UNIT 3 LABOUR MONITORING
Key Unit competence: Monitor adequately a woman in labour
Introductory activity 3By looking at the following picture A and B, respond to the questions below:
1. Describe the situation on the above pictures.
2. What are the signs that characterize the mother’s situation on both pictures
A and B.
3. What should be the elements to assess on a pregnant woman?
4. According to the picture above explain how patient’s rights are respected.
3.1. Concepts of normal labour
Learning Activity 3.1
Using different source of information (internet, libraries) search for the meaning
of the following terms and be prepared for class presentation
1. Labour
2. Uterine contractions
3. Cervical effacement
4. Cervical dilatation
5. engagement
6. Descent
7. Stations
During the last weeks of pregnancy, a woman and her fetus prepares for the labour
process. This process is considered as normal at 40 weeks (- or + 2 weeks). The
pregnant woman undergoes the various physiological changes and adaptations
during pregnancy that prepares her for childbirth and later along motherhood. The
term labor refers to the process of moving the fetus, placenta, and membranes
out of the uterus and through the birth canal. The labour process occurs with the
presence of uterine contractions which are forceful and very painful motion of the
uterus resulting in tightening and shortening of the uterine muscles.
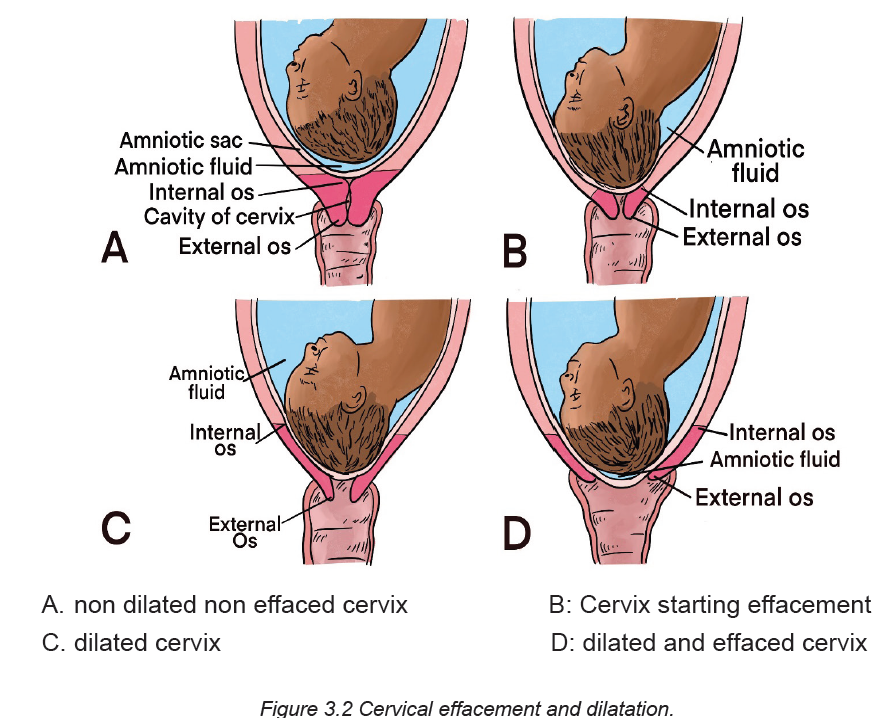
The presence of uterine contractions also facilitates the cervical effacement which
refers to the softening, thinning and shortening of the cervical canal. In primigravida,
the cervical effacement occurs before the cervical dilatation referring to the increase
in diameter of the cervical opening. Contrary to prim gravida, these two processesoccur simultaneously among multigravida women
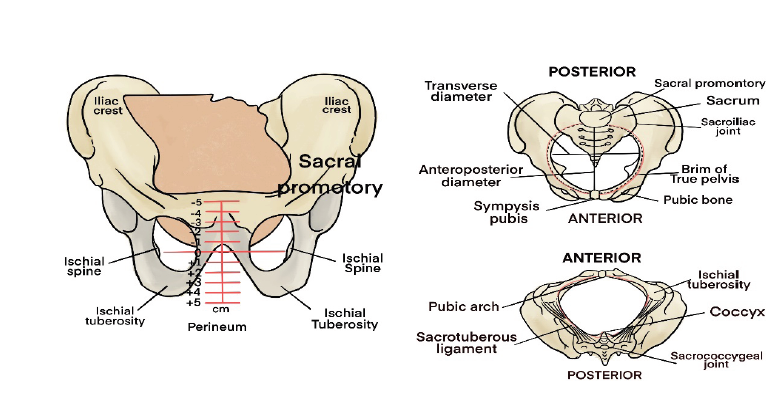
The fetus begun to enter the maternal pelvis and when then largest transverse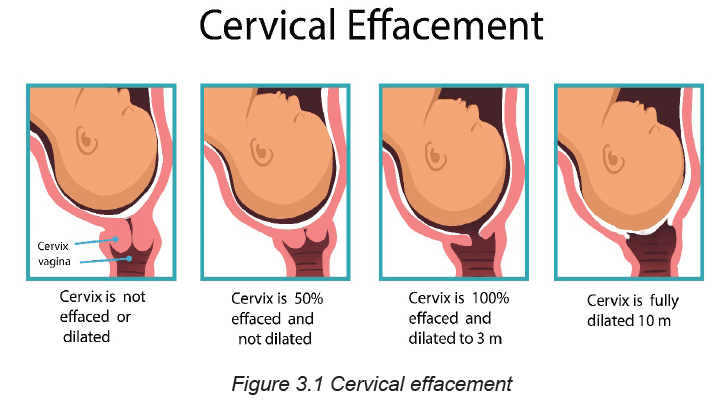
diameter of the presenting part (usually biparietal diameter in case of Cephalic
presentation or bitrochanteric diameter in breech presentation) has passed
though the maternal pelvic brim or inlet into the true pelvis this process is named
engagement. When the fetus is engaged, the presenting part continues to progress
through the pelvis (Descent). The descent of the fetus and its relationship to thelevel of ischial spines is evaluated and reported as stations.
Self-assessment 3.1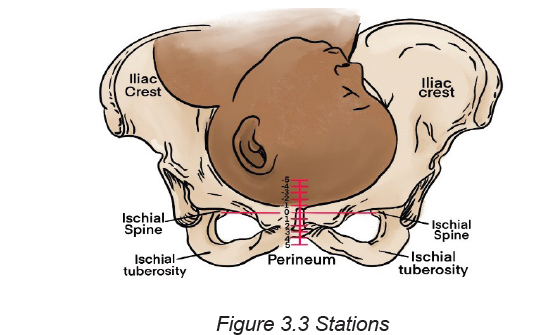
1. Define labour and uterine contractions.
2. Differentiate cervical dilatation from cervical effacement.
