UNIT4:NURSING ASSESSMENT OF SENSORY SYSTEM
Key Unit Competence
Take appropriate action based on findings of nursing assessment of Sensorysystem
Introductory activity 4
1) How many images do you see in the picture A? List them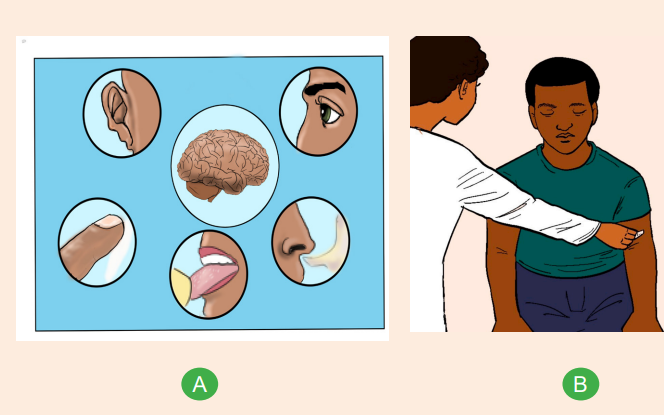
2) What is the role of each image in the picture A?
3) Which relationship between the image in the center of picture A and the
surrounding images?
4) Which image in picture A corresponding to the action of nurse in picture B
A sensory system is a part of the nervous system consisting of sensory receptors
that receive stimuli from the internal and external environment, neural pathways
that conduct this information to the brain and parts of the brain that processes this
information. We have 5 senses (vision, hearing and equilibrium, taste, smell, touch)and related sensory organs (eye, ear, tongue, nose and skin)
4.1. Specific history taking on sensory system
Learning activity 4.1
Observe the image above and respond to the following question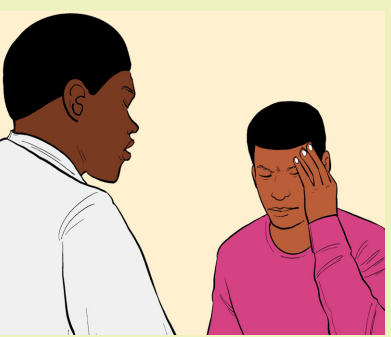
1) Describe people presented on the above figure.
2) What may be wrong with a person touching his head?
3) Enumerate the steps of a patient- health professional interaction duringconsultation
4.1.1. Assessment of the head
In clinical settings, health assessment of a patient is made of history taking and
physical examination. It is up to clinicians to develop empathetic listening, ability
to interview patients of all age, technique to assess different body part and ability
to sum up the information obtained to identify the patient’s health problem. A well
done health history should follow a chronological order as follow: identifying data,
chief complaints, history of presenting illness, past health related history, family
history, personal and social history and review of systems.
Usually, the assessment of the head goes together with the neck as the share
together the important structures such as cranial nerves, sensory organs and major
blood vessels. Headache is a very common symptom presented by patient during
the assessment of the head. Other common symptoms the head and neck are
change or loss of vision, eye pain, redness, tearing, double vision, hearing loss,
earache, ringing in the ears, dizziness, vertigo, nosebleed, Sore throat, hoarseness,swollen cervical glands and enlarged thyroid gland.
Headache is defined as the pain in any region of the head. A patient complaining
about headache will be asked to clarify on its location, severity, character,
circumstances in which it occurs, remitting or exacerbating factors, associated
manifestations and duration. Headache is subdivided into two main categories
which are primary headache and secondary headache. The primary headache is
said when it comes by its own, not a symptom of any diseases whereas secondary
headache happens as a symptom to an underling medical condition. In fact, primary
headache originates from over-activity of the structures of the head and the neck
such as nerves, muscles, blood vessels and specific areas of the brain. The causes
of secondary headache may be pregnancy, stroke, brain tumor, hypothyroidism
and systemic infections. If a patient is complaining about headaches, we have to be
careful and collect detailed information because it may be a sign of a very serious
health conditions. Migraine is a form of on side headache with a severe pulsating
sensation. Other types of primary headache include cluster, tension and chronic
daily headache. A headache which is severe, persistent, occur regularly, does
not improve with medication, accompanied with other clinical manifestations such
as fever, confusion, sensory changes and neck stiffness need to seek for medicalattention
Interview guide when taking history of the head
• Ask the patient to allocate the area of pain or discomfort. Location and
radiation patterns will allow the examiner to classify and to guide his or her
diagnosis
• Is the headache severe and of slow or sudden onset? Guide the patient to
rate the pain by explaining the rational of pain score from 0 to 10.
• How long does it last?
• Is it episodic? Does the headache recur at the same time every day?
• Chronic and recurring? Is there a recent change in pattern?
• Any associate factors such as nausea, vomiting, fever, confusion and so on?
Nausea and vomiting are common in migraine but may be seen in brain tumor
and subarachnoid hemorrhage.
• Ask about any unusual feeling before the occurrence of a headache.
Weakness, dizziness, vision changes are some of the preliminary signs for
some form of headache.
• Get to know about aggravating and alleviating factors. Sneezing, coughing,
changing position may aggravate headache in case of acute sinusitis.
– Ask about personal means to manage the headache. If a patient is using
medications for more than 2 days a week as a symptomatic treatment of a
chronic headache, consider this situation as medication overuse.
Family history is another important key to ask for to compare the patient’s
situation to his or her family member. Migraine is a good example of headachethat runs in families.
The physical assessment of the head involves the inspection and palpation of the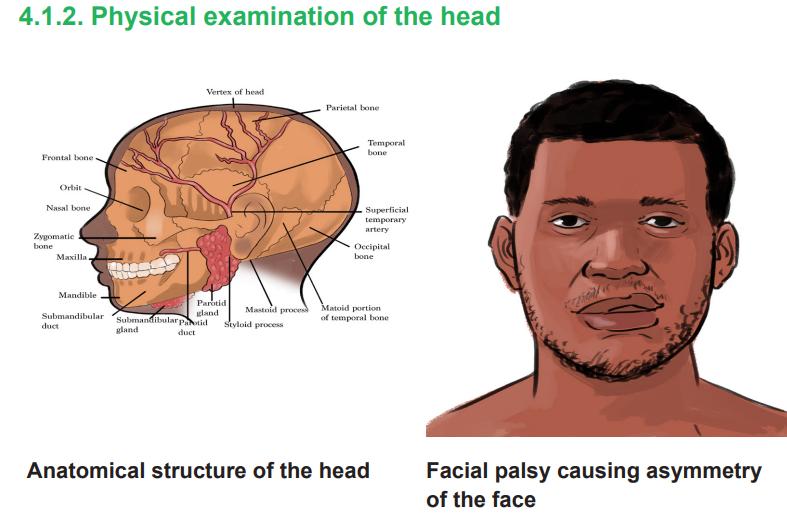
parts of the head which in turn are named in accordance to the bone of the skull.
We also assess the salivary glands: a pair of parotid glands located superficial
to behind the mandible and submandibular sited deep to the mandible. The
assessment of the head includes palpation of superficial temporal artery passing in
front of the ear, it is easily identified to its pulsation.
To assess the head, we systematically follow this order: hair, scalp, skull, face
and the skin. Remember to always ask the patient to remove head covers and
hair pieces should be removed. You may note movable fragments of dandruff.
