UNIT3:NURSING ASSESSMENT OF NEUROLOGICAL SYSTEM
Key Unit Competence
Take appropriate action based on findings of nursing assessment of neurological
system
Introductory activity 3
Neurological assessment is a sequence of questions and tests to check brain,
spinal cord, and nerve function. The exam checks a person’s mental status,
coordination, ability to walk, and how well the muscles, sensory systems, and
deep tendon reflexes work.Observe the pictures below and answer the asked questions:
1) What do you see on picture A?
2) What do you see on picture B?
3) On your point of view, what are connections between picture A and theaction which is being done on picture B?
3.1. Specific history taking on Neurological system
Learning activity 3.1
Observe the picture below:
1) Based on the picture above, what is problem does have this person?
2) What are possible questions can you ask to this person to know wellabout that problem?
Taking the patient’s history is habitually the first step in practically every clinical
meeting. Taking a detailed history and performing a careful examination can help
the health care provider to determine the site of a specific neurological lesion and
reach a diagnosis.
Always start with demographic data such as name, age, sex, educational background,
marital status, religion and address. Ask the patient history of the presenting illness
or chief complaint should include the following information: Symptom onset (acute,
sub-acute, chronic, insidious), duration, course of the condition (static, progressive,
or relapsing and remitting), associated symptoms (other features of neurological
disease): Headache, Numbness, pins and needles, cold or warmth, Weakness,
unsteadiness, stiffness) nausea, vomiting, vertigo, numbness, weakness, and
seizures.
Firstly, observe the patient’s gait as he/she enters the room. Note any abnormalities
in gait and any involuntary movement.
Ask about the symptoms: What are they? Which part of the body do they affect?
Are they localized or more widespread? When did they start? How long do they last
for? Were they sudden, rapid or gradual in onset? Is there a history of trauma? Ask
about any associated symptoms (other features of neurological disease): Headache,
Numbness, pins and needles, cold or warmth, Weakness, unsteadiness, stiffness)Self-assessment 3.1
1) Outline at list 5 questions you can use to ask patient about his/hersymptoms
3.2. Specific physical examination of neurological
system
Learning activity 3.2
Observe the image below and answer the questions
1) What do you see on image above?
2) What steps to follow in performing specific physical assessment for theabove patient?
A complete neurological assessment consists of seven steps which are mental
status exam, cranial nerve assessment, reflex testing, motor system assessment,
sensory system assessment, coordination and Gait.
3.2.1. Mental Status
Changes in memory or mood, ability to care for oneself, ability to balance a
checkbook, difficulty with language, geographical orientation,
3.2.2. Cranial nerve assessment
Abnormalities in vision, hearing, smell, taste, speech or swallowing, Facial weakness
or numbness.
3.2.3. Reflex testing
Reflex testing occurs when an initial test result meets pre-determined criteria (e.g.,
positive or outside normal parameters), and the primary test result is inconclusive
without the reflex or follow-up test. It is performed automatically without theintervention of the ordering physician.
3.2.4. Motor system assessment
History of muscular weakness, tremor, difficulty in initiating movements, loss of
muscle bulk.
3.2.5. Sensory system assessment
Numbness, tingling, or altered sensation in any limbs.
3.2.6. Coordination
Clumsiness, difficulty with hand writing or carrying out coordinated tasks.
3.2.7. Gait and station
Abnormalities of gait, frequent falling, difficulty maintaining balance.
3.3. Interpretation of specific findings on Neurologicalsystem
Learning activity 3.3
Observe the image below
1) The picture above shows a patient with facial palsy with asymmetrical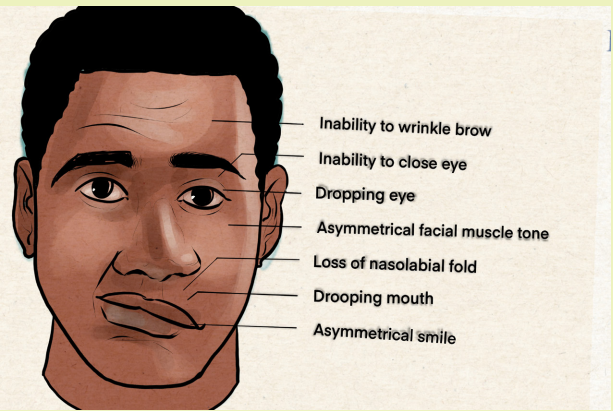
facial muscle tone. What is the most probable cranial nerve being moreaffected?
