UNIT1: MEDICAL PATHOLOGIES OF EYE
(Blepharitis, Conjunctivitis, Myopia, Hyperopia/Hypermetropia, and
Cataract).
1.1. Key unit competence:
Take appropriate decision on different common medical pathologies of the eyes.
1.2. Prerequisite (knowledge, skills, attitudes, and values)
To achieve the above competence, the associate nurse student needs the following
prerequisites: human body anatomy and physiology, fundamentals of Nursing,
pharmacology.
1.3. Cross-cutting Issues to be addressed
1.3.1. Standardization culture
In health care system, the most case of patients are presented with medical
pathology of eye such conjunctivitis, blepharitis, myopia, hypermetropia and
cataract. The learners have to learn eye diseases in order to handle and to manage
the patients with eye related diseases.
1.3.2. Inclusive education
The teacher involves the students in all learning activities concerning the kind of
learner or disabilities for example the slow learner should be reinforced in order to
catch up others, and the teacher takes into consideration respective disability of
learner.
Grouping students: Students with special educational needs are grouped
with others and assigned roles basing on individual student’s abilities.
Providing earning resources earlier before teaching session so that students get
familiar with them. After end lesson assessment, the identified slow learners are
exposed to the remedial learning activities.
Every important point is written and spoken. The written points help students with
hearing impairment and speaking aloud helps students with visual impairment.Remember to repeat the main points of the lessons.
1.3.3. Gender education
Emphasize to learners that anybody irrespective of their gender can have medical
career mainly medical sciences. Give role models who are successful medical
pathology of eye in the area where the learners come from. Make sure that during
classroom teaching and skills lab demonstration both boys and girls shares and
participate equally in practices, arranging and proper hygiene after classroom and
skills lab teaching session.
1.4 Guidance on the introductory activity
This introductory activity helps you to engage learners in the introduction of medical
pathology of eye and invite the learners to follow the next lessons.
Teacher’s activity:
• Ask students to read the text and discuss the given questions.
• Engage students in working collectively the activity• Help students with different problems
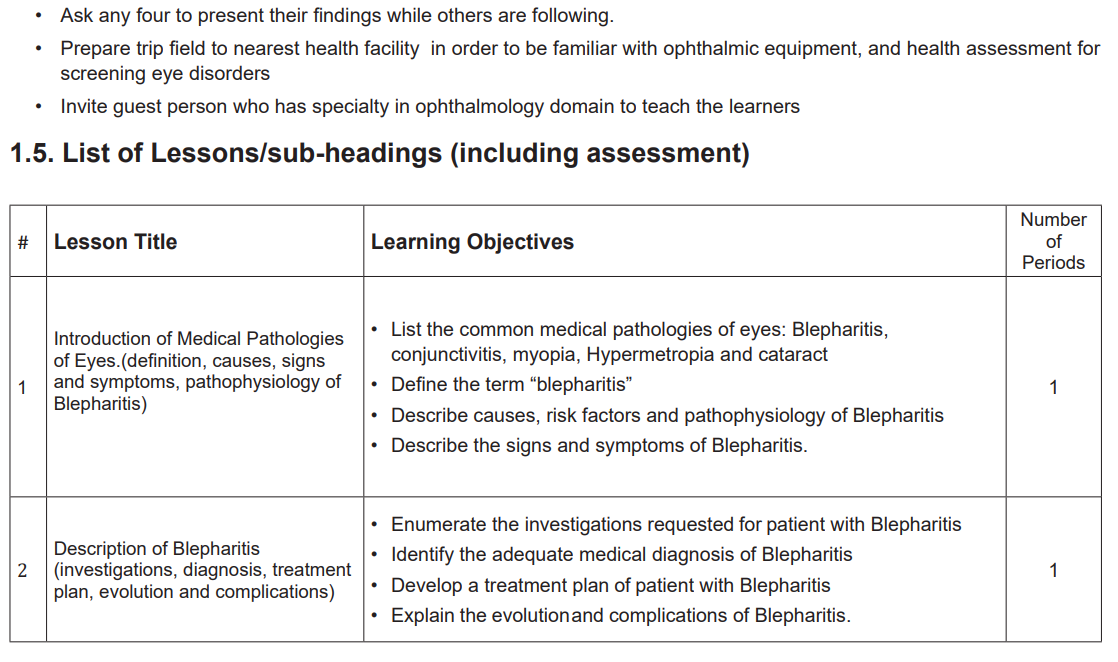
Lesson 1: Introduction of Medical Pathologies of Eyes. (Definition,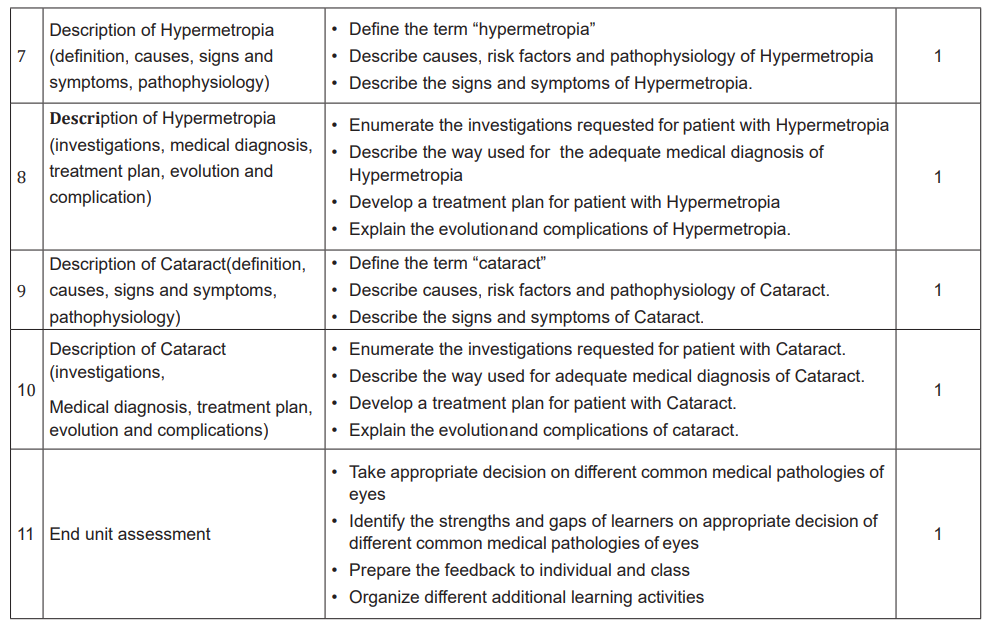
causes, signs and symptoms, pathophysiology of Blepharitis)
a) Prerequisites
This is the first lesson of the first unit on medical pathologies of eyes in sensory
system. In this lesson you will be dealing with the common medical pathologies
of eyes which are Blepharitis, Conjunctivitis, Myopia, Hypermetropia and Cataract.
The first thing to do before starting teaching is to remind learners that they have
learnt about structure and function of eyes in biology, health assessment of eyes
from fundamentals of nursing, and let them discuss the questions as indicated
in introductory activity. In addition, the students will read and try to answer the
questions provided in the case study from learning activity 1.1 so that they can
prepare themselves for this lesson.
b) Learning objectives
• List the common medical pathologies of eyes: Blepharitis, conjunctivitis,
myopia, Hypermetropia and cataract.
• Define the term “blepharitis”
• Describe causes, risk factors and pathophysiology of Blepharitis
• Describe the signs and symptoms of Blepharitis.
c) Teaching resources
The teacher could avail the Snellen chart, ophthalmoscope and ensure that the
students are able to use them. Also, the teacher should present to the students
the library textbooks on medical-surgical nursing especially eyes diseases and
indicates the pages. All students must have their student’s books. The algorithm or
protocols about eyes diseases management must be availed. There is a need of
black board and chalks or flipcharts and markers.
d) Learning activities 1.1
Teacher ‘activities and methodology:
• Ask learners to do individually activity 1.1 in their student book and answer
the question number 2 and 3.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard, flipchart, and whiteboard the main students’ ideas.
• Tick the correct responses and correct those ones which are incorrect and try
again to complete those which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
Student‘s activity
• The students answer the questions individually in learning activity 1.1 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
Expected answers to introductory activity 1.0
1. The human eye is an organ of vision. A vital organ of vision it plays a very
important role not only in life but also the human body. The human eye is the
organ which gives us the sense of sight, allowing us to learn more about the
surrounding world than we do with any of the other four senses. The eye allows
us to see and interpret the shapes, colors, and dimensions of objects in the
world by processing the light they reflect or emit. The eye is able to see in bright
light or in dim light, but it cannot see objects when there is no light
2. Left eye is not normal
3. The left eye is colored in blue while right eye is black pupil
4. The left is small then right
5. Conjunctivitis, cataract, glaucoma, blepharitis, myopia, and hypermetropia .
Expected Answers to Questions from Learning Activity 1.1
1. The different external parts of the eye structures that have been affected: Eyelid,
iris, pupil, sclara, conjunctiva (palpebral and bulbar)
2. The signs and symptoms that patient present are discharges, swollen right
eyelid, burning sensation causing itching of right eye, itching of right eye3. Conjunctivitis, blepharitis, eye infection
Lesson 2: Description of Blepharitis (investigation diagnosis, treatmentplan, evolution and complication)
a) Revision
This is the second lesson of the first unit on medical pathologies of eyes in sensory
system. In this lesson you will be dealing with the description of blepharitis such its
investigation, diagnosis treatment plan evolution and complication. The first thing to
do before starting teaching is to remind learners that they have learnt about lesson
one of blepharitis
b) Learning objectives
After completion of this lesson, the student will be to:
• Enumerate the investigations requested for patient with Blepharitis
• Identify the adequate medical diagnosis of Blepharitis
• Develop a treatment plan of patient with Blepharitis
• Explain the evolution and complications of Blepharitis.
c) Teaching resources
The teacher could avail the Snellen chart and slip lamp and ensure the students are
able to use them. In addition, the teacher should present to the students the library
textbooks on medical-surgical nursing especially Eyes Diseases and indicates
the pages. All students must have their student’s books. There is need of black
board and chalks or flipcharts and markers. Algorithms about assessment and
management of conjunctivitis must also be displayed
d) Learning activities
Teacher’s activities and methodology
• Ask learners to do individually activity 1.2 in their student book and answer
the questions related.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard the main student’s ideas.
