UNIT 1 SIMPLE WOUND CARE
Key Unit competence
Perform the techniques of simple wound dressing
Introductory activity 1.0Observe the picture provided and respond to the questions below
1. What do the following picture have in common?
2. What did you notice in the picture A, B, C, and D?
3. If you were an associate nurse, what could you do to care for patient in
picture D
The picture shown above represent a wound, process of wound healing and
related wound care. The wound is the breaking of the skin, underlying tissues
or an organ (break of skin integrity). A wound occurs when the integrity of any
tissue is compromised (e.g. skin breaks, muscle tears, burns, or bone fractures.
A wound may be caused by an act, such as a gunshot, fall, or surgical procedure.
1.1 PRINCIPLES OF SIMPLE WOUND CARE
1. What do you think should guide a comprehensive wound care?
2. According to what you have experienced, seen or heard regarding
wounds, relate causes and types of wounds
Learning activity 1.1
1.1.1.Types of wounds
There are several ways of classifying types of wounds, such as the source of the
wound, the state of skin integrity, the likelihood and degree of contamination and
how much time the wound have been existing.
a) Types of wound per etiology
Wounds are either intentional or unintentional.
• Intentional wound occurs as a result of therapeutic reasons. Examples are
surgical incisions or venipuncture. This wound is created under the sterile
conditions.
• Unintentional wound occurs as a result of unplanned event such as a
wound caused by an accident. Examples include traumatic wounds, fall, a
gunshot wound, and violence, unusual wound (snake or insect bite) or the
result of an allergic reaction.
Furthermore, unintentional wound may result from an illness such as vascular an
or neuropathic impairment. Thus, the wound may result from either ischemia or
blood stasis. Ischemia comes from reduced blood supply caused by the tightening
or blockage of blood vessels, and this leads to poor circulation.
Wounds caused by being immobile, such as bed sores or pressure injuries this is
caused by immobilization (or difficulty moving) for long periods.
The wound can be caused by friction when a body part rubs or scrapes across arough or hard surface
b) Types of wound per skin integrity
Wounds are mainly open or closed.
A closed wound is an injury that does not break the surface of the skin butcauses damage to the underlying tissues.
Open wounds break the surface of the skin and may also damage underlying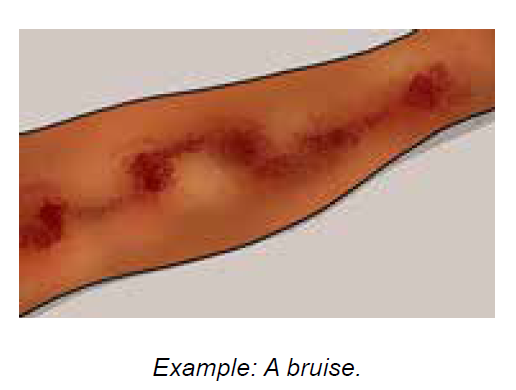
tissues.
Some examples of open wounds include
Abrasions: These form as a result of rubbing or scraping the skin against a hardsurface.
Lacerations: These are deeper cuts caused by sharp objects, such as a knife, or
sharp edges.
Punctures: These are small deep holes caused by a long, pointed object, such
as a nail.
Burns: These result from contact with an open flame, a strong heat source,
severe cold, certain chemicals, or electricity.
Avulsions: This refers to the partial or complete tearing away of skin and
tissues.
c) Types of wound per likelihood and degree of contamination
Considering the likelihood and degree of contamination, there are four types of
wounds:
• Clean wounds - are uninfected wounds in which no or minimal inflammation
is encountered and the respiratory, alimentary, genital and urinary tracts are
not entered. Clean wounds are primarily closed and surgical wounds.
• Clean contaminated wounds - are surgical wounds in which the respiratory,
alimentary, genital or urinary tract has been entered. Such wounds show no
evidence of infection.
• Contaminated wounds - include open, fresh, accidental wounds and
surgical wounds involving a major break in sterile technique or a large
amount of spillage from the gastrointestinal tract. Contaminated wounds
show evidence of inflammation.
