UNIT 1: ANTIBIOTICS
Key Unit competence:
Manage different health conditions at the primary healthcare settingsby utilizing antibiotics appropriately.
Introductory activity 1.0
The images below show different patients with bacterial infections andthey are being treated with different medications.
1) Have you even seen such kinds of patients?
2) If yes, what types of drugs you heard or saw they were taking?3) Have you ever seen some types of the drugs in these images?
1.1. Definition of antibiotics and key concepts
Learning Activity 1.1
1) Read the scenario below:
A 37-year-old female patient is on drugs that she takes every eight hours. She
was told that she has a disease that requires to be taken for 10 consecutive
days. Not all details were provided by the healthcare providers, and she heard
from different people that both antimicrobial and antibiotic agents may be used
for an extended period of time that can go beyond 10 days. She then doubts
whether she is taking an antibiotic or antimicribial, and wants to get your view.
Answer the questions below:
a) In details, differentiate antibiotic from antimicrobial agents
b) Give a difference between broad spectrum and narrow spectrumantibiotics
CONTENT SUMMARY
Antibiotics are medicines that fight bacterial infections in people and animals. They
work by killing the bacteria or by making it hard for the bacteria to grow and multiply.
Examples: Amoxicillin, Gentamicin, Cotrimoxazole.
An antimicrobial is a drug used to treat a microbial infection. “Antimicrobial” is a
general term that refers to a group of drugs that includes antibiotics, antifungals,
antiprotozoal, and antivirals. The antibiotics belong to the wide class of
antimicrobials.
Examples: Ketoconazole (antifungal), Metronidazole (antiprotozoal), and acyclovir
(Antiviral).Antibiotic drugs can be bacteriostatic or bactericidal.
“Bacteriostatic” refers to the ability of the agent (antibiotic) to prevent the growth of
bacteria while “bactericidal” is the ability of the agent to kill bacteria.
However, several antibiotics are both bactericidal and bacteriostatic, depending on
the concentration of the particular drug.
There is no perfect antibiotic that is without effect on the human host. Therefore,
health personnel try to select an antibiotic with selective toxicity, which is the ability
to strike foreign cells with little or no effect on human cells.
Antibiotics may be classified as having broad spectrum of activity or narrow spectrum
of activity. Narrow-spectrum antibiotics act against a limited group of bacteria whilebroad-spectrum antibiotics act against a larger group of bacteria.
Difference between narrow-spectrum and broad-spectrum antibiotics

Self-assessment 1.1
1) A colleague of class tells you that he is swallowing capsules of amoxicillin
as an antibiotic after having sustained an injury that developed pus. The
colleague wants to know what an antiotic is, and what it is used for. What
will you tell your colleague?2) Is there any relevance in prescribing such drug to your colleague?
1.2. Ideal antibiotics and Mechanism of action of antibiotics
Learning Activity 1.2
1) Read carefully the scenario below:
A 62-year-old female is admitted at the healthcare facility with features of an
infection. The laboratory investigations help to identify the causal agent of
the bacterial infection, and an appropriate antibiotic is prescribed basing on
the identified agent. The reason to choose the drug was mainly based on the
mechanism of action of the prescribed antibiotic against the infectious bacterial
agent. In addition, the healthcare provider chose an antibiotic basing on its
characteristics.
a) Describe the qualities of an ideal antibiotic the nurse will consider while
prescribing the antibiotic.
b) List the 5 main mechanisms of action of antibiotics?
c) Is it required to consider the mechanism of action of an antibiotic during
its prescription? Explain your answer.
Guidance: Read the book of pharmacology brought by the teacher inclass, on topic of Mechanism of action of antibiotics.
CONTENT SUMMARY
An ideal antibiotic is an antibacterial agent that kills or inhibits the growth of all
harmful bacteria in a host, regardless of site of infection without affecting beneficial
gut microbes (gut flora) or causing undue toxicity to the host. Ideal antibiotics should
be toxic to microbes, and not to humans, bactericidal rather than bacteriostatic,
effective against broad range of bacteria; active in placenta, and other body fluids;
cost effective; and should not cause allergic and hypersensitive reactions, should
not give drugs resistance, long shelf life
; and desired levels should be reached
rapidly and maintained for adequate period of time.
The antibiotics exert their effects through different mechanisms that alter or damage
the bacterial cell. This disruption of the bacterial cell function ends up in the death
of the bacteria, which is an expected outcome of the treatment with antibiotics. This
is made possible by the fact that bacterial prokaryotic cells have some differences
with the human cells, and the former become the target of antibiotic drug action.
Several different classes of antibacterials use a mechanism of “Inhibition of bacterial
cell wall synthesis” by blocking steps in the biosynthesis of peptidoglycan, making
cells more susceptible to osmotic lysis. Therefore, antibacterials that target cellwall biosynthesis are bactericidal in their action. Because human cells do not make
peptidoglycaa) Write the names of antibiotic drugs observed in the image above.
b) Put the drugs you identified in their respective classes.
c) What are the common side effects of antibiotics?n, this mode of action is an excellent example of selective toxicity.
A small group of antibacterials alter the bacterial cell membranes in their mode of
action. They interact with lipopolysaccharide in the outer membrane of gram-negative
bacteria, killing the cell through the eventual disruption of the outer membrane and
cytoplasmic membrane. For gram-positive bacteria, these antibacterials insert into
the cytoplasmic membrane of the bacteria, disrupting the membrane and killing thecell.
Other antibacterials inhibit bacterial protein synthesis. The cytoplasmic ribosomes
found in animal cells (80S) are structurally distinct from those found in bacterial
cells (70S), making protein biosynthesis a good selective target for antibacterialdrugs.
Some synthetic drugs control bacterial infections by functioning as antimetabolites,
competitive inhibitors for bacterial metabolic enzymes. In their mechanism of action,
these antibiotics may inhibit the enzyme involved in production of dihydrofolic acid,
they may inhibit the enzyme involved in the production of tetrahydrofolic acid orinterfere with the synthesis of mycolic acid.
Finally, some antibacterial drugs work by inhibiting bacterial nucleic acid synthesis.
In this case, these antibiotics inhibit bacterial RNA polymerase activity and blocks
transcription, killing the cell. Alternatively, they inhibit the activity of DNA gyrase andblocks DNA replication, killing the cell.
Self-assessment 1.2
Read the scenario below:
A 25-year-old female patient comes to the health post where you work. She
comes 3 days after starting treatment with antibiotics, complaining of additional
symptoms after starting the treatment. She reports severe diarrhea, nausea,
vomiting, many skin rashes, and difficult swallowing. The nurse receiving the
patient decided to change the antibiotic for the patient, and managed the
additional complaints.
The patient recovered after a short period of time.
1) In your understanding, was it necessary for the patient to come back to
the health post?
2) Was the first drug ideal antibiotic to the patient?
3) All of the following are the mechanisms of action of antibiotics, EXCEPT:
a) Inhibiting bacterial nucleic acid synthesis
b) Alter the bacterial cell membranes
c) Inhibit bacterial protein synthesis
d) Acting as bacterial metabolites
4) As human cells make peptidoglycan, this prevents the antibiotics fromexerting their selective toxicity effect. TRUE or FALSE
1.3. Drug resistance and prevention of antibiotic drug resistance
Learning Activity 1.3
1. Read carefully the scenario below:
A 17-year-old female adolescent was involved in unprotected sexual intercourse
and got infected with sexually transmitted bacteria. She consulted the nearest
health post and doxycycline has been prescribed as antibiotics to be taken
BID for 14 days. After taking first dose, she complained that the drug tasted
badly and refused to continue taking the drug. After 4 days, she felt severe
pain in lower abdomen with painful urination. She then took other 3 doses, the
symptoms reduced, and she stopped again. After the period of 1 month, she felt
again similar severe pain and consulted another health post and she was given
the same drug (doxycycline). She decided to take completely and correctly the
prescribed drug but after the completion of prescribed doses, the symptoms
persisted. She decided to consult the hospital to give sample for culture and
sensitivity. The laboratory results showed that doxycycline could not cure the
disease because microbes had developed the resistance against doxycycline.
a) According to you, what mistakes did the adolescent commit in taking the
initially prescribed drug?
b) Referring to the scenario above, how can antimicrobial drug resistance
develop? Explain your answer?
c) What type of resistance did this adolescent develop?
Guidance: Read the book on topic of antibiotic resistance provided by theteacher, and answer the questions above.
CONTENT SUMMARY
Antimicrobial resistance may develop anytime, when necessary, measures while
using antimicrobials are not taken. In nature, microbes are constantly evolving in
order to overcome the antimicrobial compounds produced by other microorganisms.
Human development of antimicrobial drugs and their widespread clinical use has
simply provided another selective pressure that promotes further evolution. Several
important factors can accelerate the evolution of drug resistance. These include
the overuse and misuse of antimicrobials, inappropriate use of antimicrobials,
sub therapeutic dosing, and patient noncompliance with the recommended course oftreatment. Resistance can be natural or acquired.
Anti-infectives act on specific enzyme systems or biological processes.
On one hand, many microorganisms that do not use that system or process are not affected
by a particular anti-infective drug. They are said to have a natural or intrinsic
resistance. On the other hand, microorganisms that were once very sensitive to the
effects of particular drugs have begun to develop acquired resistance to the agents.This is known as acquired resistance.
With the current use of antibiotics in humans and animals, emergence of resistant
strains of microbes is becoming a serious public health problem. Health care
providers must work together to prevent this issue, given that exposure to an
antimicrobial agent can lead to the development of resistance. It is therefore
important to limit the use of antimicrobial agents to the treatment of specific
pathogens known to be sensitive to the drug being used. Drug dosing is important
in preventing the development of resistance, and doses should be high enough
and the duration of drug therapy should be long enough to eradicate even slightlyresistant microorganisms.
