UNIT 2: HYGIENE AND COMFORT CARE OF THE CLIENT/PATIENT
Key Unit Competence:
Perform the Nursing care procedures related to hygiene and comfort of the client/
patient.Introductory activity 2
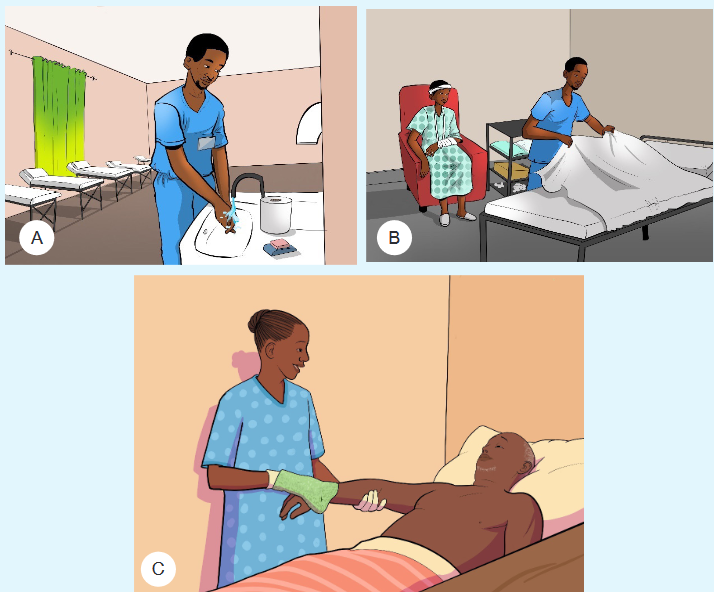
1) The nurse in image A is nearer to the hand washing facilities as it
requires her to perform hand hygiene before going to provide care to
patient. If water or sop is not available, suggest other possible means to
use while ensuring hand hygiene.2) Observe the image B and think about the hygiene and comfort care that
have been provided to the client3) Observe carefully the image C, and identify which kind of care that the
nurse has provided to the patient in bed. Suggest other care that should
be provided to such kind of client.2.1. Hands hygiene and gloving
Learning activity 2.1.
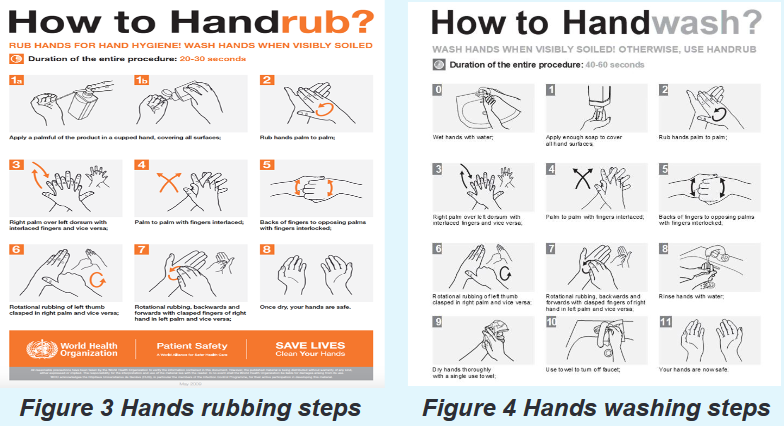
Look at the following figures (Figure 2, Figure 3 and Figure 4) and the
scenario below to respond to the learning questions asked.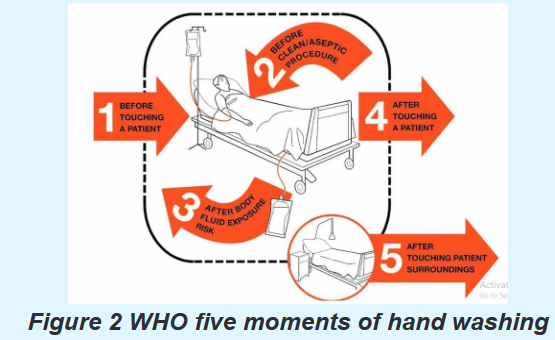
Scenario: A nurse Mary was assigned to provide care to Mr. Paul (Mr. Paul is a
patient who is very dirty) and Mary is required to wash or rub hands to prevent
the cross-infection. Before arriving to Paul, Mary was required to wear proper
gloves since Mr. Paul was bleeding and had skin rashes.1) By looking at the above pictures and by reading book from school library
or other additional resources from internet, explain the following terms:
a) Hand washing
b) Hand rubbing2) Based on the figure 1, explain the five moment of hand washing according
to WHO.3) Referring to the figure 2 and figure 3, demonstrate the technique of hand
washing and hand rubbing4) Based on the scenario, explain the purpose of wearing gloves.
2.1.1. Hands hygiene
a) Definition and importance
Hygiene refers to conditions and practices that help to maintain health and prevent
the spread of diseases (WHO,2009); this practice is very important for better health.
Hygiene includes bathing, toileting, general body hygiene and grooming.Hand hygiene is the most important aspect of the infection control. Hands, the
main pathway for germ transmission in health care settings should be carefully washed
with water and soap or rubbed with appropriate hand sanitizer to remove germs.Hand washing: is the act of cleaning hands using soap and clean water to remove
harmful germs (viruses, bacteria, and other germs), dirt, grease, or other harmful and
unwanted substances stuck on the hands. After washing the hands should be dried.Hand rubbing: Is the act of cleaning hands using an alcohol-containing
preparation (liquid, gel or foam) designed for application to the hands to inactivate
microorganisms and/or temporarily suppress their growth.b) Indications and WHO 5 moments of hand washing
It is indicated that nurses and health care providers should wash their hands more
frequently; that is before and after each procedure and each time your hands are
soiled or suspected to have contracted germs. There are 5 moments recommended
by WHO to wash hands as shown in Figure 5 Five Moments of hand washing
recommended by World Health Organization. Source: WHO, 2009.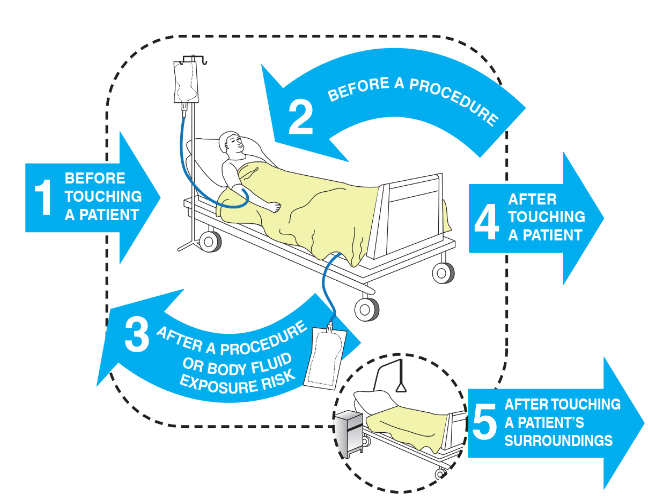
Figure 5 Five Moments of hand washing recommended by World Health
Organization. Source: WHO, 2009
The hand hygiene would not only refer to the technique but also the substance
used to clean. Hand hygiene requires the following materials: running water, soap
and single use paper dryer and appropriate hand sanitizer (when hand rubbing is
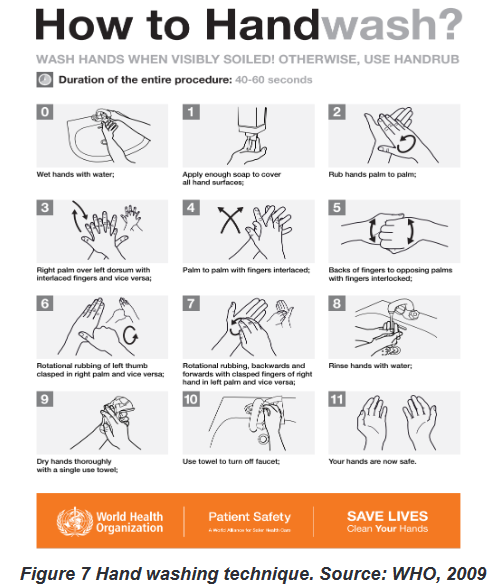
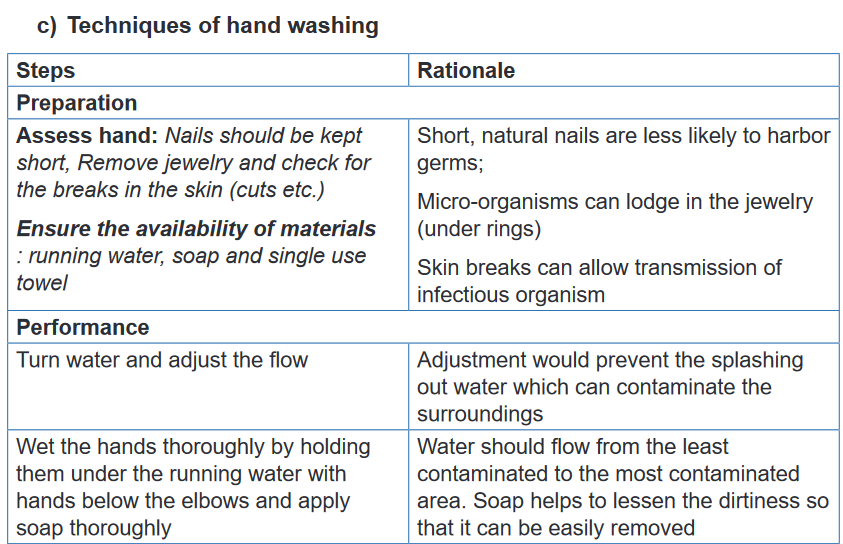
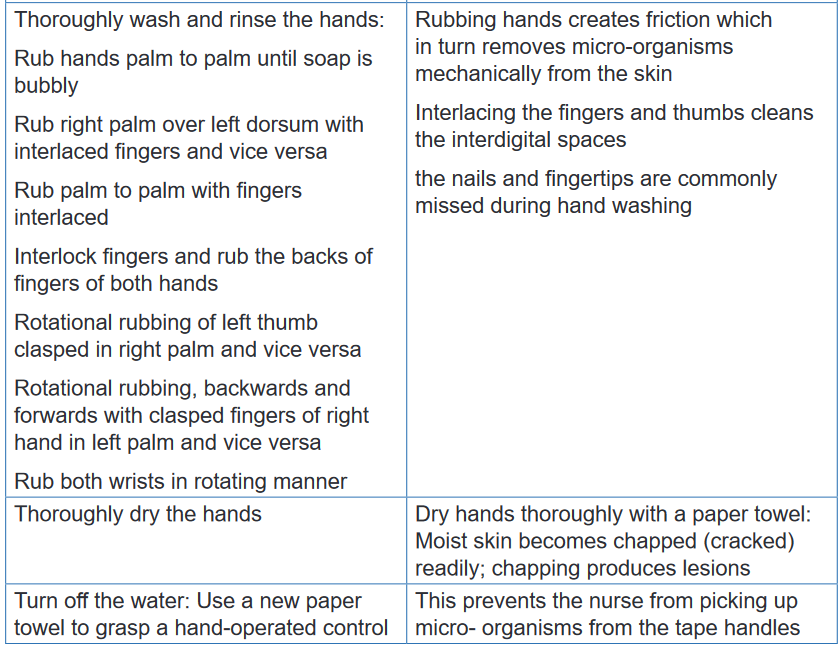
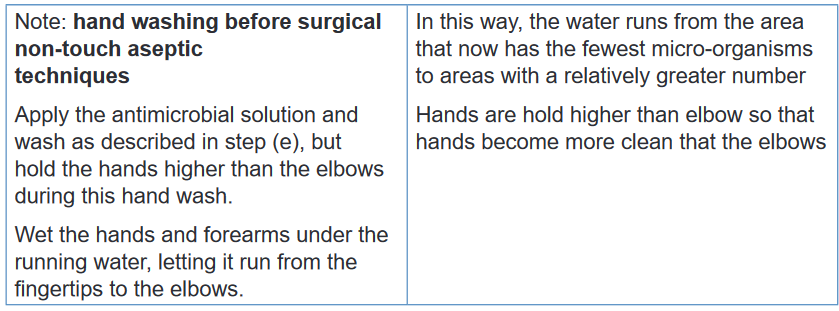
preferred).According to the WHO, there are techniques to follow while washing (see Figure 6)
or rubbing hands (see Figure 7).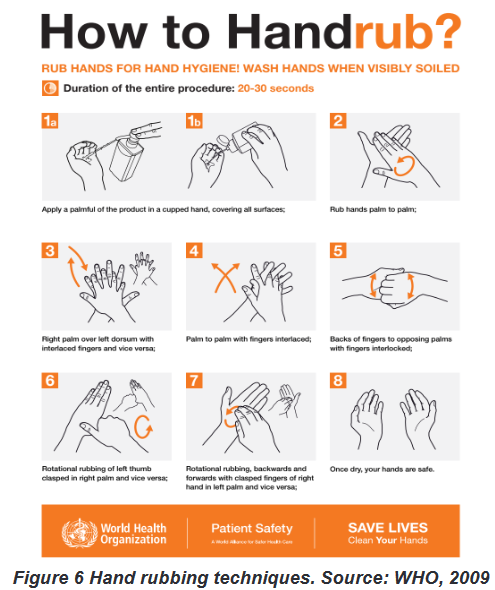
2.1.2. Hand gloving
a) Importance of hand gloving
Complementary to hand hygiene, hand gloving is one of the mechanisms to prevent
the spread of micro-organisms . There are three purposes of hand gloving: firstly,
they protect nurses’ hands when handling substances; secondly, they reduce
the likelihood of transmitting micro-organisms from nurses to the patient and
vice-versa, thirdly, they reduce the possibility of transmitting from one patient
to the other. Gloves should be changed between individuals, and one must wash
hands after removing gloves.b) Non-sterile and sterile gloving
Gloves are categorized in two types depending to the use: when performing septic
techniques, use clean disposable gloves (also called non-sterile gloves), and
when performing a sterile technique, use sterile gloves.Indications and contraindications
In health care settings the medical gloves are indicated in the following conditions:
protection of the wearer from contamination with blood, secretions, and excretions
and the associated risk of contamination with pathogens capable of reproduction.;
prevention of pathogen release from the hand into the sterile work area during
aseptic procedures; protection of hands from chemicals; pathogen barrier as
protection from biological agent and radiation protection. Gloves are contraindicated
in the following conditions: when a health care provider is away from the bedside or
laboratory bench; when health care provider is in nursing stations to handle phones
or charts; in time of handling clean linens and in case of cleaning non-contaminated
equipment or patient-care supplies (e.g. plate, cups etc.).
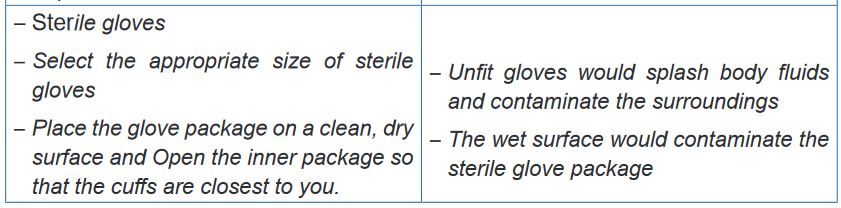
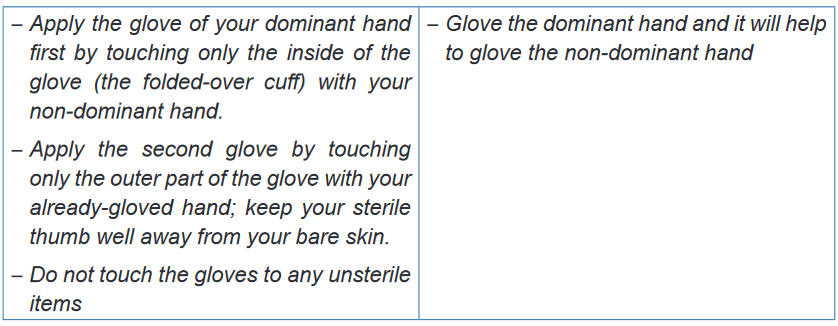
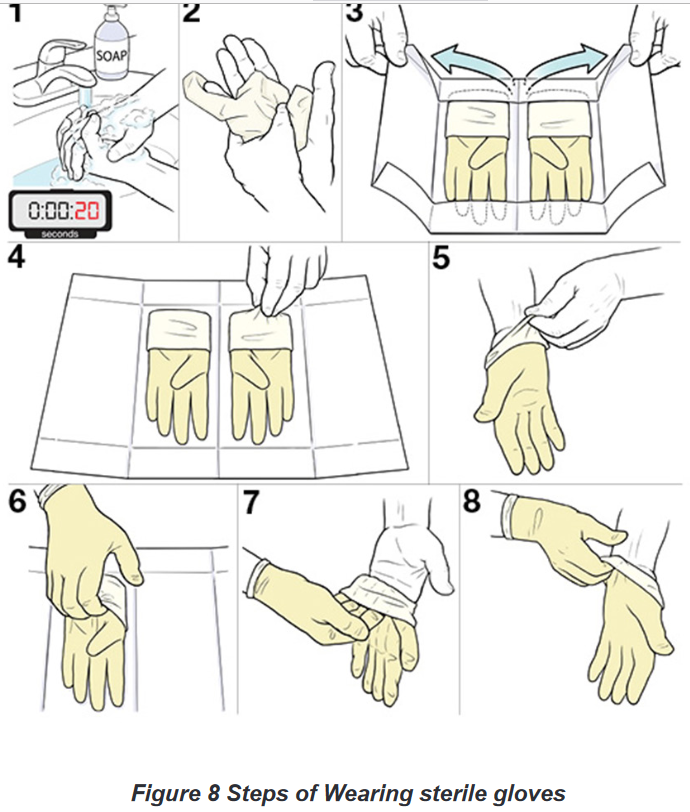
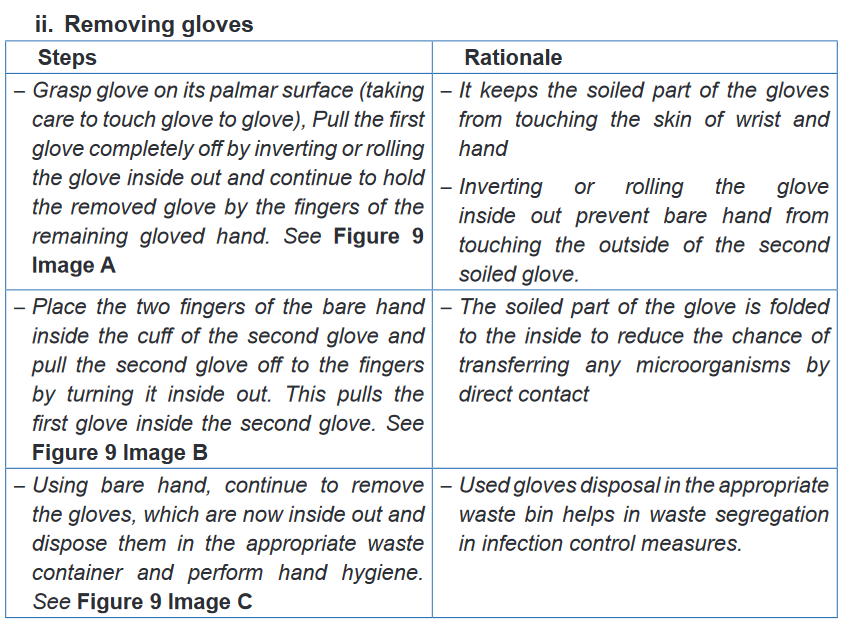
a) Techniques of gloving
Donning disposable clean gloves does not require special techniques, however
there are precautions: one’s hands must be dry, finger nails cut short and
jewellery removed to prevent tearing gloves. Donning sterile gloves on the
other hand, requires specific technique to ensure that no micro-organism is
introduced in a wound or body orifice which should be sterile.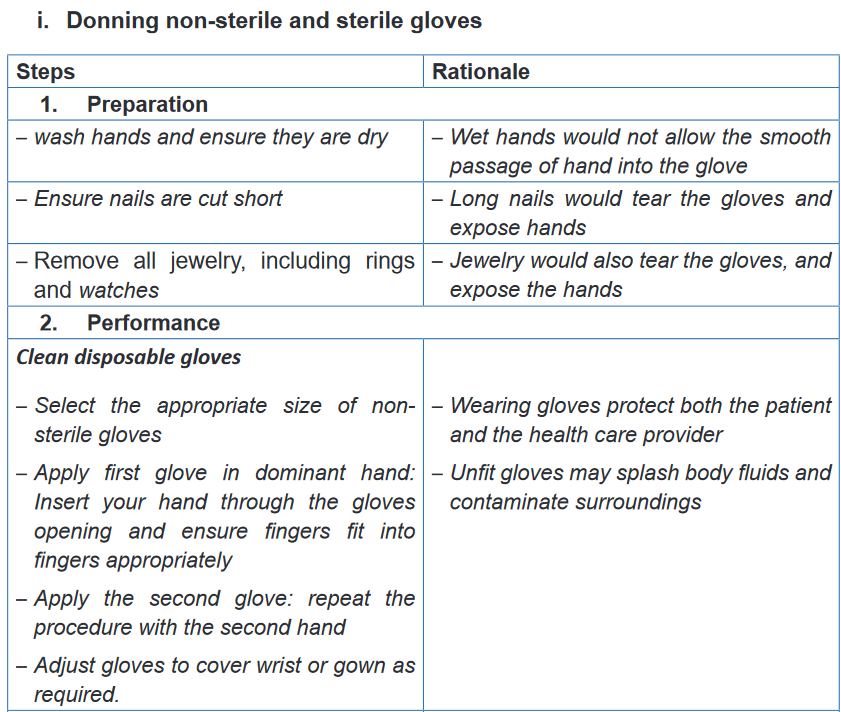
Self-assessment 2.1.
