UNIT8:INTRODUCTION TO PALLIATIVE CARE
Apply the principles of palliative care to alleviate pain, support psychologically and
spiritually the individuals, families and community during life threatening illnessesand during end-of-life period
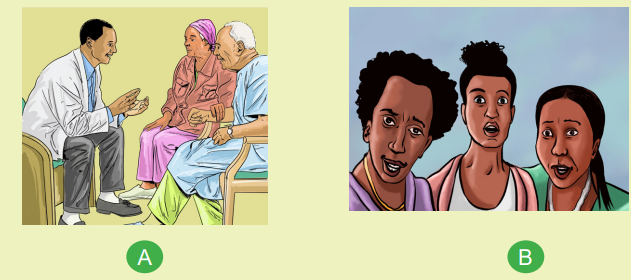
Introductory activity 8
1) What do the pictures A, B, C, D, and E have in common?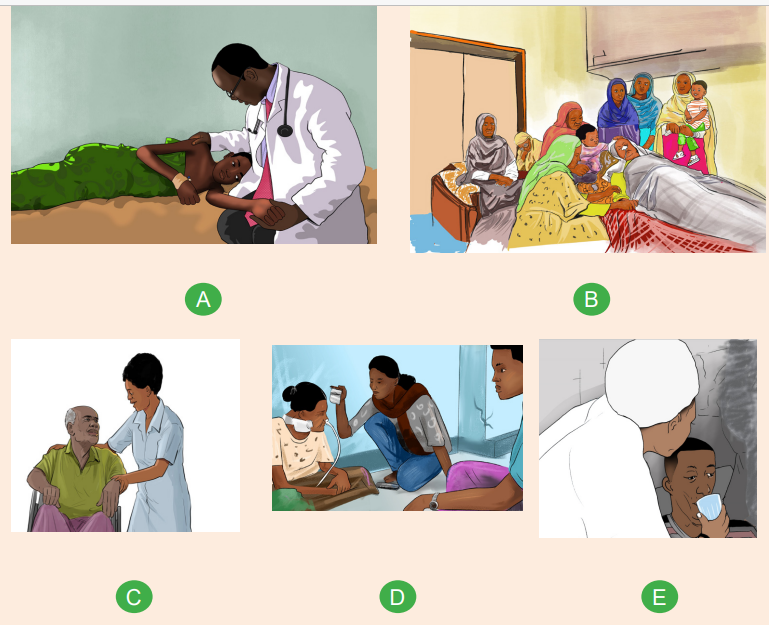
2) What do you think is the focus of this unit 8?
Definition:
The World Health Organization (WHO) defined Palliative care “as an approach
to care which improves quality of life of patients and their families facing life
threatening illness, through the prevention, assessment and treatment of pain and
other physical, psychological and spiritual problems.”
The primary goal of palliative care:
It is to help patients and families achieve the best possible quality of life.
The goals of palliative care:
For patients with active, progressive, far-advanced disease, the goals of palliative
care are
• To provide relief from pain and other physical symptoms
• To maximize the quality of life
• To provide psychosocial and spiritual care
• To provide support to help the family during the patient’s illness and
bereavement
Scope of palliative care:
Although it is especially important in advanced or chronic illness, it is appropriate
for patients of any age, with any diagnosis, at any time, or in any setting.
Patients who have complex serious illnesses often benefit from palliative care
throughout the course of their illness, even while seeking treatment for their disease.
As the goals of care change and cure for illnesses becomes less likely, the focus
shifts to more palliative care strategies. Palliative care interventions are not only
appropriate at the end of life. Making this distinction is important because some
patients, family members, or health care professionals refuse helpful palliative careinterventions, believing that palliative care is only for the dying.
to care which improves quality of life of patients and their families facing life
threatening illness, through the prevention, assessment and treatment of pain and
other physical, psychological and spiritual problems.”
The primary goal of palliative care:
It is to help patients and families achieve the best possible quality of life.
The goals of palliative care:
For patients with active, progressive, far-advanced disease, the goals of palliative
care are
• To provide relief from pain and other physical symptoms
• To maximize the quality of life
• To provide psychosocial and spiritual care
• To provide support to help the family during the patient’s illness and
bereavement
Scope of palliative care:
Although it is especially important in advanced or chronic illness, it is appropriate
for patients of any age, with any diagnosis, at any time, or in any setting.
Patients who have complex serious illnesses often benefit from palliative care
throughout the course of their illness, even while seeking treatment for their disease.
As the goals of care change and cure for illnesses becomes less likely, the focus
shifts to more palliative care strategies. Palliative care interventions are not only
appropriate at the end of life. Making this distinction is important because some
patients, family members, or health care professionals refuse helpful palliative careinterventions, believing that palliative care is only for the dying.
8.1. Historical background of palliative care
Self-assessment 8.1
1) Shortly explain at least 4 timeline of important events in the history of
palliative care
At the end of the Second World War in 1945, people in Western societies were tired
of death, pain, and suffering. Cultural goals shifted away from war-centered activities
to a focus on progress, use of technology for better living, and improvements in
the health and well-being of the public. Guided by new scientific knowledge and
new technologies, health care services became diversified and specialized andlifesaving at all costs became a powerful driving force.
End-of-life care was limited to postmortem rituals, and the actual caregiving of
dying patients was left to nursing staff. Palliative nursing in those days depended
on the good will and personal skills of individual nurses, yet what they offered was
invisible, unrecognized, and unrewarded.
Thanks to the efforts of many people across the years, end-of-life care is
acknowledged today as an important component of integrated health care services.
Much knowledge has accrued about what makes for good palliative care, and
nurses have been in the forefront of efforts to improve quality of life for patients and
families throughout the experience of illness.
The nurse gives attention to the physical, psychological, social, spiritual, and
existential aspects of the patient and family—whole person care.Below is a brief timeline of important events in the history of palliative care:
• 1967: Palliative care was born out of the hospice movement. Dame
Cicely Saunders is widely regarded as the founder of the hospice movement.
She had degrees in nursing, social work, and medicine. She introduced
the idea of “total pain,” which included the physical, emotional, social, and
spiritual dimensions of distress. Saunders opened St. Christopher’s Hospice
in London in 1967.
• 1969: Elisabeth Kübler-Ross published her book On Death and Dying. In
this book, she defined the five stages of grief through which many terminally
ill patients progress: denial, anger, bargaining, depression, and acceptance.
Although we now believe dying patients do not necessarily go through these
phases and that these phases do not necessarily occur in a set order, Kübler
Ross’s book and lectures raised public consciousness about care for patients
at the end of life.
• 1974: Florence Wald, the dean of Yale School of Nursing, was so inspired by
a lecture by Dr. Saunders at Yale that she went to visit St. Christopher’s in
1969. Florence Wald then founded the first hospice in the United States, in
Branford, Connecticut, in 1974. At the start of the hospice movement in the
United States, most hospices were home based and volunteer led.
• 1974: Dr. Balfour Mount, a surgical oncologist from McGill University, coined
the term “palliative care” to distinguish it from hospice care. While hospice
falls under the umbrella of palliative care, palliative care can be provided from
the time of diagnosis of a serious illness and concurrently with curative or life
prolonging treatment.
• 1990: The World Health Organization recognized palliative care as a
distinct specialty dedicated to relieving suffering and improving quality of life
for patients with life-limiting illness.
• 1997: The Institute of Medicine report “Approaching Death: Improving
Care at the End of Life” noted discrepancies between what the American public
wanted for end-of-life care and how Americans were experiencing end of life
in the United States. With tremendous support from multiple philanthropic
foundations, multifaceted efforts were made to promote palliative care.
• 2006: The American Board of Medical Specialties (ABMS) and the
Accreditation Council for Graduate Medical Education (ACGME) recognized
hospice and palliative care as its own specialty.
• 2010: The New England Journal of Medicine published a study by Dr.
Jennifer Temel and colleagues that showed that people with lung cancer
who received early palliative care in addition to standard oncologic care
experienced less depression and increased quality of life and survived 2.7months longer than those receiving standard oncologic care.
Self-assessment 8.1
1) What did world Health Organization do in 1990 as regards to palliative
care?
2) What are the five stages of grief according to Elisabeth Kübler-Ross 1969
book on death and dying?
3) How did Dr. Balfour Mount distinguish hospice care from palliative carein1974?
8.2. Components of palliative care
Learning activity 8.2
Use the following link and watch the video on palliative care: https://www.youtube.
com/watch?v=TZCI25C8tEQ
With use of student text book of fundamentals of nursing or any relevant book,
discusses the components of palliative care
Palliative care incorporates the whole spectrum of care—medical, nursing,
psychological, social, cultural and spiritual. A holistic approach, incorporating these
wider aspects of care is essential in palliative care.
The following table illustrates the components of palliative care, or the aspects of
care and treatment that need to be addressed, follow logically from the causes of
suffering. Each has to be addressed in the provision of comprehensive palliativecare, making a multidisciplinary approach to care a necessity.
Treatment of pain and physical symptoms are addressed first because it is not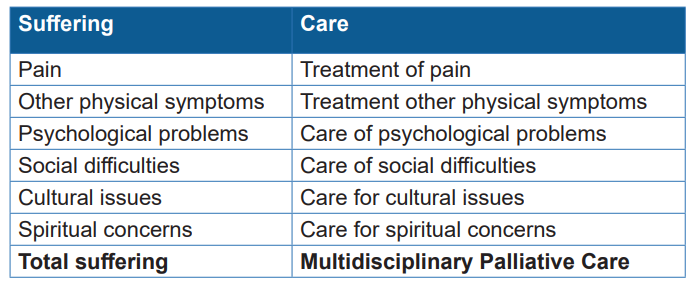
possible to deal with the psychosocial aspects of care if the patient has unrelieved
pain or other distressing physical symptoms.
The various causes of suffering are interdependent and unrecognized or
unresolved problems relating to one cause may cause or exacerbate other aspects
of suffering.
Unrelieved pain can cause or aggravate psychosocial problems. These psychosocial
components of suffering will not be treated successfully until the pain is relieved.
Pain may be aggravated by unrecognized or untreated psychosocial problems.
No amount of well prescribed analgesia will relieve the patient’s pain until the
psychosocial problems are addressed.
Palliative care nursing reflects a “whole-person” philosophy of care implemented
across the lifespan and across diverse health care settings.
Relieving suffering and enhancing quality of life include the following: providing
effective pain and symptom management; addressing psychosocial and spiritual
needs of the patient and family; incorporating cultural values and attitudes into the
plan of care; supporting those who are experiencing loss, grief, and bereavement;
promoting ethical and legal decision-making; advocating for personal wishes and
preferences; using therapeutic communication skills; and facilitating collaborative
practice.
In addition, in palliative nursing, the “individual” is recognized as a very important
part of the healing relationship. The nurse’s individual relationship with the patient
and family is seen as crucial. This relationship, together with knowledge and skills,
is the essence of palliative care nursing and sets it apart from other areas of nursing
practice.
Palliative care as a therapeutic approach is appropriate for all nurses to practice. It
is an integral part of many nurses’ daily practice, as is clearly demonstrated in work
with the elderly, the neurologically impaired, and infants in the neonatal intensivecare unit.
The palliative care nurse frequently cares for patients experiencing major
stressors, whether physical, psychological, social, spiritual, or existential.
Many of these patients recognize themselves as dying and struggle with this role.
To be dying and to care for someone who is dying are two sides of a complex social
phenomenon. There are roles and obligations for each person. To be labeled as“dying” affects how
Self-assessment 8.2
1) Identify the aspects of care and treatment that need to be addressed in
palliative care2) Explain how the various causes of suffering are interdependent
8.3. Principles of palliative care
Learning activity 8.3
Use the following link and watch the video on palliative care: https://www.youtube.
com/watch?v=TZCI25C8tEQ
With use of student text book of fundamentals of nursing or any relevant book,
discusses the principles of palliative care
The following principles have been informed by research-based evidence:
• A caring attitude
• Consideration of individuality
• Care is patient, family and carer centered
• Care provided is based on assessed need
• Cultural considerations: linking the principles of ethics, humanities, and
human values into every patient- and family-care experience
• Consent
• Choice of site of care
• Effective communication
• Clinical context: Appropriate treatment
• Comprehensive inter-professional care / Multidisciplinary care
• Care excellence
• Consistent medical care
• Coordinated care
• Care should be integrated
• Continuity of care
• Crisis prevention
• Caregiver support
• Continued reassessment
• Advance Care Planning
• Patients, families and carers have access to local and networked services to
meet their needs
• Care is evidence-based, clinically and culturally safe and effective
• Care is equitable
• Scope of care
• Timing of palliative care
• Holistic care
Here below, each of the principles of palliative care is explained:
A caring attitude:
It involves sensitivity, empathy and compassion, and demonstrates concern for the
individual. There is concern for all aspects of a patient’s suffering, not just the medical
problems. There is a non-judgmental approach in which personality, intellect, ethnic
origin, religious belief or any other individual factors do not prejudice the delivery of
optimal care.
Consideration of individuality:
There are psychosocial features and problems that make every patient a unique
individual. These unique characteristics can greatly influence suffering and need to
be taken into account when planning the palliative care for individual patients.
Care is patient, family and career centered:
Patient, family and carer centered care requires that they be actively involved in all
aspects of care, including care planning and setting holistic goals of care. Patients,
families and careers are ‘partners’ in the decision making regarding the provision
of their healthcare. This results in care that aims to ensure ‘patients receive
comprehensive health care that meets their individual needs, and considers the
impact of their health issues on their life and wellbeing. It also aims to ensure that
risks of harm for patients during health care are prevented and managed through
targeted strategies. Comprehensive care is the coordinated delivery of the total
health care required or requested by a patient. This care is aligned with the patient’s
expressed goals of care and healthcare needs, considers the impact of the patient’shealth issues on their life and wellbeing, and is clinically appropriate
Patient, family and carer centered care is an historical cornerstone of end of life
and palliative care. When patients, families and carers are supported by the health
system to actively participate, research has shown that it can lead to increased
patients’ satisfaction with health care services, improved patients’ self-perceptions,
reduced stress and increased empowerment.
Care provided is based on assessed need:
Making care available on the basis of assessed need ensures that every patient,
family and carer gets access to care that is individualised based on their goals,
wishes and circumstances.
A key learning from consultations is that “people’s needs change.” The needs of
the patient, family and carer will vary with time and across care settings during their
palliative and end of life journey.
Needs-based care requires services be available with skilled staff to meet
the needs of patients, families and carers. Regular assessment of need allows
patients, families and carers to describe their changing needs over time and helps
services be responsive, coordinated and flexible in meeting these changing needs
including reassessing care plans and goals of care. Needs-based assessment
drives effective referral and clinical handover therefore, clinical staff must have the
skills to undertake holistic needs assessments as people in their care approach
and reach the end of life helping to ensure that people get the right care in the right
place at the right time.
Cultural considerations: linking the principles of ethics, humanities, and
human values into every patient- and family-care experience:
Ethnic, racial, religious and other cultural factors may have a profound effect on a
patient’s suffering. Cultural differences are to be respected and treatment planned
in a culturally sensitive manner.
Good palliative care is significant in the manner, in which it embraces cultural, ethnic,
and faith differences and preferences, while interweaving the principles of ethics,
humanities, and human values into every patient- and family-care experience
Consent:
The consent of a patient, or those to whom the responsibility is delegated, is
necessary before any treatment is given or withdrawn. In most instances, adequately
informed patients will accept the recommendations made
Choice of site of care:
The patient and family need to be included in any discussion about the site (place/
setting) of care.
The patients with a terminal illness should be managed at home whenever possible.
Effective communication:
Good communication between all the health care professionals involved in a
patient’s care is essential and is fundamental to many aspects of palliative care.
Good communication with patients and families is also essential. Healthcare
providers should develop communication skills including listening, providing
information, facilitating decision making and coordinating care.
Important and potentially difficult discussions are frequently necessary with palliative
care patients, who have active, progressive, far-advanced disease, regarding:
• Breaking bad news
• Further treatment directed at the underlying disease
• Communicating prognoses
• Admission to a palliative care program
• Artificial nutrition
• Artificial hydration
• Medications such as antibiotics
• Do-not-resuscitate orders
• Decisions must be individualized for each patient and should be made in
discussion with the patient and family.
Clinical context: Appropriate treatment:
All palliative treatment should be appropriate to the stage of the patient’s disease and
the prognosis. Over-enthusiastic therapy that is inappropriate and patient neglect
are equally deplorable. Care must be taken to balance technical interventions
with a humanistic orientation to dying patients. The prescription of appropriate
treatment is particularly important in palliative care because of the unnecessary
additional suffering that may be caused by inappropriately active therapy or by lack
of treatment.
When palliative care includes active therapy for the underlying disease, limits should
be observed, appropriate to the patient’s condition and prognosis. Treatment known
to be useless, given because you have to do something’, is unethical.
Where only symptomatic and supportive palliative measures are employed, all
efforts are directed at the relief of suffering and the quality of life, and not necessarily
at the prolongation of life.
Comprehensive inter-professional care / Multidisciplinary care:
The provision of total or comprehensive care for all aspects of a patient’s suffering
requires an interdisciplinary team.
