UNIT4:PROMOTION OF HEALTH IN CHILDREN
Key Unit competence
Provide promotional activities for the wellbeing of a child
Introductory activity 4
At health center, a nurse receives a 24 months old child brought by his mother,
after he fell down from the bed this morning when he was crawling on the bed.
The mother told the nurse that when the child wakes up, he doesn’t pull himself
to standing position and crawls. The mother said that his child is the last born
in the family and she has other 2 children with 9 and 5 years respectively. The
child was born with 1.8kgs at 35 weeks of gestational age and delayed to cry for
about 15 min that led him to be admitted in neonatology for 42 days. The child
was fed with cow’s milk from the second day of life as the mother was unable to
breast feed. The nurse examined the child to see if there was no broken bone.
While the child was on the examination table, his head was supported by his
mother as he was unable to sit alone without being supported. The nurse only
noticed ecchymosis on the right arm but there was no broken bone.
Based on your knowledge, discuss the growth and development in gross motor
of the child in the scenario above
Health promotion in children aims to keep children healthy with a focus on early
interventions and implementing programs for the youngest children. The early
years of a child’s life lay the foundation for future physical, cognitive, emotional,
and social development.
Children’s health and well-being is influenced by a variety of factors, including
family characteristics, community dynamics, and other social determinants of health
(SDOH). These include systems, policies, and environmental conditions in which
children are born and grow up.
4.1 Key Concepts used in child health
Learning activity 4.1
Using different sources of information discuss the following concepts:
– Pediatric
– Child
– Adolescen
4.1.1 Pediatric
Branch of medicine that deals specifically with children, their development, childhood
diseases and their treatment.
4.1.2 Pediatric nursing
This is the art and science of giving nursing care to children from birth through
adolescent with emphasis on the physical growth, mental, emotional and
psychosocial and spiritual development of the child. It focuses on providing holistic
care to infants, children and adolescent.
4.1.3 Child
Biologically, a child is a human being between the stages of birth and puberty,
or between the developmental period of infancy and puberty. The United Nations
Convention on the Rights of the Child (UNCRC) defines a child as everyone under
18 years old.
4.1.4 Childhood
The period of life of the human being considered to extend from infancy to puberty.
4.1.5 Infant
Infant is defined as a child under the age of 1 year.
4.1.6 Toddler
