UNIT 5: DRUG ADMINISTRATION
Key Unit Competence:
Administer correctly drugs through enteral, topical and selected parenteral routesIntroductory activity 5.
Case study on drug administration
Shema a 16-year-old boy went for consultation to NKUNGU health center, they
prescribed anti malaria 4 tablets to be taken by mouth two times a day for
three days. On the 2nd day, he forgot the morning tablets, during the evening
he decided to take together the forgotten tablets and current ones. At 10 P.M,
he started developing vomiting, weakness and abdominal pain. His parents
took him immediately back to the health center, the nurse transferred Shema
to MIBIRIZI District hospital for further management. At the admission, the Dr
started medication in form of injections for 3 days, including anti malaria and
anti-vomiting. A nurse calculates the prescribed dose as required then she
gives to Shema, after 2 days, Shema recovered and discharged.1) After being treated at his health facility, SHEMA received different
medications. Did his health care provider give him instructions to follow
about medication before going back home?
2) In this case, discuss the instruction nurse provided to Shema before
going home to continue medication.
3) What do you think about Shema’s attitude in regards his prescribed
tablets? Give your suggestion.
4) What do you think about different ways of taking prescribed medication?
5) Do you think the action of the Dr, to change the tablet to injection
medication for Shema, was is it the right time? Explain5.1. Rights of drug administration
Learning activity 5.1.
Read the text below and answer related questions:
Nurse Brune is going to offer insulin to a patient in room 213, internal medicine
at King Faisal Hospital. She reads careful the patient file to confirm the patient’s
name, age and disease, the amount, name of the drug, expiration date and the
intervals to follow to provide everyday dose. Arriving in the patient room, she
introduces to the patient and explain the indication, purpose and the route of
medication administration. The patient agrees to receive the drug, the nurse
started by controlling blood sugar and then injected the prescribed amount of
insulin. After providing this medication, she documented the whole process in
patient file.
1) As an associate nurse, do you believe on Brune’s process of drug
administration?
2) What are the rights of drug administration observed in the above case
study?
3) Do you think that there are other drug administration right not mentioned
in this case study? If yes list them.When people become ill, they are used to go to the health centers to seek for
treatment. Some treatment mode involves prescription of medications with curative
or preventive role. To achieve intended outcomes, health professionals should
follow different rights of drug administration in order to ensure patient safety.Drug administration is the process of giving out medication to the patient in order
treat or prevent disease or complication.A medication/drug is a substance administered for the diagnosis, treatment, relief
of a symptom and prevention of disease. Nurses help the patients to develop a
proactive understanding of medications, clarifying the confusing information and
responsibly share decision making with other healthcare professionals.Right for drug administration is a guidance to health practitioners on the
appropriate way to follow while ensuring the safety of drug administration.
This is a nursing responsibility. To abide to the rights of drugs administration
help nurses to maintain patient safety, meet the quality of care and prevent
medication errors.In today’s health care delivery, nurses are accountable for their practices.
This is the reason why; we have to be aware from the beginning the rights of
drug administration to ensure both patient and healthcare professionals are
protected.5.1.1. Right patient
The first right in drug administration is to identify the correct patient to be given
medications. A nurse must carefully verify the person’s identification each time
before administration of a medication. Use the names as recorded in the patient
file, ask the patient if he or she is conscious and read patient identification band.5.1.2. Right medication
The ordered medication is appropriate for the patient. Nurses should not rely on
memory from previous interaction with the patient because beds can be changed
at any way or patent discharged and replaced.5.1.3. Right dose
The dose ordered is appropriate for the patient. A nurse should be able to calculate
the correct dose in accordance to the prescription and not expect to always exact
doses of medication from pharmacy. E.g: a dose may be a half of a tablet, two
tablets, the tenth of a bottle depending on the desired doses.5.1.4. Right time
Give the medication at the right frequency and at the time as ordered. Medications
given within 30 minutes before or after the scheduled time are considered to meet
the right time standard.5.1.5. Right route
Give the medication by the ordered way of administration. Make sure that the route
is safe and appropriate for the person.5.1.6. Right education
Explain information about the medication to the person e.g. why receiving, what to
expect, any precautions.5.1.7. Right documentation
Document medication administration after giving it, not before. Write the name and
the dose of given medication, route of administration and injection site in case of
parenteral medication, date and time lastly the name or initials of the administeringnurse. Please, note any issue encountered during this process such as lack of the
medication, vomiting after oral medication intake, any abnormal reaction5.1.8. Right to refuse
Adults have the right to refuse any medication. The nurse’s role is to ensure that the
person is fully informed of the potential consequences of refusal and to communicate
the person’s refusal to the health care provider.5.1.9. Right assessment
Some medications require specific assessment prior to administration. E.g: Check
blood pressure before giving diuretics, verify glycemia values before giving insuline.
Medication orders and manufacturer instructions may indicate specific parameters.
E.g: do not give if pulse is less than 60 beats per minute or do not give if systolic
blood pressure less than 100 mmHg”.5.1.10. Right evaluation
The nurse has to make a proper follow-up after certain time of drug administration.
That follow up will answer questions such as: Was the desired effect achieved?
Did the person experience any side effects or adverse reactions? If, yes what was
those side effects or adverse reactions?Self-assessment 5.1.
1) What do you understand by drug administration?
2) Explain different rights of drug administration.
3) An associate nurse student is asked to administer Cloxacillin 350mg
per mouth but the prescription was not very clear to read. He decided to
offer 500mg because it was difficult to read the prescription. Which right
of drug administration has been not respected in this case?5.2. Enteral routes of drug administration
Learning activity 5.2.
Nurses use various ways of drug administration as illustrated in the pictures
below.
Observe these pictures.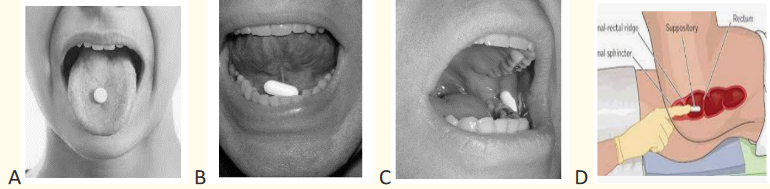
1) Observe the above picture A, B, C, D, do you think all tablets are
reserved to be swallowed?
2) What are the similarities and difference between the message from the
above pictures?
3) Give the indications of drug administration routes presented above
4) What are the advantages of the above routes of drug administration?When people become ill, they are used to go to the health centers or hospital for
treatment. Some treatment modalities involve medication provision. Usually, every
medication has a way to be administered in order to reach the site of action. The route
of drug administration is the path by which a drug, fluid or other substance is brought into
contact with the body to obtain maximum benefit. The route of administration should
be indicated when the drug is ordered. When administering a drug, the nurse should
ensure that the pharmaceutical preparation is appropriate for the route specified. The
enteral route of drug administration is the one of three categories.Enteral administration is about exposing drug to the gastrointestinal (GI) tract.
The medications are introduced in the mouth or in the rectum. The enteral route of
drug administration includes oral, buccal, sublingual and rectal route.Substances prepared for enteral administration may be available in a variety of
pills, including tablets, capsules, and syrup. Tablets are commonly round, and are
sometimes coated so that they do not easily dissolve in the mouth. Capsules have
rectangle forms and may contain granules of the active compound that release as
the outer coating is dissolved in the stomach. Children may have immature muscle
and nerve development which interfere with swallowing reflexes others may just
dislike their taste.5.2.1. Oral route
Oral route (Figure 68) is the most common, least expensive and most convenient
route for most people.In oral administration, the medication is given by mouth and then swallowed. It is
used for patients who can ingest and tolerate an oral form of medication however it
cannot be used in unconscious patients, patients with vomiting, in patient with nil
per mouth order and during emergency.Oral route of drug administration is most convenient, usually least expensive,
safe, does not break skin barrier and administration usually does not cause stress.
This route has some disadvantages as some medication have unpleasant taste,
can cause irritation of the gastric mucosa (Aspirine), poorly absorbed from the
gastrointestinal tract and may harm to the person’s teeth. For example, the liquid
preparation of ferrous sulfate (iron) can stain the teeth.For oral drug administration technic, nurse need different equipment like
prescription chart, medication pack, disposable medicines container; straw, water
or juice, kidney dish to be used in case of vomiting, examination gloves and plate.
This equipment will be needed in the below procedure:Procedural steps
1. Preparation
Review the patient’s notes and prescription.
Wash hands
Gather all necessary equipment and arrange them on the plate
Check that the details on the prescription are complete, including the pa-
tient’s name, hospital number, date of birth and allergy status
Self-introduction by name and function to the patient and obtain verbal
consent. This is an ideal opportunity to answer any questions the patient
has about their treatment and check their understanding of the medicine
regimen.