1) A Patient is bleeding on the left leg due to road accident. The nurse
has to get ready to help the patient to stop bleeding nurse is required to
perform hand hygiene before wearing the gloves. What kind or cleaning
technique should the nurse use?
a) Hand washing
b) Hand cleaning using chlorhexidine
c) Hand gloving
d) All the above2) What is the difference between hand rubbing and hand washing
3) Explain the WHO five moments of hands washing
4) Why should the nurse wash his or her hands or perform an alcohol-
based hand rub and then wear clean gloves?5) Nurse was proving bed making but before to wear gloves, she rubs
her hands with Alcohol and the patient asked her Why? Which of the
following is a benefit of an alcohol-based hand rub that the nurse should
explain?
a) Destroys active microbes but not spores
b) Provides the fastest and greatest reduction in microbial counts on
the skin
c) Leads to irritation and drying of the skin compared with soap
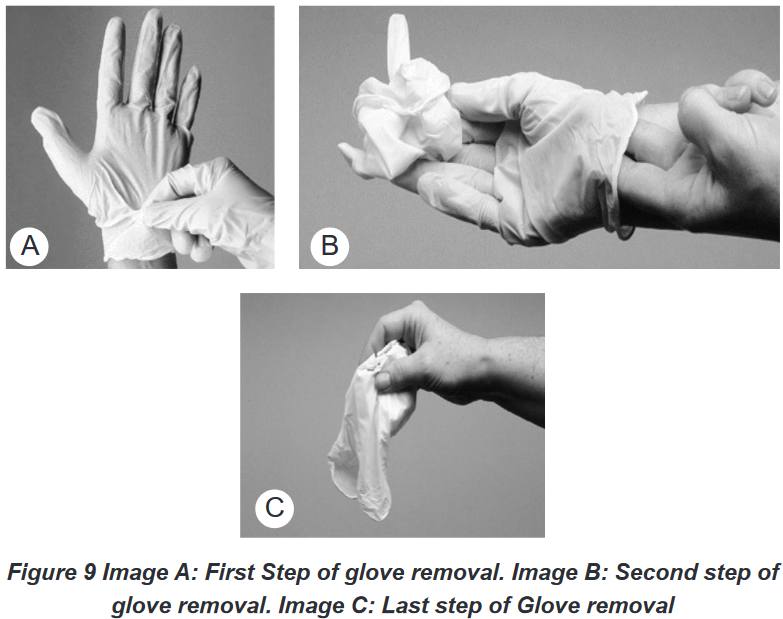
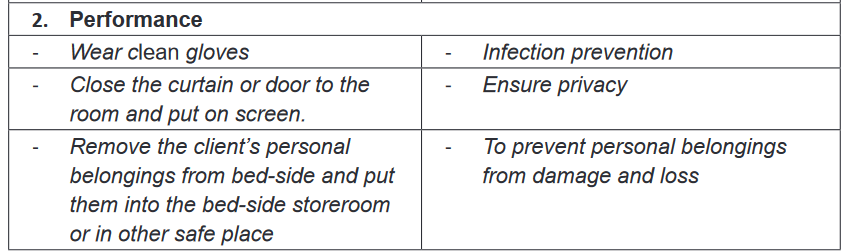
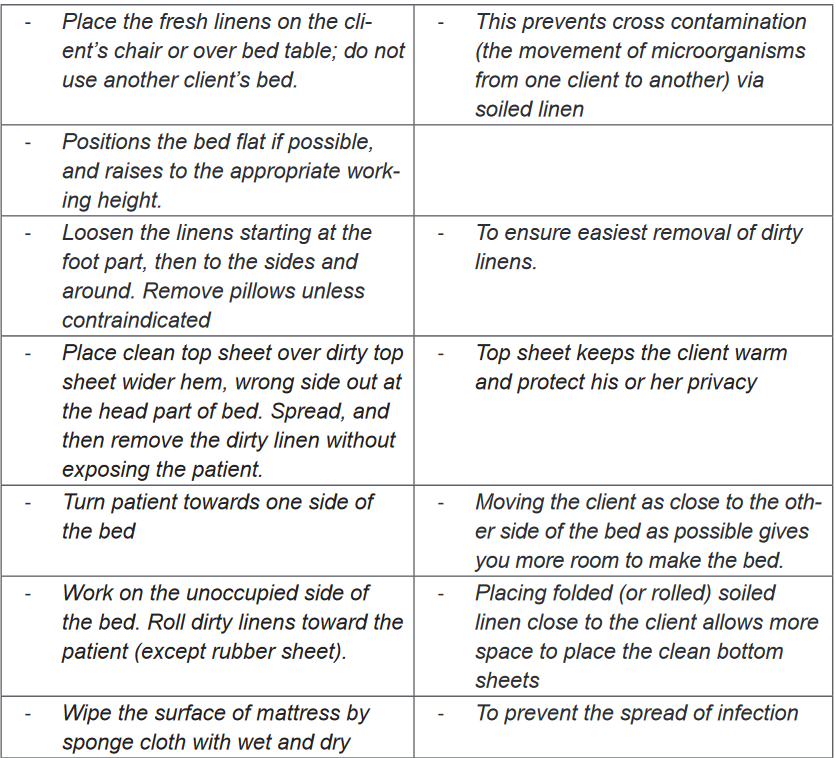
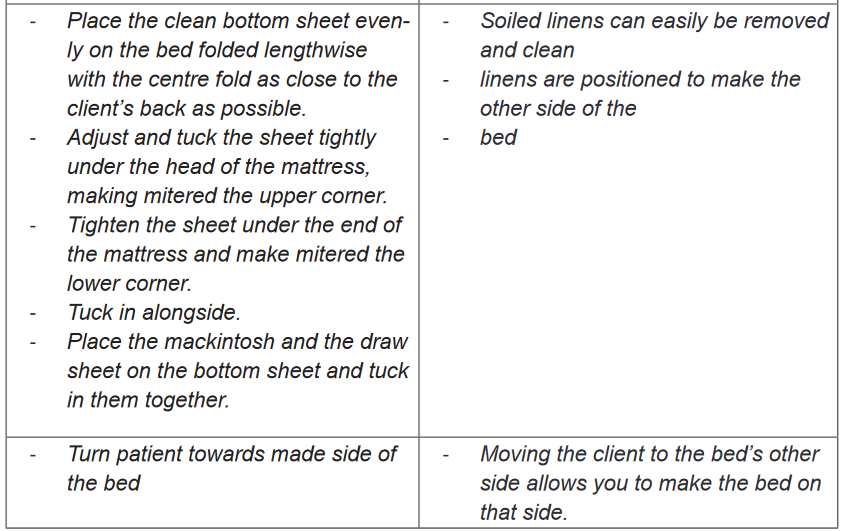
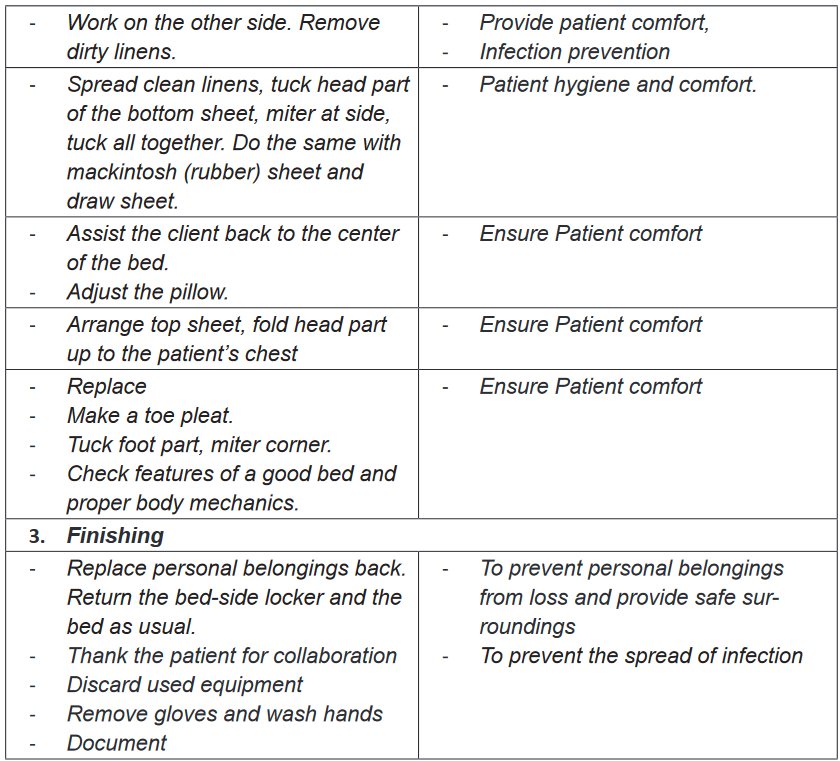
d) Controls viral replication or release from the infected cells.2.2. Bed making
Learning activity 2.2.
Question one
1) The images A & C shown above shows nurses making beds. After
observing the above image, what do you think as the purpose of bed
making?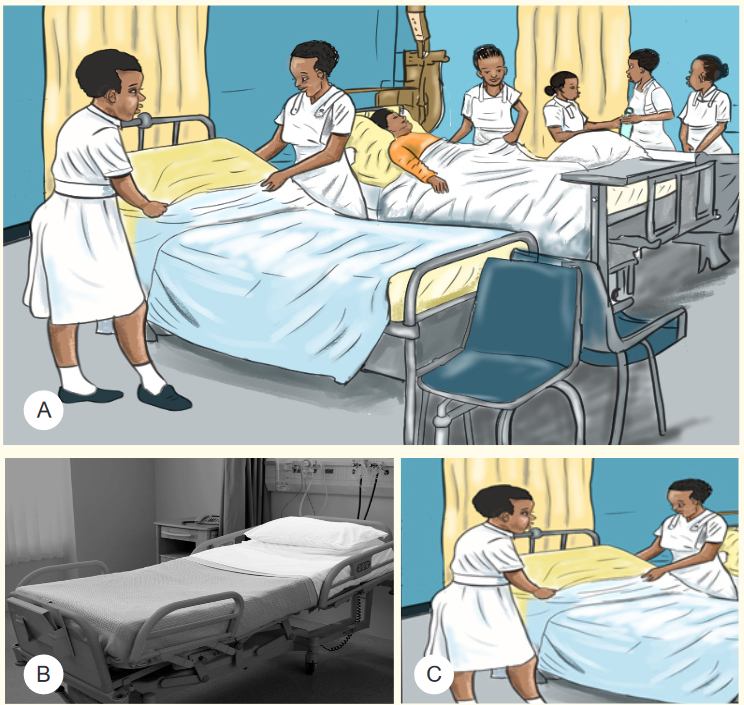

2) List the materials that you have observed in the above image A
3) Observe carefully the images A, B, C and D and highlight the difference
between them
4) Observe the well-made bed and try to make the bed in the same wayQuestion two
Mr. KARINGANIRE is on his day 7 of hospitalization at health facility, is very weak
and is not able to perform any activity, but is able to turn on his left side, he stays
in his bed, and he needs assistance for everything. One morning nurse wants to
change his bed sheets for maintaining the comfort of Mr. KARINGANIRE
1) Based on KARINGANIRE condition is it possible to change his bed
sheets? Yes/No : explain your Answer
2) What do you think as the materials will be used to make KARINGARE’S
bed?
3) What is the importance of listed materials?2.2.1. Definition and Purpose
Bed making is the technique of preparing different types of bed and is required for
all patients. Nurses need to be able to prepare hospital beds in different ways for
specific purposes. Bed making is done for providing comfort, facilitating movement
of the patient and alleviate the pain. It helps to conserve patient’s energy and
maintain current health status. It reduces the risk of infection by maintaining
a clean environment and permitting the physical rest. Bed making is one of the
measures used in prevention of bed sores.2.2.2. Principles of bed making
Prior to bed making, there are principles that have be followed, these are:
1) Arrange bed coverings in order of use
2) Wash hands thoroughly after handling a patient’s bed linen
3) Hold soiled linen away from uniform
4) Linen used for one client is never placed on another client’s bed
5) Soiled linen is placed directly in a portable linen hamper or a pillow case
before it is gathered for disposal.
6) Soiled linen is never shaken in the air because shaking can disseminate
secretions and excretions and the microorganisms they contain.
Fundamental of Nursing | Associate Nursing Program | Senior 4 43
7) When undressing and making a bed, conserve time and energy by undressing and
making up one side as completely as possible before working on the other side.
8) Keep your back straight as you work for preventing back injury
9) To avoid unnecessary movement to the linen supply area, gather all needed
linen before starting to make a bed.
10) While tucking bedding under the mattress the palm of the hand should face
down to protect your nails.2.2.3. Types of bed making
There are 2 two main types of bed making: occupied and unoccupied bed. An
unoccupied bed can be either closed or open. Generally the top covers of an open
bed are folded back (thus the term open bed) to make it easier for a client to get in.
Open and closed beds are made the same way, except that the top sheet, blanket, and
bedspread of a closed bed are drawn up to the top of the bed and under the pillows.While occupied bed is a techniques of making bed for very weak patients who are not
able to get out the bed or restricted in the bed by traction or other therapy condition.2.2.4. Techniques of bed making
a) Unoccupied bed making
Purpose: Unoccupied bed making can be done with different purposes, these are but
not limited to: To prepare the bed for the clients return, to provide a clean environmentTo provides a good appearance and to minimize source of infection.
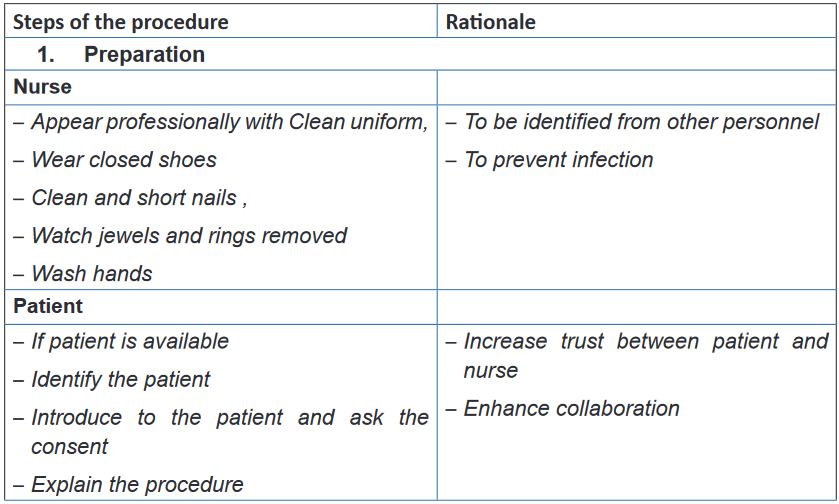
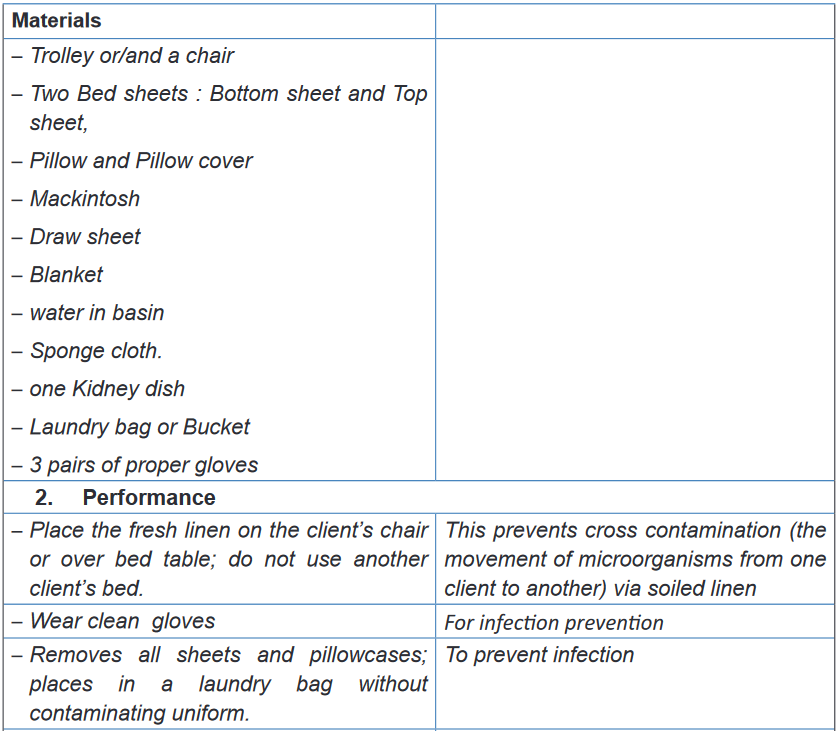
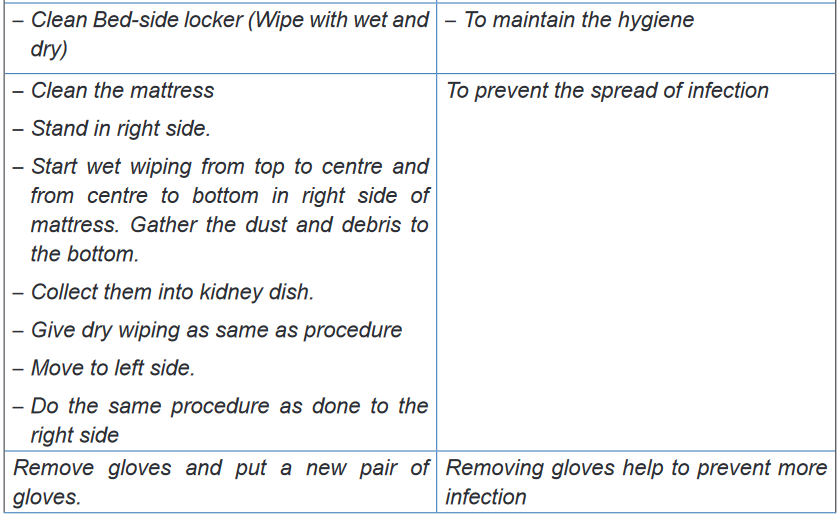
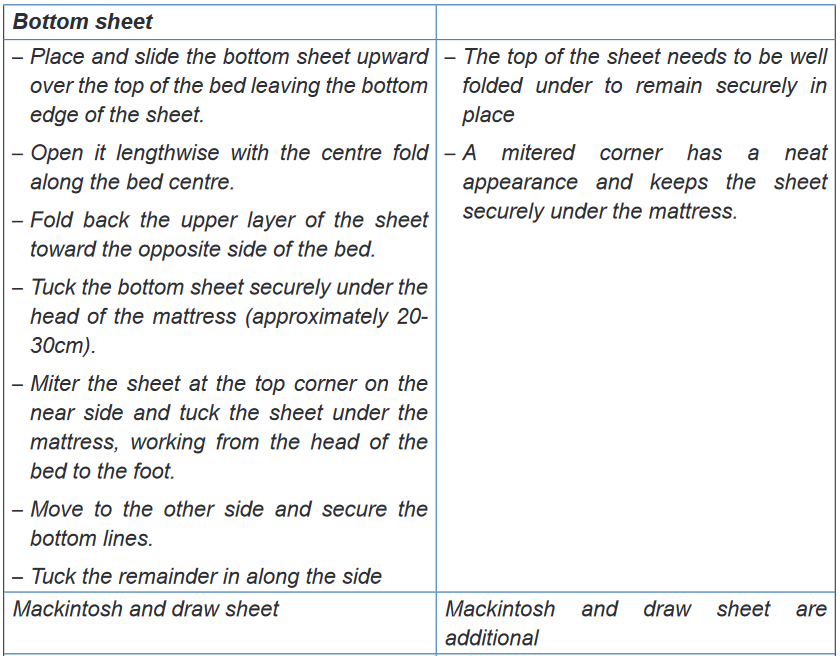
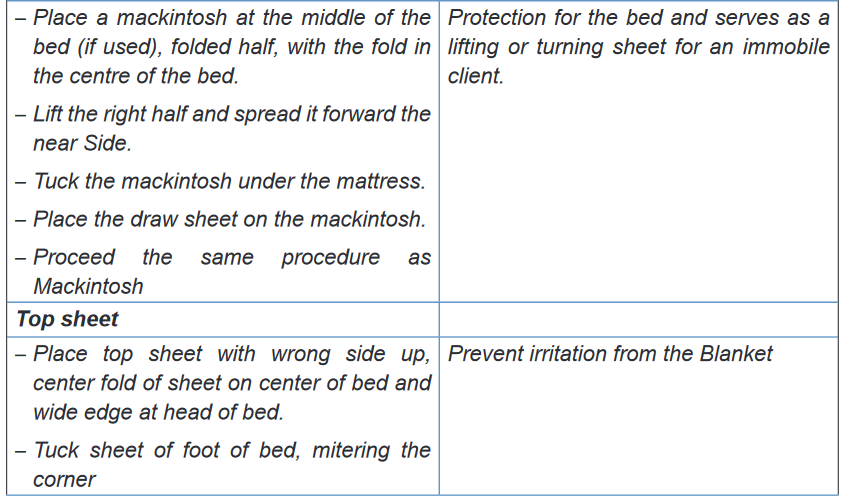
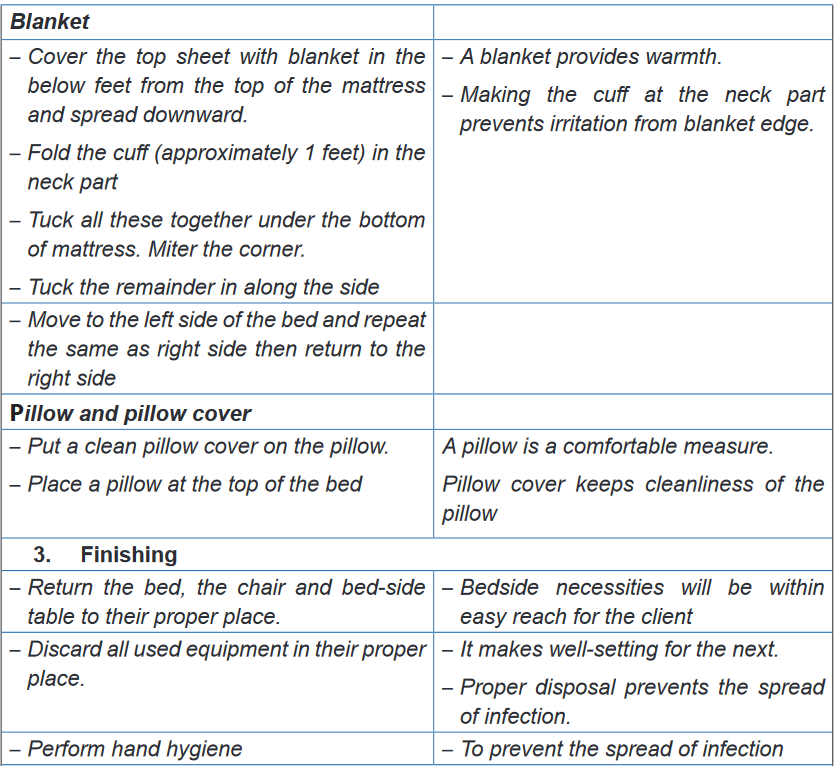
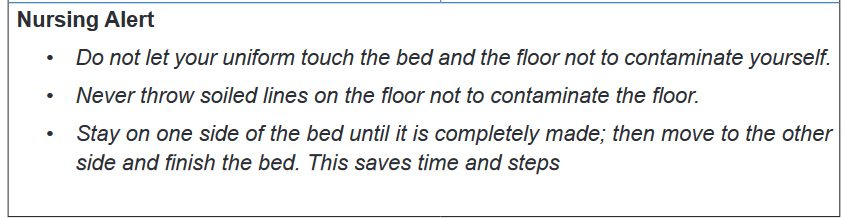
b) Occupied bed making
Purpose: the occupied bed making can be done with different purpose, these are but
not limited to: to provide clean, safe and comfortable bed for the patient, to promote
rest and sleep, to reduce the risk of infection by maintaining a clean environment,
to prevent bed sores and to observe patient and to prevent complications.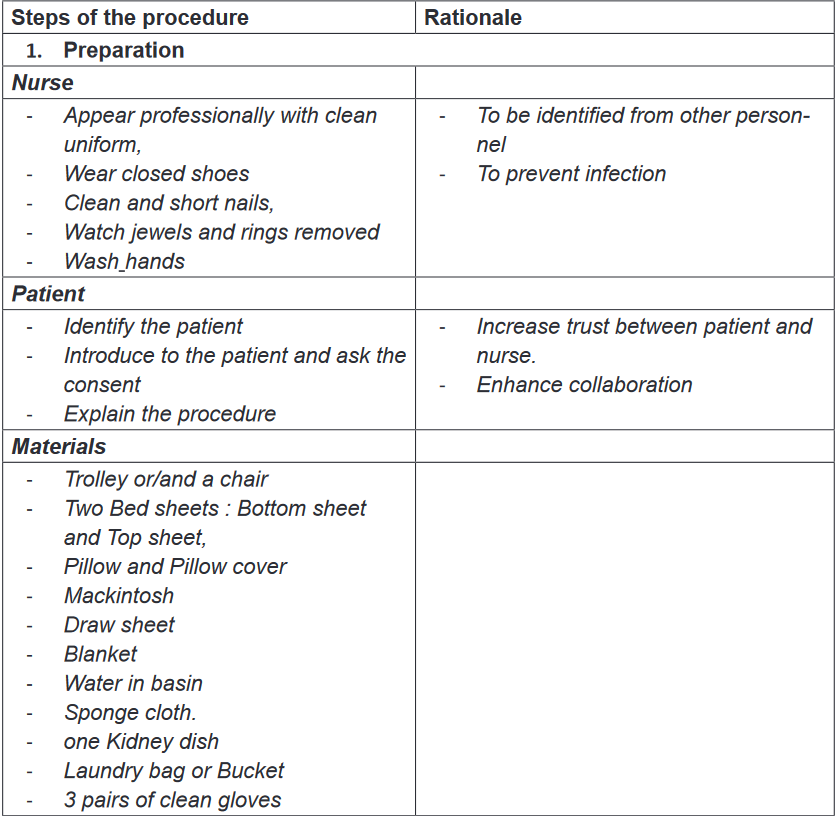
Self-assessment 2.2.