Around-the-clock dosing eliminates the peaks and valleys in drug concentration
and helps to maintain a constant therapeutic level to prevent the emergence of
resistant microbes during times of low concentration. The duration of drug use is
critical to ensure that the microbes are completely, not partially, eliminated and arenot given the chance to grow and develop resistant strains.
It was identified that it is difficult to convince people who are taking anti-infective
drugs that the timing of doses and the length of time they continue to take the
drug are important. There is a need to be cautious about the indiscriminate use
of anti-infectives, and insist that antibiotics are not effective in the treatment of
viral infections or illnesses such as the common cold. However, many patients
demand prescriptions for these drugs when they visit practitioners because theyare convinced that they need to take something to feel better.
With many serious illnesses, including pneumonias for which the causative organism
is suspected, antibiotic therapy may be started as soon as a sample of the bacteria,
or culture, is taken and before the results are known. In many cases, it is necessary
to perform sensitivity testing on the cultured microbes to evaluate bacteria and
determine which drugs are most effective. Health care providers also tend to try
newly introduced, more powerful drugs when a more established drug may be just
as effective. Use of a powerful drug in this way leads to the rapid emergence of
resistant strains to that drug, perhaps limiting its potential usefulness when it mightbe truly necessary.
Self-assessment 1.3
1) Differentiate acquired resistance from natural resistance.
2) List 2 factors that can accelerate the occurrence of antibiotic resistance.
3) Around-the-clock dosing exposes people to the occurrence of antibiotic
resistance. TRUE or FALSE
1.4. Classification of antibiotics with focus on antibioticsavailable in healthcare settings in Rwanda
1.4.1 Introduction to antibiotics
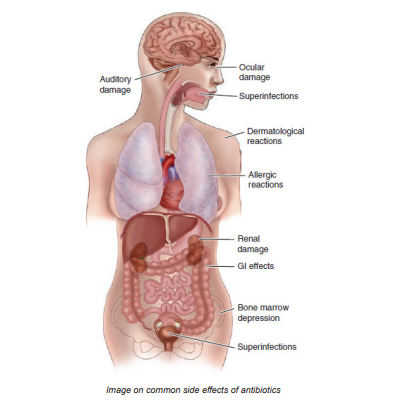
Learning Activity 1.4.1
1) Observe attentively the image below:

a) Write the names of antibiotic drugs observed in the image above.
b) Put the drugs you identified in their respective classes.
c) What are the common side effects of antibiotics?
CONTENT SUMMARY
Bacteria can invade the human body through many routes. The goal of antibiotic
therapy is to decrease the population of invading bacteria to a point at which the
human immune system can effectively deal with the invader. To determine which
antibiotic will effectively interfere with the specific proteins or enzyme systems for
treatment of a specific infection, the causative organism must be identified through
a culture. Sensitivity testing is also done to determine the antibiotic to which that
particular organism is most sensitive (e.g., which antibiotic best kills or controlsthe bacteria). Drugs with broad spectrum activity are often given at the beginning
of treatment until the exact organism and sensitivity can be established. Because
these antibiotics have such a wide range of effects, they are frequently associated
with adverse effects. Human cells have many of the same properties as bacterial
cells and can be affected in much the same way, so damage may occur to the
human cells, as well as to the bacterial cells. There is no perfect antibiotic that iswithout effect on the human host.
Certain antibiotics may be contraindicated in some patients because of known
adverse effects. Some patients for which antibiotics are contraindicated due to
known adverse reactions include: Immunocompromised patients; Patients withsevere GI disease, and Patients who are debilitated.
The antibiotic of choice is one that affects the causative organism and leads to the
fewest adverse effects for the patient involved. In some cases, antibiotics are given
in combination because they are synergistic. Use of synergistic antibiotics also
allows the patient to take a lower dose of each antibiotic to achieve the desired
effect. This helps to reduce the adverse effects that a particular drug may have. In
some situations, antibiotics are used as a means of prophylaxis, or prevention ofpotential infection.
The most common side effects of antibiotics are: Ocular damage, Superinfections
(GI and Genito-urinary tract), Allergic reactions, Bone marrow depression, GIeffects, Dermatological reactions, Auditory damage and Renal damage.
There are some pieces of advice, any patient taking antibiotics should follow:
(1) Do not demand an antibiotic when you come to see your doctor.
(2) Take your antibiotics
as prescribed and use all pills even if you are feeling better. When you stop taking
the pills before you have used them all, there’s a likely chance that all of the bacteria
have not been killed and the remaining bacteria will become stronger and replicate
new bacteria that will be more resistant to the antibiotic next time around.
(3) There should not be leftovers, and if for some reason there are, do not save them to take at another time.
(4) Never share your antibiotics with someone else.
(5) Always take
antibiotics with food to prevent stomach upset, except otherwise indicated.
(6) If the antibiotic is making you feel worse, talk to your doctor about your symptoms. You may need a different antibiotic or something that will help with the side effects.
(7) Diarrhea is a common side effect of antibiotics. As a preventive measure, you cantake an over-the-counter probiotic to help reduce diarrhea symptoms.
Antibiotics are classified into the following classes: Aminoglycosides, carbapenems,
cephalosporins, fluoroquinolones, penicillins (and penicillinase-resistant drugs),
sulfonamides, tetracyclines, disease-specific antimycobacterials (antitubercular and
leprostatic drugs), ketolides (E.g.: telithromycin), lincosamides, lipoglycopeptides(E.g.: televancin), macrolides, and monobactams (E.g.: aztreonam)
Self-assessment 1.4.1
1) What is the advantage of using synergistic drugs?2) Use of synergistic antibiotics allows the patient to increase the dose of each antibiotic to get the desired effect. TRUE or FALSE.
1.4.2. Class of penicillins and penicillinase resistant antibiotics
Learning Activity 1.4.2
1) Read the case study below and answer the questions related to it:
A 40-year-old female patient consults the health post where you are appointed in
