UNIT2:HUMAN NUTRITION AND DIETETICS
Introductory activity 2
Introductory activity 2
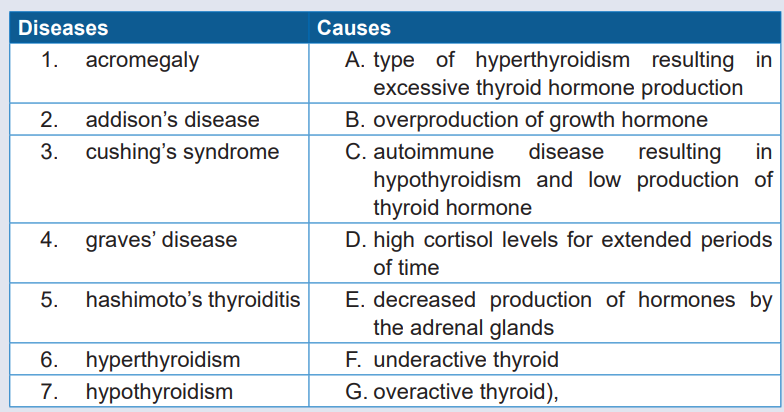
Observe the picture above and answer the following questions: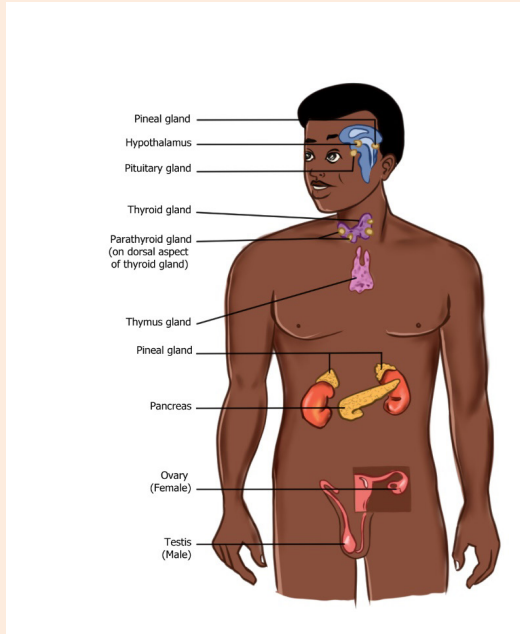
1) What do you see on the picture above?
2) On your point of view, what is the role of each part mentioned on the
picture above?
3) You receive a patient suspected of having endocrine disorder. What isgeneral assessment you are going to perform
2.1. Specific History Taking on Endocrinology System
Learning activity 2.1
Observe the picture above and answer below questions:
1) What do you see on the picture above?
2) What are history to collect when suspecting a problem arising from the
endocrine system?2.1.1. Overview of history taking of endocrine system
The endocrine system is a series of glands and tissues that produce and secrete
hormones, which are used by the body to regulate and coordinate vital bodily
functions, including growth and development, metabolism, sexual function and
reproduction, sleep and mood.
At the time of taking history of the patient focusing on endocrine system, the history
regarding illness, personal history, family history and social history will be asked to
patient. Furthermore, both subjective and objective data are assessed. Endocrine
disorders and diseases usually manifest according to which endocrine hormone is
being overproduced and secreted, or under-produced, at any given age.
History taking in endocrine system follows the general client history and focus on
history regarding illness, personal history, family history, social history as well assubjective and objective data
a. History regarding illness
The health care professional asks the patient how and when the disease started.
What are aggravating factors and what are alleviating factors of the disease.
b. Personal history
A personal history in endocrinology system is similar like other assessment and
may include information about allergies, illnesses, surgeries, immunizations, andresults of physical exams, tests, and screenings.
c. Family history
Family history is crucial in endocrinology system because a mutated gene
causes different endocrine glands in the body to develop benign and cancerous
neuroendocrine tumors. Endocrine glands secrete hormones, so tumors arising
from these glands may also overproduce hormones that result in symptoms. Hence
it can provide insight into a patient’s risk for developing certain cancers or even
give a hint as to how aggressively a particular patient’s cancer might behave.