Check that the prescription is unambiguous/legible and includes the medi-
cine name, form, route of administration, strength and dose of the medicine
to be administered.
Check the date and time when it should be administered, that the prescrip-
tion is signed and includes a start and finish date, if appropriate
Caution: A medicine should not be administered if there are any concerns
about the prescription; any such concerns should be discussed immediately
with the prescriber. Ensure you know why the medicine is being administered and you are
aware of potential complications associated with administration
Check if the medicine has not been given to the patient and signed for by
another staff member.
Take the medicine and prescription to the patient and check the identity of
the patient against the prescription using their name, hospital number and
date of birth. Check their wristband according to local policy. It is important
to ask the patient to state, rather than confirm, their name and date of birth.
Complete the necessary assessment before administering the medication.
Check whether the patient has any allergies or previous adverse drug reac-
tions.1. Implementation
Wash your hands.
Position the patient comfortably so they can swallow the medicine, (The
patient should be placed in a sitting position to prevent accidental aspiration
of the medication).
Decontaminate your hands.
Select the medicine and check the expiry date
Put the required dose into a medicine pot, avoiding touching the medicine.
Position the patient in sitting or upright position
Administer the medicine (put the tab or capsule on the tongue).
Offer a drink of water or other permitted fluid with pills, capsules, tablets
to help the patient swallow the medicine if this is allowed, and ensure they
have swallowed it.
When administering a liquid suspension, shaken the bottle before the appro-
priate dose is poured. When administering sprays, the container also needs
to be shaken2. Finishing
Thank the patient, arrange patient items, and provide appropriate health
education
Disposal of the medicine pot according to local policy.
Decontaminate your hands.
Immediately record that the medicine has been administered
If the patient refuses or is unable to take their medicine, this should be docu-
mented along with the reason for omission and inform the prescriber.
Check the client within 30min to verify response to medication
Caution: If the capsule or tablet fall down, it must be discarded and a new one
should be administered. Oral medications need to be given before sublingual or
buccal medications.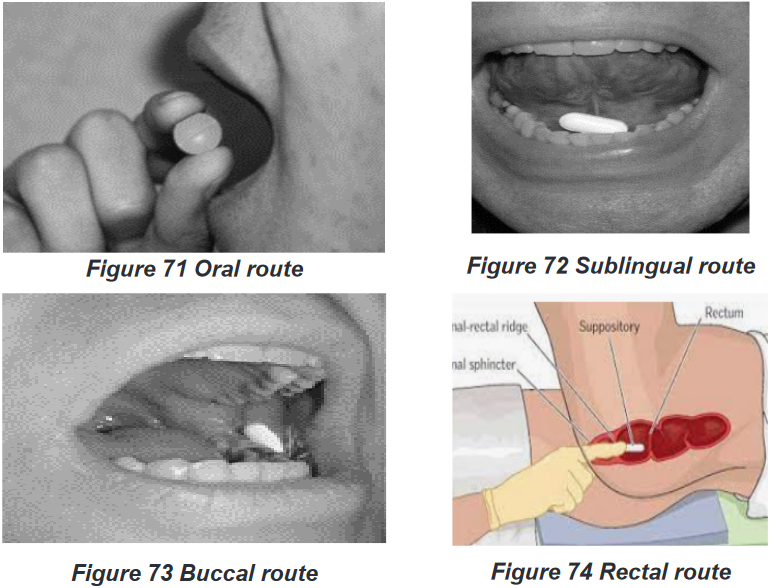
5.2.2. Sublingual route
Sublingual (Figure 72 Sublingual route) is another enteral route of drug
administration where a drug is placed under the tongue and then it dissolves there
in short time, the drug is largely absorbed into the blood vessels on the underside
of the tongue. E.g.: Nitroglycerine.Sublingual route is indicated in any of the following circumstances such as
When the drug needs to get into body system quickly, When patient has trouble
of swallowing medication, When the medication doesn’t absorb very well in the
stomach and When the effects of the drug would be decreased by digestionSublingual route is contraindicated for patients who cannot tolerate oral drugs,
such as those who have altered mental status or have nausea or vomiting.The sublingual route’s advantages are that it is more potent than oral route
because drug directly enters the blood and bypasses the liver, drug is rapidly
absorbed into the bloodstream, no need to swallow the drug, easier to take for
people who have problems of swallowing pills.However, this route has some disadvantages such as inactivation of drug by gastric
juice if swallowed, drug must remain under tongue until dissolved and absorbed,may cause irritation of the mucous membranes, not used in large amount of
medication, inconvenient to maintain the exact site. It induces nausea and vomiting
if it has unpleasant taste. Eating, drinking, or smoking, can affect how the drug is
absorbed and how well it works. Any open sores in the mouth can also become
irritated by the medication.In addition to the oral route technique basis, sublingual administration requires the
patient to open his or her mouth and raise the tongue. The tablet should then be
placed under the tongue. The nurse should examine the mucous membranes of the
patient’s mouth for irritation or sores. If there are sores in the mouth, the physician
should be contacted before any sublingual drugs administration. Alternating sites
should be used when giving regular doses of sublingual or buccal medications.
Explained to the patient that nothing should be eaten, drank, swallowed, chewed,
or smoked until the tablet has dissolved.5.2.3. Buccal route
Buccal route (Figure 73 Buccal route) of drug administration is another form of
enteral route which means that the drug is placed between cheek and gum.In buccal administration, a medication (e.g. a tablet) is held in the mouth against the
mucous membranes of the cheek until the drug dissolves. The drug may act locally
on the mucous membranes of the mouth or systemically.In buccal route drug directly enters the blood and bypasses the liver, drug is rapidly
absorbed into the bloodstream. It is contraindicated for patients who cannot tolerate
oral drugs, such as those who have altered mental status or have nausea or vomiting.Buccal route of drug administration has disadvantages like inactivation of drug
if swallowed, drug must remain between cheeks and gum until dissolved and
absorbed. Drug in buccal administration may cause stinging or irritation of the mucous
membranes. This is not used in large amount of medication, inconvenient to maintain
the exact site. It induces nausea and vomiting if drug has unpleasant taste.In addition to the oral route technic, in buccal drug administration the patient should
open his or her mouth, then tablet should be placed between the gum and the wall
of the cheek. With the mouth closed, the tablet should be held in this position for
five to 10 minutes until it has dissolve. Mouth should be examined for the presence
of sore before drug administration through this route. Alternating sites should be
used when giving regular doses of buccal medications.5.2.4. Rectal route
Rectal route is also anther enteral form of drug administration which consist of
administration of medication into rectum for absorption.It can be used as a drug delivery route for both local and systemic effects. Rectal
medication may be in suppository or in liquid form in order to facilitate administration
and absorption.It is indicated when drug has unpleasant taste or odor, drug released at slow,
steady rate provides a local therapeutic effect. To evacuate the bowel before
surgical intervention, help to relieve constipation as well as when they want to treat
hemorrhoids or anal pruritis. The most common medication in rectal routes serve as
antipyretic, analgesia and laxatives as long as the patient accept the rectal route.This route is contraindicated when patient refuse to consent, recent rectal or anal
surgery, abnormalities or trauma involving the perineal area, suspected paralytic
ileus or colonic obstruction, diarrhea and in case of active anal bleeding.The rectal route has advantages such as the absorption rate of the drug not influenced
by food or gastric emptying. The metabolism of both enteric and first-pass hepatic
elimination is avoided. It is a preferred route when drugs are administered to relieve
constipation or hemorrhoids. Drugs administered in rectal have a faster action
than via the oral route and has a higher bio-availability. Rectal administration also
reduces side-effects of some drugs, such as gastric irritation, nausea and vomiting.