Interpretation of specific finding in neurological system is a very crucial step to
guide diagnosis and treatment. It is necessary to assess each of the seven itemsassessed as discussed in previous lesson.
3.3.1. Mental status
The patient’s attention span is assessed first; an inattentive patient cannot cooperate
fully and hinders testing. Any hint of cognitive decline requires examination of
mental status which involves testing multiple aspects of cognitive function. Assess
the patient orientation to time, place, and person.
Assess the patient attention and concentration, memory, verbal and mathematical
abilities, judgment and reasoning
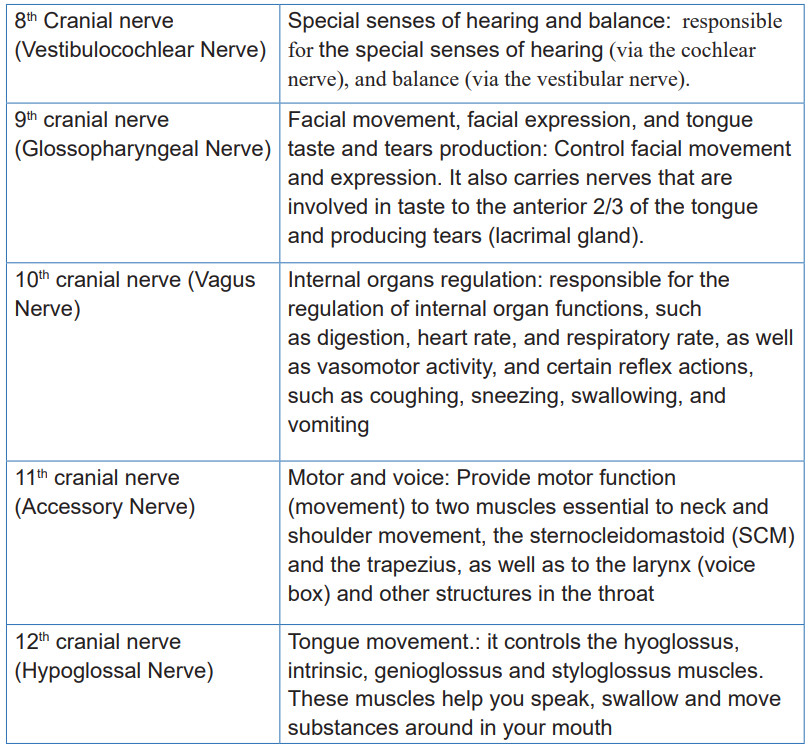
3.3.2. Cranial nerve assessment
Each cranial nerve has a well-defined function and any abnormality in cranial nervesystem should be assessed, reported and treated accordingly.
Table 3.3 1 Cranial nerves

3.3.3. Reflextesting:
A reflex is an involuntary and nearly instantaneous movement in response to a
stimulus. The reflex is an automatic response to a stimulus that does not receive or
need conscious thought as it occurs through a reflex arc.
The muscle contraction should be seen and felt and compared side-to-side. If
reflexes are diminished or absent, try reinforcing the reflex by distracting the patient
or having the patient contract other muscles (e.g., clench teeth). Note, however, that
symmetrically brisk, diminished, or even absent reflexes may be found in normal
people. The muscle stretch reflexes that are the most clinically relevant and that
you should know how to obtain include the biceps, triceps, knee, and ankle. The
superficial (cutaneous) reflexes are elicited by applying a scratching stimulus to the
skin. The only superficial reflex that you need to know other than the corneal is the
plantar reflex. An abnormal plantar reflex (extension of the great toe with fanningout of the other toes upon stimulation of the plantar surface of the foot) is a specific
indicator of corticospinal tract dysfunction and may be the only sign of ongoing
disease or the only residual sign of previous disease.
