UNIT 2 ANTENATAL CARE
Key Unit competence: Demonstrate the ability to manage a pregnant woman
during antenatal periodIntroductory activity 2.0
A 34 years old married housewife visited the health center complaining to be
pregnant. Since her pregnancy, it is her first time to visit the health center. During
interview with the nurse, the woman reported to have missed her periods 7
months ago, has increased appetite for cassava and rice only. She did not attend
earlier because of the fear of witchcraft to take her pregnancy away. She has
been using traditional medicines given by her mother in law from the beginning
of the pregnancy. She is experiencing, chills, headache, inability to carry out
daily living activities and she does not know her HIV status.
After reading and understanding the above case:
1. How can you interpret the case?2. What advice can you offer to women in this case?
Antenatal care (ANC) is an umbrella term used to describe the medical and nursing/
midwfery procedures and care that are carried out during pregnancy. It is the care
a woman receives throughout her pregnancy and is important in helping to ensure
a healthy pregnancy state and safe childbirth.
During the prenatal period, health care providers play important role in educating
women about healthy pregnancy behaviors, danger signs of complications,
breastfeeding and family planning; identify and treat pregnancy-related conditions;
refer mothers to specialized care when necessary; encourage the use of a skilled
birth attendant; and minimize the risk of mother-to-child transmission of HIV. In
addition, the ANC provides an opportunity to screen for and treat other chronicconditions and non-communicable diseases.
2.1 Key Concepts used in antenatal careLearning Activity 2.1
Using the school book of Maternal and Child Health, read the information related
to the antenatal care and take short notes on the difference between:
1. Antenatal care and focused antenatal care,
2. Health promotion, health education, health screening and diseasescreening
2.1.1 Antenatal Care
Antenatal care (prenatal care) is the care given to pregnant women from the time
conception is confirmed until the beginning of labour. The nurse provides her with
accessible and relevant information to help her make informed choices throughout
the pregnancy.
2.1.2 Focused Antenatal Care (FANC)
FANC is personalized care provided to a pregnant woman which emphasis on
the woman overall health status, her preparation for childbirth, and readiness for
complications.
2.1.3 Health Promotion
Health promotion refers to any activity that aims to achieve better health in a
community or a country.
2.1.4 Health education
It is the effective transmission of accurate, useful, health-related information to
community members; it enables individuals and groups to develop their knowledge
of health issues, and increase their self-reliance and competence to solve their
own health problems through their own initiatives. A major determinant of good or
ill health is the knowledge people have about health issues, their beliefs, attitudes
and behaviour, and their desire to bring about positive behaviour change in their
lives.
2.1.5 Health screening
Health screening is the routine testing of individuals to see if they are at risk of
developing a health problem. Health screening is an important health promotion
activity that you will conduct as part of your antenatal care service. For example,
you will take the temperature, blood pressure and pulse of every pregnant woman
at every antenatal visit to see if she may be developing a health problem that could
harm her or her baby.
2.1.6 Disease Prevention
It is any action taken to prevent a disease from developing. For example, giving
pregnant women iron supplements as a routine part of antenatal care is an action to
prevent the development of anaemia, a condition in which the body makes too fewred blood cells because the woman’s diet does not contain enough iron.
2.1.7 Booking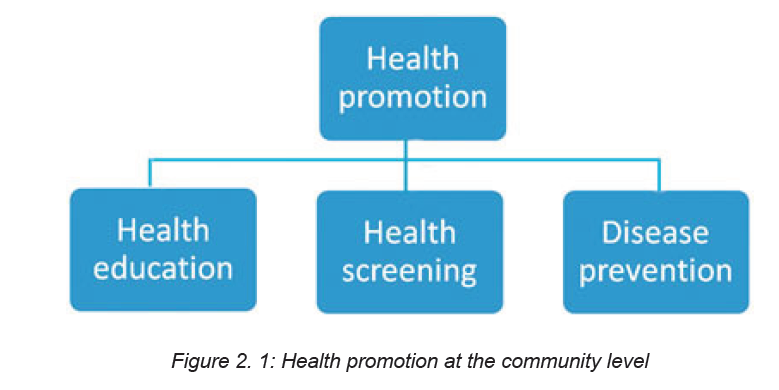
An Antenatal Booking Appointment is the APPOINTMENT where the woman enters
the maternity care pathway, characterized by information giving and detailed history
taking to help the woman choose the most appropriate Antenatal care pathway.
2.1.8 History taking
History taking is the process of collecting information to assess the past and present
obstetrical, medical and surgical problems in order to detect risk factors for thepatient and her fetus.
Self-assessment 2.1
1. Discuss the objectives of the initial assessment (booking)2. What is history taking and state the purpose for taking history.
2.2 Principles, objectives and components of Focused Antenatal
CareLearning Activity 2.2
1. On the above chart, describe the person A and B, and what you think, they
are doing
2. From the above chart, identify the importance of communication
Focused antenatal care (FANC) is a personalized care provided to a pregnant
woman which emphasizes on the women’s overall health status, her preparation
for child birth and readiness for complications or it is timely, friendly, simple safe
services to pregnant women.
Principles of FANC are as follow:
a. Developing a trusting relationship with the woman
b. Providing a holistic approach to the woman’s care that meets her individual
needs
c. Making a comprehensive assessment of the woman’s health and social status
d. Promoting an awareness of the public health issues for the woman and her
family
e. Exchange the information with the woman and her family
f. Enabling them to make informed choices about pregnancy and birth
g. Be an advocate for the woman and her family during her pregnancy
h. Supporting her to choose care appropriate for her own needs and those of
her family
i. Identifying potential risk factors and taking appropriate measures to minimize
them
j. Timely share information with relevant agencies and professionals
k. Accurate documentation of assessment, plans, care and evaluation
l. Recognizing complications of pregnancy and appropriately referring women
to the obstetric team or relevant health professionals
m. Preparing the woman and her family to meet the challenges of labour and
birth, and facilitating the development of birth plan
n. Facilitating the woman to make an informed choice about methods of infant
feeding and giving appropriate and sensitive advice to support her decision
o. Offering parenthood education within a planned programme or on individual
basis
Major goals/objectives of the FANC are as follow:
a. Promote and maintain the physical, mental, and social health of mother and
baby by providing education on nutrition, personal hygiene, and birthing
process;
b. Detect and manage complications during pregnancy, whether medical,
surgical, or obstetrical;
c. Develop birth preparedness and complication readiness plan;
d. Help prepare mother to breastfeed successfully, experience normal
puerperium, and take good care of the child physically, psychologically, and
socially.
Components of FANC are as follow:
a. Blood pressure measurement,
b. Provision of a blood sample,
c. Provision of a urine sample,
d. Tetanus vaccination,
e. Intermittent preventive treatment of malaria during pregnancy (IPTp) including
number of times,
f. Deworming treatment,
g. Iron-folic acid supplements
COMMUNICATION IN MATERNITY
The nurse requires many skills to provide optimal antenatal care. Fundamentally the
ability to communicate effectively and sensitively. Listening skills involve focusing
on what the woman is saying and how she is saying it, considering the content and
tone.in addition non-verbal communication.
Importance of communication in antenatal care
Communication skills are critical to the delivery of high-quality maternity services.
It is impossible to ensure the provision of the best possible care, using available
resources to their fullest, without accurate and complete communication with
women, their families and multi-professionals.
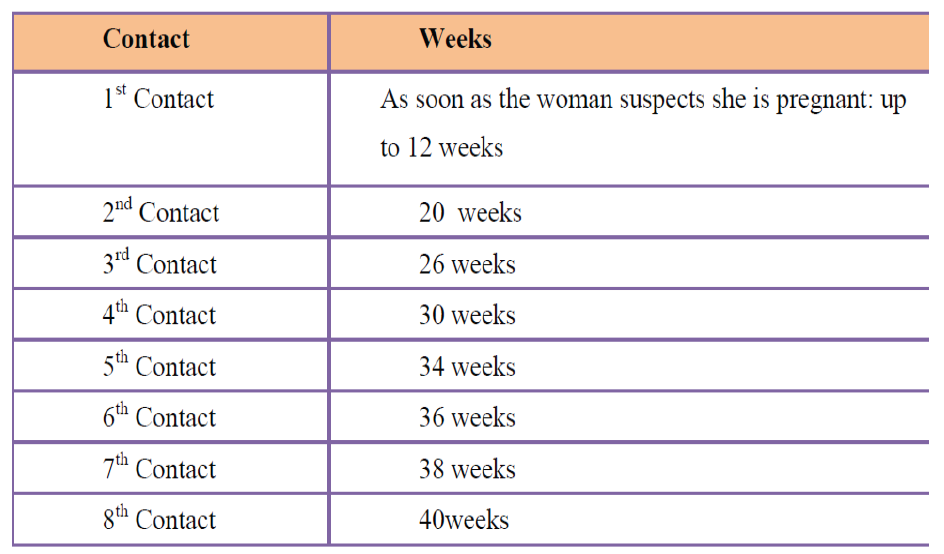
Table 2. 1: ANC schedule for the new model of eightcontacts
Self-assessment 2.2
– Discuss the principles of FANC– What are the components of antenatal care?
2.3 The diagnosis of pregnancyLearning Activity 2.3
A 22 years’ young lady, visited health care facility complaining of nausea,
tiredness, loss of appetite, she vomited two time in morning, and she stated not
having her menstrual period last month.
– What do you think would be the problem and which advice can you give
to her?
Most women are diagnosed with pregnancy after a missed menstrual cycle and a
positive urine or serum HCG. The pregnancy is diagnosed as viable with serial
exams and normal pregnancy development, a normal dating ultrasound, or positivefetal heart tones by Doppler.
Women who are aware of their bodies must begin to suspect that they are pregnant
within the first few days of pregnancy. But for most, the first sign is missing a period.
Other symptoms include nausea and vomiting, breast tenderness and fullness,
urinary frequency, and fatigue.
Traditionally, diagnosis has been based on history, and physical examination.
Issues that may confuse the diagnosis of an early pregnancy are an atypical last
menstrual period, contraceptive use, and history of irregular periods. Spotting or
light bleeding is common in early pregnancy between six and seven weeks which
may further complicate the assessment.
SIGNS AND SYMPTOMS OF PREGNANCY
PRESUMPTIVE SIGNS
Presumptive signs and symptoms of pregnancy are those signs and symptoms
that are usually noted by the client, which impel her to seek care. These signs and
symptoms are not proof of pregnancy but they will make the health provider and
woman suspicious of pregnancy.
Amenorrhea (Cessation of Menstruation)
Amenorrhea is one of the earliest clues of pregnancy. The majority of clients have
no periodic bleeding after the onset of pregnancy
Other causes for amenorrhea must be ruled out, such as:
♦ Menopause.
♦ Stress (severe emotional shock, tension, fear …)
♦ Chronic illness (tuberculosis, endocrine disorders, or central nervous system
abnormality).
♦ Anemia.
Nausea and Vomiting (Morning Sickness)
Usually occurs in early morning during the first weeks of pregnancy. It is usually
spontaneous and subsides in 6 to 8 weeks or by the twelfth to sixteenth week of
pregnancy. Nausea and vomiting are unreliable signs of pregnancy since they may
result from other conditions.
Frequent Urination:
Frequent urination is caused by pressure of the expanding uterus on the bladder.
It subsides as pregnancy progresses and the uterus rises out of the pelvic cavity. The
uterus returns during the last weeks of pregnancy as the head of the fetus presses
against the bladder. Frequent urination is not a definite sign since other factors can
be apparent (such as tension, diabetes, urinary tract infection, or tumors).
Breast changes
In early pregnancy, changes start with a slight, temporary enlargement of the
breasts causing a sensation of weight, fullness, and mild tingling. As pregnancy
continues the patient may notice Darkening of the areola--the brown part around the
nipple. Enlargement of Montgomery glands--the tiny nodules or sebaceous gland
within the areola. Increased firmness or tenderness of the breasts More prominent
and visible veins due to the increased blood supply. Presence of colostrum (thin
yellowish fluid that is the precursor of breast milk). This can be expressed during
the second trimester and may even leak out in the latter part of the pregnancy.
Vaginal changes
CHADWICK’S SIGN: The vaginal walls have taken on a deeper colour caused by
the increased vascularity because of increased hormones. It is noted at the sixth
week when associated with pregnancy. It may also be noted with a rapidly growing
uterine tumor or any cause of pelvic congestion.
Quickening (FIRST FETAL MOVEMENT FELT BY THE MOTHER)
This is the first perception of fetal movement within the uterus. It usually occurs
toward the end the fifth month because of spasmodic flutter.
♦ A multigravida can feel quickening as early as 16 weeks.
♦ A primigravida usually cannot feel quickening until after 18 weeks.
Skin changes
Striae gravidarum (stretch marks). These are marks noted on the abdomen and/or
buttocks.
These marks may be seen on a patient with Cushing’s disease or a patient with
sudden weight gain.
Linea nigra
his is a black line in the midline of the abdomen that may run from the sternum orumbilicus to the symphysis pubis.