A toddler is a child approximately 12 to 36 months old, though definitions vary; the
toddler years are a time of great cognitive, emotional and social development. The
word is derived from “to toddle”, which means to walk unsteadily, like a child of this
age.
4.1.7 Child health care
Specialized branch of medicine that promotes child health, prevent child illness,
care of the ill, disabled and dying child from birth through adolescent to maintain
physical, emotional and social wellbeing of that individual or child.
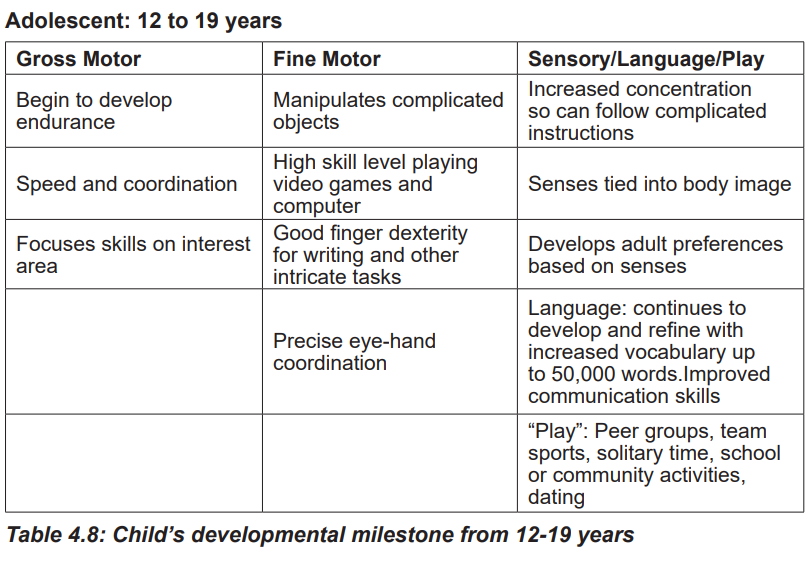
4.1.8 Adolescent
Adolescence is a transitional stage of physical and psychological development that
generally occurs during the period from puberty to legal adulthood. Adolescence is
the phase of life between childhood and adulthood, from ages 10 to 19. It is a unique
stage of human development and an important time for laying the foundations of
good health.
4.1.9 Health
Health, according to the World Health Organization, is “a state of complete physical,
mental and social well-being and not merely the absence of disease and infirmity.”
4.1.10 Family centered care
Family-centered care is a way of providing services that assures the health
and well-being of children and their families through respectful family/
professional partnerships. It honors the strengths, cultures, traditions, and
expertise that families and professionals bring to this relationship.
4.1.11 Atraumatic care
Atraumatic care is the philosophy of providing therapeutic care through the
use of interventions that eliminate or minimize the psychological and physical
distress experienced by children and families.
4.1.12 Health promotion
Health promotion is the process of enabling people to increase control over, and
to improve, their health. It moves beyond a focus on individual behavior towards a
wide range of social and environmental interventions.
Self-assessment 4.1
– Identify the differences between pediatrics and pediatric nursing.
– Describe infant, toddler and adolescent periods.
4.2 Monitoring of growth and development
Growth monitoring is a process of following the growth of a child compared with
a standard by periodic frequent anthropometric measurements and assessments.
Growth monitoring and promotion is a preventive and promotional activity. It
facilitates communication and interaction between health care providers and care
givers so as to encourage appropriate timely intervention to promote optimal child
development and growth.
The main purpose of growth monitoring is to assess growth adequacy and identify
changes at early stages before the child reaches the status of under nutrition.
Weight gain is the most important sign that a child is healthy and is growing and
developing well. Also, a health check-up can detect if a child is gaining weight too
