reaches the perineum for birth, it is deflected
anteriorly by the perineum. The occiput passes under the lower border of the
symphysis pubis first, and then the head emerges by extension
When the head presses upon the pelvic floor, however, two forces come into play.
The first force, exerted by the uterus, acts more posteriorly, and the second, supplied
by the resistant pelvic floor and the symphysis, acts more anteriorly. The resultant
vector is in the direction of the vulvar opening, thereby causing head extension.
This brings the base, first the occiput into direct contact with the inferior margin of
the symphysis pubis, then the face, and finally the chin.
P. External rotation
After the head is born it rotates briefly to the position it occupied when it was engaged
in the inlet. This movement is referred to as restitution. The 45-degree turn realigns
the infant’s head with the back and shoulders. Restitution of the head to the oblique
position is followed by completion of external rotation to the transverse position.
This movement corresponds to rotation of the fetal body and serves to bring its biacromial
diameter into relation with the anteroposterior diameter of the pelvic outlet.
Thus, one shoulder is anterior behind the symphysis and the other is posterior.
This external rotation occurs as the shoulders engage and descend in maneuvers
similar to those of the head. As noted, the anterior shoulder descends first. When
it reaches the outlet, it rotates to the midline and is delivered from under the pubic
arch. The posterior shoulder is guided over the perineum until it is free of the vaginal
introitus.
G. Expulsion
After birth of the shoulders, the head and shoulders are lifted up toward the mother’s
pubic bone and the trunk of the baby is born by flexing it laterally in the direction
of the symphysis pubis. After delivery of the shoulders, the rest of the body quickly
passes. When the baby has completely emerged, birth is complete, and the secondstage of labor ends.
Self-assessment 3.3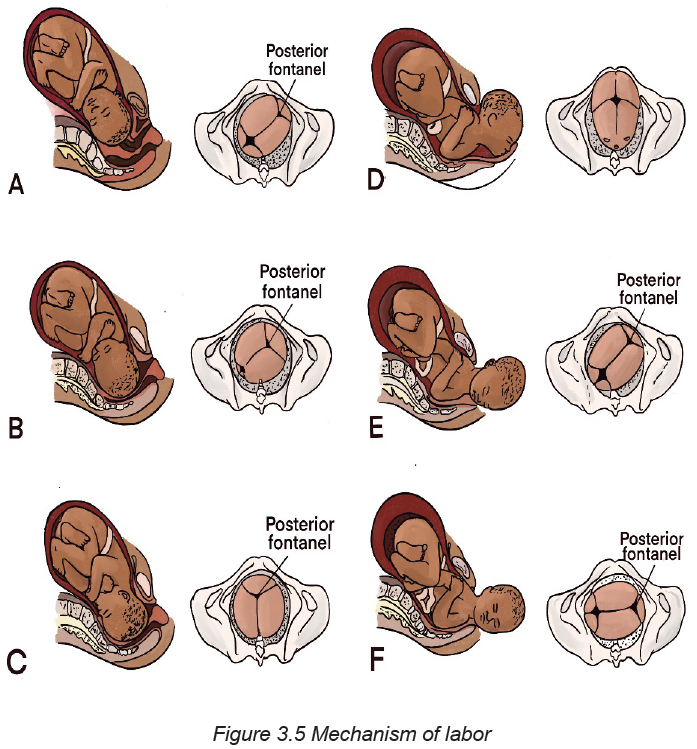
1. Define the fetal presentation?
2. Define the 5 Ps affecting labour?
3. Differentiate the first powers and secondary powers.
4. Explain the mechanism of labour
3.4. Assessment of a woman in labour: General history taking,
vital signs and physical examination
Learning Activity 3.4
Using textbooks and other resources identify different general pregnant woman’s
histories taken during history taking.
Pregnancy is typically a time of joy and anticipation. It can also be a time of anxiety
and concern. Listening and talking respectfully and sensitively with a woman and her
family can help build the woman’s trust and confidence in her health care providers.
Before starting the assessment remember to ask the woman if she has had any
danger signs (vaginal bleeding, gush of fluid or any problems such as fever, difficulty
breathing, cough, leg pain, etc.) or has any concern.
• The vital signs (temperature, blood pressure, heart rate and respiratory
rate) and parameters (Height, weight, BMI). Respond immediately to any
abnormalities in vital signs or other problems identified during the rapid initial
assessment.
• General Medical History: Ask about any serious medical diseases likely to
affect pregnancy and labour such as heart diseases, diabetes mellitus, renal
diseases, tuberculosis and sickle cell disease. Note any allergies to drugs,
Syphilis testing, VCT, HIV diagnosis or currently on any medication taken
regularly.
• Surgical history: Any previous hospitalizations for injuries to the pelvis and
spine, major or minor surgeries on the abdomen and blood transfusion.• Physical assessment includes the examination from head to toe.
Self-assessment 3.4
1. What are the vital signs and parameters taken during the pregnant woman’s
assessment?
2. What are the components of the general history taking?
3.5. Assessment of a woman in labour: Obstetrical history taking
Learning Activity 3.5
Using text books and other sources of information, identify the components of
obstetrical and gynecological history of a woman on labour.
• History of the present pregnancy: It includes the date of the first day of
the last normal menstrual period (LMP), the Parity and Gravidity. From this,
calculate and record the expected date of delivery (EDD). Ask the woman
about the history of this labour: approximate time contractions began and
membranes ruptured (when, what color and odor?).
• Past obstetric history: You should ask the mother about the outcomes
or complications of each of the previous pregnancies. Inquire whether she
delivered at home or at a hospital. Ask for the birth weights of the children,
whether they were breastfed and whether they are alive or not.
• Gynecological history: This will include the menstrual history, any past
operations for gynecological complaints and sexually transmitted infections
(STI).
Self-assessment 3.5
A pregnant woman attends the health post complaining of labour pains and
she explained that she has attended antenatal care 4 times and this is her 3rd
pregnancy and her last menstruation date is 12th/January /2021
1. Calculate her expected date of delivery (EDD)
2. What are the questions that you would ask to know the history of the present
pregnancy.
2. What are the obstetrical history would you ask her?3. What are the questions will you ask her to know her gynecological history?
3.6 Assessment of a woman in labour: Obstetrical examination
Learning Activity 3.6
Using text books and other sources, identify the steps of obstetrical examination
for a woman on labour.
Abdominal palpation: Check the woman’s abdomen for caesarean scar; a
horizontal ridge across lower abdomen (if present, ask the woman to empty her
bladder and observe her again). This examination includes Leopold maneuvers
(palpation to determine position, lie, engagement and descent of the presenting
part); uterine contraction palpation (palpate uterine contraction at the fundus,
record duration in seconds, frequency which is the number of uterine contractions
in 10 minutes, and the intensity of contractions). It also includes listening to fetal
heart rate for one whole minute (20-30 minutes baseline, External fetal monitoring
is required) and
Digital vaginal examination (DVE): To determine the cervical position, length,
thickness, dilation and effacement. Assessment of the state of membranes (intact,
ruptured, color and consistency, amount and note the time of rupture); we also
assess the pelvic floor; the diagnosis of the position and evaluation of the descent
of the fetal presenting part. Assess the descent in terms of fifths of fetal head
palpable above the symphysis pubis. A head that is entirely above the symphysis
pubis is five fifths (5/5) palpable; a head that is entirely below the symphysis pubis
is zero fifths (0/5) palpable. The vaginal examination equipment and steps to follow
are described below:
► Equipment: sterile examination gloves (clean gloves may be used if the
membranes are intact); sterile lubricant; antiseptic solution and light source
(if required); disposable wipes.
► Steps:
a. Wash and dry your hands. Explain the procedure and purpose of the
examination to the patient. RATIONALE: Hand washing helps to prevent
the spread of microorganisms. Explanations help to decrease anxiety and
promote patient understanding and cooperation.
b. Assess for latex allergies. RATIONALE: To prevent injury from latex exposure;
if patient has a latex allergy, use non latex gloves.
c. Ensure privacy. RATIONALE: Privacy promotes comfort and self-esteem.
d. Assemble necessary equipment including clean gloves (if the membranes are
intact) or sterile examination gloves (if the membranes are ruptured), sterile
lubricant, and antiseptic solution (if required).
e. Position the patient in a supine position with a small pillow or towel under
her hip to prevent supine hypotension. Instruct the patient to relax and
position herself with her thighs flexed and abducted. RATIONALE: Relaxation
decreases muscle tension and enhances patient comfort. Proper positioning
facilitates the examination by providing access to the perineum.
f. Don sterile gloves (clean gloves may be used if the membranes are intact).
g. Inspect the perineum for any redness, irritation, or vesicles.
h. Using the nondominant hand, spread the labia majora and continue
assessment of the genitalia. Note the presence of any discharge including
blood or amniotic fluid. RATIONALE: Positioning the hand in this manner
facilitates good visualization of the perineum. The presence of lesions may be
indicative of an infection and possibly preclude a vaginal birth. The presence
of amniotic fluid implies that the membranes have ruptured.
i. Gently insert the lubricated gloved index and third fingers into the vagina in
the direction of the posterior wall until they touch the cervix. The uterus may
be stabilized by placing the nondominant hand on the woman’s abdomen.
j. Assess the cervix for effacement and the amount of dilation.
k. Assess for intact membranes; if fluid is expressed, test for amniotic fluid.
l. Palpate the presenting part. RATIONALE: It is necessary to determine the
presenting part in order to assess fetal position and evaluate fetal descent.
m. Assess fetal descent and station by identifying the position of the posterior
fontanel.
n. Withdraw the fingers. Assist the patient in wiping her perineum from front to
back to remove lubricant or secretions. Help her to resume a comfortable
position. RATIONALE: Wiping from front to back prevents the transfer of
rectal contamination toward the vagina.
o. Inform the patient of the findings from the examination.
p. Wash hands. Document the procedure on the patient’s chart and on the fetal
monitor strip (if a fetal monitor is being used). Include the assessment findings
and the patient’s tolerance of the procedure. RATIONALE: Documentationprovides a record for communication and evaluation of patient care.
Laboratory investigations
Laboratory testing is a routine component of the admission process. Tests for blood
type and Rh factor, complete blood count (CBC), hemoglobin (Hb) and hematocrit
(HCT), and blood glucose/Glycemia are basically obtained. Blood tests for syphilis,
hepatitis B, and HIV are also collected. The urine specimen is tested for the
presence of protein, glucose, blood, pus, bacteria and ketones.
Self-assessment 3.6
A pregnant woman attends health post complaining of lombo pelvic pains on a
term pregnancy. When asked she told you that she started laboring for the past
two hours.
1. Explain the steps of obstetrical examination?
2. What are the required laboratory tests for her before transfer?
A. Use of partograph
Learning Activity 3.7
Observe the picture bellow and answer the following questions:
1. What is the name of this tool?
2. What is this tool used for?
3. What are the elements that are on this tool? Picture is missing here evenpicture description as part of learning activity.
The partograph was developed and extensively tested by the world health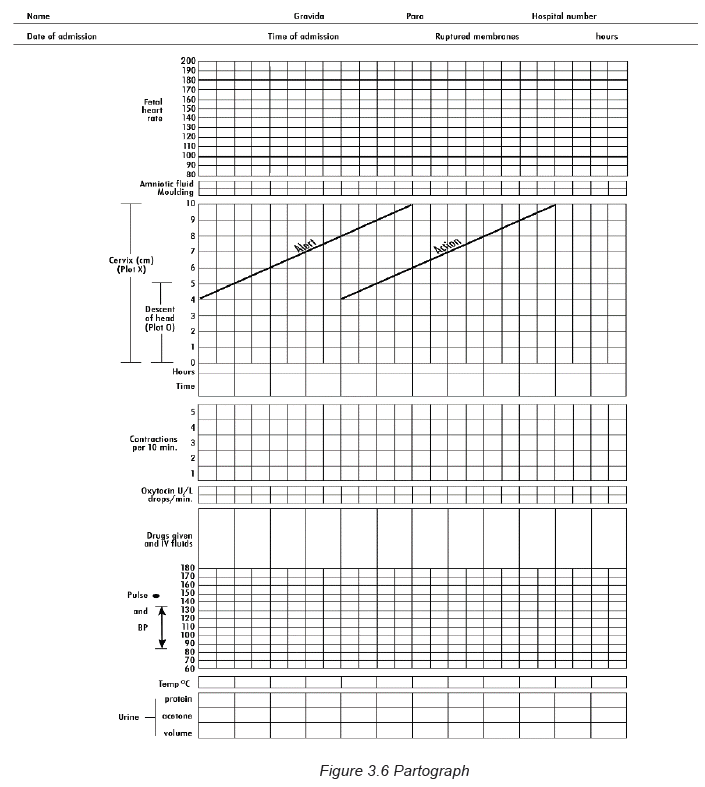
organization WHO for guiding birth attendant to have a good overview of labor
progression and therefore decide appropriate action. The partograph is accessible
in paper and electronic versions for most health care workers in maternity as the
tool of labor monitoring.
The use of partograph helps in health facilities for early detection of abnormal progress
of a labor; prevention of prolonged labor; recognition cephalopelvic disproportion;
early decision on transfer, augmentation, or termination of labor; increased quality
and regularity of all observations of mother and fetus; early recognition of maternal
or fetal problems; reduction of complications from prolonged labor for the mother
and for the newborn.
All observations and examinations like cervical dilatation; effacement; decent of
presenting part; strengths and duration of uterine contractions; maternal and fetal
wellbeing and any drug treatment are documented on partograph.
Parts of the partograph
Plotting on the partograph begins in the active phase when the cervix is 4 cm
dilated. The partograph should be enlarged to full size before use.
The following are element to be recorded on the partograph:
1. Maternal information and conditions:
Woman’s name; gravida; para, hospital number; date and time of admission; time
of ruptured membranes; Pulse recorded every30 min and mark with a dot (•); Blood
pressure every 4 hours; Temperature every 2hours; Urine output, Protein and
Glucose when urine is passed.
2. Fetal conditions:
Fetal heart rate every half hour; Colour of the amniotic fluid and the status of
membranes at every vaginal examination as I: membranes intact, R: membranes
ruptured, C: membranes ruptured, clear fluid, M: meconium-stained fluid, B: bloodstained
fluid; Moulding as 1: sutures apposed 2: sutures overlapped but reducible
sutures overlapped and not reducible.
3. Progress of labor:
Cervical dilatation at every vaginal examination and mark a cross (X) and start
to plot it at 4 cm. There are two lines Alert line which starts at 4 cm of cervical
dilatation to the point of expected full dilatation at the rate of 1 cm per hour and
Action line which is parallel and four hours to the right of the alert line; Descent
as a circle (O) at every abdominal examination. At 5/5, the sinciput is completely
above the symphysis pubis; at 4/5, the sinciput is high and occiput easily felt;
at 3/5 the sinciput is easily felt; at 2/5, the sinciput is felt and occiput just felt; at
1/5, the sinciput is felt and occiput is not felt; at 0/5, none of the head is palpable.
Assess contractions every half hour and count the number of contractions in a
10-minute time period and their duration in seconds and intensity. The contractions
are recorded as follows: less than 20 seconds: ; between 20 and 40 seconds:
; more than 40 seconds:
4. Drugs: Oxytocin when used, record the amount per volume of IV fluids in
drops per minute every 30 minutes; any additional drugs given are alsorecorded.
Self-assessment 3.7
Alexa is 38 years of age G4P3, was admitted at 10:00 am on 11 October 2021
with complaints of labour pains since 7:00 am. This is her first pregnancy. Plot
the following findings on the partograph:
At 10:00am:
• The cervix is dilated 4 cm.
• The fetal head is at 0 station, no moulding.
• The membranes are intact.
• She had 2 contractions in 10 minutes, each lasting less than 20 seconds.
• The FHR is 140 per minute.
• Her BP is 100/70 mmHg.
• Pulse: 82b/1minute.
• Her temperature is 37°C.
• Her pulse is 80 per minute• no oxytocin added
End unit assessment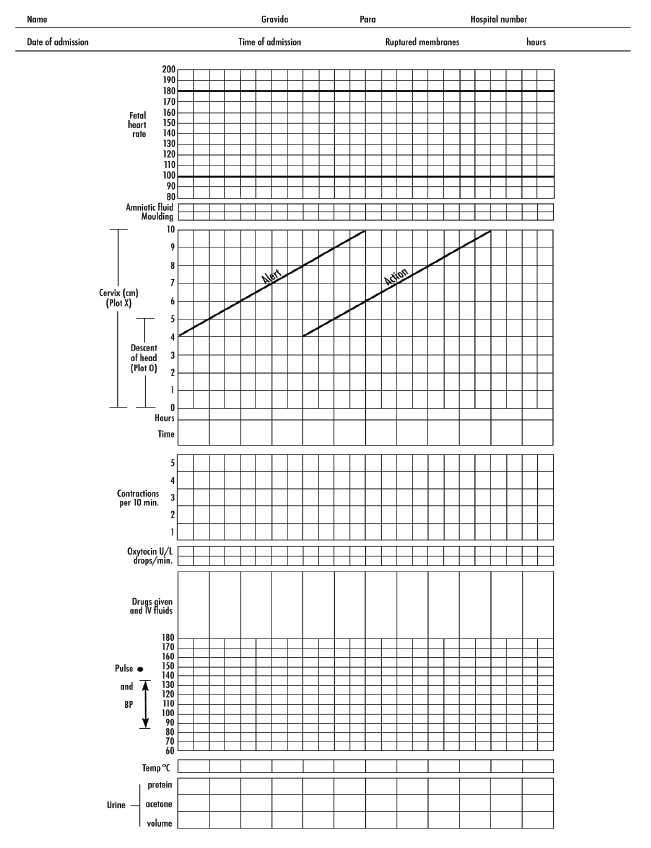
Mutesi is a 25-year-old G 1 P 0 at 39 weeks of gestation. She presents herself to
the health center at maternity ward and announces, “I’m here to have my baby. I
think I’m in labor.” Mutesi reports that she saw a thick bloody vaginal discharge
several hours ago when wiping after peeing earlier today. She states that she
has lower abdominal cramping (“It feels like the cramps I have with my periods”)
but denies leakage of vaginal fluid. Mutesi also reports active fetal movements.
In answering to your question, she replies that her current pain level is mild,
while alternating between texting on her phone and chatting with her mother,
who accompanied her to the hospital. Few hours later you observe change in
her pain. She expressed that her pain is increasing and she feels like pushing.
After assessment you realize her cervix is dilated at 6cm; effaced at 100%; the
baby’s head is at 0 station with vertex presentation; water bag is intact; the
Fetal heart rate are 140beats/min and regular; she has 3 contractions in 10 min
lasting between 20 and 40 seconds. The nurse at health post indicates that the
woman’s hemoglobin is 12g/dl; glycosuria is negative; temperature of 37.3oC;
Blood pressure is 100/80mmHg; Pulse of 86 beats/min and respiration of 20
mvts/min.
Plot all above information on partograph.
1. Define the following terminologies:
a. Labour
b. Uterine contractions
c. Stations
2. Describe the digital Vaginal examination that you would do to Mutesi?
3. What are the essential elements to focus on in your assessment?
4. Using the information you have above start plotting the partograph for thiswoman.
UNIT 4 MANAGEMENT OF THE FIRST STAGE OF LABOUR
Key Unit competence: Manage a woman in the first stage of labour
4.1. Stages of labor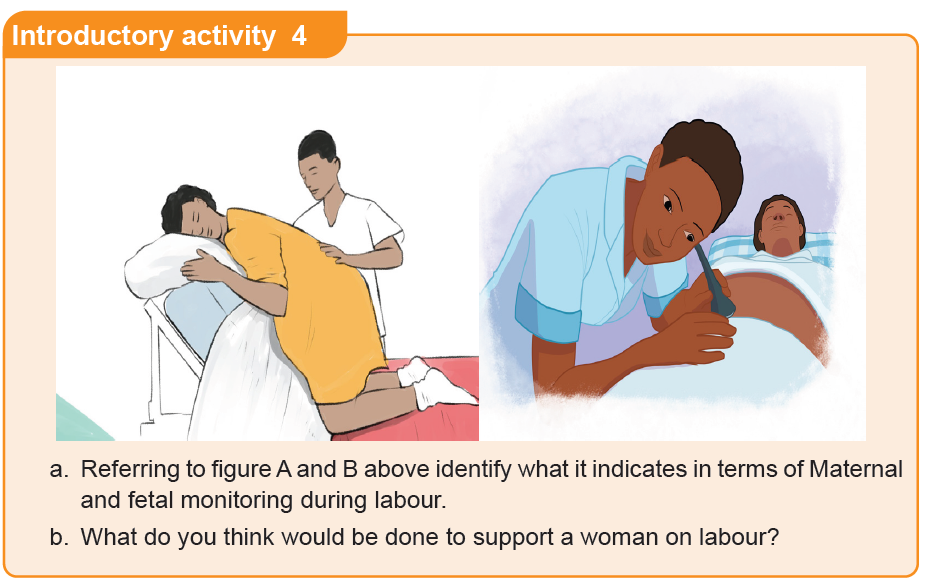
Learning Activity 4.1
Madam Kawera came in labour suite, complaining of labour pain that started
2 hours ago. She reports that a nurse earlier told her that she has a cervical
dilatation of 6 cm and the fetal descent was at 0 station, FHR was 140b/minute.
Uterine contractions were 3 in 10 minutes lasting 40 seconds. Her membranes
were intact and no any other complain.
Answer the following questions based on information given to you by madam
Kawera, previous lessons in unit 1,2 and 3 and books:
1. In which phase of labour is Madam Kawera?
2. In which stage of labour is Madam Kawera?
The labor and childbirth processes are natural phenomena during which most
women benefit from a philosophy of minimal intervention.
The first stage of labor starts from the commencement of contractions and lasts
until full dilatation of the cervix. It is a progressive process, and is divided in 3
phases: the latent phase begins with the establishment of regular contractions
(labor pains). Labor pains are often initially felt as sensations similar to painful
menstrual cramping and are usually accompanied by low back pain. Contractions
during this phase are typically about 5 minutes apart, last 30 to 45 seconds, and
are considered to be mild. The latent phase of labor can last as long as 10 to 14
hours as the contractions are mild and cervical changes occur slowly (0 to 3 cm of
dilation).
The active phase of labor is characterized by more contractions, they become
more frequent (every 3 to 5 minutes), last longer, and are of a moderate to strong
intensity. During the active phase, the cervical dilation advances more quickly (4
to 7 cm) as the contractions are often more efficient. While the length of the active
phase is variable, nulliparous women generally progress at an average speed of 1
cm of dilation per hour and multiparas at 1.5 cm of cervical dilation per hour.
The transition phase is the most intense phase of labor (8 to 10 cm of dilation).
Transition phase is characterized by frequent, strong contractions that occur every
2 to 3 minutes. Fortunately, this phase often does not take long because dilation
usually progresses at a pace equal to or faster than active labor (1 cm/hr for a
nullipara and 1.5 cm/hr for a multipara). During the transition phase, the laboring
woman may feel that she can no longer continue; rectal pressure, an increased
urge to bear down, an increase in bloody show, and spontaneous rupture of the
membranes (if they have not already ruptured).
The second stage of labor is traditionally defined as the stage from full cervical
dilation until the baby is born. Usually, the actual time of onset is uncertain because
the complete cervical dilatation does not always go with the descent and station of
the presenting part. The woman may experience vomiting, often with contractions;
show or bright red vaginal loss; spontaneous rupture of the membranes can occur
any time but often at full dilatation; urge to push; powerful, expulsive contractions
every 2–3 minutes, often lasting ≥60 seconds.
The third stage of labor refers to the period following the completed delivery of the
newborn until the completed delivery of the placenta. The length of the third stage
and its complications are affected by the uterine contractility and the duration of
placental separation.
This stage usually lasts 5 to 10 minutes, and may last up to 30 minutes. Once thebaby is born, the uterine cavity immediately becomes smaller.