• Tick the correct responses and correct those ones, which are incorrect and try
again to complete those, which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
• Use brainstorming while collecting the answers from different learners.
• Judge the answers from learners by conforming the right responses.
Student’s activities
• The students answer the questions individually in learning activity 1.2 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attempt to answer the self-assessment questions 1.1
Lesson 3: Description of conjunctivitis (definition, causes, signs and
symptoms, pathophysiology)
a) Prerequisites
This is the fourth lesson of the first unit about medical pathologies of the Eyes. In
this lesson, you will be dealing with the description of different types of conjunctivitis:
viral conjunctivitis, bacterial conjunctivitis, and allergic conjunctivitis. The first thing
to do before starting teaching is to remind learners what they have learnt about the
anatomy and physiology of the visual system (Eyes), health assessment of visual
system from fundamentals of nursing. The students will discuss the questions from
the case study from learning activity 1.2 so that they can prepare themselves for
this lesson.
b) Learning objectives:
After completion of this lesson, the student will be able to:
• Define the term “conjunctivitis”
• Describe causes, risk factors and pathophysiology of different types of
conjunctivitis.
• Describe the signs and symptoms of different types of conjunctivitis.
c) Teaching resources
The teacher could avail the Snellen chart and Ophthalmoscope and ensure the
students are able to use them. In addition, the teacher should present to the students
the library textbooks on medical-surgical nursing especially Eyes Diseases and
indicates the pages. All students must have their student’s books.
There is need of black board and chalks or flipcharts and markers. Algorithms aboutassessment and management of conjunctivitis must also be displayed.
d) Learning activities
Teacher’s activities and methodology
• Ask learners to do individually activity 1.2 in their student book and answer
the questions related.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard the main student’s ideas.
• Tick the correct responses and correct those ones, which are incorrect and try
again to complete those which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
• Use brainstorming while collecting the answers from different learners.
• Judge the answers from learners by conforming the right responses.
Student’s activities
• The students answer the questions individually in learning activity 1.3 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition
• Attempt to answer the self-assessment questions 1.3
The expected answers from Questions of learning activity1.2
1. The signs and symptoms that the patient was presenting are sticky eyelids,
watery and green ocular discharge, redness, soreness and slightly blurred vision
in both eyes for about 3 weeks.
Other additional information you would ask the patient to guide about the medical
diagnosis:
• Is there anyone from the family who had same symptoms?
• Past medical and surgical history
2. Conjunctivitis, infection of the eye, inflammation of the eye, eye diseases etc
3. The risk factors that exposed the patient to develop that medical condition:
• Other medical condition: flu syndrome
• Poor hygiene
• Possible answers for the questions
• Risk factors include exposure to infected individuals, fomite contact (e.g.,
towels, napkins, pillow, slit-lamp, chin rests and handles), wear, sinusitis,
immunodeficiency states, prior ocular disease, trauma, and exposure to
agents of sexually transmitted disease at birth.
• Poor hygiene
• Contact lens misuse
• Contaminated personal articles
• Crowded living or social conditions (elementary schools, military barracks)
• History of ocular diseases including dry eye, blepharitis, and anatomic
abnormalities of the ocular surface and lids
• Recent ocular surgery, exposed sutures, or ocular foreign bodies
• Chronic use of topical medications
• Immune compromise
• Winter/Summer months (bacterial conjunctivitis peaks in the winter and viral
conjunctivitis peaks in the summer) etc.
Lesson 4: Description of Conjunctivitis (investigation, diagnosis
treatment plan, evolution and complication)
a) Revision
This is the four lesson of the first unit about medical pathologies of the eyes. In
this lesson, you will be dealing with the investigations, diagnosis, treatment plan,
evolution and complications of conjunctivitis. The first thing to do before starting
teaching is to remind learners what they have learnt in the lesson three.
b) Learning objectives:
After completion of this lesson, the student will be able to:
• Enumerate the investigations requested for patient different types of
conjunctivitis.
Describe the way used for adequate medical diagnosis of different types of
conjunctivitis.
• Develop a treatment plan for patient with different types of conjunctivitis.• Explain the evolution and complications of different types of conjunctivitis
c) Teaching resources
The teacher could avail the Snellen chart and Ophthalmoscope and ensure the
students are able to use them. Also, the teacher should present to the students
the library textbooks on medical-surgical nursing especially Eyes Diseases and
indicates the pages. All students must have their student’s books. There is need
of black board and chalks or flipcharts and markers. Algorithms about assessment
and management of conjunctivitis must also be displayed.
d) Learning activities
Teacher’s activities and methodology
• Ask learners to do individually activity 1.2 in their student book and answer
the questions related.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard the main student’s ideas.
• Tick the correct responses and correct those ones , which are incorrect and
try again to complete those which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
• Use brainstorming while collecting the answers from different learners.
• Judge the answers from learners by confirming the right responses.
Student’s activities
• The students answer the questions individually in learning activity 1.3 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition• Attempt to answer the self-assessment questions 1.2
The expected answers from Questions of learning activity1.3
1. Investigations requested to that patient: Polymerase chain reaction (PCR),
Pus/swab culture.
2. The possible medical diagnosis the patient was having is conjunctivitis that
might be bacterial, viral or allergic
3. Different treatments options to this patients’ medical condition are: Hygiene:
washing hands properly (frequent hand washing and keeping hands away
from affected eyes), Cleaning the affected eye using warm compresses,
Antibiotics and Corticosteroids (ointments or drops).
4. If not treated well, the complications might be: reduction of visual acuity/
blindness, ciliary flush, infectious keratitis, iritis, glaucoma, photophobia,
severe foreign body sensation that prevents the patient from keeping the
eye open, corneal opacity, hyperacute bacterial conjunctivitis or epidemic
keratoconjunctivitis, dry eye, pterygium; blepharoconjunctivitis, etc.
♦ Answers for Self-Assessment 1.2
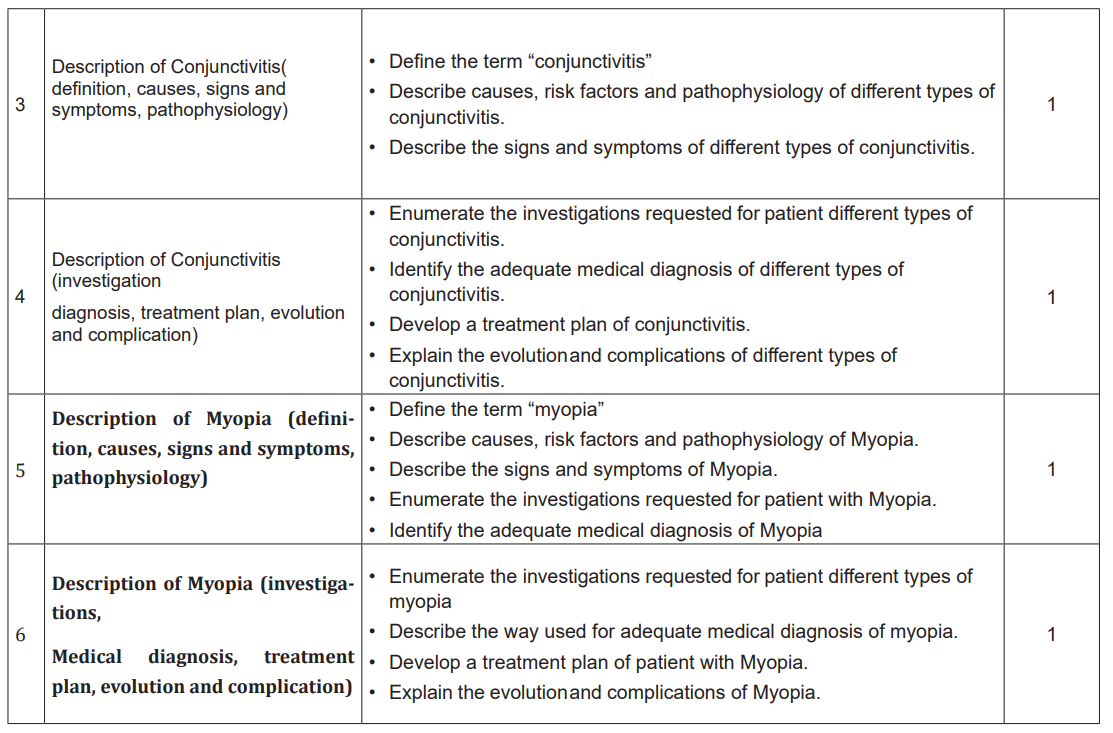
1. Difference between all types of conjunctivitis basing on their causes:
A. Bacterial conjunctivitis is commonly caused by some microorganisms
(staphylococcus aureus, streptococcus pneumoniae, haemophilus influenzae,
and moraxella catarrhalis). Staphylococcus aureus infection is more common in
adults; the other pathogens are more common in children. It is highly contagious
and is spread by direct contact with the patient and their secretions or with
contaminated objects and surfaces.
B. Hyperacute bacterial conjunctivitis: Neisseria species, particularly Neisseria
Gonorrhoeae, is the major cause of a hyperacute bacterial conjunctivitis that is
severe and sight-threatening. The microorganism is usually transmitted from the
genitalia to the hands and then to the eyes.
C. Conjunctivitis due to trachoma: most chronic keratoconjunctivitis are caused by
recurrent infection with Chlamydia trachomatis.
D. Adult inclusion conjunctivitis: It is a sexually transmitted infection (STI) caused
by certain serotypes of Chlamydia trachomatis. The microorganism is usuallytransmitted from the genitalia to the hands and then to the eyes.
E. Viral conjunctivitis: is typically caused by adenovirus, with many serotypes
implicated. Viral conjunctivitis is highly contagious; it is spread by direct contact
with the patient and their secretions or with contaminated objects and surfaces.
