UNIT 2 DRUGS ACTING ON GASTROINTESTINAL TRACT
KEY UNIT COMPETENCE:
To provide appropriate medications for common gastrointestinal medical conditions
management.
Introductory activity 2.0Observe the picture below and respond to the following questions.
1. What do you observe on images A, B, C and D?2. What do images E, F, G, H and l show you?
2.1. Definition and classification of drugs acting on gastrointestinaltract:
Learning Activity 2.1
A 22-years old male patient consults a health facility where you are placed in
the clinical practicum. He complains of lower abdominal pain, diarrhoea and
vomiting. On the arrival, you find that the patient has lost fluids, and requires
intravenous fluids. Your colleague needs you to advise him on the medications
you may use to manage his pain and vomiting.
1. Using the library textbooks, list the categories of drugs acting on the
gastrointestinal tract.
2. How can you define an antiemetic drug?
3. What are the main reasons for using the drugs acting on the gastrointestinaltract?
CONTENT SUMMARY
The anatomic structures of GI include the oral cavity, pharynx, oesophagus, stomach,
small intestine, and large intestine the digestive tract plays a role of bringing life
sustaining elements into the body, and taking waste products out of it, accessory
organs (e.g., liver, gall bladder, salivary glands, and pancreas). Regulation of these
actions is controlled by many mechanisms. One control mechanism of the GI tract
is the autonomic nervous system (ANS), which consists of the sympathetic branch
(fight-or flight response) and the parasympathetic branch (homeostatic response).
Parasympathetic stimulation increases intestinal motility and GI secretions and
relaxes sphincters. Cholinergic drugs simulate these actions. Anticholinergic
drugs inhibit these actions. Sympathetic stimulation decreases intestinal motility,
decreases intestinal secretions, and inhibits the action of sphincters. Sympatheticdrugs simulate these actions.
Gastrointestinal drugs can be administered for a variety of reasons. Some
gastrointestinal drugs encourage peristalsis, suppress it, or reduce its undesirable
by-products. Other GI drugs decrease the flow of saliva, control vomiting and
diarrhoea, loosen stool, cause vomiting, protect the GI tract, decrease acid
production, or re-establish GI normal flora.
These medications can be classified into the following categories based on their
use:
– Drugs for gastritis and peptic ulcer diseases
– Antiemetic drugs
– Oral rehydration salts (ORS)
– Intravenous fluids
– Antispasmodic drugs– Laxative drugs
Drugs that are used for gastritis and peptic ulcer disease management usually
include proton pump inhibitors, H2 receptor antagonists, antacids, and others
such antibiotics or miscellaneous drugs. Antiemetic drugs are the medications
used for management of nausea and vomiting. Dehydration can be prevented
or managed using either oral rehydration salts which are prepared solutions
administered orally or intravenous fluids. Antispasmodic dugs are medications
used in the management of different categories of visceral pain, including the pain
of gastrointestinal tract such as the pain in intestines or stomach. Finally, laxatives
are used to stimulate or facilitate evacuation of the bowels, for example in a caseof constipation.
Self assessment 2.1
A 30-year-old female patient consults a health facility where you are placed in
the clinical attachment with complaints of epigastric pain. She also complains of
nausea and vomiting associated with diarrhea. On the arrival, you find that the
patient has lost fluids, and requires intravenous fluids. Your colleague needs you
to advise him on the medications you may use to manage his pain and vomiting.
1. Which of the following classes of drugs you think may help for this patient on
pain relief?
A. Antispasmodics
B. Antiemetics
C. Laxative drugs
D. Antiulcer drugs
2. Which of the following categories of drugs you think may be helpful for this
patient?
A. Antispasmodics and Laxative drugs
B. Laxative drugs and Antiemetics
C. Antiulcer drugs and Laxative drugs
D. Antiemetics and Antispasmodics
3. Your colleague attempts to administer a laxative to the patient but needs toget your view about this decision. What can you advise him/her?
2.2. Introduction to drugs for gastritis and peptic ulcer disease
Learning Activity 2.2
Mr. MM is a middle age man who likes smoking 15 cigarettes per day. He has
history of arthritis, and for this, he used to take frequently diclofenac over the
counter to relieve his pain. Since last week, he started complaining of moderate
to severe epigastric pain and sometimes he vomits and has heartburn. Today,
he went to the pharmacy to buy medications and the pharmacist advised him to
consult the facility as he suspects Mr. MM to have peptic ulcer disease.
Using library textbooks and/internet respond to the following questions:
1. What are the risk factors for peptic ulcer diseases?
2. If you were assigned to treat that patient, suggest 4 main classes of drugs
to use in peptic ulcers with a short description of mechanism of action foreach.
CONTENT SUMMARY
An ulcer is an erosion of the gastrointestinal mucosa. It is always associated with
inflammation of the affected part. Although ulcers may occur in any portion of the
alimentary canal, the duodenum is the most common site. The term peptic ulcer is
specific to the lesion located in either the stomach that is named gastric ulcer orsmall intestine which is the duodenal ulcer.
The risk factors for developing peptic ulcers (PUD) are many and include close
family history of PUD, blood group (persons with blood group O were found at higher
risk), smoking tobacco because it leads to an increase of gastric acid secretion,
consuming the beverages and food that contain caffeine and or other irritant like
spices. Consuming some drugs expose to peptic ulcer diseases. Those drugs
are corticosteroids, nonsteroidal anti-inflammatory drugs ibuprofen for example
that causes direct cellular damage to GI mucosal cells and a reduced secretion
of protective mucus and bicarbonate ion, platelet inhibitors such as aspirin also
increase risk to PUD. In addition to that, excessive psychological stress, as well asinfection with Helicobacter pylori are the risk factors to peptic ulcer diseases.
The primary cause of PUD is infection by the gram-negative bacterium Helicobacter
pylori. Different clinical studies and research have revealed that, approximately
50% of the population has H. pylori present in their stomach and proximal small
intestine. The NSAIDs and H. pylori infection act synergistically to promote ulcers.Their combination poses a 3.5 times greater risk of ulcers than either factor alone.
The characteristic symptoms of duodenal ulcer are an aggravating or burning
upper abdominal pain that occurs 1 to3 hours after a meal. The pain is worse when
the stomach is empty and often disappears on ingestion of food. Night-time pain,
nausea, and vomiting are uncommon. If the erosion progresses deeper into the
mucosa, bleeding occurs, which may be evident as either bright red blood in vomit
or black, tarry stools. In general, most of duodenal ulcers heal spontaneously eventhough they frequently recur after months of remission.
Gastric ulcers are less common than the duodenal type and have different
symptoms. Although relieved by food, pain may continue even after a meal.
Loss of appetite, weight loss and vomiting are more common. Remissions may
be uncommon or absent. Medical follow-up of gastric ulcers should continue for
several years, because a small percentage of the erosions become cancerous.
The most severe ulcers may penetrate the wall of the stomach and cause death.
Whereas duodenal ulcers occur most frequently in males in the 30- to 50-year age
group, gastric ulcers are more common in women over age 60. The nonsteroidal
anti-inflammatory drugs related ulcers are more likely to produce gastric ulcers,
whereas H. pylori associated ulcers are more likely to be duodenal. Ulceration in
the distal small intestine is known as Crohn’s disease, and erosions in the large
intestine are called ulcerative colitis. These diseases, together categorized asinflammatory bowel disease.
Pharmacotherapy is not the first option in treating peptic ulcers and gastritis unless
the patient has helicobacter pylori infection. Before initiating drugs, the patients are
usually advised to change lifestyle factors contributing to the severity of PUD. It is
necessary to quit smoking, avoid alcohol consumption, stress reduction or completely
avoid it, avoid or limit some foods then all these measures will allow healing of ulcer
enhance it to go to. For patients who are taking NSAIDs, the initial approach to PUD
is to switch the patient to an alternative medication, such as acetaminophen or a
selective COX-2 inhibitor. This is not always possible, because NSAIDs are drugs
of choice for treating chronic arthritis and other disorders associated with pain and
inflammation. If discontinuation of the NSAID is not possible, or if symptoms persistafter the NSAID has been withdrawn, antiulcer medications are indicated.
For patients with PUD who are infected with H. pylori, elimination of the bacteria
using anti-infective therapy is the primary goal of pharmacotherapy. If the treatment
includes only antiulcer drugs without eradicating H. pylori, a very high recurrence
rate of PUD is observed. It has also been found that eradicating H. pylori
infection prophylactically decreases the incidence of peptic ulcers in patients whosubsequently take NSAIDs.
The goals of drug therapy for PUD pharmacotherapy are to provide immediate
relief from symptoms, promote healing of the ulcer, and prevent future recurrence
of the disease. Drugs for PUD are available both as on prescription and OTC drugs
are available.
The primary classes of drugs used to treat peptic ulcer diseases are:
– Proton pump inhibitors.
– H2-receptor antagonists.
– Antacids.
– Miscellaneous drugs.– Antibiotics.
Figure: Brief description on mechanism of action for main drugs for gastritis and peptic ulcerdisease.
Self assessment 2.2
An adult male patient consults the health facility where you are carrying out the
clinical attachment complaining of epigastric pain and vomiting up blood. In the
history taking, he tells you that he has been diagnosed with a gastric ulcer at
a referral hospital. He also complains of chronic arthritis that is managed with
over-the-counter pain medications.
1. Which of the following classes of drugs would you advise the client to take
with caution in order to prevent worsening the peptic ulcer disease?
A. Proton pump inhibitors
B. Antacid medications
C. NSAIDs such as diclofenac
D. H2-receptor antagonists.
2. Which of the following classes of drugs used in Peptic ulcer disease
management eradicate the Helicobacter pylori?
A. Proton pump inhibitors
B. Antibiotic medications
C. Antacid medications
D. H2-receptor antagonists.
3. Using antiulcer drugs alone suffices to cure peptic ulcer disease induced by
Helicobacter pylori. TRUE or FALSE
2.3. Proton pump inhibitors and H2-receptor antagonistsLearning Activity 2.3
The patient consulted the health facility after the symptoms of epigastric pain. In
history taking, the patient told you that he received cimetidine which did not help.
The investigations done at a teaching hospital confirmed excessive secretion of
gastric acid, and the specialist confirmed the peptic ulcer disease. The specialisttook a decision to switch to omeprazole which finally improved the client’s state.
Using library textbooks or internet, respond to the following questions
1. In which class of antiulcer drugs does cimetidine belong?
2. In which class of antiulcer drugs does omeprazole belong?
3. What are the indications of cimetidine?4. Identify the side effects of omeprazole?
CONTENT SUMMARY
The proton pump inhibitors (PPIs) are the commonly drugs used to treat
peptic ulcer diseases. They act by blocking the enzyme responsible for secreting
hydrochloric acid in the stomach. They are drugs of choice for the short-term therapy
of PUD. Proton pump inhibitors (PPIs) reduce acid secretion in the stomach by
binding irreversibly to H+, ATPase, the enzyme that acts as a pump to release acid
(also called H+, or protons) onto the surface of the GI mucosa. The PPIs reduce
acid secretion to a greater extent than the H2-receptor antagonists and have a
longer duration of action. PPIs heal more than 90% of duodenal ulcers within 4
weeks and about 90% of gastric ulcers in 6 to 8 weeks.
Several days of PPI therapy may be needed before patients gain relief from ulcer
pain. Beneficial effects continue for 3 to 5 days after the drugs have been stopped.
These drugs are used only for the short-term control of peptic ulcers. The typical
length of therapy is 4 weeks.
Among them we have Omeprazole and lansoprazole that are used concurrently
with antibiotics to eradicate H. pylori. Esomeprazole (Nexium) and pantoprazole(protonix) offer the convenience of once-a-day dosing.
Omeprazole is a widely used proton pump inhibitor. It was the first PPI to be
approved for PUD and it is available for both prescription and OTC forms. It reduces
acid secretion in the stomach by binding irreversibly to the enzyme H+, K+-ATPase.
Although this drug can take 2 hours to reach therapeutic levels, its effects last upto 72 hours.
Omeprazole is used for the short-term, 4- to 8-week therapy of active peptic
ulcers. Most patients are symptom free after 2 weeks of therapy. It is used for
longer periods in patients who have chronic hypersecretion of gastric acid, a
condition known as Zollinger–Ellison syndrome. It is the most effective drug for
this syndrome. Omeprazole is available only in oral form whereas in combination
with antacid bicarbonates, it is called Zegerid. If possible, it is better to administer it
before breakfast on an empty stomach. It may be administered with antacids. It isavailable as capsules or tablets should not be chewed, divided, or crushed.
It is pregnancy category C drug.
Adverse effects of omeprazole are generally minor and include headache, nausea,
diarrhea, rash, and abdominal pain. Although rare, blood disorders may occur,
causing unusual fatigue and weakness. Therapy is generally limited to 2 months.
Atrophic gastritis and hypomagnesaemia have been reported rarely with prolongedtreatment with PPIs.
Omeprazole interacts with other drugs, affect laboratory investigations’ results.When administered concurrently with diazepam, phenytoin, and central nervous
system (CNS) depressants may cause increased blood levels of these drugs.
Concurrent use with warfarin may increase the likelihood of bleeding; alcohol can
aggravate the stomach mucosa and decrease the effectiveness of omeprazole.
Omeprazole may increase values for ALT, AST, and serum alkaline phosphatase.There is no specific treatment for overdose for omeprazole
H2-RECEPTOR ANTAGONISTS: The discovery of the H2-receptor antagonists
in the 1970s marked a major breakthrough in the treatment of PUD. Since their
discovery, they are available as OTC and are widely used in the treatment of
hyperacidity disorders of the GI tract. Histamine has two types of receptors, H1 and
H2. Activation of H1 receptors produces the classic symptoms of inflammation and
allergy, whereas the H2 receptors are responsible for increasing acid secretion in
the stomach. The H2-receptorantagonists are effective at suppressing the volumeand acidity of parietal cell secretions. Duodenal ulcers usually heal in 6 to 8 weeks,
and gastric ulcers may require up to 12 weeks of therapy. All of the H2-receptor
antagonists are available the outer of the counter for the short-term 2 weekstreatment of gastro esophageal reflux (GERD).
All H2-receptor antagonists have similar safety profiles: Adverse effects are minor
and rarely cause discontinuation of therapy. Patients, who are taking high doses,
or those with renal or hepatic disease, may experience confusion, restlessness,hallucinations, or depression.
Cimetidine (Tagamet) is used less frequently than other H2-receptor antagonists
because of numerous drug–drug interactions that commonly lead to inhibition of
hepatic drug-metabolizing enzymes and because it must be taken up to four times
a day. Antacids should not be taken at the same time because the absorption of the
H2-receptor antagonist will be diminished. All H2-receptor antagonists have similarsafety profiles.
Cimetidine is indicated for the treatment and prevention of recurrence of duodenal
ulcer, the treatment of active and benign gastric ulcer. It is also used to manage
gastroesophageal reflux disease, to treat pathological hypersecretory conditions,
such as Zollinger-Ellison syndrome and to prevent stress-related upper GI bleedingduring hospitalization
Adverse effects are minor and rarely cause discontinuation of therapy. Patients
who are taking high doses, or those with renal or hepatic disease, may experienceconfusion, restlessness, hallucinations, or depression.
Ranitidine or zantac is a commonly used H2-Receptor antagonist. Ranitidine acts
by blocking H2 receptors in the stomach to decrease acid production. It has a higher
potency than cimetidine, which allows it to be administered once daily, usually at
bedtime. Adequate healing of the ulcer takes approximately 4 to 8 weeks, although
those at high risk for PUD may continue on drug maintenance for prolonged periods
to prevent recurrence. Gastric ulcers require longer therapy for healing to occur.
Intravenous (IV) and intramuscular (IM) forms are available for the treatment of
acute, stress-induced bleeding ulcers. Tritec is a combination drug with ranitidine
and bismuth citrate. Ranitidine is available in a dissolving tablet form (EFFER dose)
for treating GERD in children and infants older than 1 month of age. Administerafter meals and monitor liver and renal function.
Ranitidine does not cross the blood–brain barrier to any appreciable extent, so
it does not cause the confusion and CNS depression observed with cimetidine.
Although rare, severe reductions in the number of red and white blood cells and
platelets are possible; thus, periodic blood counts may be performed. High dosesmay result in impotence or loss of libido in men. It is a pregnancy category B drug.
Contraindications include hypersensitivity to H2-receptor antagonists, acuteporphyria, and OTC administration in children less than 12 years of age.