fast or too slow in comparison to his/her age
4.2.1 Steps involved in growth monitoring
5 major steps in growth monitoring are:
Step 1: Determining correct age of the child
Step 2: Accurate weighing of the child
Step 3: Plotting the weight accurately on a growth chart of appropriate gender
Step 4: Interpreting the direction of the growth curve and recognizing if the child is
growing properly.
Step 5: Discussing the child’s growth and follow up action needed with the mother.
4.2.2 Growth charts: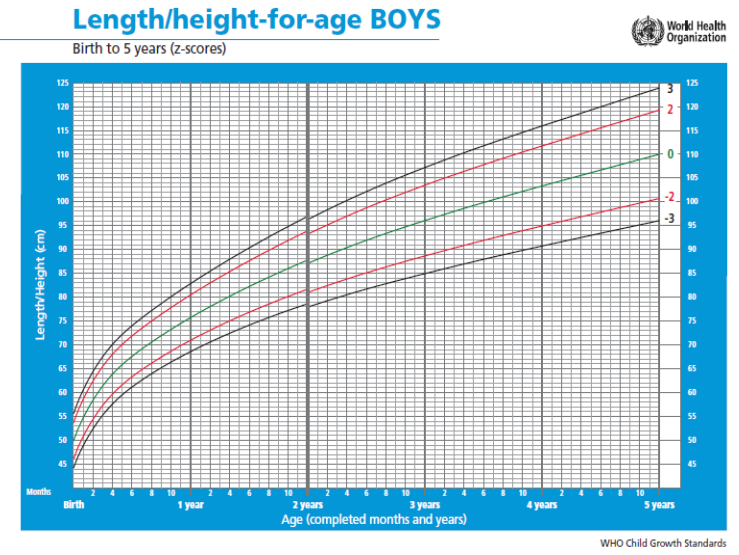
Figure 4.1: Height for age chart for boys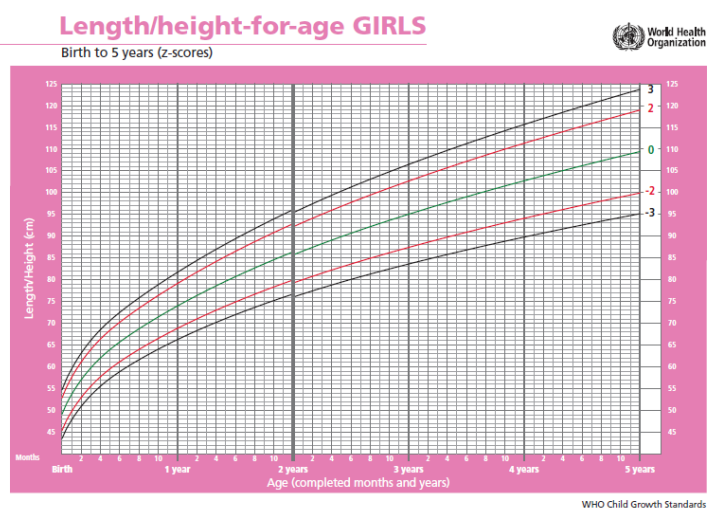
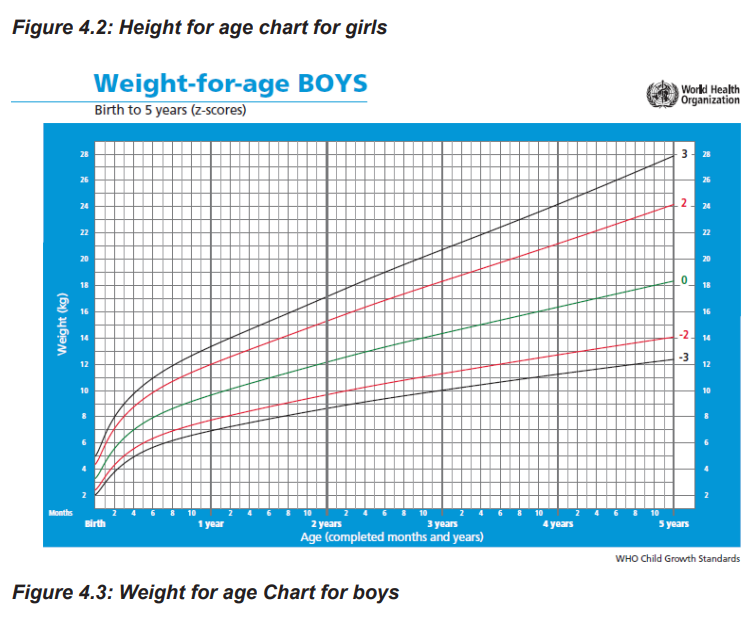
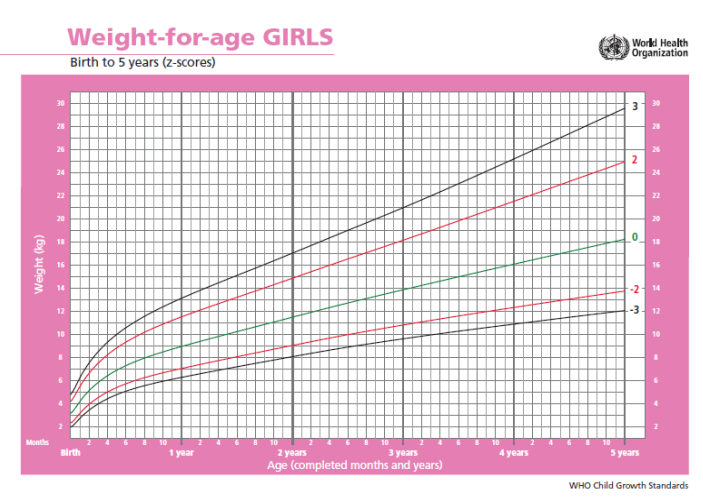
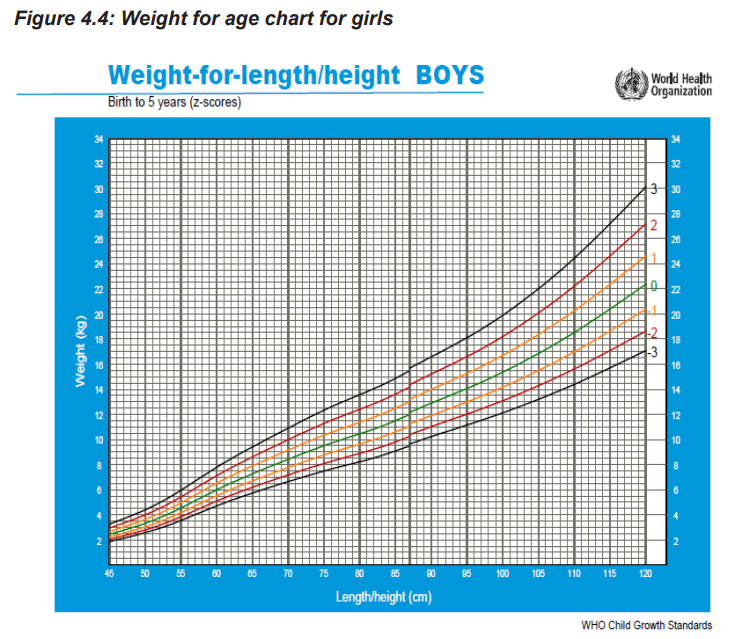
Figure 4.5: Weight for height chart for boys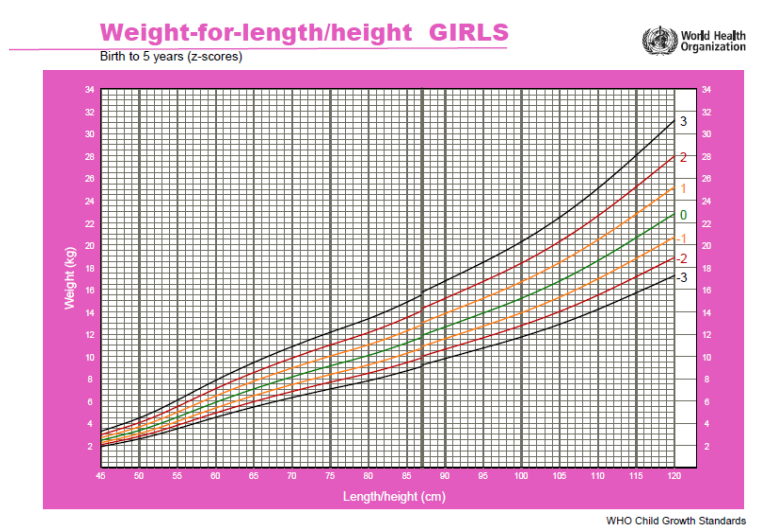
Figure 4.6: Weight for height chart for girls
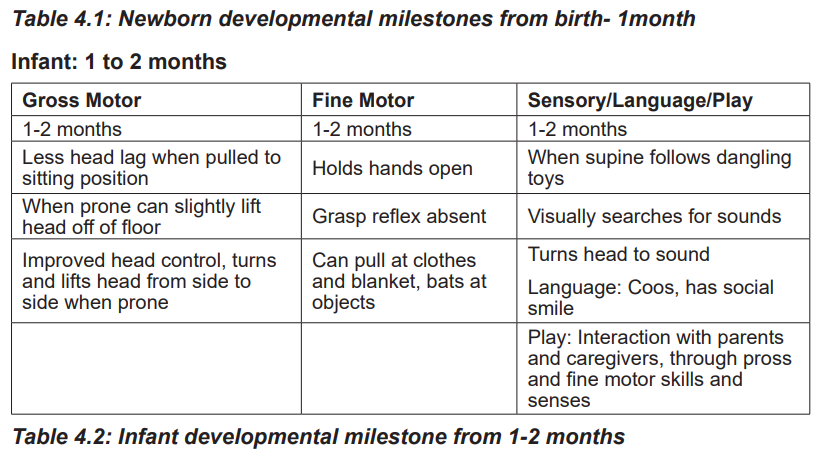
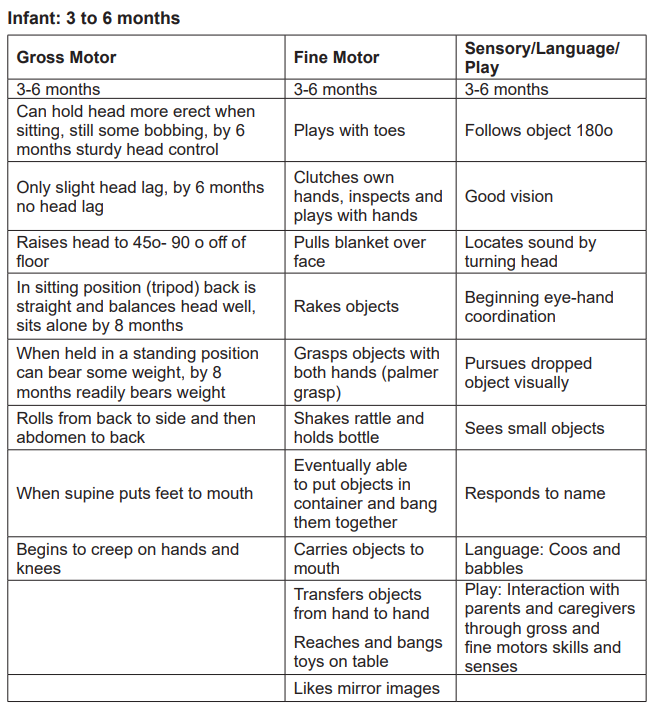
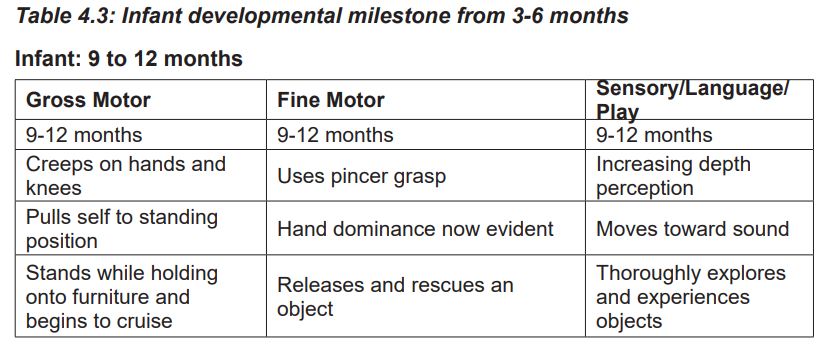
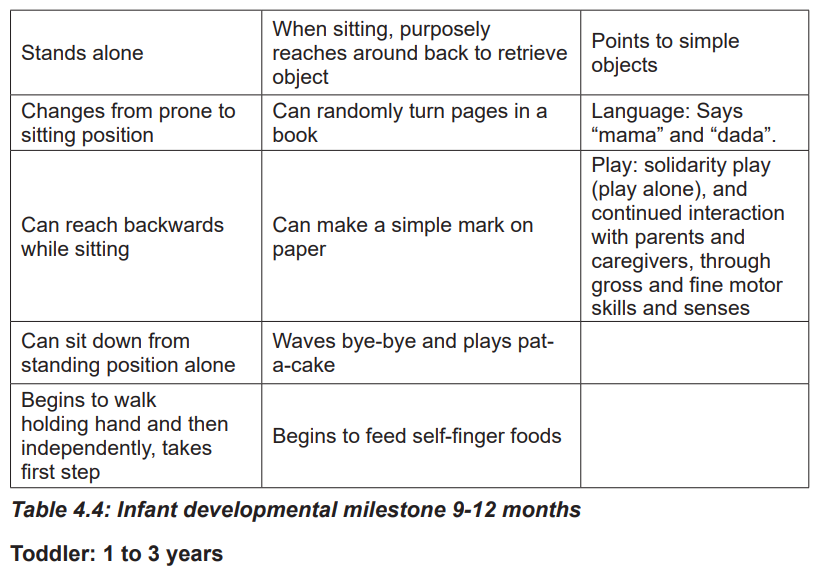
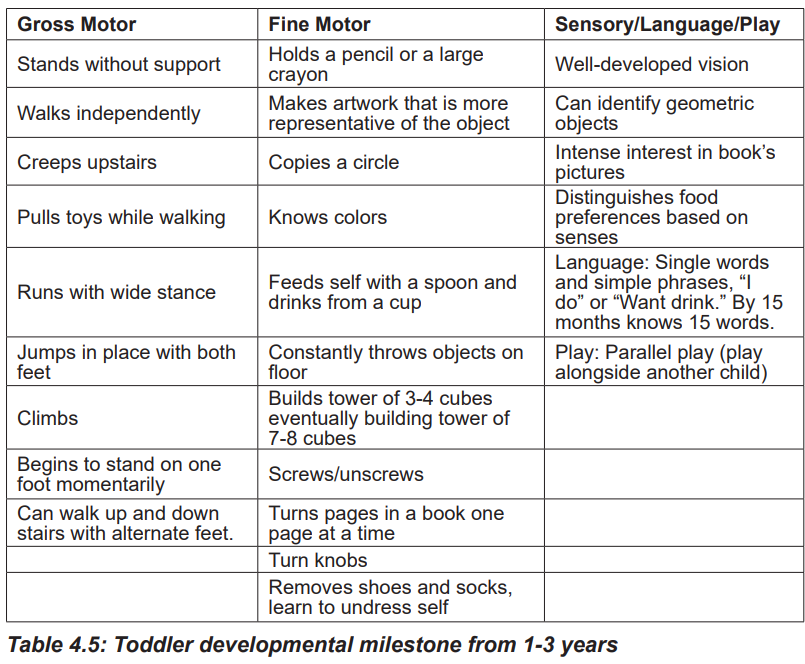
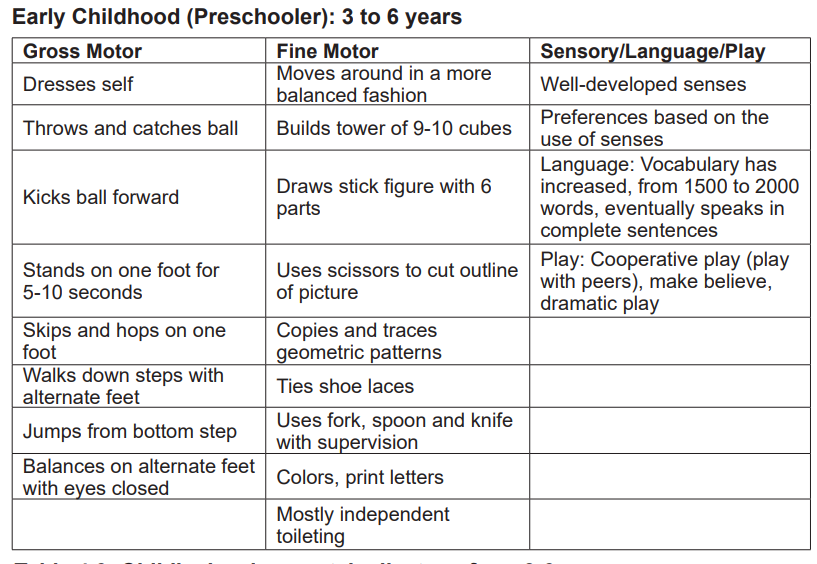
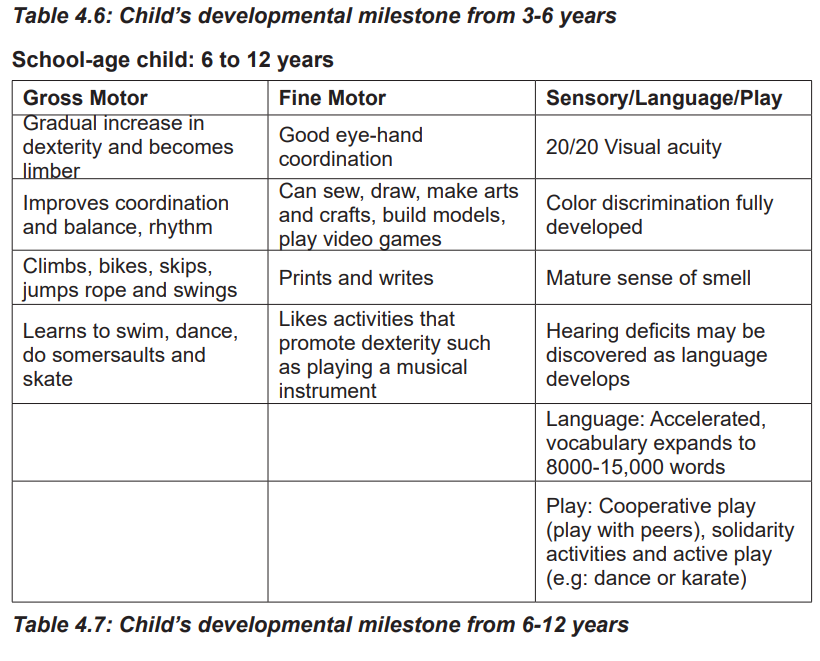
Stages of child development (developmental milestones)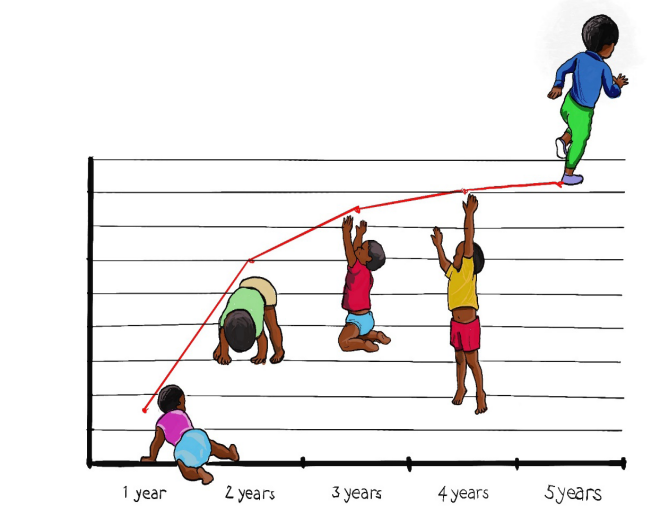
Figure 4.7: Stages of child development
Children undergo various changes in terms of physical, speech, intellectual and
cognitive development gradually until adolescence. Specific changes occur at
specific ages of life. Known as developmental milestones, these changes can
help to identify if the child is developing at the correct pace. Failure to reach these
milestones may indicate developmental disorders or genetic conditions.
Developmental milestones are behaviors or physical skills seen in infants and
children as they grow and develop. Rolling over, crawling, walking, and talking are
all considered as milestones. The milestones are different for each age range.
4.2.3 Child development theories
Child development theories focus on explaining how children change and grow over
the course of childhood. Such theories center on various aspects of development
including social, emotional, and cognitive growth.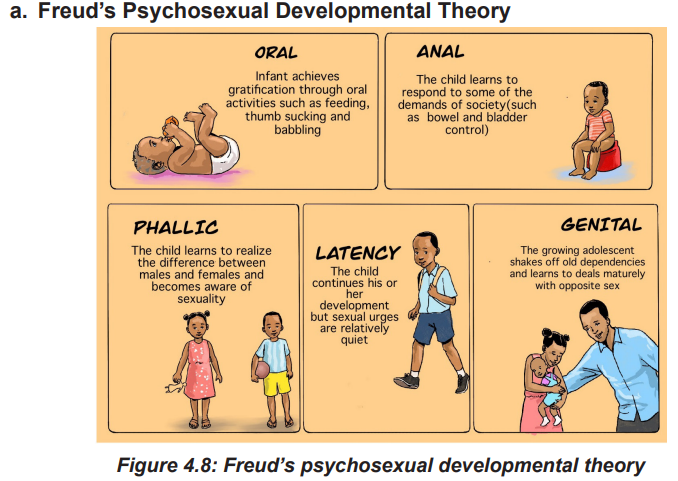
Psychoanalytic theory originated with the work of Sigmund Freud. Through his
clinical work with patients suffering from mental illness, Freud came to believe that
childhood experiences and unconscious desires influenced behavior.
According to Freud, conflicts that occur during each of developmental stages can
have a lifelong influence on personality and behavior. The child development occurs
in a series of stages focused on different pleasure areas of the body. During each
stage, the child encounters conflicts that play a significant role in the course of
development.