Table 4.1: Classification of stage and phase oflabour based on cervical dilatation
The appropriate time taken for each stage of labour depends on gravidity. In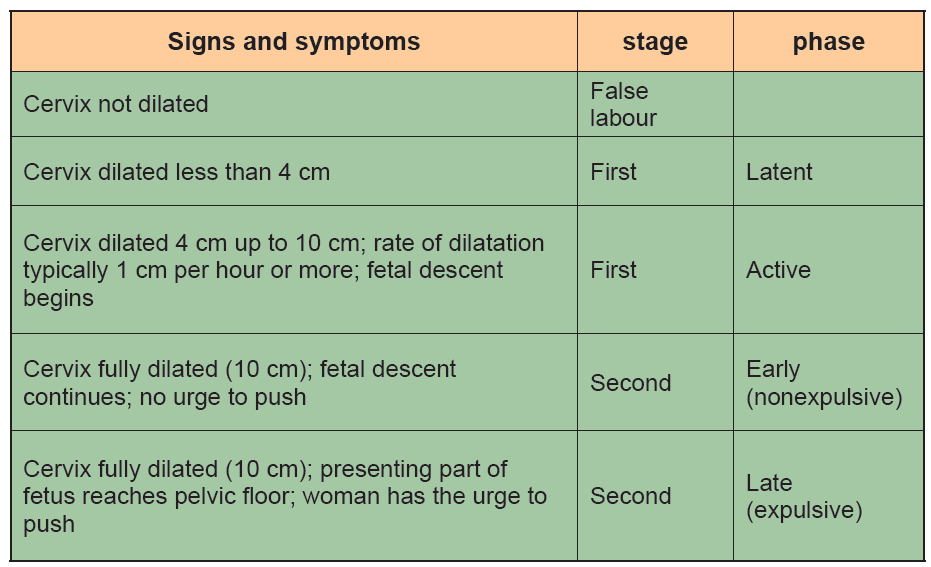
primigravidae the first stage lasts between 12 to 14 hours and 6 to 10 hours in
multigravidae; the second stage lasts 60 minutes for primigravidae and up to 30
minutes for multigravidae; the third stage lasts 20 to 30 minutes or 5 to 15 minutes
for primigraviadae and multigravidae in active management.
Self-assessment 4.1
1 Define the characteristics of the first and second stages of labor including
contractions and dilation.
2. Describe the three phases of the first stage of labor and the changes that
occur during each phase?
4.2. Care during the first stage of labour
Learning Activity 4.2
Using different source of information (internet, library) discuss in group, the care
provided to a pregnant woman during the first stage of labour.
During labour a pregnant woman receives the care that is centered to her.
The following table is showing the care provided during management of the first
stage of labour.Table 4.2 Care during the first stage of labour
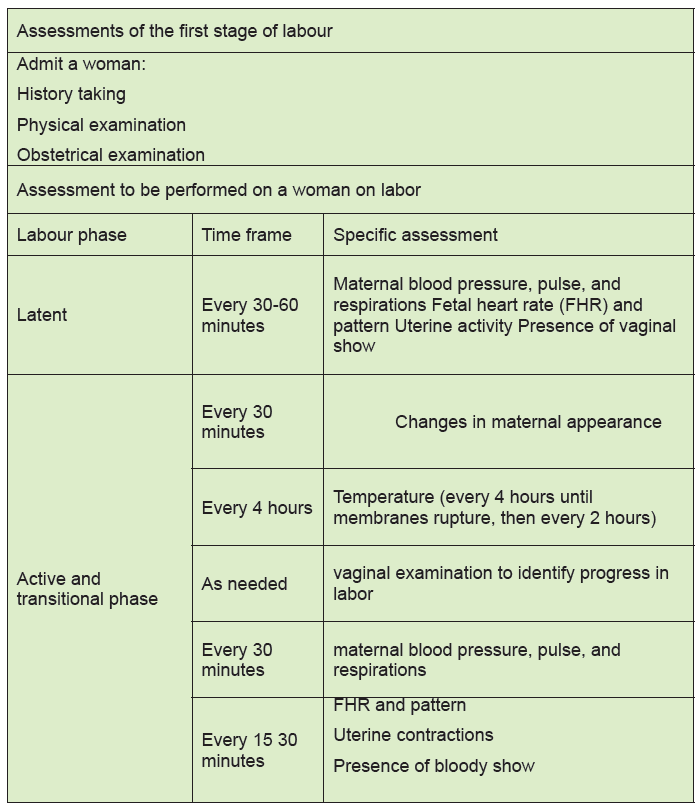
Self-assessment 4.2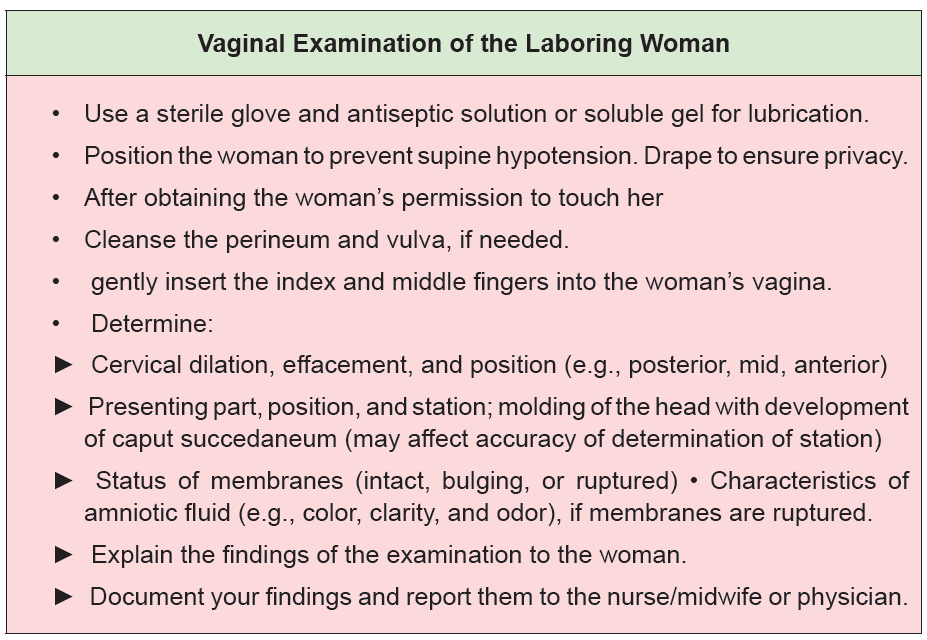
1. If a pregnant woman’s cervix is 2 cm dilated, when should you perform the
next vaginal examination?
a. After 2 hours of admission.
b. After 8 hours of physical exercises.
c. When the woman wants to bear down.
d. When there are signs that the woman is in established labour with more
regular and painful uterine contractions.2. In general, what must be monitored during the first stage of labor?
4.3 Labor Support
Whenever possible, continuous labor support should be given to women in labor and
providing this level of care has been associated with positive outcomes for mothers
and infants. Continuous labor support can be provided by health professional or by
lay people and include presence, promotion of comfort, anticipatory guidance,
caring of birth partner, and ensuring culture centered care.
• Presence: Offering one’s presence in labor can be defined simply as “physically
being with the woman.” Women find that having a skilled birth attendant present
can be reassuring because they recognize that assistance is available when
needed. Women want a healthcare professional or a person of choice to be
available, to be emotionally involved, to help create a special moment, to hear
and respond to their concerns, to share the responsibilities for keeping themsafe, and to act as a go-between for their family and the medical institution.
• Promotion of comfort: Women comfort is always needed and include different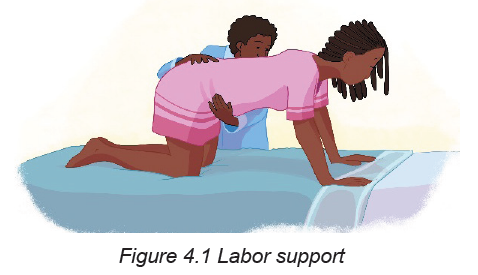
measures which are positions changes and personal comfort measures.
► Position Changes: In labor, frequent position changes are beneficial in helping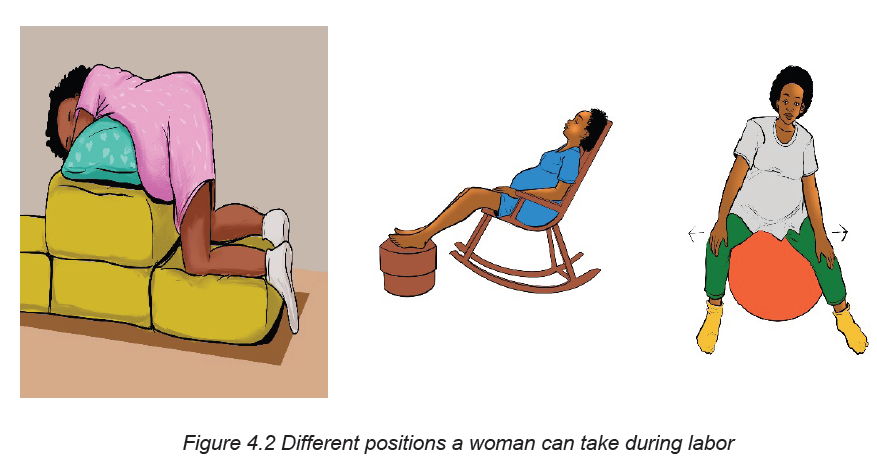
to promote the descent of the fetus. The woman’s person of choice may
assist the laboring woman to various positions and activities such as walking,
standing, sitting, squatting, leaning over a piece of furniture, or assuming ahands and knees position.
► Maternal preferences can guide the healthcare professional or her person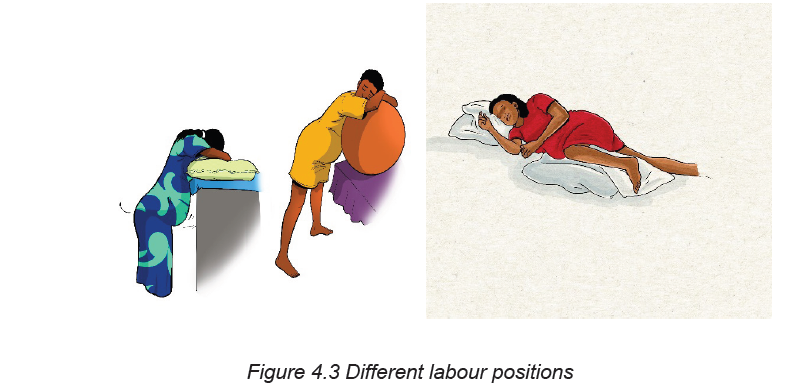
of choice in assessing which positions or activities the woman finds most
comfortable. Changes in the woman’s status may necessitate a need of bed
rest and the nurse should encourage the laboring woman to rest on her left
side to facilitate optimal uteroplacental blood flow.
In addition, position changes should be encouraged even if the woman must
remain in bed. It is important to avoid the supine position since the pressure of
the uterus on the maternal spine can cause compression of the inferior vena
cava and lead to decreased blood pressure and diminished uteroplacentalblood flow.
► Personal comfort measures: Based on laboring woman’s preferences and
needs, the nurse can provide personal comfort measures (good environment,
personal hygiene, elimination, and supportive relaxation techniques)
and encourage family members and support persons to help woman tomeet them.
• Environment: The healthcare provider will need to assess the women
environmental preferences sun streaming, lights dimmed, intolerance to hot
and remember to turn off the fan or assess the room temperature during
childbirth to ensure that the infant does not get unnecessarily chilled.
• Personal hygiene: The nurse can help promote the patient’s sense of
cleanliness and well-being by changing pads, linens, or gown especially
if the woman is leaking amniotic fluid or bloody show. Many women who
remain ambulatory are able to perform their own personal care. However,
if the laboring woman is confined to bed or exhausted from the exertion of
labor, full assistance should be provided. Frequent mouth care should be
encouraged since dry mouth is common during labor. Providing drinks, ice
chips, popsicles, or hard candy may help to alleviate the symptoms.
• Elimination: A full bladder can inhibit the descent of the fetus and contribute
to increased pain with contractions. Encouraging and assisting the woman to
the toilet (or bedpan) to void at least every 2 hours is recommended. If the
woman is unable to void and has a distended bladder a urinary catheter may
be required.
• Supportive relaxation techniques: During labor, the healthcare providers
may encourage, assist, or teach the woman about different interventions to
help decrease pain and relieve anxiety. Relaxation techniques may include
visualization, focal points, imagery, hydrotherapy, and breathing techniques.
In addition, patients may bring items from home to enhance relaxation suchas music, a picture, or a stuffed animal.
• Anticipatory guidance: Regardless of whether or not they have attended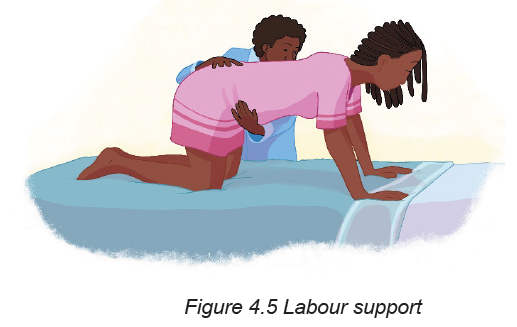
prenatal classes, most women and their families have many questions.
Women and families usually want to know what to expect. While the nurse/
midwife cannot predict exactly what will happen, helpful information can be
provided in general terms.
For example, a woman in early active labor may comment: “These contractions
are getting stronger, how strong will they get?” The nurse can empower the
woman by identifying the progress she has made to that point. Explaining
how the contractions have gradually become stronger and emphasizing how
successful the patient has been in adjusting to the changes provides factual
feedback and positive reinforcement of the progress made.
• Keeping the woman and her family informed about the process of labor and
birth is a constant and ever-changing task. For example, during the transition
phase the nurse may be teaching the woman breathing techniques to avoid
pushing with a partially dilated cervix and then with full cervical dilation, the
nurse teaches her how to push and may need to assist the woman into an
effective pushing position.
• Caring for the birth partner: Most of the nurse’s attention focuses on the
woman in labor. Efforts also should be made to help the support person feel
welcome and included whenever possible according to the woman’s wishes.
Orientation to the birth unit is helpful in identifying where to locate items such
as towels and washcloths, kitchen supplies and the restroom. Assessment of
the degree of involvement the support person would like to assume is also
important.
• Ensuring culture-centered care: It is important for nurses to remain open
minded and aware that there are a myriad of values, attitudes, beliefs, and
practices regarding childbearing that vary among cultures just as there
may be wide variations within cultures. Body language and communication
approaches provide examples of how differences in cultural practices can
be applied when caring for a woman and her family during the childbirth
experience.
Self-assessment 4.3
Max and Kate are a couple that attends the clinic and they ask a midwife on
duty to explain to them about labour support so that Kate can get a smooth and
enjoyable labour process.
1. Explain the components of the continuous labour support to Kate and Max.
4.4 Obstetric danger signs
Learning Activity 4.4
Using books and internet resources search for what can indicate a sign of danger
of a pregnant woman in the first stage of labour.
Knowledge of obstetric danger signs during labour is an important first step for
appropriate management and timely referral. Increasing knowledge of obstetric
danger signs for pregnant women would reduce delay in seeking care and improve
early detection of obstetric complications. The following are the key danger signsthat a laboring woman may present during the first stage of labour.
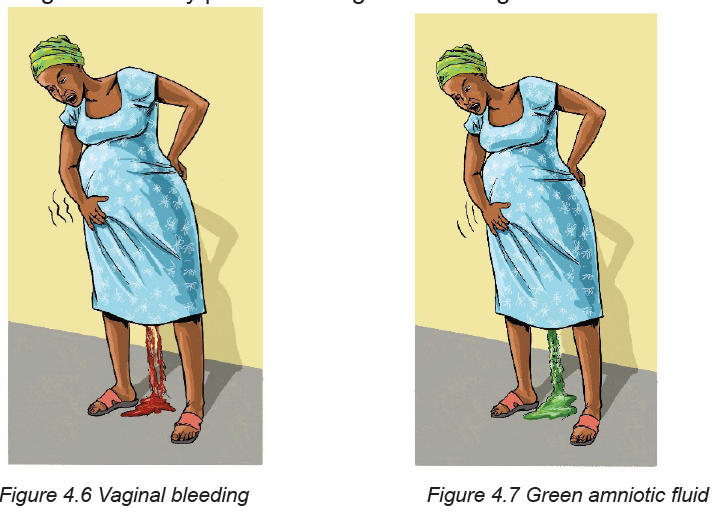
They key danger signs during labour includes severe vaginal bleeding (Figure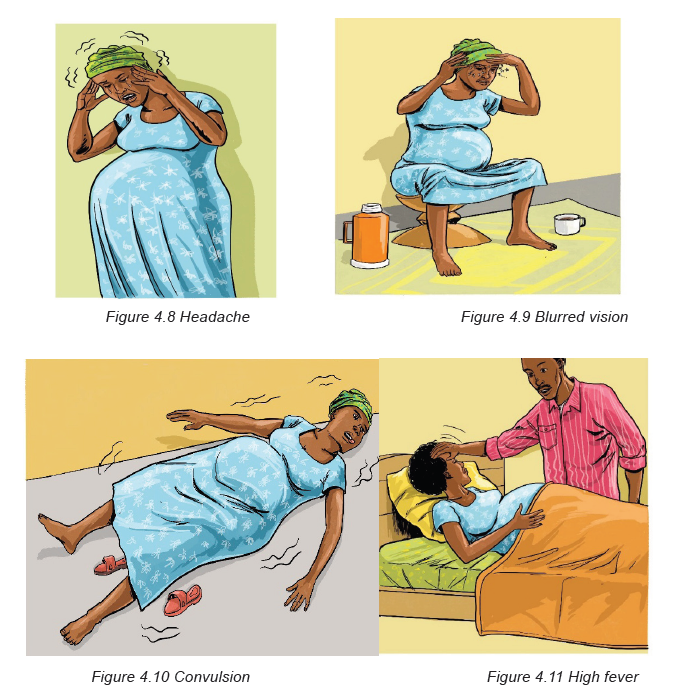
4.6) before the baby is born. Vaginal bleeding is very dangerous especially when
the bleeding is bright red because it could mean that the placenta is separating from
the uterine wall. Lack of fetal heart rate or fetal movement during labour, brown or
green amniotic fluid (figure 4.7)
Headache (Figure 4.8), blurred vision (Figure 4.9) and convulsion (Figure 4.10)
may be the results of a woman having a high blood pressure. A woman on labour
may experience also high fever (Figure 4.11), this high fever is usually a sign of
infection. Labour lasting for more than 24hours (first stage of labour) may be due
to cephalo-pelvic disproportion, malposition or malpresentation of the fetus or due
to maternal causes: insufficient contractions or inadequate pelvis.
indicates that the baby is in danger.
A woman experiencing all the above cited signs of danger is needs more attention
from healthcare and she must be transported to the nearest hospital for more
advanced obstetrical care.
Self-assessment 4.4
Zubeda is a 29 years old mother of 2 who comes in health post she stated that
she is about to give birth as her pregnancy is at term but she needs to know the
danger signs that can make her consult immediately.
1. Tell her the danger signs of the fetus and those that are maternal related
during labour.
End unit assessment 4
During labour monitoring, Olga a 23 years old prim gravida took tightly my hand
and asks me a soft drink and some snacks. Few minutes later she requested me
to rub her back because she was feeling backaches with slight lower abdominal
pain and confirm that 2 days ago a bloody show was expelled out from the
vagina. She was bed ridden for the past three days without taking anything.
“These mothers that are suffering are scaring me, it seems so hard and painful”:
She said!
“Can you please help me to get up? Now I feel better with you! At least I can cope
with my pain. Let’s turn around before the midwife come to assess me again”.
She added. As long as she continues ambulating, contractions increased, the
associate nurse continues rubbing her back, wiping her face with a cold tower and
offering drinks frequently. Suddenly Olga feels a strong contraction, and a gush
of reddish bloody amniotic fluid spreads on the flow. The associate nurse shout
out for help and the cervix was 6cm dilated and FHB were 101beats/min and the
patient was referred at the nearest district hospital for further management.
a. Throughout the scenario above remind clinical signs that characterize the
first stage of labor.
b. Compare the elements that differentiate the first and second phase of the
first stage
c. Using the text words indicate the elements that express the labor support
and monitoringd. Identify the danger signs occurred during Olga’s labor
UNIT 5MANAGEMENT OF THE SECOND AND THIRD STAGES OF LABOUR
Key Unit competence: Manage women in the second and third stages of labor
Introductory activity 5Carefully observe the pictures below and answer the questions below:
1. Based on the above pictures, how many stages of labour does a woman
go through?
2. According to what you know, what happens in each stage of labour?
3. Mention some medications that can be administered to the woman during
labour and circumstances in which these medications are indicated.
4. Which complications may likely occur during labour?
5. What can a nurse do to support a woman having labour related
complications?
5.1. Management of the second stage of labour5.1.1 Introduction to the second stage of labour
Learning Activity 5.1.1
Watch the video titled ‘Managing Second Stage and Active Management
of Third Stage of Labour Perfect’ found on this link: https://www.youtube.com/
watch?v=Yq8RJkLPOmc and answer the following questions:
a) What do you understand by the term ‘second stage of labour’?
b) Briefly describe the physiological changes occurring during the secondstage of labour?
Second stage of labor, referred to as the pushing stage, starts when the expectant
woman’s cervix is fully dilated and ends with the birth of the baby. The woman is
actively involved in giving birth with the support of skilled birth attendants.
Effective descent of the foetus through the birth canal involves not only position
and presentation but also a number of different positional alternatives termed as
‘cardinal movements’. These changes enable the smallest diameter of the foetal
head to pass through the vagina based on the diameter of the mother’s pelvis.
For this to happen, during the second stage of labour, a number of physiological
changes occur to facilitate the birth of the baby. The contractile power of the uterus
is intensified because the foetus is closely applied to the uterus, as some of the
amniotic fluid has leaked. The upper uterine segment becomes short and thick
because of the retraction of uterine muscle fibres. During each contraction, its force
is transmitted through the long axis of the foetus, directing it through the birth canaland this is termed as foetal axis pressure.
The foetal axis pressure leads to expulsive action of the abdominal muscles and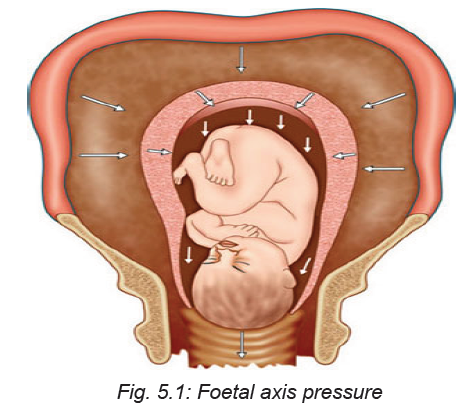
diaphragm. The abdominal muscles and diaphragm contracts, known as ‘bearing
down’ or ‘pushing’. Initially it is reflex, but can be aided by voluntary effort. With the
distension of the pelvic floor by the presenting part, the expulsive action becomes
involuntary.
Another physiological change that occur during the second stage of labour is the
displacement of the pelvic floor. The bladder is drawn up into the abdomen, the
vagina is dilated by the advancing head, the posterior segment of the pelvic floor is
pushed downwards in front of the presenting part and the reaction is compressed
by the advancing head. Further changes that takes place is pouting and gaping of
the anus, thinning out of the perineum and lengthening of the posterior wall of the
birth canal.
During the normal spontaneous vaginal birth, the next physiological change that
occurs is the expulsion of the foetus. As the woman collects her efforts to birth, the
baby’s head becomes visible at the opening of her birth canal and this biologicalmovement is called crowning (see picture below).
The head is born by extension, after which the shoulders and body are born, with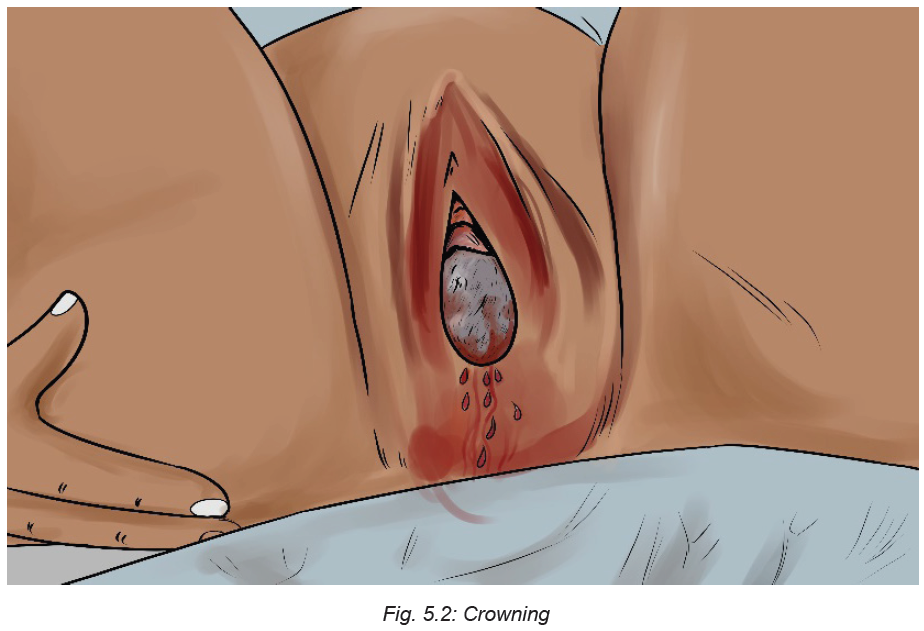
the remaining amniotic fluid.
