UNIT 4: NOSOCOMIAL INFECTIONS CONTROL AND PREVENTION
Key Unit Competence
Apply correctly the infection prevention and control techniques for nosocomial
infections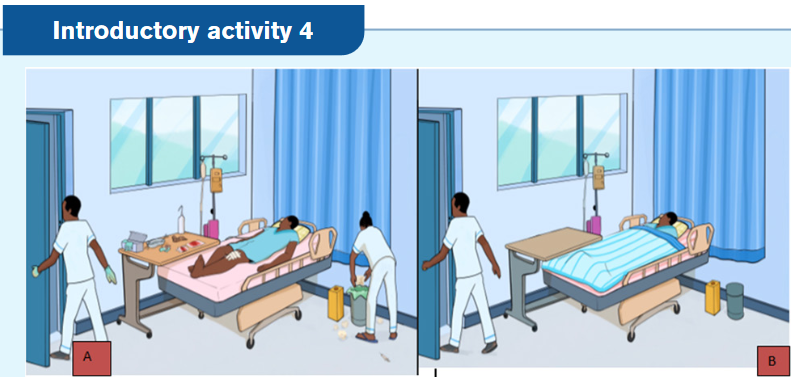
1) Is it perfect to maintain patient room A like this?
2) On your view, what should be done by the nurse room A and B if any?
3) What are potentials risks associated to this kind of patient arrangement A?
4) What do you predict to learn from this unit?4.1. Overview on nosocomial infections
Learning activity 4.1.
Observe the picture below:
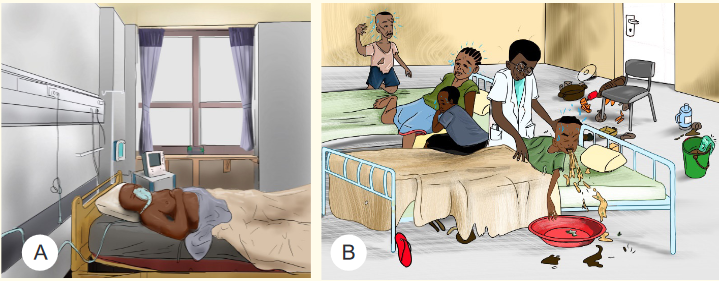
1) Analyze the pictures above and identify the probability of transmitting
diseases among them (A, B, C and D.)
2) Based on the picture above, what are the possible risk factors of nosocomial
infection for patient A and B?Nosocomial infection is a term that encompasses infections contracted in all health
care settings. Nosocomial infections also known as healthcare - associated infec-
tions (HCAI) or hospital acquired infections are defined as localized or system in-
fection, occurring at least 48 hours after hospital admission, that was not present or
incubating at the time of admission. They are those infections that occur in patients
or healthcare workers either as a direct result of healthcare intervention (such as
medical or surgical treatment) or from being in contact with a healthcare setting.4.1.1. Risk factors for nosocomial infections
The risk factors for nosocomial infection include hospitalized patients with under-
lying disease like diabetes, high blood pressure, HIV/AIDs, malnutrition, etc.; age
particularly elderly and young aged people, invasive devices and procedures
such as IV lines, surgery, intensive care; emergency hospital admission , previous
exposure to some drugs and previous hospital admission add to the risk.4.1.2. Causes of nosocomial infections
The most common pathogens that cause nosocomial infections are Staphylococ-
cus aureus, Pseudomonas aeruginosa, and E. coli. Nosocomial infections are not
just limited to bacteria; certain fungi such as Candida albicans and aspergillus, as
well as, viruses such as Respiratory Syncytial Virus and influenza have also been
implicated in a number of hospital acquired infections.4.1.3. Transmission of nosocomial infections
These infections are transmitted through direct or indirect contact from the hospital
staff, other patients or visitors; inadequately sterilized instruments; disease vector
carrying and transmitting an infectious pathogen, or blood; aerosol droplets from
other ill patients or even the food or water provided at hospitals.Direct-contact transmission involves a direct body surface-to-body surface con-
tact and physical transfer of microorganisms between a susceptible host and an
infected or colonized person, such as when a person turns a patient, gives a patient
a bath, or performs other patient-care activities that require direct personal contact.
Direct-contact transmission can also occur between two patients, with one serving
as the source of the infectious microorganisms and the other as a susceptible host.
Indirect-contact transmission involves contact of a susceptible host with a contam-
inated intermediate object, usually inanimate, such as contaminated instruments,
needles, or dressings, or contaminated gloves that are not changed between patientsSelf-assessment 4.1.
1) Define nosocomial infections
2) Explain the causes of transmission of nosocomial infections
3) What are risk factors of nosocomial infections?
4) Discuss the mode of transmission of nosocomial infections4.2. Concepts of Asepsis and Antisepsis
Learning activity 4.2.
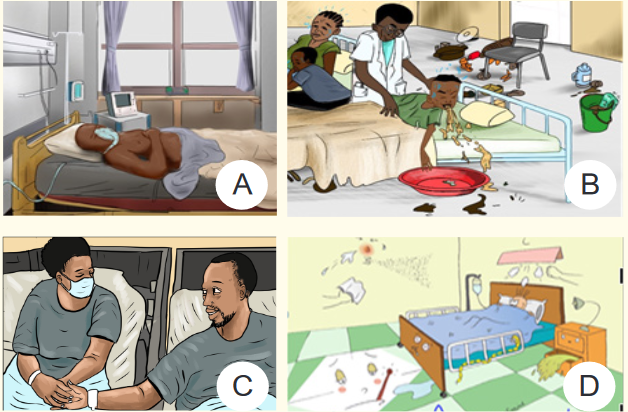
Observe the picture below:
1) Observe the activity that is being done on the picture A and tell its importance.
