UNIT 7 NURSING ASSESSMENT OF CARDIO VASCULAR SYSTEM
Key unit competence
Take appropriate action based on findings of nursing assessment of cardio vascular
system
Introductory activity 7.0Observe the image below and respond to the asked questions;
1. Look on the image A and interpret the status of the client?
2. Look on image B:
Where are these two people?
What is the person with white coat doing?3. What is the relationship between B and C
7.1. Specific history taking on cardiovascular system
Learning activity 7.1
1. The images above show the nurse and the client who is complaining for
heart problems.
a) What are the chief complaints the client may present while consulting the
nurse?
b) Outline the questions a nurse will ask to the client for more understanding
the client’s heart’s problems?2. Explain why the history taking is important for cardiovascular assessment?
7.1.1. Specific history taking on cardio vascular system
Among the assessment techniques essential to valid diagnosis, performing a factfinding
history is a key. To obtain adequate history, providers must be well organized
attentive to the patient’s verbal and nonverbal language and able to accurately
interpret the patent’s responses to questions.
In many instances, the history may be more telling than the physical examination.
It is important to take a deep history for signs and symptoms of heart diseases but
also to alert the patient to the need for lifestyle education. The evaluation regarding
smoking, hypertension, exercise habits, diet, profession and personal life behavior
should be conducted. Many complaints are to be investigated like chest pain,
pressure or heaviness, left arm or jaw pain or numbness, dyspnea on exertion,
cough, paroxysmal dyspnea, hemoptysis, syncope, palpitations, fatigue and
edema. Complaints indicating peripheral ventricular diseases such as claudication,
skin changes especially in the lower extremities, dependent edema, or pain, also
should be investigated.
Determine the date of the last chest x-ray and electrocardiogram (EKG). Inquire
about comorbid conditions or other factors that may increase the patient’s risk forheart disease and peripheral vascular diseases.
c. Past Medical History
History of heart disease includes any previous diagnoses of congenital heart disease,
murmurs, palpitations, arrhythmias, abnormal EKGs, acute coronary syndrome,
angiography (Angiography or arteriography is a medical imaging technique used
to visualize the inside, or lumen, of blood vessels and organs of the body, with
particular interest in the arteries, veins, and the heart chambers), angioplasty(is a
minimally invasive endovascular procedure used to widen narrowed or obstructed
arteries or veins, typically to treat arterial atherosclerosis), stent placement (A
stent is a tiny, expandable metal mesh coil put into the newly opened area of the
artery to help keep the artery from narrowing or closing again), or coronary artery
bypass graft (is a surgical procedure to restore normal blood flow to an obstructed
coronary artery).
In summary: Note whether there have been any heart attacks, any history of
angina and any cardiac procedures or operations (type and date of intervention
and outcome). Previous levels of lipids if ever checked or known. Ask whether there
is any history of rheumatic fever or heart problems as a child.
d. Family History
Family history is particularly important for cardiac assessment because hypertension,
hyperlipidemia, and other vascular diseases often have a familial association that
is not easily ameliorated by lifestyle changes. If there are deaths in the family
related to cardiovascular, determine the age and exact cause of death, because
cardiovascular disease at a young age in the immediate family carries an increased
risk compared with cardiovascular disease in an elderly family member.
Ask about sudden death, which might indicate a congenital disease such as
“Marfan’s syndrome” which is an inherited disorder that affects connective tissue.
This is especially important to ask during pre-sports physicals because sudden
death in athletes is often related to congenital or familial heart disease.
7.1.2. Cardiovascular review of symptoms
The review of cardiovascular symptoms is a list of questions, arranged by
cardiovascular system, designed to uncover dysfunction and disease within that
system. A thorough history is vital for the diagnosis of patients with issues such as
chest pain, heart failure symptoms, palpitations or syncope. The most essential
questions for cardiovascular system review include the following:
• Have you had any shortness of breath? Describe features.
• Do you have chest pain or discomfort?
• Do you notice that your heart is beating faster? Are you having skipped
or extra beats?
• Have you had a loss of consciousness?
• Have you noticed any swelling in your feet, legs, or hands?
• Have you been especially fatigued or tired?
• Do you have blood in your expectoration?
• Have you had difficulty sleeping? How many pillows do you use? Do you
awaken short of breath?• Have you noticed any excessive sweating? Describe features?


