UNIT 2: POSTNATAL OBSTETRIC DANGER SIGNS
Key Unit Competence:
Identify obstetrical danger signs in women during postnatal period and manage the
woman accordingly.
2.0 Introductory activityIntroductory activity 2
Observe the following pictures showing a mother with postnatal obstetric dangersigns.
1. What do you think on a mother who may deliver and continues to have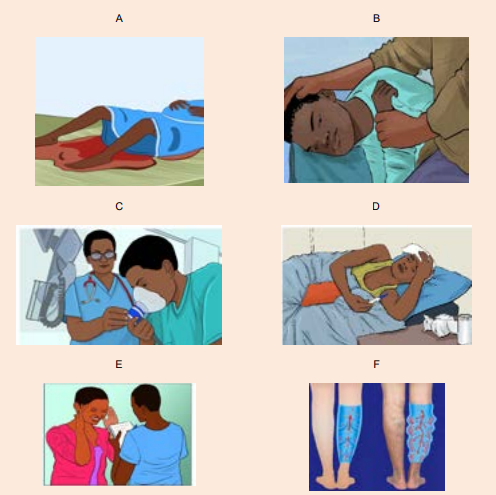
vagina bleeding? Which image that is expressing that situation?
2. What are the complications that are likely to occur to the picture A situation?
3. Did you have an exposure with the person who was presenting seizures?
What do you think that can be done to this person with seizures?
4. Have you seen a person with difficult in breathing? What do you suggest
that can help this person with breating difficulties?
5. Have you ever had hotness of the body? What do you think that can help
to reduce the body temperature for this person with hotnes of the body like
in image D situation?
6. Have youever been in contact with the person with headache? What do
you suggest that can be done in order to help this person with headache
like in picture E?
7. What do you think to the mother who may deliver and develop deep vein
thrombosis at the lower limbs? What do you suggest that can help theperson with this condition like picture F state?
2.1 Assessment of vaginal bleeding as an obstetric danger signin the postnatal period.
Learning Activity 2.1
Observe the following image and try to think about the medical condition thatcan be reflected on it.
a) Which obstetrical condition do you think that looks like this image above?
b) Have you ever seen acondition like this?c) Which clinical manifestations do you observe from this mother?
Obstetrics: is the field of study concentrated on pregnancy, childbirth and the
postpartum period.Hemorrhage means excessive bleeding.
In postnatal period, blood loss of 500 ml or less following a delivery is generally
considered as physiologically normal. However, severe postnatal blood loss is life
a threatening situation to the other. In immediate postnatal period, bleeding also
called ‘postpartum haemorrhage’ (PPH) is defined as:• Bleeding more than 500mls following vaginal delivery and 1000mls following
Caesarean section in the first 24 hours following birth.
• Constant trickling of blood after delivery in the first 24 hours following birth. or
• Blood loss sufficient to cause hemodynamic instability in the first 24 hours
following birth.
• Postpartum haemorrhage is the leading cause of morbidity and mortality
among pregnant women (approximately one third of deaths of maternal
mortality) worldwide. Therefore, early recognition of these danger signs isvery important in order to avoid delay
Vaginal bleeding risk factors
The following are the risk factors that should be watched out to the mother inpostnatal period:
•Conditions that distend the uterus beyond average capacity. Multiple
gestations, hydramnios, a large baby, and the presence of uterine myomas
predispose to postpartum haemorrhage.• Conditions that could have caused cervical or uterine lacerations. Awoman who underwent operative birth (caesarean section) or rapid birthCauses of vaginal bleeding
could develop lacerations that would cause bleeding.
• Conditions with varied placental site attachment: Placenta praevia and
abruption placenta also cause heavy maternal bleeding.
• Uterus could not contract readily: Conditions such as deep anesthesia during
caesarean delivery, advanced maternal age, and high parity could cause the
uterus not to contract and therefore result in bleeding.
• Inadequate blood coagulation: Disseminated intravascular coagulation
(DIC) in a woman could cause heavy bleeding postpartum.
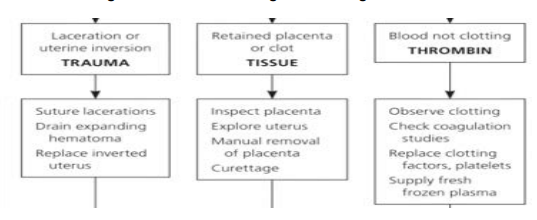
Vaginal bleeding has many potential causes but the common known 4Ts are the
following. They are arranged according to frequency:• Tone (70%)• Trauma (20%)Tone: uterine atone is the inability of the uterus to contract and may lead to continuous
• Tissue (9%)• Thrombin (1%)
bleeding. Retained placental tissue and infection may contribute to uterine atone.
Uterine atone is the most common cause of postpartum haemorrhage
Trauma: Injury to the birth canal which includes the uterus, cervix, vagina andthe perineum which can happen even if the delivery is monitored properly
Tissue: retention of tissue from theplacenta orfetusas well as placental abnormalitiessuch as placenta accreta and pericreta may lead to bleeding.
Thrombin: a bleeding disorder occurs when there is a failure of clotting, such aswith diseases known as coagulopathies.
Signs and symptoms of vaginal bleeding in postnatal period
Signs and symptoms of vaginal bleeding generally include heavy bleeding from the
vagina that doesn’t slow or stop over time. Initially there may be an increased heart
rate, feeling faint upon standing, and an increased respiratory rate. As more blood
is lost, the patient may feel cold, blood pressure drop (hypotension), and they may
become unconscious in case of severe vaginal bleeding.
Self-assessment 2.1
1. Define postpartum haemorrhage.
2. Explain the risk factors of postpartum haemorrhage.
3. Enumerate causes of postpartum haemorrhage.
2.2 Management of vaginal bleeding as an obstetric danger signin the postnatal period.
Learning Activity 2.2
Observe the following image and try to think about the management of PPH
 a) To rescue the mother with severe vaginal bleeding, what do you think canAppropriate management of postpartum haemorrhage requires prompt diagnosis
a) To rescue the mother with severe vaginal bleeding, what do you think canAppropriate management of postpartum haemorrhage requires prompt diagnosis
be done to the patient?
b) After they finish rescuing the patient in critical condition, they have to
continue close monitoring, what do you think can be closely monitored?
c) What do you think about this condition in case blood transfusion may beneeded?
and treatment.