Drug–Drug Interactions: Ranitidine has fewer drug–drug interactions than
cimetidine. Ranitidine may reduce the absorption of cefpodoxime, ketoconazole, and
itraconazole. Antacids should not be given within 1 hour of H2-receptor antagonistsbecause the effectiveness may be decreased due to reduced absorption.
Smoking decreases the effectiveness of ranitidine. For the laboratory tests, ranitidine
may increase the values of serum creatinine, AST, ALT, LDH, alkaline phosphatase
and bilirubin. It may produce false positives for urine protein. With herbal and food
absorption of vitamin B12 depends on an acidic environment; thus, deficiency mayoccur. Iron is also better absorbed in an acidic environment.
Cimetidine forms:
Tables 2.2 H2-Receptor Antagonists:
Self assessment 2.3
1. Ranitidine is one of the drugs used in the management of peptic ulcer
diseases, and it belongs to the class of H2-receptor antagonists. TRUE or
FALSE
2. The proton pump inhibitors reduce acid secretion to a lesser extent than
the H2-receptor antagonists and have a shorter duration of action. TRUE or
FALSE
3. What is an ideal duration for using omeprazole in short-term management 4
of active peptic ulcers?
A. Two to three weeks
B. Four to eight weeks
C. One to three weeks
D. Three to eight weeks4. What are the adverse effects of cimetidine when taken at high doses?
2.4. Antacid drugs
Learning Activity 2.4
An associate nurse student in the clinical attachment approaches the nurse
seeking for advice on how to manage a patient who is complaining of mild
epigastric pain and heartburn for 3 days. The nurse instructs the student to
give an antacid drug (Aluminium hydroxide). In addition, the nurse instructs the
student to educate the patient to take the prescribed drug at least 2 hours before
or after other drugs he/she is taking.
1. What is the rationale for this interval in taking other drugs with antacid?
2. Due to their acidic properties, the antacids neutralize acid in the stomach.
TRUE or FALSE
3. Combining aluminium compounds with magnesium increases theireffectiveness and reduces the potential for constipation. TRUE or FALSE
CONTENT SUMMARY
Antacids are alkaline substances that are used to neutralize stomach acid.
They provide temporary relief from heartburn or indigestion and for this they are
sometimes also called anti-heartburn drugs, but they do not promote healing of
the ulcer, nor do they help to eradicate H. pylori. The anti-acid drugs are alkaline,
inorganic compounds of aluminum, magnesium, sodium, or calcium. Combinations
of aluminum hydroxide and magnesium hydroxide, the most common type,
are capable of rapidly neutralizing stomach acid. Chewable tablets and liquid
formulations are available.
A few products combine antacids and H2-receptor blockers into a single tablet;
for example, Pepcid Complete contains calcium carbonate, magnesium hydroxide,
and famotidine. Simethicone is sometimes added to antacid preparations, because
it reduces gas bubbles that cause bloating and discomfort. For example, Mylanta
contains simethicone, aluminum hydroxide, and magnesium hydroxide. Simethicone
is classified as an antiflatulent, because it reduces gas. It also is available by itselfin OTC products such as Gas-X and Mylanta Gas.
Aluminium hydroxide is an inorganic agent used alone or in combination with
other antacids. Combining aluminium compounds with magnesium (Gaviscon,
Maalox, and Mylanta) increases their effectiveness and reduces the potential for
constipation. Unlike calcium-based antacids that can be absorbed and cause
systemic effects, aluminium compounds are minimally absorbed. Their primaryaction is to neutralize stomach acid by raising the pH of the stomach contents.
Unlike H2-receptor antagonists and PPIs, aluminium antacids do not reduce the
volume of acid secretion. They are most effectively used in combination with other
antiulcer drugs for the symptomatic relief of heartburn due to PUD or GERD. A
second aluminium salt, aluminium carbonate (Basaljel), is also available to treatheartburn.
The available forms are:
Aluminium compounds should not be taken at the same time as other medications,
because they may interfere with absorption. Use with sodium polystyrene sulfonate
may cause systemic alkalosis. When this drug is administered some lab tests may
vary. For example, the values for serum gastrin and urinary pH may increase. Serum
phosphate values may decrease. About food and herbal interaction, aluminium
antacids may inhibit the absorption of dietary iron. There is no specific treatment for
overdose for hydroxide aluminium.
When taken regularly or in high doses, aluminium antacids cause constipation.
At high doses, aluminium products bind with phosphate in the GI tract and longterm
use can result in phosphate depletion. Those at risk include those who aremalnourished, alcoholics, and those with renal disease.
This drug is not indicated for patients with suspected bowel obstruction. Precaution
should be taken while administering antacid. Administer aluminium antacids at least
2 hours before or after other drugs because absorption could be affected. They arepregnancy category C.
Tables 2.3 ANTACID DRUGS:
ANTACIDS FORMS:
Self assessment 2.4
1. Antacids are alkaline substances that are effective in eradication of Helicobacter
pylori. TRUE or FALSE
2. All the following statements best describes the effects of antacids, EXCEPT:
C. They are used to neutralize stomach acid
D. They provide relief from indigestion
E. They provide relief from heartburn
F. They promote healing of the peptic ulcer
3. Which of the following is the primary action of Aluminium hydroxide?
A. To neutralize stomach acid by raising the pH of the stomach contents.
B. To neutralize stomach acid by decreasing the pH of the stomach contents.
C. To neutralize stomach acid by decreasing reducing the volume of acid
secretion.D. To neutralize stomach acid by increasing reducing the volume of acid
2.5. Other drugs used to manage gastritis and peptic ulcer disease(Miscellaneous drugs and antibiotics)
Learning Activity 2.5
A university student in management who has been treated for peptic ulcer disease
curiously wanted to discuss with a nurse about her treatment. She said that she had used
antiulcer drugs specifically proton pump inhibitors, H2-receptors antagonist, antacids
drugs. She added that, currently her friend told her that she can even use misoprostol
and different antibiotics but when she did a Google search, she found that misoprostol
is for inducing uterine contractions, and the antibiotics have other numerous indications.
Bringing her laboratory results, the nurse found that the student was tested positive for
helicobacter pylori. Now, she is worried about the treatment she will receive today after
all investigations.
Using Library textbooks/internet explain the following
1. What is the mechanism of action of misoprostol in the treatment of peptic ulcer
diseases?
2. Give one example of antibiotic used in the management of peptic ulcer disease.
3. Which properties does bismuth have to exert effect against helicobacter pyloriwhen administered?
CONTENT SUMMARY
MISCELLANEOUS DRUGS FOR PUD
Prostaglandin Analogues
Misoprostol is a synthetic analogue of prostaglandin E1 which inhibits gastric acid
secretion, causes vasodilatation in the submucosa and stimulates the production
of protective mucus.
Indications
Even though it is used some times to terminate the pregnancy, misoprostol (Cytotec)
inhibits gastric acid secretion and stimulates the production of protective mucus. Its
primary use is for the prevention of peptic ulcers in patients who are taking high
doses of NSAIDS or corticosteroids.
The purpose of its use is to enhance the healing of duodenal ulcer and gastric ulcer,
including those induced by NSAIDs and as prophylaxis of gastric and duodenal
ulceration in patients on NSAID therapy.
Side effects
The side effects of cytotec are diarrhea, abdominal pain, nausea and vomiting,
dyspepsia, flatulence, abnormal vaginal bleeding, rashes and dizziness. It is apregnancy X drug. Misoprostol is available in tablet forms
Figure 2.5.1 Misoprostol tablet forms
Bismuth Chelate
Mechanism of action
Bismuth chelate is a colloidal tripotassium dicitratobismuthate that precipitates at
acid PH to form a layer over the mucosal surface and ulcer base, where it combines
with the proteins of the ulcer exudate. This coat is protective against acid and pepsin
digestion. It also stimulates mucus production and may chelate with pepsin, thus
speeding ulcer healing. Several studies have shown it to be as active as cimetidine
in the healing o duodenal and gastric ulcers after four to eight weeks of treatment. It
has a direct toxic effect on H. pylori.
Indications
It is used as part of triple therapy in the treatment of peptic ulcer diseases associated
with helicobacter pylori.
Bismuth chelate elixir is given diluted with water 30 minutes before meals and two
hours after the last meal of the day. This liquid has an ammoniacal, metallic taste
and odour which is unacceptable to some patients and chewable tablets can be
used instead. Antacids or milk should not be taken concurrently. Ranitidine bismuth
citrate tablets are also available for the treatment of peptic ulcers and for use in H.
pylori eradication regimes.
Adverse effects
The adverse effects include blackening of the tongue, teeth and stools causing
potential confusion with melaena and nausea. Bismuth is potentially neurotoxic.
Urine bismuth levels rise with increasing oral dosage, indicating some intestinal
absorption. Although with normal doses the blood concentration remains well below
the toxic threshold.Contraindication: It should not be used in renal failure

Figure 2.5.2 Forms of Bismuth
Antibiotics Used to Treat PUD
Peptic ulcer diseases have many risk factors and cause. Helicobacter pylori; a
gram-negative bacterium is associate with duodenal ulcer in 80% of patient and
70% of patients with gastric ulcer. If not well eradicated, it is strongly associated
with gastric cancer. This explains the magnitude of several antibiotic use’s inpatient
with peptic ulcer diseases. This bacterium has adapted well as human pathogen by
creating ways to neutralize the high acidity of its surrounding by making adhesion
which is a substance that allows the bacterium to stick tightly to the mucosa of the
GI. The infecting bacterium can remain active for life if not treated appropriately.
Elimination of this organism allows ulcers to heal more rapidly and remain in
remission longer. Because acid-reducing drugs have little or no effect of H. pylori,antibiotics must be used to eliminate the bacterium
A combination of antibiotics is used concurrently to eradicate H. pylori. Once
eliminated from the stomach, reinfection with H. pylori is uncommon. Those with
peptic ulcers who are not infected with H. pylori should not receive antibiotics
because it has been shown that these patients have a worse outcome if they
receive H. pylori treatment. Thus, patients should be tested for H. pylori before
initiating treatment for infection.
Two or more antibiotics are given concurrently to increase the effectiveness of
therapy and to lower the potential for bacterial resistance. The antibiotics are also
combined with a PPI or an H2-receptor antagonist. Bismuth compounds (Pepto-
Bismol, Tritec) are sometimes added to the antibiotic regimen. Although technically
not antibiotics, bismuth compounds inhibit bacterial growth and prevent H. pylori
from adhering to the gastric mucosa. Antibiotic therapy generally continues for 7 to14 days.
Drugs used to eradicate helicobacter pylori
The presence of the bacterium helicobacter pylori is a major causative factor
in the aetiology of peptic ulcer disease. The incidence of H. pylori infection in
patients with gastric ulcer approaches 100%. The strongest evidence of a causal
relationship between H. pylori and peptic ulcer disease is the marked reduction
in ulcer recurrence and complications following successful eradication of the
organism. It has been shown that the speed of ulcer healing obtained with acidsuppressing
agents is accelerated if H. pylori eradication is achieved concomitantly.
Eradication of H. pylori infection prior to the commencement of NSAID therapy
reduces the occurrence of gastro- duodenal ulcers in patients who have not had
previous exposure to NSAIDs. H. pylori appears to be associated with increased risk
of gastric cancer of the corpus. For these reasons, it is very important to eradicatethat pathogen.
In eradication of that pathogen, Amoxicillin, clarithromycin are the commons
antibiotics used in combination for tritherapy or Quadritherapy. A combination of 3
drugs called tritherapy or 4 drugs known as Quadritherapy is necessary. TheFollowing are possible combination:
First line: Tri-therapy
PPI+ clarithromycin+ metronidazole
PPI+ amoxicillin+ Tinidazole
Anti H2+ Clarithromycin +amoxicillinAnti H2+ Amoxicillin+ metronidazole
Examples:
1. Bismuth + metronidazole+ amoxicillin for two weeks. This combination has a
success rate of 70-80%.
2. Omeprazole 20mg bid (on empty stomach) + metronidazole 500mg at the
end of the meal+ clarithromycin 500mg for one week. This combination has a
success rate of 95-100%.
Second line: Quadritherapy
Tritherapy + misoprostol (cytotec) or add bismuth to tritherapy
Note: For persons with penicillin intolerance, tetracycline should be used in placeof tetracycline.
Non pharmacological management:
In addition to pharmacological management, it is important to educate the patient
about hygienodietetic measures of ulcer prevention and enhancement for healing.
It is recommended to consume milk as it contains calcium and avoid some food
like cabbages, sombe, and spicy foods as well as quit smoking and avoid alcoholconsumption.
Self assessment 2.5
1. One of the following antibiotics is included in tritherapy for eradication of
helicobacter pylori.
A. Cotrimoxazole
B. Doxycycline
C. Amoxicillin
D. Ampicillin
2. Which of the following is a side effect of bismuth chelate?
A. Neurotoxicity
B. Dyspepsia
C. Flatulence
D. Vaginal bleeding
3. Which statement is true about misoprostol?
A. Is diluted with water and taken 30 minutes before meals
B. Inhibits gastric acid secretion
C. It is a pregnancy B category drug
D. It should be part of quadritherapy for H. pylori eradication4. List 4 drugs used in the quadritherapy for Helicobacter pylori eradication
2.6. Antiemetic drugs
Learning Activity 2.6
In this morning you receive a patient in the health clinic where you are in the
clinical attachment. The patient complains of vomiting after each meal for the
last 3 days.
1. How can define an antiemetic drug?
2. Using library and internet, identify 2 drugs that should be given to the patient
to reduce or stop vomiting.3. What are the classes of antiemetic drugs?
CONTENT SUMMARY:
Antiemetic are drugs for treating or preventing nausea and vomiting. Their
mechanism of action is of inhibiting dopamine or serotonin receptors in the brain.
Nausea is an unpleasant, subjective sensation that is accompanied by weakness,
diaphoresis, and hyperproduction of saliva. It is sometimes accompanied by
dizziness. Intense nausea often leads to vomiting, or emesis. Vomiting is a
defense mechanism used by the body to clear itself of toxic substances. Vomiting
is a reflex primarily controlled by the vomiting center of the medulla of the brain,
which receives sensory signals from the digestive tract, the inner ear, and the
chemoreceptor trigger zone (CTZ) in the cerebral cortex.