Self-assessment 7.1
1. In case the client consults the health care provider for cardiovascular
problems, the health care provider should take a family history for the
following reason:
a) Family history taking concludes the cardiovascular diagnosis
b) Cardiovascular diseases often have a familial association that is not
easily ameliorated by lifestyle changes Exposure to outdoor allergens.
c) The families who have cardiovascular diseases history have the risks
to have also respiratory diseases
2. Cardiovascular past medical history involves the following except:
a) The history of congenital heart diseases
b) Cardiovascular exams taken (angiogram and electrocardiogram)
c) The habit of physical exercises
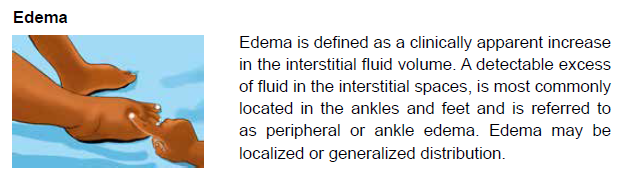
3. A clinically apparent increase in the interstitial fluid volume and detectable
excess of fluid in the interstitial spaces is most commonly located in the
ankles and feet and is referred to as:
a) General distributed edema
b) Central edema
c) Peripheral edema
4. The following are attitudes of health care provider to obtain adequate
history:
a) The provider must be well organized
b) The provider must be attentive to the patient’s verbal and non verbal
response
c) The provider must be able to interpret patient’s response to asked
questions
d) All the above
5.During cardiovascular specific history taking the questions should include
the following:
a) Smoking and diet
b) Exercise habit
c) History of intestine disorders
d) Profession and personal life behaviore) A, B, D are true
7.2.General physical examination of cardiovascularsystem
Learning activity 7.1
Analyze carefully the following images and respond to the questions below;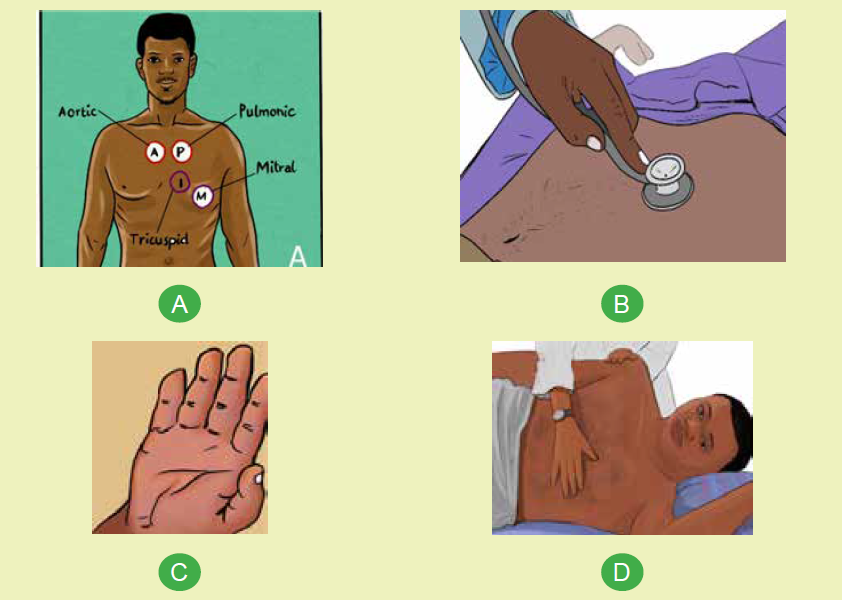
The above images show the physical examination of cardiovascular system;
a) How many heart auscultation locations shown on image A
b) The image B is showing the nurse who is auscultating the client’s heart
beat; name the equipment/material being used?
c) The image C is showing the cyanosis sign which is a bluish discoloration
of the skin due to poor circulation or inadequate oxygenation of the blood;
recall the causes of inadequate oxygenation in blood?
d) The nurse is touching on client’s chest on image D; identify what he/she
can feel on that left side of client’s chest?
The patients with impaired blood circulation may become irritable, somnolent,
restless, confused, or aggressive; the first step for a nurse is to conduct an
initial survey to determine the degree of consciousness if the patient is attentive,
cooperative, and normally oriented.