3.2. Signs preceding labor, types and onset of labour
Learning Activity 3.2
Use books or other sources of information to answer the following questions.
1. What are the common signs that may indicate that a woman will be soon
in labour?
2. What are the types of labour for a pregnant woman?
3. Describe the onset of labour for a pregnant woman.
3.2.1. Signs preceding labour
Before the onset of labor, a number of physiological changes occur that signal the
readiness for labor and birth. These changes are usually noted by the primigravid
woman at about 38 weeks of gestation. In multigravidas, they may not take place
until labor begins.
Labor itself can be discussed in terms of the mechanisms involved in the process
and the stages through which the woman moves.
3.2.2 Types of labour
False labour
Braxton-Hicks contractions As the pregnancy approaches term, most women
become more aware of irregular contractions called Braxton-Hicks contractions.
As the contractions increase in frequency (they may occur as often as every 10
to 20 minutes), they may be associated with increased discomfort. Braxton-Hicks
contractions are usually felt in the abdomen or groin region and patients may
mistake them for true labor. It is believed that these contractions contribute to the
preparation of the cervix and uterus for the advent of true labor. Braxton-Hicks
contractions do not lead to dilation or effacement of the cervix, and thus are often
termed “false labor.”
True labour
As time passes, the woman’s uterine contractions increase the intensity, regularity
and pain. A woman starting labour experiences cervical changes in preparation
for passage of the fetus. The cervix soften (cervical ripening), stretches, and thin,
and eventually is taken up into the lower segment of the uterus. This softening
and thinning is called cervical effacement. As the effacement progresses, there
may be rupture of the small cervical capillaries. The added pressure created by
engagement of the presenting part may lead to the expulsion of a brownish or
blood-tinged cervical mucus plug, called bloody show. This mucus acts as a
protective barrier for the uterus and its contents throughout the pregnancy. The
cervix becomes soft (ripens) and partially effaced and may begin to dilate.
Rupture of membranes
A few numbers of pregnant women experience spontaneous rupture of the amniotic
sac (“rupture of membranes” or “rupture of the bag of water” prior to onset of
labour. the rupture of membrane may be spontaneous or artificial. The rupture of
membrane is a critical event in pregnancy.
