UNIT 1 NORMAL PREGNANCY
Key Unit competence: Identify the characteristics of a normal pregnancy.Introductory activity 1.0
A 21 years old woman was admitted in consultation room at the health center
complaining of nausea and vomiting in early hours of the morning, frequent
urination, fatigue, loss of appetite, abdominal pain and not able to carry out
normal daily activities. During interview, she reported to be married 4 months
ago, living with a husband and missed her periods 6 weeks ago. On head-to-toe
examination, breasts were tender and full.
After reading and understanding the above scenario, based on your experiencesinterpret the above case.
1.1 Key concepts used in pregnancyLearning Activity 1.1
Pregnancy begins from the conception when the egg and sperm fuse together
and fertilization takes place. The fertilized egg becomes a zygote. Then, it
initiates organized development of a biological entity known as embryo, with a
human nuclear genome or altered human nuclear genome that has the potential
to develop up to, or beyond, the stage at which the primitive vein appears, and
has not yet reached 8 weeks of development since the first mitotic division to
become a fetus. The zygote that was formed after fertilization travels through the
oviduct to the uterus, which is a hollow muscular organ that plays a remarkable
role in pregnancy by stretching and expanding. The outer layer of the embryo
begins to merge with the endometrium (inner membrane of the uterus), and
thereafter (after getting pregnant) there is a formation of an organ which attaches
to the uterus called placenta that provides oxygen and nutrients to the growing
baby and remove waste products from the baby’s blood.
Based on the above passage, explain the following terms:
a. Pregnancy
b. Fertilization
c. Uterus
d. Placenta
e. Embryo
f. Fetus
The normal pregnancy starts from the conception, formation of the embryo and
fetus, progressive growth of uterus from the pelvic organ to become an abdominal
organ under the influence of hormones.
a. Pregnancy
Pregnancy is the time during which one or more fetus develop inside a woman.
It usually last about 40 weeks or nine months from the Last Menstrual Period.
Pregnancy can occur by sexual intercourse or assisted reproductive technology.
It always happens when a sperm fertilizes an egg after it’s released from the
ovary during ovulation. The fertilized egg then travels down into the uterus, where
implantation occurs. A successful implantation results in pregnancy.
b. Fertilization
Human fertilization also known as conception is the fusion of the genetic material of
the haploid sperm cell and the secondary oocyte to form the zygote. This process
takes approximately 12 to 24 hours and normally occurs in the ampulla of the
uterine tube.
c. Uterus
The uterus is a hollow muscular organ located in the female pelvis between the
bladder and rectum. It has three muscular layers, the internal layer (endometrium),
the middle muscular layer of the uterine wall (myometrium) and the outer layer
(perimetrium). Once the egg has left the ovary it can be fertilized and implant itself in
the lining of the uterus. The main function of the uterus is to nourish the developing
fetus prior to birth.
d. Placenta
The placenta is an organ that develops from throphoblasts in uterus during
pregnancy. This structure provides oxygen and nutrients to the growing baby and
removes wastes products from the baby’s blood. The placenta attaches to the wall
of the uterus and the baby’s umbilical cord arises from it.
e. Embryo
The embryo in human is defined as the developing organism from the fourth day
after fertilization to the end of the eighth week and undergoes early stages of growth
and differentiation.
f. Fetus
The fetus is an unborn baby that develops and grows inside the uterus (womb).The baby is referred to as a fetus from 8 weeks of gestation (pregnancy) until birth.
Self-assessment 1.1
1) Differentiate the embryo from fetus as human development stages.
2) Describe the Characteristics of Embryo & Fetus3) Where does the placenta develop from during the embryonic stage?
1.2 GametogenesisLearning Activity 1.2
A couple who has been married for over 2 years but have failed to reproduce
offspring was received in consultation. The woman is 40 years old and the
husband 52 years old. They both weigh 96kg. The husband is a tanker driver
and always exposed to the heat from the engine of the truck... He smokes 2
packets of cigarettes per day, at home, they reside near to an industrial plant
that produces pesticides, which pollute the nearby water source and their small
vegetable farm. The wife complained of irregular cycles for the past 3 years.
The wife states that before marriage, she has been using contraceptives pills
but stopped after her marriage. They came in consultation to seek solutions for
their problem.
1) With your knowledge and understanding of S3 biology, what do you think
are the possible causes for the delay in conception?
2) What advice can you give to them based on your knowledge andunderstanding of S3 biology.
In preparation for fertilization, germ cells undergo gametogenesis, which includes
meiosis, to reduce the number of chromosomes and differentiation to complete
their maturation.
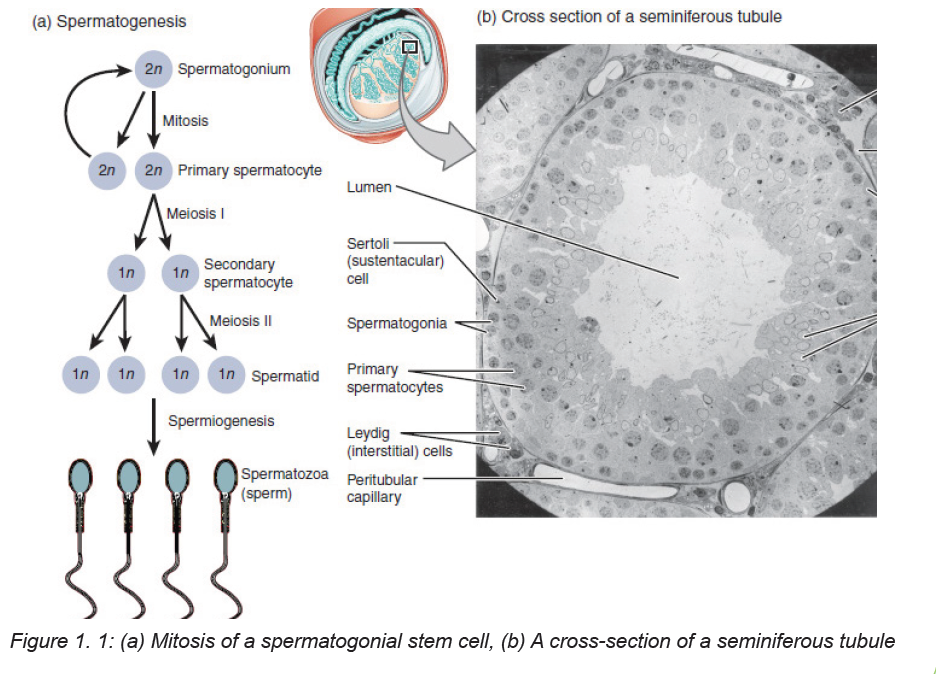
The process of differentiation of a spermatogonium into a spermatid is known as
spermatogenesis. It is a complex, temporal event whereby primitive, totipotent
stem cells divide to either renew themselves or produce daughter cells that become
specialized testicular spermatozoa over a span of weeks. Spermatogenesis involves
both mitotic and meiotic proliferation. as well as extensive cell remodeling.
Spermatogenesis can be divided into three major phases: (1) proliferation and
differentiation of spermatogonia, (2) meiosis, and (3) spermiogenesis, a complex
metamorphosis that transforms round spermatids arising from the final division
of meiosis into a complex structure called the spermatozoon. In humans, the
process of spermatogenesis starts at puberty and continues throughout the entire
lifespan of the individual. It takes place in the lumen of the seminiferous tubules.
In fact, 90% of the testis volume is determined by the seminiferous tubules and
their constituent germ cells at various stages of development. Once the gonocytes
have differentiated into fetal spermatogonia, an active process of mitotic replication
is initiated very early in embryonic development. This appears to be under FSH
control and develops the baseline number of precursor cells of the testicle.
Proliferation and Differentiation of Spermatogonia
Within the seminiferous tubule, germ cells are arranged in a highly ordered
sequence from the basement membrane to the lumen. Spermatogonia lie directly
on the basement membrane, followed by primary spermatocytes, secondary
spermatocytes, and spermatids as they progress toward the tubule lumen. The
tight junction barrier supports spermatogonia and early spermatocytes within the
basal compartment and all subsequent germ cells within the luminal compartment.
Spermatocytogenesis
The purpose of spermatogenesis is to produce genetic material necessary for the
replication of the species through mitosis and meiosis. Spermatocytogenesis takes
place in the basal compartment. Primary spermatocytes enter the first meiotic
division to form secondary spermatocytes. Prophase of the first meiotic division
is very long, and the primary spermatocyte has the longest lifespan. Secondary
spermatocytes undergo the second meiotic division to produce spermatids.Secondary spermatocytes are short-lived (1.1 to 1.7 days).
Mitosis
Mitosis involves proliferation and maintenance of spermatogonia. It is a precise,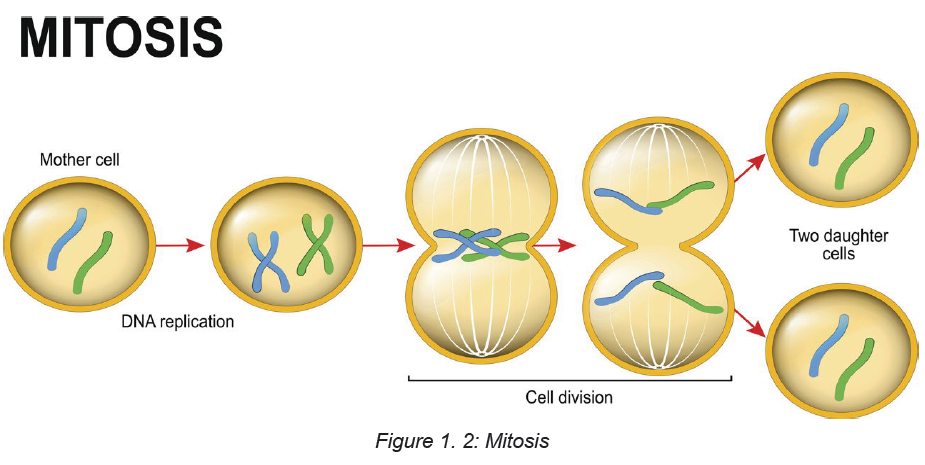
well-orchestrated sequence of events involving duplication of the genetic material
(chromosomes), breakdown of the nuclear envelope, and equal division of
the chromosomes and cytoplasm into two daughter cells. DNA is also spatially
organized into loop domains on which specific regulatory proteins interact during
cellular replication. The mitotic phase involves spermatogonia (types A and B) and
primary spermatocytes (spermatocytes I). Developing germ cells interconnected by
intracellular bridges produce the primary spermatocyte through a series of mitotic
divisions. Once the baseline number of spermatogonia is established after puberty,
the mitotic component will proceed in order to continue to provide precursor cellsand to start the process of differentiation and maturation.
Meiosis
Meiosis is a complex process with specific regulatory mechanisms of its own.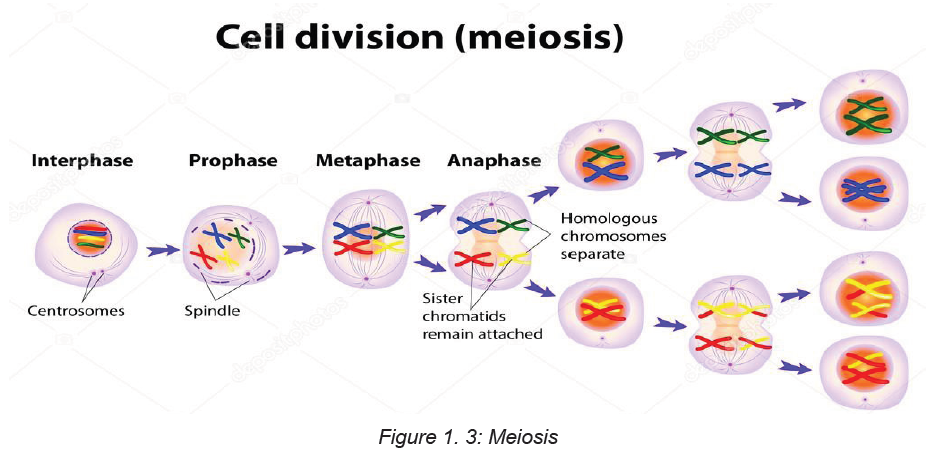
The process commences when type B spermatogonia lose their contact with the
basement membrane to form preleptotene primary spermatocytes. Thus, each
primary spermatocyte can theoretically yield four spermatids, although fewer
actually result, because some germ cells are lost due to the complexity of meiosis.
The primary spermatocytes are the largest germ cells of the germinal epithelium.
Meiosis is characterized by prophase, metaphase, anaphase, and telophase. In
this, two successive cell divisions yield four haploid spermatids from one diploid
primary spermatocyte. As a consequence, the daughter cells contain only half of
the chromosome content of the parent cell. After the first meiotic division (reduction
division), each daughter cell contains one partner of the homologous chromosome
pair, and they are called secondary spermatocytes. These cells rapidly enter the
second meiotic division (equational division), in which the chromatids then separate
at the centromere to yield haploid early round spermatids. Meiosis assures genetic
diversity and involves primary and secondary spermatocytes, which give rise tospermatids.
