UNIT 12:HUMAN REPRODUCTIVE SYSTEM, GAMETOGENESIS, PREGNANCY AND METHODS OF BIRTH CONTROL.
Key unit competence: Relate the structures of the human reproductive system to their functions and describe gamete formation and explain the role of hormones in human reproduction, stages of pregnancy, contraceptive methods and fetal development.
Introductory activity 12
Observe the photo below and answer the questions that follow:

a. The woman on the left side is pregnant. What do you think about the origin of the fetus in the womb of the pregnant woman?
b. Use the photo on the right side to make short notes on the embryonic development.
c. Use the photo and try to identify the parts of the female reproductive system and their functions.
d. The child on the photo is a boy. Can you identify the parts of the male reproductive system and their functions?
e. What do you think are the causes to the changes observed on the woman on the right side of the photo?
12.1 Male and female human reproductive systems
Activity 12.1
Aim: To dissect and identify structures of male and female reproductive system of rat.
Theory: The sex of the rat can be determined by looking for external testes and teats. Large testes are visible at the ventro-posterior side of the male rat and 6 pairs of teats ventrally in females. The major male reproductive organs of the male rat are the testes (singular: testis) which are located in the scrotal sac, along with internally placed duct systems and associated glands. Female reproductive system consists of a pair of ovaries, duct system and glands.
Procedure
• Obtain and sacrifice a rat. Place it in your dissecting tray with ventral side facing up so as to observe the external features and determine the sex of the rate you have taken.
• Examine the anal opening just posterior to the tail. Insert the scissor blades through the anus along the midline lifting the skin carefully so as not to damage the underlying organs.
In male rat, cut through the scrotum carefully to reveal the testis and also observe other internal structures: epididymis, vas deferens, seminal vesicles, prostate gland and seminiferous tubules.
In female rat, locate the urethral and vaginal openings on the ventro-posterior side of the body, under the tail, just posterior to the last pair of teats. Also, observe other reproductive organs: uterus, ovaries, oviducts and vagina.
Precautions
1. Be careful not to cut too deeply. Keep the tip of your scissors pointed upwards.
2. Always wear gloves and safety goggles when handling the rat to protect your hands and eye from chemical splattering or debris.
3. Once an incision is made, allow the rat to be drained off the fluid.
4. Handling and dissection of animals should be done in the presence of experts, following ethical guidelines.
Human beings reproduce by sexual means where the male and female involve in sexual intercourse, resulting in fertilization. During sexual intercourse, the interaction between the male and female reproductive systems results in fertilization of the woman’s ovum by the man’s sperm. The ovum and sperm are specialized reproductive cells called gametes, generated by a process called gametogenesis (i.e., spermatogenesis in males and oogenesis in females). The gametes are haploid in nature and it is when these two cells merge into one zygote cell that genetic recombination occurs and diploid condition is achieved back. After a gestation period, i.e., nine months in humans, childbirth takes place.
12.1.1 Sexual development in males
The main visible differences between boys and girls at birth are their reproductive organs. Of course, there are other differences between boys and girls at birth, but in this chapter, the focus is on their reproductive systems. As different as the male and female reproductive systems are at birth, they start out relatively similar. Before birth, the expression of genes on the male Y-chromosome brings about the differences.
Each testis contains more than 90 meters of tiny, tightly-packed tubes called seminiferous tubules. They are the functional units of the testes, where sperm are produced and testosterone is secreted.
In between the seminiferous tubules in the testes are interstitial cells, also called Cells of Leydig. These cells secrete testosterone. A high concentration of testosterone is necessary for sperm production. Testosterone is also needed throughout a man’s life to maintain his secondary sex characteristics. The seminiferous tubules join together to form the epididymis. The epididymis is a coiled tube about 6 meters long lying atop the testes inside the scrotum. Its functions are to help sperm mature and to store mature sperm until they leave the body.
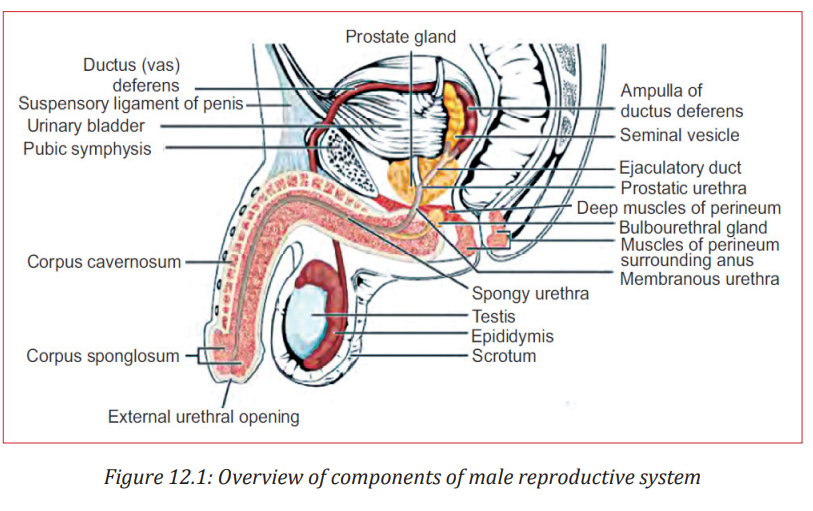
In addition to these organs, the male reproductive system consists of a series of ducts and glands.
Ducts include the vas deferens and ejaculatory ducts. They transport sperm from the epididymis to the urethra in the penis.
Glands include the seminal vesicles, prostate gland, and bulbourethral glands (also called Cowper’s glands). They secrete substances that become part of semen.
• Two seminal vesicles contribute about 60% of the volume of semen. The fluid from the seminal vesicles is thick, yellowish, and alkaline. It contains mucus, the sugar fructose (which provides most of the sperm’s energy), a coagulating enzyme, ascorbic acid, and local regulators called prostaglandins.
• The prostate gland secretes its products directly into the urethra through several small ducts. This fluid is thin and milky; it contains anticoagulant enzymes and citrate (a sperm nutrient). The prostate gland is the source of some of the most common medical problems of men over age 40. Benign (noncancerous) enlargement of the prostate occurs in more than half of all men in this age-group and in almost all men over 70. In addition, prostate cancer, which most often afflicts men 65 and older, is one of the most common human cancers.
• The bulbourethral glands are a pair of small glands along the urethra below the prostate. Before ejaculation, they secrete clear mucus that neutralizes any acidic urine remaining in the urethra. Bulbourethral fluid also carries some sperm released before ejaculation, which is one reason for the high failure rate of the withdrawal method of birth control (coitus interruptus).
Semen is the fluid that is ejaculated from the urethra. Semen contains secretions from the glands as well as sperm. The secretions control pH and provide the sperm with nutrients for energy.
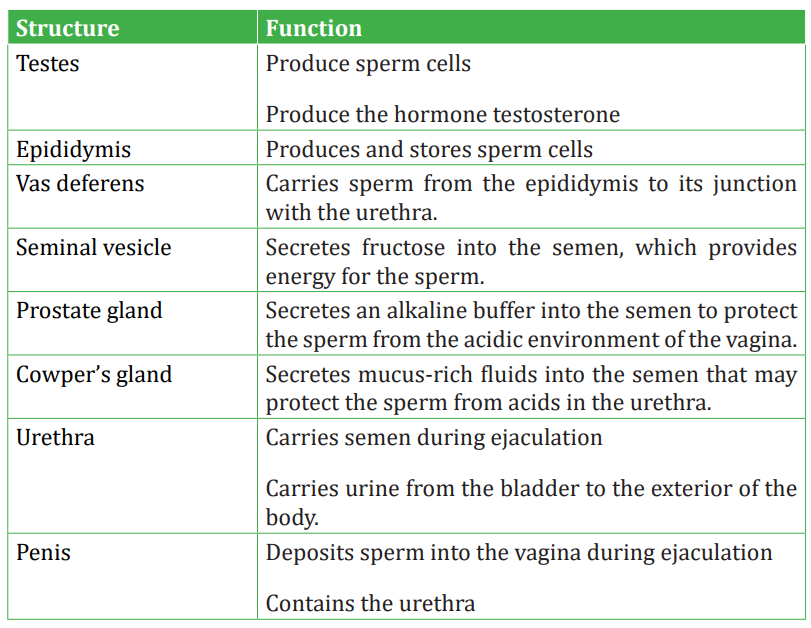
Table 12.1: Parts of the male reproductive system and their functions
12.1.2 Female reproductive system
The female reproductive system is a collection of organs and other structures located primarily in the pelvic region. Most of the structures are inside the body. The female reproductive system has several functions:
• Producing eggs, which are female gametes
• Secreting female sex hormones
• Receiving sperm during sexual intercourse
• Supporting the development of a fetus
• Delivering a baby during birth
• Breastfeeding a baby after birth During puberty, a girl develops into a sexually mature woman, capable of producing eggs and reproducing.