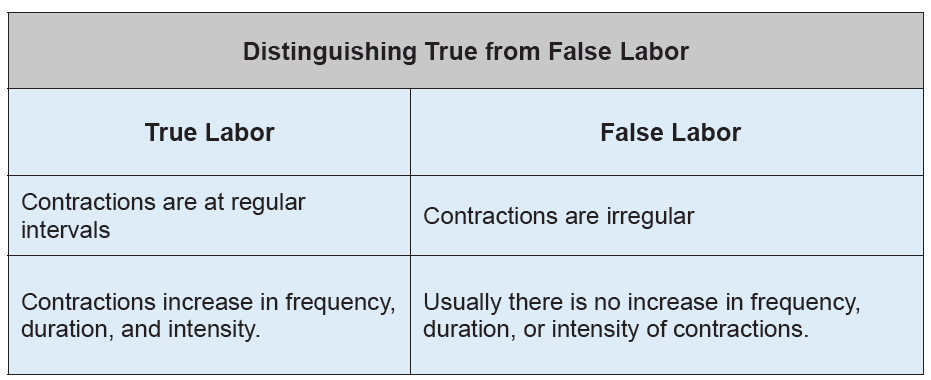
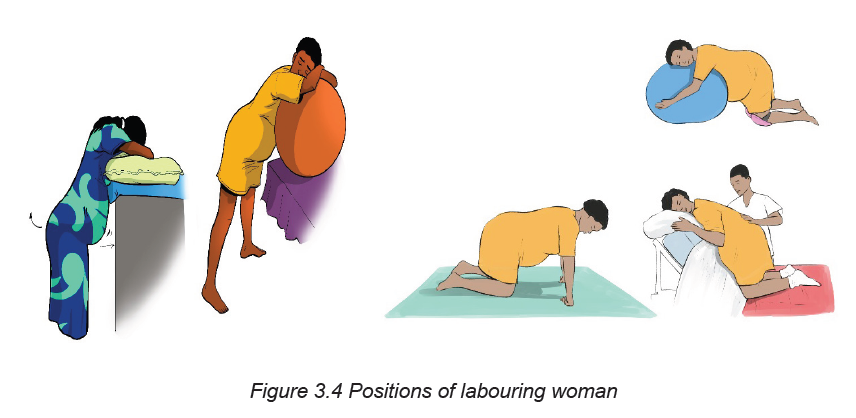
Table no 3.1 Differences between False and Truelabor
3.2.3. Onset of labor
At the onset of labor, the position of the fetus with respect to the birth canal is critical
to the route of delivery. The onset of labour is determined by a complex interaction
of maternal and fetal hormones and it is not yet well understood. Childbirth is theperiod from the onset of regular uterine contractions until expulsion of the placenta.
Self-assessment 3.2
1. List four signs that may signify impending of labour?
2. Distinguish the two types of labour for a pregnant woman
3. What determines the onset of labour of a pregnant woman?
4. Describe when a woman experiencing contractions at term should beinstructed to go to the hospital.
3.3. Factors affecting labour and Mechanism of labour
Learning Activity 3.3
When a pregnant woman is on labour there are factors that are affecting labour
process. Use books or other sources of information to answer the followings
questions:
1. List 2 factors affecting the labour process?
2. What are the 7 elements of the mechanism of labour?
The mechanisms of labor, also known as the cardinal movements, involve changes
in the position of the fetus’s head during its passage in labor. These are described
in relation to a vertex presentation.
The labour and birth process are affected by at least five factors. These factors are
known as:
A. Factors affecting labour
Five P’s : Passageway( Birth canal) , Passenger ( fetus and placenta ) ,Power
( Uterine contractions ) , Position of the mother , and psychologic response of
the mother. Based on the maternal needs and her childbearing rights, a sixth P is
added which is Partner. This partner may be her husband /life partner or a person
of her choice.
The first four factors are presented here as the basic for understanding the
physiologic process of labour. The firth and six Ps are the factors that may affect
labour indirectly but with positive impact.
• Passageway
The passageway, or birth canal, is composed of the mother’s rigid bony pelvis
and the soft tissues of the cervix, the pelvic floor, the vagina, and the introitus
(the external opening to the vagina). Even though the soft tissues, particularly
the muscular layers of the pelvic floor, contribute to vaginal birth of the fetus, the
maternal pelvis plays a far greater role in the labor process because the fetus must
successfully accommodate itself to this relatively rigid passageway.
• Passenger
During labour and birth process the fetus moves through the birth canal. These
fetal movements are affected by the following factors: The fetal presentation, lie,
attitude, position and size.