A multidisciplinary team approach is essential to address all relevant areas of
patient care. In order to facilitate a family in crisis to establish and then achieve
mutually agreed upon goals, the palliative care team integrates and coordinates the
assessment and interventions of each team member and creates a comprehensive
plan of care.
A multidisciplinary approach to assessment and treatment is mandatory. Failure to
do this often results in unrelieved pain and unrelieved psychosocial suffering.
Successful palliative care requires attention to all aspects of a patient’s suffering,
which requires input or assistance from a range of medical, nursing and allied
health personnel—a multidisciplinary approach. Established palliative care
services work as a multidisciplinary or inter-professional team.
Multidisciplinary is the term that used to be applied to palliative care teams, but if
the individuals work independently and there are no regular team meetings, patient
care may become fragmented and conflicting information given to patients and
families.
Inter-professional is the term now used for teams that meet on a regular basis to
discuss patient care and develop a unified plan of management for each patient,
and provide support for other members of the team.
Where palliative care services have not yet been established, it is important for
the few professionals providing such care to work as a team, meeting regularly,
planning and reviewing care, and supporting each other.
The patient may be considered a ‘member’ of the team (although they do not
participate in team meetings), as all treatment must be with their consent and in
accordance with their wishes.
The members of the patient’s family can be considered ‘members’, as they have
an important role in the patient’s overall care and their opinions should be included
when formulating a plan of management.
The ideal multidisciplinary team involves:
• Medical staff,
• Nursing staff,
• Social worker
• Physiotherapist
• Occupational therapist
• Dietician
• Psychologist (or liaison psychiatrist)
• Chaplain (or pastoral care worker)
• Volunteers
• Other personnel, as required
• Family members
• Patient
Volunteers play an important role in many palliative care services
Care excellence:
Palliative care should deliver the best possible medical, nursing and allied health
care that is available and appropriate.
Palliative care is active care and requires specific management for specific
conditions. It requires health care providers equipped with quality knowledge and
skills.
Consistent medical care:
Consistent medical management requires that an overall plan of care be established,
and regularly reviewed, for each patient. This will reduce the likelihood of sudden or
unexpected alterations, which can be distressing for the patient and family.
Coordinated care:
It involves the effective organization of the work of the members of the inter
professional team, to provide maximal support and care to the patient and family.
Care planning meetings, to which all members of the team can contribute, and at
which the views of the patient and the family are presented, are used to develop a
plan of care for each individual patient.
Care should be integrated:
Integration of care is an approach that aims to deliver seamless care within the
health system and its interface with social care. It laces people at the centre of care,
providing comprehensive wrap around support for individuals with complex needs
and enabling individuals to access care when and where they need it.
Palliative care is integral to all healthcare settings (hospital, emergency department,
health clinics and homecare).
A more integrated healthcare system is easy to use, navigate and access. It is
responsive to the specific health needs of local communities, providing them with
more choice and greater opportunities to actively engage with the health system.
For service providers and clinicians, integrating care supports them to collaborate
more effectively across health and with social care.
Healthcare providers and patients, families and carers at times describe health
services as being siloed / isolated in their care and in the systems they use to
support that care. This results in care that is delayed and or fragmented and not
supported with timely, transferable data that works across agencies and jurisdictions.
Integrating care is vital to improving outcomes for vulnerable and at-risk populations
and people with complex health and social needs.
Continuity of care:
The provision of continuous symptomatic and supportive care from the time the
patient is first referred until death is basic to the aims of palliative care. Problems
most frequently arise when patients are moved from one place of care to another
and ensuring continuity of all aspects of care is most important.
Crisis prevention:
Good palliative care involves careful planning to prevent the physical and emotional
crises that occur with progressive disease. Many of the clinical problems can be
anticipated and some can be prevented by appropriate management. Patients and
their families should be forewarned of likely problems, and contingency plans made
to minimize physical and emotional distress
Caregiver support:
The relatives of patients with advanced disease are subject to considerable
emotional and physical distress, especially if the patient is being managed at home.
Particular attention must be paid to their needs as the success or failure of palliative
care may depend on the caregivers’ ability to cope
Continued reassessment:
This is a necessity for all patients with advanced disease for whom increasing and
new clinical problems are to be expected. This applies as much to psychosocial
issues as it does to pain and other physical symptoms.
Advance Care Planning:
Advance care planning is a means for patients to record their end-of-life values
and preferences, including their wishes regarding future treatments (or avoidance
of them)
Advance care planning involves a number of processes:
• Informing the patient
• Eliciting preferences
• Identifying a surrogate decision maker to act if the patient is no longer able to
make decisions about their own care
It involves discussions with family members, or at least with the person who is to be
the surrogate decision maker.
The principle of advance care planning is not new. It is common for patients aware
of approaching death to discuss with their carers how they wish to be treated.
However, these wishes have not always been respected, especially if the patient
is urgently taken to hospital and if there is disagreement amongst family members
about what is appropriate treatment. There is less conflict between patients and
their families if advance care planning has been discussed.
Patients, families and carers have access to local and networked services to meet
their needs
Providing care as close to home as possible means that people have access
to high quality, services and supports required to meet their needs, wishes and
circumstances. Home can include a residential aged care facility or a relative’s
home.
Decisions about how close to home it is possible to provide care will start with a
detailed understanding of the patient, family and carer wishes combined with good
clinical judgement and decision-making about safe and practical options. As always
in a patient-centred model of care these options need to be negotiated and agreed
with the patient, family and carer.
Care is evidence-based, clinically and culturally safe and effective
This means that: people receive health care without experiencing preventable harm.
People receive appropriate evidence-based care. There are effective partnerships
between consumers and healthcare providers and organizations at all levels of
healthcare provision, planning and evaluation. Ensuring clinical, cultural and
psychological safety means patients; families and carers experience no negative
consequences.
All people in need should have equitable access to quality care based on assessed
need as they approach and reach the end of life. Ensuring that care provided is in
accordance with best practice recommendations, is organized for quality and is
driven by the collection and reflection of appropriate and meaningful clinical data
are all necessary components of quality systems. Quality and safety in palliative and
end of life care is eroded when there are gaps in resourcing and support available
to those providing such care.
Care is equitable:
We know that some population groups and clinical cohorts do not have equitable
access to care or experience care that is sub-optimal and or culturally unsafe or
inappropriate.
Equity in relation to health care means that patients, families and carers have equal
access to available care for equal need; equal utilization for equal need and equal
quality of care for all.
Evidence shows that care to people approaching and reaching the end of life is
often fragmented and under-utilized by identified population groups or clinical
cohorts. These included Aboriginal people, people under the age of 65, people who
live alone, and people of culturally and linguistically diverse backgrounds, people
with a non-cancer diagnosis, people living with dementia and people living with a
disability.
There is a growing body of evidence indicating that given a choice, patients would
prefer to die at home or as close to home as possible. However, a lack of services
to support that care means that many people die in acute care settings or for people
in rural and remote areas, death occurs far from their local community. A lack of
after-hour support services particularly inhibits carers and family members’ ability
to provide home care.
The next text discusses the principles of palliative care management:
Scope of care:
It includes patients of all ages with life-threatening illness, conditions or injury
requiring symptom relief from physical, psychosocial and spiritual suffering.
Timing of palliative care:
Palliative care should ideally begin at the time of diagnosis of a life threatening
condition and should continue through treatment until death and into the family’s
bereavement.
Holistic care:
Palliative care must endeavor to alleviate suffering in the physical, psychological,
social and spiritual domains of the patient in order to provide the best quality of lifefor the patient and family
Self-assessment 8.3
Explain the following principles of palliative care:
1) Care is integrated and coordinated
2) Care is equitable
3) Holistic care
4) Multidisciplinary care5) Effective communication
8.4. Non-pharmacological Pain management techniques
Learning activity 8.4
Observe the pictures below and answer the asked questions:
1) What are you seeing on the image above?
2) Describe the importance of this action on patient pain
8.4.1. Advantages and disadvantages of non-pharmacologicalinterventions
Non-pharmacological pain managements are ways to decrease pain without
medicine. Non-pharmacological pain management interventions are a set of
psychological and physical pain management methods that play a vital role and
can be used both complementarily and independently
a. Advantages of non-pharmacological interventions
Non pharmacological interventions lower medical costs, greater availability to
patients, diversification and ease of use and greater patient satisfaction. They also
reduce the likelihood of dependence on drug interventions by facilitating pain relief
as the first line of treatment.
b. Disadvantages
Disadvantage of non-pharmacological pain management include time consuming,
may request advanced technology such as network in case of video, need the
patient cooperation and understanding its benefits for both nurses and patients in
order to be a successful method.
8.4.2. Non-pharmacological pain management approaches
Non-pharmacological approaches to the relief of pain may be classified as follows1)
psychological interventions, (2) acupuncture and acupressure, (3) transcutaneous
electrical nerve stimulation, (4) physical therapies
a. Psychological interventions
Psychological interventions include distraction, stress management, hypnosis,
and other cognitive-behavioral interventions. For patients dealing with chronic pain,
psychological interventions plans are designed often involves teaching relaxation
techniques, changing old beliefs about pain, building new coping skills and
addressing anxiety or depression that may accompany pain.
b. Transcutaneous electrical nerve stimulation (TENS)
TENS is a therapy that uses low voltage electrical current to provide pain relief. A
TENS unit consists of a battery-powered device that delivers electrical impulses
through electrodes placed on the surface of your skin.
c. Acupuncture and acupressure
Acupuncture is a traditional Chinese technique that involves the insertion of
extremely fine needles into the skin at specific called acupoints. This may relieve
pain by releasing endorphins, the body’s natural pain-killing chemicals, and by
affecting the part of the brain that governs serotonin, a brain chemical involved with
mood.
Acupressure is a traditional Chinese medicine therapy in which pressure is applied
to a specific point on the body. It is done to free up energy blockages said to cause
health concerns from insomnia to menstrual cramps.
d. Physical therapies
Physical therapies include massage, heat and cold application, physiotherapy,
osteopathy ( a system of complementary medicine involving the treatment of medical
disorders through the manipulation and massage of the skeleton and musculature.
osteopath aims to restore the normal function and stability of the joints to help the
body heal itself.) and chiropractic which is a healthcare profession technic that
cares for a patient’s neuromusculoskeletal system like the bones, nerves, muscles,
tendons, and ligaments. A chiropractor helps manage back and neck pain throughthe use of spinal adjustments to maintain good alignment.
Self-assessment 8.4
1) What is non-pharmacological pain management?
2) Differentiate osteopath and chiropractic
3) What are advantages and disadvantages of non-pharmacological painmanagement
8.5. Additional methods of non-pharmacological painmanagement
Learning activity 8.5
Observe the following picture and answer the questions below:
1) What are you seeing on the image above?
2) Describe the importance of the video images on this patient condition
Relaxation Techniques for non-pharmacological pain management
Relaxation exercises calm the mind, lower the amount of stress hormones in the
blood, relax muscles, and elevate the sense of well-being. Using them regularly can
lead to long term changes in the body to counteract the harmful effects of stress.
There is no best relaxation technique for natural pain relief. Just choose whatever
relaxes you, like music, prayer, gardening, going for a walk, or talking with a friend
on the phone. Relaxation techniques can include:
• Aromatherapy is a way of using scents to relax, relieve stress, and decrease
pain. Aromatherapy uses oils, extracts, or fragrances from flowers, herbs, and
trees. They may be inhaled or used during massages, facials, body wraps,
and baths.
• Foursquare breathing. Breathe deeply so that your abdomen expands and
contracts like a balloon with each breath. Inhale to a count of four, hold for a
count of four, exhale to a count of four, then hold to a count of four. Repeat
for ten cycles.
• Tense your muscles and then relax them. Start with the muscles in your
feet then slowly move up your leg. Then move to the muscles of your middlebody, arms, neck and head
• Meditation and yoga may help your mind and body relaxes. They can also
help you have an increased feeling of wellness. Meditation and yoga help you
take the focus off your pain.
• Guided imagery teaches you to imagine a picture in your mind. You learn to
focus on the picture instead of your pain. It may help you learn how to change
the way your body senses and responds to pain.
• Music may help increase energy levels and improve your mood. It may help
reduce pain by triggering your body to release endorphins. These are natural
body chemicals that decrease pain. Music may be used with any of the other
techniques, such as relaxation and distraction.
• Heat helps decrease pain and muscle spasms. Apply heat to the area for 20
to 30 minutes every 2 hours for as many days as directed. Remember to be
cautious in order to avoid to burn the patient
• Ice helps decrease swelling and pain. Ice may also help prevent tissue
damage. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a
towel and place it on the area for 15 to 20 minutes every hour, or as directed.
• Massage therapy may help relax tight muscles and decrease pain.
• Physical therapy teaches you exercises to help improve movement and
strength, and to decrease pain.
• Comfort therapy: Comfort therapy may involve companionship, exercise,
heat/cold application, lotions/massage therapy, meditation, music, art, or
drama therapy, pastoral counseling and positioning.
• Physical and occupational therapy: Physical and occupational therapy
may involve aquatherapy, tone and strengthening and desensitization
• Psychosocial therapy/counseling: Psychosocial therapy/counseling may
involve individual counseling, family counseling and group counseling
• Neurostimulation: Neurostimulation may involve Transcutaneous electricalnerve stimulation (TENS), acupuncture and acupressure.
Self-assessment 8.5
1) What is non -pharmacological pain management?
2) Outline three examples non pharmacological pain management3) What is the best relaxation techniques in pain management?
8.6. Pain evaluation in palliative care
Learning activity 8.6
Watch this picture provide the answers to the questions presented below it:
The above patient is hospitalized in a district hospital and he was diagnosed with
pancreatic cancer at advanced stage. He is experiencing irresistible pain, crying
for help. You give painkiller and after 1 hour he told you that he still experiences
pain and requests additional painkiller.
1) How are you going proceed in managing this patient?
2) What are possible complications that can arise if the pain is not treated?
The pain evaluation should encompass physical, psychological, social and spiritual
components as they all interact upon one another. Untreated chronic pain can cause
different complications including decreased mobility, decreased concentration,
depression, anorexia, sleep disturbances and impaired immunity with all associated
complications that can arise from impaired immune system. Adequate management
of pain will alleviate the complications of pain.
Pain causes distress and suffering for people and their loved ones. Pain can also
increase blood pressure and heart rate, and can negatively affect healing. Pain
keeps people from doing things they enjoy. It can prevent them from talking and
spending time with others. It can affect their mood and their ability to think. Managing
the pain is very important as it helps ease suffering, improving patient comfort and
therefore patient satisfaction. Pain control can facilitate early ambulation, adequate
oxygenation and nutrition and reduce the stress. This helps the speed up the
recovery time and may reduce the risk of developing depression.
The first principle of managing pain is an adequate and full assessment of where
the underlying pain is coming from. Patients may have more than one area of pain
and different pains have different causes. The acronym SOCRATES is used toassess pain:
• Site: Where is the pain? The maximal site of the pain.
• Onset: When did the pain start, and was it sudden or gradual? Include also
whether it is progressive or regressive.
• Character: What is the pain like? An ache? Stabbing?
• Radiation: Does the pain radiate anywhere?
• Associations: Any other signs or symptoms associated with the pain?
• Time course: Does the pain follow any pattern?
• Exacerbating/relieving factors: Does anything change the pain?• Severity: How bad is the pain?
Self-assessment 8.6
1) Using SOCRATES, describe how you can assess pain
2) What is importance of managing of patient pain?3) What are complications associated with pain?
8.7. Psychosocial support
Learning activity 8.7
Mr. F aged 35 is a married with 3 children. The first born is 6 years old; the
second is 4 years old while the last is one year old. He is the chief of his family
and he was working to satisfy his family’s basic needs, his wife is a nurse at
one District hospital. Mr. F has been informed that he has stage IV Metastatic
Melanoma since 6 months ago. He has been receiving chemotherapy over the
duration of his illness. Chemotherapy can cause side effects such as nausea,
vomiting depression, tiredness and thinning or loss of hair. His family cared for
him at home until two weeks ago. He has now moved to a hospice for respite
care. Mr. is a pastor in one protestant church and therefore he receives many
visitors.
1) What do you think could be the psychological impacts of Mr. F’s disease?
2) If you are nurse caring M.r F what do you think as nursing actions that
could help Mr.F alleviate his discomfort other than medication.
End of life is a difficult time for patients and their relatives and careers. It is important
that psychosocial care is provided to palliative patients and their families in various
ways through a range of medical, nursing and allied healthcare professionals. It is
imperative for nurses in palliative care to know about any specific cultural practices,
spiritual and psychosocial conditions of the patients.
The term psychosocial denotes both the psychological, spiritual and social aspects
of a person’s life and may describe the way people make sense of the world.
Psychological characteristics include emotions, thoughts, attitudes, motivation, and
behavior, while social aspects denote the way in which a person relates to and
interacts with their environment.
Psychosocial support is care concerned with the psychological and emotional well
being of the patient and their family or careers, including issues of self-esteem,
insight into an adaptation to the illness and its consequences, communication,
social functioning and relationships. It is a form of care that encourages patients
to express their feelings about the disease while at the same time providing ways
by which the psychological and emotional well-being of such patients and their
caregivers are improved.