2) Discover the kinds of clothes and items that the people in picture B are
wearing.
3) Why the people in the picture B are wearing like that?Regardless of where nurses practice, preventing the transmission of microorgan-
isms is a concern of all health care professionals. One way that nurses accomplish
this goal is by asepsis.Asepsis means the absence of germs, such as bacteria, viruses, and other micro-
organisms that can cause disease. Healthcare professionals use aseptic technique
to protect patients from infection.Antisepsis is the practice of using antiseptics (substance that stops or slows down
the growth of microorganisms) to eliminate the microorganisms that cause disease.4.2.1. Principles of Asepsis
The principles of asepsis include the following:
1. Use only sterile items within a sterile field;
2. Sterile (scrubbed) personnel are gowned and gloved;
3. Sterile personnel operate within a sterile field (sterile personnel touch only
sterile items or areas, unsterile personnel touch only unsterile items or areas);
4. Sterile drapes are used to create a sterile field
5. All items used in a sterile field must be sterile
6. All items introduced onto a sterile field should be opened, dispensed, and
transferred by methods that maintain sterility and integrity
7. A sterile field should be maintained and monitored constantly
8. Surgical staff should be trained to recognize when they have broken technique
and should know how to remedy the situation.4.2.2. Difference between Medical and Surgical asepsis
The term medical asepsis refers to practices performed to prevent the spread of
infection. It is also sometimes described as using clean technique. These practic-
es, or techniques, include performing hand hygiene, maintaining a clean patient
environment, using standard precautions, and using transmission-based pre-
cautions when necessary.Medical asepsis is different than surgical asepsis, which refers to maintaining
a sterile environment such as that found in operating rooms. Sterile technique
means performing procedures in such a way that no pathogens will enter the pa-
tient’s body when you insert tubes or give injections.4.2.3. Levels of asepsis (Cleaning, Disinfection and Sterilization)
a) Cleaning
Cleaning is the process of removing unwanted substances using water and soap,
such as dirt, infectious agents, and other impurities, from an object or environment.
Cleaning removes dirt, dust, crumbs, and germs from surfaces or objects. When
you clean, you will likely use soap (or detergent) and water to physically clean off
the surfaces and objects. This may not necessarily kill the germs. But since you
removed some of them, there are fewer germs that could spread infection.
b) Disinfection
Disinfection is a process of using chemicals (disinfectants) to kill germs on surfaces
and objects. Some common disinfectants are bleach and alcohol solutions. You
usually need to leave the disinfectant on the surfaces and objects for a certain pe-
riod of time to kill the germs. Disinfecting does not necessarily clean dirty surfaces
or remove germs.
c) Sterilization
Sterilization refers to any process that removes, kills, or deactivates all forms
of life (in particular referring to microorganisms such as fungi, bacteria, spores,
unicellular eukaryotic organisms such as Plasmodium, etc.Note: After sterilization, an object is referred to as being sterile or aseptic.
Common methods of sterilization include physical methods and chemical
methods. Physical methods include dry heat, steam, radiation, and plasmas.Chemical methods include, for example, ethylene oxide, propylene oxide, chlorine
dioxide, ozone gases, and a variety of chemicals in liquid and vapor form, such as
glutaraldehyde, hydrogen peroxide, and peracetic acid.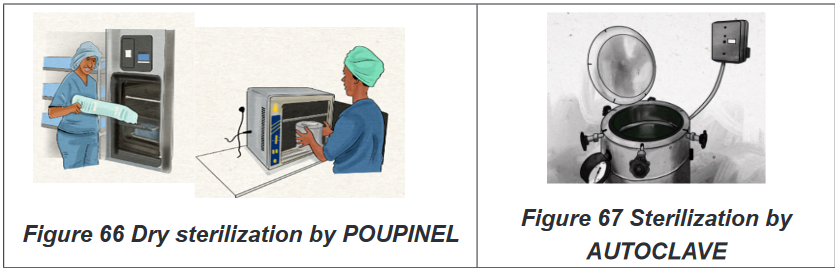
Self-assessment 4.2.
1) Differentiate asepsis and antisepsis
2) Describe the levels of asepsis4.3. Prevention and control of nosocomial infections
Learning activity 4.3.
You are working at hospital setting as associate nurse and you have a patient
suffering from malaria with high fever. He is receiving IM Arthesunate injection
and paracetamol tablets. After two days, the health professionals decided to
perform Covid19 test which become positive.