Applicable in cases of nausea, vomiting, and inability to swallow (unconscious
patients), as well as in the presence of diseases of the upper gastrointestinal tract
that affect oral drug absorption. It is a tolerable route in children. In cases of toxicity
or overdose, this effect can be rapidly terminated.The disadvantages of rectal route include the interruption of the absorption process
by defecation which leads to irregular or incomplete absorption. Low volume of
rectal fluids can lead to incomplete dissolution of the drug. Certain drugs may be
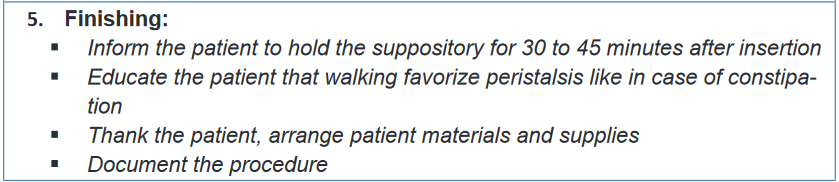
altered by microorganisms in the rectum and patient adherence may be a problem.Rectal application technique
Rectal suppositories are used mainly to local effects as laxatives and stool softener
and systemic effect such as reducing nausea, vomiting and fever. The rectal
suppositories are thinner and bullet shaped than vaginal ones. They are kept in
refrigerator until their administration, remember to always wear gloves before
insertion of rectal medication to protect your hands from fecal contamination.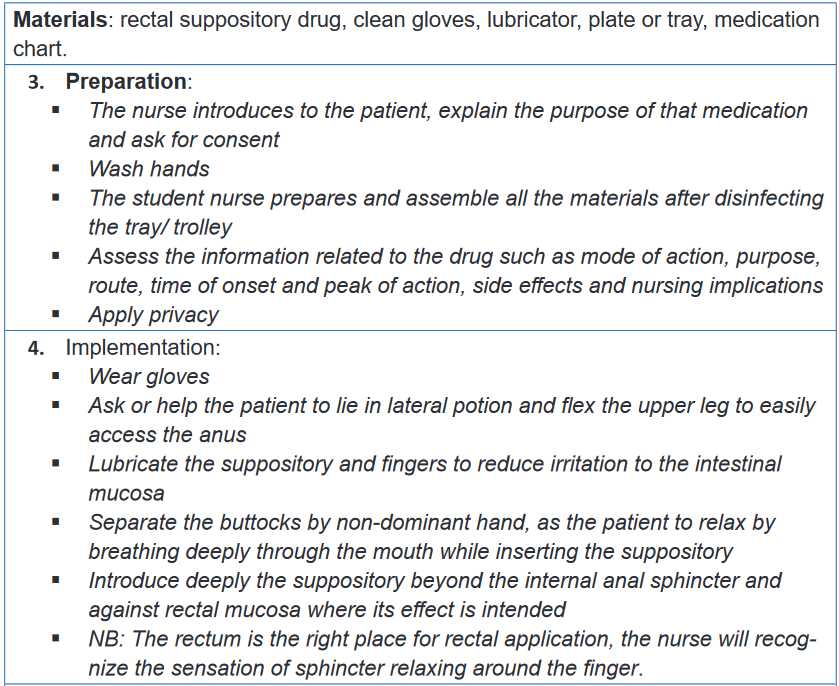
Self-assessment 5.2.
1) Illustrates the disadvantages of buccal route of drug administration?
2) What happen when a drug designated to sublingual administration is
accidentally swallowed?
3) What are the precautional measures a nurse will teach a patient who is
taking medication in sublingual?
a) Precise the location of a drug in buccal route of medication
administration
4) Where do we exactly dispose a suppository drug using rectal route5) Administration way which is least expensive, using little equipment,
and minimal training is the
a) Oral route
b) Skin application
c) Vaginal application
d) Intradermal route
6) Why will you choose to administer medication in oral route?
7) List the disadvantages of oral route of drug administration
8) Patient KANEZA is hospitalized for 3 days under treatments including
suppository, while an associate nurse going to administer the medication
found the patient has a diarrhoea. What can you do to help this patient
taking his medication as an associate nurse? Tell us the best route to
be used to treat this patient among the routes we already covered?5.3. Parenteral route- Intramuscular (IM)
Learning Activity 5.3.
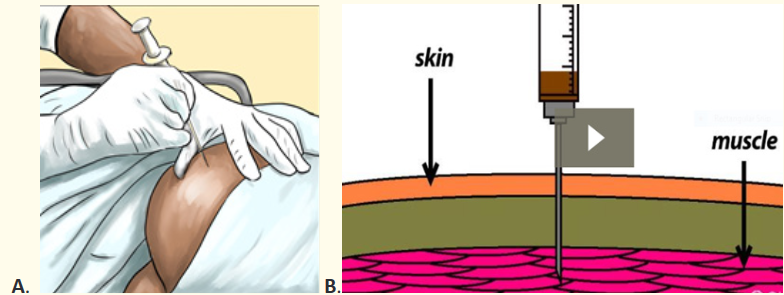
Observe the images above (A and B) and answer the following questions:
1) Talk about what a person with gloved hands is doing?
2) What is the relationship and differences between image A and B?
3) Which materials are being used on image ADepending the form of medication or patient’s conditions, different routes of drug
administration can be applied including parenteral route. Parenteral route of
drug administration is a way to administer medication in form of solution into the
body using injection to attain rapid systemic effect. It can also be injected in a
localized organ or tissue in order to achieve high concentration in the site of action
or minimize systemic effect. When selecting an injection site, avoid the area with
skin abnormalities (e.g: scar tissue, birth marks, tumor) or at bony prominences.
The intramuscular route is one of parenteral routes which is a method of installing
medications via injection into the depth of the bulk of specifically selected muscles.
The common sites for IM injection are ventrogluteal, dorsogluteal, vastus lateralis
and deltoid muscle. The basis of this process is that the large muscles have good
vascularity, and therefore the injected drug quickly reaches the systemic circulation
and thereafter into the specific region of action, bypassing the first-pass metabolism.Always remember to select safe site away from large nerves, bones and blood
vessels. Failure to do so may be the origin of different complications such as
abscess, necrosis, nerve injuries, lingering pain and periostitis. The amount of 4 ml
is considered the maximum dose in a single site for adults in the developed muscle.
IM is commonly indicated for patients who are noncompliant, uncooperative,
reluctant, and unable to receive drugs through other commonly utilized routes.It is contraindicated to use IM in case of active infection such as cellulitis or
dermatitis at the site of administration. Acute myocardial infarction- the release
of muscle enzymes may provide a confounding bias in making the diagnosis. In
case of thrombocytopenia, coagulation defects, hypovolemic shock which cause
reduced absorption of the drug due to poor perfusion of that muscle. Myopathies
and associated muscular atrophy delay drug absorption as well as adds up the risk
of neurovascular injuries.The advantages of IM route are based on its rapid and uniform absorption of the
drug, especially those of the aqueous solutions. It has a rapid onset of the action
compared to that of the oral and the subcutaneous routes. IM injection avoids the
first-pass metabolism as well as gastric factors governing the drug absorption. Has
efficacy and potency comparable to that of the intravenous drug delivery system,
highly effective in emergency scenarios such as acute psychosis and status
epilepticus. A large volume of the drug can be administered compared to that of the
subcutaneous route.The disadvantages of IM route is that the administration of medications require
a trained personnel. The absorption of the drug is determined by the bulk of the
muscle and its vascularity. It is not a best option during emergency. IM injection
at the appropriate landmarks may be difficult in a child as well as in patients
requiring physical restrain. Inadvertent injection in the subcutaneous plane of the
fascia can lead to delayed action of the drug. It is painful, can lead to anxiety inthe patient, especially in children. Self-administration of the drug can be difficult.
The precipitation of the drug following faster absorption of the solvent may lead to
delayed and prolonged action of the drug. Unintended prolonged sequelae following
delayed drug release from the muscular compartment.Common complications IM injection can be summarized as muscle fibrosis and
contracture, abscess at the injection site, gangrene, nerve injury -the sciatic nerve in
gluteal injection, the femoral nerve in vastus lateralis injection, the superior gluteal
nerve in dorso gluteal injection and radial nerve in deltoid injection, periostitis,
transmission of HIV, hepatitis virus when sharing the needle and persistent pain at
the site of injection.5.3.1. Anatomical landmarks in IM injection
There are specific landmarks to be taken into consideration while giving IM injections
so as to avoid any neurovascular injuries. The specific landmarks for the most
commonly used sites are discussed below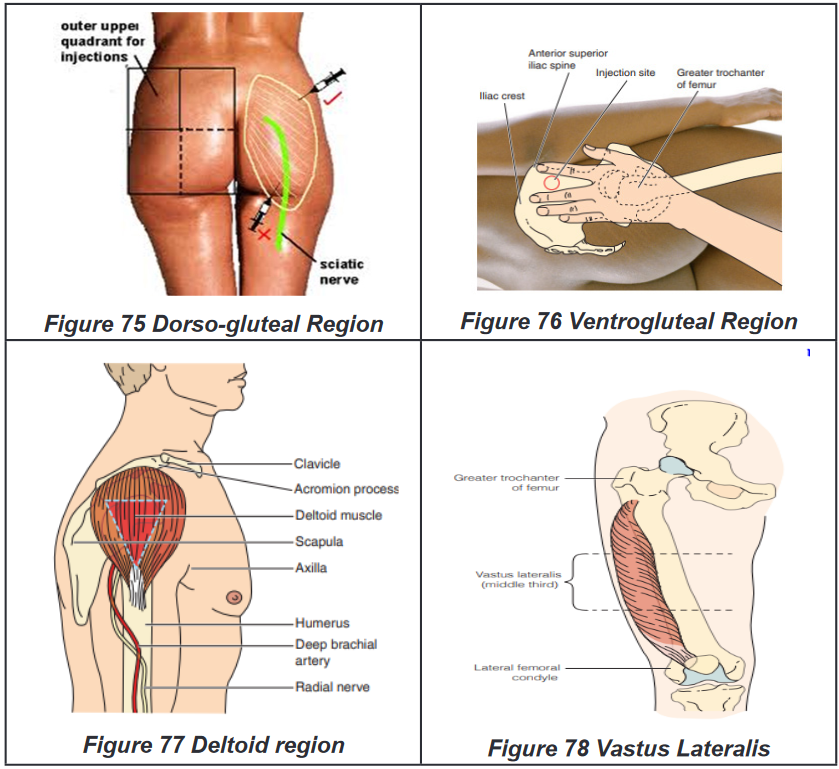
BOX 5.3.1.
