UNIT 7: NURSING ASSESSMENT OF RESPIRATORY SYSTEM
Key unit competence:
Take appropriate action based on findings of nursing assessment of respiratory
systemIntroductory activity 7
Observe the image below and respond to the asked questions
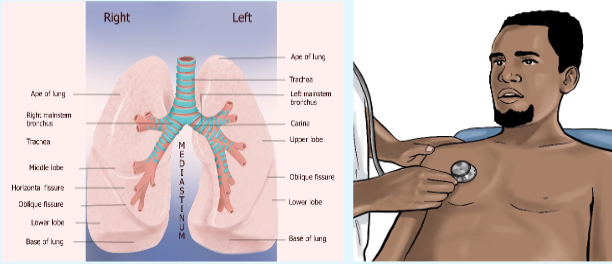
1) Identify the procedure that is being performed on picture B?
2) List the lung’s anatomy parts shown by allow on picture A on right and
left side?7.1. History taking on respiratory assessment
Learning activity 7.1.

1) Outline the types of information needed during history taking on
respiratory system?
2) State some of the 5 key questions asked by health care providers during
history taking on respiratory system?7.1.1. Respiratory history taking overview
Among the assessment techniques essential to valid diagnosis, performing a fact
finding history is key. To obtain adequate history, providers must be well organized
attentive to the patient’s verbal and nonverbal language and able to accurately
interpret the patent’s responses to questions. The history like the physical
examination is informed by the knowledge of a wide range of conditions, their
physiological basis and their associated signs and symptoms.A comprehensive nursing assessment includes an assessment of each system. In
this lesson, we are going to focus on the respiratory system. Regardless of the chief
complaint, a thorough symptom analysis is warranted.It is important to get an understanding of when the complaint started and how the
onset occurred, determine how it has evolved, starting with the initial episode or
awareness of the problem. Ask whether the problem is constant or intermittent.Determine whether a similar problem has been experienced in the past. It is
important to learn whether anything in particular, such as emotions, exposure to
outdoor allergens, or fatigue, tends to precipitate or accelerate the complaint. Also
determine whether the symptoms tend to be tied to any particular time of day, such
as night, early morning, or immediately following a meal.Another timing-related issue involves whether the complaint has continued
essentially unchanged, worsened, or improved since first noticed.The quality of the symptom is important
7.1.2. Pulmonary review of symptoms
a) Shortness of breath
If the patient experiences shortness of breath, record the amount of work or effort
that causes this symptom. Ask about nocturnal orthopnea or related difficulty
sleeping. Specifically, ask about the number of pillows the patient uses to sleep
and about the sleeping position. A patient may use no pillows and rest comfortably
only in a recliner.Determine whether the patient has had a cough and whether any cough has been
associated with the production of sputum or with hemoptysis.Also ask about wheezing, chest tightness, and sense of congestion. Ask whether
the patient has had a fever, chills, or night sweats. In addition to asking about
symptoms related to the lower respiratory tract, other systems should be explored
on the basis of the presenting symptom and symptom analysis.b) Dyspnea
The subjective sensation of difficulty in breathing is probably the most common
respiratory complaint and cannot be differentiated at first glance from dyspnea due
to cardiac disease, neuromuscular weakness, or simple obesity.Some questions can be asked to explore the origin of dyspnea;
Is the breathlessness recent or has it been present for sometimes?
Is it constant or does it comes and goes?
What can’t you do because of the breathlessness?
What makes the breathing worse?
Does anything make it better?
Duration?c) Cough
Cough is a normal defense mechanism of the respiratory tract, but when increased
in severity or frequency, cough can be a cause of disease as well as an indicator
of disease.The etiologies of cough can be:
Inflammatory: edema and hyperemia of airways and alveoli due to laryngitis,
tracheitis, bronchitis, bronchiolitis, pneumonitis, and lung abscess. Mechanical: inhalation of particulates (dust) or compression of airways
(pulmonary neoplasms, foreign bodies, granulomas, bronchospasm).