This appears on the primigravida by the third month and keeps pace with the rising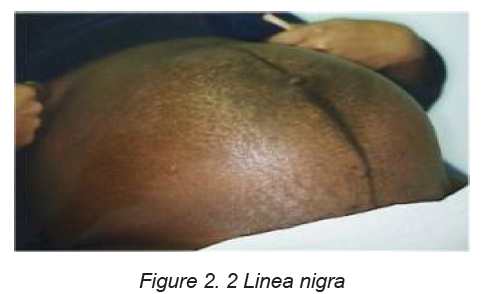
height of the fundus. The entire line may appear on the multigravida before the third
month.
Chloasma
This is called the “Mask of Pregnancy.” It is a bronze type of facial coloration seen
more on dark-haired women. It is seen after the sixteenth week of pregnancy.
PROBABLE SIGNS OF PREGNANCY
Probable signs of pregnancy are those signs commonly noted by the health providers
upon examination of the client. These signs include: uterine changes; abdominal
changes; cervical changes; basal body temperature; a positive pregnancy test and
fetal palpation.
Uterus grows - the abdomen gets larger
Position: By the twelfth week, the uterus rises above the symphysis pubis and it
should reach the xiphoid process by the 36th week of pregnancy.
Size: The uterine increases in width and length approximately five times its normal
size. Its weight increases from 50 grams to 1,000 grams.
Hegar’s Sign: This is softening of the lower uterine segment just above the cervix.
When the uterus is compressed between examining fingers
Ballottement: Ballottement is when the lower uterine segment or the cervix is
tapped by the examiner’s finger which is left in place during the procedure. The
fetus floats upwards, then sinks back and a gentle tap is felt on the finger .it is done
at 16th to 20th weeks
Abdominal Changes
This corresponds to changes that occur in the uterus. As the uterus grows, the
abdomen gets larger. Abdominal enlargement alone is not a sign of pregnancy.
Enlargement may be due to uterine or ovarian tumors, or edema.
Cervical changes
Goodell’s sign: The cervix is normally firm, like the cartilage at the end of the nose.
Goodell’s sign occurs when there is marked softening of the cervix. This is present
at the 6th week of pregnancy.
Formation of a mucous plug: This is due to hyperplasia of the cervical glands
as a result of increased hormones. It serves to seal the cervix of the pregnant
uterus and to protect it from contamination by bacteria in the vagina. The mucous
is expelled at the end of pregnancy near or at the onset of labour.
Braxton-Hick’s contractions: This involves painless uterine contractions occurring
throughout pregnancy. It usually begins at about the 12th week of pregnancy and
becomes progressively stronger. These contractions will, generally, cease with
walking or other forms of exercise.
POSITIVE SIGNS OF PREGNANCY
Positive signs of pregnancy are those signs that are definitely confirmed as a
pregnancy. They include fetal heart sounds, ultrasound scanning of the fetus,
palpation of the entire fetus, palpation of fetal movements, x-ray, and actual deliveryof an infant.
Self-assessment 2.3
– List positive signs of pregnancy– Describe the chloasma of pregnancy
2.4 Comprehensive assessment of a pregnant womanLearning Activity 2.4
A 30 years’ pregnant woman for the first time visited the health center for focused
antenatal consultation (FANC) at 12 weeks, during interview, you realized it was
her first antenatal contact, she stated that she does not have problem but she
wants to know the condition of her baby and pregnancy.
-In your opinion, suggest reasons why it is important to check the wellbeing of
mother and baby during pregnancy.
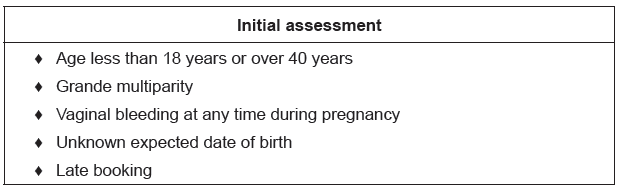
2.4.1 Introduction to Booking and history taking
The booking assessment shapes the direction of a woman ‘antenatal pathway.it is
where her risk status is determined and appropriate referral made. The information
gathered regarding the woman’s obstetric, medical and social history and current
pregnancy enables the nurse to assess her status. If a risk factor is identified, the
woman should be referred to the doctor who will discuss a plan of care for her
based on identified problem.
A comprehensive assessment is done from head to toe with the woman’s consent.
The initial assessment (Booking visit)
The purpose of this unit is to initiate the development of a trusting relationship that
facilitates positive engagement of the woman with the maternity service. This is
the most important element of ANC care. Whilst, it is crucial that risk assessment
and identification of clinical relevant information is obtained, none of these can be
undertaken if the woman does not feel able to communicate with the nurse.
Objectives for the initial assessment
♦ To assess levels of health by taking a detailed history and to offer appropriate
screening tests.
♦ To ascertain baseline recordings of blood pressure, urinalysis, blood values,
uterine growth and fetal development to be used as a standard for comparison
as the pregnancy progresses.
♦ To identify risk factors by taking accurate details of past and present history,
obstetrics, medical, family and personal history.
♦ To provide an opportunity for the woman and her family to express and discuss
any concerns they might have about the current pregnancy and previous
pregnancy loss, labour, birth or puerperium.
♦ To give public health advice and that pertaining to pregnancy in order to
maintain the health of the mother and the healthy development of the fetus.
♦ To build the foundation for a trusting relationship in which the woman and
midwife are partners in care.
♦ To make appropriate referral where additional healthcare or support needs
have been identified
First impressions
The initial observation and assessment of a woman at the start of first meeting is
very important. The observation should be carried sensitively enhancing the woman
to experiences of pregnancy birth.
Observation of physical characteristics is also important. Posture and gait can
indicate back problems or previous trauma to the pelvis; the woman may be
lethargic, which could be an indication of extreme tiredness, anemia, malnutritionor depression.
2.4.2 History taking:
This is the process of collecting all relevant information from a pregnant woman
which will build the bases for monitoring her pregnancy.
Points to consider while taking history
• Ensure privacy (respectful maternity care)
• Ensure quiet and calm atmosphere
• Make the woman comfortable and relaxed
• Maintain confidentiality
• Establish rapport
• Record all information on the patient’s file
• High light abnormal findings
History to be taken include:
A. Personal and preliminary data
♦ Woman full names
♦ Age
♦ Date and place of birth
♦ Address and phone number
♦ Ethnic or racial appartenance
♦ Profession and that of the partner or employment history
♦ Religion
♦ Marital status and number of years married
B. Chief complains: the major health problem or concern, and its time course
(e.g. abdominal pain for past 4 hours).
C. History of present illness
After determining the chief concern for a visit, the next step is to inquire about the
history of the present illness (HPI). This is often a misnomer—for example, the
reason for a visit of “I need my Pap test and birth control pills” leads to an HPI that
addresses how the woman is managing her contraception and her satisfaction with
her current method (and possibly to a discussion of screening recommendations). A
chief concern that begins with abnormal uterine bleeding leads to the more traditional
assessment of the history of the woman’s current symptoms. A common mnemonic
for the questions asked about a health problem is OLD CARTS (Onset, Location/
radiation, Duration, Character, Aggravating factors, Relieving factors, Timing, and
Severity). These questions can be followed by “What has changed now that made
you come in?” or “How did you decide it was time to come in?”
D. Social history
The social history, like the sexual history, brings up topics that may be embarrassing
or even threatening to some women. Ask these questions in a quiet, professional
tone, and respect the woman’s need to avoid certain answers. Providing information
“why” the information is needed often reassures the woman and may help the
midwife feel comfortable asking for it. Obviously if there is no reason for eliciting
sensitive information, asking it should be omitted. Relationship questions should
be asked in a pattern that allows women to reveal relationships that are more
complicated than “single” or “married with children.”Table 2. 2 Elements assessed in social history
E. General health status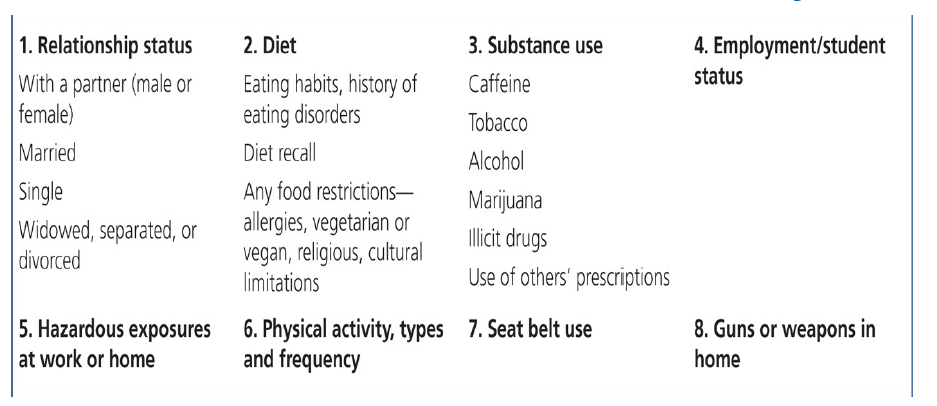
General health should be discussed and good habits reinforced, giving further
advice when required e.g exercise puts added demands on the cardiovascular and
respiratory systems, however mild exercise should be continued.
Smoking: women may be ready to cut down or give up smoking. The midwife has a
role or duty to help women to set goals throughout their pregnancy and help them
to cut down their smoking, strategies to help them cut down includes:
• Doing something else;
• Delaying having a cigarette or drinking water can help them cut down on
smoking.
Babies born to women who smoke are frequently smaller, have respiratory tract
problems at birth and in their first year, have higher rates of prematurity, still birth
and low birth weight. There is also increased risk of asthma and otitis media in
these babies for women who are more addicted should stick smoking earlier in the
day, stop last thing at night, they should be referred to appropriate organizations
for help.
• Alcohol: alcohol is less common but can affect the baby. There is no
conclusive evidence of adverse effects on the fetus at a consumption level
below 10 units per week, but it is recommended that women do not exceed
one to two unites once a week.
F. Menstrual history
An accurate menstrual history is taken to determine the expected date of delivery
(EDD). This will enable the midwife to predict a birth date and subsequently calculate
gestational age at any point in the pregnancy abdominal assessment of uterine size
can be during ANC consultation.
The duration of pregnancy could also be based on the Naegle’s rule which is
based on the mythical normal woman who has a 28 days cycle and ovulates two
weeks before the start of her next menstrual period i.e. on day 14. The rule is to add
seven days to the first day of the last menstrual period and count back three months
to reach the expected date of delivery or confinement or EDC.
The EDD is calculated by adding 9 calendar months if the last month of
menstruation is ≤ to 3 or moins 3 if month ≥ to 4 and adding 7 days to the date of
the 1st day of the woman’s last menstrual period (LMP) this method assumes that:
• The woman takes regular note of regularity and length of time between periods
• Conception occurred 14 days after the 1st day of the last period; this is true
only if the woman has a regular 28 days’ cycle.
• The last period of bleeding was true menstruation but implantation of the
ovum may cause slight bleeding.
Example on calculation of EDD
Calculating from “sure” dates by Naegele’s Rule
Cycle of 28days=LMP: 9 June 2014
EDD = 9+7days/6- 3/
EDD: 16 March 2015
NB: Gestational age in weeks of pregnancy can be calculated by using Mac Donald
formula which use the fundus height
The formula is Fundus height in cm *8 divides by 7. For example, if the fundus
height is 24 cm, gestational age is 24cm*8=192 = 27 week’s gestation.
The features to note are:
• Normality of last menstrual period; an implantation bleed may occur at about
the time of the expected period (i.e. 10-14 days after ovulation). This is almost
always much lighter and shorter than a normal period. If an implantation bleed
is mistaken for a time period, the gestational age calculation would be behind
by about four weeks.
• Cycle interruption: a calculation adjustment is needed in those women who
have not re-established regular cycles after pregnancy, lactation or the
contraceptive pills. However, as the differences in gestational age between
the two methods increase, ultrasound becomes the more accurate method
for predicting the EDD.
• The calculation is difficult if the woman does not know the date of her last
mentraual period, where cycles are irregular,or a normal cycle has not
resumed since taking the oral contraceptives pill.if the woman has a good
idea of when conception occurred ,the EDD can be calculated by adding 38
weeks to this date ,or subtracting 7 days from 9 months.
• Women should be asked to note the date when fetal movement are first felt.
Primigradae normally become aware of fetal movement between 18-20weeks
while multigradae recognize the sensation a little earlier, between 16-18weeks.
This may be used to estimate the expected date of delivery.
G. Family history
Certain conditions are genetic in origin others are familial or related to ethnicity and
some are associated with the physical or social environment in which the family
lives. The family history may reveal factors that increase the risk of blood disorder,
maternal medical complications or fetal abnormalities; e.g. Twins, Diabetes mellitus,
Hypertension, hereditary diseases like asthma.Table 2. 3 Family History (Three Generations)
H. Past medical history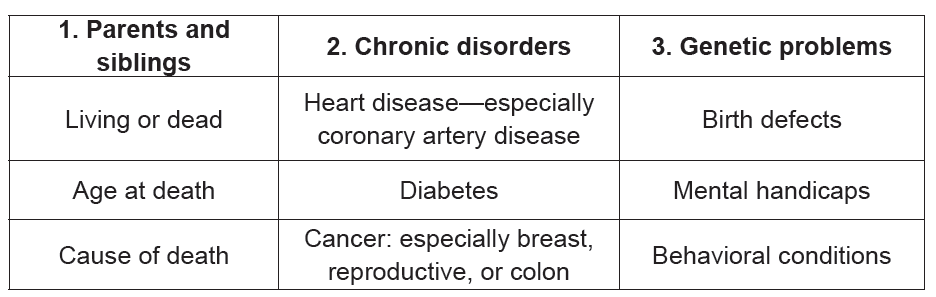
Past current medical disorders and associated medications may threaten the mother
and fetus e.g. Diabetes mellitus, Epilepsy, Rheumatics fever, Renal diseases.