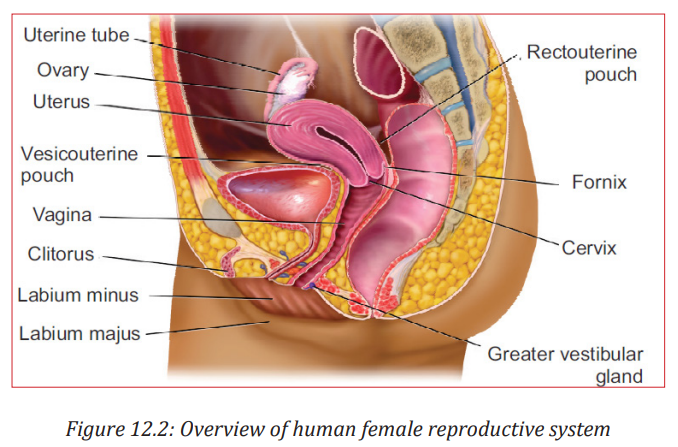
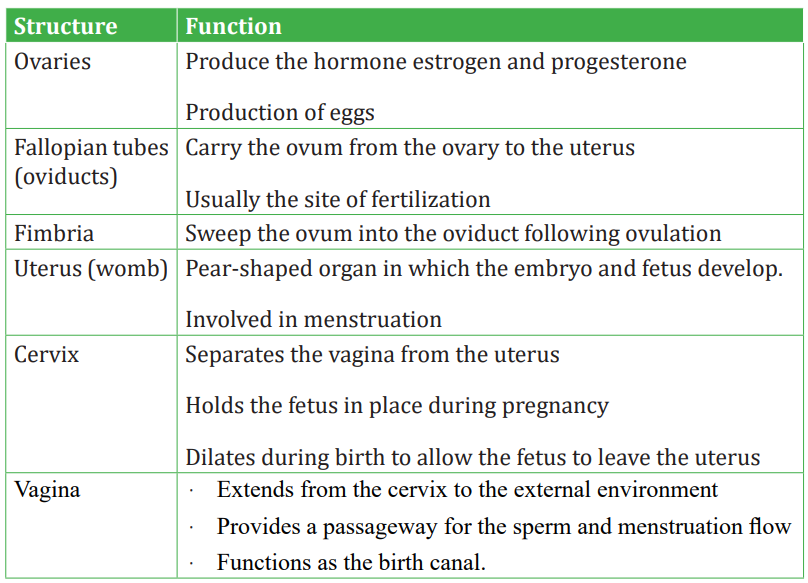
Sexual development in females
The main differences between boys and girls at birth are their reproductive organs. Unlike males, females are not influenced by the male sex hormone testosterone during embryonic and fetal development. This is because they lack a Y-chromosome. As a result, females do not develop male reproductive organs. The human female reproductive system consists of the primary sex organs or the gonads (ovaries), the genital ducts (oviducts or the uterine/fallopian tubes, uterus, cervix and vagina) and the external genitalia, along with a pair of mammary glands.
Application activity 12.1
The figure below shows the parts of the male reproductive system.
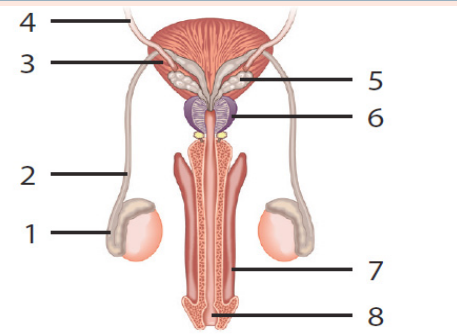
a. Identify the parts represented by the numbers 1 to 8.
b. What are the functions of the parts 1, 2, 5 and 8?
12.2 Gametogenesis
Activity 12.2
To understand the process of gametogenesis and haploid nature of gametes.
Gametes are haploid cells that are formed from diploid germ cells through the process of gametogenesis. The significance of developing haploid gametes lies in the fact that after fertilization, the developing zygote attains the diploid status back. In this way, the developing embryo gets the single copy of all the chromosomes from each parent.
Based on the chart diagrams of spermatogenesis and oogenesis shown below, compute the number of chromosomes at each stage, assuming 2n = 46.
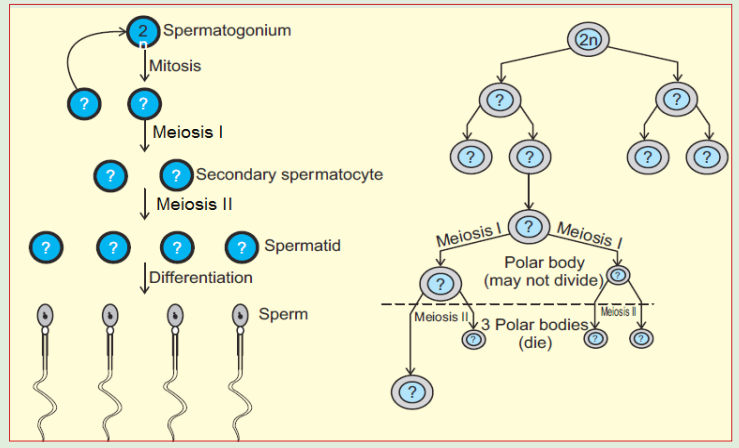
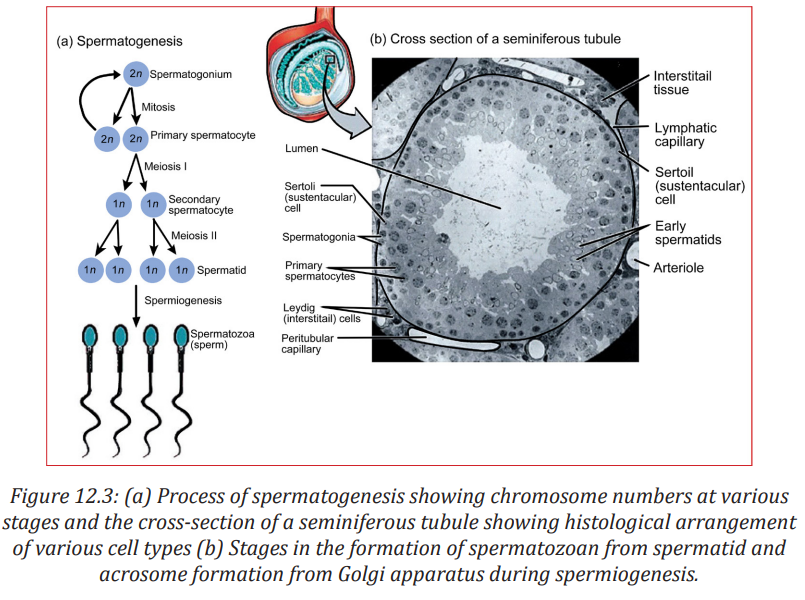
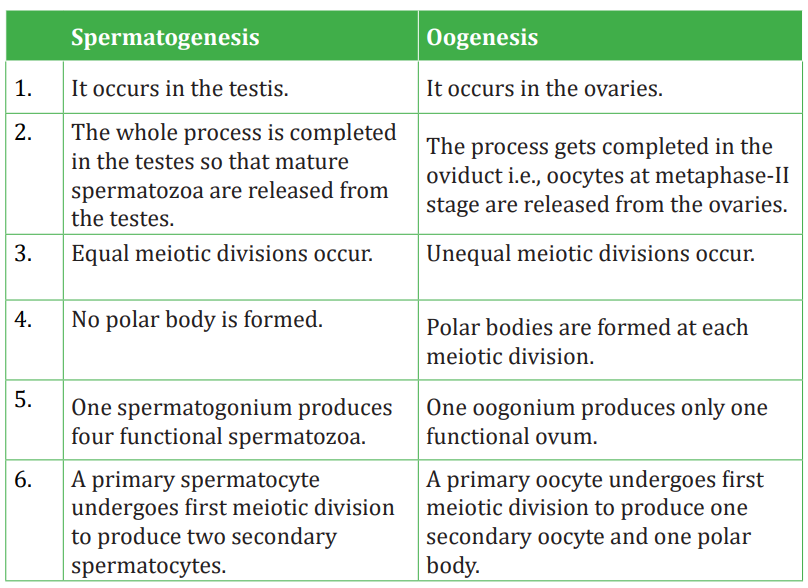
The process of formation of haploid male gametes or spermatozoa from diploid reproductive cells in males is called spermatogenesis. The complete process is broadly divided into two parts:
a. Formation of spermatids and
b. Spermiogenesis or spermatoleosis.
Formation of spermatids
The process of formation of spermatids is further divided into three stages as:
a. Multiplication phase: The primordial germ cells or sperm mother cells differentiate from germinal epithelium of testis and increase in size with prominent nuclei. These cells divide repeatedly by mitosis (i.e., equational division) and produce a number of diploid daughter cells, known as spermatogonia. Thus, in this stage, multiplication of germ cells takes place mitotically.
b. Growth phase: In this phase, spermatogonia increase in size by accumulating food reserves and are now called primary spermatocytes.
c. Maturation phase: The primary spermatocytes (which are diploid) undergo first maturation division which is meiotic division (or reductional division) to produce two haploid secondary spermatocytes. These haploid secondary spermatocytes divide further by mitosis to give rise to four haploid spermatids. This mitotic division is called second maturation division.
The spermatids so produced are non-motile rounded structures that metamorphose into functional and motile spermatozoa through a process known as spermiogenesis or spermatoleosis. The spermatozoa from testis are incapable of fertilizing an ovum. They undergo several morphological, physiological and biochemical changes as they move through the epididymis to attain this structural and physiological maturity. The epididymis i) provides a favourable environment to spermatozoa in acquiring fertilizing ability and ii) stores them until they are ejaculated or move down to the vas deferens.