Fine hair is observable during hyperthyroidism whereas coarse hair is seen during
hypothyroidism. The tiny ovoid granules adhere to the hair may be lice eggs. For
the scalp, displace the hair in several directions and search for scars, lumps, nevi
and any other particularity. The redness and scaling may suggest seborrheic
dermatitis or psoriasis whereas nevi that raises indicate melanoma. On the skull,
observe the contour and its size. Microcephaly is an abnormally small head while
macrocephaly is an abnormally large head. Consider any deformity, depression,
lump or tenderness. Get to know normal irregularity of the skull such presence of
fontanelles and sutures in infancy. The enlarged skull indicates hydrocephalus orPaget disease of the bone. Tenderness while palpating the skull suggests possible
trauma. For the face, check for patient’s facial expression and contour. Note any
identified asymmetry, involuntary movement, edema and mases. Look at the skin
of the face and the head to objectivate any change in color, texture, thickness, hairdistribution and lesions.
Self-assessment 4.1
1) What are the physical assessment techniques used to assess the head?
2) Name possible abnormalities which can be seen on the face during
physical examination.
3) Conduct an history taking for a patient complaining about a headache.
4) Mr. M was riding a bicycle, abruptly he loses control and hits the border
of the road. His neighbor took him to the nearest health center. During a
complete physical assessment, the nurse realizes tenderness on the left
parietal region.
a. What does tenderness mean?
b. Briefly list other important point to be assessed on the head.
5) An 18-year-old male college student wake up this morning complain
about headache, weakness and perspiration which prevent him to attend
class today. We took him to the school clinic for treatment, the nurse
conducted an assessment and blood smear collection and realize that
these symptoms are linked to malaria. She then provided a dose of
analgesic and anti-malarial medication.
a. Which type of headache is appropriate for the above situation?
b. What are the possible causes of a headache depending on their types?
c. What will be your focal points when conducting an interview for someonewith a headache?
4.2. Assessment of the eye
Learning activity 4.2
Observe image A, B and C and respond the following question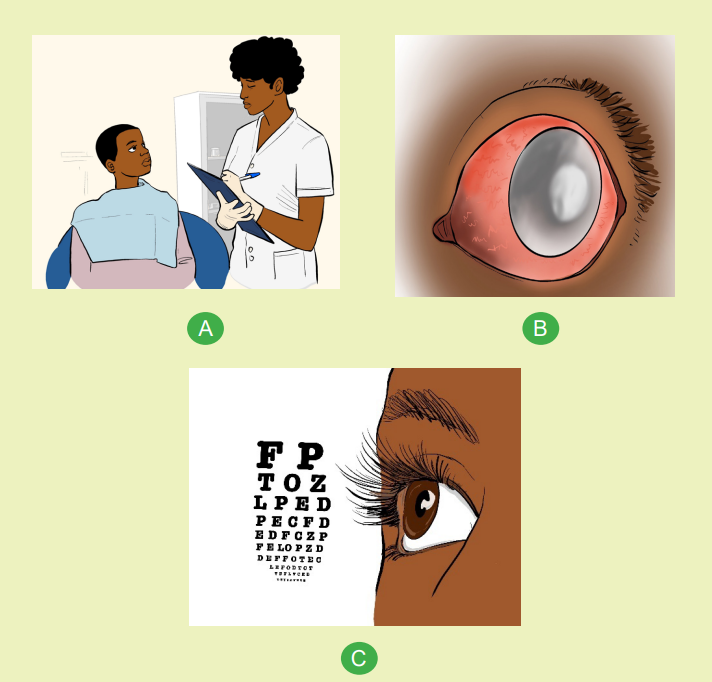
1) Describe the images A, B and C
2) Compare the eyes seen on the image B and C3) What is the meaning of the letters illustrated on the picture C?
4.2.1. Overview of the assessment of the eye
The eye is our organ of sight. The visual system consists of the external tissues and
structures surrounding the eye, the external and internal structures of the eye, the
refractive media, and the visual pathway. The external structures are the eyebrows,
eyelids, eyelashes, lacrimal system, conjunctiva, cornea, sclera, and extraocular
muscles. The internal structures are the iris, lens, ciliary body, choroid, and retina.The entire visual system is important for visual function. Light reflected from an
object in the field of vision passes through the transparent structures of the eye
and, in doing so, is refracted (bent) so that a clear image can fall on the retina. From
the retina, the visual stimuli travel through the visual pathway to the occipital cortex,
where they are perceived as an image.
4.2.2. Taking history
An eye assessment is a series of tests performed to assess vision and ability to
focus on and discern an object. Failure to take eye history can lead to missing vision
or life-threatening conditions. The structure of ophthalmological history taking is no
different than for other systems; however, it is important to take particular note of
the following:
Demographic data: Ask patient’s name, age, sex, religion, disability, Patient’s
occupation, daily tasks and hobbies. During the initial observation, observe the
patient’s overall facial and ophthalmic appearance. The eyes should be symmetric
and normally placed on the face. The globes should not have a bulging or sunken
appearance.
Chief complaints: watering/discharge from the eyes, redness, pain, itching, burning
sensation, foreign body sensation, loss of vision, double vision or swelling of an
eyelid all are the common reasons for consultation.
History of present illness- mode of onset, Sudden or gradual. Eg: Sudden visual
loss suggests retinal detachment, vitreous hemorrhage, or occlusion of the central
retinal artery, duration, severity and progression of eye disease.
a. Past eye history
Ask for detail about any previous eye problems such as:
• History of similar eye complaints in the past. This is important in recurrent
conditions such as herpes simplex keratitis, allergic conjunctivitis, uveitis and
recurrent corneal erosions.
• History of eye surgery or trauma. It is important to ask about any ocular
surgery in the past such as cataract extraction, muscle surgery, glaucoma, or
retinal surgery
• Other symptoms. Ask whether the patient has any other specific eye
symptoms.
b. General medical history
Ask about any current and past medical conditions such as diabetes, hypertension,
arthritis, HIV, syphilis, asthma and eczema.
Family history: ask patient about familial predisposition of inheritable ocular
disorders
It is important to ask the patient whether any other member of the family has a
similar
condition or another eye disease. This can help to establish familial predisposition
of inheritable ocular disorders like glaucoma, retinoblastoma or congenital eyediseases, diabetes and hypertension
c. Medication history
Ask about present and past medications for both ocular and medical conditions as
some medications are important in the etiology of ocular conditions.
It is also helpful to ask whether the patient has been able to use the medication
as prescribed (their compliance). If a medication is ineffective, you want to know
whether the patient is actually using the medication as prescribed. find out if access
to medication prescribed is easy. Assess whether a cost or other concerns are a
potential reason for non-compliance. There could also be practical issues, such as
difficulty instilling eye drops or forgetting to do so. Do not forget to ask in a non
judgmental way about traditional/herbal medication use. Consider that many cold
preparations contain a form of epinephrine (e.g., pseudoephedrine) that can dilate
the pupil. Note the use of any antihistamine or decongestant, since these drugs
can cause ocular dryness. In addition, specifically ask whether the patient uses
any prescription drugs such as corticosteroids, thyroid medications, or agents such
as oral hypoglycemics and insulin to lower blood glucose levels. Long-term use
of corticosteroid preparations can contribute to the development of glaucoma or
cataract.
d. Other history
Ask about any allergies to medications or other substances. Social history- ask the
patient about smoking habit, illegal substances and alcohol. For children, the birth
history (prematurity) and immunization status can be important.
4.2.3. Inspection of the eye
To maintain optimum vision, people need to have their eyes examined regularly
throughout life. It is recommended that people under age 40 have their eyes
tested every 3 to 5 years, or more frequently if there is a family history of diabetes,
hypertension, blood dyscrasia, or eye disease (e.g., glaucoma). After age 40, an
eye examination is recommended every 2 years. Examination of the eyes includes
assessment of the external structures, visual acuity (the degree of detail the
eye can discern in an image), extraocular muscle movement, and visual
fields (the area an individual can see when looking straight ahead). Most eye
assessment procedures involve inspection.
