UNIT 3: MEDICAL PATHOLOGIES OF THE NOSE
complaining:
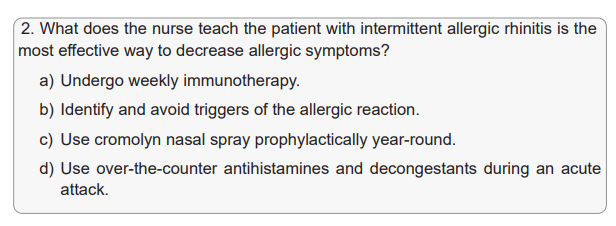
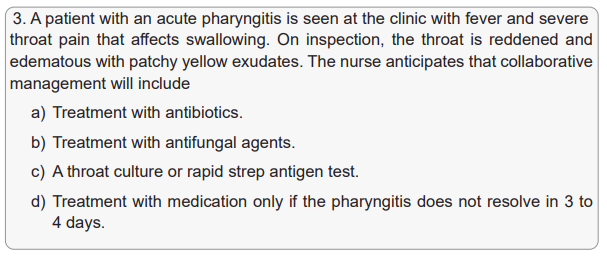
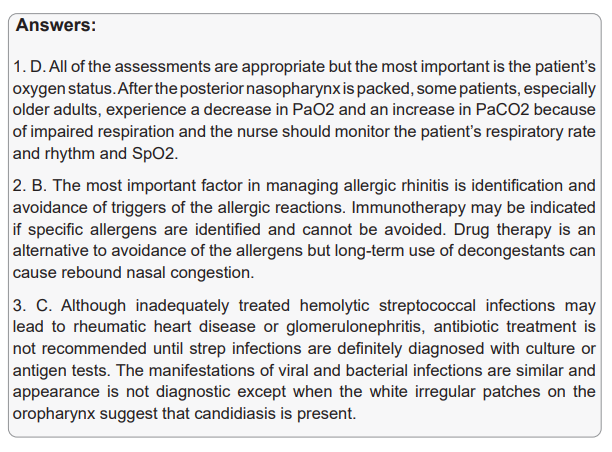
Images 1, 2 and 4: the persons might be sneezing, blowing the nose, pressing due
to pain, etc.
Image 3: the person is having nose bleeding
Images 5 and 6: the persons might be having wounds at the noses
2) The medical conditions that might be having above mentioned
as clinical presentations: flu like syndrome, rhinitis, sinusitis,
tonsillitis, epistaxis, nose-bleeding, nasal injury, pharyngitis,laryngitis, etc.
3.5 List of lessons/sub-heading (including assessment)
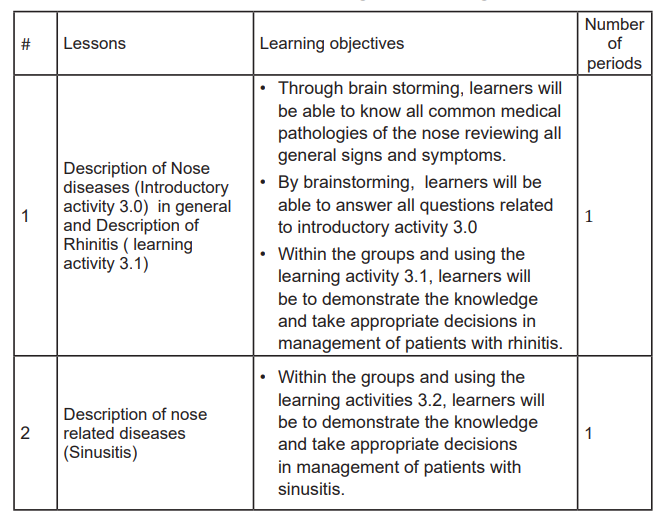
Lesson 1: Description of Nose diseases (Introductory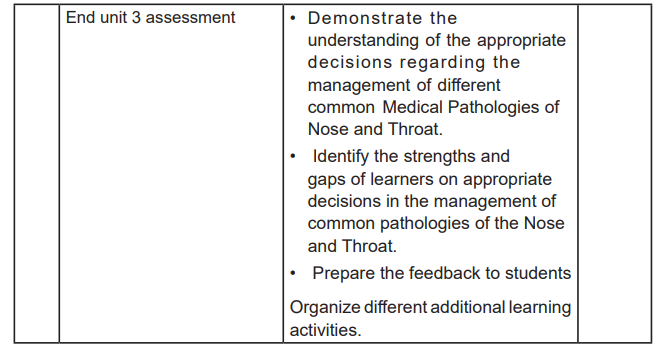
activity 3.0) in general and Description of Rhinitis(learning activity 3.1)
a) Prerequisites
This is the first lesson of the third unit on medical pathologies of sensory system
mainly the Nose and Throat. In this lesson, you will be dealing with the common
medical pathologies of the Nose and Throat. The learner will be able to revise the
anatomy and physiology of sensory system mainly the nose and throat.
The first thing to do before starting teaching is to remind learners what they have
learnt about structure and function of nose in biology, health assessment of sensory
system focusing on ear, nose and throat from fundamentals of nursing and let them
discuss the questions as indicated in introductory activity 3.0. after brainstorming
in answering the questions relate to introductory activity 3.0, learners will be given
time to be into groups and read he case from the case study from learning activity
3.1 and provide answers. All these will be preparing the learners themselves for
this lesson.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• List all signs and symptoms that the patients on the images were presenting
that are common in the common nose diseases
• List all Medical conditions that lead to all signs and symptoms listed
• Demonstrate the knowledge about rhinitis and demonstrate competencies in
taking appropriate decisions in management of patients with rhinitis.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve
learning objectives. The teaching materials are white board, flip chart, marker,
computer, screen, handout, textbook, videos. In addition, the teacher will avail
the didactic materials (all materials for physical examination focusing on sensory
system assessment mainly Nose and Throat, etc.). The teaching methods are
lecture, brainstorming, course work, and small group discussion. In addition, the
teacher guides the learners where they can find the supporting resources such
computer lab, Nursing skills lab, and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course,
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as taking notes, course work, and read textbook
related to the lesson, group assignment, listening to the video and summarize the
content, engagement in debate and other clinical learning activities such as case
study.
Teacher’s activity
• Ask learners to brainstorm while answering the questions related to the image
in the introductory activity 3.0.
• Supervise the work where the learners are grouped in small group and
teacher facilitates them to answer the questions by using the case study in
learning activity 3.1.
• Ask learners to present what they have done in group
• Identify the correct answers and complete those ones that are incomplete.
• Correct the answers that are false.
• Note on the blackboard the main student’s ideas.
• Help learners to summarize what they have learnt and make conclusion.
Student activity:
• Brainstorm in answering the questions regarding the introductory activity 3.0.
• Form group and participate in the group work
• To read carefully the case study from learning activity 3.1 and answer the
questions
• Group representatives will present their work
• Other students will follow when group representatives will be presenting
• Take notes from the correct answers• Make conclusion from what they have learnt.
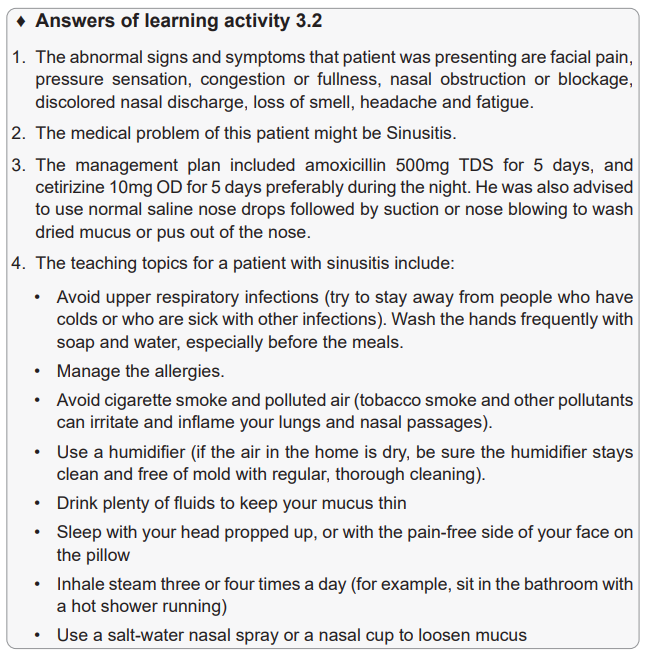
Lesson 2: Description of nose related diseases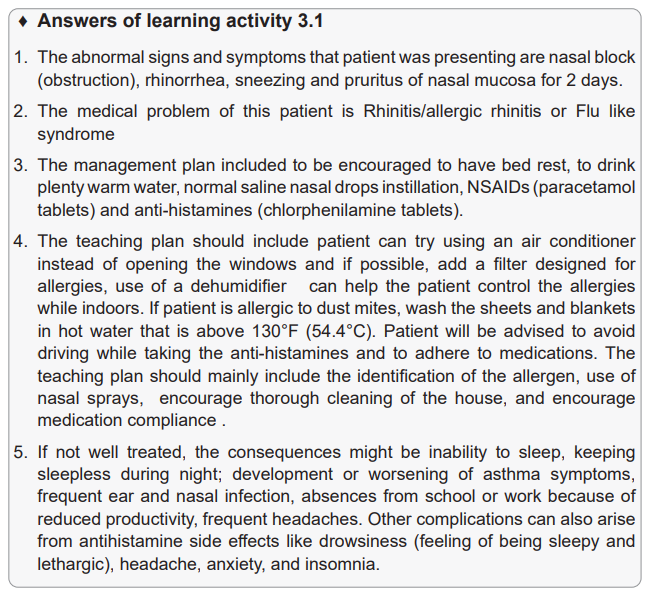
(Sinusitis)
a) Prerequisites
This is the second lesson of the third unit on medical pathologies of sensory system.
