UNIT5:INTRODUCTION TO COMMUNITY HEALTH NURSING
Key Unit Competence:
Provide basic community interventions
Introductory activity 5
Observe the pictures A, B, C, and D
1) Describe the pictures A, B, C and D
2) According to you, what do you think is the focus of this unit 5?
Introduction
As a specialty field of nursing, community health nursing adds public health
knowledge and skills that address the needs and problems of communities
and aggregates and focuses care on communities and vulnerable populations.
Community health nursing is grounded in both public health science and nursing
science, which makes its philosophical orientation and the nature of its practice
unique. It has been recognized as a subspecialty of both fields.
5.1. Overview of community health Nursing:
This sub-unit of overview of community health nursing discusses the Concepts
definition, History of community health nursing, and objectives of Community health
nursing. It also argues on characteristics of community health nursing, principles ofcommunity health nursing and community Health in Rwanda
5.1.1. Concepts definition
Learning activity 5.1.1
With use of student text book of fundamentals of nursing (senior six) or the
library text books of community health nursing / public health nursing, define
the following terms/concepts: health, a community, an aggregate, social
determinants of health, community health nursing, public health, primaryprevention, secondary prevention, and tertiary prevention.
a. Health
Health is defined in the WHO constitution of 1948 as: A state of complete physical,
social and mental well-being, and not merely the absence of disease or infirmity.
Here below, there discussion of each of those components of health (that is physical,
mental (or psychological), and social well-being).
Defining physical health
Physical health, which is one of the components of the definition of health, could
be defined as the absence of diseases or disability of the body parts. Physical
health could be defined as the ability to perform routine tasks without any physical
restriction. The following examples can help you to understand someone who is
physically unhealthy:
• A person who has been harmed due to a car accident
• A farmer infected by malaria and unable to do their farming duties
• A person infected by tuberculosis and unable to perform his or her tasks.Psychological health
Sometimes it can be really hard from the outside to tell if the person is struggling
with mental health issues, but at other times they show symptoms that suggest a
lack of self-awareness or personal identity, or an inability of rational and logical
decision-making.
At other times it might be apparent that they are not looking after themselves and
are without a proper purpose in their life. They may be drinking alcohol and have a
non-logical response to any request. You may also notice that they have an inability
to maintain their personal autonomy and are unable to maintain good relationships
with people around them. So how do we recognize a mentally healthy adult? The
mentally healthy adult shows behavior that demonstrates awareness of self, who
has purpose to their life, a sense of self understanding, self-value and a willingness
to perceive reality and cope with its difficulties.
The mentally healthy adult is active, hardworking and productive, persists with tasks
until they are completed, logically thinks about things affecting their own health,
responds flexibly in the face of stress, receives pleasure from a variety of sources,
and accepts their own limitations realistically. The healthy adult has a capacity
to live with other people and understand other people’s needs. It is sometimes
considered that the mentally healthy person shows growth and maturity in three
areas: cognitive, emotional and social. The next part will help you understand
these three components of psychological health:
Cognitive component
The cognitive component of mental health is really to do with thinking and being
able to work things out. It includes the ability of an individual to learn, to have
awareness (consciousness) and to perceive reality. At a higher level it also involves
having a memory and being able to reason rationally and solve problems, as well
as being able to work creativity and have a sense of imagination.
Emotional component
When you are implementing a health extension program, you may encounter
various feelings or emotions in households in your community such as happiness,
anger or sadness. People might cry or laugh. The emotional component of health
is the ability and skill of expressing emotions in an ‘appropriate’ way. The word
“appropriate” means that the type of response should be able to match the problem.
In the previous section you have learned something about the physical and mental
components of health. Social health is also an important component of overall
health and in the next section you will consider the definition and some examplesof social health.
Social component
A social role can be developed while taking part in communal activities such as
harvesting or other activities where teamwork is important.
The social component of health is considered to be the ability to make and
maintain ‘acceptable’ and ‘proper’ interactions and communicate with other people
within the social environment. This component also includes being able to maintain
satisfying interpersonal relationships and being able to fulfill a social role. Having
a social role is the ability that people have to maintain their own identity while
sharing, cooperating, communicating and enjoying the company of others. This is
really important when participating in friendships and taking a full part in family and
community life.
The following examples could be considered to contribute to social health:
1. Mourning when a close family member dies
2. Going to a football match or involvement in a community meeting
3. Celebrating traditional festivals within your community
4. Shopping in the market
5. Creating and maintaining friendship.
In reality all these events could have a social component and help towards building
people’s social view of health. They all involve interacting with others and gaining
support, friendship and in many instances joy from being with other people.
b. Community
The definitions of community are numerous and variable. Before 1996, definitions
of community focused on geographic boundaries combined with social attributes of
people.
In recent nursing literature, community has been defined as “a collection of people
who interact with one another and whose common interests or characteristics form
the basis for a sense of unity or belonging”.
Maurer and Smith (2013) further addressed the concept of community and
identified three defining attributes: people, place, and social interaction or common
characteristics, interests, or goals. Combining ideas and concepts, in this text,
community is seen as a group or collection of individuals interacting in social
units and sharing common interests, characteristics, values, and goals.
Maurer and Smith (2013) noted that there are two main types of communities:
geopolitical communities and phenomenological communities. Geopolitical
communities are those most traditionally recognized or imagined when the
term community is considered. Geopolitical communities are defined or formed
by natural and/or manmade boundaries and include cities, counties, states, and
nations. Other commonly recognized geopolitical communities are school districts,
census tracts, and neighborhoods.
Phenomenological communities, on the other hand, refer to relational, interactive
groups. In phenomenological communities, the place or setting is more abstract,
and people share a group perspective or identity based on culture, values, history,
interests, and goals. Examples of phenomenological communities are schools,
colleges, and universities; churches, synagogues, and mosques; and various
groups and organizations, such as social networks.
A community of solution is a type of phenomenological community. A community of
solution is a collection of people who form a group specifically to address a common
need or concern. The Sierra Club, whose members lobby for the preservation of
natural resource lands, and a group of disabled people who challenge the owners
of an office building to obtain equal access to public buildings, education, jobs, and
transportation are examples. These groups or social units work together to promote
optimal “health” and to address identified actual and potential health threats and
health needs.
c. Aggregate
It is a population group with common characteristics. Aggregates are subgroups or
subpopulations that have some common characteristics or concerns.
Depending on the situation, needs, and practice parameters, community health
nursing interventions may be directed toward a community (e.g., residents of a
small town), a population (e.g., all elders in a rural region), or an aggregate (e.g.,
pregnant teens within a school district).
d. Community-based nursing
Community-based nursing is setting-specific, and the emphasis is on acute and
chronic care and includes such practice areas as home health nursing and nursing
in outpatient or ambulatory settings. Community-based nursing practice refers to
application of the nursing process in caring for individuals, families and groups
where they live, work or go to school or as they move through the health care
system.
At present, community-based nursing is defined as minor acute and chronic care
that is comprehensive, coordinated, and delivered where people work, live, or
attends school. Community-based nursing is an extension of illness care provided
to clients and their families outside the acute care setting. Although the client’s
individual needs are met, the nurses may not be paying attention to family dynamics,
environmental health, health education, and health promotion.
For the past few decades, the title community health nurse has been used todesignate nursing care in community settings that combines the practice of
community-based nursing and public health nursing. The practice of community
health nursing is the use of systematic processes to deliver care to individual
people, families, and community groups with a focus on promoting, preserving,
protecting, and maintaining health. In doing so, the care directed to the individual
person, family, or community group contributes to the health of the population as a
whole.
e. Community health nursing
It is the use of systematic processes to deliver care to individuals, families,
and community groups with a focus on promoting, preserving, protecting, and
maintaining health.
Community-based nursing and community health nursing have different goals.
Community health nursing emphasizes preservation and protection of health, and
community-based nursing emphasizes managing acute or chronic conditions.
In community health nursing, the primary client is the community; in community
based nursing, the primary clients are the individual and the family. Finally, services
in community-based nursing are largely direct, but in community health nursing,
services are both direct and indirect.
f. Epidemiology
It is the study of the distribution and determinants of states of health and illness in
human populations.
g. Evidence-based nursing
It is the integration of the best evidence available with clinical expertise and the
values of the client to increase the quality of care.
h. Healthcare disparities
Gaps in healthcare experienced by one population compared with another.
i. Health information technology
It is comprehensive management of health information and its secure exchange
between consumers, providers, government and quality entities, and insurers.
j. Public health
Contrasting with “medical care,” which focuses on disease management and
“cure,” public health efforts focus on health promotion and disease prevention.
Health promotion activities enhance resources directed at improving well-being,
whereas disease prevention activities protect people from disease and the effects
of disease.
C. E. Winslow is known for the following classic definition of public health: Public
health is the Science and Art of (1) preventing disease, (2) prolonging life, and(3) promoting health and efficiency through organized community effort for: (a)
sanitation of the environment, (b) control of communicable infections, (c) education
of the individual in personal hygiene, (d) organization of medical and nursing services
for the early diagnosis and preventive treatment of disease, and (e) development
of the social machinery to ensure everyone a standard of living adequate for the
maintenance of health, so organizing these benefits as to enable every citizen to
realize his birthright of health and longevity
k. Public health nursing
Population-based practice, defined as a synthesis of nursing and public health
within the context of preventing disease and disability and promoting and protecting
the health of the entire community.
l. Social determinants of health:
These are the social conditions in which people live and work. The health status of
a community is associated with a number of factors, such as health care access,
economic conditions, social and environmental issues, and cultural practices, and it
is essential for the community health nurse to understand the determinants of health
and recognize the interaction of the factors that lead to disease, death, and disability.
Indeed, individual biology and behaviors influence health through their interaction
with each other and with the individual’s social and physical environments. Thus,
policies and interventions can improve health by targeting detrimental or harmful
factors related to individuals and their environment.
Community and public health nurses should understand social determinants of
health and appreciate that health and illness are influenced by a web of factors,
some that can be changed (e.g., individual behaviors such as tobacco use, alcohol
consumption, diet, physical activity) and some that cannot (e.g., genetics, age,
gender). Other factors (e.g., physical and social environment) may require changes
that will need to be accomplished from a policy perspective. Community health
nurses must work with policy makers and community leaders to identify patterns of
disease and death and to advocate for activities and policies that promote health at
the individual, family, and population levels.
m.Preventive Approach to Health
Leavell and Clark (1958) identified three levels of prevention commonly described in
nursing practice: primary prevention, secondary prevention, and tertiary preventionas illustrated in the following figure:
Primary prevention relates to activities directed at preventing a problem before it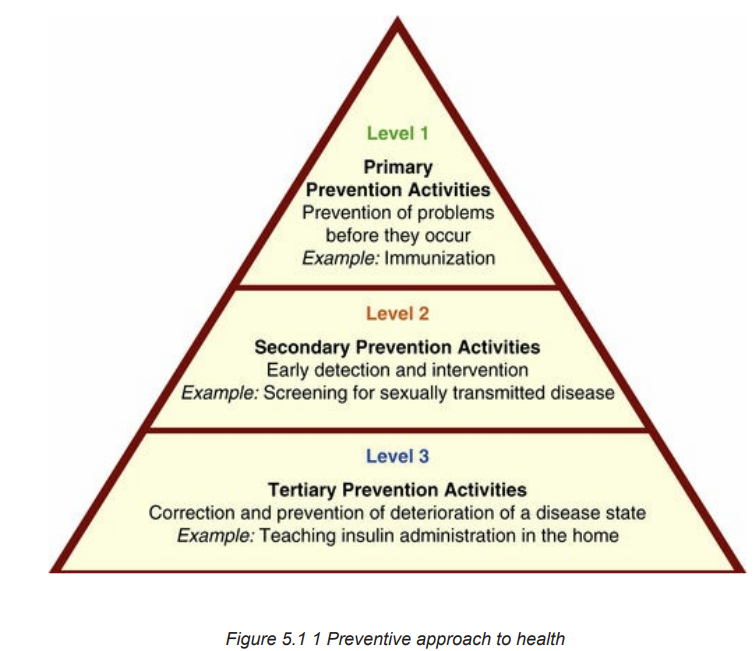
occurs by altering susceptibility or reducing exposure for susceptible individuals.
Primary prevention consists of two elements: general health promotion and specific
protection. Health promotion efforts enhance resiliency and protective factors and
target essentially well populations. Examples include promotion of good nutrition,
provision of adequate shelter, and encouraging regular exercise. Specific protection
efforts reduce or eliminate risk factors and include such measures as immunization
and water purification.
Secondary prevention refers to early detection and prompt intervention during
the period of early disease pathogenesis. Secondary prevention is implemented
after a problem has begun, but before signs and symptoms appear. It targets
those populations that have risk factors. Mammography, blood pressure screening,
scoliosis screening, and Papanicolaou smears are examples of secondary
prevention.
Tertiary prevention targets populations that have experienced disease or injury
and focuses on limitation of disability and rehabilitation. Aims of tertiary prevention
are to keep health problems from getting worse, to reduce the effects of disease
and injury, and to restore individuals to their optimal level of functioning. Examples
include teaching how to perform insulin injections and disease management to a
patient with diabetes, referral of a patient with spinal cord injury for occupational
and physical therapy, and leading a support group for grieving parents.
Much of community health nursing practice is directed toward preventing the
progression of disease at the earliest period or phase feasible using the appropriate
level(s) of prevention. For example, when applying “levels of prevention” to a client
with HIV/AIDS, a nurse might perform the following interventions:
• Educate students on the practice of sexual abstinence or “safer sex” by using
barrier methods (primary prevention)
• Encourage testing and counseling for clients with known exposure or who are
in high-risk groups; provide referrals for follow-up for clients who test positive
for HIV (secondary prevention)
• Provide education on management of HIV infection, advocacy, case
management, and other interventions for those who are HIV positive (tertiaryprevention).
Self-assessment 5.1.1
1) Give at least 4 social determinants of health
2) Differentiate a community from an aggregate
3) Differentiate community-based nursing from community health nursing.
4) With examples, differentiate physical health from psychological health
5) With examples, differentiate the three levels of prevention commonlydescribed in nursing practice
5.1.2. History of community health Nursing
Learning activity 5.1.2
By the use of community health nursing books and internet resources, found
out at least three key periods of the history of community health nursing andexplain them.
Traditionally, historians believed that organized public health efforts were eighteenth
and nineteenth-century activities associated with the Sanitary Revolution. However,
modern historians have shown that organized community health efforts to prevent
disease, prolong life, and promote health have existed since early human history.
Public health efforts developed slowly over time. The following sections briefly tracethe evolution of organized public health and highlight the periods of prerecorded
historic times (i.e., before 5000 BCE), classical times (i.e., 3000 to 200 BCE), the
Middle Ages (i.e., 500 to 1500 CE), the Renaissance (i.e., fifteenth, sixteenth, and
seventeenth centuries), the eighteenth century, and the nineteenth century, and
into the present day.
a. Prerecorded Historic Times
From the early remains of human habitation, anthropologists recognize that early
nomadic humans became domesticated and tended to live in increasingly larger
groups. Aggregates ranging from family to community inevitably shared episodes
of life, health, sickness, and death. Whether based on superstition or sanitation,
health practices evolved to ensure the survival of many aggregates. For example,
primitive societies used elements of medicine (e.g., voodoo), isolation (e.g.,
banishment), and fumigation (i.e., use of smoke) to manage disease and thus
protect the community for thousands of years.
Classical Times
In the early years of the period 3000 to 1400 BCE, the Minoans devised ways
to flush water and construct drainage systems. Circa 1000 BCE, the Egyptians
constructed elaborate drainage systems, developed pharmaceutical preparations,
and embalmed the dead. Pollution is an ancient problem. The Biblical Book of
Exodus reported that “all the waters that were in the river stank,” and in the Book of
Leviticus (believed to be written around 500 BCE), the Hebrews formulated the first
written hygiene code. This hygiene code protected water and food by creating laws
that governed personal and community hygiene such as contagion, disinfection,
and sanitation.
Greece
Greek literature contains accounts of communicable diseases such as diphtheria,
mumps, and malaria. The Hippocratic book On Airs, Waters and Places, a treatise
on the balance between humans and their environment, may have been the only
volume on this topic until the development of bacteriology in the late nineteenth
century. Diseases that were always present in a population, such as colds and
pneumonia, were called endemic. Diseases such as diphtheria and measles,
which were occasionally present and often fairly widespread, were called epidemic.
The Greeks emphasized the preservation of health, or good living, which the
goddess Hygeia represented, and curative medicine, which the goddess Panacea
personified. Human life had to be in balance with environmental demands; therefore
the Greeks weighed the importance of exercise, rest, and nutrition according to
age, sex, constitution, and climate.
Rome
Although the Romans readily adopted Greek culture, they far surpassed Greekengineering by constructing massive aqueducts, bathhouses, and sewer systems.
For example, at the height of the Roman Empire, Rome provided its 1 million
inhabitants with 40 gallons of water per person per day, which is comparable to
modern consumption rates. Inhabitants of the overcrowded Roman slums, however,
did not share in public health amenities such as sewer systems and latrines, and
their health suffered accordingly. The Romans also observed and addressed
occupational health threats. In particular, they noted the pallor of the miners, the
danger of suffocation, and the smell of caustic fumes. The ancient Romans provided
public health services that included the following:
• A water board to maintain the aqueducts
• A supervisor of the public baths
• Street cleaners
• Supervision of the sale of food
For protection, miners devised safeguards by using masks made of bags, sacks,
membranes, and bladder skins. In the early years of the Roman Republic, priests
were believed to mediate diseases and often dispensed medicine. Public physicians
worked in designated towns and earned money to care for the poor. In addition,
they were able to charge wealthier patients a service fee.
Much as in a modern health maintenance organization (HMO) or group practice,
several families paid a set fee for yearly services. Hospitals, surgeries, infirmaries,
and nursing homes appeared throughout Rome. In the fourth century, a Christian
woman named Fabiola established a hospital for the sick poor. Others repeated this
model throughout medieval times.
b. Middle Ages
The decline of Rome, which occurred circa 500 CE, led to the Middle Ages.
Monasteries promoted collective activity to protect public health, and the population
adopted protective measures such as building wells and fountains, cleaning streets,
and disposing of refuse. The commonly occurring communicable diseases were
measles, smallpox, diphtheria, leprosy, and bubonic plague. Physicians had little
to offer in the management of diseases such as leprosy. The church took over by
enforcing the hygienic codes from Leviticus and establishing isolation and leper
houses, or leprosaria.
A pandemic is the existence of disease in a large proportion of the population. One
such pandemic, the bubonic plague, ravaged much of the world in the fourteenth
century. This plague, or Black Death, claimed close to half the world’s population at
that time. For centuries, medicine and science did not recognize that fleas, which
were attracted to the large number of rodents inhabiting urban areas, were the
transmitters of plague. Modern public health practices such as isolation, disinfection,and ship quarantines emerged in response to the bubonic plague.
During the Middle Ages, clergymen often acted as physicians and treated kings and
noblemen. Monks and nuns provided nursing care in small houses designated as
structures similar to today’s small hospitals. Medieval writings contained information
on hygiene and addressed such topics as housing, diet, personal cleanliness, and
sleep.
c. The Renaissance
Although the cause of infectious disease remained undiscovered, two
events important to public health occurred during the Renaissance. In 1546,
GirolamoFracastoro presented a theory that infection was a cause and epidemic
a consequence of the “seeds of disease.” Then, in 1676, Anton van Leeuwenhoek
described microscopic organisms, although he did not associate them with disease.
The Elizabethan Poor Law, enacted in England in 1601, held the church parishes
responsible for providing relief for the poor. This law governed health care for the
poor for more than two centuries and became a prototype for later U.S. laws.
d. Eighteenth Century
Great Britain
The eighteenth century was marked by imperialism and industrialization. Sanitary
conditions remained a huge problem. During the Industrial Revolution, a gradual
change in industrial productivity occurred. The industrial boom sacrificed many
lives for profit. In particular, it forced poor children into labor. Under the Elizabethan
Poor Law, parishes established workhouses to employ the poor. Orphaned and
poor children were wards of the parish; therefore the parish forced these young
children to labor in parish workhouses for long hours.