Eye should be examined from outside to inside in systematic approach as follow
a. External structure inspection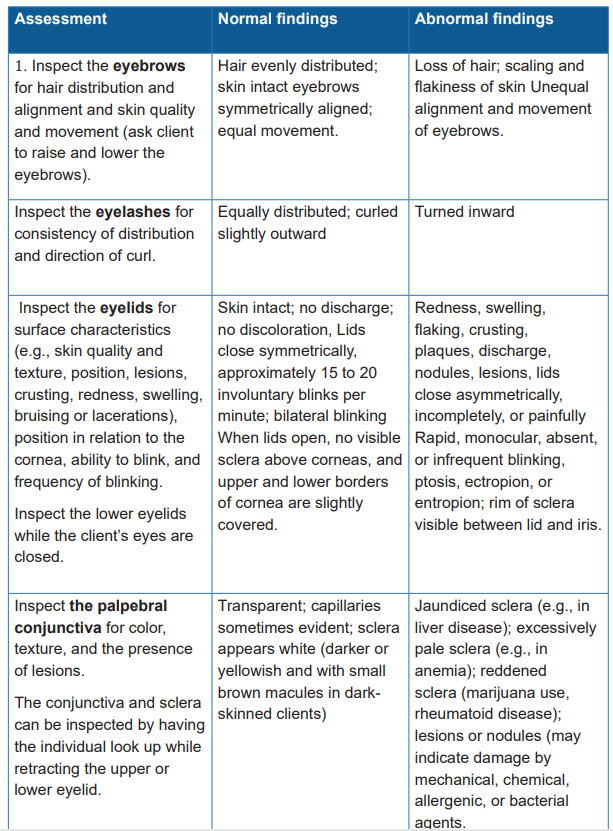
After the inspection, palpation of the orbital rim may also be desirable, depending on
the presenting signs and symptoms. The sclera and conjunctiva are the only parts
to be easily assessed. Vision tests and ophthalmoscopic test need an advanced
level of practice. Ophthalmoscope is used to examine the anterior chamber, lens,vitreous and internal surface of the retina.
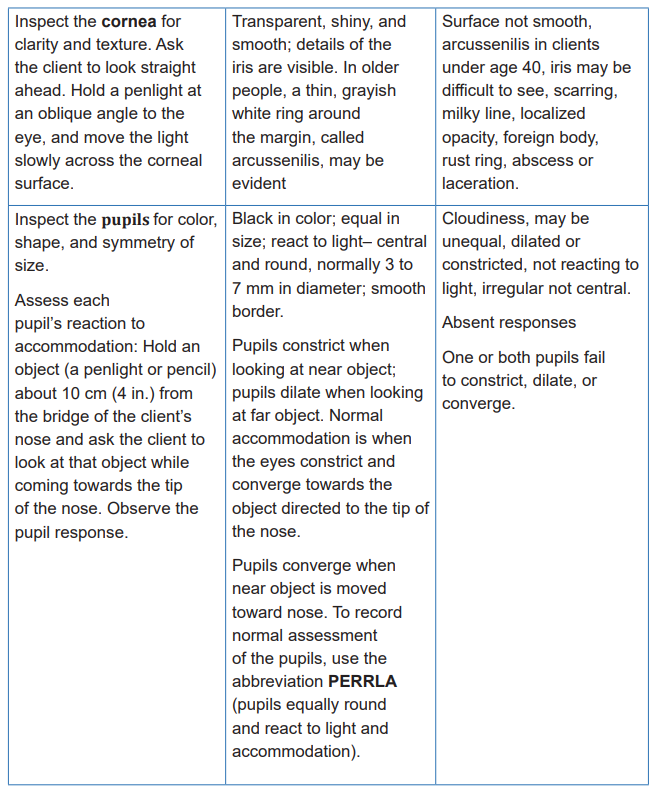
Below are the images illustrating some common features of the eyes
Table 4.2 1 Common features of the eye problems
b. . Visual acuity examination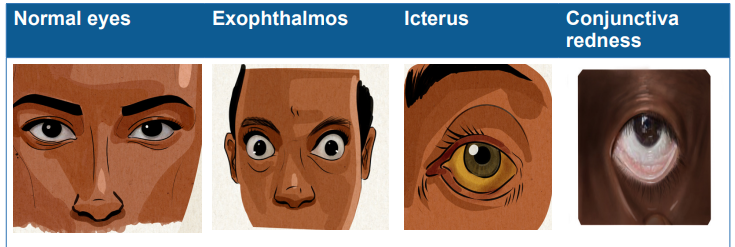
Visual acuity is the eye ability to detect fine details and is the quantitative measure
of the eye’s ability to see an in-focus image at a certain distance. The commonly
used tool for visual acuity is the Snellen Chart. Document the patient’s visual acuity
before the patient receives any ophthalmic care. Position the person on a mark
exactly 20 feet or 6 meters away from the Snellen eye chart. If the person wears
glasses or contacts, leave them on. Cover one eye at a time during the test. Ask
the person to read down the lines of the chart to the smallest line of letters possible.
Record the result using the numeric fraction at the end of the last successful line
read. Indicate whether any letters were missed and if corrective lenses were worn
(e.g., “Left eye, 20/30- 2, with contacts”). Next ask the patient to cover the other
eye, and repeat the process. Normal visual acuity is 20/20. The numerator indicates
the distance the person is standing or sitting from the chart; the denominator is
the distance at which a normal eye can read the particular line. The larger the
denominator the poorer the vision. A vision poorer than 20/30 need to be referred
to the ophthalmologist. Legal blindness is defined as the best-corrected vision inthe better eye of 20/200 or less.
Self-assessment 4.2
1) In which condition a patient may manifest yellow eyes?
a. Bacterial conjunctivitis
b. Liver diseases
c. Trauma of the eyes
d. Congenital defect of the eyes
2) The normal finding of the pupil examination is:
a. Pupil should be equal, round, reactive to light and accommodate
b. Pupil should be equal, square, reactive to light and accommodate
c. Pupil are white, dry, reactive to light and accommodate
d. Pupil is intact, pink, ovoid and reactive to light
3) Increased intraocular pressure may occur as a result of
a. Edema of the corneal stroma.
b. Dilation of the retinal arterioles.
c. Blockage of the lacrimal canals and ducts.
d. Increased production of aqueous humor by the ciliary process
4) What are the normal findings when assessing the eyebrows?
5) Which parts of the eyes can we assess by using inspection?
6) Why do we ask for other health conditions to a patient consulting for eyeproblem?
4.3. Assessment of the ear
Learning assessment 4.3
Observe the image A and B and respond the following questions
1) What is the attitude of person in image A and what do you think may be
the cause
2) Give the similarities of image A and B3) What is the name and importance of material used by Doctor in image B?
4.3.1. Overview of the assessment of the ear
The auditory system is composed of the peripheral auditory system and the central
auditory system. The peripheral system includes the structures of the ear itself: the
external, middle, and inner ear. This system is concerned with the reception and
perception of sound. The inner ear functions in hearing and balance. The central
system integrates and assigns meaning to what is heard. This system includes the
vestibulocochlear nerve (Cranial nerve 8) and the auditory cortex of the brain. The
brain and its pathways transmit and process sound and sensations that maintain
a person’s equilibrium. The role of the external and middle portion of the ear is to
conduct and amplify sound waves from the environment. This portion of sound
conduction is termed air conduction. Problems in these two parts of the ear may
cause conductive hearing loss, resulting in a decrease in sound intensity and/or a
distortion in sound. Disturbances in equilibrium can impair coordination, balance,
and orientation. Damage to or an abnormality of the inner ear or along the nerve
pathways results in sensorineural hearing loss. Sensorineural hearing loss may
affect the ability to understand speech or cause complete hearing loss. Impairment
within the auditory pathways of the brain causes central hearing loss. This type of
hearing loss causes difficulty in understanding the meaning of words that are heard.
