UNIT 3 MEDICATIONS USED FOR NON-COMMUNICABLE DISEASES
Key Unit Competence:
At the end of this unit, the learner will be able to provide appropriate medications forhypertension, diabetes mellitus and asthma
Introductory activity 3.0
1) What do you observe on these images?
2) In which medical conditions are the materials in these images used?3) What types of medications are the patients taking?
Learning Activity 3.1
As an associate Nurse Student doing a clinical placement in the hospital,
you received a 66-year-old male patient in consultation room. His vitals were:
the blood pressure was 150/100 mmHg, temperature 36.50C, heart rate 17
movements per minute, SPO2: 99%, and pulse of 65 beats per minute. The
physician concluded that the patient had hypertension.
a) What is hypertension?
b) Identify the classes of hypertension considering their grade.c) Enumerate at least 3 classes of hypertensive drugs.
3.1. Introduction to antihypertensive drugs
CONTENT SUMMARY
The cardiovascular system is a closed system of blood vessels that is responsible
for delivering oxygenated blood to the tissues and removing waste products from
the tissues. Blood pressure is the force exerted by circulating blood against the
walls of the body’s arteries, the major blood vessels in the body.
A Blood pressure is written as two numbers. The first (systolic) number represents
the pressure in blood vessels when the heart contracts or beats. The second
(diastolic) number represents the pressure in the vessels when the heart rests
between beats.
The body uses this responsiveness to regulate blood pressure on a constant basis,
to ensure that there is enough pressure in the system to deliver sufficient blood to
the brain.
Hypertension is defined as a high blood pressure. It is diagnosed if, when it is
measured on two different days, the systolic blood pressure readings on both days
is ≥140 mmHg and/or the diastolic blood pressure readings on both days is ≥90
mmHg.
As blood pressure increases, it is more difficult to control it at the target level through
lifestyle modifications alone, and treatment with antihypertensive drugs becomes
necessary. The occurrence of cardiovascular disease can be prevented by reducingthe blood pressure with antihypertensive drugs.
Table 3.1.1: CLASSIFICATION OF HYPERTENSION
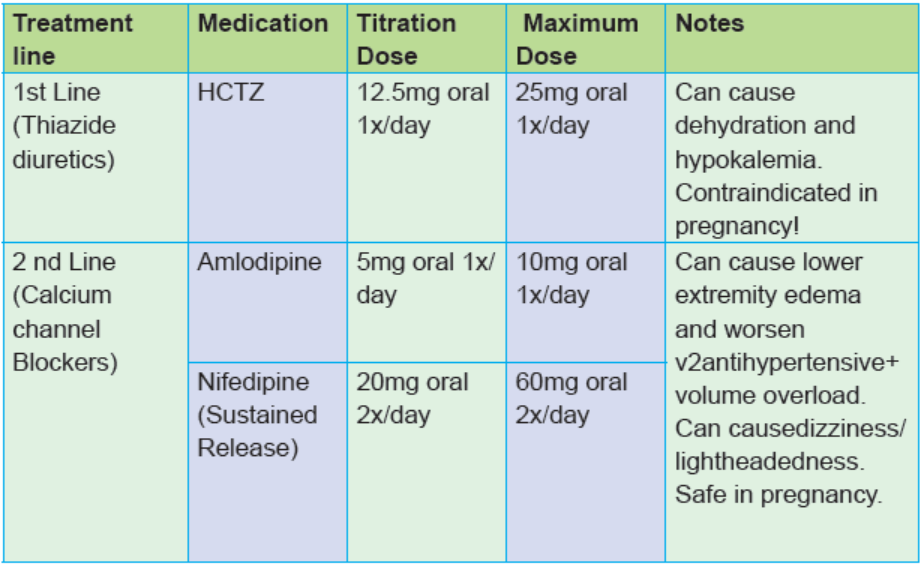
Antihypertensive drugs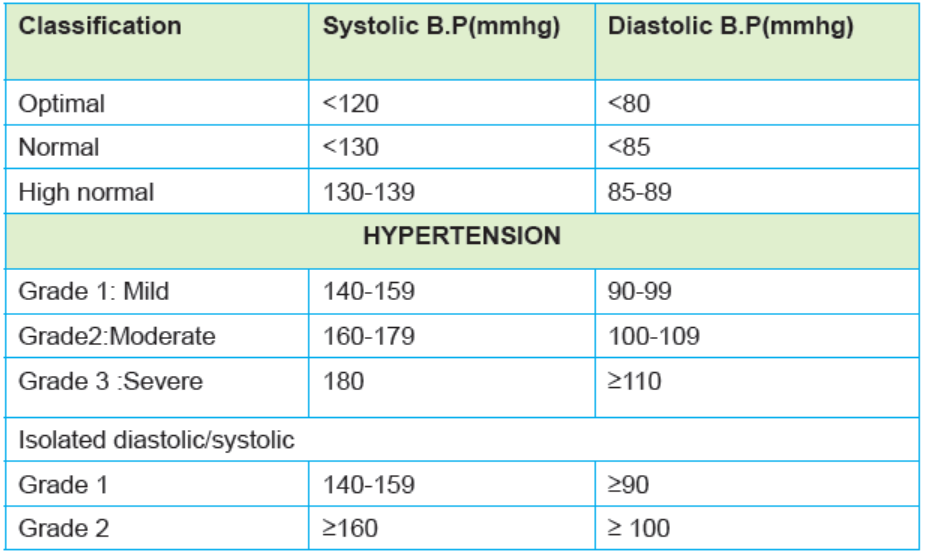
Anti-hypertensive drugs are a class of drugs that are used to treat hypertension.
Antihypertensive therapy seeks to prevent the complications of high blood
pressure, such as stroke and myocardial infarction. Appropriate antihypertensive
drugs should be selected considering compelling indications, contraindications and
conditions that require the careful use of drugs and the presence or absence of
complications. Antihypertensive drugs are administered once a day, in principle, but
as it is more important to control the blood pressure over 24 h splitting the dose into
twice a day is desirable in some situations.
A gradual reduction in blood pressure is desirable in hypertensive patients in general,
but the target control level should be achieved within several weeks in high-risk
patients, such as those with grade III hypertension and multiple risk factors. The
use of two or three drugs in combination is often necessary to achieve the target
of blood pressure control Simplification of the prescription using fixed-combination
drugs is useful for improving adherence and controlling blood pressure.
The major classes of antihypertensive drugs are:
• Diuretics
• Calcium channel blockers
• Angiotensin converting enzyme inhibitors
• Angiotensin II receptor antagonists/blockers,
• Adrenergic blockers, centrally and peripherally acting blockers
(sympatholytics),• Peripheral vasodilators
Self-assessment 3.1
You are working in a health centre and today you receive a client in the consultation
room. When you take the blood pressure you find that the patient has a B.P of
160/100mmHg, then you tell your client that he has hypertension. The latter asks
you what about the grade of his B.P.
1. What would be the response to the client?
2. Which one among the following classes of drugs is an antihypertensive?
a) Diuretics
b) Analgesics
c) Antibioticsd) Antihistamines
3.2.Diuretic drugs
Learning Activity 3.2
As associate Nurse Student in the clinical placement in hospital, you receive a
50-year-old male patient in the consultation room. His vital signs are: the blood
pressure is150/100 mmHg, temperature 36.50C, heart rate 17 movements per
minute, SPO2: 99%, and pulse of 65 beats per minute. The patient complains of
increased urination, and the nurse informs the patient that the drugs the patient
is taking are associated with an increased urination. When the student wants
more explanation, the nurse replies that the drugs fall to the class of diuretics.
Using library textbooks, read and take note while responding to the following
questions.
1) What is diuretic drug?2) Identify the categories of diuretic drugs and give an example for each.
CONTENT SUMMARY
Diuretics are drugs that increase sodium excretion and lower blood volume,
consequently lower the blood pressure. Diuretics are divided into four categories
according to their action: thiazide diuretics, loop diuretics, potassium-sparing
diuretics, and osmotic diuretics. The type of diuretic used is determined by the
condition being treated. They are used to treat mild hypertension and often first
agents used, often used in combination with other agents
Thiazide diuretics
Thiazide agents are the most commonly used type of diuretic, increasing excretion
of water, sodium, chloride, and potassium. Their site of action is proximal part of the
distal convoluted tubule, and all of them have antihypertensive effect.
They are contraindicated in case of diabetes, severe renal failure, impaired liver
function, and a history of gout.Tables 3.2.1. Thiazide diuretics
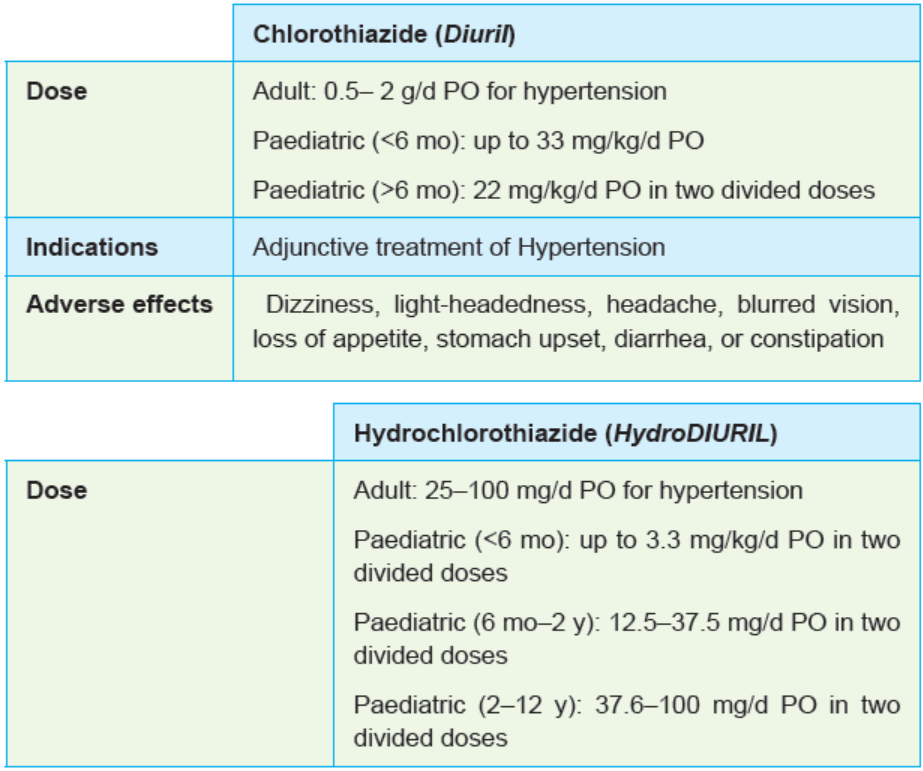
Figure 3.2.1: Thiazide diuretics
Loop diuretics
Loop diuretics are drugs that act on the Loop of Henle not prescribed routinely for
hypertension, but are used when diuresis is required. Loop diuretics are used in
the treatment of oedema associated with impaired renal kidney function or liver
disease. They are also commonly prescribed for the treatment of congestive heart
failure, pulmonary oedema, and ascites caused by malignancy or cirrhosis.
If thiazides are ineffective in the treatment of hypertension, loop diuretics sometimes
are used in combination with other antihypertensive(s).
The most commonly used loop diuretic is furosemide (Lasix). Its usual dose is
20–80 mg/d but up to 600mg /d may be given.
For Intravenous or intramuscular20–40 mg IM or IV given slowly; 40 mg IV over
1–2 min for acute pulmonary oedema, increase to 80 mg after 1 h if response is not
adequate; 40 mg PO b.i.d. for hypertension.
Pediatric: 2 mg/kg/d PO for hypertension, not to exceed 6 mg/kg/d; 1 mg/kg IV or IM
for edema, increased by 1 mg/kg as needed; not to exceed 6 mg/kg Treatment of
acute HF; acute pulmonary edema; hypertension; and edema of HF, renal disease,
or liver disease
Loop diuretics are contraindicated in dehydrated patients, those with anuria and incase of hypersensitivity to the drug or its components.
Figure 3.2.2: Dosage forms of furosemide
Potassium-Sparing Diuretics
The potassium-sparing agents are used in the management of edema associated
with congestive heart failure, hepatic cirrhosis with ascites, the nephrotic syndrome,
and idiopathic edema and used in combination with other drugs in the management
of hypertension. Their site of action is Distal tubule and collecting duct. They are
aldosterone antagonist. Potassium-sparing drugs are contraindicated for patients
with anuria, acute renal insufficiency, impaired renal function, or hyperkalemiaTables 3.2.2: Potassium sparing diuretics:
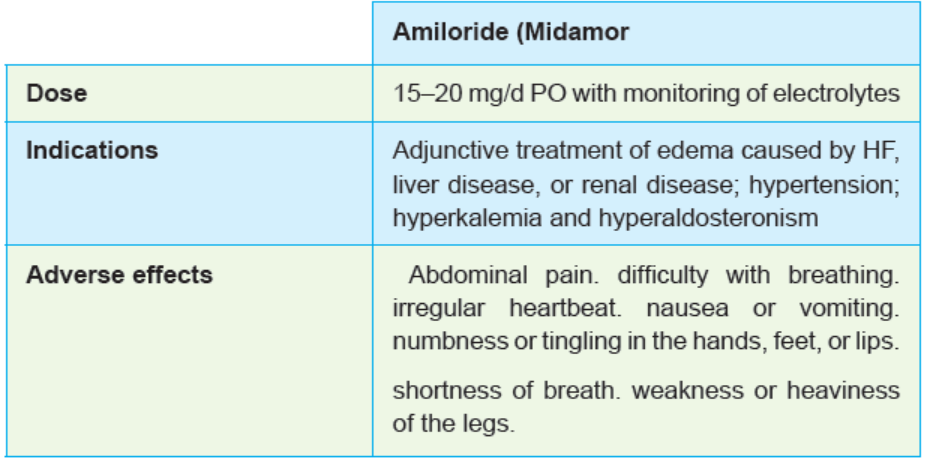
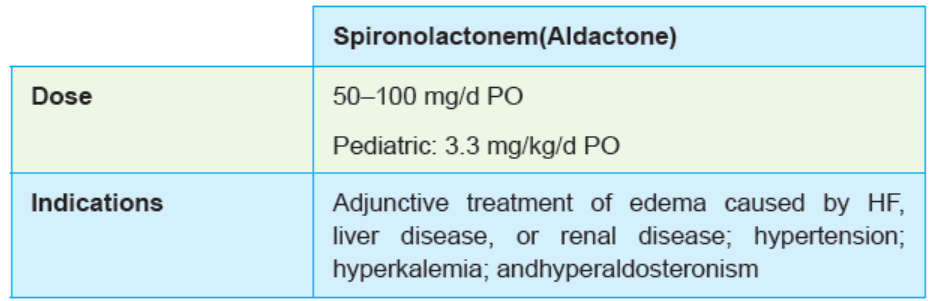
Figure3.2.3: Dosage forms of Thiazide diuretics
NURSING CONSIDERATIONS FOR PATIENT RECEIVING DIURETICS
• Assess for contraindication or cautions including any allergy or hypersensitivity
• Perform a physical assessment to establish baseline data before beginning
therapy, to determine the effectiveness of therapy, and to evaluate for
occurrence of any adverse effects associated with drug therapy.
• Obtain an accurate body weight to provide a baseline to monitor fluid balance.
• Monitor intake and output and assess voiding patterns to evaluate fluid
balance and renal function
• Administer oral drug with food or milk to buffer the drug effect on the stomach
lining if GI upset is a problem.
• Administer intravenous diuretics slowly to prevent severe changes in fluid
and electrolytes.
• Administer oral form early in the day so that increased urination will not
interfere with sleep.
• Monitor the dose carefully and reduce the dose of one or both drugs if givenwith antihypertensive agents; loss of fluid volume can precipitate hypotension.