• The dorso-gluteal site is upper outer quadrant of each buttock
• The deltoid site is 2.5 to 5 cm below the acromion process
• During the ventrogluteal site location, the heel of the opposing hand is
placed in the greater trochanter, the index finger in the anterior superior
iliac spine, and the middle finger below the iliac crest. The drug is injected
into the triangle formed by the index, middle finger, and the iliac crest
• The vastus lateralis site is the middle third of the line joining the greater
trochanter of the femur and the lateral femoral condyle of the knee.5.3.2. Intramuscular (IM) injection technique
Materials: sterile syringes and needles, alcohol-based antiseptic solution, drug,
medication chart, dry cotton swab, safety box, disposable gloves, dustbin, trolley,
plate.1. Preparation:
Introduce yourself to the patient including your name and role
Confirm the patient’s name and date of birth
Briefly explain the procedure, indication of the drug using patient-friendly
language
Gain consent to proceed with intramuscular injection
Check for any contraindications to performing an intramuscular injection
Check if the patient has any allergies
Ask if the patient has a preferred injection site. If the patient is receiving regular
intramuscular injections, ensure that the injection sites are rotated
Position the patient so that they are sitting or lying comfortably according to
selected site
Wash your hands
Gather equipment
Do final checks/ rights of drug administration:
Right patient: ask the patient to confirm their details and then compare this to
the patient’s wrist band (if present) and the prescription
Right drug: check the labelled drug against the prescription and ensure the
medication hasn’t expired
Right dose: check the drug dose against the prescription to ensure it is correct
Right time: confirm the appropriate time to be administering the medication and
check when the patient had previous doses if relevant
Right route: check that the planned route is appropriate for the medication you
are administering
Right to refuse: ensure that valid consent has been gained prior to medication
administration
Right assessment: ensure all the precautions are examined before administer
any medication2. Implementation:
Wash and dry your hands or use hand rub
Wear gloves and an apron
Draw-up the appropriate medication into the syringe using a drawing-up needle
Remove the air bubbles from the syringe
Remove the drawing-up needle and immediately dispose of it into a sharps bin,
then attach the needle to be used for performing the injection
Choose an appropriate site for the injection
Position the patient to provide optimal access to your chosen site
Clean the site
Gently place traction on the skin with your non-dominant hand away from the in-
jection site, continuing the traction until the needle has been removed from the
skin. If the patient is elderly with reduced muscle mass or the patient is emaciat-
ed, do not apply traction, instead, bunch the muscle up to ensure adequate bulk
before injecting.
Warn the patient of a sharp scratch
Holding the syringe like a projectile in your dominant hand, pierce the skin at a
90° angle.
Insert the needle quickly and firmly, leaving approximately one-third of the shaft
exposed (however this varies between sites and patients).
Aspirate to check if the needle is not in a blood vessel
If aspiration does not reveal blood (evidence of intravascular needle placement)
inject the contents of the syringe whilst holding the barrel firmly.
If the aspiration reveal blood into syringe (this is a sign of intravascular injec-
tion), do not inject medication, remove syringe and needle immediately, discard
it with contained medication and start over with anew medication.
Inject the medication slowly at a rate of approximately 1ml every 10 seconds.
Remove the needle and immediately dispose of it into a safety box
Release the traction you were applying to the skin
Apply gentle pressure over the injection site with a cotton swab or gauze. Do
not rub the site.
Discard the gauze3. Finishing:
Offer a comfortable position and arrange patient’s environment
Explain to the patient that the procedure is now complete
Thank the patient for their time
Remove of your gloves and equipment into an appropriate clinical dustbin
Arrange used materials
Wash your hands
Document the details of the procedure and the medication administered
Evaluate the client response to the medication within time flame.Self-assessment 5.3.
1) What are the advantages and disadvantages of intramuscular injection?
2) List the commonly used sites for intramuscular injection
3) List the commonly used sites for intramuscular injection
4) KALISA a 39-year-old man is admitted in surgical ward following road
traffic accident. He is still complaining about pain even though he received
diclofenac 100mg suppository every 12 hours 1gr Paracetamol tablets
every 8 hours. As an associate nurse, which route would you propose
to bring a quick control on patient’s pain? Explain why of the proposed
route.5.4. Parenteral route-Subcutaneous (SC)
Learning activity 5.4.
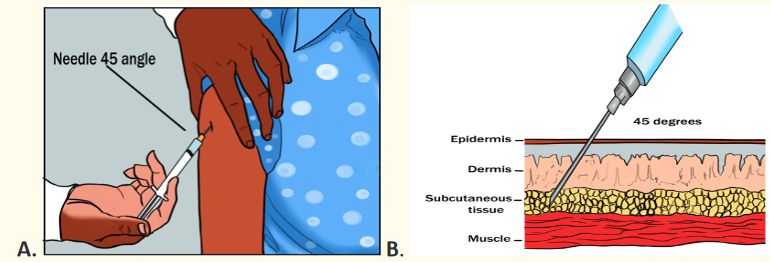
Observe the image above (A and B) and answer the following questions:
1) Describe the action which is being done on the image A
2) What is the meaning of 450C degrees on both image A and B
3) What are the advantages and disadvantages of the action on the image ASubcutaneous route of drug administration is another parenteral way of drug
administration. It consists of deposits the medication into the subcutaneous layer
below the skin and above the muscle layer. The drug to be used must be isotonic
and must be the same pH as the tissue in order to prevent irritation and tissue
damage. There are different sites of subcutaneous injection as illustrated on the
picture below: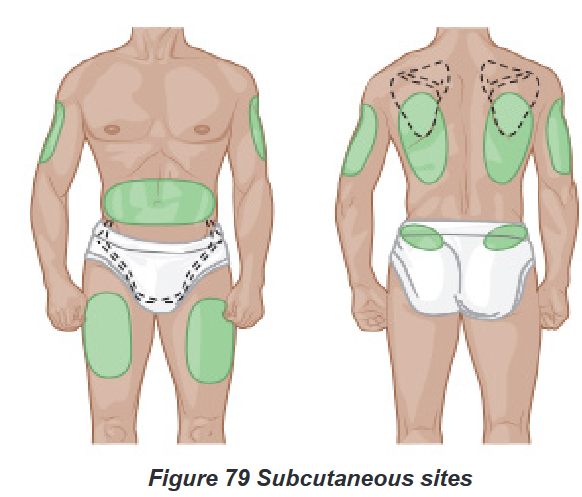
The sites for subcutaneous injection are the following: The back of the upper arms,
the abdomen (but stay a minimum of 5cm away from the umbilicus), the anterior
thighs, the area of the back just below the scapulae and the upper buttocks.SC is indicated when slow and continuous absorption is required and long duration
of action. E.g. Insulin, heparin. It is contraindicated in case of edema or inflammation
at the planned site of injection, shock and peripheral hypoperfusion (because it can
impair absorption), and when patients refusing consent to the procedure. It serves
to provide complete drug absorption. It is less invasive than intramuscular as it
ends up in the subcutaneous tissues. It is also possible to train the patient for self-
administration especially if he or she is taking lifelong medication. E.g: insulin.SC route has some disadvantages as it is expensive than oral route as it involves
some degree of education and materials. On the other hand, it is slower than
intramuscular injection. The procedure of SC injection breaks the skin barrier, causes
pain, can irritate tissues and may be a source of anxiety. SC drug administration
is applicable for limited quantities of medications not exceeding 1.5 to 2 ml, the
greater amount will cause pain.