In most cases, palliative patients have severe functional and cognitive limitations
requiring support in basic needs, such as hygiene, food, money, medication and
mobility, relying on others for daily life activities, with increasing dysfunction andpsychological repercussions.
8.7.1. Consequences of diagnosis
The psychological and social consequences of a diagnosis of life-limiting illness on
the patient need to be considered. A diagnosis of this kind may provoke a range of
emotional responses in the patient or family member. These include:
• Fear of physical deterioration/ dying; pain/suffering; losing independence; the
consequences of illness or death on loved ones
• Anger at what has happened or what may have caused/ allowed it to happen;
unsuccessful treatment Sadness at approaching the end of life; restriction of
activities due to illness
• Guilt/regret for actions; in some cases for contributing to the development of
the illness
• Changes in sense of identity, adjusting to thinking of themselves as unwell/
dependent
• Loss of self-confidence, sometimes related to loss of physical functioning/
changes in appearance Confusion about what has happened; the future andchoices available.
8.7.2. Importance of psychosocial support
Psychosocial support is very important for patients in palliative care by reducing
both psychological distress and physical symptoms through increasing quality of
life, enhancing coping and reducing levels of pain and nausea with a consequentreduction on demands for hospital resources.
8.7.3. Components of psychosocial support
Psychosocial support and services may include any or all of the following:
• Emotional support, including social activities, companionship and befriending
• Personal care, help with bathing or providing massage and other
complementary therapies
• Assistance in securing financial support
• Help inside and outside the home; for example, cleaning and shopping
• Supplying practical aids such as wheelchairs and other equipment
• Offering counseling and psychological support to help people come to terms
with dying religious/spiritual support, whatever a person’s beliefs
• Practical support in preparing for death, including saying farewell, makingend-of-life decisions and arranging funerals.
8.7.4. Features of psychosocial care
The care taken to address the psychological and social concerns of patients in
palliative care might involve:
Communication
Good communication is at the core of positive end of life experiences. Communication
underpins every aspect of care and is a conduit to psychosocial aspects of care.
Unmet communication needs of people with life limiting illnesses and of carers
can undermine the coordination of care and compromise the provision of relevant
information and subsequent decision-making.
Effective communication and meaningful ongoing conversations during care can
help facilitate knowledge about the palliative patients, their life experiences and
needs of care. Through this increased understanding of the person, it assists in
identifying any emotional, or spiritual concerns they may have which in turn can
improve physical and emotional wellbeing.
Allowing adequate time for communication to occur improves the quality of the
interaction with the person, with research showing a reduction in care time is
achieved due to greater engagement, cooperation and a reduction in distress.
Conversely, poor communication can lead to poor understanding of a person’s
concerns which has a known association with the development of depression and
anxiety.
From the perspective of the family of the person receiving palliative care, their
information needs are critical. Families often wish to be kept informed of their
relative’s condition and value open and timely communication from staff. Deficiencies
in conversations, particularly around changes in their relative’s health status, often
result in family members experiencing feelings of abandonment, anxiety, distress
and fear of the unknown. Fully engaging family members in information sharing
and decision making with honest, open communication can allow them to make
decisions around how best to spend their remaining time with their family member.
Other features:
• Helping patients understand their illness and/or symptoms
• Helping patients to understand their options and plan for the future
• Advocating on behalf of patients/those close to them to ensure they have
access to the best level of care and services available
• Enabling patients and those close to them to express their feelings and
worries related to the illness, listening and showing empathy, providing
comfort through touch as/ when it is appropriate, e.g. holding a patient’s hand
or putting a hand on his or her shoulder. Also, complementary therapies such
as massage
• Helping the patient or family member access any financial aid they may
be entitled to (including benefits, but also charitable trusts/grants where
applicable)
• Practical help with daily activities like grocery shopping
• Arranging personal/social care and organising aids for daily living — setting
up a care package, installing hand rails or other adaptations
• Career support such as making arrangements for respite
• Signposting the patient/those close to them to relevant resources like local
support groups
• Exploring spiritual issues and ensuring the patient is able to continue his or
her religious practices
• Referring the patient or family member to specialist psychological/socialsupport where appropriate
Self-assessment 8.7
1) Psychosocial support is defined as….
a. Means actions that address both the psychological and social needs of
individuals, families and communities
b. Means interventions aimed at curing mental health problems
c. Aims to enhance the self-promoted recovery and resilience of the affected
individual, group and community
d. Means interventions offered to the cadaver after death
2) What are the consequences of deficiency communication to the family
which has a patient under palliative care?
3) Explain the importance of psychosocial support
4) Enumerate three consequences resulting from emotion to palliativepatient or his/her family
8.8. Spiritual support
Learning activity 8.8
Observe the image below and answer the following questions
1) What do you see on the above picture?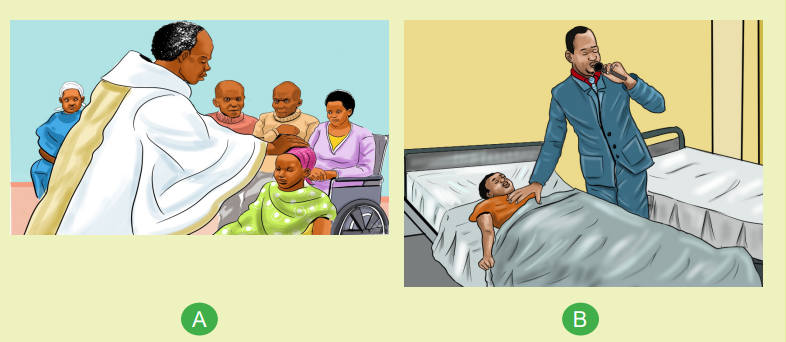
2) Describe the importance of the actions which are being done on the
above picture
It is very crucial for nurses in palliative care to know about any specific cultural
practices, spiritual and religious conditions of the patients. Spiritual variables havean important effect mediating physical symptoms and suffering.
8.8.1. Importance of spiritual support in palliative care
Spiritual care has positive effects on individuals’ stress responses, spiritual well
being (such as the balance between physical, psychosocial, and spiritual aspects
of self), sense of integrity and excellence, and interpersonal relationships. Spiritual
care improves people’s spiritual well-being and performance as well as the quality
of their spiritual life.
spiritual status of patient impact the patient decision-making at the end-of-life and
high levels of spiritual wellbeing have been associated with improved quality of life,
improved coping with disease, improved adjustment to diagnosis, better ability to
cope with symptoms and protection against depression, hopelessness and desire
of hastened death. Therefore, improving spiritual support in patients’ palliative care
is a valuable task.
8.8.2. Where to get spiritual support services
In health care system, the spiritual support services can be available either as
pastoral care workers (or spiritual care workers) or be invited from outside of the
health care system and are available to support palliative care team. Pastoral care
workers are trained professionals who can help people work through their feelings.
They can also arrange visits from spiritual leaders such as ministers, priests, rabbis
and imams. Where necessary, they can also educate and support others in caring
roles in providing culturally sensitive spiritual care.
If the person is religious, possible spiritual interventions might include (1) visits from
or referrals to chaplains, pastoral care workers or traditional healers, (2) spiritual or
religious counseling and (3) taking part in religious services.
If the person is not religious, possible spiritual interventions might include (1)
creating a life review, (2) support groups, (3) listening to music, (D) creating artwork,(E) enjoying nature, (F) enjoying other leisure activities.
Self-assessment 8.8
1) Case study: You are at hospital where you have a patient suffering from
liver cancer in advanced stage. She is catholic and the family members
need a sacrament for their patient. Where can you find that spiritual
support?2) What is the importance of spiritual support for a palliative care patient?
8.9. Legal and Ethical issues in Palliative care
Learning activity 8.9
Mr. X is hospitalized for 3 months; he was diagnosed of advanced cancer of the
lungs with metastasis in the liver. The treating team has decided to treat him as
palliative care as there is no curative treatment for his advanced lung cancer.
Mr. X has difficulty in breathing and experience severe pain; he is on strong pain
killers and oxygen via face mask. This morning during the ward round he called
the doctor in front of his wife and said that if he had a cardiac arrest he doesn’t
want to be resuscitated and that if he fails in respiratory failure he doesn’t want
any other mean of advanced respiratory support such as mechanical ventilation.
The doctor asked you to give a paper To Mr. X and to sign for his preferences atend of life.
1) Do you think that it is acceptable to accept such request? Explain your
answer2) By respecting Mr. X request which ethical principles are respected.
Learning activity 8.9
Ethics refer to the moral principles that guide behavior and decision making, and
the branch of knowledge and inquiry that deals with moral principles. Guiding moral
principles arise from a variety of beliefs about right and wrong and behavior.
Bioethics is ethics as applied to human life or health (such as decisions about
abortion or euthanasia).
Palliative and end of life issues are often delicate and controversial and require
skilled, insightful interdisciplinary care. Health care providers encounter many
challenges and ethical dilemmas; ethical principles and code conduct guide them
in decision making.
8.9.1. Ethical principles in palliative care/ end of life care
Ethical principles guide decision making in end of life/palliative care. The following
principles should be applied while providing palliative care and end of life care.
Understanding the principles underlying ethics is important for health care providers
and their patients to solve the problems they face in end of life care. The ethical
principles are autonomy, beneficence, no maleficence, fidelity, justice and veracity.
a. Autonomy
Autonomy refers to the right to make one’s own decisions. It is patient’s right to
self-determination. Everyone has the right to decide what kind of care they should
receive and to have those decisions respected. Respecting patient autonomy is
one of the fundamental principles of nursing ethics. This principle emphasizes on
protection of the patients’ right to self-determination, even for patients who havelost the ability to make decisions. This protection can be achieved by using advance
care directives.
Advance care directives (ADs): ADs are derived from the ethical principles of
patient’ autonomy. They are oral and/or written instructions about the future medical
care of a patient in the event he or she becomes unable to communicate, and loses
the ability to make decisions for any reason. ADs completed by competent person
ordinarily include living wills, health care proxies, and “do not resuscitate” (DNR)
orders.
A living will is a written document in which a competent person provides instructions
regarding health care preferences, and his or her preferences for medical
interventions such as feeding tubes that can be applied to him or her in end-of-life
care. A patient’s living will take effect when the patient loses his or her decision
making abilities.
A health care proxy (also called health care agent or power of attorney for health
care) is the person appointed by the patient to make decisions on the patient’s
behalf when he or she loses the ability to make decision. A health care proxy is
considered the legal representative of the patient in a situation of severe medical
impairment. The responsibility of the healthcare proxy is to decide what the patient
would want, not what the proxy wants.
ADs help ensure that patients receive the care they want and guide the patients’
family members in dealing with the decision-making burden. Another reason for
ADs is to limit the use of expensive, invasive, and useless care not requested by
patients. Researches show that ADs improve the quality of end-of-life care and
reduce the burden of care without increasing mortality.
In many countries, the right of people to self-determination is a legal guarantee.
Each patient’s “right to self-determination” requires informed consent in terms of
medical interventions and treatment. A patient has both the “right to demand the
termination of treatment” (e.g. the discontinuation of life support) and the “right to
refuse treatment altogether”; the exercise of these rights is strictly dependent on
the person. ADs can be updated yearly and/or prior to any hospitalization.
In many countries, the right of competent individuals to express their treatment
preferences autonomously in end-of life care should be met with ethical respect,
taking into account the use of advanced treatments and the prognosis of their
disease. However, this autonomy has some limitations. The decisions made by
a patient should not harm him or her. It is important for healthcare providers to
respect the autonomy of their patient and fulfill their duties to benefit their patientswithout harming them.
b. Non-maleficence
Non-maleficence is the duty to ‘do no harm’. Although this would seem to be
a simple principle to follow, in reality it is complex. Harm can mean intentionally
causing harm, placing someone at risk of harm and unintentionally causing harm.
However, placing a person at risk of harm has many facets. A person may be at risk
of harm as a known consequence of a nursing intervention intended to be helpful.
For example, an individual may react adversely to a medication. Unintentional harm
occurs when the risk could not have been anticipated.
Although some of the nursing interventions might cause pain or some harm, non
maleficence refers to the moral justification behind why the harm is caused. Harm
can be justified if the benefit of the nursing intervention is greater than the harm to
the patient and the intervention is not intended to harm the patient.
c. Beneficence
Beneficence means ‘doing good’. Nurses are obligated to do good; that is, to
implement actions that benefit individuals. However, doing good can also pose
a risk of doing harm. Beneficence requires physicians to defend the most useful
intervention for a given patient. Often, patients’ wishes about end-of-life care are
not expressed through ADs, and the patients’ health care providers and family
members may not be aware of their wishes about end-of-life care.
If a patient is not capable of decision-making, or if the patient has not previously
documented his or her wishes in the event he or she becomes terminally ill, the
end-of-life decision is made by the patient’s Health care provider as a result of
consultations with the patient or the patient’s relatives or the patient’s health care
proxy. In this situation, the responsibility of the Health care provider in the care of
the dying patient should be to advocate the approaches that encourage the delivery
of the best care available to the patient.
d. Justice
Justice is often referred to as fairness. Nurses face decisions where a sense of
justice should prevail. Healthcare providers have an ethical obligation to advocate
for fair and appropriate treatment of patients at the end of life. This can be achieved
through good education and knowledge of improved treatment outcomes.
e. Fidelity
Fidelity means to be faithful to agreements and promises. By virtue of their standing
as professional caregivers, nurses have responsibilities to people in their care,
employers and society, as well as to themselves. Nurses often make promises such
as ‘I’ll be right back with your pain medication’ or ‘I’ll find out for you’. Individuals
take such promises seriously and nurses are obliged to respond within appropriate
time frames. Fidelity principle requires Health Care providers to be honest with their
dying patient about the patients’ prognosis and possible consequences of patients’
disease.
f. Veracity
Veracity refers to telling the truth. Although this seems straight forward, in practice
choices are not always clear. Should a nurse tell the truth when it is known that it will
cause harm? Does a nurse lie when it is known that the lie will relieve anxiety and
fear? Lying to sick or dying people is rarely justified. The loss of trust in the nurse
and the anxiety caused by not knowing the truth usually outweigh any benefits
derived from lying. Truth telling is fundamental to respecting autonomy.
Most patients want to have full knowledge of their disease and its possible
consequences, but this desire may decrease as they approach the end of their life.
Some patients may not want information about their disease. Health care providers
should be skilled in determining their patients’ preferences for information and,
honestly yet sensitively, provide their patients with as much accurate information
as the patients want. Having effective patient-centered communication skills helps
Health Care providers learn and meet the demands of their patients.
8.9.2. Ethical issues in end of life and Palliative care
In the end of life care of a patient, the decision to implement practices to prolong the
patient’s life or to comfort the patient may be difficult for the Health care providers,
patient, family members or health care proxy. The following topics relate to some
situations where difficulty in decision making regarding end of life is encountered:
Cardiopulmonary resuscitation (CPR), advanced respiratory support such as
Mechanical ventilation (MV), artificial nutrition and hydration (ANH), terminal
sedation, withholding and withdrawing treatment, euthanasia and physician
assisted suicide (PAS).
a. Cardiopulmonary resuscitation(CPR)
Although CPR is valuable in the treatment of heart attacks and trauma, sometimes
the use of CPR may not be appropriate for dying patients and may lead to
complications and
Worsen the patients’ quality of life. For some terminally ill patients, CPR is an
undesired intervention. The decision not to perform CPR on a dying patient can
be difficult for healthcare personnel. The decision to administer CPR to a patient
depends on many factors such as patient preferences, the estimated success rate,
the risks of the procedure, and the perceived benefit.
A competent patient may not want to undergo CPR in the event of cardiopulmonary
arrest. This decision is called the” Do not attempt CPR” (DNR decision). Despite
this request, the patient’s family members may ask the Health Care provider to
perform CPR. In this case, if the patient is conscious and has the ability to make
decisions, the patient’s decision is taken into account. Physicians must learn the
CPR demands of patients at risk of cardiopulmonary arrest. DNR decision can be
considered for the following patients
• Patients who may not benefit from CPR;
• Patients for whom CPR will cause permanent damage or loss of consciousness;
• Patients with poor quality of life who are unlikely to recover after CPR.
b. Advanced respiratory support: Mechanical ventilation
Approximately 75% of dying patients experience difficulty breathing or dyspnea.
This feeling can be scary for patients and those who witness it. In end-of-life care,
mechanical ventilation is applied not to prolong the lives of patients but to reduce
their anxiety and to allow them to sleep better and eat more comfortably.
If Mechanical ventilation support does not provide any benefit to the patient or no
longer meets its intended goals, or if the outcome is not optimal, or the quality of
life is not acceptable according to the patient’s or family’s wishes, support can be
terminated. The timing of the device separation should be chosen by the patient’s
family members.
c. Advanced Nutrition and Hydration(ANH)
Nutrition and hydration are essential parts of human flourishing. ANH involves
giving food and water to patients who are unconscious or unable to swallow.
Artificial nutrition can be given through enteral feeding by tube or parenteral feeding.