During pregnancy both the mother and fetus may be affected by a medical condition
or a medical condition may be altered by the pregnancy, if untreated there may be
serious consequences for the woman’s health. Other conditions including asthma,
epilepsy, infections, and psychiatric disorders may require treatment, which may
adversely affect fetal development. Major medical complications such as diabetes
and cardiac conditions require the involvement and support of a medical specialist
♦ Urinary stasis and reflex occur during pregnancy. A urinary tract infection
(UTI) can easily develop into pyelonephritis, which, untreated may lead to
kidney damage and cause preterm labour, between 30 and 50% of women
will be asymptomatic if it is untreated;
♦ Pregnancy predisposes to deep vein thrombosis and thus pulmonary
embolism, women of increasing weight and maternal age, those who are
obese and those with a history of thromboembolic disorders are most at risk;
♦ Essential hypertension predisposes to pregnancy induced hypertension,
which can result in reduced placental function, intrauterine growth retardation,
abruption placenta, fetal compromise or death. Effect on the mother includes
congestive heart failure, intracerebral hemorrhage, acute renal failure,
disseminated intravascular coagulation (DIC) or death as a result of any of
above (Hallak 1999).
♦ Pregnancy and concomitant disease (Can be exacerbated by the pregnancy
or complicate it) especially Diabetes, Heart disease, Hypertension,
Neuromuscular disorders
♦ Medications and allergies to medications Should be identified and recorded
♦ Any current ongoing illness, e.g. diabetes, malaria
♦ Past history containing physiological and pathological data
Example: Past medical/surgical history including major illnesses, any previous
surgery/operations
I. Past surgical history
♦ General surgical procedures;
♦ Gynecological surgical procedures;
♦ Myomectomy scar may increase risk of uterine rupture;
♦ Conisation or cervical cerclage of the cervix and therapeutic abortion may
increase the risk of cervical incompetence and premature labour.
J. Past obstetric history/ General OB/GYN Assessment
Like histories in general, many complications of pregnancy have a tendency to
recur; it is for this reason that the previous obstetric history holds a wealth of
valuable relevant information:
Collect Subjective data
♦ Prenatal history
♦ Past pregnancies
♦ Gynecologic history including LPM
Obstetric History Concerns
♦ Gravida/para (G/P) status
• Number of living children?
• Number of dead children, when, how and on which pregnancy
• Complications with previous pregnancies or deliveries?
• History of preterm delivery?
• Gestational age?
• History of elective or spontaneous abortion?
• Has patient delivered vaginally after a cesarean section?
• When was, and what was length of last labor?
• With regard to current pregnancy, what is estimated date of confinement
(EDC)?
• Has patient received adequate, limited (three or fewer visits), or no prenatal
care?
• Any problem with pregnancy identified? If so, what?
• Diagnostic tests like ultrasound done? If so, what were results?
• Is patient taking any medications for obstetric or non-obstetric reasons?
• If so, which medication(s), what dose(s), and compliant schedule(s)?
• Drug or alcohol abuse suspected? If so, which substance(s), frequency of
use, date of last use? Patient smoking?
• Pregnancy weight gain normal, or patient malnourished or obese?
• Is patient having contractions? If so, when did they begin, and what are their
frequency and duration?
• Antenatal complications e.g. pre-eclampsia, premature labour, isoimmunisation;
• Induction of labour and indication; Assisted vaginal delivery;
• Caesarean section- indications, type of section and complication if any;
• Third stage complications: post-partum hemorrhage and/or manual removal
of placenta;
• Neonatal outcome, e.g. intrauterine growth restriction, macrosomia, congenital
anomaly, perinatal death or morbidity. On the other hand, one or more totally
normal pregnancies is the best prognostic factors for a successful outcome insubsequent pregnancies.
The final question in the history taking should be some variant of “Is there anything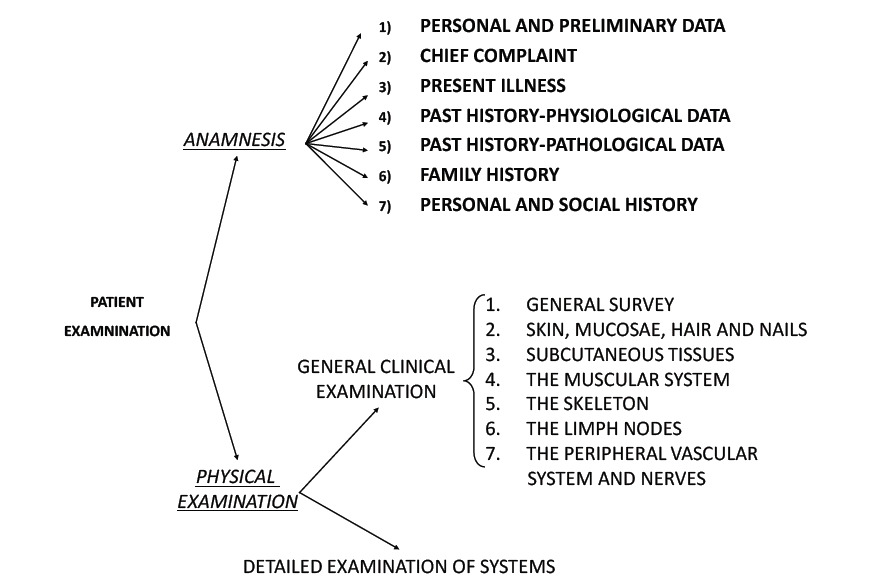
else I should have asked you today?” or, alternatively, “Is there anything else I
should know or that you want to share with me?”
Table 2.4: Factors that may require additional
antenatal support or referral to an obstetrician/physician or other health professional
Self-assessment 2.4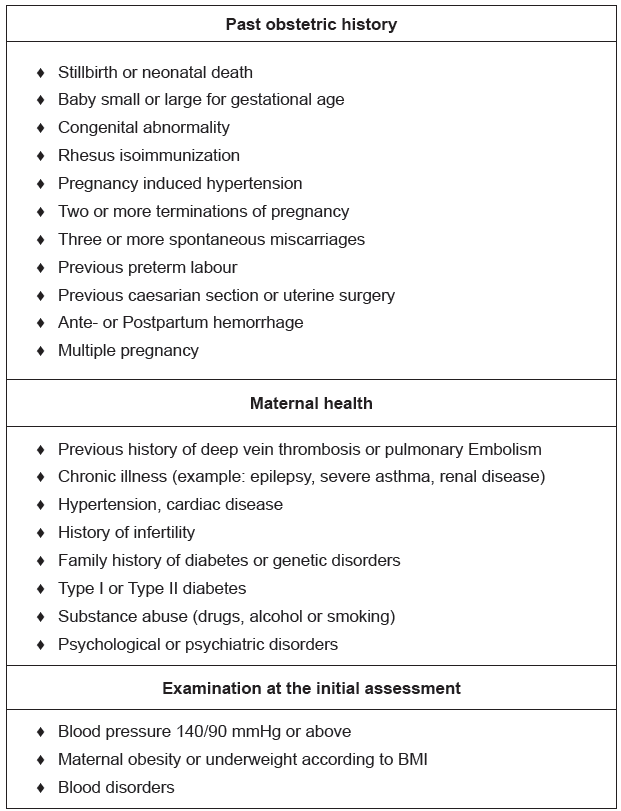
1. What are the important points to note before taking history?2.5 Physical examination
2.5 Physical examination
Learning Activity 2.5
Watch the Video on physical examination of a pregnant woman and discuss
what you have seen in your groups.https://www.youtube.com/watch?v=kSRR1HT1ENA
This is a systematic assessment of the pregnant woman from head to toe. Prior to
conducting the physical examination of a pregnant, her consent and comfort are
primary considerations. Observation of physical characteristics is important.
A thorough examination is made at the first visit. This is divided into a general
examination and an obstetric examination.
The general examination should include:
a. General appearance: Namely, the nutritional status, whether weak or sick
looking. Note the gait and if she walks with a limp.
b. Height: You may note that any woman below 150 cm in height is likely to have
cephalo-pelvic disproportion (CPD).
c. Weight: That is, a pregnant woman on average gains 2kg every month. The
total weight gain by the end of pregnancy is about 10-20 kg. Excessive weight gain
indicates accumulation of fluid in the tissues (Oedema). Lack of increase in weight
or loss may mean malnutrition. Obesity may lead to an increased risk of gestational
diabetes.
d. Blood pressure: Blood pressure is taken in order to ascertain normality and
provide a baseline reading for comparison throughout pregnancy. Systolic blood
pressure does not alter significantly in pregnancy, but diastolic falls in mid pregnancy
and rises to near non-pregnant levels at term. The systolic recording may be falsely
elevated if a woman is nervous or anxious, if a small cough is used on a large arm,
the arm is unsupported or if the bladder is full. The woman should be comfortably
seated or resting in lateral position on the couch for the measurement. Brachial
artery pressure is highest when the subject is sitting and lower when in recumbent
position.e. Other vital signs (temperature, pulse and respiration).
HEAD TO TOE ASSESSMENT
1.HEAD (HEENT):
- Hair: check for malnutrition, hygiene, any injury
- Face: the face will indicate:
♦ The general health of the woman nourished and content, or malnourished,
♦ Pallor of the conjunctiva indicates anemia,
♦ Jaundice is early recognized by the yellow conjunctiva.
♦ Edema of the face is a serious sign of pre-eclampsia. Also check for symmetry.
- Mouth:
♦ Stomatitis indicates vitamin B deficiency,
♦ Check tongue pallor.
♦ The gums are sensitive during pregnancy because of hormonal changes,
♦ Dental caries are a potential source of infection
- Ears: check for any symmetry, discharge or other abnormality
- Nose: symmetry, discharges, tumors
2. NECK:
– Swollen glands, stiffness, and thyroid enlargement.
– Veins turgescence
3. CHEST:
– Symmetry of the breasts
– Breathing movement (inspection and auscultation) or abnormalities
– Breast examination: the breasts may be examined to note pregnancy changes,
a useful aid in diagnosis of pregnancy and to note any features such as the
presence of lumps or abnormal discharges from the nipples. The breasts are
likely to feel tender in the first trimester; palpate gently with the flat of the hand
to feel for any lumps. Check if the nipple is protractile. Educate the woman on
how to examine the breasts by herself
– The heart and the lungs will be checked and any deviations noted (auscultation
for rate and rhythm).
– The back is examined for spinal deformities, back tenderness and costal
vertebral angle tenderness (CVAT) for kidney infection
4.UPPER LIMBS:
check for symmetry, pallor of the palm of hands and nails, edema
5. ABDOMEN:
– The abdomen is examined to ascertain whether the uterus is palpable and, if
so, if its size is compatible with the estimated period of gestation
– Assess the shape, the size, previous scar, fetal movements, strae gravidarum,
linea negra.
6. LOWER LIMBS:
The lower limbs are examined for:
♦ Feet and knee reflexes. If BP is high, protein in urine or woman has headache,
visual changes or epigastric pain (patellar reflex)
♦ Checking for symmetry
♦ Physiological oedema occurs after rising in the morning and worsens during
the day; it is often associated with daily activities or hot weather. At visits later
in pregnancy the midwife should observe for oedema and ask the woman
about symptoms. Often the woman may notice that her rings feel tighter and
her ankles are swollen. Pitting oedema in the lower limbs can be identified
by applying gentle fingertip pressure over the tibial bone: a depression will
remain when the finger is removed. If oedema reaches the knees, affects
the face or is increasing in the fingers it may be indicative of hypertension of
pregnancy if other markers are also present.
♦ Homan’s signs are checked in order to diagnose any thrombophlebitis (more
specific in post-partum period)
♦ Checking varicose veins. These are more likely to occur during pregnancy
and are a predisposing cause of deep vein thrombosis. The woman should
be asked if she has any pain in her legs. Reddened areas on the calf may be
due to varicosities, phlebitis or deep vein thrombosis. Areas that appear white
as if deprived of blood could be caused by deep vein thrombosis. The woman
should be asked to report any tenderness that she feels either during the
examination or at any time during the pregnancy. Referral should be made
to medical colleagues as appropriate. Support stockings will help alleviatesymptoms although not prevent varicose veins occurring.
Self-assessment 2.5
Using mannequin in simulation lab, demonstrate steps of physical examinationof pregnant woman.
