UNIT 3: ANTIPROTOZOAL DRUGS
KEY UNIT COMPETE
Utilize antiprotozoal drugs to manage
different health condition at the primaryhealthcare settings
Introductory activity 3.0
1) The images above show two
different medications used in management
of protozoal diseases.
a) Have you ever seen or used any of the
medications above?
b) Which conditions does theabove medications are indicated?
3.1. Definition and Classification
of antiprotozoal medications
Learning Activity 3.1
Read the scenario below carefully and try
to find answers to the following
questions:
A client X was received at health post complaining
of fever, chills and arthralgia
for 3 days and diarrhea for 2 days.
The laboratory results reveal positive blood
smear and Entamoeba histolytica in the stool.
a) Read the book of pharmacology in the library,
and define antiprotozoal
medication and list the classes
of antiprotozoal drugs.b) Think about the drugs you can give to the patient X in the scenario.
CONTENT SUMMARY
Protozoans are single-celled organisms that are
the smallest and simplest members
of the animal kingdom. This topic will focus on
the chemotherapy to treat diseases
caused by Trypanosoma cruzi (Chagas’ disease),
Trypanosoma b. gambiense
and Trypanosoma b. rhodesiense (sleeping sickness),
Plasmodium (malaria),
Leishmania (leishmaniasis) and amebiasis.
Protozoal diseases are less easily treated
than bacterial infections because many
of antiprotozoal drugs cause serious toxic
effects and most of them are not safe
in pregnancy and unicellular protozoal cells
have metabolic processes closer to
human cells than bacteria.
Antiprotozoal drug is a drug that destroys protozoans,
inhibits their growth, ability to
reproduce and prevent the development
of protozoans in humans. The actions of
antiprotozoal drugs against the infections
are complex and are not fully understood.
Some of them may interfere with reproduction
of or damage protozoal DNA to
limit the spread of an infection.
Antiprotozoal drugs are classified into 2 classes:
antimalarial drugs and miscellaneous antiprotozoal.
Antimalarial drugs
Antimalarial drugs include mefloquine,
chloroquine, proguanil with atovaquone and
doxycycline.
They kill or inhibit the growth of protozoa
by affecting different stage of
the parasitic life cycle.
They are used both to treat and prevent malaria.
Miscellaneous antiprotozoal.
Commonly used miscellaneous antiprotozoal
include metronidazole, tinidazole
and so on. Metronidazole is the most common treatment
for trichomoniasis and giardiasis. Its action in the treatment
of protozoal infections remains poorly
understood, however, it may work
by damaging protozoal DNA. Tinidazole works
as well as metronidazole and
has many of the same side effects, but it can be givenin a single dose. See table 3.1.1 below:
The table 3.3.1: The classifications of antiprotozoal
(Drugs of Choice forProtozoal Infection), causative protozoa, and disease
Self-assessment 3.1
The medical clinic has received 3 patients this morning. Patient A is being seen
for an intestinal disorder that he acquired after swimming in a local lake and be
diagnosed for giardiasis. Patient B has acquired immunodeficiency syndrome
(AIDS) and is showing early signs of pneumonia. After clinical review he/she
was diagnosed for pneumocytosis. Patient C is being treated and evaluated
on a regular basis for a sexually transmitted infection and was diagnosed withtrichomoniasis.
3) Select the drugs you feel the physician
is likely to prescribe for patient A
a) Chloroquine,
b) Artemisinin,
c) Amoxicillin
d) Metronidazole
4) Select the drugs you feel the physician
is likely to prescribe for patient B
a) Chloroquine,
b) Artemisinin,
c) Pentamidine
d) Nitazoxanide
5) Select the drugs you feel the physician is likely to
prescribe for patient C
a) Artemisinin,
b) Metronidazole
c) Chloroquined) Suramin
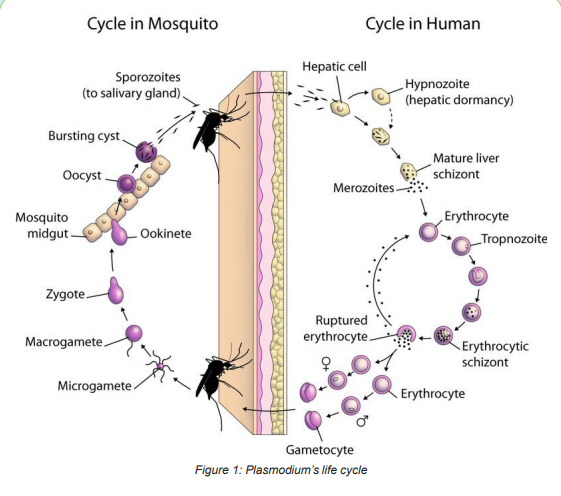
3.2. Plasmodium’s life cycle
Learning Activity 3.2
1) Read the scenario below and answer related questions: A 40 years
old female is brought to you with a history of fever for 2 days, chills,
headache, and arthralgia. On examination, you find that she weighs
63 kg, has temperature of 39.20 C. A blood slide reveals plasmodium
falciparum ring stage ++
a) According to you, what should be the diagnosis for this case?
b) What are two main phases of the disease development?
c) How is the disease transmitted?
d) Is the disease preventable?
2) Which of the following is infective form of plasmodium for human?
a) Schizont
b) Merozoite
c) Sporozoitesd) Oocyst
Content summary
Malaria is a disease characterized by a cycle of fever and chills transmitted through
a bite of a female Anopheles mosquito. Identified causes include Plasmodium
falciparum, vivax, malariae, and ovale. Malaria is endemic in many parts of theworld.
Sporozoites travel through bloodstream and become lodged in the liver and othertissues.
In approaching the antimalarial drugs, we begin by reviewing the life cycle of the
malaria parasite in order to understand the drugs, specific applications of antimalarialdrugs and the rationale behind treatment of patients with malaria.
Malaria develops via two phases: an exoerythrocytic and an erythrocytic phase.
The exoerythrocytic phase involves infection of the hepatic system, or liver,
whereas the erythrocytic phase involves infection of the erythrocytes, or red blood
cells. When an infected mosquito pierces a person’s skin to take a blood meal,
sporozoites in the mosquito’s saliva enter the bloodstream and migrate to the liver.
Within minutes of being introduced into the human host, the sporozoites infect
hepatocytes, multiplying asexually and asymptomatically for a period of over 5-16days depending on the species. Once in the liver, these organisms differentiate to
yield thousands of merozoites, which, following rupture of their host cells, escape
into the blood and infect red blood cells, thus beginning the erythrocytic stage ofthe life cycle.
Then, the merozoites infect red blood cells, where they develop into ring forms,
trophozoites and schizonts which in turn produce further merozoites over 1-3 daysdepending on the species.
This asexual multiplication can result in thousands of parasite-infected cells in the
host bloodstream, leading to illness and complications of malaria that can last for
months if not treated. Some of the merozoite-infected blood cells leave the cycle ofasexual multiplication.
Instead of replicating, the merozoites in these cells develop into sexual forms of
the parasite, called male and female gametocytes, that circulate in the bloodstream
which, if taken up by a mosquito, will infect the insect and continue the life cycle.When a mosquito bites an infected human, it ingests the gametocytes.
In the mosquito gut, the infected human blood cells burst, releasing the gametocytes,
which develop further into mature sex cells called gametes. Male and female
gametes fuse to form diploid zygotes, which develop into actively moving ookinetes
that burrow into the mosquito midgut wall and form oocysts. Growth and division
of each oocyst produces thousands of active haploid forms called sporozoites.
After 8-15 days, the oocyst bursts, releasing sporozoites into the body cavity of the
mosquito, from which they travel to and invade the mosquito salivary glands. The
cycle of human infection restarts when the mosquito takes a blood meal, injectingthe sporozoites from its salivary glands into the human bloodstream.
Some P. vivax and P. ovale sporozoites do not immediately develop into
exoerythrocytic phase (merozoites), but instead produce hypnozoites that remain
dormant for periods ranging from several months (6–12 months typically) to as long
as three years. After a period of dormancy, they reactivate and produce merozoites.
Hypnozoites are responsible for long incubation and late relapses in these twospecies of malaria.
The fever in malaria occurs at the end of erythrocytic phase. During this phase,
the merozoites lyse the RBCs and this hemolysis is accompanied by the release of
hemozoin pigment which directly goes and disturbs the hypothalamic functioning
and causes the occurrence of fever.
The erythrocytic phase occurs every 48 h in cases of P. falciparum, P. vivax and P.
ovale and 72 hours in case of P. malariae. Thus, P. falciparum causes the malignant
form of tertian fever, P. vivax and P. ovale are responsible for the benign form of
Tertian fever (fever occurring at every 3rd day or after 2 days) and P. malariae is
responsible for quartan fever (fever occurring at every 4th day or after 3 days).Then, the fever is intermittent (fever occurring at regular intervals).
Self-assessment 3.2
1) Fever during malaria disease is associated
with which of the following
phenomena in malaria cycle?
a) The exoerythrocytic phase involves
infection of the hepatic system, or
liver and gives rise fever
b) When an infected mosquito pierces
a person’s skin to take a blood
meal, sporozoites infect the liver then fever developed.
c) During the phase of erythrocytic, the merozoites lyse the RBCs and this
hemolysis is accompanied by the release of hemozoin pigment which
directly goes and disturbs the hypothalamic functioning and causes the
occurrence of fever.
d) Instead of replicating, the merozoites develop into sexual forms of the
parasite, called male and female gametocytes, that circulate in the
bloodstream and disturbs the hypothalamic function that cause fever.
2) Using library book and internet, state the body areas/parts affected in the
following phases of malaria development:
a) Exoerythrocytic phase
b) Erythrocytic phase
3) Which of the following species of
plasmodium causes quartan fever?
a) Plasmodium vivax
b) Plasmodium ovale
c) Plasmodium malariae
d) Plasmodium falciparum
4) Which of the following species of plasmodium
causes malignant form of tertian fever?
a) Plasmodium vivax
b) Plasmodium ovale
c) Plasmodium malariae
d) Plasmodium falciparum
5) Which of the following species of plasmodium causes benign form of tertian fever?
a) Plasmodium vivax
b) Plasmodium ovale
c) Plasmodium malariaed) a and b
3.3. Antimalarial medications
Learning Activity 3.3
1)The nurse is reviewing the medication history of a patient who is taking
Coartem. However, the patient’s chart reveals a history of fever, headache
and polyarthralgia. The patient is most likely taking this medication for:
a) Plasmodium.
b) Thyroid disorders.
c) Roundworms.
d) Rheumatoid arthritis.
2) Identify three antimalarial medications used in Rwanda that you know.
3) What malaria prophylaxis approach will you recommend for travellersvisiting malaria endemic area?
CONTENT SUMMARY
Our goal in this sub-lesson is to describe the Antimalarial medications. One of thegreatest protozoal problems worldwide is the treatment and prevention of malaria.
Antimalarials are agents used to attack Plasmodium at various stages of its life
cycle. Through this, it becomes possible to prevent acute malarial reaction inindividuals who have been infected by the parasite.
Antimalarial drugs can be classified according to antimalarial activity and accordingto structure.
1. According to antimalarial activity:
Tissue schizonticides for causal prophylaxis: These drugs act on the primary
tissue forms of the plasmodia which after growth within the liver, initiate the
erythrocytic stage. By blocking this stage, further development of the infection
can be theoretically prevented. Pyrimethamine and Primaquine have this activity.
However, since it is impossible to predict the infections before clinical symptomsbegin, this mode of therapy is more theoretical than practical.
Tissue schizonticides for preventing relapse:These drugs act on the hypnozoites
of P. vivax and P. ovale in the liver that cause relapse of symptoms on reactivation.Primaquine is the prototype drug; pyrimethamine also has such activity.
Blood schizonticides: These drugs act on the blood forms of the parasite and
thereby terminate clinical attacks of malaria. These are the most important drugs
in antimalarial chemotherapy. These include chloroquine, quinine, mefloquine,halofantrine, pyrimethamine, sulfadoxine, sulfones, Tetracyclines etc.
Gametocytocides: These drugs destroy the sexual forms of the parasite in the
blood and thereby prevent transmission of the infection to the mosquito. Chloroquine
and quinine have gametocytocidal activity against P. vivax and P. malariae, but
not against P. falciparum. Primaquine has gametocytocidal activity against allplasmodia, including P. falciparum.
Sporontocides: These drugs prevent the development of oocysts in the mosquitoand thus ablate the transmission. Primaquine and chloroguanide have this action.
Thus in effect, treatment of malaria would include a blood schizonticide, a
gametocytocide and a tissue schizonticide (in case of P. vivax and P. ovale). Acombination of chloroquine and primaquine is thus needed in ALL cases of malaria.
Principles of antimalarial therapy are based on therapeutic objectives. Drug
responsiveness of the malaria parasite changes as the parasite goes through
its life cycle. The erythrocytic forms are killed with relative ease, whereas the
exoerythrocytic (hepatic) forms are much harder to kill and sporozoites do not
respond to drugs at all. Because sporozoites are insensitive to available drugs,drugs cannot prevent primary infection of the liver.
Because of these differences, antimalarial therapy has three separate objectives/
Three methods used to eradicate malaria: (1) treatment of an acute attack (clinical
cure), (2) prevention of relapse (radical cure), and (3) prophylaxis (suppressivetherapy).
• Treatment of an acute attack
Clinical cure is accomplished with drugs that are active against erythrocytic forms of
the malaria parasite. By eliminating parasites from red blood cells, the erythrocyticcycle is stopped and symptoms cease.
For patients with vivax malaria, clinical cure will not prevent relapse, because
hypnozoites remain in the liver. However, for patients with falciparum malaria,successful treatment of the acute attack prevents further episodes.
For mild to moderate malaria, oral therapy is employed. Chloroquine is the drug of
choice for an acute attack caused by chloroquine-sensitive strains of P. falciparum
or P. vivax. As a rule, a 3-day course of treatment produces clinical cure. For strains
of P. falciparum or P. vivax that is chloroquine resistant, quinine is a drug of firstchoice, combined with either doxycycline, tetracycline, or clindamycin.
Malarone, a fixed-dose combination of atovaquone plus proguanil, is an effective
alternative. Mefloquine may also be used but is considered less desirable owing toconcerns about neuropsychiatric effects.
For severe malaria caused by P. falciparum or P. vivax, parenteral therapy isrequired. Quinidine gluconate is approved by the Food and Drug Administration
(FDA) for parenteral use in malaria. When used for severe malaria, IV quinidine
should be combined with doxycycline, tetracycline, or clindamycin. An alternative toquinidine, known as artesunate, is recommended by the World Health Organization.
The various antimalarial drugs work during different phases of the parasite’s
growth inside the human. The antimalarials that exert the greatest effect on all four
Plasmodium organisms during the erythrocytic or blood phase are chloroquine,hydroxychloroquine, and pyrimethamine.
Primary tissue schizonticides (eg, primaquine) kill schizonts in the liver,
whereas blood schizonticides (eg, chloroquine, quinine) kill these parasitic formsonly in the erythrocyte.
Sporonticides (proguanil, pyrimethamine) prevent sporogony and multiplication
in the mosquito. Other drugs that are known to work during the blood phase arequinine, quinidine, and mefloquine.
The most effective antimalarial drug for eradicating the parasite during the
exoerythrocytic phase is primaquine, which works during both phases. Primaquineis indicated specifically for infection with P. vivax.
