UNIT3:INTESTINAL OBSTRUCTION
Key Unit competence:
Take appropriate decision on intestinal obstruction
Introductory activity 3.0
Observe the segments of the intestines presented in figure A, B, C and D andrespond to the questions below.
1) What do you think is happening to these segments of the intestines?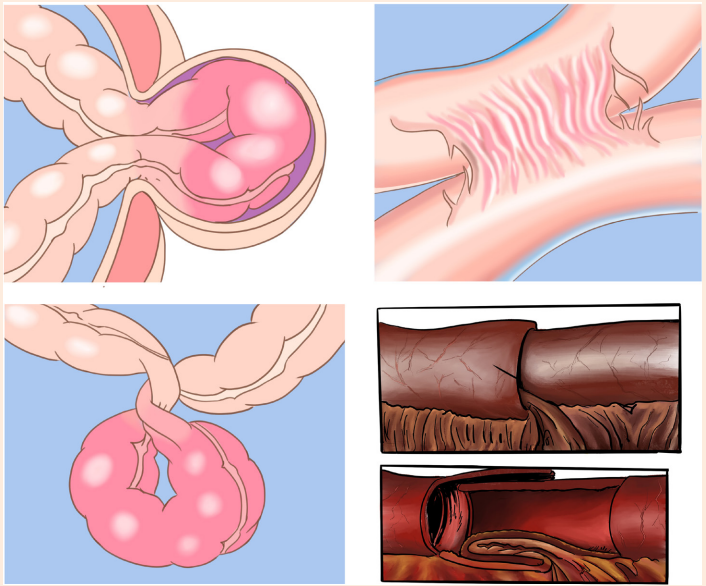
2) Is there any difference between four figures? Describe the differences
observed.
3) Reference to what you leant in anatomy and physiology, what are the
implications of such structures on food digestion?
4) What are other manifestations of such structures to the human body?
5) How can health personnel identify these structures?6) How can these segments be corrected?
3.1. Description of intestinal obstruction
Learning Activity 3.1
L.A, a 59-year-old woman was brought to the hospital with a 3-day history of
complete constipation and faeculent vomiting. She had no other medical or
surgical history and was not taking any regular medications. She lived at home
with sister and required assistance with several activities of daily living, however,
she was able to eat oh her own. On examination, her abdomen was extended
and mildly tender in the right iliac fossa, but there was no guarding or peritonism.
Chest and cardiac examination revealed tachycardia (115bpm), BP 139/102
mmHg, RR 18, T0 37.10C and saturation 98% on room air. The medical doctor
prescribed the following investigations: blood sample, abdomen x-rays and CT
scan. The results showed an increase of WBCs, urea and creatinine. A relatively
gasless abdomen with few dilated loops of small bowel was observed in the
results of X-rays. The CT scan showed small bowel obstruction within the mid
small bowel loop with the possibility of ischaemia of the small bowel loop. Therewas no evidence of bowel operation.
Questions related to the case study
1) What is the intestinal obstruction?
2) Briefly describe the pathophysiology of intestinal obstructions
3) What are the key signs and symptoms of intestinal obstructions highlightedin the case study?
3.1.1. Definition of intestinal obstruction
Intestinal obstruction occurs when the contents of intestines fail to pass through the
bowel lumen. The obstruction may take place in both small or large intestines and
can be partial or complete.
3.1.2. Causes and pathophysiology of intestinal obstruction
The two types of intestinal obstruction are mechanical and non-mechanical.
Mechanical obstruction occurs when a blockage occurs within the intestine from
conditions causing pressure on the intestinal walls such as adhesions (B), twisting
or volvulus (C) of the bowel, intussusception (D), or strangulated hernia (A). Non
mechanical obstruction may result from a neuromuscular or vascular disorder.
Paralytic ileus (lack of intestinal peristalsis and bowel sounds) is the most common
form of non-mechanical obstruction.
When an obstruction occurs, fluid, gas, and intestinal contents accumulate proximal
to the obstruction, and the distal bowel collapses.
The proximal bowel becomes increasingly distended, and intraluminal bowel
pressure rises, leading to an increase in capillary permeability and extravasation of
fluids and electrolytes into the peritoneal cavity.
This accumulation of fluids in intestines and in peritoneal cavity causes a severe
reduction in circulating blood volume, hence hypotension, hypovolemic shock and
bowel ischemia.