F. Allergic conjunctivitis: Is caused by airborne allergens contacting the eye
that trigger a classic type I immunoglobulin E (IgE)-mediated hypersensitivity
response specific to that allergen.
G. Noninfectious, non-inflammatory conjunctivitis: patients can develop a red eye
and discharge that is not related to either an infectious or inflammatory process.Usually the cause is a transient mechanical or chemical insult.
1) Using a table, here is the difference between bacterial, viral, andallergic conjunctivitis basing on their symptoms:
2) The rationale of taking swabs from discharges for laboratory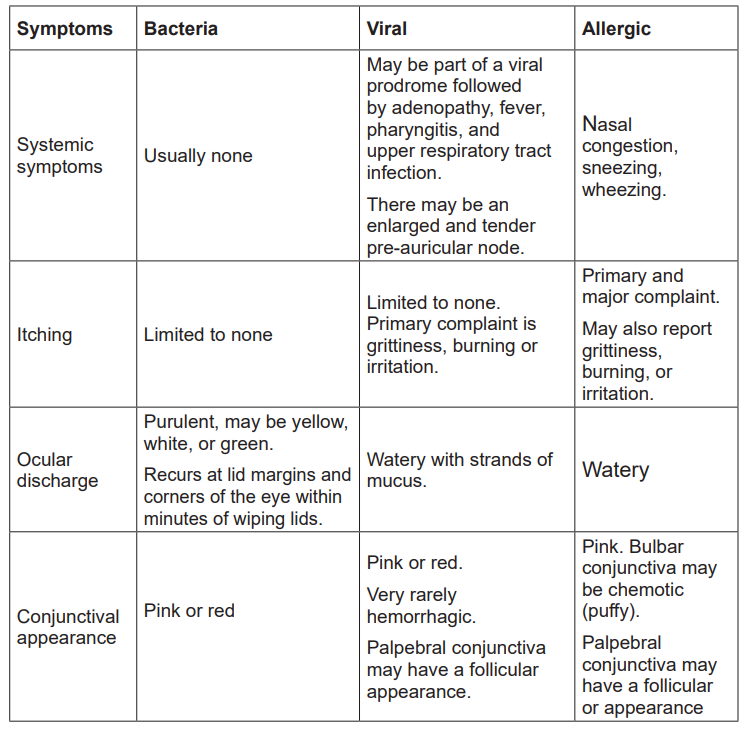
analysis among the patients with conjunctivitis is:
It is important in cases of chronic conjunctivitis or when the condition is not
responding/fail to improve or to respond to treatment. It also helps in guiding
about the medications that must be taken as sensitive to any specific type of
microorganisms. The management guide should come from the results fromswabs culture.
3) The treatments modalities specific to each type of conjunctivitis:
Bacterial conjunctivitis: antibiotic treatment is required for acute conjunctivitis in
contact lens wearers as well as for cases of adult inclusion conjunctivitis or hyper acute
bacterial conjunctivitis. Preferred choices include erythromycin, azithromycin,
chloramphenicol ophthalmic ointment or trimethoprim-polymyxin B drops. Common
alternative therapies include bacitracin ointment and bacitracin-polymyxin B ointment.
Fluoroquinolones are not first-line therapy for routine cases of bacterial conjunctivitisbecause of concerns regarding emerging resistance and cost.
Adult inclusion conjunctivitis treatment: Antibiotic treatment for
adult inclusion conjunctivitis requires systemic therapy (typically
with doxycycline, tetracycline, erythromycin, or azithromycin) to eradicate
the Chlamidia trachomatis infection.
Viral conjunctivitis: there are no specific topical or systemic antiviral agents for the
treatment of viral conjunctivitis. Symptomatic relief may be achieved with: topical
antihistamine/decongestants, warm or cool compresses, nonantibiotic lubricating
agents such as those used for noninfectious conjunctivitis.
Allergic conjunctivitis: The first step is to remove or avoid the irritant, if possible.
Cool compresses and artificial tears sometimes relieve discomfort in mild cases. In
more severe cases, nonsteroidal anti-inflammatory medications and antihistamines
may be prescribed. People with persistent allergic conjunctivitis may also require
topical steroid eye drops. Oral antihistamines may also be prescribed.
Toxic conjunctivitis: the primary approach to toxic conjunctivitis is recognition and
removal of the offending agent. Stopping as many topical agents as feasible is a
good first step.
Noninfectious noninflammatory: Symptoms relief with the use of topical lubricants
might be useful.
Chemical conjunctivitis: careful flushing of the eyes with saline is a standard
treatment for chemical conjunctivitis. People with chemical conjunctivitis also may
need to use topical steroids. Severe chemical injuries, particularly alkali burns, flushthe eye for several minutes with a lot of water before seeing your medical provider.
Persistent symptoms: patients with acute bacterial conjunctivitis usually respond
to treatment within one to two days by showing a decrease in discharge, redness,
and irritation. Patients who do not respond should be referred to an ophthalmologist.
Some effective behaviour change activities that are needed to prevent seriousness
and complications of conjunctivitis:
• Preventing contagion: Infected individuals should not share handkerchiefs,
tissues, towels, cosmetics, linens, or eating utensils. Frequent hand washing
and keeping hands away from eyes also can make a difference, even when
no problems are present.
• Avoid allergy triggers as much as possible
• Need for examination or consultation prior to therapy: Otherwise, the eye
examination must be done carefully and rely on findings to decide the
management. Complications of conjunctivitis are the major reasons for urgent
ophthalmologic referral.
4) The warning signs and symptoms of eye diseases that must
prompt urgent referral to ophthalmologist:
♦ Answers to Application Activity 1.2
reduction of visual acuity; photophobia; severe foreign body sensation that
prevents the patient from keeping the eye open; corneal opacity; fixed pupil;
severe headache with nausea; suspicion for hyperacute bacterial conjunctivitis
or epidemic keratoconjunctivitis (EKC); dry eye; medicamentosa; pterygium;blepharo conjunctivitis and adult inclusion conjunctivitis; etc.
♦ Answers to Application Activity 1.2
1. The medical condition that this patient was suffering from: Bacterial
conjunctivitis or hyperacute bacterial conjunctivitis
2. The possible risk factors that contributed to the development of such medical
condition: lack of water access, possible urinary tract infection (lower abdominal
pain and dysuria), foreign body in the eye, flu like syndrome
3. Why chloramphenicol (0.5%) was stopped until the laboratory results are
available: the Laboratory results were needed to guide the antibiogram basing
on types of microorganisms identified from culture and the sensitivity test.
4. The warning signs that show that the patient had complications and different
complications she should experience:
Warning signs: sticky eyelids, pus like discharge, lack of improvement after
antibiotic uses, photophobia.
Complications: hyperacute bacterial conjunctivitis, keratoconjunctivitis,infectious keratitis
5. The elements that should constitute the management plan of this patient:
• Health education about frequent hand washing and keeping hands away
from the infected eyes
• Health education about urinary tract infections screening
• Health education about pathogenesis and complications of eyes diseases
and relationship between eyes diseases with poor hygiene
• To request all needed investigations (urine culture, eyes swabs culture,
complete blood count, renal function tests, liver function tests, and
• Antibiotics and other symptoms relief management (cool compresses in
cleaning secretions
6. The interventions you would advise her to do in order to minimize the
seriousness of complication and avoid cross-transmission to other family
members:
• Preventing contagion: Practice frequent hand washing and keeping hands
away from eyes also can make a difference. Avoid touching the normal eye
after touching infected eye.
• Avoid allergy triggers as much as possible
• Need for examination or consultation prior to therapy: Otherwise, the eye
examination must be done carefully and rely on findings to decide the
management. Complications of conjunctivitis are the major reasons for
urgent ophthalmologic referral.
• Effective use of antibiotics prescribed• Respect of appointment for follow up
Lesson 5: Description of Myopia (definition causes, signs andsymptoms, pathophysiology)
This is the fifth lesson in the unit 1 of medical pathologies of eyes, lesson deals with
definition of myopia, causes, pathophysiology, clinical manifestation, and medical
investigation of myopia.
a) Prerequisite
For successful teaching and learning process of this lesson, learners should have
enough knowledge of the different parts of the eye and the function of the eye that
they have already studied in the previous lessons of biology, in addition the learners
should have the overview of physic especially in optic lesson. They should be well
skilled in drawing the structure of the eye.
• Students to recall the main parts of the structure of the eyes and their functions
• The knowledge and skills about optic principles in physic and eyes function
(accommodation of the eyes)
b) Learning objectives
After completion of this lesson, the student will be able to:
• Define the key concepts of myopia
• List the common causes and pathophysiology of myopia
• List the different signs and symptoms of myopia
• Describe briefly medical investigations for myopia
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. The teaching materials are white board, flip chart, marker, computer,
Snellen chart, tape measure, textbook, and videos. The teaching methods are
interactive lecture, Group discussion, course work and trip field or guest teacher.
In addition to the teacher’s guide, the learners where they can find the supporting
resources such computer lab, Nursing skills lab and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course
and provide experiences that will enable students to engage in practice and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as: taking notes, course work and reading textbook
related to the lesson, group assignment and summarize the content, engagement
in debate and other clinical learning activities such as case study.
Teacher’s activity:
• Ask learners to do individually activity 1.2 in their student book and answer
the questions related.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard the main student’s ideas.
• Tick the correct responses and correct those ones, which are incorrect and try
again to complete those, which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
• Use brainstorming while collecting the answers from different learners.• Judge the answers from learners by confirming the right responses.
Student’s activities
• The students answer the questions individually in learning activity 1.5 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition
• Attempt to answer the self-assessment questions 1.5
♦ Answer to activity 1.3
1. Difficulty reading road signs and seeing distant objects clearly, eye strain and
headaches, trouble seeing things that are far away, needing to squint to see
clearly, eye strain
2. Basing on those signs and symptoms, what could be the medical problem of
this patient?
3. The medical problem of this patient could be myopia.
4. What medical investigations might you expect to be ordered to guide the
confirmation of the medical problem?