Chemical: inhalation of irritant fumes, including cigarette smoke Thermal:
inhalation of cold or very hot air.The assessment of a cough implies also the duration. The patient will be asked for
how long has he/she been coughing. When the cough has been there for days to
weeks; it is a sub acute cough. If the cough has been there for months to years; it
is a chronic cough.d) Sputum/ Expectoration
Sputum production reflects an image the presence of inflammatory, infectious or
neoplastic disease in the airways or pulmonary parenchyma. The amount and
character of sputum provide the health care provider with helpful clues to distinguish
among possible etiologies. The color can be mucoid, purulent, mucopurulent or
bloody. Also assess the duration and presence of fever or wheezing.e) Hemoptysis
Hemoptysis is the coughing up of blood from the lungs. Before using the term
“hemoptysis,” the source of bleeding should be confirmed by both history and
physical examination. Blood or blood-streaked material may originate from the
mouth, pharynx, or gastrointestinal tract and can easily mislabel. The color of the
blood is also implied; blood originating from the stomach is usually darker than blood
from the respiratory tract and may be mixed with food particles. When it is originating
from the gastric tract, it is called “hematemesis”. For patients reporting hemoptysis,
the volume of blood produced is also assessed. Hemoptysis is confirmed by the
presence of Cough, Sputum, Alcalin PH, and Alveolar macrophage.f) Wheezes
Wheezes are sounds that are heard continuously during inspiration or expiration,
or during both inspiration and expiration .They are most commonly heard at end
inspiration or early expiration. Wheezes are caused by air moving through airways
narrowed by constriction or swelling of airway or partial airway obstruction. Wheezes
can be classified as either high pitched or low pitched wheezes. It is often inferred
that high pitch wheezes are associated with disease of the small airways and low
pitch wheezes are associated with disease of larger airways.g) Chest pain
The source of chest pain can be due to parietal pleura, chest wall, diaphragm, or
mediastinal involvement, it can be pleuritic (sharp knife-like), it can also originate
from myocardium (angor pectoris, myocardial infarction), from pericardium
(pericaditis), from aorta (dissecting aortic, aneurism) or from trachea and large
bronchi (tracheitis, bronchitis). The following questions have to be asked while
assessing pain; where?, how long?, kind, radiation.h) Clubbing
Fingers extremities change in coloration due to their poor oxygenation. Clubbing
can be caused by lung abscess, chronic cavity due to mycobacterial or fungal
infection in lungs, clubbing may also be caused by cardiovascular diseases, or
metabolic diseases.Self-assessment 7.1.
1) In case the client consults the health care provider for respiratory
problems, the health care provider should determine whether a similar
problem has been experienced in the past and rule out the factors
influencing respiratory system disorders. The one among the following
factors has no influence on respiratory problems:
a) Emotions,
b) Fatigue,
c) The number of deliveries for a woman,
d) Exposure to outdoor allergens.2) If the patient experiences shortness of breath, record the amount of
work or effort that cause this symptom and ask about:
a) The sleeping position,
b) Nocturnal orthopnea or difficulty sleeping,
c) The number of pillows the patient uses to sleep,
d) All the above3) The coughing up of blood from the lungs is the symptom reported often
by patients. The source of bleeding should be confirmed by both history
and physical examination. This symptom is called:
a) Hematemesis
b) Hemoptysis
c) Expectorant
d) Soft vomiting4) The quality of the symptom is important if a patient complains about “pain”
during history taking of respiratory system conditions, the nurse should ask
whether the pain is:
a) Mild and tickling, sharp and paroxysmal
b) Sharp, dull, aching
c) In inspiration or expiration
d) Radiating to other sites and how it relates to respirations7.2. Physical examination of respiratory system: A/
General examinationLearning activity 7.2.
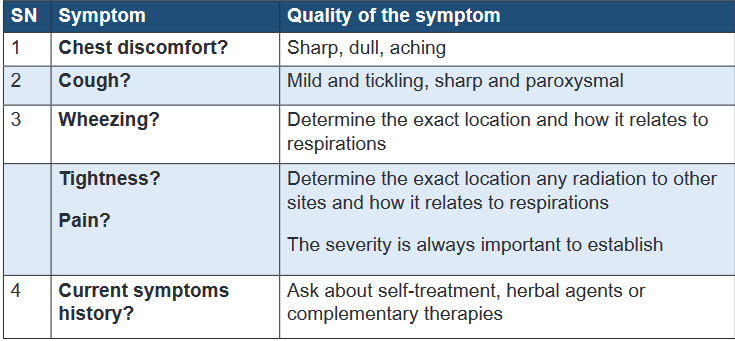
Analyze carefully the following images and respond to the questions below;
1) List the two (2) physical signs shown on above image which may indicate
poor oxygen in body?
2) Describe two signs of poor tissue oxygenation observed in nails?
3) Explain what does lymph nodes enlargement indicate in respiratory
assessment?
4) Which posture is to be observed to assess if the patient has respiratory
distress?Fundamental of Nursing | Associate Nursing Program | Senior 4 335
Initial survey is the first step to be performed by health care provider to evaluate the
level of consciousness if the patient is alert, cooperative, and normally oriented
because patients with hypoxemia may be irritable, somnolent, restless, confused,
or combative.The close assessment of the position for breathing is necessary whether the posture
is relaxed or upright because the patients in respiratory distress may lean forward
in “tripod position” a position whereby one sits or stands learning forward and
supporting the upper body with hands on knees or on another surface.