Chloroquine and hydroxychloroquine (4-aminoquinolines) are the drugs of choice
for the treatment of susceptible strains of malarial parasites. They are highly toxic
to all Plasmodium spp., except resistant strains of P. falciparum. Pyrimethamine is
an antimalarial antibiotic that is used in combination with the sulfonamide antibiotic
sulfadoxine (Fansidar) for prophylaxis against chloroquine-resistant P. falciparumand P. vivax.
The drug combination atovaquone and proguanil (Malarone) is also used forprevention and treatment of P. falciparum infection.
Antimalarial drugs administered to humans cannot affect the parasite during its
sexual cycle when it resides in the mosquito. Instead, these drugs work against the
parasite during its asexual cycle, which takes place within the human body. Often
these drugs are given in various combinations to achieve an additive or synergistic
antimalarial effect. One example is the combination of the two antiprotozoal drugs
atovaquone and proguanil (Malarone). The antibiotic combination of pyrimethamine
and sulfadoxine (Fansidar) is also commonly used, especially in cases caused bydrug-resistant organisms.
The mechanisms of action of the various antimalarial drugs differ depending on thechemical family to which they belong.
The drug effects of the antimalarial drugs are mostly limited to their ability to kill
parasitic organisms, most of which are Plasmodium species (spp.). However, someof these drugs have other effects and therapeutic uses.
Hydroxychloroquine also has anti-inflammatory effects and is sometimes used in the
treatment of rheumatoid arthritis and systemic lupus erythematosus. Quinine and
quinidine can also decrease the excitability of both cardiac and skeletal muscles.Quinidine is still used to treat certain types of cardiac dysrhythmias.
• Prevention of relapse
People infected with P. vivax harbor dormant parasites in the liver, in order to
prevent relapse, a drug that can kill these hepatic forms must be taken. The use
of drugs to eradicate hepatic P. vivax is referred to as radical cure. The agent of
choice for preventing relapse of vivax malaria is primaquine, a drug that is highly
active against the hepatic forms of P. vivax. For falciparum malaria, no treatment isneeded, since relapse does not occur following clinical cure.
P falciparum and P malariae have only 1 cycle of liver cell invasion. The other specieshave a dormant hepatic stage responsible for recurrent infections and relapses.
• Prophylaxis
Selection of drugs for prophylaxis is based on the drug sensitivity of the plasmodialspecies found in the region to which travel is intended.
Malaria can often be avoided by using the ABCD approach which are both drugs
and nondrug prevention measures (Awareness of risk, Bite prevention, Checkwhether you need to take malaria prevention tablets and Diagnosis).
a) Awareness of risk: find out whether the patient is at risk of getting malaria. It’s
important to visit a health care provider before the travel for advice, check whether
it is necessary or need to take preventative malaria treatment depending on the
country you are visiting. Some country it is not necessary to take preventative
malaria treatment before travelling. Even if you grew up in a country where malaria
is common, you still need to take precautions to protect yourself from infection ifyou’re travelling to a risk area.
NB: In area where malaria vaccine is not yet introduced, health care provider has
to educate people that nobody has complete immunity to malaria, and any level of
natural protection you may have had is quickly lost when you move out of a riskarea.
There’s vaccine available currently approved by world health organization that
offers protection against malaria. A first Malaria Vaccine Approved by W.H.O. RTS,
S/ASO1 (RTS. S), trade name Mosquirix, which was endorsed by the World Health
Organisation (WHO) on Wednesday (October 6/2021), is the first and, to date only,
vaccine shown to have the capability of significantly reducing malaria, and life threatening severe malaria, in tests on young African children and it requires fourinjections.
b) Bite prevention: avoid mosquito bites by using insect repellent, covering your
arms and legs, and using a mosquito net. It’s not possible to avoid mosquito bites
completely, but the less you’re bitten, the less likely you are to get malaria.
c) Check whether you need to take malaria prevention tablets: if you do, make
sure you take the right antimalarial tablets at the right dose, and finish the course toreduce your chances of getting the disease until vaccine become available for all.
However, antimalarials only reduce your risk of infection by about 90%, so takingsteps to avoid bites is also important.
Depending on the type you’re taking, continue to take your tablets for up to 4 weeksafter returning from your trip to cover the incubation period of the disease.
NB: In some cases, you may be prescribed emergency standby treatment for
malaria before you travel. This is usually if there’s a risk of you becoming infectedwith malaria while travelling in a remote area with little or no access to medical care.
Examples of emergency standby medications include:
Atovaquone with Proguanil
Artemether with Lumefantrine
Quinine plus DoxycyclineQuinine plus Clindamycine
The list below outlines which medications are safe or unsafe to use whilepregnant:
Mefloquine: not usually prescribed during the first trimester of pregnancy, or if
pregnancy is a possibility during the first 3 months after preventative antimalarial
medication is stopped. This is a precaution, even though there’s no evidence tosuggest mefloquine is harmful to an unborn baby.
Doxycycline: never recommended for pregnant or breastfeeding women as itcould harm the baby.
Atovaquone plus proguanil: not generally recommended during pregnancy or
breastfeeding because research into the effects is limited. However, if the risk ofmalaria is high, they may be recommended if there›s no suitable alternative.
Chloroquine combined with proguanil is suitable during pregnancy, but it is rarely
used as it’s not very effective against the most common and dangerous type ofmalaria parasite.
d) Diagnosis: Malaria can get worse very quickly, so it’s important that it’s diagnosedand treated as soon as possible.
Treatment for malaria is not initiated until the diagnosis has been confirmed by
laboratory tests and it is recommended that the treatment should be completedonce the treatment has been started.
Once confirmed, appropriate antimalarial treatment must be initiated immediately.
Treatment is guided by these main factor0s: the infecting Plasmodium species, the
clinical status of the patient, the organism’s life cycle and the drug susceptibility of
the infecting parasites, as determined by the geographic area where the infection
was acquired. Because the resistance patterns are constantly changing dependingon geographic locations.
2. According to the structure:
a) Aryl-amino-alcohols: Quinine, quinidine (cinchona alkaloids), mefloquine,
halofantrine.
b) 4-aminoquinolines: Chloroquine, amodiaquine.
c) Folate synthesis inhibitors: Type 1 – competitive inhibitors of
dihydropteroate synthase – sulphones, sulphonamides; Type 2 – inhibit
dihydrofolate reductase – biguanides like proguanil and chloroproguanil;
diaminopyrimidine like pyrimethamine
d) 8-aminoquinolines: Primaquine
e) Antimicrobials: Tetracycline, doxycycline, clindamycin, azithromycin,
fluoroquinolones
f) Peroxides: Artemisinin (Qinghaosu) derivatives and analogues –
artemether, arteether, artesunate, artelinic acid
g) Naphthoquinones: Atovaquoneh) Iron chelating agents: Desferrioxamine
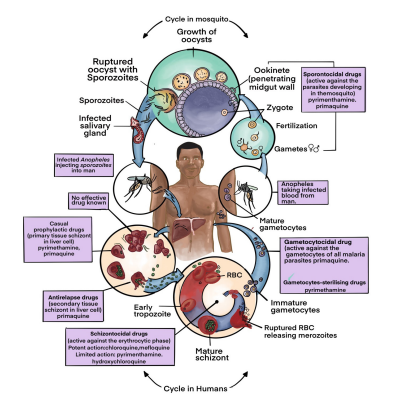
Figure 2: plasmodium’s Life cycle and antimalarial medication
Self-assessment 3.3
1) On which criteria is the selection of drugs for malaria prophylaxis based?
2) When treatment for malaria must be initiated?
3) Antimalarial therapy has three separate objectives, enumerate them.
4) The sporozoites do not respond to antimalarial drugs at all. True or False
5) Why is antimalarial treatment guided by the infecting plasmodium species,
the clinical status of the patient, the organism’s life cycle and the drugsusceptibility of the infecting parasites, considering geographic area?
3.4. Antimalarial drugs prototypes
Learning Activity 3.4
1) During your clinical practice in health center, a senior nurse diagnosed
malaria for a patient complaining of fever and arthralgia. As an associate
nurse student, list antimalarial drugs you know.
2) A 40 years old female is brought to you with a history of fever for 2 days,
chills and anorexia of 1 day. On examination you find that she looks
stable, weighs 62 kg, temperature is 39.20 C. Other systems are normal.
A blood slide reveals plasmodium falciparum ring stage ++
a) What is the treatment?b) If the malaria slide were negative, would you give antimalarial drugs?
CONTENT SUMMARY
Malaria is the most prevalent parasitic endemic disease which is preventable,
treatable, and curable. Antimalarial medication is usually given as tablets or capsules.
If someone is very ill, it will be given through a drip into a vein (intravenously) in
hospital. Many of the same antimalarial medicines used to prevent malaria can alsobe used to treat the disease.
QUININE
Quinine is the chief alkaloid of cinchona bark (known as ‘Fever Bark’), a tree found
in South America. Even today, quinine is obtained entirely from the natural sourcesdue the difficulties in synthesizing the complex molecule.
Mechanism of action: Quinine acts as a blood schizonticides although it also has
gametocytocidal activity against P. vivax and P. malariae. Because it is a weak base,
it is concentrated in the food vacuoles of P. falciparum. It is said to act by inhibitingheme polymerase, thereby allowing accumulation of its cytotoxic substrate, heme.
As a schizonticidal drug, it is less effective and more toxic than chloroquine.
However, it has a special place in the management of severe falciparum malaria inareas with known resistance to chloroquine.
Absorption, fate and excretion: Quinine is readily absorbed when given orally or
intramuscularly. Peak plasma concentrations are achieved within 1 – 3 hours after
oral dose and plasma half-life is about 11 hours. In acute malaria, the volume of
distribution of quinine contracts and clearance is reduced, and the elimination half life increases in proportion to the severity of the illness. Therefore, maintenance
dose of the drug may have to be reduced if the treatment is continued for more than
48 hours. The drug is extensively metabolized in the liver and only 10% is excretedunchanged in the urine. There is no cumulative toxicity on continued administration.
Adverse effects: Quinine is a potentially toxic drug. The typical syndrome of
quinine side effects is called as cinchonism and it can be mild in usual therapeutic
dosage or could be severe in larger doses. Mild cinchonism consists of ringing in
the ears (tinnitus), headache, nausea and disturbed vision. Functional impairment
of the eighth nerve results in tinnitus decreased auditory acuity and vertigo. Visual
symptoms consist of blurred vision, disturbed colour perception, photophobia,
diplopia, night blindness, and rarely, even blindness. These changes are due todirect neurotoxicity, although vascular changes may contribute to the problem.
Gastrointestinal symptoms like nausea, vomiting, abdominal pain and diarrhea
may be seen. Rashes, sweating, angioedema can occur. Excitement, confusion,
delirium are also seen in some patients. Coma, respiratory arrest, hypotension, and
death can occur with over dosage. Quinine can also cause renal failure. Massive
hemolysis and hemoglobinuria can occur, especially in pregnancy or on repeateduse. Hypoprothrombinemia, agranulocytosis are also reported.
Quinine has little effect on the heart in therapeutic doses and hence regular
cardiac monitoring is not needed. However it can cause hypotension in the event
of overdose. Quinine reduces the excitability of the motor end plate and thus
antagonises the actions of physostigmine. It can cause respiratory distress anddysphagia in patients of myasthenia gravis.
Quinine stimulates insulin secretion and in therapeutic doses it can cause
hypoglycemia. This can be more severe in patients with severe infection and in
pregnancy. Hypoglycemia in malaria may go unnoticed and could even cause
death. Therefore, it is advisable to monitor blood glucose levels at least once in 4-6
hours while quinine is administered, especially in severe infection and in pregnancy.
Quinine induced hypoglycemia can recur even after administration of 25% or 50%
dextrose. In such situations, maintenance with a 10% dextrose infusion is advisable.
Resistant hypoglycemia due to quinine can be managed with Injection Octreotide,50 microgram subcutaneously, every 6 to 8 hours.
Contraindications: Hypersensitivity in the form of rashes, angioedema, visual and
auditory symptoms are indications for stopping the treatment. It is contraindicated
in patients with tinnitus and optic neuritis. It should be used with caution in patients
with atrial fibrillation. Hemolysis is indication for immediately stopping the drug. It isalso contraindicated in patients suffering from myasthenia gravis.
Availability: It is available as tablets and capsules containing 300 or 600 mg of the
base. It is also available as injections, containing 300mg /ml.
Quinidine: The anti-arrhythmic drug related to quinine can also be used in the
treatment of severe P. falciparum malaria. Dose is 10 mg of base / kg by infusionover 1-2 hours, followed by 0.02 mg/kg/min with ECG monitoring.
Chloroquine
Chloroquine is the prototype antimalarial drug, most widely used to treat all typesof malarial infections.
Mechanism of action: The mechanism of action of chloroquine is unclear. Being
alkaline, the drug reaches high concentration within the food vacuoles of the
parasite and raises its pH. It is found to induce rapid clumping of the pigment.
Chloroquine inhibits the parasitic enzyme heme polymerase that converts the toxic
heme into non-toxic hemazoin, thereby resulting in the accumulation of toxic heme
within the parasite. It may also interfere with the biosynthesis of nucleic acids. Other
mechanisms suggested include formation of drug-heme complex, intercalation ofthe drug with the parasitic DNA etc.
Absorption, fate and excretion: 90% of the drug is absorbed from G.I.T and rapidly
absorbed from intra muscular and subcutaneous sites. It has a large distribution
volume due to extensive sequestration in tissues of liver, spleen, kidney, lung etc.
Hence the need for a larger loading dose. Therapeutic blood levels persist for 6-10
days and elimination half-life is 1-2 months. Half of the drug is excreted unchangedby the kidneys, remaining is converted to active metabolites in the liver.
Antimalarial activity: It is highly effective against erythrocytic forms of P. vivax, P.
ovale and P. malariae, sensitive strains of P. falciparum and gametocytes of P.
vivax. It rapidly controls acute attack of malaria with most patients becoming afebrilewithin 24-48 hours. It is more effective and safer than quinine for sensitive cases.
Adverse effects: Chloroquine is a relatively safer antimalarial. At therapeutic
doses, it can cause dizziness, headache, diplopia, disturbed visual accommodation,
dysphagia, nausea, malaise, and pruritus of palms, soles and scalp. It can also
cause visual hallucinations, confusion, and occasionally frank psychosis. Theseside effects do not warrant stoppage of treatment. It can exacerbate epilepsy.
When used as prophylactic at 300 mg of the base/ week, it can cause retinal toxicity
after 3-6 years (i.e. after 50-100 g of chloroquine). Intra muscular injections ofchloroquine can cause hypotension and cardiac arrest, particularly in children.
Contra indications: Chloroquine should be used with caution in patients with
hepatic disease, (even though it is not hepatotoxic per se, it is distributed widely in
the liver and is converted to active metabolites there; hence the caution), severe
gastro intestinal, neurological or blood disorders. The drug should be discontinuedin the event of such problems during therapy.
It should not be co-administered with gold salts and phenyl-butazone, because
all the three can cause dermatitis. Chloroquine may interfere with the antibodyresponse to human diploid cell rabies vaccine.
Availability: Chloroquine is available as Chloroquine phosphate tablets; each
250-mg tablet contains 150 mg of the base. Chloroquine hydrochloride injectioncontains 40 mg of the base per ml.
Sulfadoxine+Pyrimethamine
Pyrimethamine and sulphadoxine are very useful adjuncts in the treatment of
uncomplicated, chloroquine resistant, P. falciparum malaria. It is now used in
combination with artesunate for the treatment of P. falciparum malaria. It is alsoused in intermittent treatment in pregnancy (IPTp).