Nutrition and hydration decisions are among the most emotionally and ethically
challenging decisions in end-of-life care. Many medical associations suggest that
feeding and hydration treatments are forms of palliative care that meet basic human
needs and must be given to patients at the end of life.
ANH may improve the survival and quality of life of some patients. It may improve
the nutritional status of patients with nutritional problems. ANH is associated with
considerable risks such as the aspiration pneumonia, diarrhea, and gastrointestinal
discomfort.
For these reasons, the benefits and possible harms of the intervention should be
explained to the patient or to the other decision-makers in detail before making the
ANH decision.
If a patient is incompetent, his or her proxy decision-maker can refuse artificial
feeding and hydration on behalf of the patient.
d. Terminal Sedation
Terminal sedation is a medical intervention used in patients at the end of life, usually
as a last effort to relieve suffering when death is inevitable. Sedatives are used forterminal sedation. People have some concerns about terminal sedation because
the treatment of an unconscious patient is sensitive and risky. The purpose of
terminal sedation is not to cause or accelerate death but to alleviate pain that is
unresponsive to other means.
There are four criteria for evaluating a patient for terminal sedation:
• The patient has a terminal illness.
• Severe symptoms are present, the symptoms are not responsive to treatment,
and the symptoms are intolerable to the patient.
• A “do not resuscitate” order is in effect.
• Death is imminent (hours to days).
e. Withholding and Withdrawing treatment
Withdrawing is a term used to mean that a life-sustaining intervention presently
being given is stopped. Withholding is a term used to mean that life-sustaining
treatment is not initiated or increased.
The decision to withhold or withdraw interventions or treatment is one of the
difficult decisions in end-of-life care that causes ethical dilemmas. If a patient and
physician agree that there is no benefit in continuing an intervention, the right action
is withholding or withdrawing the interventions.
In most countries, the legal opinion is that patients cannot seek treatment that is
not in their best interest and, that physicians should not strive to protect life at all
costs. However, if there is doubt, the decision must be in favor of preserving life. All
healthcare professionals should be able to define an ethical approach to making
decisions about withholding and withdrawing treatment that takes into account the
law, government guidance, evidentiary base, and available resources.
f. Euthanasia
Euthanasia, is a Greek word meaning ‘good death’, Euthanasia is applied in two
ways as active or passive euthanasia.
Active euthanasia involves actions to bring about an individual’s death directly. In
active euthanasia, a person (generally a physician) administers a medication, such
as a sedative and neuromuscular relaxant, to intentionally end a patient’s life at the
mentally competent patient’s explicit request.
Passive euthanasia: Passive euthanasia occurs when a patient suffers from
an incurable disease and decides not to apply life-prolonging treatments. More
commonly referred to now as withdrawing or withholding life-sustaining therapy,
involves the withdrawal of extraordinary means of life support, such as removing
a ventilator or withholding special attempts to revive an individual (e.g. a ‘not for
resuscitation’ status) and allowing the individual to die of the underlying medicalcondition.
Euthanasia is not accepted legally and ethically in many counties worldwide
including Rwanda.
8.9.3. Strategies to enhance ethical decisions and practice
Several strategies help nurses overcome possible organizational and social
constraints that may hinder the ethical practice of nursing and create moral distress.
As a nurse, the following should be taken into consideration:
• Become aware of your own values and the ethical aspects of nursing.
• Be familiar with nursing codes of ethics.
• Seek continuing education opportunities to stay knowledgeable about ethical
issues in nursing.
• Respect the values, opinions and responsibilities of other health care
professionals that may be different from your own.
• Where possible, participate in or establish ethics rounds. Ethics rounds use
hypothetical or real cases that focus on the ethical dimensions of the care of
the individual rather than the individual’s clinical diagnosis and treatment.
• Serve on institutional ethics committees.
• Strive for collaborative practice in which nurses work effectively in cooperation
with other health care professionals.
Other patients’ rights
All patients have a right to dignity throughout their life, especially when the end of
life is near. Provide privacy when bathing or caring for a patient. Encourage the
person to make choices and control their own life. If they want to wear a certain
dress, let them wear it. If they want their bath in the evening instead of the morning,
let them have their bath in the evening. Allow the person to be as independent as
possible, speak to the person with respect and call the patient by their name.
All patients that are capable of making a decision must be able to do so, even when
the end of life is near. Patients have a right to have their medical information secret
and private. Never discuss a patient or their condition with friends, neighbors, other
patients or residents. Do not discuss any information about the patient unless the
patient asks you to.
Keep patient information confidential. It is against the law to tell your family member
or neighbor that a patient named x, my patient is dying with AIDS.
Nursing care does not stop when the end of life comes. All members of the health
care team play a very important role in the end-of-life care. This care meets the
person’s physical, mental, social, spiritual and financial needs. Nurse and others
health team must be able to meet these needs. Care at the end of life is a veryrewarding part of nursing care.
Furthermore, the patient has right to be treated as a living human being until He/she
die, right to maintain a sense of hopefulness, the right to express the feelings and
emotions about the approaching death in the patient own way, right to participate
in decisions concerning his care, right to expect continuing medical and nursing
attention even though cure goals must be changed to comfort goals, right not to die
alone, right to be free from pain, right to have questions answered honestly, right
to die in peace and dignity, right to discuss and enlarge patient religious and or
spiritual experiences, whatever these may mean to others and right to expect thatthe sanctity of the human body will be respected after death.
Self-assessment 8.9
1) What are advance care directives? What is its purpose in end of life care?
2) Cardiopulmonary resuscitation (CPR) is lifesaving intervention; however
in some circumstances a decision of Do not attempt Resuscitation (DNR)
may be made; for which patients a DNR may be considered?
3) In end of life care; termination sedation may be administered to
patients; What are criteria should the health care provider assess before
administration of termination sedation.
4) Define euthanasia and explain its main types
5) In caring patient in palliative care nurses may encounter constraints that
may hinder the ethical practice of nursing and create moral distress. Give4 strategies that will help the nurse to overcome those constraints?
8.10. Communication in palliative care
Learning activity 8.10
1) In which context may you encounter image A and B?
2) Which message pictures A and B communicate to you?
In situations of serious illness, communication is one of the most important tools
which the health care professionals use in giving the patient the information that
they need to know. This creates a sense of trust and security for both the patient
and the family.
Communication is the exchange of information, thoughts and feelings among
people using speech or other means. In healthcare, it is approaching every patient
interaction with the intention to understand the patient’s concerns, experiences,
and opinions.
Communication is a vital basic pre-requisite for all health care providers to provide
effective quality of care for all patients and not just in the palliative care; however
Palliative care requires excellent communication skills because at this time
communication can be particularly challenging due to patient clinical situations
where suffering, fear, and confusion can be considerable. Communication in
palliative care involves the conversation between patient, family and health care
provider about goals of care, transitions in care, progress of disease and providing
social, psychological & spiritual support. Communication can never be neutral; it is
either effective or ineffective, stress relieving or stress inducing.
The approach in communicating information, predictions, and prognoses to patients
and loved ones will have a crucial effect on their current and future behavior, as well
as potentially on treatment and illness outcomes.
Communication should be done in sense of Sensitive, honest and empathic in order
to relieve the burden of difficult treatment decisions, and the physical and emotional
complexities of death and dying, and lead to positive outcomes for people nearing
the end of life and their companions.
Effective and efficient communication is crucial for providing care and support to
people affected by life-limiting illness. However, some people are not familiar to
discussing personal psychological issues and can find these conversations difficult
Importance of communication in palliative care
Good communication between healthcare professionals and patients can lead to a
greater sense of well-being, decreasing feelings of distress commonly experienced
by those diagnosed with a terminal illness and their families.
Communication in palliative care help patients to understand their disease,
outcomes, patient behavior, ability to cope, both physical and psychological health,
as well as patient satisfaction with care, and compliance with treatment.
Also, good communication in palliative care was found to be effective in prevention
of depression and other stress related, helps patient to participate in decisionmaking during care and improve psychological and physical well-being.
Open communication is an important aspect of death and dying and of a good death
and it is thought to contribute to effective symptom control and end of life planning.
By contrast, poor communication is associated with distress, complaints and
can result in the patient -family having significant misunderstanding of end-of-life
processes.
Behavior of nurse in palliative care
During communication, the health care provider should possess the following
behavior in order to contribute in patient’s sense of hope including being present
and taking time to talk; giving information in a sensitive and compassionate manner,
answering questions and being nice, friendly and polite.
Showing empathy to the patient is a key for both verbally and nonverbally
communication. Non-verbal communication is vital as the way we interact impacts
on the relationships with our patients, as we constantly give out signals through ourbody language in the way we sit and the gestures we make
Self-assessment 8.10
1) What is communication?
2) What are factors that can influence the communication in palliative care?3) Who can be involved in communication with the patient?
8.11. Communication strategies used in palliative care
Learning activity 8.11
Observe the following pictures and respond to the related questions

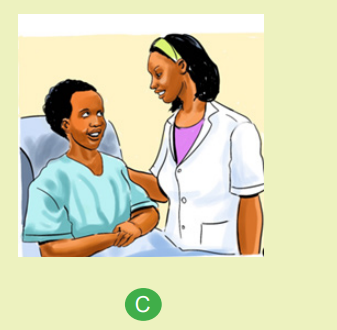
1) What is the attitude of health care provider observed in the images A, B,
and C?
2) What are the similarities of the above images?3) What is the importance of the nurse‘s attitude in the image A, B, C?
Interpersonal communication in the area of health and palliative care is understood
as a complex process that involves the perception, comprehension and transmission
of messages in the interaction between patients and health-care professionals.
This process has two dimensions: the verbal, which occurs through the expression
of spoken or written words, and the nonverbal, characterized by the manner and
tone of voice with which words are said, by gestures that accompany the speech,
by looks and facial expressions, by the body posture, and by the physical distance
that people maintain with each other.
Communication in the context of palliative care consists of verbal and nonverbal.
Verbal communication strategies include interrogative nature and were related to
the expectations and knowledge of the patients about their disease and treatment,
as well as statements of concern and interest in the multidimensional aspects of
the patient. Nonverbal consist of communication five signals or strategies including
affective touch, the look, the smile, physical proximity and active listening. It is
essential for the care of the patient undergoing the process of dying that healthcare
professionals adequately perceive, comprehend and employ verbal and nonverbal
communication.
The nonverbal communication makes it crucial in the context of terminality because
it allows the perception and comprehension of the feelings, doubts and anxieties of
the patient, as well as the understanding and clarification of gestures, expressions,
looks and symbolic language typical of someone who is experiencing a phase in
which a cure for their disease is no longer possible.Verbal communication strategies consist of asking what the patients know about
their condition, ask the patients how they feel, to encourage them to talk about
their feelings, verbalize willingness to help, talk and/or clarify doubts, ask about
the expectations of the patients regarding the treatment, ask about the interests
and preferences of the patients in order to establish pleasant conversations. The
strategies or techniques of verbal communication can be classified into three
groups: expression, clarification and validation.
The strategies allocated to the expression group were those that they allow verbal
expression of thoughts and feelings, facilitating their description and enabling the
exploration of problematic areas for the patient. In the clarification group, there
were the strategies that help to comprehend or clarify the messages received,
enabling the correction of inaccurate or ambiguous information. The validation
group contained the expressions that make the ordinary meaning of what is
expressed, certifying the accuracy of the comprehension of the message received.
Nonverbal communication strategies include:
1) Affectionate touch that refers to the physical contact that conveys messages
of an emotional nature. Several actions mentioned by the professionals that
were grouped under this denomination were: a hug, a kiss on the cheek, a
caress of the hair, a firm handshake, touching hands, arms and shoulders
and greeting with physical contact.
2) Establish/maintain eye contact and smiling: Eye contact and smiling are
facial signals that denote interest and, therefore, facilitate the interaction with
the patients. In addition to portraying emotions, the look has an important
function: to regulate the flow of the conversation. The interruption of eye
contact may denote a lack of interest in continuing the conversation, causing
the interaction to be interrupted or impaired. Thus, both show essential
signals for the approach and establishment of a bond of trust with the
patients.
3) Physical proximity: The distance that people maintain with each other
during the interaction also transmits messages.
4) Active listening: Active listening involves the therapeutic use of silence, the
conscious emission of nonverbal facial signals that denote interest in what
is being said (maintaining eye contact, positive head nods), the physical
proximity and orientation of the body with the trunk facing toward the person,
and the use of short verbal phrases that encourage continuation of thespeech, such as: and then..., and I hear you.
Self-assessment 1.1
1) Discuss non-verbal communication strategies2) Explain the groups of verbal communication
8.12. Principles of communication in palliative care
Learning activity 8.12
Observe the following images A and B:
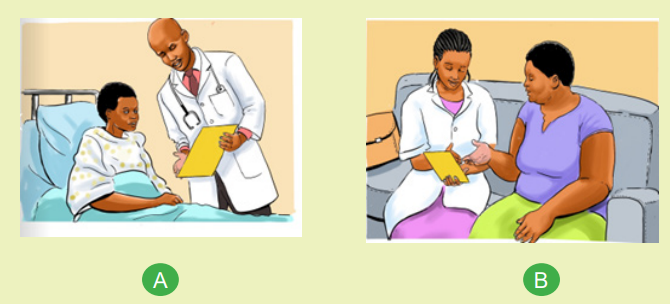
What are your observations toward the image A and B?
8.12.1.Overview of principles of communication in palliative care
There are some general communications principles that help facilitate discussion
about existential and psychological concerns, and demonstrate respect for the
person’s individuality. thus, including PREPARED and The SPIKES communicationframework
The PREPARED communication framework outlines key strategies that can be used
when communicating with a person with a life-limiting illness, their family and cares.
The PREPARED communication frameworkP) Prepare for discussion, (R) Relate
to person, (E) Elicit preferences from the person and their caregivers, (P) Provide
information tailored to the needs of both the person with a life limiting illness and
their families and carers, (A) Acknowledge emotions and concerns, (R) Realistichope, (E) Encourage questions and further discussions and (D) Document.
a. The PREPARED communication framework in clinical practice
P: Prepare for the discussion:
Ensure facts about the person’s clinical circumstances are correct, ensure privacy
and uninterrupted time for the discussion, mentally prepare yourself for the
conversation and negotiate who should be present during the discussion eg, “Is
there anyone else
you would like to be here with you while we talk?”
R: Relate to the person:
Develop a rapport, show empathy, care and compassion during the entire
conversation, propose the topic in a culturally appropriate and sensitive manner,
make eye contact (if culturally appropriate), and Sit close to the person (if culturally
appropriate). Use culturally appropriate body language and allow silence and time
for them to express feelings.
E: Elicit personal preferences:
Identify the reason for this conversation and establish the person’s expectations,
clarify their understanding of the situation and establish how much detail they want
to know and consider cultural and contextual factors that can influence information
preferences.
P: Provide information that is tailored to the personal needs of all parties
Offer to discuss what to expect, in a sensitive manner, giving the person the
option not to discuss it, provide information in small amounts at the person’s step,
engage in active listening such as attend to the person completely, reflecting and
repeating back what you think they have said. Explain the uncertainty, limitations
and unreliability of prognostic and end-of-life information, ensure consistency of
information and approach and use the words ‘death’ and ‘dying’ where appropriate.
A: Acknowledge emotions and concerns
Explore and acknowledge fears, concerns and emotional reaction and be willing
to initiate and engage in conversations about what can happen in the future and
during the dying process and respond to distress where applicable.
R: Realistic hope
Be honest without being blunt or giving more detailed information than desired. Do
not provide misleading or false information that artificially influences hope. Reassure
the person that support, treatment and resources are available to control pain and
other symptoms but avoid premature reassurance. Explore and facilitate realisticgoals, wishes and ways of coping on a day-to-day basis, where appropriate.
E: Encourage questions
Encourage questions and information clarification. Be prepared to repeat
explanations, check understanding of what has been discussed and whether the
information provided meets personal needs and Leave the door open for topics to
be discussed again in the future.
D: Document
Write a summary in the medical record of what has been discussed and speak or
write to other key healthcare providers involved in the person’s care.
b. The SPIKES communication framework in clinical practice
The SPIKES Protocol was developed to assist healthcare professionals with
breaking bad news. Effective communication when dealing with bad news can
enhance the understanding of prognosis and treatment options, and the person’s
adjustment to their situation.
THE SPIKES steps can complement the PREPARED framework by assisting with
the four most important objectives of breaking bad news which are (1) Gathering
information, (2) Transmitting medical information (3) Providing support and (4)
eliciting the person’s collaboration in developing a strategy or treatment plan for
the future.
Although some of the steps of SPIKES are similar to the steps in PREPARED,
SPIKES concentrates on delivering bad news (such as the initial diagnosis), while
PREPARED focuses on the holistic support of the person and their family throughout
their illness and can be used to frame discussions in a range of palliative contexts.
SPIKES stand for:
Setting up: organize an interview with the patient
Perception: Find out what the patient knows about his or her condition
Invitation: Get patient’s permission to impart bad news
Knowledge: Convey bad news at the level of the patient’s comprehension
Emotions: Physician must acknowledge and respond to patient’s emotions
Strategy and Summary: Summarize areas discussed, and formulate strategy and
follow-up plan.