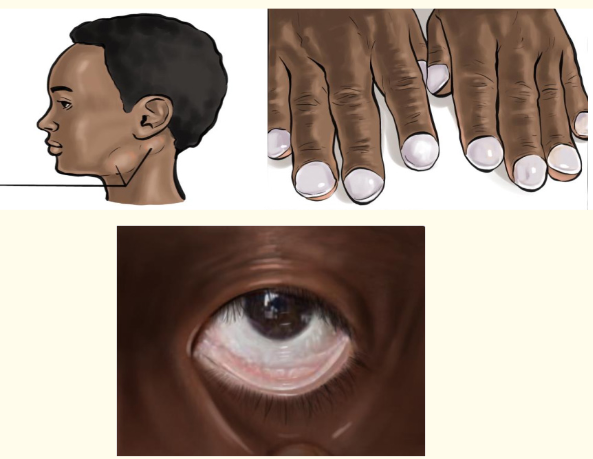
The other observation will focus on patient’s lips and nasal flaring including facial
expression as patient in respiratory distress may look anxious or show nasal flaring
and those with chronic obstructed pulmonary diseases show pursed lips; the
observation and documentation of skin color for cyanosis and pallor is also a key.
Skin color is appropriate tone for race. Cyanosis is a bluish color to the skin or
mucous membrane and is usually due to a lack of oxygen in the blood while pallor
is a condition in which a person’s skin and mucous membranes turn lighter in pale
color than they usually are secondary to respiratory distress it is often observed in
palms and nails.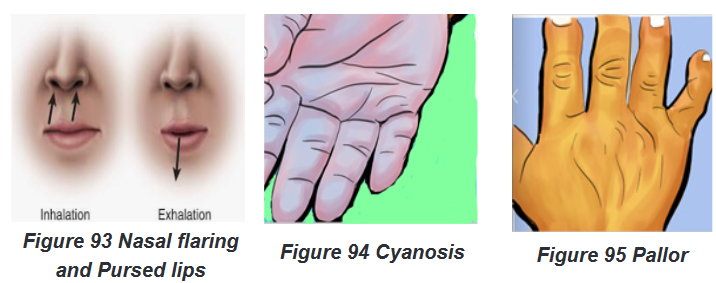
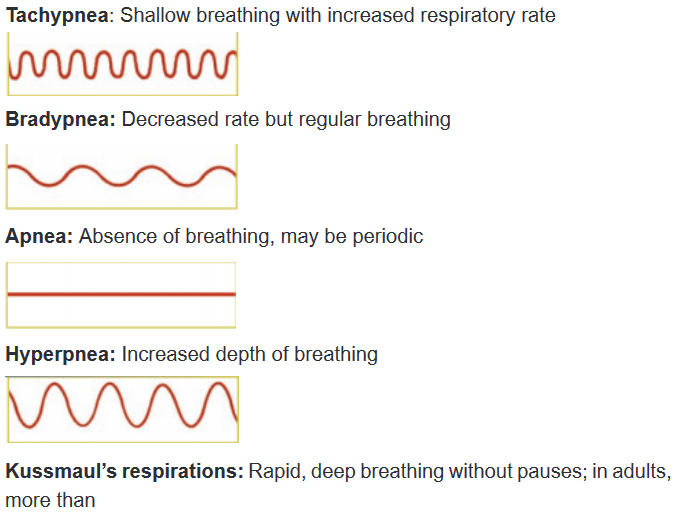
The nurse observes respiratory movements and note if the patient uses the upper
or lower chest to breathe because patients with disease that impedes outflow may
have forced expiration. Guarding may accompany respiratory pain. The observation
of respiratory movements may be accompanied by counting rate.Respiratory rate is 12 to 20 breaths per minute for adults with regular rhythm.
Tachypnea is greater than 24 breaths per minute; bradypnea is less than 10
breaths per minute. An infant’s breathing rate may reach 40 breaths per minute.
The respiratory pattern should be even, coordinated, and regular, with occasional
sighs (long, deep breaths).Assess muscles used for breathing. Diaphragm and external intercostals do most
of the work. Intercostals retractions are due to reduced air pressure inside the
chest; this can happen if the upper airway or small airways of the lungs become
partially blocked. Patients with respiratory distress may use accessory muscles.
