UNIT4:HERNIAS
Key Unit competence:
Take appropriate decision on Hernia
The below images illustrate different structures including esophagus, stomach,
diaphragm (A, B, C) umbilicus (D) and inguinal area (E). Observe them andrespond to the questions attached.
1) Identify normal and abnormal structures among the images above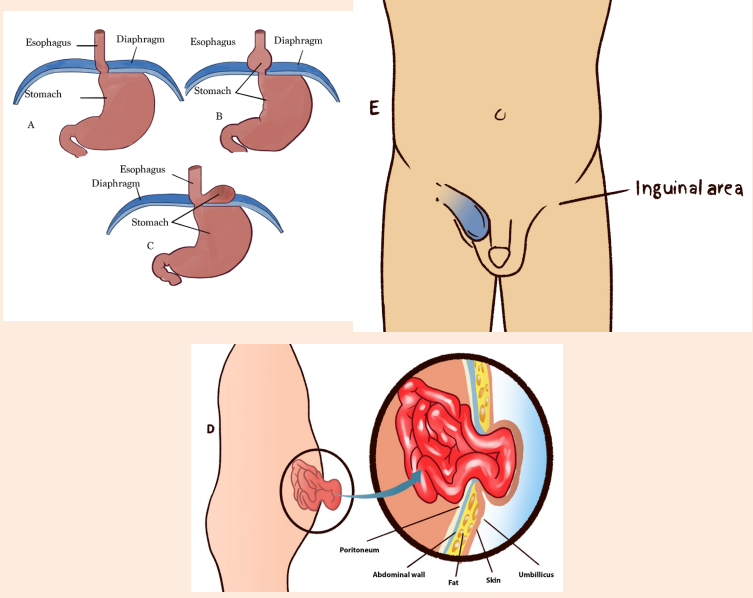
2) What is the common characteristic of the abnormal structures?
3) What could be the causes of such abnormalities?
4) What are the manifestations of such abnormalities in the human body?
5) How can health personnel identify or notice these abnormalities?6) How can these abnormalities be corrected?
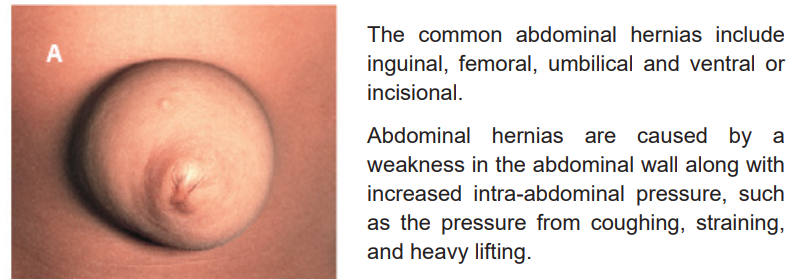
4.1. Abdominal hernias
Learning Activity 4.1
Mr. Y.A. 65 years old male, a laborer in a sawmill with low socioeconomic status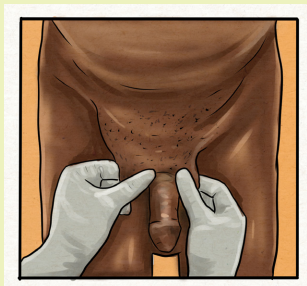
visits the hospital with chief complaints of swelling of about 10cm in right groin
since 3 years and pain in the right groin since 6 months. In the history, patient
was apparently well 3 years back, he noticed a swelling in right groin while
coughing which was initially small size (3cm) gradually increasing to present
size and reaching up to the scrotum. Mr. Y.A states that the swelling increases
when standing, coughing and lifting heavy weights. It decreases on lying down
and disappear on manipulation (pushing it using his fingers). Y.A has a history of
chronic cough with sputum since 20years but no history of chronic constipation
or urinary problems. Mr. Y.A is a known case of COPD on bronchodilators since
20 years, has habit of smoking, non-alcoholic, non-vegetarian diet, bowel and
bladder habits-regular. No history of similar history in his family. He regular takes
levasalbutamol inhaler since 20 years. No history of any allergy. On physical
examination; normal vital signs, a swelling of size 6x3cm is present above and
medial to the pubic tubercle extending into the scrotum up to upper pole of right
testis.