• Dirty or infected wounds - include wounds containing dead tissue and
wounds with evidence of a clinical infection, such as purulent drainage.
d) Types of wound per wound age
Considering how long the wound has been existing, the wound is either acute or
chronic:
• Acute wounds are relatively new and occur suddenly in nature as result of
surgery or trauma. Their healing move through the stages of healing within
the predicted time-frame.
• Chronic wounds may develop over time as results of underling chronic
condition such as diabetes, ischemic disease, pressure damage resulting
from prolonged immobilization, and inflammatory diseases and or as a resultof failed healing of an acute wound leading to a lengthened recovery.
1.1.2. Principle of simple wound care
Wound healing is a complex and dynamic physiological process that is affected by
various factors. Healthcare providers must understand how to assess these and be
able to address them accordingly to optimize the wound healing process. Though
wound care is often focused primarily on topical treatment, a comprehensive plan
of care should address three areas concerning wound healing affecting factors.
Therefore, general principles for holistic wound care are (1) correction of etiologic
factors, (2) provision of systematic support for wound healing and (3) topical
treatment that create and maintain an optimal healing environment.
Correctly identifying the cause of the wound is key to developing a comprehensive
management plan. Failure to addressing the causative factor(s) will result in failure
to heal, even if systematic support is provided and topical therapy is appropriate.
Thus, initial assessment and intervention must include identification of the etiologic
factors and initiation of measures to address these. For example, the most the most
critical intervention in the management plan of a pressure ulcer is to eliminate or
minimize the pressure that caused the wound.
Systematic support for wound healing is important as wound healing requires
increased calorie, protein, and vitamin and mineral intake; sufficient blood flow
and oxygen to support repair process; and relatively normal glycemic levels. Thus
assessment and correction of systematic conditions that adversely affect repair is
the second priority in wound healing.
The goal of topical therapy in wound care is to create a local environment that
supports healing, through appropriate cleansing and dressing selected based on
individual wound assessment and it should be matched evidence-based guidelines.
For instance, if a wound’s assessment reveals that it is in proliferative phase,
cleansing it should aim at removing exudate without damaging the proliferative
cells and newly formed tissues. Moreover, providing topical wound therapy should
ensure comfort and dignity of the patient.Self-assessment 1.1
1. Your sister accidentally cut her finger while slicing tomatoes. This injury is
a(1) ___________________ (2) _______________ (3) _____________
(4) ____________________wound
2. After finishing a wound dressing, the associated nurse undertook a five
minutes’ patient education activity regarding a balanced diet and smoking
cessation.
a. Which principle of wound care was she addressing?
b. What other wound care principles should be implemented for acomprehensive and holistic wound care?
1.2. PHASE OF WOUND HEALINGAnalyze carefully the following images and respond to the questions below
a. What do you understand with the term wound healing?
b. According to the image above showing biological changes in body tissues
during wound healing process, describe what happen in each picture
c. Imagine what would happen if one phase of wound healing did not occur?
Wound healing is the complex process in which the skin goes through as it repairs
damage from wounds. Destroyed or damaged tissue is replaced by new produced
tissue in stepwise fashion and involves the stage of hemostasis, inflammation,
proliferation, and maturation.a) Phase 1 - Hemostasis
This phase has the aim of stopping any bleeding where the body activates its blood
clotting system. When the blood clots at the opening of a wound, it prevents the
patient from losing too much blood and therefore it become the first step of the wound
closing up. Briefly when tissue is damaged, serotonin, histamine, prostaglandins,
and blood from the injured vessels fill the area. Blood platelets form a clot, and fibrin
in the clot binds the wound edges together. This step can last up 2 days depending
on the part of the skin which is affected.
b) Phase 2 - Inflammation
When phase one is complete and the body is no longer bleeding, the body activatesits key defense mechanism inflammation.
This phase works to kill bacteria and remove debris with white and other blood
cells. Inflammation ensures that the wound is clean and ready for new tissue to
start growing. This phase is the most painful. Lymphocytes initiate the inflammatory
response and this causes increasing capillary permeability. White blood cells from
surrounding vessels move in and ingest bacteria and cellular debris, demolishing
the clot and healing the wound. Redness, warmth, swelling, pain, and loss of
function may occur. Platelets heavily secrete growth factors during this phase. This
phase takes up to six days and should go away.
c) Phase 3 - Proliferation or repair
When the wound is clean, the body will begin the proliferation phase of woundhealing. This stage involves closing of the wound.