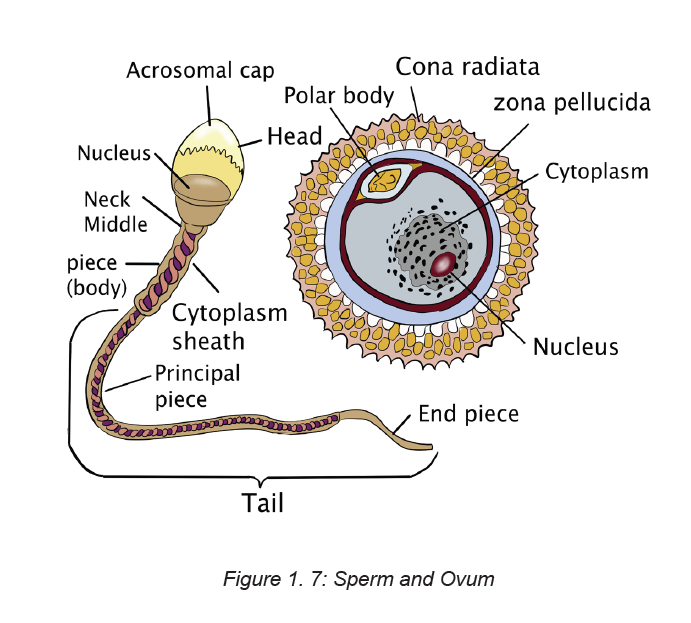
Ovum
The unequal cell division of oogenesis produces one to three polar bodies that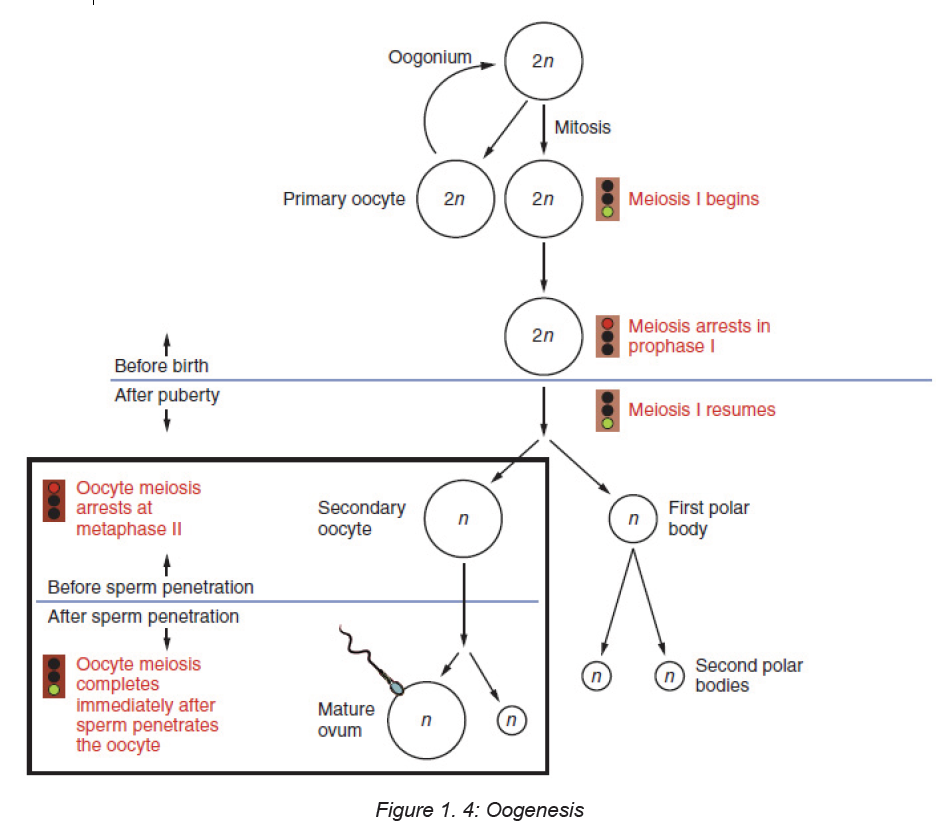
later degrade, as well as a single haploid ovum, which is produced only if there is
penetration of the secondary oocyte by a sperm cell.
Meiosis occurs in the female in the ovarian follicles and produces an egg, or ovum.
Each month one ovum matures with a host of surrounding supportive cells. At
ovulation the ovum is released from the ruptured ovarian follicle. High estrogen
levels increase the motility of the uterine tubes so their cilia are able to capture
the ovum and propel it through the tube toward the uterine cavity. An ovum cannot
move by itself. Two protective layers surround the ovum. The inner layer is a thick,
acellular layer, the zona pellucida. The outer layer, the corona radiata, is composed
of elongated cells.
Ova are considered fertile for about 24 hours after ovulation. If not fertilized by asperm, the ovum degenerates and is resorbed.
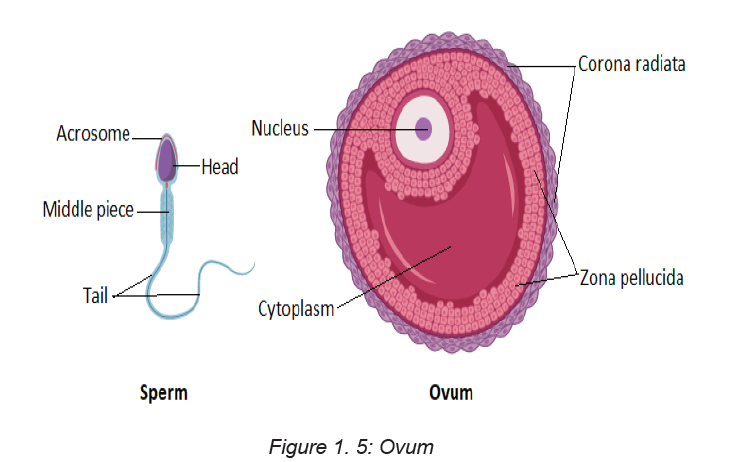
Ejaculation during sexual intercourse normally propels about a teaspoon of semen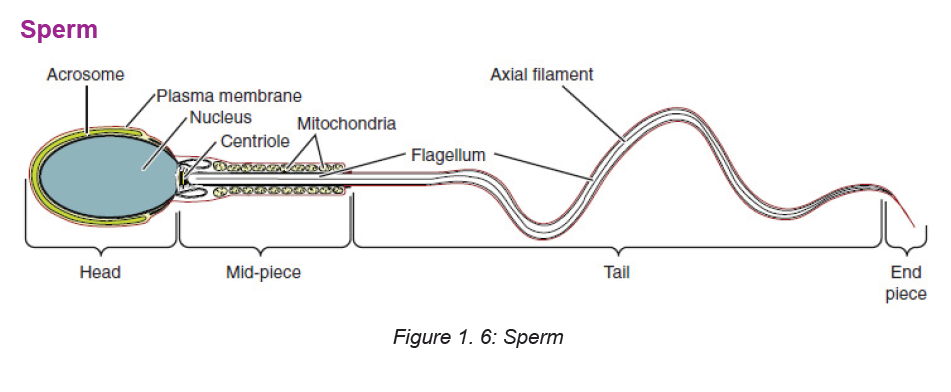
containing as many as 200 to 500 million sperm, into the vagina. The sperm swim
propelled by the flagellar movement of their tails. Some sperm can reach the site of
fertilization within 5 minutes, but average transit time is 4 to 6 hours. Sperm remain
viable within the woman’s reproductive system for an average of 2 to 3 days. Most
sperm are lost in the vagina, within the cervical mucus, or in the endometrium, or
they enter the uterine tube that contains no ovum. As the sperm travel through
the female reproductive tract, enzymes are produced to aid in their capacitation.
Capacitation is a physiologic change that removes the protective coating from
the heads of the sperm. Small perforations then form in the acrosome (a cap on
the sperm) and allow enzymes (e.g., hyaluronidase) to escape. These enzymes
are necessary for the sperm to penetrate the protective layers of the ovum beforefertilization.
Self-assessment 1.2
1) Describe the process of gametogenesis
2) Differentiate between spermatogenesis and oogenesis3) What are the differences between meiosis and mitosis?
1.3 Fertilization
Learning Activity 1.3
Using the diagram above:
a. Explain the process and stages of fertilization.b. What is capacitation?
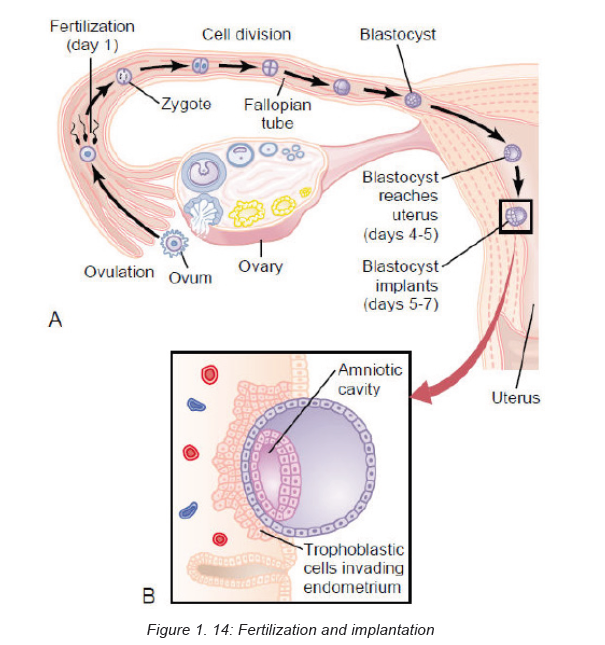
Fertilization occurs as a result of the female gamete, or oocyte, merging with the
male gamete, or spermatozoon. It is more commonly known as conception.
After the point of fertilization, the fused product of the female and male gamete is
referred to as a zygote or fertilized egg. For species that undergo internal fertilization,
such as humans, the fusion of male and female gametes usually occurs following
the act of sexual intercourse. However, the advent of artificial insemination and
in vitro fertilization have made achieving pregnancy possible without engaging in
sexual intercourse. This approach may be undertaken as a voluntary choice or dueto infertility.
The process of fertilization occurs in several steps and the interruption of any of
them can lead to failure. At the beginning of the process, the sperm undergoes a
series of changes, as freshly ejaculated sperm is unable or poorly able to fertilize.
The sperm must undergo capacitation (process where sperm undergoes changes
to the plasma membrane, resulting in the removal of the glycoprotein coat and
increased flagellation), in the female’s reproductive tract over several hours, which
increases its motility and destabilizes its membrane. By destabilizing the membrane,
the sperm prepares for the acrosome reaction, the enzymatic penetration of the
egg’s tough membrane, the zona pellucida. The sperm and the egg cell (which has
been released from one of the female’s two ovaries) unite in one of the two fallopian
tubes.
The fertilized egg, known as a zygote, then moves toward the uterus, a journey that
can take up to a week to complete until implantation occurs. Through fertilization,
the egg is activated to begin its developmental process (progressing through
meiosis II), and the haploid nuclei of the two gametes come together to form the
genome of a new diploid organism.
Nondisjunction during the completion of meiosis or problems with early cell
division in the zygote to blastula stages can lead to problems with implantation and
pregnancy failure.
Fertilization takes place in the ampulla (outer third) of the uterine tube. When a
sperm successfully penetrates the membrane surrounding the ovum, both sperm
and ovum are enclosed within the membrane, and the membrane becomes
impenetrable to other sperm; this process is termed the zona reaction. The second
meiotic division of the secondary oocyte is then completed, and the nucleus of
the ovum becomes the female pronucleus. The head of the sperm enlarges to
become the male pronucleus, and the tail degenerates. The nuclei fuse, and the
chromosomes combine, restoring the diploid number (46). Conception is said tohave taken place.
A, Ovum fertilized by X-bearing sperm to form female zygote.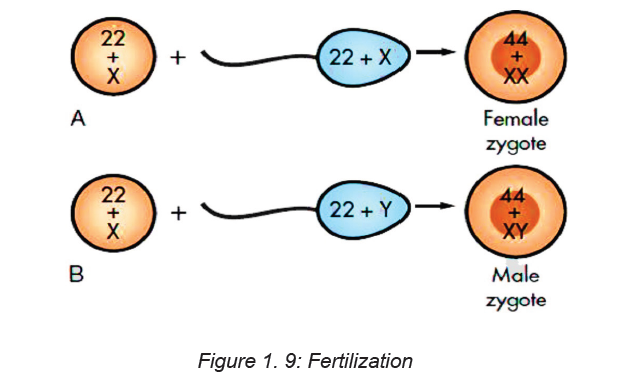
B, Ovum fertilized by Y-bearing sperm to form male zygote.
Mitotic cellular replication, called cleavage, begins as the zygote travels the length
of the uterine tube into the uterus. This transit takes 3 to 4 days. Because the
fertilized egg divides rapidly with no increase in size, successively smaller cells,
blastomeres, are formed with each division. A 16-cell morula, a solid ball of cells,is produced within 3 days and is still surrounded by the protective zona pellucida.