Antimalarial activity: Pyrimethamine inhibits the dihydrofolate reductase of
plasmodia and thereby blocks the biosynthesis of purines and pyrimidines, which
are so essential for DNA synthesis and cell multiplication. This leads to failure
of nuclear division at the time of schizont formation in erythrocytes and liver.
Sulfadoxine inhibits the utilisation of para-aminobenzoic acid in the synthesis of
dihydropteroic acid. The combination of pyrimethamine and sulfa thus offers twostep synergistic blockade of plasmodial division.
Absorption, fate and excretion: Pyrimethamine is slowly but completely absorbed
after oral administration and is eliminated slowly with a plasma half-life of about 80-
95 hours. Suppressive drug levels may be found in the plasma for up to 2 weeks.The drug is excreted in breast milk.
Sulfonamides are rapidly absorbed from the gut and are bound to plasma proteins.
They are metabolised in the liver and are excreted in the urine. They pass through
the placenta freely. Sulfadoxine is a long acting sulfonamide with a half-life of 7-9days.
Toxicity and contraindications: Pyrimethamine can cause occasional skin rashes
and depression of hematopoiesis. Excessive doses can produce megaloblasticanemia.
Sulfonamides can cause numerous adverse effects.
Agranulocytosis; aplastic anemia; hypersensitivity reactions like rashes, fixed drug
eruptions, erythema multiform of the Steven Johnson type, exfoliative dermatitis,
serum sickness; liver dysfunction; anorexia, vomiting and acute hemolytic anemiacan also occur.
At the doses employed for malaria, pyrimethamine produces few adverse effects.
However, at high doses, such as those used to treat toxoplasmosis, pyrimethaminecan produce symptoms of folic acid deficiency
Effects on the bone marrow manifest as leukopenia, thrombocytopenia, and anemia.
Effects on the GI mucosa manifest as ulcerative stomatitis, atrophic glossitis,
pharyngitis, and diarrhea. These responses reverse upon discontinuing treatment,and can be prevented by giving folic acid or folinic acid.
To minimize risk, sulfadoxine should not be given to patients with a history of
hypersensitivity to sulfonamides or chemically related drugs, including thiazidediuretics, loop diuretics, and sulfonylurea-type oral hypoglycemics (eg, tolbutamide).
The drug is contraindicated in patients with known hypersensitivity to sulfa, infants
below 2 months of age, patients with advanced renal disease and first and lasttrimesters of pregnancy.
Availability: Pyrimethamine and sulphadoxine is no longer used as a single drug,
but only in combination with artesunate.
The Artemisinin Derivatives
Antimalarial activity: Most clinically important artemisinins are metabolised to
dihydroartemisinin (elimination half-life of about 45 min), in which form they have
comparable antimalarial activity. However, their use in monotherapy is associated
with high incidences of recrudescent infection, suggesting that combination withother antimalarials might be necessary for maximum efficacy.
It is the fastest acting antimalarial available. It inhibits the development of the
trophozoites and thus prevents progression of the disease. Young circulating
parasites are killed before they sequester in the deep microvasculature. These
drugs start acting within 12 hours. These properties of the drug are very useful
in managing complicated P. falciparum malaria. These drugs are also effectiveagainst the chloroquine resistant strains of P. falciparum.
Artesunate and artemether have been shown to clear parasitaemias more effectively
than chloroquine and sulfadoxine/pyrimethamine. Meta-analysis of mortality in
trials indicated that a patient treated with artemether had at least an equal chanceof survival as a patient treated with quinine.
It has also been reported that artemisinin drugs cleared parasites faster than
quinine in patients with severe malaria but fever clearance was similar. Also,
parenteral artemether and artesunate are easier to use than quinine and do notinduce hypoglycaemia.
Gametocytocidal action: Artemisinin compounds have been reported to reduce
gametocytogenesis, thus reducing transmission of malaria, this fact being especiallysignificant in preventing the spread of resistant strains.
These drugs prevent the gametocyte development by their action on the ring stages
and on the early (stage I-III) gametocytes. In studies including over 5000 patients
in Thailand, it was shown that gametocyte carriage was significantly less frequentafter treatment with artemisinin derivatives than after treatment with mefloquine.
Absorption, fate and excretion: Artemisinin derivatives are absorbed well after
intra muscular or oral administration. The drug is fully metabolised and the major
metabolite is dihydroartemisinin, which also has Antiparasitic effects. It is rapidlycleared, predominantly through the bile.
Toxicity: Toxic effects have been reported less frequently with the artemisinins
than with other antimalarial agents. The most common toxic effects that have been
identified are nausea, vomiting, anorexia, and dizziness; these are probably due, in
many patients, to acute malaria rather than to the drugs. More serious toxic effects,
including neutropenia, anemia, hemolysis, and elevated levels of liver enzymes,have been noted rarely.
Extensive studies in many species showed that intramuscular dosing was more
toxic than oral dosing and that, by any route; fat-soluble artemisinins were moretoxic than artesunate.
Another concern about artemisinins is embryotoxic effects, which have been
demonstrated in animals. Studies from Asia and Africa, including treatment during
the first trimester, showed similar levels of congenital abnormalities, stillbirths, and
abortions in patients who received and those who did not receive artesunate during
pregnancy. Limited data are available on the use of intravenous artesunate forsevere malaria during pregnancy.
Availability: Artemisinin is available as its derivatives, artemether and artesunate.
The ether derivatives are more soluble in oil and are available as injections for intra
muscular use. Artemether is available as injections of 80 mg in 1 ml. Artemethercapsules containing 40 mg of the drug are also now available.
Artesunate is an ester derivative that is more soluble in water. The drug is available
as a powder. It should be first dissolved in 1 ml of 5% sodium bicarbonate (usuallyprovided with the vial) and shaken for 2-3 minutes.
After it dissolves completely, it is diluted with 5% dextrose or saline (for intravenous
use, dilute with 5 ml and for intramuscular use, dilute with 2 ml). Intravenous dose
should be injected slowly at a rate of 3-4 ml/minute. It is also available as tablets,each containing 50 mg of the drug.
Rectal artemisinins rapidly eliminate malarial parasites
Resistance: The short half-lives of artemisinins limit the possibility of selection
for resistance. However, at present, the likelihood of true artemisinin resistance in
malaria parasites is low, and this concern should not prevent the use of intravenousartesunate to treat severe malaria.
ARTEMETHER AND ARTESUNATE
Artemether [Artenam] and artesunate are the most effective drugs available for
multidrug resistant falciparum malaria. Both agents are derivatives of artemisinin,
a compound isolated from the sweet wormwood plant, Artemisia annua. To
be effective, artemether and artesunate must undergo conversion to an active
metabolite dihydroartemisinin which kills plasmodia by releasing free radicals that
attack the cell membrane. Kill also requires high concentrations of iron, as arefound in red blood cells.
Artemether and artesunate are remarkably safe. These drugs can produce transient
first-degree heart block, as well as a dose-related decrease in red blood cells and
neutrophils. They can also prolong coma and promote fever. However, serious orpersistent side effects have not been reported.
Indications
Treatment of severe malaria and initial treatment of uncomplicated malaria, whenpersistent vomiting precludes oral therapy.
Artesunate is an artemisinin derivative with antimalarial actions much like those
of artemether. At this time, artesunate, administered IV, is considered the drug of
choice for severe malaria. Artesunate appears to be more effective than IV quinineand safer than IV quinidine.
ARTEMETHER/LUMEFANTRINE
Indications and Efficacy
The combination of artemether (20 mg) and lumefantrine (120 mg), sold as Coartem,is indicated for oral therapy of uncomplicated falciparum malaria.
The combination is not approved for prophylaxis of falciparum malaria, for treatmentof severe falciparum malaria, or for prophylaxis or treatment of vivax malaria.
Both artemether and lumefantrine can kill erythrocytic forms of the malarial parasite,but these drugs cannot kill primary or latent hepatic forms.
In clinical trials, artemether/lumefantrine has been highly effective against
falciparum malaria: 28 days after a short course of treatment, the cure rate is more
than 95%, even against multidrug-resistant P. falciparum. Efficacy against P. vivaxis less dramatic.
Mechanism of Action
To be effective, artemether must undergo conversion to an active metabolite—
dihydroartemisinin— which appears to kill plasmodia by releasing free radicals
that attack the cell membrane. Lumefantrine probably works like chloroquine,
causing death by preventing malaria parasites from converting heme to nontoxicmetabolites.
Pharmacokinetics
The kinetics of artemether and lumefantrine differ in three important ways. First,
lumefantrine is highly lipophilic, so oral absorption is enhanced by dosing with fatty
food. Second, absorption of artemether is relatively rapid (plasma levels peak about
2 hours after dosing), whereas absorption of lumefantrine is delayed (plasma levels
peak 6 to 8 hours after dosing). Third, the half-life of artemether is short (1.5 hours),whereas the half-life of lumefantrine is prolonged (100 hours).
Adverse Effects
Artemether/lumefantrine is generally well tolerated. Approximately one-third or
more of adults taking this drug experience adverse effects such as headache,
anorexia, dizziness, weakness, joint pain, and muscle pain. Among children, themost common adverse effects are fever, cough, vomiting, anorexia, and headache.
Lumefantrine may prolong the QT interval, posing a risk of serious dysrhythmias.
Accordingly, artemether/lumefantrine should not be used by patients with electrolyte
disturbances (e.g., hypokalemia, hypomagnesemia) or congenital prolonged QT
syndrome, or by patients using other drugs that prolong the QT interval (e.g.,quinine, erythromycin, and ketoconazole).
Why Do We Combine Artemether With Lumefantrine?
Compared with lumefantrine, artemether is much more effective. As a result, when
the drugs are administered together, most of the benefit comes from artemether.Why, then, do we combine these drugs?
There are two reasons:
First, adding lumefantrine enhances efficacy. (Because lumefantrine has a much
longer half-life than artemether, lumefantrine remains in the body long enough to killthe few parasites not killed by artemether).
Second, adding lumefantrine helps prevent development of resistance to
artemether. Why? Because the odds of developing resistance to the two drugs
simultaneously are much lower than the odds of developing resistance to artemetheralone. Accordingly,
In 2006 the World Health Organization requested that all drug companies stop
selling artemisinin-only products and replace them with artemisinin combination
therapies (ACTs). Four ACTs are recommended:
• Artemether/lumefantrine [Coartem]
• Artesunate/mefloquine
• Artesunate/amodiaquine
• Artesunate/pyrimethamine/sulfadoxine
Pharmacology | Associate Nursing Program | Senior 5 87
N.B: These combinations are indicated only for the treatment of malaria not forprophylaxis.
The other medications used to treat malaria are: Chloroguanide (Proguanil),
Halofantrine, Mefloquine, Atovaquone, Pyronaridine, Piperaquine,
Clindamycin, ciprofloxacin, Norfloxacin, azithromycin, Tetracyclines, Doxycyclineand Clindamycin.
SUMMARY OF COMMON DRUGS USED TO TREAT MALARIA
Self-assessment 3.4
3) A 32-year-old female student developed fever for last 3 days. She consulted
a nearby health center and the health care provider suspect malaria
and he asked for blood film for malaria. Results showed plasmodium
falciparum and he decided to give quinine. What are the adverse effects
that can be associated with quinine at usual therapeutic doses?
4) A patient with a history of malaria presently being treated with chloroquine
is admitted to the hospital. What are the side effects should the nurse
anticipate at therapeutic doses?
5) True and false questions
a) The erythrocytic forms are not killed with relative ease whereas the
exoerythrocytic (hepatic) forms are very easy to kill. True or false
b) Tissue schizonticides for causal prophylaxis: These drugs act on the
primary tissue forms of the plasmodia which after growth within the liver,
initiate the erythrocytic stage. True or false
c) Tissue schizonticides for preventing relapse: These drugs that do not
act on the hypnozoites of P. vivax and P. ovale in the liver that cause
relapse of symptoms on reactivation. True or false
d) Blood schizonticides: These drugs act on the blood forms of the parasite
and thereby terminate clinical attacks of malaria. True or false
e) Gametocytocides: These drugs destroy the sexual forms of the parasite
in the blood and thereby prevent transmission of the infection to the
mosquito. True or false
f) Sporontocides: These drugs prevent the development of oocysts in the
mosquito and thus ablate the transmission. True or false
3.5. Antimalarial drug dosage.
Learning Activity 3.5
1) Two different patients were received at the medical clinic. Patient A was
diagnosed for simple malaria and patient B diagnosed for simple malaria
on first term pregnancy. Physician recommends quinine tablets as
treatment for patient B and Coartem for patient A.
a) The patient B who received quinine weighs 60 kilograms. Using
pharmacology book and internet, and discuss the dosage the healthcare
provider will follow while prescribing quinine injection for patient B.
b) The patient A who received coartem weighs 30 kilograms. Using
pharmacology book and internet, and discuss the dosage the healthcareprovider will follow while prescribing coartem for patient A.
CONTENT SUMMARY
Our goal in this lesson is to describe the antimalarial drug dosage calculation.
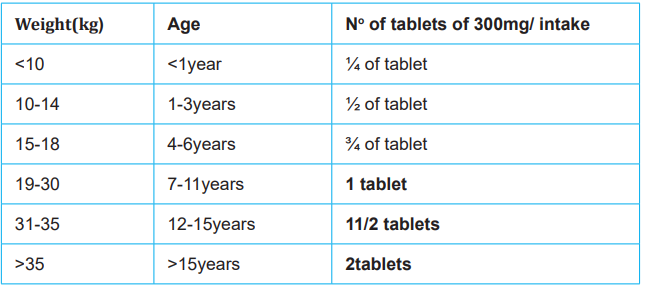
CHLOROQUINE
Chloroquine phosphate [Aralen] is available in tablets (250 and 500 mg) for oral
administration.
Adult: Malaria
Prophylaxis
Indicated for prophylaxis of malaria in geographic areas where resistance to
chloroquine is not present; 500 mg (300-mg base) weekly on the same day each
week; begin 1-2 weeks before travel, during travel, and for 4 weeks after leaving
endemic area.
Treatment
Indicated for acute attacks of malaria due to P. vivax, P. malariae, P. ovale, and
susceptible strains of P. falciparum.
Acute attack
• 1 g (600-mg base) PO, THEN
• 500 mg (300 mg-base) PO after 6-8 hr THEN
• 500 mg (300 mg-base) PO at 24 hr and 48 hr after initial dose
Total dose of 2500 mg (1500 mg-base) in 3 days
Pediatric: Malaria
Prophylaxis
Indicated for prophylaxis of malaria in geographic areas where resistance to
chloroquine is not present; 5 mg/kg PO q1Week, not to exceed 500 mg (300-mg
base), on the same day each week; begin 1-2 weeks before travel, during travel,
and for 4 weeks after leaving endemic area.
Treatment
Indicated for acute attacks of malaria due to P. vivax, P. malariae, P. ovale, and
susceptible strains of P. falciparum for adults, infants, and children
• Acute attack
Note: Dosing is based chloroquine base; chloroquine phosphate 16.6 mg is
equivalent to 10 mg chloroquine base
• First dose: 10 mg base/kg (not to exceed 600-mg base/dose)
• Second dose: (6 hr after first dose) 5 mg base/kg (not to exceed 300 mg
base/dose)
90 Pharmacology | Associate Nursing Program | Senior 5
• Third dose: (24 hr after first dose): 5 mg base/kg (not to exceed 300 mg
base/dose)
• Fourth dose36 hr after first dose): 5 mg base/kg (not to exceed 300 mg
base/dose)
Total dose of 25mg base/kg
QUININE
Dose:
Oral: 10 mg/kg 8 hourly for 7 days.