After taking history and performing physical exam, the health personnel confirmedinguinal hernia and planned a surgical treatment.
Questions related to the case study.
1) Based on the history of Y.A, what are the contributing factors of inguinal
hernia?
2) What are the signs and symptoms of inguinal hernia?
3) How inguinal hernia be diagnosed?4) What is the treatment adopted by the health personnel?
4.1.1 Definition of abdominal hernias
A hernia is an abnormal protrusion of an organ or structure through a weakness or
tear in the wall of the cavity normally containing it. Abdominal hernias are defined
as the abnormal protrusion of intra-abdominal contents through congenital/acquiredareas of weakness in the abdominal wall
4.1.2 Types of abdominal hernias
Ventral or incisional hernias are due to weakness of the abdominal wall at the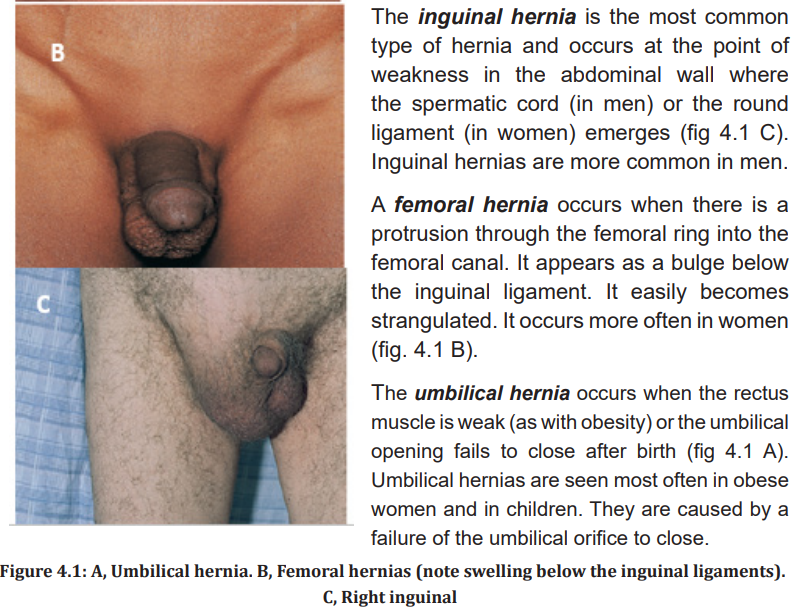
site of a previous incision (fig 4.2). They occur most commonly in patients who
are obese, have had multiple surgical procedures in the same area, or have hadinadequate wound healing because of poor nutrition or infection.
Hernias that easily return to the abdominal cavity are called reducible. The hernia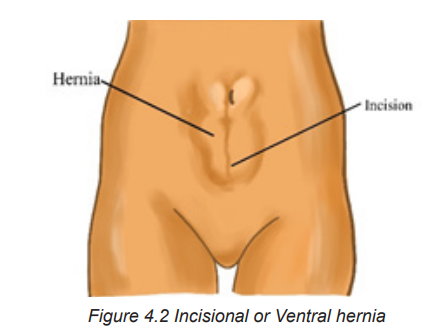
can be reduced manually or may reduce spontaneously when the person lies down.
If the hernia cannot be placed back into the abdominal cavity, it is known as irreducible
or incarcerated. In this situation the intestinal flow may be obstructed. When the
hernia is irreducible and the intestinal flow and blood supply are obstructed, the
hernia is strangulated. The result is an acute intestinal obstruction.