1) Which of the following is true about handling linen?
a) Always carry clean and soiled linen next to your uniform
b) Put the soiled line on the floor when making an occupied bed
c) Soiled linen is never upset(shaken in the air
d) Linen used for one client is directly used for another client’s bed.2) When making an occupied bed
a) The patient is in the bed
b) Keep the bed in the low position
c) Make the top first , then the bottom
d) The patient is out of the bed3) The good ways of making a patient bed are the following except:
a) Complete one side of the bed at time
b) Remove soiled linen a few pieces at a time
c) Move quickly and efficiently
d) Keep you back straight as you work4) When changing the linen that is soiled with body fluids
a) Place the linen on the floor until it can be removed
b) Wear gloves and avoid contact with your uniform
c) Fold or roll with the soiled side out
d) Ask the patient to try to make it to the bathroom next time5) When entering a patient’s room to make a bed, what are the items do
you need to have in hand before entering the patient’s room?6) In skills lab, demonstrate the following techniques of Occupied and
unoccupied bed making.2.3. Bed bath
2.3.1. Complete bed bathLearning activity 2.3.1.
Mr. GAKWAYA was hospitalized for 5 days, he was very sick and he had no
caregiver. A day duty nurse entered in Mr. GAKWAYA’s room and found there was
bad smell. In a very weak voice Mr. GAKWAYA told the nurse that he did not bath
since three days ago. The nurse approached him and found that his bed linens
were dirty and decided to provide a bath. The nurse opened the window to air the
room and went back to the nursing station to prepare the following materials: two
basins, bucket containing water, 2 pair of proper gloves, soap, body lotion/cream,
2 bath gloves, folded screen (for privacy), dirty linen container, bed sheets and
cleaned draw-sheets, individual blanket (Bed-cover), clean clothing or Hospital
gown and bed cleaning material to provide bed bath.
After bed bath Mr. GASANA thanked the nurse and reported that he was feeling
much better and that he will sleep well since last night he did not sleep well.
When the medical team come to visit Mr. GASANA, there was a fresh air in the
room and GASANA was happy.Based on the above scenario, respond to the following questions:
1) Explain the purpose of bed bath
2) Identify the materials needed in bed bath
3) What do you think as the indications of bed bath
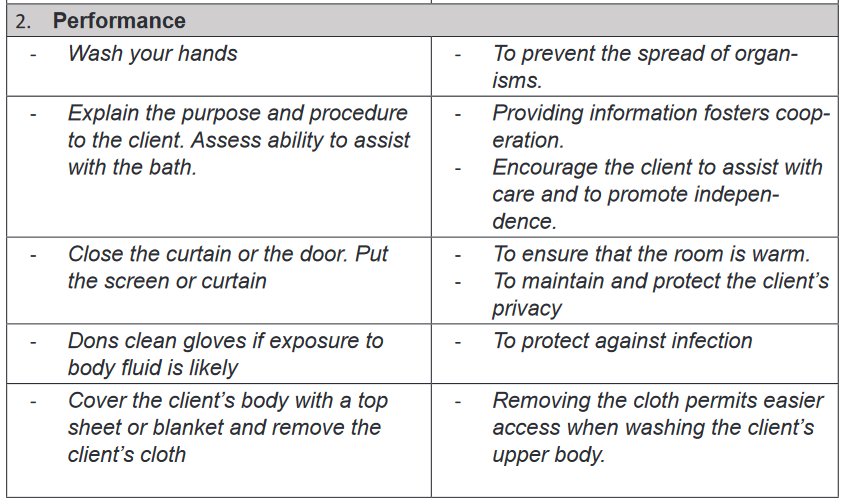
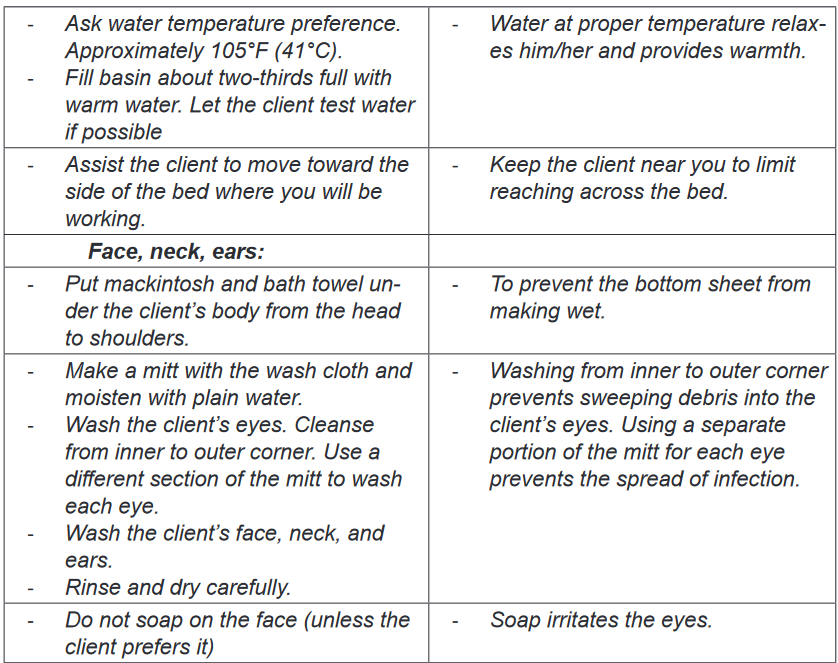
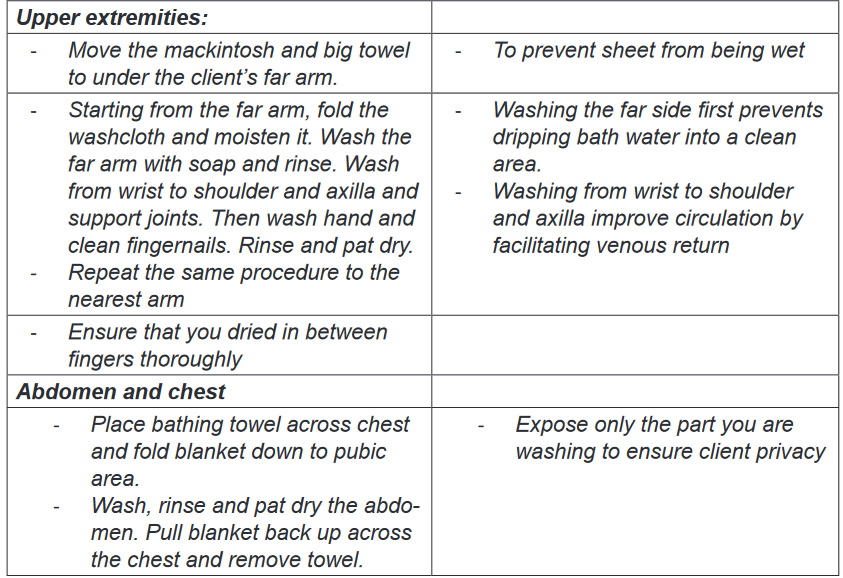
4) Watch the video in the skills lab on bed bath and list the steps of bed bath.a) Importance of bed bath
Bed bath helps to stimulate the functions of the skin and increases circulation.
The bath cleanses body of dirt, bacteria, dead skin cells, sweat and odors. Bed
bath provides the opportunity to assess the skin for lesions and breakdown. Bed
bath help the patient to feel comfortable and relaxed which enhance rest and
sleep that promote healing and restoration of health. In comatose patients, who
have neurological impairment, the bath increases sensation by providing sensory
input for the brain to process. Bathing provides improved self -esteem of the
patient. Providing a bed bath helps to establish the Nurse-patient Relationship
by creating trust and rapport between the nurse and the patient.b) Indications and contraindications
In clinical setting Bed bath is mainly indicated for patients who are physical or
mentally impaired due to different condition such as unconscious or semiconscious
patients, postoperative patients, patient with strict bed rest, paraplegic patients,
orthopedic patients in plaster, cast and traction and seriously ill patients. However,
bed bath may be contraindicated is some cases such as: Hypothermia, convulsion,
fresh burns, varicose veins and advance vascular diseases of the legs and feet.c) Principles of bathing the patient
Before performing bed bath of the patient, the nurse should assess patient
‘abilities; such as to understand and follow directions, the degree of assistance
needed during the bath and tolerance of the physical demands during a bath
such as whether the patient is too weak, too ill, or in too much pain to participate.
During the bathing procedure; patient’s preferences such as bathing timing, culture
should be respected.BOX 2.3.
Principles of bed bathing
• Keep the patient warm at all times
• Position a linen skip near the patient and dispose of used linen
immediately to reduce dispersal of microorganisms and dead skin cells
into the environment
• Only expose the area of the body being washed
• Change water if it becomes dirty or cold and always after washing the
genitalia and sacrum
• Change wash cloths if they become soiled and after washing the genitalia
and sacral area
• Check skin for pressure damage
• Avoid contaminating dressings and drains with water
• Pat the skin dry to reduce the risk of friction damage
• Separate skin folds, and wash and pat them dry
• Use the correct manual handling procedures and equipment to avoid
injury to yourself and the patient
• If the patient is unconscious, remember to talk them through what you
are doing; nurses should not talk over the patient.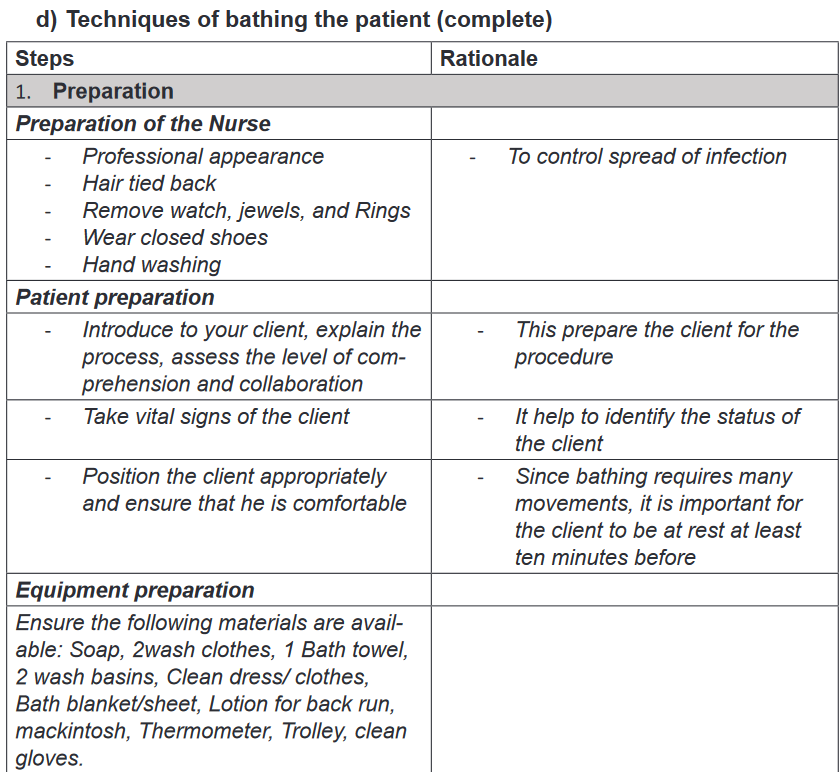
Self -assessment 2.3.1.
Answer the following exercises by marking the lettered response that best
answers the question:
1) When performing a bed bath you should change water when it becomes:
a) Cold, dirty, or excessively soapy.
b) Warm , excessively soapy or too dirty
c) Extremely soapy, dirt or too clear
d) Dirty, old, or too cold2) Which area of the body should not be exposed when washing the upper
and lower limbs?
a) Genitalia.
b) . Feet.
c) Thigh.
d) Stomach area3) When preparing to give complete bed bath to a patient, what would the
nurse do first?
a) Gather the necessary equipment and supplies.
b) Remove the patient’s gown or cloths while maintaining privacy.
c) Assess the patient’s preferences for bathing’s practices
d) Turn the patient in the lateral position4) State at least 5 guidelines that the nurse needs to follow when performing
a complete bed bath.2.3.2. Partial bed bath
Learning activity 2.3.2.
Mrs. MUKANEZA is in the hospital for several days, she is very sick and she is
not able to maintain her body hygiene without assistance. This morning Nurse
Jane did her complete bath.Nurse Jane after completing her bed bath; assisted her to brush her teeth
to ensure a good oral hygiene. While the Nurse was trying to comb the hair
of Mrs. MUKANEZA , she found that the hair were dirty and she decided to
shampooing her.Mrs. MUKANEZA had stool and urines incontinence (not able to control stool
and urines), few hours after her bed bath she passed urines in her bed. Nurse
Jane decided to clean her perineal area and to change her bed sheets.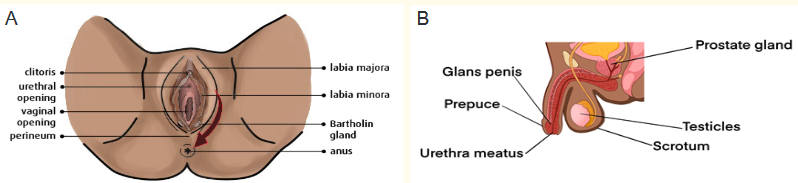
After reading the above scenario and to observe carefully the above image
respond to the following questions:
1) What do you think the oral hygiene will help Mrs. MUKANEZA?2) What do you think as the benefit of shampooing the hair of Mrs.