His theory suggested that the energy of the libido was focused on different erogenous
zones at specific stages. Failure to progress through a stage can result in fixation at
that point in development, which Freud believed could have an influence on adult
behavior. While some other child development theories suggest that personality
continues to change and grow over the entire lifetime, Freud believed that it was
early experiences that played the greatest role in shaping development. According
to Freud, personality is largely set in stone by the age of five.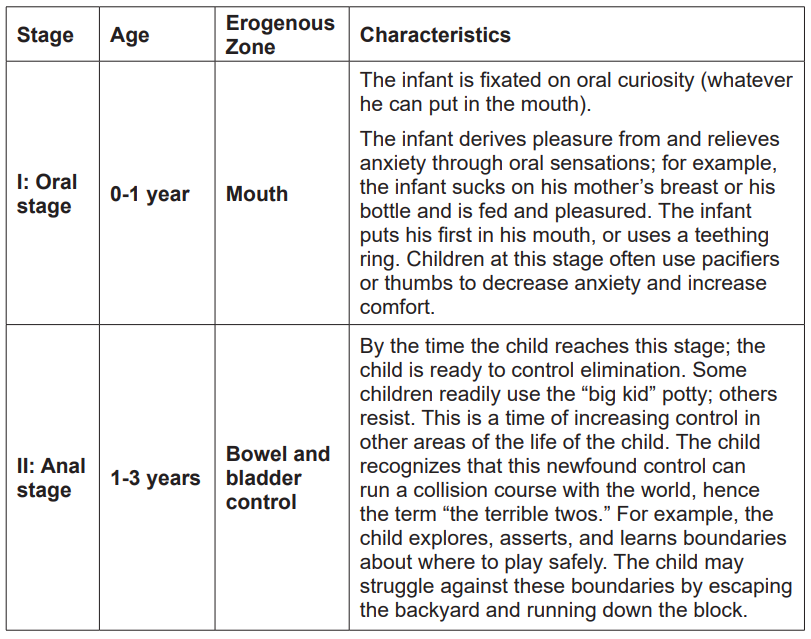
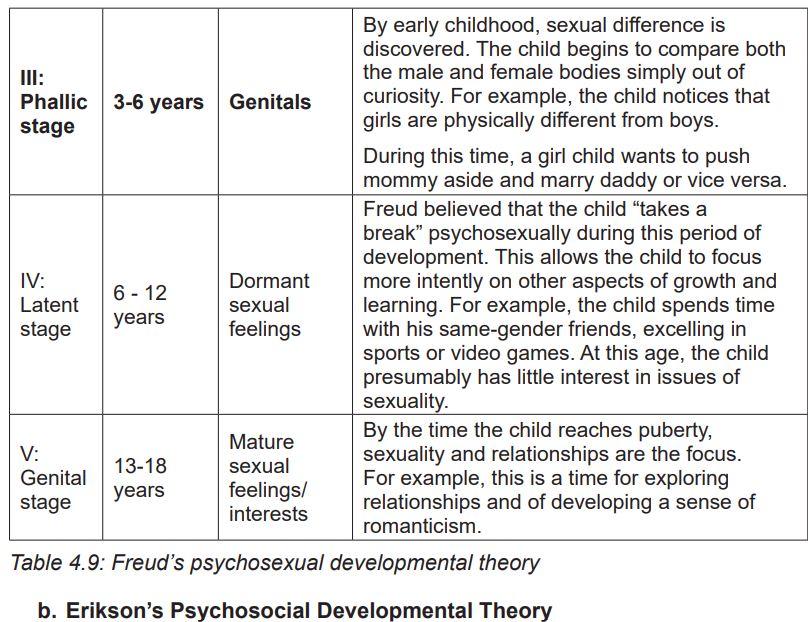
Figure 4.9: Erikson’s psychosocial developmental theory
Erikson’s eight-stage theory of psychosocial development describes growth and
change throughout life, focusing on social interaction and conflicts that arise during
different stages of development.
His eight-stage theory of human development described this process from infancy
through death. There are 5 stages in childhood until adolescence as stages are
based on the age. During each stage, people are faced with a developmental
conflict that impacts later functioning and further growth. At each stage, children
face a developmental crisis that serves as a major turning point:
A. Trust versus Mistrust
Trust versus mistrust occurs between birth and 1 year. The task of this stage
is for the baby to recognize that there are people in his life, generally parents
that can be trusted to take care of basic needs. The baby’s struggle becomes
evidenced in the recognition that not everyone or every situation is “safe.” Through
trust the baby learns to have confidence in personal worth and well-being along
with connectedness to others. Failure to master this stage leaves a sense of
hopelessness and disconnectedness.
B. Autonomy versus Shame and Doubt
Autonomy versus Shame and Doubt occurs between 1 and 3 years. The task of
this stage is for the child to balance independence and self-sufficiency against the
predictable sense of uncertainty and misgiving when placed in life’s situations. It
is the time for the child to establish willpower, determination, and a can-do attitude
about self. An example of this stage happens when the toddler wants to choose
clothing and dress independently. The struggle happens when the parents allow
the child to make personal choices yet expect the choices to be socially acceptable.
C. Initiative versus Guilt
Initiative versus guilt occurs between 3 and 6 years. The child’s task during this
stage is to develop the resourcefulness to achieve and learn new things without
receiving self-reproach. It is difficult for a young child to resolve the conflict between
wanting to be independent and needing to stay attached to parents. The child’s
writing plays or new songs, games, or jokes are good examples of initiative.
The child feels confident to try new ideas. It is important that parents and teachers
encourage this initiative to help the child develop a sense of purpose. If initiative is
discouraged or ignored, the child may feel guilt and lack of resourcefulness.
D. Industry versus Inferiority
Industry versus inferiority occurs between the ages of 6 and 12. In this stage, the
child develops a sense of confidence through mastery of tasks. This sense of
accomplishment can be counterbalanced by a sense of inadequacy or inferiority
that comes from not succeeding. The realization that the child is competent is one of
the important building blocks in the development of self-esteem. Industry is evident
when the child is able to do homework independently and regulate social behavior.
Performing the prescribed tasks at school or home also show industry. If the child
cannot accomplish realistic expected tasks, the feeling of inferiority may result.
E. Identity versus Role Confusion
Identity versus role confusion occurs between the ages of 12 and 18. This is
a time of forging ahead and acquiring a clear sense of self as an individual in
the face of new and at times conflicting demands or desires. During this stage
the adolescent wants to define “what to be when I grow up.” She begins to
concentrate on goals and life plans separate from those of peers and family.
At this point, the child has the ability to think about self as well as others and
proceeds accordingly.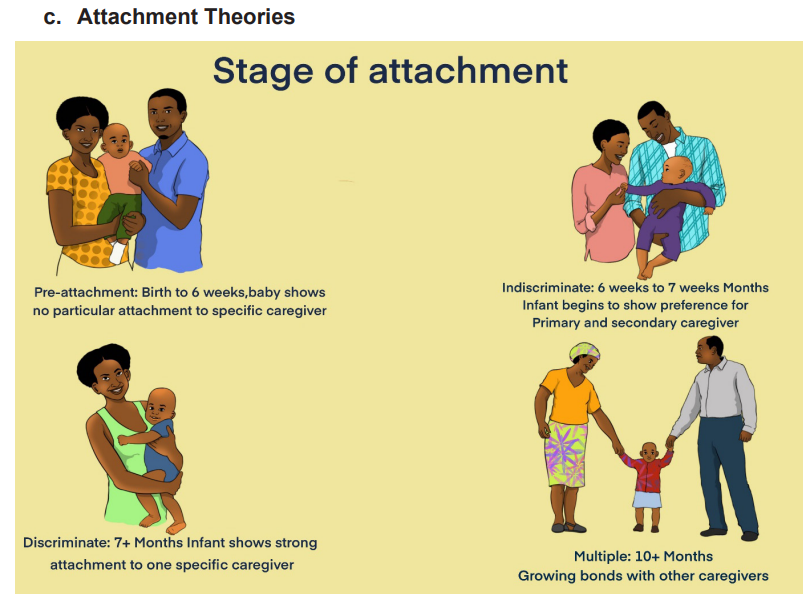
Figure 4.10: Attachment theories
Attachment refers to the bond or emotional and physical connection that develops
between an infant and caregiver that tends to endure. Early theorists associated
attachment with the mother who met the infant’s innate drive to be fed and nurtured.
Other examples of attachment behaviors are dressing, bathing, diapering, cuddling,
loving, playing, and comforting.
Both the infant and the caregiver rely on the quality of the interaction between
them. In other words, a healthy infant–mother relationship is contingent on the
characteristic value of the communication between them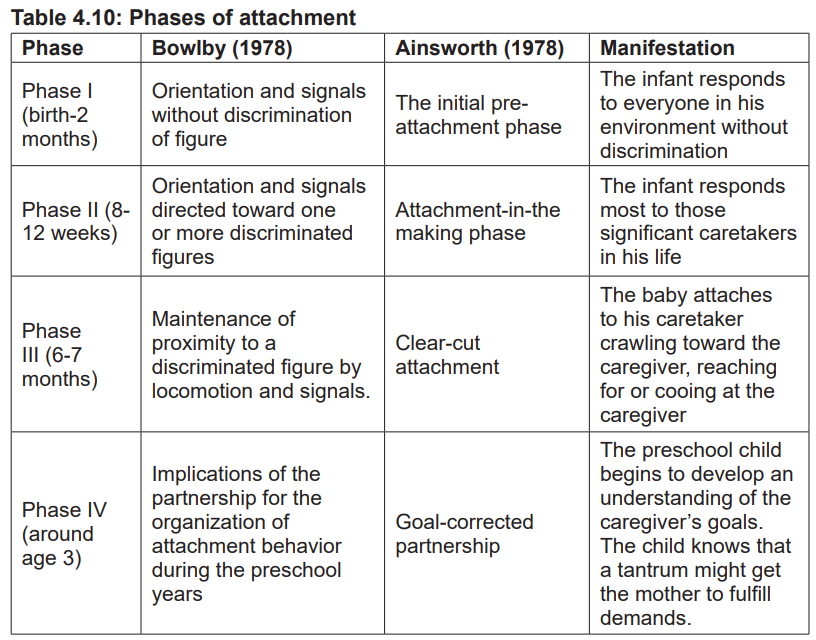