When the distension is severe the segment of the bowel becomes gangrenous a
condition known as intestinal strangulation or intestinal infarction (figure 3.1)
If it is not corrected quickly, the bowel will rupture, leading to infection, septic shock,
and death. If the obstruction is below the proximal colon or in the large bowel which
is less common and not usually as dramatic as small-bowel obstruction, dehydration
occurs more slowly because of the colon’s ability to absorb fluid and distend well
beyond its normal full capacity.
If the blood supply to the colon is cut off, the patient’s life is in jeopardy because ofbowel strangulation and necrosis
3.1.3. Signs and symptoms of intestinal obstruction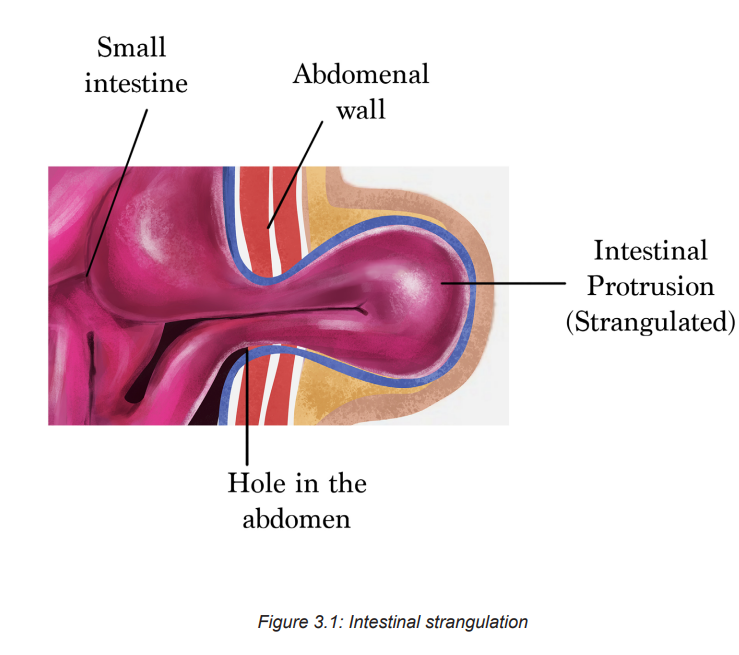
The clinical manifestations of intestinal obstruction vary, depending on its locationas displayed in table
! Consideration for practice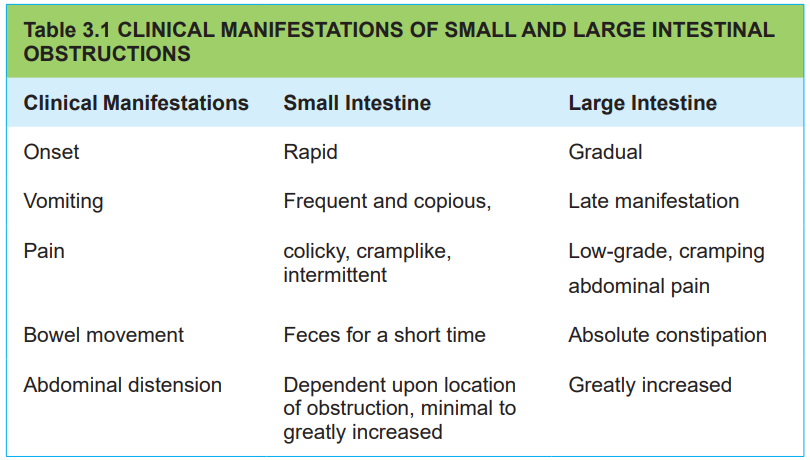
• Abdominal tenderness and rigidity are usually absent unless strangulation or
peritonitis has occurred.
• Auscultation of bowel sounds reveals high-pitched sounds above the area of
obstruction. Bowel sounds may also be absent.
• The patient often notes borborygmi (audible abdominal sounds produced by
hyperactive intestinal motility).
• The patient’s temperature rarely rises above 37.8° C unless strangulation or
peritonitis occurs.
• Promptly report any acute increase in abdominal, groin, perineal or scrotal
pain.
• An abrupt increase in the intensity of pain may indicate bowel ischaemia due
to strangulation.