2.6 Leopold’s manoeuver
The Leopold maneuvers are used to palpate the gravid uterus systematically. This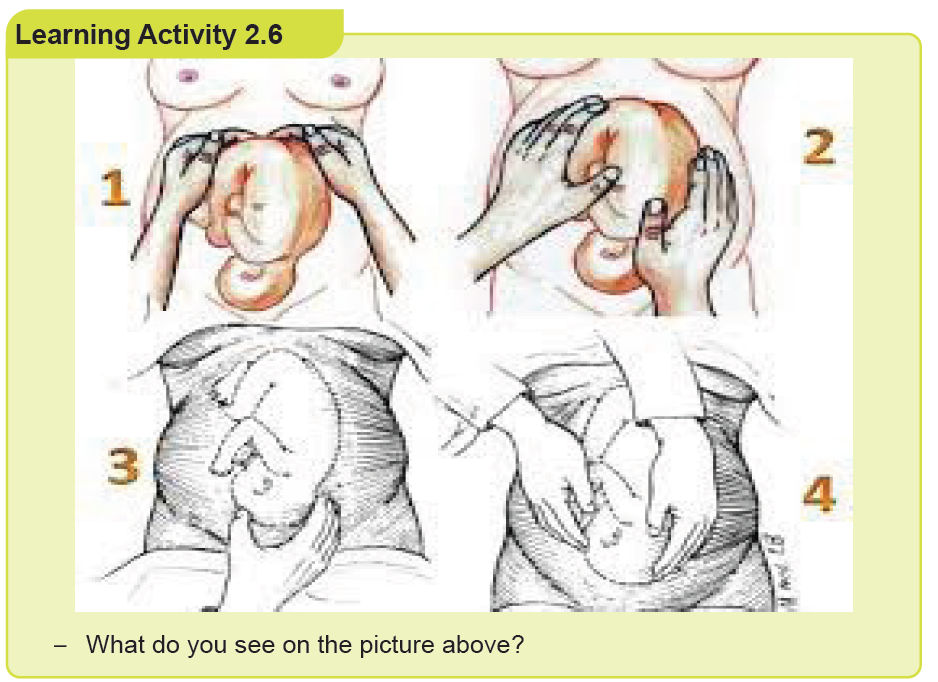
method of abdominal palpation is of low cost, easy to perform, and non-invasive.
It is used to determine the position, presentation, and engagement of the fetus in
utero.
Abdominal examination
Abdominal examination is carried out from 24 weeks’ gestation to establish and
affirm that fetal growth is consistent with gestational age during the pregnancy. The
specific aims are to:
• Observe the signs of pregnancy
• Assess fetal size and growth
• Auscultate the fetal heart when indicated
• Locate fetal parts
• Detect any deviation from normal.
Preparation
The woman should be asked to empty her bladder before making herself
comfortable on the couch. A full bladder will make the examination uncomfortable;
this can also make the measurement of fundal height less accurate. The midwife
washes her hands and exposes only that area of the abdomen she needs to
palpate, and covers the remainder of the woman to promote privacy and protect
her dignity. The woman should be lying comfortably with her arms by her sides to
relax the abdominal muscles. The midwife should discuss her findings throughout
the abdominal examination with the woman.
Inspection
The uterus is first assessed by observation. A full bladder, distended colon or obesity
may give a false impression of fetal size. The shape of the uterus is longer than it
is broad when the lie of the fetus is longitudinal, as occurs in the majority of cases.
If the lie of the fetus is transverse, the uterus is low and broad.
The multiparous uterus may lack the snug ovoid shape of the primigravid uterus.
Often it is possible to see the shape of the fetal back or limbs. If the fetus is in
an occipitoposterior position a saucer-like depression may be seen at or below
the umbilicus. The midwife may observe fetal movements, or the mother may feel
them; this can help the midwife determine the position of the fetus. The woman’s
umbilicus becomes less dimpled as pregnancy advances and may protrude slightly
in later weeks.
Lax abdominal muscles in the parous woman may cause the uterus to sag forwards;
this is known as pendulous abdomen or anterior obliquity of the uterus. In the
primigravida it is a significant sign as it may be due to pelvic contraction.
Skin changes
Stretch marks from previous pregnancies appear silvery and recent ones appear
pink. A linea nigra may be seen; this is a normal dark line of pigmentation running
longitudinally in the centre of the abdomen below and sometimes above the
umbilicus. Scars may indicate previous obstetric or abdominal surgery or self-harm.
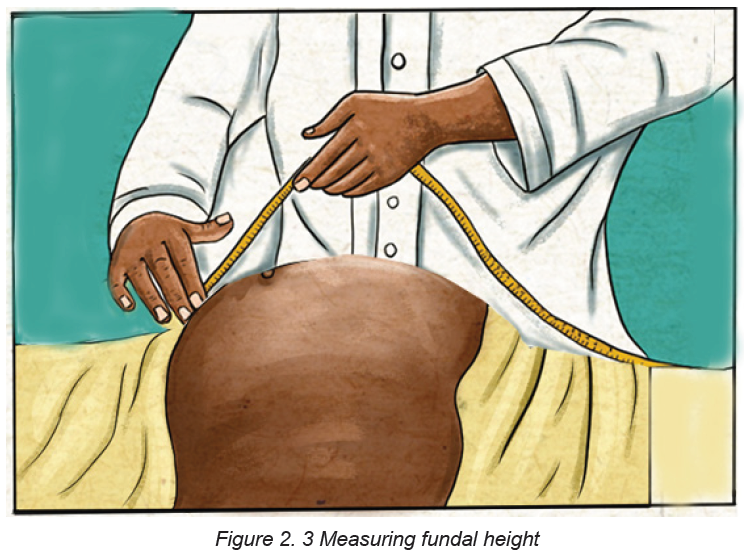
Measuring fundal height
In order to determine the height of the fundus the midwife places her hand just at
the upper border of the symphysis pubis. Pressing gently, she moves her hand
to the abdomen up to the level below the sternum where she feels the fundus.
Clinically assessing the uterine size to compare it with gestation does not always
produce an accurate result, although there are landmarks that can be used as an
approximate guide. From 25 weeks of pregnancy, the midwife should commence
serial symphysis fundal height (SFH) measurements. She uses a tape measure
(with the centimetres facing the mother’s abdomen) held at the symphysis pubis
and extended up to the fundus, to take a single measurement. This should be
recorded in the pregnancy record and plotted on a customized chart rather than apopulation-based chart.
Leopold’s manoeuvers: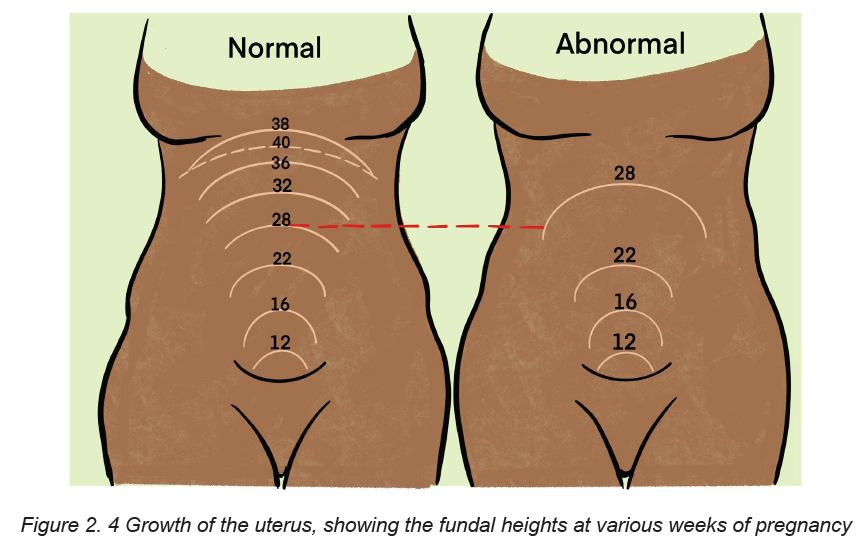
Fundal palpation
This determines the presence of the breech or the head in the fundus. This
information will help to diagnose the lie and presentation of the fetus. Talking through
the palpation with the woman, making eye contact with her during the procedure,
the midwife lays both hands on the sides of the fundus, fingers held close together
and curving round the upper border of the uterus. Gentle yet deliberate pressure is
applied using the palmar surfaces of the fingers to determine the soft consistency
and indefinite outline that denotes the breech. Palms of hands on either side of thefundus, fingers held close together palpate the upper pole of the uterus.
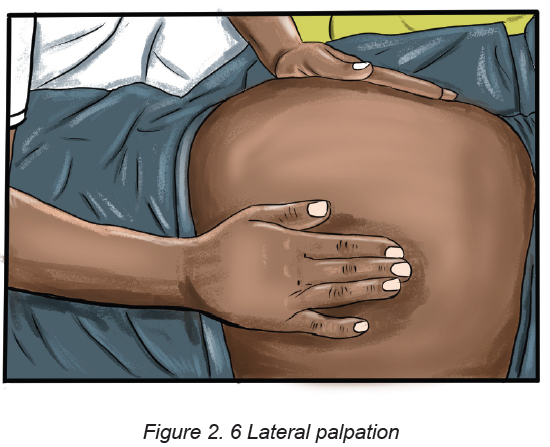
Lateral palpation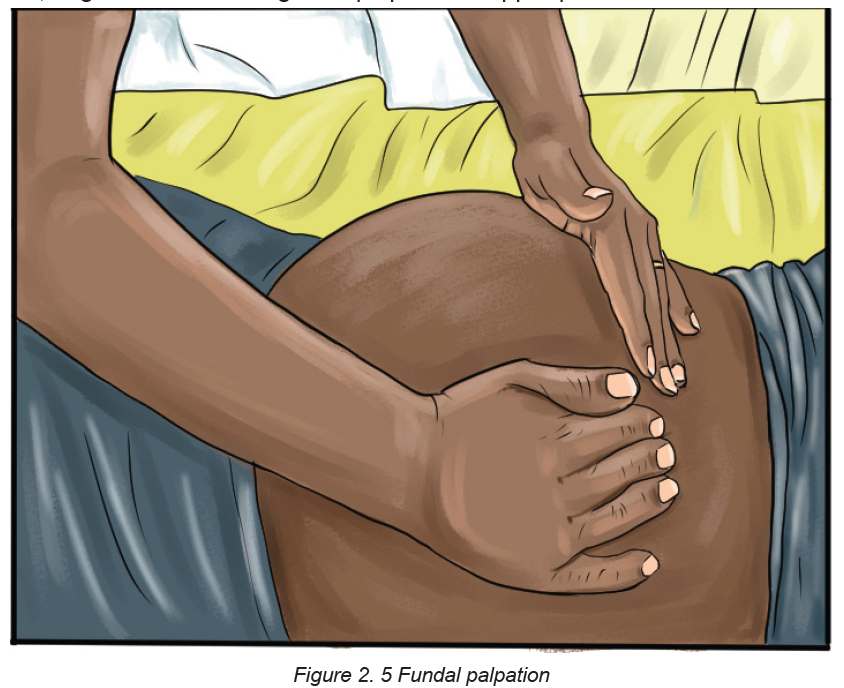
This is used to locate the fetal back in order to determine position. The hands are
placed on either side of the uterus at the level of the umbilicus. Gentle pressure
is applied with alternate hands in order to detect which side of the uterus offers
the greater resistance. More detailed information is obtained by feeling along the
length of each side with the fingers. This can be done by sliding the hands down
the abdomen while feeling the sides of the uterus alternately. Some midwives prefer
to steady the uterus with one hand, and using a rotary movement of the opposite
hand, to map out the back as a continuous smooth resistant mass from the breech
down to the neck; on the other side the same movement reveals the limbs as small
parts that slip about under the examining fingers.
‘Walking’ the fingertips of both hands over the abdomen from one side to the other
is another method of locating the fetal back. Hands placed at umbilical level oneither side of the uterus. Pressure is applied alternately with each hand.
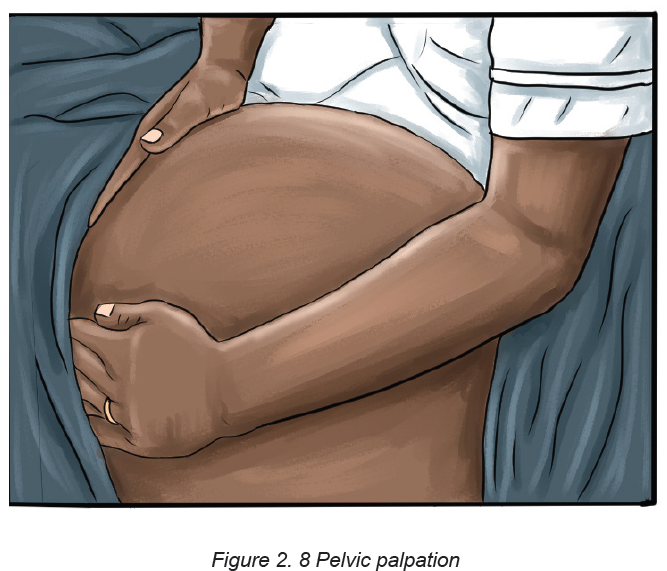
Pelvic palpation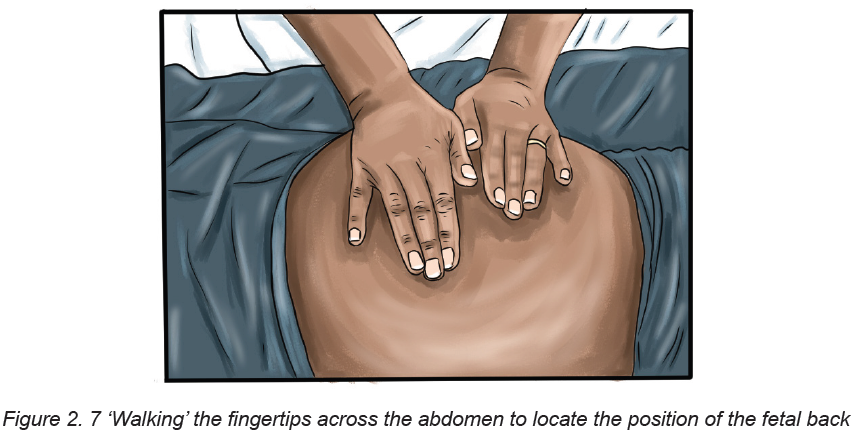
Pelvic palpation will identify the pole of the fetus in the pelvis; it should not cause
discomfort to the woman. This is done only from 36 weeks onwards.
