UNIT8:HYDROCELE AND TESTICULAR TORSION
Key Unit competence:
Take appropriate decision on Hydrocele and Testicular torsion
Introductory activity 8.0
The image A, C and c illustrate the structures of testicle. Observe image A, B, C,D and E and answer the questions below.
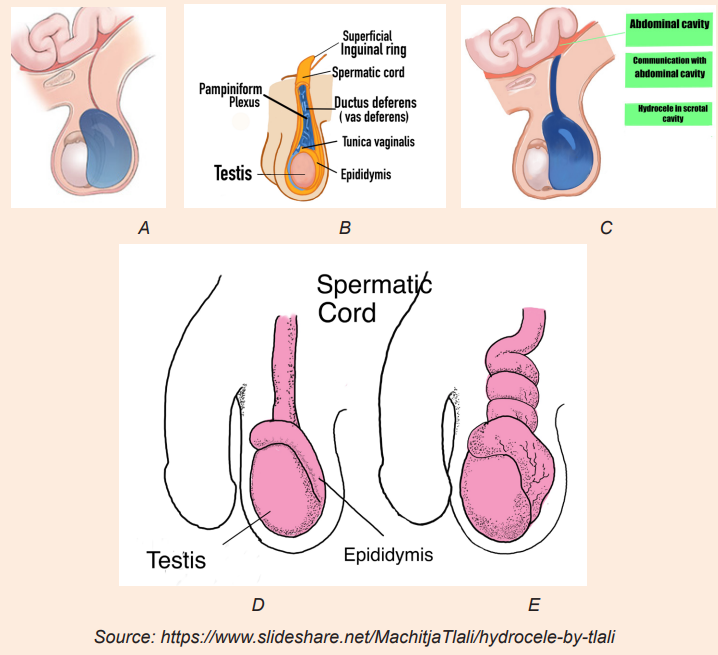
Draw the image without labels, and make image D in the black context
1) Which one of these three images (A, B, C, D) would reflect the normal
structure of testicle?
2) What is the difference between image A and B?
3) What is the difference between image A and C?
4) What is the difference between image D and E?5) How can these abnormalities be corrected?
8.1. Description of hydrocele
Learning Activity 8.1
H.K is a 5 years old boy was referred to the surgical OPD for urologist review on
20.5.2022 with swelling of right scrotum since 5 months. The mother complained
of swelling of right scrotum, which increased in size gradually. There was mild
pain when the swelling started. There was no history of fever or trauma when it
started. The physician performed trans-illumination test which become positive
and hydrocele was confirmed. The patient was scheduled for surgery to drain
the fluid accumulated in the scrotum under local anaesthesia using needle andsyringe.
Questions related to the case study
1) Identify the biography of the patient described in the case study.
2) What are the signs and symptoms described in the case study?
3) What is the probable surgical diagnosis of this H.K?
4) Which test performed to confirm surgical diagnosis described in the case
study?5) What was the management provided for this patient H.K?
8.1.1. Definition of hydrocele
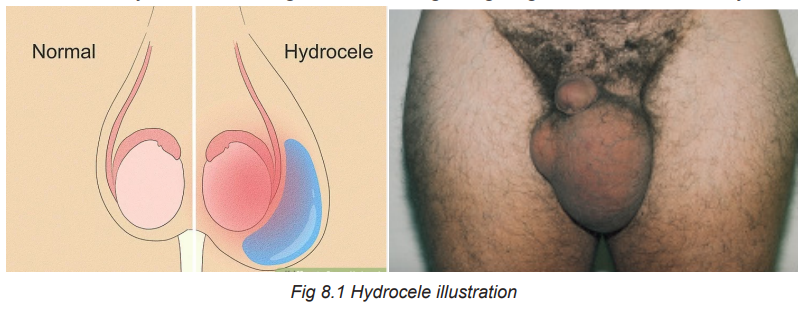
A hydrocele is a non-tender, fluid-filled mass that results from interference with
lymphatic drainage of the scrotum and swelling of the tunica vaginalis that surrounds
the testis. Hydroceles vary greatly in size. Very large hydroceles are sometimesseen in elderly men and it might have been getting larger over a number of years.
8.1.2. Causes of hydrocele
Most hydroceles occur in adults and are most common in men aged over 40 years.
The causes of hydrocele is unknown in most of cases. A few cases of hydroceles
occur when something is wrong testicles. For instance, infection, inflammation,
injury or tumours involving the testes may cause fluid be accumulated which leads
to hydrocele formation.
8.1.3. Types of hydrocele
Communicating hydrocele
In communicating hydrocele the opening does not close and fluid is able to go backbetween abdominal cavity and scrotal cavity.