4.3.2. History taking
An ear history taking it is done to screen for ear problems, such as hearing loss,
ear pain, discharge, lumps, or objects in the ear. These problems may be due to
infection, too much earwax, or an object like a bean or a bead.
The following issues should be included:
• Classic symptoms of ear disease: deafness, tinnitus, discharge (otorrhoea),
pain (otalgia) and vertigo.
• Previous ear surgery, or head injury.
• Family history of deafness.
• Systemic disease (eg., stroke, multiple sclerosis, cardiovascular disease).
• Ototoxic drugs (antibiotics (eg, gentamicin), diuretics, cytotoxics).
• Exposure to noise (eg, pneumatic drill or shooting).
• History of atopy and allergy in children.
4.3.3. Inspection of the ear
a. Inspecting the external ear
Inspect the external ear before examination with an otoscope/auriscope. Swab any
discharge and remove any wax. Look for obvious signs of abnormality.
• Size and shape of the pinna.
• Extra cartilage tags/pre-auricular sinuses or pits.
• Signs of trauma to the pinna.
• Suspicious skin lesions on the pinna, including neoplasia.
• Skin conditions of the pinna and external canal.
• Infection/inflammation of the external ear canal, with discharge.
• Signs/scars of previous surgeryb. Inspecting the ear canal and eardrum
The inspection of the ear canal and the tympanic membrane need anotoscope/
auriscope with its own light source to examine the ear. The examination technique
involves grasping the pinna and pulling it up and backwards (posteriorly and
superiorly), which helps to straighten the ear canal and for inspection of the tympanic
membrane. For the infants, only pull the pinna downwards and backwards to be
able to visualize into the ear. Enter the ear gently to avoid possible trauma, select a
correct size of speculum to achieve the best view and detach it from the otoscope
after examination for appropriate cleaning.
Note the condition of the canal skin, and the presence of wax, foreign tissue,
or discharge. The mobility of the eardrum can be evaluated using a pneumatic
speculum, which attaches to the otoscope. The drum should move on squeezing
the balloon.
For the inspection of the ear drum, move the otoscope in order to see several
different views of the drum. The drum is roughly circular (~1 cm in diameter).
The normal drum is translucent with light-gray color or a shiny pearly-white. The
common pathological conditions related to the ear include: perforations of the drum
(note size, site and position), tympanosclerosis, middle-ear effusion, retractions of
the drum, and hemotympanum (blood in the middle ear).
Check facial nerve function if ear pathology is serious.
4.3.4. Physical exam: Palpation
Palpate the pinna to looking for swelling or nodules and check for tenderness.
Press the tragus towards the ear canal. Palpate around the ear for pre and post
auricular, suboccipital and superior jugular lymph nodes and parotid glands.
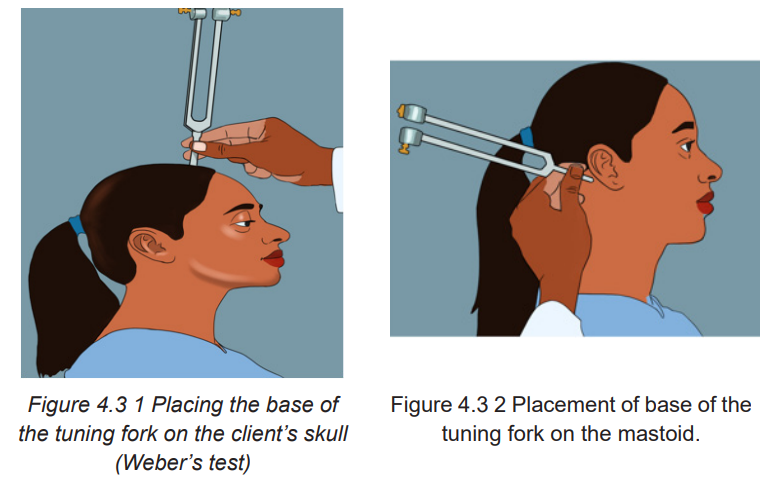
4.3.5. Basic hearing test: Tuning fork tests: Weber’s test and
Rinne’s testA patient with normal hearing should hear equally as well in both ears.
a. Weber ‘s test
This test is performed to assess bone conduction by examining the lateralization
(sideward transmission) of sounds. The vibrating fork is placed in the middle of the
forehead and the patient is asked whether any sound is heard and, if so, whether
it is equally heard in both ears or not. In a patient with normal hearing, the tone is
heard centrally (Weber negative). If the patient has unilateral hearing loss and the
sound is louder in the weaker ear, this suggests a conductive hearing loss mostly
happening in otosclerosis, otitis media, perforation of the eardrum, and cerumen. If
the sound is louder in the better ear, it is more likely to be a sensorineural hearing
loss (Weber positive). (See Figure 4.3 1)
b. Rinne’s test
Rinne’s test used to compare air conduction to bone conduction: Hold the handle of
the activated tuning fork on the mastoid process of one ear, A until the client states
that the vibration can no longer be heard. Immediately hold the still vibrating fork
prongs in front of the client’s ear canal. Making sure that it is not touching any hair.
Ask whether the client now hears the sound. Sound conducted by air is heard more
readily than sound conducted by bone. The tuning fork vibrations conducted by
air are normally heard longer. This is a positive Rinne’s test. If the Rinne’s test is
positive and there is hearing impairment, it is a sensorineural hearing loss and not
a conductive problem. If there is a negative Rinne’s test with hearing loss, then theproblem is a conductive. (See Figure 4.3 2 and Figure 4.3 3)
4.3.6. Special population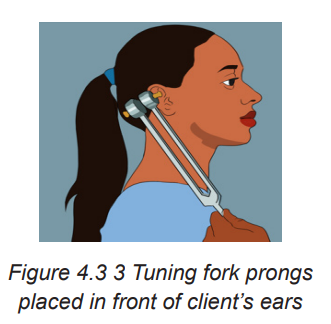
a. Infant
To assess gross hearing, ring a bell from behind the infant or have the parent call
the child’s name to check for a response. Newborns will quiet to the sound and may
open their eyes wider. By 3 to 4 months of age, the child will turn head and eyes
toward the sound.
b. Children
To inspect the external canal and tympanic membrane in children less than 3 years
old, pull the pinna down and back. Insert the speculum only 0.6 to 1.25 cm. Perform
routine hearing checks and follow up on abnormal results.
In addition to congenital or infection-related causes of hearing loss, noise-induced
hearing loss is becoming more common in adolescents and young adults as a
result of exposure to loud music and prolonged use of headsets at loud volumes.
Teach that music loud enough to prevent hearing a normal conversation can
damage hearing.
4.3.7. Identification of client’s problems
While most people know about hearing loss, many other conditions can affect the
ears too. Some are just irritating, but others can cause discomfort. What’s more,
these diseases can have a knock-on effect on your hearing or exacerbating any
existing hearing loss that you may have.
a. Hearing loss
Conductive hearing loss is the result of interrupted transmission of sound waves
through the outer and middle ear structures. Possible causes are a tear in the
tympanic membrane or an obstruction, due to swelling or other causes, in theauditory canal.
Sensorineural hearing loss is the result of damage to the inner ear, the auditory
nerve, or the hearing center in the brain.