• Monitor the patient response to the drug (e.g., blood pressure, urinary output,
weight, serum electrolytes, hydration, periodic blood glucose monitoring) to
evaluate the effectiveness of the drug and monitor for adverse effects
• Assess weight daily to evaluate fluid balance.
• Check skin turgor to evaluate for possible fluid volume deficit, and assess
edematous areas for changes, including a decrease in amount or degree of
pitting.
• Provide comfort measures, including skin care and nutrition consultation, to
increase compliance with drug therapy and decrease the severity of adverse
effects; provide safety measures if dizziness and weakness are a problem to
prevent injury.
Note:
Spironolactone can be used in children but with careful monitoring of electrolytes.Amiloride is indicated for use in children.
Self-assessment 3.2
The thiazide diuretics work at the proximal part of the convoluted tubule. TRUE
or FALSE
Which drug among the following is a potassium sparing diuretic?
a) Furosemide
b) Captopril
c) Aldactone
d) Diuril
Which of the following is a side effect of hydrochlorothiazide?
a) High blood pressure
b) Decreased urination
c) Excessive dysphagia
d) Erectile dysfunctionEnumerate the contraindications of Lasix.
3.3. CALCIUM CHANNEL BLOCKERS DRUGS
Learning Activity 3.3
A patient was given medications and he tells you that he wants to know much
about the regimen he was given to control his hypertension. When you read, you
found that among them there is one called nifedipine. Remembering that he had
only covered diuretic drugs among hypertensive drugs, you want to give him full
information about the class where nifedipine belongs.
Using library texbooks and internet, read and take note about the following:
1) In which class does nifedipine belong?
2) What are the other drugs found in this class?3) What is the mechanism of action of the drugs from this class?
CONTENT SUMMARY
Calcium channel blockers are a type of drug that block the entry of calcium into
smooth muscle cells as well as myocytes. They produce arterial vasodilation and
thereby reduce arterial blood pressure. Calcium channel blockers relax and open
up narrowed blood vessels, reduce heart rate and lower blood pressure. They lower
blood pressure by reducing myocardial contractility.Tables 3.3. 1: Commonly used calcium channel blockers:
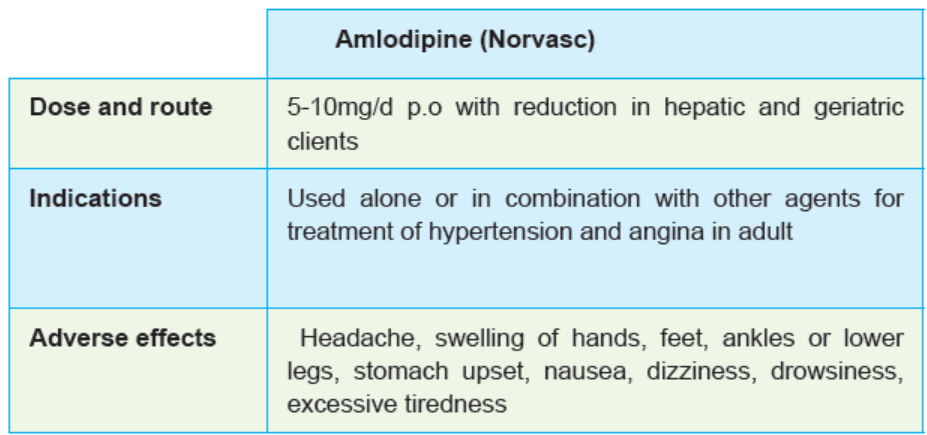
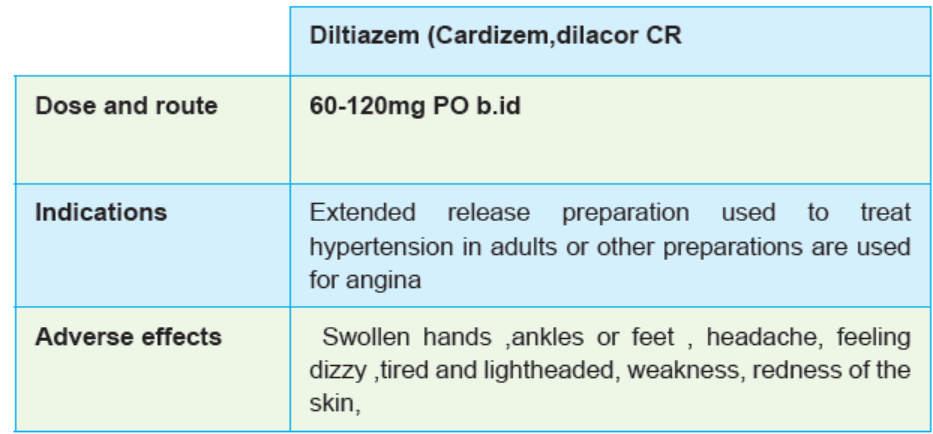
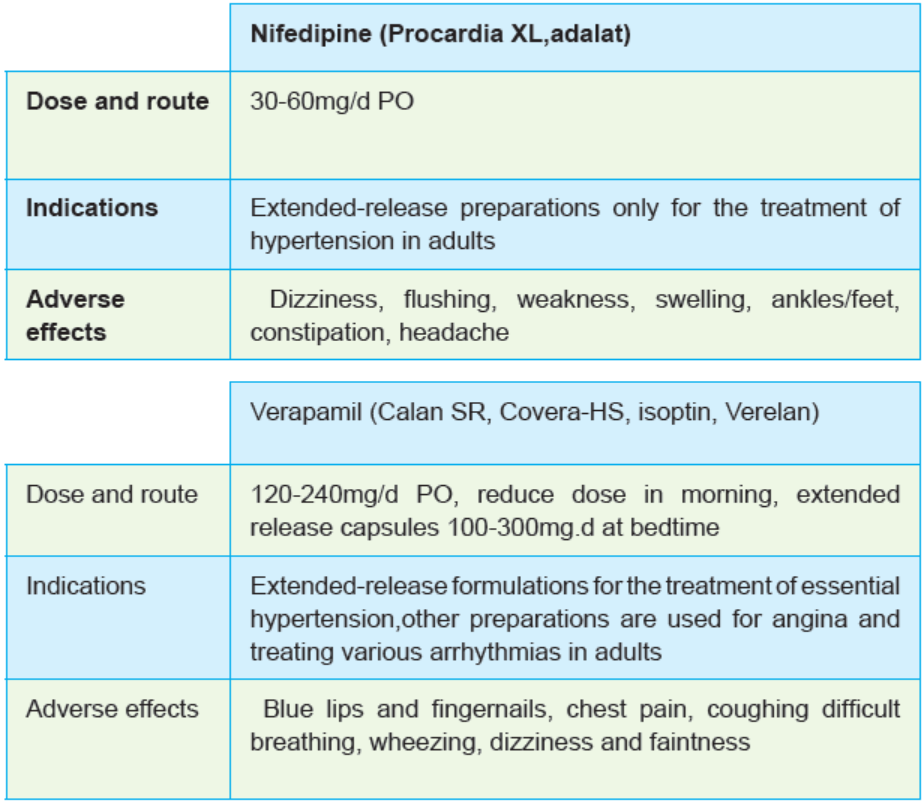

Figure 3.3.1: Forms of calcium channel blockers
Nursing considerations
• Assess for contraindications or cautions : known Allergies, impaired liver or
kidney function, heart block, and current status of pregnancy or lactation.
• Perform a physical assessment to establish baseline status before beginning
therapy and during therapy to determine the effectiveness and evaluate for
any potential adverse effects.
• Inspect skin for color and integrity to identify possible adverse skin reactions
• Assess cardiopulmonary status closely, including pulse rate, blood pressure,
heart rate, and rhythm, to determine the effects of therapy and identify any
adverse effects.
• Monitor vital signs and auscultate lungs to evaluate changes in cardiac output.
• Monitor laboratory test results, including liver and renal function tests, to
determine the need for possible dose adjustment.
• Provide comfort measures to help the patient tolerate drug effects.
• Offer support and encouragement to help the patient deal with the diagnosis
and the drug regimen.
• Provide thorough patient teaching
• Monitor patient response to the drug
• Monitor for adverse effects
• Monitor the effectiveness of comfort measures and compliance with the
regimen.• Evaluate the effectiveness of the teaching plan.
Self-assessment 3.3
1) Which among the following drugs is a calcium channel blocker?
a) Atenolol
b) Aldactone
c) Adalat
d) Furosemide
2) You are assigned to take care of a patient who is on verapamil. Give at
least five elements you must monitor while you are caring for that patient.3) Enumerate the side effects of amlodipine.
3.4. Angiotensin converting enzyme inhibitors and
angiotensin II receptor blockers
Learning Activity 3.4
In a class of pharmacology, the teacher asked her students about antihypertensive
drugs and wanted to know if they know the drugs that interfere with the activity of
angiotensin in human body.
Using library textbooks, read and take note on the following points:
a) Identify 2 categories of drugs that interfere with the activity of angiotensinb) Give one example for each category
Content summary
Angiotensin-converting enzyme (ACE) inhibitors slow the formation of angiotensin II,
which reduces vascular resistance, blood volume, and blood pressure. ACE inhibitors
are becoming the drugs of choice in the first-line treatment of essential hypertension.
ACE inhibitors are contraindicated in patients with hypersensitivity to these agents,
kidney damage, heart failure, hepatic impairment, and diabetes mellitus. ACE inhibitors
are avoided during pregnancy (category D). Safety during lactation or in children is not
established. Although ACE inhibitors as a group are relatively free of side effects or
toxicities in most patients, they do occur, and some can be life-threatening.
The adverse effects of ACE inhibitors may include: dizziness, angioedema, loss of
taste, photosensitivity, severe hypotension, dry cough, hyperkalemia, blood dyscrasias,and renal impairment.
ACE inhibitors should be used cautiously in patients with renal impairment or
hypovolemia, or who are receiving diuretics or undergoing dialysis. These drugs
are used with caution in patients with congestive heart failure, hepatic impairment,and diabetes mellitus.
Table 3.4.1 commonly used ACE inhibitors

Figures 3.4.1: ACE inhibitors
Nursing considerations
• Assess for the cautions or contraindications to use of the drug like known
allergies to these drugs to prevent hypersensitivity reactions; impaired kidney
function, pregnancy or lactation
• Physical assessment to determine the baseline status before beginning
therapy to determine any potential adverse effects.
• Encourage patient to implement lifestyle changes, including weight loss,
smoking cessation, decreased alcohol and salt in the diet, and increased
exercise, to increase the effectiveness of antihypertensive therapy.
• Administer on an empty stomach 1 hour before or 2 hours after meals to
ensure proper absorption of the drug.
• Consult with the prescriber to reduce the dose in patients with renal failure.
• Monitor the patient carefully in any situation that might lead to a drop in fluid
volume (e.g., excessive sweating, vomiting, diarrhea, dehydration) to detect
and treat excessive hypotension that may occur.
• Provide comfort measures to help the patient tolerate drug effects. These
include small, frequent meals; access to bathroom facilities; bowel program
as needed; environmental controls; safety precautions; and appropriate skin
care as needed.
• Provide thorough patient teaching, including the name of the drug, dosage
prescribed, measures to avoid adverse effects, warning signs of problems,
and the need for periodic monitoring and evaluation, to enhance patient
knowledge about drug therapy and to promote compliance.
• Offer support and encouragement to help the patient deal with the diagnosisand the drug regimen.
Angiotensin II receptor antagonists/blockers :
Angiotensin II receptor antagonist drugs work by blocking the binding of angiotensin
II to the angiotensin I receptors. By blocking the receptor site, these agents inhibit
the vasoconstrictor effects of angiotensin II as well as preventing the release of
aldosterone due to angiotensin II from the adrenal glands. This class of drugs
has been one of the most rapidly growing groups of drugs for the treatment of
hypertension
All of the ACE inhibitors are administered orally. Angiotensin II receptor antagonists
are contraindicated in patients with a known hypersensitivity to these agents. These
drugs are also contraindicated in pregnancy (category C, first trimester; category D,
second and third trimesters) and lactation.
Angiotensin II receptor antagonists are used cautiously in patients with concurrent
administration of high-dose diuretics, potassium-sparing diuretics, or potassium
salt substitutes, and in diabetes or lactation.
Angiotensin II receptor antagonists should be used with caution in patients withhepatic or renal impairment, or in elderly patients.
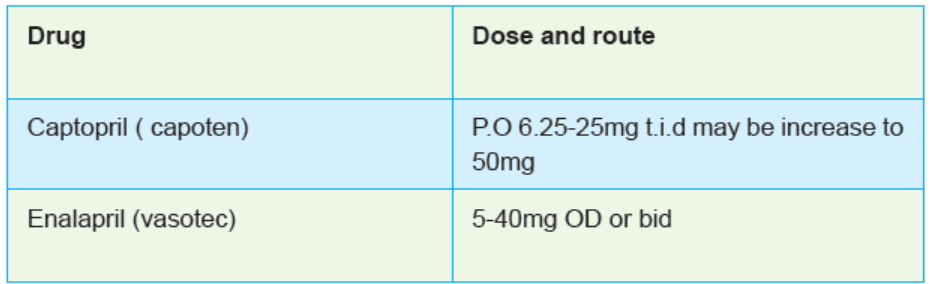
Table.3.5. Commonly used Angiotensin receptor blockers

Figure3.4.2: Angiotensin receptor blockers
Nursing considerations
• Assess for the contraindications and cautions before administration. These
include allergies, impaired kidney or liver functions, pregnancy and lactation,
hypovolemia
• Assess the baseline status before beginning therapy to determine any
potential adverse effects
• Encourage patient to implement lifestyle changes, to increase the effectiveness
of antihypertensive therapy.
• Administer without regard to meals; give with food to decrease GI distress
• Ensure that the female patient is not pregnant before beginning therapy, and
suggest the use of barrier contraceptives while she is taking these drugs
• Monitor the patient carefully in any situation that might lead to a drop in fluid
volume like excessive sweating, vomiting, diarrhea, dehydration, to detect
and treat excessive hypotension that may occur.
• Provide comfort measures to help the patient tolerate drug effects, including
small, frequent meals; access to bathroom facilities; safety precautions if
central nervous system effects occur; environmental controls; appropriate
skin care as needed; and analgesics as needed.
• Provide thorough patient teaching, including the name of the drug, dosage
prescribed, measures to avoid adverse effects, warning signs of problems,
and the need for periodic monitoring and evaluation, to enhance patient
knowledge about drug therapy and to promote compliance.
• Offer support and encouragement to help the patient deal with the diagnosis
and the drug regimen.
• Monitor patient response to the drug (maintenance of blood pressure within
normal limits).
• Monitor for adverse effects
• Evaluate the effectiveness of the teaching plan (patient can name drug,
dosage, adverse effects to watch for, measures to avoid them, and the
importance of continued follow-up).
• Monitor the effectiveness of comfort measures and compliance with theregimen.
Self-assessment 3.4
1) Which of the following drugs is an ACE inhibito?
a) Captopril
b) Lasix
c) Cozaar
d) Diovan
2) Which of the following drugs is an ARB drug?
a) Captopril
b) Lasix
c) Cozaar
d) Enalapril
3) Enumerate at least two contraindications of ARBs.4) What are the side effects of ACE inhibitors?
3.5. Vasodilators and Sympathetic Nervous SystemBlockers
Learning Activity 3.5
You are a Senior six associate nurse student in clinical practicum at the emergency
department and they receive a 39 years old female with history of hypertension.
Her blood pressure was found to be 280/150mmHg. After notifying the physician,
the latter ordered an IV drug which is a vasodilator in attempt to manage this
hypertension. You want to know more about how the vasodilators may help in
controlling the blood pressure, and you are assigned to read more about these
drugs and present in the morning staff meeting the next day. In addition, you
have been requested to read on other drugs that decrease the blood pressure
by working on the sympathetic nervous system.