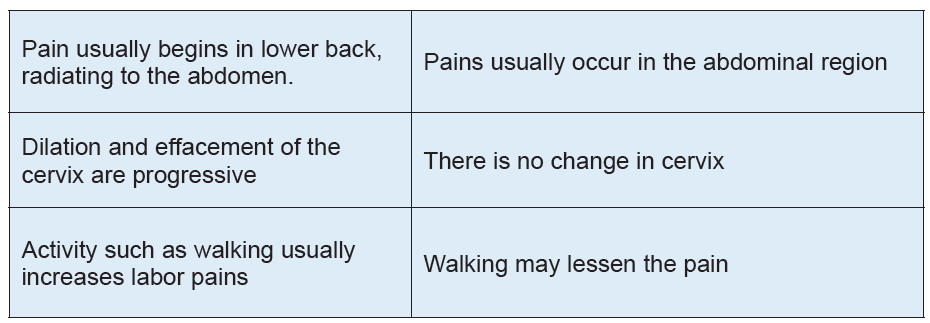
• Position of a labouring woman:
Position of the labouring woman affects the woman’s anatomic and physiologic
adaptations to labour. Frequent changes in position relieve fatigue, increase comfort,
and improve circulation. Therefore, a laboring woman should be encouraged to find
positions that are most comfortable to her. Positioning for labor may be determined
by the woman’s preference, but choices are limited by her condition or that of the
fetus, the environment, and the health care provider’s confidence in assisting in ina specific position.
B. Mechanism of Labour
The most common fetal presentation is Occiput Anterior Presentation (Vertex
presentation). During labour process, the fetus adopts positional changes in the
presenting part required to navigate the pelvic canal. These positional changes
constitute the mechanism of labour
The cardinal movements of labour are engagement, descent, flexion, Internal
rotation, extension, external rotation, and expulsion
A. Engagement
The term engagement designates the mechanism by which the biparietal diameter
“the greatest transverse diameter in an occiput presentation” passes through the
pelvic inlet is designated engagement
B. Descent
Descent refers to the progress of the presenting part through the pelvis. Descent
depends on at least four forces: (1) pressure exerted by the amniotic fluid, (2) direct
pressure exerted by the contracting fundus on the fetus, (3) force of the contraction
of the maternal diaphragm and abdominal muscles in the second stage of labor,
and (4) extension and straightening of the fetal body. The effects of these forces
are modified by the size and shape of the maternal pelvic planes and the size of the
fetal head and its capacity to mold.
C. Flexion
As soon as the descending head meets resistance from the cervix, pelvic wall, or
pelvic floor, it normally flexes so that the chin is brought into closer contact with the
fetal chest (see Fig. 16-12, B). Flexion permits the smaller suboccipito-bregmatic
diameter (9.5 cm) rather than the larger diameters to present to the outlet.
D. Internal rotation
The maternal pelvic inlet is widest in the transverse diameter; therefore, the fetal
head passes the inlet into the true pelvis in the occipito-transverse position. The
outlet is widest in the anteroposterior diameter; for the fetus to exit, the head must
rotate. Internal rotation begins at the level of the ischial spines but is not completed
until the presenting part reaches the lower pelvis. As the occiput rotates anteriorly,
the face rotates posteriorly. With each contraction the fetal head is guided by the
bony pelvis and the muscles of the pelvic floor.
E. Extension
After internal rotation, the sharply flexed head reaches the vulva and undergoes
extension. When the fetal head reaches the perineum for birth, it is deflected
anteriorly by the perineum. The occiput passes under the lower border of the
symphysis pubis first, and then the head emerges by extension
When the head presses upon the pelvic floor, however, two forces come into play.
The first force, exerted by the uterus, acts more posteriorly, and the second, supplied
by the resistant pelvic floor and the symphysis, acts more anteriorly. The resultant
vector is in the direction of the vulvar opening, thereby causing head extension.
This brings the base, first the occiput into direct contact with the inferior margin of
the symphysis pubis, then the face, and finally the chin.
P. External rotation
After the head is born it rotates briefly to the position it occupied when it was engaged
in the inlet. This movement is referred to as restitution. The 45-degree turn realigns
the infant’s head with the back and shoulders. Restitution of the head to the oblique
position is followed by completion of external rotation to the transverse position.
This movement corresponds to rotation of the fetal body and serves to bring its biacromial
diameter into relation with the anteroposterior diameter of the pelvic outlet.
Thus, one shoulder is anterior behind the symphysis and the other is posterior.
This external rotation occurs as the shoulders engage and descend in maneuvers
similar to those of the head. As noted, the anterior shoulder descends first. When
it reaches the outlet, it rotates to the midline and is delivered from under the pubic
arch. The posterior shoulder is guided over the perineum until it is free of the vaginal
introitus.