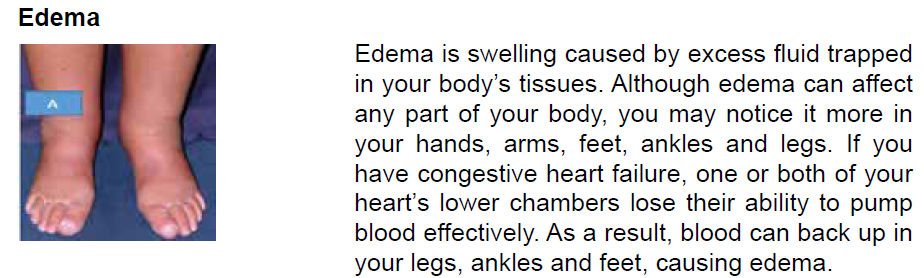
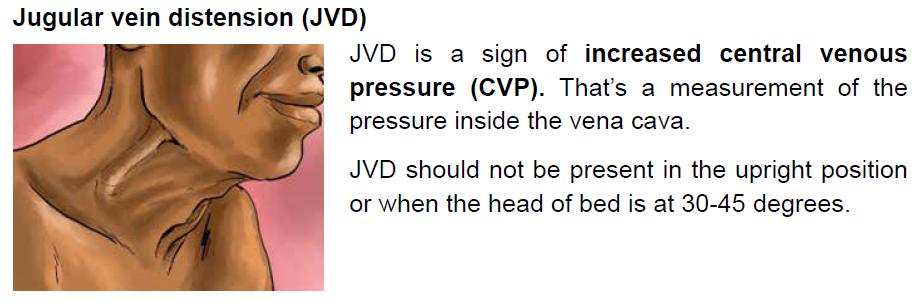
General signs of heart or circulatory disease include pallor, cyanosis, diaphoresis,
edema, restlessness, and confusion. Diminished or accentuated peripheral pulses
are indicative of Valvular Heart Diseases or tamponade. Jugular venous distention
and hepatojugular reflux suggest an increase in right ventricular pressure.The color and temperature of extremities
During general assessment, nurse may check the person’s. Color of Skin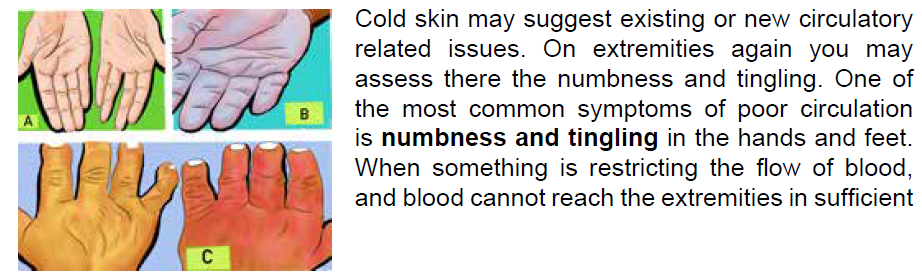
& Mucous Membrane; this may show Cyanosis (a bluish discoloration of the
skin due to poor circulation or inadequate oxygenation of the blood.) which may
suggest inadequate oxygenation and CV compromiseBlood pressure
Usually hypertension is defined as blood pressure above 140/90, and is
considered severe if the pressure is above 180/120.
High blood pressure often has no symptoms. Over time, if untreated, it can causehealth conditions, such as heart disease and stroke.
and count how many seconds until the patient’s full color returns.
• Brisk capillary refill: < (less than) 2 seconds• Delayed capillary refill: > (greater than) 2 seconds
Self-assessment 7.2
1. Explain why it is crucial to assess the level of consciousness to the client
with cardiovascular problem firstly
2. Why Capillary Refill is performed to the patient with poor blood circulation?
3. Why it is necessary to assess the skin of patient with cardiovascular
problems?
4. When you are caring the patient, you observe that he have jugular veindistension(JVD) what is the cause of this JVD ?
7.3. Focused Physical examination of cardiovascularsystem and laboratory test
Learning activity 7.3
The images below illustrate the focused cardiovascular physical exam
1. Describe what you are observing on above images A, B and C?
2. What is common between images A and B?
I. Approach to physical examination of the cardiovascular system
While the patient is in a supine or lateral position, a focused physical examination
can be used to examine the patient’s chest. Inspection, palpation, percussion, and
auscultation are the four steps or procedures used in the process.
A. Inspection
This phase/technique of assessment requires the use of the eye of health care
provider to observe the client for pallor and extremities for cyanosis. A nurse should
observe the neck for jugular vein. A thorough examination of the patient is required,
with special attention paid to short or tall stature, which could indicate Turner’s orMarfan’s syndromes, both of which are connected to congenital cardiac problems.

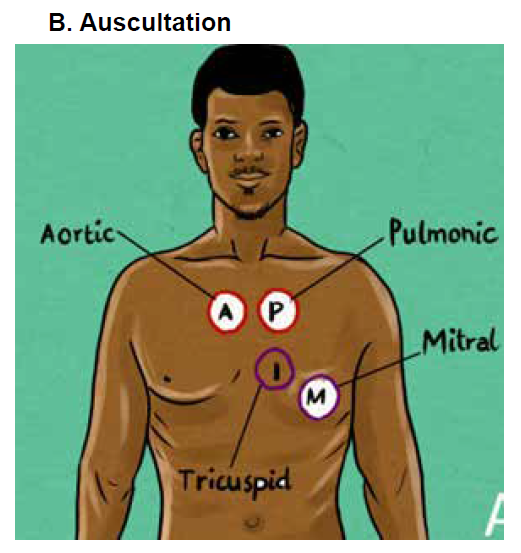
This picture is showing the Cardiac auscultation locations
The most useful element of the heart examination is usually auscultation. A
stethoscope is used to auscultation for heart sounds. Determine the heart’s rate
and rhythm first. Identify S1 (louder at the apex) and S2 (louder at the base) (heard
louder at the base). The diaphragm of the stethoscope is used to identify high-pitched
sounds, while the bell is used to identify low-pitched sounds. There are two normal
heart sounds that should be elicited in auscultation: S1 (lub) and S2 (dub).