Self-assessment activity 5.1.1
i. Define the following terms:
– crowning
– Bearing down
– Fetal axis pressure
ii. Describe the physiological stages involved in the birth of the baby during
the second stage of labour.
5.1.2 Mechanism of labour during the second stage
Learning Activity 5.1.2
Watch the video titled ‘Mechanism of Normal Labor’ found at: https://www.youtube.
com/watch?v=AKFS8I-uwHA and answer the following questions.
i. Based on the video you have watched, outline the movements that happen
before the baby is born.
The second stage of labour involves a number of cardinal movements leading to
the birth of the baby. These cardinal movements involve positional changes that
are effected by the foetus during the birth process. They encompass engagement,
descent, flexion, internal rotation, extension, external rotation, and expulsion asshown in the picture below.
a. Engagement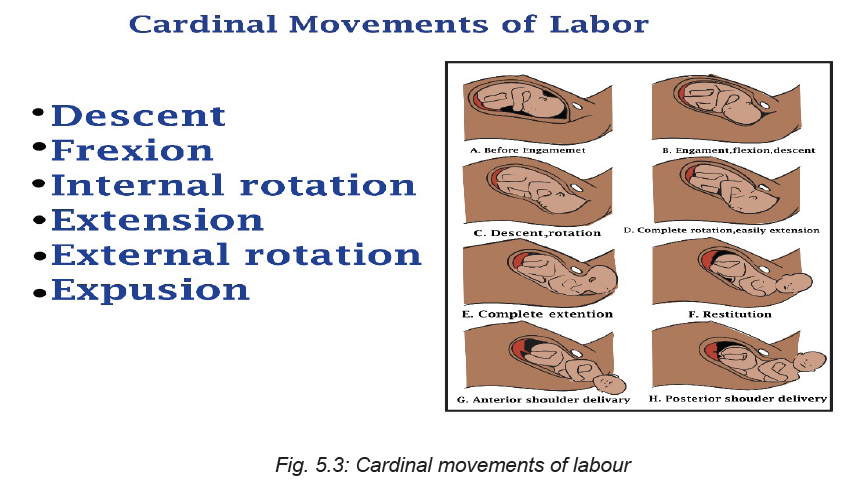
Engagement occurs when the largest transverse diameter of the head of the
foetus had passed through the pelvic inlet. When the foetal head is engaged, a
small part of the head is palpable above the pelvic brim. The healthcare provider
assesses the engagement of the presenting part during abdominal examination.
When engagement has started, the skilled birth attendant should take care of the
following:
• Assess the woman after an hour if there are no signs of foetal distress and the
maternal observations are normal.
• If the head has not engaged after waiting 1 hour, the skilled birth attendants
must carefully examine the patient for cephalopelvic disproportion which may
be present as a result of a big foetus or an abnormal presentation of the foetal
head. In this case, the skilled birth attendant refer the mother to advanced
care.
b. Descent
Descent is the downward movement of the biparietal diameter of the foetal head
within the pelvic inlet. Full descent occurs when the foetal head protrudes beyond
the dilated cervix and touches the posterior vaginal floor. Descent occurs because
of pressure on the foetus by the uterine fundus. As the pressure of the foetal head
presses on the sacral nerves at the pelvic floor, the labouring woman will experience
the typical “pushing sensation,” which occurs with labour. As a woman contracts her
abdominal muscles with pushing, this aids descent.
c. Flexion
As descent is completed and the foetal head touches the pelvic floor, the head
bends forward onto the chest, causing the smallest anteroposterior diameter (the
suboccipitobregmatic diameter) to present to the birth canal. Flexion is also aided
by abdominal muscle contraction during pushing.
d. Internal Rotation
During descent, the biparietal diameter of the fetal skull was aligned to fit through
the anteroposterior diameter of the mother’s pelvis. The head flexes at the end of
descent, the occiput rotates thus the head is brought into the best relationship to
the outlet of the pelvis, or the anteroposterior diameter is now in the anteroposterior
plane of the pelvis. This movement brings the shoulders, coming next, into the
optimal position to enter the inlet, or puts the widest diameter of the shoulders (a
transverse one) in line with the wide transverse diameter of the inlet.
e. Extension
When the occiput of the fetal head is born, the back of the neck stops beneath the
pubic arch and acts as a pivot for the rest of the head. The head extends and the
foremost parts of the head, the face and chin is born.
f. External Rotation
In external rotation, almost immediately after the head of the foetus is born, the
head rotates a final time (from the anteroposterior position it is assumed to enter
the outlet) back to the diagonal or transverse position of the early part of labor.
This brings the after coming shoulders into an anteroposterior position, which is
best for entering the outlet. The anterior shoulder is born first, assisted perhaps by
downward flexion of the foetal head.
g. Expulsion
Once the shoulders are born, the rest of the baby is born easily and smoothly
because of its smaller size. This movement, called expulsion, is the end of thepelvic division of labor.
Self-assessment 5.1.2
i) Define the following terms:
b) Engagement
c) External rotation
d) Descent
ii) As a nurse, what can you do when you notice that engagement has started?
Homework 5.1
Read Chapter about the management of the second stage of labour in book titled
‘The Continuous Textbook of Women’s Medicine Series – Obstetrics Module’.
Focus on pages 3, 4, and 5 of the chapter.
5.1.3. Factors affecting the second stage of labour
Learning Activity 5.1.3
i) Based on what you have read from the book titled ‘The Continuous
Textbook of Women’s Medicine Series – Obstetrics Module’, what are thebiological factors that may influence the second stage of labour?
A successful second stage of labour depends on four integrated factors; namely the
passage, passenger, power, and position.A. The passage (a woman’s pelvis)
The passageway refers to the route a foetus must travel through from the uterus to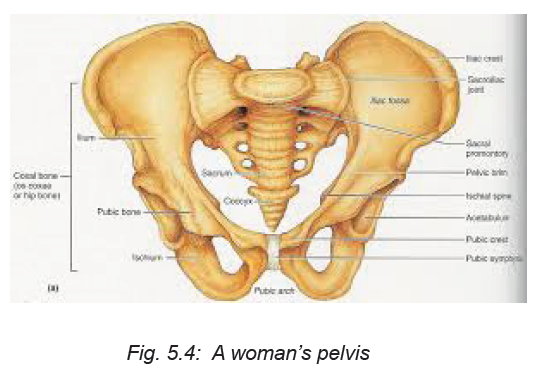
the cervix, vagina, and to the external perineum. The bony pelvis through which the
foetus must pass is divided into three sections: the inlet, mid-pelvis (pelvic cavity),
and outlet. Each of these pelvic components has a unique shape and dimension
through which the foetus must manoeuvre to be born vaginally. Because the cervix
and vagina are contained inside the bony pelvis, the foetus must also pass through
the bony pelvic ring. The two pelvic measurements that are important to determine
the adequacy of the pelvis are the diagonal conjugate (the anteroposterior diameter
of the inlet) and the transverse diameter of the outlet.
B. The passenger
The passenger can be defined as the foetus and the foetal membranes. The body
part of the foetus that has the widest diameter is the head, so this is the part least
likely to be able to pass through the pelvic ring in normal vaginal births. For birth
to occur normally, the passenger should be of appropriate size (not big for the
woman’s pelvis) and in an advantageous position and presentation. Whether a
foetal skull can pass through the woman’s pelvis depends on both its structure
(bones, fontanelles, and suture lines) and its alignment with the pelvis.
C. The powers of labour:
The powers of labour refer to the quality of contractions including frequency,
strength, and duration.
D. Position
Foetal position refers to the relationship of an arbitrarily chosen portion of the foetal
presenting part (Occiput, sacrum, mentum /chin or sinciput) to the right or left side
of the mother’s birth canal. The foetal presenting part may be in either the left or
right position to the four quadrants of the maternal pelvis, the foetal positions may
be left occipital (LO) and right occipital( RO), left mental (LM) and right mental( LM)
, and left sacral (LS) and right sacral presentations.
Self-assessment 5.1.3
With examples, explain how these factors can influence the second stage of
labour:
b) Passage
c) Passenger
d) The powers of labour.
Homework 5.2
Go to the internet and watch the video titled ‘Management of Second Stage of
Labour | Normal Labour | Nursing Lecture’ using this link: https://www.youtube.com/
watch?v=hHHA4vfWMcA
5.1.4. Nursing Management of the woman during the secondstage of labour
Learning Activity 5.1.4
Based on the video you have watched in homework, answer the following
questions.
i) Why is it very important for a skilled birth attendant to manage the second
stage of labour adequately?
ii) What assessments and observation should a skilled birth attendant perform
during the second stage of labour?
Promoting the health of women in labour is one of the measures to reduce maternal
morbidity, mortality and ensuring universal access to reproductive health services.
During the second stage of labour, a labouring woman needs optimum care in order
to prevent any complications that may affect her and that of the baby. The nurse at
this stage must coach quality pushing and support delivery.
It is very important for the skilled birth attendant to recognise the commencement of
the second stage. There are many probable signs that indicate the transition from
first to second stage as outlined below.
Table 5.1 Probable signs of the second stage oflabour
During the second stage of labour, the skilled birth attendant has to observe
maternal and foetal condition in order to ensure the safety of the second stage of
labour. Factors to observe include uterine conditions, the descent, foetal condition,
and maternal condition.
Regarding the uterine condition, the skilled birth attendant has to assess the
strength, length and frequency of contractions should be assessed continuously. In
comparison to the first stage, contractions are stronger and their duration is longer
(1 minute), with a longer resting phase.
As for the descent, the progress is observed by noting the descent of the foetus. It
accelerates during the active phase. If there is delay, a vaginal examination should
be performed to note whether internal rotation of the head has taken place to note
the station of the presenting part and for presence of caput succedaneum.
The skilled birth attendant also has to assess any presence of the colour of liquor
amnii (for meconeum staining) and changes in foetal heart pattern. The skilled birth
attendant has to perform intermittent auscultation of the foetal heart rate immediately
after a contraction for at least 1 minute, at least every 5 minutes. The caring team
has to palpate the woman’s pulse every 15 minutes to differentiate between the
two heartbeats. Ongoing consideration should be given to the woman’s position,
hydration, coping strategies and pain relief throughout the second stage.
Women in the second stage of labour will feel exhausted, and may not have the
ability to care for themselves. As a skilled birth attendant, you will have to give best
possible care to the woman and help her to cope with this stage of labour. The care
to offer encompass the following:
• Maternal comfort and hygiene
• Sponge the face and neck of the mother with a wet towel.
• Provide ice-chips or sips of water
• Apply moisturizing cream to lips to prevent dryness and cracking.
• Encourage to pass urine at the beginning of the second stage if she hasn’t
done it during the late first stage.
• Apply measures like massaging, encourage deep breathing, distraction, etc.,
to relieve pain.
• Reassure the woman. Encourage her to bear down only when instructed to.
As the woman prepares to give birth, the skilled birth attendant will have to give
the woman an appropriate position, to enable the birth process to be completed
smoothly. There are several factors that will affect the decision for adopting a specific
position, i.e., the maternal and foetal condition, the need for frequent monitoring,
the woman’s personal choice, the environment’s safety, privacy in the room, and
the birth attendant’s confidence to assist in the birthing process.
Some of the positions that can be adopted include semi-recumbent or supported
sitting position, squatting, kneeling or standing positions, and left lateral position asshown in the images below.
As for the supported sitting position, it increases the efficiency of the uterine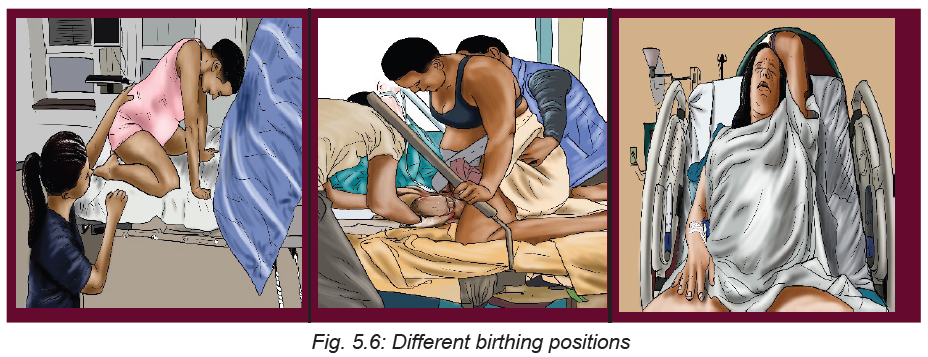
contractions and prevents hypotension and reduced placental perfusion. The
squatting position increases the transverse diameter by 1 cm and the anteroposterior
diameter by 2 cm, thereby resulting in easy delivery. The kneeling and standing
position also contribute to easy delivery. The left lateral position enables the skilled
birth attendant to view the perineum clearly. This position is useful for women who
cannot abduct their hips.
The woman should be helped to avoid ‘active pushing’ before the vertex is visible
at the vulva. This will allow the mother to conserve her effort and will permit the
vaginal tissues to stretch passively. Once the head becomes visible, the mother
should be encouraged to follow her own inclinations in relation to expulsive efforts.
The next step will involve the skilled birth attendant to facilitate the birth of the baby.
In this book, the entire process of conducting births is discussed in the skills lab and
practical checklist. To avoid complications in the mother as well as the newborn,one must conduct the delivery very skillfully in a vertex presentation.
The two phases of delivery of the foetus in a vertex presentation are: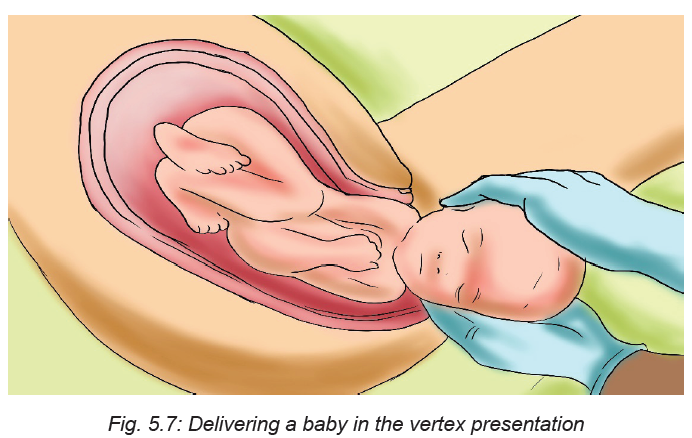
i) Delivery of the head, and
ii) Delivery of the shoulders and body.
The principles to be kept in mind while conducting the delivery is to minimise
maternal and foetal trauma and ensure a safe delivery for the baby. Principle of
asepsis must be maintained. The perineum is swabbed and the woman is draped
with sterile towels. A pad is used to cover the anus. With each contraction the head
descends and the superficial muscles of the pelvic floor especially the transverse
perineal muscles are visible. During the resting phase, the head recedes, thereby
the muscle thins gradually. The skilled birth attendant places her fingers on the
advancing head to monitor descent and prevent expulsive crowning.
During the birth, the skilled birth attendant must help the mother to prevent the
tears in the vaginal opening. Some health care providers do not touch the vagina or
baby at all during the birth. This is a good practice because interference can lead
to infection, injury, or bleeding. But the healthcare providers may be able to prevent
tears by supporting perineum during the birth.
Self-assessment 5.1.4
i) What precautions should a skilled birth attendant take while delivering the
baby?
ii) What can you base on to determine if the second stage of labour has
started?5.1.5. Assessing foetal wellbeing during the second stage of labour
Learning Activity 5.1.5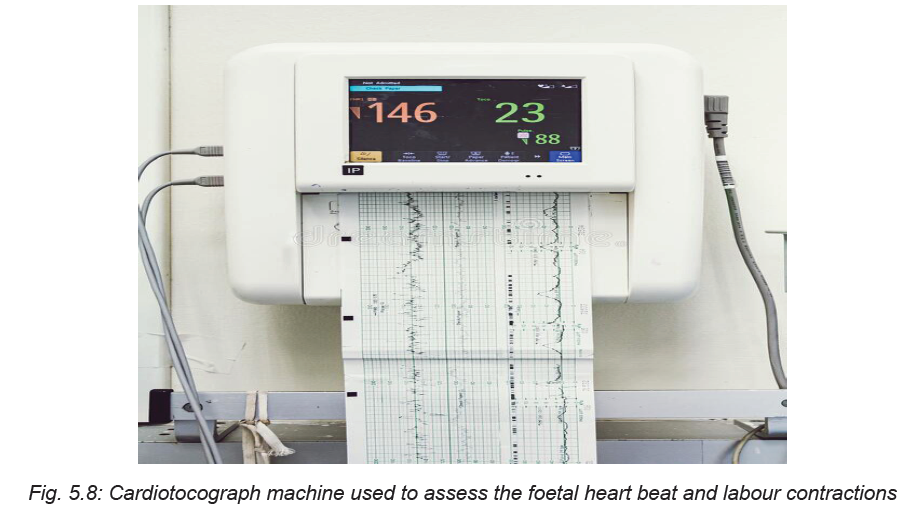
a. What is the role of the machine pictured above?
b. Why is it important to assess the foetal wellbeing during the second stage
of labour? of labour?
A foetus is at a high risk of being exposed to maximum hypoxic stress during second
stage of labour, due to a combination of maternal expulsive efforts and their impact
on the uteroplacental circulation, as well as repetitive and sustained compression
of the umbilical cord and the foetal head. Since this can lead to physiologic stress
for the foetus and hypoxic ischemic encephalopathy and foetal death, frequent
monitoring of foetal status is performed to detect early the onset of foetal hypoxic
stress. It is recommended to monitor foetal heart rate in low risk women for every
15 minutes in the active phase of the first stage of labour and every 5 minutes in
the second stage of labour and it is easiest to hear, by auscultating immediately
after a contraction. The care provider should have the skills to interpret the foetal
heart rate and take appropriate action when needed. Foetal heart rate can range
between 120 and 160 times a minute during labour.
At times, the heart may be as fast as 180 beats per minute (Tachycardia) or as slow
as 100 beats per minute (Bradycardia). Once these abnormal heart beat trends
are detected, the skilled attendant has to intervene in order to normalise these
irregularities in the foetal heart beating by for instance assisting the mother to lie incomfortable position.
Table 5.2: Causes of bradycardia
When the baby’s heartbeat is slow after a contraction is over but then goes back to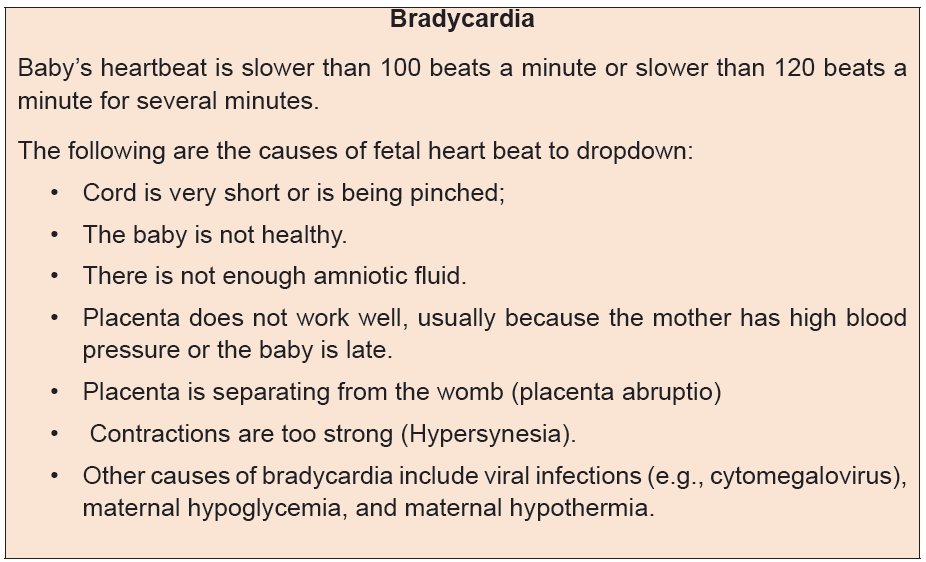
normal, the baby may be having trouble. The skilled attendant has to listen to several
contractions in a row. If the heartbeat is normal after most other contractions have
ended, there is a possibility that the baby’s heart is beating normally. However, the
skilled birth attendants should ask the mother to change position to take pressure
off the cord. They also have to listen again after she moves to see if this helps, and
keep checking the baby’s heartbeat often during the rest of labour to see if it slows
down again.Table 5.3: causes of tachycardia
If the baby’s heartbeat stays fast for 20 minutes (or 5 contractions), get medical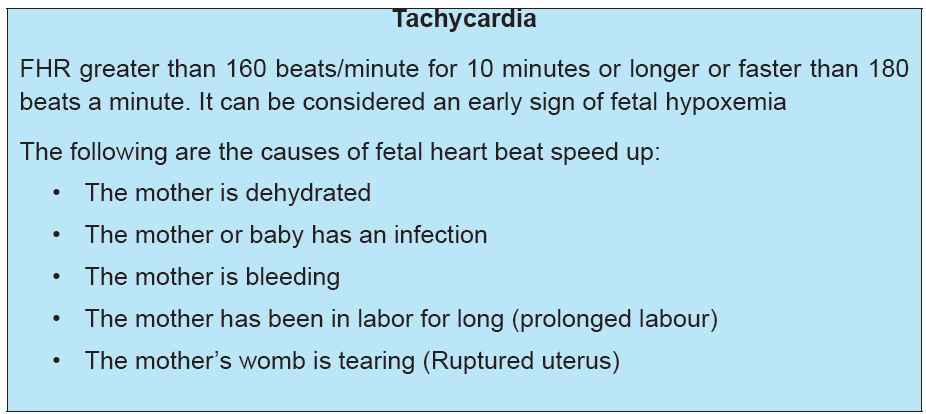
help.
Self-assessment 5.1.5
i) What is the normal foetal heart beat?
ii) Mention some of the conditions that cause foetal bradycardia.
iii) Mention some of the conditions that cause foetal tachycardia.
iv) What is the range of a slowing foetal heart rate?
v) What is the range of a speedy foetal heart beat?5.1.6. Recognising foetal compromise during second stage of labour
Learning Activity 5.1.6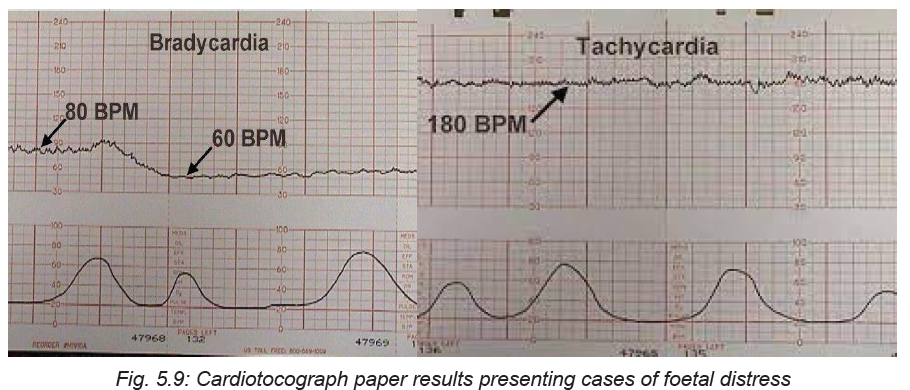
Referring to the two CTG paper results shown on the above images, answer the
following questions:
i) What is the difference between the two results of the foetal heart displayed?
ii) Which of the above results may require medical attention and why?