The midwife should ask the woman to bend her knees slightly in order to relax the
abdominal muscles and also suggest that she breathe steadily; relaxation may be
helped if she sighs out slowly. The sides of the uterus just below umbilical level
are grasped snugly between the palms of the hands with the fingers held close
together, and pointing downwards and inwards.
If the head is presenting (towards the lower part of the uterus), a hard mass with a
distinctive round smooth surface will be felt. The midwife should also estimate how
much of the fetal head is palpable above the pelvic brim to determine engagement.
This two-handed technique appears to be the most comfortable for the woman and
gives the most information.
Pawlik’s manoeuvre, where the practitioner grasps the lower pole of the uterus
between her fingers and thumb, which should be spread wide enough apart to
accommodate the fetal head, is sometimes used to judge the size, flexion and
mobility of the head, but undue pressure must not be applied. It should be used only
if absolutely necessary as it can be very uncomfortable for the woman: There is noresearch evidence to support one method over the other.
On the figure above, the fingers are directed inwards and downwards.
On the figure above, the lower pole of the uterus is grasped with the right hand, the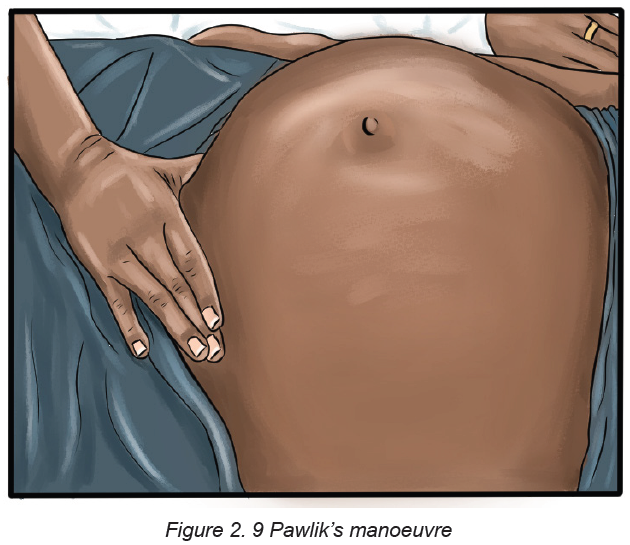
midwife facing the woman’s head.
Engagement
Engagement is said to have occurred when the widest presenting transverse
diameter of the fetal head has passed through the brim of the pelvis. In cephalic
presentations this is the biparietal diameter and in breech presentations the
bitrochanteric diameter. In a primigravid woman, the head normally engages at any
time from about 36 weeks of pregnancy, but in a multipara this may not occur until
after the onset of labour. Engagement of the fetal head is usually measured in fifths
palpable above the pelvic brim.
When the vertex presents and the head is engaged the following will be evident on
clinical examination:
• Only two- to three-fifths of the fetal head is palpable above the pelvic brim
• The head will not be mobile.
On rare occasions, the head is not palpable abdominally because it has descended
deeply into the pelvis. If the head is not engaged, the findings are as follows:
• More than half of the head is palpable above the brim
• The head may be high and freely movable (ballotable) or partly settled in the
pelvic brim and consequently immobile.
In a primigravid woman, it is usual for the head to engage by 37 weeks’ gestation;
however, this is not always the case. When labour starts, the force of labour
contractions encourages flexion and moulding of the fetal head and the relaxed
ligaments of the pelvis allow the joints to give. This is usually sufficient to allow
engagement and descent. Other causes of a non-engaged head at term include:
• Occipitoposterior position
• Full bladder
• Wrongly calculated gestational age
• Polyhydramnios
• Placenta praevia or other space-occupying lesion
• Multiple pregnancy
• Pelvic abnormalities
• Fetal abnormality
Checklist to be used when performing Leopold maneuver
a) Equipment
♦ Tray
♦ Vital signs materials
♦ Weighing and height scale
♦ Table of examination
♦ Pinard fetoscope
♦ Pregnancy wheel
♦ Preventive medication
♦ IEC materials
♦ ANC and Client records
♦ Screening materials (HIV, Syphilis, Albuminuria, Urinalysis, Full blood counts
(FBC)
♦ Gloves (examination gloves and sterile gloves)
♦ Trash can
♦ Dust bin
b) Implementation
♦ Wash and dry hands
♦ Put on examination gloves.
♦ Systematic assessment from head to toe for pregnant woman (inspection,
palpation, auscultation and percussion)
♦ Explain to the woman/client/ couple/ family each step of procedure and
provide feedback
♦ Ask the woman to lie on her back, feet posed on the bed and knees bending
(LEOPOLD MANEUVER)
♦ Assess fundal /uterine height: Use two hands to palpate the top of the uterus,
and then the measurement is taken from the upper border of the symphysis
pubis to the highest point of the fundus of the uterus by using a tape measure.
♦ First Maneuver: Feel the consistency and the mobility of the fetal part lying
in the fundus of the uterus. The fetal head is firm, hard and round, it moves
independently from the fetal body. The breech/buttock is softer and moves at
the same time as the whole fetal body. If fundus is empty suspect transverse
lie (presentation transverse)
♦ Second Maneuver: Determine the lie (presentation): the position of the fetal
back and other small parts of the fetal body). By moving the hands to half
way down the uterus, palpate the abdomen, apply gentle pressure. One hand
palpates, the other hand supports the abdomen. The fetal back, which is
on the side of the abdomen, is a continuous smooth resistant mass during
palpation. The other side of the abdomen, where limbs are felt as small parts,
is embossed or irregular.
♦ Third Maneuver: Place one hand just above the symphysis. Determine which
part of the fetus occupies the lower uterine pole: if the palpated part is the
head or the buttock of the fetus or other, and check/verify if the presentation
is engaged
♦ Change position by turning your back towards the client.
♦ Fourth Maneuver: Two hands are placed to the lower uterine pole and slide
them on the sides of the uterus towards the pubis. Identify a cephalic, a
breech or another presentation. Determine the degree of the engagement of
the presentation
♦ Auscultation of the FHR (see checklist FHR)
♦ This is a separate procedure but it should be done after this procedure
c) COMPLETION
♦ Thank the client for her collaboration and request the client if she has any
concern
♦ Assist the client to maintain a comfortable position.
♦ Clean and dispose used materials and clean the work area.
♦ Wash hand
♦ Provide preventive medications if indicated♦ Document the results of the examination and give appointment.
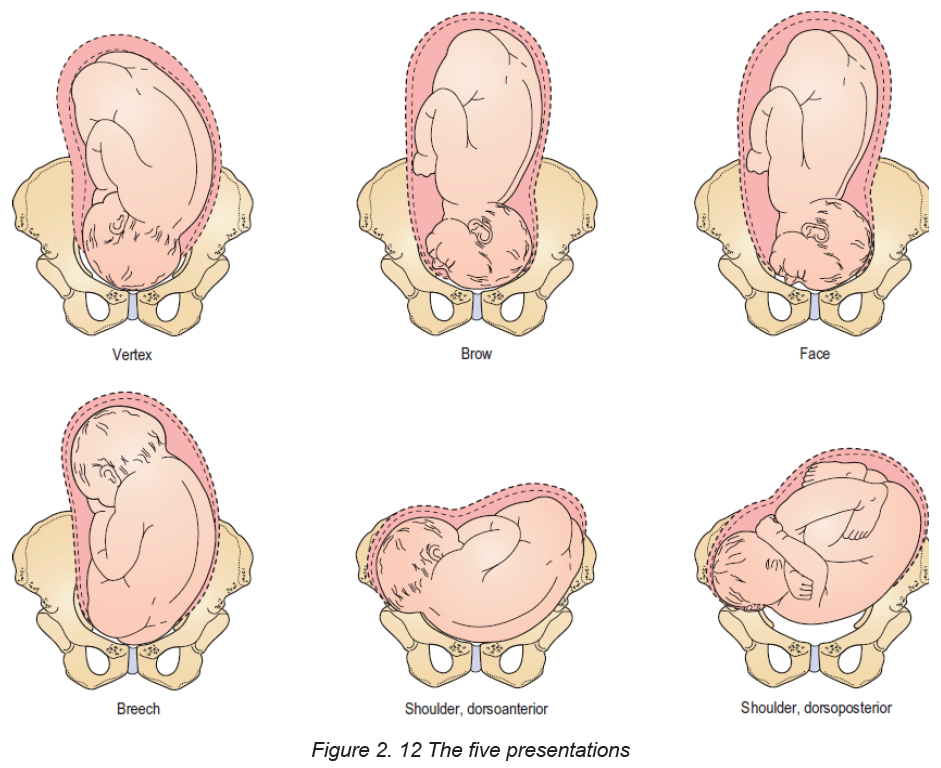
Presentation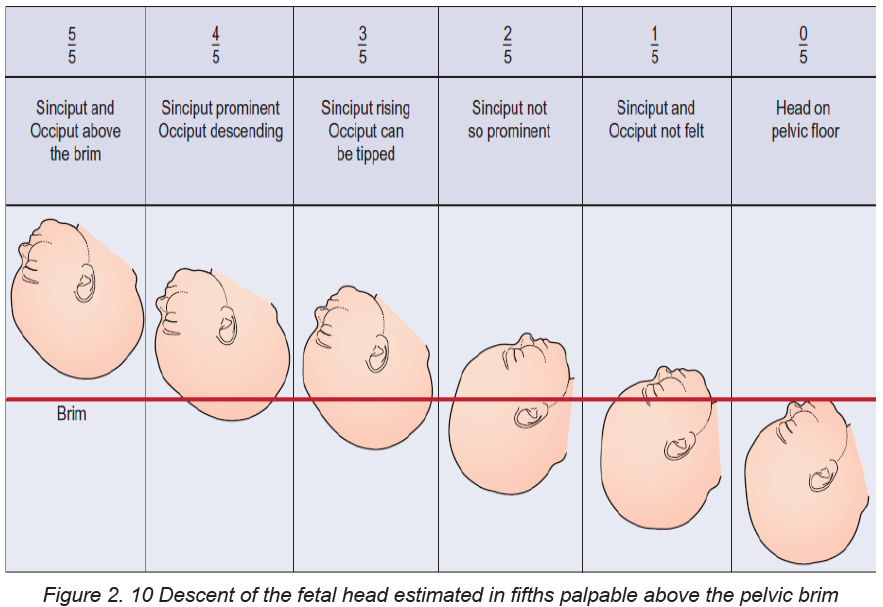
Presentation refers to the part of the fetus that lies at the pelvic brim or in the lower
pole of the uterus. Presentations can be vertex, breech, shoulder, face or brow.
Vertex, face and brow are all head or cephalic presentations. When the head is
flexed the vertex presents; when it is fully extended the face presents; and when it
is partially extended the brow presents.
Auscultation
A Pinard’s fetal stethoscope will enable the midwife to hear the fetal heart directly
and determine that it is fetal and not maternal. The stethoscope is placed on the
mother’s abdomen, at right-angles to it over the fetal back. The ear must be in close,
firm contact with the stethoscope but the hand should not touch it while listening
because then extraneous sounds are produced. The stethoscope should be moved
about until the point of maximum intensity is located where the fetal heart is heard
most clearly. The midwife should count the beats per minute, which should be in the
range of 110–160. The midwife should take the woman’s pulse at the same time aslistening to the fetal heart to enable her to distinguish between the two.
Lie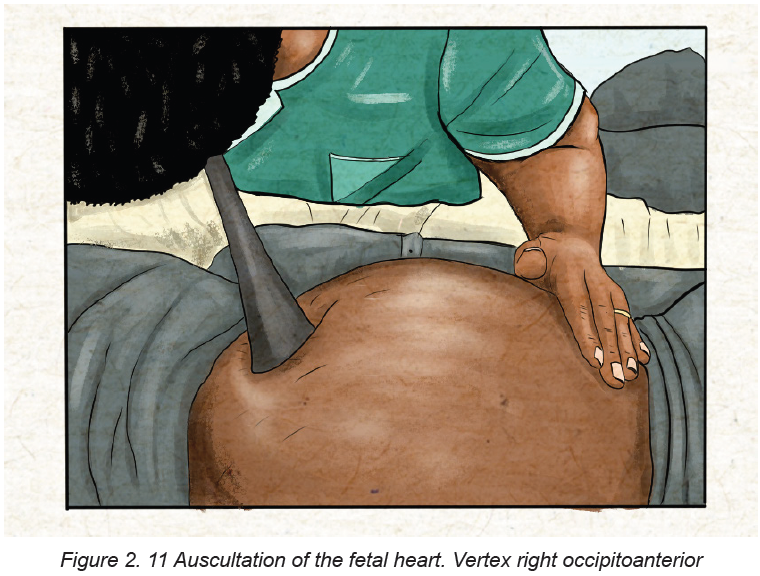
The lie of the fetus is the relationship between the long axis of the fetus and the long
axis of the uterus. In the majority of cases the lie is longitudinal due to the ovoid
shape of the uterus; the remainder are oblique or transverse.