1) How do vasodilators work to reduce the blood pressure? Give at least two
examples of vasodilator drugs.
2) Give at least two classes of drugs that work on the sympathetic nervous
system to reduce the blood pressure.Guidance: Use library textbooks and internet.
CONTENT SUMMARY
Vasodilators are used to relax or dilate vessels throughout the body. They block
the movement of calcium into the smooth muscle of the blood vessels to cause
relaxation of the smooth muscle, and dilation of the resistance vessels.
Some work on either veins or arteries; others work on both. Vasodilators are
prescribed as second-line agents to initial therapy in patients taking diuretics, betablockers,
ACE inhibitors, calcium-channel blockers, alpha adrenergic blocker, or
alpha/betaadrenergic blockers.
Vasodilator agents are reducers of hypertension. A peripheral vasodilator is
frequently used in the treatment of moderate to severe hypertension.
Common adverse effects of vasodilator drugs include headache, dizziness,
tachycardia, palpitations, anxiety, nausea, vomiting, disorientation, depression,
edema, impotence, and allergic reactions.
They are contraindicated in patients with coronary artery disease, mitral valvular
rheumatic heart disease, atriovenous shunt, and myocardial infarction. Safe use ofvasodilators during pregnancy (category C) or lactation is not established.
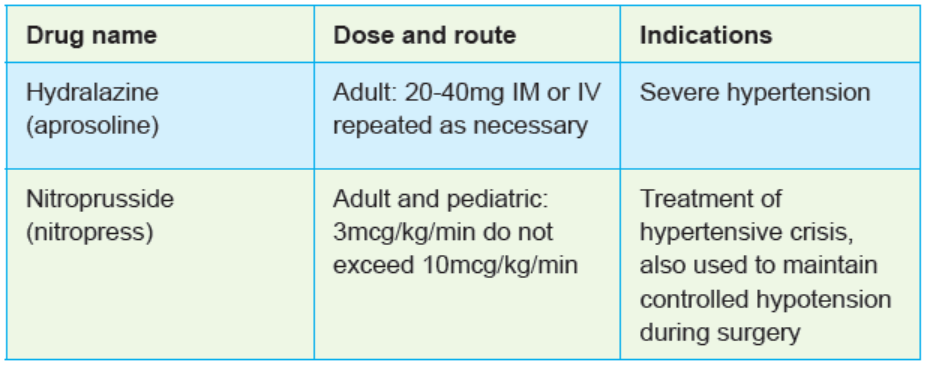
Table 3. 5. 1Commonly used vasodilators
SYMPATHETIC NERVOUS SYSTEM BLOCKERS
Drugs that block the effects of the sympathetic nervous system are useful in
blocking many of the compensatory effects of the sympathetic nervous system.
They include beta-blockers, alpha blockers, alpha and beta blockers and alphaadrenergicblockers.
Beta-blockers act by blocking vasoconstriction, decrease heart rate, decrease
cardiac muscle contraction, and tend to increase blood flow to the kidneys, leading
to a decrease in the release of renin. These drugs have many adverse effects and
are not recommended for all people. They are often used as monotherapy in step
2 treatment, and in some patients, they control blood pressure adequately. The
commonly used beta blockers are acebutolol, atenolol (Tenormin) and propranolol.
Their common contraindications are diabetes mellitus, chronic obstructivepulmonary disease (COPD) and asthma.
Table 3. 5.2: Commonly used beta blockers
Self-assessment 3.5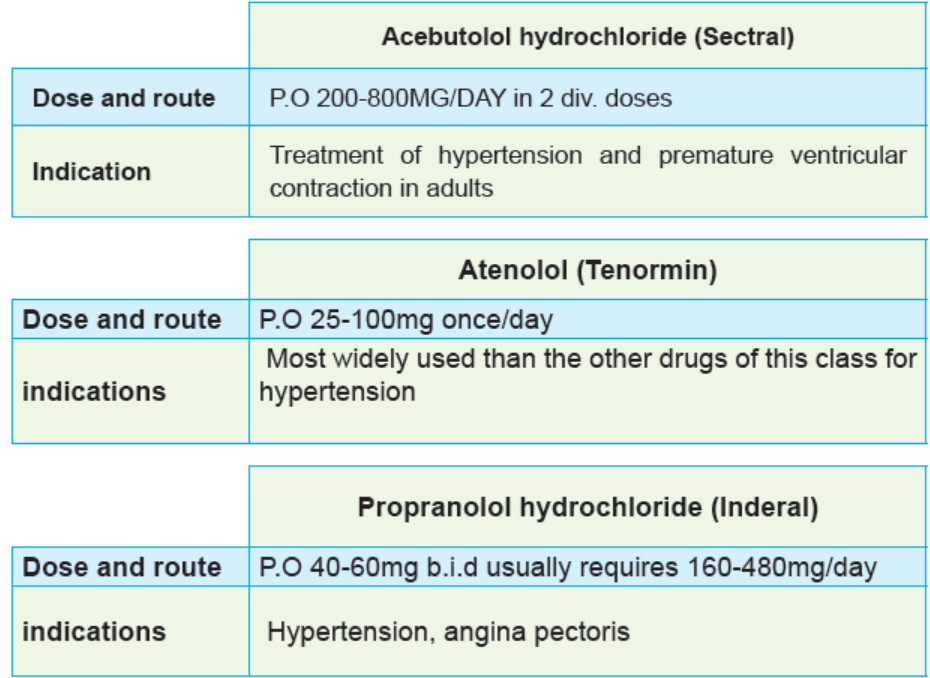
1) Among the antihypertensive drugs, which one is a vasodilator used in
case of hypertensive crisis?
a) Atenolol
b) Acebutelol
c) Carvedilol
d) Nitroprusside
2) Which of the following classes of antihypertensive drugs acts on
sympathetic nervous system?
a) Diuretics
b) Beta-blockers
c) Calcium channel blockersd) ACE inhibitors
3.6. Treatment guidelines of hypertension
Learning Activity 3.6
A 40-year-old female patient consults a health facility where you are placed
in the clinical placement. It is a known case of prehypertension who was on
lifestyle measures and on her arrival, her blood pressure is 150/90 mmHg. She
is then screened for diabetes, and the glycaemia shows that the patient meets
the criteria to be diagnosed as a diabetic patient. The fellow associate nurse
student in the clinical placement wants you to advice on the class of first line
antihypertensive medications.
1) What class of antihypertensive medications can you advise to prescribe
for this patient according the national guidelines?
2) Apart from glycemia, what other laboratory investigations may be
requested before starting the antihypertensive drugs according to thenational guidelines?
CONTENT SAMMURY
The national guideline on hypertension focus on diagnosis of hypertension,
determining the cause of increased blood pressure and to establish the follow up
visit.
A diagnosis of hypertension is only made when: Systolic blood pressure>=140
mmHg OR Diastolic blood pressure >= 90mmHg. Blood pressure needs to be
elevated on two separate visits.
There is a need to take history and do investigation and decide whether the patient
has essential or secondary hypertension. This is applicable in children and adults.
Again it is important to assess the grade of hypertension as seen in the first lesson
of this unit. Finally, establish or confirm that the patient has hypertension, identify or
confirm the stage of hypertension, assess medication compliance and hypertension
control and discuss about Life style modification.
The management of hypertension will depend on the stage and whether the patientis pregnant or is a child.
Stage I: 140/90mmhg-159/99mmHg
Stage II: 160mmhg-179/109mmHg,
Stage III: 180/110 mmHg
Before starting antihypertensive drugs, a complete history, physical examination
as well as some laboratory tests and investigation like HIV test must be taken
because HIV positive patients are managed with precaution and some regimen may
change. Again, it is very important to test the electrolytes to rule out hypokalemia
and hyperkalemia, as well as taking creatinine to rule out renal failure. In females,
a pregnancy test must be taken before initiating antihypertensive drugs because
some drugs like Ace-Inhibitors, Atenolol, and HCTZ should not be used in pregnantwomen.
Treatment of hypertensive Emergency
BP > 180/110 with evidence to damage to brain, eye, heart, kidneys or fetus
1) Give medication every 30 minutes
2) Call physician and admit to hospital3) Check blood pressure every thirty minutes until transfer
Table 3.6.1: Treatment of hypertensive emergency
Treatment of essential hypertension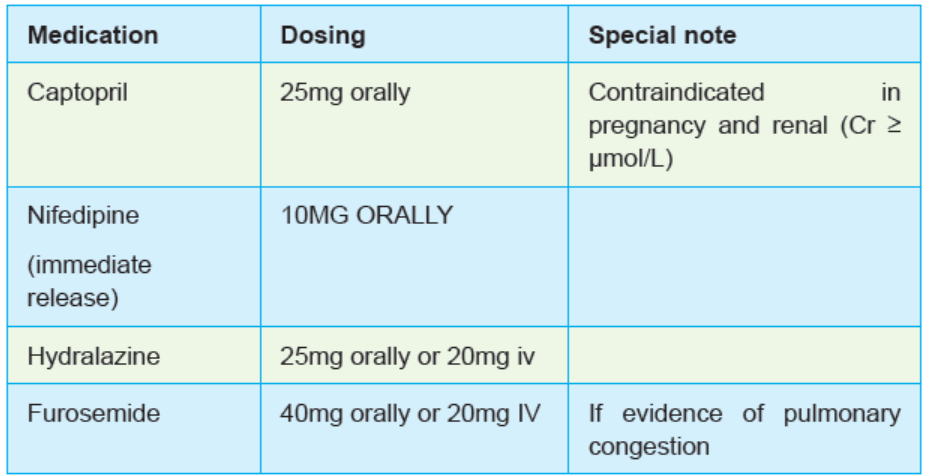
STAGE 1 (BP 140/90 – 159/99) WITHOUT RISK FACTORS
1) Encourage lifestyle modifications
2) If unable to achieve a blood pressure < 140/90 in 12 months, start one
antihypertensive3) Monitor every 3 months
STAGE 1 (BP 140/90 – 159/99) WITH RISK FACTORS:
1) Encourage lifestyle modifications
2) If unable to achieve a blood pressure <140/90 in 3 months, start one
antihypertensive
3) Monitor every 3 months
STAGE 2 (BP 160/100 – 179/109):
1) Start two hypertensive medications
2) Encourage lifestyle modifications
3) Follow-up in 1 month
4) Lifestyle Modifications:
STAGE 3 (BP > 180/110) without danger signs:
1) Start two anti-hypertensive drugs immediately.
2) Encourage lifestyle modifications.
3) Follow-up in 2 weeksTable 3.6.2: Treatment of essential hypertension
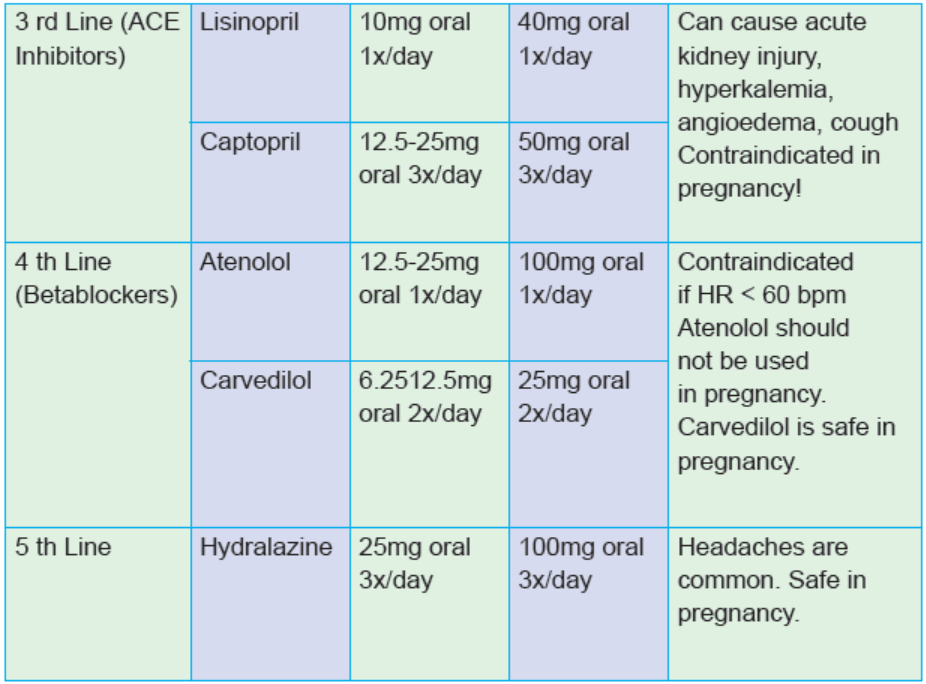
Treatment of Hypertension with complications
Diabetes: ACE-Inhibitors are first line.
Proteinuria: ACE-Inhibitors are first line.
Cardiomyopathy: Ace-Inhibitors, Beta-blockers, Spironolactone are preferred.
Chronic Renal Failure:
1st Line: Furosemide, Amlodipine or Nifedipine
2nd Line: Beta-blockers and hydralazineTable 3.6.3: Treatment of Hypertension with complications
Self-assessment 3.6
Read carefully the scenario below:
1) Two patients A and B presented to the outpatient department of the
hospital where you work as an associate nurse. The first has a high B.P
of 144/95mmHg and the second one has a BP of 198/150mmHg. Both
of them have no other risk factors.
i. All of the following are the options for patient A management, EXCEPT:
a) Encourage lifestyle modifications
b) If BP >140/90 in 12 months, start one antihypertensive
c) Monitor every 3 months
d) Administer hydralazine
ii. All of the following are the options for patient B management:
a) Encourage lifestyle modifications
b) If BP >140/90 in 12 months, start one antihypertensive
c) Administer hydralazine IV if available
d) Monitor every 3 months
2) Which of the following antihypertensive drugs is classified in the third line
of anti-hypertensive drugs based on national guidelines?
a) Captopril
b) Atenolol
c) Amlodipined) Hydralazine
3.7. Oral antidiabetic medications
Learning Activity 3.7
The patient has been followed up after episode of hyperglycemia but the advice
given on a diet and exercise do not impact on his blood glucose level. Today, the
health care providers would like to prescribe oral antidiabetic drugs.
Using library textbooks and internet respond to the following questions:
1) When are oral anti diabetic agents indicated?2) What are the contraindication of Metformin anti diabetic drug
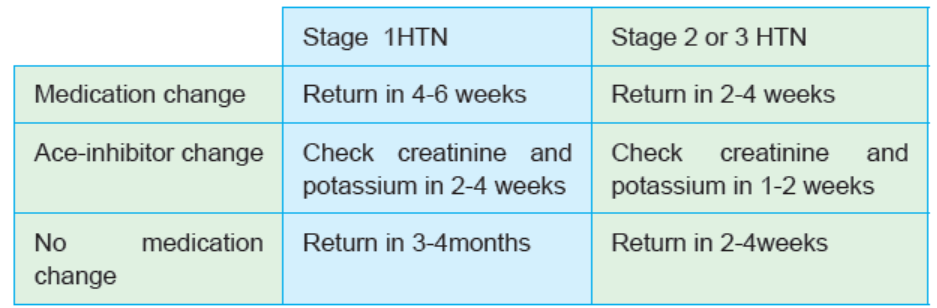
CONTENT SUMMARY
Diabetes Mellitus (DM), is a group of metabolic diseases that occur with increased
levels of glucose (hyperglycemia) in the blood. It is non-communicable disease
resulting from defects in insulin secretion, insulin action or both. It is associated with
acute complications
Insulin is a hormone that allows the body to efficiently use glucose as fuel. Diabetes
has major classifications that include type 1 diabetes, type 2 diabetes, gestationaldiabetes, and diabetes mellitus associated with other conditions.