3.1.4. Diagnostic measures of intestinal obstruction
A thorough history and physical examination. CT scans, abdominal x-rays,
Sigmoidoscopy or colonoscopy may provide direct visualization of an obstruction in
the colon. A FBC and blood chemistries may be performed. An elevated WBC count
may indicate strangulation or perforation. Elevated haematocrit values may reflect
hemoconcentration. Decreased hemoglobin and hematocrit values may indicate
bleeding from a neoplasm or strangulation with necrosis. Serum electrolytes, BUN,and creatinine are monitored frequently to assess the degree of dehydration.
Self-assessment 3.1
1) List different exams performed in order to diagnose intestinal obstruction
condition
2) What is the indication of frequent monitoring of electrolytes, BUN andcreatinine on patient suffering of intestinal obstruction?
3.2. The management of intestinal obstruction
Learning Activity 3.2
…Continuation of L.A case study
After different investigations, the medical doctor confirmed that LA is suffering
from intestinal obstruction. Intravenous catheter was inserted and IV fluids
administered; a decompressive nasal gastric tube was put in place and later
alone patient was taken to the theatre for surgery.
A laparotomy was performed and proved to be a single potato, measuring 4×3cm,
swallowed without chewing. The potato was extracted. In post-operative, the
medical doctor prescribed antibiotics, anti-emetics and pain control medications
and the patient was recovered well with no complications. The patient was
discharged with written letter to her sister regarding dietary advice. The patient
was subsequently followed up 8 weeks postoperatively and she was well.
Questions related to the case study1) What is the pre and post-operative treatment plan of Mrs. L.A?
3.2.1. The treatment plan of intestinal obstruction
The management of a bowel obstruction focuses on relieving the pressure and
obstruction and providing supportive care. The intestine is decompressed by NG
tube insertion and keeping the patient.Nothing by mouth (NPO), the dehydration
and electrolytes imbalances are corrected by administering fluid and electrolytes.
Surgery may be necessary to relieve a mechanical obstruction or if strangulation
is suspected. In post-surgery mouth care is performed, medications such as
antibiotics, antiemetics, and analgesics are administered. A teaching plan is also
elaborated.
Include the following topics when teaching a person with intestinal obstruction in
preparation for home care:
• Wound care
• Activity level,
• Return to work and any other recommended restrictions
• Recommended follow-up care
• Recurrent obstructions, explain their cause, early identification ofmanifestations and possible preventive measures.
3.2.2. Associate nurse decision making
An associate nurse who receives a patient with signs and symptoms of intestinal
obstruction must refer the case to the next level for adequate management. In the
hospital, the associate nurse works under supervision of registered nurses and
they will discuss the appropriate nursing care plan.
3.2.3. Complications of intestinal obstruction
Small intestines obstructions: Hypovolaemia and hypovolaemic shock with
multiple organ dysfunction is a significant complication of bowel obstruction and
can lead to death. Renal insufficiency from hypovolaemia leads to acute kidney
injury or dysfunction. Pulmonary ventilation may be impaired because abdominal
distension elevates the diaphragm, impeding respiratory processes. Strangulation
associated with incarcerated hernia or volvulus impairs the blood supply to the
bowel. Gangrene may rapidly result, causing bleeding into the bowel lumen and
peritoneal cavity and eventual perforation. With perforation, bacteria and toxins
from the strangulated intestine enter the peritoneum and, potentially, the circulation,
resulting in peritonitis and possible septic shock. Strangulation greatly increases
the risk of mortality.
Large intestines: If the ileocaecal valve between the small and large intestines is
competent, distension proximal to the obstruction is limited to the colon itself. This
is known as a closed-loop obstruction. It leads to massive colon dilation as the
ileum continues to empty gas and fluid into the colon. Increasing pressure within
the obstructed colon impairs circulation to the bowel wall. Gangrene and perforationare potential complications
Self-assessment 3.2
Mrs. LS is admitted for abdominal pain. She has a history of abdominal surgery.
Her abdomen is distended, firm, and tender to touch. She states that she feels
nauseated.
1) Is Mrs. L.S at risk for developing an intestinal obstruction?
2) How would the nurse know if Mrs. LS is at risk of developing a small bowel obstruction?
3.4. End of unit assessmentEnd of unit assessment
1) What are the common causes of intestinal obstruction?
2) What are the most common types of intestinal obstructions?3) What are the predicted complications on patient with intestinal obstruction?