• The Snellen eye chart is considered one of the clinical standards for
evaluating visual acuity
• A retinoscopy and pinhole occlude could be performed by an ophthalmologist
Lesson 6: Description of Myopia (investigation, diagnosis, treatment
plan, evolution and complication)
This is the Sixth lesson in the unit 1 of medical pathologies of eyes, lesson deals
with the medical and nursing management of myopia.
a) Revision
This is the fifth lesson of the first unit about medical pathologies of the eyes. In
this lesson, you will be dealing with the investigation, diagnosis, treatment plan,
evolution and complication of myopia. The first thing to do before starting teachingis to remind learners what they have learnt lesson five.
b) Learning objectives
After completion of this lesson, the learner will be able to:
• Enumerate the investigations requested for patient different types of myopia
• Describe the way used for adequate medical diagnosis of myopia.
• Develop a treatment plan of patient with Myopia.
• Explain the evolution and complications of Myopia.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. The teaching materials are white board, flip chart, marker, computer,
Snellen chart, and library textbook. The teaching methods are interactive lecture,
Group discussion, and trip field or guest teacher. In addition to the teacher’s guide,
the learners can find the supporting resources such computer lab, Nursing skills
lab, Library and clinical placement)
d) Learning activities
Learning activities should be directly related to the learning objectives of the course
and provide experiences that will enable students to engage in practice and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as: taking notes, course work and reading textbook
related to the lesson, group assignment and summarize the content, engagement
in debate and other clinical learning activities such as case study.
Teacher’s activity:
• Ask learners to do individually activity 1.2 in their student book and answer
the questions related.
• Provide the necessary materials.
• Move around in silence to monitor if they are having some problems
• Remember to assist those who are weak but without giving them the
knowledge.
• Invite any five students to provide they answers
• Ask other students to follow carefully the answers provided by students
• Note on the blackboard the main student’s ideas.
• Tick the correct responses and correct those ones which are incorrect and try
again to complete those which are incomplete.
• Harmonize and conclude on the learned knowledge and still engage student
in making that conclusion.
• Use brainstorming while collecting the answers from different learners.• Judge the answers from learners by confirming the right responses.
♦ Answers to activity 1.3
1) The decision to treat refractive disorders depends on the individual
patient’s symptoms and needs. Treatment is aimed to improve visual
acuity, visual comfort
2) First-line treatments include corrective lenses, such as glasses and contact
lenses, or refractive surgery, Eyeglasses, Contact lenses, Refractive
surgery
3) Cataract formation, retinal detachment from peripheral retinal tears, retinal
detachment, dome-shaped macula, choroidal/scleral thinning, myopic
choroidal, limitations in instrumental activities of daily living (IADLs) falls,
decreased ability to drive or work, and depression etc.
♦ Answers for self-assessment 1.3
1) The Five signs and symptoms of myopia are:
• Difficulty seeing distant objects clearly
• Eye strain
• Frontal headaches
• Trouble seeing things that are far away,
• Squinting to see clearly
• Eye strain
• Being fatigued
2) The three preventive measures for myopia complications
development are:
• Take breaks when using computers or cell phones.
• Prevent myopia from worsening, spend time outside and try to focus on
objects that are in the distance.
• Vision therapy. .
• The use of progressive or bifocal lenses (spectacles or contact lenses) mayyield a slowing of myopia by limiting eye accommodation.
3) The three cause and risk factors of myopia are:
• Genetic factors
• Increased intraocular pressure
• Prolonged reading or reading at close range
• Diabetes mellitus
• Trauma of the retina
• maternal smoking during pregnancy
4) The three main medical treatment options to correct
nearsightedness are:Prescription of eyeglasses, contact lenses or refractive surgery
Lesson7: Description of Hypermetropia (definition, causes, signs andsymptoms, pathophysiology)
a) Preriquisites
This is the Seventh lesson of the first unit Medical pathologies of eyes. In this
lesson you will be dealing with the meaning of Hypermetropia or Hyperopia. Before
to do start thinking is to remind learners that they have learnt about structure and
function of the eye in Biology and let the learners discuss the meaning of refractive
errors so that they may get prepared for this lesson. Proceed with the lesson byintroducing to them the learning activity 3.1 in the students ’books.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Define the term ‘’hypermetropia’’
• Describe the signs and symptoms of hypermetropia.
• Describe causes, risk factors and pathophysiology of Hypermetropia
• Identify the adequate medical diagnosis of Hypermetropia• Describe the investigations requested for patient with Hypermetropia
a) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. The teaching aids are white board, flip chart, markers, computers and
projectors, Snellen chart, flipchart, and library textbook. The teaching methods
are interactive lecture, Group discussion, and field trip. In addition to the teacher’sguide, the learners can find the supporting resources such computer lab, Nursing
skills lab and Library.
Teacher’s activity:
• Guide learners to form groups of five learners
• Provide learners with textbooks and guide them to brainstorm the concept
related to the refractive errors (Hyperopia).
• Supervise the work where the learners are grouped in small group of five
learners and teacher facilitates them to answer the questions by using the
case study.
• Invite some of the learner’s group members to present their findings.
• Judge the logic of the learners’ products by correcting those that are false,
complete those which are incomplete and confirming those which are correct
• Engage the learners to the clinical settings (Ophthalmology department)
• Help learners to summarize what they have learnt.
Student’s activities
• The students answer the questions individually in learning activity 1.4 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition• Attempt to answer the self-assessment questions 1.3
Answers for learning activity 1.4
1. The problem may be hypermetropia (hyperopia or farsightedness)
2. Headache, blurred vision, eye discomfort, difficult in reading his newspapers
as he did before, he states that he could clearly read only the written scripture
that are far from him3. Eye muscle test and Visual Acute Test using Snellen chart
Lesson 8: Description of Hypermetropia (investigation diagnosis,treatment plan, evolution and complication)
a) Revision
This is the eight lesson of the first unit about medical pathologies of the eyes. In
this lesson, you will be dealing with the investigation, diagnosis, treatment plan,
evolution and complication of hypermetropia. The first thing to do before startingteaching is to remind learners what they have learnt lesson five
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Enumerate the investigations requested for patient with Hypermetropia
• Describe the way used for the adequate medical diagnosis of Hypermetropia
• Develop a treatment plan for patient with Hypermetropia• Explain the evolution and complications of Hypermetropia.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. The teaching materials are white board, flip chart, markers, computers
and projectors, Snellen chart, flipchart, and library textbook. The teaching methods
are interactive lecture, Group discussion, and field trip. In addition to the teacher’s
guide, the learners can find the supporting resources such computer lab, Nursing skillslab and Library.
d) Learning activities
Teacher’s activity:
• Guide learners to form groups of five learners
• Provide learners with textbooks and guide them to brainstorm the concept
related to the refractive errors (Hyperopia).
• Supervise the work where the learners are grouped in small group of five
learners and teacher facilitates them to answer the questions by using the
case study and textbook from school library.
• Invite some of the learner’s group members to present their findings.
• Judge the logic of the learners’ products by correcting those that are false,
complete those which are incomplete and confirming those which are correct
• Engage the learners to the clinical settings (Ophthalmology department)• Help learners to summarize what they have learnt.
Student’s activities
• The students answer the questions individually in learning activity 1.4 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition• Attempt to answer the self-assessment questions 1.3
Answers for learning activity 1.3
1. The current treatment of hyperopia evolves and can be corrected with
eyeglasses, contact lenses, bifocal Glasses those includes:
• Glasses: This the standard treatment for all children and adult for the
majority
• Contact lens: contacts are great option, you can change the color of the
patient eyes and this could be tried during a contact lens examination.
• Bifocal glasses: This is an excellent and effective treatment for moderate
levels of hyperopia in you people as it enhances a young person’s ability to
see up and far away
2. Farsightedness can be associated with several problems, such as:
• Crossed eyes: Some children with farsightedness may develop crossed
eyes. Specially designed eyeglasses that correct for part or all of the
farsightedness may treat this problem’
• Reduced quality of life: With uncorrected farsightedness, the patient might
not be able to perform a task as well as he/she wish. Moreover, the limited
vision may detract from the patient enjoyment of day-to-day activities.
• Eyestrain: Uncorrected farsightedness may cause the patient to squint orstrain the eyes to maintain focus. This can lead to eyestrain and headaches.
♦ Answers to Self-assessment
1. The two signs of hypermetropia include blurred vision, the patient may need
to squint to see clearly, eyestrain, burning sensation of the eyes and aching in
or around the eyes, general eye discomfort or a headache after doing close
tasks such as reading, writing, computer work or drawing
2. The causes of hyperopia include axial shortening of the eyeball. Flattening of
the cornea, change in the refractive index of the crystalline lens, malposition
or absence of the crystalline lens.
3. The investigations to confirm hypermetropia includes Visual acute Test, Visual
field Test, Slit-lamp examination, ophthalmoscopy or Fundus copy.
4. The options of hyper metropia treatment are: Eye glasses, Contacts lens,
bifocal glasses
5. The complications of hypermetropia includes Crossed eyes, reduced qualityof life, eyestrain, impaired safety, financial burden.
Lesson 9: Description of Cataract (definition, causes, signs and
symptoms, pathophysiology)
This is the Ninth lesson in the unit 1 of medical pathologies of eyes, lesson deals
with definition of cataract, causes, pathophysiology, clinical manifestation, and
medical investigation of cataract.
a) Prerequisite
For successful teaching and learning process of this lesson, learners should have
enough knowledge of the different parts of the eye and the function of the eye that
they have already studied in the previous lessons of biology. They should be well
skilled in drawing the structure of the eye.
b) Learning objectives
On completion of this lesson, the learner will be able to:
• Define the term “cataract”
• Describe causes, risk factors and pathophysiology of Cataract.
• Describe the signs and symptoms of Cataract.
c) Teaching resources
This lesson will be taught with different aids and methods in order to achieve learning
objectives. These teaching aids are white board, flip chart, marker, computer,
Snellen chart, tape measure textbook, and videos. The teaching methods are
interactive lecture, Group discussion, and course work. In addition to the teacher’s
guide, the learners where they can find the supporting resources such computerlab, Nursing skills lab and Library.
d) Learning activities
Learning activities should be directly related to the learning objectives of the course
and provide experiences that will enable students to engage in practice, and gain
feedback on specific progress towards those objectives. The various learning
activities will be carried out such as: taking notes, course work and reading textbook
related to the lesson, group assignment and summarize the content, engagement
in debate and other clinical learning activities such as case study.
