UNIT2:APPENDICITIS
Key Unit competence:
Take appropriate decision on appendicitisIntroductory activity 2.0
Observe the images A and B below illustrating the structures of appendix inhuman body.
1) Is there any difference between two appendixes?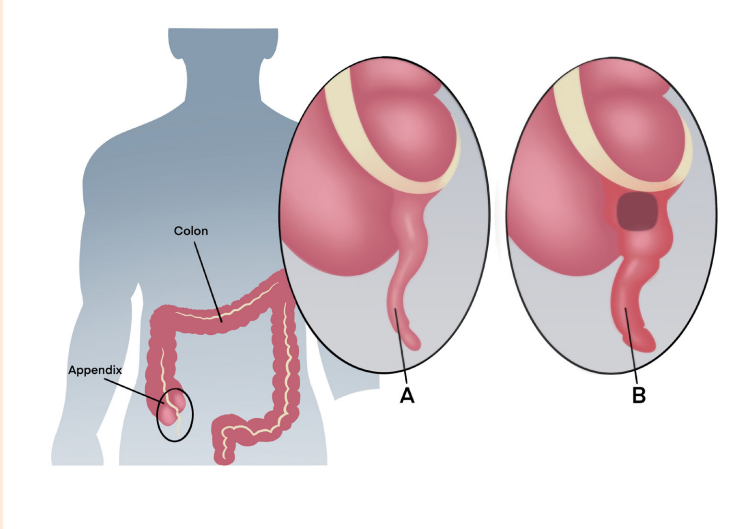
2) Which one of these two would reflect the normal structure of appendix in
the human body?
3) Describe the abnormalities that you have observed.
4) What do you think can cause the abnormalities that you have observed?
5) What are the manifestations of the observed abnormalities in the human
body?
6) How can health personnel identify these abnormalities?7) How can these abnormal structures be corrected?
2.1. Description of appendicitis
Learning Activity 2.1
M.H, a-13-year-old boy with history of constipation comes into the emergency
of referral hospital for severe abdominal pain. M.H reports that his abdomen
hurts for the past 24 hours. He notes that he initially suffered from mild pain
around his umbilicus last night and this morning he reported that the pain has
migrated to his right lower quadrant. He tells the nurse that the pain just keeps
getting worse and it is associated with nausea, vomiting and fever (39 degrees
Celsius). Upon physical assessment, M.H doesn’t allow anyone auscultate
or palpate his abdomen because of the pain. After 10 minutes he allowed the
nurse to do physical assessment. He is quite tender to mild palpation in the
right lower quadrant and he has muscle guarding. M.H prefers to lie still with the
right leg flexed. The medical doctor ordered blood sample to check the number
of WBCs. He also ordered ultrasound and CT scan. The blood test revealed
elevated WBC and neutrophil counts. An ultrasound and computed tomography
(CT) scan revealed an enlargement in the area of the cecum and appendicitis
was confirmed. Based on the case study narrated above, answer to the followingquestions.
Questions related to the case study
1) Identify the biography of M.H
2) What is the medical history of M.H?
3) Describe the signs and symptoms of M.H
4) What are the aggravating and relieving factors for M.H?5) What are the differential diagnosis M.H?
2.1.1. Definition of appendicitis
Appendicitis is inflammation of the appendix, a narrow blind tube that extends
from the inferior part of the cecum. Appendicitis, inflammation of the vermiform
appendix, is a common cause of acute abdominal pain and most common reason
for emergency abdominal surgery. It occurs at any age, but it is more common in
adolescents and young adults and slightly more common in males than females
2.1.2. Causes and pathophysiology of appendicitis
Because of the small size of the appendix, obstruction may occur, causing
inflammation and making it susceptible to infection. The obstruction is often caused
by a faecalith or hard mass of faeces. Other obstructive causes include a calculus
or stone, a foreign body, inflammation, a Tumor, parasites (e.g. pinworms) or
oedema of lymphoid tissue. Hereditary and family tendencies of appendicitis have
been noticed. Following obstruction, the appendix distends with fluid secreted by
its mucosa. As pressure within the lumen of the appendix increases, blood supply
is impaired, leading to inflammation, edema, ulceration and infection.