Procedural stepsMaterials
To perform SC injection, there is a need of different equipment such as needles
and syringe, drug for administration, medicines administration prescription, tray to
carry the drug, sharps container, alcohol swab or cotton and disinfectant1. Preparation:
Introduce yourself to the patient including your name and role
Confirm the patient’s name and date of birth
Briefly explain the procedure, indication of the drug using patient-friendly
language
Gain consent to proceed with intramuscular injection
Check for any contraindications to performing an intramuscular injection
Apply folded screen around the bed patient to ensure privacy during the
procedure.
Check whether the patient has any allergies.
Check if the prescription is correct and follow the rights of medicines admin-
istration
Wash and dry hands to reduce the risk of infection.
Assemble the syringe and needle and then draw the required amount of
drug from the ampoule. Some drugs are available in pre-filled syringes and
manufacturer’s instructions should be followed, example enoxaparin.
Remove any air bubbles from the syringe.
Change the needle to ensure that the one you are about to use for injecting
the drug is sharp, thereby reducing pain.
Dispose of the needle used to draw the drug in a sharps container according
to local policy and apply a new one.
Place the injection in a tray and take it to the patient, along with a sharps bin
so the used needle can be disposed of immediately after the procedure.
Position the patient comfortably with the selected injection site exposed.
Check the site for signs of oedema, infection or skin lesions. If any of these
are present, select a different site.
Wash and dry hands or rub the hands
Put gloves on4. Implementation:
Disinfect the skin with alcohol swab.
Inform the patient that you are going to carry out the injection. Use distrac-
tion and relaxation techniques to reduce anxiety if needed.
Hold the syringe and needle in your dominant hand and pinch the skin
together using the non-dominant hand to lift the tissue away from underlying
muscle
Insert the needle at the required angle 450 degree or 900 degrees for the
obese patients to ensure that you inject medication in subcutaneous tissue.
Aspiration to check whether the needle is not in a blood vessel, if so, re-
move the needle and discard both the needle and syringe then prepare a
new medication.
If no blood appears, inject the drug slowly over 10-30 seconds
Massage the area gently with a swab but don’t massage after insulin and
heparin SC injections (massage heparin injection after SC foster bruising
whereas it speeds up the absorption of insulin)
Release the lifted skinfold5. Finishing:
Dispose of sharps directly into the sharps bin and dispose of the syringe
according to local policy.
Ensure the patient is comfortable and wash hands.
Record administration on the prescription chart. Also record administration
site so that the same site is not repeatedly used. This is to avoid lipohyper-
trophy.
Monitor the patient for any effects of the prescribed medicine and any prob-
lems with the injection site.
Patients receiving injection in a health center or outpatient department may
need to wait for a period of time to monitor for any reaction to the drug. Lo-
cal policies should be followed.Self-assessment 5.4.
1) Dr. MUTESI writes a prescription for 5mg of morphine in SC every 12
hours. The medication is available in a concentration of 10 mg per 2ml
a) Describe the commonly used sites for subcutaneous injections?
b) What is the rational to inject at 45 degrees in subcutaneous
injection?
2) MUKASINE a 78-year-old woman needs a SC injection of anti-tetanic
vaccine. You realize that she is having generalized edema. What will do
in this situation?5.5. Parenteral route- Intradermal (ID)
Learning activity 5.5.
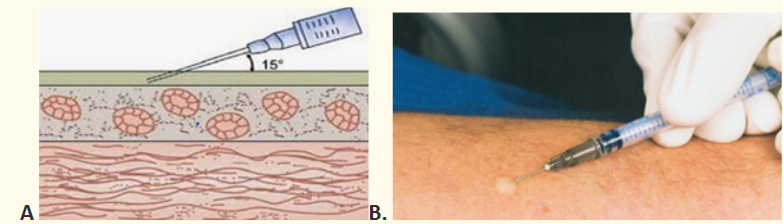
Look carefully the image posted here and respond related questions.
1) What do you see on the site of injection in picture B?
2) What is the relationship between image A and B.
3) Why is the angle of 150 appliedAnother parenteral route of drug administration is the intradermal (ID) route. ID is
the administration of a drug into the dermal layer of the skin just under the epidermis.
ID is indicated frequently for allergy testing before administering larger amounts
of drug by other routes or in case of tuberculosis vaccination and screening. The
advantage of these tests is that the body reaction is easy to visualize, and the
degree of reaction can be assessed. Before using this route choose an injection
site that is free from lesions, rashes, moles, or scars, which may alter the visual
inspection of the test results. Once the ID injection is completed, a bleb (small
blister) should appear under the skin. Its disadvantages are based on the longest
absorption time of all parenteral routes. The procedure is usually painful, so make
sure that the needle is inserted into the epidermis at an angle of 10 to 15 degrees
and not into enter the subcutaneous to reduce patient discomfort. To make the
intradermal injection, we need materials such as sterile syringes and needles
specific for ID, alcohol-based antiseptic solution, drug, medication chart, dry cotton
swab, safety box, disposable gloves, dustbin, trolley, plate.Intradermal procedure
Gather all the equipment needed and check the physician order
Explain the procedure to the patient, the purpose, site for injection, and how he/
she has to cooperate.
Wash hands and wear disposable gloves
Prepare medication from ampule or vial.
Position the patient and select the inner aspect of the forearm, upper chest, or
upper back beneath scapulae that is not very hyperpigmented or covered with
hair.
Cleanse the site with an alcohol swab in a circular motion moving outward.
Allow skin to dry. Keep cotton in the clean tray for reuse when taking out the
needle.
Remove the needle cap with the non-dominant hand by pulling it straight off.
Use the non -dominant hand to spread skin taut over the injection site.
Place the needle almost flat against the patient’s skin. Insert 0.4cm bevel up so
that needle can be seen through the skin.
Slowly inject the drug (0.01ml-0.1ml do not exceed 0.5ml) watching for a bleb
to develop (appearance of the bleb indicates that the needle is in intradermal
tissue). If not, remove the needle and restart.
Withdraw the needle quickly at the same angle as it was inserted
Do not massage the area.
Do not recap the needle. Discard syringe and needle into the appropriate recep-
tacle
Thank the patient and arrange his or her environment
Offer appropriate health education
Remove glove and wash hands.
Record the medication administration-the medication administered, amount,
dose, site, and patients’ response
Draw a circle using blue/black pen around the injection site. Write the date and
time of administration of medication.
Check the reaction within a specified interval of time; usually, it depends on the
hospital protocols.
Inform the physician of a medication reaction.Self-assessment 5.5.
1) Intradermal injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 900
2) What will indicate you that you successful injected a drug in intradermal
route?
3) Associate nurse M. is going to administer a small dose of penicillin to a
patient to test for hypersensitivity or allergy on that drug. Which route will
M. use? What is the maximum dose not to be exceeded is?5.6. Topical skin application
Learning activity 5.6.

) What this image shows to you
2) When is skin medication indicated?
3) Discuss on the side effect which may originate from skin medication
application?Sometimes the location of a disease may dictate the route of drug administration.
The outermost body parts are treated by using topical route of drug administration.
The topical route of drug administration involves applying a drug to the skin
or mucous membranes for example in the eye, external ear canal, nose andvagina. They are typically used for their action at one specific site. They usually act
locally, but they may have systemic effects. The frequency of delivery of the drug
is controlled and depends up the type of the prescribed drug and instructions from
the manufacturer.Topical dermatological preparations are in different forms such as ointment,
lotions, creams, powders, pastes, sprays and patches. The lotions, ointment and
creams are used to manage skin diseases localized on the specific area of the
skin. Lotion such as skin moisturizers prevent the complication linked to excessive
dry skin. This is the application of the drug to the desired area of the skin which
will serve as route of absorption. The ointment such zinc oxide when applied on
the skin, it protects against abrasion or moisture associated with bowel or bladder
incontinence. Patches as a form of transdermal medication which are designed to
be applied on the skin and then penetrate it to generate systematic effect. Patches
may last between 24 to 72 hours. Nitroglycerine and nicotine are the commonly
used patches. This route has fewer risks to gastro intestinal system, fewer risks
of abuse and easy to administer. In some case the drug can be sufficient enough
to enter systemic circulation and produce unwanted side effects. During the use
of topical medication there is a risk to potential production of irritant and allergic
contact dermatitis, potential rapid appearance of bacterial resistance and potential
alteration of cutaneous flora. Before application of skin preparation, we need to wash
it with water and soap then dry it throughout. The skin scurf and previous applied
medication can hinder the effective drug application and absorption. Remember to
wear gloves before application of medication on the skin and respect asepsis when
handling open skin area.To apply the medication on the skin we need the drug dedicated for skin, gloves,
some gauze, plate or trolly. In case of powder application make sure the skin
surface is dry. Spread apart any skin folds and apply the powder until the area
is covered with a fine thin layer. Cover the site with a dressing if ordered. For
suspension-based lotion, shake the container before use to distribute evenly
suspended particles. Put a little lotion on a small gauze dressing or pad and apply
the lotion to the skin by stroking it evenly in the direction of the hair growth. Rub the
lotion on the skin until it is no longer visible. For creams, ointments, pastes and
oil-based lotions: Warm and soften the preparation in gloved hands to make it
easier to apply. Spread over the affected skin evenly using long strokes that follow
the direction of the hair growth. Explain that the skin may feel somewhat greasy
after application. Apply a sterile dressing if ordered by the doctor.To apply transdermal patches, select a clean, dry area that is free of hair and
matches the manufacturer’s recommendations. Remove the patch from its
protective covering, holding it without touching the adhesive edges, and apply it by
pressing firmly with the palm of the hand for about 10 seconds. Advise the person
to avoid using a heating pad over the area to prevent an increase in circulation
and the rate of absorption same as when the patient has fever greater than 400c.