S: Setting up the conversation
Choose a setting with privacy and without interruptions, ensuring that you have a
private space, phones turned to silent, turned pagers off, allowed sufficient time forthe conversation, help the person to understand what they are hearing by confirming
and explaining medical facts, check the accuracy of all available information –
including test results and that you have the right person. Plan what you will say,
decide on general terminology to be used, consider your own emotional reaction
to providing the distressing news. Find out in advance if the person wants anyone
else to be present.
P: Assessing the Person’s perception
Find out how much the person knows already, in particular, how serious they think
the illness is and how much it will affect the future. This helps you gauge how close
to the medical reality their understanding is or if they are in denial. This information
helps you to decide on the pacing and content of the conversation.
I: Obtaining the Person’s invitation
Find out what the person wants to know, you must be committed to honesty and
respecting their wishes if they do not want to be informed.
K: Providing knowledge and Information to the Person
The health care provider should decide on the objectives for the conversation and
consider what the person knows and needs to know. The patient should be clear
on how to manage their illness about diagnosis, treatment Plan, prognosis and
support. The health care provider should be clear and direct. He should use plain
language and avoid jargon, complex medical terminology and acronyms. Whenever
necessary, use diagrams, written messages and booklets as an aid and respond to
patient concerns and questions.
E: Addressing the person’s emotion with empathic responses
The health care provider should observe the person and give them time to react and
comprehend the news and acknowledge any emotional response without criticism
or blame. Ask the person what they are thinking or feeling; listen and explore if
you are unclear about what they are expressing; resist the temptation to make the
distressing news better than it is and allow time for silence.
S. Strategy and Summary
Demonstrate a genuine understanding of the person’s concerns, distinguish the
fixable from the unfixable, make a plan or strategy and explain it by providing
information on tests, treatment options, referrals and other aspects of care and
prepare for the worst and hope for the best and schedule a follow up appointmentso that they have the opportunity for further questions.
Self-assessment 8.12
1) Briefly discuss the communications framework used in palliative care
communication and give the difference between them.
2) Respond with True or False to the following statement:
“While providing knowledge and information to the person with end of lifecondition, it is better to ask him about what he/she knows about transport.”
8.13. End of life and nursing care
Learning activity 8.13
See the pictures below
1) Explain the similarities in the images A and B
2) In which context you can see the images above?
Dying is a process of deterioration of the vital system, which ends with clinical
death. One of the most important things we can do for patients who are dying is to
provide the best possible care for them and their families during the last phase of
life through death. This is particularly important during the “imminent” phase. This
is the phase that precedes the actual death, and is also the time when the patient
typically loses consciousness. The care the nurse provides during this phase will
affect the family’s memories of their loved one’s final days and hours on earth. It is
vital that the nurse performs thorough assessments, rapid response to changes in
status, rapid titration of medications, and timely discontinuation and introduction ofinterventions aimed to promote comfort.
8.13.1.Diagnosis dying
Making a diagnosis that the patient is dying can be a complex process. In the
hospital setting where the treatment emphasis is generally “cure” orientated,
potentially useless investigations and treatments may continue at the expense of
patient comfort if the diagnosis of dying is not made.
The advantages of diagnosing dying are that emphasis of care to become comfort
based and ceasing unnecessary interventions, improving the awareness of dying,
can enhance communication for the patient and family, enable discussion about
place of care and assist the patient with their final wishes.
The following criteria generally support the diagnosis of dying: (1) A progressive
deterioration in the responsiveness of the patient (e.g. their ability to respond to
surroundings, decreased energy levels, becoming semi-comatose), (2) Reduced
ability to swallow (e.g. able to only take sips of fluid, unable to take oral medication),
(3) Deteriorating physical function (e.g. the patient has become bed-bound).
In other chronic incurable diseases predictability of the dying phase is not always
as clear. A range of factors will need to be considered including diagnosis of a life
threatening illness, no further curative treatment options, cause of deterioration
(infection, hypercalcemia, etc).
According to Kübler-Ross, there are 5 stages which precede dying and they are
widely known in the acronym DABDA (Denial, Anger, Bargaining, Depression and
Acceptance):
1. Denial: "I feel fine."; "This can't be happening, not to me. Denial is usually
only a temporary defense for the individual. This feeling is generally replaced
with heightened awareness of possessions and individuals that will be left
behind after death. Denial can be conscious or unconscious.
2. Anger: Why me? It's not fair!"; "How can this happen to me?"; '"Who is to
blame?” Once in the second stage, the individual recognizes that denial
cannot continue. Because of anger, the person is very difficult to care for due
to misplaced feelings of rage and envy. Anger can manifest itself in different
ways.
3. Bargaining: "I'll do anything for a few more years."; "I will give my life
savings if..." The third stage involves the hope that the individual can
somehow postpone or delay death. Psychologically, the individual is saying,
"I understand I will die, but if I could just do something to buy more time..."
People facing less serious trauma can bargain or seek to negotiate a
compromise.
4. Depression: "I'm so sad, why bother with anything?"; "I'm going to die
soon so what's the point?"; "I miss my loved one, why go on?" During the
fourth stage, the dying person begins to understand the certainty of death.
Because of this, the individual may become silent, refuse visitors and spend
much of the time crying and grieving. This process allows the dying person
to disconnect from things of love and affection. It is not recommended to
attempt to cheer up an individual who is in this stage. It is an important time
for grieving that must be processed.
5. Acceptance: "It's going to be okay."; "I can't fight it; I may as well prepare
for it."
In this last stage, individuals begin to come to terms with their mortality, or that of
a loved one, or another tragic event. This stage varies according to the person's
situation.
8.13.2.Phases of dying
Dying process has 3 phases including: actively dying, Transitioning, and Imminent.
a. Active phase
In active dying phase there are two typical roads to death that can occur during
the actively dying process which are the usual road or the difficult road. The
usual road is the best we can hope for when caring for persons at the end of life.
It begins with sedation and lethargy and progresses to a comatose state and then
death. The difficult road includes restlessness and confusion that often progresses
to unpleasant hallucinations and delirium. Myoclonus and seizures can also
accompany the difficult road.
Physical signs and symptoms associated with both roads including: pain, dyspnea,
fatigue, cough, constipation or diarrhea, incontinence, anorexia, cachexia, nausea
and vomiting, depression and seizures
The role of the nurse during the active dying phase is to support the patient and
family by educating them on what they might expect to happen during this time,
addressing their questions and concerns honestly, being an active listener, and
providing emotional support and guidance.
b. Transition phase
Transitioning phase describe the period of time in between the actively dying
phase and the imminent phase. In this phase, patients begin to withdraw from the
physical world around him in preparation for their final journey. Some examples of
this could include: decreased interest in activities of life, less frequent and shorter
interactions with others, this is referred to as “nearing death awareness” and
often documented by clinicians as “hallucinations.” Possible explanations of this
phenomenon from the medical community are as a result of hypoxia, acidosis, or
alterations in metabolic processes. Patients will generally not exhibit any signs orsymptoms of distress with this awareness, whereas patients whose dying is taking
the difficult road might show signs of distress or agitation with their awareness.
During transitioning, it is important to keep the patient’s area as comfortable and
peaceful as possible. Common lights and noises can contribute to restlessness and
agitation; therefore, it is advisable to keep lights soft, shades closed if possible, and
external noises limited to a minimum.
c. Imminent phase
Imminent phase is defined as what is about to happen. The patient has transitioned
into this last phase of the dying process and death can occur at any point now. Not
all individuals will present with every sign or symptom, and the symptoms will occur
in no particular order. During this phase, the body is in the process of shutting down.
Multi-system organ failure often occurs and will result in some typical symptoms. In
cardiological or circulatory system the patient may have Cool and clammy skin, cold
extremities and rapid or irregular pulse. In musculoskeletal system, the patient may
present inability to ambulate, inability to move/turn in bed and increased lethargy.
In neurological system, the patient may present more difficulty to arouse, confusion
and restlessness, in respiratory system, the patient may present periods of apnea
or Cheyne stokes respiration pattern, increased respiratory rate, inability to cough
or clear secretions and presence of increased secretions (death rattle). In urinary
system, the patient may present decreased and/or dark urine output
During this phase, the patient becomes unresponsive to those around him and
may appear to be sleeping. Sometimes the patient’s eyes will be partially open as
they are resting. The patient can still hear or sense the activity and loved ones
around them and so nurse has to teach the families to continue to talk to and gently
touch their loved ones in this phase.
8.13.3. Nursing management of dying person
a. Assessment
To gather a complete database that allows accurate analysis and identification of
appropriate nursing diagnoses for individuals who are dying and their families, the
nurse first needs to recognize the states of awareness manifested by the person
and family members. In cases of terminal illness, the state of awareness shared
by the dying person and the family affects the nurse’s ability to communicate freely
with individuals and other health care team members and to assist in the grieving
process. Three types of awareness:
• Closed awareness, the individual is not made aware of impending death.
The family may choose this because they do not completely understand why
the person is ill or they believe that they will recover. The doctor may believe it
is best not to communicate a diagnosis or prognosis to the individual. Nursing
staff are confronted with an ethical problem in this situation.
• Mutual pretence, the individual, family and health professionals know that
the prognosis is terminal but do not talk about it and make an effort not to
raise the subject. Sometimes the person refrains from discussing death to
protect the family from distress. Mutual pretence permits the person a degree
of privacy and dignity, but it places a heavy burden on them because there is
no one in whom they can confide.
• Open awareness, the individual and others know about the impending death
and feel comfortable discussing it, even though it is difficult. This awareness
gives them an opportunity to finalize affairs and even participate in planning
funeral arrangements
Clinical manifestations impending clinical death
Loss of muscle tone, characterized by the following:
• Relaxation of the facial muscles (e.g. the jaw may sag).
• Difficulty speaking.
• Difficulty swallowing and gradual loss of the gag reflex.
• Decreased activity of the gastrointestinal tract, with subsequent nausea,
accumulation of flatus, abdominal distension and retention of faeces,
especially if narcotics or tranquillisers are being administered.
• Possible urinary and rectal incontinence due to decreased sphincter control.
• Diminished body movement.
Slowing of the circulation, characterized by the following:
• Diminished sensation.
• Mottling and cyanosis of the extremities.
• Cold skin, first in the feet and later in the hands, ears and nose (the person,
however, may feel warm if there is a fever).
• Slower and weaker pulse.
• Decreased blood pressure.
Changes in respirations, characterized by the following:
• Cheyne–Stokes respirations (rhythmic waxing and waning of respirations
from very deep breathing to very shallow breathing with periods of temporary
apnoea).
• Noisy breathing, referred to as the ‘death rattle’, due to collecting of mucus
in the throat.
• Mouth breathing, dry oral mucous membranes.Sensory impairment, characterized by the following:
• Blurred vision.
• Impaired senses of taste and smell.
b. Diagnosing
A range of nursing diagnoses, addressing both physiological and psychosocial
needs, can be applied to the dying person, depending on the assessment data.
Diagnoses that may be particularly appropriate for them are Fear, Hopelessness
and Powerlessness. In addition, Risk of caregiver role strain and Interrupted family
processes are not uncommon diagnoses for caregivers and family members.
c. Planning
Major goals for individuals who are dying are (a) maintaining physiological and
psychological comfort, and (b) achieving a dignified and peaceful death, which
includes maintaining personal control and accepting declining health status.
People facing death may need help accepting that they have to depend on others.
Some people who are dying require only minimal care; others need continuous
attention and services. People need help, well in advance of death, in planning for
the period of dependence. They need to consider what will happen and how and
where they would like to die. If the dying person wishes to be at home and family or
others can provide care to maintain symptom control.
d. Implementing
The major nursing responsibility for individuals who are dying is to assist them to a
peaceful death. More specific responsibilities are the following:
• To minimize loneliness, fear and depression
• To maintain the individual’s sense of security, self-confidence, dignity and
self-worth
• To help the individual adapt to losses
• To provide physical comfort.
i. Helping people die with dignity
Nurses need to ensure that the person is treated with dignity; that is, with honor and
respect. People who are dying often feel they have lost control over their lives and
over life itself. Helping them die with dignity involves maintaining their humanity,
consistent with their values, beliefs and culture
ii. Meeting the physiological needs of the dying person
The physiological needs of people who are dying are related to a slowing of body
processes and to homeostatic imbalances. Interventions include providing personal
hygiene measures; controlling pain; relieving respiratory difficulties; assisting with
movement, nutrition, hydration and elimination; and providing measures related to
sensory changes
Table 8.13 1 Physiological need of dying people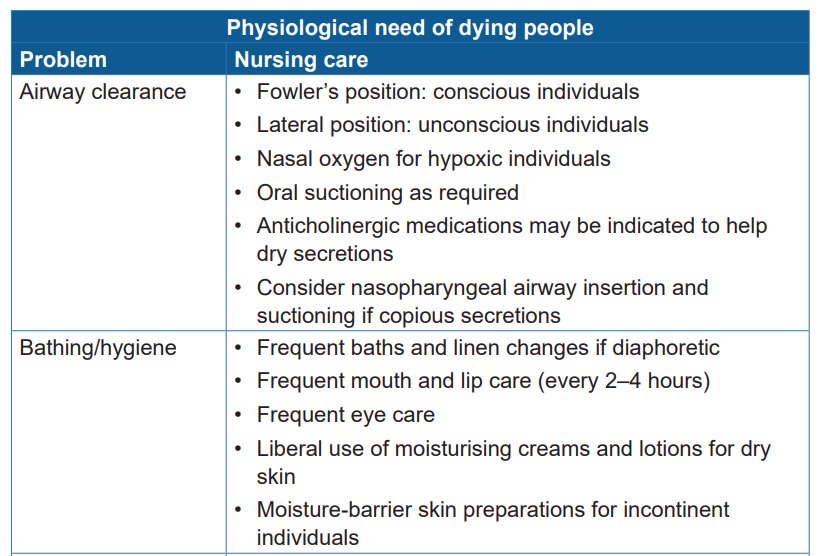
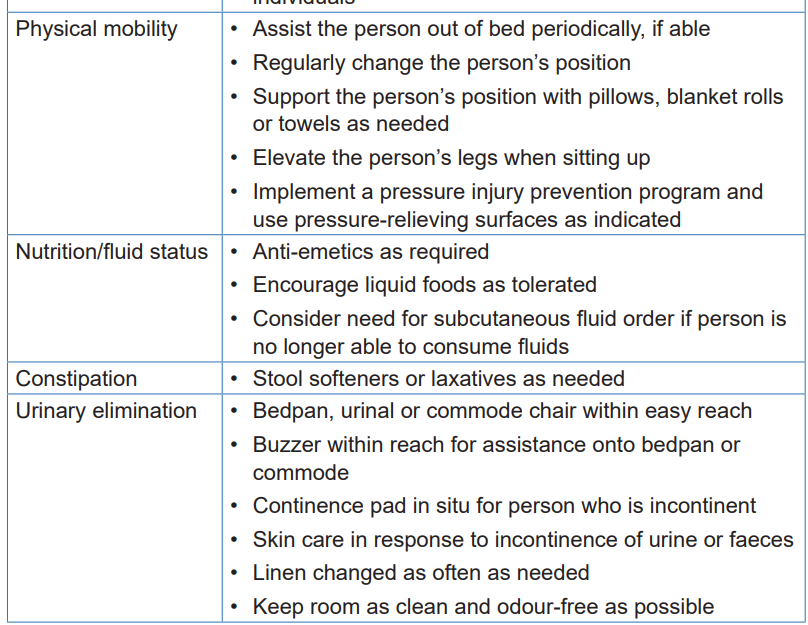
iii. Providing spiritual support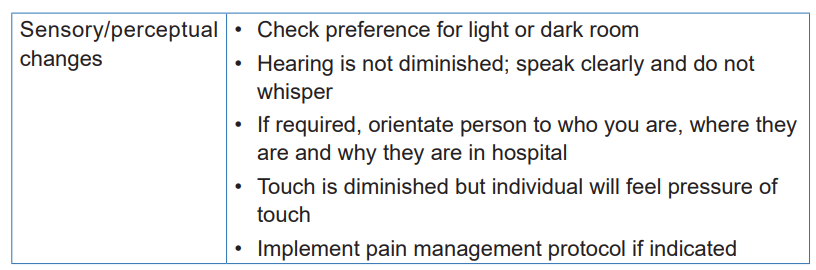
Spiritual support is of great importance in dealing with death.
Although not all people identify with a specific religious faith or belief, most have a
need for meaning in their lives, particularly as they experience a terminal illness.
The nurse has a responsibility to ensure that the individual’s spiritual needs are
attended to, either through direct intervention or by arranging access to individuals
who can provide spiritual care.
Specific interventions may include facilitating expressions of feeling, prayer,
meditation, reading and discussion with appropriate clergy or a spiritual advisor.
It is important for nurses to establish an effective interdisciplinary relationship with
spiritual support specialists
iv. Supporting the family
The most important aspects of providing support to the family members of a dying
individual involve using therapeutic communication to facilitate their expression of
feelings. When nothing can reverse the inevitable dying process, the nurse can
provide an empathetic and caring presence. The nurse also serves as a teacher,
explaining what is happening and what the family can expect. Due to the stress of
moving through the grieving process, family members may not absorb what they
are told and may need to have information repeated. The nurse must have a calm
and patient demeanor.