4.1.3 Clinical manifestations of abdominal hernias
An abdominal hernia may be readily visible; an abnormal bulging can be seen in
the affected area of the abdomen, especially when straining or coughing. There
may be some discomfort as a result of tension. If the hernia becomes strangulated,
the patient will have severe pain and symptoms of a bowel obstruction such as
vomiting, cramping abdominal pain, and distention. Strangulated hernias are painful
and inflamed hernias that cannot be reduced, they require emergency surgery.
4.1.4. Diagnostic measures
Abdominal hernias are mainly diagnosed based on history, physical examination
and ultrasound.
4.1.5 Therapeutic Measures
Treatment options include no treatment, observing the hernia, using short-term
support devices, or surgery to cure the hernia. A supportive truss or brief applies
pressure to keep the reduced hernia in place. Emergency surgery is needed for
strangulation or the threat of bowel obstruction. Surgical repair is recommended
for inguinal hernias. Surgical procedures are most often done laparoscopically
and include hernioplasty (open or laparoscopically) or herniorrhaphy (open hernia
repair).
Herniorrhaphy involves making an incision in the abdominal wall, replacing the
contents of the hernial sac, sewing the weakened tissue, and closing the opening.
Hernioplasty involves replacing the hernia into the abdomen and reinforcing the
weakened muscle wall with wire, fascia, or mesh. Bowel resection or a temporary
colostomy may be necessary if the hernia is strangulated.
Postoperative Care
Care following inguinal hernia repair is generally similar to any abdominal
postoperative care. Patients can perform deep breathing to keep lungs clear
postoperatively but should avoid coughing. Coughing increases abdominal
pressure and could affect the hernia repair. Teach patients to splint the incision
and keep their mouths open when coughing or sneezing are unavoidable. The
male patient may experience swelling of the scrotum. Ice packs and elevation of
the scrotum may be ordered to reduce the swelling. Because most patients are
discharged the same day of surgery, they are taught to change the dressing and
report difficulty urinating, bleeding, and signs and symptoms of infection, such as
redness, incisional drainage, fever, or severe pain. The patient is also instructed to
avoid lifting, driving, or sexual activities for 2 to 6 weeks. Most patients can return
to nonstrenuous work within 2 weeks.
After a hernia repair, the patient may have difficulty voiding. Measure intake and
output and observe for a distended bladder. Scrotal edema is a painful complication
after an inguinal hernia repair. A scrotal support with application of an ice bag mayhelp relieve pain and edema. Encourage deep breathing, but not coughing.
4.1.6 Associate nurse decision making
The associate nurse has to recognize the signs and symptoms of hernias and the
strangulated hernias for better referring. A post-operative teaching plan is also
important and includes the above measures mentioned in post-operative care.
4.1.8 Complications
An incarcerated hernia may become strangulated if the blood and intestinal flow are
completely cut off in the trapped loop of bowel. Strangulated hernias do not develop
in adults very often. Incarceration leads to an intestinal obstruction and possibly
gangrene and bowel perforation. Symptoms are pain at the site of the strangulation,nausea and vomiting, and colicky abdominal pain.
Self-assessment 4.1
1) What are the types of abdominal hernias?
2) Identify the common factors associated with abdominal hernia3) What are the signs and symptoms of a complicated hernia?
4.2 Hiatal hernia
Learning Activity 4.2
P.F, a 56-year-old male consults the health facility experiencing pain about 2-3cm
beneath his sternum and sharp pains in radiating towards his left shoulder. The
pain varies in intensity and is increased immediately after eating spicy foods.
After most meals, he suffers from mild heartburn. He said that the health
personnel initially prescribed a two week course of Omeprazole, which alleviated
the symptoms, but they returned after a few days.
The physical examination does not disclose any strong evidence. The patient is
obese, lacks regular physical activities and poor diet. All other findings are within
normal limits.