At 12 to 14 years of age, a child became a master’s apprentice. Those apprenticed
to chimney sweeps reportedly suffered the worst fate because their masters forced
them into chimneys at the risk of being burned and suffocated. Vaccination was
a major discovery of the times. In 1796, Edward Jenner observed that people
who worked around cattle were less likely to have smallpox. He concluded that
immunity to smallpox resulted from an inoculation with the cowpox virus. Jenner’s
contribution was significant because approximately 95% of the population suffered
from smallpox and approximately 10% of the population died of smallpox during the
eighteenth century. Frequently, the faces of those who survived the disease were
scarred with pockmarks.
e. Nineteenth Century
Europe
During the nineteenth century, communicable diseases ravaged the population
that lived in unsanitary conditions, and many lives were lost. For example, in themid-1800s, typhus and typhoid fever claimed twice as many lives each year as
the Battle of Waterloo. Edwin Chadwick called attention to the consequences of
unsanitary conditions that resulted in health disparities that shortened life spans of
the laboring class in particular. Chadwick contended that death rates were high in
large industrial cities such as Liverpool, where more than half of all children born
of working-class parents died by age 5. Laborers lived an average of 16 years. In
contrast, tradesmen lived 22 years, and the upper classes lived 36 years.
In 1842, Chadwick published his famous Report on an Inquiry Into the Sanitary
Conditions of the Laboring Population of Great Britain. The report furthered the
establishment of the General Board of Health for England in 1848. Legislation for
social reform followed, addressing prevailing concerns such as child welfare, factory
management, education, and care for the elderly, sick, and mentally ill. Clean water,
sewers, fireplugs, and sidewalks emerged as a result.
In 1849, a German pathologist named Rudolf Virchow argued for social action—
bettering the lives of the people by improving economic, social, and environmental
conditions—to attack the root social causes of disease. He proposed “a theory
of epidemic disease as a manifestation of social and cultural maladjustment”. He
further argued that the public was responsible for the health of the people; that
social and economic conditions heavily affected health and disease; that efforts to
promote health and fight disease must be social, economic, and medical; and that
the study of social and economic determinants of health and disease would yield
knowledge to guide appropriate action. In 1849, these principles were embodied
in a public health law submitted to the Berlin Society of Physicians and Surgeons.
According to this document, public health has as its objectives: (1) The healthy
mental and physical development of the citizen, (2) the prevention of all dangers to
health, and (3) the control of disease.
It was pointed out that public health cares for society as a whole by considering
the general physical and social conditions that may adversely affect health and
protects each individual by considering those conditions that prevent the individual
from caring for his or her health. These “conditions” may fit into one of two major
categories: conditions that give the individual the right to request assistance from
the state (e.g., poverty and infirmity) and conditions that give the state the right and
obligation to interfere with the personal liberty of the individual (e.g., transmissible
diseases and mental illness).
A very critical event in the development of modern public health occurred in 1854,
when an English physician, anesthetist, and epidemiologist named John Snow
demonstrated that cholera was transmissible through contaminated water. In a large
population afflicted with cholera, he shut down the community’s water resource by
removing the pump handle from a well and carefully documented changes as thenumber of cholera cases fell dramatically
f. Advent of Modern Health Care
Early public health efforts evolved further in the mid-nineteenth century.
Administrative efforts, initial legislation, and debate regarding the determinants
of health and approaches to health management began to appear on a social,
economic, and medical level. The advent of “modern” health care occurred around
this time, and nursing made a large contribution to the progress of health care.
The following sections discuss the evolution of modern nursing, the evolution of
modern medical care and public health practice, the evolution of the community
caregiver, and the establishment of public health nursing.
Evolution of Modern Nursing
Florence Nightingale, the woman credited with establishing “modern nursing,”
began her work during the mid-nineteenth century. Historians remember Florence
Nightingale for contributing to the health of British soldiers during the Crimean War
and establishing nursing education. However, many historians failed to recognize her
remarkable use of public health principles and distinguished scientific contributions
to health care reform The following review of Nightingale’s work emphasizes her
concern for environmental determinants of health; her focus on the aggregate
of British soldiers through emphasis on sanitation, community assessment, and
analysis; the development of the use of graphically depicted statistics; and the
gathering of comparable census data and political advocacy on behalf of the
aggregate.
Nightingale was from a wealthy English family, was well educated, and traveled
extensively. Her father tutored her in mathematics and many other subjects.
Nightingale later studied with Adolphe Quetelet, a Belgian statistician. Quetelet
influenced her profoundly and taught her the discipline of social inquiry. Nightingale
also had a passion for hygiene and health. In 1851, at the age of 31 years, she
trained in nursing with Pastor Fliedner at Kaiserswerth Hospital in Germany. She
later studied the organization and discipline of the Sisters of Charity in Paris.
Nightingale wrote extensively and published her analyses of the many nursing
systems she studied in France, Austria, Italy, and Germany.
In 1854, Nightingale responded to distressing accounts of a lack of care for wounded
soldiers during the Crimean War. She and 40 other nurses traveled to Scutari,
which was part of the Ottoman Empire at the time. Nightingale was accompanied
by lay nurses, Roman Catholic sisters, and Anglican sisters. Upon their arrival, the
nurses learned that the British army’s management method for treating the sick
and wounded had created conditions that resulted in extraordinarily high death
rates among soldiers. One of Nightingale’s greatest achievements was improving
the management of ill and wounded soldiers. Nightingale faced an assignment inThe Barrack Hospital, which had been built for 1700 patients. In 4 miles of beds,
she found 3000 to 4000 patients separated from each other by only 18 inches
of space. During the Crimean War, cholera and “contagious fever” were rampant.
Equal numbers of men died of disease and battlefield injury. Nightingale found
that allocated supplies were bound in bureaucratic red tape; for example, supplies
were “sent to the wrong ports or were buried under munitions and could not be
got”. Nightingale encountered problems reforming the army’s methods for care of
the sick because she had to work through eight military affairs departments related
to her assignment. She sent reports of the appalling conditions of the hospitals to
London. In response to her actions, governmental and private funds were provided
to set up diet kitchens and a laundry and provided food, clothing, dressings, and
laboratory equipment Major reforms occurred during the first 2 months of her
assignment. Aware that an interest in keeping social statistics was emerging,
Nightingale realized that her most forceful argument would be statistical in nature.
She reorganized the methods of keeping statistics and was the first to use shaded
and colored coxcomb graphs of wedges, circles, and squares to illustrate the
preventable deaths of soldiers. Nightingale compared the deaths of soldiers in
hospitals during the Crimean War with the average annual mortality in Manchester
and with the deaths of soldiers in military hospitals in and near London at the time.
Through her statistics she also showed that, by the end of the war, the death rate
among ill soldiers during the Crimean War was no higher than that among well
soldiers in Britain.
Indeed, Nightingale’s careful statistics revealed that the death rate for treated
soldiers decreased from 42% to 2%. Furthermore, she established community
services and activities to improve the quality of life for recovering soldiers. These
included rest and recreation facilities, study opportunities, a savings fund, and a
post office. She also organized care for the families of the soldiers.
After returning to London at the close of the war in 1856, Nightingale devoted her
efforts to sanitary reform. At home, she surmised that if the sanitary neglect of
the soldiers existed in the battle area, it probably existed at home in London. She
prepared statistical tables to support her suspicions.
In one study comparing the mortality of men aged 25 to 35 years in the army
barracks of England with that of men the same age in civilian life, Nightingale found
that the mortality of the soldiers was nearly twice that of the civilians. In one of her
reports, she stated that “our soldiers enlist to death in the barracks”. Furthermore,
she believed that allowing young soldiers to die needlessly of unsanitary conditions
was equivalent to taking them out, lining them up, and shooting them. She was
very political and did not keep her community assessment and analysis to herself.
Nightingale distributed her reports to members of Parliament and to the medical and
commanding officers of the army. Prominent male leaders of the time challengedher reports. Undaunted, she rewrote them in greater depth and redistributed them
In her efforts to compare the hospital systems in European countries, Nightingale
discovered that each hospital kept incomparable data and that many hospitals used
various names and classifications for diseases. She noted that these differences
prevented the collection of similar statistics from larger geographic areas. These
statistics would create a regional health-illness profile and allow for comparison
with other regions. She printed common statistical forms that some hospitals in
London adopted on an experimental basis. Nightingale also stressed the need to
use statistics at the administrative and political levels to direct health policy. Noting
the ignorance of politicians and those who set policy regarding the interpretation
and use of statistics, she emphasized the need to teach national leaders to use
statistical facts. Nightingale continued the development and application of statistical
procedures, and she won recognition for her efforts. The Royal Statistical Society
made her a fellow in 1858, and the American Statistical Association made her an
honorary member in 1874.
In addition to her contributions to nursing and her development of nursing education,
Nightingale’s credits include the application of statistical information toward an
understanding of the total environmental situation. Population-based statistics
have marked implications for the development of public health and public health
nursing. Grier and Grier (1978) recognized Nightingale’s contributions to statistics
and stated, “Her name occurs in the index of many texts on the history of probability
and statistics, in the history of quantitative graphics, and in texts on the history of
science and mathematics.” It is interesting to note that the paradigm for nursing
practice and nursing education that evolved through Nightingale’s work did not
incorporate her emphasis on statistics and a sound research base. It is also curious
that nursing education did not consult her writings and did not stress the importance
of determining health’s social and environmental determinants until much later.
Establishment of Modern Medical Care and Public Health Practice
To place Nightingale’s work in perspective, it is necessary to consider the
development of medical care in light of common education and practice during
the late nineteenth and early twentieth centuries. Goodnow (1933) called this
time a “dark age.” Medical sciences were underdeveloped, and bacteriology was
unknown. Few medical schools existed at the time, so apprenticeship was the path
to medical education. The majority of physicians believed in the “spontaneous
generation” theory of disease causation, which stated that disease organisms grew
from nothing.
Typical medical treatment included bloodletting, starving, using leeches, and
prescribing large doses of metals such as mercury and antimony. Nightingale’s
uniform classification of hospital statistics noted the need to tabulate the classification
of diseases in hospital patients and the need to note the diseases that patients
contracted in the hospital. These diseases, such as gangrene and septicemia,
were later called iatrogenic diseases. Considering the lack of surgical sanitation in
hospitals at the time, it is not surprising that iatrogenic infection was rampant. For
example, Goodnow (1933) illustrates the following unsanitary operating procedures:
Before an operation, the surgeon turned up the sleeves of his coat to save the coat,
and would often not trouble to wash his hands, knowing how soiled they soon would
be! The area of the operation would sometimes be washed with soap and water,
but not always, for the inevitability of corruption made it seem useless. The silk or
thread used for stitches or ligatures was hung over a button of the surgeon’s coat,
and during the operation a convenient place for the knife to rest was between his
lips. Instruments used for lancing abscesses were kept in the vest pocket and often
only wiped with a piece of rag as the surgeon went from one patient to another.
During the nineteenth century, the following important scientists were born: Louis
Pasteur in 1822, Joseph Lister in 1827, and Robert Koch in 1843. Their research
also had a profound impact on health care, medicine, and nursing. Pasteur was
a chemist, not a physician. While experimenting with wine production in 1854, he
proposed the theory of the existence of germs. Although his colleagues ridiculed
him at first, Koch applied his theories and developed his methods for handling and
studying bacteria. Subsequently, Pasteur’s colleagues gave him acknowledgment
for his work.
Lister, whose father perfected the microscope, observed the healing processes of
fractures. He noted that when the bone was broken but the skin was not, recovery
was uneventful. However, when both the bone and the skin were broken, fever,
infection, and even death were frequent. He found the proposed answer to his
observation through Pasteur’s work. Something outside the body entered the
wound through the broken skin, causing the infection. Lister’s surgical successes
eventually improved when he soaked the dressings and instruments in mixtures of
carbolic acid (i.e., phenol) and oil.
In 1882, Koch discovered the causative agent for cholera and the tubercle bacillus.
Pasteur discovered immunization in 1881 and the rabies vaccine in 1885. These
discoveries were significant to the development of public health and medicine.
However, physicians accepted these discoveries slowly. For example, TB was
a major cause of death in late nineteenth century America and often plagued its
victims with chronic illness and disability. It was a highly stigmatized disease, and
most physicians thought it was a hereditary, constitutional disease associated with
poor environmental conditions.
Hospitalization for TB was rare because the stigma caused families to hide their
infected relatives. Without treatment, the communicability of the disease increased.
The common treatment was a change of climate. Although Koch had announcedthe discovery of the tubercle bacillus in 1882, it was 10 years before the emergence
of the first organized community campaign to stop the spread of the disease.
The case of puerperal (i.e., childbirth) fever illustrates another example of slow
innovation stemming from scientific discoveries. Although Pasteur showed that
Streptococcus caused puerperal fever, it was years before physicians accepted
his discovery. However, medical practice eventually changed, and physicians no
longer delivered infants after performing autopsies of puerperal fever cases without
washing their hands.
Debates over the causes of disease occurred throughout the nineteenth century.
Scientists discovered organisms during the latter part of the century, supporting the
theory that specific contagious entities caused disease. This discovery challenged
the earlier, miasmic theory that environment and atmospheric conditions caused
disease.
The new scientific discoveries had a major impact on the development of public
health and medical practice. The emergence of the germ theory of disease focused
diagnosis and treatment on the individual organism and the individual disease.
State and local governments felt increasingly responsible for controlling the spread
of bacteria and other microorganisms. A community outcry for social reform forced
state and local governments to take notice of the deplorable living conditions in the
cities.
Community Caregiver
The traditional role of the community caregiver or the traditional healer has nearly
vanished. However, medical and nurse anthropologists who have studied primitive
and Western cultures are familiar with the community healer and caregiver role.
The traditional healer (e.g., shaman, midwife, herbalist, or priest) is common in non
Western, ancient, and underdeveloped societies. Although traditional healers have
always existed, professionals and many people throughout industrialized societies
may overlook or minimize their role. The role of the healer is often integrated into
other institutions of society, including religion, medicine, and morality. The notion
that one person acts alone in healing may be foreign to many cultures; healers can
be individuals, kin, or entire societies.
Societies retain folk practices because they offer repeated success.
Most cultures have a pharmacopoeia and maintain therapeutic and preventive
practices, and it is estimated that one fourth to one half of folk medicines are
empirically effective. Indeed, many modern drugs are based on the medicines of
primitive cultures (e.g., eucalyptus, coca, and opium).
Since ancient times, folk healers and cultural practices have both positively and
negatively affected health. The late nineteenth and early twentieth century practiceof midwifery illustrates modern medicine’s arguably sometimes negative impact on
traditional healing in many Western cultures. For example, traditional midwifery
practices made women rise out of bed within 24 hours of delivery to help “clear” the
lochia. Throughout the mid-1900s, in contrast, “modern medicine” recommended
keeping women in bed, often for fairly extended periods.
Establishment of Public Health Nursing
Public health nursing as a holistic approach to health care developed in the late
nineteenth and early twentieth centuries. Public and community health nursing
evolved from home nursing practice, community organizations, and political
interventions on behalf of aggregates.
Twentieth Century
In 1902, Wald persuaded Dr. Ernest J. Lederle, Commissioner of Health in New
York City, to try a school nursing experiment. Henry Street lent a public health nurse
named Linda Rogers to the New York City Health Department to work in a school
(Dock and Stewart, 1925). The experiment was successful, and schools adopted
nursing on a widespread basis. School nurses performed physical assessments,
treated minor infections, and taught health to pupils and parents. In 1909, Wald
mentioned the efficacy of home nursing to one of the officials of the Metropolitan
Life Insurance Company. The company decided to provide home nursing to its
industrial policyholders, and soon the United States and Canada used the program
successfully. The growing demand for public health nursing was hard to satisfy. In
1910, the Department of Nursing and Health formed at the Teachers College of
Columbia University in New York City. A course in visiting nursing placed nurses
at the Henry Street settlement for fieldwork. In 1912, the newly formed National
Organization for Public Health Nursing elected Lillian Wald its first president. This
organization was open to public health nurses and to those interested in public
health nursing. In 1913, the Los Angeles Department of Health formed the first
Bureau of Public Health Nursing (Rosen, 1993). That same year, the Public Health
Service appointed its first public health nurse. At first, many public health nursing
programs used nurses in specialized areas such as school nursing, TB nursing,
maternal-child health nursing, and communicable disease nursing. In later years,
more generalized programs have become acceptable. Efforts to contain health care
costs include reducing the number of hospital days. With the advent of shortened
hospital stays, private home health agencies provide home-based illness care
across the United States. The second half of the century saw a shift in emphasis to
cost containment and the provision of health care services through managed care.
Traditional models of public health nursing and visiting nursing from home health
agencies became increasingly common over the next several decades, but waned
toward the end of the century owing to changes in health care financing.g. Twenty-First Century
New Causes of Mortality
Since the middle of the twentieth century, the focus of disease in Western societies
has changed from mostly infectious diseases to chronic diseases. Increased food
production and better nutrition during the nineteenth and early twentieth centuries
contributed to the decline in infectious disease–related deaths. Other factors were
better sanitation through water purification, sewage disposal, improved food handling,
and milk pasteurization. According to McKeown (2001) and Schneider (2011), the
components of “modern” medicine, such as antibiotics and immunizations, had little
effect on health until well into the twentieth century. Indeed, widespread vaccination
programs began in the late 1950s, and antibiotics came into use after 1945. The
advent of chronic disease in Western populations puts selected aggregates at risk,
and those aggregates need health education, screening, and programs to ensure
occupational and environmental safety. Too often modern medicine focuses on the
single cause of disease (i.e., germ theory) and treating the acutely ill. Therefore
health providers have treated the chronically ill with an acute care approach even
though preventive care, health promotion, and restorative care are necessary and
would likely be more effective in combating escalating rates of chronic disease.
This expanded approach may develop under new systems of cost containment.
Hygeia versus Panacea
The Grecian Hygeia (i.e., healthful living) versus Panacea (i.e., cure) dichotomy still
exists today. Although the change in the nature of health “problems” is certain, the
roles of individual and collective activities in the prevention of illness and premature
death are slow to evolve.
Formerly, Health care has been for those living near enough to a hospital or a
doctor in times of need and for those who could spend money for medicines and
treatment. The great majority of people stayed in the village when sick and even
today many suffer and die without proper help.
The shorter length of stay in acute care facilities, as well as the increase in ambulatory
surgery and outpatient clinics, has resulted in more acute and chronically ill people
residing in the community who need professional nursing care. Fortunately, these
people can have their care needs met cost effectively outside of expensive acute
care settings. As a result, demand has increased for nurses in ambulatory clinics,
home care, care management, and case management.
Public and community health, ambulatory care, and other non-institutional settingshave historically had the largest increases in Registered Nurse employment.
Self-assessment 5.1.2
1) In which centuries was public health nursing developed as a holistic
approach to health care?
2) Who is the woman credited with establishing modern nursing?
3) Discuss the prerecorded historic times of community health nursing
5.1.3. Objectives, purposes and principles of community healthnursing
Learning activity 5.1.3
1) Use the books of community health nursing and internet resources and
found out the purposes and principles of community health nursing
a. Objectives of community health nursing
The goals and objectives of Community Health Nursing are the following:
• To assess the need and priorities of vulnerable group like pregnant mother,
children and old age persons;
• To provide health care services at every level of community including health
education, immunization,
• To make community diagnosis;
• To evaluate the health programs and make further plans;
• To prevent disabilities and providing rehabilitation services;
• To provide referral services at various health care levels;
• To increase life expectancy;
• To enhance the standard of nursing profession through:
– Conducting nursing research.
– Provide quality assurance in community health nursing.
– Performing the role of nurse epidemiologist.
• To improve the ability of the community to deal with their own health problems
• To strengthen the community resources
• To prevent and control communicable and non-communicable diseases
• To provide specialized services
b. Purpose of community health nursing
Purposes / Aims of Community Health Nursing are:
• To promote health and efficiency;
• Prevention and control diseases and disabilities;
• Need based health care to prolong life.
c. Principles of Community Health Nursing
The following are the principles of community health nursing:
• Health services should be based on the needs of individuals and the
community.
• Health services should be suitable to the budget; workers and the resources.
• Family should be recognized as a unit and the health services should be
provided to its members.
• Health services should be equally avail¬able to all without any discrimination
of age, sex, caste religion, political leaning and social or economic level etc.
• Health education is an important part of community health nursing. It should
be preplanned, suitable to conditions, scientifically true and effective.
• Community health nursing should be provided continuously, without any
interruption.
• Preparation and maintenance of records and reports is very important in
com¬munity health nursing.
• Community health nurses and other health workers should be guided and
supervised by highly educated and skilled professionals.
• Community health nurse should be responsible for:
– Responsible for professional development.
– Should continuously receive in-service training and continuing education.
– Should follow professional ethics and standards in her work and behaviour.
– Should have job satisfaction.
• Must have effective team spirit while working in the community.• Timely evaluation is must for community services.
Self-assessment 5.1.3
1) Identify the objectives of community health nursing
2) What are the principles of community health nursing?5.1.4. Characteristics of community health nursing
Learning activity 5.1.4
In the last holiday Mrs. K. and her parents went to visit their grandparents in
Masimbi village. One day two community health nurses came to visit this village
and took sufficient time meeting pregnant women and lactating mothers. They
discussed together about pregnant women health and some issues during
pregnant and lactation. The next day they hold a meeting talking about children
nutrition. These events reminded her the day nurses came to their school and
teach about malaria prevention.