Foetal compromise or foetal distress is when the baby is not well due to inadequate
oxygen during labour. Foetal compromise is caused by a number of factors
including placental insufficiency, uterine hyperstimulation, maternal hypotension,
cord compression, placental abruption, uterine rupture, and foetal sepsis. It can
also be caused by problems with the umbilical cord namely cord compression.
Foetal distress can also occur in case the mother has a health condition such as
diabetes, kidney disease or cholestasis. At some point, foetal distress can happen
as a result of contractions that are too strong or too close together.
Foetal distress is diagnosed by reading the baby’s heart rate. Another sign is
to check if there is meconium in the amniotic fluid. If the amniotic fluid is green
or brown, this signals the presence of meconium. A slow heart rate, or unusual
patterns in the heart rate, may signal foetal distress. Continuous cardiotocograph
(CTG) monitoring is recommended when either risk factors for foetal compromise
have been detected antenatally, at the onset of labour or develop during labour. A
CTG associated with a low probability of foetal compromise and is characterised by
the features presented in following tablesTable 5.4: CTG Characteristics
The following features are unlikely associated with foetal compromise when
occurring in isolation:
– Baseline rate 100-109 bpm
– Reduced or reducing baseline variability (3-5 bpm)
– Absence of accelerations
– Early decelerations
– Variable decelerations without complicating features.
– The following features may be associated with significant fetal compromise
and require further action:
– Baseline fetal tachycardia >160 bpm
– Rising baseline fetal heart rate (FHR), including where the fetal heart rate
remains within normal range
– Complicated variable decelerations
– Late decelerations
– Prolonged decelerations (a fall in baseline FHR for >90 seconds and up to 5
minutes).
The first step to manage foetal compromise is to give the mother oxygen and oral
and intra venous fluids. In addition to this, the mother can be assisted to move
position, such as turning onto one side, can reduce the baby’s distress. If the
woman had been given drugs to speed up labour, these may be stopped if there are
signs of foetal distress. If it is a natural labour, the woman can be given medicationto slow down the contractions. A baby in foetal distress needs to be born quickly.
Self-assessment 5.1.6
i) What are the maternal related possible causes of foetal compromise during
the second stage of labour?
ii) When the foetal heart rate is recognised as abnormal?iii) What major interventions are performed if foetal distress is diagnosed?
5.1.7. Duration of the second stage of labour
Learning Activity 5.1.7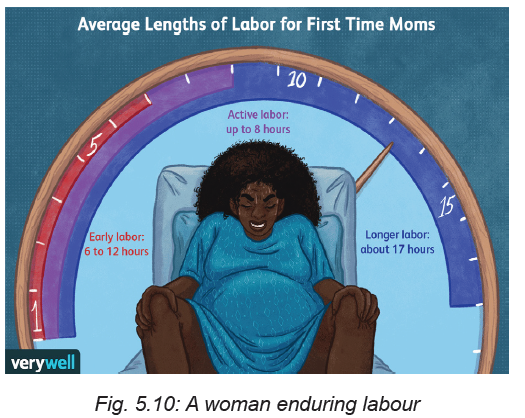
Using your prior knowledge, answer the following questions:
i) What is the estimated duration of second stage of labour?
ii) What are the maternal and foetal factors influence the second stage of
labour?
The second stage of labour commences with full dilation of the cervix and ends
with the birth of the baby. The median duration of second stage of labour is 50
to 60 minutes in nulliparous women and 20 to 30 minutes in multiparous women.
The upper limits for the duration of normal second-stage labour are 2 hours for
nulliparous women and 1 hour for multiparous women. The duration of the second
stage is variable and the length of this stage may be influenced by several factors
such as parity, maternal size and foetal weight; position, and descent; the type
and amount of pain relief administered, the frequency, intensity, and duration of
contractions, maternal efforts in pushing, and the support the woman receives
during labour.
The second stage of labour is subdivide into two phases: the latent or labouring
down phase (period of rest and relative calm) and the active pushing or descent
phase (woman has strong urges to bear down). Maternal verbal and nonverbal
behaviours, uterine activity, the urge to bear down, and foetal descent characterize
these two phases. Table 5.5 presents the expected maternal progress for each
phase and the average duration it may take.
Table 5.5. Expected Maternal Progress in theSecond Stage of Labour
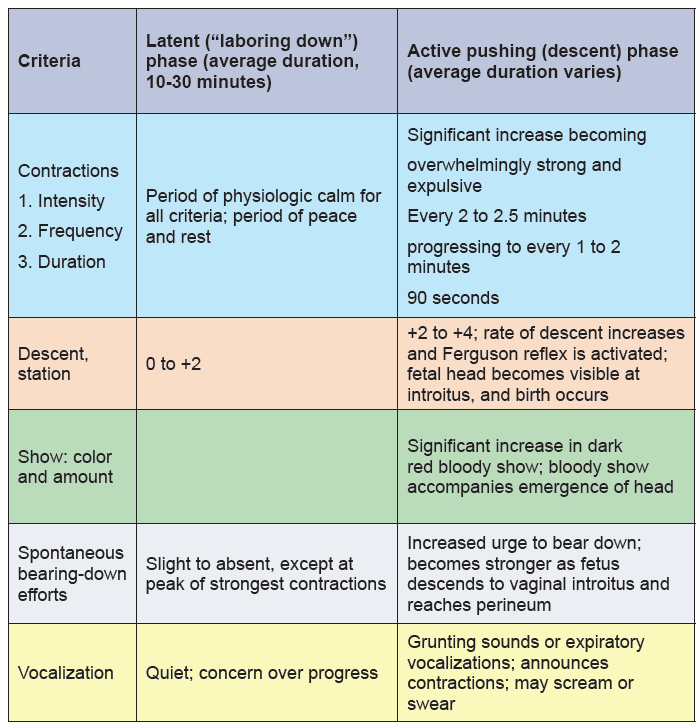
Self-assessment 5.1.7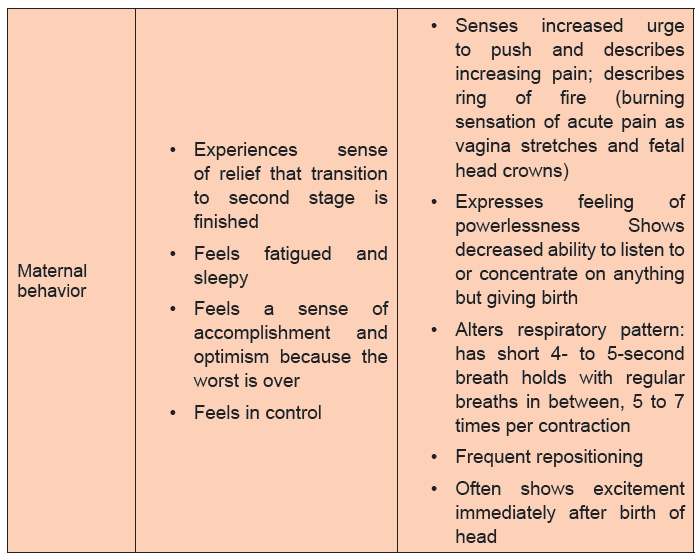
i. Using concrete examples, discuss how long is the second stage of labour
expected to last?
ii. What are the phases of the second stage of labour?
iii. Outline the criteria used to characterise the phases of the second stage of
labour.
iv. How bearing down effort is differs from each other in those phases?v. What are the factors influencing the length of the second stage of labour?
5.1.8. Reducing risks during second stage of labour
Learning Activity 5.1.8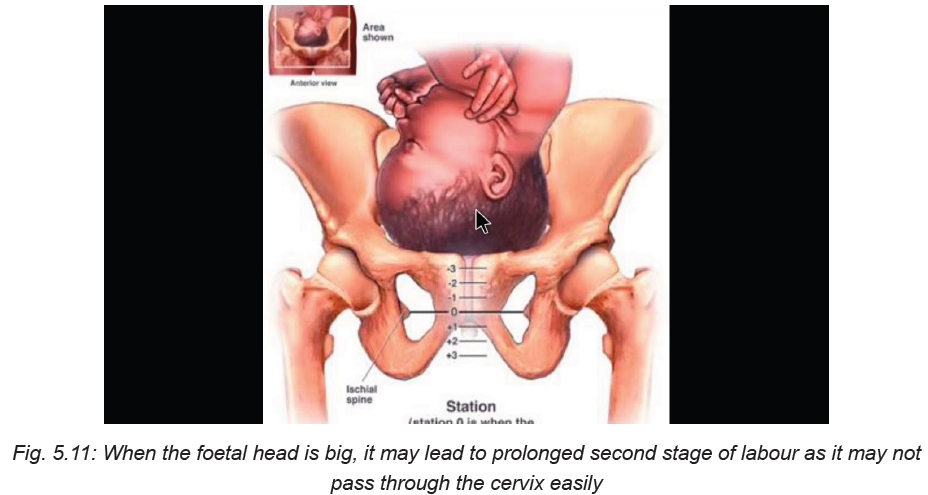
Using your prior knowledge, books, and the picture above, answer the following
questions
a) What risks may likely occur during the second stage of labour?
b) What is the main cause of risk during the second stage of labour?
The second stage of labour is very demanding for both the woman and the foetus.
When the second stage of labour is not optimally managed, the woman’s and
foetus’ life may be at risk. Complications that may occur during the second stage
of labour include but are not limited to abnormal foetal heart rate patterns, infection
particularly following membrane rupture, stillbirth, neonatal asphyxia, meconium
aspiration syndrome, fatigue, and neonatal birth injury example branchial plexus
paralysis. For the woman, some of the common risks that may occur during the
second stage of labour include chorioamionitis (membrane infection), tears (cervical
or perineal), urinary retention, increased rate of caesarean birth, and future urinary
incontinence.
Most of the risks that affect the woman and her baby result from prolonged labour.
For this reason, close monitoring and skills and capacity to offer timely intervention
are required for all births to prevent adverse maternal and neonatal outcomes such
as stillbirth and newborn complications arising from undetected hypoxia, as well as
maternal mortality and morbidity from complications such as vesicovaginal fistula,
genital tract lacerations, infection, haemorrhage, and worsening of hypertensive
disorders. In order to prevent complications associated with the delayed second
stage of labour, skilled birth attendants must not leave the labouring woman alone
after the late first stage has commenced.
Because of the increase in foetal lactate levels after the onset of active maternal
pushing, continued active maternal pushing for more than 60 minutes should be
avoided, unless a spontaneous vaginal birth is imminent and the foetal heart rate
monitoring does not show any evidence of ongoing foetal compromise. The skilled
birth attendants have to encourage active pushing once the woman’s urge to bear
down is present. They should assist the woman to adopt any position of their
preference for pushing, except lying supine which risks aortocaval compression
and reduced uteroplacental perfusion. The skilled birth attendants should listen
to the foetal heart rate frequently (at least 1 minute every 5 minutes) in between
contractions to detect bradycardia. The caring team also has to check the maternal
pulse and blood pressure, especially where there is a pre-existing problem of
hypertension, severe anaemia, intrapartum haemorrhage or cardiac disease. To
minimise prolonged second stage of labour, the frequency, strength and duration of
uterine contractions are observed, as well as the relaxation of the uterus between
contractions. The amniotic fluid is observed for meconium staining. The birth
attendant must not allow the mother’s bladder to become distended. The woman’s
bladder must always be assessed for fullness and she should be encouraged to
void if fullness of bladder is found.
Self-assessment 5.1.8
What precautions can be undertaken to prevent the risks occurring in the secondstage of labour?
5.2 Management of third stage of labour
5.2.1 Introduction to the third stage of labour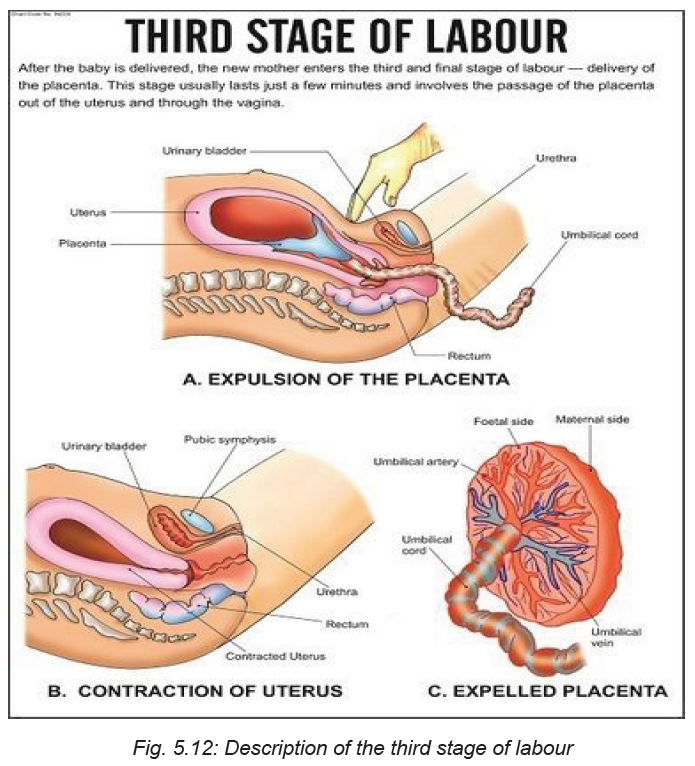
Learning Activity 5.2.1
Watch the video titled ‘Managing the Third Stage of Labour - Childbirth Series’
found on this link:and answer
the following questions:
i) What do you understand by the third stage of labour?
ii) What happens during the third stage of labour?
The third stage of labour is the period extending from the second stage of labour
the completed birth of the new-born until the completed delivery of the placenta.
Once a baby is born, the womb (uterus) continues to contract, causing the placenta
to separate from the wall of the uterus and then mother delivers it.
When the woman gives birth normally, the third stage is when natural physiological
processes spontaneously deliver the placenta and fetal membranes. For this to
happen without problem, the cervix must remain open and there needs to be good
uterine contractions. In the majority of cases, the processes occur in the following
order:
1. Separation of the placenta: The placenta separates from the wall of uterus.
As it detaches, blood from the tiny vessels in the placental bed begins to clot
between the placenta and the muscular wall of the uterus.
2. Descent of the placenta: After separation, the placenta moves down the
birth canal and through the dilated cervix.
3. Expulsion of the placenta: The placenta is completely expelled from the
birth canal.
This expulsion marks the end of the third stage of labour. Thereafter, the muscles
of the uterus continue to contract powerfully and thus compress the torn blood
vessels.
Thus the management of the third stage of labour entails the period after the birth
of the baby to help the uterus contract or return to normal, clamping the cord, and
controlled cord traction to deliver the placenta.
a) Why third stage of labour important in the care of the expectant woman
Most of the conditions that lead to maternal morbidity and even deaths occur during
the third stage of labour if the woman does not receive optimal care. Some of the
major contributors of maternal deaths, postpartum haemorrhage and sepsis can be
associated with limited proper management of the third stage of labour. When the
placenta remains inside the uterus for longer than 30 minutes after the birth of the
baby due to inadequate uterine contractions, and the rapid retraction of the cervix
which traps the placenta into the uterus, and full bladder obstructing placental
delivery can all contribute to excessive bleeding after birth.
b) How is the third stage of labour managed?
There are two options applied to manage the third stage of labour: active management
and physiological management. The physiological management is general practised
in midwife-led units and in home births. This management approach of the third stage
of labour allows the placenta to be delivered only by pushing, gravity, contractions
and sometimes by nipple stimulation. This management technique does not rely
on the use of oxytocin injections. The umbilical cord is clamped and cut once it
has stopped pulsing or when the placenta comes out. Normally the physiologic
management of the third stage of labour takes up to one hour. This requires that
the health care team helps the mother to initiate skin-to-skin contact with the baby
while breastfeeding him/her in order to stimulate more natural oxytocin production.
The physiological management of the third stage of labour is only advised if there
is no risk for the woman to bleed heavily after the birth of the baby.
The second approach and which is mostly used especially in most developing
countries is the active management of the third stage of labour. This approach
is recommended by the World Health Organisation because of it is effective in
reducing the risks of the complications of the poor management of the third stage
of labour. When applying the active management of third stage of labour, the caring
team does not wait for the spontaneous placental delivery. Instead, the interventions
are prompt and follows the following sequential order:
• Just after the baby is born, the midwife/or nurse puts the baby on the mother’s
abdomen in skin to skin contact with her;
• The midwife or nurse clamps the baby’s umbilical cord at two sites and cuts
it in between;
• Check the uterus to find out if there is any second baby;
• In less than one minute, administer a uterotonic drug to make the uterus
contract more powerfully;
• Apply controlled cord traction;
• After delivering the place, immediately start massaging the uterus;
• Examine the placenta to make sure it is complete and there are no retained
parts of the placenta in the uterus;
• Examine the woman’s vagina, perineum and external genitalia for anylacerations and active bleeding.
Self-assessment 5.2.1
iii) Explain in orderly sequence the three processes characterising the third
stage of labour.
iv) Why is it important for health professionals to take much care when
managing the third stage of labour?
v) Mention at least three things that can happen if the third stage of labour is
not appropriately managed.
Homework 5.3
Go to the internet, read an extract about uterotonic drugs from the book titled
‘Uterotonic drugs to prevent postpartum haemorrhage: a network meta-analysis’found on this link: https://www.ncbi.nlm.nih.gov/books/NBK537857/
5.2.2. Administration of uterotonic drugs
Learning Activity 5.2.2
Based on the information you read in the book ‘Uterotonic drugs to prevent
postpartum haemorrhage: a network meta-analysis’, what do you understand by
the term ‘uterotonic drugs’?
i) Why is it important to administer uterotonic drugs during the third stage of
labour
ii) Mention some of the examples of uterotonic drugs you have read?
Introduction to uterotonic drugs
Uterotonic drugs are medications given to the woman in order to stimulate the uterus
to contract or to increase the frequency and intensity of the uterine contractions.
When administered, these drugs stimulate the placenta to separate from the
uterine wall to be delivered. Uterotonic drugs, when given to the woman during the
third stage of labour act as one of the interventions package to prevent postpartum
haemorrhage. Uterotonic drugs include oxytocin, ergometrine, misoprostol,
carbetocin, prostaglandins, and ergot alkaloids, but the three frequently used
uterotonic drugs are oxytocin, prostaglandins, and ergot alkaloids.Uterotonic drugs have a number of advantages as shown in figure below:
Table 5.6: Advantages of uterotonic drugs
How to give uterotonic drugs
The uterotonic drugs can be used in all stages of childbirth when needed. In the
case of the third stage of labour, the uterotonic drugs are indicated as one of the vital
interventions of the active management of third stage of labour. When providing
uterotonic drugs, the nurse has to consider the following:
1) Administer uterotonic drugs immediately after the birth of the baby before
performing cord clamping and cutting the cord.
2) Before giving uterotonic drug to the woman, the nurse has to perform
abdominal palpation to find out if there is no any other baby. This is because,
if for instance oxytocin is administered when there is a second baby, there is
a risk that the second baby could be trapped in the uterus.
3) Administration of uterotonic drug of the choice is given after confirmation
that no any other baby inside the uterus and is given with 1 minute after
childbirth. The uterotonic of choice is oxytocin 10IU IM. The dose given to
the woman is usually IM: 10 units if a woman has an IV when she gives birth.
The nurse can either give 10 IU IM or 5 IU by slow IV injection.
4) Controlled cord traction is applied with counter-pressure on the uterus to
deliver the placenta.
Any health worker administering or dispensing the uterotonic drug should be
authorized to do so and be trained in the proper use of the drug and management of
side and adverse effects. Clear documentation of administration of any uterotonic
drugs should be part of the woman’s medical record. Documentation includes the
time, route, and dosage of any medications given, as well as a record of any side
effects.
Contraindication of uterotonic drugs
Most of the uterotonic drugs have no known contraindications when administeredin the third stage of labour.
Self-assessment 5.2.2
i) Which uterotonic of choice is used in active management of third stage of
labour?
ii) What are the advantages of using uterotonic in third stage of labour?5.2.3. Cord clamping and cutting
Learning Activity 5.2.3
Watch the video found on this link:
and answer the following questions.
i) Why do you think it important to clamp the cord after the birth of baby?
ii) Based on what you have seen in the video, describe the steps involved incord clamping.
Introduction
The umbilical cord, is typically made up of two arteries and one vein and covered
in a thick gelatinous substance known as Wharton’s Jelly. The main function of
the umbilical cord is to pass oxygen and nutrients from the mom to the baby and
to transport waste away from the baby to the mother via the placenta. Most of the
time, there is no need to cut the cord right away. Leaving the cord attached will help
the baby to have enough iron in his blood. It will also keep the baby on his mother’s
belly where the baby belongs. When the baby is just born, the cord is fat and blue. If
you put your finger on it, you will feel it pulsating. This means the baby is still getting
oxygen from his mother.
When the placenta separates from the wall of the womb, the cord will get thin and
white and stop pulsating and at this time it will not be facilitating blood circulation to
the baby from the mother. As a result the cord can be clamped, usually after about
3 minutes in order to separate the baby from the placenta. When this is done, it
facilitates the baby’s organs to start adapting to the new environment other than its
mother’s womb.
There are two approaches of clamping the cord; i) early clamping which is usually
carried out in the first 60 seconds and ii) late cord clamping carried out more than
one minute after the birth of the baby or when the cord pulsation has stopped.
The latter approach, often called delayed umbilical cord clamping, according to the
World Health Organisation facilitates placental-to-new-born transfusion and results
in an increased neonatal blood volume at birth. In addition, delayed umbilical cord
clamping may be particularly relevant for infants living in low-resource settings with
less access to iron-rich foods and thus greater risk of anaemia.
Benefits of delayed cord clamping
The evidence further shows that delayed cord clamping can have immediate and
long term benefits for babies. In preterm infants, delayed umbilical cord clamping
is associated with significant neonatal benefits, including improved transitional
circulation, better establishment of red blood cell volume, decreased need for blood
transfusion, and lower incidence of necrotizing enterocolitis and intraventricular
haemorrhage. Furthermore, delayed cord clamping further promotes cerebral
oxygenation. For term infants, delayed cord clamping can provide adequate blood
volume and birth iron stores to the baby. It further increases haemoglobin amounts
in the term infants. For the mothers, delayed clamping can decrease the incidence
of retained placenta.
Procedure for cord clamping and cutting
Before starting the procedure of cord clamping and cutting, the health provider hasto make sure that he/she has access to the following medical supplies:
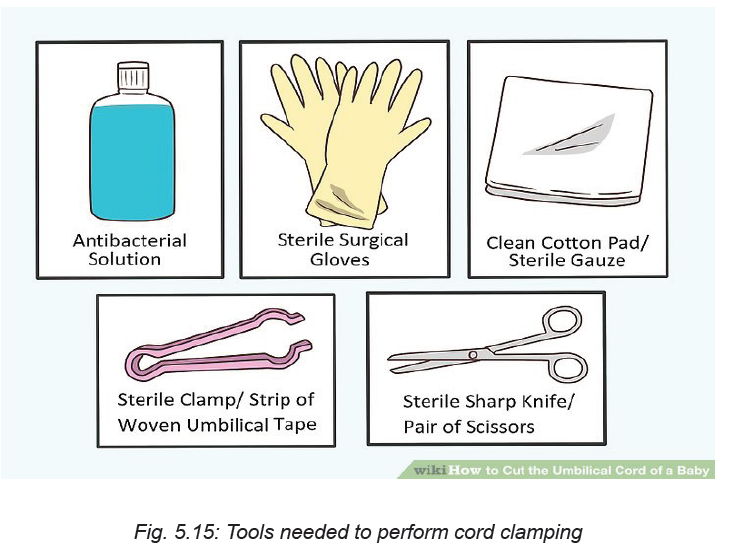
• An antibacterial solution.
• Sterile surgical gloves
• A clean cotton pad or (preferably) sterile gauze
• A sterile clamp or strip of woven umbilical tape
• A sterile sharp knife or pair of scissors
Once you have collected all the medical supplies together, the health provider has
to check if the cord is wrapped around the newborn’s neck.
If so, slide your finger under the cord and gently pull it over the newborn head. Next,
use sterile plastic clamps or sterile woven umbilical tape to tie off the cord (see the
image below).