This phase can have 3 semi phase which are: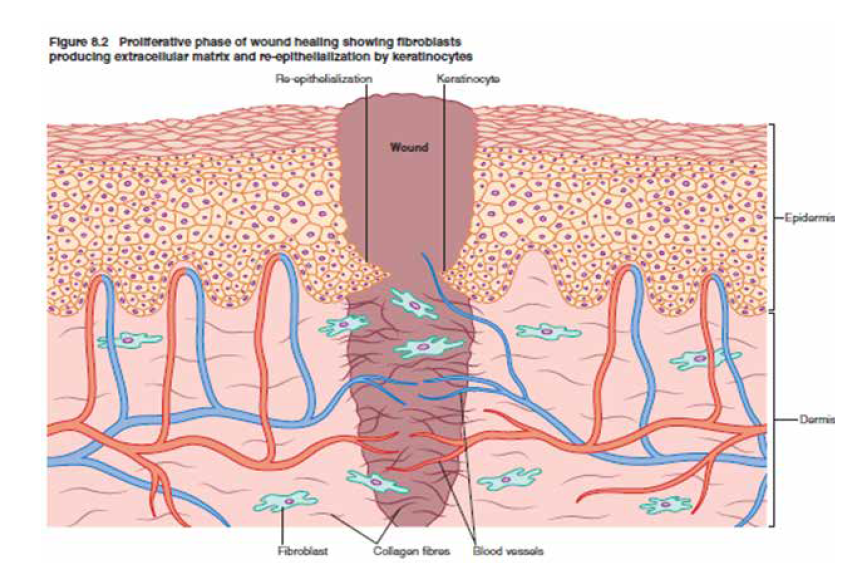
Filling the wound: with new connective tissue and blood vessels.
Contracting the edges of the wound: this will feel like the wound is tightening
towards the center.
Covering the wound: epithelial cells (cells that create a protective barrier between
the inside and outside of your body) flood in and multiply to close your wound
completely.
This phase can last four days to almost a month, depending on the surface area of
your wound.
d) Phase 4 - Maturation or remodeling
During this phase, the new tissue that body built in phase three, needs to strengthenand build flexibility.
This stage can take the longest, sometimes taking over a year to fully repair. But,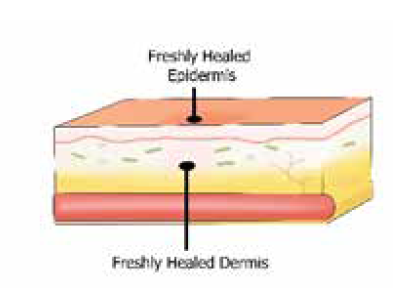
once fully recovered, the skin should be pretty close to as strong as it was before
it was wounded.
The healing process is one of the body’s most surprising functions, but it can be
delayed by aggravators like infection and poor wound care. It is good to learn how
to properly dress a wound so health care provide can maximize the body’s ability.
Self-assessment 1.2
Match phases of wound healing in column A with their respective definitions incolumn B
1.3.FACTORS AFFECTING WOUND HEALING
Learning activity 1.3Observe the following images and answer to questions below
1) After observing the above images ABCD, list different factors affecting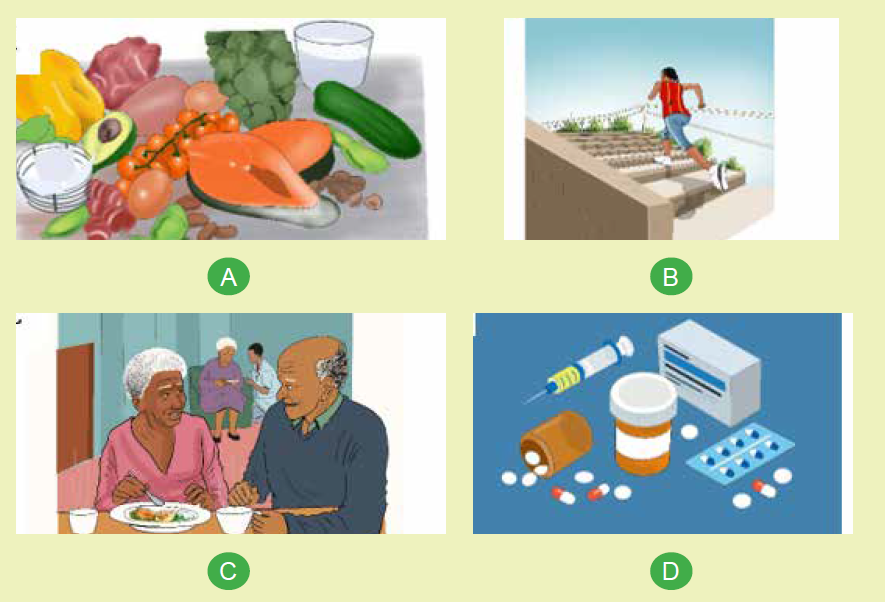
wound healing.