Table 3.7.1: Classification of diabetes based on etiology.
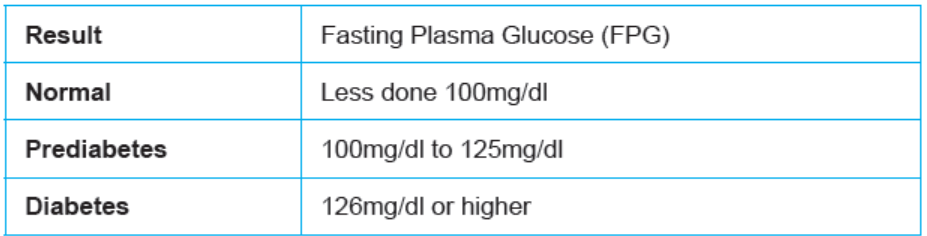
Table 3.7.2: Diagnosis of diabetes mellitus based on glycaemia
To convert mmol/l into mg/dl, multiply mmol/l by 18
Diabetes is a serious chronic disease that has no cure. However, it can be controlled
but its complications are inevitable. Their prevention is the cornerstone of therapy
and include non-pharmacological management measures like nutrition, exercise,
monitoring and education (what foods to eat, how much and how often to eat,
how to exercise and its precautions) and pharmacological management (how and
when to take medications) including oral antidiabetic medications and parenteral
antidiabetic medications. The goal is to keep the blood sugar level as close to
normal as possible to delay or prevent complications. Generally, the goal is to keep
daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 to 7.2
mmol/L) and after-meal numbers no higher than 180 mg/dL (10 mmol/L) two hoursafter eating.
ORAL ANTIDIABETIC MEDICATIONS
Oral hypoglycaemic agents stimulate the pancreas to secrete more insulin and
increase the sensitivity of insulin receptors in target tissues. Oral hypoglycaemic
agents are indicated for the treatment of uncomplicated type II diabetes in patients
whose diabetes cannot be controlled by diet or exercise only.
They are grouped in five classes: Sulfonylureas, alphaglucosidase inhibitors,
biguanides, meglitinides, and thiazolidinediones. Their common adverse effects
are nausea, vomiting, headache, blurred vision, sedation, confusion, anxiety,
nightmares, and tachycardia.
Oral hypoglycemic agents are contraindicated in patients who are receiving
sulfonamide or thiazide-type diuretics, who are hypersensitive to the agents, and
who have acidosis, severe burns, or severe diarrhea. These agents should be used
cautiously in patients with high fevers, severe infections, hyperthyroidism, or kidneyfunction impairment.
Commonly used oral hypoglycemic agents:
1) METFORMIN
Metformin hydrochloride (glucophage®):
Metformin belongs to the class of biguanides. It lowers blood glucose by helping the
body to make better use of insulin. It is an adjunct to diet to lower blood glucose in
type 2 diabetics.
Indications: Type 2 diabetes mellitus, prediabetes, Type 1 diabetes mellitus
(T1DM) Metformin is sometimes used in T1DM to limit insulin dose requirement.
Contraindications: Hypersensitivity, chronic heart failure, metabolic acidosis with
or without coma, diabetic ketoacidosis (DKA), severe renal disease, abnormal
creatinine clearance resulting from shock, septicaemia, or myocardial infarction
and lactation
The commonly reported side effects of metformin include: lactic acidosis, diarrhea,
nausea, nausea and vomiting, vomiting, and flatulence. Other side effects
include asthenia, and decreased vitamin b12 serum concentrate.
Dose: Adults: 500–850 mg/d PO in divided doses; reduce dose in geriatric and
renal-impaired patients; maximum dose: 2,550 mg/d.
Children: 10–16 y: 500 mg/d PO with a maximum dose of 2,000 mg/d; do not useextended release form.

Figure 3.7.1: Forms of metformin
2) GLIBENCLAMIDE
Glibenclamide (GBC) or glyburide is an oral hypoglycemic drug that stimulates
the pancreatic beta cells to secrete insulin and is used to treat type 2 diabetes,
including diabetes during pregnancy.
It belongs to a group of medicines called sulfonylureas. Glibenclamide lowers
blood glucose by increasing the amount of insulin produced by your pancreas. It is
recommended that it be taken together with diet and exercise. It may be used with
other antidiabetic medication and t is not recommended for use by itself in type 1diabetes.
Dose: Initially 2.5-5mg daily, adjusted in increments of 2.5mg at weekly intervals,based on patient’s response. Maximum: 20mg daily.
Dose 10mg may be given in 2 divided doses
In elderly >70 years contraindicated.

Forms of Glibenclamide
3) VILDAGLIP TIN
Vildagliptin (Galvus) is an oral anti-hyperglycaemic agent of the dipeptidylpeptidase-4 inhibitor class of drugs.
Dose: 50 mg once or twice daily. The maximum daily dose of Galvus is 100 mg. For
monotherapy, and for combination with metformin, with a TZD or with insulin (withor without metformin), the recommended dose of Galvus is 50 mg or 100 mg daily.

Figure 3.7.2: Forms of vildagliptin
Self-assessment 3.7
1) Among the following drugs, which one is an oral antidiabetic drug?
a) Insulin
b) Lasix
c) Daonil
d) Diovan
2) 2. For a patient who is taking oral antidiabetic agents, which complain a
nurse will expect from them?
a) Hypertension
b) Nightmares
c) Fever
d) Chills
3) 3. Which of the following drug is a sulfonylurea?
a) Vildagliptin
b) Glucophage
c) Glibenclamided) All of them
3.8. Parenteral antidiabetic drugs
Learning Activity 3.8
In clinical session students were shown different oral antidiabetic medications
used to treat diabetic patients. After a long discussion, students wanted to know if
apart from oral medications, there are no other forms of antidiabetic medications
available. A senior nurse replied that there are injectable antidiabetic medications
that were kept in the fridge in another room and requested them to take this as
an assignment that they will present the following week. You are among the
class members, respond the following questions to prepare that presentation.
1) Which antidiabetic drug is administered parenterally?
2) When is that drug indicated?3) What are different types of that drug?
CONTENT SUMMARY
Insulin is the only parenteral antidiabetic available for use in treatment of diabetes.
Normally, insulin is used for the treatment of type I diabetics if the pancreas does
not produce enough insulin but some patients with type 2 diabetes already on
maximum oral therapy may also require insulin injections or in case of DKA orglucose >400mg/dL, pregnancy, renal (>150mmol/L) and Children < 18 years old.
Insulin preparations are available from three different species, including cows, pigs,
and humans. Human insulin now is produced by chemical conversion from porcine
insulin and by Escherichia coli, into which the human genes for insulin have been
inserted. The recombinant product has the same physiological properties as insulinfrom beef or pork but is much less likely to cause allergic reactions.
Adverse Effects
The most dangerous adverse effect of insulin therapy is hypoglycemia. The other
adverse effects include tachycardia, sweating, drowsiness, and confusion. If severe
hypoglycemia is not immediately treated with glucose, convulsions, coma, anddeath may occur.
Indications for insulin: Insulin is used to control hyperglycemia in the diabetic
patient, and for the emergency treatment of acute ketoacidosis. It may beadministered intravenously or subcutaneously.
Contraindications and Precautions
Insulin is contraindicated in patients with hypersensitivity to insulin animal protein.
It is also contraindicated during episodes of hypoglycemia. Insulin should be used
with caution in patients with insulin-resistant hyperthyroidism or hypothyroidism,
during lactation, in older adults, during pregnancy (category B), and in those withrenal or hepatic impairment.
Drug Interactions
Alcohol, anabolic steroids, MAOIs, and salicylates may potentiate hypoglycemic
effects. Dextrothyroxine, corticosteroids, and epinephrine may antagonize
hypoglycemic effects. Herbals such as garlic and ginseng may potentiate the
hypoglycemic effects of insulin.
• Type 1 or malnutrition type diabetes
• DKA or glucose >400mg/dL
• Type 2 DM patients already on maximum oral therapy
• Pregnancy
• Renal (>150mmol/L)• Children < 18 years old
Types of insulin
Insulins are classified based on their time of pharmacological action as rapid actinginsulin, short-acting, intermediate-acting, and long-acting and mixed.
1. Rapid-acting insulin: Rapid-acting insulin starts working somewhere between
2.5 to 20 minutes after injection. Its action is at its greatest between one and 3 hours
after injection and can last up to 5 hours. This type of insulin acts more quickly after
a meal, similar to the body’s natural insulin, reducing the risk of a low blood glucose
(blood glucose below 4 mmol/L). When use this type of insulin, patient must eat
immediately or soon after injection. Eg are: insulin glulisine (Apidra), insulin lispro(Humalog) and insulin aspart (Novolog).
2. Short-acting insulin(regular) include:. Short-acting insulin takes longer to start
working than the rapid-acting insulins. Short-acting insulin begins to lower blood
glucose levels within 30 minutes, so you need to have your injection 30 minutes
before eating. It has its maximum effect 2 to 5 hours after injection and lasts for 6 to8 hours. Examples: Actrapid®, Humulin R and Novolin R
3. Intermediate-acting insulins include: Intermediate-acting and long-acting
insulins are often termed background or basal insulins. The intermediate-acting
insulins are cloudy in nature and need to be mixed well. These insulins begin to
work about 60 to 90 minutes after injection, peak between 4 to 12 hours and last
for between 16 to 24 hours. Example: Humulin® NPH (a human isophane insulin),insulin NPH (Novolin N, Humulin N), Protaphane® (a human isophane insulin).
4. Mixed insulin: Mixed insulin contains a pre-mixed combination of either very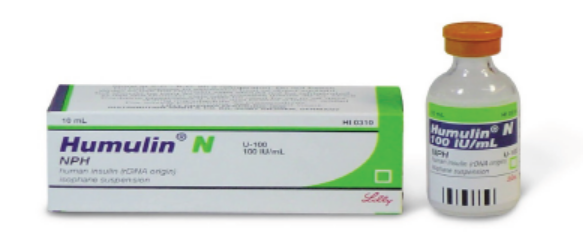
rapid-acting or short-acting insulin, together with intermediate-acting insulin
The mixed insulins currently available are:
– Rapid-acting and intermediate-acting insulin: NovoMix® 30 (30%
rapid, 70% intermediate Protaphane), Humalog® Mix 25 (25% rapid,
75% intermediate Humulin NPH), Humalog®, Mix 50 (50% rapid, 50%
intermediate Humulin NPH)
– Rapid-acting and long-acting inslulin ;Ryzodeg 70:30 (70% long acting
Degludec, 30% rapid Aspart)
– Short-acting and intermediate-acting insulin: Mixtard® 30/70 (30%
short, 70% intermediate Protaphane), Mixtard® 50/50 (50% short, 50%
intermediate Protaphane), Humulin® 30/70 (30% short, 70% intermediate
Humulin NP
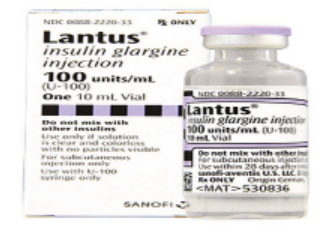
5. Long-acting insulin: Lantus® (glargine insulin) – slow, steady release of insulin
with no apparent peak action. One injection can last up to 24 hours. It is usually
injected once a day but can be taken twice daily, (glargine insulin) – this insulin has
a strength of 300 units per ml so is 3 times the concentration of another insulin. It
is given once a day and lasts for at least 24 hours. It should not be confused withregular Lantus which has a strength of 100 units per ml.
Insulin delivery devices
Different insulin devices are available. Many people who take insulin use a syringe,but there are other options as well like insulin pens and insulin pumps.
Insulin syringes: Syringes are manufactured in 30-unit (0.3 ml), 50-unit (0.5 ml)
and 100-unit (1.0 ml) measures. The size of the syringe needed will depend on the
insulin dose. The needles on the syringes are available in lengths ranging from 6 to
8 mm. For example, it is easier to measure a 10-unit dose in a 30-unit syringe and55 units in a 100 unit syringe.
Insulin pens: Insulin companies have designed insulin pens (disposable or
reusable) to be used with their own brand of insulin.
Disposable insulin pens already have the insulin cartridge in the pen. They are
discarded when they are empty, when they have been out of the fridge for onemonth, or when the use-by date is reached.
Reusable insulin pens require insertion of a 3 ml insulin catridge. The insulin
strength per ml is 100 units. When finished, a new cartridge or penfill is inserted.
Reusable insulin pens are designed by the insulin companies to fit their particularbrand of insulin cartridge/penfill.
Pen cartridges also need to be discarded one month after commencing if insulin stillremains in the cartridge.
They are available in different lengths, ranging from 4 to 12.7 mm. However,
research recommends that size 4 to 5 mm pen needles are used. The thickness
of the needle (gauge) also varies – the higher the gauge, the finer the needle. It is
important that a new pen needle is used with each injection. Your diabetes nurse
educator can advise you on the appropriate needle length and show you correctinjection technique
Insulin pumps: An insulin pump is a small programmable device that holds a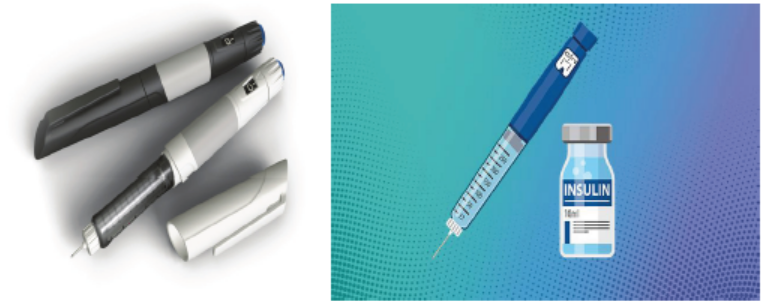
reservoir of insulin and is worn outside the body. The insulin pump is programmed
to deliver insulin into the fatty tissue of the body (usually the abdomen) through thin
plastic tubing known as an infusion set or giving set. Only rapid-acting insulin is
used in the pump.
The infusion set has a fine needle or flexible cannula that is inserted just below the
skin. This is changed every 2 to 3 days.
The pump is pre-programmed by the user and their health professional to
automatically deliver small continual amounts of insulin to keep blood glucose
levels stable between meals. Individuals can instruct the pump to deliver a burst
of insulin each time food is eaten, similar to the way the pancreas does in peoplewithout diabetes.
Insulin injection sites
Insulin is injected through the skin into the fatty tissue known as the subcutaneous
layer. It shouldn’t go into muscle or directly into the blood, as this changes how
quickly the insulin is absorbed and works. Absorption of insulin varies dependingon where in the body it is injected.
• The abdomen absorbs insulin the fastest and is used by most people.
• The upper arms, buttocks and thighs have a slower absorption rate and can
also be used.
• The proper technics is to Pinch the skin up and use a 90-degree angle. The
best angle for a thin person is 90 degrees with the skin pinched up.
• The area is not massaged and it is not necessary to warm it.
• Injections are made into the subcutaneous tissue. Most individuals are able tolightly grasp a fold of skin, release the pinch, then inject at a 90° angle.
Factors affecting insulin absorption
Variation in insulin absorption can cause changes in blood glucose levels. Insulin
absorption is increased by:
• Injecting into an exercised area such as the thighs or arms, and the abdomen
is used for a more consistent absorption
• High temperatures due to a hot shower, bath, hot water bottle, spa or sauna
• Massaging the area around the injection site
• Injecting into muscle – this causes the insulin to be absorbed more quickly
and could cause blood glucose levels to drop too low.
Insulin absorption can be delayed by:
• Over-use of the same injection site, which causes the area under the skin to
become lumpy or scarred (known as lipohypertrophy)
• Insulin that is cold (for example, if insulin is injected immediately after taking
it from the fridge)• Cigarette smoking.