In this lesson, you will be dealing with two medical conditions (Sinusitis) specifically
their definitions, causes and risk factors and pathophysiology, signs and symptoms
of sinusitis, investigations to be requested, plan of management and the possible
complications. The learner will be able to revise the anatomy and physiology of the
nose and throat. The first thing to do before starting teaching is to remind learners
what they have learnt about structure and function of nose and throat in biology,
health assessment of sensory system with focus on nose and throat. In addition, the
teacher will let students discuss the questions from the case studies from learning
activity 3.2 so that they can prepare themselves for this lesson.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Demonstrate the knowledge about sinusitis and demonstrate competencies
in taking appropriate decisions in management of patients with sinusitis.
• Demonstrate the knowledge about tonsillitis and demonstrate competencies
in taking appropriate decisions in management of patients with tonsillitis.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve
learning objectives. The teaching materials are white board, flip chart, marker,
computer, screen, hand out, textbook, and videos. In addition, the teacher will
avail the didactic materials such as materials for physical examination focusing on
sensory system assessment mainly Nose and Throat, etc. The teaching methods
are lecture, brainstorming, course work, and small group discussion. In addition,
the teacher guides the learners where they can find the supporting resources such
computer lab, Nursing skills lab, and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course,
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as taking notes, course work, and read textbook
related to the lesson, group assignment, listening to the video and summarize the
content, engagement in debate and other clinical learning activities such as case
study.
Teacher’s activity
• Ask learners to be into different small groups and ask them to read the case
studies and answer the questions from learning activities 3.2
• Supervise the work where the learners are grouped in small group and
teacher facilitates them to answer the questions by using the case studies in
learning activities 3.2
• Ask learners to present what they have done in groups
• Identify the correct answers and complete those ones that are incomplete.
• Correct the answers that are false.
• Note on the blackboard the main student’s ideas.
• Help learners to summarize what they have learnt and make conclusion.
Student activity:
• Form small groups and participate in the group work
• To read carefully the case study from learning activity 3.2 and answer the
questions related to the case.
• Group representatives will present their work
• Other students will follow when group representatives will be presenting
• Take notes from the correct answers• Make conclusion and summary from what they have learnt.
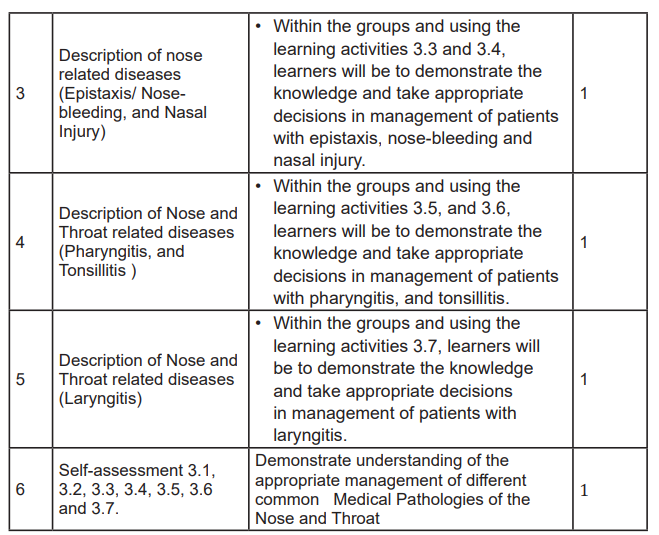
Lesson 3: Description of nose related diseases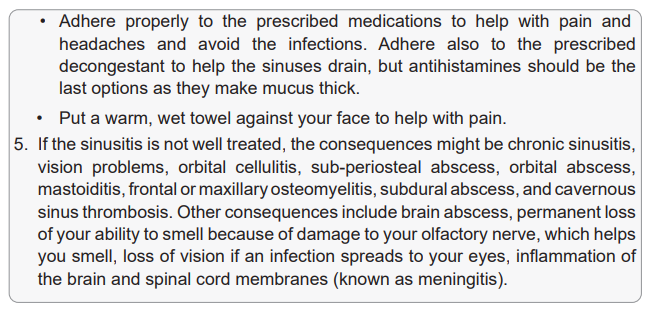
(Epistaxis, Nose-bleeding and Nasal Injury)
a) Prerequisites
This is the third lesson of the third unit on medical pathologies of sensory system.
In this lesson, you will be dealing with the medical conditions of the nose (Epistaxis,
Nose-bleeding and Nasal Injury) specifically their definitions, causes and risk factors
and pathophysiology, signs and symptoms of each one among those diseases,
investigations to be requested, plan of management and the possible complications.
The learner will be able to revise the anatomy and physiology of the nose. The
first thing to do before starting teaching is to remind learners what they have learnt
about structure and function of nose in biology, and health assessment of sensory
system with focus on nose from fundamentals of nursing. In addition, the teacher
will let students discuss the questions from the case studies from learning activity
3.3 and 3.4 so that they can prepare themselves for this lesson.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Demonstrate the knowledge about epistaxis and nose bleeding, and
demonstrate competencies in taking appropriate decisions in management of
patients with epistaxis and nose bleeding.
• Demonstrate the knowledge about nasal injury and demonstrate competencies
in taking appropriate decisions in management of patients with nasal injury.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve
learning objectives. The teaching materials are white board, flip chart, marker,
computer, screen, hand out, textbook, and videos .In addition, the teacher will
avail the didactic materials such as materials for physical examination focusing on
sensory system assessment mainly Nose, etc. The teaching methods are lecture,
brainstorming, course work, and small group discussion. Moreover, the teacher
guides the learners where they can find the supporting resources such computerlab, Nursing skills lab, and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course,
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as taking notes, course work, and read textbook
related to the lesson, group assignment, listening to the video and summarize the
content, engagement in debate and other clinical learning activities such as casestudy.
Teacher’s activity
• Ask learners to be into different small groups and ask them to read the case
studies and answer the questions from learning activities 3.3 and 3.4
• Supervise the work where the learners are grouped in small group and
teacher facilitates them to answer the questions by using the case studies inlearning activities 3.3 and 3.4
• Ask learners to present what they have done in groups
• Identify the correct answers and complete those ones that are incomplete.
• Correct the answers that are false.
• Note on the blackboard the main student’s ideas.
• Help learners to summarize what they have learnt and make conclusion.
Student activity:
• Form small groups and participate in the group work
• To read carefully the case studies from learning activities 3.3 and 3.4 and
answer the questions related to those cases
• Group representatives will present their work
• Other students will follow when group representatives will be presenting
• Take notes from the correct answers
• Make conclusion and summary from what they have learnt.
♦ Answers of learning activity 3.3
1. The abnormal signs and symptoms that patient was presenting:
Patient had history of sinus infection that he has been using antihistamine nasal
spray and developed the continuous ooze of blood from the right nostril.
2. The medical problem of this patient: Epistaxis or nose bleeding.
3. The investigations that have been ordered are: A full blood count that revealed
the hemoglobin level of 9 g/dl and the blood group type was done and revealed
type B, Rh+.
4. The management plan included to put the patient in a quiet area, advised to
apply the pressure by pinching the anterior aspect of the nose.
5. If the epistaxis is not treated, it leads to many consequences:
If epistaxis has severe form, the complications might be hemorrhagic shock, septic
shock, pneumocephalus, sinusitis, septal pressure necrosis, neurogenic syncope
during packing, epiphora (from blockage of the lacrimal duct), hypoxia (from
impaired nasal air movement), aspiration, hypovolemia in heavy bleeding, cerebralabscess.
Lesson 4: Description of nose and throat related
diseases (Pharyngitis, and Tonsillitis)
a) Prerequisites
This is the fourth lesson of the third unit on medical pathologies of sensory system.
In this lesson, you will be dealing with the medical conditions of the nose and throat
(Pharyngitis/Tonsillitis and Laryngitis) specifically their definitions, causes and
risk factors and pathophysiology, signs and symptoms of each one among those
diseases, investigations to be requested, plan of management and the possible
complications. The learner will be able to revise the anatomy and physiology of
the nose and throat. The first thing to do before starting teaching is to remind
learners what they have learnt about structure and function of nose and throat in
biology, and health assessment of sensory system with focus on nose and throat
from fundamentals of nursing. The teacher will let students discuss the questions
from the case studies from learning activity 3.5 and 3.6 so that they can prepare
themselves for this lesson.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Demonstrate the knowledge about pharyngitis, and demonstrate competencies
in taking appropriate decisions in management of patients with pharyngitis
• Demonstrate the knowledge about laryngitis and demonstrate competencies
in taking appropriate decisions in management of patients with Tonsillitis.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. These teaching aids are white board, flip chart, marker, computer, screen,
hand out, textbook, and videos. The teacher will avail the didactic materials such as
materials for physical examination focusing on sensory system assessment mainly
nose and throat, etc. The teaching methods are lecture, brainstorming, course
work, and small group discussion. In addition the teacher guides the learners where
they can find the supporting resources such computer lab, Nursing skills lab, andLibrary.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course,
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as taking notes, course work, and read textbook
related to the lesson, group assignment, listening to the video and summarize the
content, engagement in debate and other clinical learning activities such as case
study.
Teacher’s activity
• Ask learners to be into different small groups and ask them to read the case
studies and answer the questions from learning activities 3.5 and 3.6
• Supervise the work where the learners are grouped in small group and
teacher facilitates them to answer the questions by using the case studies in
learning activities 3.5 and 3.6
• Ask learners to present what they have done in groups
• Identify the correct answers and complete those ones that are incomplete.
• Correct the answers that are false.
• Note on the blackboard the main student’s ideas.
• Help learners to summarize what they have learnt and make conclusion.