Put the first tie of the clamps about 3 cm from the baby. The second tie should be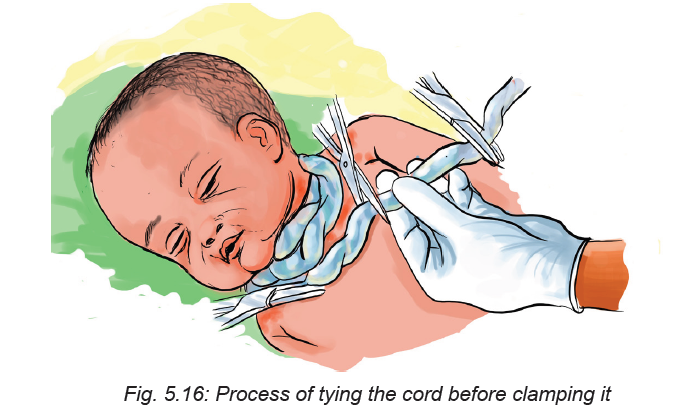
placed further away from the baby, about 5 centimetres from the first tie. Keep in mind
that although a pulse in the umbilical cord may stop shortly after delivery, significant
bleeding may still occur if the cord is not clamped or tied. Prepare the umbilical cord
by swabbing between the clamps or ties with antibacterial solution. You can use
betadine or chlorhexidine. This step should be done especially if delivery occurs
in a public or unhygienic setting. Use a sterile, sharp blade such as a scalpel or a
strong pair of scissors.
The umbilical cord is much tougher than it looks, and will feel like rubber or gristle.
Grasp the cord with a piece of gauze. The cord may be slippery so this will ensure
you have a firm grip on the cord.
Cut cleanly between the ties or clamps. Make sure you hold the cord firmly to
ensure the cut is clean.
Self-assessment 5.2.3
i) Define the term delayed cord clamping and explain why it is important to
delay cord clamping.
ii. What should a nurse do before clamping the cord?5.2.4 Controlled cord traction
Learning Activity 5.2.4
Watch the video titled ‘Placental delivery by controlled cord traction’ found on
this link:and answer the following
questions.
i) What do you understand by controlled cord traction?
ii) Why is important to perform controlled cord traction?
iii) Describe each step involved in controlled cord traction.
Controlled cord traction (CCT) can be defined as traction applied to the umbilical
cord once the woman’s uterus has contracted after the birth of her baby, and her
placenta is felt to have separated from the uterine wall. Counter-pressure is at the
same time applied to her uterus beneath her pubic bone until her placenta delivers.
Controlled cord traction is used to stabilise and deliver the placenta.
This method involves a number of steps in order the technique to be effectively
done.
Controlled cord traction involves the following steps:
• Clamp the cord close to the perineum and hold in with one hand.
• Place the other above the woman’s pubic bone and stabilise the uterus by
applying counter-pressure during controlled cord-traction
• Keep sight tension on the cord and wait for the strong uterine contraction (2-3
minutes) encourage the mother to push and very gently pull down the cord to
deliver the placenta and continue with counter-pressure to the uterus.
• If the placenta does not descend during 30-40 second of controlled cord
traction do not continue to pull on the cord.
• Gently hold the cord and wait until the uterus is well contracted again; with the
next contraction, repeat controlled cord traction with counter-pressure
• Never apply cord traction (pull) without applying counter traction (push) above
the pubic bone on a well-contracted uterus.
• As the placenta delivers, hold the placenta in two hands and gently turn it until
the membranes are twisted.
• Slowly pull to the placenta delivery
• If the membranes tear, gently examine the internal and external genitalia
wearing the sterile gloves and use sponge holding forceps to remove
fragments of membranes that are present.
• Examine carefully the placenta to rule out any missing portion of it, if you
suspect retained portions on maternal surface or tone membranes take
appropriate action.
Contraindication of controlled cord traction
The nurse should at all costs avoid controlled cord traction if there are no uterotonic
drugs available. Controlled cord traction is also contraindicated prior to signs of
separation of the placenta as this can cause partial placental separation, a rupturedcord, excessive bleeding, and/or uterine inversion.
Self-assessment 5.2.4
i. What should one avoid while doing controlled cord-traction?
ii. What important technique one should do after delivering the placenta
during controlled –cord traction?iii. In what situations controlled cord traction is contraindicated?
Homework 5.4
Go to the library and read the book titled ‘A Book for Midwives: Care for pregnancy,
birth, and women’s health’ chapter 12, from page 226 to 230.5.2.5 Delivery of the placenta
Learning Activity 5.2.5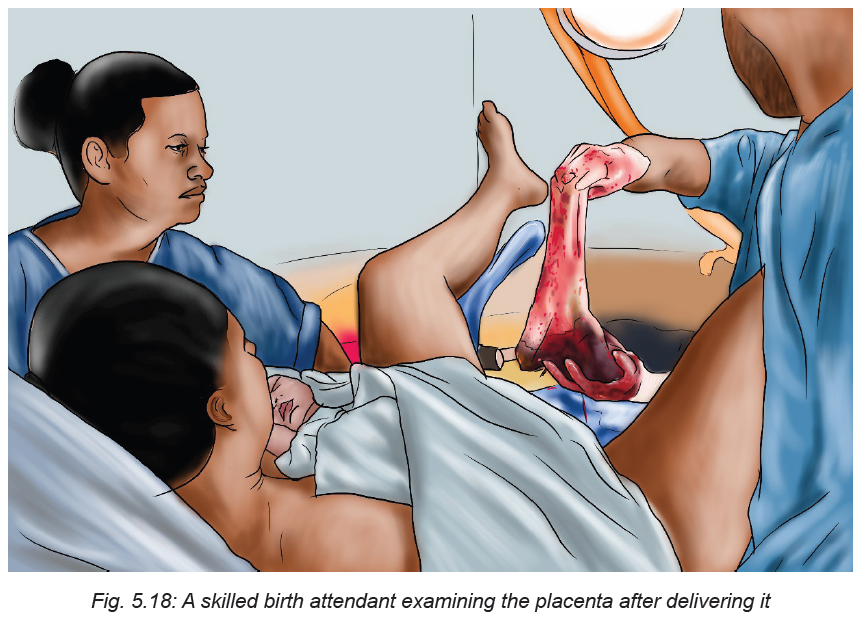
i) What should the nurse do before starting the delivery of the placenta?
ii) What signs should the nurse check to make sure if the placenta hasseparated from the uterine wall?
Before going into the details of placenta delivery, it is essential to understand the
biological events that lead to the delivery of the placenta. The placenta normally
separates with the third or fourth strong uterine contraction after the birth of the
baby. After the birth, the nurse must watch the mother for any signs of infection, preeclampsia,
and heavy bleeding. The nurse has to also check the mother’s blood
pressure and pulse within the 30 minutes after birth.
In spontaneous vaginal birth, the placenta usually separates from the womb in the
first few minutes after birth. However, in some cases it may take some time to come
out. In order to ascertain that the placenta has separated from the uterus, the care
provider has to check the following signs:
• A small gush of blood comes from the vagina. A gush is a handful of blood that
comes out all at one time.
• The cord looks longer because when the placenta comes off the wall of the
uterus, it drops down closer to the vaginal opening which makes the cord
seem a little longer because more of it appears outside the woman’s body.
• Check if the uterus has risen. This should be checked because when the
placenta separates from the uterine wall, the top of the uterus moves a little
below the mother’s navel.
If 30 minutes have elapsed since the birth of baby and there are no signs that the
placenta has separated from the uterus, the care provider should check if the baby
has started breastfeeding. Breastfeeding causes contractions and will help the
uterus push the placenta out. If the placenta does not deliver after breastfeeding,
request the mother to urinate because a full bladder can slow the birth of the
placenta.
If the placenta does not deliver by itself or if the mother is bleeding heavily, the
care provider has to deliver it. The care provider helps the mother sit up or squat
over a bowl. He/she asks her to push when she feels a contraction and the woman
can also try to push between contractions and the placenta will slip out easily. The
membranes (or bag) that holds the waters and the baby should come out with the
placenta.
Steps in delivering the placenta
Attempt delivery of the placenta only when it is fully separated from the uterus to
avoid uterine inversion or pulling off a section of placenta from the wall of the uterus
leaving the remainder attached, thus creating an open bleeding area in the uterine
wall.
The nurse has to check for separation of the placenta from the uterine wall by doing
the following:
• Placing the hand over the uterus through the abdominal wall (inside a folded
sterile towel) to note when the uterus contracts into a hard globular ball which
rises slightly under your hand.
• Requesting the mother to tell you, after the delivery of the baby, when she
next has contractions.
• Noting whether there is a small gush of blood and/or lengthening of the cord.
• Noting the time of the birth of the baby so you know how long you have waited
for separation of the placenta.
• If you are uncertain whether the placenta has actually separated, you may
also follow the cord with your hand in the vagina, up to the cervix, to determine
if the placenta is trapped in the cervical os, or whether the cord disappears
into the uterus.
Some precautions to take when delivering the placenta
♦ When the woman is bleeding a lot and cannot push the placenta out herself,
gently guide the placenta out by the cord.
♦ But, if the woman is not bleeding and there is no any danger for both the
woman and the baby, do not pull on the cord. Since the placenta is still
attached to the uterus, the cord may break or you may pull the woman’s
uterus out which may result in death. Only guide the placenta out by the cord
if you are sure that the placenta has separated.
♦ If any part of the placenta is missing, immediately report this finding to
the attending physician for intervention. Retained placental fragments cancontribute to postpartum haemorrhage or sepsis.
Self-assessment 5.2.5
i) Explain the steps involved in the delivery of the placenta by a nurse/or any
care provider.
ii) What precautions should a nurse take when delivering the placenta?
5.2.6 Uterine massage
Learning Activity 5.2.6
Using different sources of information, answer the following questions:
a) What do you understand by the term uterine massage?
b) When do we need to apply uterine massage of labour?
Introduction to uterine massage
Uterine massage is one of the interventions to manage the third stage of labour
especially after the birth of the baby and after the placenta had been delivered.
Light massage of the abdomen is performed in order to stimulate the uterus contract
in order for it to return to its normal size. The uterine massage is advantageous
because it helps in preventing massive blood loss after childbirth which can lead to
both maternal morbidity and mortality rate.
How long the uterine should be done
Uterine massage should be done immediately after third stage of labour in
spontaneous vaginal delivery.
Techniques of offering uterine massage
• Before performing uterine massage, advise the woman to empty her bladder.
A full bladder may push the uterus off to the side, which makes the massage
process both uncomfortable and ineffective.
• Ask the woman to relax her body as much as possible. The skilled birth
attendant guides the woman to practice deep breathing and muscle relaxation
immediately prior and during the massage. The woman relaxes her muscle
and take slow, calm breaths to help with the potential discomfort.
• The nurse places a hand on the woman’s lower abdomen and stimulates the
uterus by massaging.
• Ask the woman to lie down flat.
Once, she is lying flat on her back, place your flat palms on her abdomen at about
where her belly button is located. If her uterus is hard, you should not need to
massage the area. If the area is soft and you feel little resistance, a massage maybe recommended.
Take one hand and cup it slightly. Slowly move it in a circular motion over the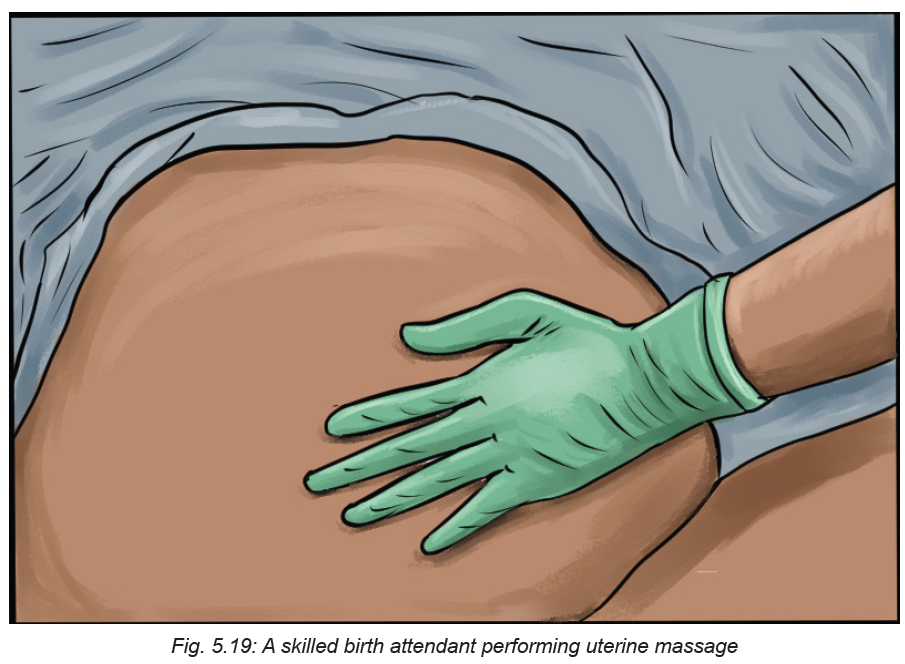
woman’s lower abdomen. Keep doing these movements until you feel her uterus
contract.
Self-assessment 5.2.6
i. When should we do uterine massage and for how long.
ii. What are the advantages of uterine massage?
iii. Briefly describe the steps involved in offering uterine massage.
iv. What precautions does a nurse should take prior and during uterinemassage?
End unit assessment 5
1. When is the second stage of labour starts and ends?
2. What are the signs indicating that the second stage of labour has begun?
3. What elements of monitoring during the second stage of labour?
4. Explain the following the following terms:
a. Engagement
b. Descent
c. Flexion
d. Internal rotation
e. Extension
f. External rotation
g. Expulsion.
5. Explain in orderly sequence the three processes characterising the third
stage of labour?
6. Why the active management of the third stage of labour is more effective
than the physiological management of the third stage of labour?
7. Which uterotonic drug of choice is used in active management of third
stage of labour?
8. What are the advantages of using uterotonic in third stage of labour?
9. Mention all uterotonic you know that can be used in third stage of labour.
10. What is the importance of delayed cord clamping in third stage of labour?
11. Describe each step involved in cord clamping.
12. What should one avoid while doing controlled cord-traction?
13. What important technique one should do after delivering the placenta
during controlled –cord traction?
14. In what situations controlled cord traction is contraindicated?
15. What should the nurse do before starting the delivery of the placenta?
16. What are the signs of placenta separation during third stage of labour?
17. Describe the steps involved in the delivery of the placenta?
18. What precautions should a nurse take when delivering the placenta?
19. When should we do uterine massage and for how long.
20. What are the advantages of uterine massage?
21. What precautions does a nurse take prior and during uterine massage?
Multiple choice questions
1. What is the drug of choice in active management of third stage management?
a) Intravenous Ergometrine
b) Intramuscular egometrine
c) Intramuscular oxytocin (Pitocin)
d) Misoprostol
2. The following are the causes of prolonged third stage of third stage except
a) Failure of the uterus to contract well
b) Abnormal placenta insertion. e.g. placenta accreta
c) Cord prolapse.
d) Failure of the placenta to separate normally.
3 Which ONE of the following options outlines the causes of postpartum
haemorrhage in third stage of labour?
a) Uterine atony, uterine inversion and Full bladder
b) Not well repaired episiotomy, clitoral tears, recto prolapse
c) Vaginal tears, perennial tears and contracted uterus
d) None of the above.
4. Normal third stage will involve the following stages except
a) placenta separation,
b) placenta descent
c) placenta expulsion
d) placenta insertion
5. Answer the following questions with true or false
a) In active management of third stage of labour oxytocin should be given
immediately after childbirth wit out palpating to find out if there is another
baby.
b) Retained placenta is not a danger sign in third stage of labour.
c) Postpartum haemorrhage is defined as blood loss of 500mls in spontaneous
vaginal delivery and 1000mls in caesarean section.
d) Prolonged third stage is when the placenta fails to separate within 2 hours
after child birth.
e) Full bladder causes postpartum haemorrhage
f) Full bladder causes postpartum haemorrhage.
Controlled cord traction is not contra-indicated before the signs of placenta
separation are noticed.
6. Answer the following questions with true or false
a)In active management of third stage of labour oxytocin should be given
immediately after childbirth wit out palpating to find out if there is another
baby.b)Full bladder causes postpartum haemorrhage.
UNIT 6IMMEDIATE CARE OF A NEWBORN
Key Unit Competence: Provide immediate care to the newborn
a. What do you think about these images demonstrating the care given to the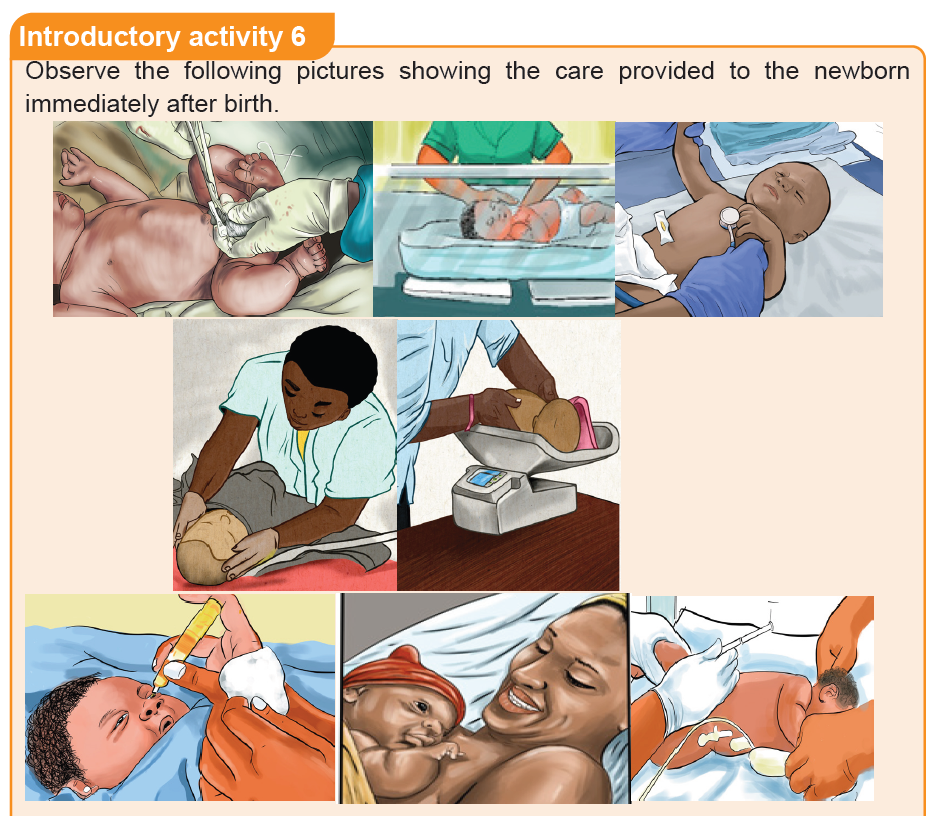
baby immediately after birth?
b. What do you think that it is necessary to have stethoscope and thermometer
while providing immediate newborn car?
c. What do you reflect to the image showing a health care provider injecting
the new-born baby?
d. What do you reflect about eye care to new born baby?
e. What do you think about the advantages of putting the baby on the mother’s
chest immediately after birth?
6.1. Concept of immediate care and components of essential
newborn care.Learning Activity 6.1
As associate nurse, you are called to care and provide essential newborn care
for a baby who was born just 3 minutes ago. While caring for that baby what can
be done to prevent hypothermia from evaporation, conduction and convection?
Based on the case described above,
a) When do you think immediate newborn care start from?
b) What do you think could be done to prevent hypothermia?
c) What do you think about the terminology of early breastfeeding in the
immediate newborn care?
d) What do you think are essential newborn care?
Key components of the essential new born care at birth:
• Thermal care or maintenance of baby’s body temperature.
• Clearing of airways only when necessary not as routine.
• Eye care
• Cord care
• Breastfeeding with in the first hour of birth
• Administration of vitamin k
• Weighing the baby and record weight.
• Routine monitoring
• Additional care if the baby was exposed to HIV or HBV.
Newborn immediate care is the care given to the neonate after birth by qualified
personnel in the delivery room.
Essential newborn care refers to key routine practices in the care of the newborn,
particularly at the time of birth and over the first hours of life, whether in the health
facility or at home.
Essential newborn care includes:
• Thermal care (including prompt drying and maximizing skin-to-skin contact
and covering the baby at birth, delayed bathing, maintaining “warm chain”)
• Early initiation and exclusive breastfeeding
• Hygiene practices (including cord-care and caregiver hand washing).
There is good evidence that adherence to recommended essential newborn care
practices substantially reduce mortality risk, especially for very small newborns.
Health service contacts (notably associated with antenatal care and the hospital
admission for childbirth) are important opportunities to influence these practices. In
some settings, community health workers (CHWs) can serve as important channels
to influence adoption of these practices among pregnant women.
Thermal protection and care of newborns:
All measures used by healthcare providers to prevent or manage hypothermia to
the newborn baby. Hypothermia contributes to neonatal morbidity and mortality.
Thermal protection and care is recommended as it reduces hypothermia, a
condition in which the body temperature falls below 36 degree Celsius. The
recommended thermal care practices include immediately drying and wrapping of
the baby; bathing practices such as delaying for at least 6 hours and using warm
water; day to day care such as covering the baby’s head; and keeping the baby
skin-to-skin.
The newborn loses heat in four ways:
• Evaporation: when amniotic fluid evaporates from the skin.
• Conduction: when the baby is placed naked on a cooler surface, such as the
floor, table, weighing scales, cold bed.
• Convection: when the baby is exposed to cool surrounding air or to a draught
from open doors and windows or a fan.
• Radiation: when the baby is near cool objects, walls, tables, cabinets, withoutactually being in contact with them
Early initiation of breastfeeding: is referred as the provision of mother’s breast milk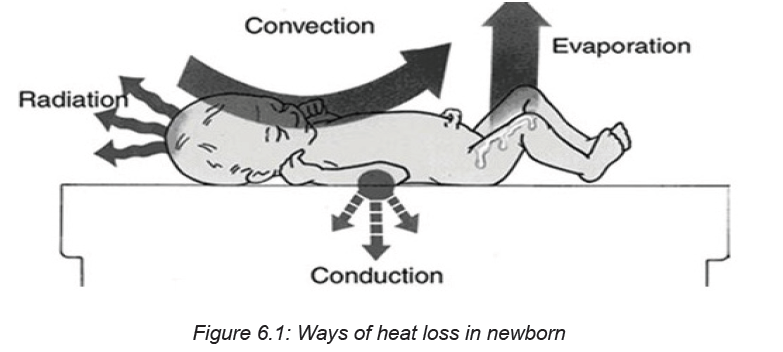
to infants within one hour of birth. This helps to ensure that the infant receives
the colostrum, or “first milk’, which is rich in protective factors. Early initiation of
breastfeeding, within one hour of birth, protects the newborn from acquiring infection
and reduces newborn mortality. It facilitates emotional bonding of the mother and
the baby and has a positive impact on duration of exclusive breastfeeding.
Newborn eye care
Newborn eye care is providing antibiotic eye drops or ointment in a newborn’s eyes
after birth. This is to protect babies from getting bacterial eye infections that can
be acquired during birth. Untreated, these infections can cause serious problems
including blindness. The antibiotic erythromycin and tetracycline are used most
often.
Umbilical Cord Care
The umbilical cord is the baby’s lifeline to the mother during pregnancy. However,
it’s no longer needed once the baby is born. Within a few minutes after birth, the
cord is clamped and cut close to the navel. The clamp helps stop bleeding from the
blood vessels in the umbilical cord.
Administration of vitamin K to newborn
Administering one intramuscular (IM) dose of vitamin K (0.5 mg for infants weighing
≤1,500 g or 1.0 mg for infants weighing >1,500 g) routinely to all newborns within the
first 6 hours post-birth and following initial stabilization and appropriate maternal/
newborn interaction, is now the recommended best practice. Vitamin K helps the
blood to clot and prevents serious bleeding. In newborns, vitamin K injections
can prevent a now rare, but potentially fatal, bleeding disorder called ‘vitamin K
deficiency bleeding’ (VKDB), also known as ‘hemorrhagic disease of the newborn’
(HDN).
Weighing the new born
According to the WHO, the average weight of a baby has born at 37–40 weeks
ranges from 2.5 to 4 kg. Newborns often lose around 226.8 g in the first 4 to 5 days
after birth but regain it by about 10 to 12 days of age. In the first month, the typical
newborn gains about 20 g a day, or about 110 g to 8 226.8 g a week.
Self-assessment 6.1
1. What are the key components of essential newborn care?
2. What is the importance of applying antibiotics drop/ ointments in the
newborn baby’s eyes immediately after birth?