the clinical placement. She reports that she had unprotected sex, and developed
a painless sore that disappeared after some period. You suspect that the patient
suffers from syphilis, and you want to prescribe a drug in the class of penicillins.
a) Is it relevant to treat syphilis with drugs in the class of penicillins?
b) Give at least 5 drugs in the class of penicillins
c) Is is advisable to combine penicillins and parenteral aminoglycosides?Explain your answer
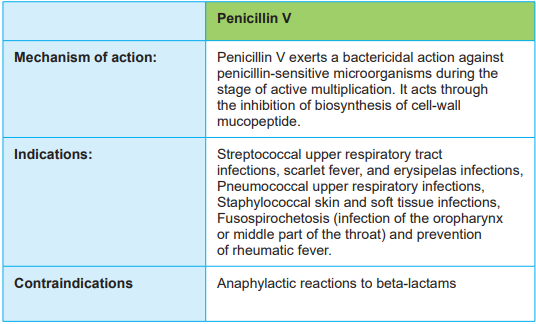
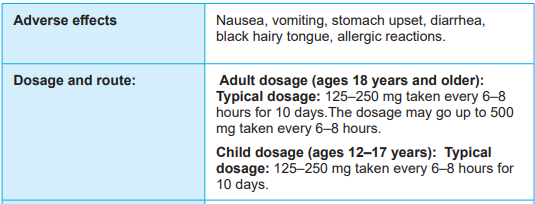
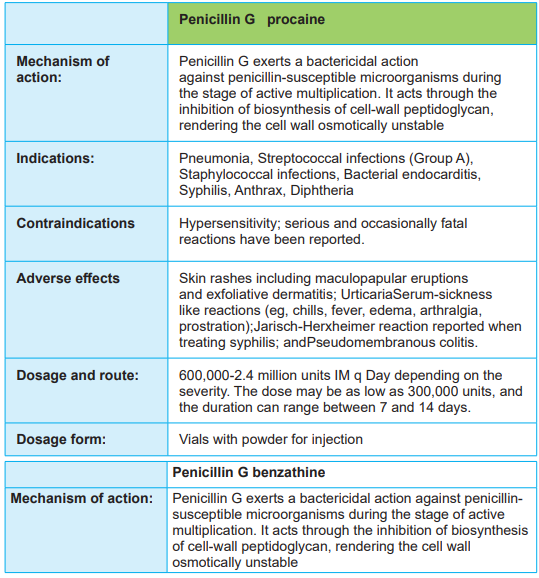
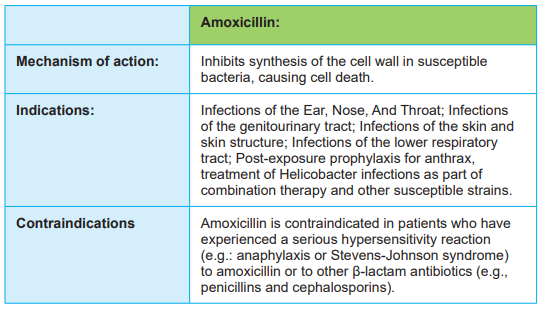
CONTENT SUMMARY
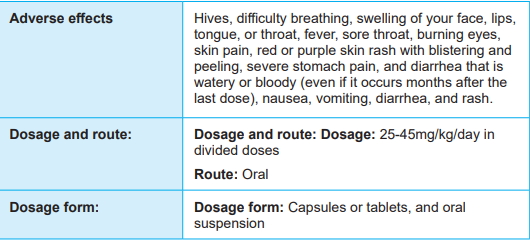
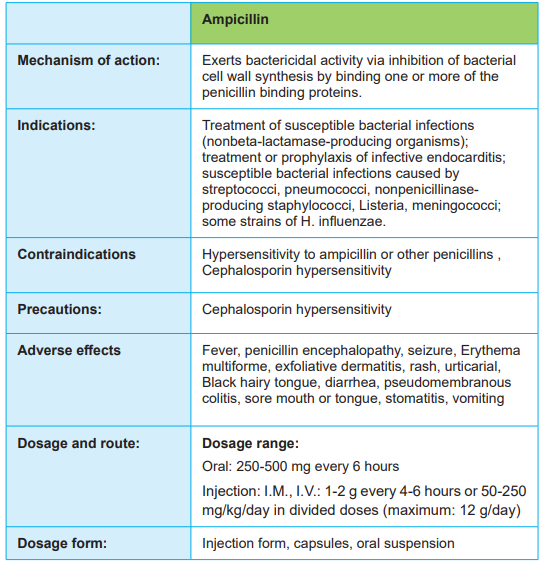
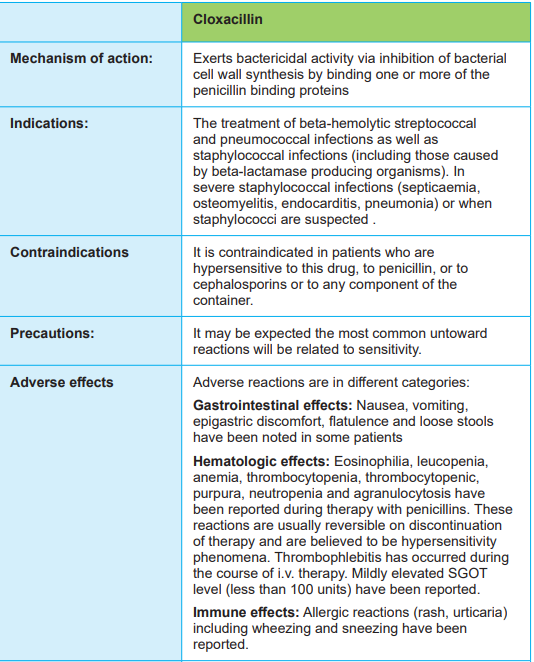
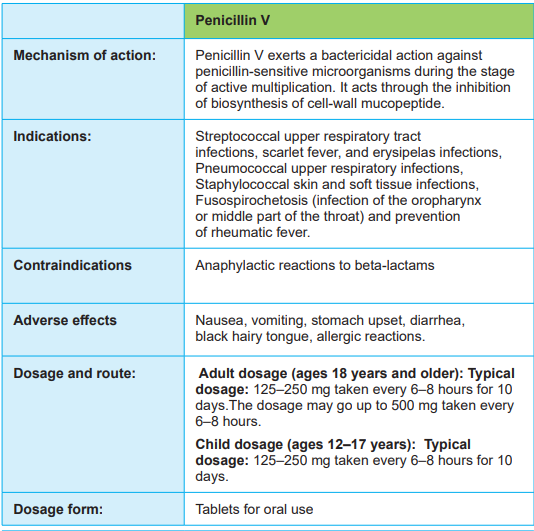
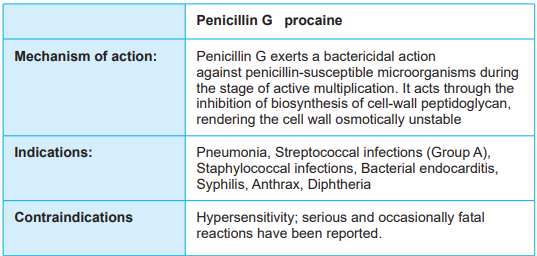
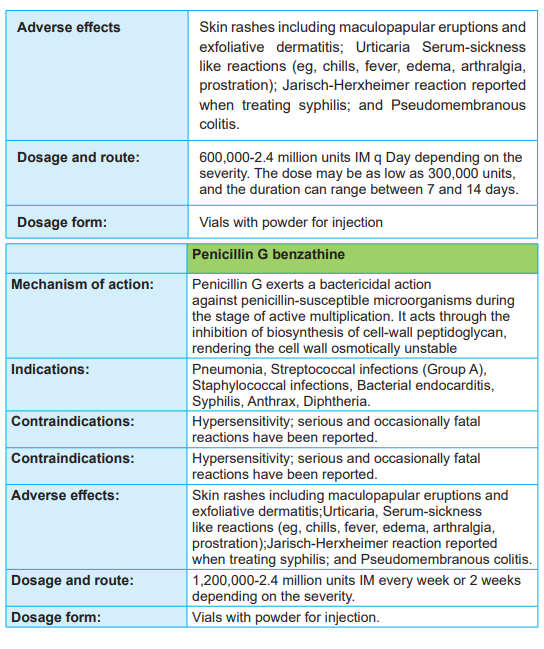
Penicillin was the first antibiotic introduced for clinical use. Penicillins include
penicillin G benzathine, penicillin G potassium, penicillin G procaine, penicillin V,amoxicillin, and ampicillin.
With the prolonged use of penicillin, more and more bacterial species have
synthesized the enzyme penicillinase to counteract the effects of penicillin. A group
of drugs with a resistance to penicillinase was developed, and this allows them toremain effective against bacteria that are now resistant to the penicillins. Penicillin resistant antibiotics include nafcillin and oxacillin.
These antibiotics produce bactericidal effects by interfering with the ability of
susceptible bacteria to build their cell walls when they are dividing. Because human
cells do not use the biochemical process that the bacteria use to form the cell
wall, this effect is a selective toxicity. The penicillins are indicated for the treatment
of streptococcal infections, including pharyngitis, tonsillitis, scarlet fever, and
endocarditis; pneumococcal infections; staphylococcal infections; fusospirochetal
infections; rat-bite fever; diphtheria; anthrax; syphilis; and uncomplicatedgonococcal
infections. At high doses, these drugs are also used to treat meningococcalmeningitis. Most of the penicillins are rapidly absorbed from the GI tract, reaching peak levels in 1 hour.
Should be taken on an empty stomach to ensure adequate absorption.
Penicillins are excreted unchanged in the urine, and enter breast milk which cancause adverse reactions.
Penicillins are contraindicated in patients with allergies to penicillin or cephalosporins
or other allergens. Penicillin sensitivity tests are available if the patient’s history
of allergy is unclear and a penicillin is the drug of choice. Use with caution in
patients with renal disease, in pregnant and lactating patients because diarrhea
and superinfections may occur in the infant. Perform culture and sensitivity before
therapy to select the right drug to the causal agent. With the emergence of manyresistant strains of bacteria, this has become increasingly important.
GI adverse effects are common and include nausea, vomiting, diarrhea,
abdominal pain, glossitis, stomatitis, gastritis, sore of the mouth, and furry tongue.
Superinfections, including yeast may also develop. Pain and inflammation at the
injection site can occur with injectable forms. Hypersensitivity reactions may include
rash, fever, wheezing, and, with repeated exposure, anaphylaxis that can progressto anaphylactic shock and death.
Different drugs may interact with penicillins, and necessary precautions should be
taken. If penicillins and penicillinase-resistant antibiotics are taken concurrently
with tetracyclines, a decrease in the effectiveness of the penicillins results. This
combination should be avoided if at all possible, or the penicillin doses should be
raised, which could increase the occurrence of adverse effects. When the parenteral
forms of penicillins and penicillinase-resistant drugs are administered in combination
with any of the parenteral aminoglycosides, inactivation of the aminoglycosidesoccurs. These combinations should also be avoided whenever possible.
There is a variety of nursing considerations that need to be taken into account
while administering the penicillins: Assess for possible contraindications or
cautions; Perform a physical assessment to establish baseline data for evaluating
the effectiveness of the drug and the occurrence of any adverse effects associated
with drug therapy; Examine skin and mucous membranes for any rashes or lesions
and injection sites for abscess formation to provide a baseline for possible adverse
effects; Perform culture and sensitivity tests at the site of infection to ensure that this
is the drug of choice for this patient; Note respiratory status to provide a baseline
for the occurrence of hypersensitivity reactions; Examine the abdomen to monitorfor adverse effects.
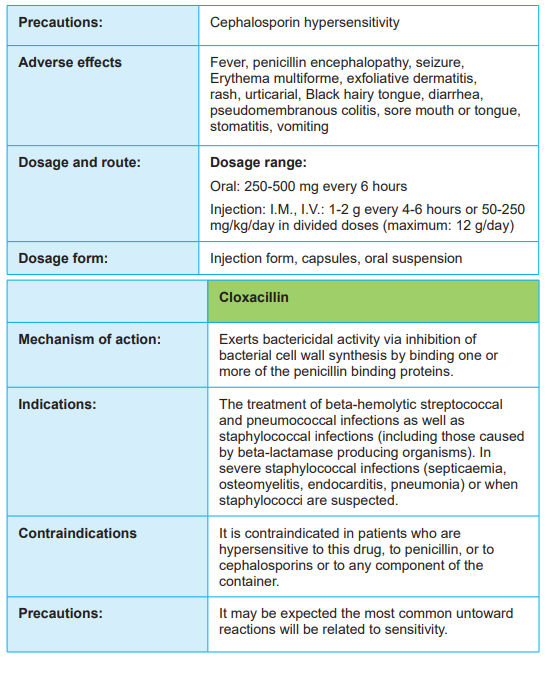
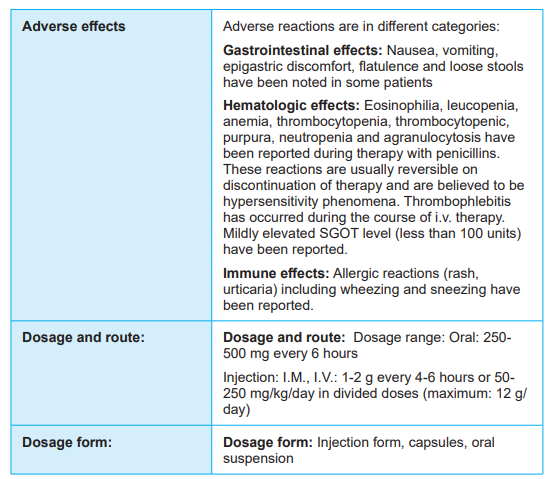
Tables 1.4.2.1: Summary of the prototype penicillins



Self-assessment 1.4.2
1) Which of the following statements describes the mechanism of action of
amoxicillin?
a) Interference with the 50S subunit of bacterial ribosomes
b) Inhibition of bacterial cell wall synthesis
c) Interference with the 30S subunit of bacterial ribosomes
d) Suppression of folate synthesis
2) One of the following penicillin drugs is effective on infections caused by
beta-lactamase producing organisms:
a) Cloxacillin
b) Amoxicillin
c) Ampicillin
d) Penicillin V
3) One of the following penicillin antibiotics can be used in the prophylaxis of
rheumatic fever and syphilis:
a) Amoxicillin
b) Ampicillin
c) Penicillin V
d) Penicillin G benzathine
4) The healthcare professionals need to take necessary caution whenadministering penicillins to people allergic to cephalosporins. TRUE or FALSE
1.4.3 Class of aminoglycosides
Learning Activity 1.4.3
1) Read the case study below and answer the questions related to it:
A 50-year-old male patient consults the health post where you are carrying out
the clinical placement. He has a serious bacterial infectious disease that requires
treatment with an aminoglycoside. You then refer the patient to the nearest district
hospital to receive an aminoglycoside through the parenteral route. Answer the
following questions related to the scenario above:
a) Give at least 3 drugs in the class of aminoglycosides
b) Which mechanism of action do aminoglycosides use to exert their
effects?