Insulin storage
Insulin needs to be stored correctly. This includes:
• Store unopened insulin on its side in a fridge.
• Keep the fridge temperature between 2 and 8 °C.
• Make sure that insulin does not freeze.
• Once opened, keep it at room temperature (less than 25 °C) for not more than
one month and then dispose of it safely.
• Avoid keeping insulin in direct sunlight.
Extreme (hot or cold) temperatures can damage insulin so it doesn’t work properly.
It must not be left where temperatures are over 30 °C. In summer your car can getthis hot (above 30 °C) so don’t leave your insulin there.
Insulin safety
All insulin should be checked for expiration date and clearness. Insulin should not
be given if it appears cloudy, Vials should not be shaken but rotated in between
the hands to mix contents, the vial in use can be stored at room temperature. Vials
should not be put in glove. compartments, suitcases, or trunks. If regular insulin
is to be mixed with NPH or Lente insulin, the regular insulin should be drawn into
the syringe first. Record of blood glucose levels and insulin doses it is important
and keeping a record of blood glucose levels helps the patient and your healthcare
professional to know when the insulin dosage needs adjustment.
When the patient is using insulin, the nurse has responsibility to educate and
support the patient about the following:
• The type and action of your insulin
• How, where and when to inject insulin
• How to rotate injection sites
• Where to get your insulin and how to store it safely
• How to manage low blood glucose
• How to keep a record of your blood glucose levels and insulin dose
Other medication used in case of diabetes
Additional medications also may be prescribed for people with diabetes milletu ,
such as:
High blood pressure medications: Angiotensin-converting enzyme (ACE)
inhibitors or angiotensin II receptor blockers (ARBs) for patients with diabetes who
have blood pressures above 140/90 millimetres of mercury (mm Hg).
Aspirin: junior or regular aspirin daily to protect the heart when there is an increased
risk for a cardiovascular event, but if there is no the potential risk of bleeding.
Cholesterol-lowering drugs as patients with diabetes have a higher risk of increasein cholesterol and elevated risk of heart disease.
Self-assessment 3.8
1) When is insulin indicated?
a) For treating hypoglycemia
b) Patient with diabetes ketoacidosis
c) Patient with high blood pressure
d) For a patient with high cholesterol
2) What is the most common route of administration of insulin?
a) Oral
b) Intra-rectal
c) Subcutaneous
d) Intradermal
3) Nurse A. is given a report on a patient who is going to start insulin therapy.
She is wondering the appropriate site where she will inject the prescribed
insulin. The correct answer will be:
a) On abdomen subcutaneously
b) Abdomen intramuscularly
c) On the back intramuscularlyd) On the back subcutaneously
3.9. Nursing considerations during diabetes mellitusdrug therapy
Learning Activity 3.9
1) Patient X, a 18-year-old female, a hard working chef accountant who
stays long time in the office presents to the health centre with complaints
of polydipsia, polyphagia, and fatigue for the past month, while she takes
antidiabetic medication regularly. The patient reveals that she has had
diabetes for the past 2 years, and likes to take often carbohydrates on
every serving of food. Which of the following nursing considerations
should the associate student nurse in the clinical placement take intoaccount while assessing this patient?
a) Do not focus on the nutritional intake as it usually has no effect on the
anticipated response to insulin therapy.
b) Monitor the patient’s food intake and ensure that the patient eats when
using insulin to ensure therapeutic effect and avoid hypoglycemia.
c) Monitor the patient’s food intake and ensure that the patient avoids any
kind of eating when using insulin as it can limit its effectiveness.
d) Focus on the nutritional intake and encourage the patient to keep taking
a lot of carbohydrates to increase the effectiveness of insulin.
2) Which the following discharge notes should the nurse include in the client
teaching for a type 1 patient who uses insulin?
a) Self-inject insulin at home by the subcutaneous route only, and rotate
injection sites regularly
b) Self-inject insulin at home by the intramuscular route only, and rotate
injection sites regularly
c) Self-inject insulin at home by the intramuscular route only, and never
rotate injection sites
d) Self-inject insulin at home by the subcutaneous route only, and neverrotate injection sites
CONTENT SUMMARY
During care of patient with diabetes under medication, nurses should provide
accurate and up-to-date information about the patient’s condition so that the healthcare
team can come up with appropriate interventions and management.A nurse will assess the following:
Assess for contraindications or cautions: any known allergy to any insulin and
current status of pregnancy or lactation so that appropriate monitoring and dose
adjustments can be completed, including possible need to use animal-source
insulin. Perform a physical assessment to establish a baseline before beginning
therapy, and during therapy to evaluate the effectiveness of therapy and for any
potential adverse effects. Assess for presence of any skin lesions; orientation and
reflexes; baseline pulse and blood pressure; respiration or adventitious breath
sounds, which could indicate response to high or low glucose levels and potentialrisk factors in giving insulin.
Assess body systems for changes suggesting possible complications associatedwith poor blood glucose control. Investigate nutritional intake, noting any problems
with intake and adherence to prescribed diet that could alter the anticipatedresponse to insulin therapy.
Assess activity level, including amount and degree of exercise, which could alteranticipated response to insulin therapy.
Inspect skin areas that will be used for injection of insulin; note any areas that
are bruised, thickened, or scarred, which could interfere with insulin absorption
and alter anticipated response to insulin therapy. Obtain blood glucose levels as
ordered to monitor response to insulin and need to adjust dose as needed. Monitorthe results of laboratory tests, including urinalysis, for evidence of glycosuria.
The nurse will also:
Ensure that the patient is following a dietary and exercise regimen and using good
hygiene practices to improve the effectiveness of the insulin and decrease adverse
effects of the disease. Gently rotate the vial containing the agent and avoid vigorous
shaking to ensure uniform suspension of insulin.
Select a site that is free of bruising and scarring to ensure good absorption of the
insulin.
Give maintenance doses by the subcutaneous route only, and rotate injection sites
regularly to avoid damage to muscles and to prevent subcutaneous atrophy. Give
regular
insulin intramuscularly or intravenously in emergency situations.
Monitor response carefully to avoid adverse effects; blood glucose monitoring is the
most effective way to evaluate insulin dose.
Monitor the patient for signs and symptoms of hypoglycemia, especially during
peak insulin times, when these signs and symptoms would be most likely to appear,
to assess the response to insulin and the need for dose adjustment or medical
intervention.
Always verify the name of the insulin being given because each insulin has a
different peak and duration, and the names can be confused.
Use caution when mixing types of insulin; administer mixtures of regular and NPH
insulins within 15 minutes after combining them to ensure appropriate suspension
and therapeutic effect.
Store insulin in a cool place away from direct sunlight to ensure effectiveness.
Predrawn syringes are stable for 1 week if refrigerated; they offer a good way toensure the proper dose for patients who have limited vision.
Monitor the patient during times of trauma or severe stress for potential dose
adjustment needs.
Monitor the patient’s food intake; ensure that the patient eats when using insulin toensure therapeutic effect and avoid hypoglycemia.
Monitor the patient’s exercise and activities; ensure that the patient considers the
effects of exercise in relationship to eating and insulin dose to ensure therapeuticeffect and avoid hypoglycemia
Protect the patient from infection, including good skin care and foot care, to prevent
the development of serious infections and changes in therapeutic insulindoses.
Monitor the patient’s sensory losses to incorporate his or her needs into safetyissues, as well as potential problems in drawing up and administering insulin.
Help the patient to deal with necessary lifestyle changes, including diet and
exercise needs, sensory loss, and the impact of a drug regimen that includes givinginjections, to help encourage compliance with the treatment regimen.
Instruct patients who are also receiving beta-blockers about ways to monitor glucose
levels and signs and symptoms of glucose abnormalities to prevent hypoglycemicand hyperglycemic episodes when SNS and warning signs are blocked.
Provide thorough patient teaching, including diet and exercise needs; measures
to avoid adverse effects, including proper food care and screening for injuries;
warning signs of problems, including signs and symptoms of hypoglycemia and
hyperglycemia; the importance of increased screening when ill or unable to eat
properly; proper administration techniques and proper disposal of needles andsyringes; and the need
to monitor disease status, to enhance patient knowledge about drug therapy andpromote compliance.
The nurse will evaluate the following
Monitor patient response to the drug (stabilization of blood glucose levels).
Monitor for adverse effects (hypoglycemia, ketoacidosis, and injection-site
irritation).
Evaluate the effectiveness of the teaching plan (patient can name drug,
dosage, adverse effects to watch for, specific measures to avoid them, and
proper administration technique).Monitor the effectiveness of comfort measures and compliance with the regimen.
Self-assessment 3.9
A nurse R is assigned to manage a patient for whom antidiabetic medications
are going to be initiated.
1) Which statement is correct about the nursing assessment before initiation
of antidiabetic administration?
a) Assess for contraindications or cautions
b) Assess the drug effect
c) Assess for the side effects
d) Monitor sensory losses
2) Which statement is NOT CORRECT about the nursing evaluation after
antidiabetic administration?
a) Evaluate the drug’s effectiveness
b) Evaluate for the side effects
c) Evaluate contraindicationsd) Evaluate the blood glucose levels
3.10. National treatment guidelines for diabetes mellitus
Learning Activity 3.10
The patient diagnosed of type 2 diabetes mellitus, and was admitted in Medical
unit in the hospital where most of health care providers were new and studied
outside of the country. The nurse had heard that the patient was shifted to the
third line of antidiabetic drugs but doesn’t know about the national guideline. The
latter wants the guidance from the matron.
1) Which information do you expect to be delivered by the matron?Guidance: Use the national guideline for NCDs book in Rwanda 2016
CONTENT SUMMARY
Management of type 1 Diabetes
Anyone who has type 1 diabetes needs lifelong insulin therapy. Treatment for type
1 diabetes includes: Taking insulin; carbohydrate, fat and protein counting; eating
healthy foods; frequent blood sugar monitoring; exercising regularly and maintaining
a healthy weight.
Management of type 2 Diabetes (Oral Therapy)
Management of type 2 Diabetes is based on Lifestyle and observe measures:
Healthy diet, physical activity, avoid /decrease alcohol, weight control. In addition to
lifestyle modification, the patients are started on oral antidiabetic drugs.Table 3.10.1: First Line
Glimepiride is alternative of Glibenclamide when there is frequent hypoglycemia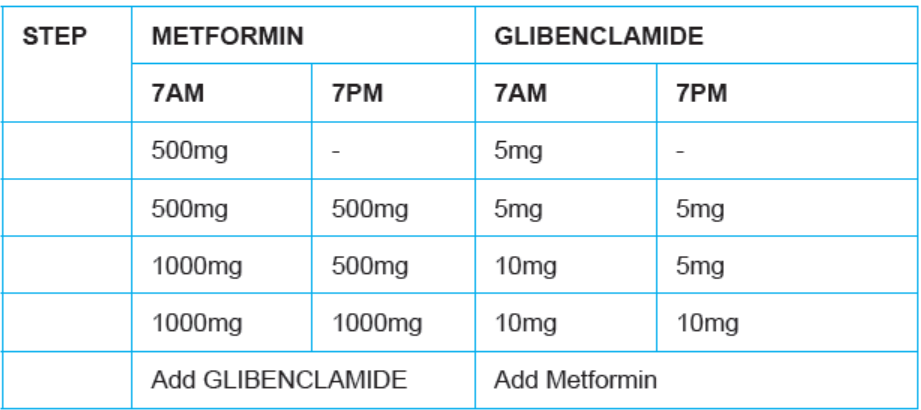
with Glibenclamide,1 or 2 mg given orally once daily with breakfast or the first major
meal of the day.
The dose may be increased by 1-2 mg in 1-2 weeks’ interval up to 4 mg maximum
based on blood sugar response and is given once daily.
Second Line
If despite adequate titration of doses of medication blood glucose targets are not
being attained after 6 months at the most (HbA1C should fall at least by 1% or
persistent hyperglycemia of more than 180mg/dl in the past 3 months). Check the
patient’s adherence (understanding of medical and self-management, reinforcement
of lifestyle factors influencing health and fitness targets). Exclude other conditions
that can disturb glycaemic control (e.g., steroids).
In addition to lifestyle measures, adherence to medication and dose Optimization
add
Vildagliptin (50mg) + Metformin (850 or 1000mg) Twice/day.Third line
On third line in addition to lifestyle measures, adherence to medication and dose
optimization. Give in preference Metformin (if tolerated) + Basal (long acting)Insulin. Add Prandial (short acting) with time if required.
Self-assessment 3.10
1) According to the national guide line for NCDs, which drug is given as first
line to treat a patient with diabetes type 2?
a) Glibenclamide
b) Insulin
c) Amoxicillin
d) Vildagliptin
2) According to the national guide line for NCDs, which drug is given as
second line to treat a patient with diabetes type 2?
a) Insulin+ metformin
b) Vildagliptin + Metformin
c) Glibenclamide+ Glucophaged) Insulin+ Glibenclamide
3.11. Anti-inflammatory drugs in asthma management
Learning Activity 3.11
Read the scenario below and answer the related questions.
During your clinical practice you receive a client in consultation room. The client
reports that he is taking anti-asthmatic drugs. Visit the library or use internet andcome with:
1) List classes of anti-asthmatic drugs
2) List four types of inhalation devices use when administering anti-asthmatic
drug by inhalation
3) Give two examples of drugs fall into Anti-inflammatory anti-asthmaticclass.
CONTENT SUMMARY
Asthma is a common chronic inflammatory disorder characterized by breathlessness
and tightness in the chest, together with wheezing, dyspnea, and cough. The
underlying cause is immune-mediated airway inflammation.
Anti-asthmatic drugs fall into two main pharmacologic classes: Anti-inflammatoryagents mainly the glucocorticoids, and bronchodilators mainly ,beta2 agonists .
For chronic asthma, glucocorticoids are administered on a fixed schedule, almost
always by inhalation. Beta2 agonists may be administered on a fixed schedule (for
long-term control) or PRN (to manage an acute attack). Like the glucocorticoids,
beta2 agonists are usually inhaled.
Most anti-asthma drugs can be administered by inhalation. This route has three
advantages:
1) Therapeutic effects are enhanced by delivering drugs directly to their site of
action,
2) Systemic effects are minimized, and3) Relief of acute attacks is rapid.
Inhalation Devices
Four types of inhalation devices are employed: metered-dose inhalers, Respimats,
dry-powder inhalers, and nebulizers.
Metered-Dose Inhalers (MDIs): are small, hand-held, pressurized devices that
deliver a measured dose of drug with each actuation. Dosing is usually accomplishedwith one or two inhalations.
Dry-Powder Inhalers (DPIs) are used to deliver drugs in the form of a dry, micronized
powder directly to the lungs.
A nebulizer: is a small machine used to convert a drug solution into a mist. The
droplets in the mist are much finer than those produced by inhalers, resulting in
less drug deposit on the oropharynx and increased delivery to the lung. Inhalation
of the nebulized mist can be done through a face mask or through a mouthpieceheld between the teeth.
Steroidal Anti-Inflammatory Drugs
The anti-inflammatory drugs, especially inhaled glucocorticoids are the foundation
of asthma treatment. These drugs are taken daily for long-term control.
The drugs used to affect inflammation are the inhaled steroids, the leukotriene
receptors, and a mast cell stabilizer, which can affect both bronchodilator and
inflammation.