Attitude
Attitude is the relationship of the fetal head and limbs to its trunk. The attitude
should be one of flexion. The fetus is curled up with chin on chest, arms and legs
flexed, forming a snug, compact mass, which utilizes the space in the uterine cavity
most effectively. If the fetal head is flexed the smallest diameters will present and,
with efficient uterine action, labour will be most effective.
Denominator
‘Denominate’ means ‘to give a name to’; the denominator is the name of the part of
the presentation, which is used when referring to fetal position. Each presentation
has a different denominator and these are as follows:
• In the vertex presentation it is the occiput
• In the breech presentation it is the sacrum
• In the face presentation it is the mentum.
Position
The position is the relationship between the denominator of the presentation andsix points on the pelvic brim.
Indicators of maternal wellbeing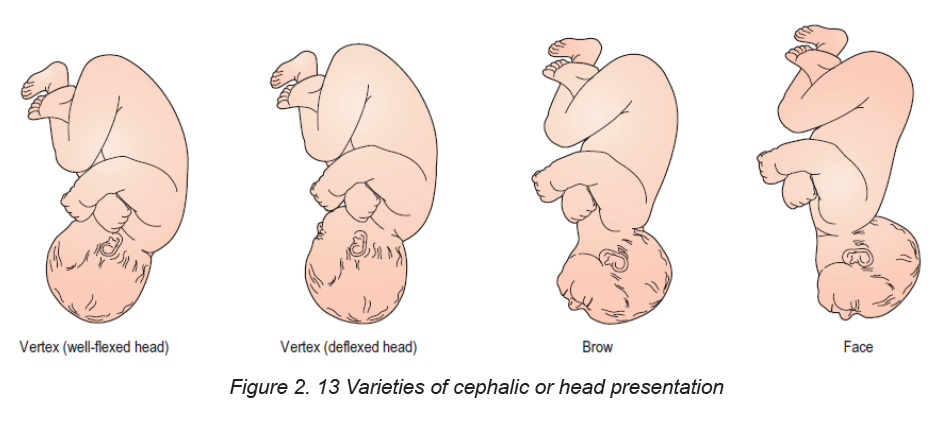
The woman’s general health and wellbeing is observed throughout and the midwife
must remain vigilant for signs of domestic abuse, emotional fragility and social
instability. Endeavouring to maintain continuity of carer will be a key process for
identifying impending problems and for encouraging free exchange of information
between the woman and her midwife.
Indicators of fetal wellbeing
These include:
• Increasing uterine size compatible with the gestational age of the fetus;
• Fetal movements that follow a regular pattern from the time when they are
first felt;
• Fetal heart rate that is regular and variable with a rate between 110 and 160
beats/minute.
Self-assessment 2.6
– Using checklist in the simulation lab, perform Leopold’s manoeuvers on
mannequin
– Practice in simulation lab, on listening to the fetal heart beat using the
pinard’s stethoscope
2.7 Calculation of gestational age based on the last menstruation
period and pregnancy wheel
Learning Activity 2.7
Madam X, aged 28 years, attend the health center for her ANC first contact; she
wanted to know how her baby is and when she will deliver.
– How will you determine the time the woman will deliver her baby?
An accurate menstrual history helps determine the expected date of birth (EDB),
enables the nurse to predict a birth date and subsequently calculate the gestational
age at any point in the pregnancy. This is particularly important for the timing of fetal
anomaly screening and measuring fetal growth. The EDB is calculated by adding
9 calendar months and seven days to the date of the first day of the woman’s last
menstrual period (known as Naegele’s Rule). This method assumes that:
a. The woman takes regular notes of regularity and length of times between
periods
b. Conception occurred 14 days after the first day of the last period, this is true
only if the woman has 28-day cycle
c. The last period of bleeding was true menstruation; implantation of the ovum
may cause slight bleeding
d. Breakthrough bleeding and anovulation can be affected by the contraceptive
pill thus impacting on the accuracy of a Last Menstrual Period (LMP)
The duration of pregnancy based on Naegele’s Rule is 280 days. However, if the
woman has 35-day cycle, then, 7 days should be added; if her cycle is less than 28
days, then the appropriate number of days is subtracted. A definitive EDB will be
given when the woman attends for her dating ultrasound scan at around 12 weeks
of pregnancy.
The EDD is calculated by adding 9 calendar months if the last month of
menstruation is≤ to 3 or moins 3 if month ≥ to 4 and adding 7 days to the date of
the 1st day of the woman’s last menstrual period (LMP) this method assumes that:
• The woman takes regular note of regularity and length of time between periods
• Conception occurred 14 days after the 1st day of the last period; this is true
only if the woman has a regular 28 days cycle.
• The last period of bleeding was true menstruation but implantation of the
ovum may cause slight bleeding.
Example on calculation of EDD
Calculating from “sure” dates by Naegele”s Rule
Cycle of 28days=LMP: 9 June 2014
EDD = 9+7days/6- 3/EDD: 16 March 2015
A pregnancy wheel is used to determine the due date of delivery. Also known as a
gestation calculator, it uses the first day of your last menstrual period to establish
your due date
It combines three things needed to derive all the dates necessary in pregnancy
care, and no other app has this combination. It contains a calendar calculator todetermine EDD (EDC) from LMP or from a sonogram report.
Self-assessment 2.7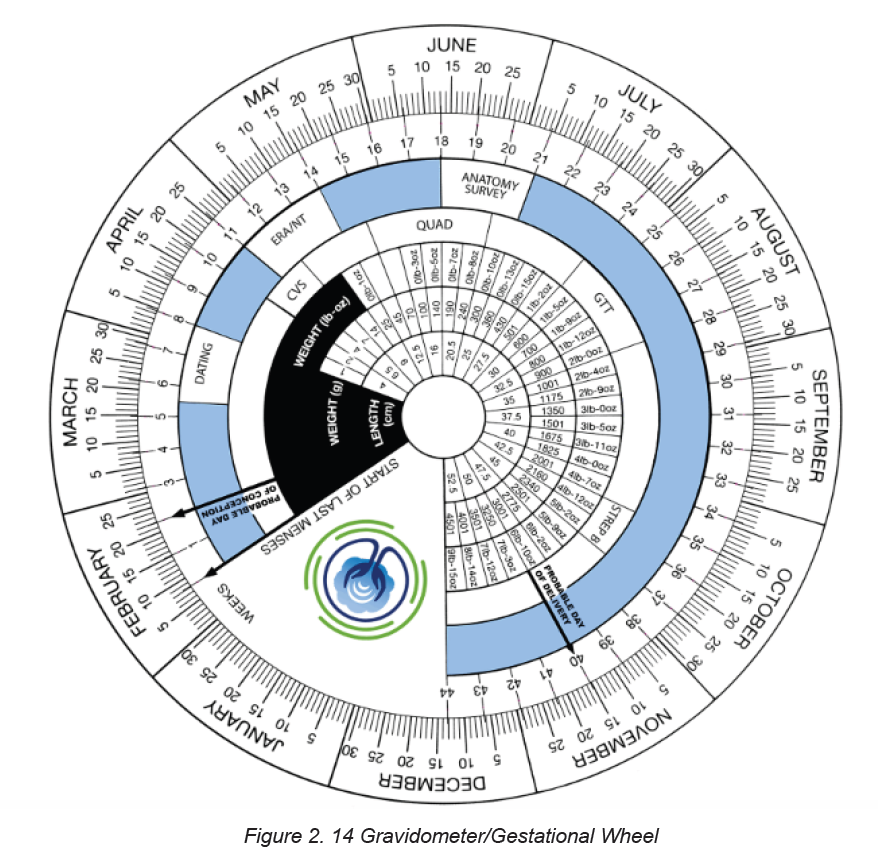
Calculate the EDD of a pregnant woman whose last menstrual period (LMP) was
on 14th December 2020.
2.8 Physiological changes during pregnancy: Changes in the
female reproductive system during pregnancy
Learning Activity 2.8
– What happens with menstruation to a pregnant woman?
Changes in the body during pregnancy are most obvious in the organs of the
reproductive system.
Uterus
When a woman becomes pregnant, the part of her body affected first and the part
that undergoes the most significant changes is the uterus. It increases to 20 times
its original weight, and 1,000 times its initial capacity. The amount of its muscle,
connective and elastic tissue, blood vessels, and nerves increases.
The cervix and vagina
Other parts of the reproductive system change along with the uterus. The cervix
and vagina have an increased blood supply, which causes a darkening in color
apparent by the sixth week.
Ovaries
The ovaries cease to ovulate. The follicle-stimulating hormone (FSH) ceases its
activity due to the increased levels of estrogen and progesterone secreted by the
ovaries and corpus luteum. The FSH prevents ovulation and menstruation.
Breasts
Breasts must undergo many changes during pregnancy to produce milk. In the first
two months of pregnancy, breasts may feel sore or full. They enlarge, and veins
may become visible. The nipples also increase in size and usually darken. By midpregnancy,
colostrum (a thick, yellowish fluid) can be expressed, but milk is not
produced until after delivery.
Self-assessment 2.8
What are the physiological changes on the breast during pregnancy?
2.9 Physiological changes in pregnancy on endocrine system
Learning Activity 2.9
– Describe 3 hormones involved in reproductive system based on your
knowledge from S3 biology?
The female endocrine system consists of the pituitary, the thyroid, the adrenal and
the thymus glands, along with the pancreas and the ovaries. All of them undergo
changes during pregnancy in order to prepare the mother’s body to effectively meet
the challenges associated with pregnancy, childbirth and breastfeeding. Some of
the most significant changes occur in the pituitary and thyroid glands to meet the
nutritional needs of the baby in the uterus, restricting reproductive organs andpassing on genetic information.
Main female reproductive hormones and their
functions in preparing the uterus for pregnancy.
Estrogens and progesterone are the chief hormones throughout pregnancy.
Oestrogens
A woman will produce more estrogens during one pregnancy than throughout her
entire life when not pregnant. During pregnancy, estrogen promotes maternal blood
flow within the uterus and the placenta.
Progesterone
A pregnant woman’s progesterone levels are also very high. Among other effects,
high levels of progesterone cause some internal structures to increase in size,
including the uterus, enabling it to accommodate a full-term baby. Levels of
progesterone and estrogens rise continually throughout pregnancy, suppressing
the hypothalamic axis and subsequently the menstrual cycle. Estrogen is mainly
produced by the placenta and is associated with fetal well–being.
HCG
Women also experience increased human chorionic gonadotropin (β-hCG); which
is produced by the placenta. This maintains progesterone production by the corpus
luteum. The increased progesterone production, first by corpus luteum and later by
the placenta, mainly functions to relax smooth muscle.
Prolactin
Prolactin levels increase due to maternal pituitary gland enlargement by 50%.
This mediates a change in the structure of the mammary gland from ductal to
lobular-alveolar.
Parathyroid hormone
Parathyroid hormone is increased which leads to increases of calcium uptake in
the gut and re-absorption by the kidney. Adrenal hormones such as cortisol and
aldosterone also increase.
HPL
Human placental lactogen (HPL) is produced by the placenta and stimulates
lipolysis and fatty acid metabolism by the woman, conserving blood glucose for
use by the fetus. It can also decrease maternal tissue sensitivity to insulin, resulting
in gestational diabetes.There are some experiences in life of a woman that cause
similar conditions like those in pregnancy, therefore correct diagnosis is very
important.
Self-assessment 2.9
– Describe two hormones that help to maintain pregnancy.
2.10 Changes in the cardiovascular and respiratory systems
Learning Activity 2.10– What is the role the heart in human being?
Changes in the cardiovascular system
During pregnancy profound but predominantly reversible changes occur in
maternal haemodynamics and cardiac function. These complex adaptations
are necessary to:
• Meet evolving maternal changes in physiological function
• Promote the growth and development of the uteroplacental–fetal unit
• Compensate for blood loss at the end of labour.