Remove the patch at the appropriate time, folding the medicated side to the inside
so it is covered. Remember to rotate the sites. Write date, time and your initials on
the patch guide your colleagues to take appropriate follow up care.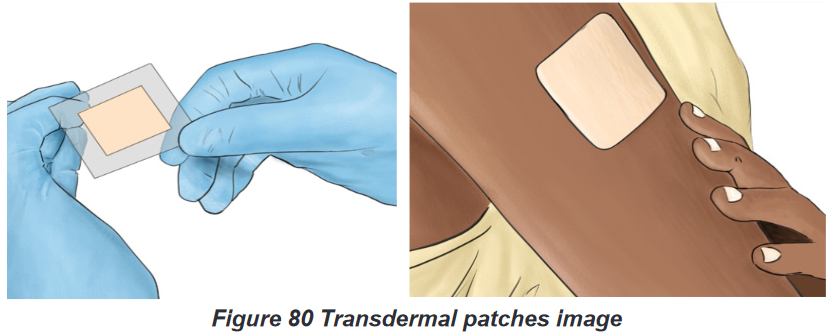
Self-assessment 5.6.
1) Before applying a powder medication, what are nursing consideration to
be respected?
2) Give different forms of skin application medication
3) Patient Y. consult for skin disorder and Dr prescribes a skin application
medication in form of cream to be applied twice a day. As an associate
nurse, give to Yvan the precautions to guide him to remove the patch.5.7. Eye medication administration
Learning activity 5.7.
Observe the image on the left and reply to these questions:
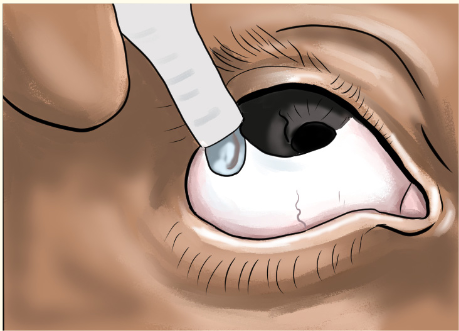
1) What this image indicates to you
2) Why is this action done?
3) Which safe measures will apply to make this activity?Medications become effective when they reach their site of action. Therefore, different
route of drug administration are used to reach the exact site of action. Ocular route
of drug administration is designed to treat eye diseases. Drugs administered to
the eye are in the form of drops or ointments and usually introduced into the lower
conjunctival sac. Eye medications may be ordered to lubricate the eye, to prevent
or treat conditions such as infection, inflammation or glaucoma or for diagnostic
purposes. E.g: of eye medications include gentamicin for bacterial infection such as
conjunctivitis, prednisolone for inflammation and timolol for glaucoma.The advantages of ocular route are that it offers direct application to the site of
action in higher concentration than when taken by other routes. It involves quicker
drug absorption and less systemic effect. It is also suitable to all type of patient as
well as easier for self-administration. The disadvantages quick elimination of drug
through tear and blink. Application of eye ointment may cause blurring vision. Few
drugs are in ocular form, they are also expensive than oral medication.BOX 5.7.
• Always remember to wash hands and if necessary, wear glove before
administer eye medications and follow other prescribers’ instructions.
• In some situations, the drug that is administered for a local effect may
be absorbed into the bloodstream and cause unwanted systemic effects.
To prevent this, after administration of the eyedrops, press your gloved
fingertip gently against the lacrimal ducts on either side of the nose for a
few secondsEye drugs are primarily in form of ointment and drops. Their administration methods
are different to ensure that they reach the maximum surface.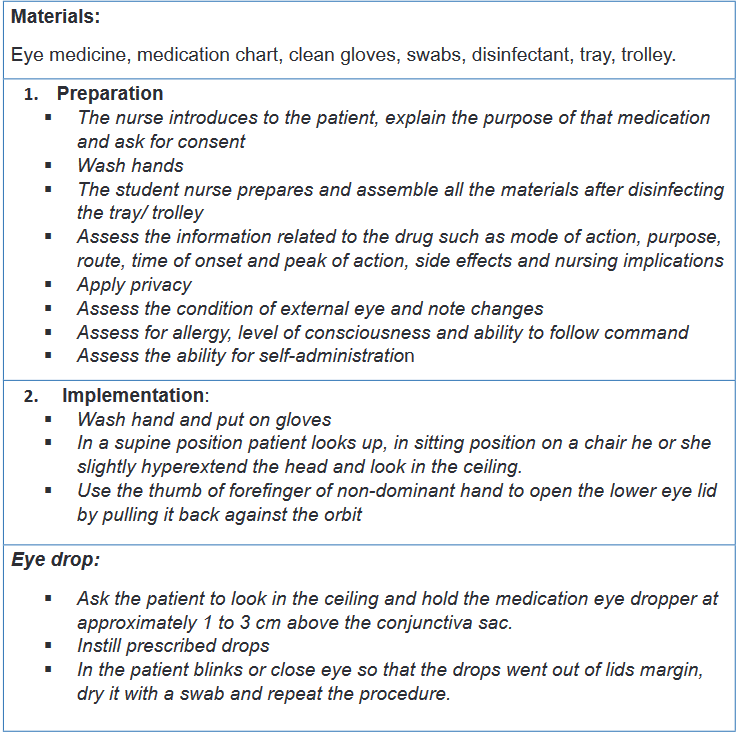
Self-assessment 5.7.
1) Explain the advantages and disadvantages eye medication administration
2) When is eye medication instillation indicated?
3) Patient K. consult for redness of the eyes and Dr prescribe an eye
ointment to be applied twice a day. As an associate nurse, give to K. the
precautions to be followed before and during medication application.5.8. Ear medications administration
Learning activity 5.8.
Look at the picture here attached and answer the given questions

1) What is this person doing
2) What do you think should the best way to instill ear drop?
3) Educate a patient whose ear drop prescription is to be taken at homeDrugs administered in the ear are in the form of drops. These drugs may be used
to soften cerumen, relieve pain, treat infection or inflammation, or facilitate removal
of a foreign body, such as an insect or a small object. It is important to control
local problems found in the ear. Its disadvantages are based difficulties for self-
administration as well as time consuming because the patient remain in a position
for a while.To instill eardrops, position the patient lying on his or her side with the affected ear
up. For adults and children older than 3 years of age, gently pull the pinna up and
back. For children younger than 3 years of age, pull the pinna down and back. This
helps straighten the ear canal, which allows the drops to penetrate to the middle
ear. Orients the dropper so that the medication drops rolls down the wall of the
canal and does not drop directly onto the tympanic membrane, which would cause
pain.Ask the patient to remain with his or her head positioned with the affected ear
up for at least 2 minutes. A cotton ball can be placed loosely in the ear to absorb
excess medication. It is advisable to avoid touching the dropper to the surface of
the ear to prevent the introduction of pathogens into the bottle of ear medication.