Mixed hearing loss is a combination of conduction and sensorineural loss.
b. Otalgia (ear pain)
Pain that originates from the ear is called primary otalgia, and the most common
causes are otitis media and otitis externa. Examination of the ear usually reveals
abnormal findings in patients with primary otalgia. Pain that originates outside the ear
is called secondary otalgia, and the etiology can be difficult to establish because of
the complex innervation of the ear. The most common causes of secondary otalgia
include temporomandibular joint syndrome and dental infections because the
nerves innervating the ear have a shared distribution to include the head, neck,
chest, and abdomen. The ear is innervated by several sensory nerves. The auricle
is affected by cranial nerves V, VII, X, the external auditory meatus and canal by
cranial nerves V, VII, and X; the tympanic membrane by cranial nerves VII, IX, and
X; and the middle ear by cranial nerves V, VII, and IX. Irritation of any portion of
these nerves can result in otalgia.
Primary otalgia is more common in children, whereas secondary otalgia is more
common in adults. History and physical examination usually lead to the underlyingcause.
c. External ear problem
Among the external ear problem, atresia defined as absence or closure of
external ear canal being a birth defect, and accompanied by auricle malformation
which is characterized by Conductive hearing loss. On clinical examination, usually
the auricle is malformed and the external auditory canal is not patent or significantly
narrowed.
Necrotizing external otitis
Infection involving primarily bony and cartilaginous external auditory canal and
adjacent structures. It occurs usually in immunocompromised persons, especially
elderly patients with diabetes mellitus, and is often initiated by self-inflicted or
iatrogenic trauma to the external auditory canal. Clinically, patients complain of
severe otalgia that worsens at night, and otorrhea. Otoscopic findings include
granulation tissue in the external auditory canal, particularly at the bony-cartilaginous
junction. On audiology there is conductive hearing loss.
d. Middle ear problem
• Traumatic opacified middle ear
Trauma to the temporal bone is usually the result of a blunt head injury. Patients
with temporal bone fracture may present at the time of trauma with evidence ofbasilar skull fracture, such as battle sign, raccoon eyes, or hemotympanum. In
addition, they may complain of hearing loss or dizziness. If a temporal bone fracture
initially goes unrecognized, delayed presentation may involve cerebrospinal fluid(CSF) otorrhea, hearing loss, or symptoms related to cranial nerve VII dysfunction.
• Non-traumatic opacified middle ear: Eustachian tube dysfunction (secretory
otitis)
Persistent mucoid or serous middle ear effusion, in the absence of acute inflammation.
Eustachian tube dysfunction is well known to be related in the pathogenesis of
secretory otitis. Secretory otitis is the most common disease in children, sometime
it can be seen in adults. In children, this can occur purely from enlarged adenoids,
with no pain or bacterial infection. In adults, secretory otitis may be found when a
growing tumor in the nasopharynx blocks Eustachian tube opening.
It is manifested by fluid filling the middle ear cavity causes tympanic membrane
bulging with no signs of acute infection (redness, pain, oedema). Over time, middle
ear fluid can become very thick and glue-like (“glue ear”), which increases thelikelihood of conductive hearing loss.
• Non-traumatic opacified middle ear: acute inflammation/infection
Acute middle ear infection (acute otitis media) usually presenting with typical clinical
image and in most cases not requiring imaging.Clinical manifestation include
earache, fever, pain, otorrhea, conductive hearing loss. On otoscopy tympanic
membrane is red and bulging.Both from clinical and radiological points of view, it is
important to differentiate between acute otitis media and secretory otitis.
Secretory otitis means fluid in the middle ear cavity without signs or symptoms of
infection; this is usually caused when the Eustachian tube patency is compromised
and fluid is trapped in the middle ear. Signs and symptoms of acute otitis media
occur when effusion in the middle ear becomes infected.
• Non-traumatic opacified middle ear: chronic inflammation/infection
When the inflammation persists at least 6 weeks and is associated with otorrhea
through a perforated tympanic membrane, chronic otitis media (COM) is diagnosed.Symptoms include conductive hearing loss, sometimes pain, vertigo, otorrhea.
Self-assessment 4.3
1) Enumerate possible signs and symptoms of a patient with ear problem
2) Which interview questions will you as to a patient with otalgia?
3) Distinguish conduction hearing loss to sensorineural hearing loss.
4) Elaborate possible clinical manifestations of acute otitis media.5) Which tests used to measure hearing capacity of a patient
4.4. Assessment of the nose
Learning activity 4.4
4.4.1. Nose assessment overview
The nose is an organ for olfactory sense. Mostly, the assessment of the nose goes
together with sinuses but our emphasis will be on the nose. The most common
patients’ presenting signs and symptoms of the nose are rhinorrhea, nasal
congestion, loss of smell, pain, itching and epistaxis. Rhinorrhea is a drainage
from the nose while nasal congestion is sense of obstruction within the nose. These
two symptoms can be followed by sneezing, watery eye, throat discomfort and
itching of the eyes, nose and throat. They are caused by viral infection or rhinitis
more precisely; itching is due to allergic causes. Periodic occurrence and presence
of environmental factors of these symptoms suggest allergic rhinitis. Bleeding from
the nose known as epistaxis can be confused to the bleeding from paranasal and
nasopharynx but the latter passes in the throat and continue to the mouth or in the
esophagus.
4.4.2. History taking
To conduct patient history on the nose, here are guiding questions:
• Do symptoms occur when colds are prevalent and last for less than sevendays?
• Do the symptoms keep coming in the same period of the year (e.g: when
pollen is in the air)?
• Are symptoms triggered by a specific animal (e.g: pet) at home or environmental
exposure (e.g: dust)
• Ask about remedies, how long is it? And its effectiveness.
• Ask if any drug was used to control these symptoms.
• Get to know if nasal congestion comes after upper respiratory infection? In
this condition the patient will experience purulent nasal discharge, loss of
smell, facial pain aggravated by bending forwards, ear pressure, cough and
fever.
• Ask if the patient is taking any medication including oral contraceptives,
alcohol and cocaine
• Get to know if nasal congestion is only on one side or both. Sometimes,
deviated nasal, nasal polyp, foreign body or cancer in that area.
• In case of epistaxis, ask the patient to pinpoint the source of bleeding
and differentiate coughing of blood (hemoptysis) to vomiting of blood
(hematemesis) because they all have different causes. The local causes of
epistaxis are from trauma, inflammation, drying of nasal mucosa, tumor and
foreign body in the nose.
• Ask the patient if epistaxis is a recurrent issue, and if there is easy bruising or
bleeding elsewhere. Some medications such as anticoagulants, non-steroid
anti-inflammatory drugs as well as diseases of coagulation and vascular
diseases contribute to epistaxis.4.4.3. Physical assessment of the nose
In the normal condition the breathing process starts when air enters the anterior
naris on both sides then reaches the vestibule and continues to the pharynx and
larynx to the trachea down to the lung. The physical assessment of the nose
involves inspection and palpation. Inspect the external parts of the nose for skin
status, sign of inflammation and symmetry. Consider any asymmetry or deformity
of the nose. It is common to find a deviated lower septum and it is easily detected
during inspection. With a gentle pressure on the tip of the nose, palpate lightly in
the normal condition the nostrils will widens. In case of tenderness on the tip of the
nose, be gentle to manipulate the nose as little as possible.
To check for nasal obstruction, press the ala nasi towards the nasal septum and
ask the patient to breathe in, and repeat he same to the other side then note any
degree of obstruction. To visualize the inner parts of the nose, use an otoscope with
the largest ear speculum. Ask extend his or her neck and introduce the speculum
into the vestibule each nostril and avoid touching the sensitive nasal septum. Enterthe otoscope posteriorly then upwards in short steps to inspect the inferior and
middle turbinate and nasal septum. Normally the nasal mucosal lining the septum
and turbinate is redder than oral mucosa. During examination, indicates the color,
swelling, bleeding and exudate.