Retractions accompany resistance to airflow (eg, in severe asthma)Observe fingers for clubbing, clubbing is a physical sign characterized by bulbous
enlargement of the ends of one or more fingers or toes due to proliferation and
edema of connective tissue result in loss of the normal angle between the skin and
nail plate and excessive sponginess of the nail base. Clubbing is noted with chronic
lung disease.The observation of lymph node enlargement is important as the most common
cause of lymph node swelling in the neck is an upper respiratory infection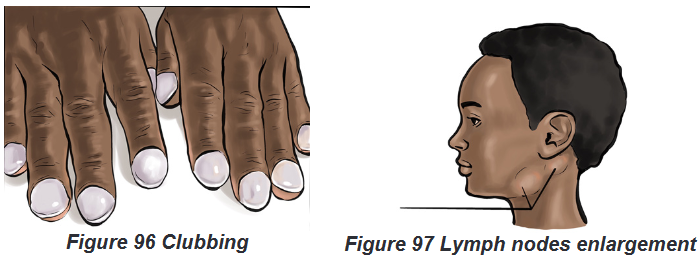
Self-assessment 7.2.
1) Recall the two observations to be noted by a health care provider related
to respiratory movements?
2) Explain intercostals retraction sign and give an example of respiratory
disease in which this sign may occur?
3) Express the importance to evaluating the level of consciousness in
respiratory assessment.
4) Recall two signs assessed on patient’s lips and nose to diagnose
respiratory problems?7.3. Physical examination of respiratory system: A/
Focused examinationLearning activity 7.3.
The images below illustrate the focused respiratory physical exam
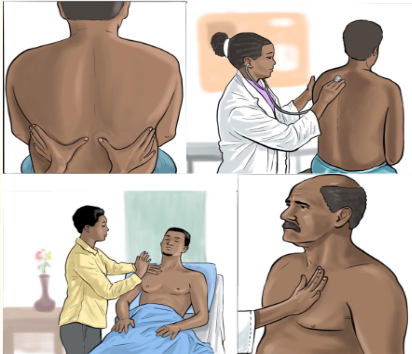
1) Describe the similarities and differences observed in images of
respiratory focused examination?The focused physical examination is helpful to examine the posterior thorax and
lungs while the patient is sitting, the anterior thorax and lungs while the patient is
supine. The process is performed in four ordered phases or techniques: inspection,
palpation, percussion and auscultation.7.3.1. Inspection
This phase/technique of inspection requires the use of the naked eye of health care
provider to observe the face for nasal flaring, pursed lips breathing, conjunctiva for
pallor and facial skin for central cyanosis. Observe neck and trachea for jugular
vein and neck veins pulsation in bronchial asthma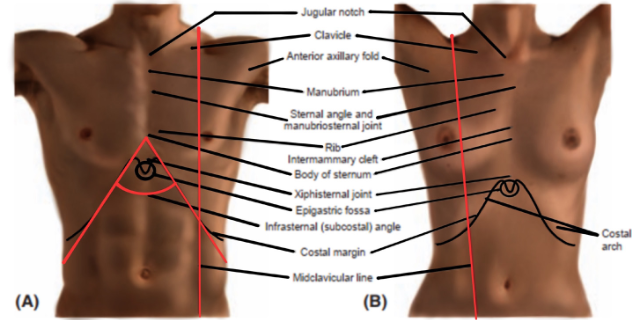
Note thoracic shape and configuration (horizontal ribs, barrel chest, kyphosis,
funnel chest), observe spontaneous chest expansion, scapulae are symmetric.
Chest wall is cone shaped, symmetric and oval. Accessory muscle use is to be
noted and hands inspection for Clubbing (base angle of nail obliterated, increased
sponginess of nail bed) and peripheral cyanosis: excessive O2 extraction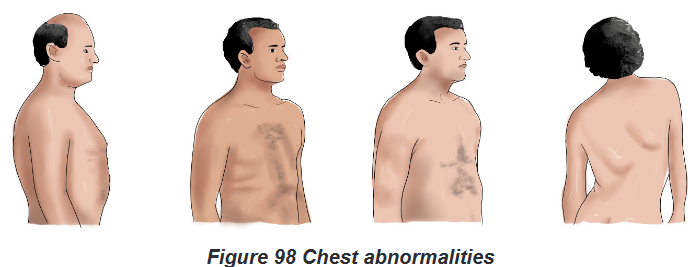
7.3.2. Palpation
Palpation technique consists of using fingertips above the scapula over the lung
apex. Move from one side to another; compare bilateral findings. End at lung base;
move laterally to midaxillary line.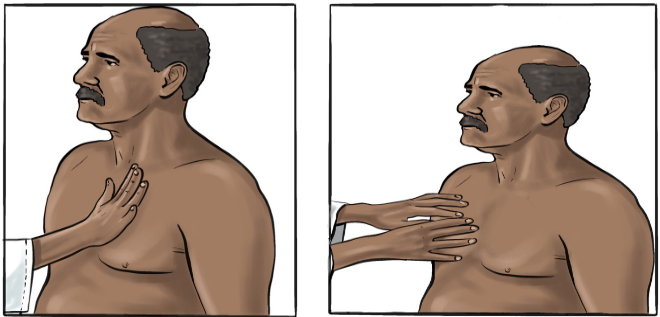