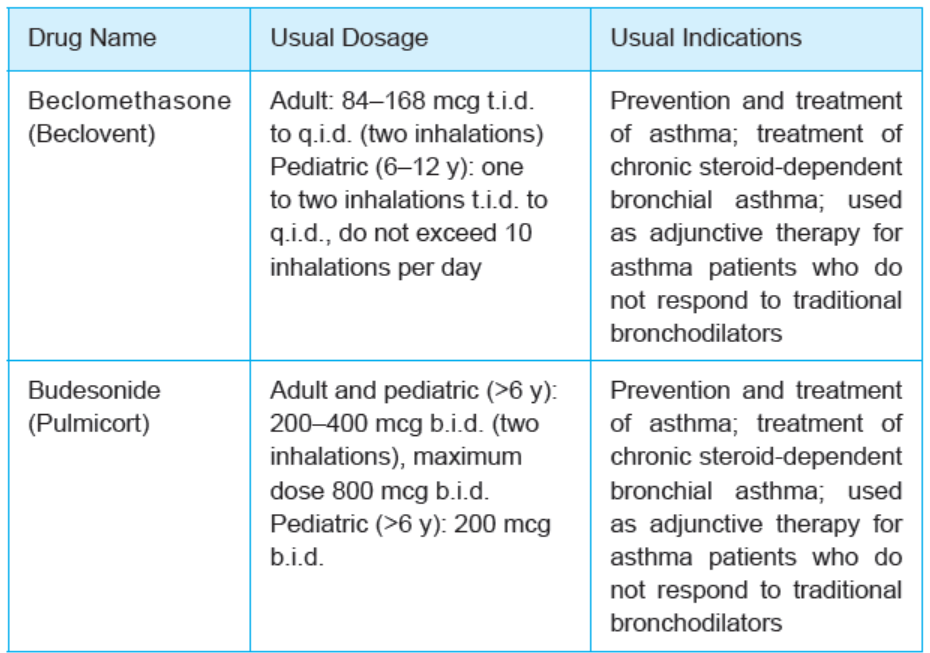
1. INHALED STEROIDS
Inhaled steroids have been found to be a very effective treatment for bronchospasm.
Agents approved for this use include beclomethasone (Beclovent and others),
budesonide (Pulmicort), ciclesonide (Alvesco), fluticasone (Flovent), and
triamcinolone (Azmacort and others). The drug of choice depends on the individual
patient’s response; a patient may have little response to one agent and do very well
on another. It is usually useful to try another preparation if one is not effective within
2 to 3 weeks.
Therapeutic Actions and Indications: Inhaled steroids are used to decrease the
inflammatory response in the airway. They have two main effects: Decreased swelling
associated with inflammation and promotion of beta-adrenergic receptor activity,
which may promote smooth muscle relaxation and inhibit bronchoconstriction.
Pharmacokinetics: These drugs are rapidly absorbed from the respiratory tract,
but they take from 2 to 3 weeks to reach effective levels, and so patients must be
encouraged to take them to reach and then maintain the effective levels. They are
metabolized by natural systems, mostly within the liver, and are excreted in urine.The glucocorticoids are known to cross the placenta and to enter breast milk.
Contraindications and Cautions: Inhaled steroids are not for emergency use and
not for use during an acute asthma attack or status asthmaticus. They should not
be used during pregnancy or lactation.
Adverse Effects: Adverse effects are limited because of the route of administration.
Sore throat, hoarseness, coughing, dry mouth, and pharyngeal and laryngeal fungal
infections are the most common side effects encountered. If a patient does not
administer the drug appropriately or develops lesions that allow absorption of the
drug, the systemic side effects associated with steroids may occur.Table 3.11.1: Inhaled steroids
2. Leukotriene Receptor Antagonists
This is a newer class of drugs, the leukotriene receptor antagonists, was developed
to act more specifically at the site of the problem associated with asthma. Because
this class is relatively new, long-term effects and the benefits of one drug over
another have not yet been determined.
Examples: Zafirlukast (Accolate) ,Montelukast (Singulair) and zileuton (Zyflo)
Therapeutic Actions and Indications: Leukotriene receptor antagonists selectively
and competitively block (zafirlukast, montelukast) or antagonize (zileuton) receptorsfor the production of leukotrienes. As a result, these drugs block many of the signs
and symptoms of asthma, such as neutrophil and eosinophil migration, neutrophil
and monocyte aggregation, leukocyte adhesion, increased capillary permeability,
and smooth muscle contraction. These factors contribute to the inflammation,
edema, mucus secretion, and bronchoconstriction seen in patients with asthma.
Pharmacokinetics: These drugs are given orally. They are rapidly absorbed from
the GI tract. Zafirlukast and montelukast are extensively metabolized in the liver
by the cytochrome P450 system and are primarily excreted in feces. Zileuton is
metabolized and cleared through the liver. These drugs cross the placenta and
enter breast milk (see Contraindications and Cautions).
Contraindications and Cautions: These drugs should be used cautiously in
patients with hepatic or renal impairment , these drugs should be used during
pregnancy only if the benefit to the mother clearly outweighs the potential risks
to the fetus. No adequate studies have been done on the effects on the baby if
these drugs are used during lactation; caution should be used. These drugs are
not indicated for the treatment of acute asthmatic attacks, because they do not
provide any immediate effects on the airways. Patients need to be cautioned that
they should not rely on these drugs for relief from an acute asthmatic attack
Adverse Effects: Adverse effects associated with leukotriene receptor antagonists
include headache, dizziness, nausea, diarrhea, abdominal pain, elevated liver
enzyme concentrations, vomiting, generalized pain, fever, and myalgia. Because
these drugs are relatively new, there is little information about their long-term
effects. Patients should be advised to monitor their use of these drugs and to report
any increase of acute episodes or lack of response to the drug, which could indicate
a worsening problem or decreased responsiveness to drug therapy
Clinically Important Drug–Drug Interactions
Use caution if propranolol, theophylline, terfenadine, or warfarin is taken with these
drugs because increased toxicity can occur. Toxicity may also occur if these drugs
are combined with calcium channel blockers, cyclosporine, or aspirin; decreaseddose of either drug may be necessary.
Table 3.11.2: Leukotriene Receptor Antagonists
3. Mast Cell Stabilizer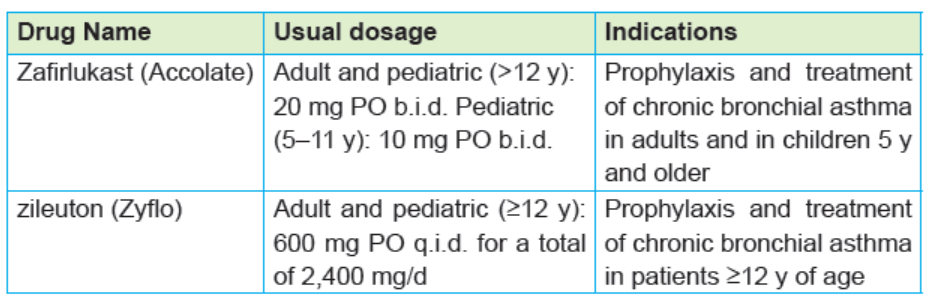
A mast cell stabilizer prevents the release of inflammatory and bronchoconstricting
substances when the mast cells are stimulated to release these substances
because of irritation or the presence of an antigen. Cromolyn (Nasacort) is the only
drug still available in this class, only available in an over-the-counter form, and it is
no longer considered part of the treatment standards because of the availability of
more specific and safer drugs.
CROMOLYN
Cromolyn is an inhalational agent that suppresses bronchial inflammation. The drug
is used for prophylaxis—not quick relief in patients with mild to moderate asthma.
Anti-inflammatory effects are less than with glucocorticoids; therefore, cromolyn is
not a preferred drug for asthma therapy. When glucocorticoids create problems,
however, cromolyn may be prescribed as alternative therapy.
Mechanism of Action: Cromolyn suppresses inflammation; it does not cause
bronchodilation. The drug acts in part by stabilizing the cytoplasmic membrane
of mast cells, preventing release of histamine and other mediators. In addition,
cromolyn inhibits eosinophils, macrophages, and other inflammatory cells.
Pharmacokinetics: Cromolyn is administered by nebulizer. The fraction absorbed
from the lungs is small and rarely produces significant systemic effects. Absorbed
cromolyn is excreted unchanged in the urine.
Therapeutic Uses
Chronic asthma: Cromolyn is an alternative to inhaled glucocorticoids for
prophylactic therapy of asthma. When administered on a fixed schedule, cromolyn
reduces both the frequency and intensity of asthma attacks. Maximal effects may
take several weeks to develop. No tolerance to effects is seen with long-term use.
Cromolyn is especially effective for prophylaxis of seasonal allergic attacks and
for acute allergy prophylaxis immediately before allergen exposure (e.g., before
mowing the lawn).
Adverse Effects: Cromolyn is the safest of all antiasthma medications. Significant
adverse effects occur in fewer than 1 of every 10,000 patients. Occasionally, cough
or bronchospasm occurs in response to cromolyn inhalation.
Preparations, Dosage, and Administration
Cromolyn is administered using a power-driven nebulizer. The initial dosage for
adults and children is 20 mg 4 times a day. For maintenance therapy, the lowesteffective dosage should be established.
NURSING CONSIDERATIONS FOR PATIENTS RECEIVING STEROIDAL ANTIINFLAMMATORYDRUGS
Before, during and after administration of steroidal anti-inflammatory drugs, a nurse
the following are nurse’s considerations:
Assessment
• Assess for possible contraindications or cautions
• Perform a physical examination to establish baseline.
• Assess vital signs and parameters
• Examine the nares to evaluate for any lesions that might lead to systemic
absorption of the drug
• Evaluate liver and renal function tests to assess for impairments that could
interfere with metabolism or excretion of the drugs.
• Perform an abdominal evaluation to monitor gastrointestinal (GI) effects of
the drug
Also the nurse will implement the following:
Taper systemic steroids carefully during the transfer to inhaled steroids; deaths
have occurred from adrenal insufficiency with sudden withdrawal.
Do not administer inhaled steroid to treat an acute asthma attack or status
asthmaticus because these drugs are not intended for treatment of acute attack
and will not provide the immediate relief that is needed.
Have the patient use decongestant drops before using the inhaled steroid to
facilitate penetration of the drug if nasal congestion is a problem.
Have the patient rinse the mouth after using the inhaler because this will help to
decrease systemic absorption and decrease gastrointestinal (GI) upset and nausea.
Monitor the patient for any sign of respiratory infection; continued use of steroids
during an acute infection can lead to serious complications related to the depression
of the inflammatory and immune responses.
Provide thorough patient teaching, including the drug name and prescribed dosage,
measures to help avoid adverse effects, warning signs that may indicate problems,
and the need for periodic monitoring and evaluation, to enhance patient knowledge
about drug therapy and to promote compliance
Instruct the patient to continue to take the drug to reach and then maintain effective
levels (drug takes 2 to 3 weeks to reach effective levels).
Offer support and encouragement to help the patient cope with the disease and the
drug regimen. Administer drug on an empty stomach, 1 hour before or 2 hours after
meals; the bioavailability of these drugs is decreased markedly by the presence of
food.
Caution the patient that these drugs are not to be used during an acute asthmatic
attack or bronchospasm; instead, regular emergency measures will be needed.
Caution the patient to take the drug continuously and not to stop the medication
during symptom free periods to ensure that therapeutic levels are maintained.
Provide appropriate safety measures if dizziness occurs to prevent patient injury.
Urge the patient to avoid over-the-counter preparations containing aspirin, which
might interfere with the effectiveness of these drugs.
Provide thorough patient teaching, including the drug name and prescribed dosage,
measures to help avoid adverse effects, warning signs that may indicate problems,
and the need for periodic monitoring and evaluation, to enhance patient knowledge
about drug therapy and to promote compliance.
Offer support and encouragement to help the patient cope with the disease and the
drug regimen.
The nurse monitors the following:
• Monitor patient response to the drug (improved breathing).
• Monitor for adverse effects (nasal irritation, fever, GI upset).
• Evaluate the effectiveness of the teaching plan (patient can name drug,
dosage, adverse effects to watch for, specific measures to avoid them, and
measures to take to increase the effectiveness of the drug).
• Monitor the effectiveness of other measures to ease breathing
• Monitor patient response to the drug (improved breathing).
• Monitor for adverse effects (drowsiness, headache, abdominal pain, myalgia).
• Evaluate the effectiveness of the teaching plan (patient can name drug,
dosage, adverse effects to watch for, specific measures to avoid them, and
measures to take to increase the effectiveness of the drug).• Monitor the effectiveness of other measures to ease breathing
Self-assessment 3.11
1) Most anti-asthma drugs can be administered by inhalation. List three
advantages of administering anti-asthmatic drugs by inhalation.
2) The main anti-inflammatory drugs used in treatment of asthma are ……
3) Patient was consulted at health post for asthma crises arriving at the
health post. The Patient met with associate nurse student G who was
in clinical placement mentored by senior nurse in the service. When the
senior nurse requested the student G to provide treatment to the patient,
the student should reflect on different classes of anti-asthmatic drugs
available to treat the asthma and she found at the health post were only
anti-inflammation drugs .
What should be the nursing evaluation during the use of this anti-inflammatory
drugs ?
3.12. Bronchodilator antiasthmatics
Learning Activity 3.12
During your clinical practice, you receive a client with signs and symptoms of
asthma.
You hear senior nurse saying that he patient will be administered an antiasthmatic
drug that belongs to bronchodilators classes.
Using pharmacology book or internet
1) How do anti-asthmatic bronchodilators facilitate respiration to treat
asthma2) Give three groups of bronchodilator anti-asthmatic drugs
CONTENT SUMMARY
Bronchodilator anti-asthmatics are medications used to facilitate respirations by
dilating the airways. They are helpful in symptomatic relief or prevention of bronchial
asthma and for bronchospasm associated with COPD.
Bronchodilators include xanthines, sympathomimetics, and anticholinergics.
1) XANTHINES
The xanthines have a direct effect on the smooth muscles of the respiratory
tract, both in the bronchi and in the blood vessels. They include aminophylline
(Truphylline), caffeine (Caffedrine and others), dyphylline (Dilor and others), and
theophylline (Slo-Bid, Theo-Dur). They have a relatively narrow margin of safety
and interact with many other drugs, they are no longer considered the first-choice
bronchodilators.
Therapeutic Actions and Indications: Xanthines work by directly affecting the
mobilization of calcium within the cell. They do this by stimulating two prostaglandins,
resulting in smooth muscle relaxation, which increases the vital capacity that has
been impaired by bronchospasm or air trapping.
Also, they inhibit the release of slow reacting substance of anaphylaxis (SRSA) and
histamine, decreasing the bronchial swelling and narrowing that occurs as a result
of these two chemicals for usual indications for these drugs.
Pharmacokinetics: The xanthines are rapidly absorbed from the gastrointestinal
(GI) tract when given orally, reaching peak levels within 2 hours. They are also
given IV, reaching peak effects within minutes. They are widely distributed and
metabolized in the liver and excreted in urine. Xanthines cross the placenta and
enter breast milk
Contraindications and Cautions: Caution should be taken with any patient with
GI problems, coronary disease, respiratory dysfunction, renal or hepatic disease,
alcoholism, or hyperthyroidism because these conditions can be exacerbated by
the systemic effects of xanthines.
Adverse Effects: Adverse effects associated with xanthines are related to
theophylline levels in the blood. Therapeutic theophylline levels are from 10 to
20mcg/mL. With increasing levels, predictable adverse effects are seen, ranging
from GI upset, nausea, irritability, and tachycardia to seizures, brain damage, andeven death.