MUKANEZA?3) Between image A and B what is the image that correspond to the above
scenario and explain why.4) As Mrs. MUKANEZA was passing urines in her bed, nurse Jane
performed her perineal care, observing the image A , what does the
arrow on the image indicate for?5) Observing the image A what do you think as the risk for Mrs. MUKANEZA
if the perineal hygiene is not well kept? And explain why.a) Definition
Partial bed bath consists of bathing selected body part that may cause discomfort if left
unbathed. Most performed partial baths are: perineal care, oral care, foot bath, hair
shampooing and therapeutic baths (SITZ bath).b) Techniques of partial bed bath
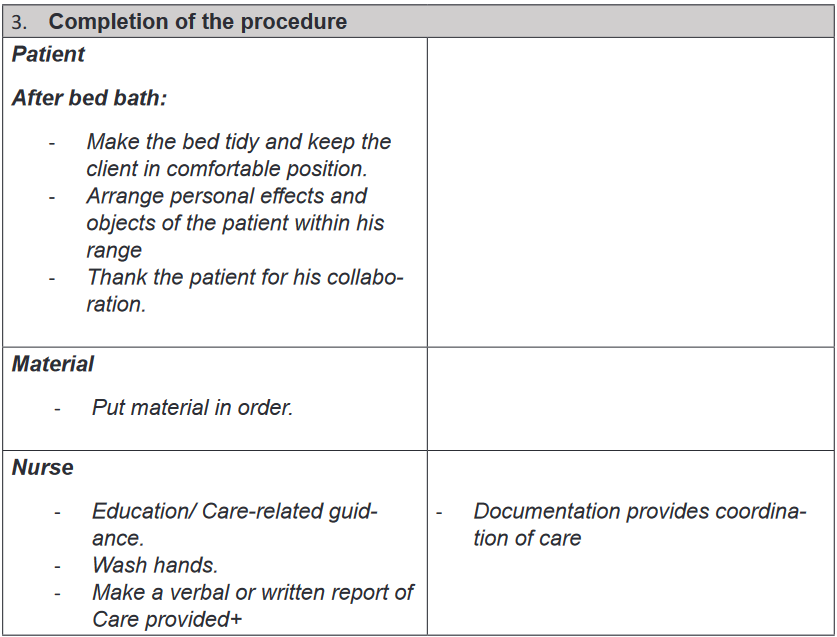
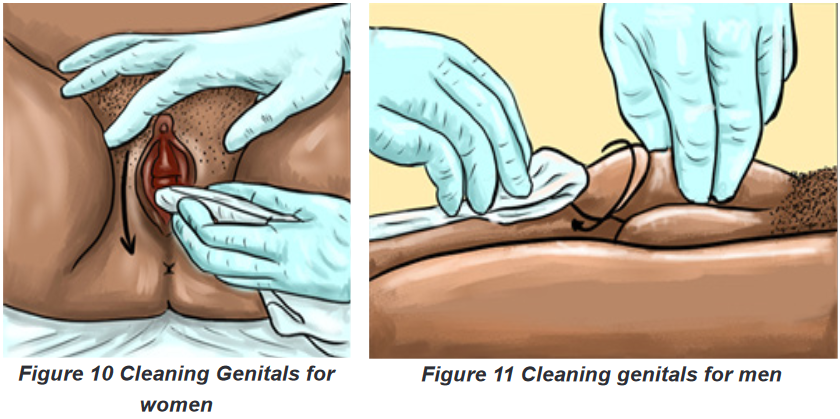
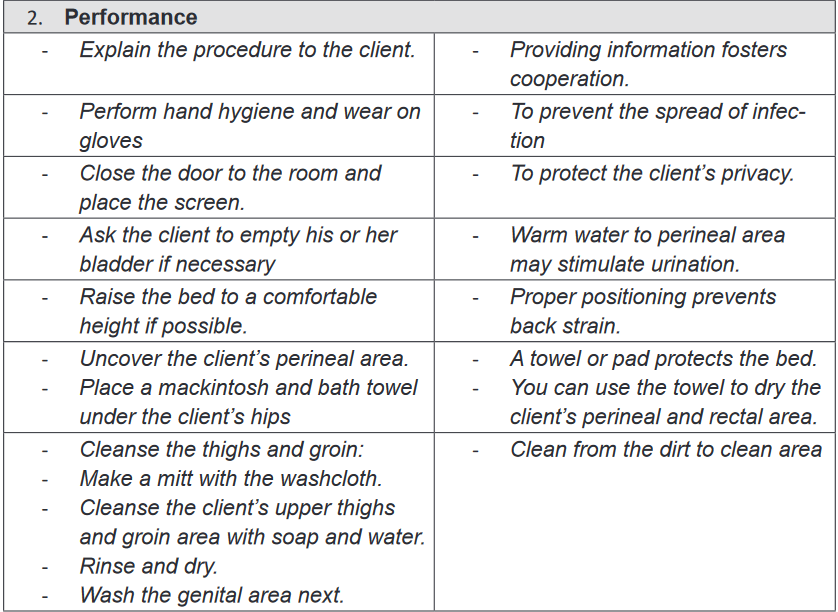
i. Perineal care
Perineal care is also called pericare consists of washing the external genitalia and
surrounding. The perineal area is very exposed to growth of pathogenic organisms
because it is warm, moist and it is not well ventilated. It has many orifices that may
be the entrance of micro-organism in the human body such as urinary meatus,
vaginal orifice and anus.The perineal area is a private part of individual and the perineal care are
embarrassing for many people. The nurse have to build strong relationship with
the client to easy the effectiveness of perineal care. Most people who require a bed
bath from the nurse are able to clean their own genital area with minimal assistance
from the nurse.The perineal care removes normal perineal secretion and odor, it helps to keep
cleanliness and prevent from infection in perineal area and improve the client
comfortable. The perineal care is mostly indicated for patient who are unable to
do self-care, patient with genito -urinary tract infection, patient with incontinence
of urine and stool, patient with indwelling catheter (urinary catheter), postpartum
patients, patients after surgery on the genitor -urinary system and patients with
injury, ulcer or surgery on perineal area.The most important principle to respect during perineal care is to clean the perineum
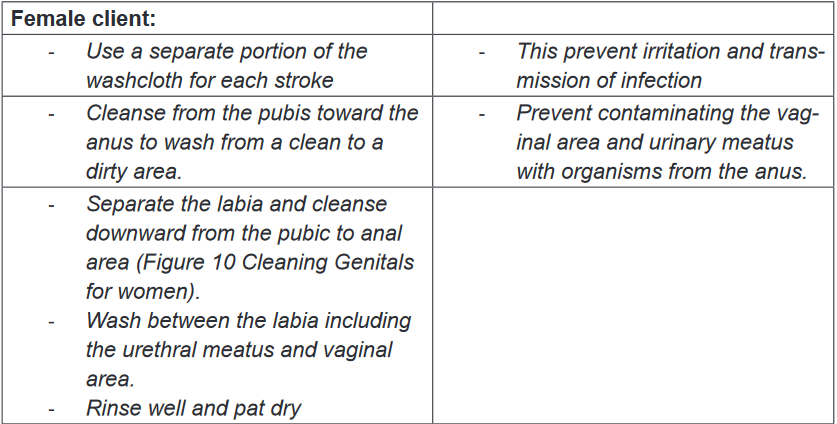
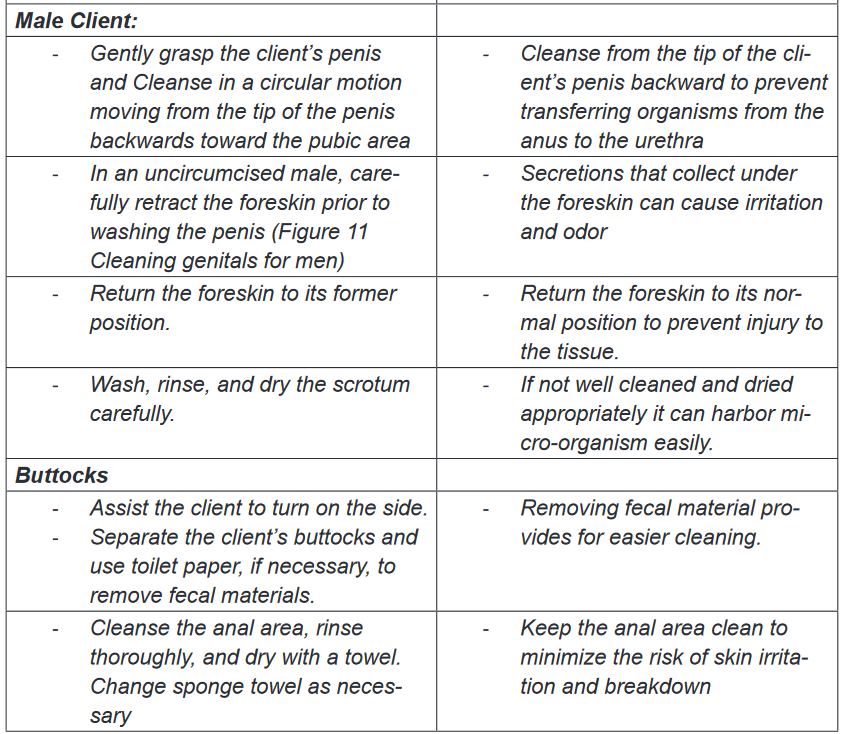
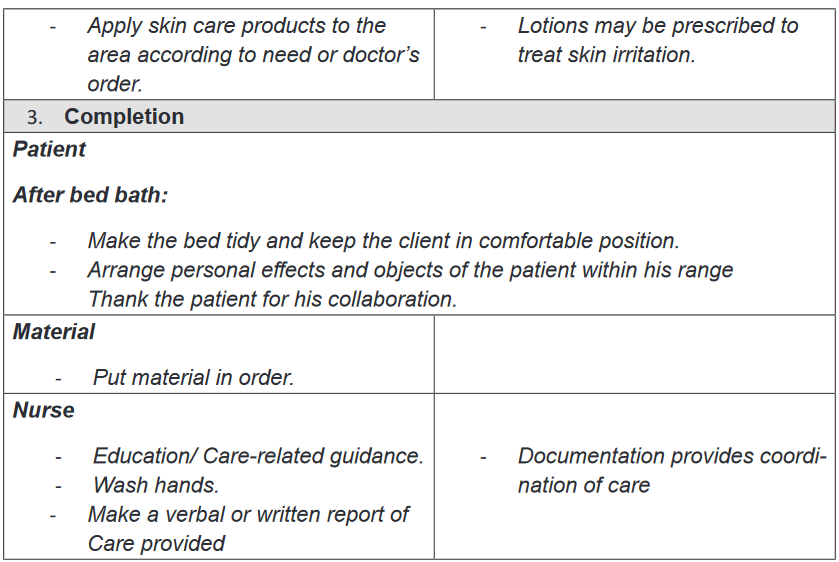
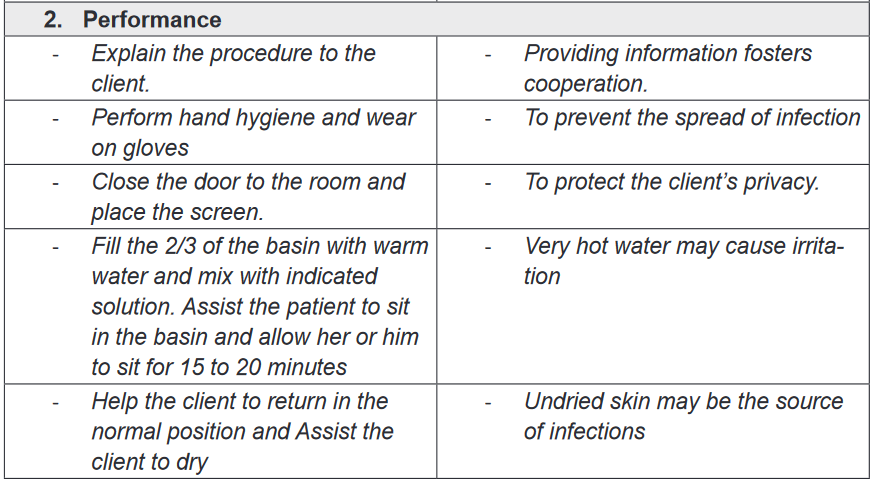
from the cleanest to less clean and to preserve patient privacy.Techniques of perineal care
Purpose: to keep cleanliness and prevent from infection in perineal area and
improve the client comfortable.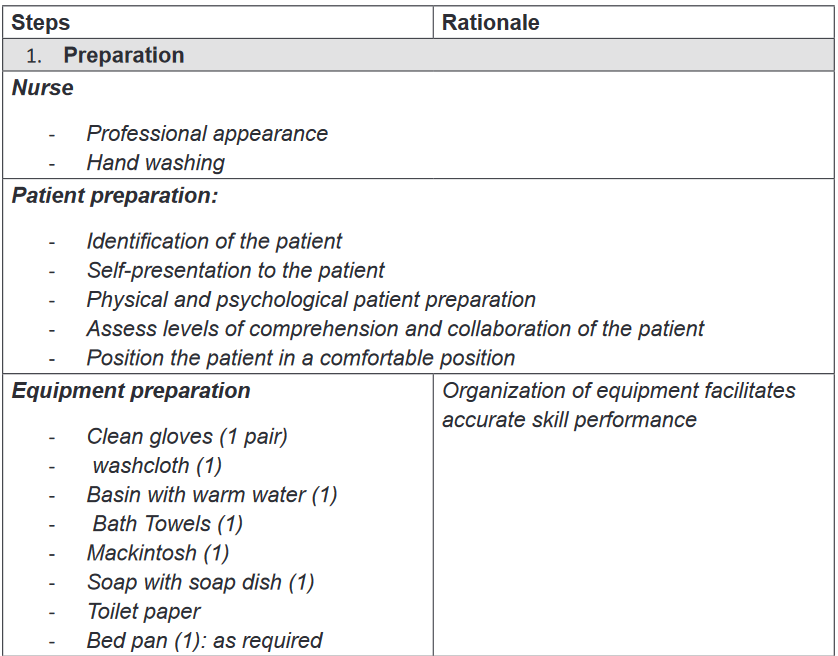
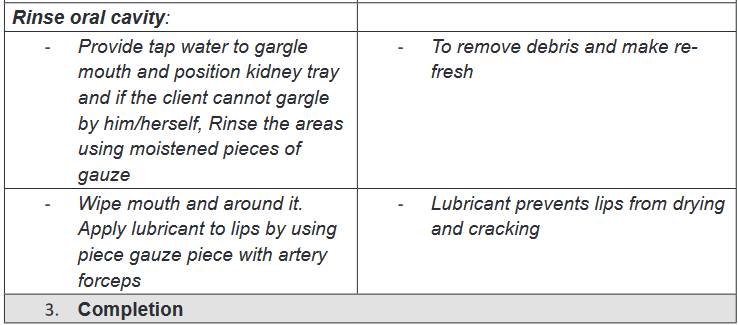
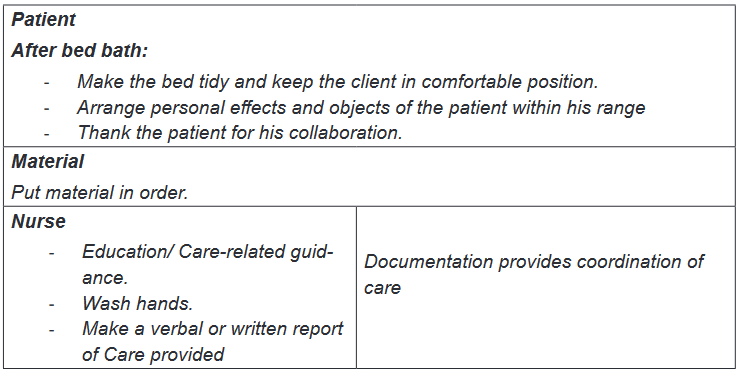
ii. Oral care
Oral care is a fundamental nursing care that consist of keeping mouth and teeth
clean and healthy. Each patient needs oral care; the patients who are confined in
bed with decreased physical and mental capacity need assistance to provide oral
carePurpose: to keep the mucosa clean, soft, moist and intact, to keep the lips clean,
soft, moist and intact, to prevent oral infections, to remove food debris as well as
dental plaque without damaging the gum, to alleviate pain, discomfort and enhance
oral intake with appetite and to prevent halitosis or relieve it and freshen the mouth.
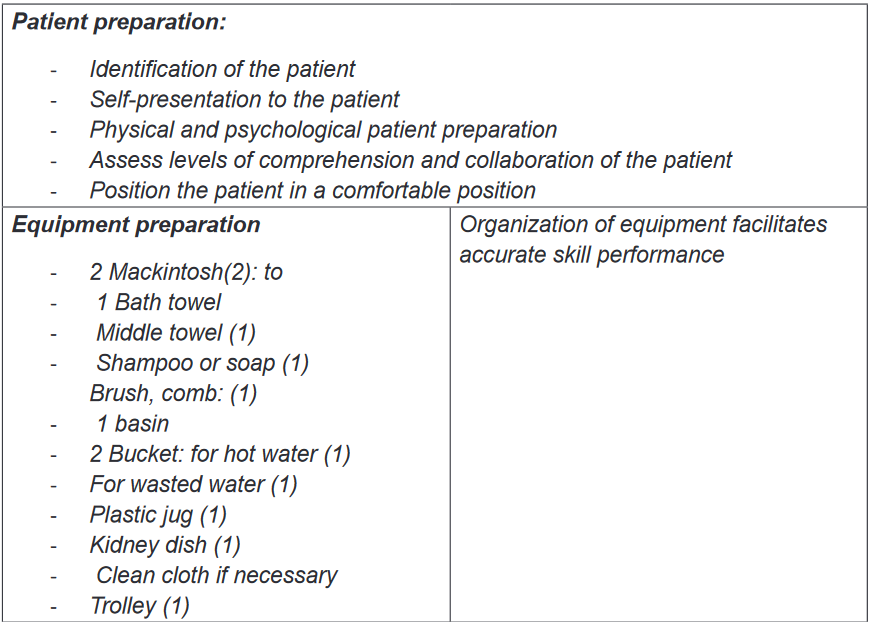
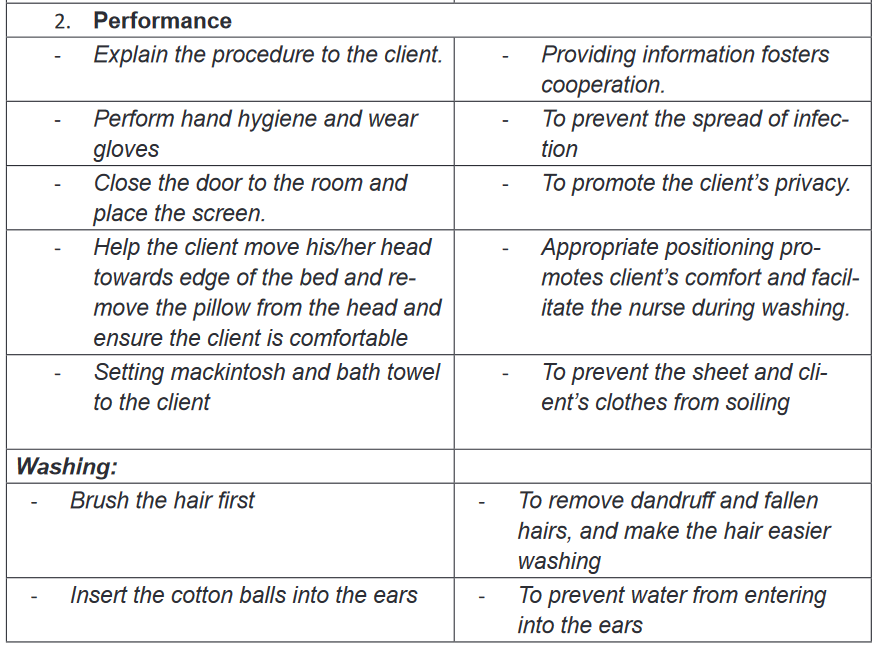
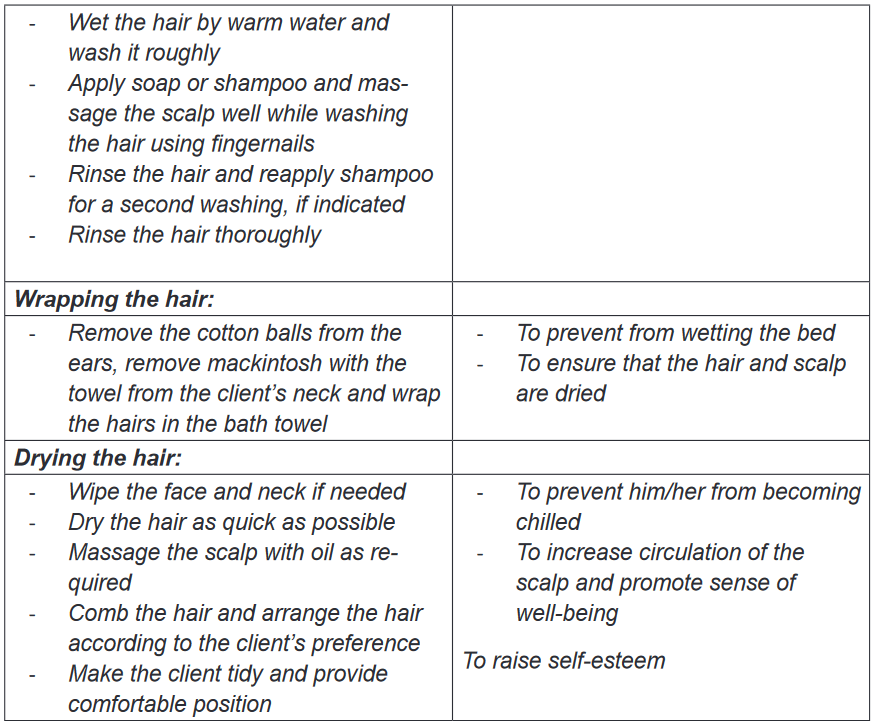
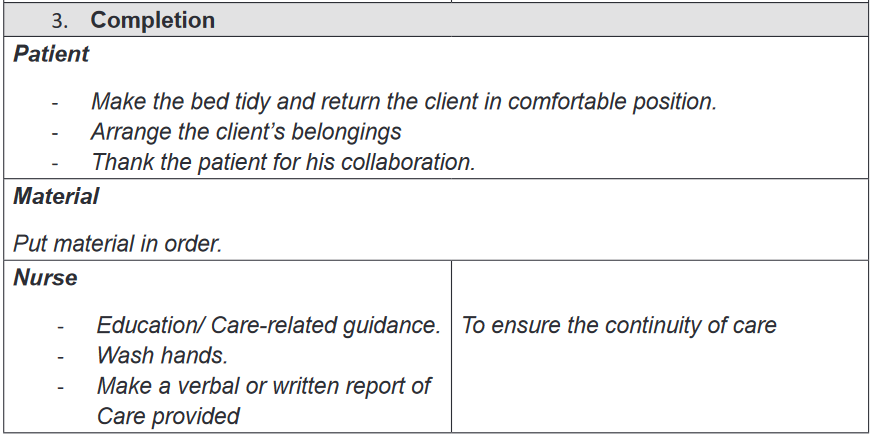
iii. Shampooing
Purpose: It helps to maintain personal hygiene of the client, to increase circulation
to the scalp and hair, promote growing of hair and to make him/her feel refreshed.