1) How are you going to behave in order to prevent you from contamination
when you are going to give the above said patient treatment?Prevention and control of infections are important concerns for all types of health
care agencies, and good infection control practices generate cost savings and im-
proved outcomes for patients.According to the World Health Organization (WHO), infection prevention and con-
trol (IPC) is a scientific approach and practical solution designed to prevent harm
caused by infection to patients and health workers.4.3.1. General information on WHO Standard precautions of
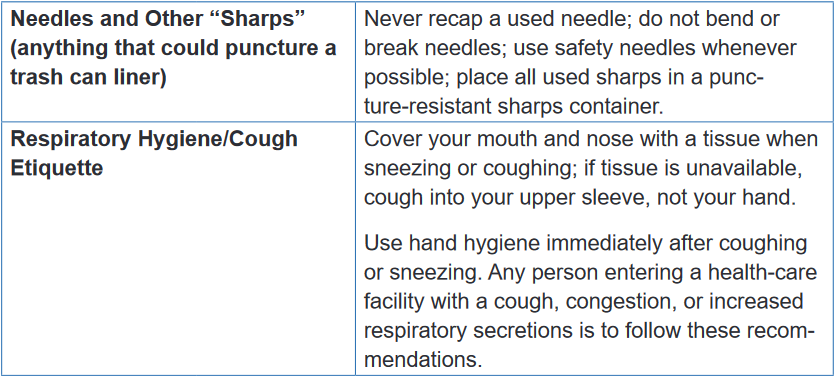
infection controlStandard precautions of nosocomial infection are the minimum set of actions
that are to be undertaken in every care environment and to be used for every care
procedure, every time. They are performed with all patients, whether or not an in-
fection has been diagnosed.They protect the health-care worker from possible transmission of illnesses spread
through contact with infected blood, such as hepatitis B, hepatitis C, and HIV. They
also protect patients from the possible spread of pathogens from one patient to
another.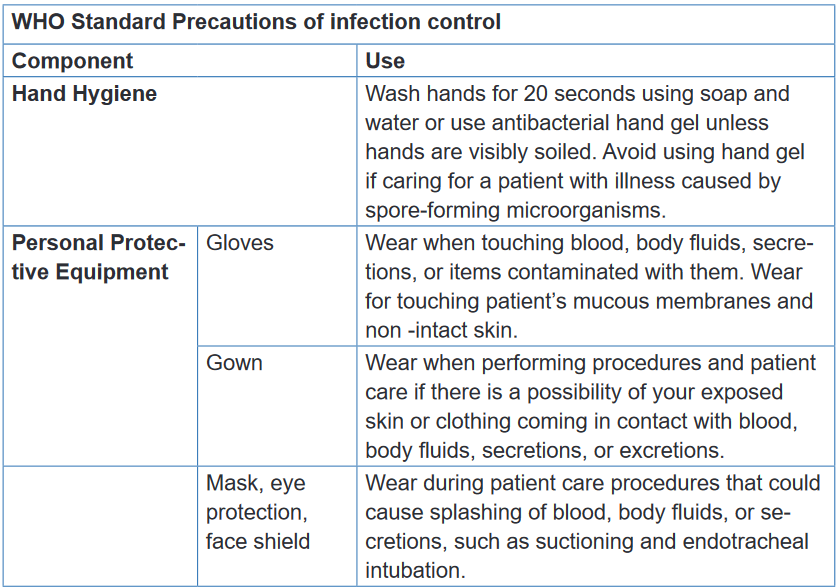
Self-assessment 4.3.
1) Which of the following are basic standard precautions for infection
control?(choose one answer)
a) Hand hygiene
b) Personal protective equipment and clothing
c) Safe handling of sharps
d) All of these are basic standard precautions2) What is the purpose of wearing gloves and gowns? (Check all that
apply).
c) Protect the healthcare worker
d) Prevent transmission of pathogens
e) Reduces hand washing requirements
f) Looks professional and identifies healthcare staff
3) What is importance of standards precautions of nosocomial infection?4.4. Overview of hand hygiene
Learning activity 4.4.
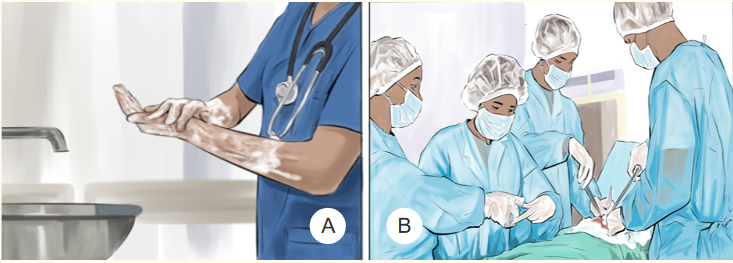
Observe the pictures and answer the questions below:

1) What are similarities and differences between picture A and B?
2) In your point of view, what is importance of the actions in pictures A and B?Hand hygiene is a general term referring to any action of hand cleansing. The term
hand rubbing is used when using an alcohol-based hand rub or hand washing with
soap and water aimed at reducing or inhibiting the growth of micro-organisms on
hands.4.4.1. When to perform hand hygiene
Hand hygiene are indicated before and after touching the patient; before handling
an invasive device for patient care regardless of whether or not gloves are used;
after contact with body fluids or excretions, mucous membranes, non-intact skin,
or wound dressings; if moving from a contaminated body site to another body site
during care of the same patient; after contact with inanimate surfaces and objects
(including medical equipment) in the immediate vicinity of the patient; after removing
sterile or non-sterile gloves; before handling medication or preparing food.4.4.2. Benefits of hand hygiene
Germs from unwashed hands can be transferred to other objects, like handrails,
table tops, or toys, and then transferred to another person’s hands. Hand hygiene
is the most important measure to avoid the transmission of harmful germs between
people and prevent health care-associated infections.Note: As much as it is necessary, perform hand hygiene. Hand rubbing never
replaces hand washing. Whenever possible, do hand washing. Soap andalcohol-based hand rub should not be used at the same time.