Before eardrops administration, make sure that tympanic membrane is intact. If in
doubt, ensure that the tympanic membrane has been examined with an otoscope
by a healthcare professional prior to administering the medication. Here is a list of
materials to be used to apply ear drug: ear medicine, ear dropper, medication chart,
clean gloves, swabs, disinfectant, trolley or plate.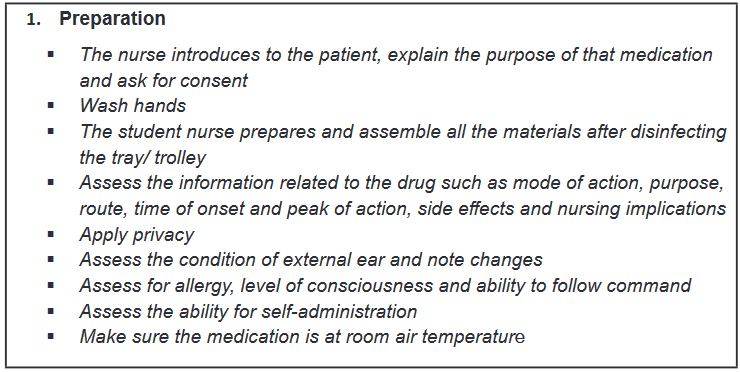
Self-assessment 5.8.
1) Proper administration of an ear medication to a 2-year-old person
includes which of the following?
a) Pull the ear straight back
b) Pull the ear down and back
c) Pull the ear up and back
d) Pull the ear straight upwards
2) Describe the indications of ear medication instillation.
3) What are the disadvantages of ear drop?
4) Patient B. age 10 years old, consult the health center for right ear pain,
as an associate nurse what do you think the doctor can pay attention to,
before prescribing an ear drops?5.9. Nasal route of drug administration
Learning activity 5.9.
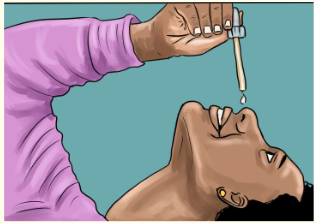
Look carefully the image posted here and respond related questions.
1) Where does this medication instilled?
2) Think on the importance of this route of drug administrationNasal route consists of drugs administration via the nasal mucosa. Some
medications are administered for local effects on the nasal mucosa other are given
for systemic effects and are simply absorbed through the nasal mucosa. Nasal
medications are administered to reduce inflammation, facilitate drainage, or treat
infections in the nasal cavity. Nasal route is contraindicated for patients with recent
radiation to the head and neck, high risk for serious bleeding due to tumour, history
of coagulopathy disorder.The advantages of easily administered and generally well tolerated, rapid onset
because medications are directly absorbed through the nasal mucosa into systemic
circulation. There is higher bioavailability than oral medications as first pass hepatic
metabolism is bypassed, may escape the blood-brain barrier through olfactory
region of the central nervous system. Provides alternate route for rapid medication
delivery when IV access is unavailable like in case of seizure or if there is a high risk
of needle-stick injury. Nasal drug administration is limited to very small volumes due
to relatively small area available for absorption. It only applicable to potent drugs
with high water solubility. It is not suitable for drugs that are irritating or injurious
to the nasal mucosa in addition to disease conditions of the nose may result in
impaired absorption. Instilling a drug into a blocked nose or a nose with watery
rhinorrhea may expel the medication from the nose. Chronic applications may lead
to more serious toxicity issues and may ultimately damage the cilia and compromise
body’s defenses. If long-term use continues, the arteries in the nasal passage will
shrink and scar, causing lesions and nosebleeds.Procedure of ear route drug administration
To perform the ear medication, we need materials such as medication in its
container, clean dropper, facial tissue, small pillow, wash cloth.
Self-assessment 5.9.
1) Explain the advantages and disadvantages nasal medication
administration.
2) When is nasal medication instillation indicated?
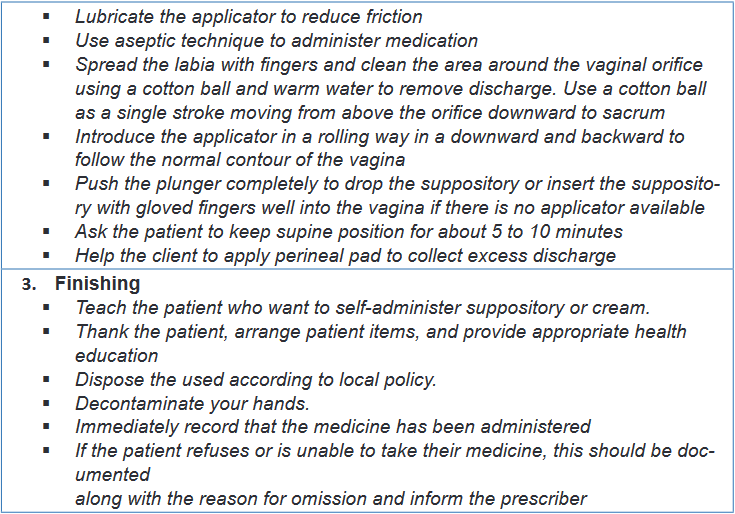
3) When is nasal medication instillation indicated?5.10. Vaginal route of drug administration
Learning activity 5.10.
Observe the images above the work on the following questions:
1) What do you see introduced in the female genitalia?
2) Why is it important to introduce drug in female genitalia?
3) Which kind of medicines used in female genitalia?Healthy vaginal has many non-pathogenic organisms than pathogenic ones. This
ratio protects the vaginal from invasion by pathogenic organisms in addition to the
acidic vaginal secretion also protect the vagina from microbial invasion. There may
be an imbalance in the above protective mechanism which originate results into
diseases to be managed vaginal drugs.Vaginal drug administration indicates the administration of medications within the
vaginal cavity to produce local or less frequently, systemic pharmacological effects.
Medications administered via the vaginal route come in the form of suppositories,
creams, aerosol foams, or tablets that are inserted into the vagina and dissolve
there to treat infection or to relieve discomfort. Vaginal administration is indicated
to treat local infections such as yeast infections, vaginitis, endometrial atrophy,
labor induction and contraception with spermicidal agents.This route offers a number of benefits over other routes of drug delivery including
avoidance of hepatic first-pass effect because absorbed drugs penetrate directly
to the systemic circulation via the inferior vena cava thus prevent hepatic toxicity
induced by some drugs. It is an easier route of administration and possible
self-insertion and removal of the dosage form. This route limits the side effects
associated with oral route such unpleasant taste, nausea and so on as well as
parental routes associated inconvenience due to pain, tissue damage, and possible
risk of infection.However vaginal route has some disadvantages like gender specificity, patient
incompliance, some drugs can cause vaginal irritation. Only a few drugs are
administered by this route. Drug absorption may be affected by menstrual cycle,
menopause, pregnancy and sexual intercourse. It affects personal hygiene due to
some medication leakage and some drugs can be inactive due to vaginal pH. Some
preparations come with a disposable tubular applicator for insertion others are just
inserted by index and thumb fingers. Medical aseptic technique is usually used
during this procedure. Suppositories are designed to melt at body temperature, so
they are generally stored in the refrigerator to keep them firm for insertion.Procedure of vaginal administration
The following materials are needed to perform vaginal drug administration; vaginal
suppository, cream or tablets, applicator (if needed), clean gloves, tower, perineal
pad, lubricant, bedpan, medication chart.
Self-assessment 5.10.
1) Explain the advantages and disadvantages vaginal administration.
2) When is vaginal medication indicated?
3) Patient C. has vaginal affection which require self-insertion of vaginal
suppository as treatment, as an associated explain her the procedure
she will follow.5.11. Drug dose calculation
Learning activity 5.11.
4) Dr. R. orders amoxicillin syrup 500 mg per feeding tube every 6 hours.
The available bottle of amoxicillin is labeled 250 mg per 5 ml.
How many milliliters needed to provide the prescribed dose of 500mg?
Calculate a daily dose for this patient.5) The prescription indicates 1000 milligrams (gm) of Erythromycin while
the available tablets are of 500gm per a tablet. How many tablets are
needed to meet the prescribed dose of 1000gm of Erythromycine?Nurses must be able to calculate the dose of medications so that the right dose is
appropriately provided to the patient. The dose of medication available to you may
be different from what the prescriber ordered. If the available medication is in a
different dose than what is ordered, you must calculate how much of the available
medication to administer to your patient. For tablets it is a matter of adding or
dividing tablets to meet the desired dose whereas for the capsule we add to get the
exact dose. For liquid medication, we calculate the amount of the drug dissolved in
liquid, expressed as milligrams per milliliter (mg/mL). You will then be required to
calculate how many milliliters of liquid to administer to give the desired milligrams
of medication. In this unit, we are going to study how to calculate the dose of
medications of different forms such as tablets, capsules, liquid forms including
injectable ones.To be able to calculate the drug dose, we have to know the abbreviations used
in drug prescription in addition to units converting process. We are going to see
the commonly used abbreviations in combination with conversion measures. It is
advisable from students to make sure what she or he is reading is correct or ask
clarification in case of confusing abbreviations to mitigate medication errors.BOX 5.11.