Intra venous: 20 mg of salt/kg in 10 ml/kg isotonic saline or 5% dextrose over 4
hours, then 10 mg of salt/kg in saline or dextrose over 4 hours, every 8 hours until
patient is able to take orally or for 5-7 days.
Intra muscular: 20 mg/kg stat, followed by 10 mg/kg 8 hourly by deep intra muscular
injections for 5-7 days.
Quinine dihydrochloride IR (intra-rectal) for children: 15 mg per kg body weight
diluted in 4 ml of distilled water or physiological solution and administered rectally
with a 5-ml syringe every eight hours. Note: If the drug is ejected during the first 10
minutes following its administration, administer other half dose.
Quinine dihydrochloride IV administration (Children and adults):
In infusion, it is administered as 10 mg per kg body weight per dose, diluted in 5 to
10 ml of 5% or 10% glucose per kg body weight, every eight hours. If the patient’s
condition does not improve within 24 hours of treatment, refer patient to the nearest
district hospital.
DOXYCYCLINE (Monodox/Vibramycin)100mg orally daily, 1-2 days before travel and for 4 weeks after return from endemic
area.
PYRIMETHAMINE/SULFADOXINE
Pyrimethamine and sulfadoxine are available in a fixed-dose combination sold as
Fansidar. Tablets contain 25 mg of pyrimethamine and 500 mg of sulfadoxine.
To treat an acute attack of chloroquine-resistant malaria, Fansidar, used inconjunction with quinine, is given as a single dose on the last day of quinine dosing.
Fansidar dosages are as follows:
• Adults, 2 to 3 tablets;
• Children 9 to 14 years, 2 tablets;
• Children 4 to 8 years, 1 tablet;
• Children under 4 years, one-half tablet.
Prevention: 1 tablet orally weekly
ARTEMETHER/LUMEFANTRINE (Coartem)
These combinations are indicated only for treatment of malaria not for prophylaxis.
The ACT used most widely is a fixed-dose combination of artemether (20 mg)
and lumefantrine (120 mg), sold as Coartem. Patients take a 3 days course, withdosage based on body weight. The cure rate is about 95%, even against multidrug resistant P. falciparum. To date, there have been no reports of resistance to either component.
Adult/Child >35 kg: PO: 4 tabs of artemether 80 mg/ lumefantrine 480 mg upon
diagnosis, then 4 tabs in 8 h, then 4 tabs b.i.d. for 2 days
Adult/Child 25-35 kg: PO: 3 tabs artemether 60 mg with lumefantrine 360 mg insame regimen
Child 15-25 kg: PO: 2 tabs artemether 40 mg with lumefantrine 240 mg in same
regimen
Child 5-15 kg: PO: 1 tab artemether 20 mg with lumefantrine 120 mg in same
regimen
Artemether by IM: administered as dose of:
• For children:3.2 mg per kg body weight immediately after a positive blood
smear or positive rapid diagnostic test, followed by 1.6 mg/kg after 12 hours
• For adults: 160 mg IM of artemether immediately after a positive blood smearor a positive rapid diagnostic test and 80 mg after 12 hours.
If the patient’s condition does not improve within 24h of treatment, refer the patient
to the nearest district hospital. If the patient’s condition improves, change to oral
Artemether-lumefantrine twice a day for three consecutive days.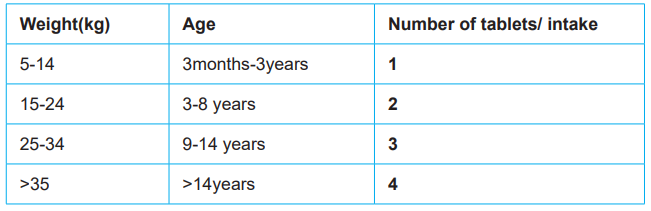
ARTESUNATE
Artesunate is antimalarial drug indicated for initial treatment of severe malaria;
should always be followed by a complete treatment course of an appropriate POantimalarial regimen (Coartem)
Dosage and duration:
• Child under 20 kg: 3 mg/kg/dose• Child 20 kg and over and adult: 2.4 mg/kg/dose
One dose given on admission (time = 0), the following dose will be administered
at 12h then at 24h, then once a day. Administer parenterally at least 24 hours (3
doses), then, if the patient can tolerate the oral route, change to a complete 3-day
course of an artemisinin-based combination. If not, continue parenteral treatment
once daily until the patient can change to oral route (without exceeding 7 days ofparenteral treatment).

Use a 1 ml syringe graduated in 0.01 ml when the dose required is less than 1 ml.
For patients over 25 kg, a second vial must be prepared to obtain the volumeneeded, a third vial for patients over 50 kg and a fourth vial for patients over 76 kg.
Self-assessment 3.5
1) In urban district of a country highly endemic for malaria, a boy aged 6
years weighing 23 kilograms wakes up in the morning and refuses to
eat. He is rather quiet but does not have fever. The mother gives three
tablets of artemether-lumefantrine (AL). That day when he returned from
school he was apparently well. The AL was stopped. Two days later in the
evening, he develops fever and vomiting. The mother then gives another
3 tablets of AL. The following morning, he again refused food, and he had
a low-grade fever to touch. The mother decides to take the child to the
clinic.
a) Was the mother right to give the AL? Explain your answer.
b) If the child had malaria, would the mother have stopped the treatment
after the initial first dose of AL when the child was apparently well?
Please explain
c) How would the health care provider manage this patient?
2) Explain how to calculate artesunate dosage to be administered via IV
3) Explain dosage calculation for quinine injection for an adult patient withsevere malaria
3.6. Treatment of simple malaria
Learning Activity 3.6
1) You are a S5 nurse student in the clinical placement at a district hospital,
and there is a patient taking coartem. During the nursing round, your
colleague from S4 asks a senior nurse why the patient is on Coartem.
The senior nurse responds to the student that it is because the patient
has been diagnosed with simple malaria and tasks you to deeply give
explanation of how to manage simple malaria at the health facility level
in Rwanda.
a) What deep explanation will you provide to your colleague regarding the
reason of taking coartem?
b) Who are in-charge of simple malaria management at the community
level?
c) What drug may be used at the health facility level when coartem iscontraindicated?
CONTENT SUMMARY
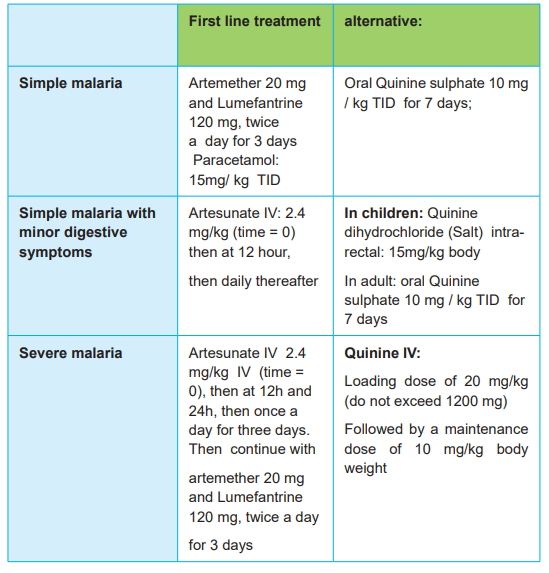
According to clinical manifestations, malaria is classified into three forms: Simple
malaria, Simple malaria with minor digestive symptoms and severe malaria.
I. Treatment of simple malaria
Information Education and Communication (IEC)at family level:
Strengthening information, education and communication (IEC):
• Knowledge of the mode of transmission of malaria in Rwanda
• Utilization of long-lasting insecticide treated nets (LLINs) as the principal
means of prevention and utilization of other preventive measures
• Membership to the community health insurance scheme as means of ensuring
early access to health care.
• Recognition by the family members of the signs of simple malaria, simple
malaria with minor digestive symptoms and severe malaria
• Seeking care in a timely manner from a community health worker or the
nearest health facility, after reducing fever, if present by using sponging.
At community level (Community health workers)
The role of the community health worker is to:
• Sensitize the population on the mode of transmission of malaria in Rwanda
• Sensitize the population on the recognition of the signs of the simple malaria,
malaria with minor digestive symptoms and severe malaria
• Sensitize the population on seeking care in a timely manner from a community
health worker or the nearest health facility, after reducing fever, if present by
using tepid sponging.
• Manage cases of children under five with malaria in accordance with the
national guidelines after confirmation using a rapid diagnostic test (RDT),
under the framework of CCM (community case management ), and when
necessary refer to a health facility
• Orient the population to the health facility for appropriate management
• Sensitize the population to the use of the long lasting insecticide treated nets
as principal means of prevention, environment hygiene and sanitation as well
as other preventive measures
• Participate in other malaria control activities at the community level such as
indoor residual spraying campaigns, application of larvicides, etc.
At the level of the health facility
It is indicated to prescribe the first line of treatment only after obtaining a positive
96 Pharmacology | Associate Nursing Program | Senior 5
blood smear or positive rapid diagnostic test. A negative blood smear or rapid
diagnostic test excludes the diagnosis of malaria and the administration of an
antimalarial. Another cause of the fever should be sought systematically and treated
accordingly.
The first line treatment recommended is an artemisinin combination therapy (ACT)
of 2 molecules in one tablet. That is: Artemether 20 mg and Lumefantrine 120 mg
to be taken preferably during meals.
The combination of artemether – lumefantrine (COARTEMR) is administered orally,
twice a day for 3 days.
Important instructions to follow:
• Respect the dose prescribed by the health provider
• Directly observe the administration of the first dose• Do not exceed the prescribed dose
Table 3.6.1: Posology of artemether-lumefantrine (COARTEMR) in function of
body weight or age
• Artemether-lumefantrine is contraindicated
– In children weighing less than 5 kg;
– During first trimester of pregnancy,
– In case of allergy to one of the two drugs in the combination and
– In cases of severe liver or renal disease.
In such cases, oral quinine sulphate is indicated as 10 mg per kg body weight perdose, taken three times a day over seven consecutive days.
Table 3.6.2: Posology of oral quinine in function of weight or age
N.B: If there is no improvement after 48 hours of treatment, verify if the patient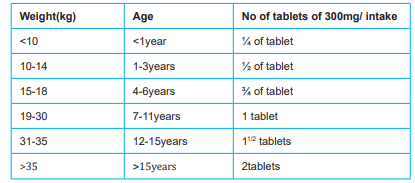
swallowed the drugs correctly, re-examine the patient carefully and do another
peripheral blood smear. If the test is positive, change the treatment to oral quinine
sulphate as 10 mg per kg body weight per dose, taken three times a day over seven
consecutive days. If the peripheral blood smear is negative, exclude and treat other
causes of illness and/or refer the patient to the nearest district hospital.
If there is no improvement after 48 hours of treatment with quinine, refer the patient
to the nearest District hospital because there is suspicion of other associated
pathologies rather than malaria.
II. The management of simple malaria with minor digestive symptoms
The minimum required criteria for treating simple malaria with minor digestive
symptoms at a health facility are the following:
• Qualified and trained staff
• The existence of a continuous system of clinical and paraclinical monitoring
of patients, 24 out of 24 hours;
• A laboratory with the capacity to do a peripheral blood smear, rapid diagnostic
tests and measure haemoglobin.
The management of simple malaria with minor digestive symptoms is done at the
health centre, or when not possible in the district hospital.
The patient must be admitted in the health centre where he/she will receive
treatment for 24 hours maximum.
After this period, a clinical and paraclinical re-evaluation is done to assess if
the patient can be discharged to go home (if there has been improvement and
transition towards simple malaria), or be transferred to the district hospital (in caseswhere there has been no improvement).
The recommended drugs are artemether IM or quinine IR or quinine in IV infusion
if diarrhoea is present.
Modes of administration of the antimalarials
Depending on the general status and level of hydration of the patient, drugs may be
administered as follows:
1) Artemether by IM: administered as dose of:
– For children:3.2 mg per kg body weight immediately after a positive blood
smear or positive rapid diagnostic test, followed by 1.6 mg/kg after 12
hours
– For adults: 160 mg IM of artemether immediately after a positive blood
smear or a positive rapid diagnostic test and 80 mg after 12 hours.
If the patient’s condition does not improve within 24h of treatment, refer the patient
to the nearest district hospital. If the patient’s condition improves, change to oral
Artemether-lumefantrine twice a day for three consecutive days.
2) Quinine dihydrochloride IR (intra-rectal) for children: 15 mg par kg
body weight diluted in 4 ml of distilled water or physiological solution and
administered rectally with a 5-ml syringe every eight hours. This dose is
justified by the slow absorption of quinine by the rectal mucosa. The drug is
administered slowly through the anus, and the buttocks are held together for
5 minutes to prevent a premature reflex ejection of the drug. If the patient’s
condition does not improve after 24 hours of treatment, refer the patient
to the nearest hospital. If the patient’s condition improves, change to oral
Artemether-Lumefantrine, twice a day for three consecutive days, or in the
case of contraindications to Artemether-Lumefantrine, give oral quinine.
Note:
– If the drug is ejected during the first 10 minutes following its administration,
administer other half dose.
– Diarrhoea and anal lesions limit the use of this route of administration.
3) Quinine dihydrochloride IV administration (Children and adults):
In infusion, it is administered as 10 mg per kg body weight per dose, diluted in 5 to
10 ml of 5% or 10% glucose per kg body weight, every eight hours. If the patient’s
condition does not improve within 24 hours of treatment, refer patient to the nearest
district hospital.
If the patient’s condition improves, change to oral Artemether-Lumefantrine, twice
a day for three consecutive days, or to oral quinine in case of contraindications to
Artemether-Lumefantrine.
NB: Whatever the medicine and the mode of administration used, (IM artemether,
IR/IV quinine), if the state of health of the patient doesn’t improve in 24 hours, do
Pharmacology | Associate Nursing Program | Senior 5 99
a rapid diagnostic test and refer the patient with the referral note or treatment file,
giving detailed information on the treatment provided so far, to the nearest hospital.
Symptomatic treatment
In case of diarrhoea and/or vomiting:
• Evaluate and monitor the hydration status of the patient;
• Rehydrate the child with ORS or other available liquids, encourage breast
feeding and other modes of feeding and if necessary use a naso-gastric tube;
• Antiemetic should be avoided.
In case of fever, give oral Paracetamol 15 mg/ kg, or any other antipyretic drug as
it may be indicated.
N.B. In case of pregnant woman with this type of malaria, the treatment is as follows:
1st trimester of pregnancy: give Quinine dihydrochloride in infusion until she is
able to take oral quinine and continue oral quinine to complete the totality of 7 days
2nd and 3rd trimester of pregnancy: give Artemether IM or quinine IV infusion until
she is able to take oral treatment and pass to oral COARTEM 4 tablets twice a dayin 3 days.
Self-assessment 3.6
1) A 38-year-old male with no significant past medical history has returned
to Rwanda from traveling to malaria endemic region. He forgot to take
chemoprophylaxis for malaria and now presents with fever, chills, rigors,
and blood smear test reveals plasmodium. Which therapy should be
initiated to this patient?
a) Coartem
b) Quinine 648 mg
c) Mefloquine 250 mg
d) Quinidine 300 mg
2) A pregnant mother in the first trimester was diagnosed with simple
malaria. The fellow student in the clinical placement asks you the reason
why quinine was given, and not coartem. What would be your answer to
this student?
