UNIT 7:PHIMOSIS AND PARAPHIMOSIS
Key Unit competence:Take appropriate decision on phimosis and paraphimosis
Introductory activity 7.0
The Image A, B, C and D illustrate the structures of male reproductive organs.Observe them and respond to the attached questions
1) What do you think on the figure A, B, C&D?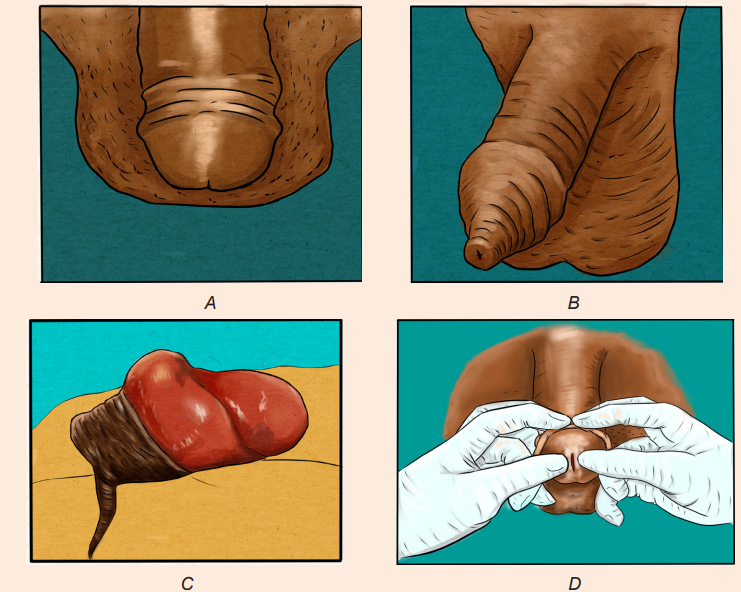
2) What are your observations on figures (A, B, C&D) would reflect the
abnormal structure of the male reproductive organ in humans?
3) What do you see in image B and C?
4) What is the difference between A and C?5) What do you think about that someone is doing in image D?
7.1. Description of Phimosis and Paraphimosis
Learning Activity 7.1
Miss D.K is associate nurse at one health facility in rural area of Rwanda.
During her night duty, she received Mr. M G, a 26 year’s old uncircumcised
male patient. He was complaining of foreskin scratching, painful urination and
painful erections. During history taking he reveals to nurse that he had inability
to pulldown the foreskin since birth and the same signs and symptom since 6
months ago. The nurse in charge of consultation examined him and a diagnosis
of phimosis was made and a rendez vous for circumcision was fixed on the
next 2 days. Arriving at home, he wanted to take shower before sleeping. While
performed genital hygiene, he tried to retract his prepuce for more visualization
but he failed to retract it back. Immediately he started to feel severe penile
pain and inability to pass urine as he felt something like a barrier to pass the
urine. During the physical exam of external genitalia, Nurse noticed that the
glans and the prepuce are inflamed, reddened. He is glans appears enlarged
and congested, with a collar of swollen foreskin around the coronal sulcus. At
this stage, the final diagnosis was made: patient was suffering from phimosis
complicated into paraphimosis. Finally, Nurse attempted the manual reduction
and failed. The decision for surgical treatment was made: Performance of sterile
circumsion under local anesthesia (emergency dorsal slit) and prescription ofpainkiller was done.
Questions related to the case study:
1) Basing on the case scenario, what are the causes and possible risk
factors which might probably exposed MG to this problem?
2) Identify the signs and symptoms Mr. MG presented at health facility
3) Why lab tests were not included in the diagnostic tests to find the diagnosis
of MG?
4) How nurse diagnosed the condition of Mr. MG?5) Which treatment did they provide to Mr. MG?
7.1.1 Definition and the Phimosis and Paraphimosis
Phimosis and paraphimosis are conditions that occur among uncircumcised male
clients when the opening of the foreskin is constricted. All these conditions affect
the penis foreskin.
Phimosis: is defined as the inability to retract the skin (foreskin or prepuce)
covering the head (glans) of the penis and leading to a tightness or constriction
of the foreskin around the head of the penis, making retraction difficult. Phimosis
may appear as a tight ring or “rubber band” of foreskin around the tip of the penis,preventing full retraction.