Family members should be encouraged to participate in the physical care of the
dying person as much as they wish to and are able. The nurse can suggest the family
assist with bathing, speak or read to the person and hold their hand. The nurse must
not, however, have specific expectations of family members’ participation. Those
who feel unable to care for or be with the dying person also require support from
the nurse and from other family members. They should be shown to an appropriatewaiting area if they wish to remain nearby
e. Evaluating
To evaluate the achievement of the goals of the dying person, the nurse collects
data in accordance with the desired outcomes established in the planning phase.
Evaluation activities may include the following:
• Listening to the individual’s reports of feeling in control of the environment
surrounding death, such as control over pain relief, visitation of family and
support people, or treatment plans.
• Observing the individual’s relationship with significant others
• Listening to the individual’s thoughts and feelings related to hopelessness orpowerlessness.
Self-assessment 8.13
1) Which criteria should generally support the diagnosis of dying?
2) List the 5 stages which precede dying according to Kübler-Ross?
3) Briefly explain 3 phases of dying process
4) What are the major responsibility and specific responsibilities of nurse
while caring a dying patient?
5) Outline three nursing diagnoses which can be formulated while caring adying patient
8.14. Death and post mortem care
Learning activity 8.14
Ms. G is a female with 23 years old hospitalized in hospice setting since 6 months
ago due to metastatic uterine cancer. Today in morning when a nurse is coming
to do morning assessment, she found the following signs: Ms.G was too cold,
the neck is stiff, and the orbits of the eyes are fixed (do not move), she doesn’t
do any body movement. The nurse monitors vital signs, she doesn’t find any
values of results (the all vital signs are not marked). Family members of Ms. G
are crying, but the surround population doesn’t know what happen
1) What do you think was happened to Ms.G?
2) What do you think could be the nursing management to Mr. G8.14.1.Death
a. Definitions and signs of death
Death is defined as a state of the total disappearance of life or irreversible cessation
of the functions of organs that are necessary for life including heart, lungs and brain.
In modern medicine death is indicated by the flat line in the record of
electroencephalography (EEG) or lack of brain function, however traditional clinical
signs of death are cessation of the apical pulse, respirations, and blood pressure
which is referred to as heart-lung death.
When patient is on assisting equipment of respiration and blood pressure death
acknowledgement is difficult but can be indicated by total lack of response to
external stimuli, no muscular movement especially breathing, no reflexes
and flat encephalogram (brain waves).
Cerebral death or higher brain death occurs when the higher brain center, the
cerebral cortex, is irreversibly destroyed. In this case, there is “a clinical syndrome
characterized by the permanent loss of cerebral and brainstem function, manifested
by absence of responsiveness to external stimuli, absence of cephalic reflexes, and
apnea.
b. Body status after death
After death, the body undergoes many physical changes, including Algor mortis,
Livor mortis and Rigor mortis..
Algor mortis is the gradual decrease of the body’s temperature after death.
When blood circulation terminates and the hypothalamus ceases to function,
body temperature falls about 1°C per hour until it reaches room temperature.
Simultaneously, the skin loses its elasticity and can easily be broken when removing
dressings and adhesive tape.
Livor mortis is characterized by cease of blood circulation, the red blood cells
break down, releasing hemoglobin, which discolors the surrounding tissue.
Rigor mortis is the stiffening of the body that occurs about 2 to 4 hours after death.
It results from a lack of adenosine triphosphate (ATP), which causes the muscles to
contract, which in turn immobilizes the joints. Rigor mortis starts in the involuntary
muscles (heart, bladder and so on), then progresses to the head, neck and trunk,
and finally reaches the extremities.
8.14.2. Post mortem care
Nurses are responsible for care of a body after death. Postmortem care should be
carried out according to the policy of the hospital or organization. Because care of
the body may be influenced by religious law, the nurse should check the deceased’sreligion and make every attempt to comply. If the deceased’s family or friends wish
to view the body, it is important to make the environment as clean and pleasant as
possible and to make the body appear natural and comfortable.
Postmortem care should be provided as soon as possible to prevent tissue damage
or deformity. Post mortem care is defined as the care given once death has occurred
through transfer to a funeral provider.
Because the deceased person’s family often wants to view the body and because
it is important that the deceased appear natural and comfortable, nurses need
to position the body, place dentures in the mouth and close the eyes and mouth
before rigor mortis sets in. Because of the reduction in body temperature and loss
of skin tone (algor mortis) after death, it is important to gently remove all tape and
dressings to prevent tissue damage.
The skin or body parts should never be pulled on. The head of the bed should be
elevated and a clean pillow placed under the head immediately after death before
beginning other activities in order to prevent purplish discoloration (livor mortis) of
the face.
Tissues after death become soft and eventually liquefied by bacterial fermentation:
the hotter the temperature, the more rapid the change. Therefore, bodies are often
stored in cool places to delay this process. Embalming prevents the process through
injection of chemicals into the body to destroy the bacteria.
8.14.3.Special consideration in end life and post mortem care
a. Pediatric considerations
Arrange for family members, especially parents, to be with the child throughout the
dying process and at the time of death, if they wish. Allow family members to hold
their child’s body after death. Make every effort to honor family members’ requests
per the organization’s practice. Family members of deceased newborns may want
a memento of their infant (picture, article of clothing, footprint, or lock of hair).
b. Older adult considerations
It is important to consider that some older adults have small families and small
circles of surviving friends. Health care team members may be the only human
presence during death. Arrange for someone to be with the person when death is
imminent.
c. Home care considerations
Consider the type of support family members need at the time of death and assist
with arrangements. After death in the home setting, follow the organization’s practice
for body preparation and transfer and for disposal of durable medical equipment
(e.g., tubing, needles, and syringes), soiled dressings or linens, and medications.
Instruct family members regarding safe and proper handling and disposal ofmedical waste.
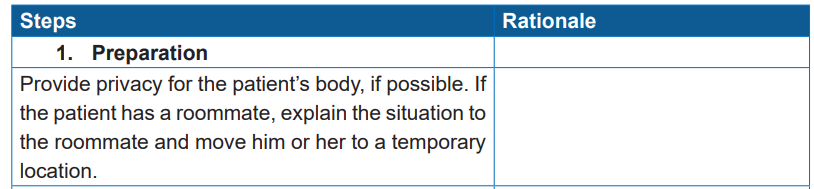
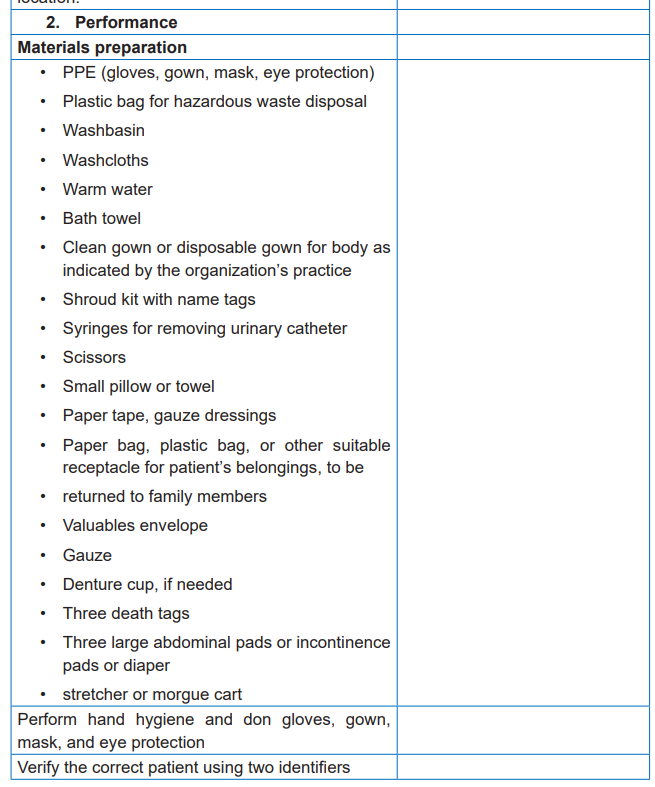
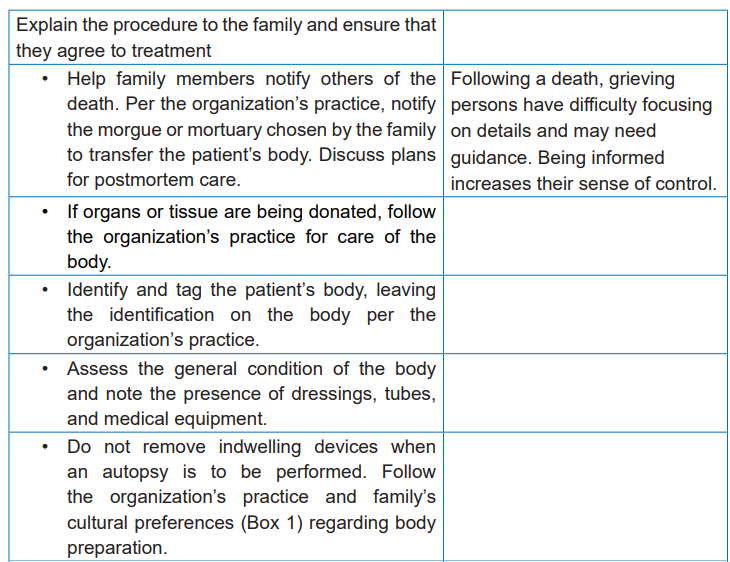
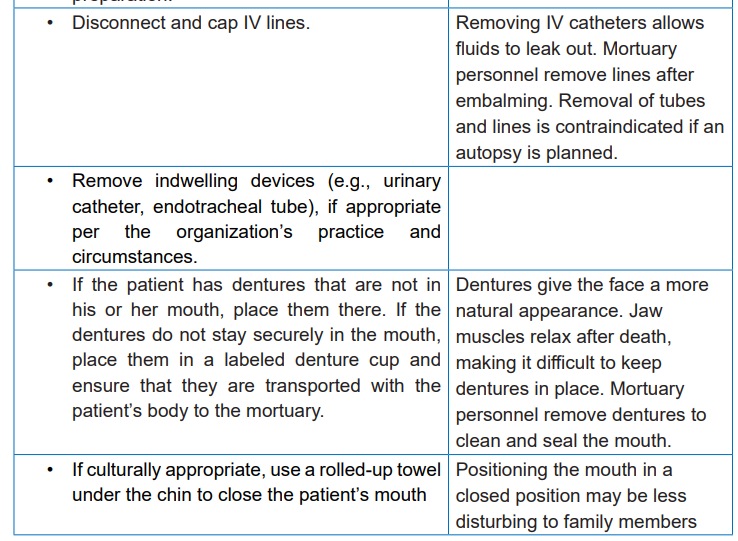
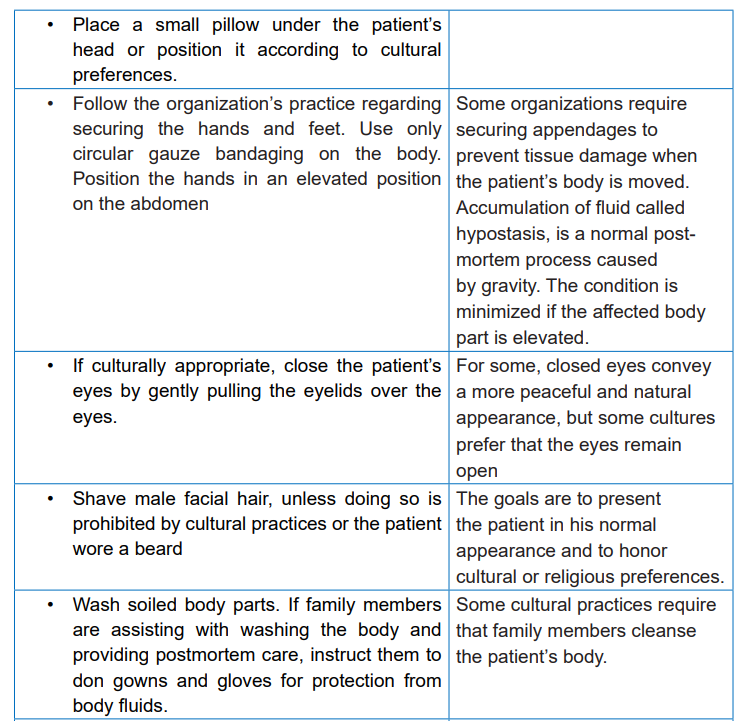
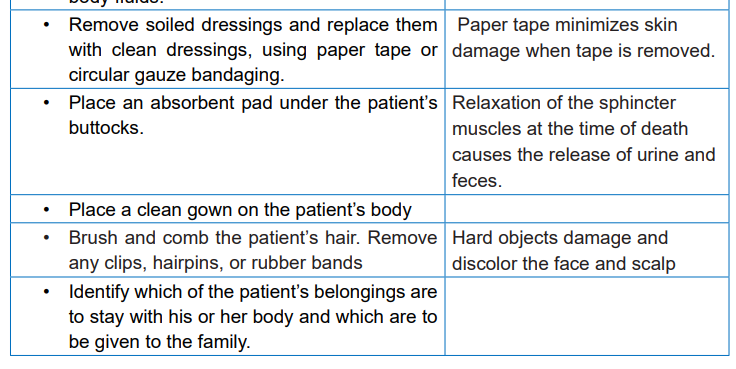
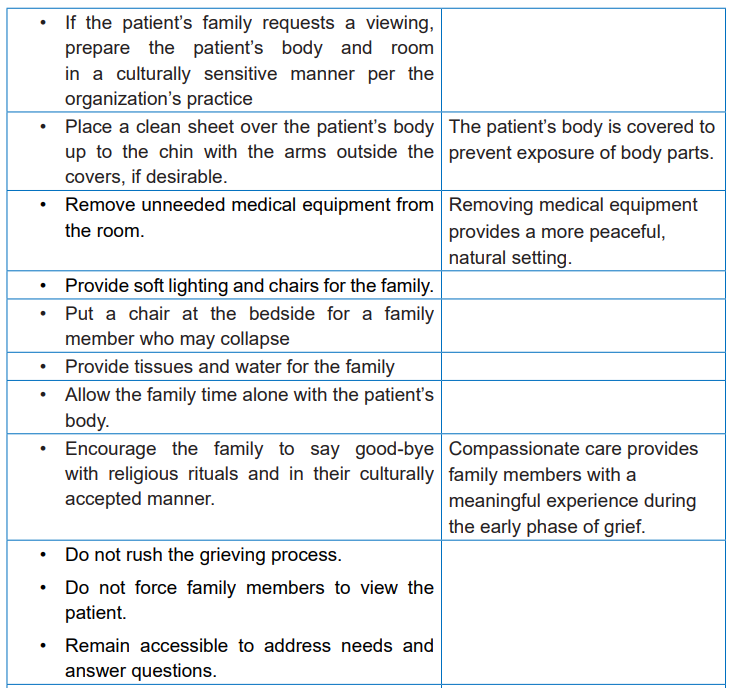
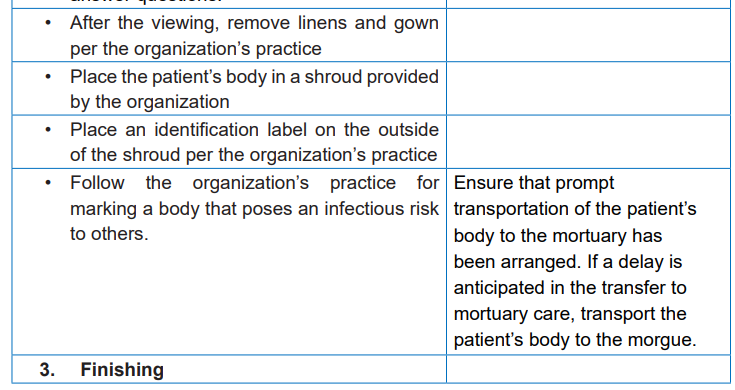
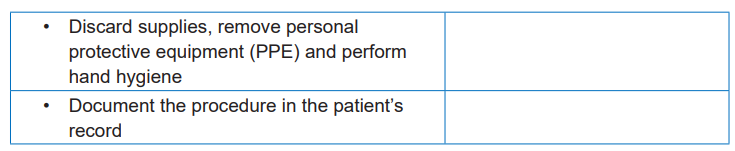
Self-assessment 8.14
1) The loss of skin elasticity and change in body temperature which occurs
after death is better referred as:
a. Algor mortis
b. Livor mortis
c. Rigor mortis
2) What is the main reason for storing the deceased body in cool place?
3) Differentiate heart-lung death from brain death4) What should the nurse do as nursing care before rigor mortis develops?