3.3.4. Motor system assessment
The motor exam is affected not only by muscle strength, but also by effort, coordination,
and extrapyramidal function. Tests of dexterity and coordination are most sensitive
to picking up upper motor neuron and cerebellar abnormalities, whereas direct
strength testing is more sensitive to lower motor neuron dysfunction. Other aspects
of the motor exam include (1) patterns of muscle atrophy or hypertrophy, (2)
assessment of muscle tone (e.g., spastic or clasp knife, rigid or lead pipe, flaccid)
with passive movement of joints by the examiner, (3) disturbances of movement
(e.g., the slowness and reduced spontaneity of movement in parkinsonism), (4)
endurance of the motor response (e.g., the fatigability of myasthenia gravis), and
(5) whether any spontaneous movements are present (e.g., fasciculation or brief
twitches within the muscle).
3.3.5. Sensory system assessment
Explain to the patient what you are going to do and what you expect of them, then
have them close their eyes for the testing. Be aware of the fact that patients may
report differences in sensation in the presence of normal sensory function because
of actual differences in the stimulus intensity applied.
3.3.6. Gait
Since walking requires integration of motor, sensory, cerebellar, vestibular, and
extrapyramidal function, assessment of gait can provide important information to
guide the focus of the rest of the exam and can obviate the need for specific testing.
It is for this reason that health care provider should watch the patient walk at the
very beginning of the exam.
Pay attention to the following;
• Posture of body and limbs (Is the patient stooped over or leaning to one side?
Is a limb held in a funny position?);
• Symmetry of arm swing (Is one side decreased?);
• Length, speed, and rhythm of steps (does the patient lurch? Are the legs stiff
and scissoring?); 4) base of gait (Are the legs held far apart because the
patient is unstable?);
• Steadiness; and
• Turns (How many steps does the patient take to turn?). More informative stillis if the patient can run and hop on one foot.
Self-assessment 3.3
1) During assessment of mental health status, a nurse should assess the
patient orientation on three aspects. What are they?
2) Give names and function of the following cranial nerves
a. 1st Cranial nerve
b. 2nd Cranial nerve
c. 4th cranial nerve
d. 11th cranial nervee. 12th cranial nerve
3.4. Identification of client problems
Learning activity 3.4
You receive a 36 years old female with balance difficulties; eyesight changes;
weakness of face muscles; left arm weakness and difficult in speech since 5
hours ago.What do you suspect?
Identification of client problem in neurological system is a key action very necessary
to lead an appropriate diagnosis and treatment. The following are six common
neurological disorders
3.4.1. Headaches
Headaches are one of the most common neurological disorders and can affect
anyone at any age. The sudden onset of severe headache as well as headache
associated with a fever, light sensitivity and stiff neck are all red flags of something
more serious such as intracranial bleeding or meningitis.
3.4.2. Epilepsy and Seizures
Epilepsy is a common neurological disorder involving abnormal electrical activity in
the brain that makes a patient more susceptible to having recurrent, unprovoked
seizures. Unprovoked means the seizure cannot be explained by exposure to or
withdrawal from drugs or alcohol, as well as not due to other medical issues such
as severe electrolyte abnormalities or very high blood sugar.
3.4.3. Stroke
A stroke is usually due to a lack of blood flow to the brain, oftentimes caused by
a clot or blockage in an artery. Many interventions can be done to stop a stroke
these days, but time is brain (not money) in this case. The B.E. F.A.S.T. mnemonic
is helpful to remember to recognize the signs of a stroke: B: Balance difficulties; E:
Eyesight changes; F: Face weakness; A: Arm weakness; S: Speech; and T: Time.
These signs and symptoms don’t always mean someone is having a stroke, but it’s
very important to request help right away.
3.4.4. Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis, also known as Lou Gehrig’s disease, is a somewhat
rare neuromuscular condition that affects the nerve cells in the brain and spinal
cord. The cause is not well known, but factors that may cause ALS include genetics
and environmental factors. Symptoms include muscle weakness and twitching,
tight and stiff muscles, slurred speech, and difficulty breathing and swallowing.