Massive transfusion protocols allow for rapid and appropriate response to
haemorrhages exceeding 1500ml of blood loss. However, blood transfusion is donein highly equipped health setting.
a. Initial management and resuscitation
Table 2.1: Initial management of PPH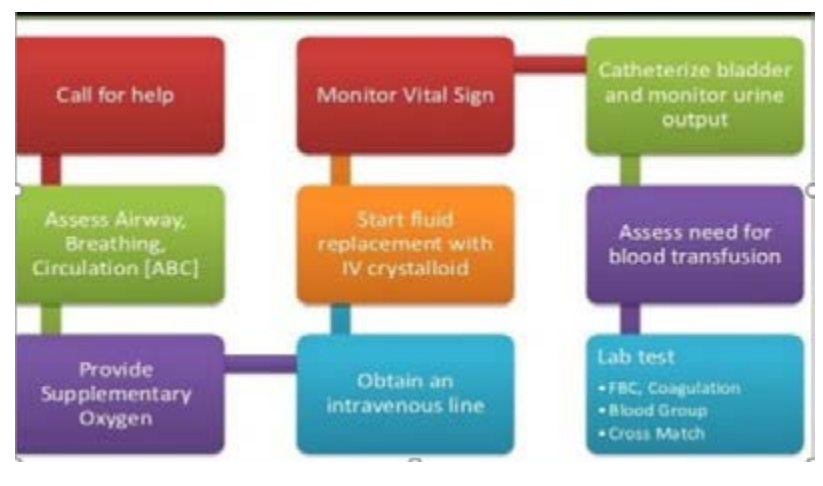
b. Management for uterine atony
Uterine Massage, bladder emptying + the following drugs
Table 2.2: Drugs used in uterine atony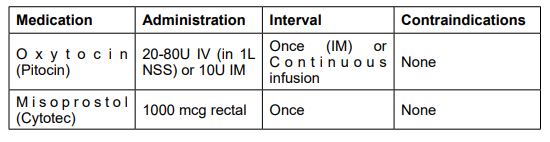
c. Management of other causes of vaginal bleedingTable 2.3: Management of causes of vaginal bleeding
d. Management of severe vaginal bleeding
The severe postpartum haemorrhage is managed through:• Transfusion of red blood cells, platelets and clotting factorse. After care
• Blood pressure vasopressor drugs to raise up blood pressure
• Uterine packing, aorta compression, balloon tamponade, and bimanualcompression of the uterus
• Monitor for ongoing blood loss (preferably quantitative measurement and vitalSelf-assessment 2.2
signs
• Assess for signs of anaemia (fatigue, shortness of breath, chest pain, lactation
problems.
• Frequently assess for bladder fullness• Report findings and hindrances met
1. What are the interventions that must be provided for initial
management of vaginal bleeding?
2. What drugs are used in management of PPH caused by uterine atony?3. Write PPH in full.
2.3 Complications and prevention of vaginal bleeding in postnatalperiod
Learning Activity 2.3
Read the following case study
24years old mother P2 delivered by spontaneous vaginal delivery, delivered
baby girl weighing 4.5kg in good condition, with in 1 hour of delivery mother
developed sudden gush of blood from the vagina. When the nurse arrived for
post-natal care realises that the uterus becomes soft, estimated amount of blood
loss is 1000mls by visual estimation.
a) What do you think about this scenario?b) What do you think about likely complications?
a) Complications of vaginal bleeding in the postnatal period
Vaginal bleeding after delivery has various complications to the mother including
but not limited to anaemia, dilutional coagulopathy, fatigue, myocardial disorders,
orthostatic hypotension, postpartum depression, anterior pituitary ischemia with
delay or failure of lactation (Sheehan syndrome or postpartum pituitary necrosis),hypovolemic shock when not detected and managed early.
b) Prevention of vaginal bleeding in the postnatal period
Postpartum haemorrhage to the mother is very critical but it can be prevented. The
following are preventive measures of postpartum haemorrhage from pregnancy,during labour and postpartum:
During pregnancy• Identification of risk factorsDuring labour
• Identification and treatment of maternal anaemia and iron deficiency during
antenatal care visit.
• Education of the mother to deliver in health setting area• Avoid routine unnecessary episiotomyAfter delivery
• Limit instrumented deliveries, especially forceps.
• Perform Active management of the third stage of labor (AMTSL) with controlled
cord traction (see the video on youtube.com), intramuscular oxytocin injection,and delivery of the placenta.
• Uterine massage and uterine retraction checking in first 6 hours postpartum
• Close blood loss amount checking
• Close monitoring of postpartum.
• Vital signs
• Emptying the bladder and avoid bladder fullness in first 6 hours postpartum• Ensuring rest of the other in first 6 hours postpartum
Self-assessment 2.3
1. What does it mean AMTSL?
2. What are the preventive measures of postpartum haemorrhage afterdelivery?
2.4 Assessment of the mother with seizures as an obstetric dangersign in postnatal period
Learning Activity 2.4
Read the following case study
A 32 years old mother presented at the accident and emergency department
on day 5 post normal delivery with a history of headache which is not relieved
by analgesics, her husband reports that she had one episode of convulsion at
home.
On arrival the vital signs revealed that BP was 178/114mmHg, pulse: 108beats
per minute, SPO2: 86% on room air and respiration rate: 18 breaths per minute.
After 10 minutes of arrival, she experienced another episode of convulsions
and these were characterised by generalised muscle spasms which terminated
spontaneously. There was no bowel or urinary incontinence during the episode.
a) After reading this case study, what do you think about this condition?
b) What do you think could be the reason of that convulsion?
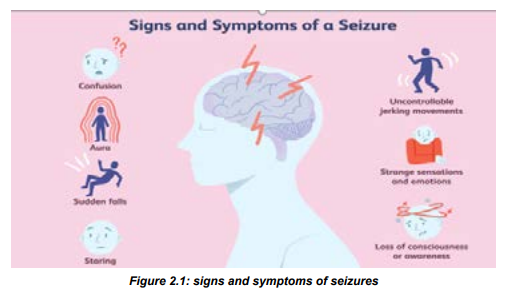
A seizure (the medical term for a fit or convulsion) is a burst of uncontrolled
electrical activity between brain cells (neurons or nerve cells) that causes temporary
abnormalities in muscle tone or movements (stiffness, twitching or limpness),
behaviours, sensations or states of awareness. Seizures may range from focal
(involve one area of your brain) or generalized (involve all areas of the brain). In
postpartum seizures are most common during the first 48 hours after delivery.
However, sudden seizures can come up at any time from delivery up to 6 weeks
after delivery.Symptoms of seizures in postnatal period
Postpartum seizures start from prodromal or early signs (Aura)that indicate that the
patient is going to enter in convulsion status. Those symptoms include:• Fear and anxiety
• Vertigo,
• Visual illusions, including flashing bright lights, spots, or wavy lines and• Nausea.