3) A 10-year-old male patient weighing 28 kilograms is admitted at the
health facility. He complains of fever, headache, vomiting, and mild
diarrhea. The laboratory exam reveals malaria. The nurse decides to
give artesunate, and she tasks to calculate the dose to administer to thispatient immediately. How would you calculate this dosage?
3.7. Treatment of severe malaria
Learning Activity 3.7
As an associate nurse student, you are carrying out clinical practice at the health
center, and you receive a patient with history of fever, inability to stand still, and
chills. On the assessment, the patient is weak with pale palpebral conjunctivae,
and you decide to order the laboratory investigations.
The blood smear reveals the plasmodium. In addition, you take the glycaemia
which reveals 40mg/dL. You take a decision to refer the patient to the district
hospital.
1) What are the antimalarial medications you may use in pretransfer
treatment?
2) What are the minimum tests should the laboratory be able to perform in
order to confirm severe malaria?3) List 2 antibiotic medications used to manage cerebral malaria in Rwanda
CONTENT SUMMARY
The management of severe malaria must be done in either district hospital or the
national referral hospital (private or public) as ordered by the ministry of health.
The management of severe malaria should be done in either a district hospital
or a national referral hospital (private or public) that meets the correspondingrequirements of the Ministry of Health.
The minimum required criteria are:
1) Qualified staff, trained in the clinical management of malaria-by-Malaria Unit;
2) The existence of a continuous system of 24 hours clinical and paraclinical
follow-up of patients;
3) A laboratory with the capacity to at least do:
– Peripheral blood smear,
– Haemoglobin and haematocrit,
– Blood sugar and
– Proteinuria
4) Capacity to do a lumbar puncture (recommended in cerebral malaria form);
5) Possibility to transfuse in case of severe anaemia;
6) Possibility to provide oxygen;
7) Availability of the drugs and consumables required for the treatment of
severe malaria (IV quinine, 50% and 5% glucose, Phenobarbital, diazepam,antipyretics and furosemide).
Pre-transfer treatment at the health centre
While preparing for the transfer of the patient, urgently administer IM artemether
or quinine IR or IV (IV infusion). Depending on the general condition of the patient
(weak pulse or not, dehydration or none), the health centre staff will administer,
either:
• Quinine, preferably by intravenous infusion as a loading dose of 20 mg per
kg body weight to run in 4 hours (not exceeding a total dose of 1200 mg for
the loading dose); or
• Quinine by intrarectal route in children, as 20 mg per kg body weight diluted
in 4 ml of distilled water or physiological solution, administered with a 5-ml
syringe. The drug is gently guided through the anus and the buttocks are held
together for 5 minutes to prevent the premature reflex expulsion of the drug.
If the drug is expelled within the first 10 minutes following its administration,
administration is repeated using half the original dose. Diarrhoea and anal
lesion limit the use of this route for the administration of drugs
• Arthemether IM 3.2 mg per kg body weight administered as a single dose
before transferring the patient.
Note:
• Regardless of the pre-transfer treatment that is given (loading dose of Quinine
or Arthemether), treatment with Quinine in intravenous infusion continues at
a dose of 10 mg of quinine per kg body weight diluted in 10ml of 5% or 10%
Glucose per kg body weight every 8 hours.
• For cerebral malaria, administer the first dose of antibiotics:
For children: Ampicillin 50 mg/kg body weight per dose, four times a day to which is
added chloramphenicol 25 mg/ kg body weight per dose, four times a day.
For adults: Ampicillin 1.5 g four times a day and chloramphenicol 1 g four times a
day;
Note: The intramuscular use of Quinine is prohibited in all health facilities in
Rwanda!!
• In case of hypovolaemia (severe anemia, rapid breathing, coma or systolic
BP < 80 mm Hg), start with normal saline or Ringer’s lactate infusion in a
dose of 20 ml/kg to run for 30 minutes to move the patient out of shock.
• For malnourished children (kwashiorkor or marasmus), give the loading dose
of quinine in IV perfusion without fluid replacement (as it is difficult to assess
hypovolaemia and dehydration, fluid replacement can increase the risk of
circulatory overload).
• The administration of quinine in intravenous infusion is preferable in cases of
signs of vital distress (repeated convulsions, coma, respiratory distress, and
cardio-vascular shock).
In the case where it has been impossible to establish
an intravenous line to administer quinine intravenously, use intramuscular
artemether or intra-rectal quinine.
Symptomatic treatment
If the temperature is higher or equal to 38°C:
• Do sponging;
• Give Paracetamol 15 mg /kg body weight by oral route or suppository form,
or any other antipyretic that may be indicated.
To prevent hypoglycaemia (characterized by lack of consciousness, severe
weakness):
• Give 20-50 ml of 50% hypertonic serum of glucose by intravenous injection
administered over 5-10 minutes in adults; and for children 3 ml/kg body weight
of 10% glucose or if not available 1 ml/kg of 50% glucose;
• Or administration of water with 10% sugar per mouth or with nasogastric
tube, at a rate of 5 ml/kg for children and 50 -100 ml for the adults.
Water with 10% sugar is readily prepared in the following way: take 100 ml of boiled
clean water and add 10 g of sugar or 2 coffee spoons.
In case of convulsions:
• Administer Diazepam 0.5 mg/kg body weight intrarectally for children and 10
mg slow IV for adults;
• If convulsions persist, give Phenobarbital 10-15 mg/kg IM;
• Treat or prevent hypoglycaemia;
• Treat fever if necessary.
Refer the patient to the nearest district hospital or national reference hospital.
Treatment of the severe malaria in the hospital
In children and adults
Administer a loading dose of 20 mg/kg body weight of quinine dihydrochloride (do
not exceed 1200 mg) diluted in an isotonic solution or 5 or 10% glucose on the
basis of 5 to 10 ml/kg body weight to run for 4 hours in IV perfusion. Then run IV
glucose 5 or 10% for 4 hours as maintenance drip.
Thereafter, i.e. 8 hours after the beginning of the administration of the loading dose
or 4 hours after the beginning of the maintenance drip, administer a maintenance
dose of 10 mg/kg body weight of quinine dihydrochloride in infusion, to run for 4
hours. This maintenance dose of quinine will be repeated every 8 hours until thepatient can swallow, normally within 48 hours at the most.
If after 48 hours the patient’s state doesn’t permit the patient to take quinine orally,
one may continue the drip of quinine by reducing the doses to 7 mg/kg every 8hours to run for 4 hours.
Change to oral quinine 10 mg/kg of quinine sulphate every 8 hours as soon as the
patient can swallow, to complete the 7 days of treatment or oral Artemether 20 mgand Lumefantrine 120 mg, as recommended for the treatment of simple malaria.
NB: For the patient whose body weight is over 60 kg, give the loading dose and
decrease the dose from 1200 mg to 800 mg after, divided into two doses for notexceeding 2000 mg per day,
• The loading dose of quinine is not administered if the patient received quinine
in the past 12 hours
• Never exceed 2 gm of daily dose of quinine.
• For the cerebral form of severe malaria (cerebral malaria or neurological
malaria), the association of IV antibiotherapy is recommended namely:
– Children: (Ampicillin 50 mg/kg /dose 4 times a day, plus Chloramphenicol
25 mg/kg/dose 4 times a day)
– Adults: (Ampicillin 1.5 g 4 times a day, plus Chloramphenicol 1g 4 times
day)
• For the anaemic form of severe malaria antibiotherapy is not indicated.
• The recommended dose for oral quinine is 10 mg Quinine salt per kg body
weight every 8 hours for 7 days;• Quinine Syrup is not nowadays recommended
Self-assessment 3.7
An adult pregnant woman is a worker in a sugar cane company. A week ago she
got tired by the end of the day. At home, she developed fever with sweating and
she vomited twice. She diagnosed herself as having malaria and she asked her
son to bring anti-malarial medication from a nearby pharmacy. She took the drug
for 2 days. Five days later she again developed fever, severe headache, nausea
and severe weakness. This time, she decided to go to the hospital. On physical
exam, the physician noticed conjunctiva pallor and laboratory results showed
haemoglobin of 5g/dL with positive blood smear. The physician diagnosed the
patient as having severe malaria, anaemic form.
1) Discuss how to manage this patient at the hospital.2) Is it advisable to give the antibiotic to this patient?
3.8. Treatment of malaria for pregnant women
Learning Activity 3.8
A health care provider working in the health centre received a call to see a
25-year-old pregnant woman presenting with fever. On examination, the provider
couldn’t detect any abnormality apart from the axillary temperature of 38.5°C.
The health care provider highly suspected malaria, although he thought of other
possible diseases. He then requested for the blood smear which showed malaria
parasite seen with + and he decided to institute the treatment.
1) What antimalarial medicine (s) would you give a pregnant woman with
uncomplicated simple malaria
2) A pregnant woman may never be treated with coartem because it canharm the baby. True or False
CONTENT SUMMARY
The malaria causes many problems to the pregnant women, prevention, early
detection and treatment are very important to reduce the mortality and morbidity
caused by malaria in pregnant women. This lesson is going to discuss the
management of malaria in pregnant women at family level, community level and
Health facility.
At the family level
Strengthen IEC on:
• Knowledge of the mode of transmission of malaria in Rwanda
• Utilisation of long-lasting insecticide treated mosquito nets as principle means
of prevention and other preventive measures
• Membership to the community health insurance schemes as a way of ensuring
better access to care
• Recognition of the signs of simple malaria, simple malaria with minor digestive
symptoms and severe malaria by the family members;
• Seeking timely care from the community health care worker or the nearest
health facility after lowering fever, if any, using tepid sponging.
At the Community level (Health Animator)
The role of the community health worker is to educate the pregnant woman on:
• The mode of transmission of malaria (mosquito bite);• The effects of malaria on pregnancy (on the mother and the baby)
• Recognition of the signs of the simple malaria, malaria with minor digestive
symptoms and severe malaria, and the ill effects of fever during pregnancy;
• The benefits of sleeping under long lasting insecticide treated nets
• Destruction of breeding sites (stagnant water)
• Seeking health care from the health facility as soon as they feel signs of
malaria
• The importance of taking all the drugs as prescribed by the health worker;
• The benefits of 4 ANC visits
At the level of the Health facility
To educate the pregnant woman on the preventive measures of malaria in pregnancy
during the antenatal consultations:
• What causes malaria and its transmission;
• The effects of malaria on the mother and the baby;
• The advantages of sleeping under long lasting insecticide treated mosquito
nets;
• The danger signs of severe malaria;
• The importance of seeking medical care when the symptoms of malaria
present;
• The importance of taking a complete dose of antimalarials,
• The benefits of 4 ANC visits.
Antenatal care
During antenatal care, the health facility staff must do the following to the pregnant
woman:
• Give her a long lasting insecticide treated mosquito net;
• Give other components of antenatal care: vaccination, iron, vitamin A and
Mebendazole;
• Discuss with her the program of the ANC visits;
• Record on the ANC card, her ANC appointment card, role of LLINs
• Register all illness relate to the pregnancy in the ANC register.
The management of malaria in pregnant women
Simple malaria
Because Malaria during pregnancy can aggravate latent anaemia, it is recommended
to do a complete clinical exam.
• The first line treatment of malaria in pregnancy is quinine sulphate per os 10
mg/kg/dose, 3 times a day for 7 days during the first trimester of pregnancy.
COARTEM is indicated during the 2nd and 3rd trimesters of pregnancy only.
Note:
• In case of fever, administer paracetamol tablets, 500 mg three times per day;
• Directly observe the woman as she swallows the first dose of antimalarials;
• Respect the dose prescribed by the health provider;
• Record all the information on the ANC card, ANC register and the hospitalization
file;
• Give advice on the prevention of the malaria and the necessity to consult in
time in case of illness;
• Recommend to the pregnant woman to come back any time if the symptoms
persist and/or she develops signs of severe malaria.
Simple malaria with minor digestive symptoms
The symptomatology of this type of malaria is similar to the one described earlier in
children and adults. The alteration of the general status can be accentuated by the
vomiting and other symptoms related to the pregnancy.
• Curative treatment
First trimester:
Administer Quinine dihydrochloride in intravenous infusion: 10 mg/kg/dose diluted
in 10 ml of 5% or 10% glucose per kg, every eight hours until patient is able to take
drugs orally making sure the treatment does not exceed 24 hours. Once the patient
can take orally, complete the remaining quinine 3 X10 mg/kg/day to make 7 days
by oral route of drug administration.
Second and third trimester:
Depending on the general status and level of hydration of the patient, drugs may be
administered as follows:
Artemether by intramuscular injection:
Administered as dose of 160 mg immediately after the diagnosis followed by 80 mg
twelve (12) hours after.
If the patient’s condition does not improve within 24 of treatment, refer the patient
to the nearest district hospital. If the patient’s condition improves, change to oral
Artemether-lumefantrine twice a day for three consecutive days.
Quinine dihydrochloride by intravenous administration:
Administered as 10 mg per kg body weight per dose, diluted in 5 to 10 ml of 5% or
10% glucose per kg, every eight hours. If the patient’s condition does not improve
within 24 hours of treatment, refer the patient to the nearest district hospital.
If the patient’s condition improves, change to oral Artemether-Lumefantrine, twice
a day for three consecutive days, or to oral quinine in case of contraindications to
Artemether-Lumefantrine.
NB: Whatever the medicine and the mode of administration used, (IM artemether,
IR/IV quinine infusion), if the state of health of the patient doesn’t improve in 24
hours, do a rapid diagnostic test or blood smear and refer the patient with the
referral note or treatment file, giving detailed information on the treatment provided
so far, to the nearest hospital.
In this case of transfer, the loading dose won’t be administered at hospital.
• Symptomatic treatment
In case of diarrhoea or vomiting:
• Evaluate and monitor the state of hydration;
• Rehydrate with ORS or other available liquids and even introduce nasogastric
tube if necessary;
• Anti-emetics are not recommended.
In case of fever, administer paracetamol 15 mg/kg orally or any other antipyretic
that may be indicated.
Severe malaria in the pregnant woman
At the health centre
Severe malaria in the pregnant woman is characterized by the same signs as those
described earlier for adults and children.
While organizing an emergency transfer, administer loading dose by intravenous
infusion of quinine 20 mg/kg body weight in 10 ml of 5% or 10 % dextrose per kg to
run for 4 hours (without exceeding 1200 mg);
Artemether, 3.2 mg/ kg can be administered by intramuscular route during the 2nd
and 3rd trimester as pre- transfer treatment. It is important to do a complete clinical
examination of the woman and to regularly check the vitality of the fœtus.
• Symptomatic treatment
If the axillary temperature is ≥ 38°C, give paracetamol 500 mg 3 times per day if the
client is able to swallow, or any other antipyretic as it may be indicated.
For the prevention of hypoglycaemia that may be manifested by loss of
consciousness, severe asthenia:
• Give 20-50 ml of 50 % of dextrose by intravenous injection to run for 5-10
minutes; or administer water with 10 % sugar orally or by NGT (50 -100 ml).Preparation of water with 10% sugar
To make 100 ml of water with 10% sugar: take 100 ml of clean water and add to it
10 g (also equivalent to 2 teaspoons) of sugar.
• In case of convulsions:
– Administer diazepam, 10 mg IV slow; and if convulsions persist, administer
diazepam, 10 mg in 500 ml of 5 % glucose to run slowly.