4.4.3. Hand rubbing and hand washing
Hand hygiene is the single most important procedure for preventing the transmission
of diseases and infections. It can be done through hand rubbing and/ or hand
washing. (For more, refer to the UNIT 2: Subtopic 2.1. )a) Hand rubbing
Hand rubbing is a hand hygiene technique with alcohol-based formulation (antiseptic
hand rubbing). It last between 20-30 seconds. The equipment to be used in hand
rubbing is the following: antiseptic hand rub: Alcohol-based, waterless, antiseptic-
containing emollientHand rubbing involves the following steps: (1) Apply an ample amount of product
to palm of one hand; (2) Rub hands together, covering all surfaces of hands and
fingers with antiseptic; (3) Rub hands together for several seconds until alcohol is
dry; (4) Allow hands to dry before applying gloves. (Refer to the UNIT 2:, Subtopic
2.1. )b) Hand washing
Action of performing hand hygiene using soap and water for the purpose of
physically or mechanically removing dirt, organic material, and/or microorganisms.
The duration of the entire procedure is 40-60 seconds.Equipment of hand washing include easy-to-reach sink with warm running water,
antimicrobial or non-antimicrobial soap, Paper towels or air dryer, Disposable nail
cleaner (optional).Self-assessment 4.4.
1) What are benefits associated with hand washing?
2) As a future associate nurse, when to perform hand washing?
3) What is the difference between hand rubbing and hand washing?4.5. Personal protective equipment (PPE)
Learning activity 4.5.
See the image below and answer the related questions:

1) What are you seeing on the image above?
2) On your view, what is importance of each item on this image?Personal protective equipment is clothing and equipment that is worn or used in
order to provide protection against hazardous substances or environments. This
can include items such as safety helmets; ear protection; high visibility clothing;
safety footwear and safety harnesses; thermal, weather and waterproof clothing;
respiratory protective equipment.4.5.1. Gloves
The use of gloves does not replace the need for hand hygiene by either hand
rubbing or hand washing. The gloves should be worn when it can be reasonably
anticipated that contact with blood or other potentially infectious materials, mucous
membranes or non-intact skin will occur. After caring for a patient all the gloves
should be removed and always the gloves are single use.It is important to wear gloves when working with hazardous chemicals and other
materials because they protect our hands from infection and contamination.
Protective gloves should be selected on the basis of the hazards involved. Rubber
gloves protect against mild corrosive material.4.5.2. Gown
Nurses wear sterile gowns when assisting at the sterile field in the operating room,
delivery room, and special treatment areas. Surgical gowns serve to protectpatients from microorganisms carried by the surgical team or patients themselves
and protecting healthcare providers from contact with infectious microorganisms
harbored by the patient.It allows the nurse to handle sterile objects and also be comfortable with less
risk of contamination. The sterile gown acts as a barrier to decrease shedding
of microorganisms from skin surfaces into the air and thus prevents wound
contamination. A fluid-resistant gown or protective apron is worn to keep the nurse’s
clothing clean when potential exists for body substances to splash.The main difference between a gown and an apron is that a gown covers the entire
torso and goes all the way down to the healthcare worker wrists.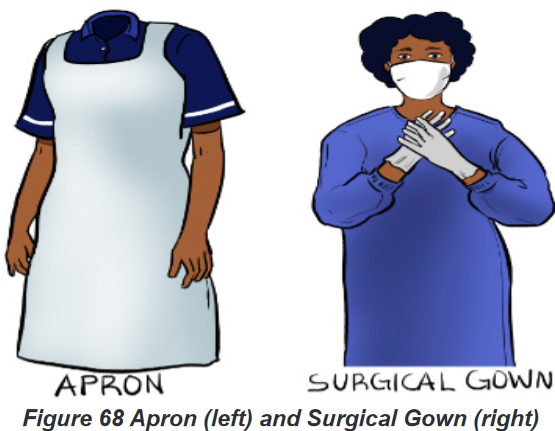
4.5.3. Mask
Masks help protect clients and healthcare personnel from respiratory infections and
certain communicable diseases.
Considerations in mask use include (1) put on the mask before the gloves;(2) do
not touch the mask until it is to be removed; (3) the mask must be changed when
moist or soiled; (4) wash hands and remove gloves before removing the mask; (5);
handle masks by the strings or elastic only; (6) dispose of a used mask immediately;
do not leave a mask dangling around the neck.4.5.4. Eye protection (goggles) and face shield
Safety goggles are important because they protect health care providers from
accidental entry of blood and other microorganisms in the eyes. They also allow
the wearer to handle potentially harmful chemicals and biological without fear ofdamaging their eyes. Safety goggles can also help to protect an individual from
harm to the eye from physical trauma.Wear goggles with side and forehead shields if any danger exists that a client’s
body fluids may splash or spray. Goggles are also available that fit over glasses.
In some types of isolation, disposable goggles are worn. In situations when extra
protection is needed, such as in the operating room, emergency department, or
morgue, full face shields are used. These protect the eyes, as well as the mouth.