G. Expulsion
After birth of the shoulders, the head and shoulders are lifted up toward the mother’s
pubic bone and the trunk of the baby is born by flexing it laterally in the direction
of the symphysis pubis. After delivery of the shoulders, the rest of the body quickly
passes. When the baby has completely emerged, birth is complete, and the secondstage of labor ends.
Self-assessment 3.3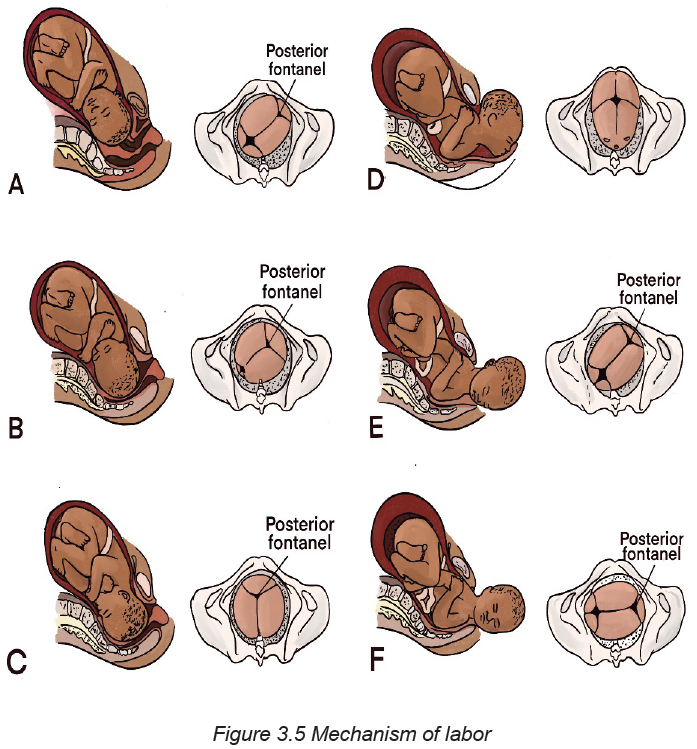
1. Define the fetal presentation?
2. Define the 5 Ps affecting labour?
3. Differentiate the first powers and secondary powers.
4. Explain the mechanism of labour
3.4. Assessment of a woman in labour: General history taking,
vital signs and physical examination
Learning Activity 3.4
Using textbooks and other resources identify different general pregnant woman’s
histories taken during history taking.
Pregnancy is typically a time of joy and anticipation. It can also be a time of anxiety
and concern. Listening and talking respectfully and sensitively with a woman and her
family can help build the woman’s trust and confidence in her health care providers.
Before starting the assessment remember to ask the woman if she has had any
danger signs (vaginal bleeding, gush of fluid or any problems such as fever, difficulty
breathing, cough, leg pain, etc.) or has any concern.
• The vital signs (temperature, blood pressure, heart rate and respiratory
rate) and parameters (Height, weight, BMI). Respond immediately to any
abnormalities in vital signs or other problems identified during the rapid initial
assessment.
• General Medical History: Ask about any serious medical diseases likely to
affect pregnancy and labour such as heart diseases, diabetes mellitus, renal
diseases, tuberculosis and sickle cell disease. Note any allergies to drugs,
Syphilis testing, VCT, HIV diagnosis or currently on any medication taken
regularly.
• Surgical history: Any previous hospitalizations for injuries to the pelvis and
spine, major or minor surgeries on the abdomen and blood transfusion.• Physical assessment includes the examination from head to toe.
Self-assessment 3.4
1. What are the vital signs and parameters taken during the pregnant woman’s
assessment?
2. What are the components of the general history taking?
3.5. Assessment of a woman in labour: Obstetrical history taking
Learning Activity 3.5
Using text books and other sources of information, identify the components of
obstetrical and gynecological history of a woman on labour.
• History of the present pregnancy: It includes the date of the first day of
the last normal menstrual period (LMP), the Parity and Gravidity. From this,
calculate and record the expected date of delivery (EDD). Ask the woman
about the history of this labour: approximate time contractions began and
membranes ruptured (when, what color and odor?).
• Past obstetric history: You should ask the mother about the outcomes
or complications of each of the previous pregnancies. Inquire whether she
delivered at home or at a hospital. Ask for the birth weights of the children,
whether they were breastfed and whether they are alive or not.
• Gynecological history: This will include the menstrual history, any past
operations for gynecological complaints and sexually transmitted infections
(STI).