Guidance: Read the textbook provided by the teacher, on the topic ofaminoglycosides, and answer the questions above.
CONTENT SUMMARY
Aminoglycosides are powerful antibiotics used to treat serious infections caused
by gram-negative aerobic bacilli. Because most of these drugs have potentially
serious adverse effects, newer, less-toxic drugs have replaced aminoglycosides in
the treatment of less serious infections. They include amikacin (Amikin), gentamicin
(Garamycin), Kanamycin (Kantrex), neomycin (Mycifradin), streptomycin, and
tobramycin (TOBI, Tobrex),promomycin and plazomycin.
The aminoglycosides are bactericidal and inhibit protein synthesis in susceptible
strains of gram-negative bacteria. These antibiotics are used to treat serious
infections caused by Pseudomonas aeruginosa, E. coli, Proteus species, the
Klebsiella, Enterobacter, Serratia group, Citrobacter species, and Staphylococcus
species such as Staphylococcus aureus.
Aminoglycosides are indicated for the treatment of serious infections that are
susceptible to penicillin when penicillin is contraindicated. They can be used in
severe infections before culture and sensitivity tests have been completed. The
aminoglycosides are poorly absorbed from the GI tract but rapidly absorbed after
intramuscular injection, reaching peak levels within 1 hour. They have an average
half-life of 2 to 3 hours. They are widely distributed throughout the body, cross the
placenta and enter breast milk, and are excreted unchanged in the urine.
Aminoglycosides are contraindicated in case of known allergy to any of the
aminoglycosides. They are also contraindicated in renal or hepatic disease that
could be exacerbated by toxic aminoglycoside effects and that could interferewith drug metabolism and excretion, leading to higher toxicity. Preexisting hearing
loss, which could be intensified by toxic drug effects on the auditory nerve is a
contraindication to the use of antibiotics. Ideally, aminoglycosides should beavoided in case of lactation.
Cautions should be taken while using during pregnancy (the benefits of the drugmust be carefully weighed against potential adverse effects on the fetus).
Test urine function frequently when these drugs are used because they depend on
the kidney for excretion and are toxic to the kidney. The potential for nephrotoxicity
and ototoxicity with amikacin is very high with the use of aminoglycosides, and
special caution for kanamycin is to ensure it is not used for longer than 7 to 10 days.
Streptomycin, once a commonly used drug, is reserved for use in special situations
because it is very toxic to the eighth cranial nerve and kidney.
Their main severe side effects may include ototoxicity, nephrotoxicity, and
neuromuscular blockade. The interaction of aminoglycoside antibiotics and
calcium channel blockers is of clinical significance because when these agents
are given concurrently during the perioperative period they may lead to respiratory
depression or prolonged apnoea.
There are some nursing considerations that need to be taken into account while
administering aminoglycosides. Assess for possible contraindications or cautions.
Perform a physical assessment to establish baseline data for assessing the
effectiveness of the drug and the occurrence of any adverse effects associated with
drug therapy. Perform culture and sensitivity tests at the site of infection to ensure
appropriate use of the drug. Conduct auditory testing to evaluate any CNS effectsof the drug, perform renal and hepatic function tests, and assess vital signs.
Tables 1.4.3.1: Summary of the prototype aminoglycosides

Self-assessment 1.4.3
1) Aminoglycosides are primarily used for infections by what type of
pathogen?
a) Gram negative aerobic bacilli
b) Both Gram negative and Gram-positive bacteria
c) Yeast and fungi
d) Gram positive bacteria only
2) Which of the following is an example of an aminoglycoside antibiotic?
a) Azithromycin
b) Erythromycin
c) Streptomycin
d) Clindamycin
3) The associate nurse considers administration of gentamicin. Which of the
following is NOT a side effect of this medication?
a) Diaphoresis
b) Ototoxicity
c) Anorexiad) Nephrotoxicit
1.4.4 Class of cephalosporins
Learning Activity 1.4.4
1) Read the scenario below:
A 18-year-old male patient comes to the health facility with compalins of chronic
wound drainage, pain, and exposed bone. On the observation, the patient is
suspected to have a chronic osteomyelitis, and he is sheduled for surgery.
Postoperatively, the patient is written a third generation cephalosporin for 14
days. Answer the following questions related to the case study above
a) Give at least 2 drugs in the class of third generation cephalosporinsb) Which mechanism of action do cephalosporins use to exert their effects?
CONTENT SUMMARY
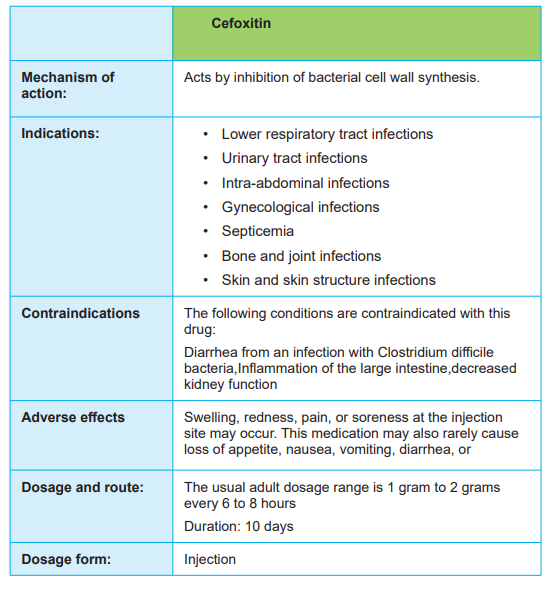
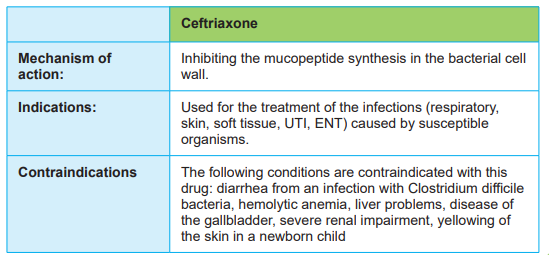
The cephalosporins are drugs similar to the penicillins in structure and in activity. This
means that their mechanism of action is through inhibition of bacterial cell wallpeptidoglycan synthesis.
Over time, different generations of cephalosporins have been introduced, each
group with its own spectrum of activity. In this book, only 3 generations will bediscussed.
First-generation cephalosporins are largely effective against the same gram positive bacteria that are affected by penicillin G, as well as the gram-negative
bacteria P. mirabilis, E. coli, and K. pneumoniae. First-generation drugs include
cefadroxil (generic), cefazolin (Zolicef), and cephalex.
Second-generation cephalosporins are effective against the previously mentioned
strains, as well as H. influenzae, Enterobacter aerogenes, and Neisseria species.
Second-generation drugs are less effective against gram-positive bacteria. These
include cefaclor (Ceclor), cefoxitin (generic), cefprozil (generic), and cefuroxime(Zinacef).
Third-generation cephalosporins, which are effective against all of the previously
mentioned strains, are weak against gram-positive bacteria but are more potent
against the gram-negative bacilli. Third-generation drugs include cefdinir (Omnicef),
cefotaxime (Claforan), cefpodoxime (Vantin), ceftazidime (Ceptaz, Tazicef),ceftibuten (Cedax), ceftizoxime (Cefi zox), and ceftriaxone (Rocephin).
The cephalosporins are both bactericidal and bacteriostatic, depending on the dose
used and the specific drug involved. In susceptible species, these agents basically
interfere with the cell wall–building ability of bacteria when they divide; that is, theyprevent the bacteria from biosynthesizing the framework of their cell walls.
Avoid the use of cephalosporins in patients with known allergies to cephalosporins
or penicillins because cross-sensitivity is common. Use with caution in patients with
hepatic or renal impairment because these drugs are toxic to the kidneys and could
interfere with the metabolism and excretion of the drug. In addition, use with caution
in pregnant or lactating patients because potential effects on the fetus and infant
are not known; use only if the benefits clearly outweigh the potential risk of toxicityto the fetus or infant.
The most common adverse effects of the cephalosporins involve the GI tract and
include nausea, vomiting, diarrhea, anorexia, abdominal pain, and flatulence. CNS
symptoms include headache, dizziness, lethargy, and paresthesias. Nephrotoxicity
is also associated with the use of cephalosporins, most particularly in patients whohave a predisposing renal insufficiency
Patients who receive oral anticoagulants in addition to cephalosporins may
experience increased bleeding. Instruct the patient receiving cephalosporins
to avoid alcohol for up to 72 hours after discontinuation of the drug to prevent a
disulfiram-like reaction, which results in unpleasant symptoms such as flushing,
throbbing headache, nausea and vomiting, chest pain, palpitations, dyspnea,
syncope, vertigo, blurred vision, and, in extreme reactions, cardiovascular collapse,
convulsions, or even death. Concurrent administration of cephalosporins with
aminoglycosides increases the risk for nephrotoxicity. Frequently monitor patients
receiving this combination, and evaluate serum blood urea nitrogen (BUN) and
creatinine levels.