The morphological changes include structural remodelling of acrosome and formation of disulfide linkages. The physiological and biochemical changes include increase in net negative charge on spermatozoa, change in pattern of motility, change in content of sialic acid, increase in specific activity and reflection power, resistance to pH and temperature and changes in metabolic patterns.
Spermiogenesis
A series of changes in spermiogenesis that transform a non-motile spermatid into motile, functional spermatozoa are listed below:
• The nucleus shrinks and flattens by losing water. Only DNA is left in the nucleus, making cells very light that aids to its motility.
• The two centrioles of a centrosome form proximal and distal centrioles. The proximal centriole lies at the posterior end of nucleus and the distal centriole gives rise to axial filament of the flagellum and acts as a basal granule.
• The mitochondria gather around axial filament and gradually unite to form spiral sheath or nebenkern. It acts as power house of the sperm and provides energy.
• The golgi bodies form the covering over nucleus called acrosome. During acrosome formation, one or more vacuoles start enlarging with a small, dense body called pro-acrosomal granule which further enlarges to form acrosomal granule. The vacuole loses its liquid content and forms the cap of spermatozoan. The remaining part of golgi apparatus is reduced and discarded from sperm.
During all these steps, head of the developing sperm remains embedded in sertoli cells for nourishment. At the end, fully formed spermatozoan shows distinct head, middle piece and tail region.
Structure of spermatozoa
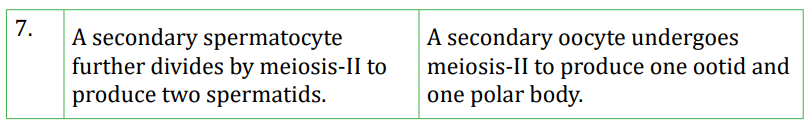
The sperms are microscopic and motile cell. Each sperm is composed of four parts—a head, a neck, a middle piece and a tail. A plasma membrane covers the whole body of sperm.
i. Head is the enlarged end of the sperm, containing an elongated haploid nucleus. The anterior of the nucleus is covered by a cap-like structure 413 called acrosome. The acrosome contains enzymes sperm lyftins or hyaluronidases, which are used to contact and penetrate the ovum at the time of fertilization.
ii. Neck is very short and is present between the head and middle piece. It contains the proximal centriole towards the nucleus which plays a role in the first cleavage of the zygote and the distal centriole which gives rise to the axial filament of the sperm.
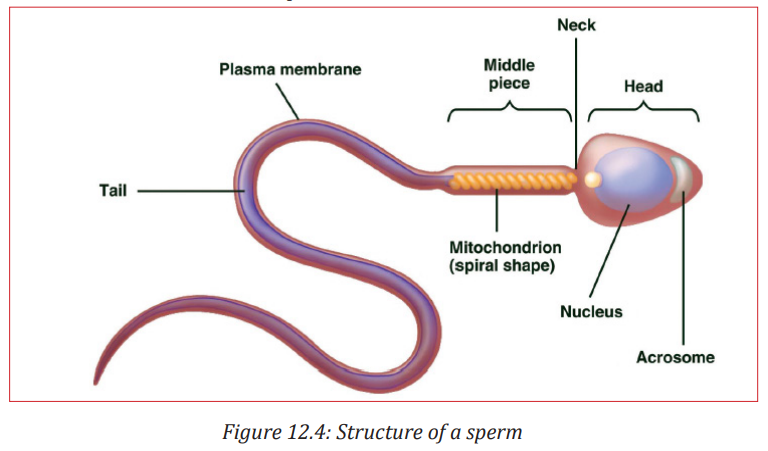 iii. Middle
iii. Middle iii. Middle piece possesses numerous mitochondria which produce energy for the movement of the sperm. At the end of the middle piece, there is a ring centriole (annulus) with unknown function.
iv. Tail is several times longer than the head. It consists of an axial filament surrounded by a thin layer of cytoplasm. The tail provides motility to the sperm, which is essential for fertilization.
The male ejaculates about 200 to 300 million sperms during a coitus. For a normal fertility, at least 60 per cent sperms of the ejaculate must have normal shape and size, and at least 40 per cent of the normal sperms must show vigorous motility. Sperms remain alive and retain their ability to fertilize an ovum from 24 to 48 hours after having been released in the female genital tract.
12.2.1 Oogenesis
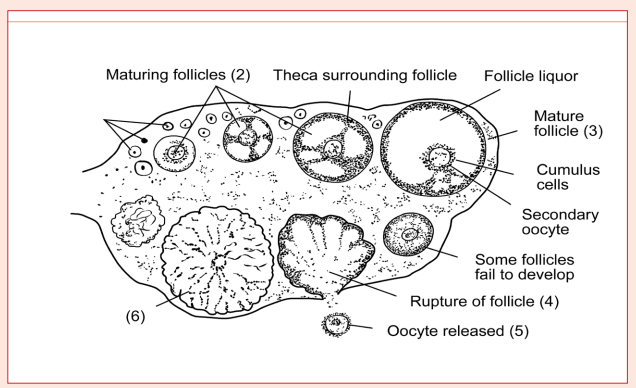
The process of oogenesis occurs in the ovaries. The three phases of proliferation, growth and maturation occur in discontinuous steps.
a. Proliferative or multiplication phase: During early foetal development, certain cells within the germinal epithelium of the ovary become enlarged.These cells proliferate by mitosis, producing undifferentiated germ cells called egg mother cells or oogonia (2n). The oogonia divide mitotically to produce groups of oogonia, termed follicles.
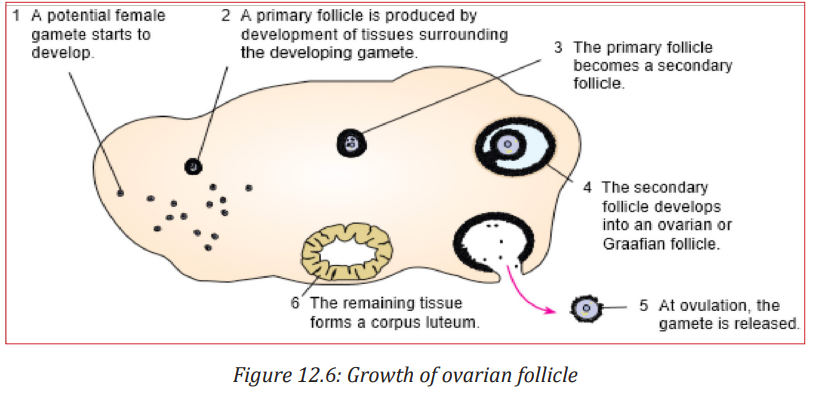
b. Growth and differentiation phase: During this long phase, which may last upto years, one cell in a follicle prepares for the formation of ovum. It starts meiotic division but gets arrested at prophase-I stage and is called primary oocyte. The remaining cells of the follicle lose the potential to become primary oocyte and are known as the follicular cells or granulosa cells. These follicular cells serve to protect and nourish the primary oocyte. The complete follicle with a primary oocyte surrounded by a layer of follicular cells is called the primary or the ovarian follicle.
c. Maturation phase: At puberty, only one of the primary oocytes resumes division per menstrual cycle, alternately in each ovary. The tertiary follicle matures into a Graafian follicle, within which the primary oocyte divides to form two very unequal cells - a large secondary oocyte
and a very small 1st polar body or polocyte
. The 1st polar body may further be divided into two polar bodies. However, the secondary oocyte again gets arrested at metaphase stage of meiosis-II and is released from the ovary during ovulation. It waits in the oviduct for the sperm to arrive. If fertilization occurs, sperm entry into the secondary oocyte marks the resumption of meiosis. The 2nd maturation division (meiosis-II) again divides the secondary oocyte into two unequal daughter cells—a large ootid and a very small 2nd polar body. The ootid undergoes maturation into a functional haploid ovum. A thin vitelline membrane develops outside the plasma membrane of the ovum that protects and nourishes the latter
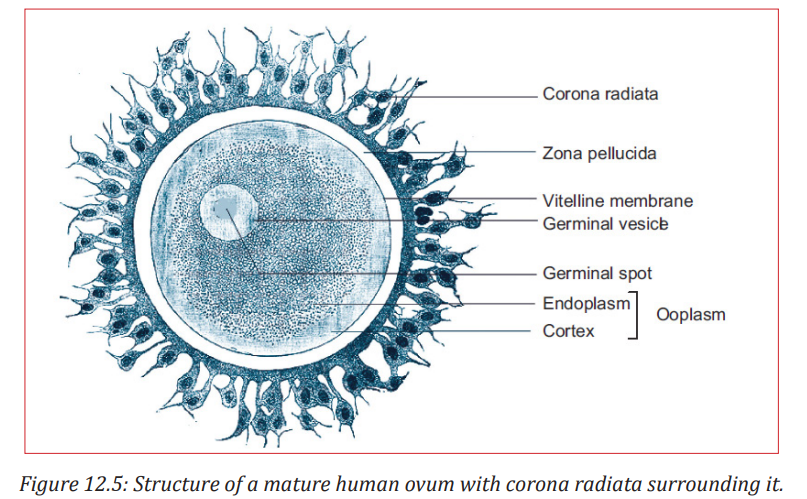
Structure of ovum An ovum is a spherical, non-motile cell, in the secondary oocyte stage of oogenesis, where the second maturation division is yet to occur. Human ovum is extremely small in size i.e., 0.15 mm in diameter, polar and microlecithal. The large nucleus is called germinal vesicle or later the female pronucleus. The nucleolus is called the germinal spot and cytoplasm is known as ooplasm.