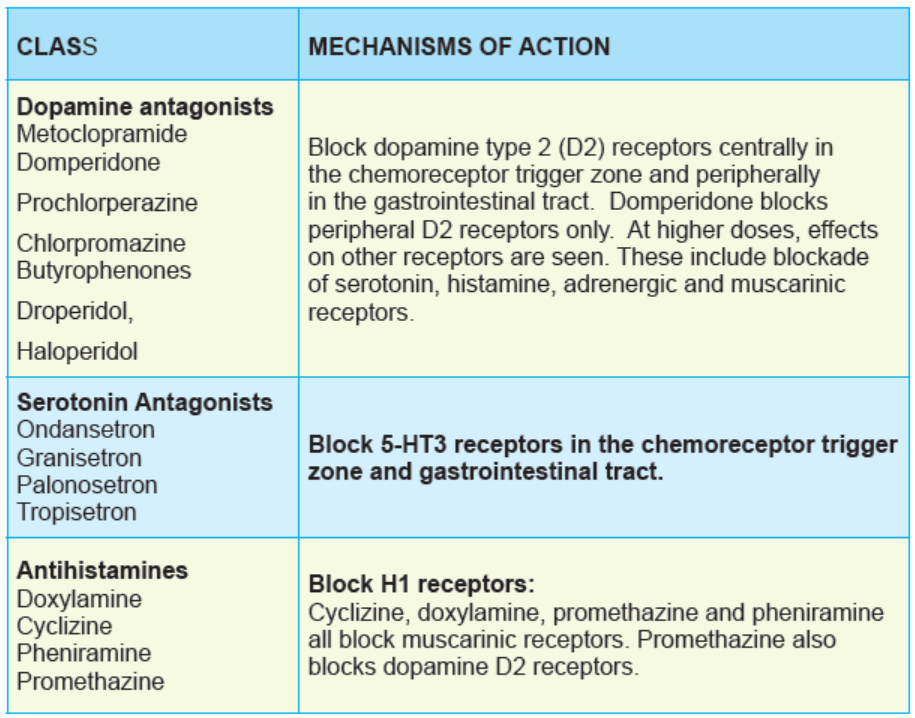
The various classes of antiemetics target different pro-emetic pathways to alleviate
nausea and vomiting. Some target more than one pathway. The classes of
antiemetics include antagonists of dopamine, serotonin, neurokinin, histamine
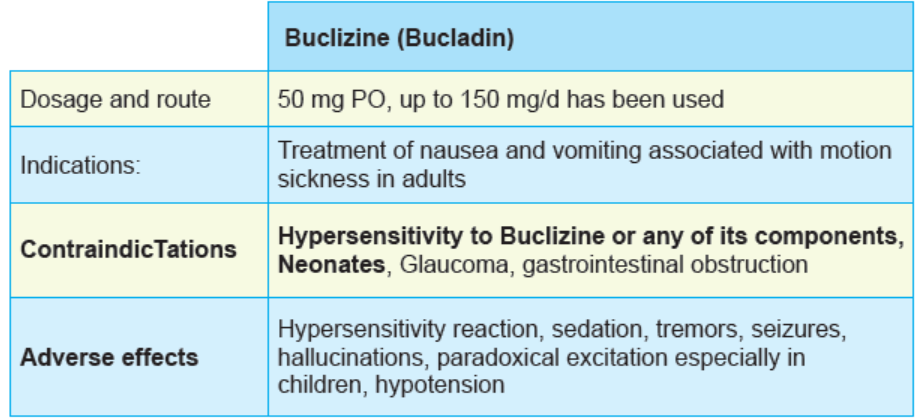
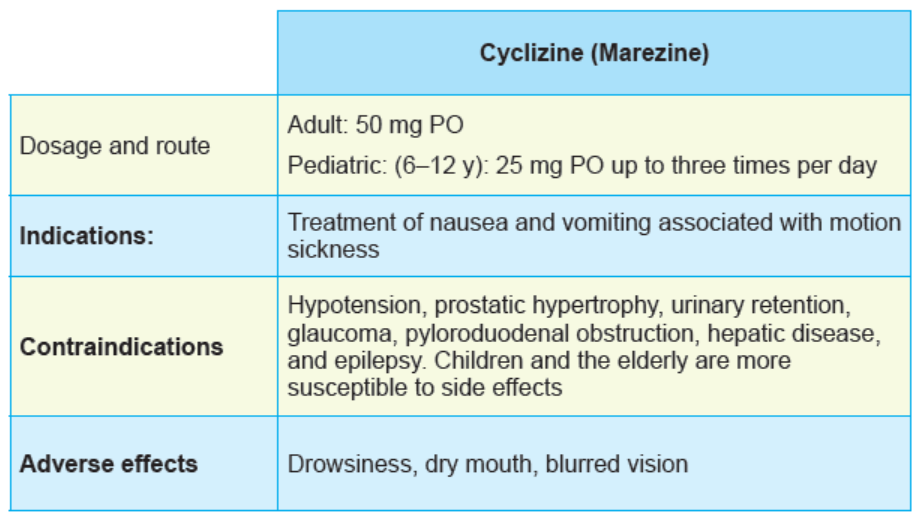
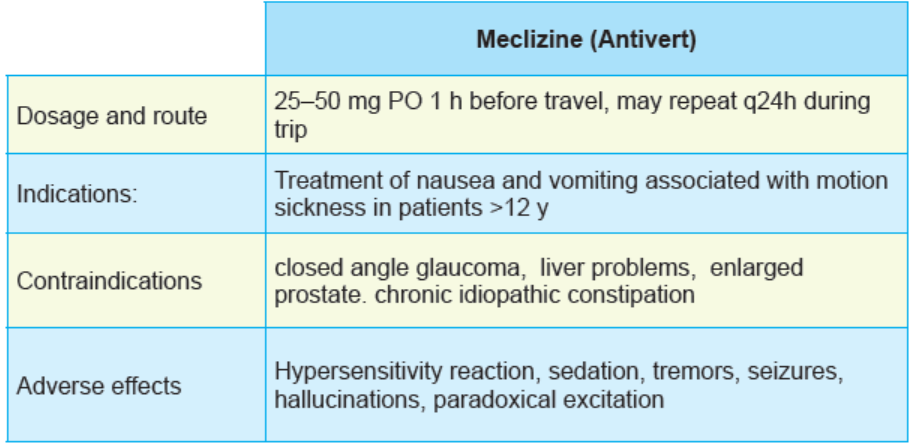
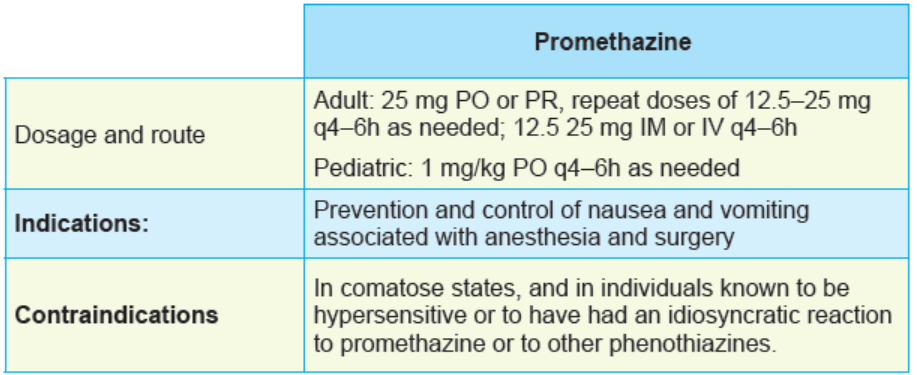
and acetylcholine, as summarized in table 1 below:Table 2. 6.1: Antiemetic drugs
Tables 2. 6. 2. Summary of Serotonin (5-HT3) blockers:
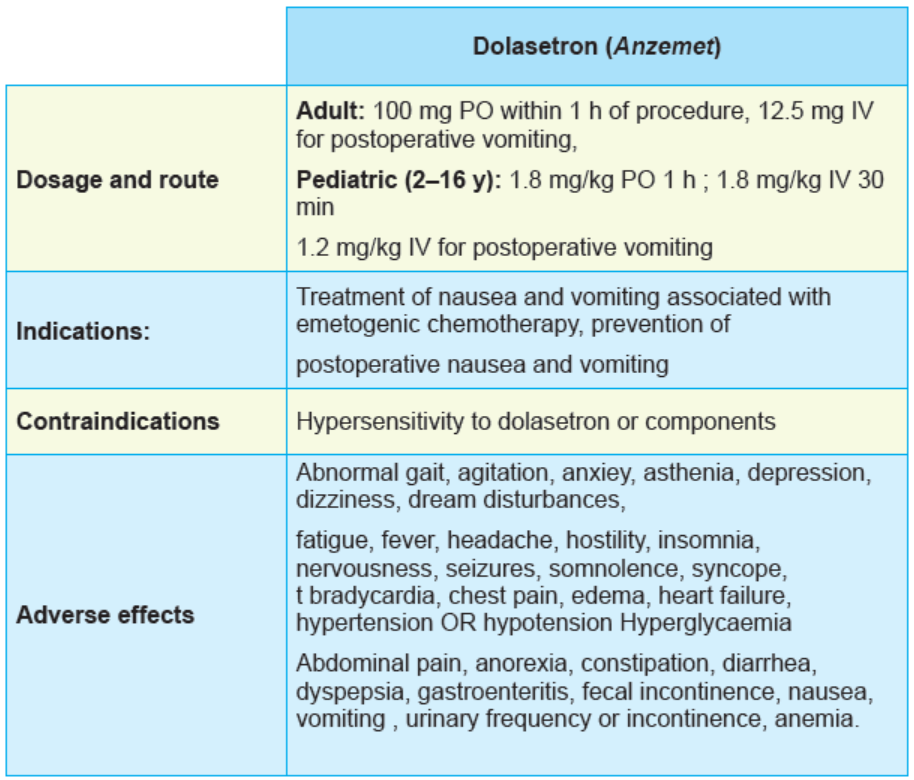
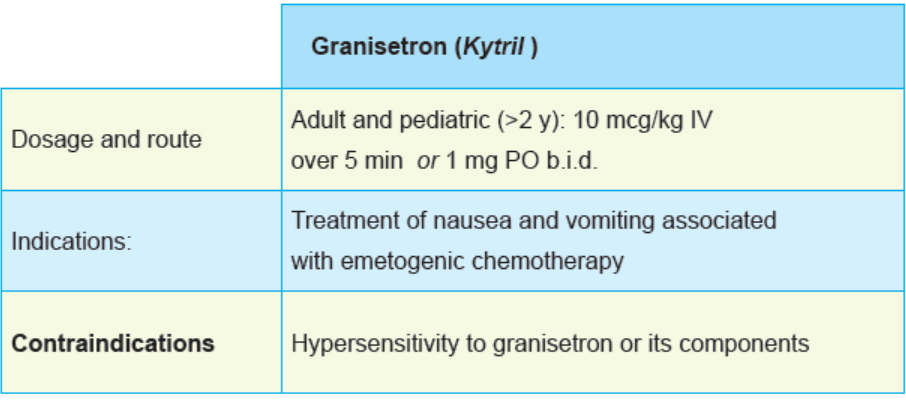
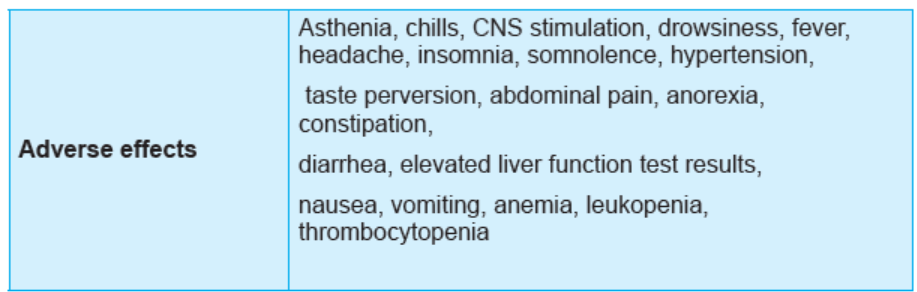
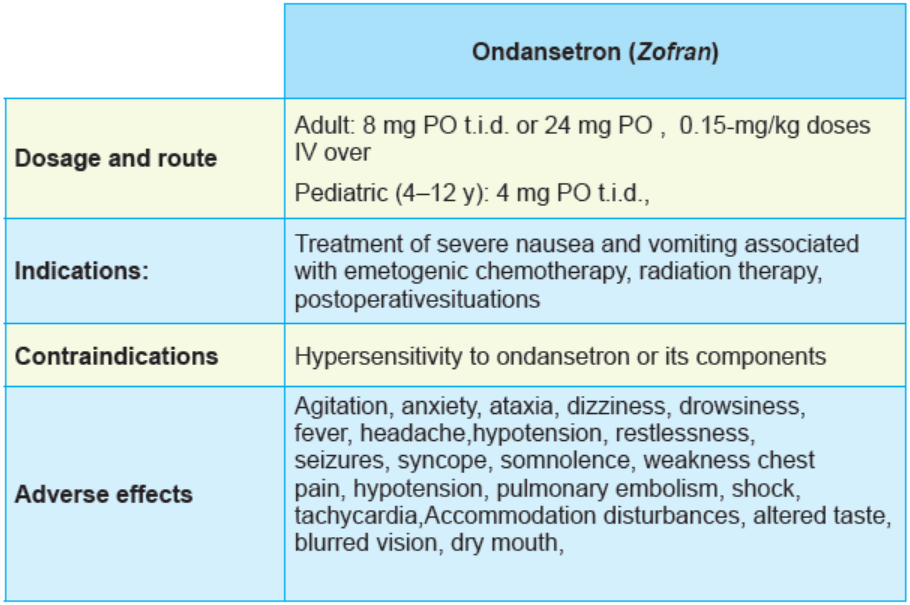
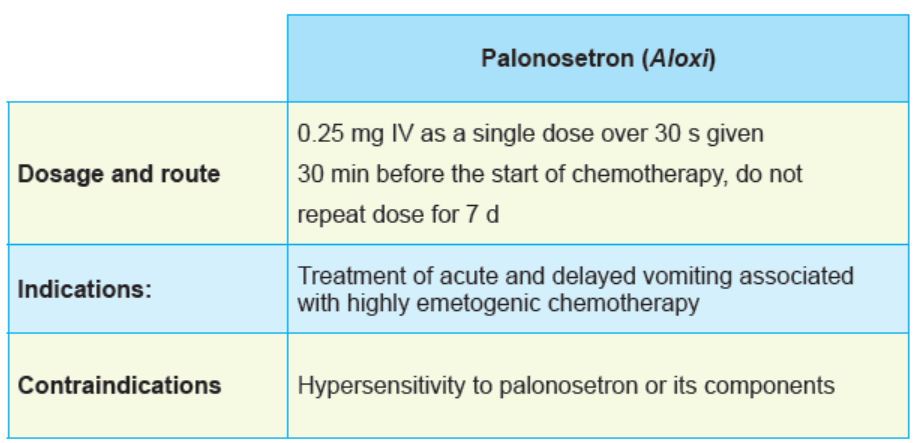
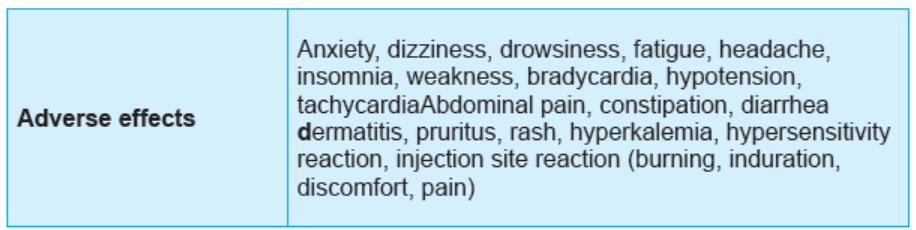

Figure 2.6.1 Serotonin (5-HT3) blockers forms
Tables 2. 6. 3. Summary of Dopamine antagonists:
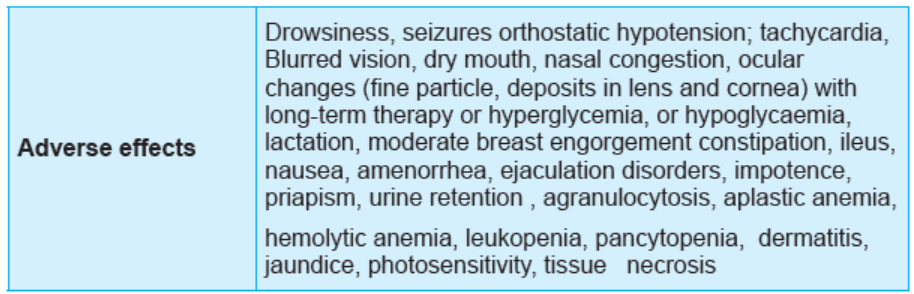
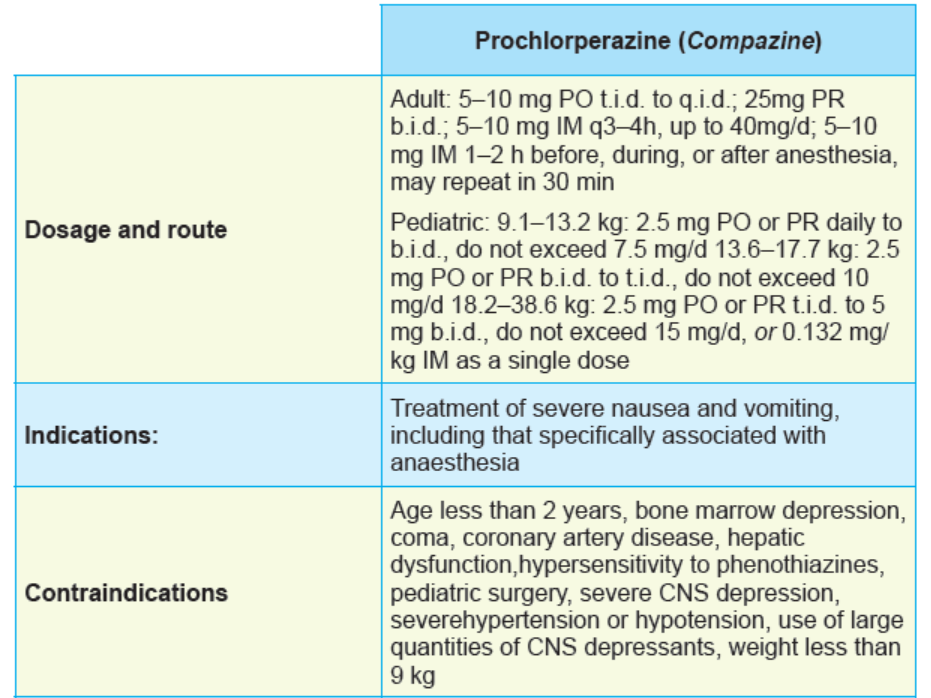
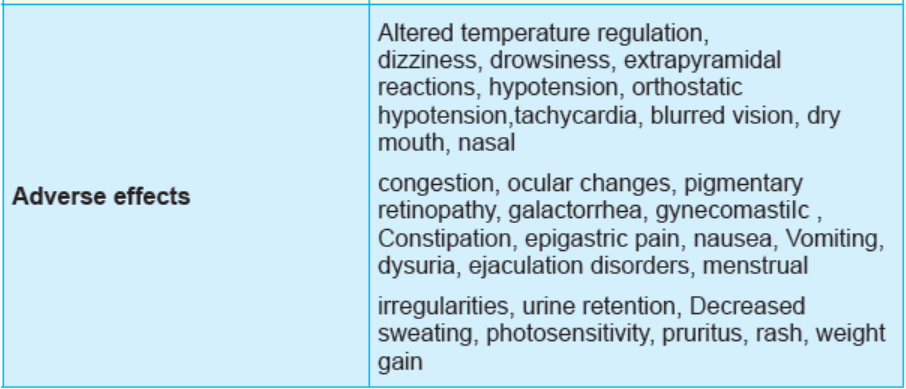

Figure 2.6.1: Dopamine antagonists
Table 2. 7. Anticholinergics/antihistamine antiemetics:
Self assessment 2.6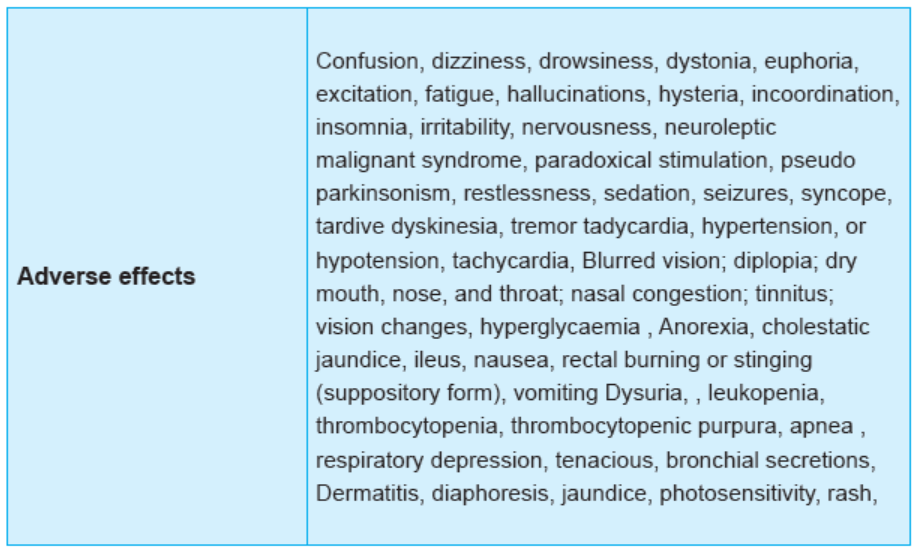
1. Which of the following antiemetic drugs is classified in antihistamine
antiemetics?