There is a variety of nursing considerations that need to be taken into account:
Assess for possible contraindications or cautions. Monitor the patient for any signs
of superinfection to arrange for treatment if superinfection occurs. Instruct the patient
about the appropriate dosage schedule and about possible side effects to enhance
patient knowledge about drug therapy and to promote compliance. Take safety
precautions, including changing position slowly and avoiding driving and hazardous
tasks, if CNS effects occur. Try to drink a lot of fluids and to maintain nutrition (very
important) even though nausea, vomiting, and diarrhea may occur. Report difficulty
breathing, severe headache, severe diarrhea, dizziness, or weakness. Avoid
consuming alcoholic beverages while receiving cephalosporins and for at least 72hours after completing the drug course because serious side effects could occur.
Tables.1.4.4.1 Summary the prototype cephalosporins
CEPHALOSPORINS OF FIRST GENERATION:


CEPHALOSPORINS OF SECOND GENERATION

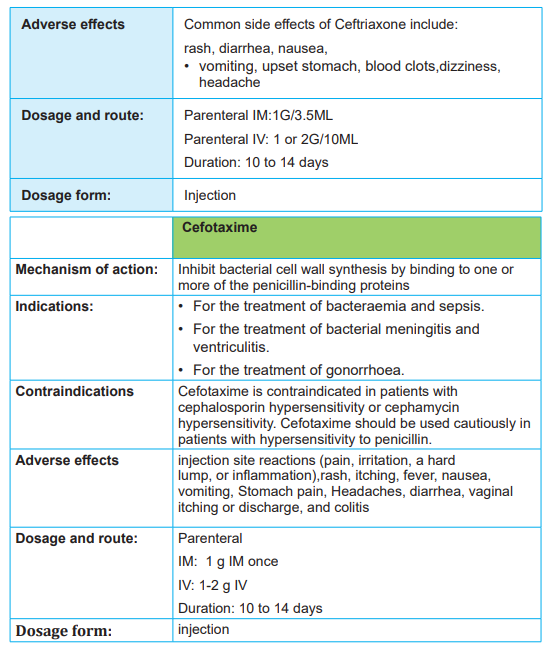
Self-assessment 1.4.4
1) Which of the following antibiotics belongs to the class of cephalosporins?
a) Amoxicillin
b) Gentamicin
c) Cefotaxime
d) Bactrim
2) Which of the following IS NOT a caution for the use of cephalosporins?
a) Allergy to penicillin
b) Allergy to aspirin
c) Renal failured) Concurrent treatment with aminoglycosides
1.4.5. Class of fluoroquinolones
Learning Activity 1.4.5
1) Read the scenario below:
A 30-year-old female patient consults the health post where you allocated
during the clinical practice, complaining of recurrent urinary tract infections on a
pregnancy of 3 months. The patient reports that he was treated with amoxicillin
without success. You then decide to prescribe a fluoroquinolone antibiotic,
bearing in mind its effectiveness in urinary tract infections.
a) List at least 4 fluoroquinolone drugs
b) Bearing in mind that this patient is pregnant, is it advisable to prescribe
fluoroquinolones?
Guidance: Read the textbook provided by the teacher, on the topic offluoroquinolones, and answer the questions above
CONTENT SUMMARY
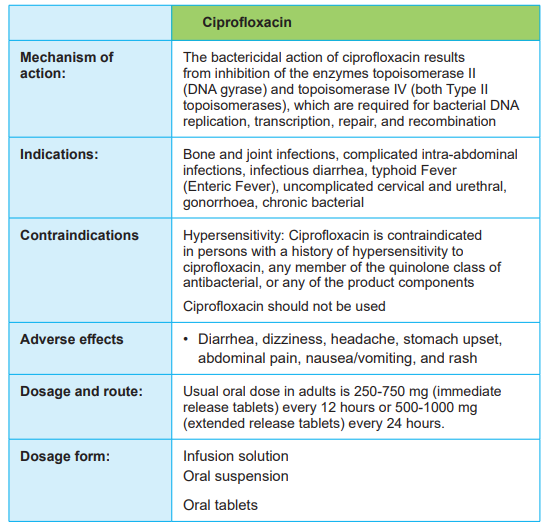
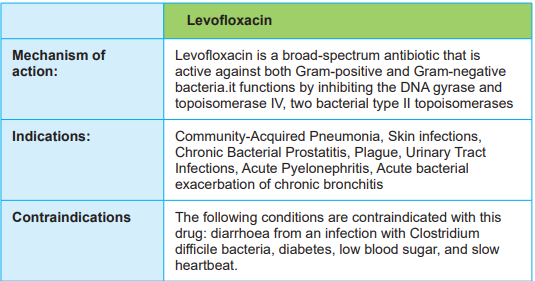
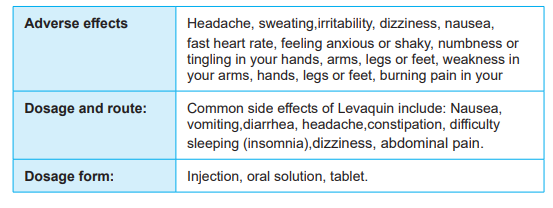
The fluoroquinolones are a relatively new synthetic class of antibiotics with a broad
spectrum of activity. Fluoroquinolones include ciprofloxacin (Cipro), which is the
most widely used fluoroquinolone; gemifloxacin (Factive), levofloxacin (Levaquin),moxifloxacin (Avelox), norfloxacin (Noroxin), and ofloxacin.
The fluoroquinolones enter the bacterial cell by passive diffusion through channels
in the cell membrane. Once inside, they interfere with the action of DNA enzymes
necessary for the growth and reproduction of the bacteria. This leads to cell death
because the bacterial DNA is damaged and the cell cannot be maintained. However,
misuse of these drugs in the short time the class has been available has led to theexistence of resistant strains of bacteria.
The fluoroquinolones are indicated for treating infections caused by susceptible
strains of gram-negative bacteria, S. aureus, Staphylococcus epidermidis, some
Neisseria gonorrhoeae, and group D streptococci. These infections frequently
include urinary tract, respiratory tract, and skin infections. Ciprofloxacin is effectiveagainst a wide spectrum of gram-negative bacteria.
Fluoroquinolones are contraindicated in patients with known allergy to any
fluoroquinolone and in pregnant or lactating patients because potential effects
on the fetus and infant are not known. Use with caution in the presence of renal
dysfunction, which could interfere with the metabolism and excretion of the drug,
and seizures, which could be exacerbated by the drugs’ effects on cell membrane
channels. The use of antacids has been recognized to impair the action offluoroquinolones, therefore, such concomitant use is not recommended.
These drugs are generally associated with relatively mild adverse reactions.
The most common are headache, dizziness, insomnia, and depression related
to possible effects on the CNS membranes. GI effects include nausea, vomiting,
diarrhea, and dry mouth, related to direct drug effect on the GI tract and possibly tostimulation of the chemoreceptor trigger zone in the CNS.
There are nursing considerations that the nurses ought to bear in mind: Assess for
possible contraindications or cautions. Perform physical assessment to establish
baseline data for assessing the effectiveness of the drug and the occurrence of
any adverse effects associated with drug therapy. Examine the skin for any rash
or lesions to provide a baseline for possible adverse effects. Perform culture and
sensitivity tests at the site of infection to ensure appropriate use of the drug. Perform
renal function tests, including blood urea nitrogen and creatinine clearance, to
evaluate the status of renal functioning and to assess necessary changes in dose.
Conduct assessment of orientation, affect, and reflexes to establish a baseline forany central nervous system (CNS) effects of the drug.
Table 1.4.5.1: Summary of the prototype fluoroquinolones
Self-assessment 1.4.5
1) Read the scenario below:
A 32-year-old female patient consults the health post where you are appointed,
complaining of recurrent urinary tract infections. The patient reports that he
was treated with amoxicillin without success. You then decide to prescribe a
fluoroquinolone antibiotic, bearing in mind its effectiveness in urinary tract
infections.
a) What are the nursing considerations you would consider beforeprescribing a fluoroquinolone to any patient?
1.4.6. Class of macrolides
Learning Activity 1.4.6
1) Read the scenario below:
You receive a 60-year-old male patient who consults the health post where you
work with complaints of respiratory tract infection. The patient reports that he
took amoxicillin in the past, and developed an allergic reaction. He was then
warned not to take any penicillin drug again in the past, because of allergy to
penicillins. You then decide to prescribe a macrolide antibiotic, as it may replace
a penicillin in such infections.
a) List at least 2 antibiotics that belong to the class of macrolidesb) What is the mechanism of action of a macrolide?
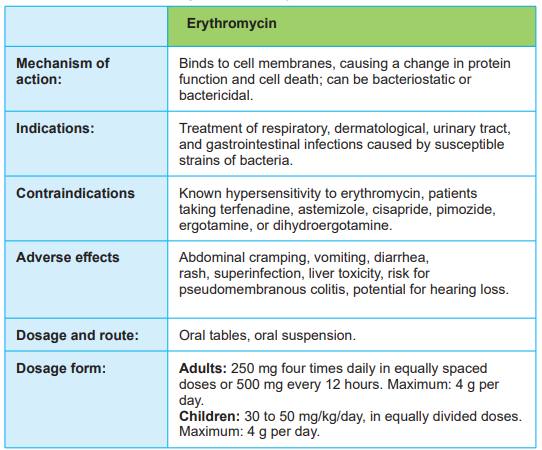
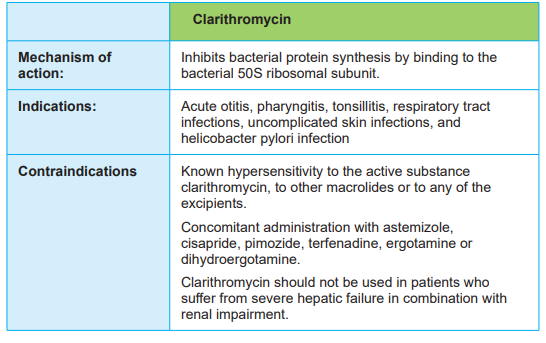
CONTENT SUMMARY
The macrolides are antibiotics that interfere with protein synthesis in susceptible
bacteria. Macrolides include erythromycin, azithromycin, clarithromycin, anddirithromycin.