Xanthines
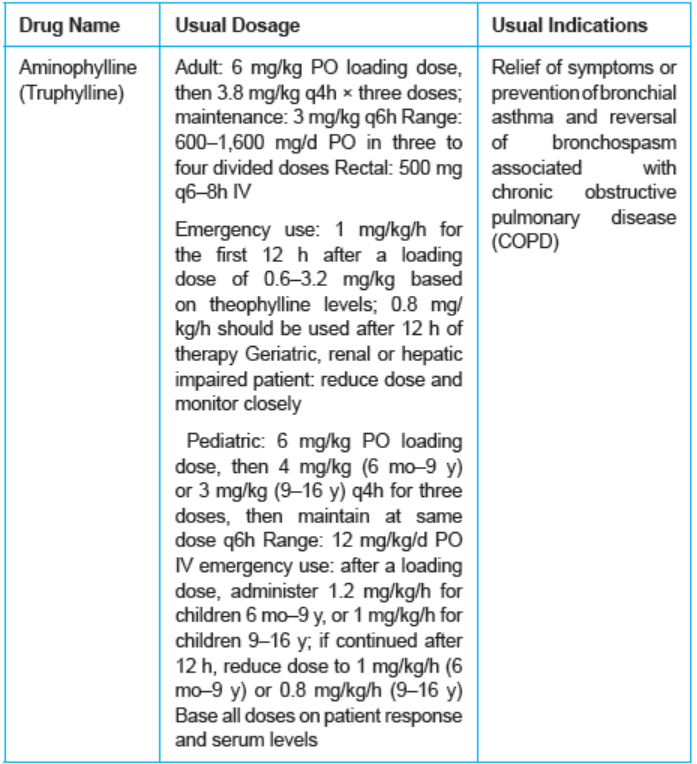
2) SYMPATHOMIMETICS
Table 3.12.1: Sympathomimetics
Sympathomimetics are drugs that mimic the effects of the sympathetic nervous
system that include the dilation of the bronchi with increased rate and depth of
respiration. The sympathomimetics that are used as bronchodilators include
albuterol/salbutamol (Proventil and others), arformoterol (Brovana), bitolterol
(Tornalate), ephedrine (generic), epinephrine (EpiPen), formoterol (Foradil),indacaterol (Arcapta), isoetharine (generic), isoproterenol (Isuprel and others),
levalbuterol (Xopenex), metaproterenol (Alupent), pirbuterol (Maxair), salmeterol
(Serevent), and terbutaline (Brethaire and others).
The therapeutic Actions and Indications: Most of the sympathomimetics used
as bronchodilators are beta2-selective adrenergic agonists, beta2- receptors found
in the bronchi,other systemic effects of sympathomimetics include increased blood
pressure, increased heart rate, vasoconstriction, and decreased renal and GI blood
flow—all actions of the sympathetic nervous system
Pharmacokinetics: Sympathomimetics available only as an inhalant include the
arformoterol, formoterol, indacaterol, isoetharine, levalbuterol, pirbuterol, and
salmeterol. They vary in their duration of action, long-acting beta adrenergics have
half-lives between 45 and 126 hours.
Other sympathomimetics are available in various forms. Albuterol and metaproterenol
are available in inhaled and oral forms. Terbutaline can be used as an inhalant and
as an oral and parenteral agent. Isoproterenol is available for intravenous use.
Ephedrine is used orally and in parenteral form (for IV, IM, and subcutaneous use).
These drugs are rapidly distributed after injection; they are transformed in the liver
to metabolites that are excreted in the urine. The half-life of these drugs is relatively
short—less than 1 hour.
They are known to cross the placenta and to enter breast milk.The inhaled drugs
are rapidly absorbed into the lung tissue. Although very little of the drug is absorbed
systemically, any absorbed drug will still be metabolized in the liver and excretedin urine
Contraindications and Cautions: These drugs are contraindicated or should
be used with caution, depending on the severity of the underlying condition, in
conditions that would be aggravated by the sympathetic stimulation, including
cardiac disease, vascular disease, arrhythmias, diabetes, and hyperthyroidism.
These drugs should be used during pregnancy and lactation only if the benefits to
the mother clearly outweigh potential risks to the fetus or neonate.
Adverse Effects: Central nervous system stimulation, GI upset, cardiac arrhythmias,
hypertension, bronchospasm, sweating, pallor, and flushing. Isoproterenol isassociated with more cardiac side effects than some other drugs.
Table 3.12.2: Sympathomimetics
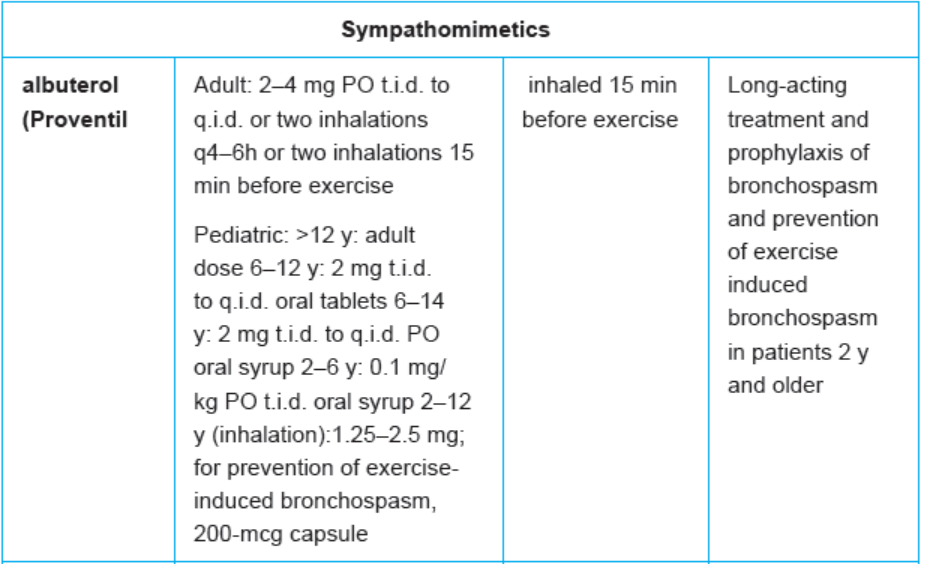
1) ANTICHOLINERGIC ANTI-ASTHMATIC DRUGS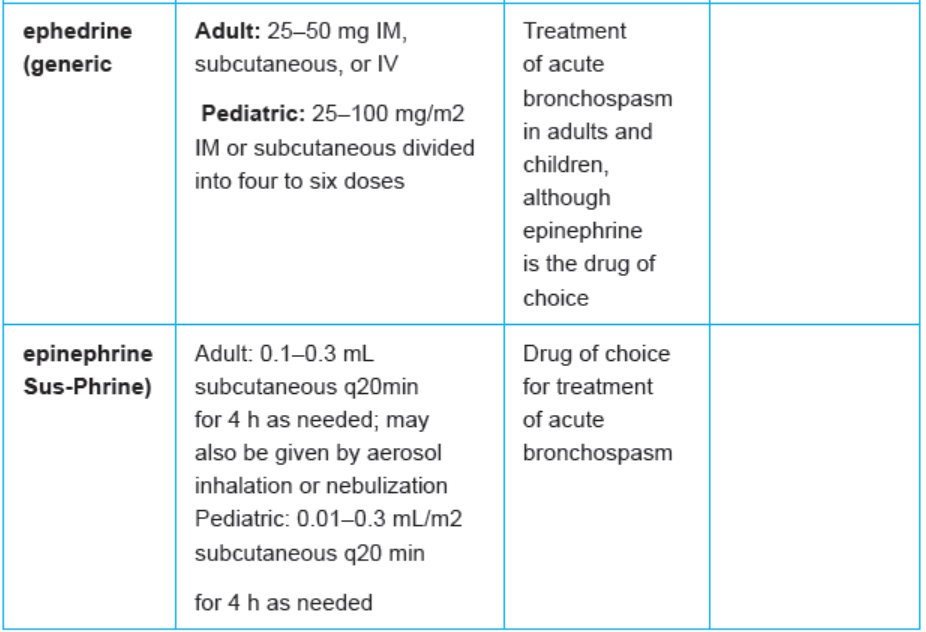
Patients who cannot tolerate the sympathetic effects of the sympathomimetics might
respond to the anticholinergic drugs ipratropium (Atrovent) and tiotropium (Spiriva).
These drugs are not as effective as the sympathomimetics but can provide some
relief to those patients who cannot tolerate the other drugs. Tiotropium is the first
drug approved for once-daily maintenance treatment of bronchospasm associated
with COPD.
Therapeutic Actions and Indications: Anticholinergics are used as bronchodilators
because of their effect on the vagus nerve, which is to block or antagonize the
action of the neurotransmitter acetylcholine at vagal-mediated receptor sites.
Normally, vagal stimulation results in a stimulating effect on smooth muscle, causing
contraction. By blocking the vagal effect, relaxation of smooth muscle in the bronchi
occurs, leading to bronchodilation.
Pharmacokinetics: These drugs are available for inhalation, using an inhaler
device. Ipratropium is also available as a nasal spray for seasonal rhinitis.
Ipratropium has an onset of action of 15 minutes when inhaled. Its peak effects
occur in 1 to 2 hours, and it has a duration of effect of 3 to 4 hours. Little is known
about its fate in the body. It is generally not absorbed systemically. Tiotropium has a
rapid onset of action and a long duration, with a half-life of 5 to 6 days. It is excreted
unchanged in urine.
Contraindications and Cautions: Caution should be used in any condition that
would be aggravated by the anticholinergic or atropine-like effects of the drug,
such as narrow-angle glaucoma (drainage of the vitreous humor can be blocked
by smooth muscle relaxation), bladder neck obstruction or prostatic hypertrophy
(relaxed muscle causes decreased bladder tone), and conditions aggravated
by dry mouth and throat. The use of ipratropium or tiotropium is contraindicated
in the presence of known allergy to the drug or to soy products or peanuts (the
vehicle used to make ipratropium an aerosol contains a protein associated with
peanut allergies) to prevent hypersensitivity reactions. These drugs are not usually
absorbed systemically, but as with all drugs, caution should be used in pregnancy
and lactation because of the potential for adverse effects on the fetus or nursing
baby.
Adverse Effects: Adverse effects are related to the anticholinergic effects of the
drug if it is absorbed systemically. These effects include dizziness, headache,
fatigue, nervousness, dry mouth, sore throat, palpitations, and urinary retention
Clinically Important Drug–Drug Interactions: There is an increased risk of
adverse effects if these drugs are combined with any other anticholinergics; thiscombination should be avoided.
Table 3.12.3: Anticholinergics
Nursing Considerations for Patients Receiving bronchodilators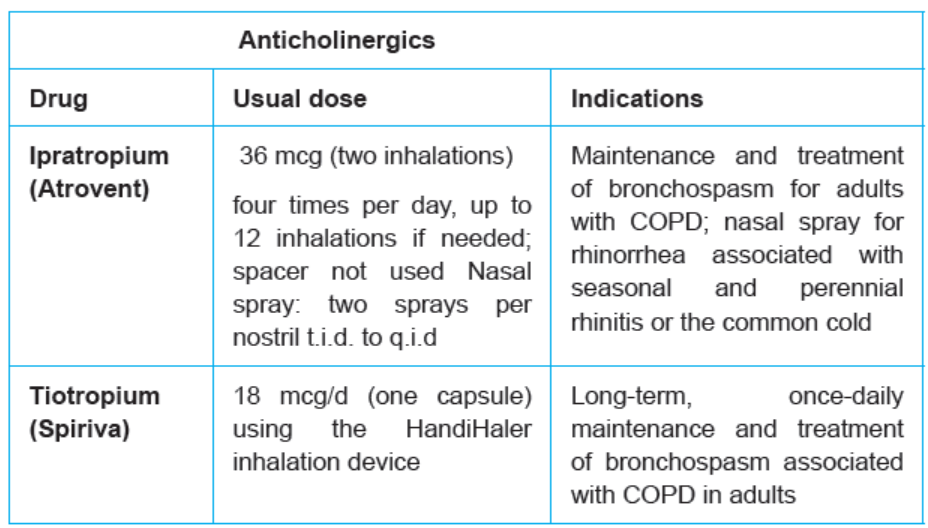
• Assess for possible contraindications or cautions.
• Perform a physical examination to establish baseline data for assessing
the effectiveness of the drug and the occurrence of any adverse effects
associated with drug therapy.
• Assess reflexes and orientation to evaluate central nervous system (CNS)
effects of the drug.
• Assess the skin color and lesions to assess for dryness or allergic reaction
and to evaluate oxygenation.
• Evaluate orientation, affect, and reflexes to evaluate central nervous system
(CNS) effects.
• Assess pulse and blood pressure to monitor cardiovascular effects of the
drug.
• Evaluate respirations and adventitious sounds to monitor drug effectiveness
and possible adverse effects.
• Evaluate urinary output and prostate palpation as appropriate to monitor
anticholinergic effects (anticholinergic drugs)
• Monitor respirations and adventitious sounds to establish a baseline for drug
effectiveness and possible adverse effects.
• Evaluate pulse, blood pressure, and, in certain cases, a baseline
electrocardiogram to monitor the cardiovascular effects of sympathetic
stimulation.
• Evaluate liver function tests to assess for changes that could interfere with
metabolism of the drug and require dose adjustment.
• Ensure adequate hydration and provide environmental controls, such as the
use of a humidifier, to make the patient more comfortable.
• Encourage the patient to void before each dose of medication to prevent
urinary retention related to drug effects.
• Provide safety measures if CNS effects occur to prevent patient injury.
• Provide small, frequent meals and sugarless lozenges to relieve dry mouth
and GI upset.
• Advise the patient not to drive or use hazardous machinery if nervousness,
dizziness, and drowsiness occur with this drug to prevent injury.
• Provide thorough patient teaching, including the drug name and prescribed
dosage, measures to help avoid adverse effects, warning signs that may
indicate problems, and the need for periodic monitoring and evaluation, to
enhance patient knowledge about drug therapy and to promote compliance.
• Review the use of the inhalator with the patient; caution the patient not to
exceed 12 inhalations in 24 hours to prevent serious adverse effects.
• Offer support and encouragement to help the patient cope with the disease
and the drug regimen
• Reassure patient that the drug of choice will vary with each individual.
The sympathomimetics are slightly different chemicals and are prepared
in a variety of delivery systems. A patient may have to try several different
sympathomimetics before the most effective one is found.
• Advise the patient to use the minimal amount needed for the shortest period
necessary to prevent adverse effects and accumulation of drug levels.
• Teach patients who use one of these drugs for exercise-induced asthma to
use it 30 to 60 minutes before exercising to ensure peak therapeutic effects
when they are needed.
• Alert patient that long-acting adrenergic blockers are not for use during acute
attacks because they are slower acting and will not provide the necessary
rescue in a state of acute bronchospasm.
• Provide safety measures as needed if CNS effects become a problem to
prevent patient injury.
• Provide small, frequent meals and nutritional consultation if GI effects interfere
with eating to ensure proper nutrition.
• Provide thorough patient teaching, including the drug name and prescribed
dosage, measures to help avoid adverse effects, warning signs that may
indicate problems, and the need for periodic monitoring and evaluation, toenhance patient knowledge about drug therapy and to promote compliance.
Carefully teach the patient about proper use of the prescribed delivery
system. Review that procedure periodically because improper use may result
in ineffective therapy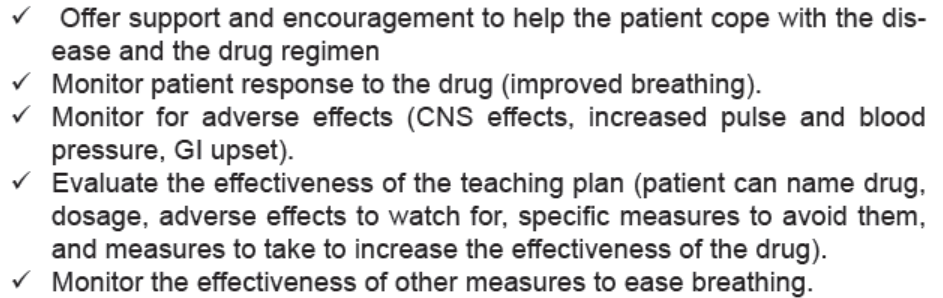
Self-assessment 3.12
1) Which of the following drugs is a xanthine?
a) Amoxicillin
b) Beclomethasone
c) Aminophylline
d) Epinephrine
2) Which of the following drugs belongs to the class of sympathomimetic
anti asthmatic drugs?
a) Amoxycilline
b) Beclomethasone
c) Aminophylline
d) Epinephrine
5) During clinical practice, you receive a client with severe episode of
asthma attack. After the assessment, the nurse recommends you to give
aminophylline via IV route instead of oral route.