Furthermore, many endocrinology systems develop along with a family because
some families are exposed to develop a given disease example of diabetes. Health
care provider asks a patient on history of the endocrinology disease in a given
family.
d. Social history
The social history covers the patient’s lifestyle, such as marital status, occupation,
education, and hobbies. It may also include information about the patient’s diet, use
of alcohol or tobacco, and sexual history. Along with the chance to connect with the
patient as a person, the social history can provide vital early clues to the presence
of disease, guide physical exam and test-ordering strategies, and facilitate theprovision of cost-effective, evidence-based care.
2.1.2. Subjective and objective data
After taking patient history, continue with subjective data and objective data
Ask the patient symptoms he /she is feeling and the patient can accuse one or
more of the following symptoms: dizziness, fatigue or lethargy, weight gain or loss,
changes in vision, feelings of depression, irritability, or anxiety, decreased libido,
change in appetite, pain, nausea and vomiting, changes in urinary or bowel habits,
intolerance to heat or cold.
Objective data will focus on endocrinology system which will be discussed in this
unit. Always assess patient from head to toe.
Note:A patient with one endocrine disease (e.g., Hashimoto’s thyroiditis) is at greater
risk for the development of other endocrine disorders (e.g., adrenal, testicular, orovarian failure).
Self-assessment 2.1
1) The key to discovering the nature of the symptoms found during
assessment is lying in understanding of the functions of the endocrine
hormones.
a. True
b. False
2) Which sign will indicate a health professional to assess the endocrine
system?
a. Fever
b. Bleeding
c. Frequent urinationd. Abdominal pain
2.2. General Survey in Endocrinology System
Learning activity 2.2
The general appearance of a patient may provide diagnostic clues to the illness,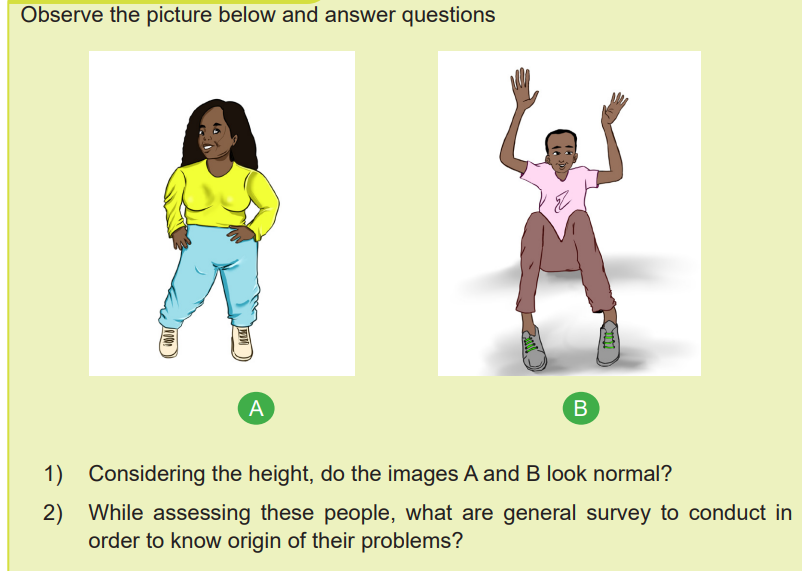
severity of disease, and the patient’s values, social status, and personality. By
gathering general survey in a person with endocrine system observing and focusing
carefully on facies, features and expression, build & stature, nutrition, decubitus,
neck vein, neck glands, anemia, cyanosis, clubbing, jaundice, edema, pulse,respiration, Temperature, BP, generalized skin & nail and extremities.
Note: stature and habitus: observe the patient’s body build. Very short stature
will be seen in dwarfism, pseudo hypoparathyroidism, Turner’s syndrome, or
prepubertal steroid therapy. Very tall and lanky people with long, thin extremities
suggest Marfan’s syndrome.Self-assessment 2.2
1) What should you focus more while conducting general survey on
endocrine system?
2) You receive a 30-year-old male with 90cm of height, what is the firstdisorder you think on your first sight?