The situation dictates the type of eye and mucous membrane protection to be used.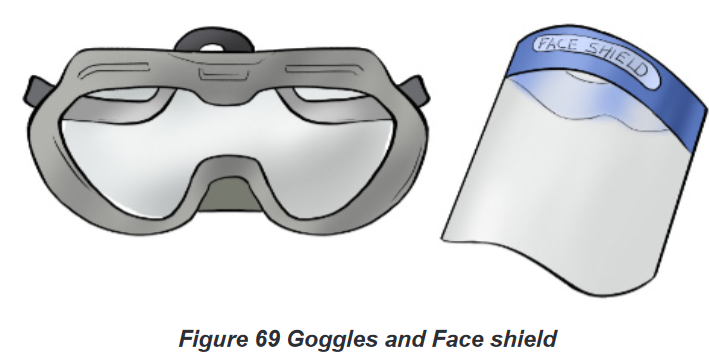
4.5.5. Boots
A pair of safety shoes also known as safety boots is personal protective equipment
(PPE) for foot protection at workplaces. Protective footwear worn in the workplace is
designed to protect the foot from physical hazards such as falling objects, stepping
on sharp objects, heat and cold, wet and slippery surfaces, or exposure to corrosive
chemicals.4.5.6. Donning (wearing) of Personal Protective Equipment
Donning involves putting on the required apparel before patient contact and must
be performed in the following order; (1) hand hygiene; (2) put on shoe covers (if
applicable);(3) wear gown; (4) wear mask;(5) put eye or face protection ;(6) and
gloves.4.5.7. Doffing (removing) of Personal Protective Equipment
Personal protective equipment must be removed in the following specified
sequence, to minimize the potential for disease transmission: (1) wash hands, (2)remove gloves, (3) remove mask by touching only the string tied behind the head,(4)
remove eye protection without touching the face, (5) wash hands, (6) remove gown
or apron touching only the inside, turn it inside out, to contain contamination, (9)
properly dispose of all PPE, (10) wash hands.Self-assessment 4.5.
1) The nurse wears a gown when:
a) The patient’s hygiene is poor
b) The nurse is assisting with medication administration.
c) The patient has acquired immunodeficiency syndrome
(AIDS) or hepatitis.
d) Blood or body fluids may get on the nurse’s clothing from
a task that he or she plans to perform.2) Match in the correct order of donning(wearing) Personal Protective
Equipment (PPE)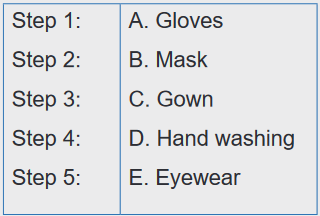
3) Match in the correct order of doffing(wearing) Personal Protective
Equipment (PPE)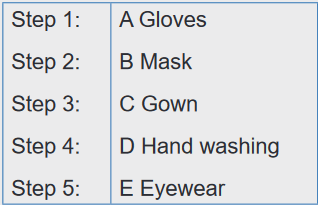
4.6. Respiratory hygiene and cough etiquette
Learning activity 4.6.
Observe the picture below and answer following questions
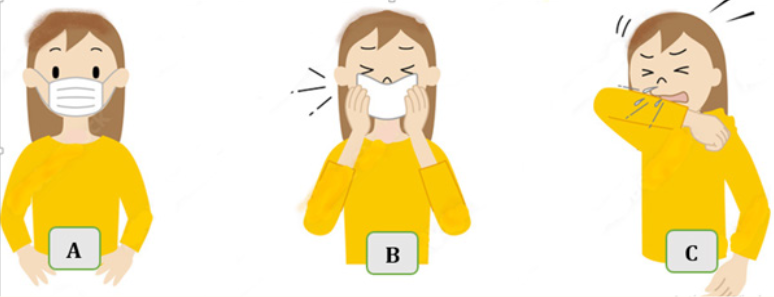
1) What are you seeing on the picture A, B and C?
2) On your view, what are similarities and differences of persons on picture
A, B and C?Respiratory hygiene and cough etiquette are terms used to describe infection
prevention measures to decrease the transmission of respiratory illness (e.g.,
influenza and cold viruses). A respiratory infection is spread when a person who is
infected with a virus coughs or sneezes.
Cough etiquette is a series of actions that should be taken when coughing or
sneezing which are designed to reduce the spread of respiratory illness to others.4.6.1. The actions to respect in respiratory hygiene
In respiratory hygiene everyone should (1) cover the mouth and nose with the tissue,
wear mask or put on elbow when coughing or sneezing; (2)Use tissues and discard
the tissue immediately into a bin; (3)wash hands or use a hand sanitizer every time
touching the mouth or nose; (4) post visual alerts (in appropriate languages) at the
entrance to outpatient facilities instructing patients and persons who accompany
them (e.g., family, friends) to inform healthcare personnel of symptoms of a
respiratory infection when they first register for care and to practice respiratory
Hygiene/cough Etiquette.4.6.2. Importance of respiratory hygiene
Respiratory hygiene and cough etiquette are very important components to protect
self and others from the transmission of respiratory illness. Like hand hygiene,
respiratory hygiene is part of the standard precautions that should be taken to
prevent the spread of disease.Self-assessment 4.6.
1) Respiratory hygiene/cough etiquette includes:
a) Posting visual alerts about signs and symptoms of infection
b) Re-using tissues to help keep costs down
c) Frequent hand hygiene, especially after contact with respiratory
secretions
d) A and C are correct answers2) What is the importance of respiratory hygiene /cough etiquette?
4.7. Sharps Safety/ Safe Injection Practices
Learning activity 4.7.
Observe the pictures and answer questions below:

1) What do you see on the picture A and B?