2) In group discussion, explain the factors affecting wound healing separately.
There are many reasons why wounds do not heal in a straightforward manner;
these reasons can be classified as intrinsic (something internal to the individual) or
extrinsic (something external to the individual).
a) Intrinsic factors of wound healing
• Age: as we age cell regeneration rates slowdown, which means that wounds
usually take longer to heal the older we get. A wound that might take 3 weeks
to heal in a youth may take 6 weeks to heal in the older individual. It is therefore
important to set realistic goals when planning care.
• Gender: the fluctuating hormone levels in females during their lifetime appear
to affect skin integrity and therefore healing rates, though in a mild way.
• Psychological: it is thought that the psychological state can impact on wound
healing, such as high levels of emotional stress, worry and negative thought
processes. Evidence of this can be seen where a person develops mouth
ulcer or cold sores when they are experiencing such emotional pressures.
• Physical/structure: the human form itself can be a factor in wound healing
rates, and one example of this is where pressure ulcers exist; the underlying
bone that caused the ulcer in the first instance will continue to delay wound
healing if pressure relief is not ensured. Other physical factors that must be
considered are for example scar tissue, physical deformities, particularly of
limbs, amputations, mobility and reduced mobility.
• Lifestyle: smoking, alcohol and drug use, although an extrinsic factor, can
impact intrinsically on the individual, which could delay healing rates.
• Nutrition: this can be both an intrinsic factor (e.g. due to malabsorption
conditions or gastric surgery) and an extrinsic factor (due to dietary choices) all
of which can result in poor nutritional intake. As wounds require an increased
nutritional intake, any reduction will impact on healing rates.
• Medications, common medications that impact on wound healing processes
and rates are steroids, anti-inflammatory and cytotoxic drugs.
• Comorbidities common medical conditions that affect wound healing rates
are:
i. Diabetes, peripheral artery disease and other conditions that affect
the blood circulation such as heart disease and hypertension means a
reduced blood supply reaches the wound bed.
ii. An inefficient cardiopulmonary circulation due to heart or lung disease
means that the wound will receive a reduced supply of essential oxygen
and nutrients that will reduce healing rates.
iii. Inflammatory diseases, such as rheumatoid arthritis and ulcerative colitis;
these conditions affect the inflammatory phase of a wound healing if
the condition is in ‘flare-up’, which can cause a prolonged inflammatory
phase; alternatively, if the condition is in remission the patient is usually
taking prescribed steroids, which also delay the healing process by
delaying or stopping the inflammatory phase. Patients on steroids who
are due to have surgery are often required to stop steroids for a short
time before and after surgery.
iv. Cancer.
v. Major or multi-organ failure.
b) Extrinsic factors
• Environment – this may include the surface the patient is lying or sitting on;
the environment they live in; the support networks available to the patient;
social and financial factors. It can also refer to the environment the wound is
kept in (see below).
• Clothing and footwear – these can impact on healing rates by causing
• pressure or restriction of blood supply, which means that there is a reduce
supply of essential oxygen and nutrients supplied to the wound.
• Wound site – wounds sited over joints (e.g. elbows, knees) will usually take
slightly longer to heal than wounds over non-mobile areas.
• Temperature – of particular importance is the temperature of the wound bed;
ideally a wound ought to be retained at body temperature (i.e. 36.9°C). If the
wound is not dressed with an appropriate (insulating) dressing the wound bed
will cool according to the atmosphere and will result in a reduced blood supply.