Physiologic VS Pathologic Phimosis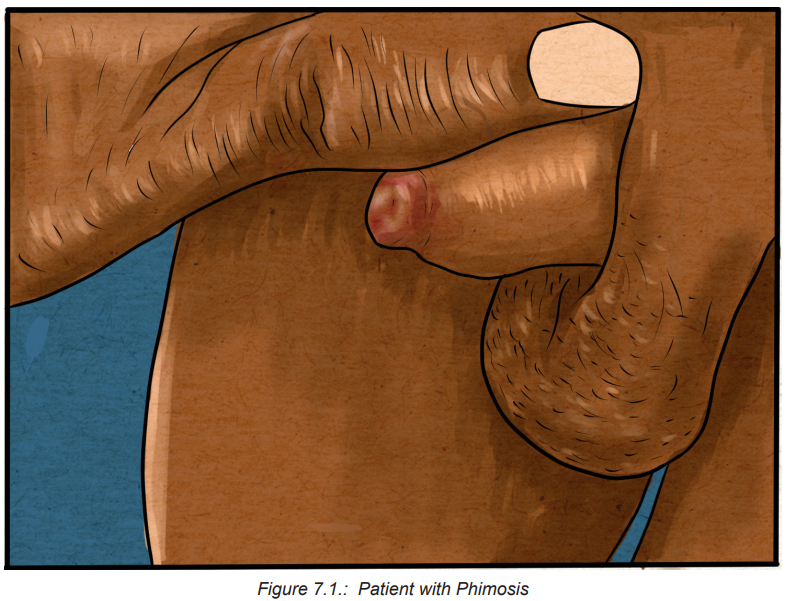
Depending on the situation, this condition may be considered either physiologic
or pathologic. Physiologic, or congenital, phimosis is a normal condition of the
newborn male and in children younger than 3 years of age, and may be a normal
finding up until the age of puberty while acquired (pathologic) phimosis is most
seen in post pubertal males, or in patients in whom scarring has developed from
chronic infection and inflammation (balanoposthitis), or as a result of repeated
forced retraction of congenital phimosis.
Smegma: is a collection of skin cells from the glans penis and inner foreskin that
is often noted with retraction of the foreskin. This natural skin shedding helps to
separate the foreskin from the head of the penis. Smegma may appear as white
pearls underneath the skin, which can easily be washed off once the foreskin is
retracted.
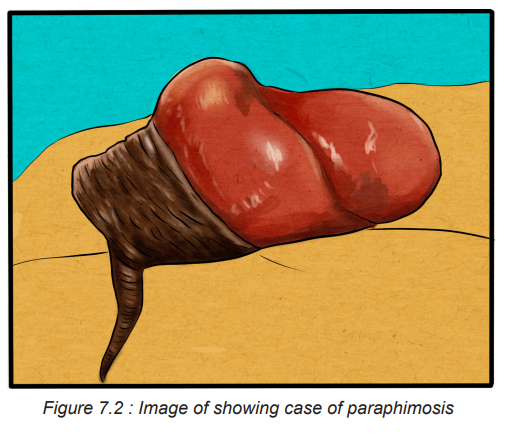
Paraphimosis: is a strangulation of the glans penis from an inability to replace the
retracted foreskin. It is a urologic emergency, occurring in uncircumcised males, in
which the foreskin becomes trapped behind the corona and forms a tight band ofconstricting tissue
7.1.2 Causes and risks factors and the Phimosis and Paraphimosis
Phimosis is a tightness or constriction of the foreskin around the head of the penis,
making retraction difficult, is caused by edema or inflammation of the foreskin,
usually associated with poor hygiene techniques that allow bacterial and yeast
organisms to become trapped under the foreskin. Congenital phimosis is expected
in children younger than 3 years of age, and may be a normal finding up until the
age of puberty. These phimotic conditions often are caused by a congenitally small
foreskin; however, chronic inflammation at the glans penis and prepuce secondary
to poor hygiene or infection also are etiologic factors.
Beside poor hygiene in young children others various reasons may also contribute
to development of phimosis including:
• Skin conditions such as eczema, psoriasis, lichen planus and lichen sclerosus.
When it affects the penis, lichen sclerosis is known as penile lichen sclerosis
or balanitis xerotic obliterans (BXO).
• Preputial adhesions, or scar tissue, that keep the foreskin attached to the tip
(glans) of your penis.
• Injuries.
• Infections, including sexually transmitted infections (STIs).
The cause of paraphimosis is most often iatrogenic. The condition is frequently
occurring after penile examination, urethral catheterization or cystoscopy.
Paraphimosis typically occurs after Foley catheter placement. Rare causes of
paraphimosis include self-inflicted injury to the penis (such as piercing a penile ringinto the glans) and paraphimosis secondary to penile erections
7.1.3 Pathophysiology and Types of Phimosis and Paraphimosis
When the foreskin becomes trapped behind the corona for a prolonged time, it
may form a tight, constricting band of tissue. This circumferential ring of tissue can
impair the blood and lymphatic flow to and from the glans and prepuce. As a result
of penile ischemia and vascular engorgement, the glans and prepuce may become
swollen and edematous. If left untreated, penile gangrene and auto amputation
may follow in days or weeks. Phimosis is divided into two forms: physiologic and
pathologic phimosisis.