The macrolides may be bactericidal or bacteriostatic, exerting their effect by binding
to the bacterial cell membrane and changing protein function. This action can
prevent the cell from dividing or cause cell death, depending on the sensitivity ofthe bacteria and the concentration of the drug.
Macrolides are indicated for treatment of the following conditions: acute infections
caused by susceptible strains of S. pneumoniae, M. pneumoniae, Listeria
monocytogenes, and Legionella pneumophila; infections caused by group A beta hemolytic streptococci; pelvic inflammatory disease caused by N. gonorrhoeae;
upper respiratory tract infections caused by H. influenzae (with sulfonamides);
infections caused by Corynebacterium diphtheriae and Corynebacterium
minutissimum (with antitoxin); intestinal amebiasis; and infections caused by C.trachomatis.
In addition, macrolides may be used as prophylaxis for endocarditis before dental
procedures in high-risk patients with valvular heart disease who are allergic to
penicillin. Topical macrolides are indicated for the treatment of ocular infections
caused by susceptible organisms and for acne vulgaris, and they may also be used
prophylactically against infection in minor skin abrasions and for the treatment ofskin infections caused by sensitive organisms.
The macrolides are widely distributed throughout the body; they cross the placentaand enter the breast milk. These drugs are absorbed in the GI tract.
Erythromycin is metabolized in the liver, with excretion mainly in the bile to feces.The half-life of erythromycin is 1.6 hours.
Azithromycin and clarithromycin are mainly excreted unchanged in the urine,
making it necessary to monitor renal function when patients are taking these drugs.
The half-life of azithromycin is 68 hours, making it useful for patients who have
trouble remembering to take pills because it can be given once a day. The half life of clarithromycin is 3 to 7 hours. Dirithromycin is converted from the prodrug
dirithromycin to erythromycylamine in the intestinal wall. Most of the drug is excreted
through the feces. It has a half-life of 2 to 36 hours. It also has the advantage ofonce-a-day dosing, which increases compliance in many cases.
Macrolides are contraindicated in patients with a known allergy to any macrolide
because cross-sensitivity occurs. Use with caution in patients with hepatic
dysfunction, which could alter the metabolism of the drug, and in those with renal
disease, which could interfere with the excretion of some of the drug.
Also use with caution in lactating women because macrolides secreted in breast milk can
cause diarrhea and superinfections in the infant and in pregnant women because
of potential adverse effects on the developing fetus; use only if the benefit clearlyoutweighs the risk to the fetus.
Relatively few adverse effects are associated with the macrolides. The most
frequent ones, which involve the direct effects of the drug on the GI tract, are
often uncomfortable enough to limit the use of the drug. These include abdominal
cramping, anorexia, diarrhea, vomiting, and pseudomembranous colitis. Other
effects include neurological symptoms such as confusion, abnormal thinking,
and uncontrollable emotions, which could be related to drug effects on the CNS
membranes; hypersensitivity reactions ranging from rash to anaphylaxis; andsuperinfections related to the loss of normal flora.
During macrolide administration, there are nursing considerations that nurses need
to consider: GI upset is common and patients can be advised to take medication
with food. Patients should also be advised to avoid excessive sunlight and to
wear protective clothing and use sunscreen when outside, as well as to report any
adverse reactions immediately. Advise patients to report symptoms of chest pain,
palpitations, or yellowing of eyes or skin. Additionally, patients should be advisedthat these medications can cause drowsiness.
Assess for possible contraindications or precautions to macrolides. Perform a
physical assessment to establish baseline data for assessing the effectiveness of
the drug and the occurrence of any adverse effects associated with drug therapy.
Examine the skin for any rash or lesions to provide a baseline for possible adverse
effects. Obtain specimens for culture and sensitivity testing from the site of infection
to ensure appropriate use of the drug. Monitor temperature to detect infection.
Conduct assessment of orientation, affect, and reflexes to establish a baseline for
any CNS effects of the drug. Assess liver and renal function test values to determine
the status of renal and liver functioning and to determine any needed alteration indosage
Tables 1.4.6.1 Summarizing of the prototype macrolides
Self-assessment 1.4.6
1) Which of the following antibiotic would be given to a patient with gastritis
associated with Helicobacter pylori?
a) Erythromycin
b) Clarithromycin
c) Gentamicin
d) Doxycycline
1) All of the following antibiotics are macrolides, EXCEPT:
a) Erythromycin
b) Clarithromycin
c) Azithromycind) Streptomycin
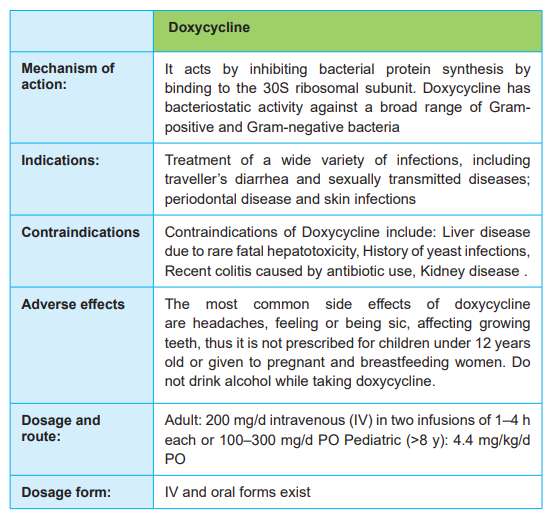
1.4.7. Class of tetracyclines
Learning Activity 1.4.7
1) Read the scenario below:
You receive a 45-year-old female patient who consults the health post
where you are doing your clinical placement, with complaints of urinary
tract infection. This infection can be treated by a tetracycline antibiotic that
is effective against some bacteria that cause urinary tract infection. As a
student nurse, you wish to prescribe a tetracycline antibiotic that will help
to clear the infection.
a) List at least 2 antibiotics that belong to the class of tetracyclinesb) What is the mechanism of action of tetracyclines?
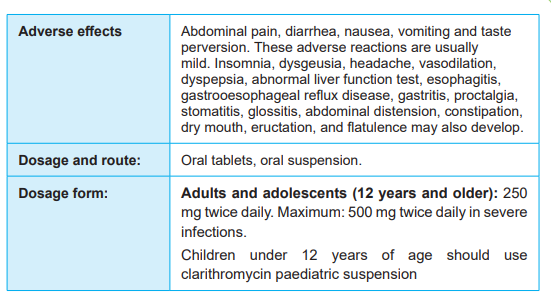
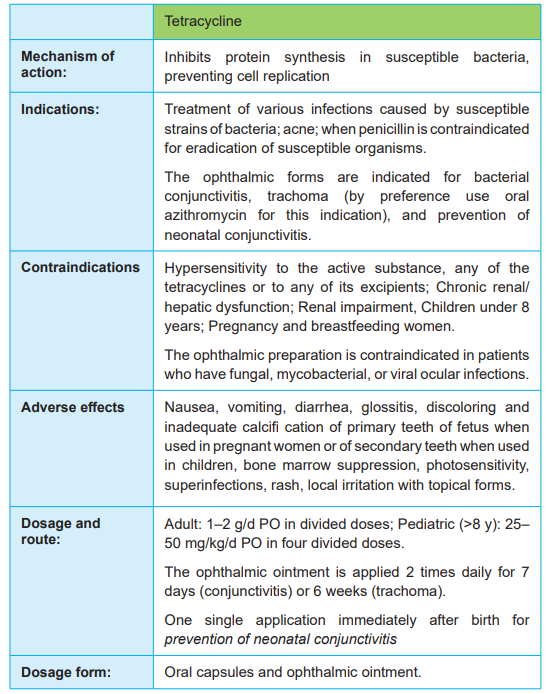
CONTENT SUMMARY
The class of tetracyclines has been developed as semisynthetic antibiotics basing
on the structure of a common soil mold. They are composed of four rings, which
defines how they got their name. Researchers have developed newer tetracyclines
to increase absorption and tissue penetration. Their use has been limited in
recent years due to their noted widespread resistance. Existing Tetracyclines
include tetracycline (Sumycin), demeclocycline (Declomycin), doxycycline (Doryx,Periostat), and minocycline (Minocin).
The tetracyclines work by inhibiting protein synthesis in a wide range of bacteria,
leading to the inability of the bacteria to multiply. Because the affected protein is
similar to a protein found in human cells, these drugs can be toxic to humans athigh concentrations.
Tetracyclines are indicated for treatment of infections caused by susceptible agents;
when penicillin is contraindicated in susceptible infections; and for treatment of
acne and uncomplicated GU infections caused by C. trachomatis. Some of the
tetracyclines are also used as adjuncts in the treatment of certain protozoalinfections such as malaria.
Tetracyclines are absorbed adequately, but not completely, from the GI tract. Their
absorption is affected by food, iron, calcium, and other drugs in the stomach.
Tetracyclines are concentrated in the liver and excreted unchanged in the urine,
with half-lives ranging from 12 to 25 hours. These drugs cross the placenta and
pass into breast milk. Tetracycline is available in oral and topical forms, in addition
to being available as an ophthalmic agent. Demeclocycline is available in oral form.Doxycycline and minocycline are available in IV and oral forms.
Tetracyclines are contraindicated in patients with known allergy to tetracyclines or
to tartrazine (e.g., in specifi c oral preparations that contain tartrazine) and duringpregnancy and lactation because of effects on developing bones and teeth.