– Treat or prevent hypoglycaemia;
– Treat the fever if necessary;
– Fill in the transfer card correctly and clearly,
– Record all the necessary information in the register and the ANC card;
– Refer the patient immediately to the nearest district or national referencehospital.
At the hospital
The treatment of severe malaria in pregnant women at the hospital level is the same
as in others adults. Some complications are more frequent in pregnant women and
require a particularly close monitoring. These include hypoglycaemia, respiratorydistress (APO) and severe anaemia.
NB: It is important to do close obstetrical follow-up in general and monitoring of the
fetal vitality in particular.
Choice of antimalarial drugs for the treatment of simple malaria with minor digestivesymptoms.

Self-assessment 3.8
1) An adult pregnant woman patient was admitted to the hospital because
of malaise, myalgia, abdominal pain, and high fever. The recent history
of the patient was significant for two paroxysmal attacks of chills, fever,
and vomiting. Physical examination revealed an acutely ill patient and
examination of a stained blood specimen revealed ring like and crescent like forms within the RBCs reflecting malaria disease.
a) Discuss curative treatment for pregnant woman suffering from malaria
with minor digestive symptoms in the first trimester
b) Discuss curative treatment for pregnant woman suffering from malaria
with minor digestive symptoms in the second and third trimesters.
c) Discuss treatment for pregnant woman suffering from malaria with minordigestive symptoms in symptomatic treatment.
3.9. Non-malarial antiprotozoal medications(miscellaneous antiprotozoals)
Learning Activity 3.9
A 35-year-old woman presents with a history of diarrhea and abdominal pain
for the past 3 days. You learnt that she recently had a trip in areas with poor
sanitation, and swallowed considerable amounts of river water. Her relative 30
years old man also presents with a history of diarrhea and abdominal pain for past
2 days after eating unfamiliar food during the trip. The first patient is diagnosed
with giardiasis after laboratory exams. The second patient is diagnosed with
amebiasis, and treatment should begin after obtaining appropriate specimens.
a) List at least three examples of drugs that can be used in the management
of the condition for the first patient with giardiasis.
b) List at least three examples of drugs that can be used in the managementof the condition for the second patient with amebiasis.
CONTENT SUMMARY
Several drugs used to treat malaria are also used to treat nonmalarial protozoal
infections, including chloroquine, primaquine, pyrimethamine, and atovaquone.
Other antiprotozoal drugs normally used against nonmalarial parasites include
iodoquinol, metronidazole, paromomycin, and pentamidine.
Use of other antiprotozoal agents may result to these adverse effects:
• CNS: headache, dizziness, ataxia, loss of coordination, peripheral neuropathy
• GI: nausea, vomiting, diarrhea, unpleasant taste, cramps, changes in liver
function
• Superinfections
The following are drug-drug interactions involved in the use of other antiprotozoal
agents:
• Alcohol: severe adverse effects with tinidazole and metronidazole. Avoid
alcohol for at least 3 days after treatment.
• Oral anticoagulants: increased bleeding with metronidazole and tinidazole
• Disulfiram: increased psychotic reactions with metronidazole and tinidazole.
Two weeks should elapse between tinidazole therapy and start of disulfiram.
AMEBIASIS
It is an intestinal infection caused by Entamoeba histolytica. It is often known as
amoebic dysentery. The disease is transmitted through fecal-oral route. Amebiasis is
characterized by mild to fulminant diarrhea. In worst cases, it is able to invade
extra intestinal tissue. Drugs of choice for amebiasis are iodoquinol, paromomycin,
metronidazole, and tinidazole.
Metronidazole
Metronidazole [Flagyl, Protostat, Metric 21], a drug in the nitroimidazole family, is
active against several protozoal species, including E. histolytica, G. lamblia, and
Trichomonas vaginalis. The drug is also active against anaerobic bacteria.
Therapeutic Uses
Metronidazole is a drug of choice for symptomatic intestinal amebiasis and
systemic amebiasis. Because most of each dose is absorbed in the small intestine,
metronidazole concentrations in the colon remain low, allowing amebas there to
survive.
To kill these survivors, metronidazole is followed by iodoquinol, an amebicidal drug
that achieves high concentrations in the colon.
Metronidazole is a drug of choice for giardiasis, and for trichomoniasis in males as
well as females. Many anaerobic bacteria are sensitive to metronidazole.
Metronidazole interacts with alcohol. Alcohol should be avoided 24 hours before
therapy and at least 48 hours after the last dose due a disulfiram type reaction.
Metronidazole decreased absorption of vitamin K from the intestines due to
elimination of the bacteria needed to absorb vitamin K, increased plasma
acetaldehyde concentration after ingestion of alcohol. Resultat: Alcohol causes a
disulfiram-like reaction; action of warfarin may be increased (increased bleeding
risk).
Adverse Effects.
Metronidazole produces a variety of untoward effects, but these rarely lead to
termination of treatment. The most common side effects are nausea, headache, dry
mouth, and an unpleasant metallic taste. Other common effects include stomatitis,
vomiting, diarrhea, insomnia, vertigo, and weakness. Harmless darkening of the
urine may occur, and patients should be forewarned. Certain neurologic effects
(numbness in the extremities, ataxia, and convulsions) occur rarely.
If these develop, metronidazole should be withdrawn. Metronidazole should not be
used by patients with active disease of the CNS. Carcinogenic effects have been
observed in rodents, but there is no evidence of cancer in humans.
Use in Pregnancy and Lactation.
Metronidazole readily crosses the placenta and is mutagenic in bacteria.
However, experience to date has not shown fetal harm in humans. Nonetheless,
it is recommended that metronidazole be avoided during the first trimester, and
employed with caution throughout the rest of pregnancy.
Metronidazole can be detected in breast milk up to 72 hours after administration.
Mothers should interrupt breast-feeding until 3 days after the last dose.
Preparations, Dosage, and Administration
Metronidazole [Flagyl, Protostat, Metric 21] is available in capsules (375 mg),
standard tablets (250 and 500 mg), and extended-release tablets (750 mg); in
solution for injection (5 mg/mL); and as a powder to be reconstituted for injection.
For protozoal infections, the oral formulations are used. Antibacterial therapy
usually requires IV treatment.
Dosages:
• adults, 500 to 750 mg 3 times a day for 7 to 10 days;
• children 35 to 50 mg/ kg/day in three divided doses for 7 to 10 days.
• Following treatment with metronidazole, iodoquinol is given for 20 days.
Tinidazole
Tinidazole [Tindamax] is an antiprotozoal drug similar to metronidazole. Both
agents are nitroimidazoles, and both have similar actions, indications, interactions,
and adverse effects.
Tinidazole has a longer half-life than metronidazole, and hence dosing is more
convenient (it’s done less often and on fewer days). However, metronidazole is
much less expensive.
Therapeutic Uses
Tinidazole is indicated for trichomoniasis in adults, and for giardiasis, intestinal
amebiasis, and amebic liver abscesses in adults and children over 3 years of
age. Like metronidazole, tinidazole is considered a drug of choice for all of these
infections.
Tinidazole has a half-life of 12 to 14 hours, nearly twice that of metronidazole.
Adverse Effects
Adverse effects are like those of metronidazole, although tinidazole is better
tolerated. Gastrointestinal effects metallic taste, stomatitis, anorexia, dyspepsia,
nausea, vomiting are most common. Like metronidazole, tinidazole carries a small
risk of seizures and peripheral neuropathy. If abnormal neurologic signs develop,
tinidazole should be immediately withdrawn. In patients with existing CNS disease,
tinidazole should be used with caution.
Use in Pregnancy and Lactation
Tinidazole is in FDA Pregnancy Risk Category C: Animal studies show a risk of fetal
harm, but no controlled studies have been done in women. Like metronidazole,
tinidazole should not be used during the first trimester of pregnancy.
Tinidazole can be detected in breast milk up to 72 hours after administration.
Mothers should not breast-feed while taking the drug and for 3 days after.
Drug Interactions
Like metronidazole, tinidazole has disulfiram-like actions, and hence patients should
not consume disulfiram itself, alcoholic beverages, or any product that contains
alcohol.
Preparations, Dosage, and Administration
Tinidazole [Tindamax] is available in 250- and 500-mg tablets. For patients unable
to swallow tablets whole, the tablets may be crushed and mixed with cherry syrup.
To minimize GI distress, tinidazole should be taken with food.
Dosages are as follows:
Intestinal amebiasis:
• adults, 2 gm once daily for 3 days;
• children, 50 mg/kg (maximum 2 gm) once daily for 3 days
Amebic liver abscess:
• adults, 2 gm once daily for 5 days;
• children, 50 mg/kg (maximum 2 gm) once daily for 5 days
TRICHOMONIASIS
It is caused by Trichomonas vaginalis, a flagellated protozoan.
A common cause of vaginitis (reddened, inflamed vaginal mucosa, itching, burning,
and yellowish-green discharge).
It is usually transmitted through sexual intercourse and Asymptomatic in men
Metronidazole is the traditional drug of choice.
Dosage:
• Adults, either 2 gm just once or 500 mg twice a day for 7 days;
• Children, 5 mg/kg 3 times a day for 7 days.
However, tinidazole is just as effective and somewhat better tolerated but much
more expensive.
Tinidazole
Dosage:
• adults, 2 gm once;
• children, 50 mg/kg (maximum 2 gm) once
TRYPANOSOMIASIS
There are two major forms of trypanosomiasis: American trypanosomiasis and
African trypanosomiasis. Both forms are caused by protozoal species in the genus
Trypanosoma.
American Trypanosomiasis (Chagas’ Disease)
Chagas’ disease is caused by T.cruzi, a flagellated protozoan. It is passed to
humans by common housefly. It is characterized by severe cardiomyopathy.
In its early phase, Chagas’ disease can be treated with nifurtimox or benznidazole.
Unfortunately, these drugs are less effective against chronic infection.
African Trypanosomiasis (Sleeping Sickness)
African trypanosomiasis, transmitted by the bite of the tsetse fly, is caused by
two subspecies of Trypanosoma brucei: T. brucei gambiense, which causes West
African sleeping sickness, and T. brucei rhodesiense, which causes East African
sleeping sickness.
During the early (hemolymphatic) phase of African trypanosomiasis, pentamidine
and suramin are the drugs of choice. (Pentamidine is preferred for disease caused
by T. brucei gambiense, and suramin is preferred for disease caused by T. brucei
rhodesiense.) During the late (CNS) stage, melarsoprol and eflornithine are drugs of
choice. (Either drug can be used against T. brucei gambiense, but only melarsoprol
is preferred for T. brucei rhodesiense).
All four drugs pentamidine, suramin, eflornithine, and melarsoprol can produce
serious side effects. Treatment is difficult and frequently unsuccessful.
Benznidazole
Benznidazole [Rochagan, in Brazil], a relative of metronidazole and tinidazole, is a
drug of choice for American trypanosomiasis (Chagas’ disease). The adult dosage
is 2.5 to 3.5 mg/kg twice daily, and the pediatric dosage is 5 mg/kg twice daily. For
adults and children, the duration of treatment is 30 to 90 days.
Pentamidine
Target Diseases and Actions.
Pentamidine [Pentam 300, Pentacarinat, NebuPent] is highly effective against
West African sleeping sickness, a disease is caused by T. brucei gambiense, and
against pneumocystis pneumonia (PCP), a disease caused by a fungus named
Pneumocystis jiroveci (formerly thought to be Pneumocystis carinii). The drug has
multiple actions, including disrupting the synthesis of DNA, RNA, phospholipids,
and proteins. However, we don’t know which of these actions is responsible for
antiprotozoal effects.
• West African Sleeping Sickness
Pentamidine is given by IM injection to treat sleeping sickness.
Pharmacokinetics
For treatment of active PCP, Pentamidine is administered IM or IV. Equivalent blood
levels are achieved with both routes. The drug is extensively bound in tissues.
Penetration to the brain and cerebrospinal fluid is poor. Between 50% and 65% of
each dose is excreted rapidly in the urine. The remaining drug is excreted slowly,
over a month or more.
Adverse Effects Associated with Parenteral Pentamidine
Pentamidine can produce serious side effects when given IM or IV. Caution is
needed.
Sudden and severe hypotension occurs in about 1% of patients. The fall in blood
pressure may cause tachycardia, dizziness, and fainting. To minimize hypotensive
responses, patients should receive the drug while lying down. Blood pressure
should be monitored closely.
Hypoglycemia and hyperglycemia have occurred. Hypoglycemia has been
associated with necrosis of pancreatic islet cells and excessive insulin levels. The
cause of hyperglycemia is unknown. Because of possible fluctuations in glucose
levels, blood glucose should be monitored daily.
Intramuscular administration is painful. Necrosis at the injection site followed by
formation of a sterile abscess is common.
Some adverse effects can be life threatening when severe. These reactions and
their incidences are leukopenia (2.8%), thrombocytopenia (1.7%), acute renal
failure (0.5%), hypocalcemia (0.2%), and dysrhythmias (0.2%).
Adverse Effects Associated with Aerosolized Pentamidine
Inhaled pentamidine does not cause the severe effects associated with parenteral
pentamidine. The most common reactions are cough (38%) and bronchospasm
(15%). Both reactions are more pronounced in patients with asthma or a history
of smoking. Fortunately, these reactions can be controlled with an inhaledbronchodilator. They rarely necessitate pentamidine withdrawal.
Preparations, Dosage, and Administration of Pentamidine
West African Sleeping Sickness
Administration of pentamidine is by IM injection. The dosage for adults and children
is 4 mg/kg/day for 7 days.
Suramin
Actions and Uses
Suramin sodium [Germanin] is a drug of choice for the early phase of East African
trypanosomiasis (sleeping sickness); for the late phase of the disease (ie, the stage
of CNS involvement), melarsoprol and eflornithine are preferred. Suramin is known
to inhibit many trypanosomal enzymes; however, its primary mechanism of action
has not been established.
Pharmacokinetics
The drug is poorly absorbed from the GI tract, and hence must be given parenterally
(IV). Suramin binds tightly to plasma proteins and remains in the bloodstream for
months. Penetration into cells is low. Excretion is renal.
Adverse Effects
Side effects can be severe, and hence treatment should take place in a hospital.
Frequent reactions include vomiting, itching, rash, paresthesias, photophobia, and
hyperesthesia of the palms and soles. Suramin concentrates in the kidneys and
can cause local damage, resulting in the appearance of protein, blood cells, and
casts in the urine. If urinary casts are observed, treatment should cease.
Rarely, a shock-like syndrome develops after IV administration. To minimize the risk
of this reaction, a small test dose (100 to 200 mg) is administered; in the absence
of a severe reaction, full doses may follow.
Preparations, Dosage, and Administration
Suramin sodium [Germanin] is available from the CDC Drug Service. The drug
is supplied in 1-gm ampules. Administration is by slow IV infusion. Suramin is
unstable, and hence fresh solutions must be made daily. The adult dosage is 1 gm
IV on days 1, 3, 7, 14, and 21. The paediatric dosage is 20 mg/kg IV on days 1,
3, 7, 14, and 21. Possible revisions in these dosage recommendations should be
obtained from the CDC.
Melarsoprol
Therapeutic Use
Melarsoprol [Arsobal, Mel-B] is a drug of choice for both East African and West
African trypanosomiasis (sleeping sickness). The drug is employed during the late
stage of the disease (ie, after CNS involvement has developed). For earlier stages,suramin and pentamidine are preferred.