The peripheral layer of ooplasm, known as cortex, is more viscous and contains cytoskeletal structures like microtubules and microfilaments, pigment granules and cortical granules of mucopolysaccharides. The inner part of cytoplasm, called the endoplasm is with cell-organelles, informosomes, tRNAs, histones, enzymes etc. The ovum is covered over by a thin, transparent vitelline membrane which is further covered over by zona pellucida. There is a narrow space between these two membranes known as perivitelline space. During discharge of ovum from the Graafian follicle, several layers of follicular cells adhere to the outer surface of zona pellucida and are arranged radially forming corona radiata.
Application activity 12.2
On the basis of your observations, draw the structure of a human spermatozoan and an ovum, labelling the following parts along with the functions of each:
12.3 Menstrual cycle in humans
Activity 12.3
Human beings grow and develop from childhood to adulthood, during such period of growth and development, there are changes in some parts of body which may occur physiologically, physically and even psychologically. These changes prepare individual adulthood to reproduce. Different researches indicated these changes to be coordinated by different types of hormones.
1. Describe the hormones involved during such period of changes in body parts?
1. Discuss the significance of these hormones you have mentioned above during such period of changes.
1. Describe the role of hormones involved during menstrual cycle and birth.
1. Which day of the cycle will ovulation take place.
12.3.1 Menstrual cycle
The menstrual cycle refers to the periodical changes in the reproductive behaviour of a female which tend to occur in a sequence of events one after the other in the periodical circle. At the onset of puberty, the cycle begins and repeats after 28 days unless interrupted by pregnancy. The changes are stimulated by the gonadotrophic hormone such as; follicle stimulating hormone (FSH) and luteinizing hormone (LH). These hormones stimulate ovaries to secrete; oestrogen (steroid) and progesterone hormones. These four hormones are involved in menstrual cycle. Two of them including; FSH and LH are produced by pituitary gland and the other two are released by ovaries respectively. The most obvious sign of the cycle is the monthly discharge of blood a process called menstruation. The first day of menstruation is regarded as the first day of the cycle. Menstrual cycle is divided into three phases or events:
a. Follicular phase
Menstrual cycle usually begins when blood is first discharged from the uterus during the first to fifth day (1-5 days). Following the reduction of progesterone, the hypothalamus releases gonadotropin releasing hormone (GnRH) which stimulates anterior pituitary gland to secrete follicle stimulating hormone (FSH). FSH brings about the following effects; -
-Stimulates the development of a primary follicle
- Contributes to the shedding of uterine wall
- Causes production of oestrogen by uterine cells. The oestrogen produced promotes healing, repair and growth of uterine lining, inhibits further secretion of FSH. Oestrogen levels keep on raising until day 13 where they stimulate secretion of luteinizing hormone (LH) by anterior pituitary gland.
b. Ovulatory phase
Around the 14th day, the high levels of oestrogen cause release of luteinizing hormone (LH) the release of LH brings about ovulation (release of mature egg from the ovary). Immediately after and slightly before ovulation, a woman is fertile and can conceive a baby if she has sexual intercourse or if sperm is present in her oviduct.
c. Luteal phase
After ovulation, the remains of ovarian follicle form corpus luteum also known as Yellow body, which secrete large amounts of progesterone hormone and smaller oestrogen. These two hormones; stimulate further development of mammary glands, inhibit release of FSH and thickening wall of uterus in anticipation of pregnancy. If oocyte (ovum) is not fertilized with in about 36 hours of being shed into oviduct, it dies and corpus luteum gets smaller. Thus levels of progesterone and oestrogen keep on reducing until day 28 days i.e. 14 days after ovulation.
Low levels of progesterone remove the inhibitory effect on FSH, causing its release thus menstruation and the cycle starts again.
Role of hormones
The same hormones that control female puberty and oogenesis also control the menstrual cycle: estrogen, LH, and FSH. Estrogen controls the secretion of the two pituitary hormones by acting on the hypothalamus, which controls the pituitary gland. When the estrogen level rises in the blood, it stimulates the pituitary (via the hypothalamus) to secrete more or less LH and FSH.
In negative feedback, rising levels of hormones feedback to the hypothalamus and pituitary gland to decrease production of the hormones. In positive feedback, rising levels of hormones feedback to increase hormone production. During most of the menstrual cycle, estrogen and progesterone provide negative feedback to the hypothalamus and pituitary gland. This keeps their levels more or less constant. During days 12–14, however, estrogen provides positive feedback to the hypothalamus and pituitary gland. This causes a rapid rise in the production of estrogen by the ovary and leads to ovulation. Another hormone involved in the menstrual cycle is progesterone. The word “progesterone” literally means “pro-gestational hormone.”
Progesterone is a hormone that promotes gestation, or the carrying of a fetus. The function of progesterone in the menstrual cycle is to maintain the endometrium of the uterus. Change in the levels of these four hormones (estrogen, LH, FSH, and progesterone) occur during the menstrual cycle. After menstruation occurs, estrogen secreted by the ovaries increases. This causes the endometrium of the uterus to thicken. FSH from the pituitary stimulates follicles in the ovary to mature. The maturing follicles produce estrogen, and 419 the level of estrogen in the blood rises. When estrogen reaches a high level in the blood, it stimulates the pituitary gland to release a surge of LH. The spike in LH stimulates the one remaining mature follicle to burst open and release its oocyte.
During the first half of the cycle, negative feedback keeps levels of FSH, LH, estrogen, and progesterone relatively stable. During ovulation, positive feedback causes a burst of FSH, LH, and estrogen. During the second half of the cycle, progesterone rises as the corpus luteum in the ovary matures and produces this hormone. Negative feedback helps keep levels of the other three hormones fairly constant. After the oocyte is released, LH stimulates the mature follicle to develop into a corpus luteum. The corpus luteum then starts secreting progesterone, which maintains the endometrium of the uterus. What happens next depends on whether the egg has been fertilized.
• If the egg has been fertilized, it will soon start producing a hormone that helps maintain the corpus luteum. As a result, the corpus luteum will continue producing progesterone and maintain the endometrium.
• If the egg has not been fertilized, the corpus luteum will disintegrate and stop producing progesterone. Without progesterone, the endometrium will break down, detach from the uterus, and pass out of the body during menstruation.
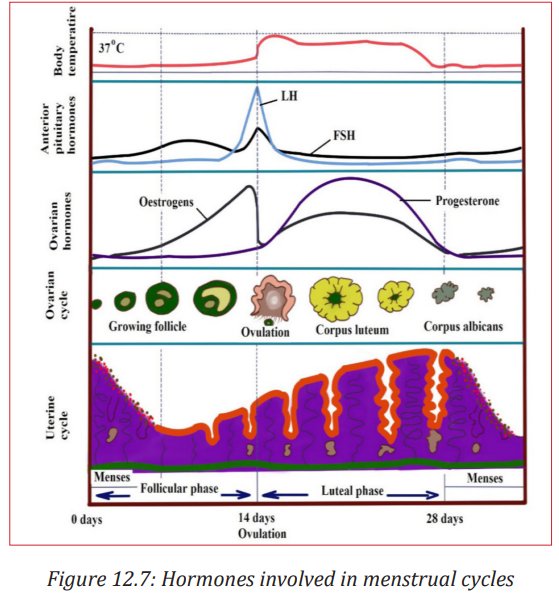
The uterine can also be divided into three phases (events):
Menstrual phase: when endometrium tissue is discharged and vaginal bleeding occurs at the end of ovulatory cycle if pregnancy has not occurred. It is called menstruation.it describes the shedding of endometrium when implantation does not occur. When pregnancy does not occur the level of progesterone falls and these results shedding of endometrium. Menstrual bleeding lasts between 3 and 5 days. The first day of the period is the first day of the cycle.
Proliferative phase: It stimulates the thickening of endometrium of the uterus. This thickness of endometrium is stimulated by oestrogen from follicles before ovulation. This results the development of ovary. It acts like follicular phase.
Secretory phase: it occurs after ovulation for describes further thickening of endometrium (endometrium tissue become more complex) in preparation for implantation. This is stimulated by progesterone which is secreted by corpus luteum and this occurs when corpus luteum is functioning. It acts like lacteal phase.
Estrous cycle
The estrous cycle (also oestrous cycle; derived from Latin oestrus meaning sexual desire) comprises the recurring physiologic changes that are induced by reproductive hormones in most mammalian eutherian females. Estrous cycles start after sexual maturity in females and are interrupted by anestrous phases or pregnancies. Typically, estrous cycles continue until death. Some animals may display bloody vaginal discharge, often mistaken for menstruation, also called a “period”.
Differences from the menstrual cycle
Mammals share the same reproductive system, including the regulatory hypothalamic system that releases gonadotropin releasing hormone in pulses, the pituitary that secretes follicle stimulating hormone and luteinizing hormone, and the ovary itself that releases sex hormones including estrogens and progesterone. However, species vary significantly in the detailed functioning. One difference is that animals that have estrous cycles reabsorb the endometrium if conception does not occur during that cycle. Animals that have menstrual cycles (primates) shed the endometrium through menstruation instead. Another difference is sexual activity. In species with estrous cycles, females are generally only sexually active during the estrus phase of their cycle. This is also referred to as being “in heat”. In contrast, females of species with menstrual cycles can be sexually active at any time in their cycle, even when they are not about to ovulate.