Self-assessment 4.2
1. Enumerate the steps involved in growth monitoring.
2. Describe the oral stage of Freud’s psychosexual developmental theory.
3. Discuss any 2 stages of Erikson’s psychosocial developmental theory.
4.3 Nutrition in children
Learning activity 4.3
Identify the differences between the two babies on the picture below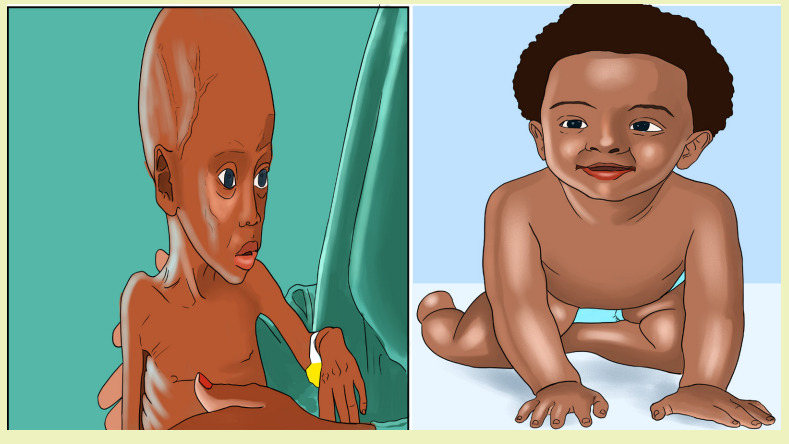
The questions a healthcare provider asks regarding nutrition are based on the
child’s age. If the infant is breastfed, information is gathered as to how often and for
how long the child is fed at each feeding, and how many wet diapers are changed
in the course of one day. With sufficient breast milk intake, the infant will have six or
more wet diapers and gain weight. Newborns often lose 10% of their birth weight.
This weight loss is usually by the 12th day of life.
For the infant who is receiving formula, information is gathered as to the type of
formula, the amount taken at each feeding, and the number of feedings per day. It
is also important to note if and when juices or solid foods have been started, and
whether supplements or vitamins have been prescribed.
When assessing children and adolescents, a 24-hour recall elicits the food items
eaten in a typical day and reflects sociocultural trends. The nurse can document
the amount and type of milk, juices, and all other liquids. In addition, the healthcare
provider must document food allergies for all children. Analysis of the food intake is
compared to the foods suggested in the Food Guide Pyramid for Young Children.
4.3.1 Importance of nutrition in children
Proper nutrition supports normal growth, development and aging. It also helps to
maintain a healthy body weight and reduces the risk of chronic diseases.
For children, adequate nutrition is one of the most important factors influencing
growth and immunity. A balanced diet must contain the proper amount of
protein, carbohydrate, fats, calcium, iron, vitamins and fiber. The foundation for
lifelong health is largely set during the first 1,000 days (this is the most critical
developmental period of brain growth and function). It is widely recognized as a
time of enormous vulnerability but also a time of tremendous potential to impact the
long-term health of the child. Due to the specific nutritional requirements during this
rapid period of growth, even small nutritional deficits may negatively impact growth,
neurodevelopment and adult health.
4.3.2 Nutrition screening and assessment
Nutrition screening is a rapid and simple identification of children who may be
malnourished or at risk of malnutrition and need more detailed nutrition assessment.
Nutrition screening requires standardized training in line with national and local
health policy.
Nutrition assessment includes taking anthropometric measurements and collecting
information about a child’s medical history, clinical and biochemical characteristics,
dietary practices, current treatment and food security situation.
Importance of nutrition assessment is to:
1. Identify children at risk of malnutrition for early intervention or referral before
they become malnourished.
2. Identify malnourished children for treatment- malnourished children who are
not treated early have longer hospital stay, slower recovery from infection
and complications and higher mobility and mortality.
3. Track child growth.
4. Identify medical complications that affect the body’s ability to digest food
and utilize nutrients.
5. Detect practices that increase the risks of malnutrition and infections.
6. Inform nutrition education and counselling.
7. Establish appropriate nutrition care plan.
Nutrition assessment should be done in:
• Infants 0 to <6 months of age: at birth and on every scheduled postnatal
visit
• Infants 6 to 59 months of age: during monthly growth monitoring sections
for children under 2 and every 3 months for older children.
• Children of 5 years and above: on every clinic visit.• Adolescents: on every clinic visit
4.3.3 Types of nutrition assessment
Types of nutrition assessment are remembered with mnemonics ABCD:
A: Anthropometric is the measurement of the size, weight and proportion of the body.
Common anthropometric measurement include weight, height, MUAC (Mid Upper
Arm Circumference), head circumference and skin folds. Body mass index (BMI)
and weight-for-height are anthropometric measurements presented as indexes.
B: Biochemical means checking level of nutrients in a child’s blood, urine or stools.
Lab tests results can give useful information about medical problems that may
affect appetite or nutritional status.
C: Clinical assessment includes checking for visible signs of nutritional deficiencies
such as bilateral pitting edema, emaciation (a sign of wasting, which is a loss of
muscle and fat tissue as a result of low energy intake and/or nutrients loss from
infection), hair loss, and change in hair color. It also includes taking a medical
history to identify co-morbidities with nutritional implications, opportunistic infections,
other medical complications, usage of medications with nutritional related side
effects, food and drug interactions and risk factors for disease, inability to suck andineffective breastfeeding.
Figure 4.11: Pitting edema on feet
Bilateral pitting edema also called nutritional edema is a swelling in both feet
or legs (bilateral) caused by accumulation of excess fluid under the skin in the
spaces within tissues. It is a sign of severe malnutrition on its own regardless of
the results of anthropometric assessment. Any child with severe bilateral pitting
edema (grade+++), even with appetite and no medical complications should be
admitted for inpatient management. A child with bilateral pitting edema Grade+ or
++ with appetite and no medical complications should be treated for severe acute
malnutrition.
D: Dietary: assessing food and fluid intake is an essential part of nutrition
assessment. It provides information on dietary quantity and quality, changes in
appetite, food allergies and intolerance, and reasons for inadequate food intake
during and after illness. To counsel the parents how to improve their diet to prevent
malnutrition or treat conditions affected by food intake and nutritional status examplecardiovascular disease, cancer, obesity, diabetes and hyperlipidemia
4.3.4 Various forms of malnutrition
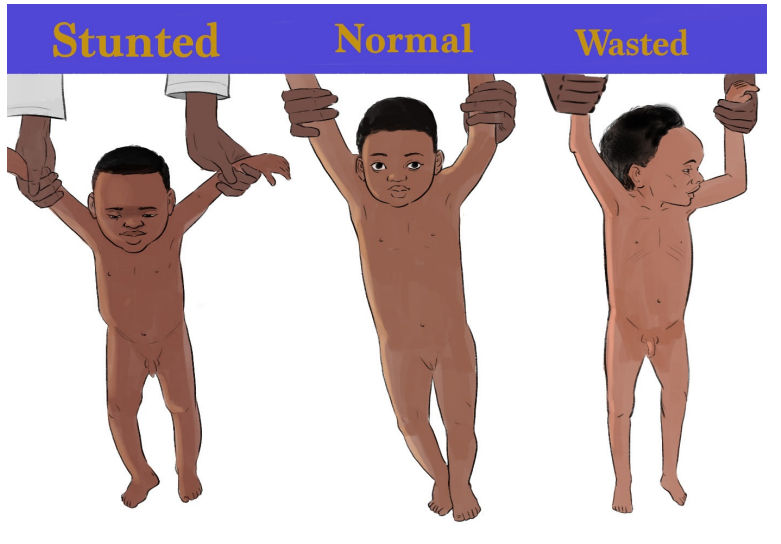
Figure 4.12: Various forms of malnutrition
a. Undernutrition
There are 4 broad sub-forms of undernutrition: Wasting, stunting, underweight and
deficiencies in vitamins and minerals. Undernutrition makes children in particular
much more vulnerable to disease and death.
Low weight-for-height is known as wasting. It indicates recent and severe weight
loss because the child has not had enough food to eat and/or they have had an
infectious disease such as diarrhea which has caused them to lose weight and thismay lead this to increase risk of death but treatment is possible.
Low height-for-age is known as stunting. It is the result of chronic reoccurrence
undernutrition usually associated with poor socioeconomic conditions, poor
maternal health and nutrition, frequent illness and/or inappropriate infant and young
child feeding and care in early life. Stunting holds children back from reaching theirphysical and cognitive potential.
Children with low weight-for-age are known as underweight. A child who isunderweight may be stunted, wasted or both.
b. Micronutrient related malnutrition
Micronutrients enable the body to produce enzymes, hormones and other
substances that are essential for proper growth and development. Iodine, vitamin
A and iron are the most important and their deficiency represents a major threat tothe health and development of the children.