Same as other types of bed bath, shampooing is indicated to all patient who are
unable to care for themselves.
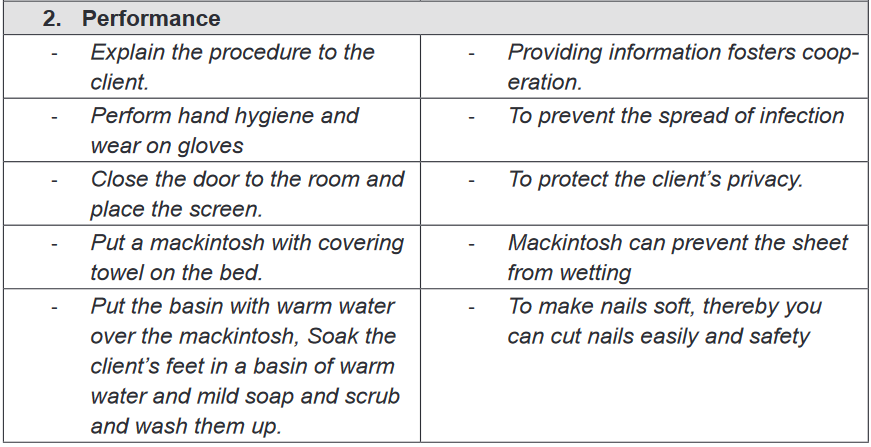
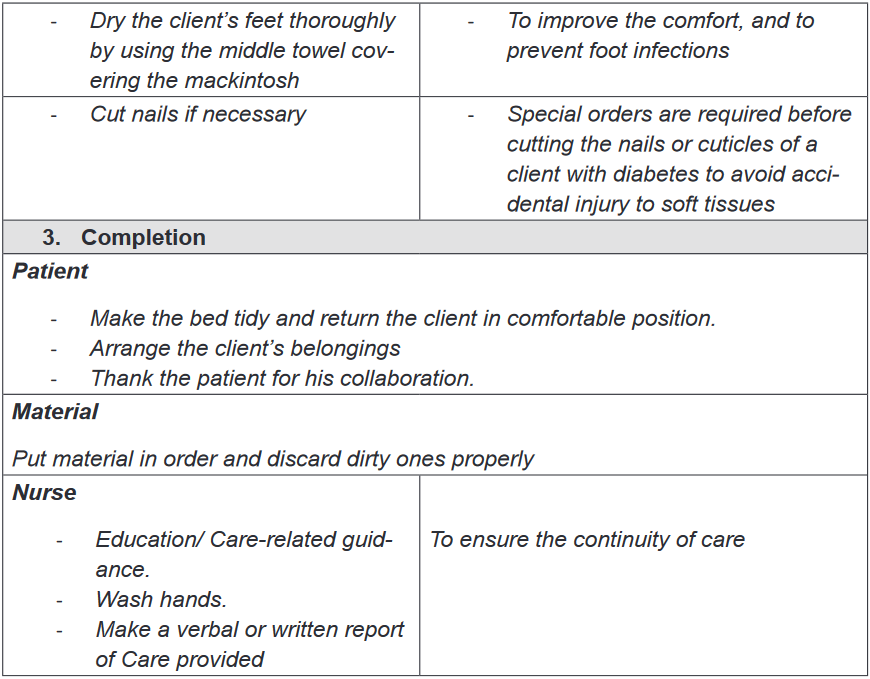
iv. Foot bath
The feet are essential for ambulation and merit attention even when people are
confined to bed. The purpose of feet bath is to maintain personal hygiene of the
client, Soothe sore muscles, to increase circulation and to make him/her feel
refreshed and relaxed. The foot bath is also indicated to all patient with physical
incapacity and is contraindicated to patient with foot injuries.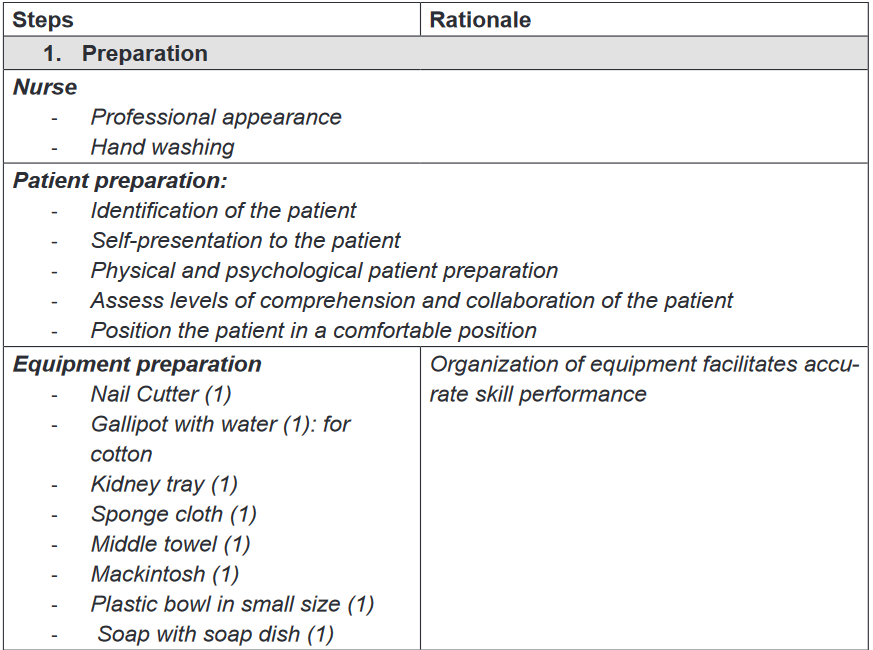 \
\
V. Therapeutic bath: Sitz bath
Definition and purpose
Therapeutic baths are baths that have physical effects; they are given to soothe
irritated skin or to treat an area such as perineum. Medications are placed in water
and the client remain in water for a designed time. A therapeutic bath often last for
20 to 30 minutes.A Sitz bath is a type of therapy that consist of sitting in warm, shallow water to clean
the perineum, which is the space between the rectum and vulva or scrotum. Sitz
is from the German word “Sitzen” which means “to sit”. A Sitz bath helps to clean
and treat certain problems in the anal area, genital area and the perineum. It helps
to increase blood flow to these areas and relax the muscle. A Sitz bath helps to
relieve from pain or itching in the anal and genital area.Indications and contraindications
Sitz bath can be hot or cold; the hot Sitz bath is indicated in case of ovarian pain,
uterine cramps, testicular pain, prostatic problems, intestinal or renal colic, sciatica,
headache; and the cold Sitz bath is indicated in case of uterine prolapse, cystocele,rectocele, constipation and heavy or prolonged menstruation. The alternate hot
and cold Sitz bath is used in case of chronic UTI (Urinary tract infection), pelvic
inflammatory disease, hemorrhoids, fissure, postpartum Contraindications.The Sitz bath is contraindicated in case of hemorrhages, menorrhagia, acute
congestion, acute inflammation, painful conditions with spasms or colic, and heart
problems.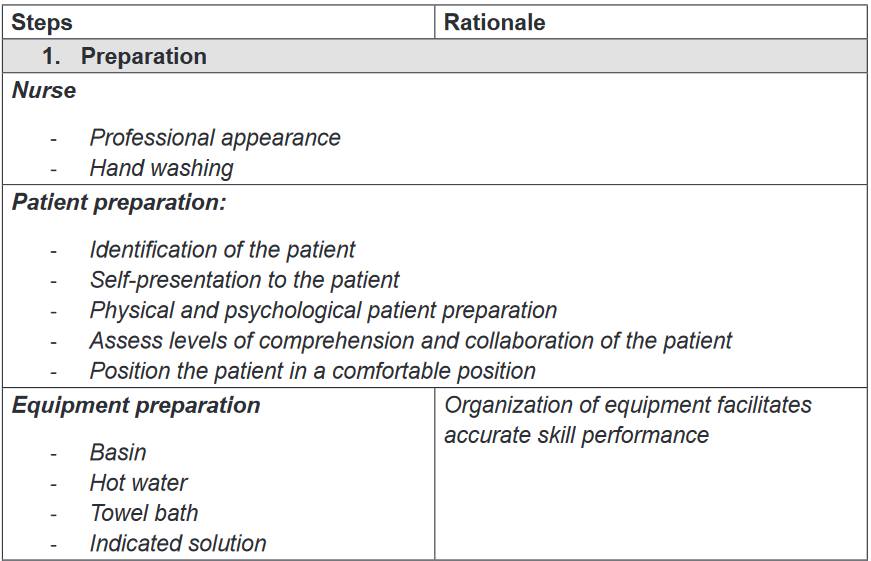
Self-assessment 2.3.
1) When providing peri-care always wash from ______ to _____
2) What is perineal care
a) Washing a patient back
b) Washing a patient’s genital and anal area
c) Giving a complete bath
d) Washing patient’s genitalia only3) For an uncircumcised male patient , the nurse needs to first:
a) Pull back the foreskin
b) Turn the penis to the side
c) Push the foreskin foreword
d) Gently pat the area with a dry towel before washing4) Which of the following statements is correct regarding perineal care?
a) Always wear gloves when providing pericare.
b) Wash the peri area with soap and cold water.
c) Wash from back to front when providing peri care.
d) The client lies on his/her stomach during peri care.5) Why the client is offered the bedpan or urinal before beginning peri care?
6) List two purposes of giving peri care.
7) You ARE giving oral care to unconscious person ,which action is incorrect
a) Provide privacy
b) Place a kidney basin under the chin
c) Place the mackintosh and towel on the neck to chest
d) With your fingers open the client’s mouth.8) In order to prevent aspiration when performing oral hygiene on a person
who is unconscious, they are placed
a) In high Fowler’s
b) In supine
c) In side lying position
d) Reverse Trendelenburg9) Enumerate at least two purposes of foot care
10) Explain the purpose of a Sitz bath
11) During a Sitz bath the patient sit in water for:
a) 45-60minutes
b) 5-10 minutes
c) 40-50 minutes
d) 20-30 minutes2.4. Bed sores or Pressure ulcers
Learning activity 2.4.
Mrs. MUKANKIKO, a 75 years old patient was hospitalized for four weeks,
she was severely sick and she couldn’t move nor turn in her bed and she was
malnourished. While providing bed bath, Mr. KWIZERA, a student nurse in his
first clinical practice, has found that she had redness on her buttocks (redness:
is one the signs of bedsores. A bedsore is a damage to an area of the skin
caused by unrelieved pressure on the area for a long time) due to prolonged
compression on the side she was lying on.Mr. KWIZERA recalled that bedsores can be prevented by changing position,
maintaining adequate nutrition, hygiene (body and surrounding hygiene), and
exercises to promote blood circulation and decided to change position every
two hours for Mrs. MUKANKIKO and to do advocacy to the nutritionist and
social workers for they can ensure good nutrition.
1) What do you think as the risk factors of bedsores?
2) What do you think Mr. KWIZERA could do to prevent bedsores?
3) Basing on the Figure 15, classify Mrs. MUKANKIKO’s bedsore stage.2.4.1. Definition of bedsores
Bed sores also called pressures ulcers or decubitus sores are lesions caused by
unrelieved pressure, including shearing and friction forces. Bed sores are a big
problem in hospital settings. Bed sores are due to localized deficiency of blood
supply to the tissues. The tissue is compressed between two surfaces, usually the
surface of the bed and the bony skeleton. When blood cannot reach the tissue, cells
are deprived of oxygen and nutrients, waste products of metabolism accumulate in
the cells and the tissue consequently dies.2.4.2. Risk factors of bed sores
Immobility that leads to unrelieved pressure to the skin over a bony prominence
is the most factor in development of pressure ulcers. Individual risk factors for
pressure ulcers may be categorized as extrinsic or intrinsic. Extrinsic factors are
external conditions in the immediate environment that place a vulnerable individual
at risk such as Friction and shearing, force (pressure) and moisture. Intrinsic factors
are conditions and comorbidities peculiar to the individual that confer risk such
as: immobility and inactivity, inadequate nutrition, fecal and urinal incontinence,
decreased mental status, diminished sensation, excessive body heat, advanced
age and certain chronic condition (Diabetes). Below are detailed risk factors• Friction and shearing force: Friction is a force acting parallel to the skin
surface. (Sheets rubbing against skin create friction).Friction can abrade the
skin, remove the superficial layers, and make it more prone to breakdown.
Shearing is a combination of pressure and friction. They damage blood
vessels and tissue area.• Immobility: refers to reduction in the amount and control of movement.
Normally people move when they experience discomfort due to pressure on
an area of the body. However decreased activity, extreme weakness, pain
or any cause of decreased activity can hinder person’s ability to change
positions independently and relieve the pressure, even if the person can
perceive pressure.• Inadequate nutrition: Prolonged inadequate nutrition causes weight loss,
muscle atrophy and loss of subcutaneous tissue. These three reduce the
amount of padding between the skin and bones, thus increasing the risk of
pressure ulcer development. Inadequate intake of protein, carbohydrates,
fluids, zinc and vitamin C contributes to pressure ulcer formation.• Fecal and urinary incontinence: Moisture from incontinence promotes
skin maceration (tissue softened by prolonged wetting or soaking), making
the epidermis more easily eroded and susceptible to injury. Digestive
enzymes in feces, gastric tube drainage and urea in urines also contribute
to skin excoriation. Any accumulation secretion or excretions irritate the skin,
harbours microorganisms and makes an individual prone to skin breakdown
and infection.• Decreased mental status: Individuals with decrease level of awareness are
at risk because they are less able to recognize and respond to pain associated
with prolonged pressure.• Diminished sensation: Loss of sensation reduces a person’s ability to
respond to trauma, to injurious heat and cold and to the tingling (pins and
needles).
Fundamental of Nursing | Associate Nursing Program | Senior 476• Excessive body heat: An elevated body temperature increases the
metabolic rate, thus increasing cellular need for oxygen. This increased need
is particularly severe in cells of an area under pressure, which are already
oxygen deficient. Severe infections with accompanying elevated body
temperature may affect the body’s ability to deal with the effects of tissue
compression.• Advanced age: ageing processes bring about several changes in skin and its
supporting structures, making the older person more prone to impaired skin
integrity. These changes are loss of lean body mass, generalized thinning
of the epidermis, decreased strength end elasticity, increased dryness,
diminished pain perception and diminished venous and arterial flow due to
ageing vascular walls.• Chronic medical conditions: Certain chronic conditions such as diabetes
and cardiovascular disease are risk factors for skin breakdown and delayed
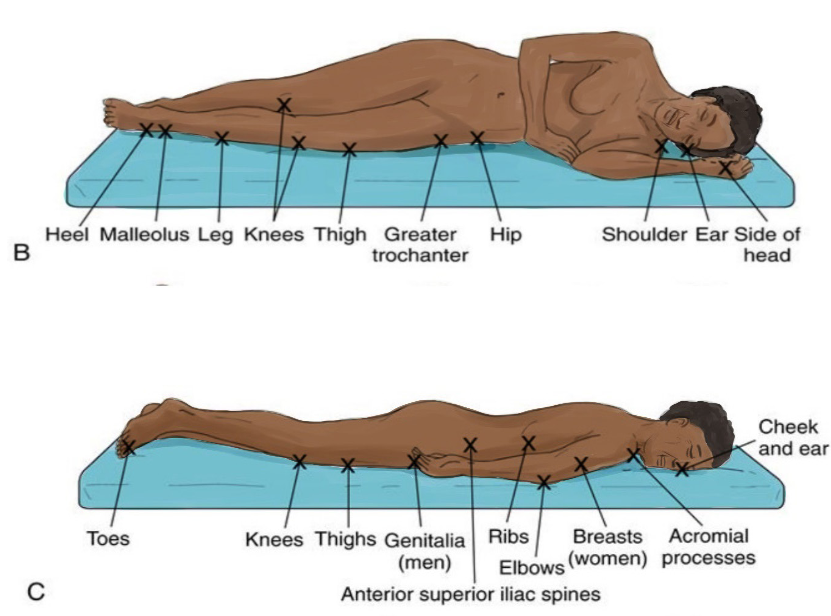
healingAreas where bedsores occur
Bed sores mostly develop in areas where bones are close to the surface (bony
prominences) and areas that are under the high pressure. For People who uses
wheelchairs, bedsores occur on tailbone or buttocks, shoulder blades and spine,
backs of arms and legs where they rest against chair. For people who stay in bed,
bed sores develop on the back or sides of the head, the should blades, the hip,
lower back or tailbone, the heels, ankles and skin behind the knees.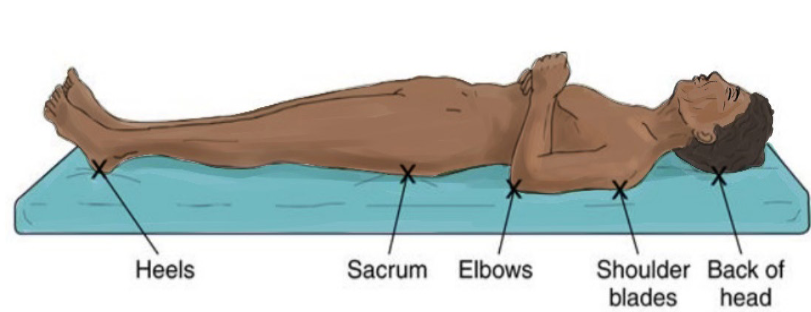
2.4.3. Stages of bed sores
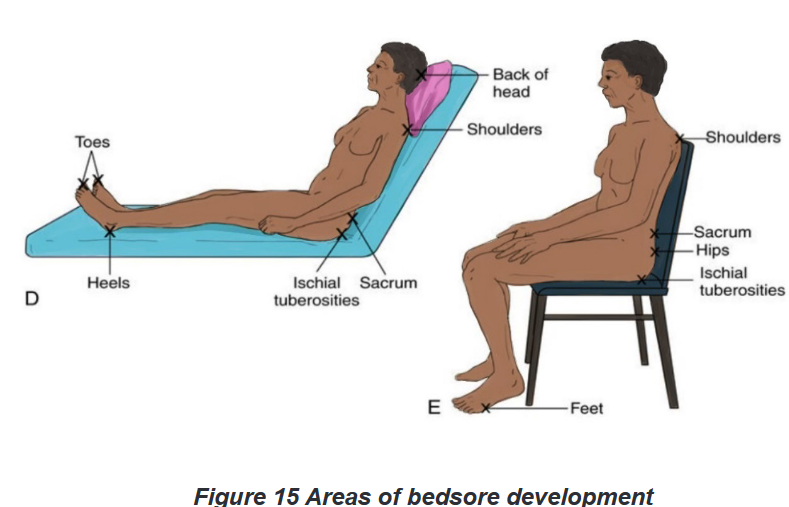
Bed sores have four clinical stages as shown s below in details:a) Staged 1-Pressure injury: Non blanchable erythema
This first stage is characterized by intact skin with non -blanchable redness of a
localized area usually over a bony prominence. In darkly pigmented skin may not
have visible blanching; its color may differ from the surrounding area. The area
may be painful, firm, soft, and warm or cool compared to adjacent tissue. It may be
difficult to detect in individuals with dark skin tones.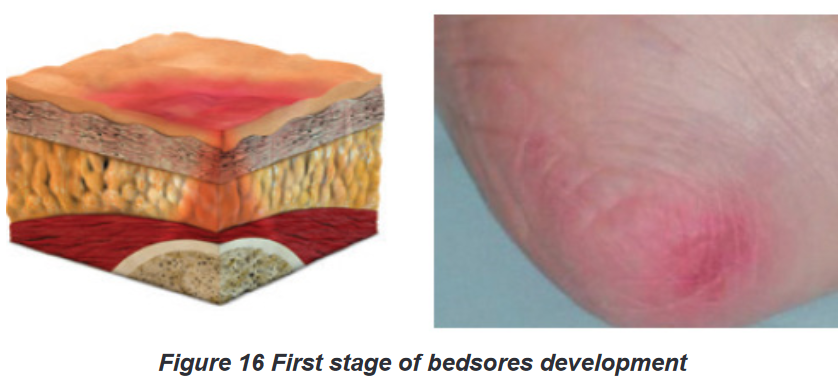
b) Stage 2- Pressure injury: partial thickness skin loss
The second stage is characterized by partial thickness loss of dermis presenting
as a shallow, open wound with a red-pink wound bed, without slough. May
also present as an intact or open/ruptured serum-filled blister. Presents as a shiny
or dry, shallow ulcer without slough or bruising.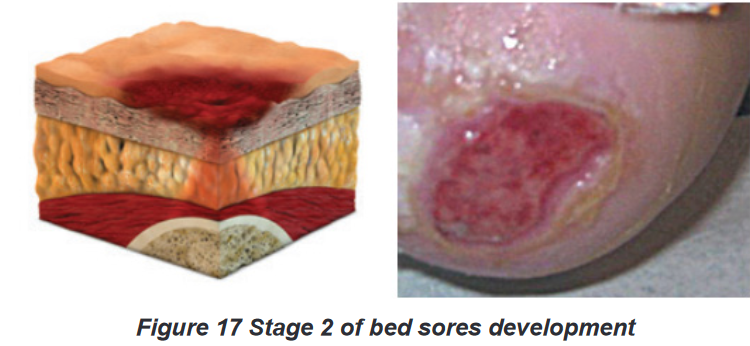
c) Stage 3-Pressure injury: full thickness skin loss
The third stage is characterized by full thickness tissue loss. Subcutaneous fat may
be visible but bone, tendon or muscles are not exposed. Slough may be present but
does not obscure the depth of tissue loss. May include undermining and tunneling.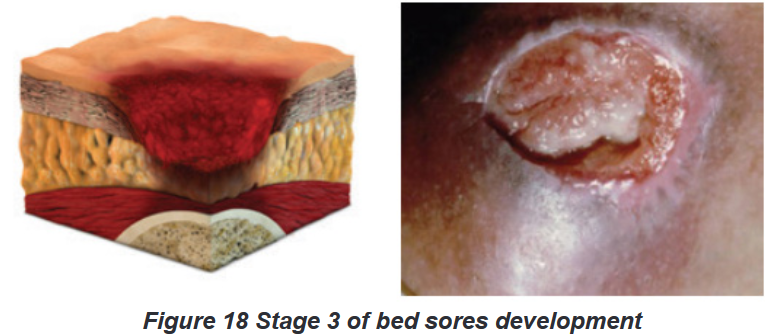
d) Stage 4- Pressure injury: full thickness tissue loss
The fourth stage is characterized by full thickness tissue loss with exposed bone,
tendon or muscle. Slough or eschar may be present on some parts of the wound bed.