Application activity 12.3
1. The diagram below represents a section through a mammalian ovary.
i. Name the structure labelled (6)
ii. What is the origin of this structure?
iii.What is the function of this structure if an ovum has been fertilized?
iv. State what will happen to this structure next if pregnancy has not occurred.
v. State which hormone is needed to cause the changes seen in the diagram and indicated by the sequence (1) (2) (3)
12.4 Copulation, fertilization and fetal development
Activity 12.4
Make a research in the books in the library about the process of fertilization and the human embryonic development. Take short notes. If possible download a movie on Youtube.com that shows the human embryonic development.
12.4.1 Copulation
It is the act of mating where sperms from male are transferred into the female tract. Male mammals have an intromittent organ called penis which becomes erect at a moment of mating for insertion into female’s vagina. The erection of penis is brought by hydraulic action (penis becomes gorged with blood). This occurs as a result of sexual arousal which brings about by ejaculation (release of sperm). The semen’s are secreted from accessory glands into vas deferens and bladder sphincter closes preventing urine from entering urethra. Sperms are expelled from epididymis into vas deferens and out of the body by a series of muscle contraction of penis. In a female, sexual arousal results in the swelling of clitoris and stimulates the secretion of mucus which lubricates vagina during sexual intercourse.
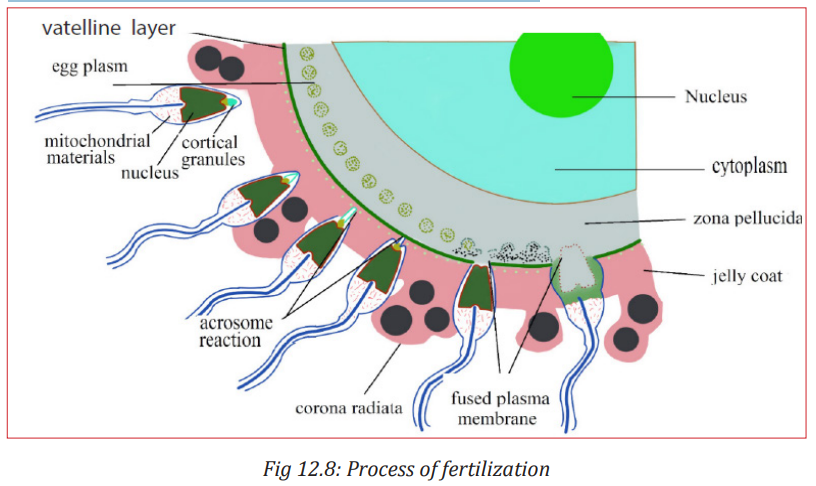
12.4.2 Fertilization
Fertilization is the fusion of male and female nuclei to form zygote. Copulation results in the ejection of spermatozoa into vagina. The spermatozoa swim in the watery mucus of vagina and uterus up into the oviduct where the fertilization takes place in the upper part of the oviduct. From the vagina or uterus spermatozoa propel using energy from mitochondria. If ovulation has already taken place, the egg and sperm meet in the upper part of oviduct and once they come into contact, acrosome raptures and release lytic enzyme which dissolve corona radiata of the egg and soften zona pellucida and vitelline membrane. The following processes take place:
a. Capacitation
This is a stage where by sperm undergoes essential changes while passing through female genital track and this takes about 7 hours. These changes include the removal of a layer of glycoprotein from outer surface of sperm, by enzyme in uterus. Cholesterol also is removed to weaken the membrane.
b. Acrosome reaction
This involves the releasing of enzyme found in acrosome such as hyaluronidases and protease. These enzymes digest corona radiata (narrow path in the follicle cells) and the zona pellucida (a protective glycoprotein surrounding the plasma membrane of the egg).
c. Fusion
In this stage the head of sperm will fuse with the microvilli surrounding the secondary oocyte and penetrate its cytoplasm.
d. Cortical reaction
This stage involves the releasing of enzymes by lysosomes in cortical granules (outer region of the secondary oocytes); the enzymes cause the zona pellucida to thicken and harden forming a fertilization membrane. This cortical reaction prevents the entry of other sperm inside ovum (polyspermy).
e. Zygote formation
The secondary oocyte is stimulated to complete meiosis II, during this time of stimulation the nucleus of sperm and secondary oocyte are called pro-nuclei and then the two nuclei fuse to form the zygote (2n).
12.4.3 Embryonic development
The zygote spends the next few days travelling down the oviduct (Fallopian tube) by peristaltic contraction and by beatings of the cilia in wall of the oviduct toward the uterus. As it travels, it divides by mitosis several times to form a ball of cells called a morula. The cell divisions, which are called cleavage, increase the number of cells but not their overall size. More cell divisions occur, and soon a fluid-filled cavity forms inside the ball of cells. At this stage, the ball of cells is called a blastocyst.
The blastocyst reaches the uterus and becomes embedded in the endometrium at roughly the 5th – 10th day. Once in the uterus the blastocyst burrows into the uterine wall a process called implantation. After implantation, the blastocyst becomes embryo. It grows through multiplication and differentiation of its cells forming tissues and organs. The heart and blood vessels are the first organs formed and embryo now called foetus.
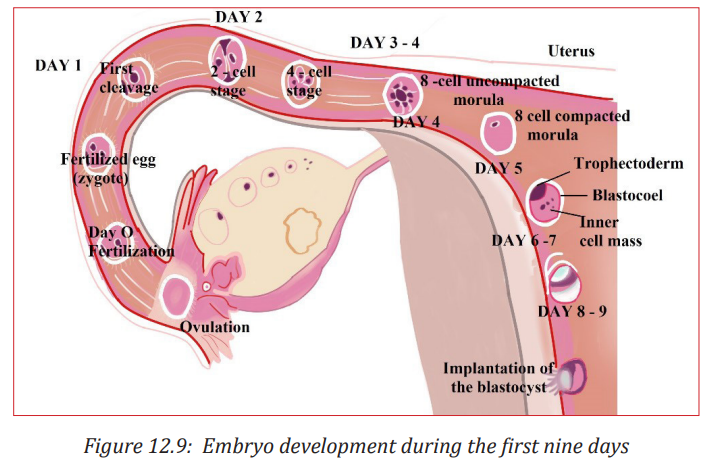
a. Stages of embryo development
There are three major stages of embryo development;
i. Cleavage
The cleavage consists of the division of zygote without increase in mass into a ball of consisting of many daughter cells.
ii. Gastrulation
It is the development of different layers of cells in the embryo. It generally occurs during the second week after fertilization. During gastrulation, cells of the embryo migrate to form three distinct cell layers: the ectoderm, mesoderm, and endoderm. Each layer will eventually develop into certain types of tissues and cells in the body of vertebrates.
• Ectoderm: it forms tissues that cover the outer body; develops into cells such as nerves skin, hair, and nails.
• Mesoderm: it forms tissues that provide movement and support; develops into cells such as muscles, bones, teeth, and blood.
• Endoderm: it forms tissues involved in digestion and breathing; develop into organs such as lungs, liver, pancreas, and gall bladder.
iii.Organogenesis and Differentiation
Differentiation of cells leads to the development of specific organs and tissues within the three cell layers. This is called organogenesis. All the major organs begin to form during the remaining weeks of embryonic development.
b. Extra-embryonic membranes
These membranes are part of placenta. The outer cells of the blastocyst, the trophoblast grow and develop into an outer layer or membrane called the chorion. This plays a major role in nourishing and removing waste products from the developing embryo.
The amnion is a thin membrane covering the embryo like an umbrella and has a protective function. Between the embryo and the amnion is the amniotic fluid. The amniotic fluid supports the embryo and protects it from mechanical shocks. The yolk sac has no significant function in humans but is important in reptiles and birds, where it absorbs food from the separate yolk and transfers food to the gut of the developing embryo.
Note: The first trimester of the development or the embryo is critical. There is high risk of spontaneous abortion or miscarriage due to alcohol, infection, radiations (X-rays), nutritional deficiencies, genetic mistakes or abnormalities in the developing embryo. From the 8th week until birth (around 38 weeks), the developing organism is called a foetus. The foetus is not as sensitive to damage from environmental exposures as the embryo, and toxic exposures often cause physiological abnormalities or minor congenital malformation. All major structures are already formed in the foetus, but they continue to grow and develop.
Application activity 12.4
The diagram below shows some of the events which take place in the ovary and oviduct (Fallopian tube) around the time of fertilization.
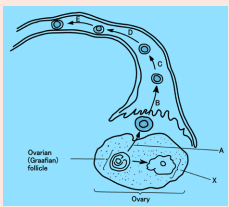
a. Name the following:
i. The process labelled A.
ii. The type of nuclear division taking place at D and E.
iii.The structure labelled X.
iv. One hormone produced by structure X.
b. On the diagram, use the letter F to label the region where fertilization took place.
12.5 Role of placenta in the development of an embryo
Activity 12.5
1. The drawing below shows a developing human fetus inside the uterus.
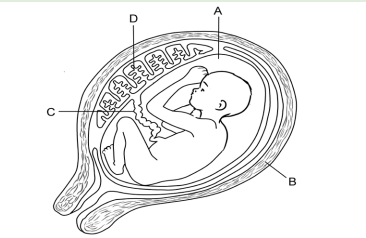
a. Name the parts marked A to D.
b. Name four substances which pass from the mother to the embryo.
c. Name one substance which passes from the embryo to the mother.
d. What are the functions of the parts labelled A to D?
e. What is the importance of the placenta?