After aura, the mother may experience the followings:
• Uncontrolled convulsions,During a seizure, a woman with eclampsia has a type of seizure called a grand mal
• Rapid eye movements or staring,
• Sudden falling, stiffening of the body,
• Confusion,
• Uncontrolled convulsions,
• Loss of bladder or bowel control,
• Temporary stop in breathing,
• Entire body shaking,• Mood changes
seizure, which begins with a sudden loss of consciousness. Throughout the first 15
to 30 seconds of a seizure, the entire body stiffens as the muscles contract. The
back and neck arch. The woman may cry out as the vocal cords contract or may
turn blue if she is having difficulty breathing.
During the next 30 to 45 seconds, the muscles jerk, or convulse, in a rhythmic
pattern. While the muscles are jerking, the woman may bite her tongue or lose
bladder or bowel control. An entire seizure lasts 1 to 2 minutes or longer. After the
seizure, the woman will be unresponsive at first but will gradually wake up within
10 to 15 minutes. She may be sleepy, confused, or dazed. She may also feel tired,
weak, or moody and may have a headache and muscle aches for the next 24 hours.
Causes of seizures
Seizures are episodes of disturbed brain activity that cause changes in attention
or behavior. Among the causes of postnatal seizures are the following; toxemia of
pregnancy ( preeclampsia and eclampsia), drug abuse, epilepsy, high fever, head
injury, heart disease, stroke, poisoning, very high blood pressure, brain tumor.
Preeclampsia: is a pregnancy related complication characterized by high blood
pressure and signs of damage to another organ system, most often the liver and
kidneys. Preeclampsia usually begins after 20 weeks of pregnancy in women whoseblood pressure had been normal.
Eclampsia: is the new onset of seizures or coma in a pregnant woman withpreeclampsia. These seizures are not related to an existing brain condition.
Table 2.4: Causes of postpartum seizures
Diagnosis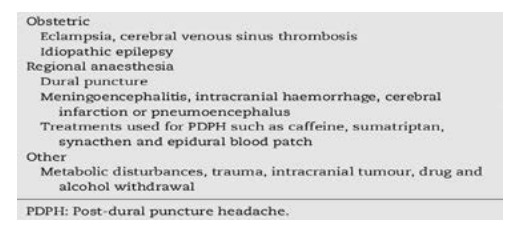
Seizures in postnatal period to the mother can be diagnosed according to the
following: Clinical manifestations, Routine blood tests, and urinalysis, Magnetic
resonance imaging (MRI) or computerized tomography (CT) scans in order to
evaluate your brain activity.
Preventive measures and management of seizures
An accurate diagnosis is important as many of these conditions are life-threatening
and require specific treatment. Convulsions in postpartum period should be treated
as eclampsia until proven otherwise. However, opportunities to identify other causes
of convulsions should be vigorously pursued.
If the mother has postpartum preeclampsia, the following treatments might be
prescribed: blood pressure lowering medicine (nifedipine), anti-seizure medicine,
such as magnesium sulfate.Self-assessment 2.4
1. Briefly state the risk factors of seizures in postpartum period.2. Identify 5 signs of seizures in postpartum period are
2.5 Nursing management of the mother with seizures in thepostnatal period
Learning Activity 2.5
Read the following case study and try to think about it.
I G is 30 years P4 in room 245 postpartum delivered by spontaneous vaginal
delivery with history of pre- eclampsia she delivered a baby boy in good condition
at 36 weeks of pregnancy, it’s now 3 hours, when nurse arrived in her room
noticed that mother is having convulsions.c) After reading this case study what do you think about it?While managing postpartum seizures, the first associate nurse ‘responsibility is tod) What do you think about this mother’s safety?
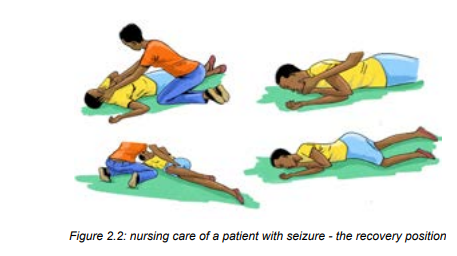
do the following:• Ensure the patient’ safety (it is one of the main considerations during seizure• Remember DRSABC: (Danger; Response; Send for help; Airway; Breathing;activity)
Circulation)
• Stay with the patient and call for help.
• Time the seizure and note its characteristics
• Protect the patient’s head, especially with any convulsive movements
occurring that may injure the patient.
• The nurse can protect the patient from harming themselves by placing
something soft under their head and shoulders.
• The surrounding area must be made clear to decrease the risk of injury,
however, do not try to physically restrict the movement of the patient’s limbs as
this can cause musculoskeletal damage, Do not put anything in the patient’s
mouth or attempt to move them.
• As soon as you are able to do so, roll the patient onto their side in the recovery
position to prevent aspiration due to excessive saliva production and ensure
their airway remains patent. If the patient has vomited or has food or fluids in
their mouth, it is crucial to do this immediately.
• Clean and clear the mouth and nose and provide oxygen
• Monitoring of vital signs is imperative, especially respiratory function.
• Following the seizure, manage any resulting injuries.
• Continue to monitor the patient’s airway, using suction as needed, and do not
disturb the patient if they fall sleep.
• When she wakes, calmly tell her where she is and she is safe.
• Provide reassurance, as this can understandably be quite distressing for the
patient
• Frequent monitoring of vital signs and neurological observations will need tobe performed in order to monitor the patient’s condition.
Self-assessment 2.5
1. What are the common causes of seizures in postnatal period?
2. Describe the nursing management of seizures in postnatal period.3. How should seizures in postpartum be treated?
2.6 Fast or difficult breathing as an obstetric danger sign in thepostnatal period
Learning Activity 2.6
 a) Basing to your observation, what do you think that can be one of theAcute dyspnea after delivery is a common symptom that can signify a wide variety
a) Basing to your observation, what do you think that can be one of theAcute dyspnea after delivery is a common symptom that can signify a wide variety
postnatal obstetric danger signs?
b) What do you think about the position that can be given to the mother with
difficulty of breathing in postpartum?
c) What do you think about oxygen administration to that mother?
of underlying etiologies.
Signs and symptoms of fast/ difficult breathing
A mother with fast breathing may present with some of the following signs andsymptoms:
• Increase in number of breaths/minute (it means that the person is havingCauses of fast or shortness of breath in postpartum period
trouble breathing or not getting enough oxygen.
• Skin color changes.
• Grunting or wheezing, and nasal flaring.
• Other signs accompanying shortness of breath include: coughing up blood,dizziness, and feeling faint.
Acute dyspnea after delivery is a common symptom that can signify variety of
underlying etiologies like: thromboembolism like thrombus and pulmonary embolism,
pulmonary edema, cardiomyopathy. I t can also be due to fluid accumulation in thelungs.