Overweight and obesity result from an imbalance between energy consumed (too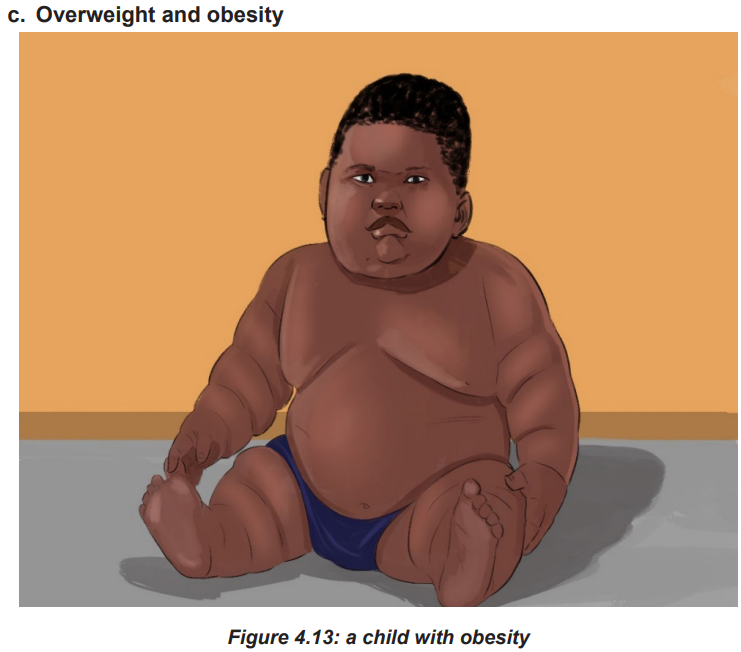
much) and energy expended (too little). Body mass index is an index of weight-forheight
commonly used to classify overweight and obesity. It is defined as a person’s
weight in kilograms divided by the square of his/her height in meters (kg/m2).Body Mass Index in children (BMI)
• A BMI-for-age plotted below the 5th percentile indicates a child who is
underweight;
• A BMI-for-age between the 5th and 85th percentile is considered a healthy
weight;
• Children with a BMI-for-age between the 85th and 95th percentile are
considered at risk for obesity;• Children with a BMI-for age _95% are considered obese.
Self-assessment 4.3
1. Discuss various forms of malnutrition.2. What are the elements of nutritional clinical assessment?
4.4 Assessment of a child: History taking
Learning activity 4.4
Children are not small adults. Taking a history with children differs from adults and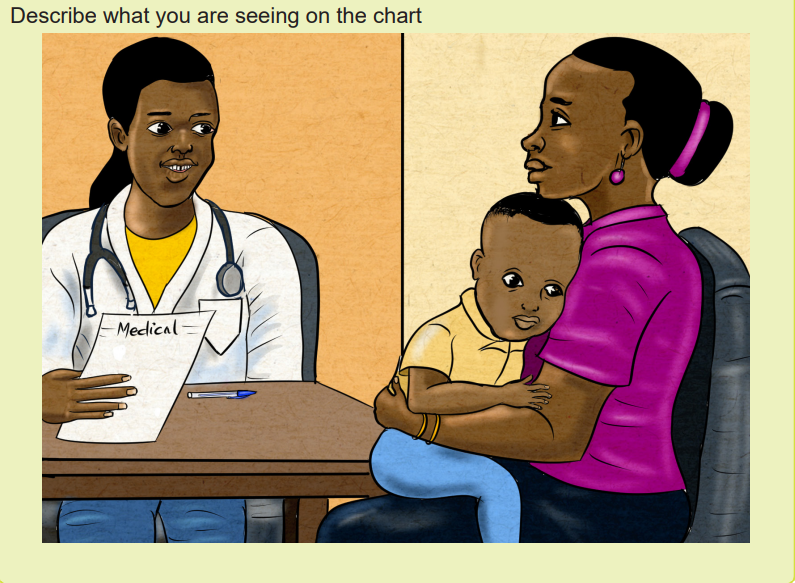
comes with a set of unique challenges. Symptoms are typically reported by a parent
or guardian, who may not be able to accurately transmit the information from the
child to the examiner and characterize the child’s concerns. To fill in the gaps, a
health care provider must have good communication skills and the ability to develop
a rapport with children as well as their families.
Taking a history from a patient is a skill necessary for examinations. It tests both
your communication skills as well as your knowledge about what to ask. Specificquestions vary depending on what type of history you are taking.
The basics components of a pediatric history
• Introduce yourself, identify your patient and gain consent from the parents
to speak with them. Should you wish to take notes as you proceed, ask the
patients permission to do so.
• Chief Complaint: brief statement of primary problem (including duration) that
caused family to seek medical attention.
• History of present illness: similar to history taking in adult population,
the history of present illness in pediatric history is to explore the patient’s
primary concerns, and must be tailored to the individual presenting complaint.
Generally, you will want to try to characterize the symptoms of concern and get
a sense of the onset, timing, aggravating and alleviating factors, associated
symptoms, and if anything, similar has happened to the patient before.
• Past History: The past history establishes a complete picture of the child’s
health to date, and should cover events from the prenatal period until the
child’s current presentation. The prenatal history includes inquiring about
maternal age, and number of previous pregnancies and the outcomes of
those pregnancies. It may be relevant to ask if the child is a product of natural
conception or if assistive reproductive technology was required. Ask about
whether prenatal care was accessed, medications used, substances and
toxins and if there were any abnormal results or concerns identified on routine
screening for infections and chronic diseases or ultrasounds. Additional
exposures that may be relevant include the mother’s occupation.
• Pregnancy and birth history:
• Maternal health during pregnancy: ask about bleeding, trauma,
hypertension, fevers, infectious illnesses, medications, drugs, alcohol,
smoking, rupture of membranes
• Gestational age at delivery
• Labor and delivery: length of labor, fetal distress, type of delivery (vaginal,
cesarean section), use of forceps, anesthesia, breech delivery
• Neonatal period: APGAR scores, breathing problems, use of oxygen, need
for intensive care, hyperbilirubinemia, birth injuries, feeding problems,
length of stay, birth weight.
• Growth History: Growth history is an important part of the pediatric history
as prolonged illness or chronic conditions may impact the child’s growth and
result in deviations from an established growth. When asking about growth
history, the pattern of growth, not just the child’s measurement at the present
is key as alterations in pattern of growth are often early signs of pathology.
Plot the child’s growth on a growth chart, and look at both numbers (z-scores)
and percentiles. It may be helpful to ask regarding growth and size of family
members, as marked deviations in a child’s growth from what is expected from
family trends could help in distinguishing constitutional or familial variants
from a pathologic growth pattern. Healthy children should achieve a minimum
growth velocity of 5 cm per year.
• Developmental History: Developmental history consists of the 5 domains
of child development: gross motor, fine motor, speech & language,
cognitive, and social/emotional development
• Ages at which milestones were achieved and current developmental
abilities - smiling, rolling, sitting alone, crawling, walking, running, 1st
word, toilet training, riding tricycle, etc
• School: present grade, specific problems, interaction with peers
• Behavior: enuresis, temper tantrums, thumb sucking, pica, nightmares
etc.
• Medical History:
• Previous hospital admissions with dates and diagnoses
• Major medical illnesses: cardiac disease, hypertension, stroke, diabetes,
cancer, abnormal bleeding, allergy and asthma, epilepsy.
• Major surgical illnesses, Trauma-fractures, lacerations, list operations
and dates
• Medication History: Medication history includes both prescription and
non-prescription medications such as over the counter medications,
vitamins and supplements. One commonly overlooked group of
medications is inhalers, so it might be helpful to ask specifically if the child
uses any inhalers. It is also important to ask specifically about herbal
or homeopathic remedies, as parents may not report this unless directly
asked. Additionally, do not forget to ask about allergies to any drugs, foods
or environmental triggers.
• Immunization History: Immunization history is an essential part of the pediatric
history. Ask if the child has received all of his/her routine immunizations, as
well as if the child has received any additional vaccines such as the seasonalinfluenza vaccine or travel immunizations. It may be relevant to ask when the
child last received a vaccination for various presentations including febrile
seizures or fever.
• Feeding History:
• Breast or bottle fed, types of formula, frequency and amount, reasons for any
changes in formula
• Solids: when introduced, problems created by specific types
• Family History: Family history may begin with clarifying ethnicity when
relevant, and then establishing if any medical conditions have occurred in the
family that may relate to the child’s current presentation. It may be helpful to
draw out a pedigree to better understand the health and relationships between
individuals in the family. Again, many items in this component of the pediatric
history may be sensitive, and it is important to approach these topics in an
open and non-judgmental manner. Mental retardation, congenital anomalies,
chromosomal problems, growth problems, etc.
• Social History: The social history includes parental employment status, any
financial issues, health coverage and drug plans, and family composition.
This part of the history may lead to discussion about the impact of the child’s
illness on both the child and the family, and can allow the care team to bettersupport the family
Self-assessment 4.4
– Identify elements to include in pediatric history taking– Why do we need to know prenatal history of pediatric patients?
4.5 Assessment of a child: Review of systems
Learning activity 4.5.1
A review of systems Much like the physical examination, the review of systems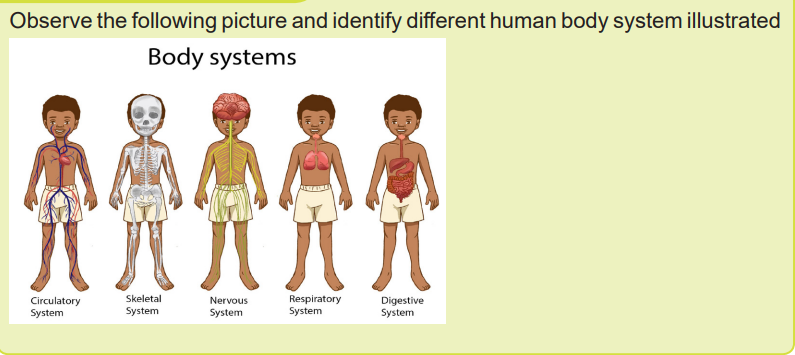
is best conducted with a “head-to-toe” approach, starting with a general question
regarding each body system. It can also be conducted by asking questions during
the physical examination.