In case of exudate reports related characteristic such as clear, mucopurulent or
purulent. In viral rhinitis the mucosa will be increasingly red and swollen whereas
in allergic rhinitis the mucosa will be pale, blue or red. The epistaxis commonly
originates to the lower anterior of nasal septum, so assess for any deviation,
inflammation, perforation and ulceration. Inspect may objectivate fresh blood or
clots while septal perforation may be due to trauma, surgery and intranasal use of
cocaine or amphetamine. The latter two medications are also responsible for septal
ulceration.
The saclike growth made of inflamed tissue which inhibit normal flow of air is known
as nasal polyps sometimes are seen during inspection. Nasal polyps are identified
in case of allergic rhinitis, aspirin sensitivity, asthma and chronic sinus infection.
Rarely, the cancerous tumors found in the nasal cavity are linked to tobacco
exposure or long-term toxin inhalation.
Remember to discard or clean and disinfect used speculum appropriately as per
your institutional policy. Palpate the frontal sinuses on both sides under the bony
brows while doing so, do not apply pressure on the eyes. Palpate also the maxillary
sinuses located below the orbits downwards to the length of the nose. In case
of tenderness in these sinuses associated with facial pain, pressure or fulness,
purulent nasal discharge, nasal obstruction, smell difficulties suggest an acute
bacterial rhinosinusitis involving frontal and maxillary sinuses.Self-assessment 4.4
1) List 5 common causes of consultation of the nose
2) Which finding can we have while assessing the nose using otoscope?
3) State the questions you will ask a patient with rhinorrhea as chief
complain?4) Mention the causes of epistaxis
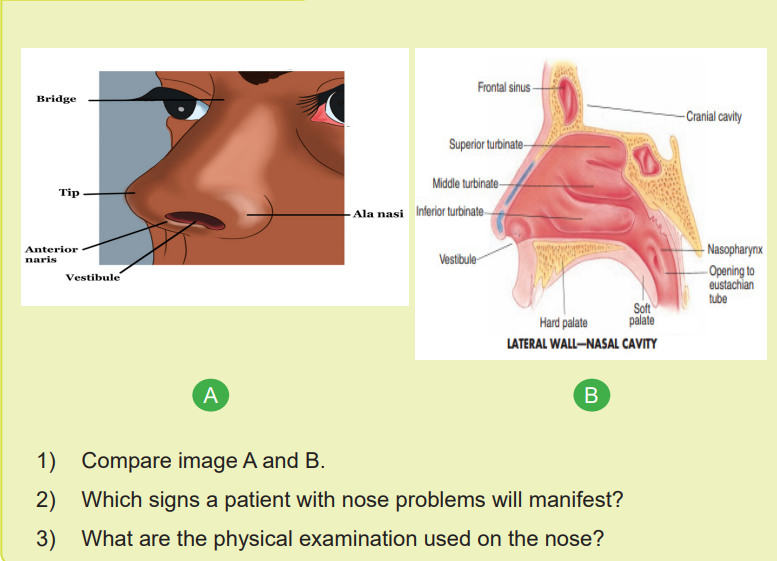
4.5. History taking of the mouth and pharynx
Learning activity 4.5
1) Which parts of the body here illustrated?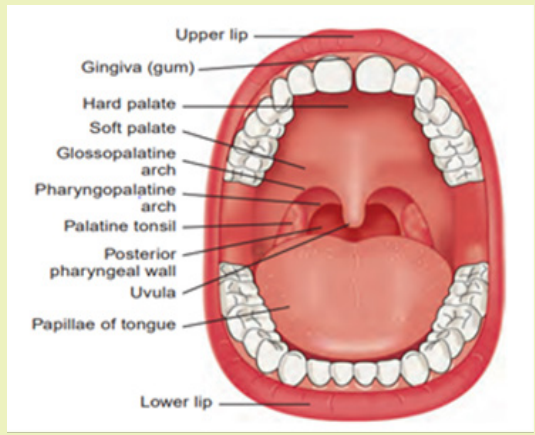
2) Enumerate at least 5 common consultation problems of the mouth.
3) Which technique of physical assessment will you use to assess the mouthand pharynx?
4.5.1. Review of anatomy and physiology of the mouth and
pharynx
The mouth is considered as organ of taste. In anatomical position the lips made
as muscular folds around the mouth, they are the only part of the mouth seen
outside. When the lips are opened, we immediately see the teeth surrounded by
the gingiva. The teeth are connected to maxillary and mandible bones in form of
arch. The gingiva is pale in light skinned people; it is influenced by the individual
level of melamine pigmentation which makes it brown to darker in black people.
In the oral cavity seen when mouth is open, there is the tongue, hard and soft
palate, uvula and two tonsils. The upper surface of the tongue present papillae
which gives a rough surface, some of the papillae are a bit red than others. In
normal circumstance, the tongue may be covered by a thin layer of white coat. On
the lower surface of the tongue, there are no papillae. Just looking at that surface,
we find midline lingual frenulum which attach the tongue to the floor of the mouthand the ducts of submandibular.
The paired sublingual glands lie just under the floor of the mouth mucosa.
Above and behind the tongue, there is an arch formed by anterior and posterior
pillars, the soft palate and uvula. The posterior pharynx is visible behind the soft
palate and the tongue. The uvula known as a hanged lobe in the middle of the
posterior border of the soft palate. Tonsils are often smaller even absent in adults.
The buccal mucosal covers the internal surface of the cheeks. The parotid ductsopen onto the buccal mucosal near the upper second molar
4.5.2. Physical examination of the mouth and pharynx
The physical assessment of the mouth and pharynx involve inspection and
palpation. The examiner observes the lips for color, moisture, ulcers, cracking
or trauma and note any deviance from normal anatomy. By using a new tongue
depressor and bright light in hand, ask the patient to open the mouth widely. Inspect
the gums for bleeding, ulcers, or swelling, and check to see if any teeth are missing,
discolored, abnormal shaped, or loose. Redness of the gingiva and swelling of the
interdental papillae are observed during gingivitis. Carefully inspect the buccal
mucosa for ulcers, nodules, or white patches. To inspect the tongue, ask the patient
to protrude the tongue and move it from side to side, assessing for symmetry, and
inspect the color and texture of its dorsal surface. Asymmetric protrusion of the
tongue suggests the lesion of hypoglossal nerve. Oral cancers most commonly
develop on the sides and base of the tongue. Men of greater than 50 years, smokers
and alcohol consumer are at high risk of tongue and oral cavity cancers. Have the
patient touch the tongue to the hard palate, and carefully inspect its undersurface
and the floor of the mouth. Using a gloved hand, gently grasp the tip of the tongue
with a square piece of gauze and move it from side to side, inspecting carefully forulcerations, plaques, masses, or discoloration.
To inspect the pharynx, the tongue will be back inside, have the patient open wide
and say “ah” or yawn. If the pharynx cannot be seen clearly, have the patient
repeat this maneuver while you firmly press down on the tongue with the tongue
depressor. Take care not to gag the patient. Observe for the soft palate rise because
it indicates the normal functioning of vagus nerve. Inability to rise the soft palate
and deviated uvula are the signs of vagus nerve paralysis. Inspect the uvula,
anterior and posterior pillars, tonsils (if present), and pharynx. When the patient is
saying “Ah” Check for symmetry, discoloration, ulcerations, swelling, masses, ortonsillar exudate.
Self-assessment 4.5
1) While making oral cavity assessment, which findings will indicate you that
the patient has gingivitis?