Diagnosis of difficulty in breathing in postnatal period
Clinical manifestations, laboratory investigations like FBC, Imaging like chest x-rayand CT scan.
Management of fast/ breathing difficulties
Position the mother in semi sitting position, monitor vital signs closely if the oxygen
saturation is below the 90%, the mother has to receive oxyenotherapy, encourage
the mother to perform regular breathing exercises. Request the mother to report
any breathing difficulties during this kind of exercise and manage according to thecause.
Self-assessment 2.6
1. What are signs and symptoms of fast breathing of a mother in postpartum
period?
2. What are the laboratory investigations that can be done?
3. Explain the management of fast breathing of a mother in postpartumperiod?
2.7 Pathogenesis, causes, symptoms and management ofpuerperal fever
Learning Activity 2.7
 a) By observing images above what do you think will be the condition?
a) By observing images above what do you think will be the condition?b) What do you think about this patient will present?
a. Pathogenesis
Postpartum fever (Puerperal fever) is defined as a temperature of 38.7 degrees
C (101.6 degrees F) or greater for the first 24 hours or greater than 38.0 degrees
C (100.4 degrees F) on any two of the first 10 days postpartum. It often results
from endometritis but can also be caused by urinary tract infection, wound infection
or phlebitis. The most common symptoms of postpartum illnesses are high fever
(21%), heavy vaginal bleeding (14%), and foul smelling vaginal discharge (10%),
and breast problems (18%).
b. Causes of fever in post-partum
The most common causes associated with postpartum fever are endometritis
(higher among patients who have a cesarean delivery, compared with those
who have a vaginal delivery), wound infections (e.g., surgical site infection),
and urinary tract infections, genital tract infection (painful inflamed perineum),
Mastitis(breast inflammation caused by nipple trauma and cellulitis) , deep venous
thrombosis(Painful, swollen calf), viral infection or chest infections.
c. Signs and symptoms of postpartum fever
Clinical manifestations of puerperal fever include; fever greater than 38 o
c, chills,
feelings of discomfort or illness, headache, loss of appetite, pain in the lower
abdomen or pelvis caused by a swollen uterus, foul-smelling vaginal discharge
In addition to fever, the following signs and symptoms should prompt urgent action
or urgent referral for hospital assessment by emergency ambulance:• Pyrexia (greater than or equal to 39°C).d) Management of fever in postpartum period
• Sustained tachycardia (≥90 beats/minute).
• Breathlessness (respiratory rate ≥20 breaths/minute).
• Abdominal or chest pain.
• Diarrhea and/or vomiting - may be due to endotoxins.
• Uterine or renal angle pain and tenderness.
• The woman is generally unwell or seems unduly anxious or distressed
Management and treatment of fever will depend on the cause.• Postpartum febrile episodes in which temperatures are less than 38.4 degrees
C (101.1 degrees F) often resolve without intervention, especially when they
occur in the first 24 hours after delivery.
• Treatment options for patients whose febrile episodes do not resolve
spontaneously or are higher than 38.7 degrees C (101.6 degrees F) during
the first 24 hours or higher than 38.0 degrees C (100.4 degrees F)
• General measures must be used: Ice packs may be helpful for pain from
perineal wounds or mastitis. Rest and adequate fluid intake are required,
particularly for mothers who are breastfeeding
• Pharmacological
• Administration of broad-spectrum antibiotics is recommended (Antibiotics
should be commenced after taking specimens and should not be delayeduntil the results are available).
Attention: Breastfeeding limits the use of some antimicrobials; hence, the advice of
a consultant should be sought at an early stage.Administration of antipyretic and analgesia may be required.
Self-assessment 2.7
1. What are the causes of fever to the mother in postpartum period?
2. What are the signs of fever to the mother in postpartum period?
3. Explain the possible management of fever to the mother in postpartumperiod?
2.8 Nursing intervention and prevention of puerperal fever
Learning Activity 2.8
Read the following case study and try to answer questions
MK 27 years readmitted in postpartum ward with temperature of 39.5oc on
D5 post caesarian section delivery, presenting chills loss of appetite and pain,
swelling S at surgical site, feeling un well and these symptoms started 3days
ago, her bay is well feeding on breast.
a) what do you think are interventions that an associate nurse must do for
that patients to relieve fever?b) what do you think can be the cause of fever to this mother in scenario?
Nursing intervention during puerperal fever• The associate nurse must play essential role in management of puerperal
fever. Therefore, the following are essential interventions and their rationale
for the associate nurse in management of puerperal fever:
• Review prenatal, intrapartum, and postpartum record. This helps to identify
factors that place client in high-risk category for development/spread of
postpartum infection.
• Demonstrate and maintain a strict hand-washing policy for staff, client, and
visitors. It helps prevent cross-contamination
• Instruct the proper disposal of contaminated linens, dressings, and peripads.
Maintain isolation, if indicated. It helps preventing the spread of infection
• Demonstrate correct perineal cleaning after voiding and defecation,
and frequent changing of peripads. Cleaning removes urinary/fecal
contaminants. Changing pad removes moist medium that favors bacterial
growth
• Demonstrate proper fundal massage. Enhances uterine contractility;
promotes involution and passage of any retained placental fragments
• Monitor temperature, pulse, and respirations. Note presence of chills
or reports of anorexia or malaise. Elevations in vital signs accompany
infection; fluctuations, or changes in symptoms, suggest alterations in client
status.
• Observe perineum/incision for other signs of infection (e.g., redness, edema,
ecchymosis, discharge and approximation [REEDA scale]). Allows early
identification and treatment; promotes resolution of infectionday. Note urine output, degree of hydration, and presence of nausea, vomiting,• Monitor oral/parenteral intake, stressing the need for at least 2000 ml fluid per
or diarrhea. Increased intake replaces losses and enhances circulating
volume, preventing dehydration and aiding in fever reduction.
• Encourage and or help the patient to be in semi-Fowler’s position. Enhances
flow of lochia and uterine/pelvic drainage.
• Promote early ambulation, balanced with adequate rest. Advance activity
as appropriate. It increases circulation; promotes clearing of respiratory
secretions and lochia drainage; enhances healing and general well-being.
Note: Presence of pelvic/femoral thrombophlebitis may require strict bed rest.
• Investigate reports of leg or chest pain. Note pallor, swelling, or stiffness
of lower extremity. These signs and symptoms are suggestive of
septic thrombus formation.
• Recommend that breastfeeding mother periodically check infant’s mouth for
presence of white patches. Oral thrush in the newborn is a common side effect
of maternal antibiotic therapy
• Instruct in proper medication use (e.g., with or without meals, take entire course
of antibiotic, as prescribed). Oral antibiotics may be continued after discharge.