Place your palm (or palms) lightly over the thorax. Palpate for tenderness, alignment,
bulging, and retractions of the chest and intercostal spaces, lumps, masses. Assess
the patient for crepitus, especially around drainage sites. Repeat this procedure on
the patient’s back. Palpation helps to examine the thoracic wall defects like pain
press and swelling and vibration sounds (tactile fremitus).Use the pads of your
fingers to palpate the front and back of the thorax. Pass your fingers over the ribs
and any scars, lumps, lesions, or ulcerations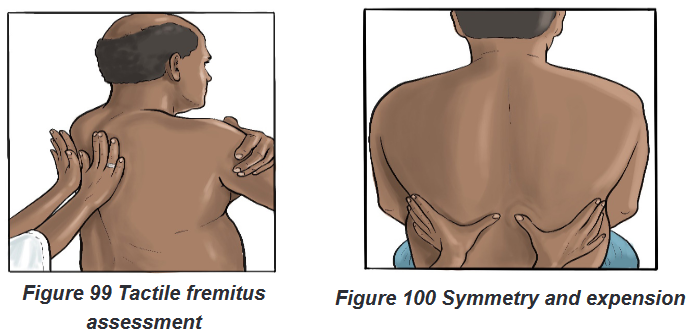
7.3.3. Percussion
Percussion is a method of tapping on a surface to determine the underlying
structure, and is used in clinical examinations to assess the condition of the thorax;
percussion is used when lung obstruction or consolidation is suspected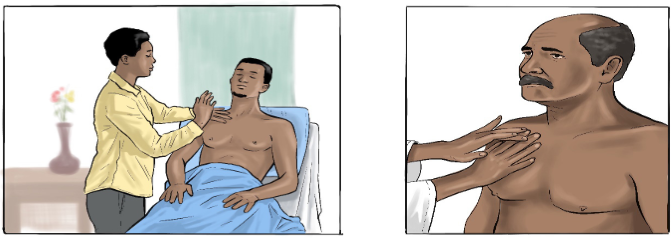
The examiner begins at the apex of the lungs. Percuss from one side to another.
Work toward the bases in the intercostal spaces. Move fingers approximately 5 cm
apart. When fingers are below the level of lung tissue, sound changes from resonant
to dull; from around T10 move laterally to percuss near the anterior axillary line and
7th and 8th Intercostals. Avoid the area over the ribs and scapulae, because normal
bone is flat.Healthy lung tissue sounds resonant.
Place your non dominant hand over the chest wall, pressing firmly with your
middle finger.
Position your dominant hand over your other hand.
Flex the wrist (not the elbow or upper arm) of your dominant hand; tap
the middle finger of your non-dominant hand with the middle finger of your
dominant hand.
Follow the standard percussion sequence over the front and back chest
walls.7.3.4. Auscultation
Auscultation is performed for the purposes of examining the respiratory system for
breath sounds. Listen from top to down alternating left and right. Ensure that the
stethoscope is in direct contact with the skin.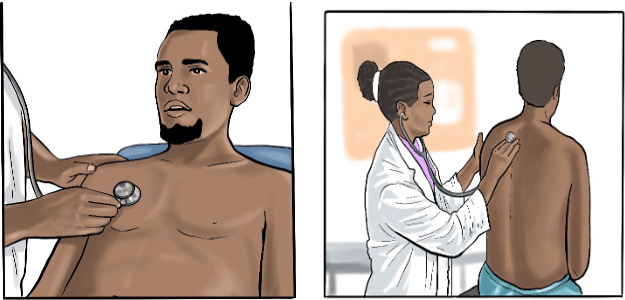
Listen for extra, abnormal sounds of breathing. Ask the patient to breathe through
the mouth. Place the flat side of the diaphragm on the chest wall firmly to block
extraneous noise. Listen to one full breath in each location. Move from one side to
another. Stand behind and beside the patient. Listen from lung apices to bases and
then laterally in the same sequence as percussion. If sounds are too soft, ask the
patient to breathe deeper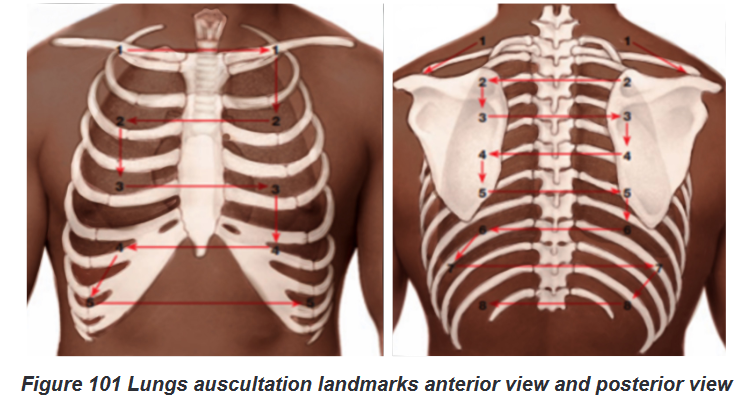
Identify vesicular, broncho vesicular, and bronchial breath sounds. Listen for
intensity of sounds, quality, pitch, and duration of inspiration versus expiration.