The placenta is a temporary organ in which nutrients and wastes are exchanged between the mother and the embryo or foetus.
The foetal part of the placenta consists of the allantoides and chorion. The chorion forms many large projections called chorionic villi which contain a dense network of foetal capillaries which in turn are connected to two umbilical arteries and umbilical vein in the umbilical cord. The umbilical arteries carry blood from the foetus to the placenta, while the umbilical vein carries blood in the opposite direction. Although maternal blood in the endometrium is in close proximity with the foetal blood in the umbilical capillaries, they do not mix because they separated by membranes of the villi and capillary.
12.5.1 Functions of the placenta:
- Allows diffusion of nutrients such as water, glucose, amino acids, simple proteins and mineral salts from maternal blood.
- It is a site of gaseous exchange: haemoglobin of the foetus has high affinity to oxygen compared to adult haemoglobin.
- It offers passive natural immunity on the foetus. Certain maternal antibodies can cross the placental barrier.
- It protects foetal circulation from the high pressure in the maternal circulation
- Prevents mixing of maternal and foetal blood which would cause agglutination (clotting) if the two blood types are incompatible.
- It produces and secretes hormones such as the HCG (human chorionic gonadotrophin), progesterone, oestrogen, and relaxin.
Note that
- The action of HCG is similar to that of LH. HCG stimulates the corpus luteum to secrete progesterone and oestrogen throughout the first trimester. HCG is produced in such large quantities that some of it is excreted in the urine of a pregnant woman (positive test of pregnancy). Secretion of HCG declines around tenth week and the corpus luteum reduces.
- The placenta does not give complete protection to the foetus. Certain pathogens, toxins, and drugs can enter the foetal circulation and cause damage. Examples are; HIV, rubella toxins, alcohol, nicotine and heroin.
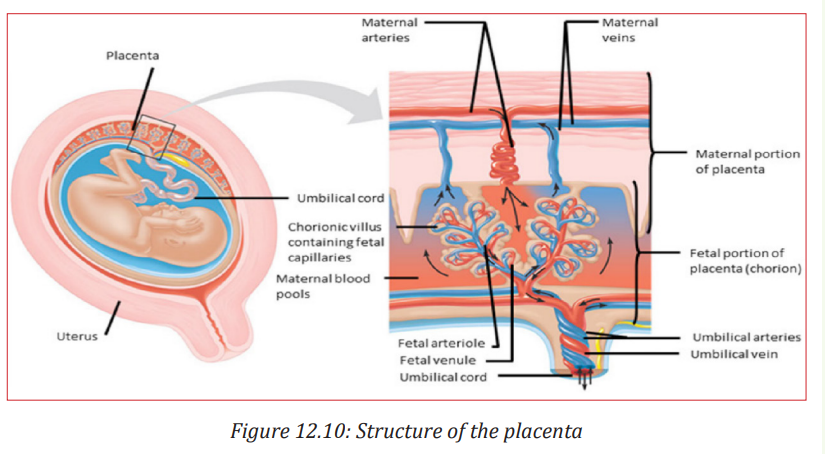
12.5.2 Working of the placenta
Blood from the mother enters the maternal blood vessels of the placenta under pressure, forcing the blood into the empty spaces. When the mother’s blood contacts the foetal blood vessels, gases are exchanged.
Oxygen from the mother’s blood is exchanged with carbon dioxide from the foetus’s blood. A release of pressure brings the mother’s blood back from the placenta and into her veins.
The substances that are moved from the mother to the foetus include:
- Water - Glucose by passive diffusion - Hormones
- Amino acids by active transport
- Lipids by membrane lipid diffusion
- Oxygen is released by the maternal haemoglobin. The haemoglobin of the foetus has a higher affinity for the oxygen. - Alcohol, many drugs, nicotine (if taken by mother during pregnancy)
– Vitamins, minerals.
The substances that are moved from the foetus to the mother include:
- Carbon dioxide is taken up by the maternal plasma and transported to the lungs of the mother for excretion.
- Urea passes into the maternal blood and passes to her kidneys for excretion.
The exchange between the mother and the foetus is possible because of specific structures in the placenta:
- The plasma surface membranes of the cells in the walls of the chorionic villi have microvilli, which increase their surface area for the exchange of substances by diffusion, facilitated transport and pinocytosis.
- Numerous mitochondria are found in these cells. They provide the energy for the active transport and pinocytosis.
- The cell surface membranes contain carrier molecules (protein) used in the uptake of materials into the villi by active transport.
- Numerous small vesicles are found inside the cells of the villi as a result of materials being taken up from the blood by pinocytosis.
Application activity 12.5 1.
The diagram shows the structure of the placenta and parts of the fetal and maternal circulatory systems.
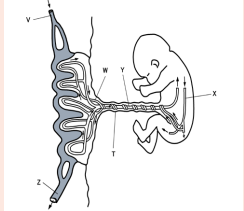
a. Complete the table by listing the blood vessels that carry oxygenated blood. Use the letters in the diagram to identify the blood vessels.
12.6 Physiological changes in females during pregnancy, gestation period, birth and Parental care.
Activity 12.6
Use the image on the introductory activity 12 to describe the physiological changes that can be observed to the pregnant woman on the photo and make short notes.
Pregnancy refers to the development that take place between fertilization of the ovum to birth of the foetus. When fertilized egg becomes implanted in uterine wall, pregnancy results. And a number of important events take place during this period.
The period from fertilization to birth is called gestation period. In human it is about nine months.
12.6.1 Changes during pregnancy
A pregnant woman’s body undergoes various; physiological, physical and behavioural changes.
a. Some physiological changes during pregnancy:
- Respiration rate rises for increased maternal oxygen consumption which is needed for demand of placenta, uterus and foetus.
- More blood vessels grow and pressure of expanding uterus on large veins causes blood to slow in its return to the heart.
- Rise up and out of pelvic cavity this action displaces the stomach and intestine.
- Blood volume increase greatly.
- Placenta produces large amount of progesterone and oestrogen by 10 to 12 week of pregnancy to control uterine activity.
- Increased requirement of calcium due to increase of parathyroid gland.
- Experiences warm (hot flashes) caused by basal metabolic rate and increased hormonal level.
- Stretching of abdomen wall and ligaments that support uterus.
- Kidney work extra hard to excrete waste products of both mother and foetus.
b. Some physical changes during pregnancy
- Breast may become large and more tender because of increased level of oestrogen hormone progesterone thus breast gets even bigger to prepare for breast feeding.
- Nipples may stick out more.
- By the end of third trimester, a yellow, watery, pre-milk may leak from nipples.
- Changes in hair and nail growth and texture due to hormone changes.
- Leg cramp caused by fatigue from carrying pregnant weight.
- Feet and ankles may swell because of extra fluid in the body during pregnancy.
c. Some behavioural changes during pregnancy
- Physical discomfort such as urinary frequency can be frustrating.
- Fear and anxiety lessen especially foetal movement are felt.
- Self-introspection
- Nesting behaviour begins. Some woman exhibit mood swings and emotional liability.
12.6.2 Delivery process
By the end of pregnancy, near the time of birth, the amniotic sac raptures (breaks) and amniotic fluid drains through birth canal and labour usually begins which involves the contractions of muscular walls of the uterus.
Initiation of birth: Uterine contractions starts when the foetal pituitary gland secretes adrenocorticotrophic hormone (ACTH) which stimulates foetal adrenal gland to secrete corticosteroids. These hormones pass into blood sinuses in placenta to cause maternal cells to secrete prostaglandins (local hormone) and cause uterine wall to contract. This contraction pushes the foetal head against the cervix to stimulating stretcher receptor to send information to mother’s brain and causes release of oxytocin hormone. The prostaglandin and oxytocin hormone together result intense contraction of uterine walls called labour which stimulates more release of oxytocin hormone and as positive feedback mechanism.
The delivery process can be summarized into three main stages
- Dilation stage: During this stage, water sac filled with amniotic fluid forms and precedes the head, widening soft tissue of birth canal, cervix, and vagina for canal of constant diameter. The amnion raptures and amniotic fluid drains through vagina.
- The expulsion stage: During this stage, cervix is fully dilated while abdominal muscle bear down in supporting rhythmic contraction of uterus shorten the uterine wall and baby is pushed into and through the birth canal. The head and shoulder align themselves first.
- Placenta stage: This stage begins with complete expulsion of baby and ends with expulsion of foetal membrane. The cord is clamped and cut when delivery of baby is complete. This leads carbon dioxide enrichment into baby’s blood which activates respiratory centre and baby begins to breath with the first cry at the same time foetal circulation changes to baby’s own systemic and pulmonary circulation.
12.6.3 Parental care
The degree of maturity in mammalian new-borns varies from one species to another. New-born in pigs can move around and eat solid food while new-born in humans, dogs and rat are quite helpless and require a lot of parental care to survive.
All mammals feed their young ones by milk which contain all the nutrients required by new born for the first few days. Parents also protect new born from predators and from unfavourable weather. Some species make nest just before delivering the new born. Some parents also become aggressive when they have young one. As the young one grow older the parent start gathering food for them. Once the new born get old enough to gather food for themselves can leave on their own. In humans’ parental care extends for very long time up over 18 years. In humans breastfeeding is associated with many benefits:
- It makes earlier a closer contact between the mother and her infant
- Breastfed babies do not get too fat
- The infant has a better control over its own milk intake, this prevents over eating in late life
- Fats and irons from breast milk are better absorbed than those in cow’s milk and milk is easily digested.