2.3. Physical exam of endocrine system
Learning activity 1.9
Physical examination techniques in a focused endocrine assessment follows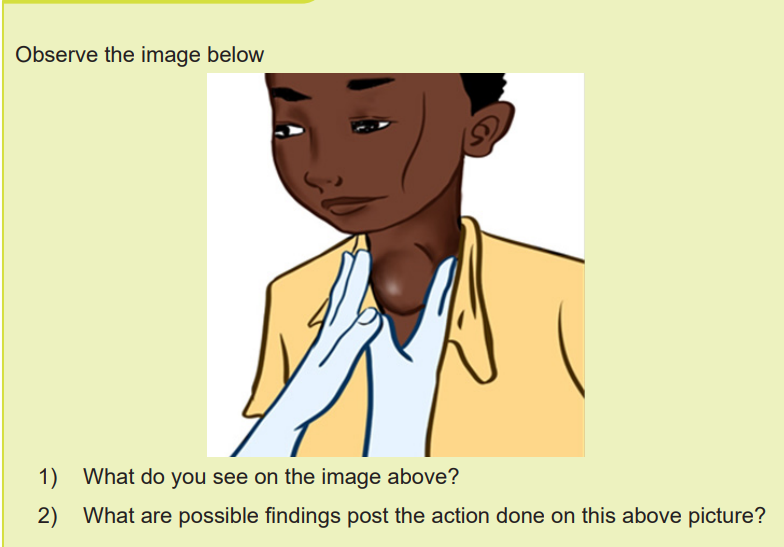
the same steps used in a general exam and it made of inspection, auscultation,
percussion and palpation.
2.3.1. Inspection
During inspection, a health professional inspect overall patient and note any
abnormalities. He/she looks for generalized appearance, skin color, any lesion and
its location, bruises or rashes, body shape and symmetry, size of body parts, any
abnormal sounds, any abnormal odors, inspect the neck from the front.
2.3.2. Auscultation
Auscultation is done before palpation and percussion.
2.3.3. Palpation
Palpation is done to assess endocrine system on the area where the organs linked
to endocrine system are located. It can be light or deep palpation. Palpation helps
health care professional to assess for texture, tenderness, temperature, moisture,
pulsations, masses, and internal organs.
When palpating the neck where located thyroid gland, the patient sits with the neck
muscles relaxed and stand behind him. Health care provider palpate gently the
thyroid on the front of the patient’s neck, with index fingers just touching lateral to
the trachea where the thyroid is located. In normal conditions, thyroid gland is not
palpable.
Shape and surface: Simple goiter is relatively symmetrical in their earlier stages
but often become nodular with time
Mobility: Most goiters move upwards with swallowing. Very large goiters may be
immobile, and invasive thyroid cancer may fix the gland to surrounding structures.
Consistency: Nodules in the substance of the gland may be large or small, and
single or multiple, and are usually benign. A very hard consistency suggests
malignant change in the gland.
Large: firm lymph nodes near a goiter suggest thyroid cancer.
Tenderness: Diffuse tenderness is typical of viral thyroiditis, whereas localized
tenderness may follow bleeding into a thyroid cyst.
Thyroid bruit: This can be found during auscultation and indicates abnormally high
blood flow and can be associated with a palpable thrill. It occurs in hyperthyroidism.
A thyroid bruit may be confused with other sounds. A bruit arising from the carotid
artery or transmitted from the aorta will be louder along the line of the artery.
Transient gentle pressure over the root of the neck will interrupt a venous hum fromthe internal jugular vein.
Endocrine organs namely testes and thyroid glands are the only endocrine glandsthat may be accessible for physical examination.
2.3.4. Percussion
Percussion helps to produce tenderness or sounds that point to underlying problems.
When percussing directly over suspected areas of tenderness, monitor the patient
for signs of discomfort.
Examples of area to percuss in endocrine disorder: enlarged pancreas, a pleural
effusion associated with specific endocrine abnormalities, or a hormone-secretingtumor
Self-assessment 2.3
1) Outline 2 examples of organs that can be assessed during palpation in
endocrine system.2) Name other endocrine organs of the human body
2.4. Interpretation of specific findings in endocrinesystem
Learning activity 10
Observe the image below
1) The image above shows a male patient, what are particularities seen on
this patient?
A comprehensive physical examination and its interpretation is required in endocrine
system. Symptoms of endocrine disturbance are varied and non-specific, and affect
many body systems.
The main endocrine glands are the pituitary, thyroid, parathyroid, pancreas, adrenals
and gonads (testes and ovaries). These glands synthesize hormones which are
released into the circulation and act at distant sites.