The temperature of an individual is also important; if a person is allowed to
cool the peripheral circulation will be reduced in order to preserve the core
temperature. This in turn reduces the amount of blood (and therefore oxygen
and nutrients) reaching the wound bed.
• Nutrition – it is vital that the patient with a wound takes in additional calories
in order to increase healing rates, particularly with regards to increased
proteins.
• Wound care skill/technique: one of the most common reasons for delayed
wound healing is the wound care technique of health professionals. This may
include the use of inappropriate dressings, causing trauma on removal of the
dressing (causing the wound to revert back to the beginning of the healing
process); leaving a dressing in situ for too long, causing saturation and
subsequent maceration/excoriation of the wound and peri-wound tissues.
• Infection: Both bacteria and endotoxins can lead to the prolonged elevation
of pro-inflammatory cytokins such as interleukin-1 and TNF-α and elongate
the inflammatory phaseSelf-assessment 1.3
Discuss the ways that intrinsic factors (age, lifestyle and medications) and
extrinsic factors (nutrition, wound site and wound care skill) affect the woundhealing process.
1.4.OVERVIEW ON SIMPLE WOUND CARE
Learning activity 1.4
Patient H. is coming to the health facility where you work as an associate nurse.
He is having the bleeding simple wound on elbow after road traffic accident. The
senior nurse decided that the wound dressing will be performed.
1) Why wound dressing will be done?2) Which type of wound dressing will be performed?
The wounds are different and therefore their dressing differ also. There is:
• Aseptic dry wound dressing - is the most common type of dressing for
simple wound, it is done using dry gauzes without products and held in place