Normal breath sounds are vesicular. Expiration is longer than inspiration, similar
to normal breathing. Note the absence of adventitious sounds when documentingSelf-assessment 7.3.
1) List the four phases/techniques of respiratory physical examination?
2) Outline the elements of inspection in respiratory physical examination?
3) Describe the difference between percussion and palpation techniques
for thorax examination?7.4. Interpretation of specific findings and client’s
problems identificationLearning activity 7.4.
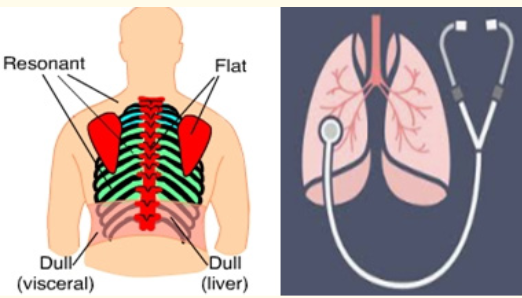
The image above shows areas of percussion and the stethoscope for lung
auscultation. Questions:
1) List the normal findings and abnormal findings of lungs percussion?
2) What are abnormal findings t of auscultation7.4.1. The normal findings and abnormal findings from
respiratory physical examination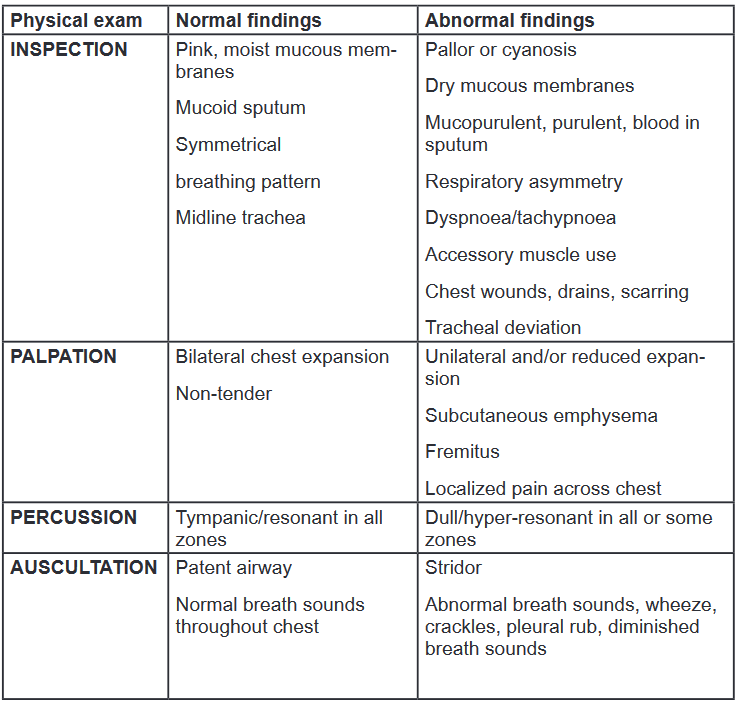
7.4.2. Normal breath sounds
Tracheal: The sound is heard over the trachea and above supraclavicular as very
loud, harsh, and high-pitched. Inspiration = expiration.Bronchial: The sound is heard just above clavicles on each side of sternum, over
the manubrium as loud, harsh, and high-pitched. Inspiration < expiration.Bronco-vesicular: The sound is heard below the clavicles, between the scapulae
as medium-pitched. Inspiration duration = expiration duration.Vesicular: Sound heard over areas of lung tissue as soft and low-pitched. Inspection
> expiration.7.4.3. Abnormal breath sounds
Wheezes: wheezes are whistling or rattling sound in the chest heard during
breathing, as a result of obstruction in the air passages. Wheezes indicate airway
restriction and are typically heard on expiration. Wheeze sound during inspiration
indicates severe airway narrowing. They are high-pitched when produced in small
bronchioles, and low-pitched when produced in larger bronchi. Monophonic (i.e.
single pitch) when heard in an isolated area, and polyphonic (i.e. multi-pitched)
when heard throughout the lung area. Causes include broncho constriction, airway
inflammation, secretions, and obstruction.Crackles: Crackles are adventitious lung sounds heard on auscultation of the chest,
produced by air passing over retained airway secretions or the sudden opening of
collapsed airways. Crackles indicate instability of airways collapsing on expiration.