Examination sequence
The initial greeting may suggest a diagnosis. Inspect the face for a ‘spot’ endocrine
diagnosis
Observe the patient behavior: if the patient restless and agitated (hyperthyroidism)?
or slow and lethargic (hypothyroidism)?
Examine the entire skin surface, looking for abnormal pallor (hypopituitarism),
vitiligo, plethora (Cushing’s or carcinoid syndrome) or pigmentation (Addison’s
disease).
If the patient is obese, is the adiposity centrally distributed (Cushing’s syndrome
and growth hormone deficiency)?
Observe the body hair in quality and amount: look for hirsutism in females with
menstrual disturbance, especially on the face, chest and abdomen
Examine the hands for excessive sweating, soft tissue overgrowth (acromegaly),
skin crease pigmentation (Addison’s disease) and wasting of the thenar muscles
due to carpal tunnel syndrome. Assess the pulse rate, rhythm and volume. Record
the blood pressure because hypertension is a feature of several endocrine
conditions. Check for postural hypotension with lying and standing blood pressures
if you suspect adrenal insufficiency.
Examine the eyes in all thyroid patients for external inflammation, proptosis, diplopia
and visual function. Assess visual acuities and fields in patients with suspected
pituitary tumors, to detect bitemporal hemianopia due to compression of the optic
chiasm. Examine the fundi for optic atrophy in patients with longstanding optic
pathway compression.
Examine the patient face and note any hirsutism (Hirsutism results in excessive
amounts of stiff and pigmented hair on body areas where men typically grow
hair, including the face, chest and back, Hirsutism can result from excess male
hormones, called androgens.
Examine the neck for goiter. If this is present, record its size, surface and consistency.Look for gynaecomastia (enlargement of a men’s breasts, usually due to hormone
imbalance or hormone therapy) and for evidence of milk production in a man or non
breastfeeding woman (galactorrhoea). Inspect the axillae for acanthosisnigricans
or loss of axillary hair
Examine the male external genitalia. Inspect the amount of pubic hair and make
a pubertal staging of all adolescents. Record testicular consistency and volume.
Inspect the legs for evidence of pretibial myxoedema (Graves’ disease), proximalmuscle wasting and weakness (Cushing’s syndrome and hyperthyroidism).
Self-assessment 2.4
1) Hypertension is a feature of several endocrine conditions
a. True
b. False
2) The initial greeting of a patient suffering from endocrine system may
suggest a diagnosis.
a. True
b. False3) Differentiate hirsutism from gynecomastia
2.5. Identification of client problem
Learning activity 2.5
Common endocrine disorders are: diabetes mellitus (a disease in which the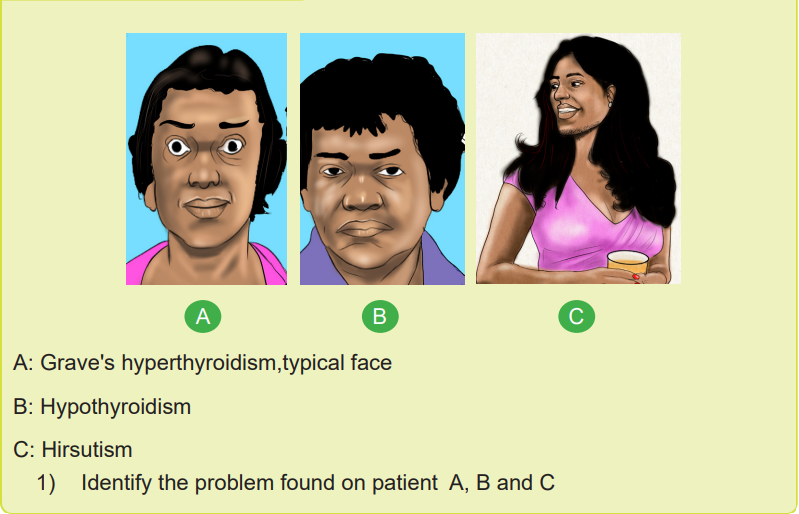
body’s ability to produce or respond to the hormone insulin is impaired, resulting
in abnormal metabolism of carbohydrates and elevated levels of glucose in the
blood),acromegaly(overproduction of growth hormone), addison’s disease
(decreased production of hormones by the adrenal glands), cushing’s syndrome
(high cortisol levels for extended periods of time), graves’ disease (type of
hyperthyroidism resulting in excessive thyroid hormone production), hashimoto’s
thyroiditis (autoimmune disease resulting in hypothyroidism and low production
of thyroid hormone), hyperthyroidism (overactive thyroid), hypothyroidism
(underactive thyroid), prolactinoma(overproduction of prolactin by the pituitary
gland). The Treatments depend on the specific disorder but frequently focus onregulating hormone balance using synthetic hormones.