It is a technique used by healthcare providers for eliciting a medical history from
a patient and often structured as a component of an admission note covering
the organ systems, with a focus upon the subjective symptoms perceived by the
patient (as opposed to the objective signs perceived by the clinician). Along with
the physical examination, it can be particularly useful in identifying conditions that
do not have precise diagnostic tests. The review of systems serves as a guide to
help identify potential or underlying illnesses or disease states subjectively, thus
allowing the health care provider to prioritize system for follow up and objective
examination. This will also help to obtain information about the chief concern as
well as the history of present illness.
Whatever system a specific condition may seem restricted to, it may be reasonable
to review all the other systems in a comprehensive history.
Review of systems includes the following areas:
a. General: usual weight, change in weight, weakness, fatigue, fever or
allergies.
b. Head, Eyes, Ears, Nose, Throat (HEENT): injury to head, headaches,
dizziness; eye infections, itching or watering eyes, behaviors indicating
change in visual acuity, use of glasses, date of last eye exam; ear
infections, behaviors indicating change in hearing; nose bleeds, colds,
hay fever, sinus infections; sore throats, tonsils, dentition, caries.
c. Neck: neck pain, enlarged lymph glands, neck range of motion
d. Skin and Lymph: rashes, adenopathy, lumps, bruising and bleeding,
pigmentation changes
e. Cardiac: cyanosis and dyspnea, heart murmurs, exercise tolerance,
squatting, chest pain, palpitations
f. Respiratory: pneumonia, bronchiolitis, wheezing, chronic cough, sputum,
hemoptysis, Tuberculosis
g. Gastro-Intestinal: stool color and character, diarrhea, constipation,
vomiting, hematemesis, jaundice, abdominal pain, colic, appetite
h. Genito-Urinary: frequency, dysuria, hematuria, discharge, abdominal
pains, quality of urinary stream, polyuria, previous infections, facial edema
i. Musculoskeletal: joint pains or swelling, fevers, scoliosis, myalgia orweakness, injuries, gait changes
j. Pubertal: secondary sexual characteristics, menses and menstrual
problems, pregnancies, sexual activity
k. Allergy: urticaria, hay fever, allergic rhinitis, asthma, eczema, drug
reactions
l. Neurological: seizures, tics, psychiatric diseases, anxiety, depression
m.Endocrine: history or symptoms of thyroid disease or diabetes or diseasesthat affect normal growth
Self-assessment 4.5
1. Describe the constitutional symptoms in the review of systems.2. Explain any 4 systems that can be reviewed during history taking.
4.6 Assessment of a child: Physical examination
Learning activity 4.6
1. What should be done during pediatric physical examination?2. Why is it relevant to perform pediatric physical examination?
In physical examination, medical examination or clinical examination, a medical
practitioner examines a patient for any possible medical signs or symptoms of a
medical condition. It generally consists of a series of questions about the patient’s
medical history followed by an examination based on the reported symptoms.
Together, the medical history and the physical examination help to determine a
diagnosis and devise the treatment plan. These data then become part of the
medical record.
Differences in Performing a Pediatric Physical Examination Compared to an
Adult:
I. General Approach
a. Gather as much data as possible by observation first
b. Position of child: parent’s lap vs. exam table
c. Stay at the child’s level as much as possible. Do not tower!!
d. Order of exam: least distressing to most distressing
e. Rapport with child:
– Include child - explain to the child’s level– Distraction is a valuable tool
f. Examine painful area last-get general impression of overall attitude
g. Be honest. If something is going to hurt, tell them that in a calm fashion.
Don’t lie or you lose credibility!
h. Understand developmental stages’ impact on child’s response. For
example, stranger anxiety is a normal stage of development, which tends
to make examining a previously cooperative child more difficult.
II. Vital signs
a. Normal differ from adults, and vary according to age
b. Temperature: Tympanic, oral, axillary and rectal
c. Heart rate: In infants, auscultate or palpate apical pulse or palpate femoral
pulse. In older children, palpate antecubital or radial pulse
d. Respiratory rate: Observe for a minute. Infants normally have periodic
breathing so that observing for only 15 seconds will result in a skewed
number.
e. Blood pressure: Appropriate size cuff - 2/3 width of upper arm
f. Growth parameters: must plot on appropriate growth curve (Weight,
Height/length, Occipital Frontal Circumference: Across frontal-occipital
prominence so greatest diameter).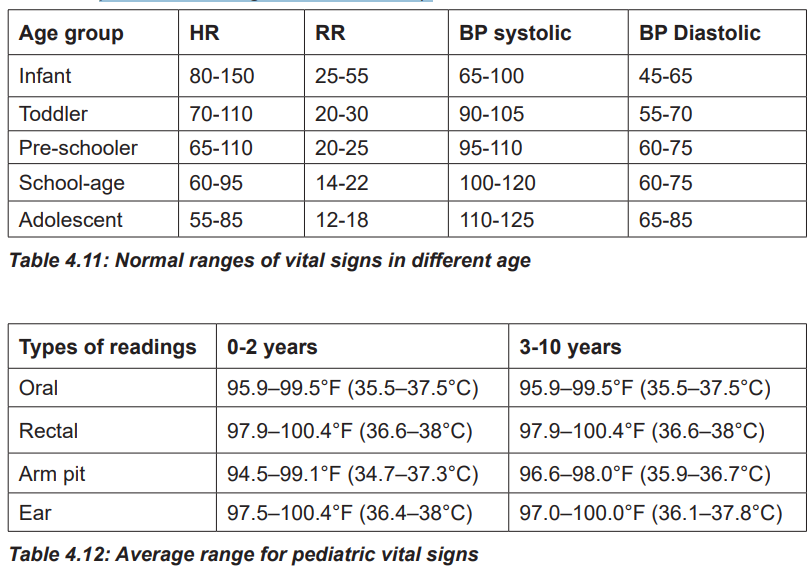
III. Unique findings in pediatric patients (See outline below)
Outline of a Pediatric Physical Examination
I. Vitals - see aboveII. General
a. Statement about striking and/or important features. Nutritional status, level
of consciousness, toxic or distressed, cyanosis, cooperation, hydration,
dysmorphology, mental state
b. Obtain accurate weight, height and OFC
III. Skin and Lymphatics
a. Birthmarks - nevi, hemangiomas, mongolian spots etc
b. Rashes, petechiae, desquamation, pigmentation, jaundice, texture, turgor
c. Lymph node enlargement, location, mobility, consistency
d. Scars or injuries, especially in patterns suggestive of abuse
IV. Head
a. Size and shape
b. Fontanelle(s): determine its Size in a calm environment and in the sitting
up position
c. Sutures - overriding
d. Scalp and hair
e. Eyes
• General: Strabismus, Slant of palpebral fissures, Hypertelorism or
telecanthus
• EOM
• Pupils
• Conjunctiva, sclera, cornea
• Plugging of nasolacrimal ducts
• Red reflex
• Visual fields - gross exam
f. Ears
• Position of ears: Observe from front and draw line from inner canthi to
occiput
• Tympanic membranes
• Hearing - Gross assessment only usually
g. Nose
• Nasal septum
• Mucosa (color, polyps)
• Sinus tenderness
• Discharge
h. Mouth and Throat
• Lips (colors, fissures)
• Buccal mucosa (color, vesicles, moist or dry)
• Tongue (color, papillae, position, tremors)
• Teeth and gums (number, condition)
• Palate (intact, arch)
• Tonsils (size, color, exudates)
• Posterior pharyngeal wall (color, lymph hyperplasia, bulging)
• Gag reflex
i. Neck
• Thyroid
• Trachea position
• Masses (cysts, nodes)
• Presence or absence of nuchal rigidity
j. Lungs/Thorax
• Inspection
• Pattern of breathing
Abdominal breathing is normal in infants
Period breathing is normal in infants (pause < 15 seconds)
• Respiratory rate
• Use of accessory muscles: retraction location, degree/flaring
• Chest wall configuration
• Auscultation
• Equality of breath sounds
• Rales, wheezes, rhonchi
• Upper airway noise
• Percussion and palpation often not possible and rarely helpful
k. Cardiovascular
• Auscultation
• Rhythm
• Murmurs
• Quality of heart sounds
• Pulses
• Quality in upper and lower extremities
L. Abdomen
• Inspection
• Shape
Infants usually have protuberant abdomens
Becomes more scaphoid as child matures
• Umbilicus (infection, hernias)
• Muscular integrity (diasthasis recti)
• Auscultation
• Palpation
• Tenderness - avoid tender area until end of exam
• Liver, spleen, kidneys: May be palpable in normal newborn
• Rebound, guarding: Have child blow up belly to touch your hand
M. Musculoskeletal
• Back
• Sacral dimple
• Kyphosis, lordosis or scoliosis
• Joints (motion, stability, swelling, tenderness)
• Muscles
• Extremities: Deformity, Symmetry, Edema and Clubbing
• Gait
• In-toeing, out-toeing
• Bow legs, knock knee: “Physiologic” bowing is frequently seen under 2
years of age and will spontaneously resolve
• Limp
• Hips: Ortolani’s and Barlow’s signs
N. Neurologic - most accomplished through observation alone
• Cranial nerves• Sensation
• Cerebellum
• Muscle tone and strength
• Reflexes: Deep Tendon Reflex, Superficial (abdominal and cremasteric),
Neonatal primitive
O. GU
• External genitalia
• Hernias and Hydrocoeles
• Almost all hernias are indirect
• Can gently palpate; do not poke finger into the inguinal canal
• Cryptorchidism
• Distinguish from hyper-retractile testis
• Most will spontaneously descend by several months of life
• Tanner staging in adolescents• Rectal and pelvic exam not done routinely
Self-assessment 4.5
• Enumerate sites for measuring body temperature.• Describe any 3 differences in physical examination of a child and adult.