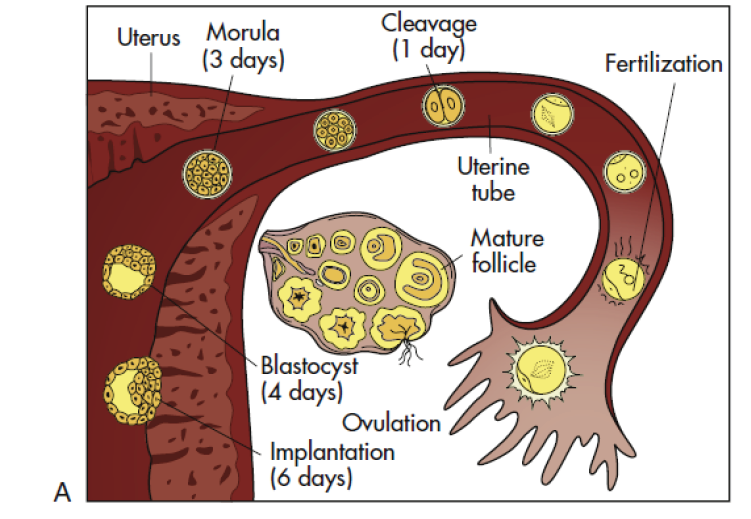
A, Follicular development in the ovary, ovulation, fertilization, and transport of the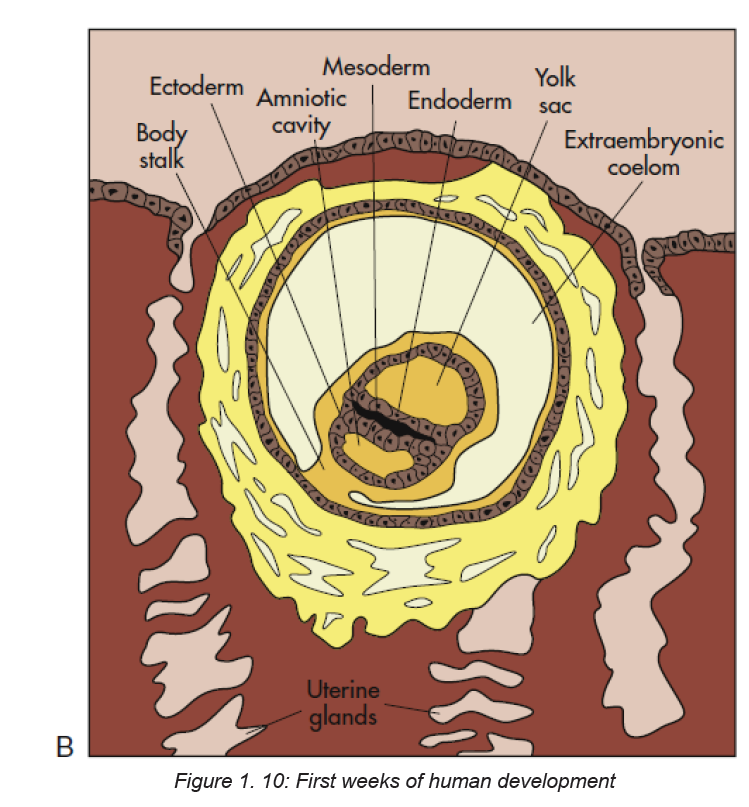
early embryo down the uterine tube and into the uterus, where implantation occurs.
B, Blastocyst embedded in endometrium. Germ layers forming.
Further development occurs as the morula floats freely within the uterus. Fluid
passes through the zona pellucida into the intercellular spaces between the
blastomeres, separating them into two parts, the trophoblast (which gives rise to
the placenta) and the embryoblast (which gives rise to the embryo). A cavity forms
within the cell mass as the spaces come together, forming a structure called the
blastocyst cavity. When the cavity becomes recognizable, the whole structure of
the developing embryo is known as the blastocyst. Stem cells are derived from the
inner cell mass of the blastocyst. The outer layer of cells surrounding the blastocyst
cavity is the trophoblast. The trophoblast differentiates into villous and extravillous
trophoblast.
Simultaneous to implantation, the embryo continuous developing. the cell of
the embryoblast differentiates into two types of cells: the epiblast (closest to thetrophoblasts) and the hypoblast (closest to the blastocyst cavity). These two layers
of cells form a flat disc known as bilaminar embryonic disc through a process of
gastrulation (three layers). The first appearance of these layers collectively are
known as the primitive streak, around day 15.
ECTODERM: this is the start of tissue that covers most surfaces of the body. the
epidermis layer of the skin, hair and nails and the nervous system
MESODERM: The mesoderm forms the muscle, skeleton, dermis of the skin,
connective tissue, the urogenital glands, blood vessels, blood and lymph cells.
ENDODERM: They form the epithelial lining of the digestive, respiratory, urinarysystems and glandular cells of organs such as the liver and pancreas.
Figure 1. 11: Extravillous trophoblasts are found outside the villus and can be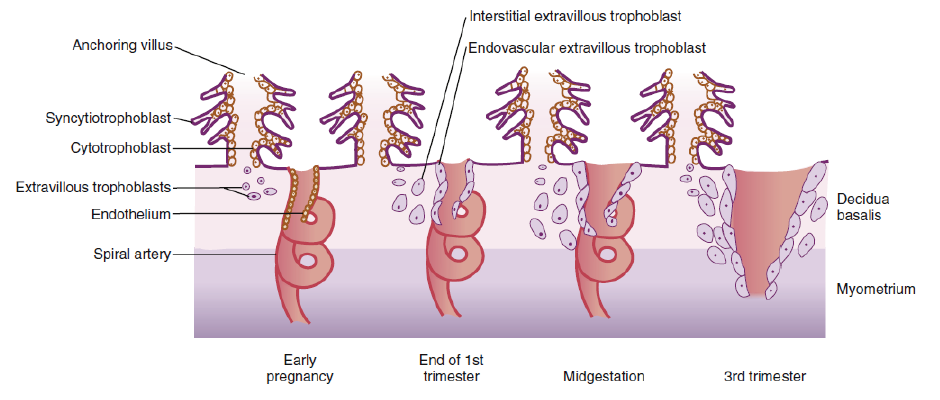
subdivided into endovascular and interstitial categories. Endovascular trophoblasts
invade and transform spiral arteries during pregnancy to create low-resistance
blood flow that is characteristic of the placenta. Interstitial trophoblasts invade thedecidua and surround spiral arteries.
Factors that may affect fertilization and implantation
Other factors include: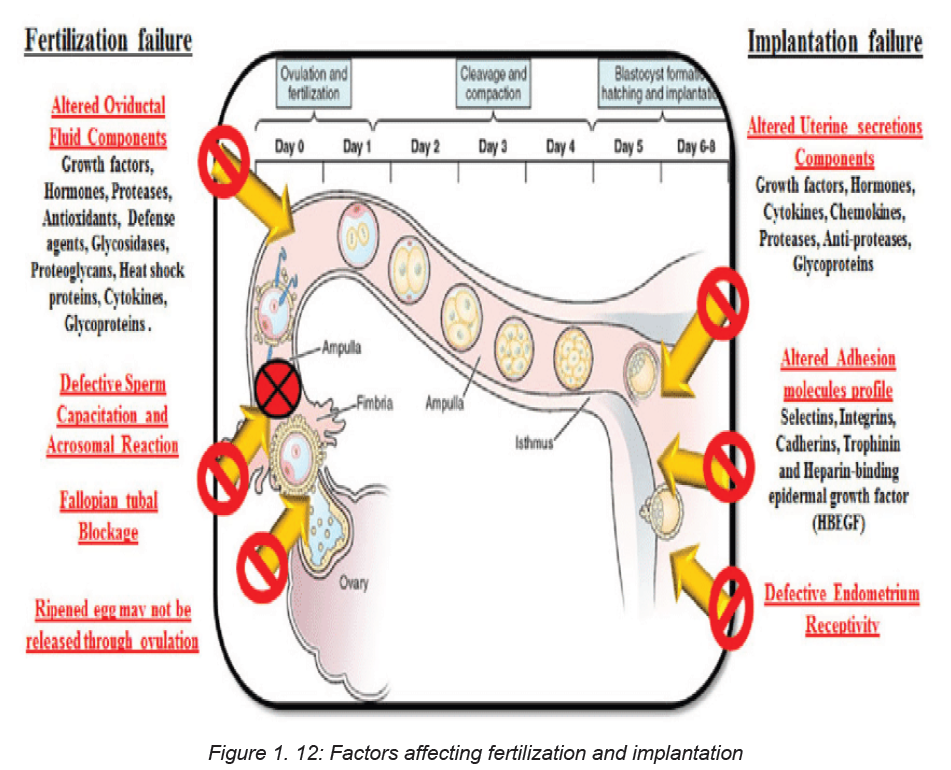
Age
Female age is the most important factor affecting fertility. Women are born with all
the eggs they will ever have and the number of eggs available decreases each day
from birth onwards. In young women the decline is fairly gradual (only a few eggs
are ‘lost’ each day), but as women approach their mid to late 30s, the decrease gets
much steeper (many more eggs are ‘lost’ each day). In addition to this decrease
in the number of eggs available, the quality of the eggs also declines as women
get older. This reduction in both the quantity and quality of available eggs means
that older women are less likely to get pregnant and, if they do get pregnant, they
are more likely to have a miscarriage. Male fertility may also decrease with age
although to a much lesser degree.
Previous Pregnancy
Couples are more likely to get pregnant if they have previously achieved a pregnancy
together (irrespective of whether or not that pregnancy resulted in the birth of a
baby) compared to couples that have never been pregnant.
Duration of subfertility
The longer couples have been trying to get pregnant, the less likely they are to be
successful. If a couple have been trying to get pregnant for less than 3 years they
are almost twice as likely to get pregnant than couples who have been trying for
more than 3 years.
Timing and Frequency of Sexual Intercourse
Most women have a 28-day menstrual cycle: this means there are 28 days between
the start of one period and the start of the next period. Ovulation (when an egg
is released from the ovary) occurs on day 14 of a 28-day cycle. Whether or not
that egg gets fertilised by a sperm depends on the day(s) in the cycle in which
intercourse occurs. The chance of getting pregnant is low at the beginning of the
cycle and starts to increase from about day 8 onwards. Women are most likely to
get pregnant if they have sex 2 days before they ovulate (i.e. on day 12 of 28-day
cycle).
Once ovulation has occurred, the chance of getting pregnant decreases dramatically:
sperm need to be present in the female genital tract prior to ovulation to maximise
the chances of getting pregnant. The reason for this is that once ovulation has
occurred, levels of the hormone progesterone increase and this causes cervical
mucus to become thick and sticky which prevents sperm from being able to swim
through it to get to the egg to fertilise.
Couples that have regular sex a week are most likely to get pregnant because this
frequency ensures that a good volume of fresh sperm will be present in the female
reproductive tract at the time of ovulation. If couples are only having sex once a
week, the chance of getting pregnant is less because there will be less fresh sperm
present in the female genital tract at the time of ovulation.
Lifestyle Factors
Weight
Overweight women who have irregular periods are less likely to release an egg
each month (ovulate) than women with regular periods. This means the chances
of getting pregnant are reduced. Losing weight, even as little as 5-10% of the total
body weight, may restore a regular menstrual cycle thereby increasing the chance
of getting pregnant.
Women who are overweight take longer to get pregnant than women who are
not, even if their periods are regular. Being overweight is also associated with
an increased risk of miscarriage and of problems during pregnancy and delivery.
Losing weight has been shown to improve fertility and increase the chance of
getting pregnant. No one diet has been shown to be better than any other but
group exercise programmes that involve both exercise and dietary advice leads to
more pregnancies than weight loss advice alone.
Men who are overweight may have suboptimal sperm and therefore reduced fertility.
Being underweight can also affect female fertility as it may mean that an egg is not
released each month. Being underweight is also associated with problems during
pregnancy. Gaining weight is likely to improve fertility.
Smoking
Women who smoke are 3 times more likely to experience a delay in getting pregnant
than non-smokers. Even passive smoking can be harmful. Smoking reduces
a woman’s ovarian reserve (so her ovaries will have fewer eggs in them than a
woman of the same age who does not smoke) and damages the cilia inside the
fallopian tube (which are important for transporting the egg and/or embryo along
the fallopian tube into the uterus). In men, smoking may reduce sperm quantity
and quality.
Caffeine
There is no clear association between caffeine consumption and infertility
Alcohol
Some studies report that drinking more than 5 units of alcohol a week may reduce
female fertility but others state that low to moderate alcohol consumption may
be associated with higher pregnancy rates than non-drinkers. Once pregnant,
excessive alcohol consumption may lead to birth defects and developmental delay.
The Royal College of Obstetricians and Gynaecologists and the Department of
Health recommend that women trying to get pregnant should avoid alcohol because
there is no ‘safe’ limit.
In men, excessive alcohol may lead to difficulties maintaining an erection, impaired
ejaculation and reduced sperm quality.
Over-the-counter and recreational drugs
Non-steroidal anti-inflammatory drugs such as ibuprofen can interfere with ovulation.
Aspirin may interfere with implantation. Recreational drugs such as marijuana
and cocaine may interfere with ovulation and/or the function of the fallopian tube.
The fallopian tube is important for transporting the egg from the ovary where it is
released, to the womb (uterus) where an embryo will hopefully implant. Fertilisation
occurs in the fallopian tube. Anabolic steroids, which are abused by some bodybuilders,
inhibit the production of sperm and this may be permanent even if the drug
is stopped.
Medical Conditions
Some women may have medical conditions that can affect their fertility. These
may or may not be known about when starting to try for a family. Some of these
conditions may be more general, for example thyroid disease and vitamin D
deficiency whilst others may be more specific, for example, polycystic ovarysyndrome and endometriosis.
Self-assessment 1.3
1. Where precisely does the fertilization normally take place?2. List the sequence of development of a fertilized egg from zygote to embryo.