Mrs. K admired the way those nurses use for helping people. Returning to their
home town, she sat down with her mother and asked many questions in order to
know more about the career of those nurses who work with people in their own
villages.
Some of those questions are the followings:
1) Do community health nurses are the same as those who work in hospitals
and clinics?
2) How do you characterize community health nursing?
3) After reading the related text in community health nursing textbooks, helpthe mother to offer responses to Mrs. K
Eight characteristics of community health nursing are particularly most important to
the practice of this specialty:
a. The client or “unit of care” is the population.
Community health nursing is population-focused, meaning that it is concerned for
the health status of population groups and their environment. A population may
consist of the elderly, scattered group with common characteristics, such as people
at high risk of developing heart disease, battered women living throughout a county.
It may include all people living in a neighborhood, district, census tract, city, state,
or province. Community health nursing’s specialty practice serves populations and
aggregates of people.
b. The primary obligation is to achieve the greatest good for the greatest
number of people or the population as a whole.
Community health nurses are concerned about several aggregates at the same
time, service will, of necessity, be provided to multiple and overlapping groups; theethical theory of utilitarianism promotes the greatest good for the greatest number.
c. The processes used by public health nurses include working with the
client(s) as an equal partner.
In order to achieve the goal of community health which is” “to increase quality
and years of healthy life and eliminate health disparities”, clients’ health status and
health behavior will change if people accept and apply the proposals (developed in
collaboration with clients) presented by the community health nurse.
d. Primary prevention is the priority in selecting appropriate activities.
In community health nursing, the promotion of health and prevention of illness are
a first-order priority. It focuses also on positive health, or wellness. These include
services to mothers and infants, prevention of environmental pollution, school health
programs, senior citizens’ fitness classes, and “workers’ right-to-know” legislation
that warns against hazards in the workplace. Less emphasis is placed on curative
care.
e. Selecting strategies that create healthy environmental, social, and
economic conditions in which populations may thrive is the focus.
The wish of community health nursing is to create healthy environments for our
clients, so that they can thrive and not simply survive.
f. There is an obligation to actively reach out to all who might benefit from
a specific activity or service.
We know that some clients are more prone to develop disability or disease because
of their vulnerable status (e.g., poverty, no access to health care, homeless).
Outreach efforts are needed to promote the health of these clients and to prevent
disease. In acute care and primary health care settings, like emergency rooms or
physician offices, clients come to you for service. However, in community health,
nurses must “focus on the whole population and not just those who present for
services” and seek out clients wherever they may be.
g. Optimal use of available resources to assure the best overall improvement
in the health of the population is a key element of the practice.
It is vital that community health nurses ground their practice in research, and use
that information to educate policy makers, and population about best practices.
They have to put more effort on the utilization of the available personnel and
resources effectively and prudently in order to assure the best overall improvement
in the health of the population for a long time.
h. Collaboration with a variety of other professions, organizations, and
entities is the most effective way to promote and protect the health of
people.
Community health nurses must work in cooperation with other team members,
coordinating services and addressing the needs of population groups. This inter
professional collaboration among health care workers, other professionals and
organizations, and clients is essential for establishing effective services and
programs. Individualized efforts and specialized programs, when planned inisolation, can lead to fragmentation and gaps in health services
Self-assessment 5.1.4
1) Explain eight characteristics of community health nursing
5.1.5. Community Health in Rwanda
Learning activity 5.1.5
Using internet and other resources like National Community Health Strategic
Plan, Community Health policies; read about community health in Rwanda and
respond to the following questions:
1) Discuss the importance of community health program in the community
and its implementation.
2) How Community health workers (CHWs) are selected, their responsibilities
and reporting?3) Discuss about CHWs supervision
In Rwanda, community health services started in 1995 as Rwanda Community
Health Worker (CHW) Program, aiming at increasing uptake of essential maternal
and child clinical services through education of pregnant women, promotion of
healthy behaviors, and follow-up and linkages to health services.
When the Ministry of Health (MOH) endorsed the program in 1995, there were
approximately 12,000 CHWs. By 2005, the program had grown to over 45,000
CHWs. From 2005, after the decentralization policy had been implemented
nationally, the MOH increased efforts to train and provide supplies to CHWs to
deliver maternal and child health (MCH) services. Between 2008 and 2011, Rwanda
introduced integrated community case management (ICCM) of childhood illness (for
childhood pneumonia, diarrhea, and malaria). In 2010, the Government of Rwanda
introduced Family Planning as a component of the national community health
policy. The program has since grown to include an integrated service package that
includes malnutrition screening, treatment of tuberculosis (TB) patients with directly
observed therapy (DOT), prevention of non-communicable diseases (NCDs),community-based provision of contraceptives, and promotion of healthy behaviors
and practices including hygiene, sanitation, and family gardens.
Program implementation
In each village of approximately 100–150 households, there is one CHW in
charge of maternal health, called an ASM (Agent de Sante Maternelle) and two
multidisciplinary CHWs called Binômes(one man and one woman working as a
pair) providing basic care and integrated community case management (ICCM) of
childhood illness. CHWs are full-time, voluntary workers who play a very key role
in extending services to Rwanda’s village communities. The CHWs are supervised
most directly by the cell coordinator and the in-charge of community services at
the catchment-area of the health center. CHWs now use Rapid SMS to submit
reports and communicate alerts to the district level and to hospitals or health
centers regarding any maternal or infant deaths, referrals, newly identified pregnant
women, and newborns in the community.
In 2010, the Government of Rwanda introduced FP as a component of the national
community health policy, and CHWs were trained not only to counsel but also to
provide contraceptive methods including pills, injectables, cycle beads (for use with
natural FP), and condoms. This program was first piloted in three districts and later
scaled nationwide.
Responsibilities of Community Health Workers
Three CHWs, with clearly defined roles and responsibilities, operate in each village
of approximately 100–150 households. ASMs have been trained to identify pregnant
women, make regular follow-ups during and after pregnancy, and encourage
deliveries in health facilities where skilled health workers are available. In addition
to following up pregnant women and their newborns, the ASM also screens
children for malnutrition, provides contraceptives (pills, injectables, cycle
beads, and condoms), promotes prevention of Non-Communicable Diseases
(NCDs) through healthier lifestyles, preventive and behavior change activities
and carries out household visits.
Between 2008 and 2011, Rwanda introduced ICCM of childhood illness (for
childhood pneumonia, diarrhea, and malaria) nationwide. Binômes were trained
and equipped to: (a) provide ICCM (assessment, classification, and treatment
or referral of diarrhea, pneumonia, malaria, and malnutrition in children younger
than 5 years of age; including treatment with antibiotics, zinc, and antimalarials) (b)
malnutrition screening (c) community-based provision of contraceptives, (d) DOT
for TB, (e) prevention of NCDs, (f) preventive and behavior change activities and
(g) household visits. They are in charge to detect cases of acute illness in need ofreferral, and to submit monthly reports
Supervision
There are two community health workers, called “cell coordinators”, who are heads
of all CHWs at the cell level, and whose aim is to follow up, and thereby strengthen,
CHWs’ activities.
The specific roles and responsibilities of the cell coordinator at the cell level include
the following:
1) Visiting of community health workers in order to monitor their activities on a
monthly basis.
2) Follow up and verify if CHW has patient registers, and if they are correctly
filled out and well-kept.
3) Monitor if drugs are distributed correctly and if these drugs are not expired
and well-kept
4) Compilation of reports of drugs that have been used by CHW in that cell and
requisition of drugs at health centers
5) Supervision of the binome and a household that was recently attended to
by a CHW
6) Check if CHW does post-visit for children she/he recently treated
7) Supervise CHW on how well she/he is able to sensitize the community on
family planning usage
8) Verification of reports brought for compilation if they have been sent by
telephone
(m’Ubuzima)
The cell coordinator is aided by an assistant cell coordinator, who is responsible for:
• Monitor if the ASM has registers and these registers are filled correctly
• Follow up and see if the ASM refers pregnant women for ANC visits at the
health center (HC)
• Follow up and verify if the ASM has sent RapidSMS reports for pregnant
mothers confirmed by health provider
• Verify if the ASM has Misoprostol drugs and the drugs are not expired
Place of CHWs in the health system
Health services are provided at different levels of the health care system – in
communities, at health posts (HP), health centers (HC), district hospitals (DH),
and referral hospitals – and by different types of providers – public, confessional,
private-for-profit and NGO. At all levels, the sector is composed of administrative
structures and implementing agencies. The area of CHW’s activities is the village.At the lowest level, those in charge of community health activities at the health
centers administratively supervise CHWs.
At the sector level, there are Health Center Committees that provide oversight on
the work from various units in the health center, its outreach, supervision activities,
and general financial controls.
At the district level, one finds district hospitals (DH), district pharmacies, community
based health insurance (CBHI) committees, and HIV/AIDS committees.
Financial support to CHWs
The CHWs receive financial compensation through performance based financing,
or PBF, for delivering a certain number of health services. Thirty percent of the
total PBF funds are shared among CHW members while 70% is deposited in the
collective funds of CHW cooperatives.
Selection, training, and retention of Community Health Workers
CHWs come from the villages in which they live. They must be able to read and write
and be between the ages of 20 and 50 years. They also must be willing to volunteer
and be considered by their peers to be honest, reliable, and trustworthy. They are
elected by village members in a process that involves gathering the volunteers
and villagers on the last Saturday of the month (Umuganda, or community service
day) and voting “with their feet” in a literal sense. The process has been described
(in conversation) as one that involves community members lining up in front of the
person they support. The individual with the most support is recruited.
Within each of the villages (Umudugudu), Binômes are trained in community-based
integrated management of childhood illnesses (IMCI) by preparing them to be first
responders to a number of common childhood illnesses, including pneumonia,
diarrhea, and malaria. The CHWs are also trained on when and how to refer
severe cases to the health facility. IMCI refresher training is provided through a
supportive supervision model, where the supervisor conducts training to strengthen
the CHW’s knowledge and skills in providing quality case management services in
their communities.
Another example of program-specific training is the ten-day training for community
based provision of FP services.
In 2009, the MOH introduced Community Performance-Based Funding (CPBF) as
a way to motivate CHWs. Community Health worker Cooperatives are organized
groups of CHWs that receive and share funds from the MOH based on the
achievement of specific targets established by the MOH. Each health center in
Rwanda supervises the CHWs that make up one CHW cooperative. By linking
incentives to performance, the MOH hoped to improve quality and utilization of
health services.Impact of Community Heath Program and challenges
The most important achievements in the health sector include an increase in facility
based deliveries, the introduction of maternal and child death audits at all health
facilities, an increase in vaccination coverage. CHW follow-up of all pregnant
women, and provision of community-based FP services. CHWs are currently testing
all suspected cases of malaria with a rapid diagnostic test and providing treatment
when indicated to children younger than 5 years of age who have malaria within 24
hours.
The challenges faced by the Rwanda CHW program are similar to challenges
faced by CHW programs in other countries. These include (1) the financial and
administrative difficulties in supporting and continuing to build the capacity of
CHWs as they increase in number and as the scope of their work expands; (2) the
challenge of supervising and effectively equipping CHWs to perform their duties;
and (3) low community participation in the health sector and the strong influence of
traditional beliefs and traditional medicines.
As the number of CHWs has risen rapidly in Rwanda and as their tasks have
increased, the Government of Rwanda faces a constant battle to increase the
capacity of CHWs and to provide them with the equipment and supplies they need.
Refresher trainings are too few and provision of essential equipment is delayed due
to insufficient financial resources. Field supervision of CHWs and the transfer of skills
and knowledge to the communities to foster ownership and enhance sustainability
is a continuing challenge. Each CHW is supposed to be supervised by either the
In-Charge of Community Health or the cell coordinator on monthly basis. However,recent findings show that supervisory visits occur only quarterly, if that.
Self-assessment 5.1.5
1) Discuss the responsibilities of an ASM
2) Explain the main activities of Binômes
3) How are CHWs selected?
4) Identify the coverage area of CHW activities.
5) Discuss the issues encountered by CH program in our country5.1.6. Characteristics of a community
Learning activity 5.1.6
Observe the images below and answer to the questions: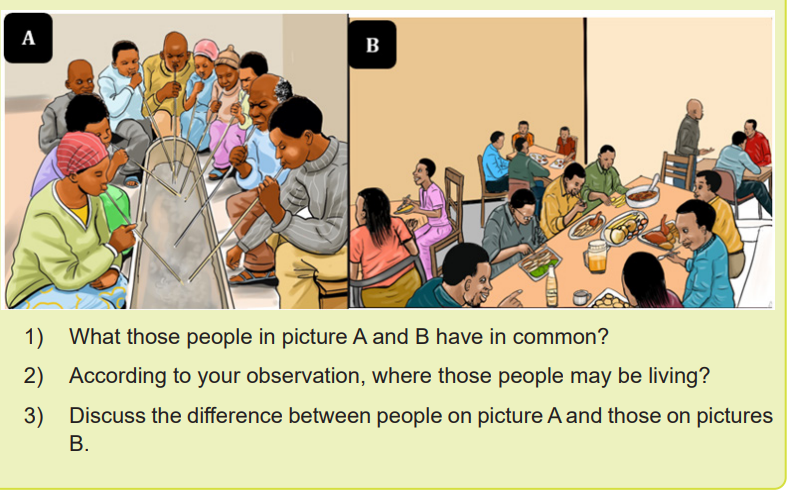
Human beings are social creatures. All of us, with rare exception, live out our lives
in the company of other people. Communities are an essential and permanent
feature of the human experience. The communities in which we live and work have
a profound influence on our collective health and well-being.
The community is a territorial group with shares a common soil as well as shared
way of life. People living in the same locality come to have a distinctive community
life. The community is more than the locality it occupies. It is also sentiment. They
share common memories and traditions, customs and institutions. Today none of
us belong to one inclusive community. Under modern conditions attachment to local
community is decreasing.
Meaning of community can be better understood if we analyze its characteristics
or elements. These characteristics decide whether a group is a community or not.
However, generally, community has the following 13 most important characteristicsor elements:
1) A group of people
A group of people is the most fundamental or essential characteristic or element
of community. This group may be small or large but community always refers to a
group of people. Because without a group of people we can’t think of a community,
when a group of people live together and share a common life and binded by a
strong sense of community consciousness at that moment a community is formed.
Hence a group of people is the first pre-requisites of community.
2) A definite locality
It is the next important characteristic of a community. Community is a territorial
group. A group of people alone can’t form a community. A group of people forms
a community only when they reside in a definite territory. The territory need not be
fixed forever. A group of people like nomadic people may change their habitations.
But majority community are settled and a strong bond of unity and solidarity is
derived from their living in a definite locality.
3) Community Sentiment
It is another important characteristic or element of community. Without community
sentiment a community can’t be formed only with a group of people and a definite
locality. Community sentiment refers to a strong sense of awe feeling among the
members or a feeling of belonging together. It refers to a sentiment of common
living that exists among the members of a locality. Because of common living
within an area for a long time a sentiment of common living is created among the
members of that area. With this the members emotionally identify themselves. This
emotional identification of the members distinguishes them from the members of
other community.
4) Naturality
Communities are naturally organized. It is neither a product of human will nor
created by an act of government. It grows spontaneously. Individuals became the
member by birth.
5) Permanence
Community is always a permanent group. It refers to a permanent living of individuals
within a definite territory. It is not temporary like that of a crowd or association.
6) Similarity
The members of a community are similar in a number of ways. As they live within
a definite locality they lead a common life and share some common ends. Among
the members similarity in language, culture, customs, and traditions and in many
other things is observed. Similarities in these respects are responsible for thedevelopment of community sentiment.
7) Wider Ends:
A community has wider ends. Members of a community associate not for the
fulfilment of a particular end but for a variety of ends.
These are natural for a community.
8) Total organized social life:
A community is marked by total organized social life. It means a community includes
all aspects of social life. Hence a community is a society in miniature.
9) A Particular Name:
Every community has a particular name by which it is known to the world. Members
of a community are also identified by that name. For example, people living in
sector of Nkombo is known as “Abanyenkombo”.
10) No Legal Status:
A community has no legal status because it is not a legal person. It has no rights
and duties in the eyes of law. It is not created by the law of the land.
11) Size of Community:
A community is classified on the basis of its size. It may be big or small. Village is an
example of a small community whereas a nation or even the world is an example of
a big community. Both the type of community is essential for human life.
12) Concrete Nature:
A community is concrete in nature. As it refers to a group of people living in a
particular locality we can see its existence. Hence it is concrete.
13) A community exists within society and possesses distinguishable
structure which distinguishes it from others.
Specifically, different types of community exist and they have their particular
characteristics including the ones described below:
a. Characteristics of village/rural Community:
The village people have a sense of unity. The relationship between people is
intimate. They personally know each other; structurally and functionally the village
is a unit.
In the village, people assist each other and thus they have close neighborhood
relations. In the village the joint family system is retained. The agricultural occupation
requires the cooperation of all the family members.
The People in the villages have deep faith in religion and duties. The village peoplelead a simple life. Their behavior is natural and not artificial. They are free from
mental conflicts. They are hard-working; their level of moralities is high. Social
crimes are less.
Ancient village community was a very small group of ten or twenty families. The
feeling of familiarity was so great that if a child wandered off from the home, the
parents had nothing to worry because there are numerous relatives in the village.
They laid a common property. Due to lack of communication and transport the
members of the community were separated due to distance.
In the modern village community, there is a rise of industrialism. Now urban group
began to dominate civilization. Urbanization is increasing and dominant rural. Social
forms are changing rapidly.
Rural people follow the urban forms of life. Kinship bond is broken due to increased
size and mobility of population. Land is no longer cultivated jointly. They continue
to work the land but then try to live in the mode of the city. Rural social forms are
changed due to urbanization.
Rural communities may have their specific major Problems such as:
• Health problems, the most common being: Malnutrition, especially in under
– five-year children; communicable diseases and infection and child deaths
and maternal deaths and clean water accessibility.
• Education problems – the problems of illiteracy, school dropouts, few
teachers, also lack of equipment and insufficient buildings or in need of repair
child labor etc.
• Problems related to transport and communications – lack of good roads,
especially in rainy season, causes problems of supplies, marketing and
taking the sick to hospital, etc. The problem of villages being cut off from other
communities and urban facilities, results in slow progress and development.
• Problems concerning agriculture – the farmer may have problems such as
insufficient water supply, especially in failure of monsoon, electricity cuts, and
repair of pump-sets, tractors etc. Delay in getting supplies of seed, fertilizers,
especially if he has no capital reserves.
• Labor problems – laborers may not be available when needed, or coolly
demands are high. Procurement price given by Government may be too low,
or demand for products is low. Sickness and death of flocks and herds (sheep
and cattle).
• Population and employment problems– Agriculture can no longer provide
enough for the growing population in rural areas. Some rural communities
have taken up handloom weaving or other small industries, but these are
not without many problems. Young men leave the village for urban areasin search of jobs. Sometimes whole groups of families migrate to a distant
place to work for a contractor (building, mining and other project). They get
advances from the contractor to buy food, and soon may become ‘bonded
laborers’ and never get bat to their own village.
b. Characteristics of urban Community:
Home decreasing is a disturbing feature of city community. The home problem in a
big city is very acute. The middle class have insufficient accommodation. The child
doesn’t get any play space. Energy and speed are the traits of a city. The people
work at a speed, day and night which stimulates other to work. People indulge in too
many activities. Cities are consumers of population. Facilities for preserving health
such as hospitals and medical specialist are many and excellent. City has more
heterogeneous than the village. It is most favorable propagation ground of new
biological and cultural hybrids. The personal traits, the occupations, the cultural and
the ideas of the members of the urban community vary widely.
Class extremes characterize urban community. In a city, the people rolling in
luxury and living, in grand mansion as well as people live in street. The best forms
of ethical behavior and the worst racketeering are both to be bound in cities.
Superior creativeness and chronic unemployment are similar. The city is the home
of opposites. In some cities, residents may treat the strangers they meet as not
human beings. They meet with speak without knowing each other’s name. A citizen
may live for several years in a city and may not know the names of one-third of the
people who live in the same city area.
Life is quite different in towns and cities than in the village. Traditions, customs and
modes do not have much influence over those living in urban areas. Family life is
less disciplined, and there is no community support. There is much more mixing
among people of very different backgrounds. This brings about changes in habits
and attitudes. Family conflicts are common. For the individuals, and for families
coming to live in the urban area, conscious efforts need to be made to form good
friendships and to live in harmony with others. There are many opportunities for
joining social groups for various activities. People need to take up the challenge
for forming a new community even in the city, for mutual help and action to solve
problems.