Auscultation of Carotid artery: A carotid bruit is a vascular sound caused by
turbulent, non-laminar blood flow through a stenotic region that can be heard with a
stethoscope over the carotid artery. A carotid bruit could indicate underlying artery
occlusive disease, which could result in a stroke. Ask the patient temporarily to stop
breathing. Look for a rushing or blowing sound a bruit. Heart sounds or murmurs
coming from the chest should not be misinterpreted.
Auscultation of the heart: Listen over each of the four main heart valve areas: the
aortic, pulmonary, tricuspid and mitral valve areas. They should also listen for any
additional sounds such as clicks, and heart murmurs which are not normal.
Murmurs are produced by blood flow turbulence and are more prolonged than
heart sounds; they may be systolic
Rubs are high-pitched, scratchy sounds often with 2 or 3 separate components,
which may vary according to body position; during tachycardia, the sound may bealmost continuous.
Location of heart auscultation points

C. Palpation
Palpation of carotid artery is performed by placing the fingers just medial to the
trachea and below the angle of the jaw. The pulse should be regular in rhythm and
have equal strength in the right and left carotid arteries. Don’t palpate both carotid
arteries at the same time or press too firmly. If you do, the patient may faint or
become bradycardia.
Palpation of a sustained apical or ventricular impulse can provide information on
heart size.
• The apex beat, also known as the point of maximal impulse (PMI), corresponds
to the lower left heart border. It is the most inferior and lateral position that the
cardiac impulse can be felt.
• Locate the PMI in the fifth intercostal space in the mid-clavicular line by
counting down from the second intercostal space adjacent to the angle of
Louis.
• Palpate with the first two fingers.
• If this cannot be palpated, ask the patient to lie on his/her left side.
• The apex beat will be displaced laterally if the heart is enlarged (cardiomegaly).
• Next, palpate for heaves and thrills (a thrill is a palpable murmur).
• Place the palm of the hand in each of the four heart zones in the pre-cordium
and then on the upper left and right chest wall. A thrill feels like a vibration or
buzzing underneath your hand.
• Place the hand at the left sternal edge. A parasternal heave is a sign of right
ventricular enlargement and feels like a “lifting feeling” under the hand.
• Assess for jugular venous distention by palpating the liver while breathing
deeply because this may cause hepatojugular which is the distension of the
neck veins caused by applying forceful pressure to the liver.
• Feel the peripheral pulses at the femoral, popliteal, anterior tibial, and dorsalis
pedis locations.
D.Percussion:
Involves tapping on the surface of the body in order to determine the underlying
structure. Because of its limited sensitivity, percussion of the heart borders is rarely
used; it is replaced by x ray
II.Laboratory tests and Interpretations
Cardiovascular screenings can detect issues in major arteries before symptoms
develop, lowering the risk of heart attack, stroke, aneurysm, heart disease, and other
dangerous diseases. These laboratory tests are helpful in diagnosing, monitoring,
and treating a variety of health conditions, including heart disease.
1. Lactate dehydrogenase (LDH), normal value: 45–90 u/L
the significance is that is damaged, an enzyme is released. Hemolytic conditions,
hyperthyroidism, kidney illness, stomach cancer, and megaloblastic anemia can all
cause an increase.
2. Creatine phosphokinase (CPK), Normal value: 55–170 u/L for men; 30–
135 u/L for women
CPK is elevated in MI but not specific to myocardial damage. Also seen with skeletal
muscle damage owing to excessive exercise or rhabdomyolysis.
3. Creatine kinase-myocardial band (CK-MB), normal value: 0–3 ng/mL
the significance is This cardiac is enzyme is most sensitive in detecting myocardial
injury within the first 3 to 8 hours after onset of ischemia symptoms.
4. Troponin I (cTnI)
The normal value is < 0.35 ng/mL. This index is useful in the diagnosis of acute
myocardial injury. After 4 hours, it is equally as sensitive as CK-MB for up to 48
hours. Troponin I remains elevated longer than CK-MB and is more cardiac specific.