Student activity:
• Form small groups and participate in the group work
• To read carefully the case studies from learning activities 3.5 and 3.6 and
answer the questions related to those cases
• Group representatives will present their work
• Other students will follow when group representatives will be presenting
• Take notes from the correct answers
• Make conclusion and summary from what they have learnt.
♦ Answers of learning activity 3.5
1. The abnormal signs and symptoms that the patient was presenting are sore
throat and cough. She has had some hoarseness in her voice over the past
few days and subjective sweats but no documented fever. She has a history of
seasonal allergies. She complains of isolated throat pain, without any rhinorrhea,
sinus pressure, or headache. She had severe unilateral sore throat, bulging of
pharyngeal wall, neck pain, swelling, and dysphagia with pharyngeal wall that
had whitish plaques.
2. The medical diagnosis the child was presenting is Pharyngitis.
3. The investigations requested to diagnose the medical condition are Full blood
count (FBC), erythrocytes sedimentation rate (VS), throat swab for culture.
4. The treatment plan of that patient include health education about home remedies
(drink plenty of fluids and rest), ibuprofen for fever management, and was given
appointment to come back when the results of culture might be available.
5. The complications that might result from untreated and poorly managed
pharyngitis:
Severe infections of the pharynx and surrounding soft tissue can be life-threatening.
Upper airway obstruction can result from severe pharyngeal inflammation. Bacterial
invasion of the deep tissue of the neck can lead to infection and/or abscess
formation in the peritonsillar, submandibular, parapharyngeal, or retropharyngeal
space suppurative thrombophlebitis (Lemierre syndrome) can arise from bacterial
invasion and clot formation of the jugular vein.
GAS (group A streptococcus) infection can lead to suppurative and nonsuppurative
complications. Suppurative complications of GAS pharyngitis are due to invasion
of the organism beyond the pharynx and include otitis media, peritonsillar cellulitis
or abscess, sinusitis, meningitis, bacteremia, and necrotizing fasciitis. Non
suppurative complications of GAS pharyngitis are immune mediated and includeacute rheumatic fever, post-streptococcal glomerulonephritis, and reactive arthritis.
♦ Answers of learning activity 3.6
1. The abnormal signs and symptoms that patient was presenting are throat is
so sore that she has difficulty swallowing even liquids. Patient also has acutely
swollen and reddened area of the soft palate is noted in her mouth, half occluding
the orifice from the mouth into the pharynx. Yellow exudate is present.
2. The medical problem of this patient is Tonsillitis.
3. The investigations that have been ordered include full blood count that revealed
elevated white blood cells.
4. The management plan included Amoxicillin 500mg TDS for 7 days, paracetamol
500mg TDS for 3 days, and ibuprofen 400mg TDS. The patient was also advised
to drink warm or very cold fluids to help with throat pain and gargle with warm
alt water.
5. If not well treated, the consequences might be:
Complications usually happen only if bacteria caused the infection. These
complications include:
• A collection of pus around the tonsil (peritonsillar abcess)
• Middle ear infection
• Breathing problems or breathing that stops and starts while sleeping
(obstructive sleep apnea)
• Tonsillar cellulitis, or infection that spreads and deeply penetrates nearby
tissues
If the patient has streptococcus bacteria and does not get treatment, the illness
could lead to a more serious problem, including rheumatic fever, scarlet fever,
sinusitis, kidney infection called glomerulonephritis.
Lesson 5: Description of nose and throat related diseases (Laryngitis)
a) Prerequisites
This is the fifth lesson of the third unit on medical pathologies of sensory system. In
this lesson, you will be dealing with the medical condition of the throat (Laryngitis)
specifically its definition, causes and risk factors and pathophysiology, signs and
symptoms, investigations to be requested, plan of management and the possible
complications. The learner will be able to revise the anatomy and physiology of the
throat. The first thing to do before starting teaching is to remind learners what they
have learnt about structure and function of nose and throat in biology, and health
assessment of sensory system with focus on nose and throat from fundamentals of
nursing. The teacher will let students discuss the questions from the case studies
from learning activity 3.7 so that they can prepare themselves for this lesson.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Demonstrate the knowledge about Laryngitis, and demonstrate competencies
in taking appropriate decisions in management of patients with laryngitis.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. These teaching aids are white board, flip chart, marker, computer,
screen, hand out, textbook, and videos. The teacher will avail the didactic materials
such as materials for physical examination focusing on sensory system assessment
mainly throat, etc. The teaching methods are lecture, brainstorming, course work,
and small group discussion. In addition the teacher guides the learners where they
can find the supporting resources such computer lab, Nursing skills lab, and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course,
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as taking notes, course work, and read textbook
related to the lesson, group assignment, listening to the video and summarize the
content, engagement in debate and other clinical learning activities such as casestudy.
Teacher’s activity
• Ask learners to be into different small groups and ask them to read the case
studies and answer the questions from learning activities 3.7
• Supervise the work where the learners are grouped in small group and
teacher facilitates them to answer the questions by using the case study inlearning activity 3.7
• Ask learners to present what they have done in groups
• Identify the correct answers and complete those ones that are incomplete.
• Correct the answers that are false.
• Note on the blackboard the main student’s ideas.• Help learners to summarize what they have learnt and make conclusion.
Student activity:
• Form small groups and participate in the group work
• To read carefully the case studies from learning activities 3.5 and 3.6 and
answer the questions related to those cases
• Group representatives will present their work
• Other students will follow when group representatives will be presenting
• Take notes from the correct answers• Make conclusion and summary from what they have learnt.
♦ Answers of learning activity 3.7
1. The abnormal signs and symptoms that the patient was presenting are acute
episode of hoarseness progressing to aphonia, which she had experienced 3
days before her appointment. She also reported a sore throat, odynophagia, andcough for 5 days.
2. The medical diagnosis of this patient is acute laryngitis.
3. The possible causes and risk factors of laryngitis:
Most cases of laryngitis are temporary and improve after the underlying cause gets
better. Causes of acute laryngitis include viral infections similar to those that cause
a cold, vocal strain caused by yelling or overusing the voice, bacterial infections,
although these are less common.
Laryngitis that lasts longer than three weeks is known as chronic laryngitis. This
type of laryngitis is generally caused by exposure to irritants over time. Chronic
laryngitis can cause vocal cord strain and injuries or growths on the vocal cords
(polyps or nodules). The other causes include inhaled irritants such as chemical
fumes, allergens or smoke; acid reflux also called gastroesophageal reflux disease
(GERD); chronic sinusitis; excessive alcohol use; habitual overuse of the voice
(such as in singers or cheerleaders); smoking
Less common causes of chronic laryngitis include bacterial or fungal infections,
Infections with certain parasites.
Other causes of chronic hoarseness include cancer, vocal cord paralysis, which
can result from nerve injury due to surgery, injury to the chest or neck, cancer, nerve
disorders, or other health conditions, bowing of the vocal cords.
Other risk factors for laryngitis include having a respiratory infection, such as a cold,
bronchitis or sinusitis, exposure to irritating substances, such as cigarette smoke,
excessive alcohol intake, stomach acid or workplace chemicals, overusing your
voice, by speaking too much, speaking too loudly, shouting or singing.
1) The treatment plan of this patient included:
She had been taking a cough suppressant (Dextromethorphan15mg 2x/day/5days),
antihistamine (azatadinex3/day/3days), decongestant (Sudafed take 1 tablet every
4 hours), and acetaminophen (Paracetamol 500mg tds/4days) to relieve her
symptoms, and she was advised the oral hydration. She was also treated with
amoxicillin-clavulanate 500mg tds/day for 10 days and a methylprednisolone 1
tablet per day in 7days.
2) The possible complications of laryngitis:
Acute laryngitis: complications are rare, as the disease is usually self-limiting.
Damage to the vocal cords is possible in patients who try to overcompensate for
the dysphonia.
Chronic laryngitis: the main complications are voice loss, obstruction of the airways
and chronic cough. Laryngeal stenosis may develop occasionally. Rarely, in severe
infections such as those with herpes viruses, laryngeal erosion and necrosis may
occur.
In some cases of laryngitis caused by infection, the infection may spread to otherparts of the respiratory tract.
4. The treatment plan of allergic rhinitis focuses on trigger avoidance (exposure to
tobacco smoke can be reduced if household members stop smoking or smoke
only outside of the home. It is also important to avoid smoke exposure in the
workplace. Exposure to pollutants and irritants can be reduced by avoiding
wood-burning stoves and fireplaces; properly venting other stoves and heaters;
and avoiding cleaning agents and household sprays that trigger symptoms.
Exposure to strong perfumes and scented products may be more difficult),
medications (daily use of a nasal glucocorticoid (steroid) and/or an antihistamine
nasal spray can be helpful for people with allergic rhinitis.
These medications may be used alone or in combination), and/or nasal rinsing or
irrigation (simply rinsing the nose with a salt water (saline) solution one or more
times per day is helpful for many patients with rhinitis, as well as for other rhinitis
conditions. Nasal rinsing is particularly useful for symptoms of postnasal drainage.
Nasal rinsing can be done before use of nasal medication so that the lining is freshly
cleansed when the medication is applied). All these include respect of remedies,
use of antihistamines (loratidine, cetirizine, etc), use of decongenstants (cetirizine,
oxymetazoline, etc), use of corticosteroids, eye drops and/or nasal sprays, and
Immunotherapy if the patient has severe allergies.
If the rhinitis is not treated well, the possible medical complications are inability to
sleep from symptoms keeping sleepless during night; development or worsening of
asthma symptoms frequent ear and nasal infection, absences from school or work
because of reduced productivity, frequent headaches. Other complications can
also arise from antihistamine side effects like drowsiness (feeling of being sleepy
and lethargic), headache, anxiety, and insomnia. In rare cases, antihistamines cancause gastrointestinal, urinary, and circulatory effects.