2.4.4. Prevention and management of bedsores
Management of bed sores is complex; early identification of risk factors is key
to prevention and management of bed sores. Prevention of bedsores consist of
providing adequate body hygiene by keeping the skin clean and dry and keeping
the bed tidy and dry; turning and repositioning the client every two hours prevent
bedsores; and adequate nutrition with enough calories, vitamins, minerals, fluids
and protein help to prevent bedsores and accelerate healing process of sores.Management of the wound depend on the stage of bedsores; consist of wound
cleaning, removing the damaged, infected or dead tissue(debridement) and
transplanting healthy skin to the wound area (skin grafts). Administration of
antibiotics may be necessary to treat infection that may associated with bedsores.Self-assessment 2.4.
1) The most common areas where pressure ulcers occur are the
a) Hands and neck
b) Coccyx and neck
c) Sacrum and coccyx
d) Back of the head and hands2) In which of the following pressure injury stages is the skin still intact?
a) Stage 1
b) Stage 2
c) Stage 4
d) Stage 33) The following are risk factors of bed sores except:
a) Advanced age
b) Physical exercise
c) Poor Nutrition
d) Diabetes4) The pressure ulcers can be caused by
a) Wrinkled linen
b) Soiled linen
c) Dragging the patient across linens
d) All the above5) Staging systems for pressure ulcers are based on the depth of tissue
destroyed. Briefly describe each stage.2.5. Moving and positioning patients in bed
Learning activity 2.5.1.
Look at the following table that describe different positions that a person may
(be assisted to) take depending on her or his status and condition and attempt
the questions which follow it.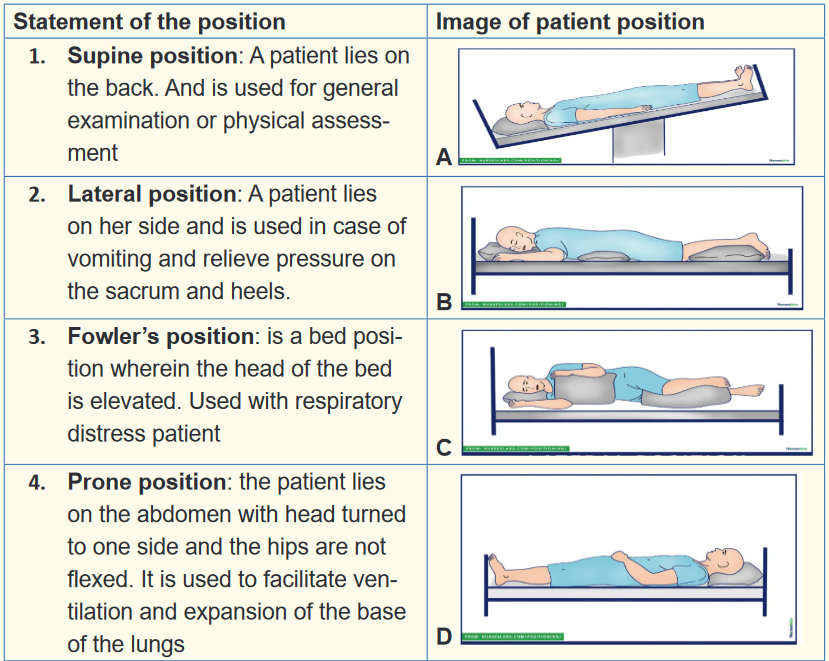
1) Match each statement with its corresponding image
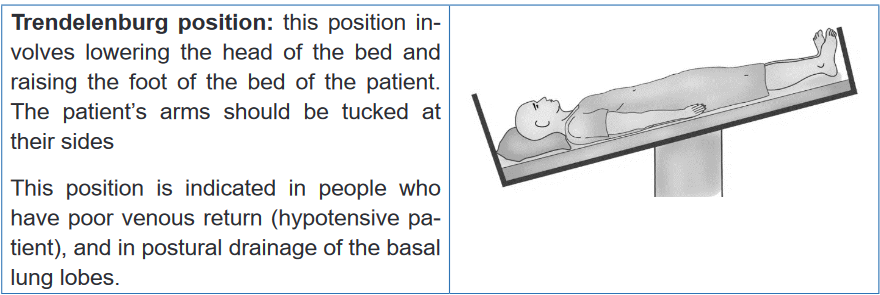
2) After sustaining a road traffic accident, Mr. RUKUNDO has bled heavily.
Which appropriate position for Mr. RUKUNDO and why?
3) Mrs. MUGWANEZA was lying on her back position and you noticed that
she is vomiting. What is the suitable position to her?Learning activity 2.5.2.
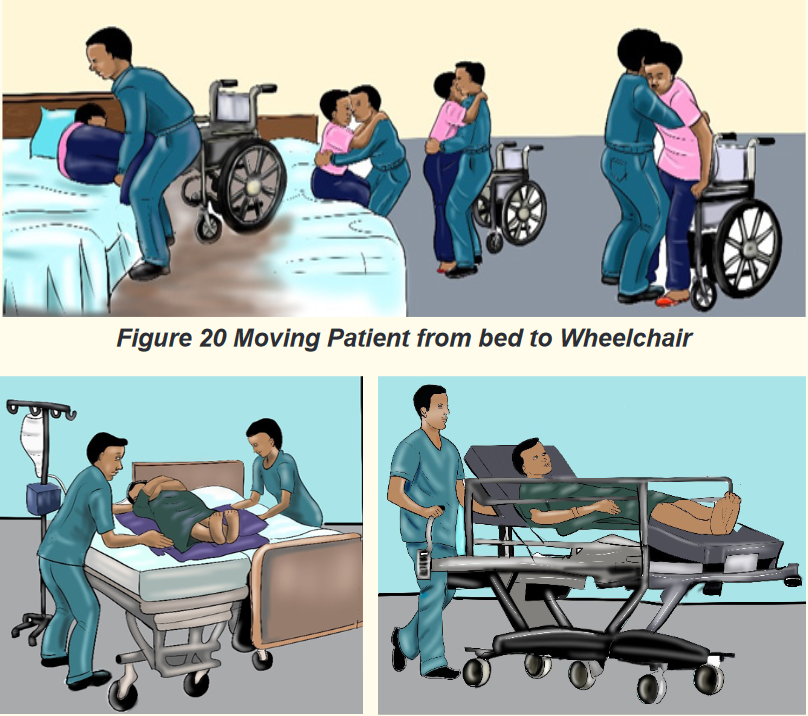
Figure 21 Moving patient from bed to stretcher (a stretcher is a device
used to carry a person who must lie flat and can’t move on their own)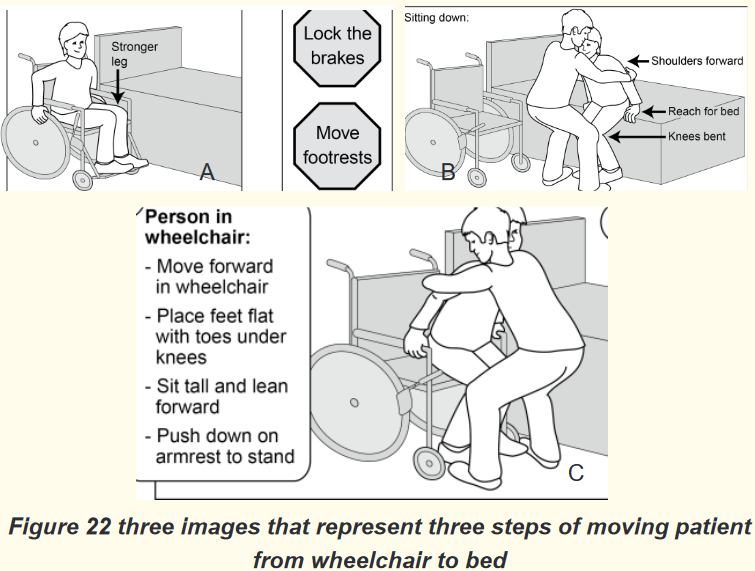
1) Look at the Figures 20, 21 &22 and think about the purpose of moving
patient from bed to wheelchair
2) From the Figure 21, what do you think is the purpose of moving
patient from bed to stretcher
3) Observe the Figure 22 and provide the chronological order of steps.
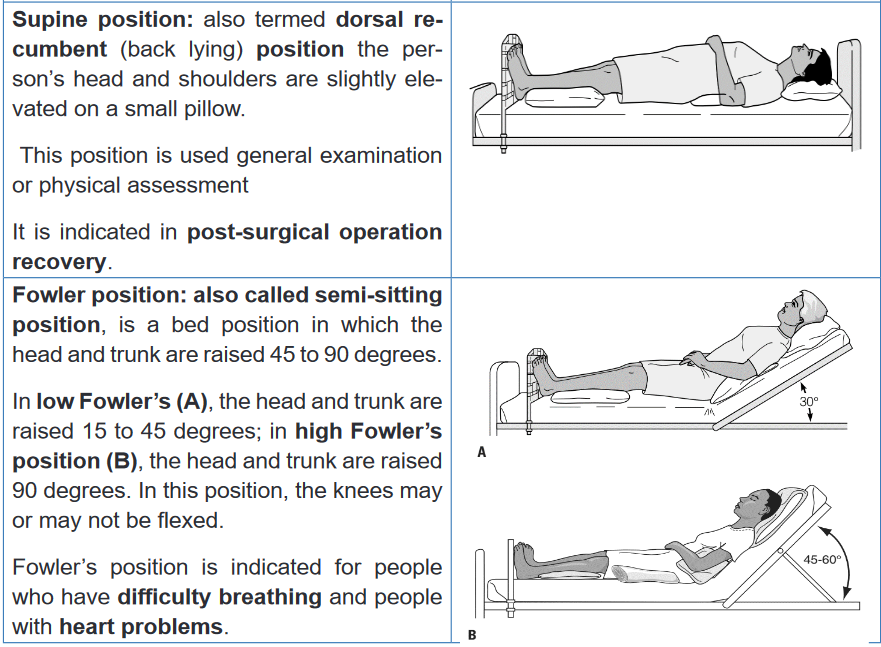
Think about how these persons will use their muscle during the move.2.5.1. Positioning patients
a) Patient positions
Patients with impaired nervous, skeletal or muscular system functioning
and increased weakness and fatigue often require assistance from nurses for
positioning while in bed or sitting and for moving. Positioning a patient in good
body alignment and changing position carefully and systematically are essential
aspect of nursing practice.Any position, correct or incorrect, can be detrimental if maintained for a prolonged
period of time. Frequent changes of position help to prevent muscle discomfort,
undue pressure resulting in pressure injuries, damage to superficial nerves and
blood vessels and contractures. Position changes also maintain muscle tone and
stimulate postural reflexes.Positioning materials and aids are available but sometimes can be made from
the available ones. Pillows, are used to protect bony prominences. Trochanter
roll, prevent external rotation when lining in supine position. The trapeze bar, a
triangular device hanged on the bed that can be used by the patient whose upper
extremities functions well.When positioning ensure the following: Mattress should be firm and level yet
has enough give to fill in and support natural body curvatures; Bed should
be clean and dry (wrinkled or damp sheets increase the risk of pressure injuries
forming; that’s why bed making is important), support devices/aids according
to patient’s position (pillows and trochanter roll are examples), avoid placing
one body part directly on top of another body part (especially one with bony
prominences) because pressure can damage veins and causes thrombus formation;
ensure the 24-hour schedule of position changes, frequent position changes
are essential to prevent pressure sores; and always obtain patient’s information
on which position is comfortable and appropriate.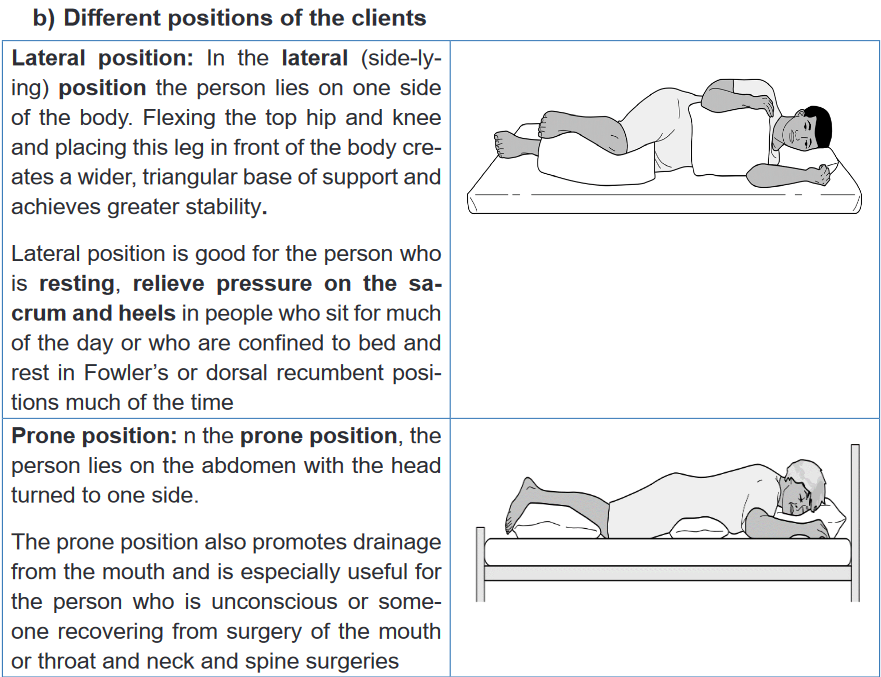
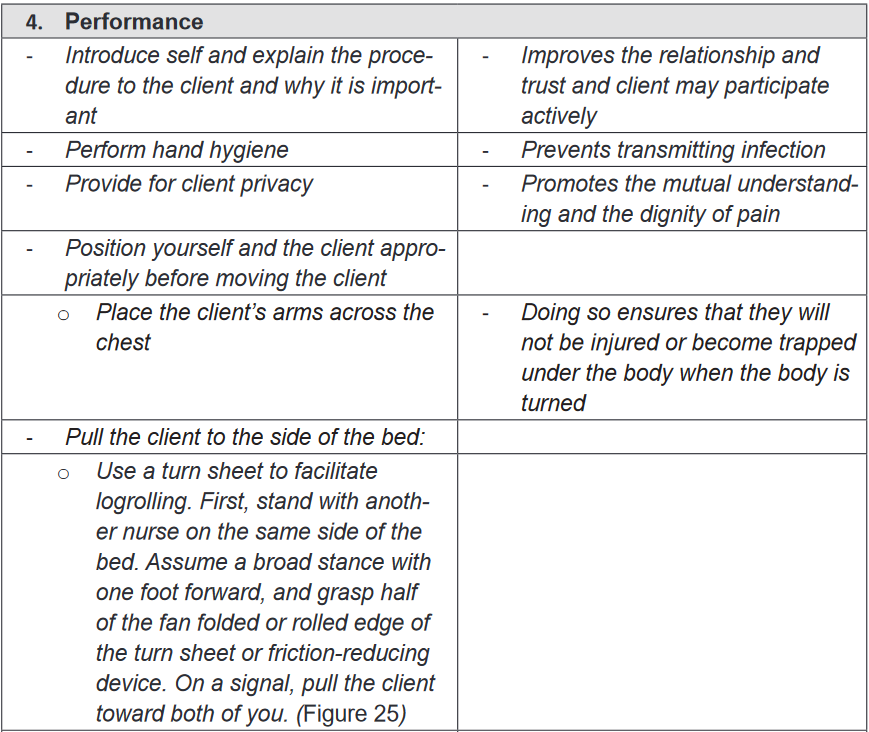
c) Principles of changing positions
Healthy people change position, with little effort, however ill people may have
difficulties of moving or changing positions even in bed. Nurses should be sensitive
to both the need of clients to function independently and their need for assistance
to move. Comfortable and correct body alignment should be maintained in order
to prevent undue stress on the musculoskeletal system. When turning the
client, nurse should ensure the appropriate number of staffs and assisting materials
needed.When positioning patient, there are couple octions and ratonales which are
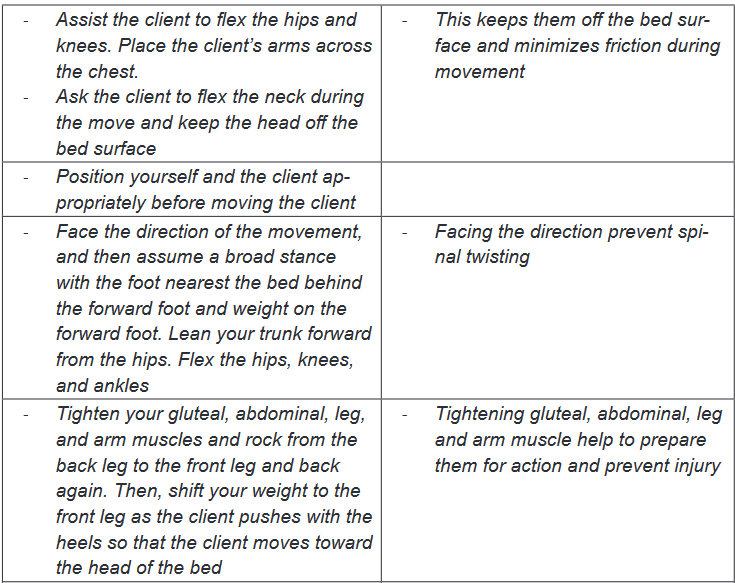
applicaple to moving and lifting:• Before moving a client, assess the client’s physical abilities, and ability
to assit with the move, degree of comfort, client’s weight, orthostatic
hypotension and your strength and ability.