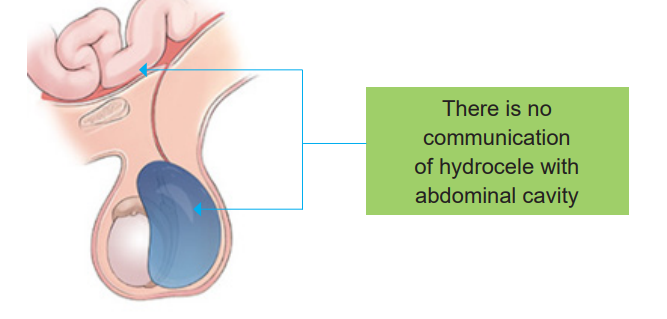
Non-communicating hydrocele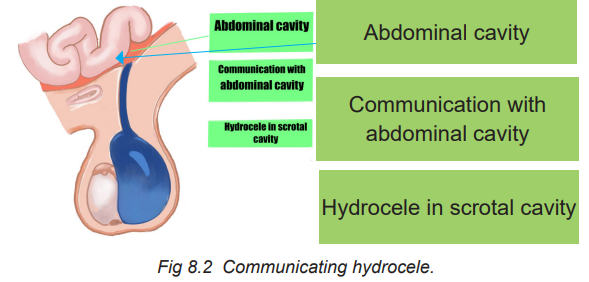
The open remains closed after the testicle is in the scrotum but there is fluid trapped
in the scrotum. This type is mostly found often in new-born and may take up to oneto resolve.
8.1.4. Signs and symptoms of hydrocele
Non-communicating hydrocele is characterized by a constant swelling.
On the other hand, in communicating hydrocele the swelling comes and goes
throughout the course of a day.Fluid around the testis does not usually cause pain or discomfort.
8.1.5. Diagnosis of hydrocele
Doctor uses the following modalities to diagnose hydrocele:
Doctors usually perform a physical examination for diagnosing Hydrocele. During
exam the doctor will not be able to feel the testicle well due to the presence of
fluid in the sac. Doctors will also check for tenderness in scrotum and shine a light
through the sac. This procedure is called “trans-illumination” and it allows the
doctor to determine presence of fluid. The scrotum will allow light transmission if
fluid is present. It will appear to light up with light passing through it. The light will
not shine through the scrotum if the swelling is due to solid mass. The doctor may
also perform an ultrasound to check for tumors, hernias or any other cause forswelling of the scrotum.
Ultrasound: This can help to check your testes to make sure if there aren’t otherunderlying causes of hydrocele.
8.1.6. Treatment plan of hydrocele
Two modalities of hydrocele management
A. Aspiration with needle and syringeB. Surgical management (hydrocelectomy)
A. Aspiration with needle and syringe
This procedure can be performed for non-communicating hydrocele once thescrotum become swollen.
B. Surgical management of hydrocele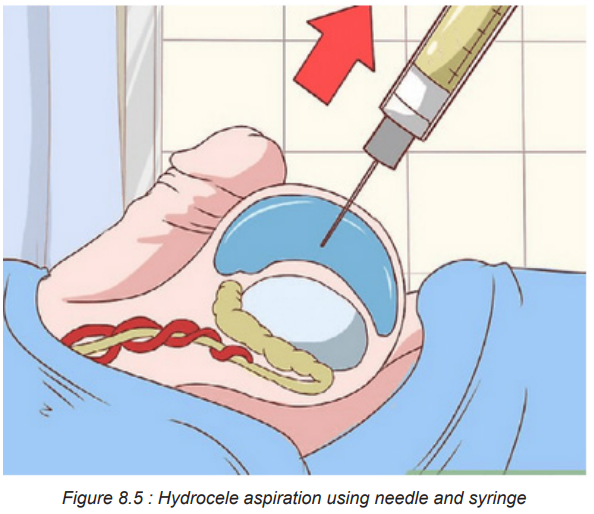
Non-communicating hydrocele: Normally resolve on its own over time and do not
require surgery. The surgery is required if swelling persists past 12 months of age.
Communicating hydrocele: This types, do not resolve on its own and it requires
surgery (hydrocelectomy). The surgery is recommended to decrease the chance of
a loop of bowel or abdominal contents getting stuck which could hurt the bowel and
the testicle. This surgery is done under anaesthesia and small incision is made inthe groin.

8.1.8. Complications and evolution of hydrocele
Left untreated Hydroceles can lead to infection of the fluid and testicular atrophy. A
large hydrocele may block the testicular blood supply leading to testicular atrophy
and subsequent impairment of fertility. Haemorrhage into the hydrocele can result
from testicular trauma. If a communicating hydrocele does not go away on its own
and is not treated, it can lead to an inguinal hernia. In this condition, part of the
intestine or intestinal fat pushes through an opening (inguinal canal) in the groin
area. The prognosis for congenital hydrocele is excellent. Most congenital cases
resolve by the end of the first year of life. Persistent congenital hydrocele is readily
corrected surgically.