2) On your view, what are consequences associated with the picture B?Safe injection is injection practice which does not harm the recipient (patient), does
not expose the provider to any avoidable risks and does not result in waste that is
dangerous for the community.Safe injection practice is achieved by administering the injection using a sterile
device (syringe, needle etc.), adopting sterile technique by a qualified and well
trained person and discarding the used devices in a puncture-proof container
specially designed for appropriate disposal. Any breach in the process makes the
injection unsafe.4.7.1. Consequences of unsafe injection
Unsafe injection practices which can transmit Hepatitis B, Hepatitis C, Human
immunodeficiency virus (HIV) and other blood borne pathogens result in substantial
burden of preventable blood borne viral diseases.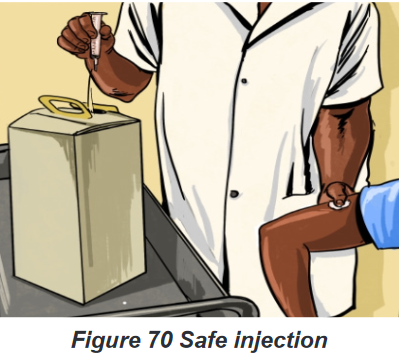
4.7.2. Management of Accidental Needle sticks or Other
ContaminationUnfortunately, the nurse may sustain an accidental stick with a contaminated
needle. If this occurs, follow these procedures:
Wash the area gently with soap and running tap water as soon as possible;
Report the incident to the direct leader and / infection prevention and; control
focal person,
Fill out an incident report,
Blood tests of the client and nurse will usually be performed.The nurse may be required to take medication as post exposure prophylaxis if the
patient has blood transmissible disease or has disappearing without being tested.
If material is splashed into the eyes or mouth, wash with copious amounts of water
and report as above.Self-assessment 4.7.
1) Which of the following is included in the steps for needle stick injuries?
a) Wash needle stick injury with soap and water
b) Report needle stick injury to your supervisor
c) Wash needle stick injury with soap and water and use alcohol
d) A and B are correct answers2) The first step after a needle stick or sharps injury is to
a) Express or suck the wound.
b) Apply caustic agents (e.g., bleach) to the wound.
c) Inject antiseptics or disinfectants into the wound.
d) Gently wash the exposed area with soap and water without
scrubbing.4.8. Sterilization and Disinfection of Patient-Care Items
and DevicesLearning activity 4.8.
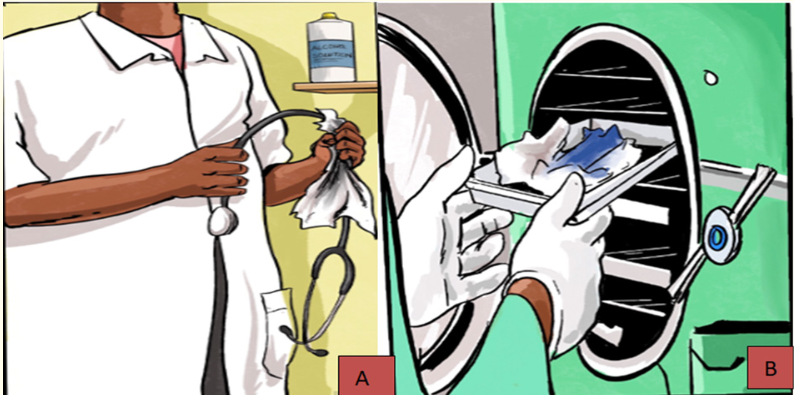
See the picture and answer the questions
1) What is the action done on picture A and picture B?
2) What is the importance of each action?Sterilization and disinfection are the basic components of hospital infection control
activities.The medical device or the surgical instrument that comes in contact with the sterile
tissue or the mucus membrane of the patient during the various processes is
associated with increased risk of introduction of pathogens into the patient’s body.4.8.1. Importance of disinfection
Frequent cleaning and disinfection helps to prevent the spread of germs that
may cause illness. The importance of respecting the proper disinfection is that it
will reduce infections associated with contaminated patient-care items.
The cleaning and disinfection of medical equipment depends on their physical
nature, character of the material it is made up of, lumen size, etc.4.8.2. Importance of sterilization
Sterilization aims to eliminate or kills all microorganisms on medical items. Sterilizing
each piece of equipment is critical to keeping each patient as safe and healthy
as possible.The level of disinfection and sterilization is dependent on the intended use of the
object: Critical items (such as surgical instruments (example forceps), which contact
sterile tissue), semi critical items (such as endoscopes, which contact mucous
membranes), and noncritical items (such as stethoscopes, which contact only
intact skin) require sterilization, high-level disinfection, and low-level disinfection,
respectively. Cleaning must always precede disinfection and sterilization.Self-assessment 4.8.
1) Remove and killing all microorganisms on materials is known as:
a) Disinfection
b) Cleaning
c) Sterilization
d) Destruction
2) What is the importance of disinfection and sterilization4.9. Cleaning and disinfection of environmental surfaces
Learning activity 4.9.
See the picture below and answer the following questions:
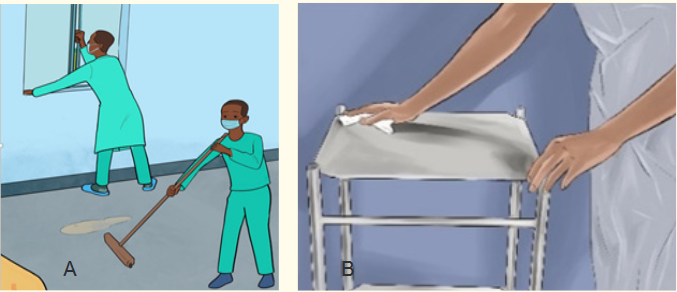
What are you seeing on picture A and B
1) What is importance of activity done on picture A and B?