- Breast feeding provides important antibodies that help to prevent respiratory infections and meningitis,
- Breastfeeding helps the mother’s reproduction organ return to a normal state more rapidly
- Breast feeding promotes the secretion of LH (and prolactin) and this makes a delay in follicle development and ovulation,
- The act of sucking on the breasts, promotes the development of the jaw, facial muscles and teeth (sucking from a bottle requires less effort).
- Pulmonary circulation. After delivery, uterus contract so that placenta separates from
- Uterine wall expelled out as the sign of birth end.
APPLICATION ACTIVITY 12.6
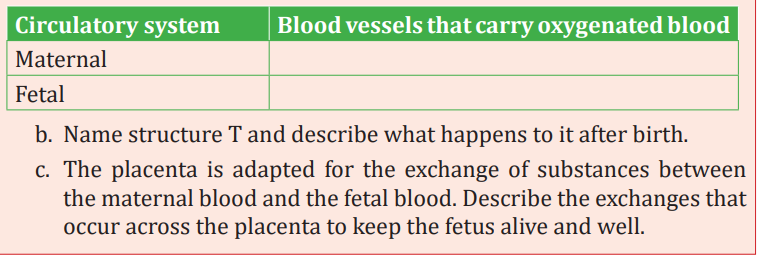
1. Copy and complete the table to show, for each hormone, the precise site of its secretion, and its effects on the ovary or on the endometrium of the uterus.
2. Identify three events that occur as a fetus grows and develops.
3. Why is an embryo generally more susceptible than a fetus to damage by toxins
12.7 Twins and multiple births
Activity 12.7
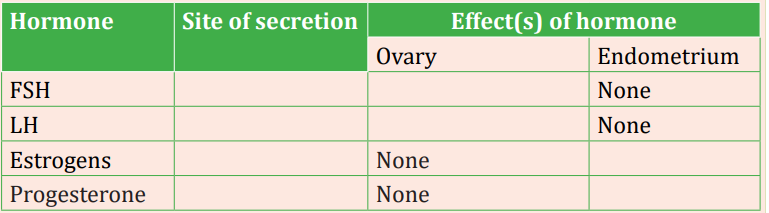
Use the image below to answer the questions that follow:
a. What is the difference between the formation of the two types of twins?
b. Which type of twins are very much alike in appearance? Why?
c. Which type of twins that can develop into individuals with different sexes?
Twins are individuals born to the same mother at the same time. Twins include;
- Fraternal twins or non-identical twins or dizygotic twins: These are twins which develop from two separate egg cells fertilised by two different sperms. Fraternal twins are genetically different since they develop from different gametes.
- Identical twins or monozygotic twins: these are twins which develop from the same fertilised egg. Identical twins are genetically similar since they develop from the same sperm and the same egg.
- Siamese twins: are conjoined twins i.e. they have not completely separated during the embryo development. As consequence, they share same organs. Conjoined twins develop without separating completely and are born attached to one another. Such twins may be separated surgically.
Fraternal twins or dizygotic twins are the result of two separate ova fertilized by separate sperm. This may occur when two ovarian follicles reach maturity and rupture at the same time. Fraternal twins may be of the same sex or different sexes. Even if of the same sex, however, they are as genetically different as any siblings might be.
Identical twins or monozygotic twins are the result of the splitting of the very early embryo before the cells start to become specialized (usually within 8 days after fertilization).
For example, if a 16-cell stage becomes separated into two groups of 8 cells each, each group will usually continue to develop in the usual way. Another possible cause is the development of two inner cell masses within the blastocyst. This, too, is before significant specialization has taken place and each inner cell mass may develop into a complete individual. Twins of this type may be called monozygotic, meaning that they have come from one fertilized egg. Identical twins are always of the same sex, are very much alike in appearance, and in other respects are genetically identical.
Siamese twins (also known as conjoined twins) are monozygotic twins whose bodies are joined together during pregnancy. This occurs when the zygote starts to split after fertilization and fails to separate completely.
Multiple births arise when several eggs are released at the ovulation and are fertilised or when a zygote splits into several zygotes. It is commonly occurring in mammals such as; pigs, dogs and cats.
APPLICATION ACTIVITY 12.7
1. The diagram below illustrates two types of reproduction.
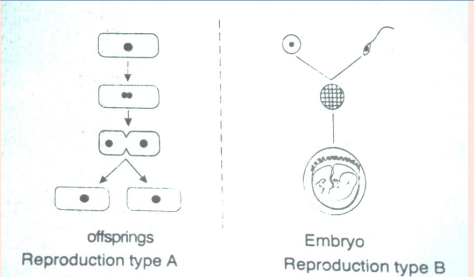
a. Name reproduction types A and B.
b. State 2 advantages of type A.
c. How does the reproduction type A differ from identical twins?
12.8 Infertility and in-vitro fertilization
ACTIVITY 12.8
You may have understood different couples with infertility problems being able to conceive by using artificial methods that involves fusing the sperm and the egg on the outside of the female body.
What do you know about those techniques?
Infertility
Infertility is the failure to achieve pregnancy when no contraceptive method is used.
In females, infertility may be due to:
- Failure to ovulate due to the lack of some hormones
- Damage of the Fallopian tubes / oviducts, for example the tubes may be completely blocked by nature or after an infection,
- Damage on the uterus; for example, the endometrium can be destroyed
- Damage on the cervix, for example the cervix may be narrow or too wide or may stop producing cervical mucus needed for the sperm to reach uterus
- Antibodies against sperms, for example, the cervix, the uterus or the oviduct of a woman can produce antibodies against her husband’s sperms.
Some causes of infertility/barrenness in males include
- Absence of sperms in the semen (Azoospermia).
- Low sperm count e.g. when ones ejaculate less than 1cm3 of semen.
- Abnormal sperm e.g. sperms with 2 tails, or without tail, or without acrosomes,
- Auto-immunity e.g. antibodies attack one’s sperms
- Premature ejaculation: the man has orgasm before copulation
- Impotence i.e. inability to achieve or maintain an erection of the penis.
a. Some social consequences include
- Isolation including exclusion from ceremonies and social gathering.
- Rejection being an outcast and physical abuse perpetrated by community members.
- Stigmatization or recognizable marginalization.
- Status loss that is no respect and social fail.
- Ridicule including insults and verbal abuse.
b. Some economic consequences include
- Cost of infertility by either modern biomedical or traditional treatments.
- A feeling of rejection.
- Having few relations, receiving few gifts and less land.
- Marital instability including fear of husband taking second wife.
- Divorcing childless woman
- Violence perpetrated by partner.
Note: While infertility may result into conflicts between couples and families, producing many children also brings about some economic challenges. Many children affect families’ financial wellbeing and some parents admit that children are expensive. Consequences of many children per one family include:
- High rate of maternal depression.
- Low rate of immunization and parental care.
- Baby taxing both physical and emotional especially off work after birth.
- I come tend to go up when new members of the family arrive. Men see the boost in their earnings after birth of child.
- There is economic wellbeing decline in time around birth.
c. Increasing fertility
Increasing fertility can be done in various techniques such as:
- Fertility drugs: a synthetic chemical which stimulates ovulation by either proving gonadotrophins such as FSH which stimulates growth of follicles. Or proving chemical which inhibits natural production of oestrogen.
- Artificial insemination: sperm from donor is inserted artificially through cervix of mother to be.
- Using in-vitro fertilization
12.8.1 In-vitro-fertilization
In-vitro fertilization is the process of fertilization where an egg is fertilized by sperm outside the body. It involves the fertilization of egg cell outside the body which are then artificially implanted in the uterus to produce test tube baby. The process involves monitoring and stimulating of woman’s ovulatory process removing ovum (egg) from woman’s ovaries and letting sperm to fertilize them in liquid laboratory. The fertilized egg (zygote) undergoes embryo cultured for 2 to 6 days and then transferred to the same or another uterus for successful pregnancy. The embryo is implanted in woman’s uterus.
Advantages of in vitro-fertilization techniques include
- Simplicity: living organisms are extremely complex functional system with protein molecules, RNA molecules and genes. Therefore, the work of Vitro simplifies system under study to focus on small number of components.
- Species specificity in human cells in-vitro method can be studied without extrapolation from experimental animal’s cellular response.
- Automation and convenience: In-vitro method can be automated, high yielding throughout screening methods for testing molecule in pharmacology.
- In vitro-fertilisation can be used to achieve successful pregnancy but the process usually produces more embryos which some scientists wish for research design to improve our knowledge about disease.
Application activity 12.8
Outline the techniques of in-vitro-fertilization.
12.9 Family planning and contraceptive methods
Activity 12.9
Use the photo below shows various contraceptive methods. Identify each of them.
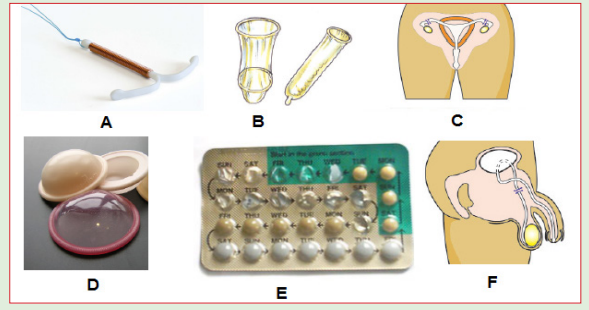
Which two contraceptive methods among others on the photo are more effective?