The main urban problems may be listed as follows:
a) Growth of slums
b) Lack of employment, leading to poverty, under – nutrition, disease, and
anti-social activities. Failure of people to adjust, causing mental illness or
delinquency.
c) Crime and delinquency, begging and prostitution.
d) Overcrowding in dwellings, buses and streets.
e) Failure in administration (e.g. public services such as refuse collection and
disposal) to cope with the rapid growth of the population.
f) Road accidents.
g) Health problems due to overcrowding and to stress of urban living.
h) Political and industrial unrest and conflicts.
c. Characteristics of common-interest Community
A community also can be identified by a common interest or goal. A collection
of people, even if they are widely scattered geographically, can have an interest
or goal that binds the members together. This is called a common-interest
community. The members of a church in a large urban area, the members of a
national professional organization, and women who have had mastectomies are
all common-interest communities. Sometimes, within a certain geographic area, a
group of people develop a sense of community by promoting their common interest.
Disabled individuals scattered throughout a large city may emerge as a community
through a common interest in promoting adherence to federal guidelines for
wheelchair access, parking spaces, toilet facilities, elevators, or other services for
the disabled.
The residents of an industrial community may develop a common interest in air or
water pollution issues, whereas others who work but do not live in the area may not
share that interest. Communities form to protect the rights of children, stop violence
against women, clean up the environment, promote the arts, preserve historical
sites, protect endangered species, develop a smoke-free environment, or provide
support after a crisis. The kinds of shared interests that lead to the formation of
communities vary widely.
Common-interest communities whose focus is a health-related issue can join with
community health agencies to promote their agendas. A group’s single-minded
commitment is a mobilizing force for action. Many successful prevention and health
promotion efforts, including improved services and increased community awareness
of specific problems, have resulted from the work of common-interest communities.
d. Community of Solution
A type of community encountered frequently in community health practice is a group
of people who come together to solve a problem that affects all of them. The shape
of this community varies with the nature of the problem, the size of the geographic
area affected, and the number of resources needed to address the problem. Such
a community has been called a community of solution. Example: club against HIV/AIDS
Self-assessment 5.1.6
1) Identify 13 most important characteristics of a community in general2) Discuss the characteristics of urban people
5.1.7. Characteristics and functions of a healthy community
Learning activity 5.1.7
With use of community health text books taken from library or internet, ready,
understand, discuss and write brief notes on: characteristics of healthy
community, roles and responsibilities of a community health nurse; and corefunctions of community health nursing
This sub-unit discusses the following four points: characteristics of healthy
community, roles and responsibilities of a community health nurse, qualities of a
community health nurse and functions of community health nursing.
a. Characteristics of a Healthy Community
A healthy community is one in which all residents have access to a quality education,
safe and healthy homes, adequate employment, transportation, physical activity,
and nutrition, in addition to quality health care. Unhealthy communities lead to
chronic disease, such as cancers, diabetes, and heart disease.
Just as health for an individual is relative and will change, all communities exist in
a relative state of health. A community’s health can be viewed within the context
of health being more than just the absence of disease, and including things that
promote the maintenance of a high quality of life and productivity.
Just as there are characteristics of healthy individuals, so are there characteristics
of healthy communities. These include the following:
• The healthy community ensures that community resources are available to
all members and groups within the community. It ensures there is access to
appropriate health care services that focus on both treatment and prevention
for all members of the community; a clean and safe physical environment;
and roads, schools, playgrounds, and other services to meet the needs of the
people in that community
• Emergency preparedness: a healthy community has a well-organized base of
community resources available to meet the needs and to intervene in a crisisor natural disaster
problems and collaborates and coordinates a response among members and
groups to meet their identified needs.
• Communication through open channels. It ensures that communication
remains open and information flows among all members and groups in every
direction within the community.
• Resolution of disputes through legitimate mechanisms
• The healthy community ensures there is participation by citizens in
decision making and subgroups participate in community affairs. It provides
opportunities for and encourages participation of individuals and groups in
decision making related to issues affecting the community.
• A high degree of wellness among its citizens: the healthy community focuses
on promoting a high level of wellness and health among all members and
populations within the community.
• A healthy community has an awareness of its members, populations, and
subgroups as being part of the community.
• The historical and cultural heritage is promoted and celebrated.
• There is a diverse and innovative economy.
• There is a sustainable use of available resources for all.
b. Roles and Responsibilities of Community Health Nurse:
Some key roles and responsibilities of community health nurse are discussed below:
A community health nurse performs various functions while she works in any
defined community health setting. In general, the community health nurse performs
the following functions according to her roles:
a) Clinician Role or Direct care provider
She provides a continuous and comprehensive care to the family, group of people
and community at large. She emphasizes more on promotive and preventive health
care. The community health nurse approaches the family and persuades them to
implement promotive and preventive measures. Care during illness is beneficial
gaining acceptance, trust and confidence.
She also provides care during illness for which usually the family members come
forward to seek help. As care is given, the nurse educates and helps the family
members to develop their abilities and overcome their barriers so that they can take
care of their health and nursing needs, promote their health and prevent illness.
The care is provided at home, clinic, school, work place etc.
b) Health educator:
The community health nurse educates the individual, family, groups of people and
the community at large. Health education thus given focuses on promoting health,
preventing illness and aspects related to care during illness and rehabilitation &
disability prevention. The nurse conducts planned health education sessions for
organized community groups e.g., school children, antenatal mothers, eligible
couples, elderly etc. Health education for the family is planned and implemented
as part of the family care plan. The community nurse assesses the knowledge,
attitudes, values, beliefs, behaviours, practices, stage of change, and skills of the
community people and provides health education according to knowledge level.
The community health nurses are involved in giving incidental/casual/spontaneous
health education according to the situation. (Washing of hands before a child eats).
c) Counselor:
The community health nurse helps individual, families and the community at large
to recognize and understand their problems to be solved, find solutions with-in
resources and implement feasible and acceptable solutions.
d) Resource person:
The community health nurse explores community resources in terms of money,
manpower, material, agencies etc. She makes use of these resources in helping
individual, family groups and community to meet their health and nursing needs.
e) Care manager/Managerial Role:
The community health nurse implements the care which is planned for the family
and community. She directly provides the care with the active participation of family
and community members. She makes use of family and community resources.
She guides the family and community and refers when required. She maintains
a record of the care given to families and the community. The community health
nurse evaluates the effectiveness of care given in terms of change in health status,
health behavior, reduction in illness, improvement in clinic attendance-immunization
& rate of utilization of the community health services.
As a manager the nurse exercises administrative direction towards the
accomplishment of specified goals by assessing clients’ needs, planning and
organizing to meet those needs, directing and controlling and evaluating the
progress to assure that goal are met.
f) Planner:
The community health nurse while giving comprehensive care to family and
community, she/he makes a plan on the basis of identified health problems
and health & nursing needs. She/he plans with other team members to provide
appropriate care.g) Research Role:
In the researcher role community health nurses engage in systematic investigation
of any untoward change in health behavior and health status of the community,
people, their surroundings, and unusual occurrence of disease. She/he carries out
collection, and analysis of data to solve problems and enhance community health
nursing practice. Based on the research results, a community nurse improve their
service quality and improve their health accordingly, for examples by providing
information, health education to people to improve their behavior and health status,
working with the family and providing direct care during illness, notification to health
authority about communicable disease.
h) Advisor:
The community health gives some suggestions on practical situation which requires
immediate actions and where there is little scope of health education. For example,
in case of a client with diabetes mellitus, the community health nurse advices with
concern on the foods to be included and avoided according to the socio –economic
condition of the individual & family.
i) Advocate Role:
The issue of clients’ rights is important in health care today. Every patient or client
has the right to receive just equal and humane treatment. A community health nurse
is an advocate of patient’s rights about their care. They encourage the individuals
to take the right food for maintaining health, the right drugs for the treatment, and
the right services at the right place where ever needed. They provide sufficient
information to make necessary health care decisions, promote community
awareness of significant health problems.
j) Collaborator Role:
Community health nurses seldom practice in isolation. They must work with
many people including clients, other nurses, physicians, social workers, and
community leaders, therapists, nutritionists, occupational therapists, psychologists,
epidemiologists, biostatisticians, legislators, etc. as a member of the health team.
k) Leader Role:
Community health nurses are becoming increasingly active in the leader role. As a
leader, the nurse instructs influences or persuades others to effect change that will
positively affect people’s health. The leadership role’s primary function is to use a
change of health policy based on community people’s health; thus, the community
health nurse becomes an agent of change.
c. Qualities of a community health nurse
A best community health nurse is characterized by the following qualities:
1. Interest in community health nursing.
2. Good interpersonal relationship skills.
3. Interested in people.
4. Emotional stability.
5. Good communicability.
6. Guiding & helping nature.
7. Sensitive observation.
8. Good listener.
9. A friendly disposition.
10. Initiative/creativity
11. Resource fullness.
12. Endurance & patience.
d. Functions of community health nursing
The four core functions of community health nursing practices are displayed below:
1. Identification of community culture and resources that lead as a key factor in
the community health care delivery system.
2. Evaluate community health conditions, health risks, and problems to identify
the health-care demands of the people.
3. Plan and implementation of comprehensive community health interventions,
care, services, and programs.
4. Develop health policy at the local community level to drive policies/
agreements at the state and national levels for collaborative endeavors andactions.
Self-assessment 5.1.7
1) Give the four core functions of community health nursing practice
2) Mention any 4 characteristics of a healthy community
3) Explain any 2 roles and responsibilities of a community health nurse.
5.2. Determinants of health and the factors affectingcommunity health
Learning activity 5.2
Get community health nursing books and/or internet resources and provide the
answers to the following questions:
1) Explain any 2 determinants of health
2) Write a short description on each of the following factors affecting the
community health nursing: Physical factors, Social/Cultural factors,Community organization, and Individual behavior
5.2.1. Determinants of health
Determinants of Health and Disease: The health status of a community is associated
with a number of factors, such as health care access, economic conditions,
social and environmental issues, and cultural practices, and it is essential for the
community health nurse to understand the determinants of health and recognize
the interaction of the factors that lead to disease, death, and disability. Indeed,
individual biology and behaviors influence health through their interaction with each
other and with the individual’s social and physical environments. Thus, policies and
interventions can improve health by targeting detrimental or harmful factors related
to individuals and their environment. Some causes of death resulting from individual
behavior are: tobacco, poor diet and physical inactivity, alcohol consumption and
its association with accidents, suicides, homicides, and cirrhosis and chronic liver
disease. Other leading causes of death are microbial agents, toxic agents, motor
vehicle crashes, firearms, sexual behaviors and illicit use of drugs.
Although all of these causes of mortality are related to individual lifestyle choices,
they can also be strongly influenced by population-focused policy efforts and
education. For example, the prevalence of smoking may be fallen dramatically,
largely because of legal efforts (e.g., laws prohibiting sale of tobacco to minors
and much higher taxes), organizational policy (e.g., smoke-free workplaces), and
education. Likewise, concerns about the widespread increase in incidence of
overweight and obesity may lead to population-based measures to address the
issue (e.g., removal of soft drink, regulations prohibiting the use of certain types of
fats in processed foods).
Indeed, at the population level, better health can be attributed to higher standards
of living, good nutrition, a healthier environment, and having fewer children.
Furthermore, public health efforts, such as immunization and clean air and water, and
184 Fundamental Of Nursing - Senior 6 - Student's Book
medical care, including management of acute episodic illnesses (e.g., pneumonia,
tuberculosis) and chronic disease (e.g., cancer, heart disease, diabetes mellitus),
may also contribute significantly to the increase in life expectancy. Community
and public health nurses should understand these concepts and appreciate that
health and illness are influenced by a web of factors, some that can be changed
(e.g., individual behaviors such as tobacco use, diet, physical activity) and some
that cannot (e.g., genetics, age, gender). Other factors (e.g., physical and social
environment) may require changes that will need to be accomplished from a policy
perspective. Community health nurses must work with policy makers and community
leaders to identify patterns of disease and death and to advocate for activities and
policies that promote health at the individual, family, and population levels.
5.2.2. The factors affecting community health
The factors affecting community health can be grouped into: Physical factors,
Social/Cultural factors, Community organization, and Individual behavior
a. Physical factors
• Industrial development: Communities that are industrially developed are more
likely to be affected by numerous diseases due to the toxic waste products
from the industries that are released into water bodies and the atmosphere
and due to congestion of settlement leading to slum development hence
contagious diseases compared to areas that are not industrially developed.
Water contamination from industrial discharge and air pollution may be ones
of the consequences of industrial development.
• Community size: A densely populated or over populated community can
easily be attacked by communicable diseases
• Geographical location: Some communities are more prone to diseases due
to the geographical location. For example, some communities located in
swampy areas are more prone to diseases, especially during heavy rains
these communities are affected by floods which can lead to manipulation of
organisms causing disease. If the water is stagnant, there is risk of spread of
organisms which cause diseases such as malaria and diarrhea disease.
• Environment: A clean environment is very vital to the proper health of a
community which minimizes the occurrence and transmission of diseases,
unlike a dirty environment which easily leads to outbreak of diseases.
b. Social/cultural factors
• Traditions Beliefs: Beliefs or traditions such as female genital mutilation
(FGM) possessed by communities greatly affect the health of its people.
• Economy: A community that is economically well off has low chances of
suffering from disease breakouts because they have proper health care andwater drainage systems unlike a poor community.
• Government: since the government involves planning, implementing and
provision of community services such as water supply, medical supplies and
other needs which can directly affect the community health
• Educational factors: poor education or illiteracy affects the health of a community
when people don’t have education on how they can prevent themselves from
diseases. For example, health education on the use of mosquito treated nets
to prevent malaria, health education on the environmental hygiene so as to
prevent diseases such as cholera and trachoma.
c. Community organization
This is about the ways in which communities organize their resources such as
taxes which can be very helpful in control of diseases and supply of sufficient and
efficient medical care, even in times of crisis. Unlike communities without proper
accountability of their taxes which can partly be allocated to the health sector, may
suffer from lack of adequate resources to prevent diseases, protect and promote
the health of its citizens.
d. Individual behavior
Community health is greatly influenced by individuals, their personal health, habits,
etc.
In order to achieve a healthy community, it requires a team work for example in the
following in activities:
• Proper disposal of waste products from individuals’ compound,
• Clearing all stagnant water in the compound to prevent harboring of
mosquitoes,
• Active smokers to quit smoking to avoid passive smokers thus preventing lung
cancer, Abstinence from sexual activities and for sexually active individuals to
use protection to prevent the spread of HIV/AIDs and STDs etc.
Thus proper individual healthy living can greatly promote a healthy communitySelf-assessment 5.2
1) Describe the 4 factors that affect the health of the community
2) Explain the issues related to biology and individual behavior asdeterminants of health
5.3. Community health needs assessment
Learning activity 5.3
Using internet and Community Health Nursing Textbooks; read about community
health needs assessment and respond to the following questions
1) What is the meaning of community health assessment?
2) Discuss types of community assessment.
3) Describe the methods of community assessment
4) Identify the sources of data in community assessmentThe primary concern of community health nurses is to improve the health of the
community. This process involves using demographic and epidemiological methods
to assess the community’s health and diagnose its health needs.
After considering the importance of community partnerships and coalitions, the
community health nurse is ready to determine the community’s needs. Assessment
is the key initial step of the nursing process. Assessment for nurses means collecting
and evaluating information about a community’s health status to discover existing
or potential needs and assets as a basis for planning future action.
Assessment involves two major activities. The first is collection of pertinent data,
and the second is analysis and interpretation of data. These actions overlap
and are repeated constantly throughout the assessment phase of the nursing
process. While assessing a community’s ability to enhance its health, the nurse
may simultaneously collect data on community lifestyle behaviors and interpret
previously collected data on morbidity and mortality.
Community needs assessment is the process of determining the real or perceived
needs of a defined community. In some situations, an extensive community study
may be the first priority; in others, all that is needed is a study of one system or even
one organization. At other times, community health nurses may need to perform
a quick examination or “windshield survey” to familiarize them with an entire
community without going into any depth.
The next text discusses the types of community needs assessment, the methods of
community health assessment, and sources of data.
a. Types of Community Needs Assessment
Although it is difficult to determine the type of assessment needed in advance,
understanding the various types of community assessment in advance helps to
facilitate your decision. Here below there is a short description of the types ofcommunity needs assessment.
Familiarization or Windshield Survey
A familiarization assessment is a common starting place in evaluation of a community.
It involves studying data already available on a community, then gathering
a certain amount of firsthand data in order to gain a working knowledge of the
community. Such an approach may utilize a windshield survey—an activity often
used by nursing students in community health courses and by new staff members
in community health agencies. Nurses drive (or walk) around the community of
interest; find health, social, and governmental services; obtain literature; introduce
them-selves and explain that they are working in the area; and generally, become
familiar with the community and its residents. This type of assessment is needed
whenever the community health nurse works with families, groups, organizations,
or populations. The windshield survey provides knowledge of the context in which
these aggregates live and may enable the nurse to better connect clients with
community resources.
Problem-Oriented Assessment
A second type of community assessment, problem-oriented assessment, begins
with a single problem and assesses the community in terms of that problem.
The problem-oriented assessment is commonly used when familiarization is
not sufficient and a comprehensive assessment is too expensive. This type of
assessment is responsive to a particular need. The data collected will be useful in
any kind of planning for a community response to the specific problem. Data should
address the magnitude of the problem to be studied (e.g., prevalence, incidence),
the precursors of the problem, information about population characteristics, along
with the attitudes and behaviors of the population being studied.
Community Subsystem Assessment
In community subsystem assessment, the community health nurse focuses on a
single dimension of community life. For example, the nurse might decide to survey
churches and religious organizations to discover their roles in the community. What
kinds of needs do the leaders in these organizations believe exist? What services
do these organizations offer? To what extent are services coordinated within the
religious system and between it and other systems in the community? Community
subsystem assessment can be a useful way for a team to conduct a more systematic
community assessment. If five members of a nursing agency divide up the ten
systems in the community and each person does an assessment of two systems,
they could then share their findings to create a more comprehensive picture of thecommunity and its needs
Comprehensive Assessment
Comprehensive assessment seeks to discover all relevant community health
information. It begins with a review of existing studies and all the data presently
available on the community. A survey compiles all the demographic information on
the population, such as its size, density, and composition.
Key informants are interviewed in every major system—education, health, religious,
economic, and others. Key informants are experts in one particular area of the
community or they may know the community as a whole. Examples of key informants
would be a school nurse, a religious leader, key cultural leaders, the local police
chief or fire captain, a mail carrier, or a local city council person. Then, more detailed
surveys and intensive interviews are performed to yield information on organizations
and the various roles in each organization. A comprehensive assessment describes
the systems of a community, and also how power is distributed throughout the
system, how decisions are made, and how change occurs.
Because comprehensive assessment is an expensive, time-consuming process, it
is not often undertaken. Performing a more focused study, based on prior knowledge
of needs is often a better and less costly strategy. Nevertheless, knowing how to
conduct a comprehensive assessment is an important skill when designing smaller,
more focused assessments.
Community Assets Assessment
The final form of assessment presented here is assets assessment, which focuses
on the strengths and capacities of a community rather than its problems. The
type of assessment depends on variables such as the needs that exist, the goals to
be achieved, and the resources available for carrying out the study.
Assets assessment begins with what is present in the community. The capacities
and skills of community members are identified, with a focus on creating or rebuilding
relationships among local residents, associations, and institutions to multiply power
and effectiveness. This approach requires that the assessor looks for the positive.
Assets assessment has three levels:
1. Specific skills, talents, interests, and experiences of individual community
members such as individual businesses, cultural groups, and professionals
living in the community.
2. Local citizen associations, organizations, and institutions controlled largely
by the community such as libraries, social service agencies, voluntary
agencies, schools, and police.
3. Local institutions originating outside the community controlled largely outsidethe community such as welfare and public capital expenditures.
The key, however, is linking these assets together to enhance the community from
within. The community health nurse’s role is to assist with those linkages.
b. Community Assessment Methods
Community health needs may be assessed using a variety of methods. The choice of
assessment method varies depending on the reasons for data collection, the goals
and objectives of the study, and the available resources. It also varies according to
the theoretical framework or philosophical approach through which the nurse views
the community. In other words, the community health nurse’s theoretical basis for
approaching community assessment influences the purposes for conducting the
assessment and the selection of methodology.
Regardless of the assessment method used, data must be collected. Data collection
in community health requires the exercise of sound professional judgment, effective
communication techniques, and special investigative skills. Four important methods
are discussed here: surveys, descriptive epidemiologic studies, community forums
or town meetings, and focus groups.
Surveys
A survey is an assessment method in which a series of questions is used to collect
data for analysis of a specific group or area. Surveys are commonly used to provide
a broad range of data that will be helpful when used with other sources or if other
sources are not available.