Direct visualization with a good directed light source, a nasal speculum, and nasal
suction should be sufficient in most patients. However, computed tomography (CT)
scanning, magnetic resonance imaging (MRI), or both may be indicated to evaluate
the surgical anatomy and to determine the presence and extent of rhinosinusitis,
foreign bodies, and neoplasms. Nasopharyngoscopy may also be performed if a
tumor is the suspected cause of bleeding. Sinus films are rarely indicated for a
nosebleed.
The diagnosis of posterior epistaxis is diagnosed by focusing on:
• Complete Blood Count (CBC), which is a blood test to check for blood
disorders.
• Partial Thromboplastin Time (PTT) or INR, which is a blood test that checks
how long it takes for the blood to clot.
• Nasal endoscopy.
• CT scan of the nose.• X-ray of the face and nose.
4. The management plan of epistaxis include the following elements:
The first treatment is direct pressure. Grasp the nose firmly between the thumb
and forefinger and squeeze it for 10 to 30 minutes without stopping. Putting an ice
pack on the neck or bridge of the nose may help slow blood flow. Leaning forward
to spit out blood instead of letting it run down the throat and be swallowed may help
prevent vomiting. Using salt water nasal sprays and humidifying the air may help
dryness.
Most anterior nosebleeds can be stopped by applying direct pressure, which helps
by promoting blood clots. Those who suffer a nosebleed should first attempt to blow
out any blood clots and then apply pressure for at least five minutes and up to 20
minutes. Pressure should be firm and tilting the head forward helps decrease the
chance of nausea and airway obstruction as seen in the picture on the right. When
attempting to stop a nosebleed at home, the head should not be tilted back.
Patient will be advised to breathe through the mouth, use a tissue or damp washcloth
to catch the blood, use the thumb and index finger to pinch together the soft part of
the nose. Make sure to pinch the soft part of the nose against the hard bony ridge
that forms the bridge of the nose. Squeezing at or above the bony part of the nose
will not put pressure where it can help stop the bleeding.
B. Nasal packing: if pressure and chemical cauterization cannot stop bleeding, nasal
packing is the mainstay of treatment. There are several forms of nasal packing
that can be contrasted by anterior nasal packing and posterior nasal packing.
Traditionally, nasal packing was accomplished by packing gauze into the nose,
thereby placing pressure on the vessels in the nose and stopping the bleeding.
Traditional gauze packing has been replaced with products such as Merocel and
the Rapid Rhino. The Merocel nasal tampon is similar to gauze packing except it is
a synthetic foam polymer (made of polyvinyl alcohol and expands in the nose after
application of water) that provides a less hospitable medium for bacteria. The Rapid
Rhino stops nosebleeds using a balloon catheter, made of carboxymethylcellulose,
which has a cuff that is inflated by air to stop bleeding through extra pressure in the
nasal cavity.
C. Medications: use of tranexamic acid: helps promote blood clotting. For nosebleedsit can be applied to the site of bleeding, taken by mouth, or injected into a vein.
Vasoconstrictive medications such as oxymetazoline (Afrin) or phenylephrine
are widely available for treatment of allergic rhinitis and may also be used to
control benign cases of epistaxis. Those with nosebleeds that last longer than 20
minutes (in the setting of direct pressure as seen in the image to the right) should
seek medical attention. Oral and topical antibiotics to prevent rhinosinusitis and
possibly toxic shock syndrome. Avoidance of aspirin and other nonsteroidal anti
inflammatory drugs (NSAIDs). Medications to control underlying medical problems
(e.g., hypertension, vitamin K deficiency) in consultation with other specialists.
D. Cauterization: this method involves applying a chemical such as silver nitrate to
the nasal mucosa, which burns and seals off the bleeding.
E. Surgery: ongoing bleeding despite good nasal packing is a surgical emergency
and can be treated by endoscopic evaluation of the nasal cavity under general
anesthesia to identify an elusive bleeding point or to directly ligate (tie off) the blood
vessels supplying the nose. The bleeding can also be stopped by intra-arterial
embolization using a catheter placed in the groin and threaded up the aorta to the
bleeding vessel by an interventional radiologist.
There is no difference in outcomes between embolization and ligation as treatment
options, but embolization is considerably more expensive. All these other
alternatives are also considered: foreign body removal should be considered if the
foreign body is the cause of the nose bleed, surgical repair of a broken nose or
correction of a deviated septum if this is the cause of the nosebleed, and ligation (in
this procedure, the culprit blood vessel is tied off to stop the bleeding).
5. If epistaxis is not well managed treated, it will lead to some severe forms of the
complications like hemorrhagic shock, septic shock, pneumocephalus, sinusitis,
septal pressure necrosis, neurogenic syncope during packing, epiphora (from
blockage of the lacrimal duct), hypoxia (from impaired nasal air movement),aspiration, hypovolemia from heavy bleeds, cerebral abscess.
Nasal obstruction: Nasal blockage usually occurs after the injury due to swelling
inside the nose and this may take a few days to settle. If the nose is still blocked
after three weeks, it may be due to the septum being deviated and buckled which
blocks the nasal passage. Septal deviation may require surgical correction if theblockage is significant.
Nosebleeds (epistaxis): Nosebleeds are common and usually settle on their own
with simple first aid by gently pinching the lower half of the nose for 15 minutes.
Nasal packing or cautery in hospital is reserved for nosebleeds that do not stop of
their own accord.
Cerebrospinal fluid leak: severe nasal trauma can push the nasal bones into the
face, giving the face a pug-like appearance. The thin cribriform plate at the roof
of the nose may fracture causing the cerebrospinal fluid that bathes the brain to
leak out. Small fractures seal spontaneously with conservative management (95%
within two weeks). Antibiotics are not given unless infection is proven to be present.
If fluid leak continues, more treatment may be required.
Loss of sense of smell (anosmia): the smell organ in the roof of the nose can alsobe damaged.
The clinical syndrome of diphtheria is characterized by pharyngitis, low-grade fever,
malaise, and cervical lymphadenopathy. Symptom onset is usually gradual. The
hallmark of diphtheria, the formation of a tightly adherent gray membrane that bleeds
when dislodged, occurs in at least one-third of patients. Although diphtheria is rare,
suspicion should be raised in patients who have recently lived in or traveled to
areas where diphtheria remains endemic and in unvaccinated patients), Francisella
tularensis (can cause pharyngeal tularemia, particularly when infection is acquired
by ingestion of contaminated food or water. Pharyngeal tularemia is characterized by
fever and severe exudative pharyngitis, which is often accompanied by oral ulcers
and painful cervical lymphadenopathy. As with diphtheria, a pharyngeal membranemay be present). Rare causes of bacterial pharyngitis include also gonorrhea.
The most common noninfectious causes of pharyngitis include allergic rhinitis or
sinusitis, gastroesophageal reflux disease, smoking or exposure to second-hand
smoke, and exposure to dry air (particularly in the winter). Trauma (e.g., caused by
tracheal intubation) or vocal strain have also been reported to cause sore throat.
Other risks include the use of angiotensin-converting enzyme (ACE) inhibitors and
some chemotherapeutics, autoimmune disorders like Kawasaki disease, periodic
fever. Frequent exposure to colds and flus can increase your risk for pharyngitis.
Allergy, frequent sinus infections and exposure to second hand smoke may alsoraise your risk.
2) Investigations to diagnose the pharyngitis focus on:
• The complete history taking and physical exam that will mainly focus on ear,
nose, throat and neck.
• Throat swab culture: this involves using a cotton swab to take a sample
of the secretions from the throat for the rapid strep test in the consultation
room for Group A beta-hemolytic streptococcal rapid antigen detection test
(preferred diagnostic method in emergency settings), or the swab is sent to
a lab for further testing and results. This is criterion standard for diagnosis of
GAS infection (90-99% sensitive).
• Testing for coronavirus 2 (SARS-CoV-2) by rapid test after taking nasal swabs
or polymerase chain reaction (PCR) with oro-pharyngeal swab.
• Blood tests: mainly to determine whether the patient has mononucleosis.
A complete blood count (CBC) may be done to look for any other type of
infection. Other laboratory studies that may be helpful include peripheral
blood smear, erythrocytes sedimentation rate, blood culture or gonococcal
culture if indicated by the history.
• Imaging studies generally are not indicated for uncomplicated viral or
streptococcal pharyngitis. However, the following may be considered: lateral
neck x-ray in patients with suspected epiglottitis or airway compromise, soft
tissue neck CT if concern for abscess or deep-space infection exists
3) The treatment plan of pharyngitis include:
The main goals in evaluation of adults with pharyngitis are the exclusion of serious
or potentially life-threatening conditions and the identification of treatable causes.Viral infections do not need to be treated with antibiotics, and treatment is
complications. Suppurative complications of GAS pharyngitis are due to invasion
of the organism beyond the pharynx and include otitis media, peritonsillar cellulitis
or abscess, sinusitis, meningitis, bacteremia, and necrotizing fasciitis. Non
suppurative complications of GAS pharyngitis are immune mediated and includeacute rheumatic fever, post-streptococcal glomerulonephritis, and reactive arthritis.