Self-assessment 3.5
A pregnant woman attends the health post complaining of labour pains and
she explained that she has attended antenatal care 4 times and this is her 3rd
pregnancy and her last menstruation date is 12th/January /2021
1. Calculate her expected date of delivery (EDD)
2. What are the questions that you would ask to know the history of the present
pregnancy.
2. What are the obstetrical history would you ask her?3. What are the questions will you ask her to know her gynecological history?
3.6 Assessment of a woman in labour: Obstetrical examination
Learning Activity 3.6
Using text books and other sources, identify the steps of obstetrical examination
for a woman on labour.
Abdominal palpation: Check the woman’s abdomen for caesarean scar; a
horizontal ridge across lower abdomen (if present, ask the woman to empty her
bladder and observe her again). This examination includes Leopold maneuvers
(palpation to determine position, lie, engagement and descent of the presenting
part); uterine contraction palpation (palpate uterine contraction at the fundus,
record duration in seconds, frequency which is the number of uterine contractions
in 10 minutes, and the intensity of contractions). It also includes listening to fetal
heart rate for one whole minute (20-30 minutes baseline, External fetal monitoring
is required) and
Digital vaginal examination (DVE): To determine the cervical position, length,
thickness, dilation and effacement. Assessment of the state of membranes (intact,
ruptured, color and consistency, amount and note the time of rupture); we also
assess the pelvic floor; the diagnosis of the position and evaluation of the descent
of the fetal presenting part. Assess the descent in terms of fifths of fetal head
palpable above the symphysis pubis. A head that is entirely above the symphysis
pubis is five fifths (5/5) palpable; a head that is entirely below the symphysis pubis
is zero fifths (0/5) palpable. The vaginal examination equipment and steps to follow
are described below:
► Equipment: sterile examination gloves (clean gloves may be used if the
membranes are intact); sterile lubricant; antiseptic solution and light source
(if required); disposable wipes.
► Steps:
a. Wash and dry your hands. Explain the procedure and purpose of the
examination to the patient. RATIONALE: Hand washing helps to prevent
the spread of microorganisms. Explanations help to decrease anxiety and
promote patient understanding and cooperation.
b. Assess for latex allergies. RATIONALE: To prevent injury from latex exposure;
if patient has a latex allergy, use non latex gloves.
c. Ensure privacy. RATIONALE: Privacy promotes comfort and self-esteem.
d. Assemble necessary equipment including clean gloves (if the membranes are
intact) or sterile examination gloves (if the membranes are ruptured), sterile
lubricant, and antiseptic solution (if required).
e. Position the patient in a supine position with a small pillow or towel under
her hip to prevent supine hypotension. Instruct the patient to relax and
position herself with her thighs flexed and abducted. RATIONALE: Relaxation
decreases muscle tension and enhances patient comfort. Proper positioning
facilitates the examination by providing access to the perineum.
f. Don sterile gloves (clean gloves may be used if the membranes are intact).
g. Inspect the perineum for any redness, irritation, or vesicles.
h. Using the nondominant hand, spread the labia majora and continue
assessment of the genitalia. Note the presence of any discharge including
blood or amniotic fluid. RATIONALE: Positioning the hand in this manner
facilitates good visualization of the perineum. The presence of lesions may be
indicative of an infection and possibly preclude a vaginal birth. The presence
of amniotic fluid implies that the membranes have ruptured.
i. Gently insert the lubricated gloved index and third fingers into the vagina in
the direction of the posterior wall until they touch the cervix. The uterus may
be stabilized by placing the nondominant hand on the woman’s abdomen.
j. Assess the cervix for effacement and the amount of dilation.
k. Assess for intact membranes; if fluid is expressed, test for amniotic fluid.
l. Palpate the presenting part. RATIONALE: It is necessary to determine the
presenting part in order to assess fetal position and evaluate fetal descent.
m. Assess fetal descent and station by identifying the position of the posterior
fontanel.
n. Withdraw the fingers. Assist the patient in wiping her perineum from front to
back to remove lubricant or secretions. Help her to resume a comfortable
position. RATIONALE: Wiping from front to back prevents the transfer of
rectal contamination toward the vagina.
o. Inform the patient of the findings from the examination.
p. Wash hands. Document the procedure on the patient’s chart and on the fetal
monitor strip (if a fetal monitor is being used). Include the assessment findings
and the patient’s tolerance of the procedure. RATIONALE: Documentationprovides a record for communication and evaluation of patient care.
Laboratory investigations
Laboratory testing is a routine component of the admission process. Tests for blood
type and Rh factor, complete blood count (CBC), hemoglobin (Hb) and hematocrit
(HCT), and blood glucose/Glycemia are basically obtained. Blood tests for syphilis,
hepatitis B, and HIV are also collected. The urine specimen is tested for the
presence of protein, glucose, blood, pus, bacteria and ketones.