2) Mention at least 3 risk factors to develop oral cancer
3) Which features will you note on the patient’s lips during inspection?4) Draw an illustration of the oral cavity with all the parts
4.6. Skin assessment
Learning activity 4.6
Observe the images below and respond the questions that follow
1) Compare the images A, B and C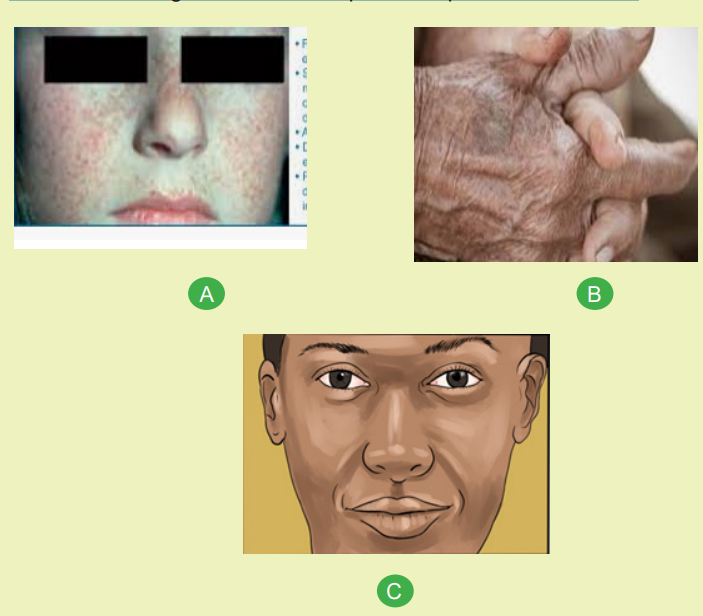
2) Do you think the skin in image b is normal? Explain your answer3) What are the characteristics of a normal skin?
Assessment of the skin involves inspection and palpation. The entire skin surface
may be assessed at one time or as each aspect of the body is assessed. In some
instances, the nurse may also use the olfactory sense to detect unusual skin odors.
4.6.1. History taking of the skin
Ask if the client has any history of the following: pain or itching; presence and
spread of lesions, bruises, abrasions, pigmented spots; previous experience with
skin problems; associated clinical signs; presence of problems in other family
members; related systemic conditions; use of medications, lotions, home remedies;
excessively dry or moist feel to the skin; tendency to bruise easily; association
of the problem to season of year, stress, occupation, medications, recent travel,
housing, and so on; recent contact with allergens (e.g., metal paint).
4.6.2. Physical examination of the skin
The entire skin surface should be examined as well as hair, nails and mucosal
surfaces. Explain the necessity of complete examination to the patient. Use an
appropriate light source and magnification. Identify the presenting complaint and
incidental skin conditions. Always patient privacy should be respected during
examination. Assess distribution, morphology and arrangement i.e. the number,
size and color of skin lesions, which sites are involved, their symmetry, shape and
arrangement. What types of lesions are present?
4.6.3. Inspection
• Inspect skin color, (Pallor, cyanosis, jaundice, erythema) (best assessed
under natural light and on areas not exposed to the sun).
• Inspect uniformity of skin color. Generally, the skin must be uniform except
in areas exposed to the sun; areas of lighter pigmentation (palms, lips,
nail beds) in dark-skinned people. Areas of either hyperpigmentation or
hypopigmentation indicate some abnormalities.
• Assess edema, if present (i.e., location, color, temperature, shape, and the
degree to which the skin remains indented or pitted when pressed by a finger).
Measuring the circumference of the extremity with a millimeter tape may be
useful for future comparison.
• Inspect, palpate, and describe skin lesions. Apply gloves if lesions are open
or draining. Palpate lesions to determine shape and texture. Freckles, some
birthmarks that have not changed since childhood, and some longstanding
vascular birthmarks such as strawberry or port-wine hemangiomas, some flat
and raised nevi; no abrasions or other lesions.
• Touch the skin to palpate individual lesions and more diffuse rashes, noting
surface and deep characteristics. Does the lesion involve epidermis, dermis?If scaly, does the surface flake off easily? If crusted, what is underneath?
• Look carefully for signs of systemic disease, such as xanthomas
(hyperlipidaemia), café-au-lait macules (neurofibromatosis),
acanthosisnigricans (insulin resistance) etc.
• Various interruptions in skin integrity; irregular, multicolored, or raised
nevi, some pigmented birthmarks such as melanocystic nevi, and some
vascular birthmarks such as cavernous hemangiomas. Even these deviations
from normal may not be dangerous or require treatment.
• Observe and palpate skin moisture. Moisture in skin folds and the axillae
(varies with environmental temperature and humidity, body temperature, and
activity) Excessive moisture (e.g., in hyperthermia); excessive dryness (e.g.,
in dehydration).
• Palpate skin temperature. Compare the two feet and the two hands, using the
backs of your fingers. Generalized hyperthermia (e.g., in fever); generalized
hypothermia (e.g., in shock); localized hyperthermia (e.g., in infection);
localized hypothermia (e.g., in arteriosclerosis)
• Note skin turgor (fullness or elasticity) by lifting and pinching the skin on an
extremity or on the sternum. When pinched, skin springs back to previous
state (is elastic); may be slower in older adults Skin stays pinched or tented
or moves back slowly (e.g., in dehydration). Count in seconds how long the
skin remains tented.
• Examine the hair and nails.
• Document findings in the client record using forms or checklists supplemented
by narrative notes when appropriate. Draw location of skin lesions on body
surface diagrams.
Common causes of skin disorders include: bacteria trapped in skin pores and hair
follicles, fungus, parasites, viruses, a weak immune system, contact with allergens,
irritants, or another person’s infected skin, genetic factors, sun exposition, systemic
conditions with skin effect such as thyroid, immune system, kidneys and so on.
4.6.4. Lifespan considerations
a. Infants
Physiological jaundice may appear in newborns 2 to 3 days after birth and usually
lasts about 1 week. Pathologic jaundice, or that which indicates a disease, appears
within 24 hours of birth and may last more than 8 days. Newborns may have
milia (whiteheads), small white nodules over the nose and face, and vernixcaseosa
(white cheesy, greasy material on the skin). Premature infants may have lanugo, a
fine downy hair covering their shoulders and back.
In dark-skinned infants, areas of hyperpigmentation may be found on the back,
especially in the sacral area. Diaper dermatitis may be seen in infants. If a rash ispresent, inquire in detail about immunization history
Assess skin turgor by pinching the skin on the abdomen.
b. Children
Children normally have minor skin lesions (e.g., bruising or abrasions) on arms and
legs due to their high activity. Lesions on other parts of the body may be signs of
disease or abuse, and a thorough history should be taken. Secondary skin lesions
may occur frequently as children scratch or expose a primary lesion to microbes.
With puberty, oil glands become more productive, and children may develop acne.
Most persons ages 12 to 24 have some acne.
Measles is a highly infectious, airborne caused by morbilivirus. It is very prevalent
in babies who are too young to be vaccinated, pregnant people, and others who did
not get vaccine. One symptom of measles is a red or brown rash that spreads down
the body. Other symptoms include a fever, watery eyes and a runny nose, a cough,
and small reddish spots inside the mouth. There is no cure, but treatment tend to
address the symptoms and monitor to prevent complications.
Impetigo defined as a contagious bacterial infection is one of the most common
skin infections in young children. It usually causes itchy sores and blisters to appear
around the mouth and elsewhere on the face. These sores then burst and leave a
crust. The crust dries and leaves a red mark that fades without scarring. Treatment
usually involves an antibiotic.
Cellulitis is a bacterial infection in the deeper layers of the skin. It develops quickly
and can spread rapidly throughout the body. The affected skin may be red, swollen,
hot, and painful or tender. Cellulitis is most common in the legs but can occur
anywhere in the body. Severe cellulitis may be life threatening, and the treatment
generally involves antibiotics.
Acne, the most common skin disorder, can be a source of anxiety for every teen,
caused by blocked hair follicles and sebaceous glands of the skin, often triggered
by hormonal changes. Acne affects mostly the face and sometimes the back and
chest. Acne needs to be treated by a dermatologist because untreated forms cause
permanent scars and dark facial spots.