Unfortunately, this condition is difficult to diagnose and often requires the evaluation
of a neuromuscular neurologist.
3.4.5. Alzheimer’s disease and Dementia
Memory loss is a common complaint, especially in older adults. A certain degree of
memory loss is a normal part of aging. For example, walking into a room and forgetting
why may be totally normal. However, there are signs that may indicate something
more serious, such as dementia or Alzheimer’s disease. These symptoms may
include getting lost, having difficulty managing finances, difficulties with activities of
daily living, leaving the stove on, forgetting the names of close family and friends
or problems with language. Behavioral changes along with these memory changes
could also raise concerns. Dementia is a slowly progressive condition. While there
is no cure, there are medications and therapies that can help manage symptoms.
3.4.6. Parkinson’s disease
Parkinson’s disease is a progressive nervous system disorder that primarily affects
coordination. Generally, it becomes more common as a patient get older.
Symptoms of Parkinson’s disease usually get worse over time. Patient may
experience changes in posture, walking and facial expressions early on in the
disease, and cognitive and behavioral problems could develop later in the disease
Self-assessment 3.4
1) Memory loss is a common complaint:
a. True
b. False
2) Parkinson’s disease is a progressive nervous system disorder that
primarily affects coordination
a. True
b. False
3) State six common neurological disorders
3.5. Nursing intervention based on patient’s problem.Learning activity 3.5
You have received a 27years old male with epileptic disorder. He is seizing.
1) What are your interventions after seizure stop?
Nursing interventions in patient with neurological disorders are very crucial to
alleviate the client discomforts. Any client complaints should be monitored andtreated accordingly.
3.5.1. Interventions for Headache
• Encourage the client to rest in a quiet, dark room.
• Avoid noises
• Encourage relaxation techniques
• Collaborate with other health professionals to identify and treat the cause of
headache
3.5.2. Interventions for Epilepsy/Seizure
The patient will be placed in a horizontal plane and care will be taken that he does
not receive trauma to the skull, with the head tilted and the clothing lopsided.
Control and assess in the patient: assess the duration of the seizure, type of seizure,
the level of consciousness, the coloring of the skin and mucous membranes.
Monitor vital signsHeart rate, breathing frequency, blood pressure, O2
saturation…), perform capillary blood glucose.
a. Tonic-clonic onset seizures
In those patients with previous epileptic seizures or with significant risk factors
in treatment with antiepileptic drugs, severe brain injury, exposure to drugs and
hallucinogens, etc.:
• Maintain the necessary material for oxygen therapy and aspiration, in optimal
conditions.
• Facilitate the accessibility of calls to the nursing staff, especially if there are
prodromes.
• Provide a suitable and safe environment, free of furniture and objects that can
cause harm during the epileptic seizure.
• Protect the patient from all potentially harmful objects.
• Maintain a patent venous line if necessary.
• Inform the patient and the family about the action before the appearance of
prodromes:
• Remove the teeth or other objects from the mouth.
• Remove the eye lenses.
• Lay him down on the floor or in bed.
b. During tonic-clonic onset epileptic seizures
• Keep calm and serenity as much as possible and we will transmit it to the
patient, relatives.
• Identify that it is a tonic-clonic epileptic seizure.
• Alert: Notify the doctor on duty.
• Protect the patient:
• If the patient is out of bed, help him to lie down if possible, or lay him on the
floor; avoiding as much as possible the fall.
• Do not leave the patient alone under any circumstances and monitor him.
• Remove nearby objects and / or furniture with which it may hit.
• Loosen clothing that is tight.
• Remove the glasses if you wear them.
• Do not immobilize or restrain the patient by force during the epileptic seizure,
but control and guide their movements to avoid injuries.
• Protect the head by placing a pillow or a towel underneath.
c. Guarantee the patency of the airway:
• Remove, if possible, dentures and dental implants that are not permanent.• Remove food from the mouth in case this process is carried out.
• Aspirate secretions, if necessary.