4.7 Beliefs that affect Child health
Learning activity 4.7
Discuss different beliefs in your community that may affect the child health
It is observed that traditional healthcare practices and cultural beliefs have a
significant place and are widely used in all societies. Traditional cultural practices
reflect values and beliefs held by members of a community for periods often
spanning generations. Every social grouping in the world has specific traditional
cultural practices and beliefs, some of which are beneficial to all members, while
others are harmful to a specific group, such as children and pregnant women.
Health beliefs are what people believe about their health, what they think constitute
their health, what they consider the cause of their illness, and ways to overcome
their illness. These beliefs are culturally determined and all come together to form
larger health belief systems.
A. Cultural practices affect children’s and families’ conceptions of health, as well
as children social development, attitudes towards health problems they experienceconception of illness, reactions to illness and therapy.
Children learn their beliefs, values, capabilities, knowledge and skills from
their families and their culture. Furthermore, culture plays an important role in
socialization and development of children. Cultural background holds a significant
place in children’s social and emotional development, as well as improvement of
their motor and cognitive skills.
B. Religion
Along with cultural values, concepts of religion and spirituality hold a significant
place in lives of the individual and society. Although the terms ‘spirituality’ and
‘’religion’ are often used alternately, spirituality is inclusive of the concept of religion.
Religion is a factor that affects life style of the society and conception of health and
illness.
Religion is a concept that may affect individuals’ and society’s philosophy of life,
conceptions of health and illness, types of food consumed, rituals of birth and death,
and healthcare practices. Societies are found to use various religious practices
in care and treatment. Religious practices may have various effects on children’s
social and moral development. Healthcare practices based on religious and spiritual
values may play a significant role in shaping children’s and family’s lifestyle and
may have a great impact on children’s health. Various religions and sects are able
to affect children’s health and care practices, nutrition, and medical practices.Concepts affected by culture
C. Geographical region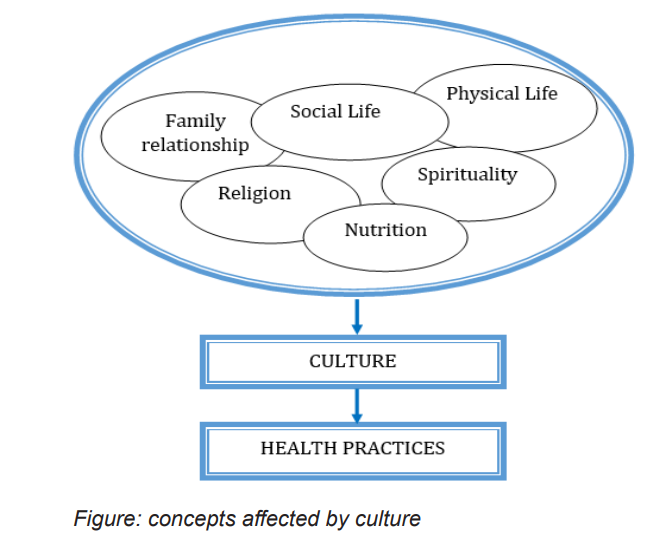
Child’s and family’s cultural values, as well as their environment of habitation result
in various differences in their conception and expression of health, illness, pain,
and their reflection to healthcare practices.
For example, it was observed in some rural areas in Africa that food items such
as eggs and meat were limited due to the fear that children may turn to thieves,
witches or sorcerers. It was detected that, in certain societies, there are differences
in individuals’ conception and attribution of meaning to verbal and non-verbal
communication.
Self-assessment 4.7
Discuss 2 concepts of culture and the way they can affect child’s health.4.8 Practices that affect Child health
Learning activity 4.8
1. Describe what you are seeing on the above picture and discuss different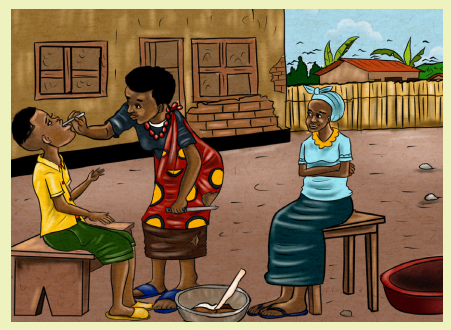
traditional practices that affect child health in your community
2. What is the impact of those practices to the child health?
Traditional practices
It is observed that individuals resort to traditional healthcare practices before
professional practices of care. It is noted that, in certain cultures the patients are
treated by individuals who are named traditional physicians or medicine man andwho are believed to possess divine Powers to cure illnesses.
It is observed that traditional healthcare practices and cultural beliefs have a
significant place and are widely used in all societies. According to current medical
knowledge, traditional methods applied to the child may be classified as practices
that adversely affect the child’s health and practices that have no adverse effect
on the child’s health. Among practices that may adversely affect the child’s health
are attitudes such as delaying breastfeeding for a certain time after childbirth, not
feeding the newborn with colostrum, coating the newborn with salt, placing soil
under the baby, and wrapping the baby tightly to make its legs grow straight. On
the other hand, practices such as placing a yellow kerchief on the baby’s face to
prevent newborn jaundice, to dress the baby with red-colored clothing, praying,
placing an evil eye talisman in the baby’s room are characterized as having no
adverse effect on the child’s health but may nevertheless be efficient in comforting
the family.
Health is influenced by culture which is a dynamic factor as well as biological
and environmental factors. Health practices are the outcome of health beliefs
generally originated from the culture of individual. Cultural practices of families
are directly related with the child health. Cultural practices affect children’s and
families’ conceptions of health, as well as children’s social development, attitudes
towards health problems they experience, conception of illness, reaction to illness
and therapy. There exist different practices that affect the child health. These are
named differently in Rwanda depending on the region. These includes Milk teeth
extraction (gukura ibyinyo), Uvulectomy (guca ikirimi), Tonsilectomy (guca
ibirato), Extracting millet (gukura uburo).Milk teeth extraction (Gukura ibyinyo)
Normally the development of deciduous teeth begins while the baby is in utero and
about sixth weeks gestation, the first buds of primary teeth appear in the baby’s
jaw. The lower teeth are formed first followed by the upper anterior teeth. At birth
the baby has a full set of 20 primary teeth (10 in upper jaw, 10 in lower jaw) hidden
within the gums. Crown formation of the milk canine tooth in the upper jaw (maxilla)
is complete 9 months and the crown formation of a deciduous canine tooth in the
lower jaw (mandible)is complete between 8 and 9 months after birth.
Milk teeth extraction is a process of gouging out an infant’s healthy baby canine buds
imbedded underneath the gums, using unsterile tools such as a hot or sharpened
nail, a bicycle spoke or knitting needle, with no anesthesia. It is a dangerous and
sometimes fatal traditional practice. Milk teeth extraction believed to cure a tooth
disease known as Ibyinyo. In reality, this so-called disease is the natural teething
stage that all babies go through, beginning at around 6 months of age. Teething
in babies causes mouth pain, fever and sometimes even vomiting or diarrhea,
prematurely extracting the teeth is not a cure, and causes serious permanentdamage of the child.
Uvulectomy (Guca ikirimi)
Uvulectomy consists of cutting the uvula which has a function of blocking the passage
into the nasal cavity when swallowing so that the foods or fluids do not enter the
nasal passages. The uvula also involves in articulation of voice to form sounds of
speech. When uvulectomy is performed, there is likelihood of an infant developing
the conditions of hypernasal speech known as velopharyngeal insufficiency (VPI)
and/or nasal regurgitation (entering of food into the nasal cavity).
Tonsilectomy (gukata ibirato)
It consists of cutting the baby’s tonsils.
Extracting millet (gukura uburo)
It consists of skin cuts that are performed on chest wall of some children claimed to
be the remedy for chest infections in infants.
A. Complications of traditional practices
All of those mentioned above traditional practices have different complications such
as loss of blood that may lead to shock later on Anaemia, blood infections, tetanus,
HIV/AIDS (because the materials used are not sterilized), facial disfigurement and
can be fatal. The underlying permanent tooth buds can be damaged or eradicated,
causing malformations and long-term crowding in the anterior region of the maxilla
and mandible.
B. Prevention
The prevention of traditional practices involves a multidisciplinary team. This
goes beyond changing particular beliefs and behaviors within communities and
societies: it is about fundamental social change. There is need of increased, access
especially for poor and vulnerable people, to all essential services, including health
and education, social welfare and legal services. The community needs a sound
understanding of the importance of religion, faith and other belief systems: how
they can support work to end traditional practices that are harmful to children.
Conclusion
Nurses should be cautious about the children’s and families’ cultural beliefs’ and
practices’ reflections on the child’s health. In this context, the individual should be
conceived in spiritual and psychosocial aspects from birth to death and holistic careshould be provided
Self-assessment 4.8
1. Discuss the complications of traditional practices that affect child health.
2. What is your role in the prevention of traditional practices that affect thechild health?
End unit assessment 4
1. What is health Promotion?
2. Which children should you monitor growth?
3. What does the psychosexual development theory of Sigmund Freud say
about the development of personality which is different from what was
said by other theorists?
4. Describe different types of nutritional assessment
5. Describe the elements assessed during the pediatric physicalassessment.