1.4. ImplantationLearning Activity 1.4
Based on your knowledge and understanding of biology what is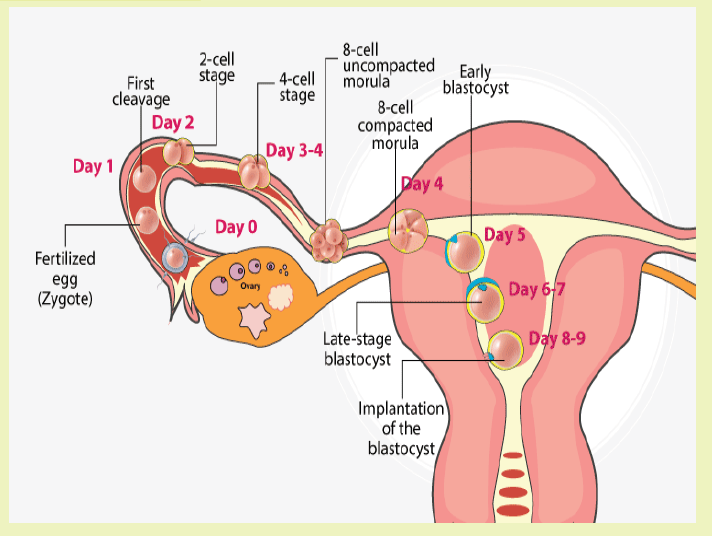
implantation?
At the end of the first week, the blastocyst comes in contact with the uterine wall and
adheres to it, embedding itself in the uterine lining via the trophoblast cells. Thus
begins the process of implantation, which signals the end of the pre-embryonic
stage of development. Implantation can be accompanied by minor bleeding.
The blastocyst typically implants in the fundus of the uterus or on the posterior
wall. However, if the endometrium is not fully developed and ready to receive the
blastocyst, the blastocyst will detach and find a better spot. A significant percentage
(50–75 percent) of blastocysts fail to implant; when this occurs, the blastocyst is
shed with the endometrium during menses. The high rate of implantation failure is
one reason why pregnancy typically requires several ovulation cycles to achieve.
When implantation succeeds and the blastocyst adheres to the endometrium,
the superficial cells of the trophoblast fuse with each other, forming the
syncytiotrophoblast, a multinucleated body that digests endometrial cells to firmly
secure the blastocyst to the uterine wall. In response, the uterine mucosa rebuilds
itself and envelops the blastocyst. The trophoblast secretes human chorionic
gonadotropin (hCG), a hormone that directs the corpus luteum to survive, enlarge,
and continue producing progesterone and estrogen to suppress menses. These
functions of hCG are necessary for creating an environment suitable for the
developing embryo. As a result of this increased production, hCG accumulates in
the maternal bloodstream and is excreted in the urine. Implantation is complete by
the middle of the second week. Just a few days after implantation, the trophoblast
has secreted enough hCG for an at-home urine pregnancy test to give a positiveresult.
Most of the time an embryo implants within the body of the uterus in a location that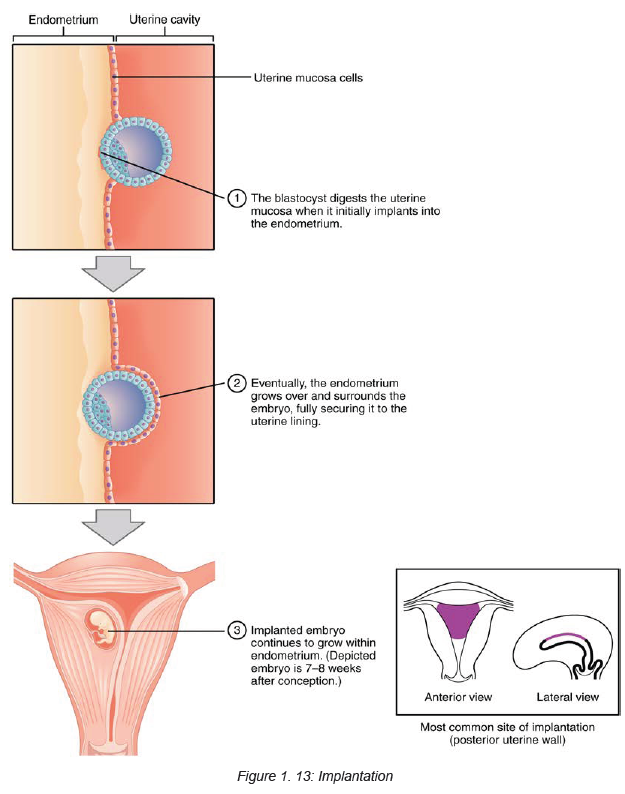
can support growth and development. However, in one to two percent of cases, the
embryo implants either outside the uterus (an ectopic pregnancy) or in a region of
uterus that can create complications for the pregnancy. If the embryo implants in
the inferior portion of the uterus, the placenta can potentially grow over the openingof the cervix, a condition call placenta previa.
Self-assessment 1.4
1. How do you know that an embryo has been successfully implanted?2. Differentiate implantation bleeding and normal menstrual bleeding.
1.5 Embryological and fetal development.Learning Activity 1.5
1. From the knowledge and understanding gained in biology Describe the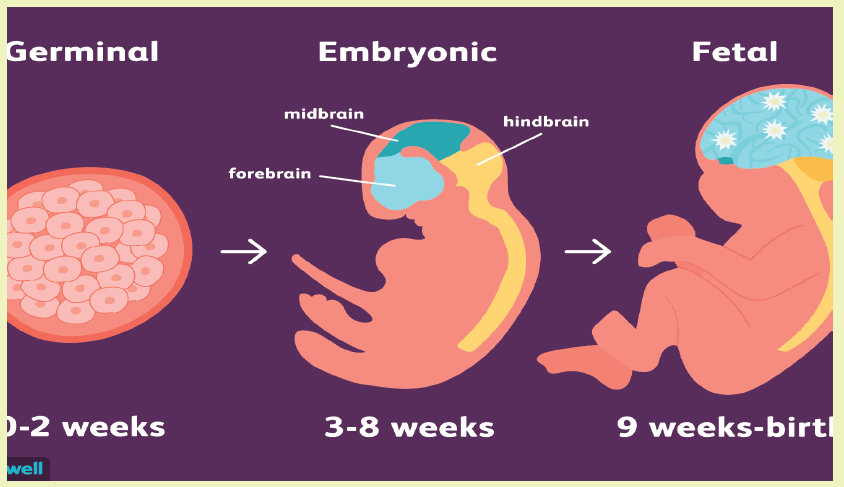
embryological stages of development.2. What is amniotic fluid? Discuss its functions in pregnancy.
Embryological and fetal periods of development.
a. Development of the embryo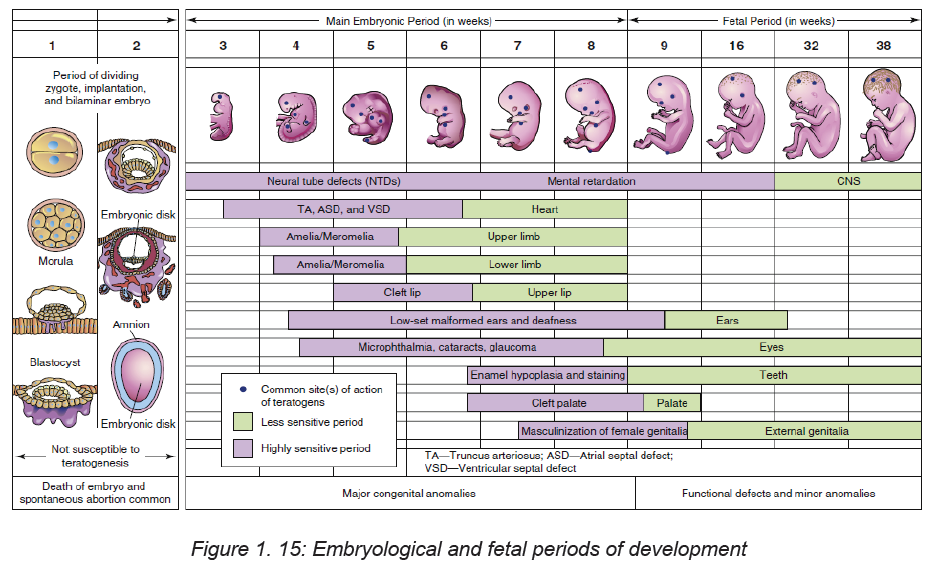
The stage of the embryo lasts from day 15 until approximately 8 weeks after
conception, when the embryo measures 3 cm from crown to rump. This
embryonic stage is the most critical time in the development of the organ
systems and the main external features. Developing areas with rapid cell
division are the most vulnerable to malformation caused by environmental
teratogens (substances or exposure that causes abnormal development).
At the end of the eighth week, all organ systems and external structures are
present, and the embryo is unmistakably human.
b. Membranes
At the time of implantation, two fetal membranes that will surround the
developing embryo begin to form. The chorion develops from the trophoblast
and contains the chorionic villi on its surface. The villi burrow into the decidua
basalis and increase in size and complexity as the vascular processes
develop into the placenta. The chorion becomes the covering of the fetal side
of the placenta.
The inner cell membrane, the amnion, develops from the interior cells of the
blastocyst. The cavity that develops between this inner cell mass and theouter layer of cells (trophoblast) is the amniotic cavity.
c. Amniotic fluid
Amniotic fluid is present at the formation of the amniotic sac. This is a thin-walled
sac that contains the fetus during pregnancy. Amniotic fluid is a clear alkaline
and slightly yellowish liquid contained within the amniotic sac.it is derived
from maternal circulation across placental membranes and exuded from the
fetal surface. The fetus contributes to the amniotic fluid through metabolism
in small quantities of urine and fluids from its lung. Amniotic fluid is made
up of 98% water and electrolytes, along with peptides, carbohydrates, and
signaling molecules. The remaining 2% is made up of lipids and hormones.
Function
Amniotic fluid serves a number of purposes during pregnancy, primarily to protect
the fetus from harm. The functions of the amniotic fluid include:
• Acting as a cushion: This protects the fetus from injury should the mother’s
abdomen be the subject of trauma or a sudden impact.
• Protecting the umbilical cord: Amniotic fluid flows between the umbilical
cord and fetus.
• Protecting from infection: Amniotic fluid has antibacterial properties.
• Containing essential nutrients: These include proteins, electrolytes,
immunoglobulins, and vitamins that assist in the development of the fetus.
• Allowing for the fetus to move: Amniotic fluid also allows the developing
fetus to move around in the womb, which in turn allows for proper development
and growth of the musculoskeletal system, gastrointestinal system, and
pulmonary system.
• Maintaining temperature: Amniotic fluid assists in keeping a constant steady
temperature around the fetus throughout pregnancy, protecting the baby from
heat loss.
d. Umbilical cord
By day 14 after conception, the embryonic disk, the amniotic sac, and the
yolk sac are attached to the chorionic villi by the connecting stalk. During the third
week the blood vessels develop to supply the embryo with maternal nutrients and
oxygen. During the fifth week the embryo has curved inward on itself from both
ends, bringing the connecting stalk to the ventral side of the embryo. The connecting
stalk becomes compressed from both sides by the amnion and forms the narrower
umbilical cord.
Two arteries carry blood from the embryo to the chorionic villi, and one veinreturns blood to the embryo.
e. York sac
When the amniotic cavity and amnion are forming, another blastocyst cavity forms
on the other side of the developing embryonic disk. This cavity becomes surrounded
by a membrane, forming the yolk sac. The yolk sac aids in transferring maternal
nutrients and oxygen, which have diffused through the chorion, to the embryo.
Summary of embryological and fetal development
Embryo
0–4 weeks
• Blastocyst implants
• Primitive streak appears
• Conversion of bilaminar disc into trilaminar disc
• Some body systems laid down in primitive form
• Primitive central nervous system forms (neurulation)
• Primitive heart develops and begins to beat
• Covered with a layer of skin
• Limb buds form
• Optic vessels develop
• Gender determined
4–8 weeks
• Very rapid cell division
• More body systems laid down in primitive form and continue to develop
• Spinal nerves begin to develop
• Blood is pumped around the vessels
• Lower respiratory system begins to develop
• Kidneys begin to develop
• Skeletal ossification begins developing
• Head and facial features develop
• Early movements
• Embryo visible on ultrasound from 6 weeks
Fetus
8–12 weeks
• Rapid weight gain
• Eyelids meet and fuse
• Urine passed
• Swallowing begins
• Distinguishing features of external genitalia appear
• Fingernails develop
• Some primitive reflexes present 12–16 weeks
• Rapid skeletal development – visible on X-ray
• Lanugo appears
• Meconium present in gut
• Nasal septum and palate fuse
• Eternal genitalia fully differentiate into male or female by week 12
• Fetus capable of sucking thumb
16–20 weeks
• Constant weight gain
• ‘Quickening’ – mother feels fetal movements
• Fetal heart heard on auscultation
• Vernix caseosa appears
• Skin cells begin to be renewed
• Brown adipose tissue (BAT) forms
20–24 weeks
• Most organs functioning well
• Eyes complete
• Periods of sleep and activity
• Ear apparatus developing
• Responds to sound
• Skin red and wrinkled
• Surfactant secreted in the lungs from week 20
24–28 weeks
• Legally viable and survival may be expected if born
• Eyelids open
• Respiratory movements
28–32 weeks
• Begins to store fat and iron
• Testes descend into scrotum
• Lanugo disappears from face
• Skin becomes paler and less wrinkled 32–36 weeks
• Weight gain 25 g/day
• Increased fat makes the body more rounded
• Lanugo disappears from body
• Hair on fetal head lengthens
• Nails reach tips of fingers and toes
• Ear cartilage soft
• Plantar creases visible.