Physiologic phimosis: Children are born with tight foreskin at birth and separation
occurs naturally over time. Phimosis is normal for the uncircumcised infant/child
and usually resolves around 5-7 years of age, however the child may be older.
Pathologic phimosis: Phimosis that occurs due to scarring, infection or
inflammation. Forceful foreskin retraction can lead to bleeding, scarring, and
psychological trauma for the child and parent. If there is ballooning of the foreskin
during urination, difficulty with urination, or infection, then treatment may be
warranted.
7.2 Signs and Symptoms of Phimosis and Paraphimosis
Clients with phimosis report pain with erection and intercourse and difficulty cleaning
under the foreskin.
Clients with paraphimosis often presents with penile pain. However, pain may
not always be present. The glans appears enlarged and congested, with a collar
of swollen foreskin around the coronal sulcus. If the condition continues, severe
edema and urinary retention may occur. A tight, constricting band of tissue appearsimmediately behind the head of the penis as shown in the figure below.
The physical examination should focus on the penis, urethral catheter (if present)
and scrotum. The penis should be inspected for the presence of foreskin, the color
of the glans, the degree of constriction around the penile corona and turgor of the
prepuce. Absence of foreskin excludes the diagnosis of paraphimosis. A pink orsalmon hue to the glans indicates a good blood supply.
Self-assessment 7.1
1) What are the signs and symptoms of paraphimosis?
2) Briefly explain the pathophysiology of the paraphimosis?
3) Differentiate Physiologic phimosis from pathologic phimosis4) List the risks factors associated to paraphimosis?
7.4 Treatment plan of Phimosis and Paraphimosis
Treatments for phimosis and paraphimosis vary depending on the child and
severity of phimosis. It involves reducing the penile edema and restoring the
prepuce to its original position and may include: gentle daily manual retraction,
topical corticosteroid ointment and application or circumcision. Several noninvasive
or minimally invasive methods are used to reduce the penile swelling, but due to
extreme pain patients may require a penile nerve block or topical analgesic or oralnarcotics before penile manipulation.
• Manual reduction of phimosis and Paraphimosis:
The goal of treatment is to return the foreskin to its natural position over the glans
penis through manual reduction. Manual pressure may reduce edema. A gloved
hand is circled around the distal penis to apply circumferential pressure and disperse
the edema. One strategy involves pushing the glans back through the prepuce by
applying constant thumb pressure while the index fingers pull the prepuce
over the glans. Ice and/or hand compression on the foreskin, glans, and penis
may be done before this technique to reduce edema. Topical corticosteroid cream
applied two or three times daily to the exterior and interior of the tip of the foreskinmay also be effective.
Ice packs are also useful in reducing swelling of the penis and prepuce. The penis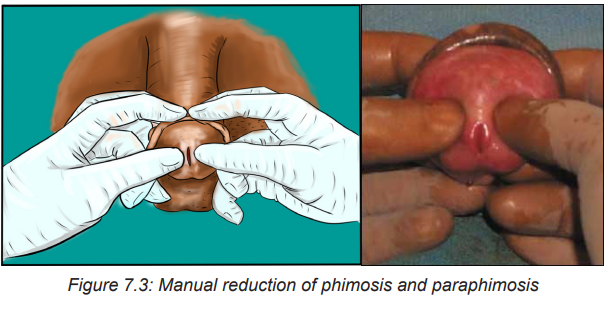
is first wrapped in plastic, with ice packs applied intermittently until the swelling
subsides .To reduce edema, a compressive elastic dressing is then wrapped
circumferentially around the penis from the glans to the base. This dressing
should be left in place for five to seven minutes, and the penis should be checked
periodically to monitor the resolution of swelling. Once the swelling has subsided,
the wrap should be removed.
• Pharmacologic therapy
Injection of hyaluronidase into the edematous prepuce is effective in resolving
edema and allowing the foreskin to be easily reduced. Degradation of hyaluronic
acid by hyaluronidase enhances diffusion of trapped fluid between the tissue planes
to decrease the preputial swelling. Hyaluronidase is well suited for use in infants
and children.
Granulated sugar has shown to be effective in the treatment of paraphimosis based
on the principle of fluid transfer occurring through osmotic gradient. Granulated
sugar is generously spread on the surface of the edematous prepuce and glans.