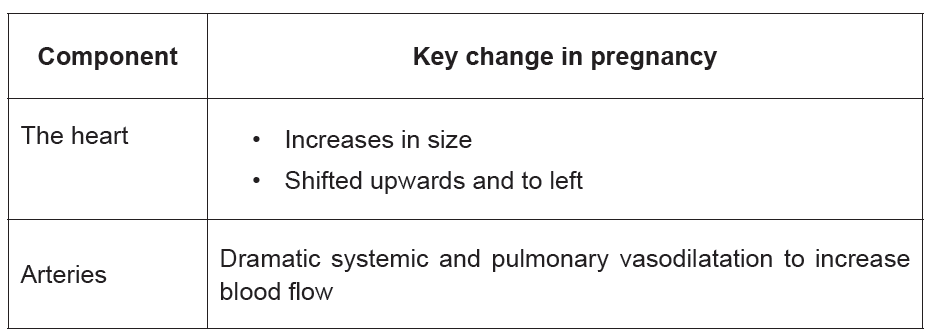
Table 2. 4 A summary of the key components of
the cardiovascular system and adaptations inpregnancy
Changes in the respiratory system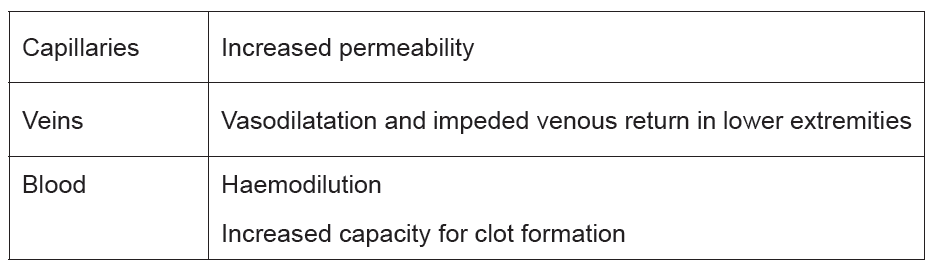
To accommodate increased oxygen requirements and the physical impact of the
enlarging uterus intricate changes occur in respiratory physiology.
•Breathlessness
The respiratory changes can be extremely uncomfortable and may lead to dyspnoea,
dizziness and altered exercise tolerance. Up to 75% of pregnant women with no
underlying pre-existing respiratory disease experience some dyspnoea, possibly
due to an increased awareness of the physiological hyperventilation.
Self-assessment 2.10
How does pregnancy affect the heart?
2.11 Changes in the urinary and Gastro-intestinal system
Learning Activity 2.11
A pregnant woman of 32 weeks visited your antenatal care facility complaining
of not sleeping at night and urinate all the time. She is worried and want you to
help her with this problem.
1. What advice can you give to her?
2. Describe the reason why you think she is having this problem.
The striking anatomical and physiological changes occurring in the urinary system
are critical for an optimal pregnancy outcome. Systemic vasodilatation in the first
trimester and an increase in blood volume and cardiac output results in a massivevasodilatation of the renal circulation that increases the renal plasma flow.
Gastrointestinal system changes:
Anatomical and physiological changes take place in each organ of the gastrointestinal
system. Influenced by oestrogen and progesterone.
Anatomical and physiological changes take place in each organ of the gastrointestinal
system. Influenced by oestrogen and progesterone.
♦ Ptyalism
Ptyalism is the excessive production of saliva throughout pregnancy. Ptyalism
causes a bad taste in the mouth and women complain that swallowing the excessive
or thickened saliva perpetuates a sense of nausea and that they need to spit it out.
♦ Nausea and vomiting
Nausea and vomiting (morning sickness) has varying levels of severity and has farreaching
effects for some women in terms of ability to carry out day-to-day tasks,
care for children and take part in full-time employment.
Symptoms usually begin in the 4th week of pregnancy with a marked increase
between 5 and 10 weeks when hCG levels are at their highest, followed by a steady
decline until 20 weeks.
♦ Pica
Pica is the persistent craving and compulsive consumption of substances such as
ice, clay, soap, coal or starch.
♦ Heartburn
Troublesome symptoms of retrosternal and epigastric pain, regurgitation and acid
taste in the mouth can all affect the woman’s quality of life. Increasing gestational
age, heartburn before pregnancy and multiparity may also predispose women to
gastrooesophageal reflux in pregnancy which usually resolves after the birth of the
baby.
Management
• Skip foods and drinks that can make it worse, such as citrus; spicy, fatty
(especially fried or greasy) foods; caffeine; and carbonated drinks.
• Eat several small meals throughout the day.
• Take your time when eating.
• Drink liquids between — not during — meals.
♦ Abdominal distension
Abdominal distension and a bloated feeling occur when nutrients and fluids remain
in the intestinal tract for longer, particularly in the third trimester due to the prolonged
transit time
♦ Constipation and hemorrhoids
Hemorrhoids are varicosities of the anal and perianal venous plexus. They are
caused by the rise in intra-abdominal pressure and restriction of venous return in
the lower extremities and pelvis.
♦ Maternal weight
A variety of components contribute to weight gain during pregnancy.
These includes:
Fetus 27%, the placenta, amniotic fluid and uterus 20%, Breasts 3%, blood volume
and extravascular fluid 23%, and maternal fat stores 27%. Most weight is gained in
the second and third trimesters at rates of 0.45 kg and 0.40 kg per week respectively.Table 2. 5 Distribution of average increase in weight
Self-assessment 2.11
What contributes to weight gain during pregnancy?
Discuss Heart burns and how it can be managed.
2.12 The basic laboratory investigations during antenatal care
Learning Activity 2.12
– Which test can you request to a couple who visited the hospital and
complained that the wife has not seen her monthly period?
This is a process of identifying pregnant women who may be at an increased risk
of a disease or condition, they can then be offered information, further tests and
appropriate treatment to reduce their risk and/or any complications arising from the
pregnancy.
Screening of a mother and baby is now a major part of care for all pregnancies. The
underlying principles of screening are that the condition being screened for must be
important and well understood (i.e. something that makes a difference to health and
wellbeing and does more good than harm).
a) CLINICAL URINE TEST
Results of a clinical urine test can vary depending on the medical facility that you
visit. However, you can usually expect your results within a week of taking the test
b) BLOOD TEST
A laboratory tests of blood to detect human chorionic gonadotropin level (HCG).
There are two types of pregnancy blood tests:
Qualitative HCG blood test: This test checks to see whether any HCG is being
produced in the body. It gives a simple yes or no answer as to whether woman is
pregnant.
Quantitative HCG blood test: This test measures the specific level of HCG in the
blood. Quantitative HCG blood tests are very accurate because they measure the
exact amount of HCG in the blood. They can detect smaller amounts of the hormone
than a qualitative HCG blood test or a urine test.
Blood tests can detect HCG earlier than urine tests.
Progesterone test
♦ Progesterone is given to women with amenorrhea.
♦ If she is pregnant, no bleeding will follow, otherwise, bleeding should occur
within 7-10 days of progesterone administration.
♦ This is reliable in the non-pregnant patient only if there is adequate estrogenstimulation of the endometrium
Self-assessment activity 2.12
– Explain the most accurate test done to confirm pregnancy
2.13 Common laboratory investigations to rule out medical
conditions during antenatal care.
Learning Activity 2.13
– Why is it important to rule out sexual transmitted diseases in pregnant
women?
First antenatal screens usually include Complete blood count, Blood group and
antibody screen, rubella antibody status, syphilis serology, Hepatitis B serology and
HIV abs testing.
The most important test in the second antenatal testing screen is gestational
diabetes screening and protein detection in urine to rule out preeclampsia.
Complete blood count
Anemia is one of the commonest complications of pregnancy. The most common
reason for iron deficiency anemia in pregnancy is the increased demands of the
fetus for iron. Anemia in pregnancy is defined as Hb < 11 g/dL (severe anemia as
Hb < 7 g/dL) at any gestational age.
Anemia is generally defined as hemoglobin level less than 11g/dl or specifically:
♦ HB <11g/dL in 1st trimester
♦ HB <10.5g/dL in 2nd trimester
♦ HB <11g/dL in 3rd trimester
Blood group and antibody screen
Identifying ABO blood group, rhesus D status and red cell antibodies in pregnant
women is important to prevent “haemolytic disease of the new-born” in subsequent
pregnancies. If the foetus is rhesus D-positive (and the mother is negative),
the mother may form anti-D antibodies, which may affect a subsequent rhesusD-positive foetus. Haemolytic disease of the new-born in subsequent pregnancies.
Rubella antibody status
All pregnant women should be screened for rubella antibodies. Congenital Rubella
Syndrome occurs when the rubella virus infects the developing foetus, especially
during the first trimester when up to 90% of affected infants will be born with a birth
defect, e.g. deafness, eye defects, heart defects, mental retardation.
Syphilis serology
All pregnant women should be screened for syphilis, mothers infected with syphilis
can experience long-term morbidity and the complications for pregnancy are
significant. Treponema Elisa Screen assay is used to screen for syphilis as this can
detect primary or secondary infection.
Hepatitis B serology
Transmission of the hepatitis B virus from mother to infant can be prevented by
administration of the hepatitis B vaccine and immunoglobulin to the infant at birth,
therefore screening is important.
HIV screening
All pregnant women should be screened for HIV. Women who are HIV positive can
be given treatment to reduce the risk of HIV being transmitted to their infant (risk
reduced from 32% to less than 1%).
Screening for gestational diabetes
Gestational diabetes affects 5–8% of pregnant, it is recommended that testing for
gestational diabetes occurs for all women between 26 and 28 weeks of gestation.
Screening for Group B streptococcus
Group B streptococcal (GBS) infection is a significant cause of serious neonatal
infection. Women may have a vaginorectal culture collected at 35 to 37 weeks’
gestation to prevent this infection.
Malaria
All women with malaria symptoms will receive early detection and management of
malaria. During antenatal care, the health facility staff must do the following to the
pregnant woman:
• Give her a long-lasting insecticide treated mosquito net;
• Rapid Diagnostic Tests (RDT) in case of signs and symptoms.
Additional testing in pregnancy
Testing for chlamydia and gonorrhoea should be considered for those who may be
at increased risk based on age (e.g. less than 25 years) and sexual history.
Vitamin D
It is required for normal bone growth development in the fetus. Mothers with known
vitamin D deficiency or at risk for deficiency (e.g. dark-skinned women, women whowear a veil) should receive vitamin D supplementation.
Self-assessment 2.13
– Discuss some laboratory investigations you know that can be done in
pregnancy based on your knowledge and understanding from biology in
S3
2.14 Danger signs of pregnancy
Learning Activity 2.14
In a community work “umuganda”, they were discussing about maternal health,
and chief of village identifies you as a scientist and asked to explain to those
pregnant women the bad signs that may show on pregnancy.
Every woman needs to be aware of the danger signs that occur during pregnancy,
as complications can be unpredictable. These danger signs usually indicate the
presence of an obstetric complication that may arise during pregnancy, delivery or
post-delivery. Knowledge of these danger signs will help women and the nurse to
make the right decisions and take appropriate healthcare seeking actions
These danger signs include:
♦ Vaginal bleeding
♦ Sudden gush of fluid or leaking of fluid from vagina
♦ Severe headache not relieved by simple analgesics (e.g. paracetamol)
♦ Dizziness and blurring of vision
♦ Sustained vomiting
♦ Swelling (hands, face, etc.)
♦ Decrease or Loss of fetal movements
♦ Convulsions
♦ Premature onset of contractions (before 37 weeks)
♦ Severe or unusual abdominal pain,
♦ Chills or fever
If a patient should develop any of the above signs during pregnancy the nurse mustquickly refer the patient for expert management.
Self-assessment 2.14
– What will the knowledge of the danger signs of pregnancy help the nurse
to achieve in the care pathway for the woman?
2.15 Management of minor pregnancy complications
Learning Activity 2.15
Based on what you have learnt; what problems do you think a pregnant woman
can have?
Early morning sickness
Around half to two-thirds of all pregnant women will experience morning sickness.
Possible causes include high levels of hormones, blood pressure fluctuations and
changes in carbohydrate metabolism. Severe morning sickness, called hyperemesis
gravidarum, may require hospitalisation. Symptoms of morning sickness may be
relieved by eating a few dry crackers before you get up in the morning, avoiding
foods and smells that make you nauseous, drinking plenty of fluids and choosing
high-carbohydrate and high-protein foods.
Pregnant women should be informed that symptoms of nausea and vomiting
usually resolve in the second half of pregnancy. Ginger, chamomile, and vitamin B6
are recommended for the relief of nausea in early pregnancy, based on woman’s
preferences and available options.
Pregnant women with persistent vomiting or with severe symptoms and signs of
dehydration, reduced urine output, and dark-colored urine should be referred to
hospital level.
Tetanus
Tetanus is an acute disease caused by an exotoxin produced by Clostridium tetani.
Neonatal infection usually occurs through the exposure of the unhealed umbilical
cord stump to tetanus spores, which are universally present in soil, and newborns
need to have received maternal antibodies via the placenta to be protected at birth.
Neonatal disease usually presents within the first two weeks of life and involves
generalized rigidity and painful muscle spasms, which in the absence of medical
treatment leads to death in most cases. Global vaccination programs have reducedthe global burden of neonatal tetanus deaths and continue to do so.
In Rwanda, 34% of women who had a live birth received two or more doses of antitetanus
vaccine during their most recent pregnancy. This figure has not changed
since 2010. Considering mothers who had previous protection against tetanus, the
proportion protected against tetanus rises to 82 percent, an increase from 79 percent
in 2010. This means that 18 percent of pregnant women were not protected against
tetanus. Because tetanus spores are ubiquitous in the environment, eradication is
not biologically feasible and high immunization coverage remains essential.