36 weeks to birth
• Birth is expected
• Body round and plump
• Skull formed but soft and pliable
Self-assessment 1.5
a. Describe the Amnion and chorion and their specific characteristics.b. How many arteries and vein does the umbilical cord contain.
1.6 Development of Placenta and functionsLearning Activity 1.6
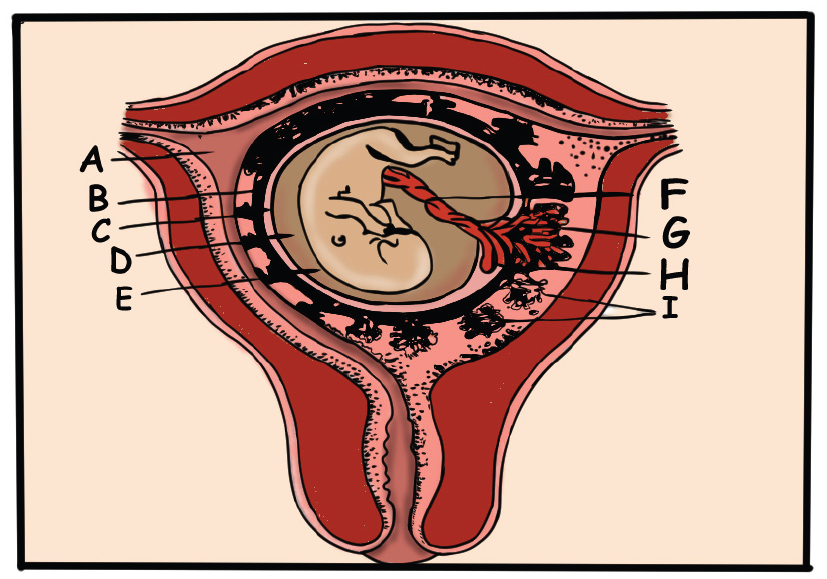
On the above diagram, show the structure of foetal membranes and the placenta
Development of placenta:
The human placenta develops from the trophectoderm (TE), the outer layer of the
pre-implantation embryo, which forms at 5 days’ post fertilization. At this stage, the
pre-implantation embryo (termed a blastocyst) is segregated into two lineages: theinner cell mass (ICM) and the trophectoderm.
Structure
The placenta begins to form at implantation. During the third week after conception
the trophoblast cells of the chorionic villi continue to invade the decidua basalis. As
the uterine capillaries are tapped, the endometrial spiral arteries fill with maternal
blood.
The placenta functions as a means of metabolic exchange. Exchange is minimal
at this time because the two cell layers of the villous membrane are too thick.
Permeability increases as the cytotrophoblast thins and disappears; by the fifth
month, only the single layer of syncytium is left between the maternal blood and thefetal capillaries.
Placenta at term
At term the placenta is discoid in shape, about 20 cm in diameter and 2.5 cm thick
at its centre and weighing approximately 470 g, which is directly proportional to the
weight of the fetus. The weight of the placenta may be affected by physiological
or active management of the third stage of labour owing to the varying amounts of
fetal blood retained in the vessels. The placenta is no longer routinely weighed in
clinical practice; however, some maternity units may do so as part of clinical trialsand research activities.
The maternal surface of the placenta (i.e. the basal plate) is dark red in colour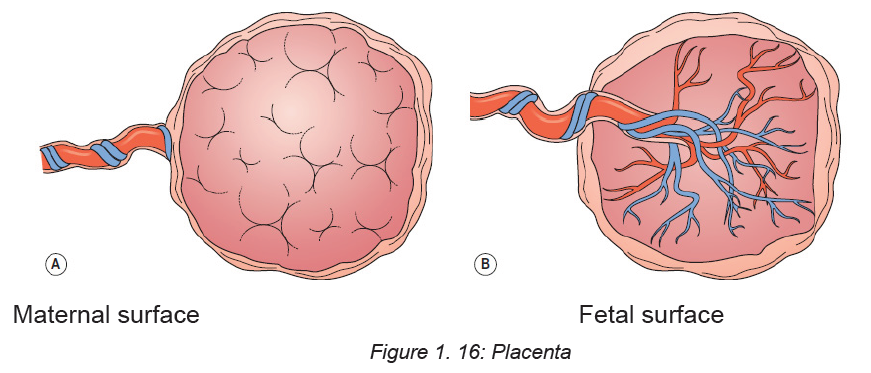
due to maternal blood and partial separation of the basal decidua. The surface is
arranged in up to 40 cotyledons (lobes), which are separated by sulci (furrows),
into which the decidua dips down to form septa (walls). The cotyledons are made
up of lobules, each of which contains a single villus with its branches. Sometimes
deposits of lime salts may be present on the surface, making it slightly gritty. This
has no clinical Significance.
The fetal surface of the placenta (i.e. the chorionic plate) has a shiny appearance
due to the amnion covering it.
Branches of the umbilical vein and arteries are visible, spreading out from the
insertion of the umbilical cord, which is normally in the centre. The amnion can be
peeled off the surface of the chorion as far back as the umbilical cord, whereas the
chorion, being derived from the same trophoblastic layer as the placenta, cannot
be separated from it.
Functions
The placenta performs a variety of functions for the developing fetus which can bedetermined by the mneumonic SERPENT
Storage
The placenta metabolizes glucose, stores it in the form of glycogen and reconverts
it to glucose as required. It can also store iron and the fat-soluble vitamins.
Endocrine
The many and varied endocrine functions of the placenta are complex, requiring
maternal and fetal input. Both types of trophoblasts produce steroidal hormones
(oestrogens and progesterone) in addition to many placental protein hormones
necessary for pregnancy.
Steroid hormones
There are three important oestrogens: oestrone, oestradiol and oestriol. Both
maternal and fetal adrenal production provide precursors for oestrogen production
by the placenta.
Protein hormones
Human chorionic gonadotrophin (hCG) is produced under the influence of placental
gonadotrophic releasing hormone (GnRH) by the trophoblasts.
Respiration
Gaseous exchange to and from the fetus occurs as a result of diffusion. Transfer
of gases is assisted by a slight maternal respiratory alkalosis in pregnancy. The
fetal hemoglobin level is high in utero to facilitate transport of gases. The fetal
hemoglobin also has a high affinity for oxygen.
Protection
The placenta provides a limited barrier to infection. Few bacteria can penetrate with
the exception of the treponema of syphilis and the tubercle bacillus. However, many
types of virus can penetrate the placental barrier, such as human immunodeficiency
virus (HIV), hepatitis strains, human cytomegalovirus (CMV) and rubella. In addition
to this, some parasitic and protozoal diseases, such as malaria and toxoplasmosis,
will cross the placenta.
The placenta filters substances of a high molecular weight therefore some drugs
and medicines may transfer to the fetus.
Immunoglobulins will be passed from mother to fetus transplacentally in late
pregnancy, providing about 6–12 weeks’ naturally acquired passive immunity to the
baby. In the case of Rhesus disease, if sensitization occurs and fetal blood cells
enter the maternal circulation, responding antibodies produced by the mother may
cross the placenta and destroy fetal surface antigens and consequently fetal cells,
causing haemolysis, hydrops fetalis and potential fetal demise.
Excretion
The main substance excreted from the fetus is carbon dioxide. Bilirubin will also
be excreted as red blood cells are replaced relatively frequently. There is very little
tissue breakdown apart from this and the amounts of urea and uric acid excreted
are very small.
Nutrition
The fetus requires nutrients for its ongoing development, such as amino acids and
glucose which are required for growth and energy, calcium and phosphorus for
bones and teeth, and iron and other minerals for blood formation. These nutrients
are actively transferred from the maternal to the fetal blood through the walls of the
villi.
The placenta is able to select those substances required by the fetus, even depleting
the mother’s own supply in some instances. Water, vitamins and minerals also pass
to the fetus. Fats and fat-soluble vitamins (A, D and E) cross the placenta only with
difficulty and mainly in the later stages of pregnancy. Some substances, including
amino acids, are found at higher levels in the fetal blood than in the maternal blood.
Transfer of substances
Substances transfer to and from the fetus by a variety of transport mechanisms, as
stated below:
♦ Simple diffusion of gases and lipid soluble substances.
♦ Water pores transfer water-soluble substances as a result of osmotic and
potentially hydrostatic forces.
♦ Facilitated diffusion of glucose using carrier proteins.
♦ Active transport against concentration gradients of ions, calcium (Ca) and
phosphorus (P).♦ Endocytosis (pinocytosis) of macromolecules
Self-assessment 1.6
1. A natural cleavage plane between the placenta and the uterine wall is formed
when the cotyledons of the maternal surface of the placenta extend into the:
a. Myometrium
b. Uterine wall
c. Decidua’s basalis
d. Amniotic membrane
2. Which of the following is the portion of the placenta that is contributed by the
embryo?
a. Chorion
b. Yolk sac
c. Amnion
d. Allantois
3. Which of the following blood vessels transports blood rich in oxygen and
nutrients to the fetus?
e. Ductus arteriosus
f. Ductus venosus
g. Umbilical vein
h. Umbilical artery4. What are the nutritive and protective functions of the placenta?
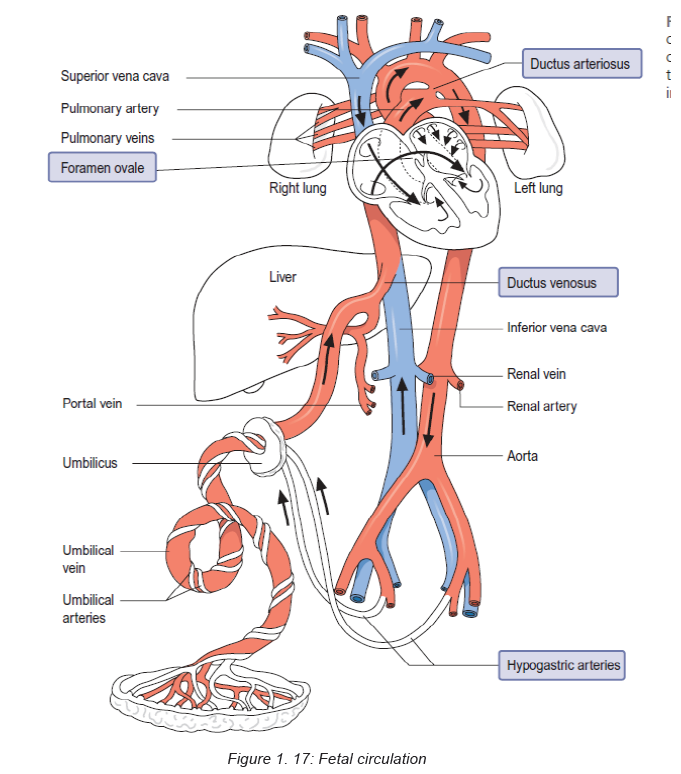
1.7 Fetal circulationLearning Activity 1.7
Blood circulation in fetuses is done to avail oxygen and nutrients for body use
and remove waste products. Based on the competences developed in senior 3,
please brainstorm on how fetal circulation is done.
The placenta is the source of oxygenation, nutrition and elimination of waste for the
fetus. There are several temporary structures in addition to the placenta and the
umbilical cord that enable the fetal circulation to occur. These include:
♦ The ductus venosus, which connects the umbilical vein to the inferior vena
cava.
♦ The foramen ovale, which is an opening between the right and left atria.
♦ The ductus arteriosus, which leads from the bifurcation of the pulmonary
artery to the descending aorta.
♦ The hypogastric arteries, which branch off from the internal iliac arteries and
become the umbilical arteries when they enter the umbilical cord. The fetal
circulation takes the following course:
Oxygenated blood from the placenta travels to the fetus in the umbilical vein. The
umbilical vein divides into two branches – one that supplies the portal vein in the
liver, the other anastomosing with the ductus venosus and joining the inferior vena
cava. Most of the oxygenated blood that enters the right atrium passes across the
foramen ovale to the left atrium, which mixes with a very small amount of blood
returning from the lungs from where it passes into the left ventricle via the bicuspid
valve, and then the aorta. The head and upper extremities receive approximately
50% of this blood via the coronary and carotid arteries, and the subclavian arteries
respectively. The rest of the blood travels down the descending aorta, mixing with
deoxygenated blood from the right ventricle via the ductus arteriosus.
Deoxygenated blood collected from the head and upper parts of the body returns to
the right atrium via the superior vena cava. Blood that has entered the right atrium
from the superior vena cava enters at a different angle to the blood that enters from
the inferior vena cava and heads towards the foramen ovale. Hence there are two
distinct blood flows entering the right atrium. Most of the lesser oxygenated blood
entering the right atrium from the superior vena cava passes behind the flow of
highly oxygenated blood going to the left atrium and enters the right ventricle via
the tricuspid valve. There is a small amount of blood mixing where the two blood
flows meet in the atrium. From the right ventricle a little blood travels to the lungs
in the pulmonary artery, for their development. Most blood, however, passes from
the pulmonary artery through the ductus arteriosus into the descending aorta. This
blood, although low in oxygen and nutrients, is sufficient to supply the lower body
of the fetus. It is also by this means that deoxygenated blood travels back to the
placenta via the internal iliac arteries, which lead into the hypogastric arteries, and
ultimately into the umbilical arteries. This circulation means that the fetus has a
well oxygenated and perfused head, brain and upper body compared to its lowerextremities.
Self-assessment activity 1.7
a. Differentiate ductus venosus from ductus arteriosusb. What are temporary structures formed during intra-uterine life?