Teacher’s activity:
• Ask the learners to brainstorm the meaning of myopia, identify the
common signs and symptoms of the patient with cataract
• Teacher guide to use textbook in school library, computer lab.
• Supervise the work where the learners are grouped in small group of 5
learners and teacher facilitates them to find the books which are related
the subjects
• After 30 minutes, ask learners to comeback and to present what they have
done in their groups
• Help learners to summarize what they have learnt.
• Engage the learners to the clinical settings (Ophthalmology department)
Student’s activities
• The students answer the questions individually in learning activity 1.4 in their
student book
• The students ask the problems that may be raised from the provided activity
if any in order to get clarification
• Some students present the findings from the learning activity while others are
following carefully
• Summarize the content with the teacher and coming up with conclusion.
• Attend the library for reading related book of eye condition• Attempt to answer the self-assessment questions 1.4
♦ Answer to activity 1.4
1. Differentiate the normal and abnormal eye on the above observed diagram
• Right eye is big than left eye,
• Right eye has black color pupil, and
• Left eye blue color
2. Which diseases do you think could affect the abnormal eyes?
Common Eye Disorders and Diseases
• Refractive Errors.
• Age-Related Macular Degeneration.
• Cataract.
• Diabetic Retinopathy.
• Glaucoma.
• Amblyopia.
• Strabismus.
♦ Answers to self-assessment 1.4
a) The most common symptoms of cataracts include:
• Clouded, blurred or dim vision
• Increasing difficulty with vision at night
• Sensitivity to light and glare
• Need for brighter light for reading and other activities
• Seeing “halos” around lights
• Frequent changes in eyeglass or contact lens prescription
• Fading or yellowing of colors
• Double vision in a single eye
1) The causes of cataract are:
Most cataracts develop when aging or injury changes the tissue that makes up the
eye’s lens. Proteins and fibers in the lens begin to break down, causing vision to
become hazy or cloudy.
Some iherited genetic disorders that cause other health problems can increase
your risk of cataracts. Cataracts can also be caused by other eye conditions, past
eye surgery or medical conditions such as diabetes. Long-term use of steroidmedications, too, can cause cataracts to develop.
2) The types of cataract are:
Cataract types include:
• Cataracts affecting the center of the lens (nuclear cataracts).
• Cataracts that affect the edges of the lens (cortical cataracts
• Cataracts that affect the back of the lens (posterior subcapsular cataracts
• Cataracts you’re born with (congenital cataracts)
3) The complications of cataract are:
Over time, cataracts become worse and start to interfere with vision. Important skills
can be affected, such as driving, and loss of vision can affect the overall quality of
life in many ways including reading, working, hobbies and sports. If left untreated,
cataracts will eventually cause total blindness.
1.6. Summary of the unit
Medical pathology is a branch of medical science primarily concerning the diseases
affects different human organs such as respiratory tract organs, cardio-vascular
organs, digestive organs, urino-genetal organs, sensory organs etc. This unit of
medical pathology of the eye described the most common eye conditions that met
in Rwanda such conjunctivitis, blepharitis, myopia, hypermetropia, and cataract.
This unit describes the eye conditions by providing their definition, clinical features,
investigation, treatment plan, evolution and complications. The student who learns
this content will be able to take appropriate decision on different common medical
pathologies of eyes in terms of diagnosing, treatment and prevent the complication
of conjunctivitis, blepharitis, myopia, hypermetropia, and cataract.
1.7 Additional Information for teachers
Common additional eye disorders and diseases.
• Diabetic Retinopathy.
• Glaucoma.
• Amblyopia.
• Strabismus.Age-Related Macular Degeneration.
Definition
Age-related macular degeneration (AMD) is a common condition that affects the
middle part of your vision. It usually first affects people in their 50s and 60s.
It does not cause total blindness. However, it can make everyday activities like
reading and recognizing faces difficult.
Without treatment, your vision may get worse. This can happen gradually over
several years (“dry AMD”), or quickly over a few weeks or months (“wet AMD”).
The exact cause is unknown. It has been linked to smoking, high blood pressure,
being overweight and having a family history of AMD.
Symptoms
The first symptom is often a blurred or distorted area in your vision.
Other symptoms include:
• seeing straight lines as wavy or crooked
• objects looking smaller than normal
• colors seeming less bright than they used to
• seeing things that are not there (hallucinations)
Diagnosis
• Sometimes the patient may be referred to an eye doctor (ophthalmologist).
• This is usually only necessary if there is a possibility the patient will need to
start treatment quickly within a day.
• The patient may have more tests, such as a scan of the back of the eyes.
If the patient is diagnosed with AMD, the specialist will give the information about
the type of disease and the treatment options.
Treatment depends on the type of AMD you have.
• Dry AMD – there is no treatment, but vision aids can help reduce the effect on
the patient life. Read about living with AMD.
• Wet AMD – you may need regular eye injections and, very occasionally, alight treatment called photodynamic therapy, to stop your vision getting worse.
1) Glaucoma
Definition
Glaucoma is a condition that damages your eye’s optic nerve. It gets worse over
time. It’s often linked to a buildup of pressure inside your eye. Glaucoma tends to
run in families. You usually don’t get it until later in life.
The increased pressure in the eye, called intraocular pressure, can damage your
optic nerve, which sends images to your brain. If the damage worsens, glaucoma
can cause permanent vision loss or even total blindness within a few years..
If you lose vision, it can’t be brought back. But lowering eye pressure can help you
keep the sight you have. Most people with glaucoma who follow their treatmentplan and have regular eye exams are able to keep their vision.
Glaucoma Causes
The fluid inside your eye, called aqueous humor, usually flows out of your eye
through a mesh-like channel. If this channel gets blocked, or the eye is producing
too much fluid, the liquid builds up. Sometimes, experts don’t know what causes
this blockage. But it can be inherited, meaning it’s passed from parents to children
Less-common causes of glaucoma include a blunt or chemical injury to your eye,
severe eye infection, blocked blood vessels inside your eye, and inflammatory
conditions. It’s rare, but eye surgery to correct another condition can sometimes
bring it on. It usually affects both eyes, but it may be worse in one than the other.
Glaucoma Risk Factors
It mostly affects adults over 40, but young adults, children, and even infants
can have it. African American people tend to get it more often, when they’re
younger, and with more vision loss.
• Are over 40
• Have a family history of glaucoma
• Are nearsighted or farsighted
• Have poor vision
• Have diabetes
• Take certain steroid medications such as prednisone
• Take certain drugs for bladder control or seizures, or some over-the-counter
cold remedies
• Have had an injury to your eye or eyes
• Have corneas that are thinner than usual
• Have high blood pressure, heart disease, diabetes, or sickle cell anemia• Have high eye pressure
Types of Glaucoma
There are two main kinds:
Open-angle glaucoma: this is the most common type. The doctor may also call
it wide-angle glaucoma. The drain structure in your eye (called the trabecular
meshwork) looks fine, but fluid does not flow out, as it should.
Angle-closure glaucoma: This is more common in Asia. The patient may also hear it
called acute or chronic angle-closure or narrow-angle glaucoma. The eye does not
drain, as it should because the drain space between iris and cornea becomes too
narrow. This can cause a sudden buildup of pressure in your eye. It is also linked to
farsightedness and cataracts, a clouding of the lens inside the eye.
Less common types of glaucoma include:
Secondary glaucoma. This is when another condition, like cataracts or diabetes,
causes added pressure in the eye.
Normal-tension glaucoma. This is when the patient has blind spots in the vision
or the optic nerve is damaged even though the eye pressure is within the average
range. Some experts say it is a form of open-angle glaucoma.
Pigmentary glaucoma. With this form, tiny bits of pigment from your iris, the colored
part of your eye, get into the fluid inside your eye and clog the drainage canals.
Glaucoma Symptoms
Most people with open-angle glaucoma do not have symptoms. If symptoms do
develop, it is usually late in the disease. That is why glaucoma is often called the
“sneak thief of vision.” The main sign is usually a loss of side, or peripheral, vision.
Symptoms of angle-closure glaucoma usually come on faster and are more obvious.
Damage can happen quickly. If the patient has any of these symptoms, he/she may
get medical care right away:
• Seeing halos around lights
• Vision loss
• Redness in your eye
• Eye that looks hazy (particularly in infants)
• Upset stomach or vomiting• Eye pain
Glaucoma Diagnosis
Glaucoma tests are painless and do not take long. Your eye doctor will test your
vision. They will use drops to widen (dilate) your pupils and examine your eyes.
They will check your optic nerve for signs of glaucoma. They may take photographs
so they can spot changes at your next visit. They will do a test called tonometry to
check the eye pressure. They may also do a visual field test to see if there is a loss
of peripheral vision.
If the doctor suspects glaucoma, they may order special imaging tests of the optic
nerve.
Glaucoma Treatment
Your doctor may use prescription eye drops, oral medications, laser surgery, or
microsurgery to lower pressure in the eye.
Eye drops. These either lower the creation of fluid in the eye or increase its flow
out, lowering eye pressure. Side effects can include allergies, redness, stinging,
blurred vision, and irritated eyes. Some glaucoma drugs may affect the heart and
lungs. Because of potential drug interactions, be sure to tell the doctor about any
other medical problems.
Oral medication. The doctor might also prescribe medication to take by mouth,
such as a beta-blocker or a carbonic anhydrase inhibitor. These drugs can improve
drainage or slow the creation of fluid in the eye.
Laser surgery. This procedure can slightly raise the flow of fluid from the eye if the
patient has an open-angle glaucoma. It can stop fluid blockage if the patient has an
angle-closure glaucoma. Procedures include:
• Trabeculoplasty. This opens the drainage area.
• Iridotomy. This makes a tiny hole in the iris to let fluid flow more freely.
• Cyclophotocoagulation. This treats areas of the middle layer of the eye to
lower fluid production.
2) Trachoma
Trachoma is an infectious disease caused by bacterium Chlamydia trachomatis.