To plan and conduct community health surveys, the goal should be to determine
the variables (selected environmental, socioeconomic, and behavioral conditions
or needs) that affect a community’s ability to control disease and promote wellness.
The nurse may choose to conduct a survey to determine such things as health
care use patterns and needs, immunization levels, demographic characteristics, or
health beliefs and practices.
The survey method involves self-report, or response to predetermined questions,
and can include questionnaires, telephone or in person interviews. It can also be
combined with other measures.
The process of gathering data consists to interview key informants in the community.
These may be knowledgeable residents, elected officials, or health care providers.
It is essential that the community health nurse recognize that the views of these
people may not reflect the views of all residents.
Descriptive Epidemiologic Studies
A second assessment method is a descriptive epidemiologic study, which
examines the amount and distribution of a disease or health condition in a populationby person (Who is affected?), by place (Where does the condition occur?), and by
time (When do the cases occur?).
In addition to their value in assessing the health status of a population, descriptive
epidemiologic studies are useful for suggesting which individuals are at greatest
risk and where and when the condition might occur. They are also useful for health
planning purposes and for suggesting hypotheses concerning disease etiology.
Geographic Information System Analysis
The geographic information systems (GIS) “mapping and visualization of health
disparities and their relationship to the geographical location of health care services
can allow for better resource allocations to disparate and underserved populations”.
It is now commonly used in community health assessment, in general, and for
specific populations and problems. For example, GIS has been useful in identifying
air pollutant risk exposure, planning or rapid public health response during a
natural disaster, and identification of colorectal screening resources for medically
underserved communities.
GIS data are often combined with field observation or census data and other survey
results to provide powerful visualizations of data for analysis and intervention.
Community Forums or Town Hall Meetings
The community forum or town hall meeting is a qualitative assessment method
designed to obtain community opinions. It takes place in the neighborhood of the
people involved, perhaps in a school gymnasium or an auditorium. The participants
are selected to participate by invitation from the group organizing the forum.
Members come from within the community and represent all segments of the
community that are involved with the issue. For instance, if a community is
contemplating building a swimming pool, the people invited to the community
forum might include potential users of the pool (residents of the community who do
not have pools and special groups such as the Girl Scouts, elders, and disabled
citizens), community planners, health and safety personnel, and other key people
with vested interests. They are asked to give their views on the pool: Where should
it be located? Who will use it? How will the cost of building and maintaining it be
assumed? What are the drawbacks to having the pool? Any other pertinent issues
the participants may raise are included. This method is relatively inexpensive, and
results are quickly obtained. A drawback of this method is that only the most vocal
community members, or those with the greatest vested interests in the issue, may
be heard.
This format does not provide a representative voice to others in the community who
also may be affected by the proposed decision. This method is used to elicit public
opinion on a variety of issues, including health care concerns, political views, and
feelings about issues in the public eye, such as gangs.
Focus Groups
This fourth assessment method, focus groups, is similar to the community forum
or town hall meeting in that it is designed to obtain grassroots opinion. However,
it has some differences. First, only a small group of participants, usually 5 to 15
people, is present. The members chosen for the group are homogeneous with
respect to specific demographic variables. For example, a focus group may consist
of female community health nurses, young women in their first pregnancy, or retired
businessmen.
Leadership skills are used in conjunction with the small group process to promote
a supportive atmosphere and to accomplish set goals. The interviewer guides the
discussion according to a predetermined set of questions or topics. The best use
of focus group data includes not only analysis of individual communications, but of
the interactions between participants.
Nurses who conduct focus groups must carefully select participants, formulate
questions, and analyze recorded sessions. These sessions can produce greater
interaction and expression of ideas than surveys and may provide more insight
into an aggregate’s opinions. In addition to encouraging community participation
in the identification of assets and needs, focus groups may lay the groundwork for
community involvement in planning the solutions to identified problems.
Major advantages of focus groups are their efficiency and low cost, similar to the
community forum or town hall meeting format. A focus group can be organized to be
representative of an aggregate, to capture community interest groups, or to sample
for diversity among different population groups. One example is a research study
involving youths and adults. Eight focus groups were held to determine perceptions
of healthy diet and exercise among parents and children. Whatever the purpose,
however, some people may be uncomfortable expressing their views in a group
situation.
c. Sources of Community Data
The community health nurse can look in many places for data to enhance and
complete a community assessment. Data sources can be primary or secondary,
and they can be from international, national, or local sources.
Primary and Secondary Sources
Community health nurses make use of many sources in data collection: Community
members, including formal leaders, and informal leaders. The community members
can frequently offer the most accurate insights and comprehensive information.
Information gathered by talking to people provides primary data, because the
data are obtained directly from the community. Secondary sources of data
include people who know the community well and the records such people create
in the performance of their jobs. Specific examples are health team members,
client records, community health (vital) statistics, census bureau data, reference
books, research reports, and community health nurses. Because secondary data
may not totally describe the community and do not necessarily reflect community
self-perceptions, they may need augmentation or further validation through focus
groups, surveys, and other primary data collection methods.
International Sources
International data are collected by several agencies, including the World Health
Organization (WHO) and its six regional offices and health organizations. In
addition, the United Nations and global specialty organizations that focus on certain
populations or health problems, such as the United Nations Children’s Fund, are
major sources of international health-related data. The WHO publishes an annual
report of their activity, and international statistics for diseases and illness trends can
be found on the Internet.
Information from these official sources can give the nurse in the local community
information about immigrant and refugee populations he serves.
National Sources
Community health nurses can access a wealth of official and nonofficial sources
of national data. Official sources develop documents based on data compiled by
the government. Example of national data sources: National Institute of Statistics
of Rwanda, Ministry of Health, Rwanda through its department like Rwanda
Biomedical Center, etc.
d. Steps of community health needs assessment
The following are the required steps in conducting a needs assessment:
1) Identify aggregate for assessment
2) Identify required information
3) Select method of data gathering
4) Develop questionnaire or interview questions
5) Develop procedures for data collection
6) Train data collectors
7) Arrange for a sample representative of the aggregate
8) Conduct needs assessment
9) Tabulate and analyze data
10) Identify needs suggested by data11) Develop an action plan
Self-assessment 5.3
1) Discuss the Sources of data for community health needs assessment.
2) Describe different methods used for community health assessment.3) What are the steps in conducting community health needs assessment?
5.4. Basic community interventions
5.4.1. Community education
Learning activity 5.4.1
Using Community Health Nursing Textbooks and internet; read about community
education and respond to the following questions:
1) Discuss different methods used for providing a community health
education.
2) What do you understand for the factors that affect readiness to learn
among community health members?
3) Discuss any four teaching materials used for providing a community
health education session.a. Overview on community health education
Health education is an integral part of the nurse’s role in the community for
promoting health, preventing disease, and maintaining optimal wellness. Moreover,
the community is a vital link for the delivery of effective health care and offers
the nurse multiple opportunities to provide appropriate health education within the
context of a setting that is familiar to community members.
At the core of health education is the development of trusting relationships based
on nurturing and healing interactions, the use of community-based participatory
methods that highlight community strengths, and the creation of sustainable
collaborations and partnerships
Health education is any combination of learning experiences designed to predispose,
enable, and reinforce voluntary behavior conducive to health in individuals,
groups, or communities. Its goal is to understand health behavior and to translate
knowledge into relevant interventions and strategies for health enhancement,
disease prevention, and chronic illness management. Health education aims toenhance wellness and decrease disability; attempts to actualize the health potential
of individuals, families, communities, and society; and it includes a broad and varied
set of strategies aimed at influencing individuals within their social environment for
improved health and well-being.
Aim of health education is not just about giving health information, but also involves
the process of changing a person or community towards favorable healthy behaviors
and maintaining optimum health.
The most important goal of health teaching in community-based care is to assist the
client and family in achieving independence through self-care.
When client learning needs are considered within the context of the client, family
and community, care is improved.
Likewise, staff satisfaction improves when teaching results are positive. It is
professionally satisfying to prepare a client for discharge and receive subsequent
feedback that the discharge was satisfactory. Likewise, it is professionally satisfying
for the home care nurse to prepare a client to successfully manage self-care at
home. On the other hand, it is stressful when a nurse sees a client with inadequate
preparation trying to manage home care unsuccessfully.
Quality health education provides continuity between settings of care. Providing
information about diet, activity, medications, equipment, and follow-up appointments
enhances self-care capacity.
Community health education is especially a matter of working with community
organizations, voluntary bodies, and groups. Informal leadership based on respect
and not on the office holdings, is often very influential. Political leadership is
usually the most powerful, but professional and voluntary leadership also need
understanding and collaboration.
Studying the community: it means especially studying those who have leadership
positions in the community, and then the organizations, bodies, and groups through
which their influence is spread. To build co-operation with those who have authority
can make difference between success and failure in disease control or a health
improvement campaign. Informal leadership is of those people who, though holding
no offices, are nevertheless respected by particular groups. Such groups may meet
for drinking and the exchange of news and gossip. Those who are respected and
listened to in these groups can powerfully influence many people’s thinking and
attitudes, and the co-operation they give to, or withhold from, health staff. The official
leadership of greatest importance is the political leadership. Mutual understanding
with those who carry the responsibility for the administration is very essential.
Professional leadership in the village is found not only in the agricultural extensionservice, in education, rural or community development, social welfare, etc. but also
in the churches, and sometimes other voluntary bodies. It is necessary to work
together closely with all these agencies. For example, a health education campaign
which succeeds in persuading people to eat more eggs will lead to a quick rise in
the price of eggs unless the agricultural staff also works successfully persuading
farmers to produce more eggs.
Schools, Farmers’ clubs, literacy programs, Scouts and Guides, Red Cross,
women’s progress movements, etc. are all interested in health improvement. They
can help in health education in substantial and effective way. Their co-operation
with programs of the health services can be valuable and fruitful.
No opportunity should be missed to explain health programs to these agencies and
to enlist support for particular health education campaigns.
A community health education program needs to Centre upon a recognized
problem and be well planned. Rumors can do great damage and need to be
systematically and quickly contradicted.
The community health nurses need to study and seek to understand their community,
its hopes and fears, its personalities and power structure, its priorities and methods
of decision making, and also the problems involved in implementing the decisions
made.
Working in the community: it depends upon developing and maintaining good
working relationships with official leaders, informal opinion leaders, and voluntary
leaders. All must be kept informed, taken into our confidence, and have a clear
understanding of our plans and objectives. Regular meetings providing for cross
representation on their committees can help. Health education is not confined to
formal activities but goes an all the time as people meet. Our aim must be to work
from within the community.
In planning community health education: it is better to start with a problem
and to choose one which has widespread importance and which the community
recognizes and wants to reduce or eliminate. Scabies, worms, colds, or nuisance
pests like rats and flies, can all be important in the thinking and life of a community.
Then co-operation and confidence can be built up by actively following the five
steps scheme:
• Recognition of the problem
• Analysis of the problem-educational diagnosis
• Educational prescription
• Educational treatment
• Recording and review of results, with evaluation.
Mobilizing the community for action: is the road to success. Community healthnurse set targets, to be reached as the work progresses. The community members
should be involved in the solving of the community health problems, and wherever
it is possible the use of community available resources is advised.
Divisions, rival groups, and damaging rumors are the chief dangers. As health
education program moves to success, the confidence created should give rise to
growing interest in tackling more serious problems. These can range from maternal
and infantile mortality to tuberculosis, measles, or other causes of high morbidity
and mortality. Some problems are however so tied to deep-rooted habits and
customs that are very difficult to make much headway. Smoking and the resulting
respiratory conditions, alcoholism, venereal disease and malaria are examples.
Where a sustained long term health education program is needed it is wise to be
sure you have the experience, the resources and the staff to get deeply involved
before commencing such program. Skilled advice from a health education specialist
can be a substantial help.
b. Factors that affect readiness to learn
Factors that affect readiness to learn are the followings:
Physiologic factors: Age, gender, disease process currently being treated,
intactness of senses (hearing, vision, touch, and taste), and preexisting condition.
Psychosocial factors: Sociocultural circumstances, occupation, economic stability,
past experiences with learning, attitude toward learning, spirituality, emotional
health, self-concept and body image, sense of responsibility for self.
Cognitive factors: Developmental level, level of education, communication skills,
primary language, motivation, reading ability, learning style, problem-solving ability.
Environmental factors: Home environment, safety features, family relationships/
problems, caregiver (availability, motivation, abilities), other support systems.
Developmental considerations: It is helpful for the nurse to understand various
theories of development. Just as the need to learn will be different at various age
levels, the cognitive domain will differ and life experiences will differ. For example,
teaching a 6-year-old girl about insulin administration will be different from teaching
a 24-year-old woman, which would in turn be different from teaching a 69-year-old
woman.
The nurse must consider these factors when developing teaching plans.
c. Learning domains
Teaching and learning occur in three learning domains: cognitive, affective, and
psychomotor. All three domains must be considered in all aspects of the teaching
and learning process. Thus, the nurse must assess the client’s need, readiness,and past experience in the cognitive, affective, and psychomotor domains
Cognitive learning involves mental storage and recall of new knowledge and
information for problem solving. Sometimes this domain is referred to as the critical
thinking or knowledge domain. An example of cognitive learning is seen in the client
who has recently been diagnosed with insulin-dependent diabetes. Not only will
this client need information about diet, insulin, and exercise, but he or she will also
need to use the information to formulate menus and an exercise plan. In addition,
as blood sugar levels fluctuate, a client with diabetes must alter food intake and
exercise. All this requires cognitive learning.
Affective learning involves feelings, attitudes, values, and emotions that influence
learning. This is also referred to as the attitude domain.
In the last decade the role emotion plays in learning has been speculated to be the
most influential of all the domains in impacting motivation, thus the first domain that
educators should assess. For example, the client who has just been identified as
having diabetes may have to talk about his or her feelings about having diabetes
before being ready to learn about insulin. Some of the client’s feelings may stem
from his or her prior knowledge and preconceived ideas about diabetes.
Psychomotor learning consists of acquired physical skills that can be demonstrated.
This may be referred to as the skill domain. For example, the client with newly
diagnosed insulin-dependent diabetes must learn to give self-injections, which will
require learning the skill of using syringes.
d. Teaching and levels of prevention
Teaching, whether it is in the acute care or community-based setting, occurs
at all levels of prevention. An important goal of teaching is to prevent the initial
occurrence of disease or injury through health promotion and prevention activities.
The examples of primary prevention: A nurse teaching a nutrition class to parents
an example of health promotion. A school nurse teaching parents about preventing
malaria, childhood injuries focusing on health protection. Teaching parents about
the importance of immunization, promotion of healthy lifestyle, food hygiene, weight
control, growth and development of children, are also primary prevention.
Secondary prevention teaching is targeted toward early identification and
intervention of a condition. A home care nurse teaching the parents of a ventilator
dependent child about early signs of upper respiratory infection and when to contact
the health facility, breast self-examination and treatment of cancer, is focusing on
secondary prevention.
Tertiary prevention: Most teaching in the home setting addresses tertiary
prevention because most home care clients have chronic conditions or are
postsurgical. Tertiary prevention arises from teaching that attempts to restore healthand facilitate coping skills. Examples: skill of self-care for rehabilitation at centre or
home (e.g., post stroke, palliative care, care of wound, care for special needs child).
e. Methods of health education
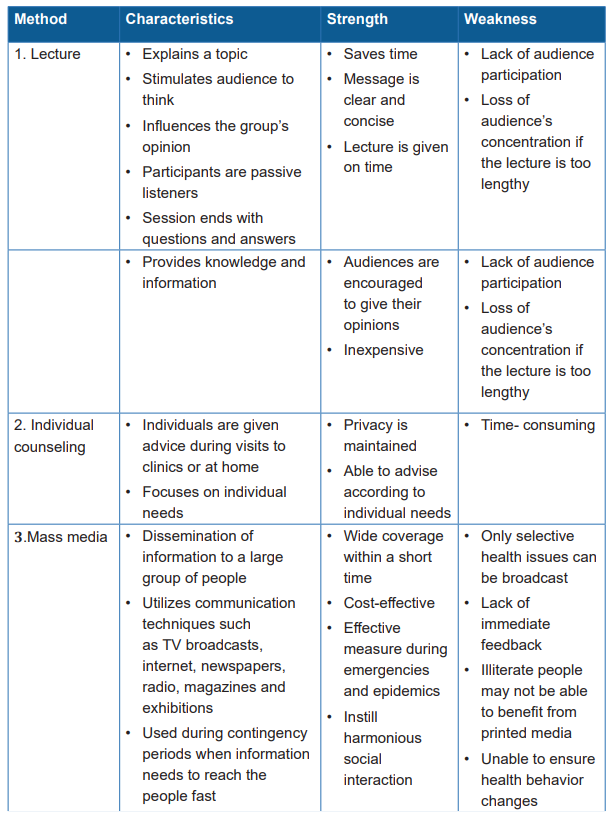
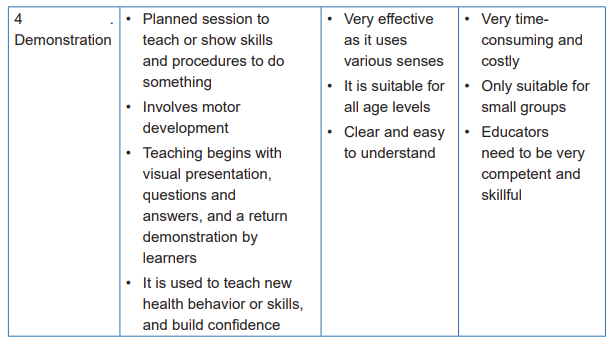
Description of certain methods of health education and their uses
a. Illustrated lecture:
It is a teaching method in which the teacher delivers information through an
interactive oral presentation, often using visual aids to support the presentation.
Because you may present information formally in a classroom or informally during
a clinical practice session, the term “interactive presentation” is used rather than
illustrated lecture. No matter where you are presenting information, remember the
following keys to a successful presentation:
Define learning objectives: Decide what the learners should know or be able to do
after this presentation.
Plan your presentation: Create an outline based on your objectives to help
organize the content and keep focused. The outline should include key points,
questions, reminders of activities and visual aids, and summary points.
Introduce each presentation: A good introduction grabs attention and clearly
communicates the objectives of the session. Vary introductions used in different
presentations to maintain learners’ interest.
Use effective presentation skills. Involve learners by asking questions, moving
around the room when possible, and maintaining eye contact. Provide clear
transitions between topics and summaries.
Use questioning techniques. Asking questions is essential to maintaining learners’
interest, checking their understanding, and developing their problem-solving skills.It helps learners assess information and learn to make appropriate choices.
Summarize your presentation. A good summary supports the presentation’s main
points and reinforces the most important information.
Note: Use this check list to assess your presentation skills. Check each skill was
performed. Which areas need improvement?
Planning the presentation:
1) Review the objectives.
2) Prepare an outline of key points and presentation aids such as visual
materials
3) Note questions for students
4) Note reminders for planned activities
5) Note reminders to use specific visual aids.
6) Note summary questions or other activities
Introducing the presentation:
1) State the objective(s) of the presentation as part of the introduction.
2) Use a variety of introductions to capture interest, make learners aware of the
objectives, and create a positive learning climate.
3) Relate the content to previously covered and related topics
Using effective presentation skills:
1) Follow a plan and use an outline
2) Communicate clearly with students. Project your voice, move about the
room, provide clear transitions between topics, and maintain eye contact.
3) Interact with learners by asking and responding to questions, using their
names, and providing feedback.
4) Use visual materials to illustrate and support main points.
Using questioning techniques during a presentation:
1) Target questions to the group and to individuals.
2) Provide feedback and repeat correct responses.
3) Use students’ names.
4) Redirect questions that are typically or totally incorrect until the correct
answer is revealed.
Summarizing the presentation:
1) Stress the main points
2) Relate information to the objectives.
3) Provide an opportunity for questions.
b.Creation and facilitation of role play
The steps to be followed in creating a role play:
To create a role play, follow these steps:
• Decide what the students should learn from the role play (the objectives).
• Select an appropriate situation: it may be drawn from students ‘experiences,
your experiences, or clinical records. The situation should be relevant and
similar to situations that students will encounter during their professional
careers. Keep the situation simple; the interaction is more important than the
content. Because the same role play may be used with a number of students
in various learning settings, keep the situation as general as possible.
• Identify the roles that students will act out during the role play. In most clinical
learning situations, there will be a clinician and a patient. Specify any specific
roles or points of information that students should cover. For example, if
the student acting the role of the patient should resist advice, ask certain
questions, or give certain answers, clearly explain the desired “patient”
behavior in the role play.