1.8 Characteristics of a normal pregnancyLearning Activity 1.8
A 27 years old married lady is accompanied by her husband to the health center
to get medical care. She presents the signs and symptoms of nausea and
vomiting every morning in the last 4 days, pain in lower abdomen and nausea,
mood changes and selection of food. She also reported to have missed her
periods for the last two months. She states that she treated herself for malaria
last three months
Use the knowledge of S3 biology on the topic of pregnancy to recall the signs ofpregnancy in woman who is pregnant.
Pregnancy is a time of profound physical, physiological and psychological change.
In addition to the reproductive organs, all maternal physiologic systems make
adaptions needed to support the developing fetus and, at the same time, maintain
maternal homeostasis.
1.8.1 Physical and physiological characteristics of a normal
pregnancy
Some pregnant women experience a lot of physical changes and others
only a few.
♦ Aches and pain (possibly in your lower abdomen and in your joints)
♦ Morning sickness which may be nausea or actual vomiting, and does not just
happen in the morning
♦ Food cravings and aversions
♦ Heartburn and indigestion
♦ Constipation
♦ A need to urinate more often
♦ Skin change and itching and possibly skin tags.
♦ Larger and tender breasts.
1.8.2 Psychological characteristics of a normal pregnancy
Pregnancy is always associated with changes in the psychological functioning of
pregnant women. It is usually associated with ambivalence, frequent mood changes,
varying from anxiety, fatigue, exhaustion, sleepiness, depressive reactions to
excitement. During pregnancy, changes include body appearance, affectivity and
sexuality, whereas the position and role of women attains a new quality. Even
thoughts of pregnancy can bring about numerous worries about its course and
outcome, and especially of the delivery itself, which may be so intense that they
acquire a feature of phobia (which may be the reason for avoiding pregnancy).
Pregnancy as a stressful event: Pregnancy is identified as a potent stressor
that can seriously affect the psychic status of pregnant women, perinatal outcome,
but also psychic functioning of the new-born individual. Appropriate relationship
of partners and support of the society play an important role in overcoming stress
during pregnancy.
Conclusion: Pregnancy is an event that involves numerous somatic and
psychological changes. However, pregnancy can also be a potent stressor.
Existence of prenatal maternal stress may lead to different perinatal complications
that may have long-term consequences on the newborn. In prevention of maternal
stress emphasis has to be put on partner’s emotional support, as well as empathy of
the social environment. However, in certain cases, professional psychotherapeutic
support is necessary, in form of short supportive treatment. Preventive measures
should include adequate psychological support during pregnancy, especially the
first one, provided for all pregnant women, but also for those women that plan toget pregnant in the near future.
Self-assessment 1.8
Discuss the psychological characteristics of pregnancy
Learning Activity 1.9
A 16 years old boy who study science subjects including biology in S3 comes
home for holiday and realizes that his mother who is 30 weeks pregnant had an
accident which affected her pelvic bone thereby leading to unsteady gait when
walking as the pregnancy progresses. During interview with the mother states
that she feels more pain on her back as the pregnancy progress and difficulty
to stand straight. The child is concerned with the long-term effects that this gait
deviation will have on his mother’s vertebra column especially now that the
mother is pregnant.
a. Based on your knowledge and understanding of biology in S3
What is pelvis?
b. Which body part do you think might be an underlying cause of this gaitpattern?
Pregnancy and its changes is a normal physiological process that happens in all
mammalian in response to the development of the fetus. These changes happen in
response to many factors; hormonal changes, increase in the total blood volume,
weight gain, and increase in fetus size. All these factors have a physiological impact
on all systems of the pregnant woman; musculoskeletal, endocrine, reproductive
system, cardiovascular, respiratory, gastrointestinal system, and renal changes.1.9.1 Anatomy background of pelvis
♦ The pelvis is the region found between the trunk and lower limbs.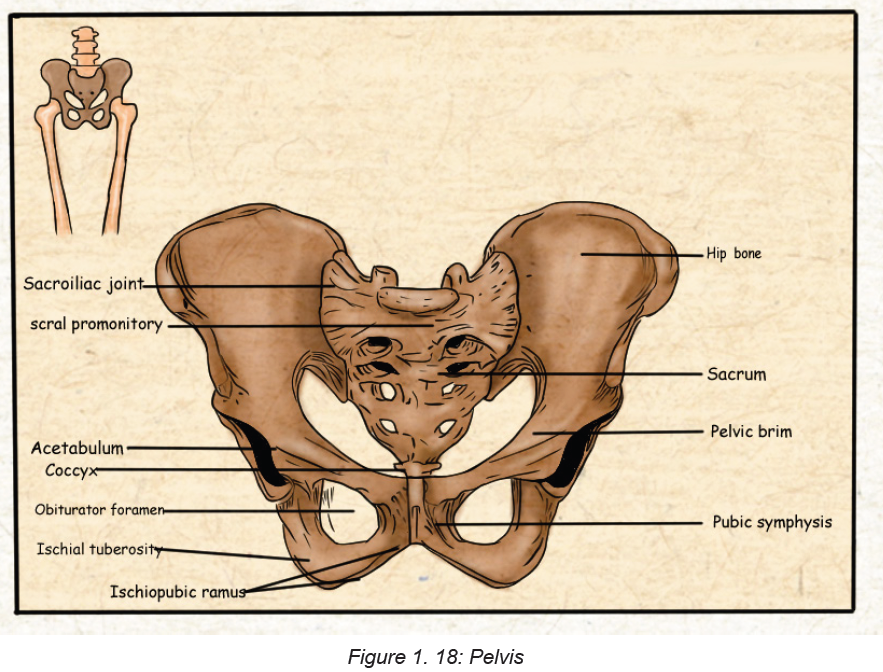
♦ In females, the pelvis is wider and lower than that of their male counterpart,
making it more suited to accommodate a fetus during both pregnancy and
delivery.
♦ It protects and supports the pelvic contents, provides muscle attachment and
facilitates the transfer of weight from trunk to legs in standing, and to the
ischial tuberosities in sitting.
♦ The cross-sectional anatomy of the female pelvis shows five bones: two hip
bones, sacrum, coccyx, and two femurs The joints are supported by some of
the strongest ligaments in the body which become laxer during pregnancy
leading to increased joint mobility and less efficient load transfer through the
pelvis.
♦ The pelvic outlet at the base of the pelvis is narrower in its transverse
diameter when compared with the pelvic inlet; it comprises the pubic arch,
ischial spines, sacrotuberous ligaments, and coccyx.
♦ Four pairs of abdominal muscles combine to form the anterior and lateral
abdominal wall and may be termed the abdominal corset.
♦ Transversus abdominis lies deep to the internal abdominal oblique and
external abdominal oblique with the rectus abdominis central, anterior and
superficial abdominal oblique, external oblique and transversus abdominis
insert into an aponeurosis joining in the midline at the linea alba. The deep
abdominal muscles, together with the pelvic floor muscles, multifidus, and
diaphragm, can be considered as a complete unit and may be termed the
lumbopelvic cylinder. This provides support for the abdominal contents and
maintains intraabdominal
pressure.
♦ Organs of the female reproductive system present in the pelvis are subdivided
into internal and external genitalia.
1.9.2 Types of pelvis
The pelvis is a group of bones located in the lower part of torso, between the lower
back and thighs. The shape of the pelvis often differs between males and females.
There are four main types of pelvis:
a. Gynecoid. This is the most common type of pelvis in females and is generally
considered to be the typical female pelvis. Its overall shape is round, shallow,
and open.
b. Android. This type of pelvis bears more resemblance to the male pelvis. It’s
narrower than the gynecoid pelvis and is shaped more like a heart or a wedge.
c. Anthropoid. An anthropoid pelvis is narrow and deep. Its shape is similar to
an upright egg or oval.
d. Platypelloid. The platypelloid pelvis is also called a flat pelvis. This is the least
common type. It’s wide but shallow, and it resembles an egg or oval lying onits side.
Table 1. 1: Types of pelvis
Pelvis shape can vary greatly among females around the world.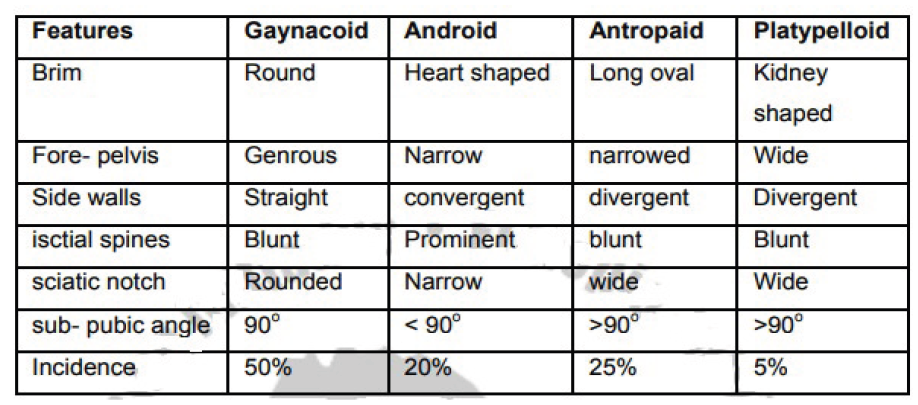
1.9.3 Pelvis in relation to pregnancy and child birth
The term pelvis is applied to the skeletal ring formed by the innominate bones and
the sacrum, the cavity within and even the entire region where the trunk and the
lower limb meet. The pelvis is divided by an oblique plane which passes through
the prominence of the sacrum, the arcuate line (the smooth rounded border on the
internal surface of the ilium), the pectineal line (a ridge on the superior ramus of
the pubic bone) and the upper margin of the symphysis pubis, into the true and the
false pelvis.
a. THE TRUE PELVIS: The true pelvis is the bony canal through which the fetus
must pass during birth. It is divided into a brim, a cavity and an outlet.
i. The pelvic brim:
The superior circumference forms the brim of the true pelvis; the included
space being called the inlet. The brim is round except where the sacralpromontory projects into it.
There are fixed points on the pelvic brim that are known as its landmarks.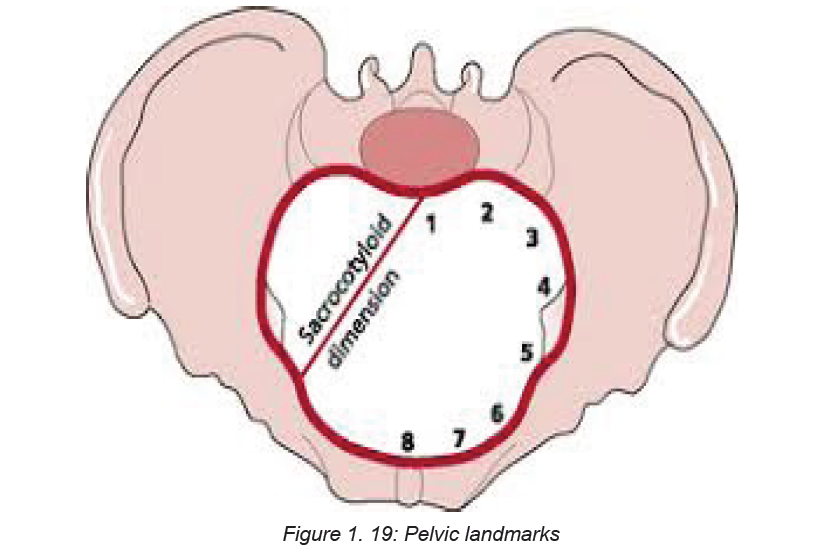
Commencing posteriorly, there are:
♦ Sacral promontory (1)
♦ Sacral ala or wing (2)
♦ Sacroiliac joint (3)
♦ Iliopectineal line, which is the edge formed at the inward aspect of the ilium(4)
♦ Iliopectineal eminence, which is a roughened area formed where the superior
ramus of the pubic bone meets the ilium (5).
♦ Superior ramus of the pubic bone (6)
♦ Upper inner border of the body of the pubic bone (7)
♦ Upper inner border of the symphysis pubis (8)
ii. The pelvic cavity:
The cavity of the true pelvis extends from the brim superiorly to the outlet inferiorly.
The anterior wall is formed by the pubic bones and symphysis pubis and its depth
is 4 cm. The posterior wall is formed by the curve of the sacrum which is 12 cm in
length. Because there is such a difference in these measurement, the cavity forms
a curved canal.
The cavity contains the pelvic colon, rectum, bladder and some of the reproductive
organs. The rectum is placed posteriorly, in the curve of the sacrum and coccyx, the
bladder is anterior behind the symphysis pubis.
iii. The pelvic outlet:
The lower circumference of the true pelvis is very irregular, the space enclosed by
it is called the outlet. Two outlets are described: the anatomical and the obstetrical.
The anatomical outlet is formed by the lower borders of each of the bones together
with the sacrotuberous ligament. The obstetrical outlet is of greater practical
significance because it includes the narrow pelvic strait through which the fetus
must pass. The obstetrical outlet is the space between the narrow pelvic strait and
the anatomical outlet. This outlet is diamond-shaped.
b.THE FALSE PELVIS: It is bounded posteriorly by the lumbar vertebrae and
laterally by the iliac fossae, and in front by the lower portion of the anterior abdominal
wall. The false pelvis varies considerably in size according to the flare of the iliacbones. However, the false pelvis has no significance in midwifery.