The medical doctor requested some diagnostic studies including an esophagram
(barium swallow) and an endoscopy to visualization the lower esophagus. The
results of these tests showed that there is a bulging mass in the low part of
the esophagus and confirmed that it was the stomach prolapsing through the
diaphragmatic esophageal hiatus i.e. hiatal hernia. Considering that omeprazole
did not act before, the medical doctor proposed a surgical treatment that was
scheduled in 2 weeks. While waiting for the surgical intervention, the patient was
taught to observe some conservative treatment including:
• Elevation of head of bed
• Avoid reflux-inducing foods (fatty foods, chocolate, peppermint)
• Avoid alcohol
• Reduce or avoid acidic pH beverages (red wine, orange juice)
• Antacids were prescribed (omeprazole)
Questions related to the case study.
1) Identify the biography of the patient described in the case study
2) What is the medical history of patient described in the case study?
3) Describe the signs and symptoms that the patient present and are
described in the case study
4) What are the diagnostic studies?5) What was the proposed management plan?
4.2.1 Definition of hiatal hernia
Hiatal hernia is a condition in which the stomach slides up through the hiatus of
the diaphragm into the thorax. It is also referred to as diaphragmatic hernia andesophageal hernia.
4.2.2 Causes and pathophysiology of Hernia
Many factors contribute to the development of hiatal hernia. Structural changes,
such as weakening of the muscles in the diaphragm around the esophagogastric
opening, occur with aging. Factors that increase intraabdominal pressure, including
obesity, pregnancy, ascites, tumors, intense physical exertion, and heavy lifting ona continual basis, may also predispose patients to development of a hiatal hernia
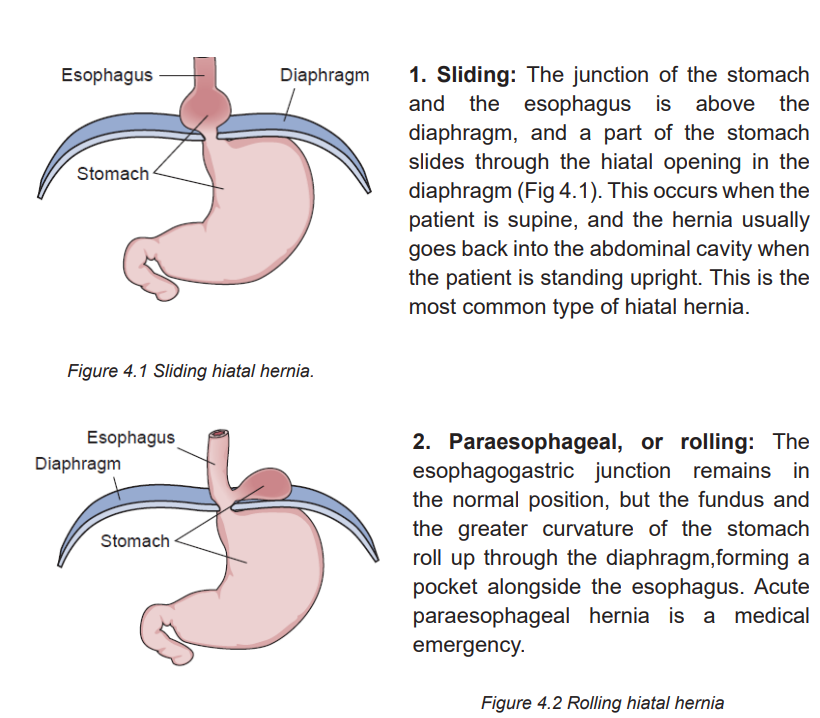
Hiatal hernias are classified into the following two types:
4.2.3 Signs and symptoms of Hernia
A small hernia may not produce any discomfort or require treatment. However, a
large hernia can cause pain, heartburn, a feeling of fullness, or reflux (regurgitation),
which can injure the esophagus with possible ulceration and bleeding.
The chest pain can mimic angina and is described as burning; squeezing; or radiating
to the back, neck, jaw, or arms. Complaints of chest pain are more common in
older adults with hiatal hernia or gastro esophagus reflux (GERD) disease. Unlike
angina, hiatal hernia and GERD-related chest pain is relieved with antacids.