2.1.3. Signs and symptoms of appendicitis
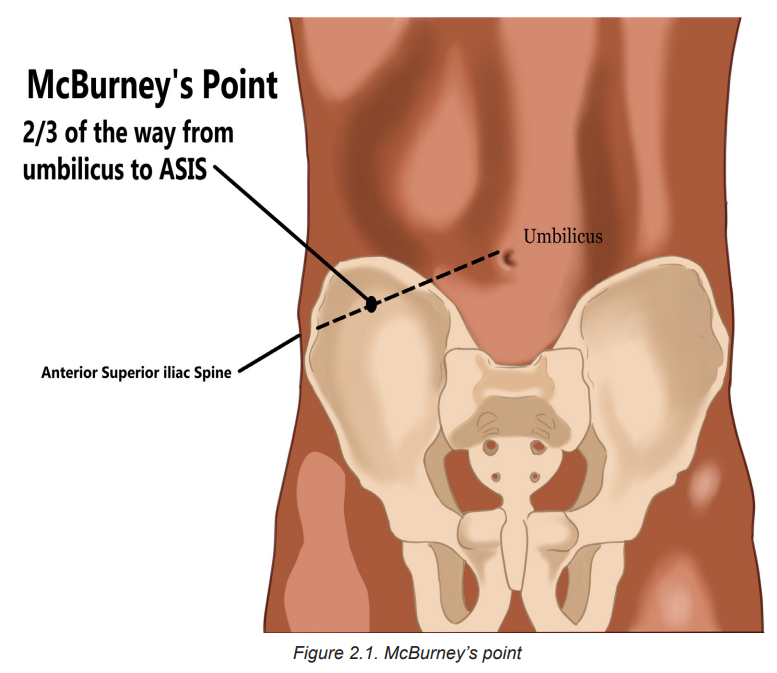
Signs and symptoms of appendicitis include fever, generalized pain in the upper
abdomen. Within hours of onset, the pain usually becomes localized starts on the
periumbilical area to the right lower quadrant at McBurney’s point, midway between
the umbilicus and the right iliac crest. This is one of the classic symptoms of
appendicitis. Nausea, vomiting, and anorexia are also usually associated. Physical
examination reveals slight abdominal muscular rigidity (guarding), normal bowel
sounds, and local rebound tenderness (intensification of pain when pressure is
released after palpation) in the right lower quadrant of the abdomen. The pain is
aggravated when patient straightens the leg, coughs, walks and makes any shaking
movement. The patient may keep the right leg flexed for comfort.
! Consideration for practice
• Sudden relief of preoperative pain may signal rupture of the distended and
edematous appendix.
• Assess abdominal status frequently, including distension, bowel sounds and
tenderness: Increasing generalized pain, a rigid, boardlike abdomen andabdominal distension may indicate developing peritonitis.
2.1.4. Diagnostic measures
The appendicitis can be diagnosed through a complete history, physical examination,
and a differential WBC count. The WBC count is mildly moderately elevated in most
cases. CT scan is the preferred diagnostic procedure, but ultrasound is also used. A
urinalysis is done to rule out genitourinary conditions that mimic the manifestations
of appendicitis. Other differential diagnostic includes intestinal obstruction,
inflammation and stones of gall bladder, stones in urinary organs such as ureter,
ruptured ovarian follicle, a ruptured tubal pregnancy, perforation of stomach orduodenal ulcer and inflammation of the right colon
Self-assessment 2.1
1) Who are people most likely to develop appendicitis?
2) Among the cells of WBC, which ones would increase in case ofappendicitis?
2.2. The management of appendicitis
Learning Activity 2.2
2.2.1. The treatment plan
The patient is kept NPO, and surgery (check appendectomy collaboration care in
box 2.1) is done immediately unless there is evidence of perforation or peritonitis.
Medications prior to surgery, intravenous fluids are given to restore or maintain
vascular volume and prevent electrolyte imbalance. Antibiotic therapy with a third
generation cephalosporin effective against many gram-negative bacteria, such as
cefotaxime (Cefotaxime Sandoz), ceftazidime (Fortum) or ceftriaxone (Rocephin)
is initiated prior to surgery. The antibiotic is repeated during surgery and continued
for at least 48 hours postoperatively. Post-operative analgesic medications are
administered as prescribed.
Following an uncomplicated appendectomy, the person is often discharged either
the day of, or the day following, surgery. Postoperative teaching includes:
• Wound or incision care, including hand hygiene and dressing change
procedures as indicated.