Failure to complete medication may lead to relapse
• Discuss the importance of pelvic rest as appropriate (avoidance of douching,
tampons, and intercourse). Promotes healing and reduces the risk of
reinfection
• Ensure laboratory studies results are available. Helps identifying infectious
process/causative organism and appropriate treatment
• Encourage application of moist heat in the form of sitz baths and of dry heat
in the form of perineal lights for 15 min 2–4 times daily. Water promotes
cleansing. Heat dilates perineal blood vessels, increasing localized blood
flow and promotes healing.
• Demonstrate perineal application of antibiotic creams, as appropriate. It helps
eradicating local infectious organisms, reducing risk of spreading infection
• Administer medications as indicated (Antibiotics, oxytocics, such as Pitocin)• Arrange for transfer to intensive care setting as appropriate. May be necessary
for client with severe infection (e.g., peritonitis, sepsis) or pulmonary emboli.• Assist with procedures, such as incision and drainage (I&D) if necessary.
Prevention of puerperal fever
• Scrupulous attention to hygiene should be used during all examinations and
use of instrumentation during and after labour.Self-assessment 2.8• The use of prophylactic antibiotics during prolonged labour or caesarian• Any infection identified during pregnancy or labor should be treated
section should be done.
• Catheterization should be avoided where possible or should be done with
strict hygiene.
• Perineal wound should be cleaned and sutured as soon as possible after
delivery.
• All blood losses and the completeness of the placenta should be recorded at
all deliveries.
• Early mobilization of delivered mothers will help to protect against venous
thrombosis.
• New mothers should be helped to acquire the skills required for successful
hygiene, and breastfeeding in order to reduce the risk of mastitis and otherpossible infections.
1. Why the associate nurse must review prenatal, intrapartum, and postpartum2.9 Postpartum hypotension
record while managing puerperal fever?
2. Why the associate nurse must promote early ambulation, balanced with
adequate rest while managing puerperal fever.
3. Enumerate at least 5 measures that an associate nurse can do to preventpuerperal fever
Learning Activity 2.9
Read the following case study on one of the obstetric danger signs and try to think on it.
A 34 years old mother; Para 1, at 8 hours post normal delivery developed sudden
dizziness, generalised body weakness and feeling like going to faint while sitting on her
bed. Her vital signed showed that BP; 86/48mmHg, pulse; 118beats per minute, SPO2;
96%, body temperature; 36oC, respiration rate; 18 cycles per minute.
The associate nurse was told that the mother experienced unusual vaginal bleeding
2 hours post-delivery and the whole pamper was soaked unfortunately the bleeding
stopped after receiving misoprostol.a) What do you think to be the condition for this mother?After childbirth, the blood pressure remains about the same as it was during labour,
b) After reading this case study, what do you think can be the cause of the abovecondition?
and the pulse gradually decrease. A low blood pressure is helpful in diagnosing
potential complications such as hemorrhaging or spinal anesthesia complications.
Severe hypotension is related to shock. Shock occurs when vital organs do not
get the blood and oxygen they need to function properly. Severe hypotension, in
postnatal period can be life-threatening if not treated promptly. When the maternal
blood pressure suddenly drops in postnatal period, for whatever reason, it can havefrom short to long term harmful effects to the mother.
Signs and symptoms of hypotension
Signs and symptoms of postpartum hypotension include the following:• Severe lightheadedness when standingCauses of hypotension in postpartum period
• Dizziness.
• Feeling sick.
• Blurred vision.
• Generally feeling weak.
• Confusion.• Faintness
• Severe postpartum hemorrhageManagement of postnatal period hypotension
• Inadequate intake of fluids
• Severe nauseous and vomiting• spinal anesthesia
The management will depend on the underlying cause of hypotension. Treatment
could include:• medications for heart disease, diabetes, or infectionSelf-assessment 2.9
• Assist and encourage drinking plenty of water to avoid hypotension due to
dehydration
• Provision of IV fluids (normal saline)
• Blood transfusions in case of severe postpartum related to hypervolemia
caused by postpartum hemorrhage
• Encourage the patient to take salty food
• Taking and monitoring frequently blood pressure and pulse rate of the patient• Take safety measures to avoid risks for falling.
1. What are the signs and symptoms of hypotension in mothers during2.10 Assessment of the severe headache as an obstetric danger
postnatal period?
2. What are the causes of hypotension in mothers during postnatal period?
3. Explain briefly what will be done in case the postpartum hypotension isdiscovered to the mother
sign in the postnatal period.
Learning Activity 2.10
Look at the following picture and try to think on this obstetric danger sign.
 a) What do you think that can be the obstetric danger sign basing on thePostpartum headache or postnatal headaches refers to the appearance or increase
a) What do you think that can be the obstetric danger sign basing on thePostpartum headache or postnatal headaches refers to the appearance or increase
above image?b) What do you think about the link of above condition in postnatal period?
in headaches in women who have just had a baby, typically within the first six weeks
after they deliver. Headaches affect approximately 40% of women in the postpartum
period and are more common in women with a prior headache history, older age,
increased parity, or a shorter second stage of labor. Postnatal headaches areclosely linked to significant oestrogen and progesterone levels drop after delivery
Types of postpartum headaches
There are primary headaches and secondary headaches. Both can happen in the
postpartum period.
A primary headache is not caused by another condition. The pain can be hard to livewith, but the headache is not dangerous. In in this headache, the brain can’t sense
pain, the pain felt by the client is caused by swelling in blood vessels, muscles, and
nerves of the neck and head. Primary headaches are divided into:• Migraines: Typically felt on one side of the head and they cause throbbingA secondary headache is more serious. They usually come from underlying condition
pain, nausea, and sensitivity to light, noise, and smells.
• Tension headache: This usually includes the pain on both sides and sometimes
sensitivity to light and sound.
• Cluster headache: Often felt on one side of your head, behind one eye. It can
happen at the same time of day for several weeks.
• Hypnic headache: This occurs at night, typically in people between the agesof 40 and 80.
cause severe pain. They trigger pain in your neck and head, like; Head injury, Neckinjury; Brain infection; Brain tumor; High blood pressure; Aneurysm; etc.
Causes and risk factors of postpartum headaches
Almost half of all women have a headache in the first few weeks after they give birth
to their baby, and it’s especially common in the first week. Causes of postpartum
headaches include: A sharp drop in hormones, Not enough fluids, Not eating
enough, Not enough sleep, Muscle tension from pushing out your baby, High
blood pressure, Preeclampsia (high blood pressure in pregnancy), Sinus infection,
Blood clot, Major bleeding, Having an epidural or spinal anesthesia, cortical veinthrombosis, some medications, caffeine withdrawal.