4.2.4 Diagnostic measures
An x-ray studies such as an esophagram (barium swallow) may show the protrusion
of gastric mucosa through the esophageal hiatus. Endoscopic visualization of the
lower esophagus provides information on the degree of mucosal inflammation or
other abnormalities.
4.2.5 The management of Hernia
Conservative treatment includes lifestyle changes to alleviate symptoms of hiatal
hernia; losing weight, taking antacids, eating small meals that pass easily, through
the esophagus, not reclining for 3 to 4 hours after eating, elevating the head of the
bed 6 to 12 inches to prevent reflux, and avoiding bedtime snacks, spicy foods,alcohol, caffeine, and smoking.
4.2.6. Complications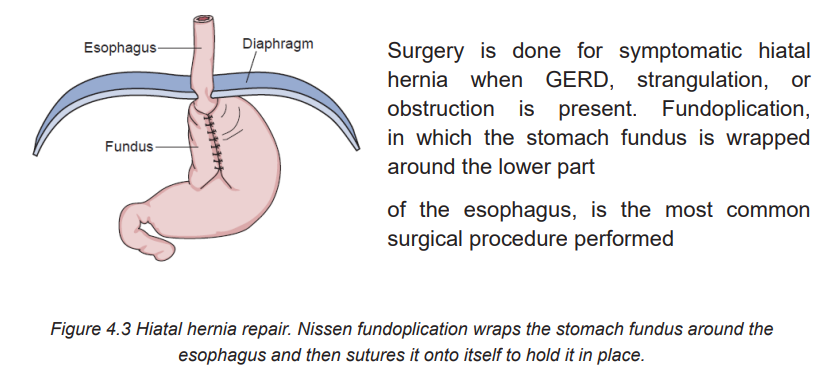
A paraesophageal hernia is rarer but serious as part of the stomach squeezesthrough the hiatus and is at risk for strangulation (blood supply is cut off).
4.2.7. Associate nurse decision making
In the hospital, the associate nurse will perform tasks that are delegated by registered
nurses. The primary focus of care for hiatal hernia disease is educating patients.
The teaching guide will include detail the following: The patient is taught lifestyle
interventions to reduce the symptoms of hiatal hernia. If the patient undergoes
surgery, general postoperative nursing care is provided. In addition,
following fundoplication, patients are assessed for dysphagia during their first
postoperative meal. If dysphagia occurs, the physician should be notified becausethe repair may be too tight, causing obstruction of the passage of food.
Self-assessment 4.2
1) Explain the types of hiatal hernia
2) What are other diseases that can mimic the signs and symptoms ofhiatal hernia?
4.3 End unit assessment
End of unit assessment
1) How should the nurse teach the patient with a hiatal hernia or GERD to
control symptoms?
a) Drink 295 to 355ml of water with each meal.
b) Space six small meals a day between breakfast and bedtime.
c) Sleep with the head of the bed elevated on 4- to 6-inch blocks
d) Perform daily exercises of toe-touching, sit-ups, and weight lifting.
2) The patient calls the clinic and describes a bump at the site of a previous
incision that disappears when he lies down. The nurse suspects that this
is which type of hernia (select all that apply)?
a) Ventral
b) Inguinal
c) Femoral
d) Reducible
e) Incarceratedf) Strangulated
3) The patient asks the nurse why she needs to have surgery for a femoral,
strangulated hernia. What is the best explanation the nurse can give the
patient?
a) The surgery will relieve her constipation.
b) The abnormal hernia must be replaced into the abdomen.
c) The surgery is needed to allow intestinal flow and prevent necrosis.
d) The hernia is because the umbilical opening did not close after birth as
it should have.
4) What are the most frequent symptoms of abdominal Hernia?
5) What are the diagnostic measures of hiatal hernia?
6) What are the do’s and don’ts after inguinal hernia surgery?