8.15. Resilience and self-care
Learning activity 8.15
Observe the following images:
1) Discover the activities that are being done by the persons in images A, B,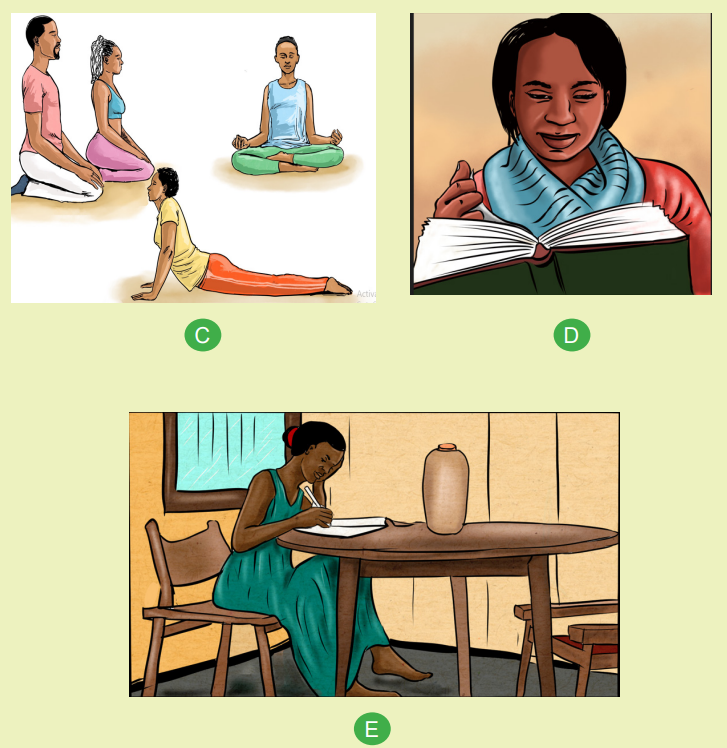
C, D and C presented above.2) What could be the importance of those activities to human health?
8.15.1. Self-care
Self-care refers to activities and practices that we can engage in on a regular
basis to reduce stress, maintain and enhance our short/long-term health and well
being. Self-care is necessary for your effectiveness and success in honoring your
professional and personal commitments. Thus help to reduce stress, cope with the
challenges of work, enhance subjective sense of well-being, and replenish energylevels.
A key point for supporting one’s self-care lies in the ability to identify and manage
the general challenges that personnel face, such as the potential for stress
and burnout or interpersonal difficulties; to be aware of your own personal
vulnerabilities, such as the potential for re-traumatization; and as well as striving
for balance in your life, by maintaining and enhancing the attention you pay to thedifferent domains of your life in a way that makes sense to you.
c. Strategies to support self-care
The following are some strategies/tips for taking care of your-self:
1. Physical self-care
Get enough sleep. Regularly do physical activity that you enjoy. Eat regularly, well
balanced meals. Reduce alcohol and caffeine consumption.
Access medical care when needed (both preventative and acute). Take time off
when sick. Calm the body. Release tension in healthy ways. Practice healing
through movement and music.
Take deep breaths. Limit or eliminate exposure to media. Balance work, play, andrest.
2. Emotional self-care
Know your vulnerabilities. Engage socially to avoid feeling isolated. Spend time with
non-work friends, family and acquaintances. Set limits, if necessary, when others
are too overwhelmed demanding of your time or energy (Give yourself time to heal
and renew). Stay in contact with important people in your life.
Use relaxation skills that work best for you. Acknowledge when you have done
well. Value yourself. Identify energizing /positive activities, people and places, and
actively seek them out.
Reestablish a routine, if possible- allow your-self to cry or be upset. Find things that
make you laugh. Express your opinion on social issues outside of work. Listen to
music that soothes you.
3. Psychological self-care
Take time out (trips out of town, to the beach or a weekend away). Take time away
from telephones, email, social media and the internet. Make time for self-reflection.
Notice your inner dialogue (listen to your thoughts and feelings). Have your own
personal development and/or external supervision.
4. Spiritual self-care
Do some forms of reflective practice (meditate, pray or reflect). Spend time in
natural environments. Connect to a community or network with shared values. Beopen to feeling inspiration, awe and other positive emotions. Nurture your optimism
and hope. Be open to not knowing. Identify what is meaningful to you and notice
its place in your life. Contribute to causes in which you believe in outside of work.
5. Interpersonal self-care
Schedule regular time with significant others (e.g. partner, kids, friends, family). Stay
in contact with friends and networks. Make time to reply to personal correspondence.
Allow others to do things for you (meet new people; ask for help when you need it).
Share your feelings: good, bad or other with someone you trust.
6. Self-care in personal settings
Effective self-care strategies used outside of the workplace settings included a
range of health behaviors, including, meditation and spiritual practice, a healthy
diet, adequate sleep, and moderation of alcohol intake were considered important.
In addition to exercising for fitness, other physical activities such as yoga and
massage were found to be effective self-care strategies. Rest and relaxation
at home in a bath were described as effective self-care strategies when feeling
overwhelmed or needing to wash away thoughts of the workplace and socializing
and maintaining positive relationships with friends and family, finding harmony
between personal and professional roles was consistently described as an effective
self-care strategy and establishing and maintaining boundaries between home and
the workplace was considered an effective self-care strategy.
7. Self-care in workplace settings
Self-regulation of workload is important, but often difficult to achieve. It involves
being assertive about one’s capacity in relation to workload and wellbeing.
Take breaks during the work day for example during lunch or between meetings;
taking meal breaks, taking recreation leave for regular holidays, and taking personal
leave during illness were also considered effective self-care strategies. For some,
choosing to work part-time was an effective self-care strategy that provided ongoing
regulation of workload in relation to other competing demands. Having a cohesive
team was important and this contributed to a supportive working environment.
Mindfulness exercises were an effective self-care strategy in the workplace, both
in individual and group contexts. A sense of allowing oneself to be human, in the
context of displaying emotion in the clinical setting, was also part of effective self
care practice.
Take time to chat with colleagues. Create uninterrupted time to complete tasks. Set
boundaries with clients and colleagues. Balance your workload so that you are not
overwhelmed. Arrange your work space so that it is comfortable and comforting.
B. Barriers to self-care
Multiple impediments to self-care were identified in the workplace including busyness.
Workplace culture: in some workplace cultures there is a stigma associated with
self-care, making it difficult for individuals to engage in self-care practice without
feeling judged as being selfish. Bringing work home can be described as a barrier
to self-care, and related to workplace culture and expectations. Self-worth was also
discussed as a common concern for effective self-care, where self-criticism and a
lack of self-worth undermined self-care as an important priority and lack of planning
for self-care.
C. Factors facilitating Self-care
Several factors were described as facilitators of effective self-care including
recognizing the importance of self-care. Some became conscious of this through
previous experiences of illness or being unwell after having initially neglected selfcare.
Prioritizing self-care was an important enabler which correlated with noticeable
benefits. Adopting a preventative approach to self-care was important, Positive
workplace cultures supportive of self-care were described as vital to effective self
care practice. Leadership and positive role models were considered key enablers
to effective self-care. This also related to the allocation of reasonable workloads.
Other facilitators of effective self-care were more intrapersonal. These included
having a positive outlook, self-awareness and positive emotions. Self-awareness
was described as central to effective self-care practice. Gratitude and taking
a positive perspective, even in the face of negative circumstances enable self
care. Self-compassion was considered essential to self-care, and relational to
compassion for others.
Authenticity and courage were also described as self-care enablers. These
encompassed self-advocacy and self-acceptance – in terms of being realistic about
limitations; and being, in the words of one participant, authentically human.
8.15.2. Resilience
Resilience has been defined by the American Psychological Association as the
human ability to adapt in the face of tragedy, trauma, adversity, hardship, and
ongoing significant life stressors. Resilience is the ability to cope under pressure
and recover from difficulties. A person who has good resilience copes well under
pressure and can bounce back more quickly than someone whose resilience is less
developed.
a. Behaviors associated with resilience
A person who has a good resilience exhibit understanding and valuing the meaning
of what he/she do, greeting new situations, people and demands with a positive
attitude. He/ she is doing what you can to get on with other people, taking a problem
-solving approach to difficulty, keeping a sense of perspective when things go wrong.
Furthermore, he is being flexible and willing to adapt to change, drawing on a rangeof strategies to cope with pressure, recognizing your thoughts and emotions, and
managing them, asking for help when you need it.
Several attributes are common in resilient people: Resilient people have a positive
image of the future. That is, they maintain a positive outlook, and envision brighter
days ahead. Resilient people have solid goals, and a desire to achieve those goals.
Resilient people are empathetic and compassionate; however, they don't waste
time worrying what others think of them. They maintain healthy relationships, but
don't bow to peer pressure. Resilient people never think of themselves as victims –
they focus their time and energy on changing the things that they have control over.
How we view adversity and stress strongly affects how we succeed, and this is one
of the most important reasons that having a resilient mindset is so important. The
fact is that we're going to fail from time to time: it's an inevitable part of living that
we make mistakes and occasionally fall flat on our faces.
b. Signs of Resilience
Based on years of research into those who tend to be more resilient after hardship,
these six abilities represent some of the core skills in bouncing back:
• Ability to think clearly and flexibly in changing and challenging situations
• Ability to regulate one’s emotions (including stress) and remain emotionally
composed
• Ability to problem-solve, make sensible decisions and mobilize the right
resources that we need
• Ability to maintain positive connections and relationships with others who
support us
• Ability to maintain self-belief and persist in the face of challenging
circumstances (also called grit; ability to face up and continue after a set
back; a positive sense of one’s ability to manage things)
• Ability to maintain a state of wellbeing where we feel well fit and energized
enough to tackle life’s demands (including the demands of work, study, and
home-life and balancing all of our chosen activities/priorities)
c. factors that build resilience
Factors influencing resilience include personality, past experience, current
circumstances and the people around. Other factors contributing to resilience
include having the capacity to make realistic plans, setting goals and taking steps
to carry them out – no matter how small. Resilience is as well influenced by the
capacity to be connected with others and staying social. This is important to have
caring and supportive relationships within and outside the work, family, and in the
community. Resilience is moreover influenced by ability to have a sense of purposein life. Resilient people should be physically stronger. They should monitor their
selves and have mindfulness and the capacity to manage effectively their strong
feelings and impulses in a healthy manner. To be resilient you should focus on
learning and have good communication skills and confidence in your strengths and
abilities.
d. Importance of resilience
Being resilient will help to manage stressful situations, protect from mental illness
and improve health and wellbeing. At work, this ensures that you can continue to
do your job well, and deliver high quality care and support. It can also support in
personal life.
e. Tips of resilience
Tip 1 Focus: Don’t try and do everything. Focus on your priorities. Go back to your
assessments and tools and see what you could be doing at this point.
Tip 2: Find a change partner: Find a colleague you can bounce ideas off inside
or outside your organization. Most people will provide a sounding board to help you
work through an issue or change. It’s ok to talk about your fears – it helps reduce
them.
Tip 3: Know what helps you: You should be aware of what helps you manage
your stress or bring you back to ground or centre. Release the negative self-talk
around making time to decompress. Tip 4: Pragmatist or perfectionist: Sometimes
we care too much and expect too much. Beware of your inner perfectionist and
what purpose it serves. A perfect solution is often not possible. Focus on what you
can actually achieve.
Tip 5: Keep your perspective: We need to live to fight another day - in the end;
some changes are just not going to go well. Do your best and take care of yourself
- both mentally and physically. Take time out to rest and refresh over the break. Set
your work or life boundaries.
f. Pathways to building resilience
Self-care practices help us to build resilience. Even by choosing to put in place
some simple and reliable activities such as exercise, hobbies and catching up with
friends, we’re making a real difference to our minds and bodies – releasing happy
hormones, reducing stress and building healthy self-belief and habits that can
support us when the ‘chips are down’. Choose self-care activities and routines that
include and build on these things:
i. Wellbeing
Maintain basic health: healthy lifestyle routines such as exercise, good nutrition,
sleep and recreation. Practice self-reflection: regularly take time to think and identify
what you honestly need in order to thrive. Choose your attitude: adopt a deliberateand constructive attitude toward life and life’s challenges. Connect to positives:
recall and reconnect to your values, accomplishments and sources of gratitude/joy.
Flex your strengths: identify your strengths and use these more in work and life;
engage in interests/hobbies. Purposeful activity: do things that provide a sense of
purpose, connection and meaning in your life.
ii. Stress management
Social support: spend quality time talking with mates, family and others who can
support you when needed. Recognize stress: acknowledge that stress is normal
and know your early signs of stress (checklists, feelings). Regulate stress: develop
ways to relax and calm yourself on cue, e.g. relaxation exercises, positive thinking.
Problem-solve: adopt a problem-solving approach to life’s hassles – create a written
action plan with options. Manage energy: work around your energy cycle (dips and
peaks); use breaks and healthy energizer activities.
iii. Grit
Develop self-belief: focus on what you can do; visualize success; rehearse
your approach; give things a go. Reframe perspective: be realistic, identify and
‘reframe’ crooked/unhelpful thinking – review your thoughts. Bounce back: (growth
mindset) be open to feedback, learn from mistakes and try again; revise your
approach. Practice Grit: one mental toughness training activity is to persist longer
with uncomfortable or boring tasks. Develop mindfulness: the ability to pay calm
attention, on purpose in the present moment, non-judgmentally.
Professional help and coaching are good ways to proactively build self-care and
resilience, by developing a personalized plan, around the barriers and towards one’s
objectives. Remember that resilience levels change over time and require active
maintenance. You can be hassled or stressed– even if you’re normally resilient and
unbothered by things. In this way we caution that having some ‘resilience’ is not
enough on its own to cope with some very significant events. In these cases, othertools, actions and help will fill the gap.
Self-assessment 8.15
1) Differentiate self-care from resilience
2) Discuss the strategies for physical and psychological self-care3) Discuss the factors that build up resilience
8.16. Practice (return demonstration) of post mortemnursing procedures in skills lab
Learning activity 8.16
This activity should be done by associate nurse learners in simulation
laboratory, under the following instructions:
1) Identify the materials/equipment required for post mortem nursing care2) Use the following check list and practice post –mortem nursing skills
Table 8.16 1 Check list for practicing post mortem nursing technique
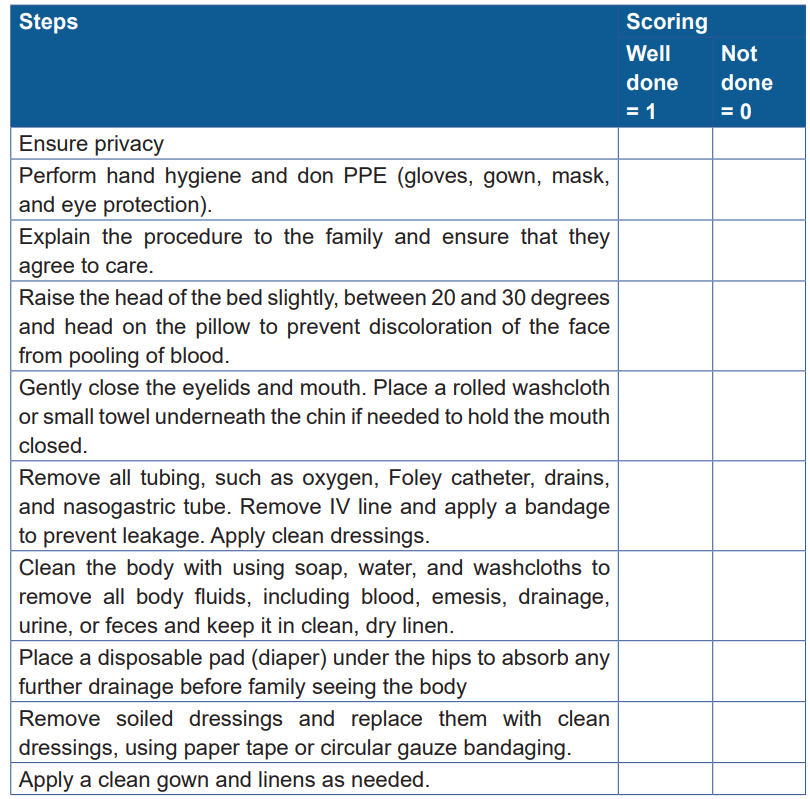
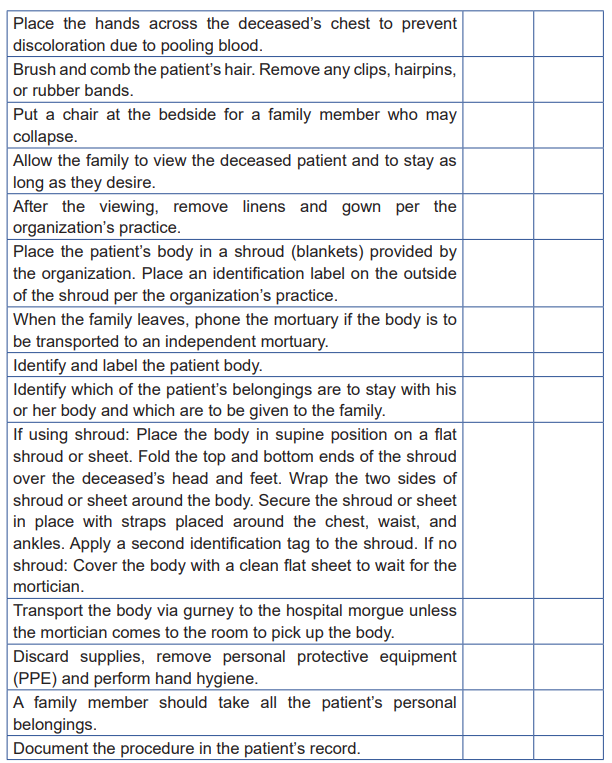
Self-assessment 8.16
In simulation laboratory use the check list presented above and score yourselfafter practicing post mortem care
End unit assessment 8
This end unit assessment 8 includes theoretical assessment of knowledge
acquired evaluation of practical skills which involves the organization of Objective
Structured Clinical Evaluation (OSCE) in skills laboratory.