• Prepare assitive materials available (e.g: pillows, trochanter roll);
• Plan around incumbrances to movement (e.g: IV, Urinary catheter, cast);
• Be aware of medications effects (e.g: effect on alertness, balance, strenth
and mobility);
• Ensure assistance (if needed) from other people is available;
• Explain the procedure and listen suggestions from patient, or support
people have;
• Provide privacy;
• Perform hand hygiene;
• Raise the bed of the client to bring the client to your center of gravity;
• Lock the wheels on the bed and raiserails on the other side to ensure
client safety;
• Face the direction of the movement to prevent spinal twisting;
• Stand appropriately to increase the stability and provide balance;
Fundamental of Nursing | Associate Nursing Program | Senior 4 87
• Lean your trunk forward and flex you hips, knees and ankles to lower
your center of graity, ensure stability and ensure use of large muscle groups
during movements;
• Tighten your gluteal, abdominal, leg and arm muscle to prepare them for
action and prevent injury;
• Rock from the front leg to the back leg when pulling or from the back leg
to the front leg when pushing to overcome inertia counteracy the client’s
weight and help attain a balanced smooth motion;
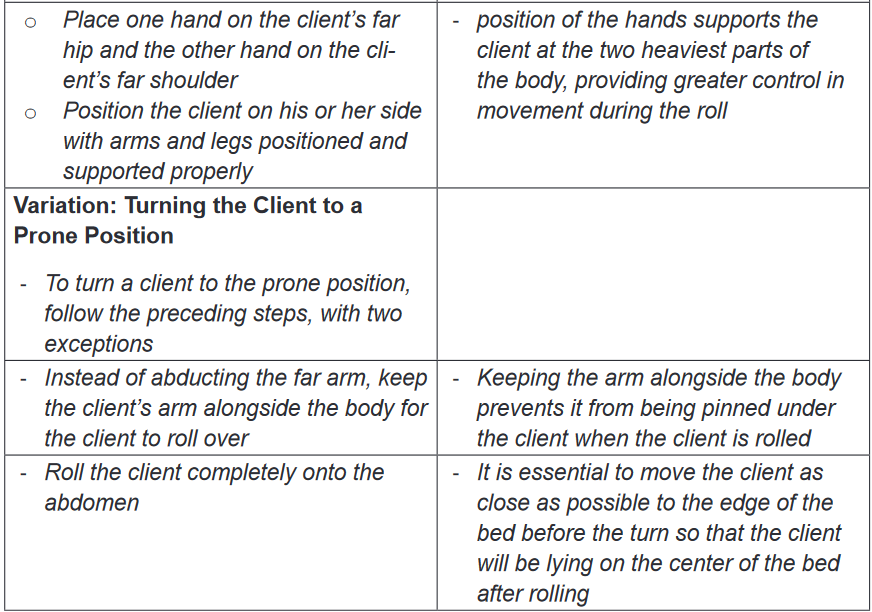
• After moving determine and document the client’s comfort, body
alignment tolerance of the activity (check pulse rate, blood pressure),
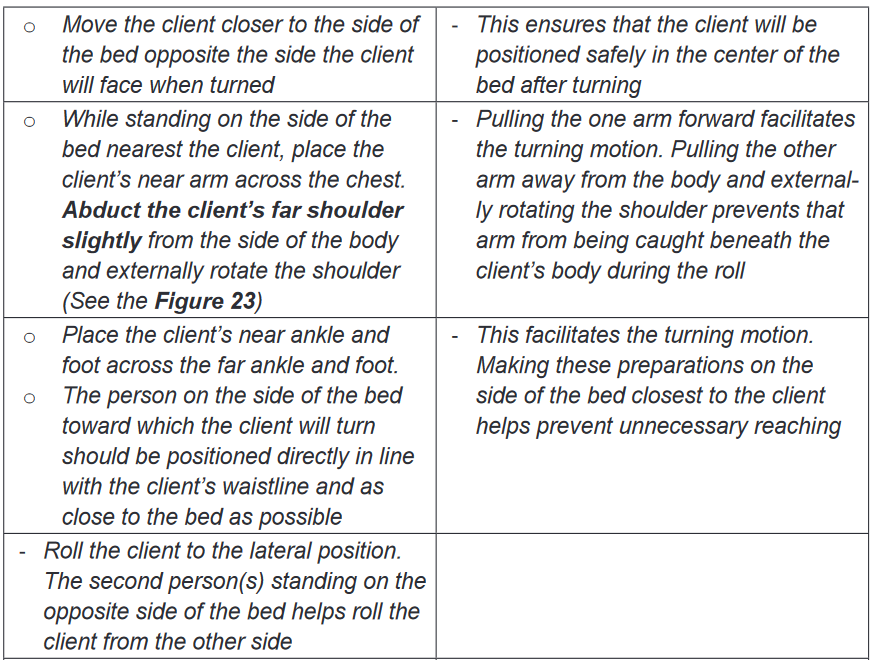
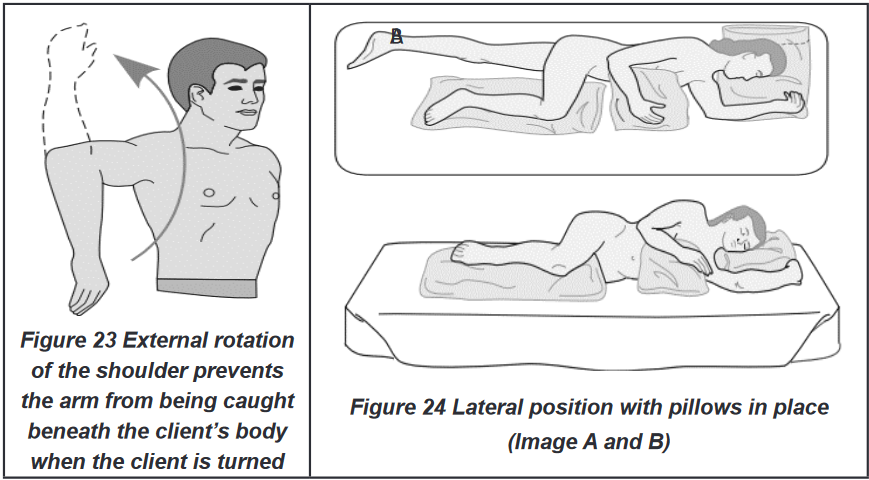
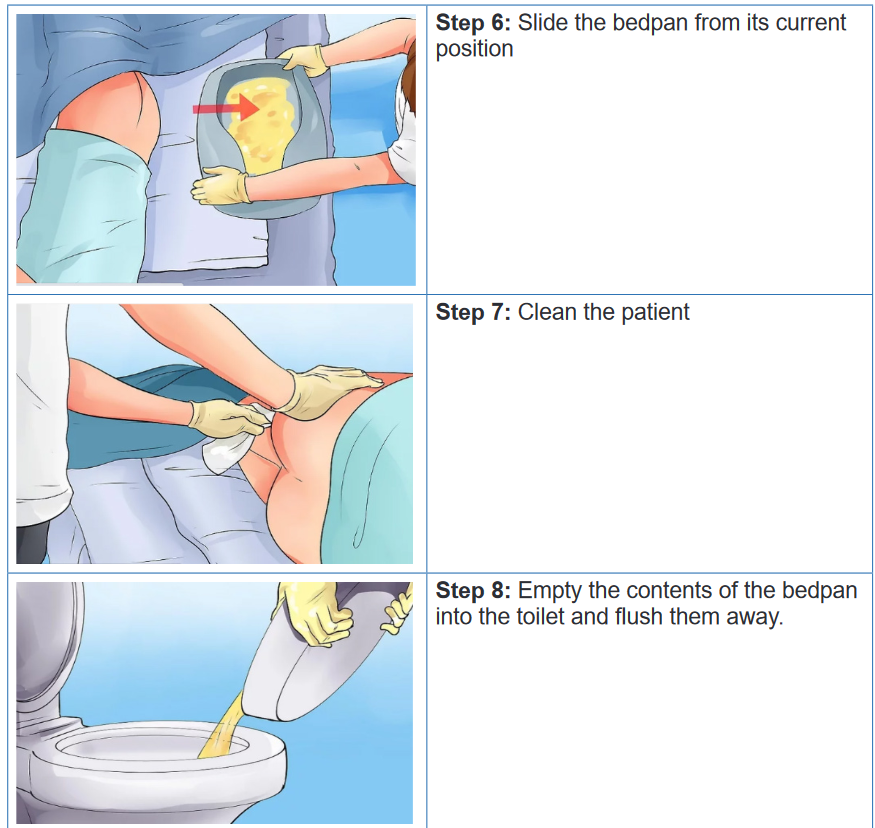
abilty to assit and understand and safety precautions required.d) Techniques of changing position of the patient
i. Turning client to the lateral or prone position in bed
Purpose: the lateral positioning maybe needed when placing a bed pan, changing
bed linen or repositioning the client.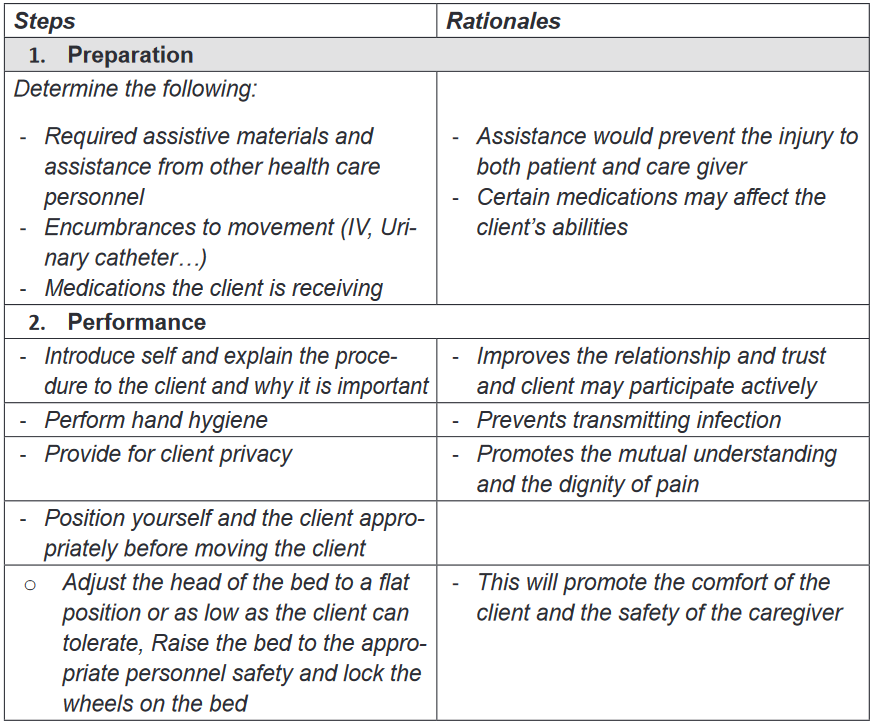
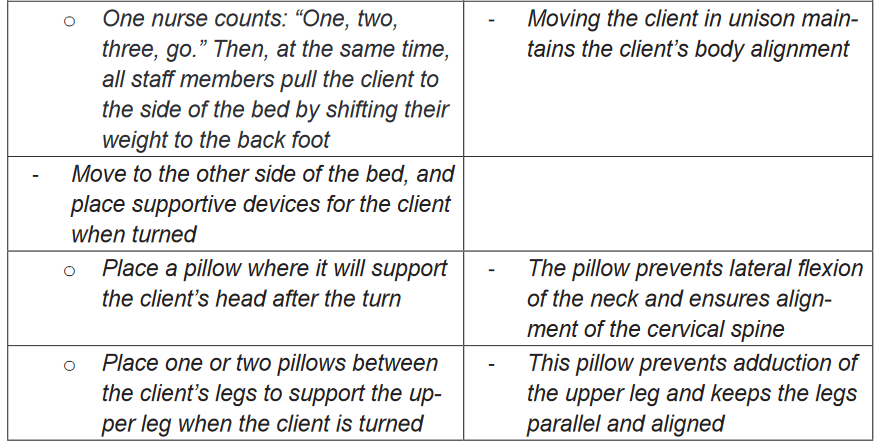
ii. Logrolling a client
Purpose: the purpose it to turn the client whose body must at all times be kept in a
straight alignment. E.g. client with back surgery or spinal injury.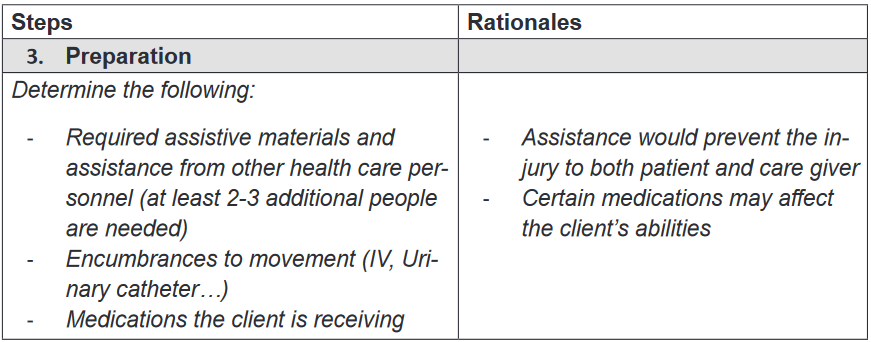
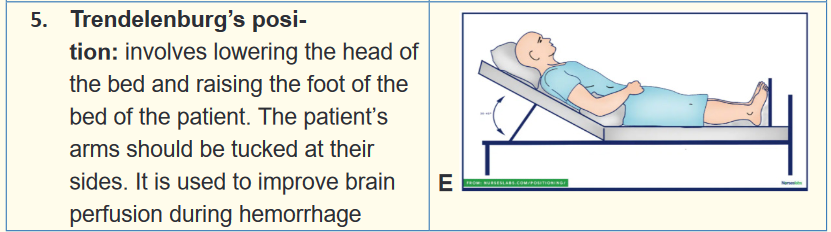
2.5.2. Moving the patient
a) Purpose of moving patient
Many clients may require some help in transferring between bed and chair or
wheelchair, wheelchair and the toilet, and from bed to stretcher (mostly with
clients who cannot sit on wheelchair. Whenever the client is able to move him/
herself from bed to chair, wheelchair or stretcher encourage him to do so and
provide the required and appropriate assistance.b) Techniques of moving the patient
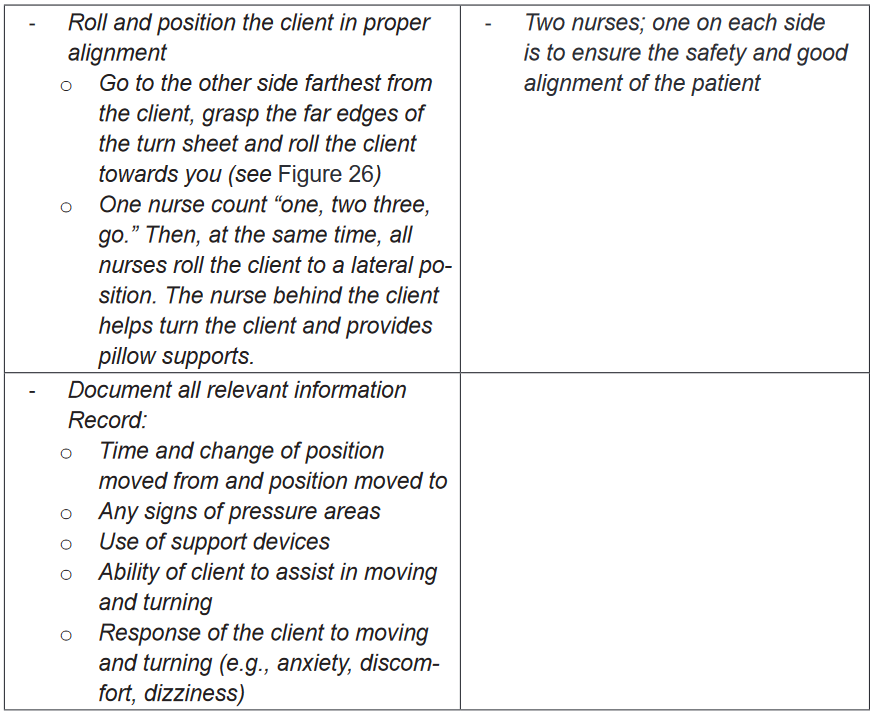
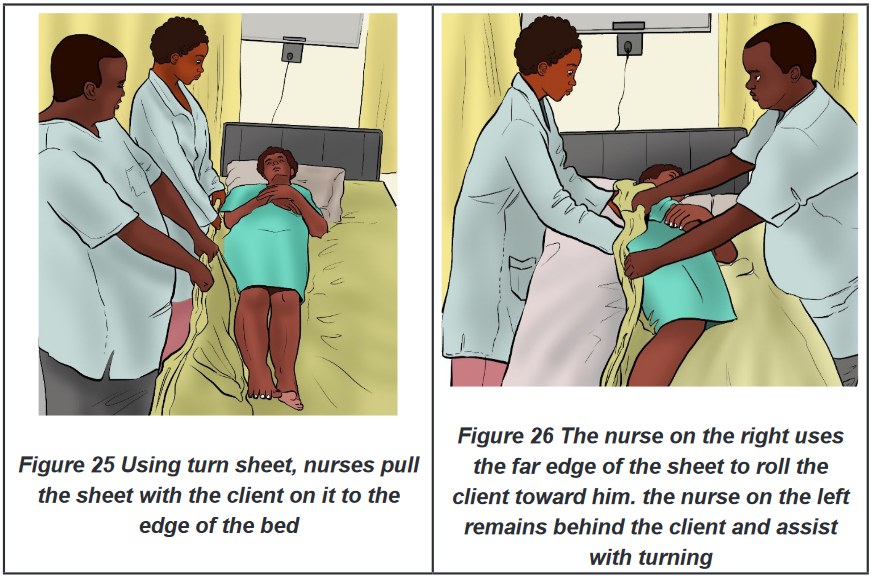
i. Moving patient in bed (two nurses using turn sheet)
Purpose: To assist clients who have slid down in bed from the Fowler’s position to
move up in bed.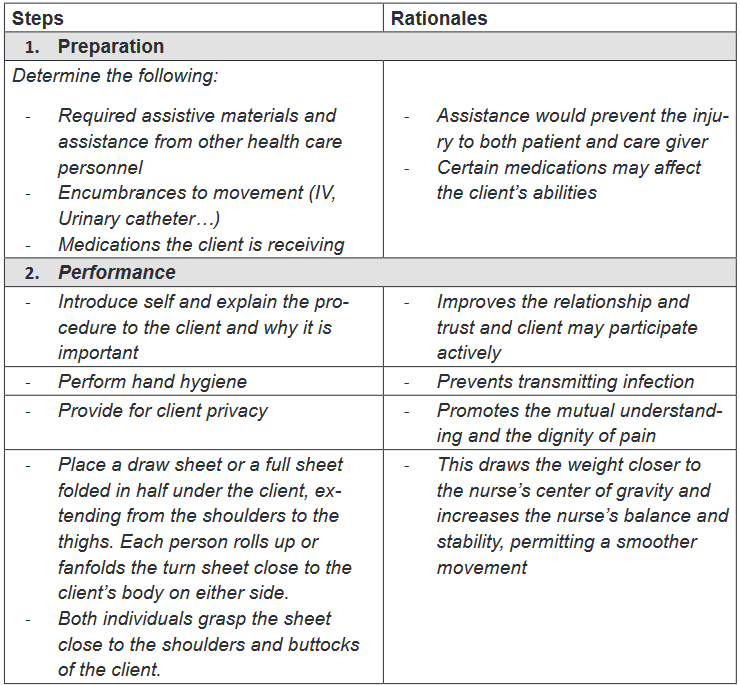
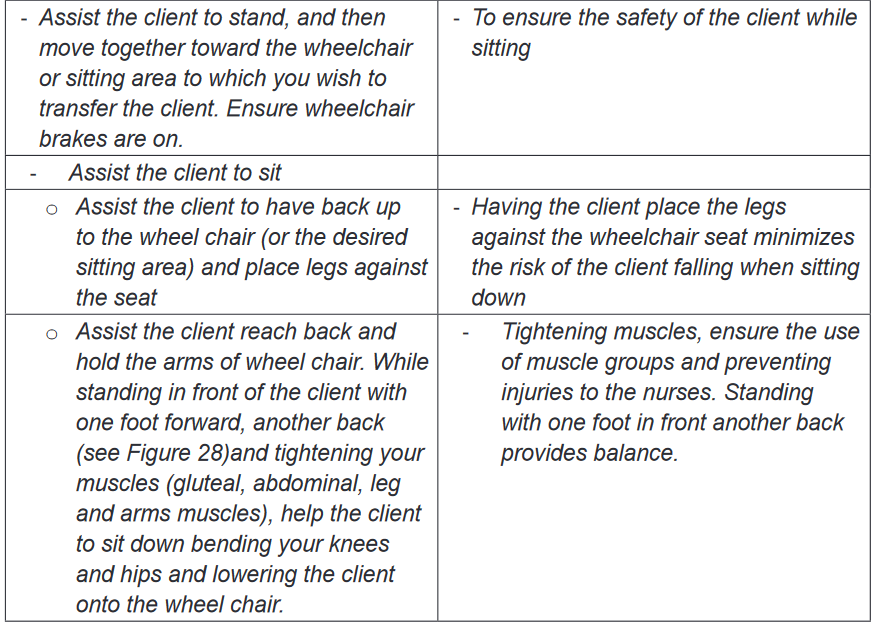
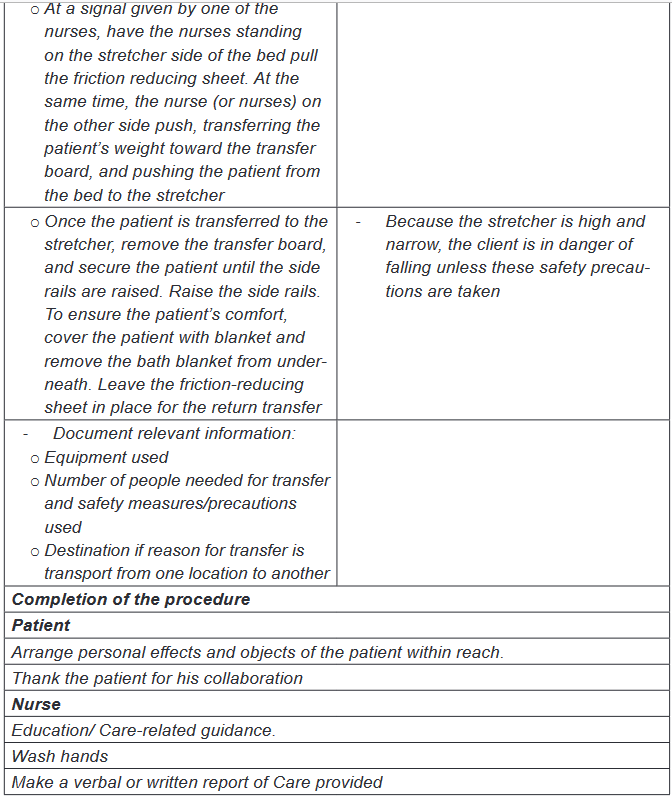
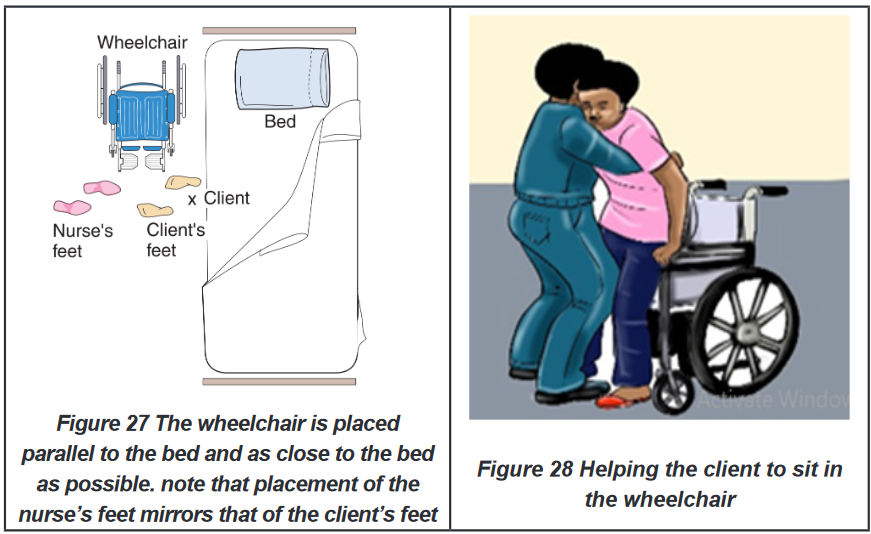
ii. Moving the patient from bed to chair or wheel chair (one nurse and two
nurses)
Purpose: clients who cannot move by themselves but can sit may need to be
transferred from bed to chair, or wheelchair due to different purpose: changing
position, ambulation, or transfer to operating room.