2) What are the similarities and differences among the picture A and B?Environmental surfaces in health-care settings include furniture and other fixed
items inside and outside of patient rooms and bathrooms, such as tables, chairs,
walls, light switches and computer peripherals, electronic equipment, sinks, toilets
as well as the surfaces of non-critical medical equipment, such as blood pressure
cuffs, stethoscopes, wheelchairs and incubators.4.9.1. Cleaning and disinfection of environmental surfaces
Environmental surfaces are more likely to be contaminated in health-care settings
where certain medical procedures are performed. Therefore, these surfaces, are
being cared for, must be properly cleaned and disinfected to prevent infection
transmission.4.9.2. Principles used in cleaning and disinfection
Cleaning helps to remove pathogens or significantly reduce their load on
contaminated surfaces and is an essential first step in any disinfection process.
Cleaning with water, soap (or a neutral detergent) and some form of mechanical
action (brushing or scrubbing) removes and reduces dirt, debris and other organic
matter such as blood, secretions and excretions, but does not kill microorganisms.Organic matter such as stool, vomits etc. can inhibit direct contact of a disinfectant
to a surface and inactivate the germicidal properties or mode of action of several
disinfectants that is why the cleaning should be done first. Moreover, the disinfectant
concentration and contact time are also critical for effective surface disinfection.
Therefore, a chemical disinfectant, such as chlorine or alcohol, should be appliedafter cleaning to kill any remaining microorganisms.
Disinfectant solutions must be prepared and used according to the manufacturer’s
recommendations for volume and contact time. Concentrations with inadequate
dilution during preparation (too high or too low) may reduce their effectiveness.
High concentrations increase chemical exposure to users and may also damage
surfaces. Enough disinfectant solution should be applied to allow surfaces to
remain wet and untouched long enough for the disinfectant to inactivate pathogens,
as recommended by the manufacturer.Self-assessment 4.9.
1) Why cleaning and disinfection of environmental surfaces?
2) Give four examples of environmental surfaces in health-care settings4.10. Safe handling of linens
Learning activity 4.10.
Observe the pictures below and answer the following questions
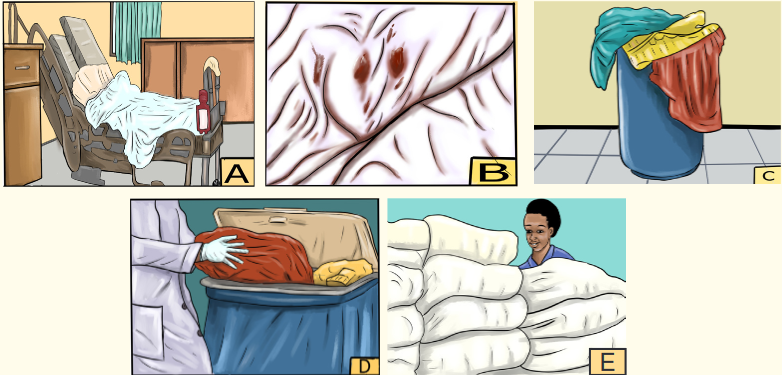
1) What are you seeing on the picture A, B, C, D and E?
2) What is the similarities and differences and on picture C and D?Linen is a kind of cloth that is made from a plant called flax. It is used for making
clothes and things such as tablecloths and sheets4.10.1. Handling linens in health settings
Clean linens should be stored in a clean, designated area, preferably an enclosed
cupboard. If clean linen is not stored in a cupboard then the trolley used for storage
must be designated for this purpose and completely covered with an impervious
covering that is able to withstand decontamination.All soiled linen should be placed into a clearly labeled, leak-proof container (e.g.,
bag, bucket) in the patient care area. Never transport soiled linen by hand outside
the specific patient care area from where it was removed. Never carry soiled linen
against the body; carefully roll up soiled linen to prevent contamination of the air,
surfaces, and cleaning staff and do not shake linen.All used linen should be handled with care to avoid dispersal of microorganisms into
the environment and to avoid contact with staff clothing.General principals of handling the linen consist of hand hygiene protocol respected by
all personnel when handling linen; standard precautions followed when handling
soiled linen, clean linen and soiled linen should be handled, stored, and transported
separately . Furthermore, linen should be maintained in good repair.Self-assessment 4.10.
1) How the soiled linen should be handled in health setting?
4.11. Hazardous wastes management
Learning activity 4.11.
Observe the picture below and answer following questions
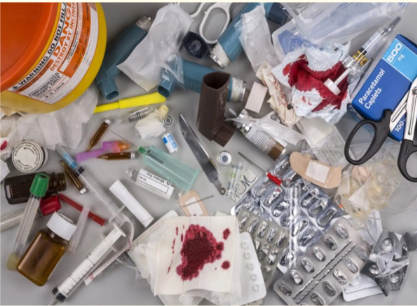
1) What do you see on this picture?
2) What are risks associated with the above hazardous wastes ?A hazardous waste is a waste with properties that make it dangerous or capable
of having a harmful effect on human health or the environment. Hazardous waste
when improperly handled can cause substantial harm to human health.4.11.1. Types of hazards waste
The hazardous nature of health-care waste is due to one or more of the following
characteristics:
Presence of infectious agents
A genotoxic or cytotoxic chemical composition
Presence of toxic or hazardous chemicals or biologically aggressive
pharmaceuticals
Presence of radioactivity
Presence of used sharpsHazardous-waste management consists of the collection, transport, disposal and
treatment of waste material safety. They may cause damage during inadequate
storage, transportation, treatment, or disposal operations.a) Collection of hazardous wastes:
Hazardous waste must be accumulated and stored at the point of generation until removed
by and must be: Collected in a container that is compatible with its contents under all
conditions that it might be subjected to during accumulation, storage, and shipment.