Contraception is the prevention of conception that is preventing the fusion of the male gamete with the female gamete. Both natural and artificial methods exist.
Artificial methods
- Oral Contraceptive pills: a chemical method of contraception. One version uses a combination of progesterone and oestrogen that inhibits ovulation. Others are single hormones that require very careful management when taken. - Intrauterine device (IUD) the coil is placed inside the uterus an exact understanding how this works is unclear. A possible explanation is that it ‘irritates’ the endometrium such that rejects implantation of embryos. The device is made from plastic or copper and inserted by a doctor. Nevertheless, this device is very effective.
- Condom is another mechanical method of contraception that prevents the sperm from reaching the egg. Composed of a thin barrier of latex this is placed over the erect penis and captures semen on ejaculation. This is also a good barrier to prevent the transmission of sexual diseases.
- Cap (diaphragm) is another barrier method again made from latex. The cap is placed over the cervix to prevent the entry of sperm in semen. This technique requires that the cap is put in position in advance of sexual intercourse and that it is used in combination with a spermicidal cream. When used correctly this is an effective contraceptive however this is not a barrier against the transmission of sexual diseases.
- Sterilisation is a surgical and near permanent solution for contraception such as: Vasectomy. In men this involves cutting the vas deferens and prevents sperm entering the semen. In this state, man still ejaculates normally and releases semen however this does not contain sperm. Tubal ligation involves the cutting of fallopian tube so that eggs cannot reach the uterus. In women the surgery cuts or ties the oviducts thus preventing sperm from reaching the egg in fertilisation.
Natural methods
- Natural birth control methods include specific actions that people can do naturally to help prevent an unintended pregnancy.
- Abstinence: the individual makes the choice to delay sexual intercourse until the decision to conceive a child is made. - Withdrawal is a behavioural action where a man pulls his penis out of the vagina before he ejaculates. The withdrawal method also relies on complete self-control. You must have an exact sense of timing to withdraw your penis in time.
- Fertility awareness methods: This require a woman to monitor her body to determine when she is most fertile. You then avoid having unprotected sex around the time of ovulation. This natural birth control method involves paying attention to different body changes (such as basal body temperature or cervical mucus) and recording them to predict when you will ovulate. To be successful, you need to be willing to record and chart your fertility signs. Then, you (and your partner) must agree to not have sex (or to use backup birth control) for 7 days before and 2 days after you ovulate. Fertility awareness methods include the Billings Method and temperature method
- Continuous (Lactational Amenorrhea Method) can postpone ovulation for up to 6 months after giving birth. This natural birth control method works because the hormone required to stimulate milk production prevents the release of the hormone that triggers ovulation.
Advantages and disadvantages of birth control
Some advantages of birth control/contraceptives
- Gives great protection against unplanned pregnancy if one follows instructions.
- Condoms to some extent protect against pregnancy and STDS.
- Combinations of pills reduce/prevent cysts in breasts and ovaries.
- Improved family wellbeing.
- Improved maternal and infant health.
Some disadvantages of birth control/contraceptives
- Necessity of taking medication continually.
- High cost of medication.
- Hormonal contraceptive does not protect against STDS.
- Eggs may fail to mature in the ovary for a woman who uses hormonal contraceptives.
- Woman must remember to take them regularly.
- Woman must begin using hormonal contraceptive in advance before they become effective.
- Some women experience several; headaches, breast tenderness, chest pain, discharge from vagina, leg cramps and swelling or pain.
Application activity 12.9
1. Which contraceptive methods can protect against sexually transmitted diseases / infections?
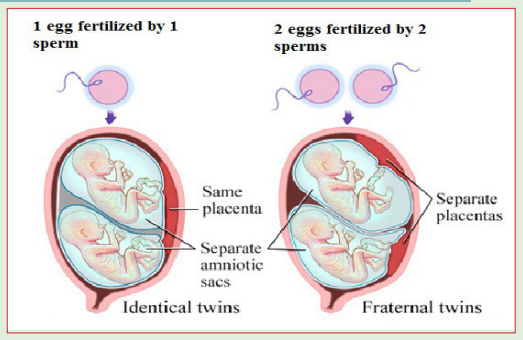
2. The diagram shows the sequence of events in the development of a mature ovarian (Graafian) follicle and corpus luteum
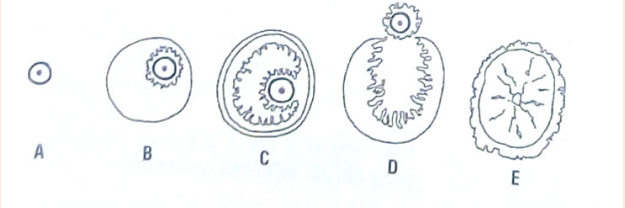
a. What is the main hormone produced by the ovary when stage B is present?
b. Which two of stages A to E would you expect to find in the ovary of a woman during the early stages of pregnancy?
c. Give the reason for your answer on b.
d. Some oral contraceptives contain only estrogens. Which of the stages A to E would you expect to find in the ovary of a woman who had been taking such an oral contraceptive for a prolonged period of time?
e. Give reasons for your answer on d.
Skills lab 12
1. Determining the fertile period
Count the number of days of your menstrual cycles and count the number of days for 10 consecutive cycles. Choose the cycle with the highest number of days and the cycle with the lowest number of days. Substract 18 from the lowest cycle and 11 from the highest cycle.
Example: Mary has 27 days as her shortest cycle and 36 as her longest cycle. She has had her menstruation on 09/08/2019. What will be her fertile period?
First fertile period: 27 – 18 = 9 (August 9 + 9 =August 17)
Last fertile period: 36 – 11 = 25 (August 9 + 25 =September 3)
The fertile period of Mary will be from 17 August to 3 September 2019
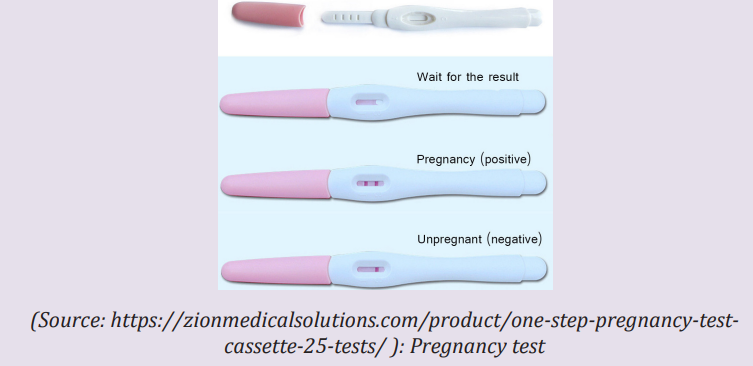
2. Pregnancy test
The pregnancy test works by checking your urine for a hormone called human chorionic gonadotropin (HCG). Your body only makes this hormone if you are pregnant. HCG is released when a fertilized egg attaches to the lining of your uterus when pregnancy begins. If your pregnancy test is positive, it means that you are pregnant. If the pregnancy test is negative, it means that you are not pregnant. Pregnancy tests are most accurate when you take them after you have missed your period.
End unit assessment 12
1. Which of the following do sperm NOT travel through?
a. Ureter, b. Urethra, c. Vas deferens, d. Epididymis
2. The placenta in humans is derived from the:
a. Embryo only, b. Uterus only, c. Endometrium and embryo
d. None of the above
3. The graph below shows the level of reproductive hormones in the blood of an un-named mammal during its reproductive cycle.
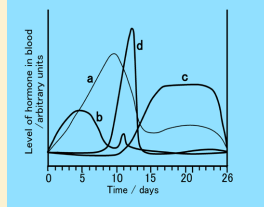
a. Name the hormones labelled (a) to (d)
b. Give the likely day of the cycle on which ovulation takes place and give reasons for your answer.
4. Answer the following questions:
a. Define the term fertilization
b. The diagram below shows the structure of a human sperm.
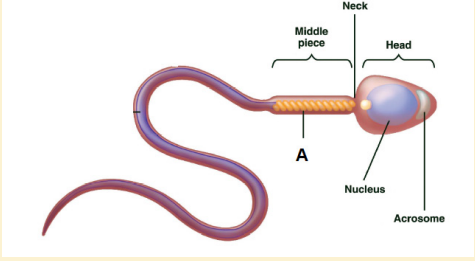
i. Explain the part played by the organelle labelled A in the process leading to fertilization.
ii. The acrosome contains an enzyme that breaks down proteins. ii)The acrosome contains an enzyme that breaks down proteins. Describe the function of this enzyme in the process leading to fertilization.
5. In humans, widening of the female hips is one example of physical changes that distinguish the sexes but are not essential for reproduction.
To what term does the definition in italics refer?
a. What term is used for the time in a young person’s life when such changes take place?
b. Name the hormone that maintains such changes throughout the life of a male.
c. Describe the role of estrogen and progesterone in the control of the events of the menstrual cycle.
d. Answer the following questions in relation to the development of a human zygote.
i. By which type of cell division does the zygote divide?
ii. The placenta forms from tissues of the mother and the fetus. Give two roles of the placenta.
iii.Give one change experienced by the mother that indicates to her that the birth process is starting.