4) The management plan of tonsillitis: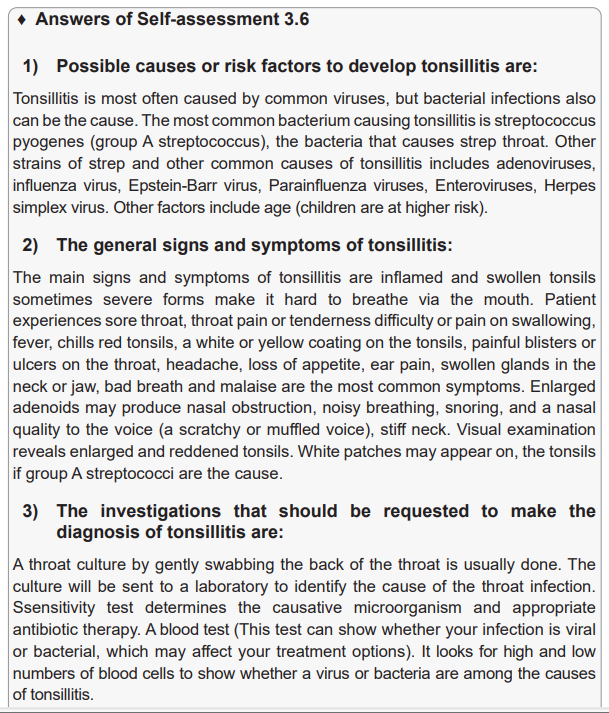
The treatment of tonsillitis depends on the causes:
A. Medications: if the tests find bacteria, client will get antibiotics. These drugs might
be given in a one-time injection or in pills that patient will swallow for several days.
The antibiotics usually used are Penicillins for tonsillitis due to group Astreptococcus.
Other antibiotics might also be used if patient is allergic to penicillin.
Antibiotic therapy, analgesics such as acetaminophen, and saline gargles may
be used to treat the infection and associated discomfort. Chronic tonsillitis and
adenoiditis may require tonsillectomy.
B. Home remedies: if client has a virus, antibiotics won’t help, and the body will fight
the infection on its own. In the meantime, client can try some home remedies:
• Get lots of rest
• Drink warm or very cold fluids to help with throat pain
• Eat smooth foods, such as flavored gelatins, ice cream, and applesauce
• Use a cool-mist vaporizer or humidifier in your room
• Gargle with warm salt water
• Suck on lozenges with bensoine or other medications to numb the throat
• Take over-the-counter pain relievers such as acetaminophen or ibuprofen
• If the causative organism is group A streptococcus, the nurse ensures that the
client and family members can manage self-care at home by communicating
the following points:
– Report any signs of bleeding to the physician, this is particularly important in
the first 12 to 24 hours, and then 7 to 10 days after surgery as the throat heals.
– Gently gargle with warm saline or an alkaline mouthwash to assist in removing
thick mucus.
– Maintain a liquid and very soft diet for several days after surgery, avoid spicy
foods and rough-textured foods.
– Also, avoid milk and milk products if the client does not tolerate them well.
Streptococcus, prompt treatment is needed to prevent potential cardiac and
renal complications.
C. Surgery
Tonsils are an important part of the immune system, so the best option is to do all
best to ensure they kept. But if the tonsillitis keeps coming back or won’t go away, or
if swollen tonsils make it hard to breathe or eat, client might need to have the tonsils
taken out. This surgery is called tonsillectomy (usually, a sharp tool called a scalpel
is used to take out the tonsils. But other options are available including lasers, radio
waves, ultrasonic energy, or electrocautery to remove enlarged tonsils). The criteria
for performing tonsillectomy are repeated episodes of tonsillitis, hypertrophy of the
tonsils, enlarged obstructive adenoids, repeated purulent otitis media, hearing
loss related to serous otitis media associated with enlarged tonsils and adenoids,
and other conditions (e.g., asthma, rheumatic fever) exacerbated by tonsillitis.
Tonsillectomy and adenoidectomy are generally done as outpatient procedures.
Post tonsillectomy recovery, patient will be advised to get plenty of rest and drink
lots of fluids while recovering, but don’t eat or drink any dairy products for the first24 hours.
5) The complications for tonsillitis:
Complications usually happen only if bacteria caused the infection. These
complications include:
• A collection of pus around the tonsil (peritonsillar abcess)
• Middle ear infection
• Breathing problems or breathing that stops and starts while sleeping
(obstructive sleep apnea)
• Tonsillar cellulitis, or infection that spreads and deeply penetrates nearby
tissues
If the patient has streptococcus bacteria and does not get treatment, the illness
could lead to a more serious problem, including rheumatic fever, scarlet fever,sinusitis, kidney infection called glomerulonephritis.
Laryngitis that lasts longer than three weeks is known as chronic laryngitis. This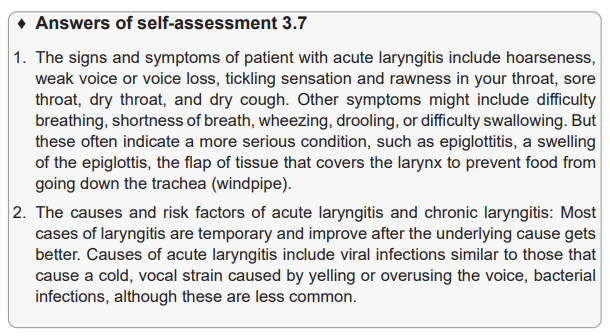
type of laryngitis is generally caused by exposure to irritants over time. Chronic
laryngitis can cause vocal cord strain and injuries or growths on the vocal cords
(polyps or nodules). The other causes include inhaled irritants such as chemical
fumes, allergens or smoke; acid reflux also called gastroesophageal reflux disease
(GERD); chronic sinusitis; excessive alcohol use; habitual overuse of the voice
(such as in singers or cheerleaders); smoking
Less common causes of chronic laryngitis include bacterial or fungal infections,
Infections with certain parasites.
Other causes of chronic hoarseness include cancer, vocal cord paralysis, which
can result from nerve injury due to surgery, injury to the chest or neck, cancer, nerve
disorders, or other health conditions, bowing of the vocal cords.
Other risk factors for laryngitis include having a respiratory infection, such as a cold,
bronchitis or sinusitis, exposure to irritating substances, such as cigarette smoke,
excessive alcohol intake, stomach acid or workplace chemicals, overusing your
voice, by speaking too much, speaking too loudly, shouting or singing.
3. The treatment plan for someone who has signs and symptoms of laryngitis
involve:
Supportive care: no matter what the cause, laryngitis is best treated by giving the
voice a rest by reducing vocal activity as much as possible. Steam inhalation and
drinking fluids also help to soothe irritated tissue, moderate symptoms, and speed
healing. Topical medications or remedies such as saltwater, over-the-counter throat
lozenges, sore throat syrups, hard candy, herbal teas, herbal sprays, or herbal
lozenges only work by coming in contact with inflamed or irritated tissues and so
will help only with irritation in the throat itself. The larynx, however, is the doorway
to the lungs. If topical medications like saltwater, lozenges, or cough syrup could
enter the larynx, the result would be choking or drowning.
Medications: pain, sore throat, and dry cough are most effectively relieved with
over-the-counter pain relievers. In severe cases, or for voice professionals, a
doctor may use oral or inhaled corticosteroids to rapidly reduce swelling. Other
medications will be used only to treat the underlying cause, not the laryngitis itself.
Because laryngitis is not usually caused by a bacterial infection, doctors rarely use
antibiotics unless if the cause is bacterial. Pain relievers such as acetaminophen,
ibuprofen, naproxen, or aspirin are also used. Corticosteroids as prednisone might
be used for severe laryngitis cases or voice professionals, an oral or inhaled
corticosteroid helps to rapidly reduce swelling. Because of the side effects, which
include laryngitis, corticosteroids are only rarely used
Treating the underlying cause: when identified, the underlying condition must be
managed. If laryngitis is caused by acid reflux, dietary changes and medications
that reduce stomach acid may be prescribed. Laryngitis caused by medications or
irritants will be treated by discontinuing the medication or avoiding the irritant. In
particular, tobacco users will be advised to quit smoking to relieve chronic laryngitis
due to smoking. Allergies will be treated with allergy medications and lifestyle
changes. Laryngitis due to an upper respiratory infection caused by a bacteria
or fungus will be treated with the appropriate antimicrobial medications, eitherantibiotics or antifungals.
Voice therapy: in cases of chronic laryngitis, voice therapy trains patients in vocal
behaviors and lifestyle changes that help preserve the voice. Sessions are directedby speech-language therapists and usually last for four to eight weeks.
There is no “best” medication for laryngitis. In most cases, the best treatment for
laryngitis is vocal rest, steam inhalation, and proper hydration. Medications areused to treat a possible underlying cause or to provide symptom relief.
To prevent dryness or irritation to your vocal cords avoid smoking and stay away
from secondhand smoke, limit alcohol and caffeine, drink plenty of water, keep
spicy foods out of your diet, include a variety of healthy foods in your diet, avoidclearing your throat, avoid upper respiratory infections.
4. Diagnosis of laryngitis focus on:
Complete physical exam and review of medical history and symptoms.
Listen to the voice and examine the vocal cords (Laryngoscopy: using the
laryngoscope, the health care provider can visually examine the vocal cords by
using a light and a tiny mirror to look into the back of the throat. The doctor may
use fiber-optic laryngoscopy, and he or she may refer you to an ear, nose and throat
specialist).
Taking the oro-pharyngeal swab for culture and/or Biopsy: If the doctor sees a
suspicious area, he or she may do a biopsy, taking a sample of tissue for examination
under a microscope.
5. The complications if the laryngitis is not treated:
Acute laryngitis: complications are rare, as the disease is usually self-limiting.
Damage to the vocal cords is possible in patients who try to overcompensate for
the dysphonia.
Chronic laryngitis: the main complications are voice loss, obstruction of the airways
and chronic cough. Laryngeal stenosis may develop occasionally. Rarely, in severe
infections such as those with herpes viruses, laryngeal erosion and necrosis may
occur.
In some cases of laryngitis caused by infection, the infection may spread to otherparts of the respiratory tract.