3. What is done to protect the newborn baby against hypothermia?
4. Describe the 4 ways of loosing heat to the newborn baby after birth.6.2 APGAR score assessment
Learning Activity 6.2 APGAR SCOREObserve these images illustrating an associate nurse assessing APGAR SCORE
From the observation of above pictures,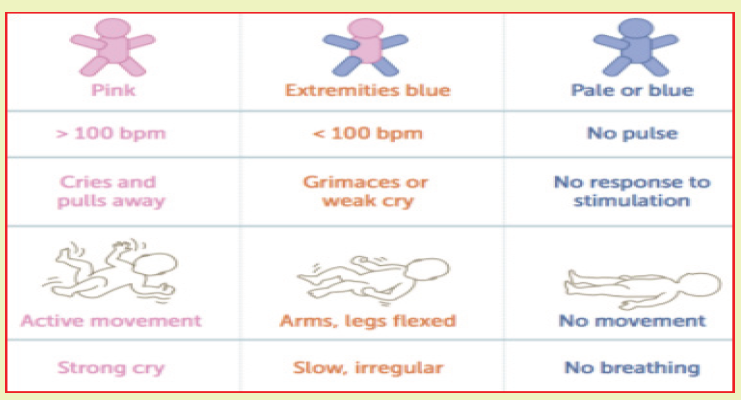
a. Have you come in contact with word APGAR SCORE previously? If yes
What is it?
b. What do you think about the importance of assessing APGAR score to the
newborn baby immediately after birth?
c. what do you think about APGAR at 5 minutes?
History and description of APGAR SCORE
One of the first assessments is a baby’s Apgar score. At one minute and five
minutes after birth, infants are checked for heart and respiratory rates, muscle tone,
reflexes, and color. This helps identify babies that have difficulty breathing or have
other problems that need further care.
Apgar is a quick test performed on a baby at 1 and 5 minutes’ score after birth, the
1 minute score determines how well the baby tolerated the birth process. The 5
minutes’ score tells the healthcare provider how well the baby is doing outside the
mother’s womb.
Dr. Virginia Apgar was an obstetrical anesthesiologist designed and introduced the
APGAR Score, the first standardized method for evaluating a new-born’s transition
to life outside the womb. She created a system in 1952 and used her name as
MNEMONIC for each of the 5 elements that a person will score.
A = APPEARANCE
0 Points = Bluish-gray or pale all over
1 Point = Normal color (but hands and feet are bluish)
2 Points = Normal color all over (hands and feet are pink)
P = PULSE
0 Points = Absent (no pulse)
1 Point = Pulse below 100 beats per minute (bpm)
2 Points = Pulse over 100 beats per minute (bpm)
G = GRIMACE
0 Points = Absent, no response to stimulation
1 Point = Facial movement only, grimacing with stimulation
2 Points = Pulls away, sneezes, coughs, or cries with stimulation
A = ACTIVITY
0 Points = No movement, or “floppy” tone
1 Point = Flexed arms and legs with little movement
2 Points = Active, spontaneous movement
R = RESPIRATION
0 Points = Absent, no breathing
1 Point = Slow or irregular breathing, weak crying2 Points = Normal rate of breathing and effort, good crying
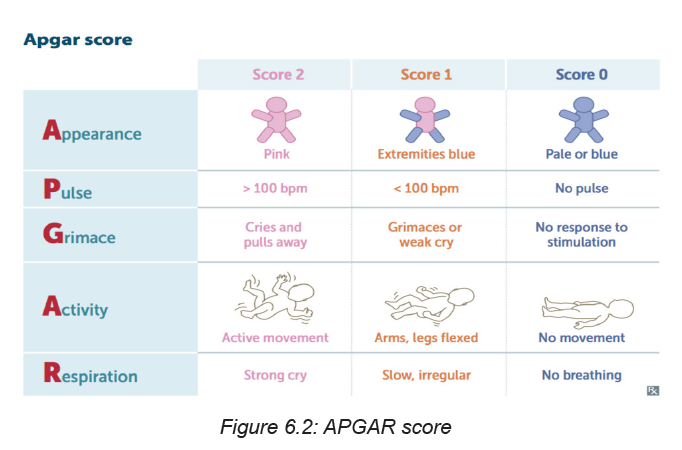
Self-assessment 6.2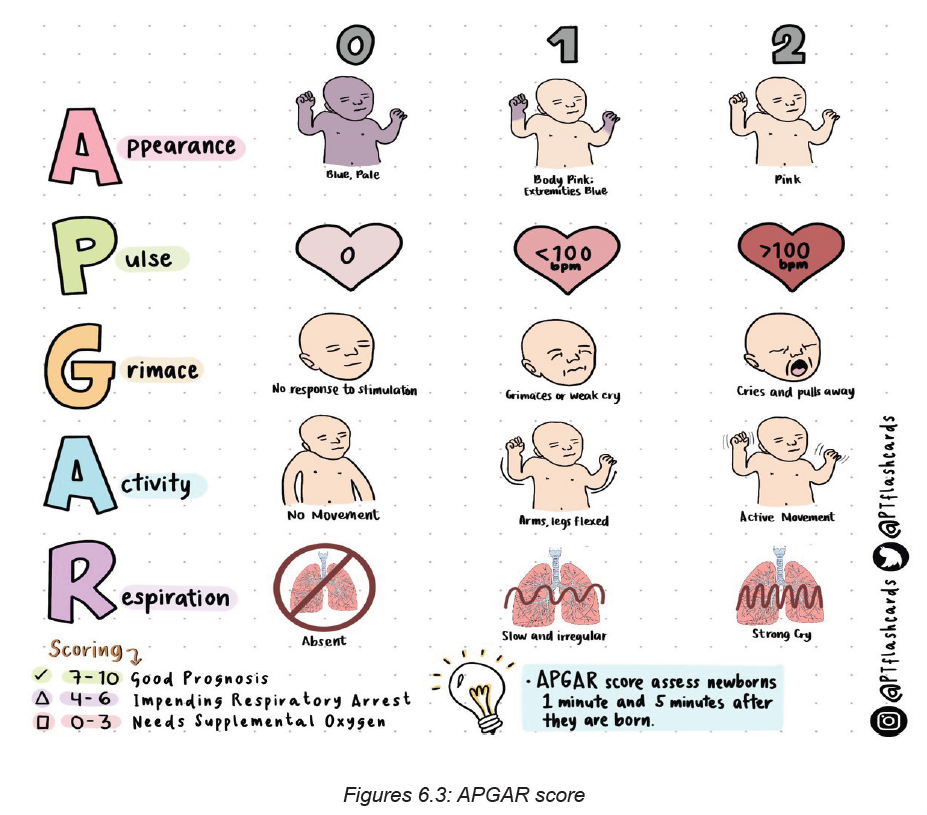
1. What is APGAR score?
2. What does mean the mnemonic APGAR in full words?
3. Who discovered APGAR?
4. In which year DR Virginia Apgar created the system?
6.3. Requirements, aims and importance of the assessment of the
newborn immediately after birth.
Learning Activity 6.3
As an associate nurse, you are called to perform assessment for a newborn
baby boy who was born in past 10 minutes. In that call, you are told to examine
the baby from head to toes
From the above call,
a. What do you think will be the materials that you will use to assess that
newborn baby?
b. What do you think about the aim and importance of assessing that newborn
baby immediately after birth?
c. What do you think about the role of health care provider in examination of
newborn?
Roles of the associate nurse in assessing/examining the newborn baby
immediately after birth.
The role of the nurse/midwife is:
• To carry out good interpersonal communication.
• To take complete history about the mother and neonate.
• To be sure that the neonate has identification band.
• To perform complete physical assessment (General appearance, vital signs,
growth measurements, gestational age assessment).
• Prevention of hemorrhage (administer vitamin K if not given in the delivery
room).
• Documentation.
Aims of assessing/examining the newborn baby immediately afterbirth
The aim of assessing/examining the newborn baby immediately afterbirth is to:
• To describe and carry out an examination of a baby soon after birth
• To screen for malformations
• To observe smooth transition to extra uterine life
• An ass overall of baby’s condition
Principles of examination of the newborn baby immediately afterbirth
The Principles of examination of the newborn baby immediately afterbirth include:
♦ Assess
♦ Ask, Check, Record
♦ Look, Listen, Feel
♦ Classify
♦ Treat/refer or advise
Types and stages of newborn assessment
The following are types and stages of newborn assessment:
1. The initial assessment: done in the 1st 10 minutes
APGAR scoring system
Purpose: is to assess the newborn’s immediate adjustment to extra-uterine life.
2. Transitional assessment (Periods of reactivity):
I) First period of reactivity:
Stage 1: During the first 30 minute through which the baby is characterized as
physiologically unstable, very alert, cries vigorously, may suck a fist greedily, &
appears very interested in the environment.
Stage 2: It lasts for about 2-4 hours, through this period; all V.S & mucus production
are decreased. The newborn is in state of sleep and relative calm.
II) Second period of reactivity: It lasts for about 2-5 hours,
In Second period of reactivity the newborn is alert and responsive, heart &
respiratory rate, gastric & respiratory secretions are increased & passage of
meconium commonly occurs.
Following this stage is a period of stabilization through which the baby becomes
physiologically stable & a vacillating pattern of sleep and activity
Minimum prerequisites of examination of the newborn baby immediately
afterbirth:
The Minimum Requirements of examination of the newborn baby immediately
afterbirth includes:
• Mother & baby together
• Warm room, fresh clean sheet/clothes
• Thermometer
• Weighing scale
• Watch with seconds• Stethoscope
Self-assessment 6.3
1. Outline 3 roles of the associate nurse in assessing/examining the newborn
baby immediately after birth?
2. What is the Aim of assessing/examining the newborn baby immediately
after birth?
3. What are the minimum requirements of examination of the newborn baby
immediately afterbirth?
4. What includes the first period of reactivity?
6.4 Anthropometric measurements
Learning Activity 6.4
Observe these images illustrating an associate nurse taking measurements tothe newborn baby.
From the observation of above pictures,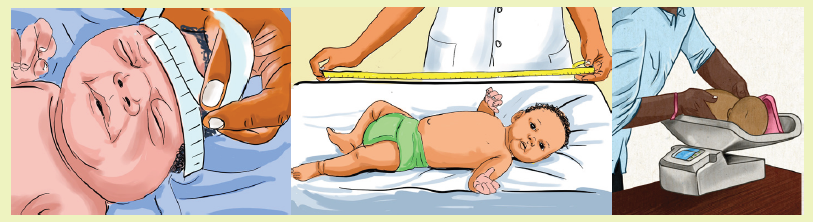
a. What measurements do you think the nurse is taking to that baby?
b. What do you think about the importance of weighing baby after birth?
c. What do think about about normal head circumference?
Weight measurement
Birth weight is an important marker of health. Full-term babies are born between
37 and 41 weeks of pregnancy. The normal birth weight ranges between
2500-4000grams. In general, very small babies and very large babies are at greater
risk for problems. Babies are weighed every day in order to look for growth. If the
baby weighs less than 1,500 gm or more than 4000grams, the associate nurse
must quickly refer the baby for further advanced care.
While taking the baby’s weight, the associate nurse must keep in mind that the new
born baby loses 10% of their birth weight in the first 10 days. Thereafter, the babies
gain about 25-30gms/day. Babies will usually gain this weight back within the first
2 weeks after birth. Premature and sick babies may not begin to gain weight right
away.
Length measurement
This is the measurement taken from crown of head to the heel. The normal range
is 45 to 50 cm.
Head circumference
This is the distance around the baby’s head. Immediately after birth, molding of the
skull may give inaccurate measurement of the head circumference. So it should
be measured after 48 hours after birth. The normal range of head circumference is
33 to 37 cm and it may be larger in case of hydrocephalus and smaller in case of
microcephaly.
Chest circumference
This is the distance around the baby’s chest and it is about 2-3cm less than head
circumference. Head and chest circumference may be equal for the first 24 to 48hours of life.
Self-assessment 6.4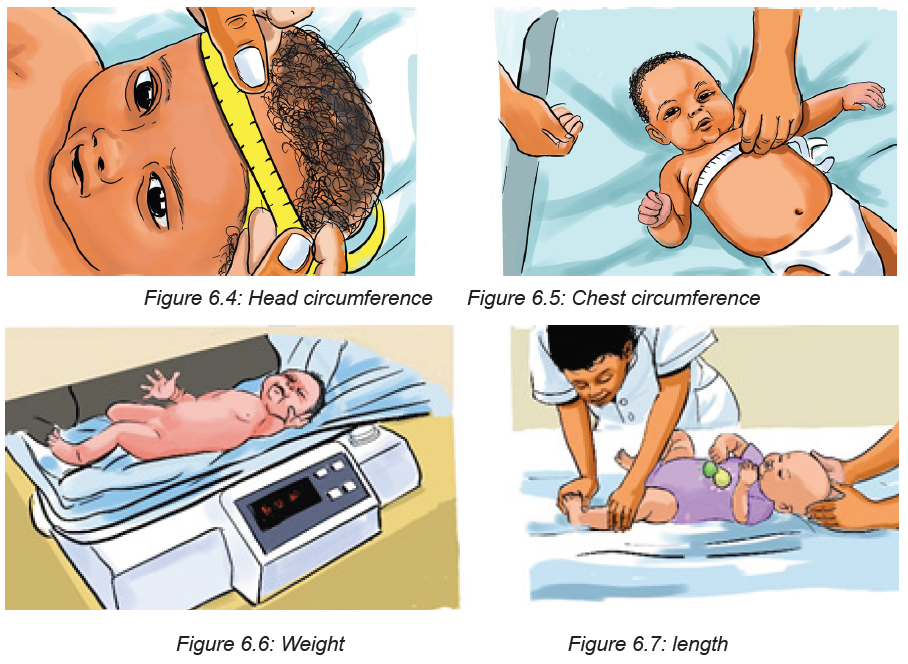
1. a. What are the essential measurements that are taken when the baby is
born?
b. What are the normal range findings for those measurements?
2. How molding can affect results of head circumference measurement?
3. What will the associate nurse do if the baby weighs less than 1,500 gm or
more than 4000grams?
4. The newborn loses weight during the first week of life at which percentage
in the following
a. 5%
b. 15%
c. 10%
d. 20%e. None of the above
6.5 Vital signs measurements of the newborn
Learning Activity 6.5
Observe these images illustrating an associate nurse taking vital signs to thenewborn baby.
From the observation of above pictures,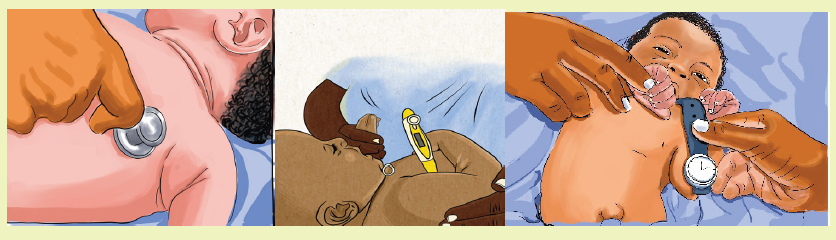
a. What vital signs do you think the nurse is taking to that baby?
b. What do you think can be normal regarding body temperature of newborn?c. What do you think to be normal range of respiratory rate in new born?
Vital Signs and Measurements
Temperature: Normal range 36.5 to 37.5 axillary
Common variations:
Crying may elevate temperature
Stabilizes in 8 to 10 hours after delivery
Signs of potential distress or deviations from expected findings:
Temperature is not reliable indicator of infection
A temperature less than 36.5 oc
Heart rate: Normal range: 120 to 160 beats per minute
Common variations:
Heart rate range to 100 when sleeping to 180 when crying
Color pink with acrocyanosis
Heart rate may be irregular with crying
Signs of potential distress or deviations from expected findings:
• Although murmurs may be due to transitional circulation-all murmurs
• should be followed-up and referred for medical evaluation
• Deviation from range
• Faint sound
Respiration rate: Normal range 30 to 60 breaths per minute
Common variations:
• Bilateral bronchial breath sounds
• Moist breath sounds may be present shortly after birth
Signs of potential distress or deviations from expected findings:
• Asymmetrical chest movements
• Apnea >15 seconds
• Diminished breath sounds
• Seesaw respirations
• Grunting
• Nasal flaring
• Retractions
• Deep sighing
• Tachypnea - respirations > 60
• Persistent irregular breathing
• Excessive mucus
• Persistent fine crackles
• Stridor (Crowing respiratory sound)Blood Pressure - not done routinely
Self-assessment 6.5
1. When does the temperature stabilize after birth?
2. What is the heart rate of the crying baby?
3. What changes may occur regarding the baby’s body temperature when the
baby is crying
4. Enumerate signs of potential distress.
6.6 Head and neck assessment
Learning Activity 6.6
Observe these images illustrating an associate nurse that is assessing thenewborn’s head and neck.
From the observation of above pictures,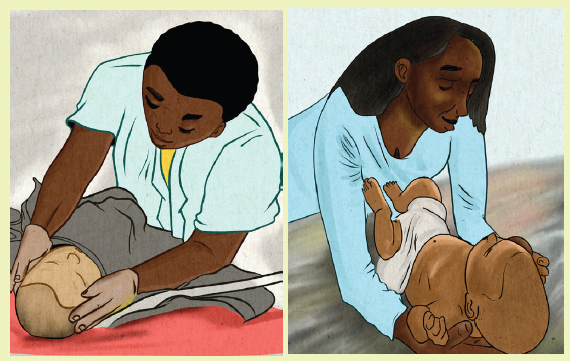
a. What elements do you think the nurse will assess to that baby’s head and
neck?
b. Have you heard a word fontanel? If yes, when do you think anterior fontanel
closes?
c. What do you understand by the word fontanel?
Head: It consists of skulls bones that are not closed completely, due to this, the
skull is easily molded during the passage through the birth canal at the time of birth
where the suture lines are joined and form the fontanelles.
Fontanel is a space between the bones of the skull in an infant, where ossification
is not complete and the sutures not fully formed.Sutures are fibrous bands of tissue that connects the borns of the skull.
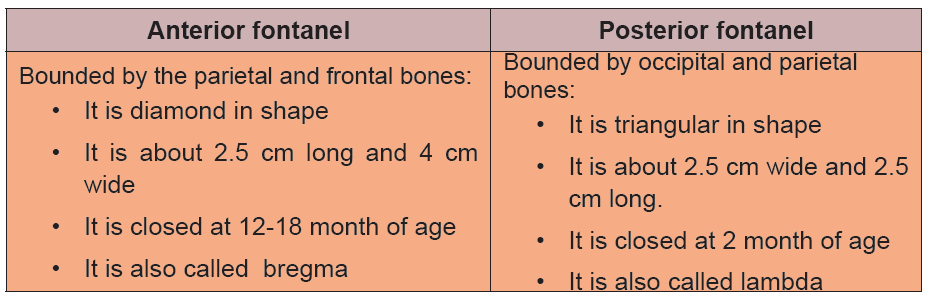
Table 6.1 Difference between fontanelles
If the sutures are wide and fontanels are bulged, this indicates the increased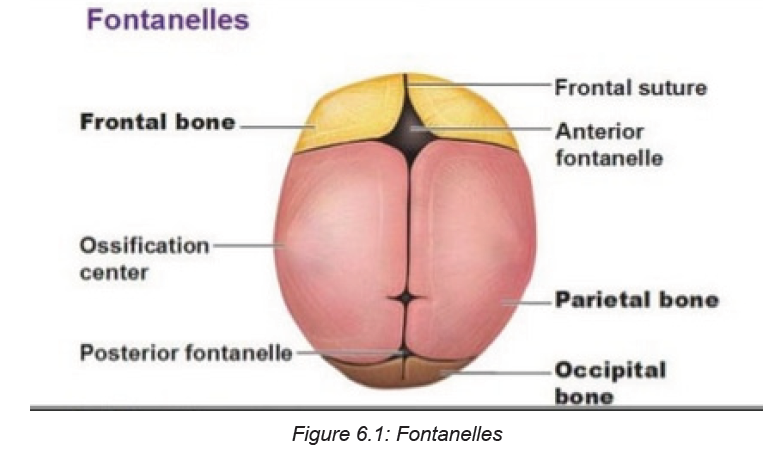
intracranial pressure which is commonly seen in hydrocephalus condition. When
fontanel depressed, it indicates dehydration. The associate nurse should also
observe the caput succedaneum and cephalohematoma.
Face
The associate nurse looks at the eyes, ears, nose, and cheeks. He/ She he also
examines the face for any asymmetry or obvious malformations.
Eyes
On the eyes of the newborn, the associate nurse will check for any asymmetry,
spacing, and movement. He/ She he also checks for oedema, discharge, colour of
sclera. Yellow color indicates jaundice. Position of the eyes and distance between
inner canthus of both eyes should be checked, it should be 2 cm in diameter. If it is
more than 2 cm; it is known as hypertelorism and if it is less than 2 cm; it is known
as hypotelorism. Neonate’s pupils are round in shape and react to the light.
Ear
On the ear, the associate nurse will check for symmetry and to make sure ears
are parallel to the eyes and not low set, which can indicate a problem. Also the size
and shape will be assessed. The ear cartilage is full in term infants and it is fully
developed and returns its shape. Observe the startle reflex by the loud noise which
indicates audibility of the neonates.
Nose
The associate nurse will check for patency, depression or low nasal bridge. He/
she will also assess for nasal discharge, deviated nasal septum, and nasal flaring.
Mouth and throat
The associate nurse will check for cleft palate and cleft lips. He/she will observe the
natal teeth. To assess for cleft palate or abnormality, the palpation of the palette willbe done. A small jaw could also indicate a problem.
Neck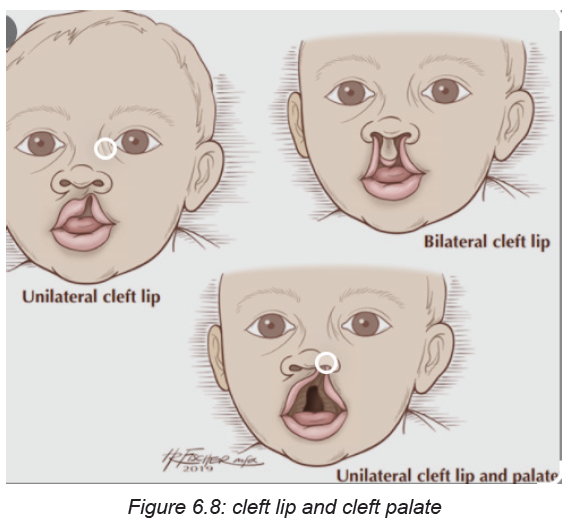
For the neck, the associate nurse will palpate for masses and the clavicles are
palpated for crepitus, which could indicate an injury. Neck of the new born is short
and has various folds and it should be checked for mobility, and webbing of theneck.
Self-assessment 6.6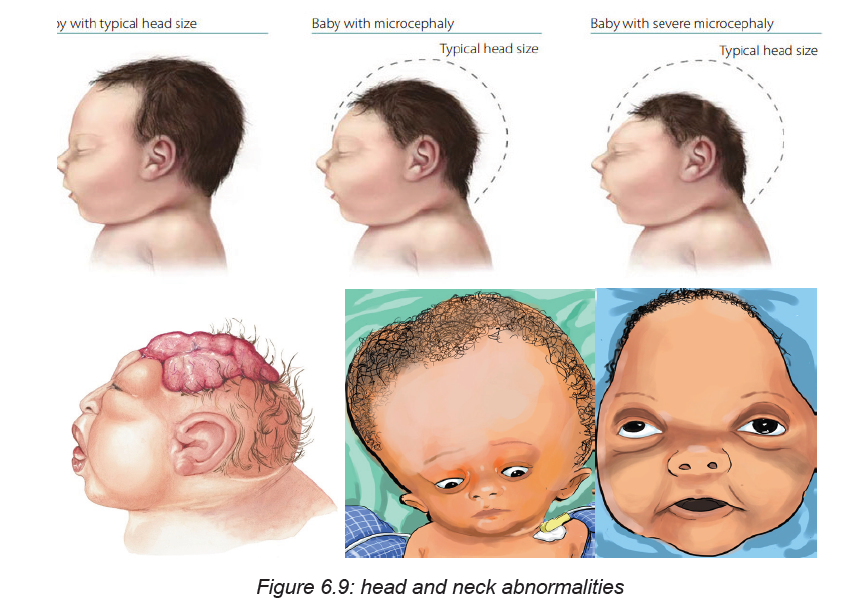
1. When the anterior fontanel closes?
2. When the posterior fontanel closes?
3. What will the associate nurse check on newborn’s eyes?
4. What will the associate nurse observe on newborn’s face5. Define the word sutures?
6.7 Chest and lungs assessment
Learning Activity 6.7
Observe these images illustrating an associate nurse assessing the newborn’schest.