Patterns of headaches to be reported immediately
Although headaches are a relatively common occurrence in postnatal period, the
following are patterns of headache that should be reported immediately to the
senior or transferred to high level of care: are severe, peak in intensity after a short
period of time, are accompanied by other concerning symptoms like fever, neck
stiffness, nausea or vomiting, visual changes, or cognitive problems, change over
time or when the patient moves into a different position, wake the patient up fromsleep, occur after physical activity
In addition, the sharp drop in estrogen and progesterone levels after delivery can
also cause postpartum night sweats. A combination of hormone changes, waterloss from sweating, and not enough sleep can cause a postpartum headache.
Women with headaches before being pregnant, older, or have had many births, arealso at risk of having a postpartum headache.
Self-assessment 2.10
1. What are the causes of headache to the mothers in postpartum period?
2. Explain the types of headache to the mothers in postpartum period.3. What are the mothers that are more likely to have postpartum headache?
2.11 Management and prevention of postpartum headaches
Learning Activity 2.11Read the case and answer questions in the box
a. What do you think that can be the treatment of her headaches?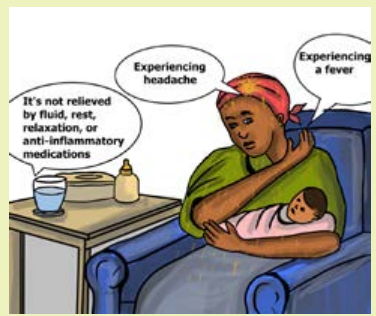
b. What do you think can be done to prevent this headache for next time tothis mother?
Management of postpartum headaches
Management of postpartum headaches varies and most of the time depend on
severity and cause the headache. In addition, most often, postpartum headaches
can treat at home. But, more severe secondary headaches should be seen by the
doctor immediately and may require a higher level of treatment to prevent moreserious symptoms or complications from occurring.
Tension and migraine headaches can be treated with over-the-counter non steroidal
anti-inflammatories, such as naproxen (Aleve) and ibuprofen (Advil). Most of these
are safe to take while breastfeeding, with the exception of aspirin. Beyond analgesia,
the bed rest and intravenous hydration, and caffeine supplementation are also
methods of management of postpartum headaches in health setting area. Patients
who do not respond to the treatment within 48 hours require a quick transfer to thesuperior level of care.
The treatment of secondary causes of headache in the postpartum period often
requires collaboration with consulting services both for acute management and risk
factor modification. Headaches caused by preeclampsia resolve with treatment
of the condition, including initiation of magnesium sulfate and anti-hypertensive
medications and admission to an obstetrics service for monitoring.
Ischemic and thrombolytic related headache the management will be done with
the aid of the cardiologist and neurologist. For puerperal stress related headache,
the management can be done through psychological counseling and relationtechniques.
Prevention of postpartum headache
For the side of health care provider:• Prompt recognition of vital sign abnormalities and risk factors assessmentTaking of self-care is an important way to prevent tension and migraine headaches.
by nursing and immediate physician notification can help reduce delays in
diagnosis or misdiagnosis.
• Identification of social stressors contributing to or causing the patient’s
presentation with subsequent referral to case management professionals or
social support services prevent bounce-back visits and readmission.
• Recognition of traumatic causes of headache by members of the healthcare
team can lead to a referral to resources for safe-houses .
• Assisting the patient to get enough and adequate fluids and food can help
reducing risks of postpartum headaches.For the side of the patient
Here are some tips to teach the patient for preventing the occurrence of primary
headaches:• Get enough rest: Try to take naps when the baby naps and ask the partner or
a friend to watch over the baby between feedings.
• Drink plenty of fluid: Put a large water bottle around or make sure you have a
glass of water by your side.• Eat healthy foods regularly: Stock the refrigerator and pantry with nutritiousSelf-assessment 2.11
foods that are convenient to prepare and eat.
• Try to relax in order to reduce stress: Take an easy walk, read a book, or chatwith a friend to alleviate stress.
1. Explain briefly the management of puerperal headaches.2.12 Blurred vision as an obstetric danger sign in the postnatal
2. What are the tips of education that can the associate nurse teach thepatient in order to prevent puerperal headaches?
period
Learning Activity 2.12
Read the following case study for the mother with postnatal obstetric danger
sign.
A 26 years old mother arrived at accident and emergency department at 8th day
of postpartum period. This mother delivered by c/section and on arrival, she was
complaining of severe headache, unable to see variety of things clearly, during
assessment, the associate nurse asked this mother to state what he was holding
in his hand and the mother responded that she was not seeing it clearly. Then he
rushes to take vital signs of this mother; the findings were: BP: 154/102 mmHg,
Pulse rate: 101 beats/ minute, respiration: 20 cycles, body temperature: 36.2 o
c,
oxygen saturation: 98%, pain score: 3/10.a) After reading the scenario above, what do you think about this motherPhysiology of vision after delivery
condition?b) What do you think can be done to this mother?
A woman’s body goes through a lot of changes during and after pregnancy, and
hormones are responsible for these changes. One such change that most new
mothers would notice is related to their vision. The changing levels of hormones and
fluids within the body can cause changes in vision. About fifty percent of pregnant
women are prone to these changes. Changes in vision become more prominent
in the second trimester and postpartum. Hormonal changes can also lead to dry
eyes after pregnancy. Most of the changes abate the vision and the vision becomenormal after a few months of childbirth.
Postpartum blurred vision is defined as a type of vision impairment that affects
the sharpness or focus of an image and experience a decreased clarity in vision
after delivery. The frequency of blurred vision depends on the underlying cause and
may only occur in certain situations. The intensity also varies and can be unilateral
or bilateral with other visual distortions.Causes of blurred vision in postpartum period
Postpartum blurred vision is caused by hormonal changes after delivery. However,
it may also be due to a cause not related to pregnancy or postpartum changes. The
following are some causes or risk factors of postpartum blurred vision:• Preeclampsia (Due to high blood pressure, there is CNS irritation or cerebralSymptoms of blurred vision in postpartum period
edema which result in blurred vision)
• Gestational diabetes (due to diabetes, the blood vessels attached to the
retina may get damaged. This affect the eyesight and cause blurred vision)
• Pituitary Adenoma (tumor in the pituitary gland of the women may alter the
functioning of the hormone secretion and lead to vision problems)
• Lower Fluid Retention (After delivery, the fluid retention capacity of a woman’s
eye ducts lowers. This can alter the shape of the cornea, leading to blurred
or distorted vision).• Certain medications
The symptoms of postpartum vision loss or eye problems include:• Sensitivity to light: Bright lights may irritate the eyes.Management of blurred vision
• Dizziness: Blurred vision may lead to a feeling of dizziness and nausea.