Theoretical questions
1) Explain any 10 principles of palliative care
2) Explain the components of palliative care
3) Explain the importance of psychosocial support
4) Explain any 5 methods/techniques of non-pharmacological pain
management in palliative care
5) Explain ethical aspects in palliative care
6) Explain the strategies of communication in palliative care
7) Explain any 6 strategies for self-care 8) Explain any 5 ways of
building up resilience
Objective Structure Clinical Evaluation in skills laboratory
After you have practiced palliative care skills, the OSCE in simulation lab should
be organized on the following nursing care: nursing care to the dying patient andpost mortem nursing technique.
REFERENCES
Patricia A. Potter, Anne Griffin Perry, Patricia A. Stockert (2021). Fundamentals of
Nursing, Tenth edition, Elsevier.
Oxford University Press (2002). Essentials of Human Nutrition, SECOND EDITION
Susan G. Dudek (2014).NutritionEssentialsfor NursingPractice, seventh edition,
Lippincott Williams & Wilkins.
Patricia Williams (2016). Basic Geriatric Nursing Sixth edition, Elsevier.
Patricia A. Potter, Anne Griffin Perry, Patricia A. Stockert, Amy M. Hall, (2013).
Fundamentals of nursing, Eighth edition, Mosby, Elsevier.
Berman, Audrey T.; Snyder, Shirlee; Frandsen, Geralyn (2018).Kozier and Erb’s
Fundamentals of Nursing. Concepts, Process and Practice, fourth edition, Pearson
austrarian group.
Peggy S. Stanfield and Hui Y. H., (2010). Nutrition and Diet Therapy, Self
Instructional Approaches, Jones and Bartlett Publishers, LLC
Nix, Staci, (2017).Williams’Basic Nutrition and Diet Therapy, fifteen edition, Elsevier
Inc.
John Wiley & Sons (20080.Nutrition: A Handbook for Nurses, Wiley-Blackwell.
Norman J. Temple and NeliaSteyn (2016).Community nutrition for developing
countries, AU Press, Athabasca University, Canada.
Anne Griffin Perry, Patricia A. Potter, Wendy R. Ostendorf (2014). Clinical Nursing
Skills & Techniques, p790, 8th Edition, Mosby, Inc., an imprint of Elsevier Inc.
Jayne Marshall and Maureen Raynor (2014).Myles Textbook for Midwives, sixteenth
edition, Churchill Livingstone, Elsevier.
Bevan, J. S. (2009). The endocrine system. Macleod’s Clinical Examination. 12th
ed. London: Elsevier Health Sciences, 88-104.
Johnstone, C., Hendry, C., Farley, A., &McLafferty, E. (2014). Endocrine system:
part 1. Nursing Standard, 28(38).
Chaney, D., & Clarke, A. (2014). Nursing care of conditions related to the endocrine
system. s of related interest. Bickley, L. S., & Szilagyi, P. G.(2017) Bates’ Guide for
Physical Examination and History Taking
Lewis S.L. et al (2014) Medical-Surgical Nursing: Assessment and Management of
Clinical Problems
Luis, F., & Moncayo, G. (2018). Health systems policy, Finance and Organization
(G. Carrin, K. Buse, H. K. Heggenhougen, & S. R. Quah (eds.)). World health
Organisation Redional Office of the Eastern Mediterranean.
Takusewanya, M (2019) How to take a complete eye history.community y eye
health journal.32,107
Fotedar -Dr, D. (2018, April 2). Difference Between Myopia and Hypermetropia.
Difference Between Similar Terms and Objects. http://www.differencebetween.net/
science/health/difference-between-myopia-and-hypermetropia/.
Gwenhure T, Shepherd E (2019) Principles and procedure for eye assessment and
cleansing. Nursing Times [online]; 115: 12, 18-20.
Valerie Watson, V(2021)What is ear pain?
Knott,L,Willacy,H, (2021) Ear, Nose and Throat Examination
Prasad, A., Hasan, S., &Gartia, M. R. (2020).Optical Identification of Middle Ear
Infection.Molecules (Basel, Switzerland), 25(9), 2239.https://doi.org/10.3390/
molecules25092239
Earwood, O, S; Rogers, S, T, E Rathjen, N, A, DO, Dwight D (2018)Ear Pain:
Diagnosing Common and Uncommon Causes. Eisenhower Army Medical Center,
Fort Gordon, Georgia
Anderson, L, A, (2021)10 of the Most Common Skin Conditions: Photos and
Treatments
Gail A. Harkness, Rosanna F. DeMarco (2012). Community and Public Health
Nursing, EVIDENCE FOR PRACTICE, Wolters Kluwer Health | Lippincott Williams
& Wilkins.
Hunt, Roberta. (2009). Introduction to community-based nursing, 4th ed. Wolters
Kluwer Health | Lippincott Williams & Wilkins.
Judith A. Allender, Cherie Rector, Kristine D. Warner (2010). Community health
nursing : promoting and protecting the public’s health 7th ed. Wolters Kluwer Health
| Lippincott Williams & Wilkins.
Judith A. Allender, Cherie Rector, Kristine D. Warner (2014).Community &Public
health nursing: Promoting the Public’s Health 8th ed. Wolters Kluwer Health |
Lippincott Williams & Wilkins.
Loue, Sana (2006). Community health advocacy.Journal of epidemiology and
community health 60(6):458-63 DOI:10.1136/jech.2004.023044, retrieved from
https://www.researchgate.net/publication/7082449_Community_health_advocacy
Mary A. Nies, Melanie McEwen (2015). Community/Public Health Nursing:
Promoting the Health of Populations, 6th edition, Elsevier Inc. Saunders.
Matt Vera (2018). Principles of Community Health Nursing, Nurseslabs, Retrieved
from https://nurseslabs.com/community-health-nursing-principles/
Moana M. (2015). Community Nurses Role in Health Promotion. Nursing Exercise
http://nursingexercise.com/community-health-nursing-overview/
National Institute of Statistics of Rwanda (NISR) [Rwanda], Ministry of Health
(MOH) [Rwanda], and ICF International.(2015). Rwanda Demographic and Health
Survey 2014-15. Rockville, Maryland, USA: NISR, MOH, and ICF International.
National Institute of Statistics of Rwanda (NISR) [Rwanda], Ministry of Health (MOH)
[Rwanda], and ICF.(2020). Rwanda Demographic and Health Survey 2019-20 Key
Indicators Report. Kigali, Rwanda, and Rockville, Maryland, USA: NISR and ICF.
Rwanda Ministry of Health (2008).National Community Health Policy.
Rwanda Ministry of Health (2013).National Community Health Strategic Plan, July
2013–June 2018.
Taylor & Francis (2018). A Textbook of Community Nursing, second edition,
Routledge.
WHO (2002). Community home-based care in resource-limited settings, a framework
for action, retrieved from: https://www.who.int/chp/knowledge/publications/comm_
home_based_care.pdf
Wiley Blackwell (2013).Community and Public Health Nursing, 5th edition, John
Wiley & Sons, Ltd.
World Health Organization (1998).Health promotion glossary, World Health
Organization (2005).Effective teaching, A Guide for Educating Healthcare Providers
Bishai, D., & Schleiff, M. (2020). Achieving Health for All Primary Health Care in
Action (Vol. 4). Johns Hopkins University Press.
Donev, D., Kovacic, L., & Laaser, U. (2013). The Role and Organization of Health
Care Systems. In B. G & Z.-K. L (Eds.), Health: Systems – Lifestyles – Policies (2nd
editio, Issue October, pp. 3–14). https://www.researchgate.net/publication/http://
www.seejph.com/category/books/
Greenhalgh, T. (2007). Primary health care Theory and Practice. Blackwell
Publishing Inc.
Przybylska, D., Borzęcki, A., Drop, B., Przybylski, P., & Drop, K. (2014). Health
education as an important tool in the healthcare system. Journal of Public Health
Policy, 124(3), 145–147. https://doi.org/10.2478/pjph-2014-0032
WHO. (2008). Public policies for the public’s health. In World Health Report: Primary
Health Care - Now More Than Ever (pp. 63–77).
WHO. (2017). Primary health care systems ( Primasys ): Case study from Rwanda.
Alliance for Health Policy and Systems Research, 1–16. http://apps.who.int/iris.
Luis, F., & Moncayo, G. (2018). Health systems policy, Finance and Organization
(G. Carrin, K. Buse, H. K. Heggenhougen, & S. R. Quah (eds.)). World health
Organisation Redional Office of the Eastern Mediterranean.
Amadi CC, Okeke OC, Amadi DC, State I. Hazardous Waste Management: a
Review of Principles and Methods. Int J Adv Acad Res | Sci Technol Eng [Internet].
2017;3(8):12. Available from: https://www.ijaar.org/articles/Volume3-Number8/
Sciences-Technology-Engineering/ijaar-ste-v3n6-jn17-p3.pdf
Aime T. Guidelines for Faecal Sludge management [Internet]. KIGALI:
RwandaUtilities Regulatory Autholoty; 2018. Available from: https://rura.rw/
fileadmin/Documents/Water/RegulationsGuidelines/Draft_Guidelines_for_Faecal_
Sludge_Management_for_Rwanda.pdf
Gabriel Adebayo M, Bolu Aliyu SM, Abiodun S. Sustainable Animal Manure
Management Strategies and Practices. Intech [Internet]. 2012;13. Available from:
http://dx.doi.org/10.1039/C7RA00172J%0Ahttps://www.intechopen.com/books/
advanced-biometric-technologies/liveness-detection-in-biometrics%0Ahttp://
dx.doi.org/10.1016/j.colsurfa.2011.12.014
Skibinski K, Smith P, Cross D, Skidmore B. Introduction to Wastewater Management.
Handb Wastewater Manag [Internet]. 2015;1–18. Available from: http://efc.syr.edu/
wp-content/uploads/2015/03/Chapter1-web.pdf
Maeda K, Nitta H. Environmental health. Vol. 6, Journal of Epidemiology. 1996.
Theodore L, Dupont RR. Environmental Health and Hazard Risk Assessment:
Principles and Calculations [Internet]. Taylor & Francis Group. 2012. 636 p. Available
from: https://books.google.com/books?id=d5gyMbKPUXYC&pgis=1
Howard G. Excreta disposal. Heal villages a Guid communities community Heal
[Internet]. 2002;38–47. Available from: https://www.who.int/water_sanitation_
health/hygiene/settings/hvchap4.pdf
MININFRA. National sanitation policy. Development [Internet]. 2006;(March):1–12.
Available from: https://www.mininfra.gov.rw/water-and-sanitation
WHO. Guidelines on sanitation and health. [Internet]. World Health Organization.
2018. 1–220 p. Available from: http://www.who.int/water_sanitation_health/
publications/guidelines-on-sanitation-and-health/en/
Sen S, Roy S, Sarkar A, Chaki N, Debnath NC. Wastewater management. J
Comput Sci [Internet]. 2014;5(4):675–83. Available from: https://www.unwater.org/
app/uploads/2017/05/UN-Water_Analytical_Brief_Wastewater_Management.pdf
Oladoja NA. Appropriate technology for domestic wastewater management in
under-resourced regions of the world. Appl Water Sci. 2017;7(7):3391–406.
Naughton C, Mihelcic J. Introduction to the Importance of Sanitation. Water Sanit
21st Century Heal Microbiol Asp Excreta Wastewater Manag (Global Water Pathog
Proj [Internet]. 2019; Available from: https://www.pseau.org/outils/ouvrages/unicef_
introduction_to_the_importance_of_sanitation_2017.pdf
A UMF, Nhapi I, Wali UG, Banadda N. Assessment of Wastewater Management
Practices in Kigali City , Rwanda. 2010;21–8.
Delahoy MJ, Wodnik B, Mcaliley L, Penakalapati G, Swarthout J, Freeman MC, et al.
International Journal of Hygiene and Pathogens transmitted in animal feces in low
and middle-income countries. Int J Hyg Environ Health [Internet]. 2018;221(4):661–
76. Available from: https://doi.org/10.1016/j.ijheh.2018.03.005 ;
Kennedy, Lloyd-Williams. M (2006) Maintaining Hope: Communication in Palliative
Care.
Manopriya ,V. Renuka, K(2018) Communication Skills in Palliative Care. Pondicherry
journal of nursing.vol.11
Clayton, J., Hancock, K., Butow, P., Tattersall, M. & Currow, D. (2007). Clinical
practice
guidelines for communicating prognosis and end-of-life issues with adults in the
advanced stages of a life-limiting illness, and their caregivers. MJA, 186 (12),
S77-S108.
PCC4U Implementation Guide I (2020) Communication principles
Caissie A, & Zimmermann C (2017). Communication skills for end-of-life care.
McKean S.C., & Ross J.J., & Dressler D.D., & Scheurer D.B.(Eds.), Principles and
Practice of Hospital Medicine, 2e. McGraw Hill. https://accessmedicine.mhmedical.
com/content.aspx?bookid=1872§ionid=14698719 Archer,W, Latif,A & Faull,C
(2017) Communicating with palliative care patients nearing the end of life, their
families and cares
Woogara,N. (2021)Communicating at the end of life.
Kozier, B et al, 2008, Fundamentals of Nursing: Concepts, process and practice,
first publication, Pearson Education Limited
Kozier & Erb’s, 2008, Fundamentals of Nursing: Concepts, Process and Practice,
8th Edition, Pearson Education, Inc, page 850
Kerig, P. (2020). Strengthening your resilience: Take care of yourself as you care
for others. Los Angeles, CA,and Durham, NC: National Center for Child Traumatic
Stress.
Mills, J., Wand, T. & Fraser, J.A. Exploring the meaning and practice of self-care
among palliative care nurses and doctors: a qualitative study. BMC Palliat Care 17,
63 (2018). https://doi.org/10.1186/s12904-018-0318-0
Huggard P., Huggard J. (2019) Self-Care and Palliative Care. In: MacLeod R.,
Van den Block L. (eds) Textbook of Palliative Care. Springer, Cham. https://doi.
org/10.1007/978-3-319-77740-5_44
Austin health (2016) guidelines for care of the dying patient
Marianne M., Deborah W. S., (2010). Palliative Care Nursing, Quality Care to the
End of Life, Springer Publishing Company, LLC.
Margaret O’C., Sanchia A., Susie W., (2003). Palliative Care Nursing, A Guide to
Practice, Second Edition, Taylor and Francis group.
Robert Wood Johnson Foundation (2010).PALLIATIVE CARE, Transforming the
Care of Serious Illness, Jossey-Bass, Sanfrancisco.
Oxford University Press (2010). Oxford Textbook of Palliative Nursing, third edition,
New York.
Derek D.,Roger W. (2008).International Association for Hospice & Palliative Care,
Promoting Hospice & Palliative Care Worldwide, The IAHPC Manual of Palliative
Care
2nd Edition
Kia, Z., Allahbakhshian, M., Ilkhani, M., Nasiri, M., & Allahbakhshian, A. (2021).
Nurses’ use of non-pharmacological pain management methods in intensive care
units: A descriptive cross-sectional study. Complementary Therapies in Medicine,
58, 102705.
Khalil, N. S. (2018). Critical care nurses' use of non-pharmacological pain
management methods in Egypt. Applied Nursing Research, 44, 33-38.
Lewis, M. J. M., Kohtz, C., Emmerling, S., Fisher, M., & Mcgarvey, J. (2018). Pain
control and nonpharmacologic interventions. Nursing2020, 48(9), 65-68
Rego, F., Pereira, C., Rego, G., & Nunes, R. (2018). The psychological and spiritual
dimensions of palliative care: a descriptive systematic review. Neuropsychiatry,8(2), 484-494
Cerit, E., & Özkan, B. (2021). The Importance of Spiritual Care in Nursing. Turkish
Journal of Science and Health, 2(2), 33-39.
Shipman C, Levenson R, Gillam S. Psychosocial Support. King’s fund [Internet].
2009;66(8):828–37. Available from: https://www.kingsfund.org.uk/sites/default/
files/PsychosocialSupport.pdf
Anderson L. Psychosocial Support for the Palliative Care Patient. Wound Essentials.
2011;6:84–6.
Bouleuc C, Burnod A, Angellier E, Massiani MA, Robin ML, Copel L, et al. Early
palliative care in oncology [Internet]. Alt-Epping B, Nauck F, editors. Vol. 106,
Bulletin du Cancer. New york: Springer-Verlag Berlin Heidelberg; 2019. 796–804 p.
Available from: https://usa1lib.org/book/2528204/959e1