[2] The infection causes a roughening of the inner surface of the eyelids.[2] This
roughening can lead to pain in the eyes, breakdown of the outer surface or cornea
of the eyes, and eventual blindness.[2] Untreated, repeated trachoma infections
can result in a form of permanent blindness when the eyelids turn inward
Signs and symptoms of trachoma
The bacterium has an incubation period of 6 to 12 days, after which the affected
individual experiences symptoms of conjunctivitis, or irritation similar to “pink
eye”. Blinding endemic trachoma results from multiple episodes of reinfection that
maintains the intense inflammation in the conjunctiva. Without reinfection, theinflammation gradually subsides.
The conjunctival inflammation is called “active trachoma” and usually is seen in
children, especially preschool children. It is characterized by white lumps in the
undersurface of the upper eyelid (conjunctival follicles or lymphoid germinal centres)
and by nonspecific inflammation and thickening often associated with papillae.
Follicles may also appear at the junction of the cornea and the sclera (limbal
follicles). Active trachoma often can be irritating and have a watery discharge.
Bacterial secondary infection may occur and cause a purulent discharge
Most commonly, children with active trachoma do not present with any symptoms,
as the low-grade irritation and ocular discharge is just accepted as normal, but
further symptoms may include:
• Eye discharge
• Swollen eyelids
• Trichiasis (misdirected eyelashes)
• Swelling of lymph nodes in front of the ears
• Sensitivity to bright lights
• Increased heart rate
• Further ear, nose, and throat complications
Cause of trachoma
Trachoma is caused by Chlamydia trachomatis, serotypes (serovars) A, B,
and C. It is spread by direct contact with eye, nose, and throat secretions from
affected individuals, or contact with fomites (inanimate objects that carry infectious
agents), such as towels and/or washcloths, that have had similar contact with
these secretions. Flies can also be a route of mechanical transmission. Untreated,
repeated trachoma infections result in entropion (the inward turning of the eyelids),
which may result in blindness due to damage to the cornea. Children are the most
susceptible to infection due to their tendency to get dirty easily, but the blinding
effects or more severe symptoms are often not felt until adulthood.
Blinding endemic trachoma occurs in areas with poor personal and family hygiene.
Many factors are indirectly linked to the presence of trachoma including lack of
water, absence of latrines or toilets, poverty in general, flies, close proximity to
cattle, and crowding.The final common pathway, though, seems to be the presence
of dirty faces in children, facilitating the frequent exchange of infected ocular
discharge from one child’s face to another. Most transmission of trachoma occurswithin the family.
Diagnosis
McCallan’s classification
Mc Callan in 1908 divided the clinical course of trachoma into four stages:
WHO classification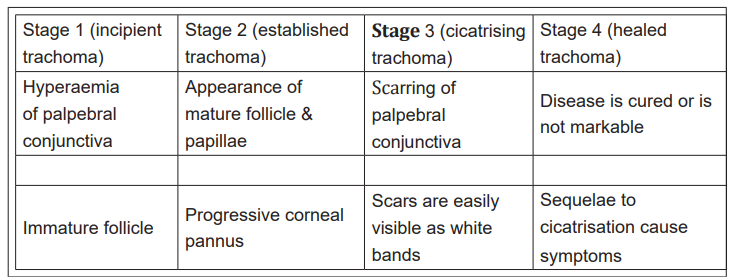
The World Health Organization recommends a simplified grading system for
trachoma. The Simplified WHO Grading System is summarized below:
Trachomatous inflammation, follicular (TF)—Five or more follicles of >0.5 mm on
the upper tarsal conjunctiva
Trachomatous inflammation, intense (TI)—Papillary hypertrophy and inflammatory
thickening of the upper tarsal conjunctiva obscuring more than half the deep tarsal
vessels
Trachomatous scarring (TS)—Presence of scarring in tarsal conjunctiva.
Trachomatous trichiasis (TT)—At least one ingrown eyelash touching the globe, or
evidence of epilation (eyelash removal)
Corneal opacity (CO)—Corneal opacity blurring part of the pupil margin
Management.
Azithromycin (single oral dose of 20 mg/kg) or topical tetracycline (1% eye ointmenttwice a day for six weeks). Azithromycin is preferred because it is used as a single
Management
Azithromycin (single oral dose of 20 mg/kg) or topical tetracycline (1% eye ointment
twice a day for six weeks). Azithromycin is preferred because it is used as a single
oral dose. Although it is expensive, it is generally used as part of the international
donation program organized by Pfizer. Azithromycin can be used in children from
the age of six months and in pregnancy. As a community-based antibiotic treatment,
some evidence suggests that oral azithromycin was more effective than topical
tetracycline, but no consistent evidence supported either oral or topical antibiotics
as being more effective. Antibiotic treatment reduces the risk of active trachoma in
individuals infected with chlamydial trachomatis.
Surgery
For individuals with trichiasis, a bilamellar tarsal rotation procedure is warranted to
direct the lashes away from the globe. Evidence suggests that use of a lid clamp
and absorbable sutures would result in reduced lid contour abnormalities and
granuloma formulation after surgery. Early intervention is beneficial as the rate of
recurrence is higher in more advanced disease.
Lifestyle measures
The WHO-recommended SAFE strategy includes:
• Surgery to correct advanced stages of the disease
• Antibiotics to treat active infection, using azithromycin
• Facial cleanliness to reduce disease transmission
• Environmental change to increase access to clean water and improved
sanitation
Children with visible nasal and eyes discharge, or flies on their faces are at least
twice as likely to have active trachoma. The children with clean faces can also
have it. Intensive community-based health education programs to promote face
washing can reduce the rates of active trachoma, especially intense trachoma. If an
individual is already infected, washing one’s face is encouraged, especially a child,
to prevent reinfection. Some evidence shows that washing the face combined with
topical tetracycline might be more effective in reducing severe trachoma compared
to topical tetracycline alone. The same trial found no statistical benefit of eye
washing alone or in combination with tetracycline eye drops in reducing follicular
trachoma amongst children
3) Strabismus
Strabismus is a condition in which the eyes do not properly align with each other
when looking at an object the eye that is focused on an object can alternate. The
condition may be present occasionally or constantly. If present during a large part
of childhood, it may result in amblyopia or lazy eyes and loss of depth perception. Ifonset is during adulthood, it is more likely to result in double vision.
Signs and symptoms
When observing a person with strabismus, the misalignment of the eyes may be
quite apparent. A person with a constant eye turn of significant magnitude is very
easy to notice. However, a small magnitude or intermittent strabismus can easily be
missed upon casual observation. In any case, an eye care professional can conduct
various tests, such as cover testing, to determine the full extent of the strabismus.
Symptoms of strabismus include double vision and eye strain. To avoid double
vision, the brain may adapt by ignoring one eye. In this case, often no noticeable
symptoms are seen other than a minor loss of depth perception. This deficit may not
be noticeable in someone who has had strabismus since birth or early childhood,
as they have likely learned to judge depth and distances using monocular cues.
However, a constant unilateral strabismus causing constant suppression is a risk
for amblyopia in children. Small-angle and intermittent strabismus are more likely
to cause disruptive visual symptoms. In addition to headaches and eye strain,
symptoms may include an inability to read comfortably, fatigue when reading, and
unstable or “jittery” vision.
The extraocular muscles control the position of the eyes. Thus, a problem with
the muscles or the nerves controlling them can cause paralytic strabismus. The
extraocular muscles are controlled by cranial nerves III, IV, and VI. An impairment
of cranial nerve III causes the associated eye to deviate down and out and may or
may not affect the size of the pupil. Impairment of cranial nerve IV, which can be
congenital, causes the eye to drift up and perhaps slightly inward. Sixth nerve palsy
causes the eyes to deviate inward and has many causes due to the relatively long
path of the nerve. Increased cranial pressure can compress the nerve as it runs
between the clivus and brain stem. In addition, if the doctor is not careful, twisting
of the baby’s neck during forceps delivery can damage cranial nerve VI.
Pathophysiology
Evidence indicates a cause for strabismus may lie with the input provided to the
visual cortex. This allows for strabismus to occur without the direct impairment of
any cranial nerves or extraocular muscles.
Strabismus may cause amblyopia due to the brain ignoring one eye. Amblyopia is the
failure of one or both eyes to achieve normal visual acuity despite normal structural
health. During the first seven to eight years of life, the brain learns how to interpret
the signals that come from an eye through a process called visual development.
Development may be interrupted by strabismus if the child always fixates with one
eye and rarely or never fixates with the other. To avoid double vision, the signal
from the deviated eye is suppressed, and the constant suppression of one eyecauses a failure of the visual development in that eye.
In addition, amblyopia may cause strabismus. If a great difference in clarity occurs
between the images from the right and left eyes, input may be insufficient to correctly
reposition the eyes. Other causes of a visual difference between right and left eyes,
such as asymmetrical cataracts, refractive error, or other eye disease, can also
cause or worsen strabismus.
Accommodative esotropia is a form of strabismus caused by refractive error in
one or both eyes. Due to the near triad, when a person engages accommodation to
focus on a near object, an increase in the signal sent by cranial nerve III to the medial
rectus muscles results, drawing the eyes inward; this is called the accommodation
reflex. If the accommodation needed is more than the usual amount, such as with
people with significant hyperopia, the extra convergence can cause the eyes to
cross.
Diagnosis
During an eye examination, a test such as cover testing or the Hirschberg test is
used in the diagnosis and measurement of strabismus and its impact on vision.
Retinal birefringence scanning can be used for screening of young children for eye
misalignment. A Cochrane review to examine different types of diagnosis test found
only one study. This study used a photoscreener which was found to have high
specificity (accurate in identifying those without the condition) but low sensitivity
(inaccurate in identifying those with the condition)
Management
Strabismus is usually treated with a combination of eyeglasses, vision therapy, and
surgery, depending on the underlying reason for the misalignment. As with other
binocular vision disorders, the primary goal is comfortable, single, clear, normal
binocular vision at all distances and directions of gaze.
Whereas amblyopia (lazy eye), if minor and detected early, can often be corrected
with use of an eye patch on the dominant eye or vision therapy, the use of eye
patches is unlikely to change the angle of strabismus.