• Double vision: Outlines may seem blurred and the mother might see images
overlapping.
• Intermittent blur: This can happen occasionally, where certain things, like
road signs, appear blurred.
• Strain on eyes: The eyes will feel tired and stressed all the time.
• Flashes and floaters: Bright flashes of light or wavy lines in the sight of the
vision and may appear due to retinal detachment, caused by strained pushingduring labour.
Postpartum vision problems rarely cause permanent vision changes after pregnancy.
Many of the changes can go back to normal a few months after the baby is born.
But, in a few women, this warrants a new prescription, due to permanent changes
in vision.
Despite best way to manage blurred vision is to avoid triggers and making
some simple changes can make vision clear again, the following are some tips of
postpartum blurred vision management.
For Dry Eyes
Dry eyes can be one of the main reasons for blurred vision. saline drops, like the
ones used by contact lens users.
For Blurred Vision
Blurred vision often abates after pregnancy, but if it continues, refer the patient to
the ophthalmologist to get eyes tested.
For Preeclampsia.
It is important to send the patient to the gynecologist to keep blood pressure
managed
For Gestational Diabetes.
The first step is to switch to a healthy diet and lifestyle to avoid the risk factors of
gestational diabetes. If you already have high sugar levels, the gynecologist can
prescribe medications to keep it under control.
Regardless of the cause, informing and teaching about postpartum blurred vision,it is the best way to deal with the problem.
Self-assessment 2.12
1. Define the term postpartum blurred vision2. Enumerate the symptoms of blurred vision in postnatal period.
2.13 Assessment of the signs of deep vein thrombosis (DVT) as anobstetric danger sign in the postnatal period.
Learning Activity 2.13
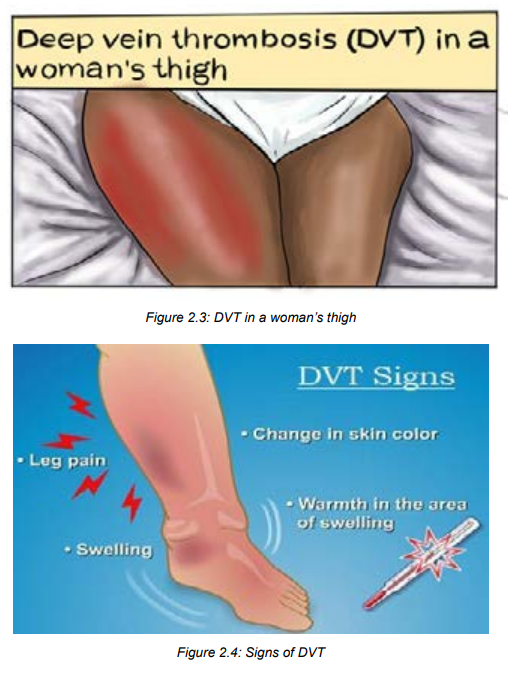
Observe the following images and start thinking on the postnatal obstetricdanger signs that this mother may present.
a) From your observation, what do you think that this mother is suffering from?
b) Have you ever come in contact with condition like this?
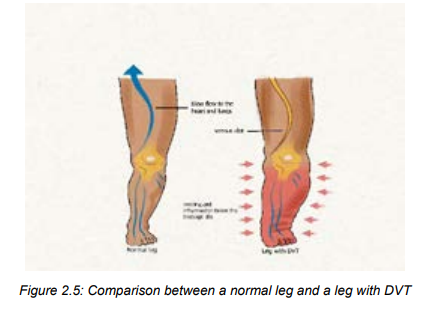
Deep vein thrombosis (DVT),is the development of a blood clot in a deep vein.
blood clots occur in a deep vein of the leg, calf or pelvis. 90% of DVTs occur in the
left leg. Deep venous thrombosis (DVT) during pregnancy is associated with high
mortality, morbidity, and costs. The risk of developing blood clots (thrombophlebitis)
is increased for about 6 to 8 weeks after delivery. Pulmonary embolism (PE), is
the most feared complication, and it is the leading cause of maternal death in the
developed world. Other complications include post-thrombotic syndrome, chronic
venous insufficiency, and vein valve destruction.
Pathogenesis of DVT
Pregnancy is a prothrombotic state; it has all components of Virchow’s triad: venous
stasis, endothelial damage and hypercoagulability. Thus, during normal pregnancy,
a hypercoagulable state is initiated. This is the most important risk factor contributing
to thrombosis (DVT after delivery). Pulmonary embolism results from the blood
clots that breaks, loose and travels through the bloodstream into the lungs, where itlodges in a blood vessel in the lung and blocks the blood lung’s flow.
DVT risk factors
The risk for DVT increases in the postpartum period. Factors that increase the risk
of developing DVT in the postpartum period include:• Cesarean sectionSigns and symptoms of deep vein thrombosis (DVT) during postpartum
• Stillbirth
• High blood pressure (hypertension)
• Eclampsia or preeclampsia
• Postpartum infection
• Obstetric hemorrhage
• Preterm delivery at less than 36 weeks
• Other underlying medical conditions (diabetes, infections, pre-eclampsia, etc)
• BMI (body mass index) of 25 or greater
• Over 35 years of age
• Smoking
• BMI of 25 or greater
• Over 35 years of age• Smoking
The most common symptoms of deep vein thrombosis during pregnancy and
postpartum usually occur in just one leg and include:• A heavy or painful feeling in the leg (a lot of people say that it feels like a really
bad pulled muscle that doesn’t go away)
• Calf or thigh is painful, tender to the touch, warm, and swollen.
• redness in the calf or thigh
• Slight to severe swelling of the calf or thigh
• A fever that develops after delivery may be caused by a blood clot.• A blood clot in the pelvis may not cause symptoms.
Self-assessment 2.13
1. Define the term deep vein thrombosis.2. What are the signs of deep vein thrombosis?
2.14 Nursing management of deep vein thrombosis as an obstetric
danger sign in the postnatal period.
Learning Activity 2.14
Read the following case study and start thinking on the management, preventionand nursing interventions that can be done
During puerperium period following caesarean section in a referral teaching hospital,
a woman a DVT with superficial blood clots diagnosis was made after finding that that
patient had unilateral leg oedema and pelvic and lower left limb pain The attending
obstetrician on duty started to tell the nurse on shift that the DVT management must be
initiated immediately. In addition, the Doctor told to that nurse that the other patient who
was lying at the opposite bed was at risk of developing DVT too. Then, the nurse was
asked to remain vigilant and start doing preventive measures to that other patient.