5. Troponin T (cTnT), normal value: <0.2 mg/L
The sensitivity of cTnT for detecting acute MI is 100% from 10 hours to 7 days after
onset. The sensitivity begins to decrease after 7 days.
6. Potassium (K+), normal value:
3.5–5 mEq/L. Above all, high K+ levels can lead to ventricular fibrillation. Wider
P waves, peaked T waves, expanded QRS complex, depressed ST-segment,
and heart block are further EKG alterations. Inverted T waves, U waves, and a
depressed ST segment are all symptoms of low K+. Patients with low K+ levels are
at risk of digitalis toxicity.
7. Sodium (Na+), Normal value:135–145 mEq.
Na+ is important for fluid balance particularly when dehydration may be an issue or
in heart failure, where Na+ less than 130 indicates a poor prognosis.
8. Calcium (Ca+), normal value: 8.5–10.6 mg/dL
The hypercalcemic effects on the heart include shortening of the QT interval and
atrioventricular block. The effect of hypocalcemia is prolongation of the ST-segment.
9. Glucose, normal value: 70–100 mg/dL
Changes in blood glucose can have indirect effects on the heart. Diabetes
significantly increases the risk for MI and hyperlipidemia.
10. Creatinine, normal value: 0.6–1.2 mg/dL
Chronic renal illness can raise blood pressure, increasing the risk of cardiovascular
and cerebrovascular disease over time. When prescribing certain drugs for
hypertension and heart failure, such as ACE inhibitors and diuretics, the level of
creatinine is also significant. If the creatinine level is higher than 1.5, a loop diuretic
should be used instead of a thiazide diuretic.
11. Cholesterol, normal value: Total, < 200 mg/dl, LDL, < 130 mg/dL HDL,
> 40 mg/dL
Increased total and LDL cholesterol, as well as lower HDL, raise the risk of coronary
artery disease. Obesity, thyroid problems, or a high-fat diet may be the cause, which
can be hereditary or acquired.
12. Triglycerides, normal value: < 150 mg/dL
Elevated levels increase the risk for heart disease.
13. Thyroid-stimulating hormone (TSH), normal value: 0.4–4.2 mIU/L
Hypothyroidism in the elderly may lead to the development of HF. In adults over the
age of 50, hyperthyroidism can manifest as atrial fibrillation or other arrhythmias.
14. Hemoglobin (Hgb), normal value: 11.5–15 g/dL
Many types of cardiac disease can cause or be caused by anemia.
15. Hematocrit (Hct), normal value: 34%–44%
Anemia may be a cause or a result of many forms of heart disease.
16. Oxygen saturation, normal value: 95%–97%
Pulse oximetry can be used to assess clinical state in individuals with severemyocardial injury and HF.
Self-assessment 7.3
1. Explain element which is most useful during cardiovascular physical
examination
2. Patient with cardiovascular problem may have hypoxia, what will you
focus on the skin during inspection
3. Explain why it is important to know Hemoglobin to the patient who have
cardiovascular problems4. What do you understand with the term hepatojugular
7.4. Interpretation of specific findings on cardiovascularsystem
Learning activity 7.4
The above images B and C show the abnormal hearts and a nurse who is
interpreting heart sounds with stethoscope;
1) Recall the heart normal findings from auscultation
2) Recall the heart normal findings from inspection
3) List the cardiovascular abnormal findings from palpation
The image A is showing a nurse taking hematologic sample;
1) What is normal value of hemoglobin?2) What is the condition which can cause a decreased level of hemoglobin?
7.4.1. The normal findings and abnormal findings fromcardiovascular physical examination

7.4.2. Normal heart sounds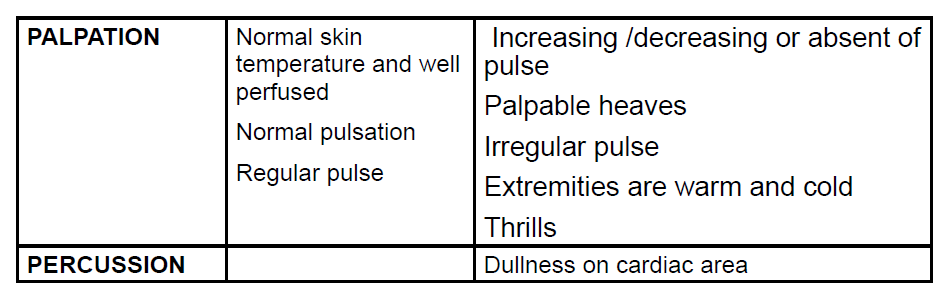
Normal heart sounds are S1 and S2. Identify S1 as lub and S2 as dub. S1 is heard
in the tricuspid area. S2 signals the end of systole and beginning of diastole as the
aortic and pulmonic valves close.