Glasses
In cases of accommodative esotropia, the eyes turn inward due to the effort of
focusing far-sighted eyes, and the treatment of this type of strabismus necessarily
involves refractive correction, which is usually done via corrective glasses or contact
lenses, and in these cases surgical alignment is considered only if such correctiondoes not resolve the eye turn.
In case of strong anisometropia, contact lenses may be preferable to spectacles
because they avoid the problem of visual disparities due to size differences
(aniseikonia) which is otherwise caused by spectacles in which the refractive
power is very different for the two eyes. In a few cases of strabismic children with
anisometropic amblyopia, a balancing of the refractive error eyes via refractive
surgery has been performed before strabismus surgery was undertaken.
Early treatment of strabismus when the person is a baby may reduce the chance
of developing amblyopia and depth perception problems. However, a review of
randomized controlled trials concluded that the use of corrective glasses to prevent
strabismus is not supported by existing research. Most children eventually recover
from amblyopia if they have had the benefit of patches and corrective glasses.
Amblyopia has long been considered to remain permanent if not treated within
a critical period, namely before the age of about seven years; however, recent
discoveries give reason to challenge this view and to adapt the earlier notion of a
critical period to account for stereopsis recovery in adults.
Eyes that remain misaligned can still develop visual problems. Although not a cure
for strabismus, prism lenses can also be used to provide some temporary comfort
and to prevent double vision from occurring.
Glasses affect the position by changing the person’s reaction to focusing. Prisms
change the way light, and therefore images, strike the eye, simulating a change in
the eye position.
Surgery
Strabismus surgery does not remove the need for a child to wear glasses. Currently
it is unknown whether there are any differences for completing strabismus surgery
before or after amblyopia therapy in children.
Strabismus surgery attempts to align the eyes by shortening, lengthening, or
changing the position of one or more of the extraocular eye muscles. The procedure
can typically be performed in about an hour, and requires about six to eight weeks
for recovery. Adjustable sutures may be used to permit refinement of the eye
alignment in the early postoperative period. It is unclear if there are differences
between adjustable versus non-adjustable sutures as it has not been sufficiently
studied. An alternative to the classical procedure is minimally invasive strabismussurgery (MISS) that uses smaller incisions than usual.
1.8 Answers to end unit 1 assessment
Section A: Short Answer Questions
1. BLEPHARITIS
2. CONJUNCTIVITIS
3. KERATITIS
4. CATARACT
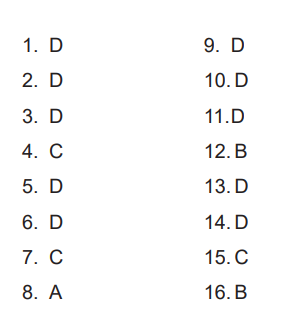
5. CONVEXSection B: Multiple Choice Questions
1.9 Additional activities
1.9.1 Remedial activities
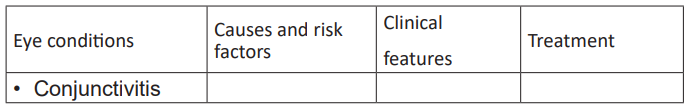
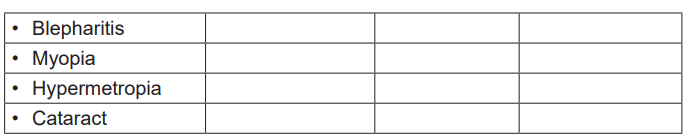
a. Using different literature define the following medical pathology eye
condition
• Conjunctivitis
• Blepharitis
• Myopia
• Hypermetropia
• Cataractb. Complete the following table
1.9.2 Consolidation activities
1. Label the following diagrammed of eye
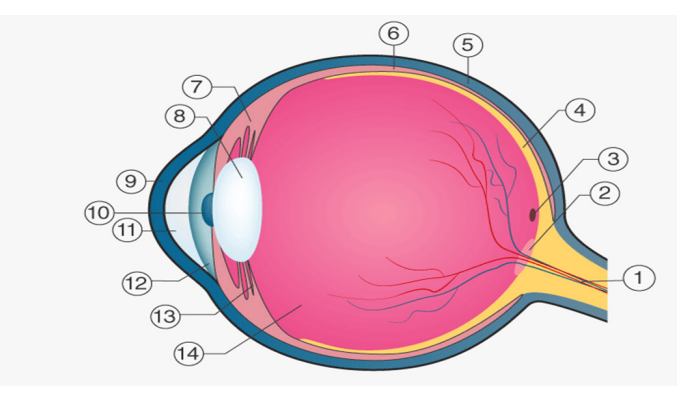
Answers
2. What are the functions of human eye?
The human eyes are the most complicated sense organs in the human body. From
the muscles and tissues to nerves and blood vessels, every part of the human eye
is responsible for a certain action. Furthermore, contrary to popular belief, the eye
is not perfectly spherical; instead, it is two separate segments fused together. It
is made up of several muscles and tissues that come together to form a roughly
spherical structure. From an anatomical perspective, the human eye can be broadlyclassified into external structure and internal structure.
The External Structure of an Eye
The parts of the eye that are visible externally include the following:
Sclera: It is a white visible portion. It is made up of dense connective tissue and
protects the inner parts.
Conjunctiva: It lines the sclera and is made up of stratified squamous epithelium.
It keeps our eyes moist and clear and provides lubrication by secreting mucus and
tears.
Cornea: It is the transparent, anterior or front part of our eye, which covers the pupil
and the iris. The main function is to refract the light along with the lens.
Iris: It is the pigmented, coloured portion of the eye, visible externally. The main
function of the iris is to control the diameter of the pupil according to the light source.
Pupil: It is the small aperture located in the centre of the Iris. It allows light to enter
and focus on the retina
The Internal Structure of an Eye
The internal components of an eye are:
Lens: It is a transparent, biconvex, lens of an eye. The lens is attached to the ciliary
body by ligaments. The lens along with the cornea refracts light so that it focuses
on the retina.
Retina: It is the innermost layer of the eye. It is light sensitive and acts as a film of a
camera. Three layers of neural cells are present in them, they are ganglion, bipolar
and photoreceptor cells. It converts the image into electrical nerve impulses for the
visual perception by the brain.
Optic nerve: It is located at the posterior portion of the eyes. The optic nerves carry
all the nerve impulses from the retina to the human brain for perception.
Aqueous Humour: It is a watery fluid present between the cornea and the lens. It
nourishes the eye and keeps it inflated.
Vitreous Humour: it is a transparent, jelly-like substance present between the lens
and the retina. It contains water (99%), collage, proteins, etc. The main function of
vitreous humour is to protect the eyes and maintain its spherical shape
1.9.3. Extended activities
1. What are the common eye problems according the ageCommon eye problems by age:
Answers
Babies’ eye infections need to be treated. Some of these are prevented by cleaning
the baby’s eyes and using eye ointment at birth (see page 33).
Young children’s vision problems may be hard to notice. Starting at 6 months old,
see if the child’s eyes move and follow a light or a toy when you move it around. A
child with a wandering or crossed eye can be helped (page 24) and glasses may
help with poor vision. For children with very limited or no vision, Hesperian’s book
Helping Children Who Are Blind shows many ways to help a blind child develop her
skills.
School-age children who cannot see clearly cannot tell you they need
eyeglasses because they do not know what good vision would be like.
A child who has headaches, squints a lot or is having difficulty in school
or playing games may have a vision problem and need eyeglasses. It
is also a good idea to learn what to do if there is an eye injury from sports or
fighting at school.
Any child can get eye injuries. Keep chemicals and sharp objects locked
away and out of reach of children. Adult vision may change at any age and sometimes
eyeglasses can help. If a person has diabetes or high blood pressure, treatment to
manage these problems will help prevent further harm to the eyes. Different kinds of
work make some eye injuries or eye conditions more likely.
Older adults are more likely to develop cataracts and need
reading glasses.
2. What are the illnesses that can affect the eyes
♦ Answers
Some infections or illnesses affecting the whole body can harm the eyes.
When someone has eye problems, it is wise to consider if the cause could
be another illness.
Tuberculosis can infect the eyes and cause redness or poor vision. Most
often, signs of tuberculosis will appear first in the lungs or other parts of
the body. HIV and AIDS: Eye problems and loss of vision in people with HIV are
prevented by treatment with HIV medicines, called ART. Get tested so you
can start treatment if you need it.
Herpes (cold sores) occasionally spreads to the eye, causing an ulcer of the
cornea with pain, blurred vision, and watery eyes. Antiviral medicines arehelpful. Do not use steroid eye drops—they make the problem worse.
Problems in the liver: Jaundice, when the white part of the eye is yellow
(or the skin of a light-colored person gets yellow), can be a sign of hepatitis.
People with diabetes may develop vision problems. As the disease
advances, diabetes can damage their eyes (a serious condition called
diabetic retinopathy). Without treatment, diabetes can lead to blindness.
Blurred vision can be an early sign that blood sugar is high and a person
may have diabetes. If someone with blurred vision also is very thirsty and
has to urinate a lot, it is likely they have diabetes. Inexpensive tests can let
them know for sure.
Help people with diabetes get treatment to bring down their blood sugar
levels and encourage them to visit an eye specialist once a year to check
their eyes for damage from diabetes. Eye disease from diabetes can be
treated if found early.
High blood pressure can affect the eyes and vision by damaging the
blood vessels inside the eye. Checking blood pressure during health care
visits is the best way to know if it is too high. Preventing and treating high
blood pressure will help protect the eyes.
1. What are the treatment of following eye conditions
• Cataract
• Glaucoma
• Fleshy growth across eye ( pterygium)
• Blood in the white of the eye
• Vitamin A deficiency (night blindness, xerophthalmia)• Crossed eyes, wandering eye, squint (strabismus)
♦ Answers
Cataract
Non-Surgical Cataract Treatment
Early cataract treatment is aimed at improving the quality of vision. When cataract
symptoms appear, client may experience cloudy or blurry vision, light sensitivity,
poor night vision, double vision, and changes the eyewear prescription. Certain
changes can significantly reduce these symptoms.