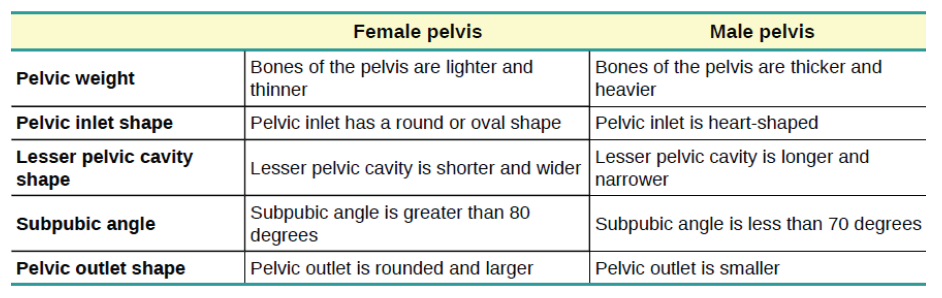
Table 1. 2: Differences between the Female and Male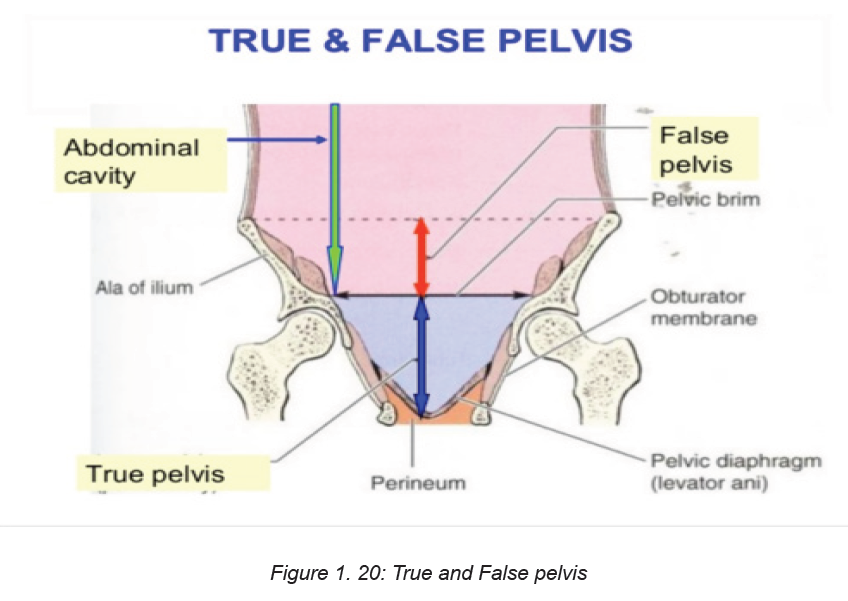
Pelvis
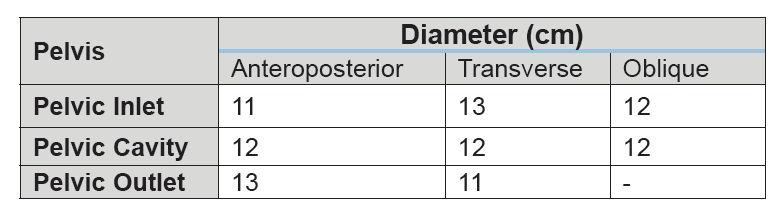
1.9.4 Pelvic diameters
Knowledge of the diameters of the normal female pelvis is essential in the practice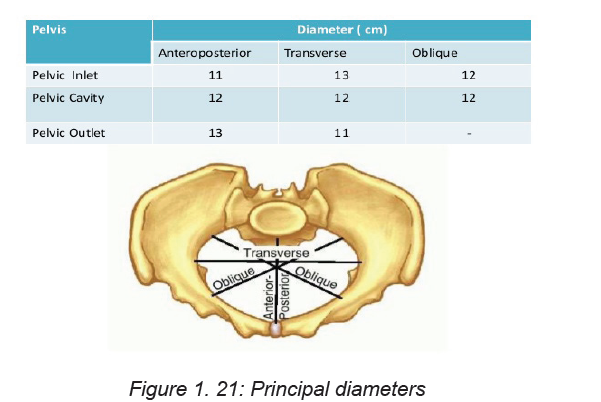
of midwifery because contraction of any of them can result in malposition or
malpresentation of the presenting part of the fetus.
Diameters of the pelvic inlet
The brim has four principal diameters: the anteroposterior diameter, the
transverse diameter and the two oblique diameters. The anteroposterior or
conjugate diameter extends from the midpoint of the sacral promontory to the upper
border of the symphysis pubis. Three conjugate diameters can be measured: the
anatomical (true) conjugate, the obstetrical conjugate and the internal or diagonal
conjugate The anatomical conjugate, which averages 12 cm, is measured from the
sacral promontory to the uppermost point of the symphysis pubis. The obstetrical
conjugate which averages 11 cm, is measured from the sacral promontory to the
posterior border of the upper surface of the symphysis pubis. This represents the
shortest anteroposterior diameter through which the fetus must pass and is hence
of clinical significance to midwives. The obstetrical conjugate cannot be measured
with the examining fingers or any other technique.
The diagonal conjugate is measured anteroposteriorly from the lower border of the
symphysis to the sacral promontory.
The transverse diameter is constructed at right-angles to the obstetric conjugate
and extends across the greatest width of the brim; its average measurement is
about 13 cm. Each oblique diameter extends from the iliopectineal eminence of one
side to the sacroiliac articulation of the opposite side; its average measurement is
about 12 cm.
Each takes its name from the sacroiliac joint from which it arises, so the left oblique
diameter arises from the left sacroiliac joint and the right oblique from the right
sacroiliac
joint. Another dimension, the sacrocotyloid, passes from the sacral promontory to
the iliopectineal eminence on each side and measures 9–9.5 cm. Its importance is
concerned with posterior positions of the occiput when the parietal eminences of
the fetal head may become caught.
Diameters of the cavity
The cavity is circular in shape and although it is not possible to measure its diameters
exactly, they are all considered to be 12 cm.
Diameters of the outlet
The outlet, which is diamond-shaped, has three diameters: the anteroposterior
diameter, the oblique diameter and the transverse diameter. The anteroposterior
diameter extends from the lower border of the symphysis pubis to the sacrococcygeal
joint. It measures 13 cm; as the coccyx may be deflected backwards during labour,
this diameter indicates the space available during birth. The oblique diameter,
although there are no fixed points, is said to be between the obturator foramen
and the sacrospinous ligament. The measurement is taken as being 12 cm. The
transverse diameter extends between the two ischial spines and measures 10–11
cm. It is the narrowest diameter in the pelvis. The plane of least pelvic dimensions
is said to be at the level of the ischial spines.
Orientation of the pelvis
In the standing position, the pelvis is placed such that the anterior superior iliac
spine and the front edge of the symphysis pubis are in the same vertical plane,
perpendicular to the floor. If the line joining the sacral promontory and the top of
the symphysis pubis were to be extended, it would form an angle of 60° with the
horizontal floor. Similarly, if a line joining the centre of the sacrum and the Centre of
the symphysis pubis were to be extended, the resultant angle with the floor would
be 30°. The angle of inclination of the outlet is 15°. When in the recumbent position,
the same angles are made as in the vertical position; this fact should be kept in
mind when carrying out an abdominal examination.
Pelvic planes
Pelvic planes are imaginary flat surfaces at the brim, cavity and outlet of the pelvic
canal at the levels of the lines described above.
Axis of the pelvic canal
A line drawn exactly half-way between the anterior wall and the posterior wall of the
pelvic canal would trace a curve known as the curve of Carus. The midwife needs
to become familiar with this concept in order to make accurate observations on
vaginal examination and to facilitate the birth of the baby.Table 1. 3: Summary of pelvic diameters
Self-assessment activity 1.9
1. What is the narrowest diameter for the fetus to pass through?
2. Which of the following statements is false? In each case, say why it is
incorrect.
a. The female bony pelvis is broader and flatter than the male pelvis.
b. The pelvic inlet is narrower than the pelvic outlet.
c. The iliac crest is an important landmark in measuring the progress of the
fetus down the birth canal.
d. The sutures in the fetal skull are strong hard joints that hold the skull bones
rigidly in place.e. A newborn baby’s pulse can be seen beating in the anterior fontanel.
Match the terms with the appropriate explanation
1.10 The fetal skull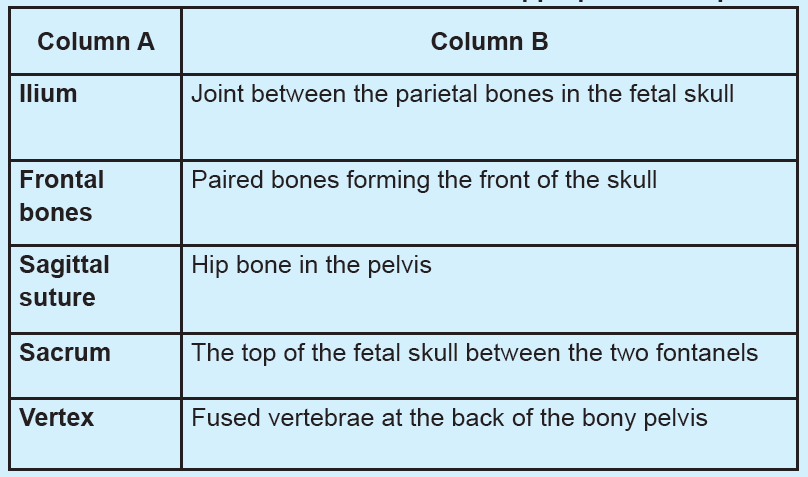
Learning Activity 1.10
Study the following structure of the fetal skull, a bony structure that protects thebrain:
1. Describe the above structure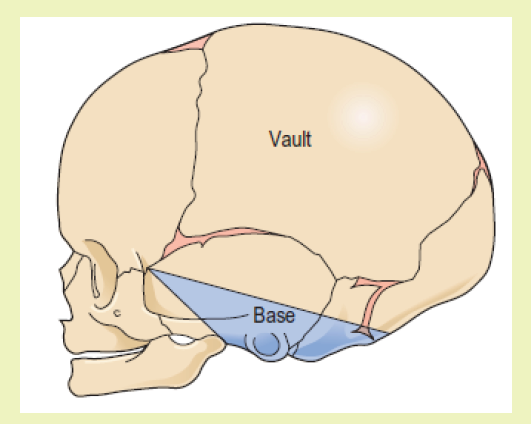
2. Predict how the fetal skull protects the brain in fetuses.
The fetal head is large in relation to the fetal body compared with the adult.
Additionally, it is large in comparison with the maternal pelvis and is the largest part
of the fetal body to be born. Adaptation between the skull and the pelvis is necessary
to allow the head to pass through the pelvis during labour without complications.
The bones of the vault are thin and pliable, and if subjected to great pressure
damage to the underlying delicate brain may occur.
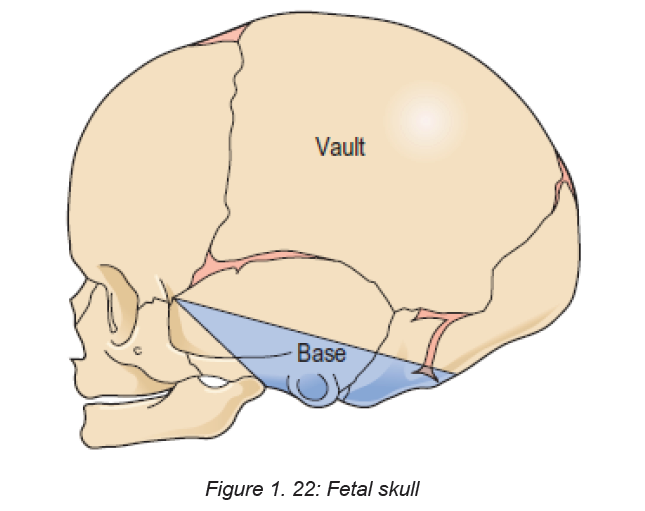
1.10.1 Divisions of the fetal skull
The skull is divided into the vault, the base and the face. The vault is the large,
dome-shaped part above an imaginary line drawn between the orbital ridges and
the nape of the neck. The base comprises bones that are firmly united to protect
the vital centres in the medulla oblongata. The face is composed of 14 small bonesthat are also firmly united and non-compressible.
1.10.2 Bones of the vault
The bones of the vault are laid down in membrane. They harden from the centre
outwards in a process known as ossification. Ossification is incomplete at birth,
leaving small gaps between the bones, known as the sutures and fontanelles. The
ossification centre on each bone appears as a protuberance. Ossification of the
skull is not complete until early adulthood. The bones of the vault consist of:
The occipital bone, which lies at the back of the head. Part of it contributes to the
base of the skull as it contains the foramen magnum, which protects the spinal cord
as it leaves the skull. The ossification centre is the occipital protuberance.
♦ The two parietal bones, which lie on either side of the skull. The ossification
centre of each of these bones is called the parietal eminence.
♦ The two frontal bones, which form the forehead or sinciput. The ossification
centre of each bone is the frontal eminence. The frontal bones fuse into a
single bone by eight years of age.
♦ The upper part of the temporal bone on both sides of the head forms part ofthe vault.