b) Disposing of Biohazardous Wastes
After cleaning up a spill, the nurse is responsible for properly disposing of the
materials. In addition to spilled body fluids, other biohazardous wastes include
soiled dressings, used blood tubes, syringes, catheters, or IVs. Many bio hazardous
items are placed in red “biohazard” bags for disposal. (It is important not to place
inappropriate materials in these bags, because there is an additional charge for
their disposal.) Remember to put sharps, such as needles, lancets, razor blades
or disposable razors, suture removal scissors, or scalpel blades, in the designated
sharps container. Any broken glass must be carefully disposed of as well. Be sure
to ask if you have any questions regarding disposals. The nurse in a community-
based setting or in home care is responsible for disposal of biohazardous wastes
and for teaching clients and families how to dispose of them as well.c) Hazardous waste transport
Hazardous waste generated at a particular site often requires transport to an
approved treatment, storage, or disposal facility. Because of potential threats
to public safety and the environment, transport is given special attention by
governmental agencies. It is highly prohibited to intentionally spilled or abandoned
at random hazardous waste in any locations no designed for that.d) Treatment of hazardous wastes:
Hazardous waste can be treated by chemical, thermal, biological, and physical
methods.Chemical methods include ion exchange, precipitation, oxidation and reduction,
and neutralization.Thermal methods are high-temperature incineration, which not only can detoxify
certain organic wastes but also can destroy them. Special types of thermal
equipment are used for burning waste in either solid, liquid, or sludge form. Theseinclude the fluidized-bed incinerator, multiple-hearth furnace, rotary kiln, and liquid-
injection incinerator. One problem posed by hazardous-waste incineration is the
potential for air pollution.Biological treatment of certain organic wastes, such as those from the petroleum
industry, is also an option. One method used to treat hazardous waste biologically
is called land farming. In this technique the waste is carefully mixed with surface soil
on a suitable tract of land. Microbes that can metabolize the waste may be added,
along with nutrients. In some cases a genetically engineered species of bacteria
is used. Food or forage crops are not grown on the same site. Microbes can also
be used for stabilizing hazardous wastes on previously contaminated sites; in that
case the process is called bioremediation.The chemical, thermal, and biological treatment methods outlined above change
the molecular form of the waste material.Physical treatment, on the other hand, concentrates, solidifies, or reduces the
volume of the waste. Physical processes include evaporation, sedimentation,
flotation, and filtration.So far another process is solidification, which is achieved by encapsulating the
waste in concrete, asphalt, or plastic. Encapsulation produces a solid mass of
material that is resistant to leaching. Waste can also be mixed with lime, fly ash,
and water to form a solid, cementike product.4.11.2. Health risks of hazardous waste
Health-care waste contains potentially harmful microorganisms that can infect
hospital patients, health workers and the general public. Other potential hazards
may include drug-resistant microorganisms which spread from health facilities into
the environment.Adverse health outcomes associated with health care waste and by-products also
include:
Sharps-inflicted injuries;
Toxic exposure to pharmaceutical products,
Chemical burns arising in the context of disinfection, sterilization or waste
treatment activities;
Air pollution arising as a result of the release of particulate matter during
medical waste incineration;
Thermal injuries occurring in conjunction with open burning and the opera-
tion of medical waste incinerators; and
Radiation burns.Self-assessment 4.11.
1) What is the problem associated with hazardous-waste incineration?
2) What is hazardous waste?End unit assessment 4
1) Which of the following is not the effective way to break the
chain of infection?
a) Wearing gloves
b) Hand hygiene
c) Placing patients in isolation
d) providing private rooms for patients2) Which of the following are basic standard precautions for infection
control?
a) Hand hygiene
b) Personal protective equipment and clothing
c) Safe handling of sharps
d) All of these are basic standard precautions3) The nurse wears a gown when:
a) The patient’s hygiene is poor
b) The nurse is assisting with medication administration.
c) The patient has acquired immunodeficiency syndrome (AIDS) or
hepatitis.
d) Blood or body fluids may get on the nurse’s clothing from a task
that he or she plans to perform.4) Respiratory hygiene/cough etiquette includes:
a) Posting visual alerts about signs and symptoms of infection
b) Re-using tissues to help keep costs down
c) Frequent hand hygiene, especially after contact with respiratory
secretions
d) A and C are corrects5) Remove and killing all microorganisms on materials is known as:
a) Disinfection
b) Cleaning
c) Sterilization
d) Destruction6) Which of the following is included in the steps for needle stick injuries?
a) Wash needle stick injury with soap and water
b) Report needle stick injury to your supervisor
c) Wash needle stick injury with soap and water and use alcohol
d) A and B are correct answers7) Match in the correct order of donning(wearing) Personal Protective
Equipment (PPE) :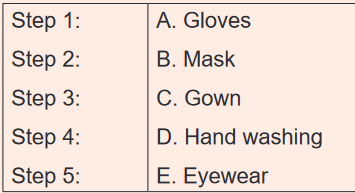
8) Arrange in the correct order of doffing (removing) Personal Protective
Equipment: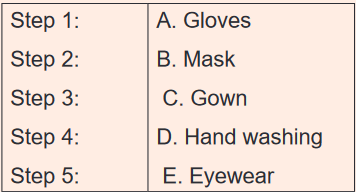
9) Define nosocomial infections
10) Explain the causes of transmission of nosocomial infections
11) Discuss the mode of transmission of nosocomial infections
12) Differentiate asepsis and antisepsis
13) What is importance of standards precautions of nosocomial infection?
14) What are benefits associated with hand washing?
15) What is the importance of respiratory hygiene /cough etiquette?