S1 is generated by vibrations created by the closing of the mitral and tricuspid
valves in the heart. When the two ventricles contract and pump out blood into the
aorta and pulmonary artery, these valves close to prevent the blood flowing back
into the atria.
The ventricles relax to receive blood from the atria after pumping blood, and the
diastole phase begins. The second heart sound, S2, is produced when the aortic
and pulmonic valves close and induce vibrations. The increase in volume of this
sound could suggest a number of things.
7.4.3. Abnormal heart sounds
A heart murmur is an unusual sound heard between heartbeats.
A murmur is a blowing, whooshing, or rasping sound that occurs during your
heartbeat.
S4 in late diastole, right before S1, sounds like “lub-lub dub.” It is usually abnormal.
The third heart sound is a low-pitched sound audible with the rapid rush of blood
from the atrium into the ventricle as it starts relaxing. This may be a normal sound
in some people but in people with heart conditions, S3 may indicate heart failure
A low intensity sound heard right before S1 in the cardiac cycle is the fourth. This
sound is caused by the ventricle’s rapid slowing of blood flow as the atrial contracts,
which could be a sign of heart disease.
7.4.4. Abnormal percussion sounds
Dullness: Indicates a solid structure on the heart with a fluid-filled area occur due to
dilation of the heart chambers and to a lesser extent due to thickening (hypertrophy)
of myocardial wall. Also, it can occur to patient with pericardial effusion.
7.4.5. Abnormal findings from inspection
Chest deformity (in case of marfan syndrome) With Marfan syndrome, the heart
muscle may enlarge and weaken over time, causing cardiomyopathy, even if the
heart valves are not leaking.
Jugular vein distension: due to the increased pressure of the superior vena
cava causes the jugular vein to bulge, making it most visible on the right side of a
person’s neck.
Clubbing of Nails: This is due to chronic low blood-oxygen levels.
Edema: When the heart’s diseased or overworked left ventricle (heart’s lower
chamber) isn’t able to pump out enough of the blood it receives from the lung
Pallor: This is due to the decreased blood supply to the skin.
7.4.6. Abnormal findings from palpation
Bruits: While you are palpating each carotid artery medial to the sternomastoid
muscle in the neck. Those bruit are (swooshing sounds similar to the sound of
blood pressure) result from turbulent blood flow related to atherosclerosis.
A thrill: a vibratory sensation felt on the skin overlying an area of turbulence and
indicates a loud heart murmur usually caused by an incompetent heart valve.
Irregular pulse: This can be due to current heart attack or scarring from a previous
heart attack, locked arteries in the heart (coronary artery disease), and Changes to
the heart’s structure, such as from cardiomyopathy, diabetes, high blood pressure.
Bounding pulse: The pulse will probably feel strong and powerful if you have
a bounding pulse. You may feel the pulse in the arteries of the neck or throat.
Sometimes it can be seen as it moves the skin in a more forceful way.
Warm or cold extremities: due to the plaque buildup, blood clots or narrowed
blood vessels which lead to poor circulation. When obstacles or narrow paths slow
down blood flow, it›s difficult for the body to send blood to every part of your body
in an efficient way.
7.4.7. Abnormal cardiovascular pattern
Tachycardia: Excessive cardiac frequency, high to the normal, more than 100beatings per minutes for adult
Tachyarrhythmia: when heart beat is fast and irregular.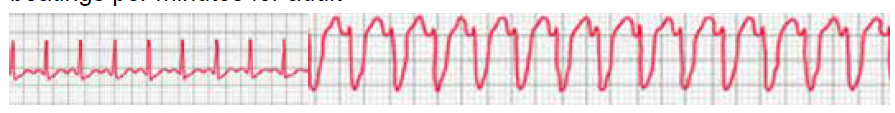
Bradycardia: Low heartbeat rate, less than 60 beatings per minute for an adultperson
Bradyarrhythmia: when heart beat is slow and irregular.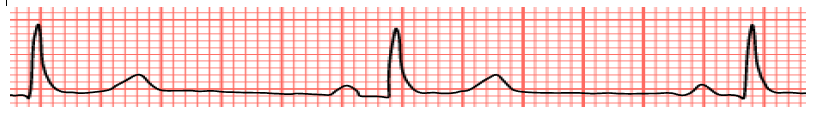
Dysrhythmia or arrhythmia: a pulse with an irregular rhythm
Bounding pulse or dense pulse: When the power of beating is exaggerated, that
means strong contractions, blood volume increases strongly, strong beatings as”
knock”
Falling, weak, depressed or thready pulse: When the pulse becomes difficult to
feel, that it is hardly audible, that means that the power of the beating is lower than
normal.