Cataract symptoms may be improved with new eyeglasses, anti-glare sunglasses,
or magnifying lenses. Certain tints and coatings also can be added to lenses toreduce symptoms.
Early cataract treatment is aimed at improving the quality of vision. When cataract
symptoms appear, client may experience cloudy or blurry vision, light sensitivity,
poor night vision, double vision, and changes the eyewear prescription. Certain
changes can significantly reduce these symptoms.
Cataract symptoms may be improved with new eyeglasses, anti-glare sunglasses,
or magnifying lenses. Certain tints and coatings also can be added to lenses toreduce symptoms.
a) Surgical Cataract Treatment
If non-surgical measures do not help, surgery is the only effective treatment. It
is considered when a cataract progresses and decreases vision to a point that it
interferes with the lifestyle and daily activities.
♦ Glaucoma
The treatment will largely depend on which type of glaucoma. The most common
type, primary open angle glaucoma, is usually treated with eye drops. Laser
treatment or surgery may be offered if drops do not help.
Treatment for other types of glaucoma may include:
• primary angle closure glaucoma (immediate treatment in hospital with
medicine to reduce the pressure in the eye, followed by laser treatment)
• secondary glaucoma (eyedrops, laser treatment or surgery, depending on the
underlying cause)
• childhood glaucoma ( surgery to correct the problem in the eye that led to the
build-up of fluid and pressure)
The main treatments are described below.
• Eye drops are the main treatment for glaucoma. There are several different
types that can be used, but they all work by reducing the pressure in your
eyes.
• Eye drops can cause unpleasant side effects, such as eye irritation, and some
are not suitable for people with certain underlying conditions.
Laser treatment
Laser treatment may be recommended if eye drops do not improve your symptoms.
This is where a high-energy beam of light is carefully aimed at part of your eye to
stop fluid building up inside it.
Types of laser treatment include:
• laser trabeculoplasty – a laser is used to open up the drainage tubes within
your eye, which allows more fluid to drain out and reduces the pressure inside
• cyclodiode laser treatment – a laser is used to destroy some of the eye tissue
that produces the liquid, which can reduce pressure in the eye
• laser iridotomy – a laser is used to create holes in your iris to allow fluid to
drain from your eye
Surgery may be recommended in rare cases where treatment with eyedrops orlaser have not been effective.
The most common type of surgery for glaucoma is called trabeculectomy. It involves
removing part of the eye-drainage tubes to allow fluid to drain more easily.
Glaucoma surgery may be carried out under local anaesthetic (while the patient is
awake) or general anaesthetic (while the patient is asleep).
Most people will not need to take eye drops any more after trabeculectomy, and you
should not be in a lot of pain after surgery.Fleshy growth across eye (pterygium)
Treatment
A pterygium often does not cause problems or require
treatment. However, two main treatment approaches can be
considered if the pterygium causes discomfort or affects vision.
Medication Short-term use of topical corticosteroid eye drops may be
used to reduce redness and inflammation. Where dryness of the eyeis a problem, artificial tears are used to keep the eye well lubricated.
Surgery
Surgery may be recommended if vision is affected or symptoms are particularly
problematic.
During surgery, the pterygium is carefully removed and a section of the conjunctiva
is taken from under the eyelid and is grafted onto the area where the pterygium
was. Surgery is performed using a local anaesthetic and takes approximately 30
minutes to perform.
It is possible for pterygia to recur after surgical removal, though this only happensin a small percentage of cases.
Prevention
To reduce the risk of developing pterygia:
• Use sunglasses that block out UV light (close-fitting, wrap around styles are
best)
• Wear sunglasses and a hat with a wide brim when outdoors
• Avoid exposure to environmental irritants, e.g.: smoke, dust, wind, and
chemical pollutants• Use appropriate eye safety equipment in work environments.
Blood in the white of the eye
Treatment for hyphemas and other types of eye bleeding may include:
• laser surgery to bring eye pressure down
• eye surgery in severe cases, such as non-clearing hyphemas that surgeons
need to evacuate in the operating room
• eye drops to control inflammation, pain, and pressure
The type of eye drop an ophthalmologist prescribes will depend on the cause of the
bleeding. Some examples include antibiotic, antiviral, and steroid eye drops.
Sub conjunctival hemorrhages do not usually require treatment. The healing time
can vary from a few days to a few weeks, depending on the size of the spot.
People can use artificial tears to relieve irritation or dryness. Artificial tears are
available in drug stores, pharmacies, and online.
A doctor may prescribe antibiotic eye drops if the red spot is the result of a bacterial
infection.People should not be alarmed if the red spot changes colors from red to
yellow or orange. This is a sign that the hemorrhage is healing. Like a bruise, it may
slowly fade over time.
Treatments for diabetic retinopathy include:
• injectable medications to reduce swelling
• laser eye surgery to close leaking blood vessels
• vitrectomy, or surgery that involves removing vitreous gel and blood from the
back of the eye
Floaters (seeing small spots)
Fortunately, two different treatments can be performed to reduce the presence of
eye floaters, and sometimes even eliminate them:
1. Vitrectomy
2. Vitreolysis
What is a vitrectomy?
A vitrectomy is the primary treatment for eye floaters.
This procedure involves removing the vitreous in order to eliminate
the collagen fibers that are causing the eye floaters.What to expect during a vitrectomy procedure
A vitrectomy is a safe and relatively quick procedure that is generally performed
under local anesthesia. During this procedure, a small incision is made and the
vitreous is removed. A new fluid made of saline or silicone oil is then inserted intothe space of the vitreous.
What to expect following a vitrectomy
Following this procedure, an antibiotic ointment is applied to the eye to prevent
infection, and an eye patch is placed over the eye to protect it while it heals.
It may take a couple of weeks to notice total vision improvement, though it is
important to speak with your doctor to find out what is to be expected in your
individual circumstances.
Are there any complications associated with vitrectomy?
As with any surgical procedure, there are some risks to consider before undergoing
a vitrectomy. The most common risks include eye damage, infection, bleeding,
high eye pressure, retinal detachment, cataracts, and changes to any pre-existing
refractive error.
If you are not a candidate for a vitrectomy, your eye doctor may recommend a laser
procedure, called a vitreolysis, to treat your eye floaters.
If you suspect you have eye floaters, contact an eye doctor near you, who can
diagnose and treat the condition.
Vitreolysis uses a laser to diminish the size and thickness of eye floaters.
This reduces the retinal shadows and visual disturbances caused by eye floaters in
order to restore clear vision and allow patients to return to their daily activities with
improved functioning and quality of life.
What to expect during a vitreolysis procedure
This in-office procedure is performed under local anesthesia, and typically takes
around 20-30 minutes to perform. Some patients require up to three laser treatments
over the course of four to six weeks in order to gain the full benefits of the procedure.
♦ Vitamin A deficiency (night blindness, xerophthalmia)
Treatment for night blindness will vary depending on the cause.
Treatment may include wearing specific types of glasses or contact lenses, which
can help to support correct vision.
Wearing sunglasses can also protect the eye from ultraviolet light, which can causefurther eye damage. When the cause is a lack of vitamin A, treatment involves
adding more Vitamin A to the diet. Good sources of vitamin A include:
• eggs
• fortified cereals
• fortified milk
• orange and yellow vegetables and fruits
• cod liver oil
• dark, leafy green vegetables
Treatment can occur in two ways: treating symptoms and treating the deficiency.
Treatment of symptoms usually includes the use of artificial tears in the form of
eye drops, increasing the humidity of the environment with humidifiers, and
wearing wraparound glasses when outdoors. Treatment of the deficiency can be
accomplished with a Vitamin A or multivitamin supplement or by eating foods rich
in Vitamin A. Treatment with supplements and/or diet can be successful until the
disease progresses as far as corneal ulceration, at which point only an extreme
surgery can offer a chance of returning sight.
♦ Crossed eyes, wandering eye, squint (strabismus)
Strabismus is usually treated with a combination of eyeglasse, vision therapy, and
surgery, depending on the underlying reason for the misalignment. As with other
binocular vision disorders, the primary goal is comfortable, single, clear, normal
binocular vision at all distances and directions of gaze.
Whereas amblyopia (lazy eye), if minor and detected early, can often be corrected
with use of an eye patch on the dominant eye or vision therapy, the use of eye
patches is unlikely to change the angle of strabismus.
(Otitis, Cerumen plug/ear wax, Deafness, Hearing loss and
hearing impairment, and Ear trauma).
2.1. Key unit competence:
Take appropriate decision on different common medical pathologies of ear.
2.2. Prerequisite (knowledge, skills, attitudes, and values)
To achieve the above competence, the associate nurse student needs the following
prerequisites: human body anatomy and physiology, fundamentals of Nursing andpharmacology.
2.3. Crosscutting Issues to be addressed
2.3.1. Standardization culture
In health care system, the most case of patients is presented with medical pathology
of Otitis, Cerumen plug (earwax), Deafness, Hearing and hearing impairment).
The learners have to learn oral diseases and esophagus in order to handle and to
manage the patients with oral cavity and esophagus related diseases.
2.3.2. Inclusive education
The teacher involves the students in all learning activities concerning the kind of
learner or disabilities for example the slow learner should be reinforced in order to
catch up others, and the teacher takes into consideration respective disability of
learner.
Grouping students, Students with special educational needs are grouped
with others and assigned roles basing on individual student’s abilities.
Providing earning resources earlier before teaching session so that students get
familiar with them. After end lesson assessment, the identified slow learners are
exposed to the remedial learning activities.
Every important point is written and spoken. The written points help students with
hearing impairment and speaking aloud helps students with visual impairment.
Remember to repeat the main points of the lessons.
2.3.3. Gender education
Emphasize to learners that anybody irrespective of their gender can have medical
career mainly medical sciences. Give role models who are successful medical
pathology of oral and esophagus in the area where the learners come from. Make
sure that during classroom teaching and skills lab demonstration both boys and
girls shares and participate equally in practices, arranging and proper hygiene after
classroom and skills lab teaching session.
2.4. Guidance on the introductory activityThis introductory activity helps you to engage learners in the introduction of medical