A. Promethazine
B. Chlorpromazine
C. Ondansetron
D. Metoclopramide
2. Which of the following antiemetic drugs is classified in serotonin (5-HT3)
blockers?
A. Promethazine
B. Chlorpromazine
C. Ondansetron
D. Metoclopramide
3. State the contraindications of chlorpromazine.
2.7. Laxative drugs
Learning Activity 2.7
As an associate nurse student in the clinical attachment, you receive a patient
complaining of difficulty passing stool. In your assessment, you realize that
the patient usually has a sedentary life and drinks fluids less frequently. You
diagnose the condition to be constipation, and you wish to administer drugs that
increase bowel movements.
1. How do we call a broad class of medications that increase bowel movements
such as in case of constipation?
2. List the categories of drugs used to treat constipation, and give one examplefor reach category.
CONTENT SUMMARY
Laxatives are drugs that promote bowel movements. Laxatives promote the
evacuation of the bowel, or defecation, and are widely used to prevent and treat
constipation. Indications for laxative include either the prophylaxis of constipation
or treatment of chronic constipation. Prophylactic laxative pharmacotherapy is
appropriate following abdominal surgeries. Such treatment reduces straining or
bearing down during defecation a situation that has the potential to precipitate
increased intra-abdominal, intraocular, or blood pressure. Prophylactic laxative
therapy may be initiated in pregnant women, patients and iron supplements are
just some of the medications that promote constipation. Foods that can cause
constipation include alcoholic beverages, products with a high content of refinedwhite flour, dairy products, and chocolate.
In addition, certain diseases such as hypothyroidism, diabetes, and irritable bowel
syndrome (IBS) can cause constipation. The normal frequency of bowel movements
varies widely among individuals, from two to three per day, to as few as one per
week. Constipation occurs more frequently in older adults, because faecal transit
time through the colon slows with aging; this population also exercises less and has
a higher frequency of chronic disorders that cause constipation.
All patients should understand that variations in frequency are normal, and that a
daily bowel movement is not a requirement for good health. Occasional constipation
is self-limiting and does not require drug therapy. Lifestyle modifications that
incorporate increased dietary fibers, fluid intake, and physical activity should beconsidered before drugs are used for constipation.
Chronic, infrequent, and painful bowel movements, accompanied by severe
straining, may justify initiation of treatment. In its most severe form, constipation
can lead to a fecal impaction and complete obstruction of the bowel for people who
are unable to exercise, or patients who are taking drugs that are known to causeconstipation.
The most common use for laxatives is to treat simple, chronic constipation.
Occasionally, laxatives are administered to accelerate the movement of ingested
toxins following poisoning or to remove dead parasites in the intestinal tract following
anthelminthic therapy. In addition, laxatives are often given to cleanse the bowel
prior to diagnostic or surgical procedures of the colon or genitourinary tract. Themain classes are chemical stimulants, bulk stimulants and lubricants.
CHEMICAL STIMULANT LAXATIVES
These are a group of medications that stimulate the normal gastrointestinal reflexes
by chemically irritating the lining of the gastrointestinal wall, leading to increasing
of its activity. The drugs found in this group are bisacodyl (Dulcolax), cascara
(generic), castor oil (Neoloid), and senna (Senokot). Castor oil is used when a
thorough evacuation of the intestine is desirable. All of these agents begin working
at the beginning of the small intestine and increase motility throughout the rest of the
GI tract by irritating the nerve plexus. Because castor oil blocks absorption of fats
(including fat-soluble vitamins) and may lead to constipation from GI tract exhaustion
when there is no stimulus to movement, its frequent use is not desirable. Bisacodyl
acts in a similar manner but is somewhat milder in effect; it can also be given in a
water enema to stimulate the activity in the lower GI tract. Cascara is somewhat
milder than castor oil and is often used when effects are needed overnight. Sennais available orally in tablet and syrup form and as a rectal suppository.
Most of these agents are only minimally absorbed and exert their therapeutic effect
directly in the GI tract. Changes in absorption, water balance, and electrolytes
resulting from GI changes can have adverse effects on patients with underlying
medical conditions that are affected by volume and electrolyte changes. Castor oil
has an onset of action in 2 to 6 hours; the remaining chemical stimulants have an
onset of action of 6 to 8 hours, making them preferable if one wants the drug to
work overnight and see effects in the morning.
Laxatives are contraindicated with allergy to any component of the drug to prevent
hypersensitivity reactions and in acute abdominal disorders, including appendicitis,
diverticulitis, and ulcerative colitis, when increased motility could lead to rupture or
further exacerbation of the inflammation. Laxatives should be used with caution in
heart block, coronary artery disease (CAD), or debilitation, which could be affected
by the decrease in absorption and changes in electrolyte levels that can occurand with great caution during pregnancy and lactation because, in some cases,
stimulation of the GI tract can precipitate labor and many of these agents cross theplacenta and are excreted in breast milk.
The adverse effects most commonly associated with laxatives are GI effects such
as diarrhea, abdominal cramping, and nausea. Central nervous system (CNS)
effects, including dizziness, headache, and weakness, are not uncommon and may
relate to loss of fluid and electrolyte imbalances that may accompany laxative use.
Sweating, palpitations, flushing, and even fainting have been reported after laxative
use. These effects may be related to a sympathetic stress reaction to intenseneurostimulation of the GI tract or to the loss of fluid and electrolyte imbalance.
A very common adverse effect that is seen with frequent laxative use or laxative
abuse is cathartic dependence. This reaction occurs when patients use laxatives
over a long period of time and the GI tract becomes dependent on the vigorous
stimulation of the laxative. Without this stimulation, the GI tract does not move for a
period of time which could lead to constipation and drying of the stool and ultimately
to impaction. Specifically related to chemical stimulants, cascara, although a
reliable agent, may have a slow, steady effect or may cause severe cramping and
rapid evacuation of the contents of the large intestine. Castor oil blocks absorption
of fats (including fat-soluble vitamins) and may lead to constipation from GI tractexhaustion when there is no stimulus to movement.
Interactions: because laxatives increase the motility of the GI tract and some
interfere with the timing or process of absorption, it is advisable not to take laxatives
with other prescribed medications. The administration of laxatives and othermedications should be separated by at least 30 minutes.
Tables 2. 7.1: Chemical stimulant laxatives
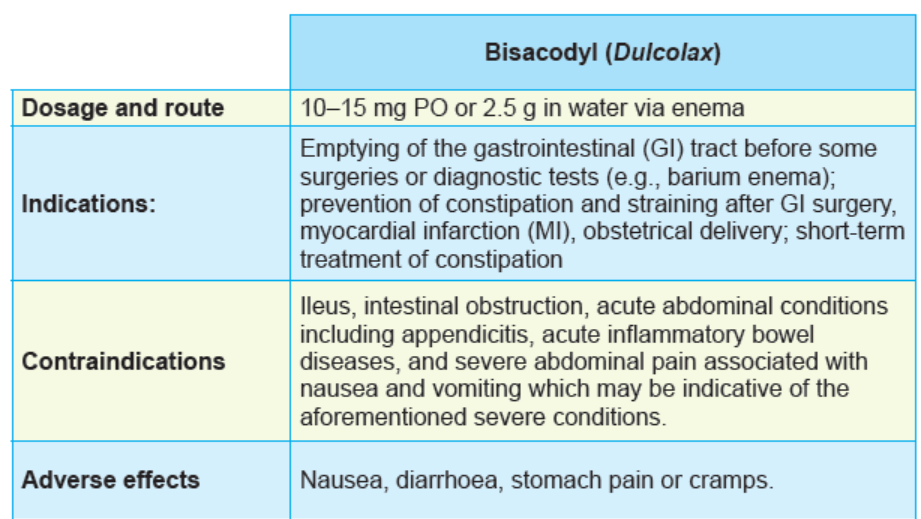
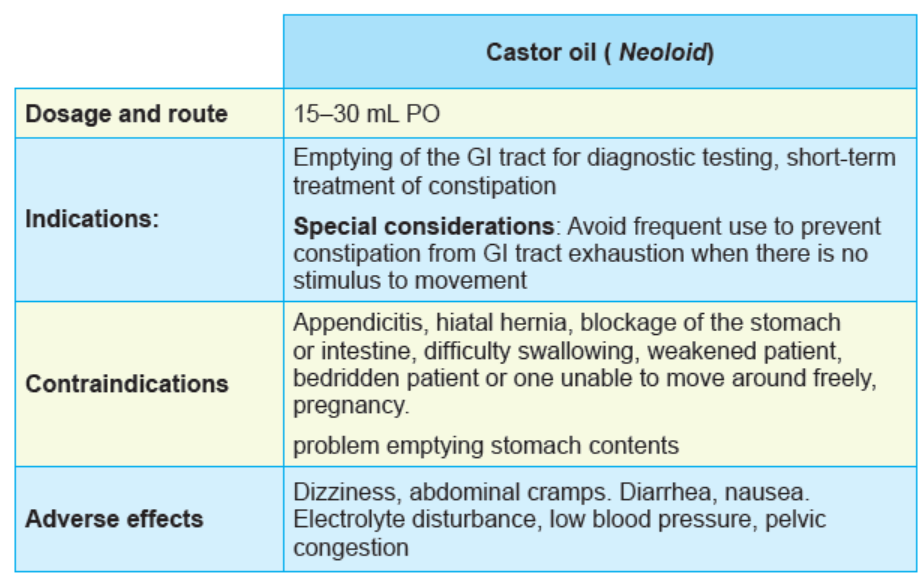
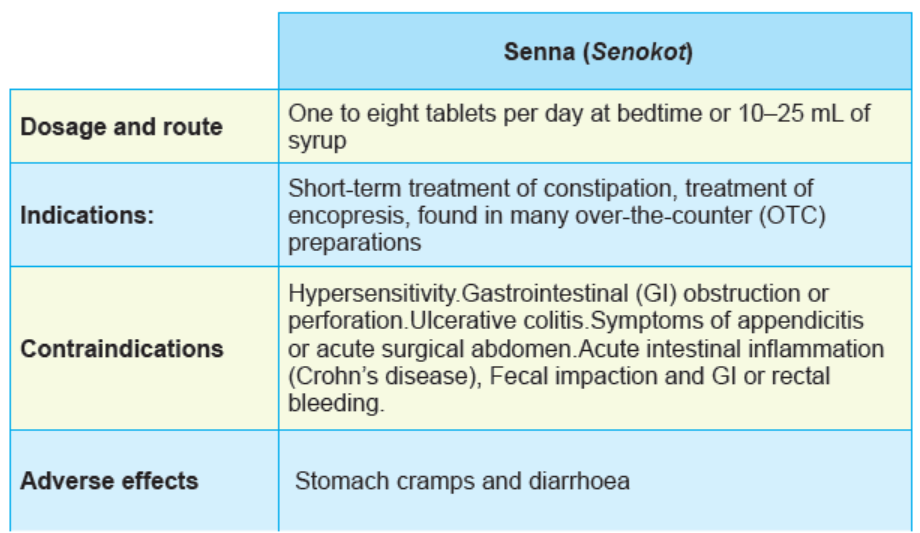

Figure 2.7. 1: Forms of chemical stimulant laxative
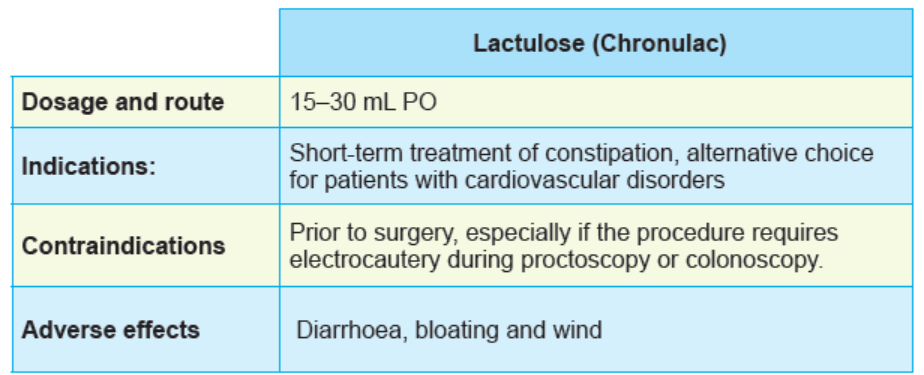
BULK STIMULANT LAXATIVES
Bulk stimulant laxatives increase the bulk by osmotic pull of fluid into the feces.