Self-assessment 7.4
1. Examination of a patient in spine position reveals distended jugular vein
from the base of neck to the angle of jaw. This finding indicates:
a) Increased pulmonary pressure
b) Muddle site heart failure
c) Increased central venous pressure
d) Decreased venous return
2. When you are auscultating the patient heart rate and rhythm you detect
twice an irregular heart beat. You should :
a) Document this normal findings
b) Schedule the patient for another appointment
c) Assess the patient for sign and symptoms of lung diseases
d) Refer the client to a physician
3. The sound generated by the turbulent flow of blood within the heart is:
a) S1
b) Murmur
c) S2
d) Diastole
7.5. Identification of client’s problems and nursing
interventions based on client’s problems
Learning activity 7.5Analyze carefully the following images and respond to the questions below;
Question 1: Describe the image A about different observations hosted in it?
Question 2: Relate the observations of image A with cardiovascular problems
identification?
Question 3: What are different nursing interventions are observed on image B
and their relation with cardiovascular system ?
7.5.1 Cardiovascular client’s problems
Cardiovascular diseases are conditions that affect the structures or functions of
heart; cardio cardiovascular diseases are the leading cause of death. It is important
for a nurse to know about hearts’ problems in order to prevent, assess or provide
nursing interventions to patients who have different heart’s problems.
Types of cardiovascular diseases can have various causes; it is better to know their
difference;
a. Abnormal heart rhythms or arrhythmias
The heart is an amazing organ. It beats in a steady, even rhythm, about 60 to
100 times each minute. That’s about 100,000 times each day. Sometimes your
heart gets out of rhythm. Your doctor calls an irregular or abnormal heartbeat an
arrhythmia. An arrhythmia (also called a dysrhythmia) can bring on an uneven
heartbeat or a heartbeat that is either too slow or too fast.
b. Aorta disease and Marfan syndrome
The aorta is the large artery that leaves your heart and brings oxygen-rich blood
to the rest of your body. The number of conditions can cause the aorta to widen or
tear. This raises the chance of things like: Atherosclerosis (hardened arteries), High
blood pressure and Connective tissue disorders.
c. Congenital heart disease
This is a problem in one or more parts of the heart or blood vessels. It happens
before birth. Genes may play a role, or it can happen if a baby is exposed to viral
infections, alcohol, or drugs before it’s born.
d. Coronary artery disease (narrowing of the arteries)
It’s when plaque builds up and hardens the arteries that give your heart vital oxygen
and nutrients. That hardening is also called atherosclerosis.
e. Deep vein thrombosis and pulmonary embolism
Blood clots can form in your deep veins, usually in your legs. This is deep vein
thrombosis (DVT). They can break loose and travel through your bloodstream to
your lungs, where they can block blood flow. This condition is called pulmonary
embolism. It’s life threatening and needs immediate medical attention.
You might be at higher risk of DVT because of your genes or family history. Other
things that can increase risk include sitting for a long time, like in a car or on a
plane; long-term bed rest; pregnancy; and using birth control pills or hormone
replacement.
f. Heart attack
A heart attack, also called a myocardial infarction, happens when a part of the heart
muscle doesn’t get enough blood.
g. Heart failure
It means your heart doesn’t pump as strongly as it should. This will cause your body
to hold in salt and water, which will give you swelling and shortness of breath.
h. Heart muscle disease (cardiomyopathy)
This is the term for diseases of the heart muscle. They’re sometimes simply called
enlarged heart. People with these conditions have hearts that are unusually big,
thick, or stiff. Their hearts can’t pump blood as well as they should. They can lead
to heart failure and abnormal heart rhythms. Cardiomyopathy may sometimes run
in families, but it can also be caused by high blood pressure, diabetes, obesity,
metabolic diseases, or infections.
i. Heart valve disease
Your valves sit at the exit of each of your four heart chambers. They keep blood
flowing through your heart. Sometimes, there are problems with these valves
j. Pericardial disease
This condition is rare and means the lining surrounding your heart is inflamed. An
infection often causes this cardiac condition.
k. Rheumatic Heart Disease
This happens when rheumatic fever, an inflammatory disease that’s most common
in children, damages your heart valves. Rheumatic fever starts with untreated strep
throat and can affect many parts of your child’s body.
l. Stroke
Strokes happen when something slows or blocks blood flow to your brain. Your
brain can’t get the oxygen and nutrients it needs, and brain cells start to die. When
blood can’t get to the part of your brain that controls a certain function, your body
doesn’t work like it should. A stroke can happen because of a blocked artery or a
leaking or burst blood vessel. It needs immediate treatment to limit brain damage
and other complications.
m. Peripheral vascular disease
Your circulatory system is made up of the vessels that carry blood to every part
of your body. Vascular disease includes any condition that affects your circulatory
system. These include diseases of the arteries that go to your legs (peripheral
vascular disease) and slow blood flow to your brain, causing strokes.