Mechanism of Action
Melarsoprol is an organic arsenical compound that reacts with sulfhydryl groups of
proteins. Antiparasitic effects result from inactivation of enzymes. This same action
appears to underlie the serious toxicity of the drug.
Melarsoprol is more toxic to parasites than to humans because it penetratesparasitic membranes more easily than human cells.
Adverse Effects
Melarsoprol is quite toxic, and hence adverse reactions are common. Frequent
effects include hypertension, albuminuria, peripheral neuropathy, myocardial
damage, and Herxheimer-type reactions. Reactive encephalopathy develops in10% of patients, and carries a 15% to 40% risk of death.
Preparations, Dosage, and Administration
Melarsoprol [Arsobal, Mel-B] is administered by slow IV injection. The drug is highly
irritating to tissues, and hence avoiding extravasation is important. Because of its
toxicity, melarsoprol should be administered in a hospital setting. Melarsoprol canbe obtained through the CDC Drug Service. The drug is not available commercially.
East African Trypanosomiasis
Treatment for adults and children consists of an initial course (2 to 3.6 mg/kg IV
daily for 3 days) followed in 7 days by a second course (3.6 mg/kg IV daily for 3days), followed in 7 days by a third course (3.6 mg/kg IV daily for 3 days).
West African Trypanosomiasis
The dosage for adults and children is 2.2 mg/kg/day for 10 days.
Eflornithine
Actions and uses
Eflornithine [Ornidyl] is indicated for patients with late-stage African trypanosomiasis
(sleeping sickness). The drug is highly effective against T. gambiense (West African
sleeping sickness), but only variably active against T. rhodesiense (East African
sleeping sickness). In both cases, benefits derive from irreversible inhibition of
ornithine decarboxylase, an enzyme needed for biosynthesis of polyamines, which
are required by all cells for division and differentiation. Parasites weakened by
eflornithine become highly vulnerable to lethal attack by host defenses. Because
cells of the host can readily synthesize more ornithine decarboxylase to replace
inhibited enzyme, cells of the host are spared. Eflornithine is also available in a
topical formulation, marketed as Vaniqa, for use by women to remove unwantedfacial hair.
Pharmacokinetics
Eflornithine is given IV. Once in the blood, the drug is well distributed to body fluids
and tissues, including the CNS. Eflornithine has a half-life of 100 minutes and iseliminated largely unchanged in the urine.
Adverse Effects
The most common adverse effects are anemia (48%), diarrhea (39%), and leukopenia
(27%). Seizures may occur early in therapy but then subside, despite continued
treatment. Because IV administration of eflornithine requires large volumes of fluid,
fluid overload may develop over the course of treatment. Eflornithine can also causehair loss. In fact, the drug is now available for topical use to remove facial hair.
Preparations, Dosage, and Administration
Eflornithine is supplied as a concentrated solution (200 mg/mL in 100-mL vials) and
must be diluted for IV infusion. To treat West African sleeping sickness in adults andchildren, the dosage is 100 mg/kg IV 4 times a day for 14 days.
Nifurtimox
Therapeutic Use
Nifurtimox [Lampit] is a drug of choice for American trypanosomiasis (Chagas’
disease). The drug is most effective in the acute stage of the disease, curing about
80% of patients. Chronic disease is less responsive.
Pharmacokinetics
Nifurtimox is well absorbed from the GI tract and undergoes rapid and extensivemetabolism. Metabolites are excreted in the urine.
Adverse Effects
Therapy is prolonged, and significant untoward effects occur often. Gastrointestinal
effects (anorexia, nausea, vomiting, abdominal pain) and peripheral neuropathy are
especially common. Weight loss resulting from GI disturbance may require treatment
to stop. Additional common reactions include rash and CNS effects (memory loss,
insomnia, vertigo, headache). In people with a deficiency of glucose-6-phosphatedehydrogenase, nifurtimox can cause hemolysis.
Preparations, Dosage, and Administration
Nifurtimox [Lampit] is supplied in 100-mg tablets. In the United States, the drug is
available only from the CDC Drug Service. The adult dosage is 8 to 10 mg/kg/day
(in three or four doses) for 90 to 120 days. For young children (ages 1 through 10
years), the dosage is 15 to 20 mg/kg/day (in four doses) for 90 to 120 days. For
older children (ages 11 to 16 years), the dosage is 12.5 to 15 mg/kg/day (in fourdoses) for 90 to 120 days.
PNEUMOCYSTOSIS
It is caused by Pneumocystis jirovecii (formerly Pneumocystis carinii), used to be
classified as a protozoal infection; however, it is now classified as fungal infection. It
is a common infection that complicates HIV and AIDS. It is discussed in this chapter,
as opposed to the antifungal, because antifungal drugs are not effective to treat it.
For therapy of PCP, pentamidine is given parenterally and by inhalation. Parenteral
therapy is used to treat active PCP. In contrast, inhalational therapy is used to
prevent PCP in high-risk HIV positive patients, defined as patients with (1) a history
of one or more episodes of PCP or (2) peripheral CD4 lymphocyte counts below
200 cells/mm3. Bronchospasm or cough is more likely to occur when inhaled
treatments of pentamidine are given.
Pentamidine isethionate for injection [Pentam 300, Pentacarinat] is supplied in 300-mg, single-dose vials.
For treatment of active PCP, the dosage for adults and children is 3 to 4 mg/kg IV
daily for 2 to 3 weeks. Administration must be done slowly (over 60 minutes).
Pentamidine isethionate aerosol [NebuPent] is used for prophylaxis of PCP in
patients with AIDS. The dosage is 300 mg once every 4 weeks. Administration is
performed with a Respirgard II nebulizer by Marquest. Solutions should be freshly
prepared.
TOXOPLASMOSIS
Toxoplasmosis is caused by infection with Toxoplasma gondii, a protozoan of the
class Sporozoa. The treatment of choice is pyrimethamine plus sulfadiazine.
Pyrimethamine
Pyrimethamine [Daraprim], combined with sulfadiazine, is the treatment of choice
for toxoplasmosis. Pyrimethamine (combined with sulfadoxine) is also used to treat
malaria. For toxoplasmosis, the adult dosage is 25 to 100 mg PO daily for 3 to 4
weeks. The pediatric dosage is 2 mg/kg PO daily for 2 days, followed by 1 mg/kg
PO daily for 4 weeks.
For adults and children, each dose of pyrimethamine should be accompanied by
10 mg of folinic acid (to reduce side effects). In addition, the regimen must include
sulfadiazine: for adults, 1 to 1.5 gm 4 times a day for 3 to 4 weeks; for children, 100to 200 mg/kg/day for 3 to 4 weeks.
GIARDIASIS
Giardiasis is an infection with Giardia lamblia, also known as G. duodenalis.
Transmission is through contaminated water or food, and trophozoites.
Characterized by diarrhea, rotten egg-smelling stool, and pale and mucus-filled
stool. Some patients experience epigastric pain, weight loss, and malnutrition.
Drugs of choice are metronidazole, Tinidazole, and nitazoxanide.
Metronidazole: •adults, 250 mg 3 times a day for 5 days; children, 5 mg/kg 3 times
a day for 5 days. (more information on Metronidazole check on amebiasis drugs).
Tinidazole: adults, 2 gm once; children, 50 mg/kg (maximum 2 gm) once
Nitazoxanide
Nitazoxanide [Alinia] is the treatment of choice. The drug is very effective in
immunocompetent patients, and may also work in some who are immunosuppressed.
Therapeutic Uses
Nitazoxanide [Alinia] is approved for diarrhea caused by G. lamblia in children and
adults. Although we have other effective drugs for giardiasis (eg, metronidazole,
tinidazole), nitazoxanide is our first effective drug for cryptosporidiosis. Unfortunately,
when used for C. parvum infections, nitazoxanide is only effective in children who
are immunocompetent; among children who are immunosuppressed, the drug is no
more effective than placebo.
Results in immunocompromised adults may be more favorable: When given to
adults with cryptosporidiosis and AIDS, a dosage of 1000 mg twice a day for 14
days cured 67% of patients, compared with 25% of those receiving placebo.
Actions
Nitazoxanide appears to work by disrupting protozoal energy metabolism.
Specifically, the drug blocks electron transfer mediated by pyruvate: ferredoxin
oxidoreductase, and thereby inhibits anaerobic energy metabolism.
In addition to its activity against C. parvum and G. lamblia, nitazoxanide is active
against other enteric protozoa (Isospora belli and Entamoeba histolytica) as well as
some helminths, including Ascaris lumbricoides, Ancylostoma duodenale, Trichuris
trichiura, Taenia saginata, and Fasciola hepatica.
Pharmacokinetics
Nitazoxanide is well absorbed following oral administration. In the blood, the
drug undergoes rapid conversion to its active metabolite, tizoxanide, which
then undergoes nearly complete (more than 99.9%) binding to plasma proteins.
Tizoxanide levels peak between 1 and 4 hours after nitazoxanide administration,and then decline owing to excretion in the urine, bile, and feces.
Adverse Effects
Nitazoxanide is generally well tolerated. In clinical trials, the most common adverse
effects were abdominal pain, diarrhea, vomiting, and headache. However, theseeffects were just as common in subjects taking placebo.
In some patients, the drug caused yellow discoloration of the sclerae (whites of the
eyes), which resolved following drug withdrawal. Nitazoxanide is in FDA PregnancyRisk Category B: Animal studies show no evidence of impaired fertility or fetal harm.
Drug Interactions
Because nitazoxanide is highly protein bound, it might interact with other agents
that are highly bound. Specifically, nitazoxanide might displace other drugs from
their binding sites, thereby increasing their effects and, conversely, other highly
bound agents could displace nitazoxanide, thereby increasing its effects.Preparations, Dosage, and Administration
Oral Suspension
Nitazoxanide oral suspension [Alinia] is indicated for diarrhea caused by G. lamblia
or C. parvum in children ages 1 through 11 years, and for diarrhea caused by G.
lamblia (but not C. parvum) in adults. Nitazoxanide is supplied as a pink powder
that, when mixed with 48 mL of water, forms a strawberry-flavored, 20-mg/mL
suspension. Administration is done with food. The suspension may be stored at
room temperature for 7 days, after which it should be discarded. Dosage depends
on age as follows:
• For children ages 12 to 48 months, give 100 mg (5 mL) every 12 hours for 3
days.
• For children ages 4 to 11 years, give 200 mg (10 mL) every 12 hours for 3
days.
• For patients 12 years and older, give 500 mg (25 mL) every 12 hours for 3
days.
Nitazoxanide tablets [Alinia] are indicated only for diarrhea caused by G. lamblia,
and only for patients at least 12 years old. The dosage is 1 tablet (500 mg) every 12hours for 3 days. Administration is done with food.
LEISHMANIASIS
The term leishmaniasis refers to infestation by certain protozoal species belonging
to the genus Leishmania.
It is a disease caused by a protozoan that is passed from sand flies to humans. It
is characterized by serious lesions in the skin, viscera, and mucous membranes ofhost.
For all forms of leishmaniasis, sodium stibogluconate (given IM or IV) is the
traditional treatment of choice. Amphotericin B (given IV) is an effective alternative.
Miltefosine, an oral agent, is highly curative against visceral leishmaniasis, and
probably against cutaneous disease. The drug appears reasonably safe and, owing
to oral administration, is more convenient than stibogluconate or amphotericin B,both of which are given parenterally.
Sodium Stibogluconate
Sodium stibogluconate [Pentostam] is a drug of choice for leishmaniasis. The
mechanism of action is unknown. The drug is poorly absorbed from the GI tract,
and hence must be given parenterally (IM or IV). Sodium stibogluconate undergoes
little metabolism and is excreted rapidly in the urine. Although severe side effects
can occur, the drug is generally well tolerated. The most frequent adverse reactionsare muscle pain, joint stiffness, and bradycardia.
Changes in the electrocardiogram are common and occasionally precede serious
dysrhythmias. Liver and renal dysfunction, shock, and sudden death occur rarely.
Sodium stibogluconate is supplied in aqueous solution for IM and IV injection. For
leishmaniasis, the usual adult and paediatric dosage is 20 mg/kg/day (IM or IV) for20 to 28 days.
Miltefosine
Miltefosine [Impavido] is the first oral agent for leishmaniasis. The drug was originally
developed to treat cancer. Antiprotozoal activity wasn’t revealed until miltefosine was
tested in cancer patients who also had leishmaniasis. The mechanism underlyingbenefits in leishmaniasis is unclear.
Studies conducted in India indicate that oral miltefosine is both safe and effective
for treating visceral leishmaniasis. Preliminary studies indicate the drug is alsohighly effective against cutaneous disease.
Because miltefosine is taken by mouth, rather than by injection, the drug is much
more convenient than the alternatives, namely, sodium stibogluconate (administeredIM or IV) and amphotericin B (administered IV).
Miltefosine is better tolerated than either sodium stibogluconate or amphotericin B.The most common reactions are vomiting (38%) and diarrhea (20%).
Mild hepatotoxicity is seen in some patients, but it resolves during the second week
of treatment. Reversible renal damage may also occur. Miltefosine causes fetal
abnormalities in laboratory animals, and hence must not be used during pregnancy.
Effective contraception is required while taking the drug and for 2 months after.The recommended dosage for adults and children is 2.5 mg/kg/day for 28 days.
CRYPTOSPORIDIOSIS
Cryptosporidiosis is caused by Cryptosporidium parvum, a protozoan of the
subclass Coccidia. Nitazoxanide [Alinia] is the treatment of choice. The drug is
very effective in immunocompetent patients, and may also work in some who areimmunosuppressed.
Nitazoxanide [Alinia] is approved for diarrhea caused by C. parvum in children only.
Unfortunately, when used for C. parvum infections, nitazoxanide is only effective in
children who are immunocompetent; among children who are immunosuppressed,the drug is no more effective than placebo.
Results in immunocompromised adults may be more favorable: When given to
adults with cryptosporidiosis and AIDS, a dosage of 1000 mg twice a day for 14
days cured 67% of patients, compared with 25% of those receiving placebo. Moreinformation on Nitazoxanide please read on G. lamblia.
Self-assessment 3.9
1) Which drug is used mainly for the management of Pneumocystis jirovecii
(formerly Pneumocystis carinii) pneumonia?
a) Metronidazole (Flagyl)
b) Pentamidine (NebuPent)
c) Iodoquinol (Yodoxin)
d) Chloroquine
2) An adult woman complains of itching and burning around her vagina and
foul-smelling vaginal discharge. A nurse suspects trichomoniasis. Which
of the following drugs would be appropriate for this patient?
a) Iodoquinol
b) Suramin
c) Sulfadoxine
d) Metronidazole
3) In which of the following conditions may suramin be indicated?
a) Trypanosomiasis
b) Trichomoniasis
c) Giardiasis
d) Amebiasis
4) All of the following are the uses of metronidazole, EXCEPT:
a) Amebiasis
b) Giardiasis
c) Trichomonas vaginitisd) Malaria
3.10. Health Education about Malaria and Amebiasis Treatment
Learning Activity 3.10
1) Why is it important to take a person with symptoms of malaria to the
nearest health centre or hospital immediately?
2) Why is it important to finish all medications even if patient starts feeling
better?
3) The nurse teaches a patient who is prescribed metronidazole (Flagyl) that
it is very important to report which possible adverse effect of the drug to
the prescriber?
a) Darkening of the urine
b) Metallic taste
c) Mouth ulcers
d) Both A and B
4) The following precaution should be advised to the patient who is taking
metronidazole
a) To avoid driving
b) To get leucocyte count checked every second day
c) To avoid alcoholic beveragesd) To avoid fatty/ fried food
CONTENT SUMMARY
A health education interventional is important to take appropriate prevention
measures to promote success of treatment and prevention of protozoal diseases.