using a tap or a bandage if a non-adhesive dressing material is used. The
wound is previously cleaned with sterile gauzes soaked in an appropriate
fluid like normal saline 0.9%.
• Sterile wet wound dressing - Gauze or other dressing materials is be
moistened with saline to keep the surface of open wounds moist. A moist
wound surface enhances the cellular migration necessary for tissue repair
and healing.
Purpose of wound dressing
• To keep the wound clean
• To prevent the wound from injury and contamination
• To keep in position, the drugs applied locally
• To keep the edges of the wound together
• To apply pressure
Self-assessment 1.4
Mr. J. underwent hernia repair and was discharged home the following day. He
presents to you with a discharge summary at a health center.
1) What is the type of wound dressing is indicated for Mr. J.?
2) Differentiate aseptic dry dressing from sterile wet wound dressing3) What is the purpose of wound dressing for Mr. J?
1.5 ASEPTIC DRY WOUND DRESSING TECHNIQUES
Learning activity 1.5
1) According to your understanding, what do you think the health care
provider should do in order to keep the aseptic wound dry?
2) What do you think should be attention of nurse to make aseptic wound
dressing procedure?
3) Perform dry aseptic wound dressing technique to a mannequin aswatched on video
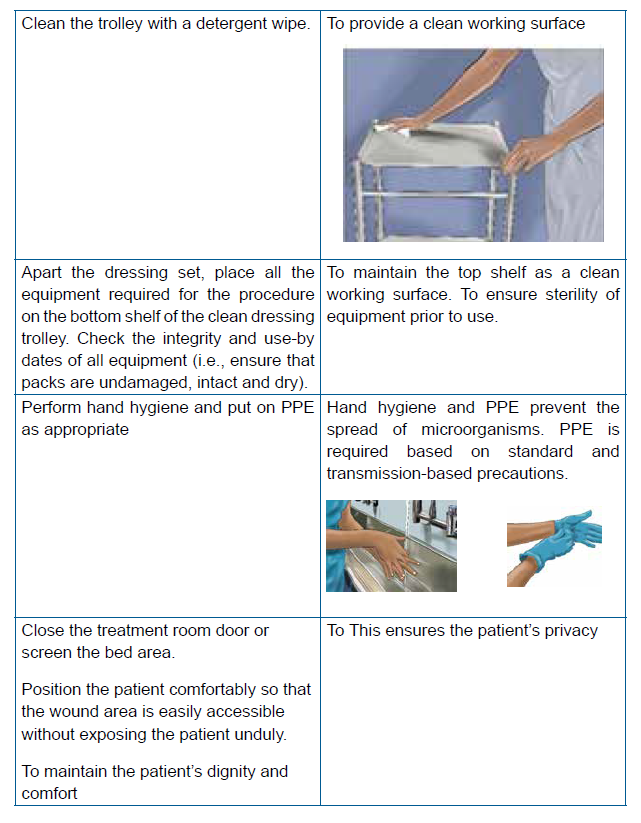
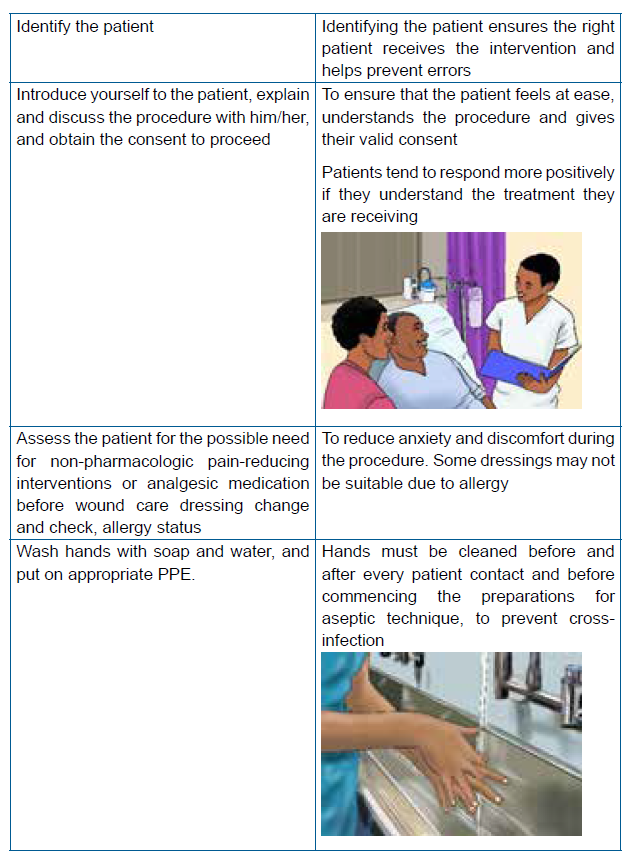
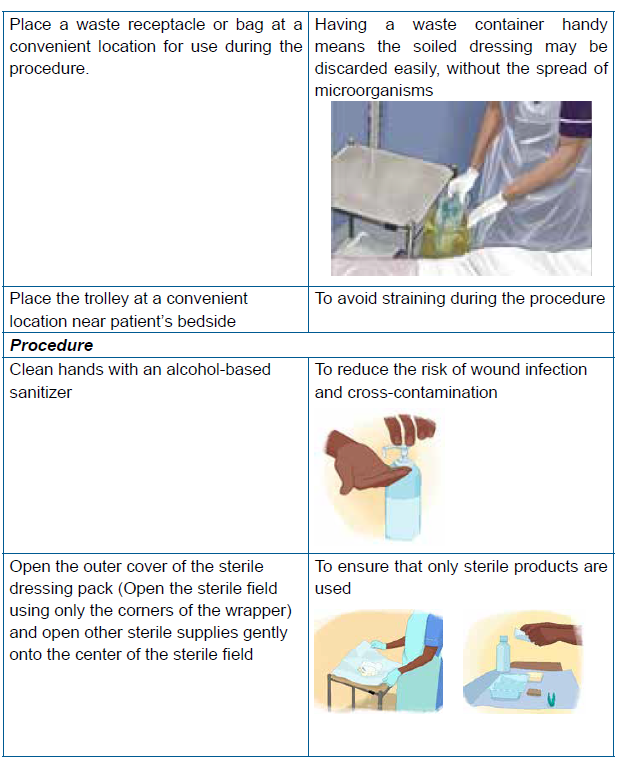
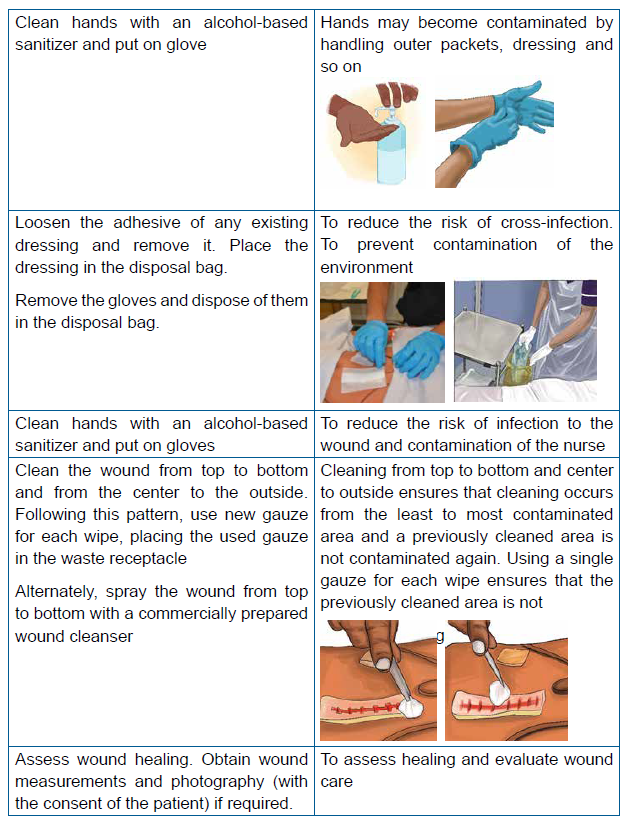
Steps of dry wound dressing technique





Self-assessment 1.5
Use the simulation lab and perform aseptic dry wound dressing technique on themannequin respecting the steps of aseptic dry wound dressing.
1.6.WET DRESSING TECHNIQUE
Learning activity 1.6