Explain why the nurse chose the IV route instead of oral route.
3.13. National treatment guidelines for asthma
Learning Activity 3.13
The patient with known with simple intermittent episodes of asthma comes to
the health facility where you are conducting the clinical practice as an associate
nurse student. The patient has developed as a simple asthma attack that needs
management. The nurse tasks you to manage the patient with reference to the
Rwanda national guidelines of asthma management.
1) Which of the following management options may be instituted for this
patient?
a) Use an inhaled short-acting beta2 agonist (SABA) for quick relief.
b) Use an inhaled glucocorticoid for quick relief of the asthma attack
c) Use salbutamol, beclamethasone and aminophylline for quick relief.
d) Use a combination of beclamethasone and aminophylline for quick
relief.
2) After two days later, the patient comes with complicated episode of asthma
attack and a deep assessment classifies that patient to be managed by
step 2 in the national guidelines of asthma management. Which of the
following drugs may be used?
a) Beclamethasone and aminophylline
b) Salbutamol and aminophylline
c) Salbutamol and beclamethasone
d) Beclamethasone and amoxicillin
CONTENT SUMMARY
Use Respiratory emergency method to treat asthma
If a patient is having an asthma attack, then classify severity based on IUATLD(International Union Against Tuberculosis and Lung Disease) guidelines below:
Table 3.13.1: asthma attack classification
• Position upright, give continuous salbutamol nebulizer, administer I.V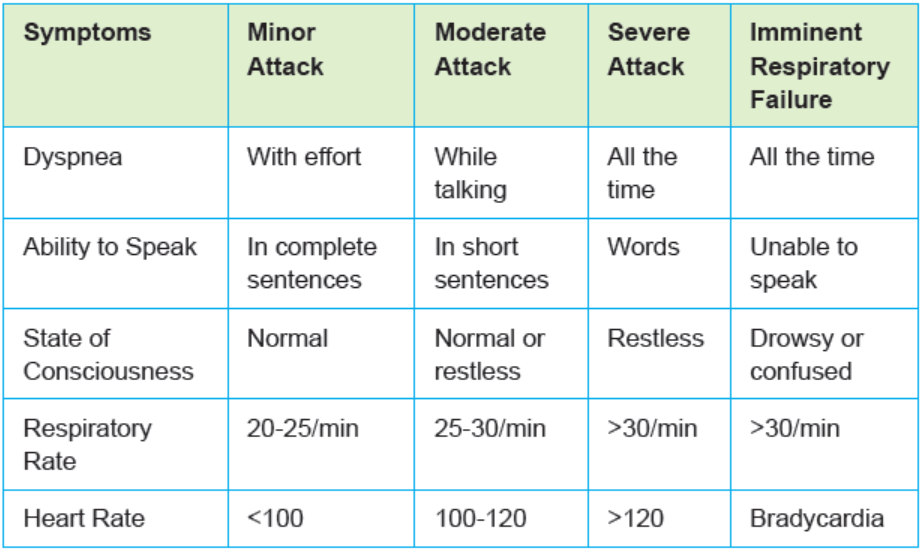
hydrocortisone 100 mg or prednisolone po 60mg if I.V not available.
• Oxygen by facial mask 6l/min if O2 saturation is magnesium 2g IV x 1.
• Give amoxicillin 500mg PO x 1 if pneumonia suspected.
• Give furosemide 40mg IV x 1 if HF suspected.
• Call physician and admit to hospital.
• Intubation if decreased level of consciousness, exhaustion, silent chest,
acidemia, cyanosis.
• Directed therapy if the triggering factor is evident: e.g antibiotics in case of
infection.
Use the step method to treat asthma
Drug dosages and drug classes are stepped up as needed, and stepped down
when possible. Six steps are described. The basic concept is simple.
First, all patients, starting with step 1, should use an inhaled short-acting beta2
agonist (SABA) as needed for quick relief.
Second step all patients except those on step 1 should use a long-term control
medication (preferably an inhaled glucocorticoid) to provide baseline control.
Third, when patients move up a step, owing to increased impairment and risk,
dosage of the control medication is increased or another control medication isadded (typically an LABA), or both.
Fourth, after a period of sustained control, moving down a step should be tried.
For patients just beginning drug therapy, the step they start on is determined by the
pretreatment classification of asthma severity. For example, a patient diagnosed
with intermittent asthma would begin at step 1 (PRN use of an inhaled SABA),
whereas a patient diagnosed with moderate persistent asthma would begin at step
3 (daily inhalation of a low-dose glucocorticoid plus daily inhalation of a long-actingbeta2 agonist (LABA), supplemented with an inhaled SABA as needed).
After treatment has been ongoing, stepping up or down is based on assessment of
asthma control. Like the diagnosis of pretreatment severity, assessment of control
is based on two domains: current impairment and future risk. In EPR-3, three
classes of control are defined: well controlled, not well controlled, and very poorlycontrolled.
Classify asthma severity: Intermittent, Persistent-Mild, Persistent-Moderate andPersistent-Severe (Asthma Attack)
Step-up therapy: When patient’s asthma severity worsens.
Step-down therapy: When the patient achieves 3 months of symptom relief
STEP 5: ASTHMA ATTACK 1. Revert to Respiratory emergency
STEP 4: Persistent – Severe
1) Salbutamol Inh 2 puffs every 4 hr PRN
2) Beclamethasone 1500mcg 2 puff BD3) Aminophylline 100mg PO 3x/day
STEP 3: Persistent – Moderate
1) Salbutamol Inh 2 puffs every 6 hrs2) Beclamethasone 1000mcg 1puff BD
STEP 2: Persistent – Mild
1) Salbutamol Inh 2 puffs every 6 hrs PRN2) Beclamethasone 500mcg 1puff BD
STEP 1: Intermittent1) Salbutamol Inh 2 puffs every 6 hrs PRN
In emergency room treatment must be started while the evaluation is still
going on. Position upright, give continuous salbutamol nebulizer,
• You may be given aerosolized beta-agonist medications through a face
mask or a nebulizer, with or without an anticholinergic agent. Administer I.V
hydrocortisone 100 mg or prednisolone po 60mg if I.V not available.
• Oxygen by facial mask 6l/min if O2 saturation is <92% RA You may be given
oxygen through a face mask or a tube that goes in your nose. If symptoms
uncontrolled after 30 minutes -> magnesium 2g IV x 1.
• Give amoxicillin 500mg PO x 1 if pneumonia suspected.
• Give furosemide 40mg IV x 1 if HF suspected.
• Call physician and admit to hospital.
• Intubation if decreased level of consciousness, exhaustion,
• Silent chest, acidemia, cyanosis.
• Directed therapy if the triggering factor is evident: e.g antibiotics in case of
infection,a) Use the step method to treat asthma
b) Oxygen therapy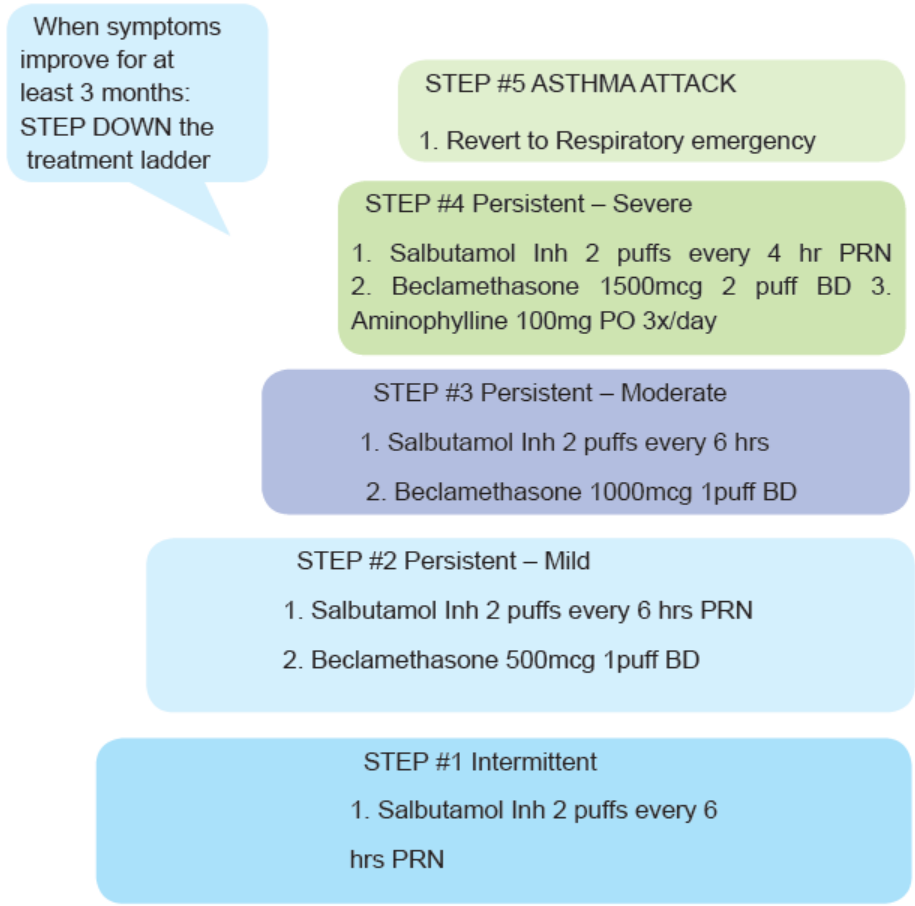
Oxygen therapy is a form of treatment that provides the body with additional oxygen,
oxygen therapy used to treat various conditions, including severe asthma attacks.
Typically, oxygen treatments are delivered through a face mask or nasal prongs,
or sometimes an oxygen tent. Oxygen treatments can be done both in the hospital
and in your home. Additionally, oxygen treatments may be required short term or
long term.
Oxygen treatments can be delivered through a device like a tank of liquid or gas
oxygen. (concentrators), Nasal cannula, simple face mask, nonrebreather mask,venturi mask, Bipap.
Self-assessment 3.13
The patient was admitted at the health center for signs and symptoms of asthma.
When asked to provide the drugs to the patient, the student in the clinical
placement consulted the national guidelines for treatment of asthma disease.
1) How is asthma classified based on national guidelines for treatment of
asthma?
2) Give management options used to treat each class of asthma, anddosages of drugs used if any
3.14. End unit Assessment
End of unit assessment
1) Diuretics alone are used to treat which of the following conditions?
a) Severe hypertension
b) Moderate hypertension
c) Mild hypertension
d) Hypertension with complication
2) Which of the following is a nursing consideration regarding the time of
diuretic administration?
a) Administer oral form early in the day so that increased urination will not
interfere with sleep.
b) Administer oral form at night so that increased urination will not disturb
the work of the patient.
c) Administer oral form at noon to ease the digestion of the patient
d) Administer oral form early in the day so that increased urination will not
interfere with other drug action.
3) Which of the following describes the mechanism of action of calcium
channel blockers?
a) Block the effects of the sympathetic nervous system are useful in
blocking many of the compensatory effects
b) Inhibit the formation of angiotensin II and reduces vascular resistance
c) They increase excretion of water, sodium, chloride, and potassium.
d) They relax and open up narrowed blood vessels
4) Among the following is NOT a contra-indication of beta-blockers:
a) Diabetes mellitus,
b) Chronic obstructive pulmonary disease (COPD) and
c) Hypertension
d) Asthma
5) Which of the following drugs is a vasodilator?
a) Captopril
b) Hydralazine
c) Nifedipine
d) Atenolol
6) The medical management of diabetes mellitus is aimed at:
a) Regulating blood glucose levels.
b) Controlling caloric intake.
c) Increasing exercise levels.
d) Decreasing fluid loss.
7) A patient has a BP of 179/109 mmHg, which of the following IS NOT
among the management measures?
a) Start two hypertensive medications
b) Start one antihypertensive
c) Encourage lifestyle modifications
d) Lifestyle Modifications
8) Which of the following drugs is an oral hypoglycemic agent?
a) Metronidazole
b) Metoclopramide
c) Metformind) Methanol
REFERENCES
1) Amy M. Karch. (2013). Focus on Nursing Pharmacology. Sixth edition:
Wolters Kluwer Health | Lippincott Williams &6 Wilkins.
2) Center for Diseases Control and Prevention. (2015). Staying on Track with
Tuberculosis Medicine.
3) Karch (2013). Focus on Nursing Pharmacology, 6th edition. Wolters Kluwer
Health | Lippincott Williams & Wilkins
4) Michael Patrick Adams, Leland Norman Holland, Jr, and Carol Quam Urban
(2014). Pharmacology for Nurses: A Pathophysiologic Approach. 4th edition.
Pearson Education, Inc.
5) David E. Golan, Ehrin J. Armstrong, and April W. Armstrong (2017).
PRINCIPLES of PHARMACOLOGY THE PATHOPHYSIOLOGIC BASIS OF
DRUG THERPY.4th edition. Wolters Kluwer
6) Bertram G.K, Susan B.M., and Anthony.J.Trevor (2012). Basic and Clinical
Pharmacology, 12th Ed.Mc Graw Hill LANGE.
7) Sharkey KA, MacNaughton WK. Pharmacotherapy for gastric acidity, peptic
ulcers, and gastroesophageal reflux disease. In, Brunton LL, Hilal-Dandan
R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of
therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 909-20, pp. 921-44, 945-54
8) Dicyclomine Capsule/Tablet (A-S Medication Solutions). DailyMed. Source:
U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/.
Accessed 04/10/2019.
9) Dicyclomine Solution for Injection (Leucadia Pharmaceuticals, Inc.).
DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.
nih.gov/dailymed/. Accessed 04/10/2019.
10) https://www.pharmacologyeducation.org/clinical-pharmacology/clinicalpharmacokinetics
11) https://www.nestle-watersna.com/sites/g/files/pydnoa606/files/asset-library/
documents/pdfs/fluid_requirements.pdf
12) https://www.nutritioninnovationlab.org/node/437
13) https://www.ebmconsult.com/app/medical-calculators/maintenance-fluidcalculator
14) https://www.google.com/
search?q=homemade+oral+rehydration+salt+preparation+images&
15) tbm=isch&ved=2ahUKEwjNpbfBteP0AhULxeAKHQy_DcMQ2-cCegQIABA16) https://www.google.com/search?q=NORMAL+SALINE&rlz=1C1GCEU_en-A&oq=homemade+oral+rehydration+salt
GBRW877RW877&sxsrf=AOaemvLqWlPhzLJXFwYQOG5PvTJsKx8k5Q :1639575757401&source=lnms&tbm=isch&sa=X&ved=2ahUKEwjftuLU9-
X0AhURZMAKH
17) .https://www.google.com/search?q=5%25+Dextrose+&tbm=isch&ved=2ah
UKEwikqNya-eX0AhXBw4UKHd71CxYQ2
- c C e g Q I A B A A & o q = 5 % 2 5 + D e x t r o s e + & g s _
lcp=CgNpbWcQAzIHCCMQ7wMQJzIFCAAQgAQyBQgAEIAEMgUIA
18) Infusion Nurses Society (INS). (2016). Infusion therapy standards of practice.
Standard 34: Needleless connectors.Journal of Infusion Nursing, 39(Suppl.1), S68-S70. (Level D)