The hypotonic fluid from the edematous prepuce travels down the osmotic gradient
into the sugar, reducing the swelling and allowing for manual reduction. Both of the
procedures mentioned here should be performed by a physician experienced in
these techniques
• Minimally invasive therapy
The “puncture” technique is a minimally invasive therapy in which a hypodermic
needle is used to directly puncture the edematous prepuce. Puncture sites permit
safe and effective evacuation of the trapped fluid. External drainage of the trapped
fluid allows for manual reduction of paraphimosis.
Blood aspiration of the tourniqueted penis may be attempted .The base of the penis
is temporarily tied off with a rubber tourniquet. An 18-gauge needle is inserted
into the penis, and corporal blood is aspirated to reduce penile swelling. These
techniques should only be performed by a physician experienced in the procedures.
N.B: All of these techniques are geared toward reducing the swelling so that
manual reduction can be performed.
After the preputial swelling has subsided, paraphimosis is reduced .To reduce the
prepuce, the thumbs of both hands are placed on the glans and the fingers wrap
behind the prepuce. A gentle but steady and forceful pressure is applied to the glans
with the thumbs, and counter traction is applied to the foreskin with the fingers as
the prepuce is pulled down. When performed properly, the constricting band oftissue should come down distal to the glans with the prepuce.
• Surgical therapy
Severe constricting band of tissue precludes all forms of conservative or minimally
invasive therapy, an emergency circumcision dorsal slit type is recommended to
relieve these conditions permanently .This procedure should be performed with
the use of a local anesthetic by a physician or a trained health care personnel
experienced with the technique. Circumcision, a definitive therapy, should be
performed at a later date to prevent recurrent episodes, regardless of the methodof reduction used.
7.4 Evolution and complications of Phimosis and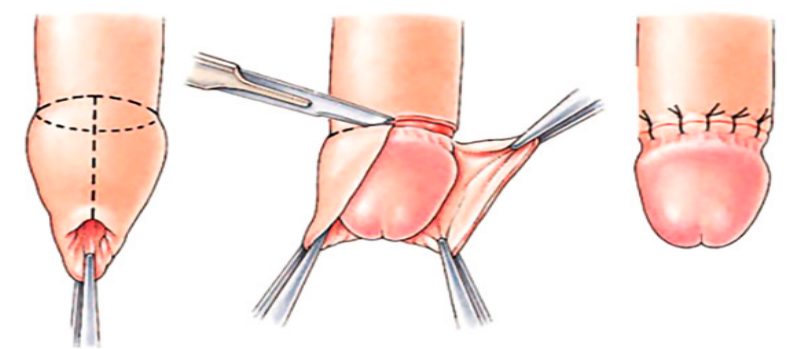
Paraphimosis
The prognosis for phimosis is usually very good. A small amount of bleeding can
occur as the skin is retracted but long term negative outcomes are very rare.
Complications of phimosis include balanitis, posthitis, paraphimosis, voiding
dysfunction, painful erection and penile carcinoma. Patients may present with
complaints of erythema, itching, discharge, or pain with sexual intercourse.
The prognosis for paraphimosis depends on the speed of diagnosis and reduction
constricting band of tissue. With prompt treatment, the outlook is excellent.
But without effective or delayed treatment, complications that can occur with
paraphimosis will range from mild to severe and life threatening condition. These
include pain, infection, and inflammation of the glans penis. If the condition is not
relieved in a sufficiently prompt timeframe, the distal penis can become ischemic
or necrotic. When this happens, paraphimosis can result in: a severe infection,
damage to the tip of the penis, gangrene, or tissue death, resulting in the loss of
the tip of the penis.
7.6 End unit assessment
1) Which patient is at the greatest risk for developing Paraphimosis
condition?
a) Circumsed Patient with chronic sexual transmitted diseases
b) Patient with urinary tract infection
c) A 17-year-old man with pre-existence congenital phimosis
d) A 65-year-old circumcised patient with urinary incontinence
2) What is the most important cause of the paraphimosis among the
following?
a) Skin conditions such as eczema, psoriasis and lichen planus
b) Iatrogenic cause like urethral catheterization or cystoscopy.
c) Injury to genital organ
d) Multiple Sexual activity
e) for cirumsed men
3) List the 4 components of treatment plan for phimosis and paraphimosis
4) Explain the importance of pain killer before manual reduction of
paraphimosis.
5) Explain the goal of manual reduction of phimosis and paraphimosis.
6) What can you do to reduce edema if you are called to care for patient with
paraphimosis?
7) When surgical therapy will be decided in case of paraphimosis?
8) What can be done to prevent complications to paraphimosis?9) List 4 complications of phimosis and paraphimosis?