Serious symptoms that might indicate a life-threatening condition
In some cases, endocrine disorders can be life threatening. The patient can have
symptoms/signs like: confusion or loss of consciousness for even a brief moment,
dangerously low blood pressure (extreme hypotension), dangerously slow heart
rate, dehydration, depression or anxiety, difficulty breathing, eye problems, including
dryness, irritation, pressure, pain or bulging severe fatigue or weakness, severe,
unexplained headache, severe vomiting and diarrhea, sleep disturbances.
Self-assessment 2.5
1) Define the term acromegaly
2) Outline five Serious symptoms that might indicate a life-threateningendocrine condition
2.6. Nursing intervention based on client problem
Learning activity 2.6
A 35 years old patient, was admitted in medical word complaining of
generalized body weakness, increased sensitivity to cold, constipation, dry
skin, weight gain, puffy face, hoarseness, muscle weakness, pain, stiffness
or swelling in joints, slowed heart rate, depression, impaired memory and
enlarged thyroid gland (goiter).
1) What is the suspected diagnosis (problem) for this patient?2.6.1. Interventions
Nursing intervention in endocrine system depends the client disorder.
For diabetic patient, Monitor the patient’s signs of hyperglycemia and
hypoglycemia and intervene accordingly. Monitor the patient weight to avoid
obesity and help assess the adequacy of nutritional intake and vitals signs
monitoring
Education the importance of physical activity. Education on how to self inject insulin
if any and how to take other medications. Physical activity helps lower blood glucose
levels. Regular exercise is a core part of diabetes management and reduces therisk for cardiovascular complications.
Monitor patient for evidence of excess physical and emotional fatigue because
hyperthyroidism results in protein catabolism, over activity, and increased
metabolism leading to exhaustion.
Monitor cardiorespiratory response to activity (e.g., tachycardia, other dysrhythmias,
dyspnea, diaphoresis, pallor, blood pressure [BP], and respiratory rate) because
decompensation of cardiopulmonary function can occur with hypermetabolism.
Assist with regular physical activities (e.g., ambulation, transfers, turning, and
personal care) to make certain patient’s daily needs are met.
Assist the patient to understand energy conservation principles (e.g., the requirement
for restricted activity or bed rest) to avoid fatiguing patient.
Assist the patient to schedule rest periods and avoid care activities during scheduledrest periods to promote adequate rest.
2.6.2. Nutrition Management
Determine, in collaboration with the dietitian, the number of calories and type of
nutrients needed to meet nutrition requirements.
Ascertain patient’s food preferences to determine extent of the problem and plan
appropriate interventions.
Provide patient with high-protein, high-calorie, nutritious finger foods and drinks
that can be readily consumed because hyperthyroidism increases metabolic rate
with resulting need to prevent muscle breakdown and weight loss.
Offer snacks (e.g., frequent drinks, fresh fruits/juice) to maintain adequate caloric
intake.
Monitor recorded intake for nutritional content and calories to evaluate nutritional
status.
Weigh patient at appropriate intervals to evaluate effectiveness of nutritional plan.
Provide appropriate information about nutritional needs and how to meet them topromote self-care.
Assist the patient in receiving help from appropriate community nutritional programs.
2.6.3. Weight Management
Discuss with individual the medical conditions that may affect weight to reassure
patient that optimal weight can be maintained with treatment of hypothyroidism.
Discuss with individual the relationship between food intake, exercise, weight gain,
and weight loss to promote understanding of weight management.
Determine the individual’s ideal body weight to plan weekly weight loss goals.
Assist in developing well-balanced meal plans consistent with level of energy
expenditure.
Develop with the individual a method to keep a daily record of intake, exercise
sessions, and/or changes in body weight to promote progress toward final goal.