• Instructions to report fever, increased abdominal pain, swelling, redness,drainage, bleeding or warmth of the operative site to the doctor.
• Activity limitations (e.g. lifting, driving), if any.
• When it is appropriate to return to work.Summary of appendectomy care is indicated in table 2.1
2.2.2. Associate nurse decision making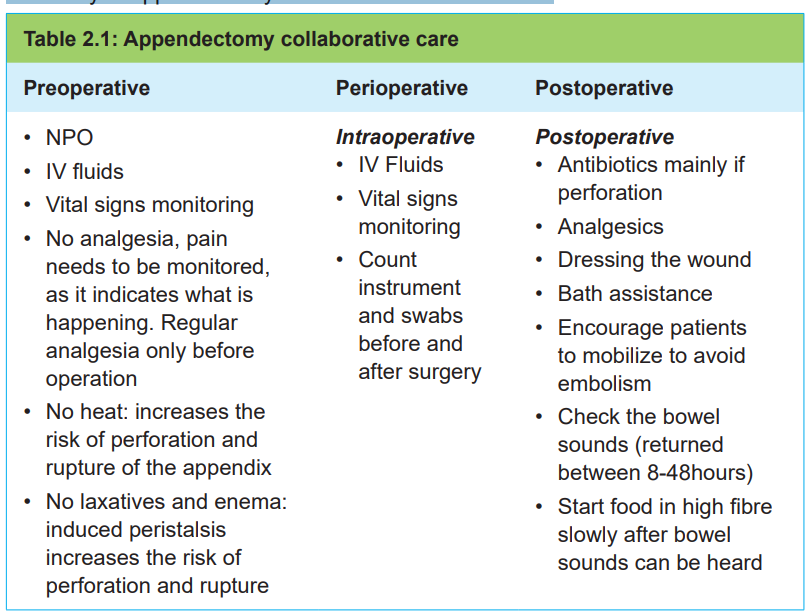
An associate nurse who receives a patient with signs and symptoms of appendicitis
must refer the case to the next level for adequate management. In the hospital, the
associate nurse works under supervision of registered nurses and they will discuss
the appropriate nursing care plan.
2.2.3. Complications of appendicitis
Most patients recover quickly after an appendectomy and frequently are discharged
from the hospital after few days. Preventing complications during the perioperative
period is a primary nursing care goal. Perforation and peritonitis are the most likely
preoperative complications. With perforation, the pain is severe, and temperature is
elevated to at least 37. 7°C. Postoperative complications include wound infection,abscess and possible peritonitis.
Self-assessment 2.2
1) What is the rationale of avoiding the use of warm/heating pads to relieve
the pain resulting from appendicitis?2) Explain the treatment options for a patient with appendicitis
2.3. End unit assessment
End of unit assessment
1) Within hours of onset, the pain of appendicitis usually becomes localized
starts on the ___________ area to the ___________ quadrant.
2) What are the diagnostic measures of appendicitis?
3) The patient has persistent and continuous pain at McBurney’s point. The
nursing assessment reveals rebound tenderness and muscle guarding
with the patient preferring to lie still with the right leg flexed. What should
the nursing interventions for this patient include? Choose the best answer
a) Laxatives to move the constipated bowel
b) NPO status in preparation for possible appendectomy
c) Parenteral fluids and antibiotic therapy for 6 hours before surgery
d) NG tube inserted to decompress the stomach and prevent aspiration
4) Appendicitis may occur:
a) After complications of an episode of flu
b) After complications of a viral infection of the digestive
c) After opening to the appendix becomes blocked by stool
d) After an enema to evacuate the stool
5) If you suspect the appendicitis, what type of medicine should you not
take?
a) Analgesics
b) Laxatives
c) Anti-inflammatory
d) Allergy medicines
6) BA 19-year-old student in her second year of a dental degree. BA arrives
at the emergency department at 0200hrs. She presents a general lower
abdominal pain which started the previous evening. She is also nauseated
and reports episodes of vomiting. The physical assessment reveals the
T 37. 8 o C, R 16, BP 110/70; abdomen flat and guarded. BA WBC was
14000/mm3
.
a) What are the missing characteristics/features of the abdominal pain to
confirm appendicitis?
b) What are the disturbed needs of BA?
c) Is appendectomy indicated for this patient? Justify your response7) List the complications of appendicitis