That increase the increased bulk stretches the gastro-intestinal wall, leading to
the stimulation and increased GI movement. The bulk stimulants are also called
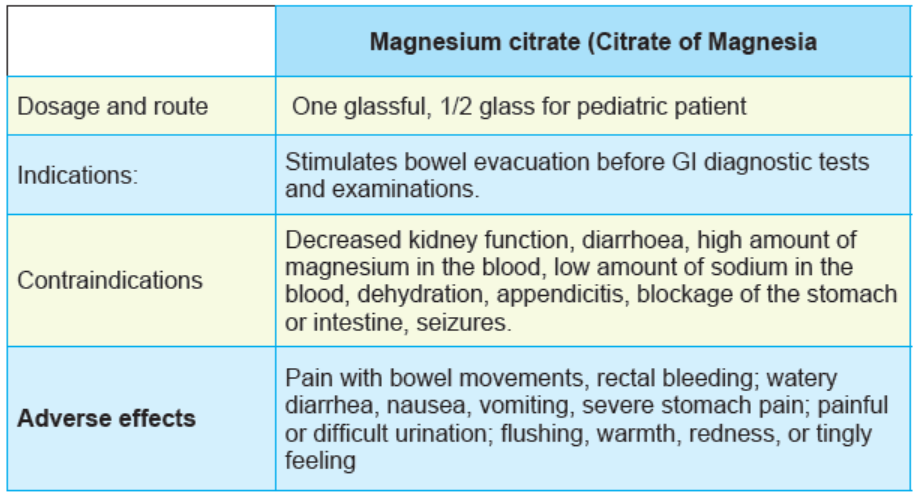
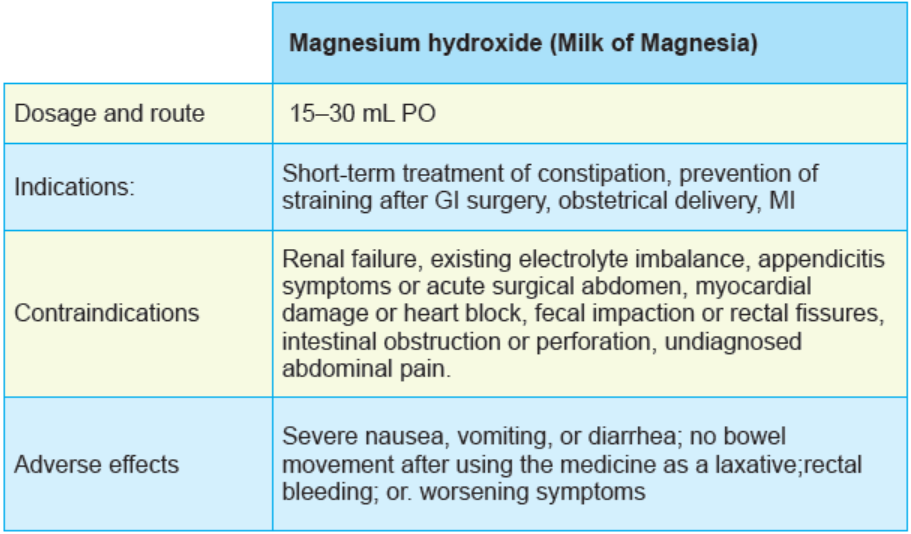
mechanical stimulants. The commonly used bulk stimulants include magnesium
sulfate (Epsom salts), magnesium citrate (Citrate of Magnesia), magnesium
hydroxide (Milk of Magnesia), lactulose (Chronulac), polycarbophil (FiberCon),
psyllium (Metamucil), and polyethylene glycol-electrolyte solution (GoLYTELY,MiraLAX).
Therapeutic action
Lactulose is a saltless osmotic laxative that pulls fluid out of the venous system
and into the lumen of the small intestine. Magnesium citrate is a milder and sloweracting
laxative. It works by a saline pull, bringing fluids into the lumen of the GI tract.
Magnesium hydroxide is a milder and slower-acting laxative. It also works by a
saline pull, bringing fluids into the lumen of the GI tract. Magnesium sulfate acts by
exerting a hypertonic pull against the mucosal wall, drawing fluid into the intestinalcontents.
Polycarbophil is a natural substance that forms a gelatin-like bulk out of the
intestinal contents. This agent stimulates local activity. It is considered milder and
less irritating than many other bulk stimulants. Patients must use caution and take
polycarbophil with plenty of water. Polyethylene glycol-electrolyte solution is a
hypertonic fluid containing many electrolytes that pulls fluid out of the intestinal wallto increase the bulk of the intestinal contents.
Psyllium, another gelatin-like bulk stimulant, is similar to polycarbophil in action
and effect
These drugs are all taken orally. They are directly effective within the GI tract and
are not generally absorbed systemically. They are rapidly acting, causing effects asthey pass through the GI tract.
Bulk laxatives are contraindicated with allergy to any component of the drug
to prevent hypersensitivity reactions and in acute abdominal disorders, like
appendicitis, diverticulitis, and ulcerative colitis, when increased motility could leadto rupture or further exacerbation of the inflammation.
Laxatives should be used with caution in heart block, CAD and debilitation, which
could be affected by the decrease in absorption and changes in electrolyte levelsthat can occur.
They are used with great caution during pregnancy and lactation because, in some
cases, stimulation of the GI tract can precipitate labor and many of these agentscross the placenta and are excreted in breast milk.
Polyethylene glycol electrolyte solution should be used with caution in any patient
with a history of seizures because of the risk of electrolyte absorption causingneuronal instability and precipitating seizures.
The most common adverse effects most commonly associated with bulk laxatives
are GI effects such as diarrhea, abdominal cramping, and nausea CNS effects,
including dizziness, headache, and weakness, are not uncommon and may relate
to loss of fluid and electrolyte imbalances that may accompany laxative use,palpitations, flushing, and even fainting

Figure 2.7.2 Forms of bulk laxatives
TABLE 2.7.2 BULK LAXATIVES DRUGS:
LUBRICANT DRUGS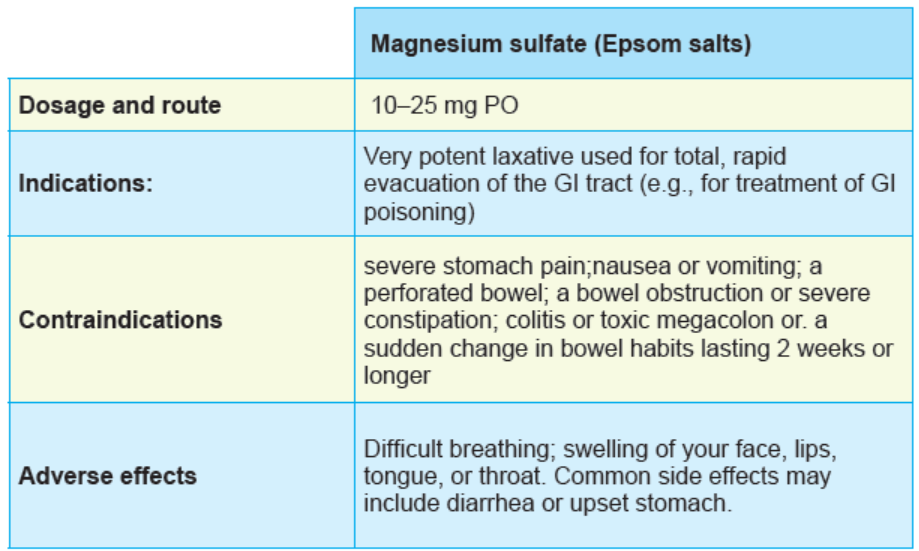
For some persons, there may be a need to make defecation easier without using
drugs designed to stimulate the gastrointestinal tract, in this case they benefit
from lubricants usage. Patients with hemorrhoids and those who have recently
had rectal surgery may need lubrication of the stool. Some patients who could be
harmed by straining might also benefit from this type of laxative. The type of laxative
recommended depends on the condition of the patient, the speed of relief needed,
and the possible implication of various adverse effects. Lubricating laxatives include
docusate (Colace), glycerin (Sani-Supp), and mineral oil (Agoral Plain).
Therapeutic actions
Docusate has a detergent action on the surface of the intestinal bolus, increasing
the admixture of fat and water and making a softer stool. Glycerin is a hyperosmolar
laxative that is used in suppository form to gently evacuate the rectum without
systemic effects higher in the GI tract.
Mineral oil is the oldest of these laxatives. It is not absorbed and forms a slippery
coat on the contents of the intestinal tract. When the intestinal bolus is coated
with mineral oil, less water is absorbed out of the bolus, and the bolus is less
likely to become hard or impacted. These drugs are not absorbed systemically and
are excreted in the feces. Docusate and mineral oil are given orally. Glycerin isavailable as a rectal suppository or as a liquid for rectal retention.
These laxatives are contraindicated with allergy to any component of the drug
to prevent hypersensitivity reactions and in acute abdominal disorders, including
appendicitis, diverticulitis, and ulcerative colitis, when increased motility could leadto rupture or further exacerbation of the inflammation.
The adverse effects most commonly associated with lubricant laxatives are GI
effects such as diarrhea, abdominal cramping, and nausea. In addition, leakage
and staining may be a problem when mineral oil is used and the stool cannot be
retained by the external sphincter. CNS effects, including dizziness, headache,
and weakness, are not uncommon and may relate to loss of fluid and electrolyte
imbalances that may accompany laxative use. Sweating, palpitations, flushing, and
even fainting have been reported after laxative use. These effects are less likely to
happen with the lubricant laxatives than with the chemical or mechanical stimulants.
Frequent use of mineral oil can interfere with absorption of the fat-soluble vitaminsA, D, E, and K.
Tables 2.9. Lubricant laxatives:
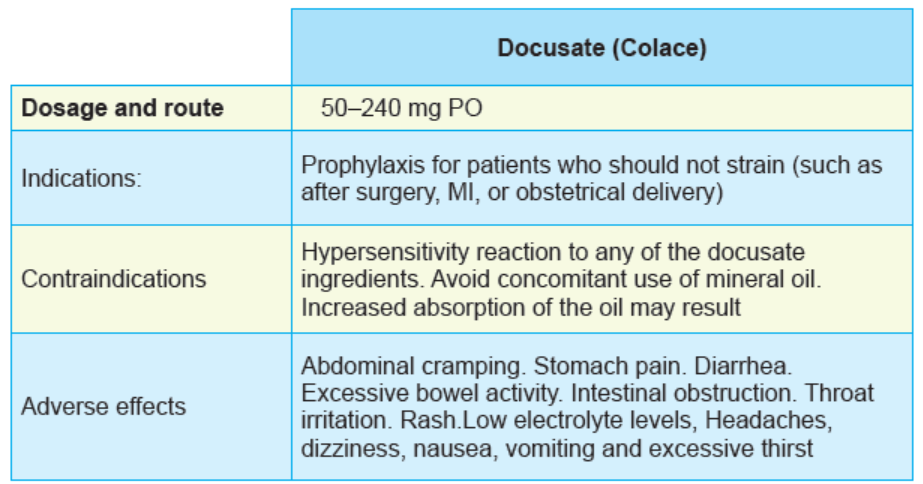
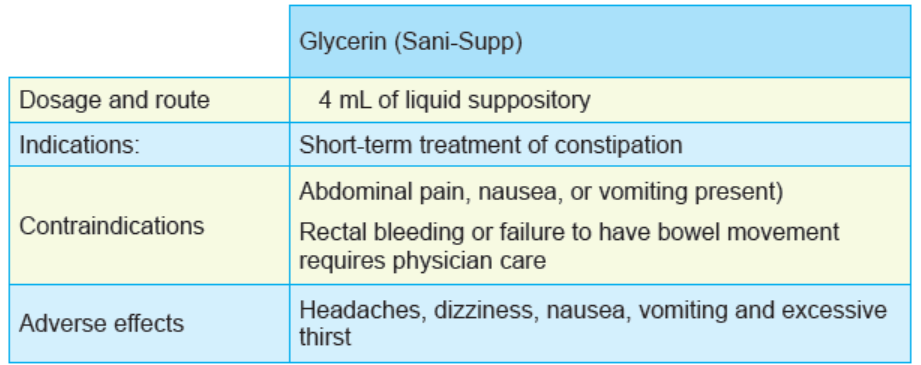
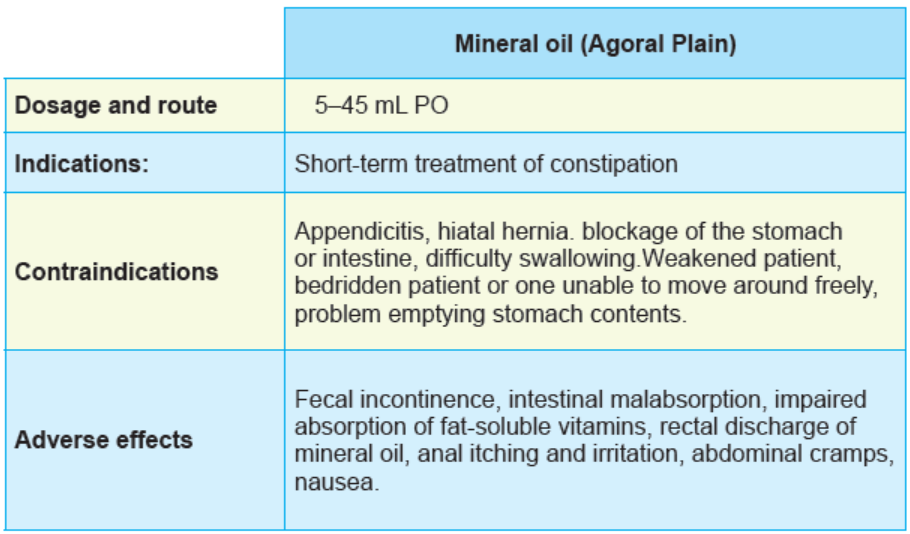

Figure 2.7.2 Forms of lubricant laxatives
Self assessment 2.7
1. All of the following drugs are bulk laxatives, EXCEPT:
A. Polycarbophil
B. Glycerin
C. Lactulose
D. Magnesium hydroxide
2. Which of the following drugs is a lubricant laxative?
A. Bisacodyl
B. Lactulose
C. Mineral oil
D. Magnesium hydroxide
3. All of the following conditions are indications of laxatives, EXCEPT:
A. To treat simple, chronic constipation.
B. To accelerate the movement of ingested
C. Before diagnostic procedures of the colon
D. To treat mild to moderate diarrhea
4. Explain the mechanism of action of bulk laxatives.5. Explain the mechanism of action of chemical stimulant laxatives.
2.8. Body fluid compartments
Learning Activity 2.8
On your first day of clinical practice in a hospital you find Mr.MN a 34 year-old
male patient who has been hospitalized since yesterday. In the file you find that
on the prescription that the patient must be given intravenous fluids, namely
ringer lactate and normal saline 4l/24hrs in alternation, with close monitoring of
vital signs. The nurse working at that health facility is explaining the mechanism
of action of intravenous fluids, and factors to consider while prescribing the
fluids. After 2 days, one of your colleagues wants you to remind the content you
covered with the nurse in that teaching session. Answer the following questionsrelated to the fluids in order to help your colleague:
1. What are the 3 key factors in the movement of fluids?
2. What are the 4 components of extracellular fluid?
3. Which of the following statements are the 2 main compartments of fluids
in the body?
A. Extracellular fluid and interstitial fluid compartments
B. Intracellular fluid and extracellular fluid compartments
C. Intracellular fluid and interstitial fluid compartmentsD. Transcellular fluid and interstitial fluid compartments
CONTENT SUMMARY
In human body, the fluids travel between compartments that are separated by
semipermeable membranes. Control of water balance in the various compartments
is indispensable to homeostasis. The imbalances of body fluids are frequent and
require the treatment most of the times using drugs.
The body fluids are mostly consisted with water, which serves as the universal
solvent in which most nutrients, electrolytes, and minerals are dissolved. Water
alone is responsible for about 60% of the total body weight in a middle- age adult.
A new-born may contain approximately 80% water, whereas an older adult may
contain only 40%.
In a simple model, water in the body can be located in one of two places, or
compartments. The intracellular fluid (ICF) compartment, which contains water that
is inside cells, accounts for about two thirds of the total body water.
The remaining one third of body fluid resides outside cells in the extracellular fluid
(ECF) compartment. The ECF compartment is further divided into two parts: fluid inthe plasma, or intravascular space, and fluid in the interstitial spaces between cells.
The extracellular fluid is divided into:
1. Plasma
2. Interstitial fluid and lymph
3. Bone and dense connective tissue water
4. Transcellular (cerebrospinal, pleural, peritoneal, synovial, and digestive
secretions)
The plasma and interstitial fluids are the two most important because of constant
exchange of fluid and electrolytes between them. Plasma and interstitial fluid are
separated by the capillary endothelium. Plasma circulates in the blood vessels,whereas the interstitial fluid bathes all tissue cells except for the formed elements
of blood. For this reason, Claude Bernard, the French physiologist, called the
interstitium “the true environment of the body”. For fluids movement, the osmolality,
tonicity and osmolarity are key. The osmolality is a fluid is a measure of the number
of dissolved particles, or solutes, in 1 kg (1 L) of water. In most body fluids sodium,
glucose, and urea, determine the osmolality. Sodium is the greatest contributor to
osmolality due to its abundance in most body fluids. The normal osmolality of body
fluids ranges from 275 to295 milli-osmols per kilogram (mOsm/kg). Tonicity is the
ability of a solution to cause a change in water movement across a membrane due
to osmotic forces. Whereas osmolality is a laboratory value that can be precisely
measured, tonicity is a general term used to describe the relative concentration ofIV fluids.