Fine crackles can be heard in small airways, and coarse crackles can be heard in
larger airways. Causes include pulmonary oedema, secretions, atelectasis, and
fibrosis.Pleural rub: indicates inflammation of the parietal and visceral layers of the pleura.
Stiff creaking sound heard throughout inspiration and expiration. Causes include
pleurisy.Diminished or absent breath sounds: indicate lack of ventilation and/or respiration.
Causes include pneumothorax, pleural effusion, gas trapping, and collapse
Stridor: Loud high-pitched crowing or honking sound louder in upper airway. The
causes may include laryngeal or tracheal inflammation or spasm from epiglottitis,
croup, or aspiration of a foreign object can cause stridor.7.4.4. Abnormal percussion sounds
Dullness: indicates a solid structure, a consolidated or collapsed area of lung, or a
fluid-filled area, which produces a dull note on percussion. Causes include pleural
effusion, infection, and lung collapse.Hyper-resonance: indicates a hollow structure, which produces a hyper-resonant
note on percussion. Causes include pneumothorax.7.4.5. Abnormal findings from inspection of thorax
Normal adult: Anterior-posterior: lateral ratio is 1:2, wider than it is deep, oval
shaped. Cone shaped from head to toe.Kyphoscoliosis: With kyphosis, the thoracic spine curves forward, compressing
the anterior chest and reducing inspiratory lung volumes. With scoliosis, a lateral
S-shaped curvature of the spine causes unequal shoulders, scapulae, and hips. In
severe cases, asymmetry may impede breathing.Barrel chest: Anterior-posterior: lateral ratio near 1:1, round shaped. Ribs are more
horizontal and costal margin is widened. Barrel chest is associated with COPD,
chronic asthma, and normal aging.Pectus excavacum: Depression in lower part of an adjacent to sternum. Congenital
condition may compress heart or great vessels and cause murmurs.Pectus carinatum (pigeon chest): Sternum is displaced anteriorly, depressing the
adjacent costal cartilages. Congenital condition with increased anteroposterior
diameter.Flail chest: Sternum is displaced anteriorly, depressing the adjacent costal
cartilages. It may be a congenital condition with increased anteroposterior diameter.7.4.6. Abnormal findings from palpation of thorax and neck
Tender areas: may indicate muscle strain, rib fracture, or soft tissue damage. With
trauma, air can enter lungs and escape, creating a crackling sensation (crepitus).
Subcutaneous emphysema migrates and may be found in the head and neck. If the
amount is large, mark borders with a pen to note changes.Asymmetrical movements: indicate collapse or blockage of lung. Patients with
muscle weakness, respiratory disease, recent surgery, chest wall abnormalities, or
obesity may have reduced chest expansion.Tactile fremitus: Conditions that may lead to decreased or absent fremitus include
obstructed bronchus, COPD, pleural effusion, fibrosis, tumor, pneumothorax,
obesity, or an extremely large chest. Increased fremitus may accompany severe
localized pneumonia or lung tumor.Tracheal deviation: There are several causes for a tracheal deviation, and the
condition often presents along with difficulty breathing, coughing and abnormal
breath sounds. The most common cause of tracheal deviation is a pneumothorax,
which is a collection of air inside the chest, between the chest cavity and the lung.7.4.7. Abnormal findings from general inspection
Breathlessness, use of accessory muscles, and exhalation with pursed lips:
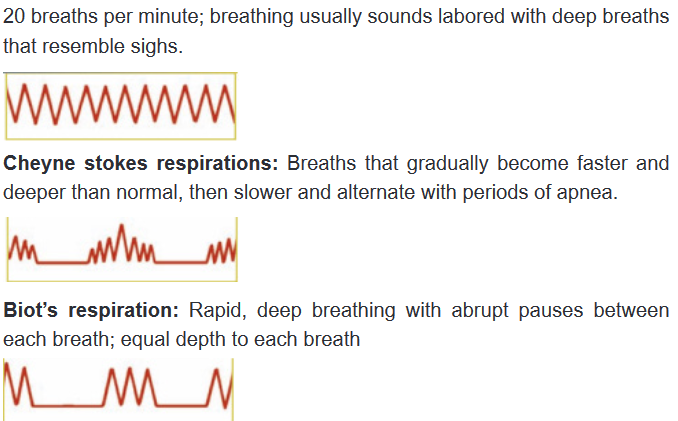
The combination of mentioned signs indicates the evidence of respiratory distress.Respiratory movements and rate: respiratory rate is 12 to 20 breaths per minute
for adults, with regular rhythm. Tachypnea is greater than 24 breaths per minute;
bradypnea is less than 10 breaths per minute.Oxygen saturation: oxygen saturation level normal is 95% to 100%. Pulmonary