From the observation of above pictures,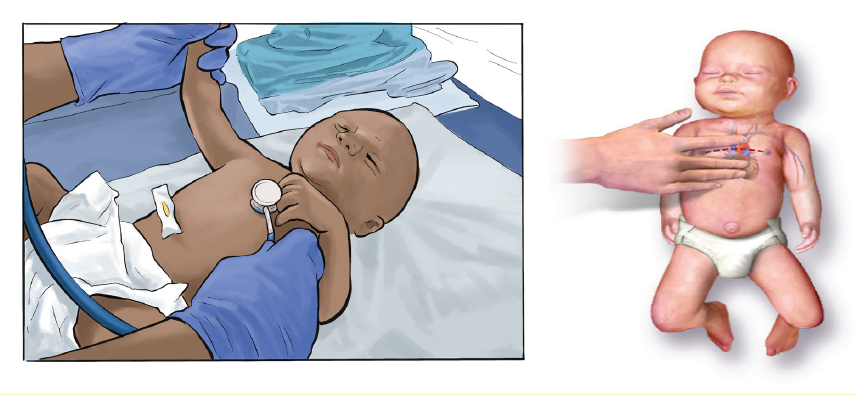
a. What elements do you think the nurse will assess newborn ‘chest?b. What do you think about inter costal retractions during breathing?
Normally, the chest is barrel shaped. A malformed chest could indicate a problem.
Retractions may be observed with respiratory difficulty.
The associate nurse observes the nipple and breast tissue. Breast size and location
should be assessed. He/she observes witch’s milk (milky discharge due to effect
of maternal hormones). Parents of the baby should not be worry because it will be
resolved slowly and there is no treatment for it.
Check the rate and rhythm of the respiration, neonate’s abdomen rises and falls
during each breathe. The lungs should be auscultated while the infant is quiet.
Respirations should be observed and counted for a full minute. Heart rate should
be assessed with a stethoscope while listening for murmurs.
Clinical evaluation of breath sounds is the first and most common method of
assessing lung health. The stethoscope placed on the back and chest lets the
physician listen to the breath sounds. This process is called auscultation.
Intercostal retractions: One of the most important physical findings to be able to
recognize in a new-born is the presence of retractions. Sepsis, pulmonary pathology,
cardiac disease, metabolic disorders, polycythaemia, cold stress, and others can
all cause retractions -- it is a sign of a new-born in distress. In the photo, taken
during inspiration, the shadows between the ribs can be clearly seen. Retractions
may or may not occur in combination with other signs of distress: nasal flaring,grunting, and tachypnea.
Self-assessment activity 6.7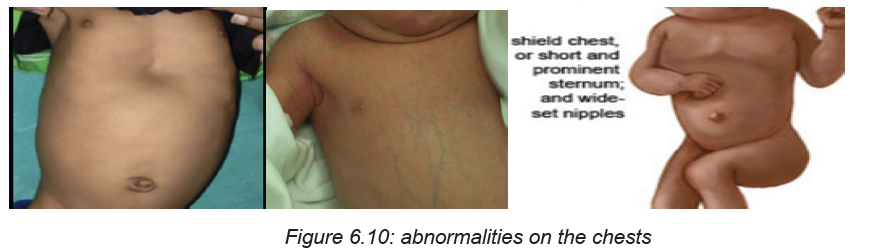
1. What the associate nurse assesses on the newborn’s chest?
2. What the associate nurse tells and explains to the mother is worried about
the witch’s milk found on his baby?
3. What is normal shape of the chest?4. When to auscultate the lungs of the newborn?
6.8 Abdomen, back and genitalia assessment
Learning Activity 6.8
Observe these images illustrating an associate nurse assessing the newborn‘abdomen, back and genitalia.
From the observation of above pictures,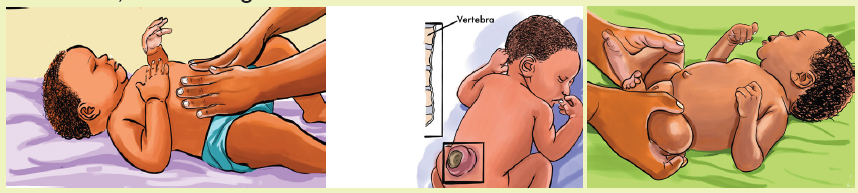
a. What elements do you think the nurse will assess to the back, abdomen,
spine and genitalia of the newborn?b. What do you think to be observed on umbilical cord after birth?
Abdomen
On abdomen, the associate nurse will check for the shape and distension. He/
she will also check for bowel sounds, and observe the umbilical cord for infection
and any discharge, redness and observe two arteries and one vein. Check for anyhernia or any abnormalities. Abdomen should feel soft during palpation.
Back and spine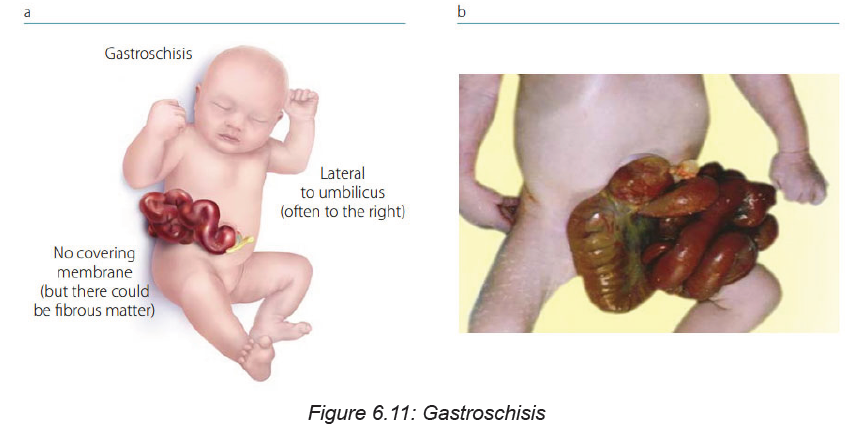
On the back, the associate nurse will check for any abnormal spinal curvature, hair
on the skin, depression in the spine, spina bifida, meningocele, meningomyelocele
Buttocks: Buttocks should be observed for any mass. Perineal area should bechecked for anal opening, anal fissure or any other abnormalities.
Genitalia
On female genitalia the associate nurse will check if the labia major cover the labia
minor (sign of maturity) and if the clitoris is visible on separating the labia. Urethral
opening should be below the clitoris. Pink red mucous vaginal discharge may be
found during the first week due to sudden decrease of maternal hormones, which
is known as pseudomenstruation.
On male neonates, testes should be inspected and palpated for descend; scrotum
appears pigmented and wrinkled with rugae. Penis should be inspected for urethralopening. Check for hydrocele and inguinal hernia.
Self-assessment activity 6.8
1. What will the associate nurse assess on umbilical cord of the newborn?
2. What will the associate nurse assess on back and spine of the newborn?
3. What will the associate nurse assess on male neonate’s genitalia?4. Define the term pseudo menstruation?
6.9 Assessment of the limbs
Learning Activity 6.9
Observe these images illustrating an associate nurse assessing the newborn‘upper and lower limbs.
From the observation of above pictures,
a. What elements do you think the nurse will assess newborn ‘limbs?b. Define the term polydactyl?
Each newborn baby is carefully checked at birth for signs of problems or
complications. The healthcare provider will do a complete physical exam, on limbs,
the associate nurse assesses arms, Legs, Hands, and Feet. He/she checks for any
symmetricity, abnormal length and deviations, fractures, paralysis, and weakness.
He/she also assesses if there is polydactyly, syndactyly and abnormal skin creases.
Polydactyl condition of having more than the normal number of fingers or toes.
Hips: On hips, the associate nurse assesses the range of motion adequate and click.
If any deviation, it indicates congenital hip dislocation through these maneuvers;
The Barlow manoeuvre involves flexing the new-born’s hips and knees at 90
degrees and applying gentle pressure downwards. The Barlow test is considered
to be positive if the examiner feels the head of the femur slip out of the hip socket.
The Ortolani manoeuvre is performed after the Barlow manoeuvre. It confirms hip
displacement and returns the displaced bone back into the hip socket. The Ortolani
manoeuvre involves abducting (moving apart) the flexed legs while applying a
gentle forward pressure with the middle finger against the head of the femur. An
audible ‘clunk’ can be heard when the femoral head returns to the hip socket.
Plantar creases: These are creases on the soles of the feet. They can range from
absent to covering the entire foot, depending on the maturity.
Various Congenital malformations that can be detected while doing limbsassessment.
Self-assessment 6.9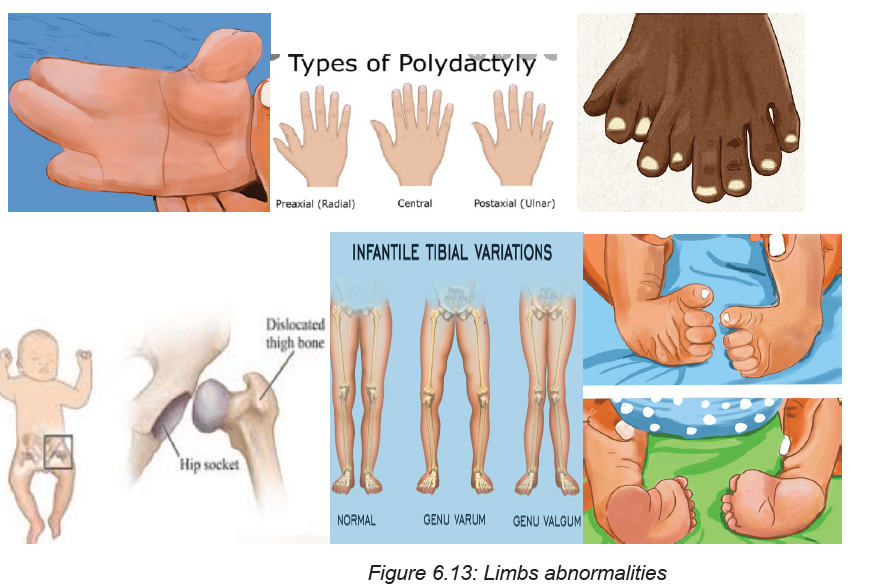
1. What the associate nurse assesses on the newborn’s hands?
2. What the associate nurse assesses on the newborn’s legs and feet?
3. What will the associate assess on the newborn’s hips?4. Define the term plantar creases?
6.10 Assessment of the skin
Learning Activity 6.10Observe these images illustrating the newborn ‘skin
From the observation of above pictures,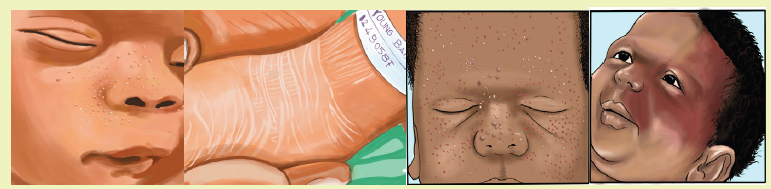
a. What elements do you think the nurse will assess for the newborn ‘skin?b. What do you think about lanugo hair?
The skin of a healthy newborn at birth has:
• Deep red or purple skin and bluish hands and feet. The skin darkens before
the infant takes their first breath (when they make that first vigorous cry).
• A thick, waxy substance called vernix covering the skin. This substance
protects the foetus’s skin from the amniotic fluid in the womb. Vernix should
wash off during the baby’s first bath.
• Fine, soft hair (lanugo) that may cover the scalp, forehead, cheeks, shoulders,
and back. This is more common when an infant is born before the due date.
The hair should disappear within the first few weeks of the baby’s life.
• New-born skin will vary, depending on the length of the pregnancy. Premature
infants have thin, transparent skin. The skin of a full-term infant is thicker.
• By the baby’s second or third day, the skin lightens and may become dry and
flaky. The skin still often turns red when the infant cries. The lips, hands, and
feet may turn bluish or spotted (mottled) when the baby is cold.
The associate nurse assesses the following on the newborn’s skin:
Normal - Short-term (resolves in days to months)
For normal short-term skin conditions, the associate nurse checks for
• Miliaria (Heat Rash)
• Petechiae on scalp and face after vertex delivery
• Vernix Caseosa (Cheesy white skin covering present at birth)
• Transient vascular phenomena like skin mottling related to cold exposure and
positional erythema on the dependent side of the body)
Normal - Short-term (resolves in days to months):
The associate nurse checks for:
• Erythema toxicum neonatorum (Yellow papules on red base affected face
and trunk, disappearing within days to a week
• Neonatal Pustular Melanosis(Milky fluid filled Vesicles without erythema, <5
mm on torso, buttock, forehead, chin
• Milia (Pinpoint white, keratin-filled Papules (blocked sebaceous glands) on
nose and cheeks
• Lanugo (Fine hair on Shoulders and back). If too much, it can indicate
prematurity
• Spontaneous Fat Necrosis
• Acne Neonatorum
Normal - Birthmarks, Long-term (Persists for months to years - some do not
resolve)
• See abnormal or risk-associated Birthmarks below (e.g. Congenital
Melanocytic Nevi)
• Mongolian Spots (Large up to 10 cm bluish-gray pigment patches on
extremities as well as lumbar, sacral and buttock region
• Nevus Simplex (Macular pink to red capillary dilations that fade with time,
occurring on upper Eyelids, forehead, nape of neck
• Hemangioma (Benign vascular lesions)
Important skin infection related lesions
• Neonatal Herpes Simplex Virus (Vesicular Lesions in infant born to mother
with HSV
• Congenital Syphilis (Lesions on palms and soles)
• Staphylococcal Scalded Skin
• Impetigo
Abnormal or lesions that require evaluation, specific management or
observation
• Pallor (indicates bleeding or Anemia)
• Jaundice onset within first day of life(indicates Hemolytic Disease of the
Newborn and Neonatal Jaundice)
• Cyanosis(can indicate respiratory distress, cardiovascular
disorders,hypoxia,etc)
• Mottling( can indicate Sepsis,or Hypothermia)
• Gray Skin Coloration( is a sign of metabolic Acidosis)
• Vesicles( can indicate Neonatal HSV)
• Bullae
• Nevus Sebaceus.It is a yellow hairless Plaque on scalp or face. It may be
associated with epidermal nevus syndrome and carries risk of future skin
cancer in 10-15% of cases
• Hyperpigmentation
• Cafe-Au-Lait Macule”Coffee with milk” (tan to brown) colored flat• Macule, <4 cm located on trunk
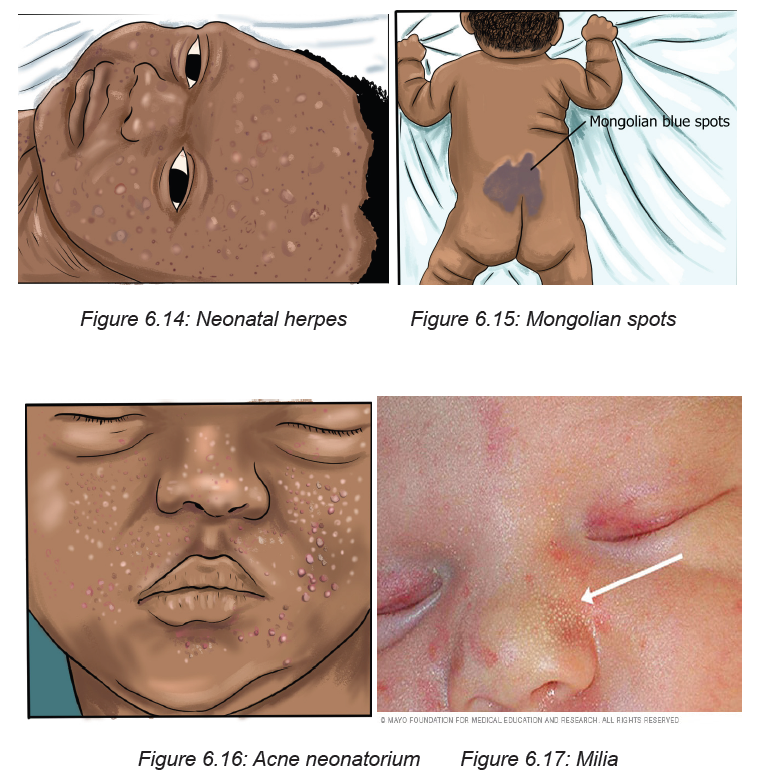
Self-assessment 6.10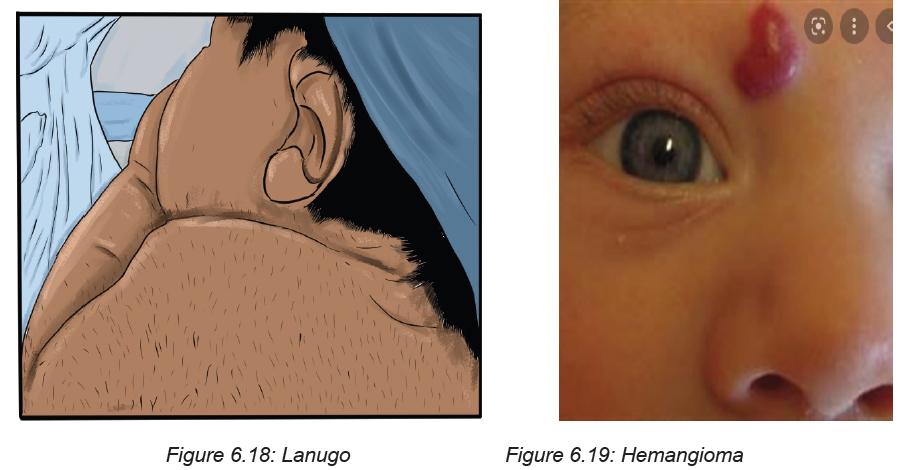
1. What are the normal short-term skin conditions that the associate nurse
checks on the newborn?
2. What are the Normal Birthmarks that the associate nurse checks on thenewborn?
6.11 Reflexes assessment
Learning Activity 6.11
Observe these images illustrating an associate nurse taking measurements tothe newborn baby.
From the observation of above pictures,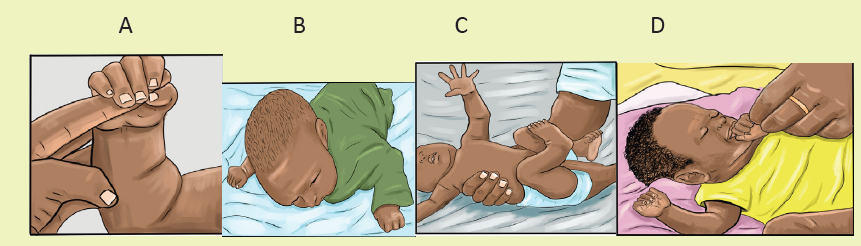
a. What reflex do you think the nurse is taking to that baby in the picture A,
B, C, D?b. What do you think about necessity of assessing reflexes on baby?
Reflexes are involuntary movements or actions. Some movements are spontaneous
and occur as part of the baby’s normal activity. Others are responses to certain
actions. Healthcare providers check reflexes to determine if the brain and nervous
system are working well. The presence and strength of a reflex is an important sign
of nervous system development and function. Many infant reflexes disappear as
the child grows older, although some remain through adulthood
Exam 1: Foot
a. Stroke Inner Sole: Toes curl around (“grasp”) examiner’s finger
b. Stroke Outer Sole (Babinski): Toes spread, great toe dorsiflexion
Exam 2: Doll’s Eyes and grasping reflexes
A. Give one forefinger to each hand - baby grasps both
1. Pull baby to sitting with each forefinger
B. Eyes open on coming to sitting (Like a Doll’s)
1.Head initially lags
2.Baby uses Shoulders to right head position
Exam 3: Primitive Stepping (Walking Reflex)
A. Hold baby up with one hand across chest
B. As feet touch ground, baby makes walking motion
Exam 4: Protective Reflex
a. Soft cloth is placed over the baby’s eyes and nose
b. Baby arches head and turns head side to side
c. Brings both hands to face to swipe cloth away
Exam 5: Rooting and sucking reflexes
a. Touch newborn on either side of cheek
b. Baby turns to find Breast
c. Sucking mechanism on finger is divided into 3 steps
1. Front of Tongue laps on finger
2. Back of Tongue Massages middle of the finger
3. Esophagus pulls on tip of finger
Exam 6: Tonic Neck (Fencing) Reflex
A. If the Babies’ head is rotated leftward
1. The left arm (face side) stretches into extension
2. The right arm flexes up above head
B. Opposite reaction if head is rotated rightward
Exam 7: Moro Reflex (Startle Reflex)
A. Hold supine infant by arms a few inches above bed
1.Gently drop infant back to elicit startle
B. Baby throws Arms out in extension and baby grimace
Exam 8: Hand-to-Mouth (Babkin) Reflex
A. Stroke newborns cheek or put finger in baby’s palm
B. Baby will bring his fist to mouth and suck a finger
Exam 9: Swimmer’s (Gallant) Response
A. Hold baby prone while supporting belly with hand
1. Stroke along one side of babies’ spine
B. Baby flexes whole body toward the stroked side
Exam 10: Crawling Reflex
A. Newborn placed on AbdomenB. Baby flexes legs under him and starts to crawl
Self-assessment 6.11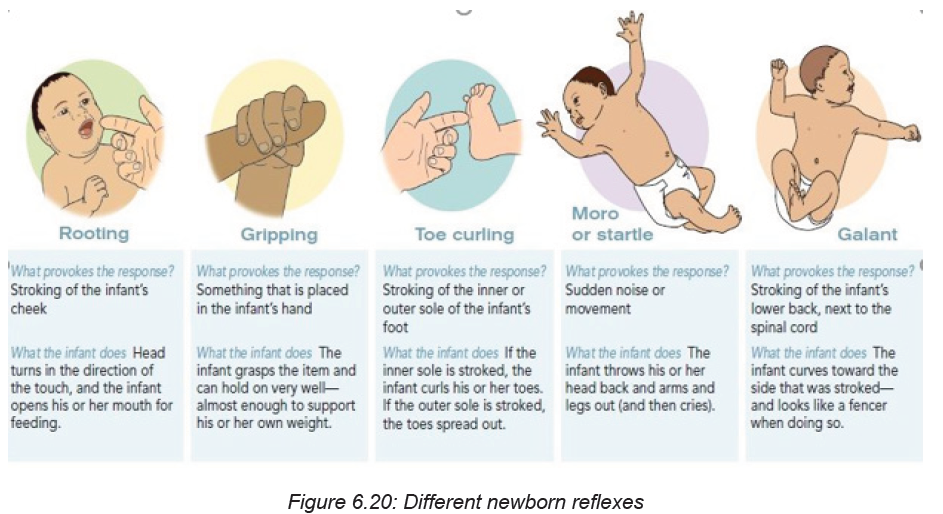
1. How will the associate nurse to check for Babinski reflex?
2. How the associate nurse checks for Moro Reflex (Startle Reflex)
3. Define the term reflex?4. What does it mean when reflexes are present?
6.12 Helping the Baby Breathe (HBB)
Learning Activity 6.12Observe these images illustrating steps of Helping the Baby Breathe (HBB)
1. What do you think about the Helping the Baby Breathe (HBB) program?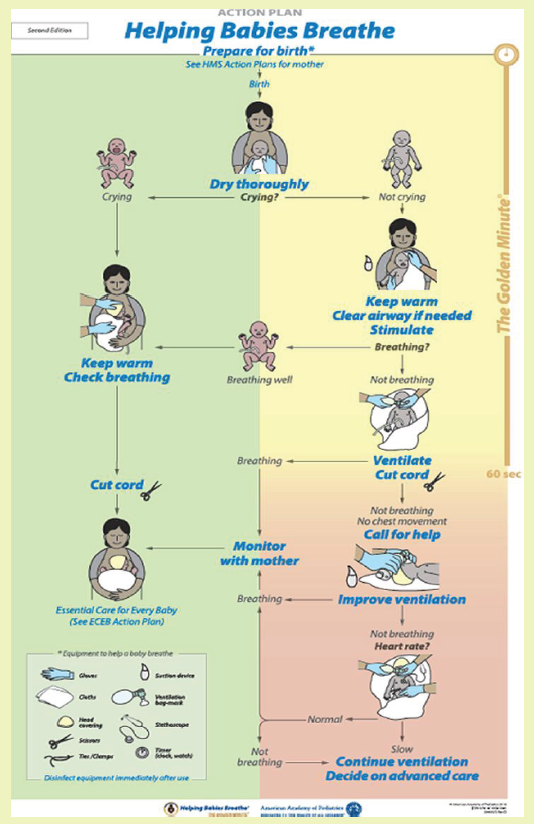
2. What do you think will be done to help the baby breathe in the first minute(Golden) of birth?
The first minutes after birth are critical to reducing neonatal mortality. Helping
Babies Breathe (HBB) is a simulation-based neonatal resuscitation program for low
resource settings.