• Perform other nursing intervention are necessary such as oxygen
administration, a peripheral line should be installed as soon as the seizures
stop, monitoring of vital signs: (temperature, blood pressure, heart rate,
breathing frequency), carry out the complementary tests as requested by the
doctor.
• It is very important to control and assess the duration of the tonic-clonic phase,
type of epileptic seizure, where does the movement or begin contracture, eye
position and / or eye movements, the pupils (relationship between them, size
and reactivity) and time the patient is unconscious. Assess any urinary and
fecal incontinence. When the epileptic seizures cease, place the patient in the
recovery position.
• Do not administer anything by mouth.
• If after the crisis he is excited, calm him down and reassure him.
• Administer the drug directed by the doctor.
• If there is any bleeding lesion, press with a sterile compress until the bleeding
stops.
• Ensure that the environment is quiet and safe, without excessive lighting or
noise.
• Carry out a new check of vital signs and serum glycemia.
• In case of incontinence, proceed to clean the patient.
• In case of drowsiness, let him rest.
• When he wakes up, redirect and reassure him.
• Carry out the complementary tests requested by the doctor.
• Control and assess: Duration of the post-seizure phase, assessment of the
level of consciousness (GLASGOW SCALE), degree of confusion, if he is
drowsy, let him sleep and do not wake him up or shake him, color of the skin
and / or mucous membranes, whether he speaks or not. If there is paralysis
or weakness in the arms and / or legs.
3.5.3. Interventions for stroke
• When a patient is having stroke, immediately call for ambulance because
as he/she delays to get appropriate treatment, more serious complications
develop
• Note the time the first symptom occurs
• Provide appropriate positioning.
• Prevent flexion and adduction• Monitor closely vital signs
3.5.4. Interventions for Amyotrophic Lateral Sclerosis (ALS)
• Assess motor strength; presence of spasticity, flaccidity and presence
contracture.
• Assess skin daily, especially those areas susceptible to breakdown.
• Promotion of activity and exercise.
• Encourage continuation of daily routines and activities.
• Range-of-Motion (ROM) exercises to prevent contracture and pain in joints;
first Active ROM, then passive.
• When weakness in the extremities begins to compromise mobility, safety,
or independence in Activities of daily living (ADL), refer to a physical or
occupational therapist.
• Promotion of proper positioning to prevent decubitus ulcers. Use as many
different positions as possible when in bed. Change positions every two
hours, or on skin tolerance. After each change of position, check for redness
over bone prominences, and provide an eggshell or circulating mattress when
immobility prevents independent repositioning.
• Repositioning in the wheelchair based on the patient’s skin tolerance. Use of
a wheelchair cushion to prevent skin breakdown.
• Proper positioning when ambulating or in a wheelchair, i.e., use of a sling for
a weak upper extremity.
• Promote adequate nutritional intake.
3.5.5. Interventions for Alzheimer’s disease and Dementia
• Frequently orient client to reality and surroundings.
• Encourage caregivers about patient reorientation.
• Enforce with positive feedback and discourage suspiciousness of others.
• Avoid cultivation of false ideas
• Monitor client closely
3.5.6. Interventions for Parkinson’s Disease
• Improving functional mobility and independence in performing activity of daily
living.
• Assess bowel elimination and encourage patient on good diet to avoid
constipation
• Improve and maintaining acceptable nutritional status,• Promote effective communication and developing positive coping mechanisms.
Self-assessment 3.5
1) When the epileptic seizures cease, what is the best position to give to the
patient?
2) Give 2 primary nursing interventions for each of following
a. Headache
b. Epilepsy/Seizurec. Stroke
End unit assessment 3
1) Memory loss is a common complaint:
a. True
b. False
2) Parkinson’s disease is a progressive nervous system disorder that
primarily affects coordination
a. True
b. False
3) State six common neurological disorders
4) Give 2 primary nursing interventions for each of following
a. Headache
b. Epilepsy/Seizure
c. Stroke
5) Outline at list 5 questions you can use to ask a neurological patient about
his/her symptoms.6) List 7 steps of complete neurological assessment