embolism produces hypoxemia.Lymph nodes enlargement: Patients with pneumonia may present with unusually
enlarged mediastinal lymph nodes, which are most likely, a result of a strong
immune response to pneumonia.7.4.8. Abnormal respiratory pattern
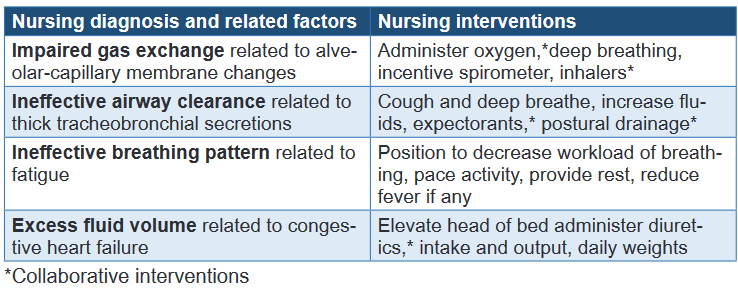
7.4.9. Common associated nursing diagnosis and interventions
Self-assessment 7.4.
1) When multiple ribs are fractured, paradoxical movements of the chest
may occur. As the diaphragm pulls down during inspiration, negative
pressure causes the injured area to cave inward; during expiration it
moves out. This situation happens in case of:
b) Barrel chest
c) Flail chest
d) Kyphoscoliosis
e) Pectus carinatum2) The normal level of oxygen saturation is:
a) 100%
b) 95%
c) 90-100%
d) 95-100%3) Tachypnea is a condition in which respiratory rate becomes greater than:
a) 24 breaths per minute
b) 20 breaths per minute
c) 22 breaths per minute
d) None of the above4) The lymph node enlargement observed during respiratory assessment
may indicate:
a) Bronchial asthma
b) Respiratory distress
c) Pulmonary embolism
d) Pneumonia5) Recall at least four (4) respiratory abnormal patterns that may be assessed?
6) List two normal breath sounds obtained through lungs auscultation?
7) Differentiate wheezes from crackles abnormal lung sounds?
8) Outline two nursing diagnoses related to respiratory system?
End unit assessment 7.
Select the bests answer, only one option is accepted:
1) Respiratory history taking is the key element of respiratory assessment
to:
a) Valid diagnosis
b) To make a therapeutic plan for patient
c) To help health care provider filling patient’s file
d) To prevent complications related to the patient’s diagnosis2) Dyspnea due to respiratory problems cannot be differentiated at first
glance from dyspnea due to cardiac disease, neuromuscular weakness,
or simple obesity, the following questions can be asked to explore the
origin of dyspnea but the one has no impact on respiratory history taking:a) What makes the breathing worse?
b) Does anything make breathing better?
c) What is family planning used method?
d) What can’t you do because of the breathlessness?3) Wheezes are sounds that are heard continuously during inspiration
or expiration, or during both inspiration and expiration .They are most
commonly heard at end inspiration or early expiration and they are caused
by:
a) Airways narrowed by constriction,
b) Air passing through a solid structure,
c) Laryngeal or tracheal inflammation,
d) A hollow structure producing hyper-resonant sound4) There are several causes for a tracheal deviation observed through
palpation or inspection of neck. The condition often presents along with:
a) Cyanosis
b) Pallor
c) Poor oxygen saturation
d) Difficult breathing, coughing and breath sounds5) The most common cause of tracheal deviation is:
a) Pneumonia
b) Pneumothorax
c) Bronchial asthma
d) Chest asymmetry6) Patients with pneumonia may present with unusually enlarged mediastinal
lymph nodes, which are most likely, a result of:
a) Neck indicate muscle strain
b) Thick tracheo-bronchial secretions
c) Alveolar-capillary membrane changes
d) A strong immune response to pneumonia7) The impaired gas exchange is the respiratory nursing diagnosis observed
among patients consulted for respiratory problem; the most related
nursing factor include the following:
a) Thick tracheo-bronchial secretions
b) Alveolar-capillary membrane change
c) Increased fluid volumed) Fatigue
8) The nursing interventions to perform towards patient with ineffective
airway clearance include the following except one:
a) Increase fluids, expectorants
b) Administer anti-histamine drugs
c) Cough and deep breathe
d) Postural drainage
9) Outline the sequences of respiratory focused physical examination?
10) List four respiratory abnormal pattern findings ?