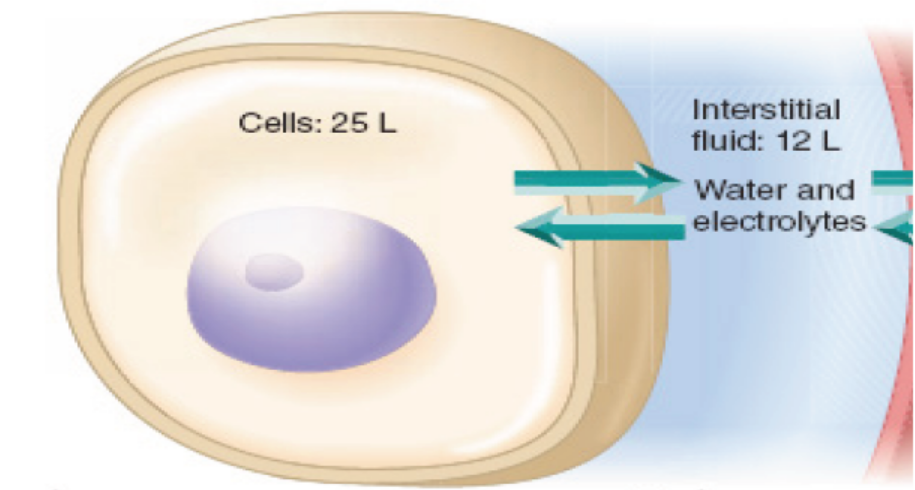
Figure 2.8.1. Fluid compartments
There is a continuous exchange and mixing of fluids between the various
compartments, which are separated by membranes. For example, the plasma
membranes of cells separate the intracellular fluid (ICF) from the extracellular
fluid (ECF). The capillary membranes separate plasma from the interstitial fluid.
Although water travels freely among the compartments, the movement of large
molecules and those with electrical charges is governed by processes of diffusion
and active transport. Movement of ions and drugs across membranes is a primary
concept of pharmacokinetics.
Normally there should be a balance between fluid input and output. When the
output is greater than fluid intake, body fluid deficit may result and the person has
dehydration, electrolytes imbalances and / or shock that may be fatal depending onthe severity.
Fluid requirements
In human, body fluid requirement varies according across the life span and its
calculation is based on weight and there is a need to adjust up or down based on
specific medical conditions.
In general, infants, children and adolescents have higher ml/kg requirement
than adults.Table 2.8.1: In adults, the fluid requirements are as follows:
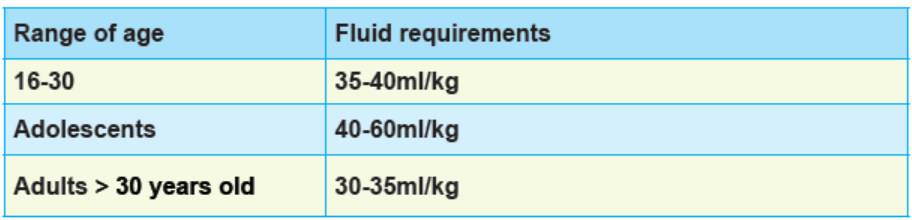
Table 2.8.2.Fluid requirements in children
In pediatric population, fluid requirements are calculated considering the child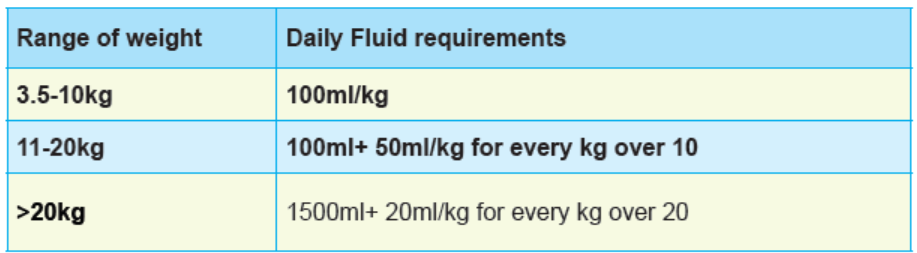
weight.
Self assessment 2.8
1. Which of the following statements indicates the fluid requirements in adults
aged 30 years and above?
A. 30-35ml/kg
B. 10-15 ml/kg
C. 5-10 ml/kgD. 3-5 ml/kg
2. Which of the following would be a basis to ideally calculate body fluid
requirements in humans?
A. Gender
B. Height
C. Weight
D. Race
3. Children and adolescents have higher ml/kg requirement than adults. TRUEor FALSE
2.9. Intravenous fluids and calculation of drop rate
Learning Activity 2.9
MM a 60 kg female was treated with ORS after a consultation for diarrhoea with
mild to moderate dehydration. After 24 hours ,you notice that she presents the
signs of severe dehydration and change in vital signs. You decide to administer
normal saline 500ml for 1hr as an intravenous infusion.
Using library textbooks and internet, discuss the following:
1. Discuss the classifications of intravenous fluids
2. List the indications of IV fluids and give an example for each class
3. Demonstrate how drop rate is calculated. How many drops of NS will run
per minute to make 500ml of NS to flow in 2hrs, with a drop factor of 20drops per mL?
CONTENT SUMMARY
In human, there must be a balance between fluid input and fluid output. The latter
should not exceed the intake, if this is the case then, there will be manifestations
of fluid volumes deficits if the opposite edema is the result. In general, fluid is
lost through gastrointestinal tract when a person vomits, has diarrhea, with chronic
laxative use, gastric suctioning but also with excessive sweating, athletic activity,
prolonged fever, severe burns, hemorrhage, excessive diuresis, complications of
diabetes like diabetic ketoacidosis etc.
In clinical practice, restoring and maintaining proper fluid volume, composition, and
distribution is a significant problem in the treatment of seriously ill patients andthose with or at risk of fluid and electrolytes imbalance. Nurses are in good position
for the intravenous fluid administration and monitoring. Fluids are administered to
refill total body water, restore blood volume and pressure and/or shift water from
one fluid compartment to another, restore and maintain electrolyte and acid–base
balance.
Classification of intravenous fluids
The IV fluids are classified considering the effect that they may cause to cells when
reach human body. According to their tonicity, intravenous fluids are classified as
isotonic, hypertonic and hypotonic.
Solutions that are isotonic have the same concentration of solutes (same
osmolality) as plasma. Hypertonic solutions contain a greater concentration of
solutes than plasma, whereas hypotonic solutions have a lesser concentration of
solutes than plasma. If hypertonic solution is administered, the plasma gains more
solutes than the interstitial fluid. Water will move, by osmosis, from the interstitial
fluid compartment to the plasma compartment. This type of fluid shift removes water
from cells and can result in dehydration. Water will move in the opposite direction,
from plasma to interstitial fluid, if a hypotonic solution is administered. This type of
fluid shift could result in hypotension due to movement of water out of the vascularsystem. Isotonic solutions will produce no net fluid shift.

Figure 2.9.1: Movement of fluids
Another important classification considering the components of the IV fluid. There
are crystalloid and colloidal IV fluids.
Crystalloids are IV solutions that contain electrolytes and other substances that
closely mimic the body’s ECF. They are used to replace depleted fluids and to
promote urine output. Crystalloid solutions are capable of quickly diffusing across
membranes, leaving the plasma and entering the interstitial fluid and ICF. It is
estimated that two thirds of infused crystalloids will distribute in the interstitial space.Isotonic, hypotonic, and hypertonic solutions are available.
Table 2.9.1. CRYSTALLOID IV SOLUTIONSt
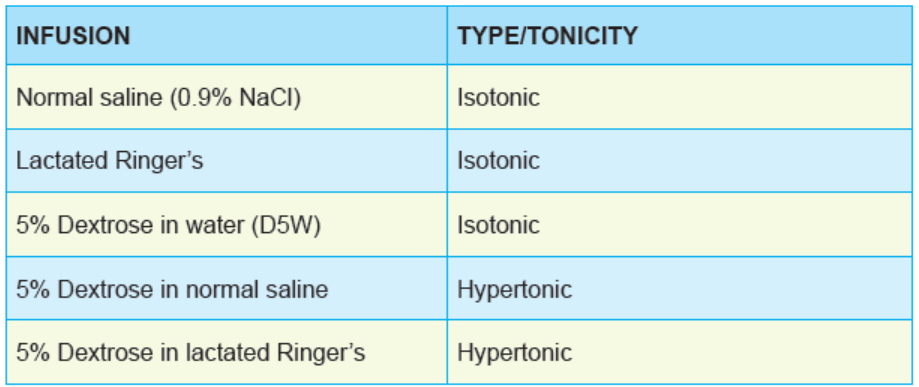

Figure 2.9.2 Crystalloids
Note: 5% of dextrose in water (D5W) is quickly metabolized, it is considered as
hypotonic solution.
COLLOIDS IV FLUID
Colloids contain large molecules like proteins that remain in the blood for a long
time because they are too large to easily cross the capillary membranes. When theyare circulating, they have the same effect as hypertonic solutions. They pull water
molecules from the cells and tissues into the plasma through their ability to increase
plasma osmolality and osmotic pressure. They are plasma volume expanders that
are used in treatment of hypovolemic shock due to burns, haemorrhage or aftersurgery.
Table 2.9.2. COLLOIDS IV FLUID
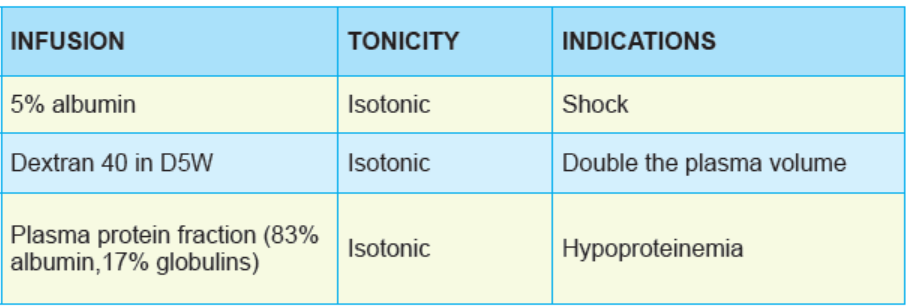

Figure 2.9.3: Colloids
DROP RATE CALCULATION
In all health facilities across health care system, many different types of medications
are delivered as continuous IV infusions in acute, ambulatory, long-term and critical
care settings. With poor attention before during even after IV drug medications,
Medication error arise. These errors, which may be having serious negative
consequences, can be eliminated or kept to a minimum by knowing the standard to
medication errors. The drop rate calculation is very important for all continuous or
intermittent IV infusion Continuous IV infusions are often used when the medication
needs to be greatly diluted, the drug level in the blood must be tightly controlled, or
large volumes of fluids need to be infused.The drop rate calculation requires to have the following information
1. Amount of infusion/medication to be given(volume)
2. Ordered dose
3. Time or length of administration in minutes
4. Drop factor: the number of the drops in the iv chamber that is equivalent to 1mlHaving all this information the drop rate or flow rate is calculated as follow:

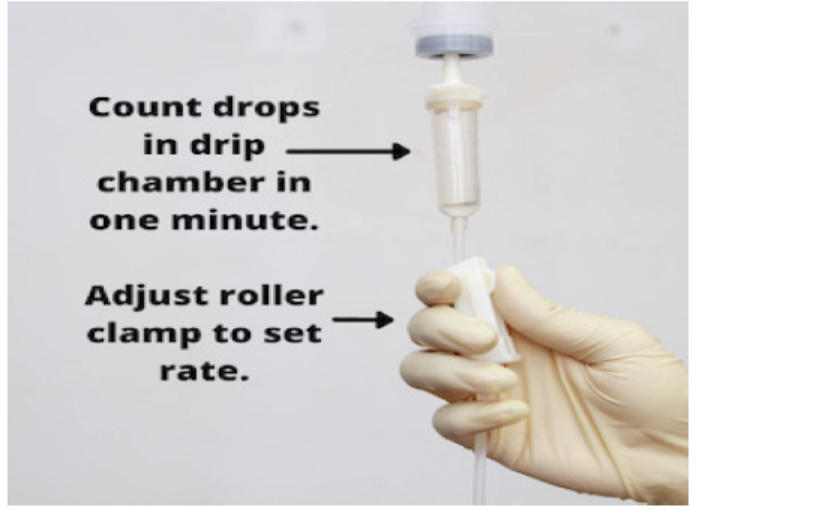
For IV infusion, tubing varies in size. The macrodrip tubing delivers 10 to 20 gtts/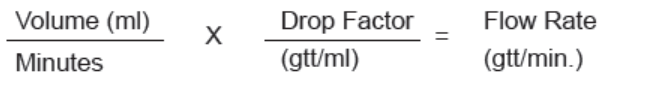
mL and is used to infuse large volumes or to infuse fluids quickly. Microdrip tubing
delivers 60 gtts/mL and is used for small or very precise amounts of fluid, as with
neonates or pediatric patients. In general, the drop factor is considered as 20 but
may change depending on the manufacturer of the infusion set. Before administeringIV fluid a nurse must verify it on the available set.
If you simply need to figure out the mL per hour to infuse, take the total volume inmL, divided by the total time in hours, to equal the mL per hour.
An IV drip rate is a way of describing the rate of an intravenous infusion based on
the number of drops (gtt) that are administered to the patient per minute. This is
influenced by the type of the tubing (microdrip or macrodrip), the total volume that
is required to be infused, and the time over which the infusion is ordered to run.
An IV drop factor reflects the specific size of the drops of IV fluid that the tubing
set creates. This is a predetermined number based on the tubing required andavailable to administer the medication
NURSING CONSIDERATONS FOR IV INFUSIONS ADMINISTRATION
1. Assess baseline assessment prior to administration:
• It is the responsibility of a nurse to take a complete health history prior to
IV fluid administration. This may include but not limited to cardiovascular
conditions like hypertension, neurologic conditions, and endocrine, hepatic,
renal….
• Also obtain a drug history including allergies, current prescription and overthe-
counter (OTC) drugs, and herbal preparations.
• Obtain baseline weight and vital signs, level of consciousness (LOC), breath
sounds, and urinary output as appropriate.
• Evaluate appropriate laboratory findings like electrolytes, full blood count, if
possible, urine specific gravity and urinalysis, blood urea nitrogen [BUN] and
creatinine, total protein and albumin levels, renal and liver function studies
• Assess for desired therapeutic effect
• Double check doses with another nurse before giving any IV fluids.
2. After administration, a nurse should continue the monitoring
• Continue frequent assessments for therapeutic effects.
• Monitoring of vital signs, urinary output, and the level of consciousness.
• Assess for and promptly report adverse effects: tachycardia, HTN,
dysrhythmias, decreasing LOC, increasing dyspnea, lung congestion,
decreased urinary output, muscle weakness or cramping, or allergic reactions.
• Monitor for signs of fluid volume excess or deficit like increasing or decreasing
BP , tachycardia, changes in quality of pulse
• Monitor for signs of potential electrolyte imbalance including nausea,
vomiting, GI cramping, diarrhea, muscle weakness, cramping or twitching,
paresthesias, and irritability.
• Weigh the patient daily and report a weight gain or loss of 1 kg ormore in a
24-hour period
• Assist the patient with obtaining fluids and with eating as needed.
• Closely monitor for signs and symptoms of allergy if colloids are used.
• Closely monitor IV sites when infusing potassium or ammonium.
• Monitor nutritional status and encourage appropriate fluid intake toprevent
electrolyte imbalances as electrolyte imbalances may occur dueto inadequatenutrition or fluid intake as well as from drug therapy-like diuretics.
3. Teaching
• Instruct the patient to immediately report dyspnea, itching, feelings of Throat
tightness, palpitations, chest pain or tightening, or headache.
• Instruct the patient to report any irritation, pain, redness, or swelling at the IV
site or in the arm where the drug is infusing.
• Teach the patient to continue to consume enough liquids to remain adequately,
but not overly, hydrated. Drinking when thirsty, avoiding alcoholic beverages,
maintaining a healthy diet, and ensuring adequate but not excessive salt
intake will assist in maintaining normal fluid and electrolyte balance.