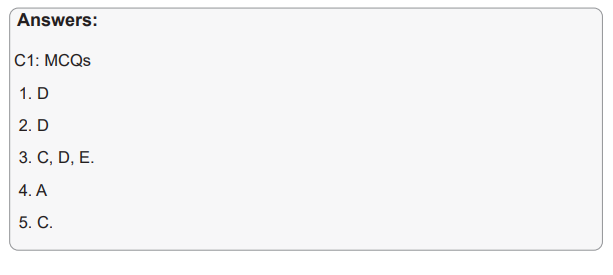
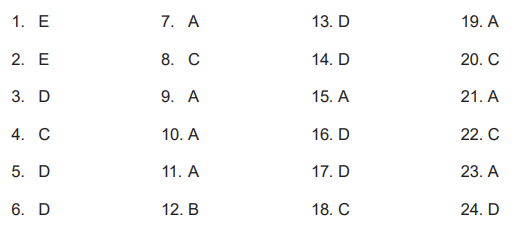
End Unit 3 Assessment♦ Answers to multiple choice questions
3.6 Additional information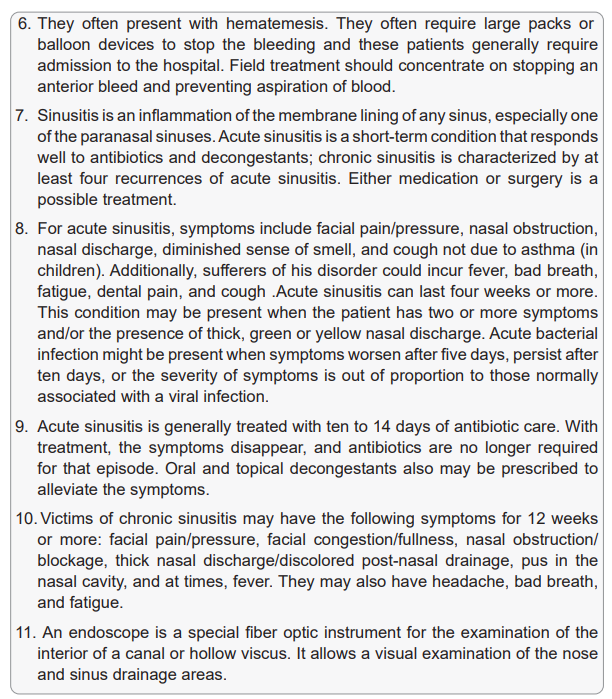
The Heimlich maneuver for dislodging an airway obstruction:
• Ask the person if he or she is choking. (Note: Hands crossed at the neck is
the universal sign of choking.)
• Assess ability to speak and cough. If the person cannot talk or cough, say that
you can help and place your arms around his or her waist.
• Make a fist with one hand and place the thumb toward the victim above the
umbilicus.
• Hold your fist with the other hand and thrust upward into the abdomen
• Repeat thrusts.
• If the object is dislodged and the victim can cough effectively, encourage him
or her to do so to eject the object.
• If the object is not ejected or coughed out and the victim loses consciousness,
lower the victim to the ground.
• Straddle the victim’s body and place the heel of one hand on top of the other.
Position the hands midway between the umbilicus and the xiphoid process.
• Deliver thrusts and repeat.
• Open the mouth to assess if the object can be swept out with a hooked finger
(do not sweep the mouth in children).
• If the airway remains obstructed, repeat the procedure.
• Clients with serious airway conditions require aggressive treatment tomaintain an airway or relieve airway obstruction.
TRACHEOTOMY AND TRACHEOSTOMY
A tracheotomy is the surgical procedure that makes an opening into the trachea.
A tracheostomy is a surgical opening into the trachea into which a tracheostomy
or laryngectomy tube is inserted. A tracheostomy may be temporary or permanent.
A permanent opening in the trachea is required for certain disorders, such as a
laryngectomy for laryngeal cancer.
Tracheostomy tubes come in several sizes and differ from laryngectomy tubes in
their length and diameter. A cuffed tracheostomy tube has a cuff on the lower end
that is inflated with air to provide a snug fit.
The cuff prevents aspiration of liquids or escape of air when a mechanical ventilator
is used. The physician specifies the amount of air to be injected into the cuff, usually
to achieve a pressure between 20 and 25 mm H2O. The amount of air determines
the seating of the cuff in the trachea. The pressure in the cuff requires monitoring
with a pressure gauge every 8 hours. During the immediate postoperative period,
the physician
may change the tracheostomy tube every 3 to 5 days. To pass a tracheostomy tube
into the tracheal opening, an obturator is placed in the tube to facilitate placement.
Once the tracheostomy tube is in place, the obturator is removed. The outer tube is
held snugly in place by tapes inserted in openings on either side of it and tied at the
side of the client’s neck. The respiratory passages react to the creation of the new
opening with inflammation and excessive mucus secretion. Copious respiratory
secretions are life-threatening. The client cannot be left unattended during the
immediate postoperative period because the secretions make frequent suctioning
necessary. Additionally, inspired air passes directly into the trachea, bronchi, and
lungs without becoming warmed and moistened by passing through the nose. Dry
secretions can subsequently develop, which easily form crusts and can break off,
obstruct the lower airway, and cause serious respiratory problems. Humidification
by a mist collar is usually necessary to prevent drying and incrustation of the mucous
membrane in the trachea and the main bronchus.
The longterm and short-term complications of tracheostomy include infection,
bleeding, airway obstruction resulting from hardened secretions, aspiration,
injury to the laryngeal nerve, erosion of the trachea, fistula formation between the
esophagus and trachea, and penetration of the posterior tracheal wall.
Nursing Management
After surgery, the nurse monitors vital signs and auscultates breath sounds.
He or she assesses skin color, level of consciousness, and mental status. The
nurse monitors for potential complications and checks airway patency frequently.
Secretions can rapidly clog the inner lumen of the tracheostomy tube, resulting in
severe respiratory difficulty or death by asphyxiation. If the airway is obstructed, the
client becomes cyanotic, restless, and frightened. To facilitate breathing during the
immediate postoperative period, the nurse positions the client as ordered. When
the client is fully awake and blood pressure is stable, the nurse elevates the head of
the bed to about 45 degrees. This position decreases edema and makes breathingeasier.
The nurse inspects the tracheostomy carefully, ensuring that tapes are secure. If
the tube is not tied securely, the client can cough it out, a serious occurrence if the
edges of the trachea have not been sutured to the skin. This may be the case in a
temporary tracheostomy. The nurse keeps a tracheal dilator at the bedside at all
times. If the outer tube accidentally comes out, the nurse inserts the dilator to hold
the edges of the stoma apart until the physician arrives to insert another tube. A
tracheal tube must never be forced back in place.
Use of force may compress the client’s trachea (by pushing the tube alongside and
compressing the trachea, rather than inserting the tube into the stoma). Such actioncould cause respiratory arrest.
Suctioning the Client with a Tracheostomy:
• Use sterile equipment (e.g., gloves, suction catheter, normal saline) and
aseptic technique for tracheal suctioning.
• Place client in Fowler’s position.
• Pre-oxygenate client for at least 1 to 2 minutes.
• Check that suction pressure is at a low setting.
• Open the suction kit, don gloves, lubricate a sterile, 10 to 14 sized French
disposable catheter with sterile saline, and insert it into the lumen of the tube.
• Do not apply suction while the catheter is inserted down the trachea because
this irritates the lining of the trachea.
• Begin intermittent suctioning while slowly withdrawing and rotating the
catheter. Do not suction for more than 10 seconds at a time.
• Allow client to rest and deep breathe before repeating if more suctioning is
necessary.
• Discard the suction catheter after use.
Providing Tracheostomy Care:
• Maintain aseptic technique, washing hands before, during, and after the
procedure.
• Position client in a supine or low Fowler’s position.
• Using a clean glove, remove the soiled stomal dressing and discard it, glove
and all, in an appropriate receptacle.
• Open the tracheostomy kit without contaminating the contents.
• Don sterile gloves—keep the dominant hand sterile.
• Pour hydrogen peroxide and normal saline into respective containers.
• Unlock the inner cannula by turning it counterclockwise.
• Remove it and place in hydrogen peroxide. Clean the inside and outside of
the cannula with pipe cleaners.
• Rinse the cleaned cannula with normal saline.
• Tap the cannula and wipe the excess solution with sterile gauze.
• Replace the inner cannula and turn it clockwise within the outer cannula.
• Clean around the stoma with an applicator moistened with normal saline.
• Place a sterile dressing around the tracheostomy tube.
• Change the tracheostomy ties by placing the new ones on first, and removing
the soiled ones last.
• Tie the new ends securely, but not tightly, at the side of the neck.
3.7. End unit 3 summary
Disorders of the nose and throat are considered as disorders of the upper airway
and range from common colds to cancer. The severity depends on the nature of the
disorder and the client’s physiologic response. Most people experience common
colds and sore throats and find them more inconvenient than serious. For others,
even the most common disorders of the upper respiratory airway are of great
concern because other physical problems compound their effects.
Laryngitis is inflammation and swelling of the mucous membrane that lines the
larynx. Edema of the vocal cords frequently accompanies laryngeal inflammation.
Laryngitis may follow a URI and results from spread of the infection to the larynx.
Other causes include excessive or improper use of the voice, allergies, and smoking.
Hoarseness, inability to speak above a whisper, or aphonia (complete loss of voice)
are the usual symptoms.
In addition, clients complain of throat irritation and a dry, nonproductive cough. The
diagnosis is based on the symptoms. If hoarseness persists more than 2 weeks,
the larynx is examined (laryngoscopy). Persistent hoarseness is a sign of laryngeal
cancer and thus merits prompt investigation. Treatment involves voice rest and
treatment or removal of the cause. Antibiotic therapy may be used if a bacterial
infection is the cause. If smoking is the cause, the nurse encourages smoking
cessation and refers the client to a smoking-cessation program.