• Determine whether the role play will be informal, formal, or a clinical
demonstration. These are defined as:
– Informal: the teacher gives the role players a general situation and asks
them to “act it out” with little or no preparation time. For example, if a question
about a patient counseling session comes up in class, you may ask two of
the students to take a few minutes to plan and present a brief role play that
addresses the situation. This type of role play is not prepared in advance.
– Formal: The teachers give the role players a set of instructions that outline
the scope and sequence of the role play. Using the counseling example, the
students would be given a situation with specific roles they are to act out,
often with specific points of information to cover.
– Clinical demonstration: this type of role play is often part of a clinical
simulation. The clinical demonstration role play, which is similar to the
formal role play, typically uses an anatomic model, simulated patient, or
real patient, and often occurs as part of a coaching session. For example,
you demonstrate a pelvic examination using a pelvic model, or demonstrate
counseling a woman about oral contraceptives. Following the demonstration,
you ask two of the students to role play the procedure. One student assumes
the patient or caretaker role, while the other assumes the role of the clinician.
If an anatomic model is used, the student playing the patient sits or stands bythe model and speaks as a patient would, asking questions and responding
to the clinician. The student playing the clinician will not only perform the
physical examination but also will verbally interact with the “patient”.
– Determine whether students will report the results of their discussion of the
role play in writing or orally to entire group.
Facilitation of a role play:
To facilitate a role play:
• Explain the nature and purpose of the exercise (the objectives).
• Define the setting and situation of the role play.
• Brief the participants of their roles.
• Explain what the other students should observe and what king of feedback
they should give. Tell students what to look for and how to document their
questions or feedback. Should they observe for verbal communication skills?,
The use of questioning?, Nonverbal communication?
• Provide the students with questions or activities that will help them to focus
on the main concept (s) being presented.
• Keep the role play brief and to the point. Be ready to handle unexpected
situations that might arise (confusion, arguments, etc.).
• Engage students in a follow-up discussion. Discuss important features of the
role play by asking questions of both the players and observers.
• Provide feedback, both positive and suggestions for improvement.
• Summarize what happened in the session, what was learned, and how it
applies to the skill being learned.
Note: A role play will be effective only if it is clearly related to the learning objectives.
Explain the objectives of the role play before beginning the activity. When the role
play is completed, summarize and discuss the results of the role play and relate the
role play to the learning objectives.
c.Facilitating a brainstorming session
Brainstorming is generating a list of ideas, thoughts, or alternative solutions that
focus on a specific topic or problem. Brainstorming is a teaching method that
stimulates thought and creativity and is often used along with group discussions.
Brainstorming sessions should not be interrupted to discuss or criticize ideas. The
compiled list may be used as the introduction to a topic or form the basis for a group
discussion.
Once the brainstorming process has been completed, the group can organize the
ideas into themes. The key to successful brainstorming is to separate the generationof ideas, or possible solutions to a problem, from the evaluation of these ideas or
solutions.
Plan for brainstorming by determining the objectives of the activity and making sure
that there is a way to record responses and suggestions.
Brainstorming is useful to:
• Stimulate interest in a topic.
• Encourage broad or creative thinking.
Facilitation of a Brainstorming session:
• Share the objective of the brainstorming session.
• Explain the ground rules before the session. There are three basic rules: all
ideas will be accepted, discussions of suggestions are delayed until after the
activity, and no criticism of suggestions is allowed.
Example: “During this brainstorming session, we will be following three basic rules.
All ideas will be accepted; Peter will write them on the flipchart. At no time will we
discuss or criticize any idea. Later, after we have our list of suggestions, we will go
back and discuss each one. Is there any question? If not,”
• State the topic or problem. Clearly state the focus of the brainstorming session.
Example: During the next few minutes we will be brainstorming and will follow our
usual rules. Our topic today is “Benefits of Family Planning.” I would like your full
participation. Janet will write these on the board so that we can discuss them later.”
• Maintain a written record on a flipchart or writing board of the ideas and
suggestions. This will prevent repetition, keep learners focused on the topics,
and be useful when it is time to discuss each item.
• Provide opportunities for anonymous brainstorming by giving the learners
cards on which they can write their comments or questions. Post the cards
and use them for a later discussion. This technique allows learners to share
thoughts or questions without revealing their identities.
• Involve all of the students and provide positive feedback in order to encourage
more input. Avoid allowing a few learners to monopolize the session, and
encourage those not offering suggestions to do so.
• Review written ideas and suggestions periodically to stimulate additional
ideas.
• Conclude brainstorming by summarizing and reviewing all of the suggestions,
and by placing ideas in categories, if this is useful and possible.
d. Facilitating a discussion
A discussion is an opportunity for learners to share their ideas, thoughts, questions,and answers in a group setting with a facilitator.
A discussion that relates to the topic and stays focused on the learning objectives
can be a very effective teaching method. Guide the learners as the discussion
develops and keep it focused on the topic at hand.\Group discussion is used to
support other teaching methods, particularly to:
• Conclude a presentation.
• Summarize the main points of a videotape.
• Check students’ understanding of a clinical demonstration.
• Examine alternative solutions to a case study.
• Explore attitudes exhibited during a role play.
• Analyze the results of a brainstorming session.
Considerations when preparing for a discussion:
When preparing for a discussion, consider the following:
• What are the objectives of this discussion? How long should it last?
• Do learners have some knowledge of or experience with the topic? Attempting
a group discussion when students have limited knowledge or experience in
the topic will often result in little or no interaction.
• Is there enough time available? Discussion requires more time than a
presentation because of the interaction among students.
• Are you prepared to direct or control the discussion? A poorly directed
discussion may move away from the subject and never accomplish the
learning objectives. If the teacher does not maintain control, a few students
may dominate the discussion while others lose interest.
Key points to be followed to ensure successful group discussions
How do you choose a topic for discussion? Group discussions are best planned
ahead of time, although sometimes they arise spontaneously from the students.
The following key points should be followed to ensure successful group discussions:
• Have a very clear idea in mind of what the group will discuss and what you
hope to gain through the discussion. State the topic as part of the introduction.
Example: “To conclude this presentation on counseling the sexually active
adolescent, let’s take a few minutes to discuss the importance of confidentiality.”
• Shift the conversation to the learners. Allow the learners to discuss the topic
and ensure that the discussion stays on the topic at hand. Encourage shy
learners to speak up so that everyone has a chance to share their thoughts.
Examples:
– “James, would you share your thoughts on…?”– “Mary, what is your opinion?”
– “Luck, do you agree with my statements that…”
• Allow the group to direct the discussion; act as a referee and intercede only
when necessary.
Example: “It is obvious that Peter and Rose are taking opposite sides in this
discussion. Peter, let me see if I can clarify your position. You seem to feel that…”
• Summarize the key points of the discussion periodically. Provide feedback on
learners’ comments when appropriate.
Example:
– Let’s stop here for a minute and summarize the main points of our discussion.”
– “Actually, confidentiality is essential for counseling and testing for HIV. Can
anyone tell me why?”
• Ensure that discussion stays on the topic.
Examples:
– “Sandra, can you explain a little more clearly how that situation relates to our
topic?”
– “Monica, would you clarify for us how your point relates to the topic?”
– “Let’s stop for a moment and review the purpose of our discussion.”
• Use the contributions of each learner and provide reinforcement. Point out
differences or similarities among the ideas presented by different people.
Examples:
– “That is an excellent point, John. Thank you for sharing that with the group.”
– “Alex has a good argument against the policy. Mark, would you like to take
the opposite position?”
• Encourage all learners to get involved.
Example: “Sylvia, I can see that you have been thinking about these comments.
Can you give us your thoughts?”
• Ensure that no one learner dominates the discussion.
Example: “Paul, you have contributed a great deal to our discussion. Let’s see if
someone else would like to offer…”
Note: your role as the discussion facilitator is to keep the discussion focused,
ensure that all students have equal opportunity to participate, and to intervene
when the discussion moves away from the objectives. Conclude the discussion
with a summary of the main ideas and how they relate to the objectives presentedduring the introduction.
e. Demonstration
Note that giving a good demonstration is worth a thousand words. There are four
steps to a demonstration:
1. Explaining the ideas and skills that you will be demonstrating
2. Giving the actual demonstration
3. Giving an explanation as you go along, doing one step at a time
4. Asking one person to repeat the demonstration and giving everyone a
chance to repeat the
Qualities of a good demonstration
For an effective demonstration you should consider the following features: the
demonstration must be realistic, it should fit with the local culture and it should use
familiar materials. You will need to arrange to have enough materials for everyone
to practice and have adequate space for everyone to see or practice. People need
to take enough time for practice and for you to check that everyone has acquired
the appropriate skill.
f. Traditional means of communication
Traditional means of communication exploit and develop the local means, materials
and methods of communication, such as poems, stories, songs and dances, games,
fables and puppet shows.
g.Preparation and using the teaching / learning materials (aids)
After completing this sub-session, you will be able to prepare and use a variety of
the following teaching/learning materials:
• A writing board
• A flipchart
• A video
• Slides and a computer to prepare and project a presentation
• Leaflets
1) A writing board:
A writing board is the most commonly used visual aid. It can display information
written with chalk (chalkboard or blackboard) or special pens (whiteboard). You
can use a writing board for announcements, informal discussions, brainstorming
sessions, and note taking. A writing board is also an excellent tool for illustrating
subjects like anatomy and physiology and for outlining procedures.
Some possible uses of a writing board:
• Document ideas during discussions or brainstorming exercises,
• Draw a sketch of anatomy or a physiological response,
• Note points you wish to emphasize,
• Diagram a sequence of activities for working through the process of making
a clinical decision,
Tips (instructions, guidelines) for using a writing board:
Most teachers use a writing board of some kind. Sometimes the board will look
messy at the end of a presentation, with untidy diagrams and no pattern to the
words. For using a writing board, follow the following guidelines:
• Before you start, decide what you will illustrate on the board.
• During the presentation, write the key words or phrases in order, according to
the structure of the presentation.
• Remember that learners tend to copy the words and the layout as they appear
on the board, so make sure that what you write on the board is what you want
the learners to write in their notes.
• Keep the board clean
• Use chalk or pens that contrast with the background of the board so the
learners can see the information clearly.
• Make text and drawings large enough to be seen in the back of the room.
• Underline headings and important or unfamiliar words for emphasis
• Do not talk while facing the board.
• Do not block the learners’ view of the board; stand aside when you have
finished writing or drawing.
• Allow sufficient time for learners to copy the information from the board.
• Summarize the main points at the end of the presentation.
2) A flipchart
A flipchart is a large tablet or pad of paper, usually a tripod or a stand. You can use
a flipchart for displaying prepared notes or drawings as well as for brainstorming
and recording ideas from discussions. You can also use flipcharts before and after
clinical practice visits to introduce objectives and group exercises, or to summarize
the experience.
The possible uses of a flipchart are the same as those listed for the writing board,
but also include the following:
• Note objectives or outcomes before or after clinical practice sessions.
• Create flowcharts to work through clinical decision-making in different
situations, such as during a complicated labor and childbirth.
• Record discussions or ideas during small group exercises.
Tips for using a flipchart:
• Make it easy to read. Use bullets (*) to highlight items on the page. Leave
plenty of white space, and avoid putting too much information on one page.
Print in block letters using wide-tipped pens or markers.
• Make the flipchart page attractive. Use different colored pens to provide
contrast, and use headings, boxes, cartoons, and borders to improve the
appearance of the page.
• Have masking tape available to hang flipchart pages on the walls during
brainstorming and problem-solving sessions.
• To hide a portion of the page, fold up the lower portion of the page and tape
it; when you are ready to reveal the information, remove the tape and let the
page drop.
• Face the learners, not the flipchart, while talking.
• When you finish with a flipchart page, tape it to the wall where you and the
learners can refer to it.
Note: When you use the flip chart in health education you must discuss each
page completely before you turn to the next and then make sure that everyone
understands each message. At the end you can go back to the first charts to review
the subject and help people remember the ideas.
3) Preparation and using computer generated slides
When preparing slides:
• Limit each slide to one main idea; detailed information should be put into a
handout, not on a slide.
• Make sure slides support the text or objectives. Slides should clearly
demonstrate their objective.
• Be sure that the material on the slide is legible. A good rule is that if a slide
can be read by the naked eye-without a projector- it will be legible to learners
in the back of the room when it is projected.
• When using a computer to develop a presentation, keep the presentation
simple and clear.
• Be consistent, Use the same general style and tone throughout.
• Proofread. You are more likely to catch errors if you proofread before creating
slides.
• Limit the information on each slide to one idea that can be grasped in 5-10
seconds.
• State the main idea in the title.
• Use about three to five bullets per slide. Use no more than seven lines of text.
• Limit a bulleted item to six to eight words.
• Whenever possible, use pictures, or graphs to support or replace text. Bar
graphs and line graphs are effective tools to show trends and statistics.
Photographs and line drawings are foe example useful for showing clinical
signs and symptoms and demonstrating clinical procedures.
• Make graphics and drawings large enough to be seen easily in the back of the
room. Use large lettering (at least 5 mm tall, preferably larger if printing, or 18
point or larger if using a computer).
• If you are using a computer to prepare slides use only one typeface (font) per
slide. Use italics or bold to emphasize points rather than using another font.
• Make sure that technical assistance is available to deal promptly with
problems. Practice the computer program for creating and projecting your
presentation until you are comfortable with it.
• Avoid busy or confusing background. Use a color for the text that has a very
high contrast with the background. A simple white background with dark
lettering is very effective.
• I you are preparing a projected presentation, minimize the transition between
slides. Use sound effects sparingly and only to emphasize a point. If there is
animation, it should be used consistently throughout the presentation.
• Remember that your slides should highlight your key points. They should not
contain the full text of the presentation.
• Charts and tables should be large and simple for the message to be clear.
• Always save the presentation on the computer’s hard drive and on other USB
like flash disk or CD-Rom in case something happens to the computer (e.g.
sometimes computers “crash” or “freeze” and information can be lost if not
saved.
The following are some instructions for using a slide projector:
• Arrange the room so that all learners can see the screen; make sure that
there is nothing between the projector and the screen.
• Set up and test the slide projector and computer before the learners arrive
• Once the projector is on, move away from the projector to avoid blocking the
learners’ view of the screen.
• Face the learners, not the screen, while talking.
• Allow plenty of time for the learners to read what is on the screen and takenotes, if necessary
• Determine if all or some of the lights can be left on during the slide presentation;
this will help learners pay attention and make taking notes easier.
• During presentation, avoid rushing through a series of slides. This can be
very frustrating for learners, take time to view and discuss each slide. When
appropriate, ask learners questions about what they are seeing on a slide.
4) Use Video
Videos can be very versatile visual aids. Videos can be used by a single learner
for individual learning, by a group of learners for independent learning, or by the
teacher for involving learners in a discussion. One of the most important aspects
of teaching a skill is showing how an expert would perform it. Video is particularly
useful for this purpose. A bank for prerecorded videos provides a valuable resource
for demonstrating various aspects of clinical practice. When the resources are
available, you can use video to record individual learners’ performances and provide
valuable feedback on their acquisition of clinical skills.
Note: Video can also be recorded on a CD-ROM to be played on a computer and
on a DVD to be played on a DVD player. Video from a CD-ROM or DVD can also be
projected onto a screen, allowing a large group of learners to see the video. When
this approach is used, external speakers may be needed so that all learners can
hear the audio portion of the video.
Possible uses for video:
• Provide an overview or introduction to a topic to stimulate interest and
discussion.
• Allow the teacher to model a technique or procedure, such as how to counsel
adolescents about reducing their HIV risks, assess breastfeeding attachment,
or insert an Intra-uterine Device (IUD), in a clear, step-by-step manner.
• Allow learners to practice identifying clinical signs such as sunken eyes and
fast breathing.
Tips for using Videos:
• In the classroom, use several short video segments with pauses in between
for explanation or discussion, rather than one long video.
• Preview the videotape to ensure that it is appropriate for the learners and
consistent with the course objectives.
• Make sure that the information presented in the video is up-date with current
practices and standards. If there are some differences, be sure to tell the
learners about them before showing the video. If there are considerable
differences, do not show the video.
• Before the classroom session, check to be sure that the video is compatiblewith the video player. Run a few seconds of the tape to ensure that everything
is functioning properly. Cue the video to the beginning of the program or to the
section of the video that you will show.
• Arrange the room so that all learners can see the video monitor or screen and
hear the video.
• Prepare the learners to view the video:
• State the objective
• Give the learners an overview of the content they will see on the video.
• Focus learners ‘attention by asking that they look for a number of specific
points as they watch the video.
Remember: Use videos as an interactive tool. When appropriate, stop the video
to point out things the learners should notice, or ask questions to check their
understanding. Discuss the video after it has been shown. Review the main points
that the learners were asked to watch for as they viewed the video. This will make
the video a much more effective teaching tool than if the learners watch it without
your guidance.
Summary for using visual aids: No matter which visual aids you use, remember
the following:
• Keep it simple: each flipchart or slide should present only one main point,
with supporting information in a bulleted list. This will help learners remember
important information.
• Keep it relevant: Use up-to date videos and slides. Present information and
demonstrate skills in a manner consistent with best practices.
• Keep it focused: prepare or use visual aids that support the learning
objectives and highlight main points.
• Practice using visual aids in advance
• Set up or prepare your visual aids in the room before the learners arrive
• Check that all audiovisual equipment is working before the learners arrive
• Make sure that all learners can see the writing board, flipchart, screen, and
video monitor.
• Prepare any copies of handouts related to the visual aids in advance and
have them in the room when the learners arrive.
• When appropriate, have questions or exercises (e.g. case studies, role plays)
prepared for use after using the visual aids.
• Make notes about how effective the visual aids were in helping the learners
and how you might use the visual aids in future presentations.
5) Leaflets
Leaflets are the most common way of using print media in health education. They
can be a useful reinforcement for individual and group sessions and serve as a
reminder of the main points that you have made. They are also helpful for sensitive
subjects such as sexual health education. When people are too shy to ask for
advice, they can pick up a leaflet and read it privately.
In terms of content, leaflets, booklets or pamphlets are best when they are brief,
written in simple words and understandable language. A relevant address should
be included at the back to indicate where people can get further information.
Notes: Visuals materials are one of the strongest methods of communicating
messages, especially where literacy is low amongst the population. They are good
when they are accompanied with interactive methods. It is said that a picture tells a
thousand words. Real objects, audio and video do the same. They are immediate
and powerful and people can play with them!
You might take with you real visual materials to a health education meeting. We’ve
already mentioned bed netting for demonstrating prevention of malaria, but there
are other real objects too. Think about family planning, nutrition, hygiene and so on.
If your display is on ‘family planning methods’, display real contraceptives, such as
pills, condoms, diaphragms, and foams. If your display is on weaning foods, display
the real foods and the equipment used to prepare them.
Audio material includes anything heard such as the spoken word, a health talk
or music. Radio and audio cassettes are good examples of audio aids. As the
name implies; audio-visual materials combine both seeing and listening. These
materials include Television (TV), films or videos which provide a wide range of
interest and can convey messages with high motivational appeal. They are good
when they are accompanied with interactive methods. Audio-visual health learning
materials can arouse interest if they are of high quality and provide a clear mental
picture of the message. They may also speed up and enhance understanding or
stimulate active thinking and learning and help develop memory.
f. fScheme of health education
Identification:
Names of health educator:
Topic name:
Duration (in minutes):
Time: from: ….. to: …..