• Teach the patient to rise from lying or sitting to standing slowly to avoid
dizziness or falls.
• Instruct the patient to call for assistance prior to getting out of bed or attempting
to walk alone,
• Teach the patient that excessive heat conditions contribute to excessive
sweating that leads to fluid and electrolyte loss, and extra caution is warrantedin these conditions.
Self assessment 2.9
True or false
1. By their mechanism of action, the isotonic intravenous fluids expand plasma
volume True or false
2. By their mechanism of action, hypotonic solutions cause a decrease in
plasma volume True or false
3. Colloids IV fluids frequently cause allergies compared to crystalloids. True
or false
4. It is optional to take history before intravenous fluid administration True or
false
Choose the correct answer
1. The following are examples of crystalloids isotonic IV fluids, EXCEPT
B. Ringer lactate
C. Normal saline
D. Dextran
E. Dextrose 5%
2. One of the following is a colloid that is mostly indicated in treatment of shock
F. Normal saline
G. Albumin 5%
H. Dextran
I. Dextrose 5%
3. Which of the following options is a nursing consideration before intravenous
fluids administration?
A. Closely monitor for signs and symptoms of allergy if colloids are used.
B. Obtain baseline weight and vital signs
C. Instruct the patient to report any irritation or swelling at the IV siteD. Monitor for signs of fluid volume excess
4. Which of the following statements is the nursing consideration after
intravenous fluid administration?
A. Complete history taking
B. Obtain baseline weight and vital sign
C. Double check the prescriptionD. Monitor for signs of fluid volume exces
Case study
You receive a 45 years old female with history of nausea and vomiting. When you
take vital signs, you realize that this client has mild hypotension. The prescription
for this patient is 1l of normal saline in 3hrs. Considering the available infusion
set, the drop factor is 20drops/min.Calculate the drop rate.
2.10. Oral Rehydration Salts (ORS) and homemade rehydration
solution
Learning Activity 2.10
A nurse receives a 23years old female patient in health centre who is complaining
of diarrhea. When a patient is asked about frequency, she responded that she
is passing 3 watery stool every 12hrs and this started 2days ago. The nurse
decided to give oral rehydration salts to that patient for rehydration.
Using internet, work on the following topics and make notes
1. Discuss the composition of oral rehydration salt
2. What are the indications of oral rehydration salts?3. Discuss how you can prepare homemade rehydration solutions
CONTENT SUMMARY
The oral rehydration solution (ORS) is an oral powder that contains mixture of
glucose, sodium chloride, potassium chloride, and sodium citrate. It is dissolvable
in water and after being dissolved in the requisite volume of water they are intendedto be used for the prevention and treatment of dehydration due to diarrhea. It is
always combined with zinc are recommended by the WHO and UNICEF to be
used collectively to ensure the effective treatment of diarrhea. ORS replaces the
essential fluids and salts lost through diarrhea. Zinc decreases the duration and
severity of an episode and reduces the risk of recurrence in the immediate short
term. ORS and zinc are highly effective and affordable products for treatment ofchildhood diarrhea that could prevent deaths in up to 93% of diarrhea cases.
ORS is a powder for dilution in 200ml, 500ml and 1L and they are hermetically
sealed, laminated sachets made of multiply laminations with aluminium foil or
polyethylene foil. They are two types of ORS; high osmolality rehydration salt
that has the osmolality of 311molm/L, low osmolality oral rehydration solution
that has 245molm/L. The latter,being very effective, it is recommended by WHO for
use due to its great pharmacological and therapeutic effect. It is available as lowosmolarity 20.5g/1L and low osmolarity 10.2g/0.5L
Table 2.10.1: COMPOSITIONS OF ORAL REHYDRATION SALUTION
ORS has contributed to life saving due to the pharmacokinetics and therapeutic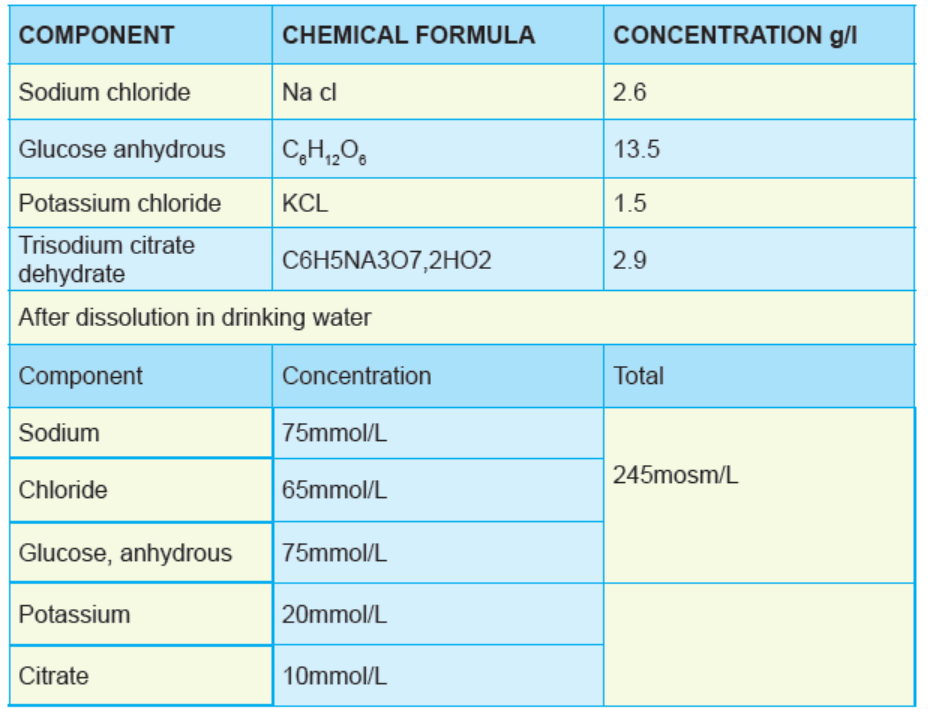
values of its components.
Glucose facilitates the absorption of sodium and hence water in small intestine.Sodium and potassium are important in replacement of losses of the essential ions
during diarrhea and vomiting. Citrate corrects the acidosis that occurs as a resultof diarrhea and dehydration.

Figure 2.10.1 ORS FORMS
In clinical practice, ORS is indicated for the treatment of fluid losses especially in
case of diarrhea in infants, children and adults with mild to moderate dehydration.
The amount to be given is determined on basis of weight and the amount of solution
require depend largely on child status. For child with marked signs of dehydration
or who combines to pass frequently watery stools will require more solution than
those with less marked signs or who are not passing frequent stools.
The approximate amount of ORS solution to give in the first 4 hours:
Below 4 months / less than 5 kg: 200–400 mL
4–11 months / 5–7.9 kg: 400–600 mL
12–23 months / 8–10.9 kg: 600–800 mL
To 4 years / 11–15.9 kg: 800–1,200 mL
To 14 years / 16–29.9 kg: 1,200–2,200 mL
15 years or older / 30 kg or more: 2,200–4,000 mL
If a child wants more than the estimated amount of ORS solution, and there are no
signs of overhydration, give more.
In case the child’s weight is unknown, use patient’s age and if the weight is known
the amount of ORS is estimated by multiplying the child’s weight in kg times 75ml.
During the initial stages of therapy, while still dehydrated, adults can consume up
to 750 mL per hour, if necessary, and children up to 20 mL/kg body weight per
hour. Normal feeding can continue after the initial fluid deficit has been corrected.Breastfeeding should continue between administrations of ORS.
Edematous (puffy) eyelids are a sign of overhydration. If this occurs, stop giving
ORS solution, but give breast milk or plain water, and food. Do not give a diuretic.
When the edema has gone, resume giving ORS solution or home fluids according
to Treatment Plan A. After 4 hours, reassess the child fully. Then decide what
treatment to give next: If signs of severe dehydration have appeared, IV therapyshould be started following WHO Treatment Plan C
If the patient still has signs indicating some dehydration, continue oral rehydration
therapy by repeating the treatment described above. At the same time, start to offer
food, milk and other fluids, as described in WHO Treatment Plan A. If there are nosigns of dehydration, the patient should be considered fully rehydrated.
ORS should not be taken when a patient has cirrhosis of liver, congestive heart
cardiac failure, nephrotic syndrome acute and renal failure, ischemic heart diseases
,adrenocortical insufficiency, hyperkalemic periodic paralysis, hyperkalemia,
hypoventilatory states, chloride depletion due to continuous gastric fluid loss,
metabolic or respiratory alkalosis, hypocalcaemia, hyperosmolar states in anuria
or oliguria, edematous sodium retaining conditions, hypertension, peripheral
or pulmonary edema or toxaemia of pregnancy, severe vomiting, diarrhea and
dehydration requiring fluid therapy, dextrose malabsorption, diabetes mellitus,
thiamine deficiency, severe under nutrition as another specific solution ’’ReSoMal’’is appropriate, hemodilution, hypophosphatemia, sepsis, and trauma.
ORS is also contraindicated for use in patients undergoing treatment with the
following: sodium-retaining drugs such as corticosteroids, NSAIDs, carbenoxolone,or diuretics known to produce hypochloremic alkalosis.
It is very important to note that, ORS is administered with care in cases of acute
dehydration, heat cramps, extensive tissue destruction, or if patients are receiving
potassium-sparing diuretics. Concurrent use with other potassium-containing drugsmay precipitate hyperkalemia.
It is very important to dissolve ORS in water of the correct volume. A weak solution
will not contain optimum glucose and electrolyte concentration and a strong
solution may give rise to electrolyte imbalance. Diarrhea can have very serious
consequences in children under 3 years old. Immediate medical advice should
be sought. In other age groups, if symptoms persist for more than 24–48 hours,consult a doctor.
If nausea and vomiting are present with the diarrhea, small and frequent amounts
of ORS should be drunk first. In infants, immediate medical assistance should
be obtained. Use within 1 hour of reconstitution, or within 24 hours if stored in arefrigerator.
ORS interact with other medicinal products.
It increases excretion of lithium, resulting in a reduced plasma-lithium concentration.
Potassium chloride ACE inhibitors (hyperkalemia); cyclosporine leads to increased
risk of hyperkalemia; potassium-sparing diuretics where hyperkalemia may result.No known interactions to other actives.
For more details, see also under “Contraindications” section.
Undesirable effects
Adverse effects are not very common but in case of excessive amount, hypernatremia,
edema, nausea, vomiting, diarrhea, abdominal cramps, thirst, reduced salivation,
lachrymation, sweating, fever, tachycardia, renal failure, respiratory arrest,
headache, dizziness, restlessness, irritability, weakness, muscular twitching, coma,
convulsions, hyperkalemia, gastrointestinal ulceration, metabolic alkalosis, musclehypertonicity, flatulence, dehydration, and raised blood pressure may arise
In case of overdose, sodium, potassium restriction, and water intake plus measures
to increase renal sodium, potassium and water output by using loop diuretics forexample are recommended.
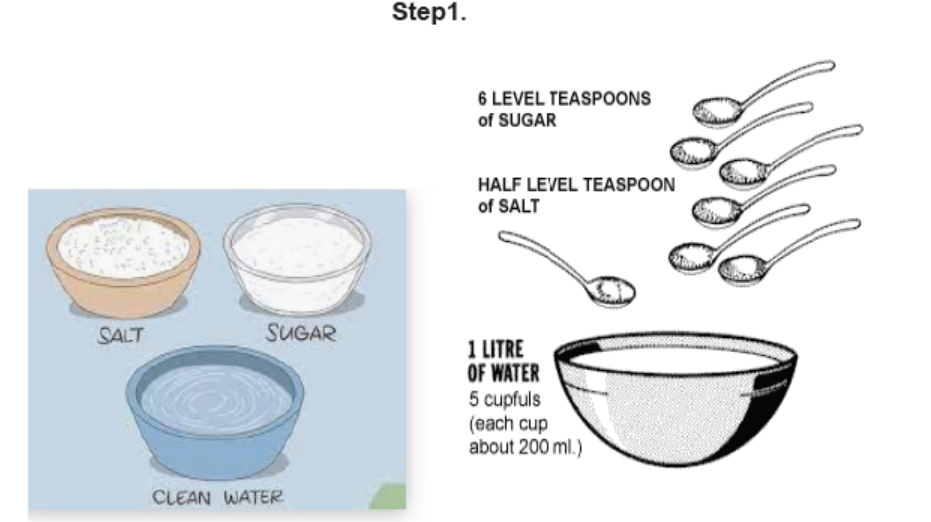
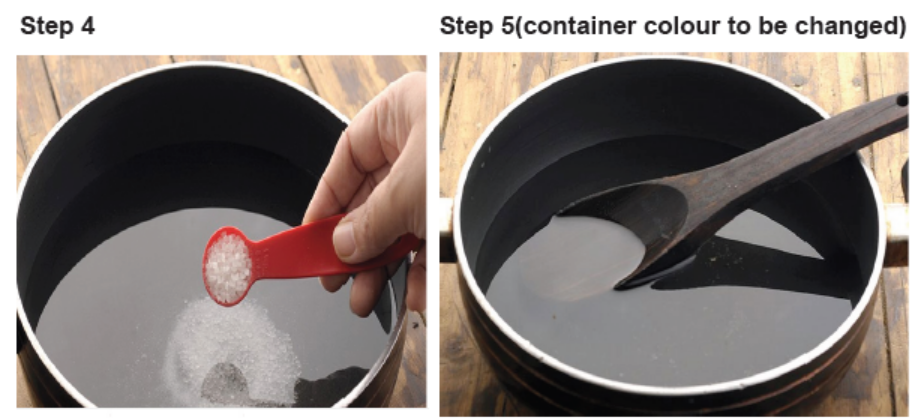
HOMEMADE ORAL REHYDRATION SALT
Homemade oral rehydration solution is a rehydration solution prepared at home
using sugar, salt and water locally available at home. It less expensive most effective
but require attention in preparation as in case of error in preparation it may worsendiarrhoea or cause imbalances.
Table 2.10.2: COMPONENTS OF HOMEMADE ORAL REHYDRATION SALTSAND DOSAGE
Materials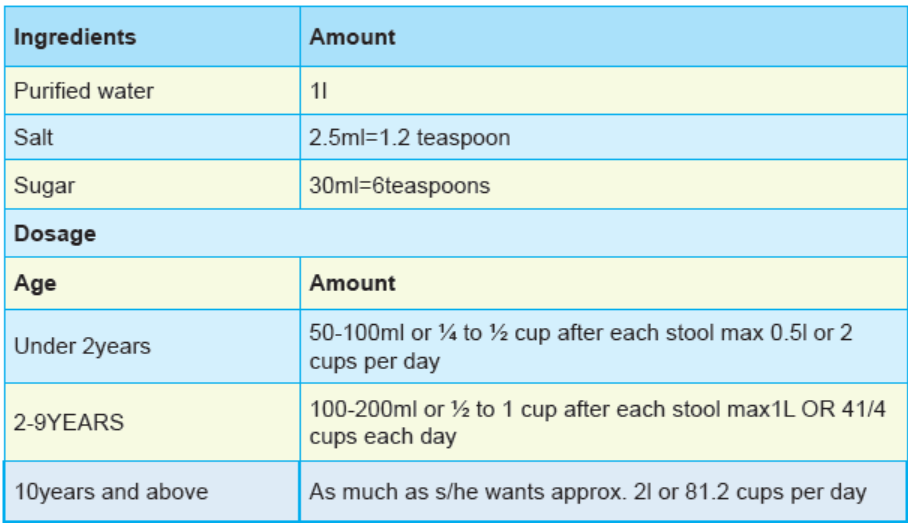
Teaspoon
Salt
Sugar
Clean or boiled waterContainer 1 L OR above

Self assessment 2.10
Respond by True or false
4. High osmolality oral rehydration solutions are more effective than low
osmolality solutions.
5. Oral rehydration salt is indicated in case of diarrhea with mild dehydration.
6. You have to avoid oral rehydration salt for a patient with severe acute
malnutrition.
7. When treating a child with mild diarrhea, there is no need to go to the healthfacility as you can offer homemade oral rehydration solution.
Chose the correct answer
1. The components of oral rehydration salt include the following Except
A. Sodium
B. Magnesium
C. Sugar
D. Citrate
2. What is the amount of ORS to be given to a patient weighing 30Kg in the first
4hours?