After having an overview on techniques of wound dressing
1) Which techniques do you find as mostly indicated for the illustrated wound
image?
2) Explain the rationale of choosing that wound dressing technique?3) Perform the indicated wound dressing technique
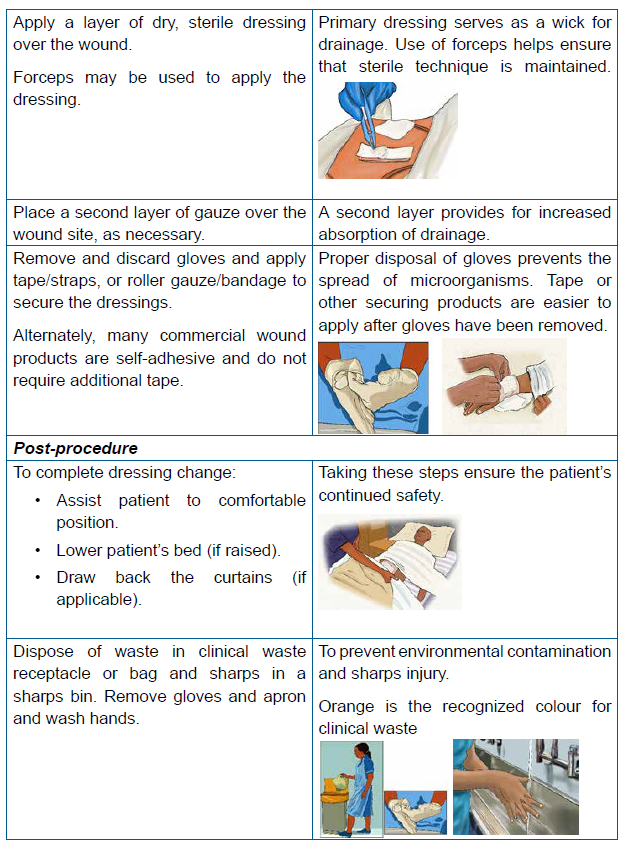
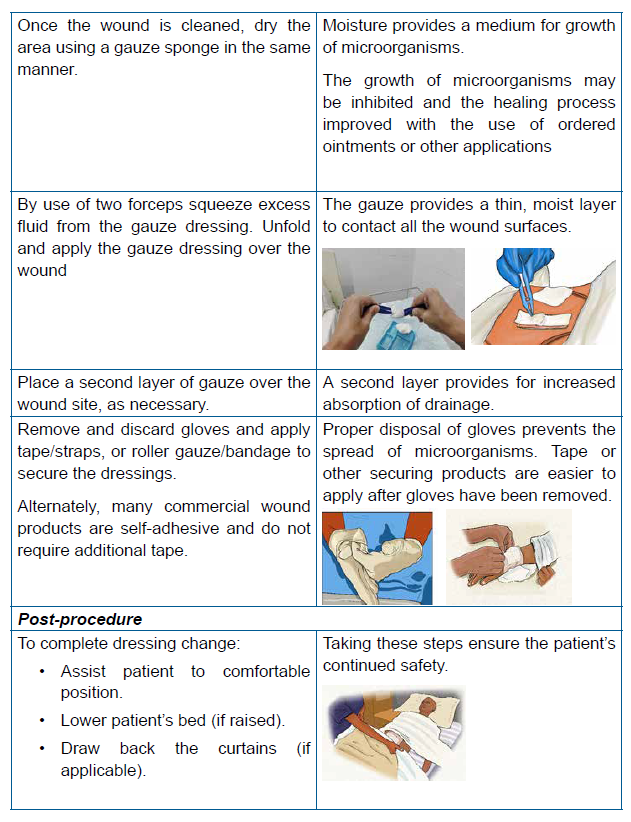
A saline-moistened dressing promotes moist wound healing and protects the wound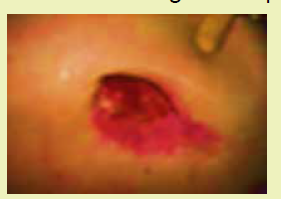
from contamination and trauma. A moist wound surface enhances the cellular
migration necessary for tissue repair and healing. It is important that the dressing
material be moist, not wet, when placed in open wounds. Dressing materials are
soaked in normal saline solution and squeezed to remove excess saline so that the
dressing is only slightly moist.Steps of wet wound dressing


Self Assessment 1.6
Mr. P. A 29 years old male is a patient who comes regularly at the health center
for wound dressing of his right heel which he got from a road traffic accident from
his motorcycle. Today is his day-10 to be dressed, and in his small book from
the health center (carnet), it is indicated that Mr. P.’s wound is mildly infected. On
your observation after removing the old dressing, you find that there are some
yellowish discharges coming from the wound in small amount
1) Identify the type of dressing technique indicated2) Perform the indicated wound dressing technique
End unit assessment 1
1. Why good hand hygiene is important in wound care?
a) Clean hands smell nicer for the patient.
b) Prevent the spread of infection
c) Dressings don’t work if there is any dirt on a wound.
d) Nurses don’t like dirty hands
2. Which of the following is the correct sequential order of the phases of
wound healing?
a) Inflammation, remodeling, hemostasis, and repair