2.6.4. Constipation/Impaction Management
Encourage increased fluid intake (e.g., 2-3 L of fluids per day) to maintain soft stool.
Instruct patient/family on high-fiber diet to increase knowledge of how to increase
fecal mass.
Monitor bowel movements, including frequency, consistency, shape, volume, and
color, to plan appropriate interventions.
Suggest use of laxatives/stool softeners to stimulate bowel evacuation.
Teach patient/caregivers about timeframe for resolution of constipation because
elimination patterns will improve with treatment of hypothyroidism.
2.6.5. Reality Orientation
Monitor for changes in orientation, cognitive and behavioral functioning, and quality
of life to determine appropriate interventions.
Inform patient of person, place, and time to decrease confusion.
Provide a low-stimulation environment for patient in whom disorientation is increased
by overstimulation.
Speak to patient in slow, distinct manner with appropriate volume to allow patient
to understand.
Avoid requests that exceed the patient’s capacity (e.g., abstract thinking when
patient can think only in concrete terms, decision making beyond preference or
capacity) to decrease frustration and loss of self-esteem.Use environmental cues (e.g., signs, pictures, clocks, calendars) to maintain
orientation to time and day.
2.6.6. Infection Protection
Monitor for systemic and localized signs and symptoms of infection so infection can
be detected early and treatment initiated promptly.
Provide private room.
Maintain asepsis for patient at risk.
Screen all visitors for communicable diseases to reduce the risk of infection
exposure.
Monitor absolute granulocyte count, WBC count, and differential results to detect
infection and plan treatment.
Obtain cultures as indicated to identify and treat infectious organisms.
Inspect skin and mucous membranes for redness, extreme warmth, or drainage
because other signs and symptoms of infection may be minimal or absent.
Teach patient and family members how to avoid infections (e.g., hand washing).
Teach the patient and family about signs and symptoms of infection and when to
report them to the health care provider.
2.6.7. Self-Esteem Enhancement
Encourage patient to identify strengths to promote awareness of capabilities.
Reinforce the personal strengths that patient identifies.
Make positive statements about the patient to boost morale by providing positive
feedback.
Encourage increased responsibility for self to improve patient’s appearance and
self-esteem.
2.6.8. Teaching: Disease Process
Provide reassurance about patient’s condition (e.g., explaining physical and
emotional changes will resolve with hormonal balance) to increase their
understanding and assist with coping.
2.6.9. Skin Surveillance
Observe extremities for color, warmth, swelling, pulses, texture, edema, and
ulcerations for early detection of skin impairment.
Monitor for sources of pressure and friction to prevent injury to easily traumatized
tissue.
Monitor skin for rashes and abrasions to promote early treatment.
Monitor skin and mucous membranes for areas of discoloration, bruising, and
breakdown to provide early treatment.
Document skin or mucous membrane changes to provide early intervention.
2.6.10.Skin Care: Topical Treatments
Provide support to edematous areas to promote circulation to edematous areas.Use devices on the bed (e.g., sheepskin) that protect the patient.
Self-assessment 2.6
1) Outline 5 action of nurse in prevention of infection for the patient with
endocrine disorders.
2) The nurse should ensure skin Surveillance in order to
a. Maintain skin color
b. Detect early signs of skin impairment.c. Keep the skin clean
End unit assessment 2
1) Explain the hormones produced by each gland in the diagram above and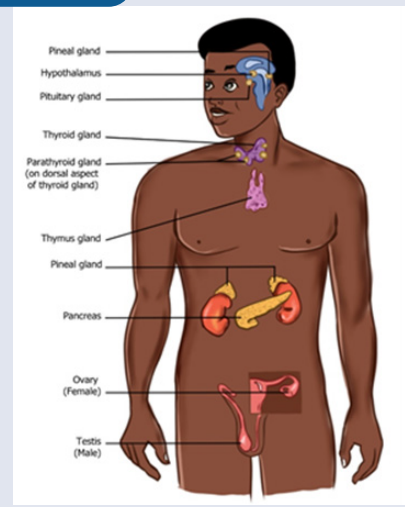
its role in human body.
2) What is the result of overproduction and hypo production of each gland
shown in this diagram in human body?
3) Explain the component of history taking in endocrine assessment4) Observe the table below and match a disease with its cause