Self-assessment 3.6
A pregnant woman attends health post complaining of lombo pelvic pains on a
term pregnancy. When asked she told you that she started laboring for the past
two hours.
1. Explain the steps of obstetrical examination?
2. What are the required laboratory tests for her before transfer?
A. Use of partograph
Learning Activity 3.7
Observe the picture bellow and answer the following questions:
1. What is the name of this tool?
2. What is this tool used for?
3. What are the elements that are on this tool? Picture is missing here evenpicture description as part of learning activity.
The partograph was developed and extensively tested by the world health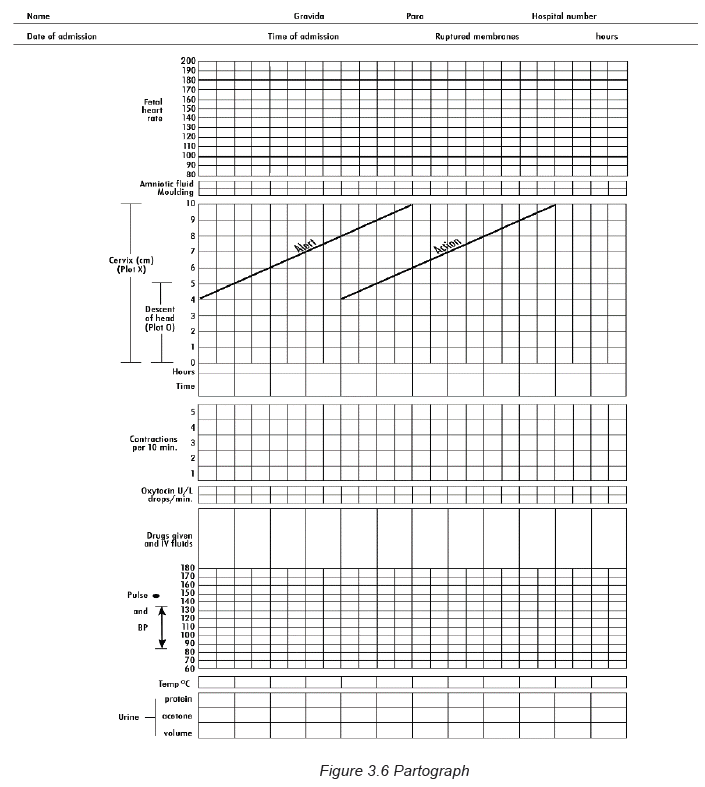
organization WHO for guiding birth attendant to have a good overview of labor
progression and therefore decide appropriate action. The partograph is accessible
in paper and electronic versions for most health care workers in maternity as the
tool of labor monitoring.
The use of partograph helps in health facilities for early detection of abnormal progress
of a labor; prevention of prolonged labor; recognition cephalopelvic disproportion;
early decision on transfer, augmentation, or termination of labor; increased quality
and regularity of all observations of mother and fetus; early recognition of maternal
or fetal problems; reduction of complications from prolonged labor for the mother
and for the newborn.
All observations and examinations like cervical dilatation; effacement; decent of
presenting part; strengths and duration of uterine contractions; maternal and fetal
wellbeing and any drug treatment are documented on partograph.
Parts of the partograph
Plotting on the partograph begins in the active phase when the cervix is 4 cm
dilated. The partograph should be enlarged to full size before use.
The following are element to be recorded on the partograph:
1. Maternal information and conditions:
Woman’s name; gravida; para, hospital number; date and time of admission; time
of ruptured membranes; Pulse recorded every30 min and mark with a dot (•); Blood
pressure every 4 hours; Temperature every 2hours; Urine output, Protein and
Glucose when urine is passed.
2. Fetal conditions:
Fetal heart rate every half hour; Colour of the amniotic fluid and the status of
membranes at every vaginal examination as I: membranes intact, R: membranes
ruptured, C: membranes ruptured, clear fluid, M: meconium-stained fluid, B: bloodstained
fluid; Moulding as 1: sutures apposed 2: sutures overlapped but reducible
sutures overlapped and not reducible.
3. Progress of labor:
Cervical dilatation at every vaginal examination and mark a cross (X) and start
to plot it at 4 cm. There are two lines Alert line which starts at 4 cm of cervical
dilatation to the point of expected full dilatation at the rate of 1 cm per hour and
Action line which is parallel and four hours to the right of the alert line; Descent
as a circle (O) at every abdominal examination. At 5/5, the sinciput is completely
above the symphysis pubis; at 4/5, the sinciput is high and occiput easily felt;
at 3/5 the sinciput is easily felt; at 2/5, the sinciput is felt and occiput just felt; at
1/5, the sinciput is felt and occiput is not felt; at 0/5, none of the head is palpable.