The ophthalmic preparation is contraindicated in patients who have fungal,
mycobacterial, or viral ocular infections because the drug kills not only the
undesired bacteria but also bacteria of the normal flora, which increases the risk
for exacerbation of the ocular infection that is being treated. Tetracyclines should
be used with caution in children younger than 8 years of age because they can
potentially damage developing bones and teeth and in patients with hepatic or renaldysfunction because they are concentrated in the bile and excreted in the urine.
The major adverse effects of tetracycline therapy involve direct irritation of the
GI tract and include nausea vomiting, diarrhea, abdominal pain, glossitis, and
dysphagia. Fatal hepatotoxicity related to the drug’s irritating effect on the liverhas also been reported. Skeletal effects involve damage to the teeth and bones.
Because tetracyclines have an affinity for teeth and bones, they accumulate there,
weakening the structure and causing staining and pitting of teeth and bones.
Dermatological effects include photosensitivity and rash. Superinfections, including
yeast infections, occur when bacteria of the normal flora are destroyed. Local effects,
such as pain and stinging with topical or ocular application, are fairly common.
Hematological effects are less frequent, such as hemolytic anemia and bone
marrow depression secondary to the effects on bone marrow cells that turn over
rapidly. Hypersensitivity reactions reportedly range from urticaria to anaphylaxisand also include intracranial hypertension
When penicillin G and tetracyclines are taken concurrently, the effectiveness of
penicillin G decreases. If this combination is used, the dose of the penicillin should be
increased. When oral contraceptives are taken with tetracyclines, the effectiveness
of the contraceptives decreases, and patients who take oral contraceptives shouldbe advised to use an additional form of birth control while receiving the tetracycline.
Because oral tetracyclines are not absorbed effectively if taken with food or dairy
products, they should be administered on an empty stomach 1 hour before or 2 to3 hours after any meal or other medication.
The following nursing considerations should be taken into account as the
nurses are providing care to patients receiving tetracyclines: Assess for possible
contraindications or cautions. Perform a physical examination to establish baseline
data for assessing the effectiveness of the drug and the occurrence of any adverse
effects associated with drug therapy. Examine the skin for any rash or lesions to
provide a baseline for possible adverse effects. Perform culture and sensitivity tests
at the site of infection to ensure that this is the appropriate drug for this patient.
Note respiratory status to provide a baseline for the occurrence of hypersensitivity
reactions. Evaluate renal and liver function test reports, including blood urea nitrogen
and creatinine clearance, to assess the status of renal and liver functioning, whichhelps to determine any needed changes in dose.
Tables 1.4.7.1 summarizing the prototype tetracyclines
Self-assessment 1.4.
1) Which of the following antibiotics belongs to the class of tetracyclines?
a) Doxycycline
b) Erythromycin
c) Amoxicillin
d) Azithromycin2) Why are tetracyclines contraindicated in children aged less than 8 years?
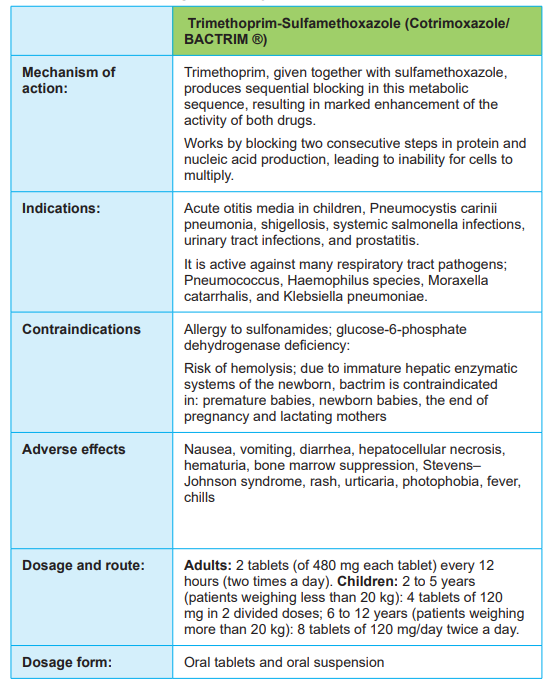
1.4.8. Class of sulphonamides (sulfonamides)
Learning Activity 1.4.8
1) Read the scenario below:
You receive a 52-year-old male patient who consults the health post where you
are assigned in the clinical placement, with history of HIV infection. The patient
says that he takes an antibiotic drug in addition to the antiretroviral drugs. He
specifies that he was told that the antibiotic intends is to prevent the pneumonia
caused by pneumocystis carinii. As a student nurse, you anticipate that the
antibiotic may belong to the class of sulfonamides.
a) List at least 2 antibiotics that belong to the class of sulfonamidesb) What is the mechanism of action of sulfonamides?
CONTENT SUMMARY
The sulfonamides, or sulfa drugs, are drugs that inhibit folic acid synthesis.Sulfonamides include sulfadiazine, sulfasalazine, and cotrimoxazole (Bactrim).
Folic acid is necessary for the synthesis of purines and pyrimidines, which are
precursors of RNA and DNA. For cells to grow and reproduce, they require folic acid.
Humans cannot synthesize folic acid and depend on the folate in their diet to obtain
this essential substance. Bacteria are impermeable to folic acid and must synthesize
it inside the cell. The sulfonamides competitively block paraaminobenzoic acid to
prevent the synthesis of folic acid in susceptible bacteria that synthesize their own
folates for the production of RNA and DNA. This includes gram-negative and gram positive bacteria such as Chlamydia trachomatis and Nocardia and some strains ofH. influenzae, E. coli, and P. mirabilis.
Because of the emergence of resistant bacterial strains and the development of newer antibiotics, the sulfa drugs are no longer used much.
However, they remain an inexpensive and effective treatment for UTIs and trachoma,
especially in developing countries and when cost is an issue. These drugs are
used to treat trachoma (a leading cause of blindness), nocardiosis (which causes
pneumonias, as well as brain abscesses and inflammation), UTIs, and sexually
transmitted diseases. Sulfasalazine is used in the treatment of ulcerative colitis andrheumatoid arthritis.
The sulfonamides are teratogenic; they are distributed into breast milk. These
drugs, given orally, are absorbed from the GI tract, metabolized in the liver, and
excreted in the urine. The time to peak level and the half-life of the individual drug
vary. Sulfadiazine is an oral agent slowly absorbed from the GI tract, reaching
peak levels in 3 to 6 hours. Sulfasalazine is a sulfapyridine that is carried by
aminosalicylic acids (aspirin), which release the aminosalicylic acid in the colon
where is provides direct antiinflammatory effects. In a delayed-release form, this
sulfa drug is also used to treat rheumatoid arthritis that does not respond to other
treatments. It is rapidly absorbed from the GI tract, reaching peak levels in 2 to 6
hours. After being metabolized in the liver, it is excreted in the urine with a half-life of
5 to 10 hours. Cotrimoxazole is a combination drug that contains sulfamethoxazole
and trimethoprim, another antibacterial drug. It is rapidly absorbed from the GI tract,
reaching peak levels in 2 hours. After being metabolized in the liver, it is excreted inthe urine with a half-life of 7 to 12 hours.
The sulfonamides are contraindicated with any known allergy to any sulfonamide,
to sulfonylureas, or to thiazide diuretics because cross-sensitivities occur; during
pregnancy because the drugs can cause birth defects, as well as kernicterus; and
during lactation because of a risk of kernicterus, diarrhea, and rash in the infant.
They should be used with caution in patients with renal disease or a history ofkidney stones because of the possibility of increased toxic effects of the drugs.
Adverse effects associated with sulfonamides include GI effects such as nausea,
vomiting, diarrhea, abdominal pain, anorexia, stomatitis, and hepatic injury, which
are all related to direct irritation of the GI tract and the death of normal bacteria.
Renal effects are related to the filtration of the drug in the glomerulus and include
crystalluria, hematuria, and proteinuria, which can progress to a nephrotic
syndrome and possible toxic nephrosis. CNS effects include headache, dizziness,
vertigo, ataxia, convulsions, and depression (possibly related to drug effects on
the nerves). Bone marrow depression may occur and is related to drug effects on
the cells that turn over rapidly in the bone marrow. Dermatological effects include
photosensitivity and rash related to direct effects on the dermal cells. A wide rangeof hypersensitivity reactions may also occur.
Nursing considerations: Assess for possible contraindications or cautions.
Perform a physical assessment to establish baseline data for assessing the
effectiveness of the drug and the occurrence of any adverse effects associated
with drug therapy. Examine skin and mucous membranes for any rash or lesions to
provide a baseline for possible adverse effects. Obtain specimens for culture and
sensitivity tests at the site of infection to ensure that this is the appropriate drug
for this patient. Note respiratory status to provide a baseline for the occurrence of
hypersensitivity reactions. Conduct assessment of orientation, affect, and reflexes
to monitor for adverse drug effects and examination of the abdomen to monitor
for adverse effects. Monitor renal function test findings, including blood urea
nitrogen and creatinine clearance, to evaluate the status of renal functioning and to
determine any needed alteration in dosage. Also perform a complete blood count(CBC) to establish a baseline to monitor for adverse effects.
Table1.4.8.1 Summarizing the prototype sulfonamide
Self-assessment 1.4.8
1) Which of the following antibiotics belongs to the class of sulphonamides?
a) Tetracycline
b) Ciprofloxacin
c) Streptomycin
d) Cotrimoxazole2) It is advisable to administer sulphonamides to pregnant women when indicated because they are safe during pregnancy. TRUE or FALSE
1.5. Medications used in treatment of bacterial sexually
transmitted diseases and tuberculosis
1.5.1. Medications used in treatment of bacterial sexually transmitted
diseases
Learning Activity 1.5.1
Read carefully the scenario below and answer the questions related to it:
1) A 35-year-old-female patient finds you in the consultation room at the
health post where you are placed in the clinical practice. She complains
of lower abdominal pain and unusual whitish vaginal discharge that
occurred two weeks after unprotected sexual intercourse. The patient
is not pregnant and the physical assessment revealed that the patient
has a tenderness of lower abdomen and the features of the urinary tract
infection (UTI) have been excluded.
a) In which category of syndromic management of STIs would you classify
the symptoms of the client in the above scenario?
b) Name the antibiotics that can be used in the syndromic management ofthis client?