Self-assessment 8.1
1) Define hydrocele
2) What are the signs and symptoms of hydrocele?
3) Differentiate communicating and non-communicating hydrocele.
4) How is trans-illumination test done?5) Outline three complications of hydrocele.
8.2. Description of Testicular torsion
Learning Activity 8.2
A 15 year-old male was admitted to the Emergency Department of a tertiary
Hospital presenting with a sudden and continuous pain in the left testicle. The
pain was progressive, radiated to the abdomen and left inguinal area, it was
accompanied with nausea and vomiting of more than 12 h since its onset. On
physical examination the left testicle was found to be larger in volume to the right
one, was painful, local temperature had risen and there was a negative Prehn
sign (exacerbation of pain upon elevation of the testicle on raising the affected
testicle). There was also an absence of the cremasteric reflex which is an
indicative of testicular torsion. Doppler ultrasound showed changes suggestive
of testicular torsion. Emergency surgery was performed on the day of admission
to correct this problem. This showed findings of a necrotic left testicle with a
360° rotation of the spermatic cord for which a left orchiectomy was performed.
The pathology study reported hemorrhagic testicular infarction. There were no
complications during recovery and the patient was discharged the day aftersurgery.
Questions related to the case study
1) Identify the biographic data of the patient from the case study above.
2) List the signs and symptoms presented by patient on his arrival to the
Emergency Department.
3) What are the findings identified by physician on physical examination?
4) What is the surgical diagnosis of this patient found on Doppler ultrasound?5) How was this surgical diagnosis corrected?
8.2.1. Definition of Testicular Torsion
Testicular torsion involves a twisting of the spermatic cord that supplies blood to thetestes and epididymis. It is most commonly seen in males younger than age 20.
8.2.2. Causes and pathophysiology of Testicular Torsion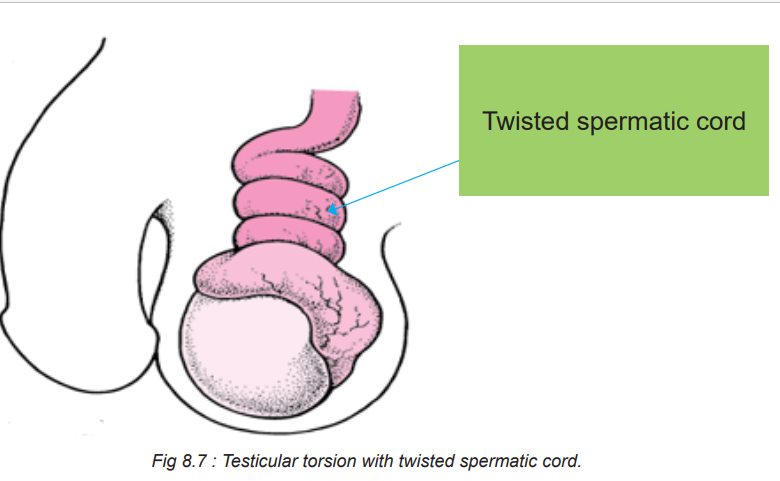
Testicular torsion can occur spontaneously, as a result of trauma, or as a result of
an anatomic abnormality. As the testicle twists around the spermatic cord, venous
blood flow is cut off, leading to venous congestion and ischemia of the testicle.
The testicle becomes tender, swollen, and possibly erythematous. As the testicle
further twists, the arterial blood supply is cut off which leads to further testicular
ischemia and eventually necrosis. In most individuals, the testicle rotates between
90-180 degrees and compromised blood flow. Complete torsion is rare and quickly
decreases the viability of the testes. The correction is possible if the torsion is lessthan 8 hours but rare if more than 24 hours have elapsed.
8.2.3. Signs and symptoms of Testicular Torsion
Signs and symptoms of testicular torsion include:
Unilateral scrotal pain: The pain may be constant or intermittent, but not positional.
Associated symptoms: Nausea and vomiting, abdominal pain and inguinal pain.
Scrotal swelling and erythematous.
The testicle may be in an abnormal or transverse lie and maybe in a high position.
Absence of cremasteric reflex (Stroking of the skin causes the cremaster muscle
to contract and pull up testicle toward the inguinal canal) but it is not reliable in
patients less than one year. In absence of cremasteric reflex, the stroke of skin willnot allow the pulling up of testicle towards inguinal canal.