Place:
Audience (or target population/group/person):
Objectives/learning outcomes: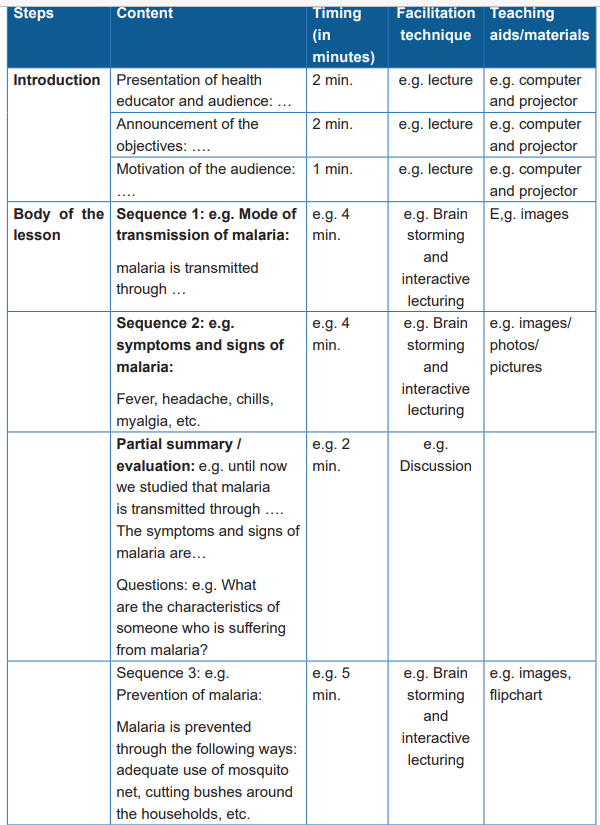
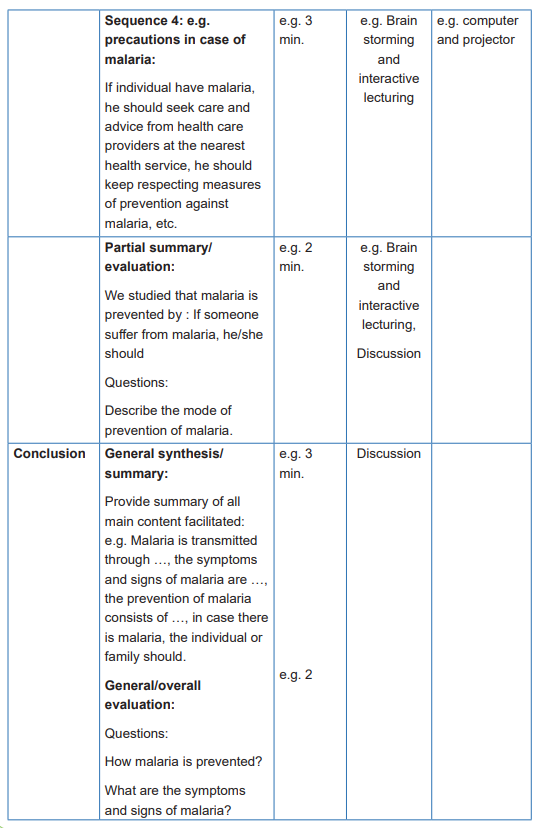
g. Barriers to Successful Teaching
It is helpful to be aware of some of the potential obstacles to successful teaching.
Conditions and barriers to successful teaching differ between the acute care setting
and community setting. Likewise, there may be barriers to successful teaching that
differ between community-based settings. In the next section barriers to successful
teaching are presented and followed by characteristics of successful teaching.
These barriers have the potential to interrupt the coordination of and consistency in
teaching and communication with the care giving team.
Nursing students and novice home care nurses often express dismay over their
diminished control of client behavior when providing care in settings other than the
acute care setting. For instance, teaching in the home often requires adaptation to
the particular home environment, where the client is in control. Further, the nurse
is faced with accommodating the specific needs of the client and family within their
own schedule and circumstances.
Another barrier relates to difficulty in coordinating client teaching among multiple
providers. Often, many care providers are involved with the client’s care.
Other professionals may include other nurses, physical therapists, social workers,
home health aides, nurse practitioners, and physicians. Each provider may teach a
procedure, treatment, or process in a different way, confusing the client. It is difficult
to maintain ongoing communication among multiple caregivers in several diverse
settings.
Lack of time is a barrier to home care teaching. The time factor in acute care
settings may prohibit teaching, and many home care referrals come from clinics or
physicians’ offices. As a result, the first teaching, in many cases, may be done in the
home. Home care nurses are often pressed for time. It may be difficult for the home
care nurse to feel teaching is ever complete or even adequateSelf-assessment 5.4.1
1) Explain 5 factors that affect the readiness to learn
2) Explain 3 domains of learning
3) Describe how the following teaching methods should be used during
health education session: Lecture, demonstration, role play
4) Describe how the following teaching materials/aids should be used during
health education session: a writing board, a video and slides & a computer
to prepare and project a presentation5.4.2. Advocating for the community
Using Community Health Nursing Textbooks and internet; read about
advocating for the community and respond to the following questions:
1) Discuss the purpose of advocacy, advocacy methods, and principles of
advocacy
2) What do you understand about approaches used in advocacy?3) Discuss the advocacy strategies.
Advocacy is the act of ‘‘taking a position on an issue, and initiating actions in a
deliberate attempt to influence private and public policy choices’’. It is an act of
delivering an argument so that you can gain commitment from your political and
community leaders, and help your community organize itself to face a particular
health issue.
Advocacy involves the selection and organization of information to make sure that
your argument is convincing. Advocacy is not just one thing or one way of doing
things; it can be delivered through a variety of interpersonal and media channels.
Advocacy also includes organizing and building alliances across a wide variety of
stakeholders.
Advocacy is strategic and it should be geared to using well-designed and organized
activities in order to influence policy or decision makers about all the important
issues that you think will affect the health of your community. This might include
a wide range of possible issues, including health policy, laws, regulations, and
programmes or funding from the public and private health sectors.
A community health advocate (or CHA) works to ensure that members of a particular
community are treated fairly and adequately in all health care matters. Community
health advocates generally work for a government agency or an independent
nonprofit organization.
Advocacy can address single or multiple health issues, during which time-limited
campaigns as well as ongoing work may be undertaken on a range of health issues.
Community advocacy efforts can be implemented on a group, local, national,
transnational basis or at all levels at the same time.
The level at which advocacy is conducted is often determined by a number of
factors, including the scope of the issue, the short term and/or long term nature of
the issue, and the availability of resources. Many issues are amenable to, but donot necessarily require, advocacy efforts at multiple levels.
a. Purpose of advocacy
The main purpose of advocacy is to bring about positive changes to the health
of your population. Sometimes advocacy will address health issues through the
implementation of a national health policy, or through the implementation of public
health policy — and it can also address health issues related to harmful traditional
practices. Moreover, advocacy could help to meet the goals of health extension
programme policies, where specific resource allocation and service delivery models
are formulated for advocacy campaigns.
Advocacy is about helping you to speak up for your community; to make sure that
the views, needs and opinions of your community are heard and understood. It
should always be an enabling process through which you, as a Health Extension
Practitioner, together with individuals, model families and others in your community
— take some action in order to assist the community to address their health needs.
Advocacy is person-centered and people-driven. It is always community-rights
based. That is to say that advocacy is dealing with what your community needs to
improve its health. You could also say that advocacy is the process of supporting
people to solve health issues. It includes single issues and time-limited campaigns,
as well as ongoing, long-term work undertaken to tackle a range of health issues
or health problems.
Remember, advocacy is your opportunity to influence polices or programs of
health. It also means putting important health problems on the agenda. Advocacy
may be able to provide a solution to specific health problems, and build support
and networks that can tackle health issues that are affecting the health of your
community
b. The goals and objectives of advocacy
The goals and objectives of advocacy are to facilitate change and the development
of new areas of policy, in order to tackle unmet health needs or deal with emerging
health needs in a given community.
Here the goal means the desired result of any advocacy activity. An advocacy goal
will usually be a long-term result, and it may take three to five years of advocacy
work to bring about the desired result. It is unlikely that your advocacy network can
achieve a goal on its own; it will probably require other allies to bring about the
required change. It is vital to know what you are trying to do before you start your
advocacy work. This involves developing a goal that applies to the situation that
needs to change.
Important points to note about goals are as follows:
• A goal is the overall purpose of a project. It is a broad statement of what you
are trying to do.
• A goal often refers to the benefit that will be felt by those affected by an issue.
• A goal is long term and gives direction — it helps you know where you are
going. It needs an accompanying route map or strategy to show you how to
get there.
• Without a goal, it is possible to lose sight of what you are trying to do.
• A goal needs to be linked to the mission and vision of your organization.
An objective is the intended impact or effect of the work you are doing, or the
specific change that you want to see. The word ‘objective’ often refers to the
desired changes in policy and practice that will be necessary to help you and your
community meet that goal. It is the most important part of your strategy, and is the
next step after developing the goal itself. It is worth spending time writing clear
objectives, because you will find you are able to write the rest of the advocacy
strategy much more clearly — and you are likely to be more effective in achieving
change.
When you set an advocacy objective, always consider or keep in mind the
resources available in your locality. It is important that an advocacy objective
identifies the specific policy body in the authority that should be approached to
fulfil the objective, as well as detailing the policy decision or action that is desired.
For example, if you want to overturn the ban on community-based distribution of
contraceptives, then the right target to direct your advocacy towards would be the
Ministry of Health.
In contrast to a goal, an advocacy objective should be achievable by the network
on its own. It is a short-term target, which means it should be achievable within the
next one or two years. The success of your advocacy objectives should always be
measured.
SMART objectives
‘SMART’ is a way of reminding you that your objectives should be:
S: Specific — by this we mean that you need to set a specific objective for each of
your health programmes.
M: Measurable — your objective should be measurable.
A: Achievable — the objective should be attainable or practicable.
R: Realistic — which also means credible.
T: Time-bound — and should be accomplished and achieved within a certain
amount of time
c. The advantages of advocacy
The success of advocacy as a method of problem solving or resolution is tied in
part to the advocates’ philosophy of searching for solutions rather than problems.
As a health worker acting as an advocate, you may be able to find ways to resolve
the community’s health-related problems. In some situations, you may have to
act as a health advocate and provide ongoing representational advocacy for your
community. Advocates should be particularly good at identifying the strengths of
their own community, and should help them find ways of solving health-related
problems.
There are several benefits of advocacy:
• Advocacy helps your community’s voice to be heard
• It provides you with information, support, and services to help you make
choices.
• It helps you to get people to understand your point of view
• Makes it easier for you to get information in a way that you can understand
• Helps you to see what other services are available
• Helps you choose what you want to do
• Helps with expressing your views effectively
• Represents your community’s views faithfully and effectively
• Helps influential people understand the issues.
d. Advocacy methods
Before starting advocacy, the community health nurse has to choose a method(s)
which will be used in order get the desired results. These methods are:
1) Lobbying, this means influencing the policy process by working closely with
key individuals in political and governmental structures, together with other
decision makers.
2) Meetings, usually it is used as part of a lobbying strategy or negotiation, to
reach a common position.
3) Project visits are another useful tool of advocacy to demonstrate good
practice and information, education and communication as various means
of sensitizing the decision makers.
4) Community organizing is another important tactic that can be used.
e. Principles of advocacy
The use of the following principles may help you to get a common understanding
and get support for your advocacy activities:• Use several tools for advocacy to reach a wide audience
• (for example, not only the public, but also officials and decision makers), and
be sure to form good relationships with your local media representatives.
• Have good relations with the private sector and all the NGOs working in the
area around you. Collaborate with them and all the people who can help your
advocacy work.
• Have good strategic planning.
• Use effective monitoring tools.
f. Approaches to advocacy
The advocacy approach uses many different methods of reaching people. Inter
personal meetings or face-to-face approaches with the decision makers are the
most effective advocacy approaches for those people. However, with the limited
availability of advocates in the field, the potential number of people reached is limited
using this form of communication, and further work like that may be expensive. As
mentioned in earlier sessions, you can also use other channels for reaching the
public, for example newsletters, flyers/leaflets, booklets, fact sheets, posters, video
and dramas.
As an advocacy coordinator, you will need support and technical assistance, and
possibly extra personnel to carry out your advocacy activities. You may need
help in the areas of identifying health issues, planning, and message or material
production. Some organizations that can help you carry out an advocacy campaign
will have expertise in conducting advocacy campaigns, or be able to help you carry
out needs assessment and issue identification. Other organizations may help with
advocacy activities such as message development and broadcast work. Some
will have expertise in audio-visual and media message production, while others
may have expertise in training field workers for developing their advocacy and
networking skills.
Here below certain advocacy approaches are described:
1) ‘‘Grassroots’’ or ‘‘bottom-up’’ approaches to advocacy are based on the
identification of needs and goals by community members themselves. It is
defined as efforts by which groups sharing a common interest are assisted
in identifying their specific needs and goals, mobilizing resources within their
communities, and in other ways taking action leading to the achievement of
the goals they have set collectively.
2) top-down models emphasize the identification of needs or goals by
experts outside of the community or by only the community leaders. These
advocates may be professional staff of non-profit organizations, or national
or international professional health organizations.
Organizing is critical to the success of advocacy efforts, whether they are
conducted from a bottom-up or top-down approach. For instance, a non-
profit or non-governmental organization that is spearheading efforts to
improve health related services in a particular locale or to prohibit smoking
must organize, at a minimum, its staff and constituents to further/promote
these goals.
3) Community organizing has been defined as ‘‘the process of organizing
people around problems or issues that are larger than group members’ own
immediate concerns’’. As such, it is relevant to bottom-up advocacy efforts.
Community readiness is a prerequisite for mobilization for a specific goal. The
stronger the community’s sense of identity, cohesion, and connectedness,
the more likely it is that the community is ready to mobilize and to address
a specific issue.
Organizing efforts using a bottom-up approach may rely on indigenous community
organizers, that is, community leaders who are able to influence and represent the
larger constituency of the community.
Other mechanisms used in bottom-up advocacy efforts include reliance on small
groups, often called the locus of change because they help to create a group
identity and a sense of purpose, and town hall meetings, which are used to inform
the relevant community and to consider a variety of solutions.
Organizing and mobilizing a community is often a cyclical process that comprises
assessment, research, action, and reflection. As an example, an advocacy group
may find that there are multiple issues to deal with and that each of these issues
falls within its mission or vision. Because each issue demands an allocation of time
and resources, it would be impossible to begin all of them simultaneously with the
same degree of attention and intensity. One option open to the organization is to
survey its membership about which issues or activities the members feel are most
critical.
Alternatively, an organization may choose to conduct a needs assessment and,
from the information gathered through this assessment, prioritize the needs to be
addressed, and the activities to be pursued.
Assessment, then, is the process by which members identify and define the
critical issues that affect their community. Although ‘‘needs assessment’’ has been
variously defined, it is frequently viewed as a systematic process that is ‘‘designed
to determine the current status and unmet needs—sometimes, both the present
and future needs—of a defined population group or geographic area with regard
to a specified program or subjects area’’. This process is often founded upon
research, which is the examination of causes and correlates of issues identified
in the assessment phase: the nature of the issue, including any barriers to access
and/or limitations of current policies and how the allocation of community resources
relates to it; political influences, how organizations or other players exercise social
power around it; and solutions.
A community needs assessment that is both valid and credible is characterized by:
1) A multidisciplinary team that includes individuals with expertise in community
assessment procedures, knowledge about strategies relevant to the issue
under study, and members of the population to be affected;
2) Broad agreement on the objectives focus, and scope of the needs
assessment;
3) A study design that uses both primary and secondary data effectively;
4) A realistic study design, time frame, and allocation of resources;
5) A process for regular reviews and input by community representatives; and
6) a plan for the utilization of the findings.
This, in turn, raises yet another issue: How do we define ‘‘need’’?
A need is a difference between ‘‘what is’’ and ‘‘what should be.’’ Some researchers
have defined need as ‘‘a gap—between the real and ideal conditions—that is both
acknowledged by community values and potentially amenable to change’’.
The values mean an idea about what is good, right, and desirable; values are
central to judgment and to behavior.
Before embarking on this process, however, it is critical that the community to be
assessed be clearly defined.
Geographical, health, social, and/or demographic characteristics may provide the
basis for this decision. The research question that the needs assessment is to
answer must then is clearly defined. These two elements will provide the basis for
the design of the needs assessment process. During the first phase of the needs
assessment process, the pre-assessment, those conducting the assessment will
conduct all preliminary planning and background research activities.
This requires the identification of the data to be collected, the sources of the data,
the methods for collecting and analyzing the data, and the use of the data after
its collection and analysis. The pre-assessment phase provides those conducting
the assessment with an opportunity to consider such key issues as the cost of
conducting the assessment; any special needs of the target population that may
have an impact on the methods to be used to collect the data, such as literacy
levels or primary language; and the timeline for completion of the assessment.
The assessment phase is the second phase of the needs assessment process.
The focus of this stage is the collection of data and its analysis. The methods
used for data collection should permit triangulation, defined as the use of different,
independent approaches to address research questions. Data collection strategies
may include, for instance, survey instruments, structured interviews, and secondary
data from existing databases. Triangulation strengthens the basis for conclusions
to be drawn from the study. The post-assessment phase is often referred to as an
action phase because it requires that the results of the data analysis be put into
action. This phase is used to determine how the information gathered through the
needs assessment process can best be put to use.
g. How to get supporters
During these activities a community health nurse need support to form an advocacy
network because of the amount of work and the number of activities that may be
involved. She/he may need help in order to design effective messages, to form a
task force, to decide the strategy, and for fundraising, as well as for calculating the
cost of the activities.
As advocator you also need to identify potential supporters. This can be achieved by
attending local events, enlisting the support of the media, holding public meetings,
and talking to all the influential people in your community. To do these things
effectively, you will also need to do a community diagnosis and get to understand
the resources in your community or locality. To get good support for advocacy
campaigns, you need to form a cooperative team for your advocacy activities, and
you need to know the stages to go through in order to achieve the best results.
It is indicated to implement the following stages in order to build the capacity of the
team which will help you in the advocacy activities. These stages are called the
stages of team growth.
• Stage 1 Team forming
When a team or network is forming, you need to explore the boundaries of
acceptable group behavior as the people change from individuals to gain member
status. At this stage, the members of the team may feel excitement, anticipation
and optimism, as well as possibly suspicion, fear and anxiety about the advocacy
activities ahead. Members attempt to define the task at hand and decide how it will
be accomplished. They also try to determine acceptable group behavior and how
to deal with group problems. Because so much is going on to distract members’
attention, the group may only make a little progress. However, be aware that a slow
start is a perfectly normal phenomenon.
• Stage 2 Storming
At the storming stage, the team members begin to realize that they do not know
the task, or may consider it is more difficult than they imagined. They may become
irritable or blameful, but are still too inexperienced to know much about decision
making. Team members argue about what actions they should take, even when
they agree on the issues facing them. Their feelings include sharp fluctuations
in attitude about the chance of success. These pressures mean that membershave little energy to spend in meeting common goals, but they are beginning to
understand each other.
• Stage 3 Norming
During the norming stage, members reconcile competing loyalties and
responsibilities. They accept the team ground rules or norms, their roles, and the
individuality of each member. Emotional conflict is reduced. There is increased
friendliness as members begin to trust one another. As members begin to work out
their differences, they have more time and energy to spend on their objectives, and
to start making significant progress.
• Stage 4 Performing
At the performing stage, members begin diagnosing and solving problems, and
implementing changes. They have accepted each other’s strengths and weaknesses
and learnt their roles. They become satisfied with the team’s progress and feel a
close attachment to one another. The team or network is now an effective support,
and ready to help you in your health advocacy work.
h. The role of community advocator
The main role in advocacy will be to secure the resources necessary to meet
the health needs of the communities. To do this effectively requires, undertaking
several key tasks, such as understanding the health needs of the communities and
identifying the government officials and stakeholders with the power to determine
health policy. The advocator also needs to be able to identify fundamental barriers
and their solutions as well as identify the main problems or issues to be addressed.
There is also a need to develop effective messages. So find a support group, or
form a network and collaborate with them. To do this you need to develop your
advocacy leadership skills.
i. Advocacy strategies
Advocacy requires action, which requires that the social power of the organizations
be exercised through public events that are intended and formulated to demonstrate
that power. Multiple strategies through which that power can be exercised and
demonstrated include advocacy through media, through courts, through legislative
bodies, and through regulatory processes.
1) Advocating through the media
Media advocacy, one of the most common advocacy strategies used to advocate
on health-related issues, requires the identification of issues and concerns
related to the community wellbeing, an emphasis on the broader context of those
concerns, the maintenance of media attention to those concerns, and the provision
of ‘‘entertainment’’ to the audience hearing of those concerns.The issues that provide the focus of the media advocacy must be appropriately
framed using sound bites, which are brief, quotable statements; visual images; and
social math, which explains statistical data while placing it in a relevant context.
Various strategies can be used to prepare for contact with the media including:
• The development of a Fact Sheet, that briefly conveys the message to be
made;
• A Source List or roster of people who are available to speak competently on
the issue to be discussed;
• Talking Points, which is a listing of the main messages to be conveyed;
• A Question and Answer Sheet, which addresses in question and answer
format the most commonly raised issues associated with the matter to be
discussed; and
• A Press List comprised of all media outlets in a specific geographical area.
Press releases, meaning a written pitch for a particular issue, should be released to
all media contact. The press release consists of no more than one page and includes
the name and contact information of the media contact person on a particular issue.
Other strategies that can be used to engage the media include letters to the editors
of newspapers and journals, op-ed columns, interviews with reporters, the staging
of media events, paid advertising, and public service announcements.