1.10.3 Regions of landmarks’ diameters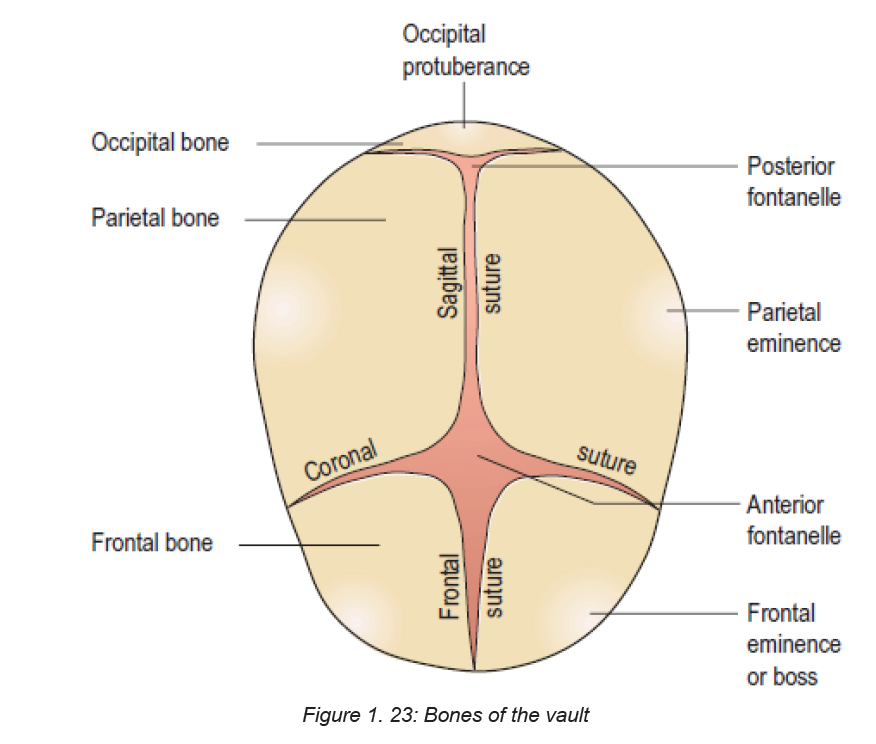
The skull is further separated into regions, and within these there are important
landmarks. These landmarks are useful to the midwife when undertaking a vaginal
examination as they help ascertain the position of the fetal head. The occiput region
lies between the foramen magnum and the posterior fontanelle. The part below the
occipital protuberance (landmark) is known as the sub-occipital region.
The vertex region is bounded by the posterior fontanelle, the two parietal eminencesand the anterior fontanelle.
The forehead /sinciput region extends from the anterior fontanelle and the coronal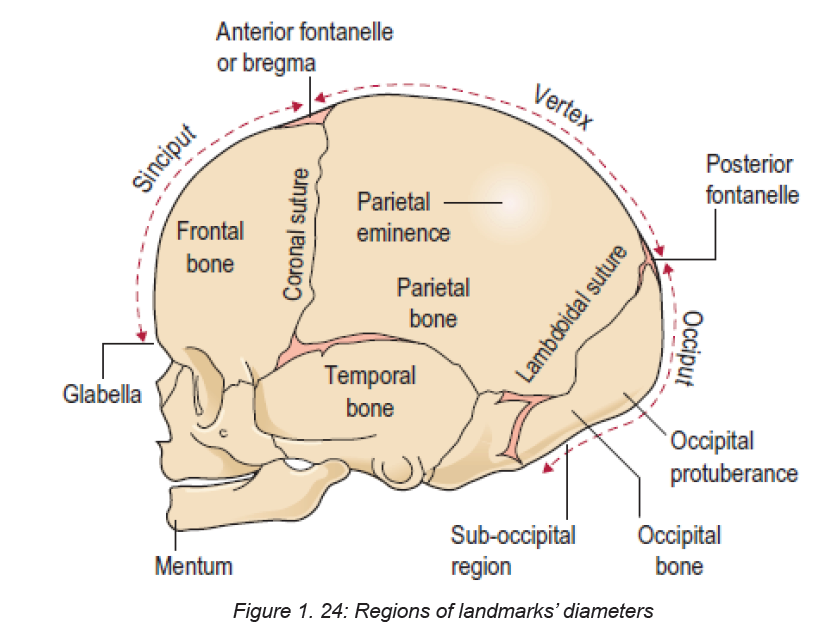
suture to the orbital ridges.
The face extends from the orbital ridges and the root of the nose to the junction of
the chin or mentum (landmark) and the neck. The point between the eyebrows is
known as the glabella.
1.10.4 Sutures and fontanels
The sutures are the cranial joints formed where two bones meet. Where two or
more sutures meet, a fontanelle is formed. The sutures and fontanelles described
below permit a degree of overlapping of the skull bones during labour, which is
known as moulding.
♦ The lambdoidal suture separates the occipital bone from the two parietal
bones.
♦ The sagittal suture lies between the two parietal bones.
♦ The coronal suture separates the frontal bones from the parietal bones,passing from one temple to the other.
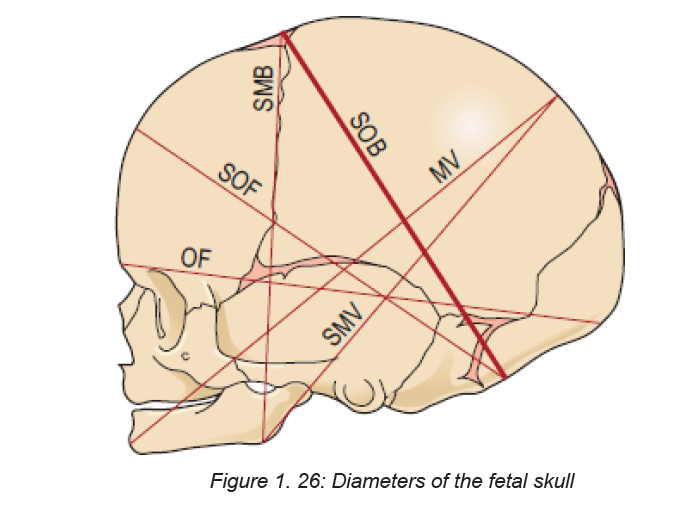
1.10.5 Diameters of the fetal skull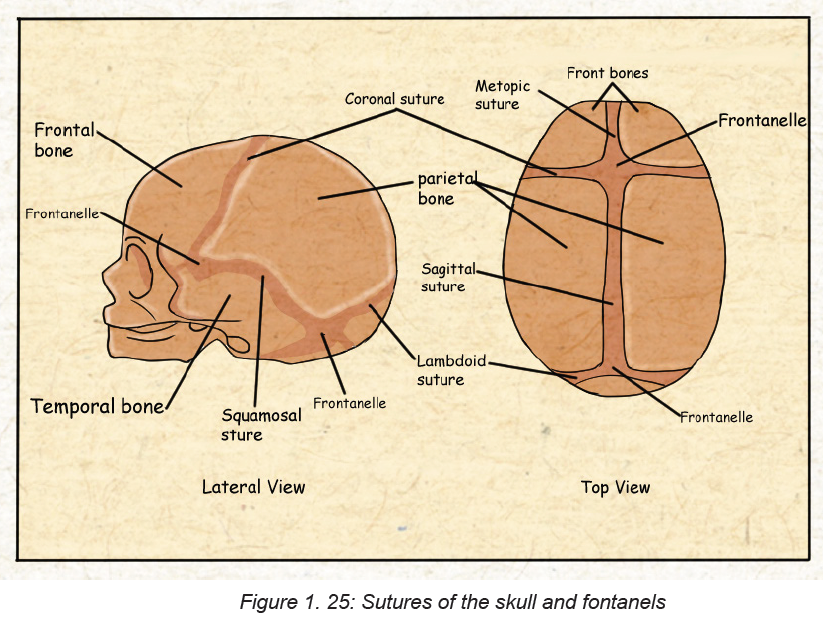
Knowledge of the diameters of the skull alongside the diameters of the pelvis allows
the midwife to determine the relationship between the fetal head and the mother’s
pelvis. There are six longitudinal diameters.
The longitudinal diameters are:
♦ The sub-occipito bregmatic (SOB) diameter (9.5 cm) measured from below
the occipital protuberance to the centre of the anterior fontanelle or bregma.
♦ The sub-occipitofrontal (SOF) diameter (10 cm) measured from below the
occipital protuberance to the centre of the frontal suture.
♦ The occipitofrontal (OF) diameter (11.5 cm) measured from the occipital
protuberance to them glabella.
♦ The mentovertical (MV) diameter (13.5 cm) measured from the point of the
chin to the highest point on the vertex.
♦ The sub-mentovertical (SMV) diameter (11.5 cm) measured from the point
where the chin joins the neck to the highest point on the vertex
♦ The sub-mentobregmatic (SMB) diameter (9.5 cm) measured from the pointwhere the chin joins the neck to the centre of the bregma (anterior fontanelle).
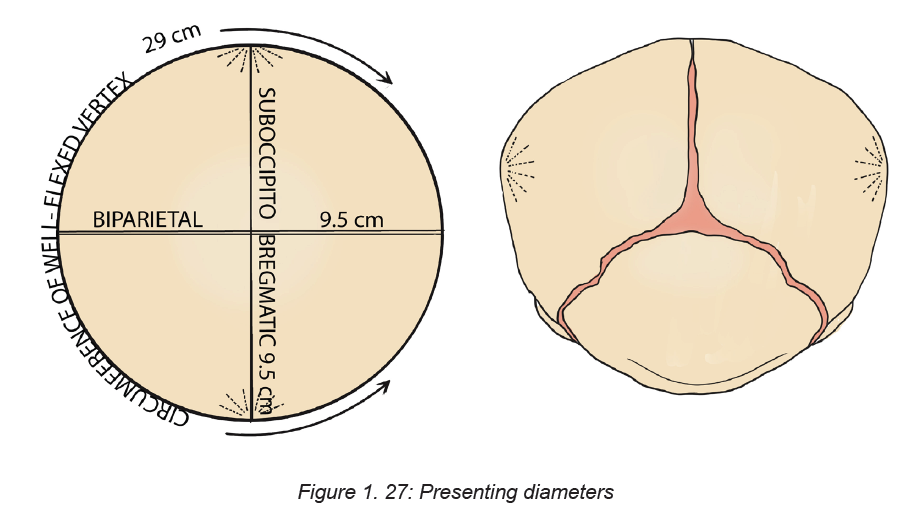
Presenting diameters
Some presenting diameters are more favourable than others for easy passage
through the maternal pelvis and this will depend on the attitude of the fetal head.
This term attitude is used to describe the degree of flexion or extension of the
fetal head on the neck. The attitude of the head determines which diameters will
present in labour and therefore influences the outcome. The presenting diameters
of the head are those that are at right-angles to the curve of Carus of the maternal
pelvis. There are always two: a longitudinal diameter and a transverse diameter.
The presenting diameters determine the presentation of the fetal head, for which
there are three:
1. Vertex presentation. When the head is well flexed the sub-occipitobregmatic
diameter (9.5 cm) and the biparietal diameter (9.5 cm) present.
As these two diameters are the same length the presenting area is circular, which is
the most favourable shape for dilating the cervix and birth of the head. The diameter
that distends the vaginal orifice is the sub-occipitofrontal diameter (10 cm). When
the head is deflexed, the presenting diameters are the occipitofrontal (11.5 cm) and
the biparietal (9.5 cm). This situation often arises when the occiput is in a posterior
position. If it remains so, the diameter distending the vaginal orifice will be the
occipitofrontal (11.5 cm).
2. Face presentation. When the head is completely extended the presenting
diameters are the submentobregmatic (9.5 cm) and the bitemporal (8.2 cm). The
sub-mentovertical diameter (11.5 cm) will distend the vaginal orifice.
3. Brow presentation. When the head is partially extended, the mentovertical
diameter (13.5 cm) and the bitemporal diameter (8.2 cm) present. If this presentationpersists, vaginal birth is unlikely.
Self-assessment activity 1.10
– Explain the role of the sutures and fontanelles during child birth
– State the six longitudinal diameters of the fetal skull.
Identify the three major types of head presentation of the fetus?– Identify the three major types of head presentation of the fetus?
End unit assessment
1. What is fertilization?
2. How long does the process of fertilization take? And at which portion of the
fallopian tube does fertilization take place.
3. What is the main function of the uterus during pregnancy?
4. Describe the major phases of spermatogenesis?
5. Describe the process of capacitation
6. Give the differences between spermatogenesis and oogenesis
7. Give the differences between spermatogenesis and oogenesis
8. Define the following terms:
– Trophoblast
– Embryoblast
– Blastocyst
9. Zygote Describe the factors that can affect fertilization
10. Explain the term “implantation”, what condition favors successful
implantation
11. What are the functions of the amniotic fluid during pregnancy?
12. In relation to embryology and fetal development, explain which organs
forms at 4-8 weeks of pregnancy
13. What is a placenta? And how does it form in embryological stage
14. Describe the functions of the placenta
15. What are the differences between the female and male pelvis.
16. List eight fixed points on the pelvic brim?
17. What is the primary role of the female pelvis?
18. Which type of pelvis is adequate for a normal child birth and why?
19. What is the largest part of the fetal fetus?
20. Explain the sutures and bones of the fetal head and the role they play in
childbirth.
21. What are the temporary structures in addition to the placenta and umbilical
cord that enables fetal circulation?
22. Describe the physical and physiological characteristics of a normal
pregnancy
23. In a table format, show the different types of pelvis and their characteristics
24. Among the four types of pelvis which is more adaptable to child birth and
why?
25. What are the divisions of the pelvis?
26. What are the functions of the female pelvis?
27. List the land marks of the pelvic brim, cavity and outlet and relate their
relevance to child birth28. List the bones and sutures that make up the fetal head.