7.5.2 Nursing interventions for a client with cardiovascular
problems
Nursing Interventions
• Monitor for symptoms of heart failure. *Observe for chest pain or discomfort.
• Place patient on cardiac monitor.
• Assess blood pressure carefully
• Administer nitroglycerin with Medical Doctor order.
• Place oxygen.
• Ensure that the IV is in place for emergency use.
• Notify physician.
• Monitor edema, intake, and output.
• Weigh patient daily.
• Auscultate lung and heart sounds. *Administer diuretic with order.
• Elevate head of bed for dyspnea
• Collaborative interventions.
Self-assessment 7.5
1) Cardiomyopathy is the term for diseases of the heart muscle;
A) How is the structure of heart muscle in this condition?
B) List at least causes of cardiomyopathy?
2) Explain how does stroke happen and what can a nurse observe on
client in case of this condition?3) List the nursing interventions toward a client with cardiovascular problems?
End unit 7 assessment
Multiple choices questions
Select the bests answer, only one option is accepted:
1. Rheumatic heart disease happens when rheumatic fever, an inflammatory
disease that’s most common in children, damages your:
a) Heart valves
b) Heart ventricles
c) Heart coronary arteries
d) Heart coronary veins
2. This condition is rare and means that the lining surrounding your heart is
inflamed. An infection often causes this cardiac condition which is called:
a) Heart valves disease
b) Heart muscle disease
c) Pericardial disease
d) Myocardiopathy
3. It is important to take a deep history for signs and symptoms of heart
diseases but also to alert the patient to the need for lifestyle education.
The elements of lifestyle education include the following except:
a) Diet,
b) Smoking,
c) Exercise habits,d) Number of hospitalization
4. If there are deaths in the family related to cardiovascular, the history
taking should determine the age and exact cause of death because:
a) Cardiovascular disease at a young age have low impact in family
b) Cardiovascular disease at a young age has a chance to be cured
c) Cardiovascular disease at a young age carries an increased risk in
family
d) Cardiovascular disease in an elderly family member carries an increased
risk in family
5. Which instrument is used to listen to the heart sounds of the human body?
a) Sphygmomanometer
b) Reflex hammer
c) Stethoscope
d) Heart scope
6. While palpating the apex, left sternal border, the base in an adult client,
you detect a thrill. You should further assess the client for”
a) Pericarditis
b) Cardiac murmurs
c) Congestive heart
d) Left side heart failure
7. While assessing an older adult client, you detect a bruit over the carotid
artery. You should explain to the client that a bruit is
a) A normal sound heard in adult’s patient
b) Wheezing sound
c) Heard when the artery is almost totally occluded
d) Associated with occlusive arterial disease
8. You are planning to auscultate a female patient for carotid arteries. You
should plan to:
a) Ask the patient to hold the breath
b) Palpate the arteries before auscultation
c) Place the stethoscope over the artery
d) Ask the patient to breath as usual
9. The nurse is preparing to assess the patient with cardiovascular problem.
Which phase is most used in physical assessment:
a) Inspection
b) Palpation
c) Auscultation
d) Percussion
10. Bradycardia is a condition in which the pulse rate becomes greater than:
a) 50 beats per minute
b) 60 beats per minute
c) 90 beats per minutes
d) None of the above
Matching questions:A. Relate the heart symptom with its meaning
Short answer questions: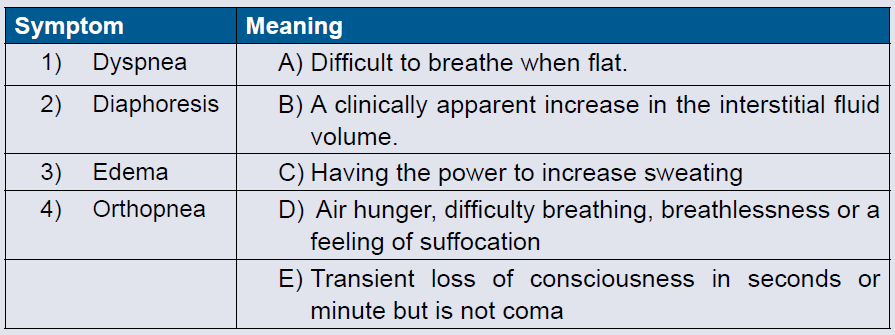
1. List four symptoms of cardiovascular problems the client can present
when is visiting clinic?
2. Label the subjective sensation of conscious perception of heart beats?
3. Recall the elements of family history a nurse should assess forcardiovascular problems?