The Golden Minute:
A key concept of HBB is The Golden Minute. Within one minute of birth, a baby
should be breathing well or should be ventilated with a bag and mask. The Golden
Minute identifies the steps that a birth attendant must take immediately after birth to
evaluate the baby and stimulate breathing.
HELPING BABY BREATHE INCLUDE:
Routine care
• Dry thoroughly
• Is the baby crying?
• Keep warm, check for breathing
• Clamp or tie the umbilical cord
Before delivery
• Identify a helper and review emergency plan
• Prepare the area for delivery
• Wash hands
• Prepare the area for ventilation
• Assemble disinfected equipment and supply
• Test the ventilation bag, mask
Materials
• Gloves
• Suction device
• Cloths
• Ventilation bag mask
• Head covering
• Stethoscope
• Scissors
• Ties or cord clamp
• Timer
Procedure
Dry the baby thoroughly at birth. Drying help keeping the baby to stay warm and
stimulates breathing. A newly born baby is wet and may become cold even in a
warm room.
• Dry the body, head, arms, and legs by rubbing gently with a cloth
• Drying the back provides important stimulation to breathe. Wipe the face,
clean of feces and blood.
• Drying can be done on the mother’s abdomen.
• Place a clean cloth on the mother’s abdomen before birth.
• Position the baby on the cloth and dry thoroughly.
• Remove the wet cloth and place the baby on skin to skin with the mother and
cover with a dry one. A baby who is crying is receiving routine care and kept
warm and check breathing.
• If the baby is not crying after drying he needs help to breathe in the golden
minute.
• Keep warm on mother abdomen or chest, or a warm area with dry blanket
beside the mother and cover the head
• Clear airway if needed
• Position the head. Position the neck slightly extended to keep airway open.
– The nose will be as far forward as possible.
– If the neck is flexed or extended too far, air may not enter freely.
– If secretions are not seen and there is no meconium, move directly to stimulate
breathing. Some babies will have a shallow, irregular, slow, or noisy breathing
immediately after birth. Other may have chest in-drawing or retractions. These
babies with abnormal breathing will require continued monitoring or their
breathing, heart rate, and color to decide if they need more help to breathe
• Decide what care the baby needs after clearing the airway and stimulation.
If the baby is breathing well, the baby can receive routine care. Continue to check
the breathing. Clamp or tie and cut the umbilical cord. Encourage breastfeeding in
the first hour.
If the baby is not breathing well (gasping or not breathing at all), begin ventilation
with bag and mask. Quickly move the baby to the area for ventilation. Delayingventilation may result in death or brain damage.
Self-assessment 6.12
1. What would happen within one minute of birth?
2. What are the routine cares provided in HBB?
3. Why is it important to dry thoroughly the baby in the golden minute?4. What are preparations of delivery area before delivery?
6.13 Breastfeeding
Breastfeeding is when baby is feed with breast milk, it is also called nursing. Breast
milk is the ideal food for infants. It is safe, clean and contains antibodies which
help protect against many common childhood illnesses. Breast milk provides all the
energy and nutrients that the infant needs for the first months of life, and it continues
to provide up to half or more of a child’s nutritional needs during the second half
of the first year, and up to one third during the second year of life. It’s best to try to
breastfeed the baby in the first hour after birth because by latching on and sucking
rhythmically, the breast begins switching on the cells to initiate the body’s breast
milk supply. is Exclusive breastfeeding recommended for 6 months. Even, after the
introduction of other foods, it recommends continuing to breastfeed through the
baby’s first year of life. Normally, newborns often want to feed every 2-3 hours.
Signs showing that the baby is hungry
One of the most common ways to know that the baby is hungry is ‘’cry’’. Other signs
showing that the baby wants to breastfeed include:
• Licking their lips or sticking out their tongue
• Rooting, which is moving their jaw, mouth, or head to look for your breast
• Putting their hand in their mouth
• Opening their mouth
• Fussiness
• Sucking on things.
Benefits of breastfeeding for the Baby
Breast milk provides the ideal nutrition for infants. It has a nearly perfect mix
of vitamins, protein, and fats it has everything that baby needs to grow. And it’s all
provided in a form more easily digested than infant formula.
• Breast milk contains antibodies that help your baby fight off viruses and
bacteria.
• Breastfeeding lowers your baby’s risk of having asthma or allergies. Plus,
babies who are breastfed exclusively for the first 6 months, without any formula,
have fewer ear infections, respiratory illnesses, and bouts of diarrhoea.
• They also have fewer hospitalizations and trips to the health care provider;
Breastfeeding has been linked to higher intellectual quatience (IQ) scores in
later childhood in some studies.
• What’s more, the physical closeness, skin-to-skin touching, and eye contact
all help your baby bond with you and feel secure. Breastfed infants are
more likely to gain the right amount of weight as they grow rather than
become overweight children.
Benefits of breastfeeding for the mother
• Breastfeeding burns extra calories, so it can help losing pregnancy
weight faster. It releases the hormone oxytocin, which helps uterus to
return to its pre-pregnancy size and may reduce uterine bleeding after birth.
Breastfeeding also lowers risk of breast and ovarian cancer.
• Breastfeeding is economic because no need to measure formula, sterilize
nipples, or warm bottles, it saves time and money.
• It also gives regular time to relax quietly to the mother with the newborn as
they bond.
The first few days after birth, breasts make ideal “first milk.” It’s called colostrum.
Colostrum is thick, yellowish, and there’s not a lot of it, but there’s plenty to meet
the baby’s nutritional needs. Colostrum helps a new-born’s digestive tract develop
and prepare itself to digest breast milk.
Colostrum is the first phase of breast milk, which changes over time the baby grows.
The second phase is called transitional milk. The colostrum is gradually replaced
with the third phase of breast milk, called mature milk.
The transitional milk starts few days after birth. By 10 to 15 days after birth, the
body make mature milk, which gives to the baby all the nutrition they need.
LATCHMENT
Position the baby facing the mother, so the baby is comfortable and doesn’t have to
twist the neck to feed. With one hand, the mother cups the breast and gently strokes
her baby’s lower lip with the nipple. The baby’s instinctive reflex will be to open
the mouth wide. With the mothers’ hand supporting the baby’s neck, brings the
mouth closer around her nipple, trying to centre the nipple in the mouth above the
baby’s tongue.
The mother will know the baby is “latched on” correctly when both lips are pursed
outward around the nipple. The baby should have all of nipple and most of the
areola in the mouth. While the mother feels a slight tingling or tugging, breastfeeding
should not be painful.
If the baby isn’t latched on correctly and nursing with a smooth, comfortable rhythm,
the mother gently nudges her pinky between the baby’s gums to break the suction,
remove the nipple, and try again. Good “latching on” helps prevent sore nipples.
Signs of a Good Latch
• The latch is comfortable and pain free.
• The baby’s chest and stomach rest against your body, so that baby’s head is
straight, not turned to the side, the chin touches your breast.
• The baby’s mouth opens wide around your breast, not just the nipple.
• The baby’s lips turn out.
Breast feeding positions
The associate nurse must teach and assist the mother to be in best, comfortable
and relaxed position and the mother must not strain to hold the position or keep
nursing. Here are some common positions for breastfeeding the baby:
Cradle position: The mother rests on the side of the baby’s head in the crook of
her elbow with the whole baby’s body facing the mother. The mother positions the
baby’s belly against her body so they feel fully supported. Other, “free” arm can
wrap around to support the baby’s head and neck or reach through the baby’s legsto support the lower back.
Football position: The mother lines the baby’s back along the mother’s forearm to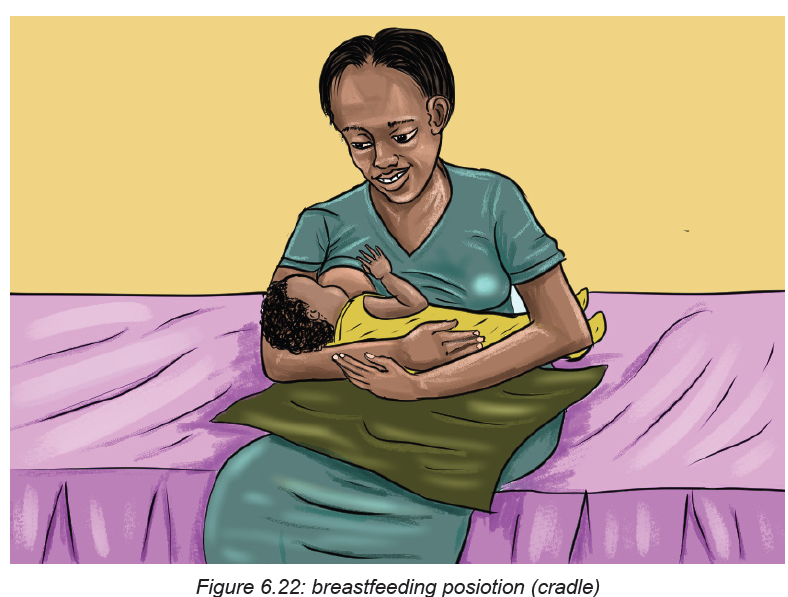
hold the baby like a football, supporting the head and neck in her palm.
This works best with new-borns and small babies. It’s also a good position for the
mother recovering from a cesarean birth and need to protect the belly from thepressure or weight of the baby.
Side-lying position: This position is great for night feedings in bed. Side-lying also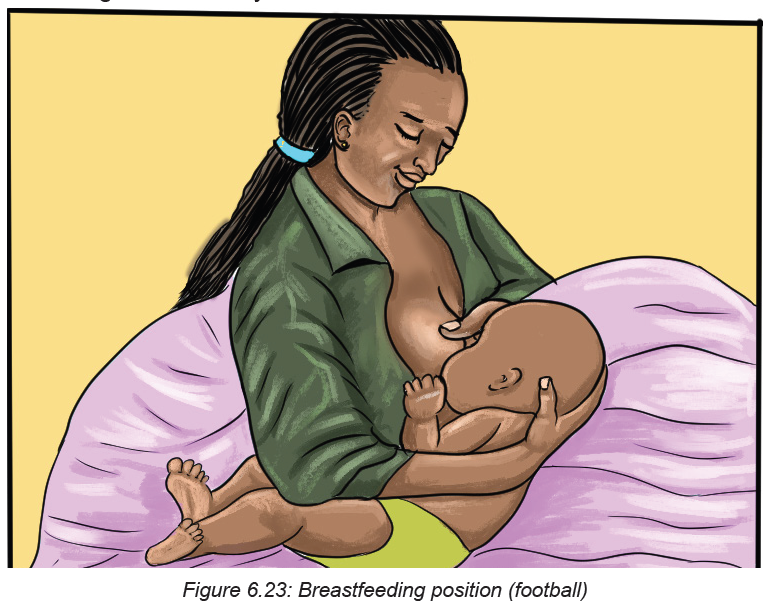
works well if the mother is recovering from an episiotomy, an incision to widen
the vaginal opening during delivery. The mother uses pillows under head to get
comfortable. Then snuggle close to the baby and the mother use her free hand to
lift the breast and nipple into the baby’s mouth. Once the baby is correctly “latched
on,” the mother supports the baby’s head and neck with her free hand so there’s notwisting or straining to keep nursing.
Cross-cradle hold: The mother sits straight in a comfortable chair that has armrests.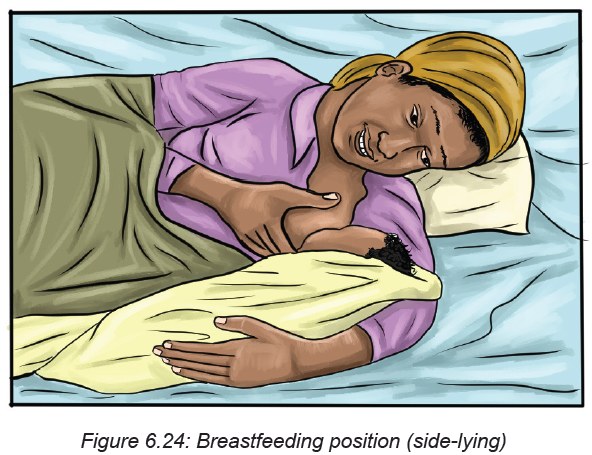
The mother holds her baby in the crook of her arm that’s opposite the breast she will
use to feed them. The mother supports the baby’s head with her hand. She brings
the baby across her body in a way that her tummies face each other. She uses her
other hand to cup the breast in a U-shaped hold. She brings the baby’s mouth toher breast and cradles them close, and does not lean forward.
Laid-back position: This position, also called biological nurturing, is a lot like it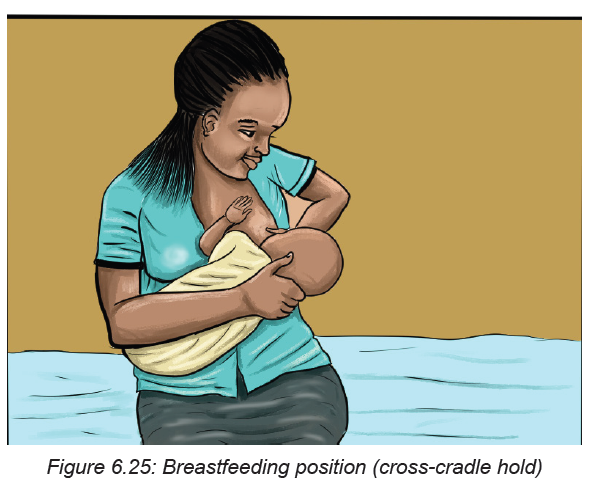
sounds. It’s meant to tap into the natural breastfeeding instincts the mother and
baby have. The mother leans back, but not flat, on a couch or bed. The mother
ensures good supports of her head and shoulders. She holds the baby in entire
fronts touch. She lets the baby take any position they’re comfortable in as long ascheek rests near her breast. The mother helps the baby latch on if he needs it.
Self-assessment 6.13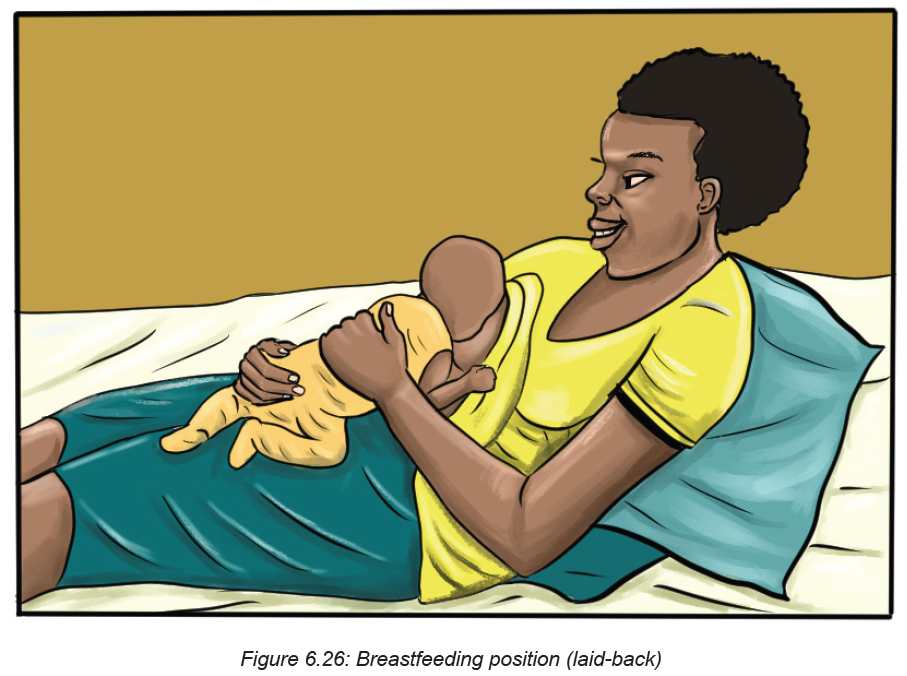
1. When the newborn has to start breastfeeding after birth
2. What are the advantages of breastfeeding to the mother?
3. Which period fit for exclusive breast feeding?
4. What is colostrum?
5. What are the advantages of breastfeeding to the baby?
6. Enumerate comfortable positions that the mother can take whilebreastfeeding.
End unit assessment 6
SECTION A. MULTIPLE CHOICE QUESTIONS
1. The associate nurse is assessing the one minute APGAR score of a newborn
baby. On assessment, the associate nurse notices the following complains on the
newborn patient: heart rate 130, pink body and hands with cyanotic feet, weak
cry, flexion of the arms and legs, active movements and crying when stimulated.
What is the newborn’s APGAR score?
g. APGAR 9
h. B. APGAR 10
i. APGAR 8
j. APGAR 5
2. The associate nurse is assessing the one minute APGAR score of the newborn
baby. On the assessment, he/ she notice the following problems on the newborn
patient: heart rate 101, cyanotic body and extremities, no response to stimulation,
no flexion of extremities, and weak cry. What is the newborn’s APGAR score?
a. APGAR 4
b. APGAR 6
c. APGAR 3
d. APGAR 2
3. A newborn’s fifth minute APGAR score is 5. Which of the following nursing
interventions will the associate nurse provide to this newborn?
e. Routine post-delivery care
f. Continue to monitor and reassess the APGAR score in 10 minutes
g. Some resuscitation assistance such as oxygen and rubbing baby’s back
and reassess APGAR score
h. Full resuscitation assistance is needed and reassess APGAR score.
4. The associate nurse in a delivery room is assisting for the delivery of a
newborn baby. After the delivery, which nursing intervention that the associate
nurse should perform in order s to prevent the heat loss in the newborn as the
result of result of evaporation:
a. Warming the crib pad
b. Turning on the overhead radiant warmer
c. Closing the doors to the room
d. Drying the infant in a warm towel
5. The associate nurse in a newborn nursery is performing an assessment
of a newborn baby. The associate nurse is preparing to measure the head
circumference of the baby and he/ she would most appropriately:
a. Wrap the tape measure around the infant’s head and measure just above
the eyebrows.
b. Place the tape measure under the infant’s head at the base of the skull and
wrap around to the front just above the eyes.
c. Place the tape measure under the infant’s head, wrap around the occiput,
and measure just above the eyes.
d. Place the tape measure at the back of the infant’s head, wrap around
across the ears, and measure across the infant’s mouth.
6. During an assessment of the new born, the associate nurse notes that when
the baby’s head is turned to the right side, the leg and arm on the right side will
extend, while the leg and arm on the left side will also flex. The associate nurse
documents this as what type of reflex?
a. Rooting Reflex
b. Sucking Reflex
c. Moro Reflex
d. Tonic Neck Reflex
7. The associate nurse notes that when a finger is placed under the toes of the
newborn, the toes will curl downward. This is known as the ……?
a. Babinski reflex
b. Plantar grasp reflex
c. Tonic neck reflex
d. Step reflex
8. When does the sucking reflex in an infant disappear and become voluntary?
a. 6 months
b. 2 months
c. 4 months
d. 12 months
9. Speeding of postpartum recovery is the one of the benefits of breastfeeding to
the mother. Respond by True or False.
a. True
b. False
10. True or False: To maintain a schedule, a breastfed baby should only be fed
every three hours.
a. True
b. False
c. SECTION B: SHORT ANSWERS
11. What is the difference between the baby’s chest and head circumferences?
12. When the head and chest circumference may be equal?
13. How to check for audibility while assessing the newborn baby?
14. How will the associate nurse know the clavicle injury to the newborn?
15. What will the associate nurse check on newborn’s nose?
16. What is hypotelorism and hypertelorism?
17. What is the pseudo menstruation?
18. What are the signs of potential distress or deviations from expected findings
the associate nurse will notice while assessing the respiration patterns for the
baby?
19. List 5 Abnormal findings or lesions on the newborn ‘skin that require
evaluation, specific management or observation
20. Why does the healthcare providers need to check for reflexes
21. In HBB, what is done by the health care provider before delivery?
22. What are the signs showing that the baby is hungry and needs to breastfeed?
REFERENCES
1. Annama, J. (2012). A COmprehensive Textbook Of Midwifery & Gynecological
Nursing
2. Breastfeeding. A Guide for the Medical Profession Book • Ninth Edition •
2021. By Ruth A. Lawrence & Robert M. Lawrence
3. Committee, F. S. M. and N. H. (SMNH) (2012) ‘Management of the second
stage of labor’, International Journal of Gynecology & Obstetrics, 119(2), pp.
111–116. doi: https://doi.org/10.1016/j.ijgo.2012.08.002.
4. Deitra, L., Shannon, E., Kitty, C. (2016). Maternity women’s health care. 11th
Edition
5. Durham, R. and Chapman, L. (2013) Maternal-newborn nursing: The critical
components of nursing care. FA Davis.
6. Early essential newborn care. Clinical practice pocket guide. First Embrace.
By World Health Organization
7. Edmonds, K. (2018) Dewhurst’s Textbook of Obstetrics & Gynaecology. John
Wiley & Sons.
8. Examination of the Newborn. A Practical Guide. By Helen Baston,Heather
Durward. 2017.
9. Fuwa, K. et al. (2021) ‘Umbilical cord milking versus delayed cord clamping in
term infants: a systematic review and meta-analysis’, Journal of Perinatology,
41(7), pp. 1549–1557.
10. Hadlow, N. (2017). Biochemical Changes in Pregnancy-What Should A
Clinician Know ?, 4(1), 8–11. https://doi.org/10.19080/JGWH.2017.04.555626
11. Jacob, A. (2018) A Comprehensive Textbook of Midwifery & Gynecological
Nursing. Jaypee Brothers Medical Publishers.
12. Kloser, N. jayn., & Hatfield, N. T. (2010). Introductory Maternity and Pediatric
Nursing. China. Edition 2
13. Macdonald, S., & Magill-Cuerden, J. (2010). Mayer’s Midwifery Fourteeth
Edition. Bailliere Tindall Elsevier.
14. Marshall, H. K., John, H. K., & Phyllis, H. K. (2012). THE DOULA BOOK :
How a trained Labor Companion can help you have a Shorter , Easier,
and Healthier Birth (Third Edit). MERLOYD LAWRENCE BOOK DA CAPO
PRESS.
15. Marshall, J., & Raynor, M. (2014). Myles TEXT BOOK FOR MIDWIVES
(sixteen ed). Elsevier.
16. PCEP Maternal and Fetal Evaluation and Immediate Newborn Care (Book
I) (3rd Edition). By Robert A. Sinkin, MD, MPH, FAAP;Christian A. Chisholm,
MD, FACOG
17. Perry, L., & Alden, C. (2016). Maternal &Women’s Health Care. (E. F.olshansky,
Ed.) (11th Editi). St. Louis, Missouri: Elsevier.
18. Physical Assessment of the Newborn: A Comprehensive Approach to the
Art of Physical Examination, Fifth Edition. By Ellen P. Tappero&Marry Ellen
Honeyfield.
19. Regan, J., VanPutte, C., & Russo, A. (2016). SEELEY’S ESSENTIALS OF
ANATOMY & PHYSIOLOGY (Ninth edit). MC Graw Hill Education.
20. The Student Guide to the Newborn Infant Physical Examination. By Tracey
Jones.2020.
21. Weeks, A. (2007) ‘Umbilical cord clamping after birth’, BMJ (Clinical research
ed.), 335(7615), pp. 312–313. doi: 10.1136/bmj.39282.440787.80.
22. WHO (2009) WHO guidelines for the management of postpartum haemorrhage
and retained placenta. World Health Organization.
23. WHO (2018) WHO recommendations on intrapartum care for a positivechildbirth experience. World Health Organization.