Atopic dermatitis is one of the most common forms of eczema seen in children.
The exact cause of atopic dermatitis is not known, possibly it involves genetics, the
environment, and/or the immune system. Atopic dermatitis can appear on the face
especially in infants, hands, feet and folds of the skin. Clinically, the skin looks dry,
scaly and itchy skin are the norm, and constant scratching may lead to a thickened
area. Topical steroids are often used to control the symptoms.
Cutaneous candidiasis caused by overgrowth of the Candida albicansis
manifested as lesions or small pustules. Candidiasis typically develops in skinfolds, such as the armpit or around the groin, sometimes affect the face. People
can usually prevent Candidiasis by improving their skin hygiene and avoiding
the overuse of antibiotics. The treatment consist of antifungal and corticosteroidcreams.
c. Older adults
Changes in white skin occur at an earlier age than in black skin. The skin
loses its elasticity and develop wrinkles. Wrinkles first appear on the skin of the
face and neck, which are abundant in collagen and elastic fibers. The skin appears
thin and translucent because of loss of dermis and subcutaneous fat.
The skin is dry and flaky because sebaceous and sweat glands are less active. Dry
skin is more prominent over the extremities. The skin takes longer to return to its
natural shape after being tented between the thumb and finger. Due to the normal
loss of peripheral skin turgor in older adults, assess for hydration by checking skin
turgor over the sternum or clavicle. Vitiligo tends to increase with age and is thought
to result from an autoimmune response which trigger loss of skin pigmentation.
Vitiligo generally causes white patches to appear on the skin, usually in areas
exposed to sunlight, it is more remarkable in dark skinned people and currently nocure for vitiligo.
Shingles or Herpes Zoster results in a red, blistered rash that may wrap around
the trunk or appear anywhere on your body. Other signs and symptoms include
fever, fatigue and headache. Shingles is caused by the same virus that causes
chickenpox - the varicella-zoster virus. People who suffered from chickenpox are
at risk for shingles as the chickenpox virus lies dormant in their nervous system
for years. The treatment of measles is symptomatic, the preventive measure is a
vaccine called measles, mumps, rubella (MMR) vaccine.
Skin cancer involves uncontrollable skin cells growth. We have several types of
skin cancer but common ones are basal cell carcinoma, squamous cell carcinoma
and melanoma. Early recognition of cancer may allow its effective treatment. These
cancers tend to occur after prolonged exposure to the sun. Darker skin produces
more melanin, which gives the skin more protection from harmful sun rays. The
Basal cell carcinoma which is the most common skin cancer. It typically develops
on the neck, arms, or head but can affect any area of the body. In a person with
lighter skin, basal cell carcinoma may appear as a pink, round bump or patch. In
someone with darker skin, the bump may be brown or black and may look like a
common mole.
Squamous cell carcinoma is the second most common type of skin cancer. The
skin appears dry, scaly, patches called actinic keratoses. The late diagnostic will let
it grow deeper into the skin and cause disfigurement. People with lighter skin tend
to develop this cancer in areas often exposed to the sun whereas in darker skinned,it affects the legs, genitals, and anus. It is a good idea to consult for any lesion that
grows, changes, bleeds or looks unusual in any other way.
Melanoma is the most serious of the skin cancers because it spreads most easily
to other parts of the body. It is can develop from a mole or another pigmented
area of skin. If any mole is asymmetrical, has ragged edges or an uneven color, or
changes in size, there is a need for medical attention. Melanoma may be harder to
identify in darker skinned people, so checking carefully is important. Remember to
include the toenails and fingernails, as this type of cancer is more common in these
areas for People of color. The treatment of cancer involves radiotherapy, surgery,and chemotherapy.
4.6.5. Specific test of the skin
Specialized techniques used in examination of the skin include:
• Dermoscopy for pigmented lesions to diagnose melanoma.
• Skin biopsy for histology and direct immunofluorescence.
• Patch tests to identify type 4 contact hypersensitivity reactions.
• Skin scrapings or nail clippings for mycology (fungal infections).
• Wood’s light (long wave UVA) examination for pigmentary changes and
fluorescence resulting from certain infections.
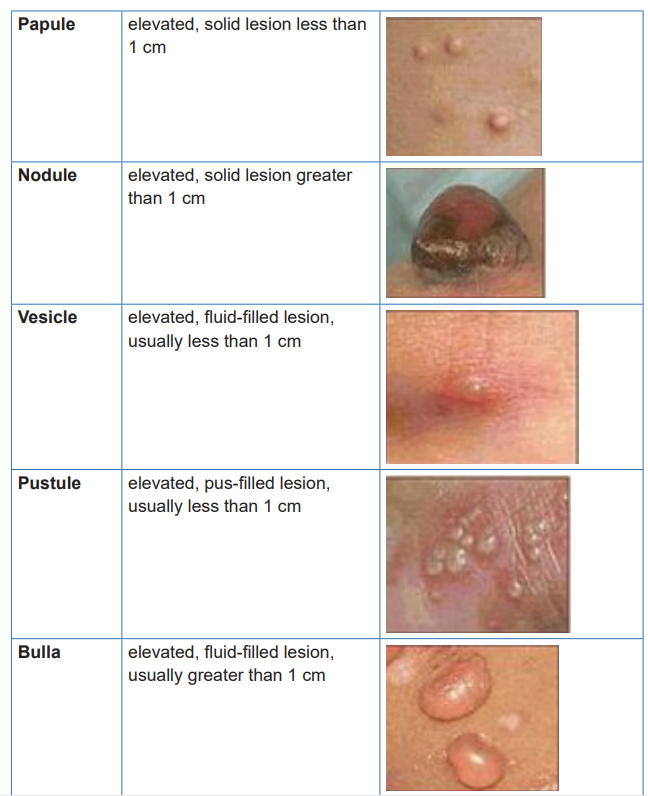
Table 4.6 1How to describe a skin lesion

4.6.6. Preventing skin disorders
Certain skin disorders aren’t preventable, including genetic conditions and some
skin problems due to other illnesses. However, it’s possible to prevent some skin
disorders by:
• Washing hands with soap and warm water frequently.
• Avoid direct contact with the skin of other people who have an infection.
• Clean things in public spaces, such as gym equipment, before using them.
• Don’t share personal items, such as blankets, hairbrushes, or swimsuits.
• Sleep for at least seven hours each night.
• Drink plenty of water.
• Avoid excessive physical or emotional stress.
• Eat a nutritious diet.
• Get vaccinated for infectious skin conditions, such as chickenpox.
Noninfectious skin disorders, such as acne and atopic dermatitis, are sometimes
preventable. Prevention techniques vary depending on the condition. Here are
some tips for preventing some noninfectious skin disorders:
• Wash face with a gentle cleanser and water every day.
• Use moisturizer.
• Avoid environmental and dietary allergens.
• Avoid contact with harsh chemicals or other irritants.
• Sleep for at least seven hours each night.
• Drink plenty of water.
• Eat a healthy diet.• Protect your skin from excessive cold, heat, and wind.
Self-assessment 4.6
1) What are the skin characteristics to note during physical examination?
2) What are the causes of acne?
3) Enumerate common skin conditions in children
4) Which physical assessment technique used to examine the skin5) List the element of education for the prevention of skin conditions?
End unit assessment 4
1) List 5 infectious diseases of the skin
2) Why do old adults lose skin elasticity and develop wrinkles?
3) Why do we insert the otoscope differently in children and adult patients?
4) What does a deviated uvula present during buccal cavity assessment?
5) What are the inspectional findings of the lips?
6) Enumerate the signs and symptoms of tonsillitis7) Which sinuses are palpable during physical examination?