CONTENT SUMMARY
Sexually transmitted infections are infections caused by bacteria, viruses and
parasites that are transferred mainly via sexual contact, be it vaginal, anal, and
oral or in some instances via non-sexual means, i.e. by means of blood or blood
products. Mother-to-child transmission of for example chlamydia, gonorrhea, and
syphilis occurs during pregnancy and childbirth. The most common causal agents
are Chlamydia, Neisseria gonorrhoeae, treponema pallidum and trichomonasvaginalis.
Treatment of STIs relies on the syndromic approaches by taking note of observable
clinical signs and symptoms patients complain of, and by making use of clinical
algorithms or flow charts. Examples of observed syndromes include genital ulcers,abdominal pain, vaginal discharge and urethral discharge.
Vaginal discharge syndrome (VDS)
Vaginal discharge can be due to trichomoniasis, vaginosis (bacterial) and candidiasisbut may also arise from N. gonorrhoeae and Chlamydia trachomatis infections.
Lower abdominal pain (LAP)
Pain in the lower abdominal region may be the result of pelvic inflammatory diseasecaused by N. gonorrhoeae and C. trachomatis infections.
Genital ulcer syndrome (GUS)
The presence of genital ulcers may be due to H. simplex, T. pallidum and H. ducreyi or a combination of these pathogens.
Male urethritis syndrome (MUS) and scrotal swelling (SSW)
N. gonorrhoeae or C. trachomatis or a combination of both may cause urethral discharge and scrotal swelling.
Table 1.5.1.1: COMMON SEXUAL TRANSMITTED DISEASES AND THEIR TREATMENT:
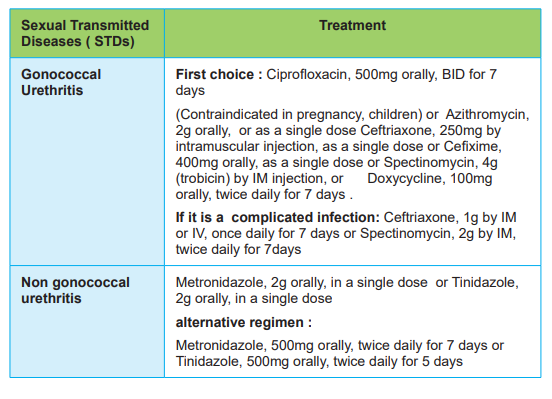

NOTICE: All the time, the treatment guidelines and protocols are established byRwanda Biomedical Canter and changed periodically
Self-assessment 1.5.1
Read carefully the scenario below and answer the questions related to it:
1) Your colleague calls you for advice. He tells you that he receives a client
in the consultation room presenting non painful ulcer on the opening of
his penis, post unprotected sexual intercourse in the last 2 months. The
physical examination reveals that the patient has no inguinal bubo. He
also adds that it is the first time he meets with such case and he asks you
the following questions:
a) What is the diagnosis for this client based on the syndromic management
of STIs?
b) What antibiotic that can be used in this case based on the syndromicmanagement of STIs?
1.5.2. Medications used in treatment of tuberculosisLearning Activity 1.5.2
Read the case study below:
A 45-year-old female patient, weighing 65 kilos, is admitted to the health facility
with cough, nocturnal hyperthermia, anorexia, asthenia, weight loss, and night
sweating. She reports that these signs and symptoms have been there for thelast 4 weeks.
She also reports having taken the full course of treatment with amoxicillin for 7
days that didn’t help. The healthcare provider took a decision to take the sputum
smear which became positive for Mycobacterium tuberculosis. The client is
informed that she contracted pulmonary tuberculosis, and she is counselled that
she will need to take all the antituberculosis drugs as prescribed. It is the first
time for the patient to suffer from tuberculosis, and there is a need to immediatelyinstitute antituberculosis treatment.
a) What are the names of antituberculosis drugs that must be used in the
treatment of this patient?b) What are the treatment phases of tuberculosis?
CONTENT SUMMARY
Tuberculosis treatment refers to the medical treatment of tuberculosis (TB) which
is an infectious disease that usually affects the lungs, but can affect other parts of
the body. The standard “short” course treatment for TB is isoniazid, rifampicin (also
known as rifampin in the United States), pyrazinamide, and ethambutol for two
months, then isoniazid and rifampicin alone for a further four-month period. The
patient is considered cured at six months (although there are still some cases of
relapse rate of about 2 to 3%). For latent tuberculosis, the standard treatment is six
to nine months of isoniazid alone. If the organism is known to be fully sensitive, then
treatment is with isoniazid, rifampicin, and pyrazinamide for two months, followed by
isoniazid and rifampicin for four months. Ethambutol needs not be used. However,
ethambutol is always part of the initial treatment of tuberculosis in Rwanda. Using
the drugs in combination helps to decrease the emergence of resistant strains andto affect the bacteria at various phases during their long and slow life cycle.
First line anti-tuberculous drug names have a standard three-letter and a single letter abbreviation: Ethambutol is EMB or E; Isoniazid is INH or H; Pyrazinamide is
PZA or Z and Rifampicin is RMP or R. Drug regimens are similarly abbreviated in
a standardized manner. The drugs are listed using their single letter abbreviations
(in the order given above, which is roughly the order of introduction into clinical
practice).
A prefix denotes the number of months the treatment should be given for; a subscript
denotes intermittent dosing (so 3 means three times a week) and no subscriptmeans daily dosing.
Most regimens have an initial high-intensity phase, followed by a continuation
phase (also called a consolidation phase or eradication phase): the high-intensity
phase is given first, then the continuation phase, the two phases divided by a slash.
So, 2HREZ/4HR3 means isoniazid, rifampicin, ethambutol, pyrazinamide daily for
two months, followed by four months of isoniazid and rifampicin given three timesa week.
There are six classes of second-line drugs (SLDs) used for the treatment of TB. A
drug may be classed as second-line instead of first-line for one of three possible
reasons: it may be less effective than the first-line drugs (e.g.: p-aminosalicylic acid);
or, it may have toxic side-effects (e.g.: cycloserine); or it may be unavailable in many
developing countries (e.g., fluoroquinolones): Aminoglycosides: e.g., amikacin
(AMK), kanamycin (KM); Polypeptides: e.g., capreomycin, viomycin, enviomycin;
Fluoroquinolones: e.g., ciprofloxacin (CIP), levofloxacin, moxifloxacin (MXF);
Thioamides: e.g. ethionamide, prothionamide; Cycloserine (the only antibiotic in itsclass); and P-aminosalicylic acid (PAS or P).
In Rwanda, the following are the therapeutic diagrams of tuberculosis treatment:
Primotreatment: 2HREZ7/4HR7 (for a person who suffers from pulmonarytuberculosis for the first time).
Retreatment: 2S7RHZE7/1RHZE7/5RHE7: A person who received TB treatment
for some time in the past, and has a positive sputum smear or needs to take/resume
antituberculosis drugs again. In this case, injectable streptomycin is added to thetherapeutic diagram (protocol) for the first 2 months, administered intramuscularly.
Self-assessment 1.5.2
1) After 5 months of tuberculosis treatment in the learning activity 1.6.2, thepatient still has positive sputum smear that reveals tuberculosis bacteria.
The healthcare personnel decide that such patient requires antituberculosis
retreatment, and the treatment is immediately started.
As the relative, you need to give clear details on the drugs to receive, with focus
on the additional drugs, their mode of administration, and for how long thesedrugs will be taken.
Referring to the data above, answer the following questions:
a) Which drug will be added on the usual tuberculosis primo-treatment
drugs?
b) What is the route of administration for the added drug?c) For how long will the added drug be given to the patient?
1.6. End unit assessment
End of unit assessment
After going through the unit of antibiotics, attempt the following
questions:
1) Which of the following terms refers to the ability of an antimicrobial drug
to harm the target microbe without harming the host?
a) Mode of action
b) Therapeutic level
c) Spectrum of activity
d) Selective toxicity
2) Selective toxicity antimicrobials are easier to develop against bacteria
because they are ________ cells, whereas human cells are eukaryotic
3) The spectrum of activity of an anti-infective indicates:
a) The anti-infective’s effectiveness against different invading organisms.
b) The acidity of the environment in which they are most effective.
c) The cell membrane type that the anti-infective affects.
d) The resistance factor that bacteria have developed to this anti-infective.
4) A bacteriostatic substance is one that:
a) Directly kills any bacteria it comes in contact with.
b) Directly kills any bacteria that are sensitive to the substance.
c) Drevents the growth of any bacteria.
d) Prevents the growth of specific bacteria that are sensitive to the
substance.
5) Ciprofloxacin, a widely used antibiotic, is an example of:
a) A penicillin
b) A fluoroquinolone.
c) An aminoglycoside.
d) A macrolide antibiotic
6) Which of the following is ototoxic and nephrotoxic?
a) Erythromycin
b) Doxycycline
c) Ampicillin
d) Gentamicin
7) Which of the following antibiotics is contraindicated in pregnant women
and small children due to its tendency to irreversibly stain developing
teeth?
a) Aminoglycosides
b) Tetracyclines
c) Penicillins
d) Fluoroquinolones
8) Which of the following is an example of an aminoglycoside antibiotic?
a) Azithromycin
b) Erythromycin
c) Streptomycin
d) Clindamycin
9) Differentiate a bacteriostatic antibiotic from bactericidal antibiotic.
10) Classify antibiotics into 5 categories according to their mechanism of action.