b) Inflammation, hemostasis, proliferation, and maturation
c) Hemostasis, inflammation, repair, and remodeling
d) Inflammation, maturation, proliferation, and hemostasis
3. Why is it important to include the patient in your selection of wound
dressing?
a) Because the ward manager has told you to talk to patients
b) Because the league of friends won’t supply any more extras for the
ward if you don’t talk to patients
c) Because patients will respond to treatment in a more positive manner
if they understand what you are doing and the likely outcomes.
d) Because talking to your patient helps the time to pass more quickly
when you’re doing the dressing explain and discuss the procedure
with the patient
True or false questions
1) Normal saline solution is the only completely safe cleansing agent and is
the treatment of choice for use of wounds
2) Use the same swab to cleanse a circular wound more than once
3) As long as the aseptic wound dressing is done properly, documentation is
unnecessary after performing it
Short answer questions
1) Mention the principles of performing wound dressing
2) Explain how comorbidities as intrinsic factors affect wound healing
process
Case Scenario
Mr. T with 30 years old comes to the health facility where you work, he has
bleeding wound on left tibia after road traffic accident. Your senior prescribe for
him daily Wound dressing with Normal saline. As a student future associate
nurse assigned to take care of Mr.
1) List at list 3 purpose of wound dressing
2) Outline at least 5 precautions that you are going to implement for
preventing infections to Mr. T during performing wound dressing
3) During the procedure, explain to him the role of diet as well as the example
of most preferred nutrient in promoting wound healing4) Which phase of wound healing for Mr. T,s wound