2) Using the courts
The courts system provides yet another avenue for advocacy efforts. The process
of filing a lawsuit (claim) differs across countries. The system in use in the USA is
used as an example here because it may be relevant in an international, as well
as national, context, as exemplified by the following situation. In 1996, after an
outbreak of meningitis in Kano, Nigeria that resulted in 109 580 cases of illness
and 11 717 deaths, the international pharmaceutical company Pfizer provided
supplies, medical staff, and ‘‘treatment.’’ This ‘‘treatment,’’ however, consisted of
Trovan (trovafloxacin), an experimental drug for the treatment of meningitis. After
the departure of Pfizer’s personnel from Kano, local residents reported severe
health problems. Investigations conducted by news reporters raised questions
about the validity of company research documents, the apparent lack of oversight
and approval of research procedures, and the failure to give effective treatment
to ill people. In August 2001, the families of the children who were given Trovan
(trovafloxacin) in Kano brought a lawsuit in US courts, alleging that Pfizer had
violated international and national laws in carrying out its research with Trovan.
This advocacy effort represented the first lawsuit in US history of non-US residents
bringing a lawsuit against a private corporation for wrongful experimentation in
violation of US and international law. In this lawsuit against Pfizer, the families of
the children claiming injury or harm to the children by Pfizer (plaintiffs) started their lawsuit through the filing in court of a complaint, which states the nature of the claim
that one party is bringing against another, the facts to support the claim, and the
amount in controversy. The defendant Pfizer (the party being sued) was served
with a copy of the complaint, together with a summons. The summons indicated
that the defendant was required to respond to the complaint in a specified period
of time or the plaintiff will win the lawsuit by default. The defendant must, in some
way, respond to the complaint. Each allegation/accusation in the complaint may be
admitted or denied or the plaintiff may plead ignorance. Pfizer also had the option
of filing a countersuit, that is, a lawsuit against the plaintiff or another third party.
Alternatively, Pfizer could have sought dismissal of the plaintiff’s lawsuit, claiming
that the court has no jurisdiction (authority to hear the case) or that the plaintiff
failed to state a cause of action. In fact, Pfizer actually did attempt to have the court
dismiss the lawsuit. After the filing of the lawsuit and the answer by the defendant,
the plaintiff and defendant will have a period of discovery, during which they will
each have an opportunity to discover facts about the other side’s case, the identity
of expert witness being used by the other side, and weaknesses in the other side’s
case. The forms of discovery that are most commonly used in cases involving
advocacy efforts include depositions, the questioning under oath of individuals who
will be testifying for the other party, including that party; a request for the production
of documents, so that one side can review documents it deems relevant but that
are in possession of the other party; a request for a mental or physical examination,
such as when members of a community might be claiming that they have been
injured by a toxic exposure; and a request for admissions.
3) Legislative and regulatory advocacy
Regulatory and legislative advocacy are strategies that are often used by
organizations seeking to have their voices heard. Although the specific procedures
vary depending upon the legal jurisdiction, the strategies are common across
countries. As an example, in Australia, the Coalition on Food Advertising to Children
is seeking more severe protection of children from food advertising. In Ireland, the
Broadcasting Commission of Ireland is seeking consultation from interested entities
in the development of an advertising code that will provide additional protections for
children. In the USA, the National Association of Social Workers has been engaging
in regulatory and legislative advocacy in an attempt to establish parity for mental
health care and to promote child welfare.
4) Using coalitions
Regardless of which strategies are ultimately used, the development of a coalition
may be critical to the success of the advocacy effort. ‘‘Coalitions are sets of groups
with a shared goal and some awareness that ‘united we stand, divided we fall’’’.
Accordingly, coalitions may consist of groups of community members, groupsof organizations, or both. Groups participating in a coalition must have a shared
vision and mission, or intentionality that is clear to all of the participants and that
is directly related to their goals and objectives. Organizations participating in the
coalitions must have the structure or organizational capacity that will support such
efforts, that is, the staff, volunteers, task forces, membership, and leadership, as
well as a clear allocation of roles and responsibilities. Technical assistance, such
as consultation, training, and support for advocacy efforts, may be necessary to
enable organizations to build and participate in coalitions.
j. Evaluation of advocacy efforts
A formative evaluation, also known as formative research, is conducted at the
beginning of a program and focuses on research that must be done to develop
a program or intervention. The focus of a process evaluation is to examine the
procedures and tasks involved in implementing an effort or program. In contrast,
an outcome evaluation focuses on an examination of the value of the program or
effort and whether short term objectives have been achieved. An impact evaluation
focuses on an examination of whether long term change has resulted from the
program or effort; this is the most comprehensive type of evaluation effort. The
data that are used in an evaluation may be qualitative, resulting from ‘‘nonnumeric”
observations collected systematically through established social science methods,’’
or quantitative, meaning ‘‘numeric variables which are either discrete or continuous’’
k. Challenges in advocating for health
Community health advocates may encounter significant obstacles in attempting to
effectuate their goals. One of the major challenges of community health advocacy
is finding a way to engage the public in a specific issue. Mothers Against Drunk
Driving (MADD) in the USA has been notably successful in engaging the media,
the public, and legislators in its campaigns to eliminate plea bargaining for drunken
driving offences, institute mandatory jail sentences for drunk driving, reclassify
alcohol related injuries and death accidents to felonies (major crimes), institute
‘‘dram shop’’ laws holding proprietors of restaurants and bars liable for accidents
resulting from serving alcohol to excess, and increase the minimum legal drinking
age. To MADD’s successes are attributable to a number of factors.
In addition to difficulties that may be encountered in garnering understanding and
support for a particular position, community health advocates may face additional
barriers and attacks on a systemic level. The difficulties encountered by Brazil
exemplify the types of obstacles that may confront advocates in the political and
legal domains. As an example, Brazil was forced to defend against a complaint
filed against it by the USA, which claimed that Brazil’s efforts to make antiretroviral
drugs more widely available to HIV infected people in that country through its
patent laws discriminated against US imports of antiretroviral drugs. The World
Trade Organization ultimately commissioned a legal dispute panel in an attempt toresolve the grievance
Self-assessment 5.4.2
1) Describe briefly the approaches to advocacy
2) Discuss the advocacy strategies.3) Identify the advocacy principles
5.4.3. Home based car
Learning activity 5.4.3
Using internet and Community Health Nursing Textbooks; read about Home
Based Care and respond to the following questions:
1) What is the meaning of home-based care?
2) Who needs home based care?
3) Who may be in-charge for providing home-based care?
4) Discuss the principles and objectives of home-based care?5) Discuss the types of home-based care?
Home care is defined as the provision of health services by formal and informal
caregivers in the home in order to promote, restore and maintain a person’s
maximum level of comfort, function and health including care towards a dignified
death.
Home care services can be classified into preventive, promotive, therapeutic,
rehabilitative, long-term maintenance and palliative care categories.
It is an integral part of community-based care. Community-based care is the care
that the consumer can access nearest to home, which encourages participation by
people, responds to the needs of people, encourages traditional community life and
creates responsibilities.
HBC is also defined as any professional care given to sick people in their homes,
which includes physical, psychosocial, palliative, and spiritual activities.
a. Who needs home based care?
Home based cares are services that may be provided to:
Health people, someone who is aging and needs assistance to live independently;
or managing a chronic health issue; recovering from a medical condition in need
of assistance e.g. post deliveries or after specific treatment.; at risk people with
moderate to severe functional disabilities. It includes also terminally ill persons;
persons living with HIV/AIDS or any other debilitating disease and/or conditions
e.g. mental illness, substance abusers; any other disadvantaged group/person in
need of such care e.g. people in crisis.
b. Who are the caregivers?
Families; caregivers from the formal system e.g. professionals like nurses,
physicians, therapists; caregivers from the non-formal system e.g. NGOs; caregivers
from the informal system e.g. community health worker (CHW), volunteers, other
community caregivers and church groups provide short-term or long-term care in
the home, depending on a person’s needs.
c. Principles of home-based care and community-based care
Home-based care and community-based care are:
• Holistic: they involve together physical, social, emotional, economic and
spiritual aspects. Community needs, to be addressed, but integrated into
existing systems.
• Person- centered: the provision of care should be sensitive to culture,
religion and value systems to respect privacy and dignity (community-driven,
customer-centered).
• Comprehensive, interdepartmental and all-encompassing; preventative,
promotive, therapeutic, rehabilitative and palliative (multi-sectoral
involvement).
• Empowering and allows capacity building to promote the autonomy and
functional independence of the individual and the family or caregivers.
Leadership is from within the community.
• Ensure access to comprehensive support services.
• Cover total lifespan.
• Sustainable and cost-effective resource responsibilities to be identified and
shared.
• Promote and ensure quality of care, safety, commitment, cooperation and
collaboration.
• Allow choice and control over to what extent partners will participate.
• Recognize diversity.
• Promote and protect equal opportunities, rights and independent living.
• Specific in what needs to be done and achieved.
• Focus on a basic and essential component of PHC.
• Adhere to a basic principle in health care and development, namely community
involvement.
d. Purposes
Community-Based Care (CBC) provides complete quality health services at home
and in communities to help restore and maintain people’s health standards and a
way of living by providing health services, supported self-care and health education
at home.
e. Goals and objectives of home-based care
• To move the emphasis of care to the beneficiaries (care are given in the
comfort and familiarity of home, in the community)
• To ensure access to care and follow-up through a functional referral system.
• To integrate a comprehensive care plan into the informal, non-formal and
formal health system.
• To empower the family and/or community to take care of their own health.
• To empower the client, the caregivers and the community through appropriate
targeted education and training.
• To reduce unnecessary visits and admissions to health facilities.
• To eliminate duplication of activities and enhance cost-effective planning and
delivering of services.
• Be pro-active in approach
f. Advantages of the home-based care and community-based care
• Reduce the pressure on hospital beds and other resources at different levels
of service.
• Reduce and share the cost of care within the system.
• Feelings of ownership and accountability are evoked.
• Allow people to spend their days in familiar surroundings and reduce isolation.
• Enable family members to gain access to support services.
• Promote a holistic approach to care and ensure that health needs are met.
• Create awareness of health in the community
• Bring care providers in touch with potential beneficiaries.
• Intervention is pro-active rather than reactive.
• Right to decide about care within own environment.
• Commonly occurring diseases/conditions can be effectively managed at
home.
• Promotes job creation especially in non-formal system.
• Decision making is inclusive
• Beneficial to family and friends as it allows more direct time with clients and
involvement in care giving
• Care will be individualistic and person centered.
• Avoid unnecessary referrals to and from higher levels.
• Avoid unnecessary and/or prolonged admission to health care facilities or
institutions.
• Ensure that partners in caregiving know and play their roles to avoid
duplication.
• Ensure that caregivers and all key role players are well informed
(knowledgeable), received adequate skills training and utilize other partners
in care.
• Caregivers are fully involved and informed about the individual care plans.
• Ensure adequate documentation and encourage proper use of recorded
information.
• Ensure continuity and consistency in service, quality assurance and
management.
g. Challenges of home-based care
While providing home-based care some caregivers or clients may have some of the
following challenging problems which may be a barrier to an appropriate provision
of care.
• Social environment is restricted because of a set believes and customs,
ideologies and local conflicts, inappropriate housing.
• Caregivers may experience emotional and physical strain and stress.
• Caregivers and clients may lack sufficient empowerment regarding care or
resources and diagnosis.
• Uncertainty about the duration of the situation.
• Inadequate support structures for the caregiver.
• Social isolation, related to confinement of the person to bed and the home.
• Emotions such as rejection, anger and grieving.
• Economic constraints and exhaustive care needs.
• Focus too often on health service activities only – no common vision.
• Fear or mistrust of the primary caregivers.
• Barriers to access-built environment, communication and information.
• Poor resource allocation, e.g., respite centers/care, equipment.
• Lack of and confusion around volunteerism.
• Negative past experiences.• Programs are not community driven and fragmented.
• Emphasis on “sick” role and “disabilities” rather than on “quality of life” and
“abilities”.
• Self-neglect - often refusal of intervention/care.
• Level of readiness of communities to accept their roles and functions.
• The concept of partnerships is misunderstood e.g., government is the one
and only provider.
• Confidentiality of diagnosis - unwillingness to disclose.
• HIV/AIDS epidemic may decrease caregiver pool
h. Types of Home-Based Care
a) Personal care and companionship
Those are the care related to help with everyday activities like bathing and dressing,
meal preparation, and household tasks to enable independence and safety. Those
cares are also known as non-medical care, home health aide services, senior
care, homemaker care, assistive care, or companion care.
It may include but not limited to the following:
• Assistance with self-care, such as grooming, bathing, dressing, and using the
toilet,
• Enabling safety at home by assisting with ambulation, transfer (e.g., from bed
to wheelchair, wheelchair to toilet), and fall prevention,
• Assistance with meal planning and preparation, light housekeeping, laundry,
medication reminders, and escorting to appointments,
• Companionship and engaging in hobbies and activities,
• Supervision for someone with dementia or Alzheimer’s disease
• Personal care and companionship does not need to be prescribed by a doctor.
They are the cares provided on an ongoing basis on a schedule that meets
a client’s needs.
b) Private Duty Nursing Care
This type of care includes long-term, hourly nursing care at home for adults
with a chronic illness, injury, or disability. They are also known as home-based
skilled nursing, long-term nursing care, catastrophic care, tracheostomy care,
ventilator care, nursing care, shift nursing, hourly nursing, or adult nursing
Examples of Private Duty Nursing Care services:
• Care for diseases and conditions such as Traumatic brain injury and /or Spinal
cord injury
• Ventilator care
• Tracheostomy care
• Monitoring vital signs
• Administering medications
• Ostomy/gastrostomy care
• Feeding tube care
• Catheter care
Private duty nursing care needs to be prescribed by a professional health care
specialized in the concerned domain. Those are the cares which should be provided
and monitored every day 24 hours over 24 hours.
c) Home Health Care services
They are short-term, physician-directed care designed to help a patient to prevent or
to recover from an illness, injury, or hospital stay. They are also known as Medicare
certified home health care, intermittent skilled care, or visiting nurse services. They
may include:
• Short-term nursing services
• Physical therapy
• Occupational therapy
• Speech language pathology
• Medical social work
• Home health aide services
Home health care needs to be prescribed by a professional health care specialized
in the concerned domain. The care is provided through visits from specialized
clinicians or other health care provider specialized in the related domain, on a
short-term basis until individual goals are met
Self-assessment 5.4.3
1) Identify people who need home based care?
2) Describe the types of home-based care.3) What are the principles of home-based care and community-based care
End unit assessment 5
1) Geopolitical communities are defined or formed by:
a. Natural and/or manmade boundaries
b. A group perspective or identity based on culture
c. A group specifically to address a common need
d. Are subgroups or subpopulations that have some common characteristics
2) Primary prevention:
a. Relates to activities directed at preventing a problem before it occurs
b. Is implemented after a problem has begun, but before signs and symptoms
appear
c. Focuses on limitation of disability and rehabilitation
d. Refers to early detection and prompt intervention during the period of early
disease pathogenesis
3) The objectives of community health nursing include the following, except:
a. To assess the need and priorities of vulnerable group like pregnant mother,
children and old age persons;
b. To provide health care services at every level of community including
health education, immunization,
c. To prevent and control communicable and non-communicable diseases
d. To deliver health services as determined by the private stakeholders
4) The principles of community health nursing include the following, EXCEPT:
a. The health workers should be elected by the multidisciplinary health care
team.
b. Health services should be based on the needs of individuals and the
community.
c. Health services should be suitable to the budget; workers and the resources.
d. Family should be recognized as a unit and the health services should be
provided to its members.
5) The types of Community Needs Assessment are identified here below,
EXCEPT:
a. Familiarization or Windshield Survey
b. Problem-Oriented Assessment
c. Community Subsystem Assessment
d. Geographic Information System Analysis6) The following examples describe someone who is physically unhealthy,
EXCEPT:
a. A person who has been harmed due to a car accident.
b. A farmer infected by malaria and unable to do their farming duties.
c. A person who has an inability of rational and logical decision-making.
d. A person infected by tuberculosis and unable to perform his or her tasks.
7) ____________ is one of the characteristics of the person who is
psychologically healthy
a. Having a memory and being able to reason rationally and solve problems,
b. Going to a football match or involvement in a community meeting,
c. Celebrating traditional festivals within your community,
d. Having an ability to perform routine tasks without any physical restriction,
8) Which of the following activities should be considered as secondary
prevention?
a. Preventing an established disease such as hypertension from becoming
worse
b. Breast self-examination for early diagnosis and prompt treatment of cancer
c. Distributing insecticide treated bed nets to prevent people from getting
infected with malaria
d. Immunizing less than five years children against an infectious disease like
Tuberculosis
9) ___________________is an interactive process in which learners share
their ideas, thoughts, questions, and answers in a group setting with a
facilitator.
a. Demonstration
b. Role play
c. Discussion
d. Lecture
10) Which one of the following teaching methods is more appropriate for
teaching the diabetic patient a skill like “injecting insulin?”
a. Brainstorming
b. Discussion
c. Interactive presentationd. Demonstration
11) As a facilitator who is introducing a teaching session using an interactive
presentation (illustrated lecture) as teaching method, the first step to
consider is the following:
a. Relate the content to previously covered and related topics.
b. State the objective(s) of the presentation.
c. Provide an opportunity for asking questions.
d. Use visual materials to illustrate and support the main points.
12) Deliberate on the confirmations given below. What is real about the writing
board as a teaching / learning material?
a. When using the writing board, the text and drawings should be little enough.
b. The facilitator (health educator) should talk while facing the writing board.
c. The board can be used to document ideas during discussions or
brainstorming exercises.
d. The writing boards are expensive and require more electricity for displaying
information.
13) The following affirmations are true about flipchart, EXCEPT:
a. The flipchart may be used to note objectives or outcomes before or after
clinical practice sessions.
b. The pages of information can be prepared in advance and revealed at
appropriate points in the presentation.
c. When you use the flip chart in health education you must discuss each
page completely before you turn to the next.
d. The teacher should use the same colored pens to provide contrast for
making the flipchart page attractive.
14) Among the options presented below, what the health educator / teacher
should do when preparing computer generated slides?
I. Limit the information on each slide to one idea that can be grasped in 5-10
seconds.
II. Use about six to eight bullets per slide and limit a bulleted item to three to
five words.
III. Use no more than seven lines of text per each slide.
IV. Use several typefaces (fonts) per slide to emphasize points.
a. I and III
b. I and IV only
c. II and IVd. II and III only
15) The following are the instructions for health educator/teacher, who is using
a slide projector, excluding:
a. Making sure that there is nothing between the projector and the screen so
that all learners can see.
b. Setting up and testing the slide projector and computer before the learners
are present.
c. Rushing through a series of slides for allowing learners enough time to
study during presentation.
d. Allowing plenty of time for the learners to read what is on the screen and
take notes, if necessary.
16) The assertions mentioned below are TRUE about videos as health
education material, with the exception of one of them. Which one?
a. Commercially developed videos are often outdated and may show
techniques that are inconsistent with currently approved practices.
b. Preferably, using one long video should be encouraged rather than several
short video segments with pauses in between for explanation or discussion.
c. The teacher should preview the videotape to ensure that it is appropriate
for the learners and consistent with the course objectives.
d. The teacher should make sure that the information presented in the video
is up-date with current practices and standards.
17) Decide which one of the following declarations is TRUE about the role
play?
a. The clinical demonstration role play is similar to the informal role play, and
often occurs as part of a coaching session.
b. In informal role play, the teachers give the role players a set of instructions
that outline the scope and sequence of the role play.
c. Clinical demonstration role play is often part of a clinical simulation. It
typically uses an anatomic model, simulated patient, or real patient,
d. In formal role play, the teacher gives the role players a general situation
and asks them to “act it out” with little or no preparation time.
18) The following are classified as traditional means of communication,
EXCEPT:
a. Lecture and discussion,
b. Poems and stories,
c. Songs and dances,d. Games and fables.
19) Tips for a better use of a flipchart are the following EXCEPT:
a. Leave plenty of white space, and avoid putting too much information on
one page.
b. Print in block letters using wide-tipped pens or markers.
c. Use different colored pens to provide contrast, and use headings, boxes,
cartoons, and borders to improve the appearance of the page.
d. Face the learners, not the flipchart, while talking.
e. When you finish with a flipchart page give it to the group for better
understanding.
20) Explain any 4 characteristics of community health nursing
21) Discuss the responsibilities of an ASM (Agent de Santé Maternelle).
22) Discuss the challenges faced by Rwanda community health program
23) Explain any 5 important characteristics of a community
24) Characterize the different types of a community
25) Describe the factors affecting community health
26) Discuss any four Characteristics of a Healthy Community
27) Outline the required steps in conducting community health needs
assessment?
28) Describe the methods used for conducting an advocacy for a community.
29) You are appointed to do advocacy for the people living near Kabeza
industrial zone because of toxic waste coming from the industries.
Describe any two advocacy approaches to be used.
30) Outline the principles of home-based care
31) Explain the types of Home Based Care
32) Identify any 4 factors that contributed to the decline in infectious disease–
related deaths during the nineteenth and early twentieth centuries.