A. 2,200–4,000 mL
B. 3000-5000ml
C. 1000-2100mlD. 500ml-1500ml
3. For a child with diarrhea, which advice will you give to the caregiver about
moment of ORS administration
A. When child wake up
B. When the child asks
C. After each stool
D. B and C
4. The ingredients for homemade oral rehydration solution are
A. Salt, beans, sugar and water
B. Rice, sugar and beans
C. Sugar, salt and water
D. Sugar, salt and rice
5. Which action should be taken for a patient when there is no improvement and
the dehydration worsened, after 4hrs of ORS administration?
A. Increase the amount
B. Start IV fluids
C. Administer antibioticsD. Continuation of monitoring
2.11. Anti-spasmodic drugs
Learning Activity 2.11
1. What is an antispasmodic drug?2. Give 4 indications of antispasmodic drugs?
CONTENT SUMMARY
Gastrointestinal antispasmodics are medications used to treat spasms of the
gastrointestinal tract muscles, which can occur in diseases like irritable bowel
syndrome, or IBS for short, biliary colic, and pancreatitis it relieves some of the
symptoms of Irritable Bowel Syndrome (IBS) , prevents, or lowers the incidence of
muscle spasms(colic), bloating and tummy (abdominal) pain, especially those of
smooth muscle such as in the bowel wall, and it reduce the movement (motility) ofthe gut (intestines).
Antispasmodics are also used in some other conditions such as:
• Diverticular disease.
• Prevention of nausea, vomiting, and dizziness associated with motion
sickness.
• Adjunctive therapy for treatment of GI ulcers
• Decrease secretions before anesthesia or intubation
• Maintenance treatment of bronchospasm associated with COPD.• Treatment of irritable or hyperactive bowel in adults.
The most common antispasmodic contain anticholinergic properties, which is
helpful in relieving symptoms, such as abdominal pain. They are classified into
two main types: smooth muscle relaxant such as alveline and mebeverine, and
anticholinergics such as hyoscin. However not everybody with IBS finds that
antispasmodics work well, but they are worth trying, as they work well in a goodnumber of cases.
There are two main types antispasmodic drugs: Antimuscarinics drugs andSmooth muscle relaxants:
Smooth muscle relaxants work directly on the smooth muscle in the wall of the
gut. Here they help to relax the muscle and relieve the pain associated with acontraction of the gut.
A. Antimuscarinic drugs
Antimuscarinic medications are a group of anticholinergic agents, specificallyknown for blocking the activity of muscarinic receptors. These receptors play an
important role in mediating the functions of the parasympathetic nervous system,
which controls many involuntary functions to conserve energy, including the
contraction of smooth muscle, dilation of blood vessels, increased bodily secretions,
gastrointestinal activity, and heart rate. Because muscarinic receptors are also
found in other parts of the body, taking an antimuscarinic can have other effects.
For example, muscarinic receptors also help to control the production of saliva in
the mouth.
Therefore, antimuscarinics work by inhibiting the functions of the parasympathetic
nervous system. The two most commonly prescribed antimuscarinics
are atropine and scopolamine(Hyoscine), derived from the Atroppa belladonna
plant.1. Hyoscine (Buscopan 10 mg Tablets)
Hyoscine butylbromide are indicated for the relief of spasm, by helps dismiss lower
tummy (abdominal) muscle cramp and pain, it one of antispasmodic medicine
which is indicated to treat cramps in the stomach, the genito-urinary tract or gastrointestinal
tract and for the symptomatic relief of Irritable Bowel Syndrome or bladder.
In gastro- intestinal tract, specificaly it helps to ease bloating and the spasm-type
pain that can be associated with irritable bowel syndrome and diverticular disease. It
works by relaxing some of the muscles in your gastrointestinal and urinary systems.Each tablet contains hyoscine butylbromide 10 mg.
Posology and method of administration
Buscopan 10 mg tablets are for oral administration only.
Buscopan 10 mg tablets should be swallowed whole with adequate water.
Adults: 2 tablets four times daily. For the symptomatic relief of Irritable Bowel
Syndrome, the recommended starting dose is 1 tablet three times daily, this can be
increased up to 2 tablets four times daily if necessary.Children: 6 - 12 years: 1 tablet three times daily.
Contraindications
Buscopan 10 mg Tablets are contraindicated in: patients who have demonstrated
prior hypersensitivity to hyoscine butylbromide or any other component of the
product, myasthenia gravis, mechanical stenosis in the gastrointestinal tract,paralytic or obstructive ileus, megacolon, narrow angle glaucoma.
Special Precautions: Buscopan 10 mg Tablets should not be taken on a
continuous daily basis or for extended periods without investigating the cause of
abdominal pain. In case severe, unexplained abdominal pain persists or worsens,or occurs together with symptoms like fever, nausea, vomiting, changes in bowel
movements, abdominal tenderness, decreased blood pressure, fainting, or blood instool, medical advice should immediately be sought.
Interaction with other medicinal products and other forms of interaction
The anticholinergic effect of drugs such as tri- and tetracyclic antidepressants,
antihistamines, quinidine, amantadine, antipsychotics (e.g. butyrophenones,
phenothiazines), disopyramide and other anticholinergics (e.g. tiotropium,
ipratropium, atropine-like compounds) may be intensified by Buscopan. Concomitant
treatment with dopamine antagonists such as metoclopramide may result in
diminution of the effects of both drugs on the gastrointestinal tract. The tachycardiceffects of beta-adrenergic agents may be enhanced by Buscopan.
Adverse Reactions:
Many of the listed undesirable effects can be assigned to the anticholinergic
properties of buscopan
• Immune system disorders: anaphylactic shock, anaphylactic reactions,
dyspnoea, other hypersensitivity
• Cardiac disorders: tachycardia
• Gastrointestinal disorders: dry mouth
• Skin and subcutaneous tissue disorders: skin reactions (e.g. urticaria,
pruritus), abnormal sweating• Renal and urinary disorders urinary retention (Rare)
Overdose
Serious signs of poisoning following acute overdosage have not been observed in
man. In the case of overdosage, anticholinergic effects such as urinary retention,
dry mouth, reddening of the skin, tachycardia, inhibition of gastrointestinal motility
and transient visual disturbances may occur, and Cheynes-Stokes respiration hasbeen reported.
Pharmacokinetics
Absorption
As a quaternary ammonium compound, hyoscine butylbromide is highly polar and
hence only partially absorbed following oral (8%) or rectal (3%) administration. After
oral administration of single doses of hyoscine butylbromide in the range of 20 to
400 mg, mean peak plasma concentrations between 0.11 ng/mL and 2.04 ng/mLwere found at approximately 2 hours.
Distribution
Because of its high affinity for muscarinic receptors and nicotinic receptors, hyoscine
butylbromide is mainly distributed on muscle cells of the abdominal and pelvic
area as well as in the intramural ganglia of the abdominal organs. Plasma protein
binding (albumin) of hyoscine butylbromide is approximately 4.4%. Animal studies
demonstrate that hyoscine butylbromide does not pass the blood-brain barrier, butno clinical data to this effect is available.
Metabolism and elimination
Following oral administration of single doses in the range of 100 to 400 mg, the
terminal elimination half-lives ranged from 6.2 to 10.6 hours. The main metabolic
pathway is the hydrolytic cleavage of the ester bond. Orally administered hyoscine
butylbromide is excreted in the faeces and in the urine. Studies in man show that
2 to 5% of radioactive doses is eliminated renally after oral, and 0.7 to 1.6% after
rectal administration. Approximately 90% of recovered radioactivity can be found in
the faeces after oral administration. The urinary excretion of hyoscine butylbromide
is less than 0.1% of the dose. The mean apparent oral clearances after oral doses of
100 to 400 mg range from 881 to 1420 L/min, whereas the corresponding volumes
of distribution for the same range vary from 6.13 to 11.3 x 105 L, probably due to
very low systemic availability. The metabolites excreted via the renal route bind
poorly to the muscarinic receptors and are therefore not considered to contribute to
the effect of the hyoscine butylbromide.
2. Atropine
Atropine is a type of medicine called an antimuscarinic (or sometimes called an
anticholinergic). It works by relaxing the involuntary muscle that is found in the
walls of the stomach and intestines (gastrointestinal tract). Cholinergic antagonism
with atropine reduces proximal gastric emptying, reduces atrial contractility and
notably slows gastric emptying. Atropine is also used in case of hypersalvation,
bronchial secretions, or bradycardia. This drug can be used also before anesthesiato prevent the mucus secretion.
Indication
Relieving stomach cramps or colicky-type abdominal pain, for example associatedwith conditions such as irritable bowel syndrome (IBS).
Therapeutic action
Atropine is a type of medicine called an antimuscarinic (or sometimes called an
anticholinergic). It works by relaxing the involuntary muscle that is found in the walls
of the stomach and intestines (gastrointestinal tract). Atropine works by blocking
receptors called muscarinic (sometimes called cholinergic) receptors that are found
on the surface of the muscle cells in the walls of the gut. This prevents a natural
body chemical called acetylcholine from acting on these receptors. Normally when
acetylcholine acts on these receptors it causes the muscle in the gut to contract.
By preventing this, atropine helps the muscle in the gut to relax. This reduces
involuntary contractions and spasms of the muscle. Spasms in the muscle of the
gut wall can cause colicky abdominal pain, cramps, bloating, wind and discomfort.Atropine relieves these symptoms by relaxing the muscle.
Administration
Atropine tablets should be swallowed whole with a glass of water. They can be
taken either with or without food. The usual dose is one or two tablets to be takenat night. Follow the instructions given by your doctor or pharmacist.
Use with caution in Elderly people, Children, People with Down’s syndrome. Gastro-
esophageal reflux disease (GORD). Inflammation of the bowel and back passage
(ulcerative colitis), Diarrhea, People with a high temperature (fever). People with
disorders of the involuntary nervous system that controls body functions such as
blood pressure, heart rate, sweating, bowel and bladder emptying, and digestion
(autonomic neuropathy), People with an overactive thyroid gland (hyperthyroidism),
High blood pressure (hypertension), Heart attack (myocardial infarction) and
Glaucoma.
Atropine should not be used in people with a condition called myasthenia gravis,
where there is abnormal muscle weakness, people with inactivity of the muscle in
the gut that is causing a blockage or obstruction of the gut (paralytic ileus), people
who have narrowing of the outlet of the stomach, making it difficult for food to
pass into the intestines (pyloric stenosis), Men with an enlarged prostate gland
(prostatic hypertrophy) and people with allergic of its ingredients. If you feel you
have experienced an allergic reaction, stop using this medicine and inform yourdoctor or pharmacist immediately.
Pregnancy and breastfeeding
This medicine should be used with caution during pregnancy, and only if the
expected benefit to the mother is greater than any possible risk to the developing
baby, it passes into breast milk in small amounts. It should be used with caution
by breastfeeding mothers, and only if the expected benefit to the mother is greater
than any possible risk to the nursing infant.
Side effects
Medicines and their possible side effects can affect individual people in different
ways. The following are some of the side effects that are known to be associated
with Atropine. Just because a side effect is stated here, it does not mean that all
people using this medicine will experience that or any side effect.Pregnancy and breastfeeding
This medicine should be used with caution during pregnancy, and only if the
expected benefit to the mother is greater than any possible risk to the developing
baby, it passes into breast milk in small amounts. It should be used with caution
by breastfeeding mothers, and only if the expected benefit to the mother is greater
than any possible risk to the nursing infant.
Side effects
Medicines and their possible side effects can affect individual people in different
ways. The following are some of the side effects that are known to be associated
with Atropine. Just because a side effect is stated here, it does not mean that allpeople using this medicine will experience that or any side effect.
Constipation, dry mouth, flushing and dryness of the skin, increased body
temperature, blurred vision, dilated pupils and dislike of bright light, faster than
normal heartbeat (tachycardia), awareness of your heartbeat (palpitations), irregular
heartbeats (arrhythmias), difficulty passing urine (urinary retention), confusion(especially in elderly people), feeling or being sick, closed angle glaucoma.
Interaction
It is important to tell your doctor or pharmacist what medicines you are already
taking, including those bought without a prescription and herbal medicines,
before you start treatment with this medicine. Similarly, check with your doctor or
pharmacist before taking any new medicines while using this one, to make sure
that the combination is safe. There may be an increased risk of antimuscarinic side
effects, such as dry mouth, blurred vision, constipation, difficulty passing urine and
confusion in elderly people, if this medicine is taken with other medicines that have
antimuscarinic effects, for example the following:
• Amantadine: antihistamines, e.g. brompheniramine, chlorphenamine
• Antimuscarinic medicines for Parkinson’s symptoms, eg procyclidine,
orphenadrine, trihexyphenidyl
• Certain antipsychotic medicines, e.g. haloperidol, chlorpromazine, clozapine
• Other antispasmodic medicines, e.g. hyoscine
• Antidepressants, e.g. phenelzine, tranylcypromine• Tricyclic antidepressants, e.g. amitriptyline, clomipramine.
Drug interactions
This medicine may reduce the effects of the following medicines: Cisapride,
domperidone, ketoconazole, metoclopramide. If you experience a dry mouth as
a side effect of this medicine you may find that medicines that are designed to
dissolve and be absorbed from under the tongue, e.g. sublingual glyceryl trinitrate
(GTN) tablets, become less effective. This is because the tablets do not dissolve
properly in a dry mouth. To resolve this, drink a mouthful of water before taking
sublingual tablets.
B. Smooth muscle relaxants
Smooth muscle relaxants work directly on the smooth muscle in the wall of the gut.
Here they help to relax the muscle and relieve the pain associated with a contraction
of the gut. A muscle relaxant is a drug that affects skeletal muscle function and
decreases the muscle tone. It may be used to alleviate symptoms such as muscle
spasms, pain, and hyperreflexia. The term “muscle relaxant” is used to refer to two
major therapeutic groups: neuromuscular blockers and spasmolytic. Neuromuscular
blockers act by interfering with transmission at the neuromuscular end plate and
have no central nervous system (CNS) activity. They are often used during surgical
procedures and in intensive care and emergency medicine to cause temporary
paralysis. Spasmolytics, also known as “centrally acting” muscle relaxant, are used
to alleviate musculoskeletal pain and spasms and to reduce spasticity in a variety
of neurological conditions. While both neuromuscular blockers and spasmolytics
are often grouped together as muscle relaxant, the term is commonly used to refer
to spasmolytics only. The most common Smooth muscle relaxant prototype arealverine, mebeverine, peppermint oil (colpermin ) and papaverine
Self assessment 2.11
1. The antimuscarinics are used:
B. To accelerate the parasympathetic system
C. To block the parasympathetic system
D. As the drugs of choice for treating ulcers
E. To stimulate gastrointestinal activity
2. Atropine belongs to the class of antimuscarinics. True or False.
3. All of the following antispasmodic drugs belongs to the class of smooth
muscle relaxants, EXCEPT:
A. Atropine
B. Papaverine
C. AlverineD. Peppermint oil
2.12. END UNIT ASSESSMENT
End of unit assessment
1. Which of the following is NOT a risk for peptic ulcer diseases?
B. Smoking
C. NSAIDs use
D. Skin color
E. Stress
2. Which of the following groups of drugs is used to treat peptic ulcer diseases?
A. Antifungals
B. Antivirals
C. Analgesics
D. Antacids.
3. Which statement is true about the mechanism of action of H2 receptor
antagonists?
A. The occupy the histamine receptors and prevent acid secretion
B. They bind to enzyme H-,K-ATPase and increase histamine release
C. They block prostaglandin secretion and decrease histamine release
D. They neutralize the secreted acid directly in the stomach lining
4. Which of the following is among the side effects of metoclopramide?
A. Constipation
B. Drowsiness
C. Fever
D. Headache
5. Which of the following laxatives acts without causing the systemic effect?
A. Bisacodyl
B. Lactulose
C. GlycerinD. Magnesium citrate
6. Which one among the following conditions reflects a contraindication of
antispasmodic drugs?
A. Irritable bowel syndrome
B. Biliary colic
C. Pancreatitis
D. Gastrointestinal obstruction
7. Which of the following options is a nursing consideration before intravenous
fluids administration?
A. Closely monitor for signs and symptoms of allergy if colloids are used.
B. Obtain baseline weight and vital signs
C. Instruct the patient to report any irritation, pain, redness, or swelling at
the IV site
D. Monitor for signs of fluid volume excess
8. The patient should receive ½ l of dextrose 5% in 3hrs. Knowing that the dropfactor is 20 drops per mL . Calculate the drop rate