Assess contractions every half hour and count the number of contractions in a
10-minute time period and their duration in seconds and intensity. The contractions
are recorded as follows: less than 20 seconds: ; between 20 and 40 seconds:
; more than 40 seconds:
4. Drugs: Oxytocin when used, record the amount per volume of IV fluids in
drops per minute every 30 minutes; any additional drugs given are alsorecorded.
Self-assessment 3.7
Alexa is 38 years of age G4P3, was admitted at 10:00 am on 11 October 2021
with complaints of labour pains since 7:00 am. This is her first pregnancy. Plot
the following findings on the partograph:
At 10:00am:
• The cervix is dilated 4 cm.
• The fetal head is at 0 station, no moulding.
• The membranes are intact.
• She had 2 contractions in 10 minutes, each lasting less than 20 seconds.
• The FHR is 140 per minute.
• Her BP is 100/70 mmHg.
• Pulse: 82b/1minute.
• Her temperature is 37°C.
• Her pulse is 80 per minute• no oxytocin added
End unit assessment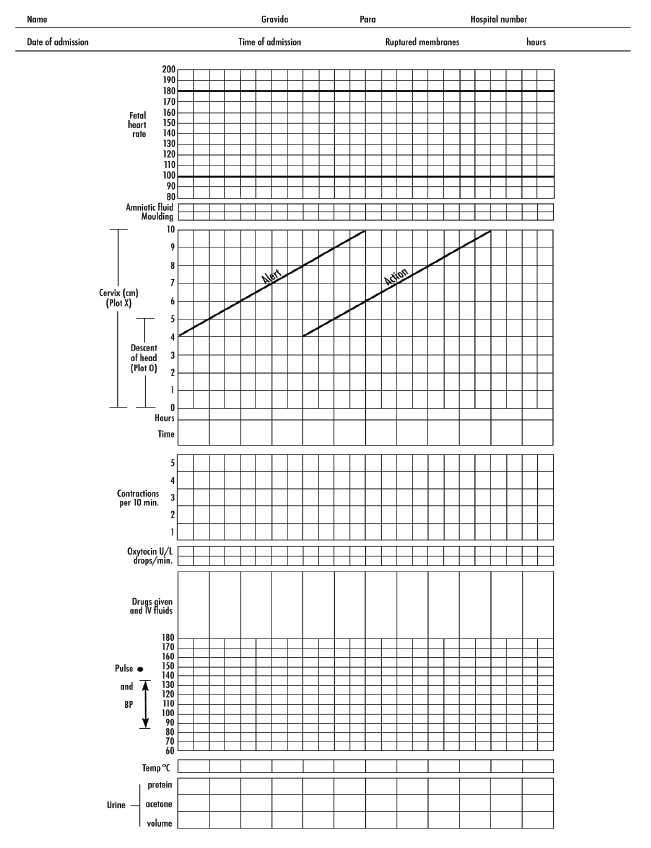
Mutesi is a 25-year-old G 1 P 0 at 39 weeks of gestation. She presents herself to
the health center at maternity ward and announces, “I’m here to have my baby. I
think I’m in labor.” Mutesi reports that she saw a thick bloody vaginal discharge
several hours ago when wiping after peeing earlier today. She states that she
has lower abdominal cramping (“It feels like the cramps I have with my periods”)
but denies leakage of vaginal fluid. Mutesi also reports active fetal movements.
In answering to your question, she replies that her current pain level is mild,
while alternating between texting on her phone and chatting with her mother,
who accompanied her to the hospital. Few hours later you observe change in
her pain. She expressed that her pain is increasing and she feels like pushing.
After assessment you realize her cervix is dilated at 6cm; effaced at 100%; the
baby’s head is at 0 station with vertex presentation; water bag is intact; the
Fetal heart rate are 140beats/min and regular; she has 3 contractions in 10 min
lasting between 20 and 40 seconds. The nurse at health post indicates that the
woman’s hemoglobin is 12g/dl; glycosuria is negative; temperature of 37.3oC;
Blood pressure is 100/80mmHg; Pulse of 86 beats/min and respiration of 20
mvts/min.
Plot all above information on partograph.
1. Define the following terminologies:
a. Labour
b. Uterine contractions
c. Stations
2. Describe the digital Vaginal examination that you would do to Mutesi?
3. What are the essential elements to focus on in your assessment?
4. Using the information you have above start plotting the partograph for thiswoman.