Tonsillitis is inflammation of the tonsils, and adenoiditis is inflammation of the
adenoids. These conditions generally occur together—the common diagnosis is
tonsillitis. Although both disorders are more common in children, they also may be
seen in adults. The tonsils and adenoids are lymphatic tissues and common sites
of infection. Primary infection may occur in the tonsils and adenoids, or the infection
can be secondary to other URIs. Chronic tonsillar infection leads to enlargement
and partial upper airway obstruction. Chronic adenoidal infection can result in acute
or chronic infection in the middle ear (otitis media). If the causative organism is
group A streptococcus, prompt treatment is needed to prevent potential cardiac and
renal complications.
Pharyngitis, inflammation of the throat, is often associatedwith rhinitis and other
URIs. Viruses and bacteria cause pharyngitis. The most serious bacteria are the
group A streptococci, which cause a condition commonly referred to as strep
throat. Strep throat can lead to dangerous cardiac complications (endocarditis and
rheumatic fever) and harmful renal complications (glomerulonephritis). Pharyngitis
is highly contagious and spreads via inhalation of or direct contamination with
droplets. The incubation period for pharyngitis is 2 to 4 days.
The first symptom is a sore throat, sometimes severe, with accompanying dysphagia
(difficulty swallowing), fever, chills, headache, and malaise. Some clients exhibit a
white or exudate patch over the tonsillar area and swollen glands. A throat culture
reveals the specific causative bacteria. Rapid identification methods, such as the
Biostar or the Strep A optical immunoassay (OIA), are available to diagnose group
The first symptom is a sore throat, sometimes severe, with accompanying dysphagia
(difficulty swallowing), fever, chills, headache, and malaise. Some clients exhibit a
white or exudate patch over the tonsillar area and swollen glands. A throat culture
reveals the specific causative bacteria. Rapid identification methods, such as the
Biostar or the Strep A optical immunoassay (OIA), are available to diagnose group
A streptococcal infections. These tests are done in clinics and physician offices.
Standard 24-hour throat culture and sensitivity tests identify other organisms.
Early antibiotic treatment is the best choice for pharyngitis to treat the infection
and help prevent potential complications. Penicillin or its derivatives are generally
the antibiotics of choice. Clients sensitive to penicillin receive erythromycin. Theantibiotic regimen is 7 to 14 days.
Sinusitis is inflammation of the sinuses. The maxillary sinus is affected most often.
Sinusitis can lead to serious complications, such as infection of the middle ear or
brain. The principal causes are the spread of an infection from the nasal passages
to the sinuses and the blockage of normal sinus drainage. Interference with sinus
drainage predisposes a client to sinusitis because trapped secretions readily
become infected. Impaired sinus drainage may result from allergies (which cause
edema of the nasal mucous membranes), nasal polyps, or a deviated septum.
Rhinitis is inflammation of the nasal mucous membranes. It also is referred to as
the common cold, or coryza. Rhinitis may be acute, chronic, or allergic, depending
on the cause. The most common cause is the rhinovirus, of which more than 100
strains exist. Colds are rapidly spread by inhalation of droplets and direct contact
with contaminated articles (e.g., telephone receivers, doorknobs). Allergic rhinitis is
a hypersensitive reaction to allergens, such as pollen, dust, animal dander, or food.
Rhinitis is usually not a serious condition; however, it may lead to pneumonia and
other more serious illnesses for debilitated, immunosuppressed, or older clients.
Symptoms associated with rhinitis include sneezing,
nasal congestion, rhinorrhea (clear nasal discharge), sore throat, watery eyes,
cough, low-grade fever, headache, aching muscles, and malaise. With the common
cold, these symptoms continue for 5 to 14 days. A sustained elevated temperature
suggests a bacterial infection or infection in the sinuses or ears. Symptoms of
allergic rhinitis will persist as long as the client is exposed to the specific allergen.
For most clients, treatment for rhinitis is minimal. Unless specific bacteria are
identified as the cause of the infection, antibiotics are not used. Clients may be
advised to use antipyretics, such as acetaminophen or nonsteroidal analgesics, for
fever. Decongestants such as pseudoephedrine may be recommended for severe
nasal congestion.
For clients experiencing a prolonged cough, antitussives may be ordered. Saline
gargles are useful for a sore throat, as is saline spray for nasal congestion and
prevention of crusting. For allergic rhinitis, antihistamines are often used. An
example of a first-generation antihistamine is diphenhydramine (Benadryl). Newer
antihistamines include loratadine (Claritin), fexofenadine (Allegra), and cetirizine
(Zyrtec). Combination decongestants and antihistamines may also be helpful. An
example of this is brompheniramine/pseudoephedrine (Dimetapp). Medications
that desensitize or suppress immune responses, such as cromolyn (Nasalcrom)
or intranasal glucocorticosteroids, such as fluticasone (Flonase) may also beprescribed for allergic rhinitis.
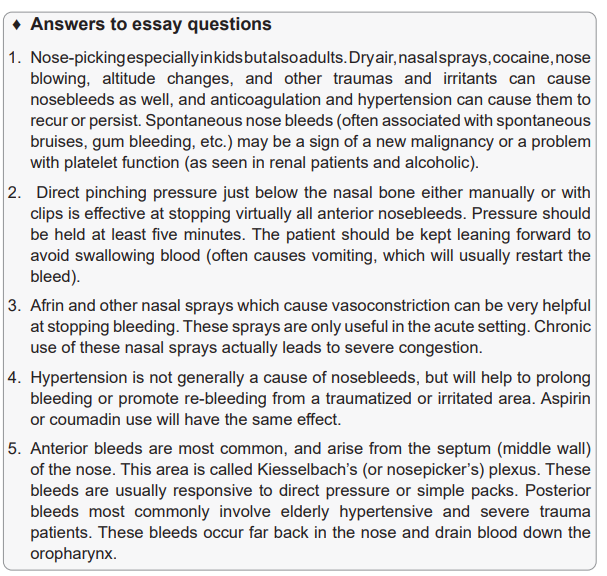
Epistaxis, or nosebleed, is a common occurrence. It is not usually serious but can
be frightening. Nosebleeds are the rupture of tiny capillaries in the nasal mucous
membrane.
They occur most commonly in the anterior septum, referred to as Kiesselbach’s
plexus. Causes of nosebleed include trauma, rheumatic fever, infection,
hypertension, nasal tumors, and blood dyscrasias. Epistaxis that results from
hypertension or blood dyscrasias is likely to be severe and difficult to control. Those
who abuse cocaine may have frequent nosebleeds. Foreign bodies in the nose
and deviated septum contribute to epistaxis, along with forceful nose blowing and
frequent or aggressive nose picking.
Obstruction of the nasal passage interferes with air passage. Three primary
conditions lead to nasal obstruction: a deviated septum, nasal polyps, and
hypertrophied turbinates.
A peritonsillar abscess is an abscess that develops in the connective tissue between
the capsule of the tonsil and the constrictor muscle of the pharynx. It may follow a
severe streptococcal or staphylococcal tonsillar infection. Clients with a peritonsillar
abscess experience difficulty and pain with swallowing, fever, malaise, ear pain,
and difficulty talking. On visual examination, the affected side is red and swollen,
as is the posterior pharynx. Drainage from the abscess is cultured to identify the
microorganism. Sensitivity studies determine the appropriate antibiotic therapy.
Immediate treatment of a peritonsillar abscess is recommended to prevent the
spread of the causative microorganism to the bloodstream or adjacent structures.
Penicillin or another antibiotic is given immediately after a culture is obtained and
before results of the culture and sensitivity tests are known. Surgical incision and
drainage of the abscess are done if the abscess partially blocks the oropharynx.
A local anesthetic is sprayed or painted on the surface of the abscess, and the
contents are evacuated. Repeated episodes may necessitate.
a tonsillectomy. Nursing management of the client undergoing drainage of an
abscess includes placing the client in a semi-Fowler’s position to prevent aspiration.
An ice collar may be ordered to reduce swelling and pain. The nurse encourages
the client to drink fluids. He or she observes the client for signs of respiratory
obstruction (e.g., dyspnea, restlessness, cyanosis) or excessive bleeding.
A nasal fracture usually results from direct trauma. It causes swelling and edema
of the soft tissues, external and internal bleeding, nasal deformity, and nasal
obstruction. In severe nasal fractures, cerebrospinal fluid, which is colorless and
clear, may drain from the nares. Drainage of cerebrospinal fluid suggests a fracture
in the cribriform plate. The diagnosis of a nasal fracture may be delayed because of
significant swelling and bleeding. As soon as the swelling decreases, the examiner
inspects the nose internally to rule out a fracture of the nasal septum or septal
hematoma. Both conditions require treatment to prevent destruction of the septal
cartilage. If drainage of clear fluid is observed, a Dextrostix is used to determine
the presence of glucose, which is diagnostic for cerebrospinal fluid. Radiographystudies are done to ascertain any other facial fractures.
Laryngeal trauma occurs during motor vehicle accidents when the neck strikes
the steering wheel or other blunt trauma occurs in the neck region. Endoscopic
and endotracheal intubations are other possible causes. Although uncommon, a
fracture of the thyroid cartilage is also traumatic to the larynx. Laryngeal obstruction
is an extremely serious and often life-threatening condition. Some causes of upper
airway obstruction include edema from an allergic reaction, severe head and neck
injury, severe inflammation and edema of the throat, and aspiration of foreignbodies.