Based on the scenario described abovea) What do you think can be done to that mother to attenuate the pain, oedema andManagement of postpartum DVT
blood clot?
b) What do you think can be done to prevent the occurrence of DVT to that mother
lying in the opposite bed?
Early assessment of DVT risks factors and complications and prompt treatment
can keep a clot from breaking off and traveling through the circulatory system to the
lungs (pulmonary embolism). PE is the life-threatening in postpartum period.• For superficial blood clots: The associate nurse can apply warm compresses,Prevention of deep vein thrombosis
compression bandages, and elevation of the limb.
• For deep vein thrombosis or pulmonary embolism: At hospital the gynecologist
and cardiologist prescribe drugs such as: Heparin (subcutaneous) or Warfarin
Among the preventive measures for clots and deep vein thrombosis, keep the blood
flow in the following ways:• Getting plenty of pregnancy-safe exercise.Nursing interventions in management and prevention of DVT
• Encourage early ambulation
• Walking and stretching if the mother has been sitting for more than two to
three hours
• Moving the legs while the mother is sitting (elevates and lowers the heels and
then the toes).
• Taking extra precautions when the mother is on travel, including drinking lots
of water, getting up frequently to walk (or stretching the legs from a seated
position).
• Use of anti-embolism stockings for those women at risk• Encourage the woman not to smoke
The goal of nursing care for a client with postpartum DVT include enhance tissue
perfusion, facilitate resolution of thrombus, promote optimal comfort, preventcomplications and provide information and emotional support.
The following are nursing care interventions to manage and prevent
postpartum DVT:• Monitor capillary refill time; Assess for positive Homans’ sign (calf pain at
dorsiflexion of the foot)
• Assess circulation, asymmetry, sensory and motor function of extremity;
Observe edema from groin to foot; Measure and record calf/thigh circumference
of both legs as appropriate. Report proximal progression of inflammation,
traveling pain.
• Assess respiration and auscultate for lung sounds, noting crackles or friction
rub.• Investigate reports of chest pain or feelings of anxiety.
• Instruct client to avoid massaging or rubbing the affected extremity. Instruct
client to avoid massaging or rubbing the affected extremity.
• Maintain bed rest with elevation of feet and lower legs in above heart level
during the acute phase.
• Elevate client’s legs when resting or sitting in a chair. Elevate client’s legs
when resting or sitting in a chair. Elevate client’s legs when resting or sitting
in a chair.
• Instruct client to avoid crossing the legs or wear constrictive clothing. Instruct
client to avoid crossing the legs or wear constrictive clothing.
• Encourage increased fluid intake of 2500 ml/day unless contraindicated
• Emphasize the importance of deep-breathing exercises.
• Facilitate and assist with active or passive (Range of motion) ROM while on
bed rest; Assist with gradual resumption of ambulation as advised.
• Apply warm, moist compresses or heating pad to affected extremity as
ordered.
• Apply elastic support hose. Caution is advised to prevent a tourniquet effect.• Apply mechanical devices such as sequential compression stockings,Self-assessment 2.14
thromboembolic (TED) stockings as indicated.
• Monitor laboratory studies
• Administer medication as indicated• Prepare client for surgical intervention as indicated.
1. What intervention will the associate nurse do if the the superficial blood
clots are detected in postpartum?
2. How the mother moves the legs while in sitting in order to prevent
postpartum DVT?3. Enumerate at least 4 ways that can be used to prevent Postpartum DVT
2.15End unit assessment for unit 2
End of unit assessment
SECTION A
Multiple choice questions.
4. The following statements defines postpartum hemorrhage excepta) Bleeding of 350mls- 500mls following vaginal delivery and 850mls-1000mls
post caesarian section.
b) Bleeding more than 500mls following vaginal delivery and 1000mls
following Caesarean section in the first 24 hours following birth.
c) Blood loss sufficient to cause hemodynamic instability in the first 24 hours
following birth.d) A and C.2. Among the causes of postpartum heamorrhage known as 4Ts the
fallowing are not correct except.a) Tone (70%), Trauma (30%), Tissue (10%) and Thrombin (1%)3. The following are not medications used in prevention of convulsions
b) Tone (70%), Trauma (20%), Tissue (9%) and Thrombin (1%)
c) Tone (70%), Trauma (20%), Tissue (10%) and Thrombin (1%) .
d) A and C.
except.a) Nifedipine4. Acute dyspnea after delivery is a common symptom that can signify variety
b) Aldomet
c) Magnesium sulphate
d) Adalate
of underlying etiologies and can lead to low oxygen supply in the blood .
so the following measures shows you when to administer oxygen, pic the
correct answer.a) oxygen saturation of 95%5. The risk factors of postpartum hemorrhage are grouped into 2(ante natal
b) oxygen saturation of less than 90%
c) oxygen saturation of more than 90%
d) oxygen saturation of 92-94%
risk factors and intrapartum risk factors) so the following are antenatal risk
factors except.a) Antepartum haemorrhag6. The most feared complication of the Deep Venous thrombosis (DVT):
b) Previous macrosomic baby above 4500g
c) Incomplete 3 rd stage of labor.
d) Polyhyramnios.a) DeathANSWER THE FOLLOWING STATEMENTS BY TRUE OR FALSE.
b) Pulmonary embolism (PE)
c) Chronic venous insufficiency
d) Vein valve destruction.
7. Bleeding disorder occurs when there is a failure of clotting is called embolism.
8. Sheehan syndrome is defined as postpartum pituitary necrosis secondary to
postpartum hemorrhaged.
9. The type of headache typically felt on one side of the head and they cause
throbbing pain, nausea, and sensitivity to light, noise, and smells is called
Tension headache.
10. The type of headache characterized the pain on both sides and sometimes
sensitivity to light and sound is called Migraine headache.
11. The type of headache often felt on one side of your head, behind one eye iscalled Cluster headache.
SECTION B: Short answer questions.
12. Define the term postpartum blurred vision.
13. Describe general measures to be used while managing puerperal fever
14. Describe the pharmacological method while managing puerperal fever
15. In assessing puerperal fever for the mother, what are the signs and symptoms
that should prompt urgent action or urgent referral for hospital assessment?
16. What will the associate nurse suspect if he/she finds the blood pressure of
60/30 mmHg associated with severe lightheadedness and vomiting? The blood
loss amount after delivery is < 500ml and a caesarian section was done to the
mother.
17. Explain Flashes and floaters
18. What is the cause of Flashes and floaters?
19. Why the associate nurse must monitor oral/parenteral intake, assessing the
need for at least 2000 ml fluid per day?
20. Enumerate at least 5 interventions that the associate nurse can do in
management and prevention of postpartum DVT.