• To convert larger units to the smaller ones, requires to multiply.
Kiligrams (Kg)to Grams (g)=Kg×1000
Kilograms (kg) to grams(g)= Kg×1000
Grams to milligrams (mg) =g × 1000
Milligrams to micrograms (mcg) = mg ×1000
Liters(L) to milliliters(ml)= L ×1000
• To convert the smaller units to the larger ones, we divide.
Grams to kilograms = g/ 1000
Milligrams to grams = mg/1000
Microgram to milligrams = mcg/1000
Milliliters to liters = ml/100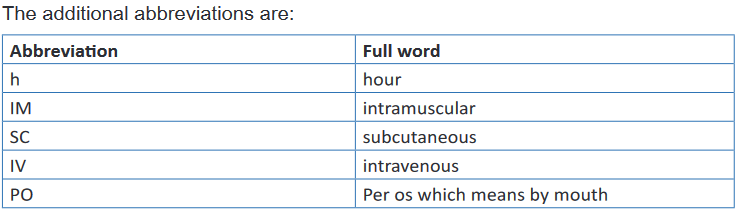
Many ways of dose calculation are acceptable as their result into exact responses.
The calculations use simple mathematic formula which nurse need to be aware off
to ensure correct dose is ready for administration. It is necessary for students and
novice nurses to get guidance while performing dose calculation avoid confusion
and error which may arise leading medication error. To be able to find the dose to
administer (), we need the dose we have on hand () or the dose available, the dose
that is ordered by the prescriber () and () stands for the vehicle, which is either a
tablet or liquid.The first fraction is: H/V=D/x
The next step is to cross multiply: HX = VD
Now x equals to: X= DV/H = (Dose prescribed*vehicle)/(Dose in hand )
Example 1: The ophthalmologic officer MUGISHA orders 200 mg of Ibuprofen,
and 50 mg tablets are available, how many tablets should be given to the patient?
We know that 50 mg = 1 tablet,
We need 200 mg in an unknown number of tablets.
Step one: Set up a fraction operation: 50mg/(1 tab)=200mg/(x )
Step two: Do cross multiplication 50 mg * X= 1 tab *20 mg
Step three for ‘’x’’: X tab= (1tab * 200mg)/(50 mg )= 4 tabThe nurse needs four tablets to administer 200mg of ibuprofen using 50mg tablets.
Using simple explanation of this equation, the dose to administer equals the dose
we want times what is in over the dose we have.Here is a typical example:
Prescription states 200mg (milligrams)
You have an ampoule of 500mg (milligrams) in 4ml (millilitres).
What volume contains the dose you need?
H/V=D/x gives us; 500/(4 )=200/x; 500X=200*4; 500x= 800; x=800/500; x= 1.6It means that we need 1.6ml to be able to administer 200mg of the prescribed drug.
Self-assessment 5.11
1) Mrs. B have been prescribed the following medication: Cloxacillin 500mg
to be given 3 times a day for 7 days and Ibuprofen 400mg to be given
2 times a day for 3 days. The available cloxacillin in health center’s
pharmacy has 500mg per capsule while ibuprofen is 200mg per tablet
a) Calculate the daily and total dose of cloxacillin for Benitha
b) Calculate the daily dose and total dose of Ibuprofen for Benitha2) Dr. I. writes a prescription for 25 mg of morphine in SC every 12 hours.
The medication is available in a concentration of 100 mg per ml. How
many ml will the nurse administer to meet the prescribed dose?End unit assessment 5.
1) Select the right of medication administration among the following
concepts:
a. Patient file
b. Concentration
c. Route
d. Thermometer2) Proper administration of an ear medication to a 2-year old person
includes which of the following?
a. Pull the ear straight back.
b. Pull the ear down and back.
c. Pull the ear up and back.
d. Pull the ear straight upwards.3) The administration route for a drug injected just beneath the top layer
of the skin is called:
a) Intradermal
b) Subcutaneous
c) Vaginal application
d) Transdermal application4) The drug administration route where the needle is inserted at 45 degrees is:
a) Intradermal
b) Subcutaneous
c) Intramuscular
d) Sublingual5) If blood appears in the syringe when the plunger is pulled back during
subcutaneous and intramuscular injections the nurse should
a) Inject drug
b) Inject drug followed by a small amount of bubble air
c) Insert needle one cm further
d) Start over with new syringe
e) Ignore it because the presence of blood has no significance6) Drug administration way which is least expensive, using little equipment,
and minimal training is the:
a) Enteral route
b) Skin application
c) Vaginal application
d) Intradermal route7) Intramuscular injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 9008) Hand Hygiene is a part of standard precautions before any nursing
procedure
a) True
b) False9) Intradermal injections should be administered at a ___ degree angle
a) 10-150
b) 250
c) 450
d) 90010) How much medication can the nurse safely administer into the deltoid
muscle?
a) 4 ml
b) 1-2 mL
c) 10 ml
d) 2-3 mL11) When giving injections in the buttocks the nurse must properly identify
appropriate land marks to prevent damage to the ___
a) Sciatic nerve
b) Spinal cord
c) Coccyx
d) Atlas12) Nurse Carine has completed giving Ms. Smith her injection. Which
method is the BEST method for Nurse Carine to use to dispose of the
needle after giving the injection?
a. Nurse Carine should sit the needle on the bedside table and make
sure she disposes of the needle before she leaves the room.
b. Nurse Carine should immediately discard used needle in the nearest
sharps container.
c. Nurse Carine should discard needle when she completes the
injection.
d. Nurse Carine should recap needle and place into the nearest sharps
container.13) What is most important reason to press firmly but not to massage an
applied medicated patch?
a. Massaging a medicated patch can result in the untimely release of
medication.
b. Massaging a medicated patch can cause the medicated patch to
become dislodged.
c. Massaging a medicated patch can result in skin irritation.14) You go to place a transdermal patch on Mrs. LOWERY and note that the
patch from yesterday is still applied to her chest.
a. As an associate nurse, what do you expect to find on the applied
patch?
b. How long a transdermal patch should last?15) Nurse AKALIZA is going to administer amoxicillin to Mr. KALISA through
enteral route,
a. Discuss different ways of enteral route should be used to administer
a medication.
b. Outline the advantages and disadvantages of each enteral route16) The Dr. prescribe to Mr. JO an injectable cyanocobalamin 10mg to be
administered in intramuscular, the available vial has a concentration of 2
mg/1 ml.
a. Calculate the correct volume of cyanocobalamin to be administered
to Mr. JO.
b. Discuss the advantages and disadvantages of IM injection?
c. What are the indications and contra indications of IM route of drug
administration?d. Give 3 nursing considerations before administer a prescribed
medication to MR JO.
e. What are the complications may be associated to associated to IM
injection17) Describe the process used to perform each of the topical drug
administration.18) Name the materials used in IM technique of medication administration
19) When assessing a person’s response to medication therapy, how
does the nurse best recognize that the medication is therapeutic or
subtherapeutic?20) How do Three Checks facilitate a culture of safety in medication
administration?21) Mrs. LOWERY prefers to insert her own nose drops. As you observe her
doing so, what key aspects of the administration procedure should she
be doing to ensure correct technique?22) Subcutaneous route of drug administration consists of deposits the
medication into the subcutaneous layer below the skin, give out the 3
commonly used site in this route.23) Outline the 3 indications of rectal drug administration route
24) ISARO and KEZA, 3 and 7 years old girls admitted in general word of
pediatric unit. ISARO has persistent fever of 38.70C whereas KEZA
is having vomiting and diarrhea. The physician prescribed for ISARO,
paracetamol 250mg to be inserted in anus three times a day. KEZA
received Metronidazole 500mg by mouth to be taken 2 times a day. The
word nurse is coming for a new shift, is assigned to care for the above
patients. She read their files and discover that it is time to give medication
to ISARO. She went in the patients’ room and starts identifying these
children by asking the mothers and compare the names on the files.
She takes body temperature of Isaro and finds that it is now 38.30C. She
approaches the ISARO’S mother to explain that her child is still having
fever and a need to administer the paracetamol 250mg to control fever.
The mother accepts the request of the nurse. She then takes the drug
from patient’s box and prepare it and introduce in the anus of ISARO as
it was written in the file. She thanks the patient and write this activity in
the patient file. After 30 minutes she returned to ISARO and take again
her body temperature which is now 37.20C. Finally reassure the mother
on the effectiveness of the medication.a) What are the key actions done by the nurse while caring for
ISARO?
b) Which route of drug administration used in this case?
c) Compare and contrast the intramuscular to intradermal routes of
drug administration.