3.8 Additional activities
A. Remedial activities
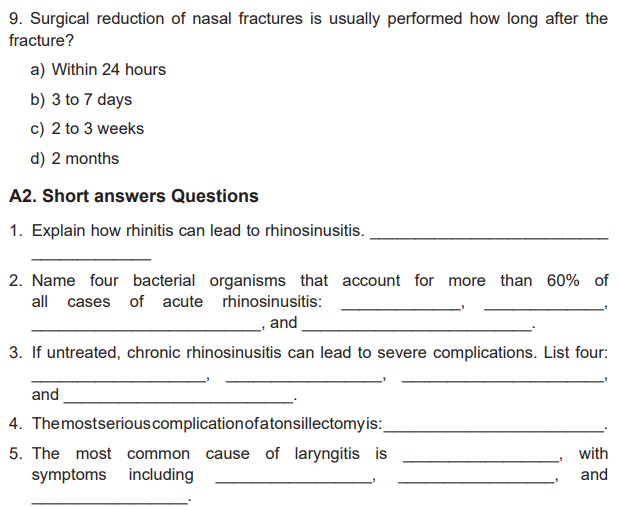
A1. Multiple choices Questions
1. Nursing measures associated with the uncomplicated common cold include all
of the following except:
a) Administering prescribed antibiotics to decrease the severity of the viral
infection.
b) Informing the patient about the symptoms of secondary infection, the major
complication of a cold.
c) Suggesting adequate fluid intake and rest.
d) Teaching people that the virus is contagious for 2 days before symptoms
appear and during the first part of the symptomatic phase.
2. Health teaching for viral rhinitis (common cold) includes advising the patient to:
a) Blow his or her nose gently to prevent spread of the infection.
b) Blow through both nostrils to equalize the pressure.
c) Rest, to promote overall comfort.
d) Do all of the above.
3. About 60% of cases of acute rhinosinusitis are caused by bacterial organisms.
The antibiotic of choice is:
a) Augmentin.
b) Amoxil.
c) Erythromycin.
d) Septra.
4. Acute pharyngitis of a bacterial nature is most commonly caused by:
a) Group A, beta-hemolytic streptococci.
b) Gram-negative Klebsiella.
c) Pseudomonas.
d) Staphylococcus aureus.
5. A complication of acute pharyngitis can be:
a) Mastoiditis.
b) Otitis media.
c) Peritonsillar abscess.
d) All of the above.
6. Nursing management for a patient with acute pharyngitis includes:
a) Applying an ice collar for symptomatic relief of a severe sore throat.
b) Encouraging bed rest during the febrile stage of the illness.
c) Suggesting a liquid or soft diet during the acute stage of the disease.
d) All of the above measures.
7. The most common bacterial pathogen associated with tonsillitis and adenoiditis is:
a) Group a, beta-hemolytic streptococcus.
b) Gram-negative klebsiella.
c) Pseudomonas.
d) Staphylococcus aureus.
8. Nursing intervention for a patient with a fractured nose includes all of the following
except:
a) Applying cold compresses to decrease swelling and control bleeding.
b) Assessing respirations to detect any interference with breathing.
c) Observing for any clear fluid drainage from either nostril.
d) Packing each nostril with a cotton pledget to minimize bleeding and helpmaintain the shape of the nose during fracture setting
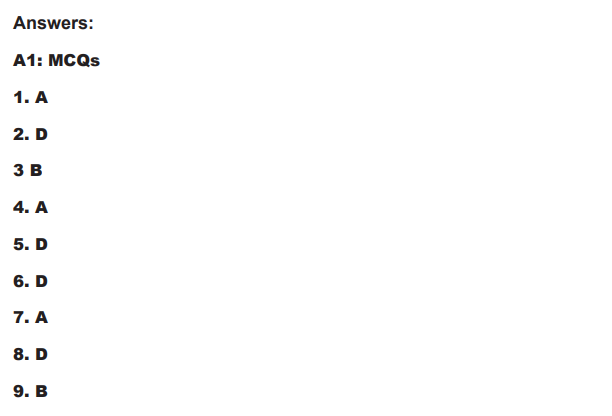
C. Extended activities
C1: Multiple choice Questions:
1. A patient was seen in the clinic for an episode of epistaxis, which was controlled
by placement of anterior nasal packing. During discharge teaching, the nurse
instructs the patient to:
a) Use aspirin for pain relief.
b) Remove the packing later that day.
c) Skip the next dose of antihypertensive medication.
d) Avoid vigorous nose blowing and strenuous activity.
2. A patient with allergic rhinitis reports severe nasal congestion; sneezing; and
watery, itchy eyes and nose at various times of the year. To teach the patient to
control these symptoms, the nurse advises the patient to:
a) Avoid all intranasal sprays and oral antihistamines.
b) Limit the usage of nasal decongestant spray to 10 days.
c) Use oral decongestants at bedtime to prevent symptoms during the night.
d) Keep a diary of when the allergic reaction occurs and what precipitates it.
3. A patient is seen at the clinic with fever, muscle aches, sore throat with yellowish
exudate, and headache. The nurse anticipates that the collaborative management
will include (select all that apply)
a) Antiviral agents to treat influenza.
b) Treatment with antibiotics starting asap.
c) A throat culture or rapid strep antigen test.
d) Supportive care, including cool, bland liquids.
e) Comprehensive history to determine possible etiology.
4. The best method for determining the risk of aspiration in a patient with a
tracheostomy is to:
a) Consult a speech therapist for swallowing assessment.
b) Have the patient drink plain water and assess for coughing.
c) Assess for change of sputum color 48 hours after patient drinks small amount
of blue dye.
d) Suction above the cuff after the patient eats or drinks to determine presence
of food in trachea.
5. Which nursing action would be of highest priority when suctioning a patient with
a tracheostomy?
a) Auscultating lung sounds after suctioning is complete
b) Providing a means of communication for the patient during the procedure
c) Assessing the patient’s oxygenation saturation before, during, and after
suctioningd) Administering pain and/or antianxiety medication 30 minutes before suctioning
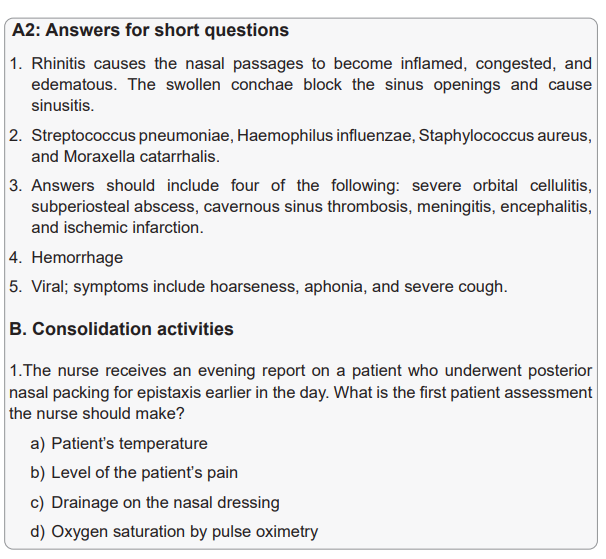
Case studies
A. Isabel, a 14-year-old girl, has just undergone a tonsillectomy and adenoidectomy.
The staff nurse assists her with transport from the recovery area to her room.
1. On the basis of knowledge about tonsillar disease, the nurse knows that Isabel
must have experienced symptoms that required surgical intervention. Clinical
manifestations may have included:
a) Hypertrophy of the tonsils.
b) Repeated attacks of otitis media.
c) Suspected hearing loss secondary to otitis media.
d) All of the above.
2. The nurse assesses Isabel’s postoperative vital signs and checks for the most
significant postoperative complication of:
a) Epiglottis.
b) Eustachian tube perforation.
c) Hemorrhage.
d) Oropharyngeal edema.
3. The nurse maintains Isabel in the recommended postoperative position of:
a) Prone with her head on a pillow and turned to the side.
b) Reverse trendelenburg with the neck extended.
c) Semi-fowler’s position with the neck flexed.
d) Supine with her neck hyperextended and supported with a pillow.
4. Isabel is to be discharged the same day of her tonsillectomy. The nurse makes
sure that her family knows to:
a) Encourage her to eat a house diet to build up her resistance to infection.
b) Offer her only clear liquids for 3 days, to prevent pharyngeal irritation.
c) Offer her soft foods for several days to minimize local discomfort and supply
her with necessary nutrients.
d) Supplement her diet with orange and lemon juices because of the need for
vitamin c to health tissues.
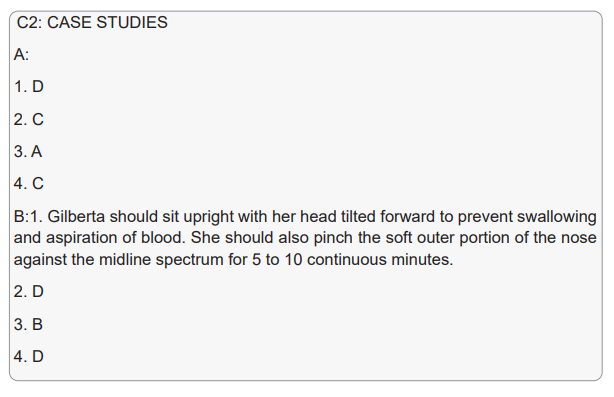
B. Gilberta, a 14-year-old high school student, is sent with her mother to the
emergency department of a local hospital for uncontrolled epistaxis.
1. Describe what the school nurse should tell Gilberta to manage the bleeding sitewhile being transported to the hospital.
2. Initial nursing measures in the emergency department that can be used to stop
the nasal bleeding include:
a) Compressing the soft outer portion of the nose against the midline septum
continuously for 5 to 10 minutes.
b) Keeping Gilberta in the upright position with her head tilted forward to prevent
swallowing and aspiration of blood.
c) Telling Gilberta to breathe through her mouth and to refrain from talking.
d) All of the above.
3. The nurse expects that emergency medical treatment may include insertion of a
cotton pledget moistened with:
a) An adrenergic blocking agent.
b) A topical anesthetic.
c) Protamine sulfate.
d) Vitamin K.
4. The nurse can advise the mother that nasal packing used to control bleeding can
be left in place:
a) No longer than 2 hours.
b) An average of 12 hours.
c) An average of 24 hours.d) Anywhere from 2 to 6 days.