Health education messages can provide information and address a variety
of misconceptions regarding the use of antiprotozoal drugs to prevent drug
administration’s errors.
Patient education is also a basic right of the patients and healthcare members.
People should receive instruction in clear language or information on treatment
and prevention measures from health care providers by using posters, video clips,
radio, and other forms of mass media. Other methods include peer education,mobilization at all levels of public sectors, and school-based programs.
Health education about malaria treatment is guided by many main factors
include: the infecting species/parasites, the clinical status of the patient, and the
drug susceptibility of the infecting parasites. People should receive instruction or
information on treatment and prevention when traveling to known malaria-endemic
regions of the world.
When health care provider is preparing health education about malaria treatment
he/she must emphasize on why it is important to take a person with symptoms of
malaria to the nearest health care facility immediately.
– Because to be tested for malaria or other illness. The only way to know for
sure if you have malaria is to be tested. If you test positively, then you can
receive the proper treatment for malaria.
– because to get proper diagnosis and appropriate treatment help health
care providers to avoid complications that might lead to serious condition
or even death of patient.
Emphasize also on why it is important to finish all medications even if patient start
feeling better? Patients should receive instruction to take medication as prescribed
and adhere to the full prescription regimen in order to promote success of treatment
(kills the parasite in the sick person & saving the life of an infected person), to
prevent treatment failure, stops transmission to healthy people, ensure complete
cure, on-going protection and will prevent the drug from becoming less effective to
malaria infection (development of drug resistance).
Advice the patient to read carefully and follow carefully drugs manufacturer’s
instructions because every drug differs to another.
Explain to the patient and family members what they should do if they missed a
dose.
In the instance that you miss a dose, take it as soon as possible that day. For daily
regimes, if you miss the dose completely for that day, skip the missed dose entirely
and continue with your next dose. Never take a double dose to make up for a
missed dose.
It’s important to take your antimalarial medication consistently and for the full course
of your prescription. If your medication regime requires you to take it daily, take it
at the same time each day (follow dosing orders and instructions as prescribed,
with specific attention to the loading doses, subsequent doses, and prophylactic
dosing). For weekly regimes, take it on the same day each week.
It’s always advisable to purchase all necessary medication prior to your departure.
However, in the event that you need antimalarial medication at your destination,you should only purchase medication from a reputable pharmacy.
With antimalarials, encourage adequate dietary and fluid intake while the patient is
fighting the infection and taking the medications. Oral doses need to be taken with
water or other fluid. Increase fluids unless contraindicated, because antimalarialsconcentrate in the liver first.
Never take more than the prescribed dose. Taking too much quinine can cause
serious problems. Also, quinine is dangerous if it is taken by a child, so keep the
tablets away from children. If you suspect that someone has taken an overdose ofquinine or has swallowed some by accident, you must contact a doctor straightaway.
Alternatively, go to the accident and emergency department of a local hospital. Do
not delay. Take the container with you, even if it is empty. This helps the doctor to
know what patient has been taken. If you are being treated for diabetes, quinine
can lower the level of sugar in your blood. Your doctor will be able to advise youabout this.
Keep all medicines out of the reach and sight of children. Store in a cool and dryplace away from direct heat and light.
Photosensitivity may occur with quinine; provide adequate teaching about the
use of sunscreen and sun safety. Sun protection must include coverage againstultraviolet rays.
Educations session on malaria prevention must emphasize on both drug and
nondrug (controlling Anopheles Mosquitoes) prevention measures by using the
using the ABCD approach (Awareness of risk, Bite prevention, Check whether youneed to take malaria prevention tablets and Diagnosis).
For awareness of risk: find out whether the patient is at risk of getting malaria. It’s
important to visit a health care provider before the travel for advice, check whether
it is necessary or need to take preventative malaria treatment depending on the
country you are visiting. Some country it is not necessary to take preventative
malaria treatment before travelling. Even if you grew up in a country where malaria
is common, you still need to take precautions to protect yourself from infection ifyou’re travelling to a risk area.
NB: In area where malaria vaccine is not yet introduced, health care provider has
to educate people that nobody has complete immunity to malaria, and any level of
natural protection you may have had is quickly lost when you move out of a riskarea.
For bite prevention: An Integrated Mosquito Management (IMM) program helps
to prevent mosquito bites and transmission of serious vector diseases. To target
all phases of the mosquito’s life cycle, four approaches are useful in controllingAnopheles Mosquitoes.
1) Public Education: we rely on a well-educated public in order to have a
successful mosquito control program. Educating the public empowers
people to take control of the mosquitoes.
2) Surveillance: allows us to detect mosquito species in a given area as well
as any changes in populations. With this surveillance, we are able to have
more effectively time larvicides applications and more accurately target
adulticide activities.
3) Larval Mosquito Control: sources of standing water and any newly
discovered sites for the presence of mosquito larvae. Eliminating mosquitoes
prior to their becoming adults is an important element of controlling malaria
and other mosquito-borne diseases because it stops mosquitoes before
they acquire the virus and have the opportunity to transmit it to people.
4) Adult Mosquito Control: when necessary, adulticide applications are
conducted to prevent them from developing resistance; thereby, minimizing
the number of applications needed to control the population.
For prevent mosquito bites and transmission of serious vector diseases:
avoid mosquito bites by using insect repellent, covering your arms and legs, and
using a mosquito net. It’s not possible to avoid mosquito bites completely, but the
less you’re bitten, the less likely you are to get malaria.
To avoid being bitten:
• Stay somewhere that has effective air conditioning and screening on doors
and windows. If this isn’t possible, make sure doors and windows close
properly.
• If you’re not sleeping in an air-conditioned room, sleep under an intact
mosquito net that’s been treated with insecticide.
• Wear light, loose-fitting trousers rather than shorts, and wear shirts with long
sleeves particularly during early evening and at night, when mosquitoes
prefer to feed.
• Use insect repellent on your skin and in sleeping environments. Remember
to reapply it frequently. The most effective repellents contain diethyltoluamide
(DEET) and are available in sprays, roll-ons, sticks and creams.
The chemical DEET is not recommended for babies who are less than 2 months
old.
DEET is safe for older children, adults and pregnant women if you follow the
manufacturer’s instructions: use on exposed skin, don’t spray directly on to your
face, spray into your hands and pat on to your face, avoid contact with lips and
eyes, wash your hands after applying, don’t apply to broken or irritated skin andmake sure you apply DEET after applying sunscreen, not before.
For check whether you need to take malaria prevention tablets: if you do, make
sure you take the right antimalarial tablets at the right dose, and finish the course toreduce your chances of getting the disease until vaccine become available for all.
However, antimalarials only reduce your risk of infection by about 90%, so taking
steps to avoid bites is also important. Depending on the type you’re taking, continue
to take your tablets for up to 4 weeks after returning from your trip to cover theincubation period of the disease.
Check with your health care provider to make sure you’re prescribed a medication
you can tolerate. You may be more at risk from side effects if you: have HIV or AIDS,
have epilepsy or any type of seizure condition, are depressed or have another
mental health condition, have heart, liver or kidney problems, take medicine, such
as warfarin, to prevent blood clots and use combined hormonal contraception, suchas the contraceptive pill or contraceptive patches.
If you’ve taken antimalarial medication in the past, don’t assume it’s suitable for
future trips. The antimalarial you need to take depends on which strain of malaria
is carried by the mosquitoes and whether they’re resistant to certain types ofantimalarial medication.
NB: In some cases, you may be prescribed emergency standby treatment for
malaria before you travel. This is usually if there’s a risk of you becoming infectedwith malaria while travelling in a remote area with little or no access to medical care.
Pregnant women: If you’re pregnant, it’s advisable to avoid travelling to areas
where there’s a risk of malaria because a pregnant women have an increased risk
of developing severe malaria, and both the baby and mother could experience
serious complications. It’s very important to take the right prophylactic measures
of malaria prevention (both drug and nondrug) if you’re pregnant and unable to
postpone or cancel your trip to an area where there’s a malaria risk. Some of the
antimalarials used to prevent and treat malaria are unsuitable for pregnant womenbecause they can cause side effects for both mother and baby.
Malaria is also particularly life-threatening and dangerous to pregnant women
and their babies. Malaria is harmful to pregnant women and their babies as the
malaria parasite destroys the blood cells and makes women anaemic. Anaemia in
the mother and malaria parasites in the placenta can lead to women giving birth to
babies early (pre mature) or born very small or die while still in the womb. Babies
who are born too early or are very small at birth as less likely to survive and behealthy.
For diagnosis: seek immediate medical advice if you have malaria symptoms,
including up to a year after you return from travelling. You must seek medical help
straight away if you become ill while travelling in an area where malaria is found, orafter returning from travelling, even if you’ve been taking antimalarial tablets.
Malaria can get worse very quickly, so it’s important that it’s diagnosed and treatedas soon as possible.
If you develop symptoms of malaria while still taking antimalarial tablets, either
while you’re travelling or in the days and weeks after you return, remember to
tell the health care provider which type you have been taking. The same type ofantimalarial shouldn’t be used to treat you as well.
Health education about amebiasis treatment
When health care provider is preparing health education about malaria treatment
he/she must emphasize on appropriate information on treatment and preventivemeasures.
When an Antiparasitic is prescribed on an outpatient basis; give the patient or
family member complete instructions about taking the drug, as well as householdprecautions that should be followed until the parasite is eliminated from the body.
When developing a patient education plan, be sure to include the following:
• Follow the dosage schedule exactly as prescribed to eradicate the parasite.
It is important to explain to the patient how amebiasis treated, once your
health care provider has told you that you have amebiasis, you have to take
medication. Treatment must be prescribed by a health care provider and
specific treatment will vary from person to person.
• Advice the patient to read carefully and follow carefully drugs manufacturer’s
instructions because every drug differs to another.
• Follow-up stool/urine specimens will be necessary after taking Antiparasitic
drugs because this is the only way to determine the success of drug therapy.
• When an infection is diagnosed, multiple members of the family may beinfected, and all household members may need to be treated.
It is important to explain to the patient how is amebiasis spread. Amebiasis is
transmitted from person to person by the fecal-oral route. The spread of amebiasis
can occur if an infected person does not wash their hands properly after going to
the bathroom. When people touch objects or eat contaminated food they can get
the parasite on their hands and into their mouths. People are infectious as long
as the parasite is shed in the stool. The spread of amebiasis can be prevented by
public education about the importance of hand hygiene (perform wash hand withsoap and water) after defecation and before preparing or eating food.
It is important to ask patient inform if is pregnancy or breast feeding because some
antiprotozoal drugs should not be taken by women who are pregnant or breastfeeding.
• It is important to wash all bedding and bed clothes once treatment has started.• Daily bathing (showering is best) is recommended.
Disinfect toilet facilities daily, and disinfect the bathtub or shower stall immediately
after bathing. Use the disinfectant recommended by the primary health care provideror use chlorine bleach.
Scrub the surfaces thoroughly and allow the disinfectant to remain in contact withthe surfaces for several minutes.
During treatment for a ringworm infection, keep towels and facecloths for bathing
separate from those of other family members to avoid the spread of the infection. Itis important to keep the affected area clean and dry.
• Wash the hands thoroughly after urinating or defecating and before preparing
and eating food. Clean under the fingernails daily and avoid putting fingers in
the mouth or biting the nails.
• Food handlers should not resume work until a full course of treatment is
completed and stools do not contain the parasite.
• Child care workers should be especially careful of diaper disposal and proper
hand washing to prevent the spread of infections.
• Inform the patient taking metronidazole/Tinidazole for a sexually transmitted
disease like trichomoniasis to avoid sexual intercourse (as they may become
reinfected) until a full course of treatment is completed and samples (urine
or/and stool) do not contain the parasite , and advise the client that sexualpartners must be treated also.
If you are having giardiasis, you should wash your hands regularly and avoid
sharing utensils or towels to prevent the spread of infection among your householdmembers.
Before taking metronidazole, it is important that your health care provider knows:
If you are pregnant or breastfeeding.
• If you feel you will be unable to stop drinking alcohol for the duration of your
treatment.
• If you have any problems of liver function.
• If you are taking any other medicines• If you have ever had an allergic reaction to a medicine.
Advise the patient to take the tablets or liquid medicine exactly as prescribed.
Space your doses evenly throughout the day, and keep taking the medicine untilthe course is finished, unless he/she is told to stop by his/her doctor.
• Take each of your doses with a snack or just after eating a meal. Swallow the
tablets whole (that is, without chewing or crushing them) with a full glass of
water.
• If patient forget to take a dose, advise him/her to take it as soon as he/she
remember and try to space the remaining doses evenly throughout the restof the day. Do not take two doses together to make up for a forgotten dose.
• Advise the patients to avoid drink alcohol while they are on metronidazole and
for 48 hours after finishing the course of treatment. This is because drinking
alcohol with metronidazole is likely to make you feel very sick (nauseated) and
cause other unpleasant effects, such as the sensation of having a ‘thumping
heart’ (palpitations), hot flushes and headache.
• Tell the patients that while they are taking metronidazole their urine may look
a darker colour than normal. On its own this is nothing to worry about.
• When the patient is taking metronidazole for amebiasis instruct the patient
how to collect stool samples correctly and safely and how to dispose ofsamples properly.
Self-assessment 3.10
1) What should a patient do when he/she misses a dose of antiprotozoals?
2) What should patient do if she/he runs out or loses an antimalarial
medication?
3) What should patient do if he/she thinks that he/she has malaria?
4) A patient tells a nurse that he/she has been infected with malaria in the
past and asks a nurse whether he/she still needs to take antimalarialmedication?
3.11. End unit assessment
End of unit assessment
1) Which of the following are the factors which determine antimalarial agent
efficacy?
a) Species of the plasmodium
b) Life-cycle stage-dependencies
c) Both A and B are correct
d) Neither of the above
2) Which of the following drugs can cause cinchonism?
a) Chloroquine
b) Quinine
c) Artenisinind) Primaquine
3) A patient is infested by plasmodium ovale and is suffering from repeated
relapses. Which ONE of the following drugs can be used to prevent
relapses?
a) Chloroquine
b) Quinine
c) Artenisinin
d) Primaquine
4) Neuropsychiatric reactions are most likely to occur in persons treated
with:
e) Halofantrine
f) Quinine
g) Mefloquine
h) Artemisinin derivatives
5) All of the following are uses of metronidazole EXCEPT
a) Amebiasis
b) Giardiasis
c) Trichomoniasis
d) Malaria
6) For which of the following diseases is pentamidine the first line drug?
a) Toxoplasmosis
b) Pneumocystis carinii pneumonia
c) Actinomycosis
d) Leishmaniasis
7) Which of the following diseases is treated with metronidazole?
a) Roundworm infestation
b) Hookworm infestation
c) Kala-azard) Giardiasis
8) Tick the drug used for toxoplasmosis treatment:
a) Chloroquine
b) Tetracycline
c) Suramin
d) Pyrimethamine
9) Tick the drug used for amebiasis treatment:
a) Nitrofurantoin
b) Tinidazole
c) Pyrazinamide
d) Mefloquine
10) Choose correct answer Treatment of malaria is guided by;
a) The infecting plasmodium species
b) The clinical status of the patient
c) All the responses are correctd) The stage of the organism’s life cycle