The following chart summarizes the signs and symptoms of testicular torsion
8.2.4. Diagnosis of Testicular Torsion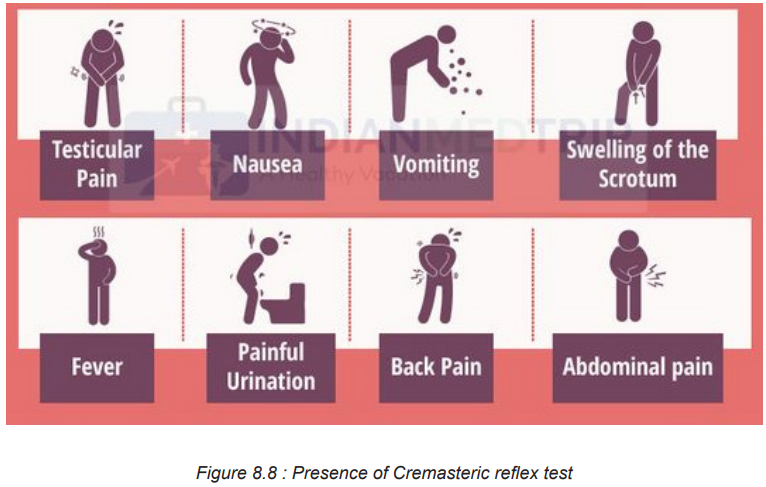
To diagnose testicular torsion, Doppler ultrasound is typically performed to assess
blood flow within the testicle. Decreased or absent blood flow confirms the diagnosis.
MRI and CT scan may also be performed. Although surgical exploration is invasive,
it remains the gold standard in the diagnosis of testicular torsion.
8.2.5. Treatment plan of Testicular Torsion
Manual detorsion
Manual detorsion was first described in 1893 to reverse ischemia and provide
instantaneous pain relief. This procedure may limit testicular infarction while
preparations are being made for surgical exploration. The procedure is done by
rotating the affected testicle at 180 degrees in clockwise direction. The procedure
may need to be repeated 2–4 times, as torsion can involve rotations of 180–720
degrees. Manual detorsion should be guided by instantaneous resolution of painand re-establishment of blood.
Surgical Exploration
Torsion constitutes a surgical emergency because, if the blood supply to the
affected testicle is not restored within 4 to 6 hours, ischemia to the testis will occur,
leading to necrosis and the possible need for removal. Unless the torsion resolves
spontaneously, surgery to untwist the cord and restore the blood supply must beperformed immediately

8.2.6. Complications and evolution of Testicular Torsion
The common complications of testicular torsion include the following:
• Loss of testis
• Infection
• Infertility
• Loss or diminished exocrine and endocrine function in men
Evolution of testicular torsion
Since many years ago there has been a markable improvement in the recovery of
the testes following torsion. However, poor results still occur especially in African
Americans, young patients, and those who lack health insurance. Better outcome
is obtained if the surgery is done within 8 hours. The outcomes of testicular torsion
depend on when the patient presents to the hospital and how quickly the diagnosis
is made and treatment is undertaken. Delays in diagnosis and treatment always
lead to testicular atrophy. About 20-40% of cases of testicular torsion result in an
orchiectomy. The risk of losing a testis is much higher among AfricanAmericans and
younger males. For those who present within the first 6 hours of symptoms, the
survival rate is nearly 100% but this number quickly drops to less than 50% if thedelay in seeking help is more than 12-24 hours.
8.3. End unit assessment
End of unit assessment
1) Define testicular torsion.
2) State two main causes of testicular torsion.
3) The following are the signs and symptoms of testicular torsion EXCEPT:
a) Scrotal pain
b) Nausea and vomiting
c) Scrotal swelling
d) Presence of cremasteric reflex
4) The following are complications of testicular torsion EXCEPT:
a) Loss of testis
b) Infection
c) Infertility
d) Increased exocrine and endocrine function in men
5) Identify which one among A and B is representing communicatinghydrocele and non-communicating hydrocele in the following illustrations:
6) What is the most common imaging study performed to diagnose a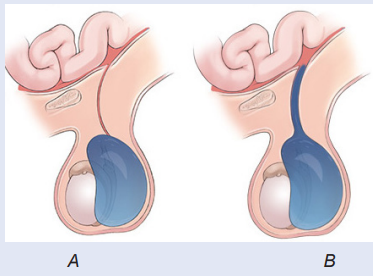
testicular torsion?
7) State two treatment modalities of hydrocele and testicular torsion foreach.
REFERENCES
1) Lewis, S. L., Dirksen, S. R., Heitkemer, M. M., & Linda Bucher. (2014).
MEDICAL-SURGICAL NURSING Assessment and mManagement of clinical
problems (NINTH). Canada: ELSEVIER MOSBY.
2) Williams, L. S., & Hopper, P. D. (2015). Understanding Medical Surgical
Nursing (Fifth edit). Philadelphia: F.A. Davis Company.
3) Hinkle, J. L., & Cheever, K. H. (2018). Brunner and Suddarth’s textbook of
medical-surgical nursing. Wolters kluwer india Pvt Ltd.
4) Winkelman, C. (2016). Medical-surgical nursing: Patient-centeredcollaborative care. Elsevier