Table 2. 6 Schedule for Tetanus Toxoidadministration
If Hb < 7 g/dL, especially if symptomatic, then blood transfusion. Transfuse rapidly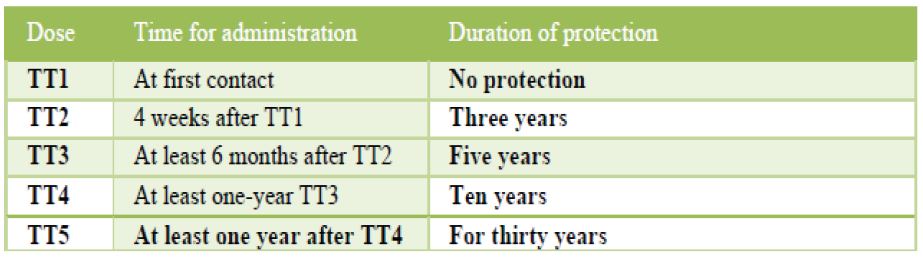
in anaemia due to acute blood loss.
Transfuse slowly if chronic anaemia (Consider use of diuretics like Lasix 20-
40mg stat as necessary to reduce risk of congestive cardiac failure due to sudden
circulatory overload).
♦ IF Hb is <7 and asymptomatic manage according to clinician judgement treat
the cause + Fe supplement
♦ If Hb < 8 g/dL, treat as per FBC results
• If MCV < 80, then send blood for iron studies (ferritin, TIBC and %
saturation (% sat) if available.
• If MCV 80-93, then send blood for peripheral smear and consult
hematologist
• If MCV ≥ 94, then treat for folate or vitamin B12 deficiency
♦ If Hb > 8 g/dL, then treat with folate and FeSO4 325 mg PO BD and recheck
Hb in 2-4 weeks
♦ Treat with Albendazole
♦ Treat for malaria or schistosomiasis if indicated
♦ Mixed anemia may occur and complicate laboratory findings
♦ If iron deficiency, then treat with elemental iron 200 mg PO OD. Titrate up to
reduce side effects and encourage compliance. Take iron on empty stomach
with vitamin C and without antacids.
♦ If folate deficiency, then treat with folate 1 mg PO OD.
♦ If vitamin B12 deficiency, then treat with vitamin B12 1000 mg IM monthly.
♦ If hemolytic anemia, then send blood for direct and indirect Coombs tests.
♦ Treat with corticosteroids. Of note, drug-induced (i.e. methyldopa, penicillin,
cephalosporin) hemolytic anemia is typically milder and is treated by stopping
the offending medication.
Leg cramps
Non-pharmacological treatment options like muscle stretching, dorsiflexion,
relaxation, heat therapy, massage can be used for the relief of leg cramps in
pregnancy, based on a woman’s preferences and available options.
In addition to multivitamin, Magnesium and calcium supplementation can also be
prescribed according to the woman preferences and options.
Low back and pelvic pain
Regular exercise throughout pregnancy is recommended to prevent low back and
pelvic pain. There are a several number of different treatment options, such as
physiotherapy and support belts based on a woman’s preferences and availability.
Refer to hospital level if exercise does not improve symptoms.
Varicose veins and edema
Non-pharmacological options, such as compression stockings and leg elevation
can be used for the management of varicose veins and edema in pregnancy, based
on a woman’s preferences and available options. Refer to hospital level if symptoms
are severe.
Self-assessment 2.15
A 22 years old pregnant woman at 34 weeks of pregnancy tells you that she
craves to eat clay soil. She also tells you that she has developed darker brown
patches on her face, and that her feet and ankles swell up during the day.
1. Identify the minor disorders of pregnancy this woman is displaying, using
their medical names.
2. What advices should you give her to manage her symptoms?
2.16 Anemia in pregnancy
Learning Activity 2.16
Mrs. A. aged 23 is a married pregnant female student who lives in the campus
as she is studying at the University.
She is not able to eat the food from the university restaurant and she is having a
lot of nausea and sometimes vomiting. Her gestational age is 28 weeks. Today
she comes for consultation and complaining of dizziness, tiredness and not able
to stand for long time.
What problem do you think she maybe having?
Anemia results from a lack of red blood cells or dysfunctional red blood cells in the
body. This leads to reduced oxygen flow to the body’s organs.
A serum ferritin concentration <30 μg/L together with an Hb concentration <11 g/dL
during the 1st trimester, <10.5 g/dL during the 2nd trimester, and <11 g/dL during
the 3rd trimester are diagnostic for anemia during pregnancy.
How does iron deficiency anemia during pregnancy affect the baby? Severe anemia
during pregnancy increases your risk of premature birth, having a low birth weight
baby and postpartum depression. Some studies also show an increased risk of
infant death immediately before or after birth.
Types of Anemia during Pregnancy
Iron-deficiency anemia. This type of anemia occurs when the body doesn’t have
enough iron to produce adequate amounts of hemoglobin. That’s a protein in red
blood cells. It carries oxygen from the lungs to the rest of the body.
Types of anemia during pregnancy:
In iron-deficiency anemia, the blood cannot carry enough oxygen to tissues
throughout the body.
♦ Iron deficiency is the most common cause of anemia in pregnancy.
♦ Folate-deficiency anemia. Folate deficiency can directly contribute to certain
types of birth defects, such as neural tube abnormalities (spina bifida) and
low birth weight.
♦ Vitamin B12 deficiency. The body needs vitamin B12 to form healthy red
blood cells.
♦ Blood loss during and after delivery can also cause anemia.
RISK FACTORS
♦ Are pregnant with multiples (more than one child)
♦ Have had two pregnancies close together
♦ Vomit a lot because of morning sickness
♦ Are a pregnant teenager
♦ Don’t eat enough foods that are rich in iron
♦ Had anemia before you became pregnant
Symptoms of Anemia during Pregnancy
♦ Pale skin, lips, and nails
♦ Feeling tired or weak
♦ Dizziness
♦ Shortness of breath
♦ Rapid heartbeat
♦ Trouble concentrating
Preventing Anemia
To prevent anemia in pregnancy, encourage pregnant women to consume food like:
♦ lean red meat, poultry, and fish
♦ leafy, dark green vegetables (such as spinach, broccoli, and kale)
♦ iron-enriched cereals and grains
♦ beans, lentils, and tofu
♦ nuts and seeds
♦ eggs
Foods that are high in vitamin C and iron. These include:
♦ citrus fruits and juices
♦ strawberries
♦ kiwis
♦ tomatoes
♦ bell peppers
♦ leafy green vegetables
♦ citrus fruits and juices
♦ dried beans♦ breads and cereals fortified with folic acid
Self-assessment 2.16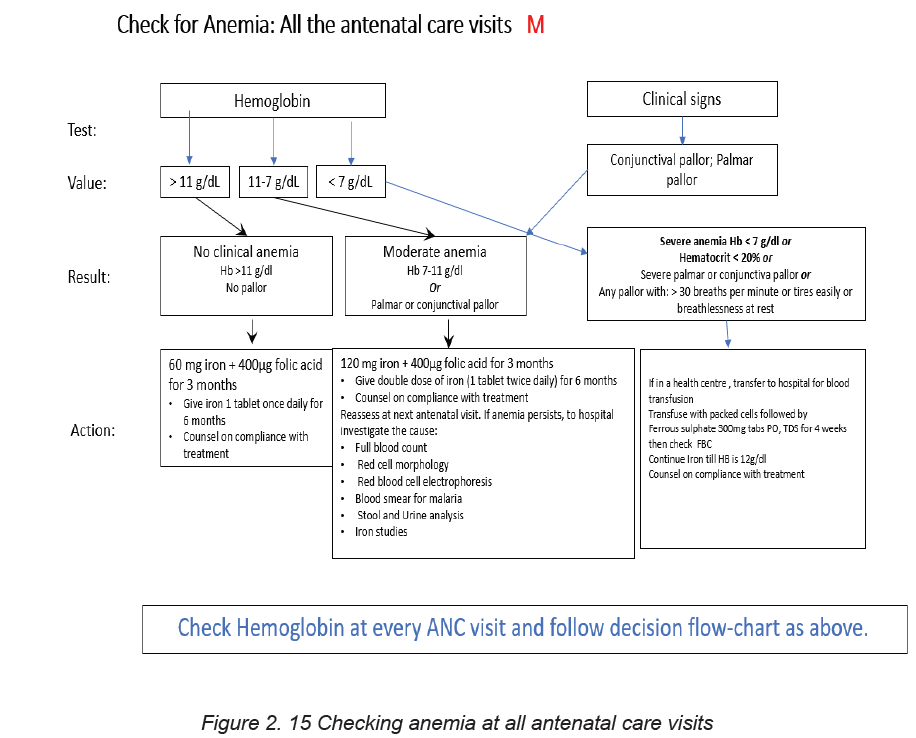
– How does iron deficiency anemia affect the fetus during pregnancy?
2.17 Nutrition during pregnancy
Learning Activity 2.17
In village, pregnant women and other families with under five years’ children
were being taught the importance of kitchen garden (“akarima k’igikoni”), and
you were asked to talk about what the pregnant need to eat to be healthy.
– Describe a balanced diet and its benefits to human body.
To maintain a healthy pregnancy, approximately 300 extra calories are needed each
day. These calories should come from a balanced diet of protein, fruits, vegetables
and whole grains. Sweets and fats should be kept to a minimum. A healthy, wellbalanced
diet can also help to reduce some pregnancy symptoms, such as nausea
and constipation.
Key messages on nutrition for a positive pregnancy:
♦ All pregnant women should be counseled on healthy eating for a positive
pregnancy at each ANC visit. These messages should be reinforced by the
CHWs during home visits;
♦ Pregnant women should receive 3 meals and at least one additional snack
using diverse food types to improve the quality and micronutrient intake;
♦ Pregnant women should avoid coffee, energy drinks, Coca-Cola, alcohol,
fatty foods, raw or undercooked meats in pregnancy;
♦ Pregnant women who are obviously malnourished need special attention,
counselling and advice from a trained nutritionist or a trained health care
provider;
♦ Adolescent girls who are pregnant have their own need for growth and
additional needs for fetus growth. Adolescent girls who become pregnant
needs very special care with at least 3 meals and 2 snacks daily, using a
variety of foods including animal source foods in every meal.
Education for appropriate infant feeding:
Health providers should discuss the importance and management of breastfeeding
with all pregnant women and their families. All pregnant women must have basic
information about breastfeeding, in order to make informed decisions.
Where facilities provide antenatal care, pregnant women and their families should
be counselled about the benefits and management of breastfeeding.
The health facility could organize classes with practical sessions on breastfeeding
and how to overcome breastfeeding difficulties.
The message given during antenatal discussion, group’s education and
communication materials should include at a minimum:
• Importance of breastfeeding;
• Exclusive breastfeeding for the first 6 months, the risks of giving formula or
other breast-milk
• Substitutes, and the fact that breastfeeding continues to be important after 6
months;
• Importance of immediate and sustained skin to-skin contact;
• Importance of early initiation of breastfeeding within one hour after birth;
• Importance of rooming-in;
• Basics of good positioning and attachment;
• Recognition of feeding cues;
• Importance of starting to give other foods at 6 months of age;
• Importance of gradually introducing a variety of foods from 6 months to one
year;
• Importance of continuing to breastfeed the child up to 24 months;
If the mother’s HIV test is positive, she should receive ARTs and be counselled and
supported for infant feeding; the mother can breastfeed like for other infants, except
that breastfeeding should gradually be interrupted at 18 months.
Micronutrient supplementation during pregnancy:
During pregnancy, women have additional needs in all nutrients and micronutrients.
For some micronutrients such as iron, folic acid and calcium, the needs are difficult
to be covered by food intake alone and micronutrients supplements are needed.
a. Iron and folic acid supplementation:
Pregnant women should be prescribed a daily dose of oral iron (60mg) and folic
acid supplementation (400μg =0.4 mg) during the whole course of pregnancy to
prevent maternal anemia, puerperal sepsis, low birth weight, and preterm birth.
b. Calcium supplementation:
Given the insufficient intake of calcium in women in Rwanda, pregnant women
should receive a daily calcium supplementation (1.5–2.0 g oral elemental calcium)
to reduce the risk of pre-eclampsia.
Dividing the dose of calcium may improve acceptability. The suggested scheme
for calcium supplementation is 1.5–2 g daily, with the total dose divided into three
doses, preferably taken at mealtimes.
Calcium supplementation is recommended to woman with high risks to develop
pre-eclampsia during pregnancy:
• Primigravidae, teenagers and elderly primigravidae.
• Women of age 35 years and above.
• Previous pregnancy complicated by pre-eclampsia.
• Previous abruptio placentae or intra-uterine death.
• Multiple pregnancies.
• Medical complications such as chronic hypertension, renal disorders,diabetes, connective tissue disorders or antiphospholipid syndrome
Self-assessment 2.17
– Differentiate micro nutrients from macro nutrients
End unit assessment 2
1. What is focused FANC?
2. Differentiate the terms: Health promotion and health education
3. Describe the components of focused ANC
4. Using a table, show the new model of eight contacts in FANC5. List the issue that may confuse the diagnosis of an early pregnancy