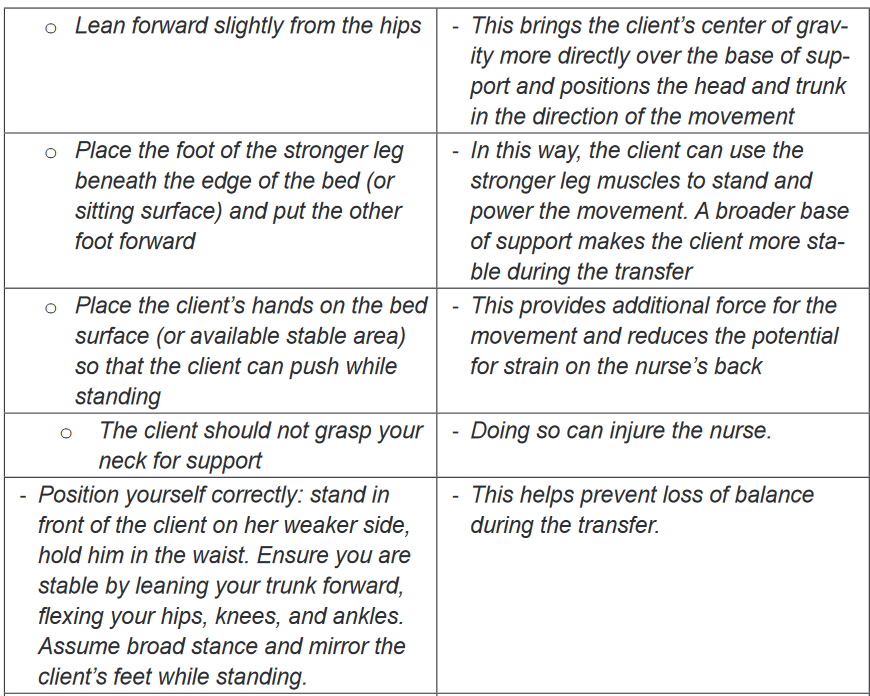
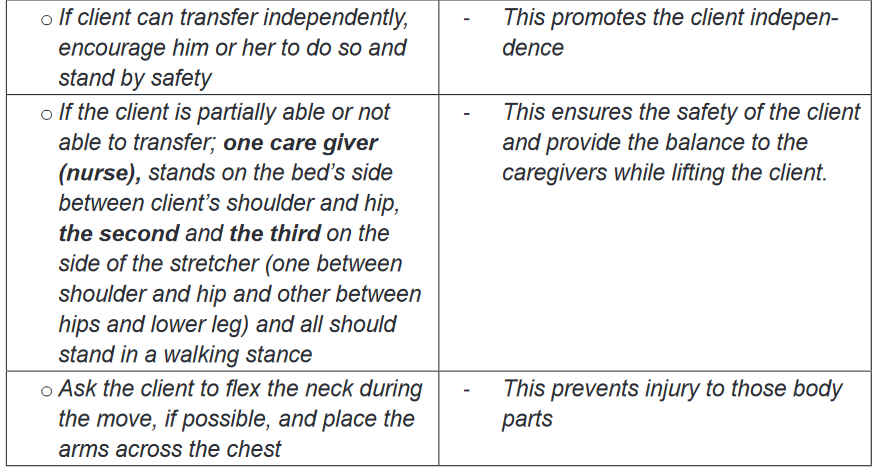
iii. Moving the client from bed to stretcher
Purpose: the stretcher is used to transfer the client in supine position from one
location to another (post-operated patients, patient with spinal injuries etc.)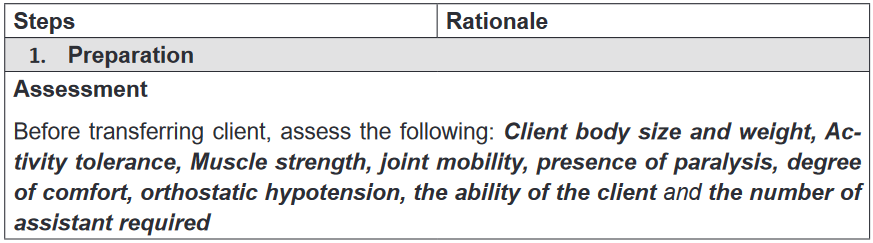
BOX 2.5.
Positioning, moving, and transferring clients reduce the potential for disuse
syndrome. Disuse syndrome is a term for the physical decline and other
problems that arise when the human body is deprived of physical activity.Self-assessment 2.5.
Mr. MUNYAKAYANZA, is hospitalized altered patient who is at risk of
developing bedsores, nurse decided to change position every two hours. Mr.
MUNYAKAYANZA is not breathing well, and his abdomen is distended.
1) What are the possible positions for Mr. MUNYAKAYANZA and explain
why?2) What are the contraindicated positions for Mr. MUNYAKAYANZA and
explain why?
After two weeks, Mr. MUNYAKAYANZA condition is being improved, he has
requested a nurse to help him for going outside on sunlight. However, he can
turn in the bed and sit but cannot walk.3) How a nurse will a nurse help Mr. MUNYAKAYANZA to move to the
sunlight and explain why?4) What are indications and contraindications of the chosen technique?
2.6. Application of local heat and cold
Learning activity 2.6.
Mr. NDAYISABA, an athletes who sustained a sprain (sprain: twist of the
ligaments of (an ankle, wrist, or other joint) violently that causes pain and
swelling) while running, the nurse AKAZUBA wanted to calm down the pain
and to prevent the progress of swelling by applying ice bags to the area. The
ice bag will cause vasoconstriction.
1) How do you think the vasoconstriction can lead to the reduction of
swelling?
2) What do you think are other alternatives to use in spite of ice bag?2.6.1. Definition of local heat and cold application
Heat application: is an application of warmed object, above body temperature, on
a body part to increase blood flow or provide relief of pain. While Cold application
refers to the placement of cold object cooler than skin, on the surface of the skin.
Heat and cold can be applied to the body in both dry and moist forms. Heat or cold
can be applied generally or locally. General application of heat or cold is used
when a very high or very low body temperature puts the patient’s health at risk or
makes the patient very uncomfortable. Local application of heat or cold is very
commonly used, and there are many different therapies. Common uses are to treat
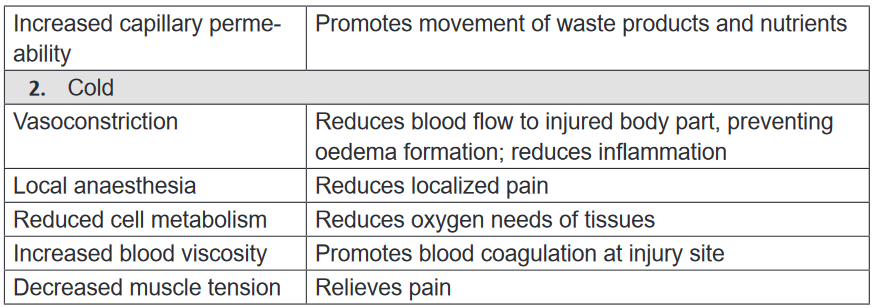
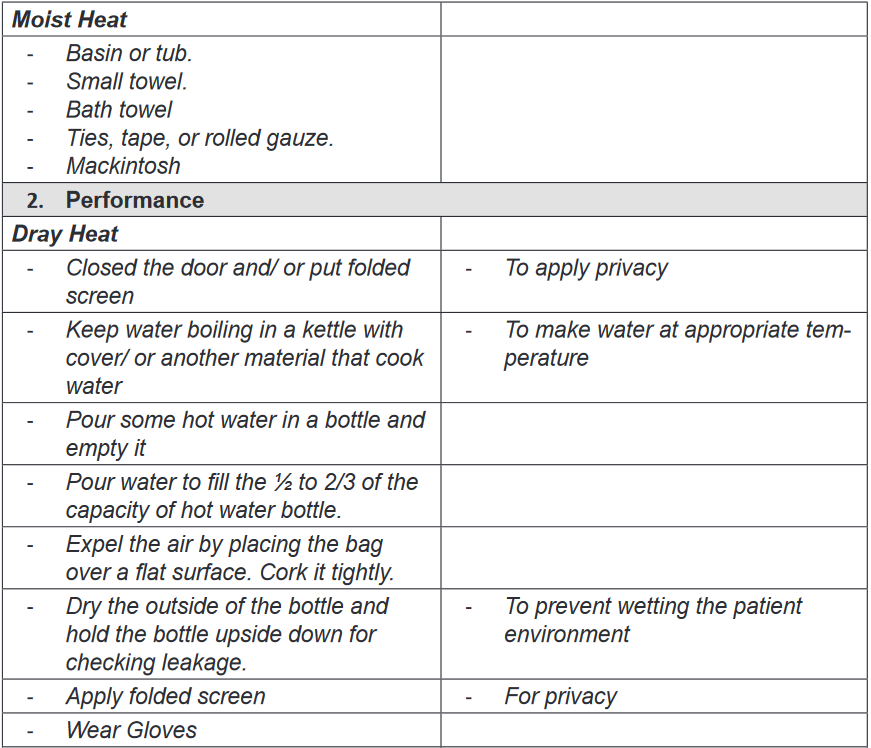
sprains muscle pulls, arthritic joints, or local infections.2.6.2. Purpose of Local heat and cold application
Heat and cold stimuli create different physiological responses. The choice of heat
or cold therapy depends on local responses desired for wound healing as shown in
the below table.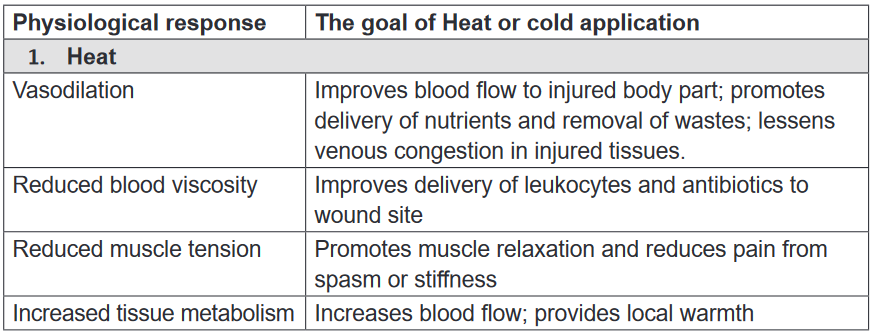
2.6.3. Principles of heat or cold applications
The following are principles of heat and cold applications:a) Heat application principles
• Measures the temperature of moist heat applications by putting at the back
of your palm.
• Do not apply very hot application, because it may cause burn
• Measure the patient temperature; Lower temperature is used for those at risk,
if it is too hot for the patient add cold water.
• Cover dry heat applications with cloth/ towel before applying them and be
sure that you are applying at the right location
• Do not let the person increase the temperature of the application.
• Carefully watch the time. Heat should not be applied for more than 30 minutes4
• Expose only the body part where the cold is to be applied.b) Cold application
• Measure the temperature of moist cold applications. It should not be freezing
cold
• Very cold applications can damage tissue
• Be sure about the exact location for the cold application
• Cover dry cold application with cotton or soft cloth before applying them.
• Carefully watch the time. Cold should not be applied for more than 30 minutes.
• Observe the skin for any problem, discontinue immediately if patient
experience: Pain, numbness or burning, Excessive redness, Blisters, Pale,
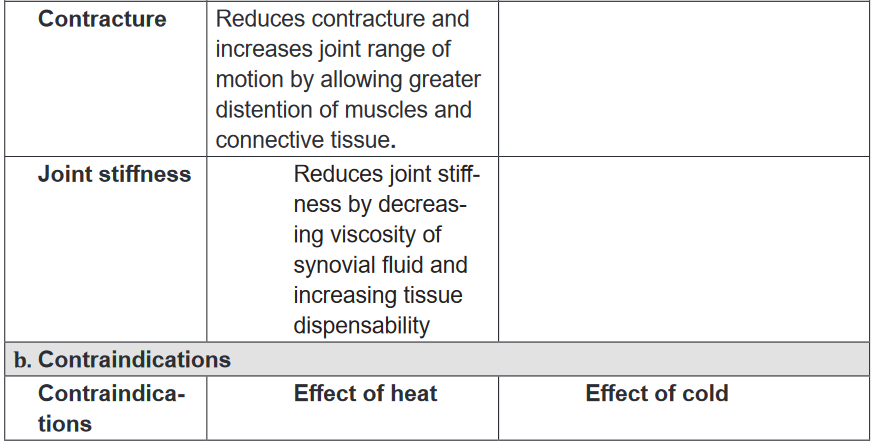
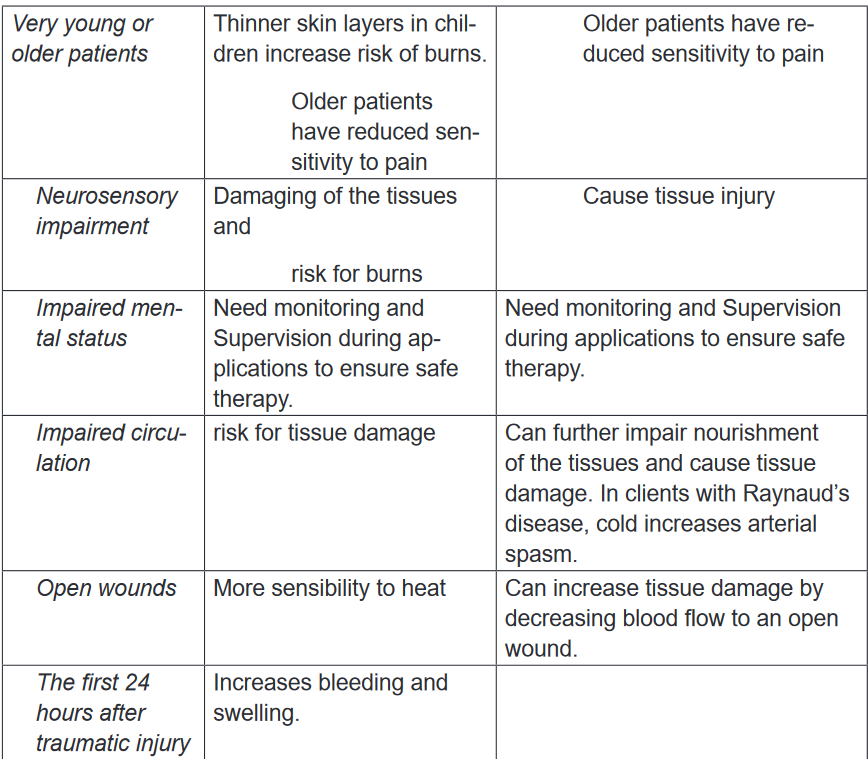
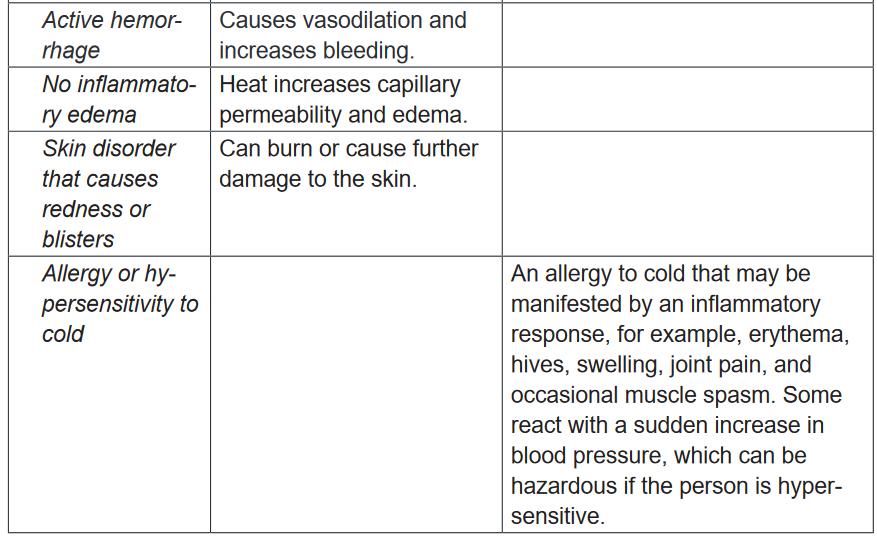
white or gray skin, Blue Patch and Shivering.2.6.4. Indication and contraindication of local heat and cold
application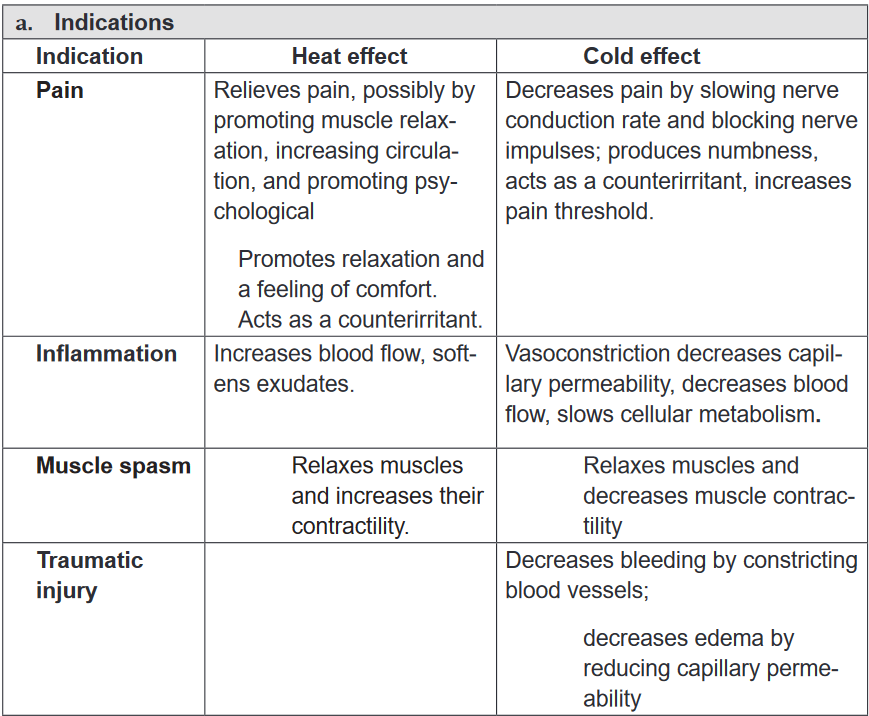
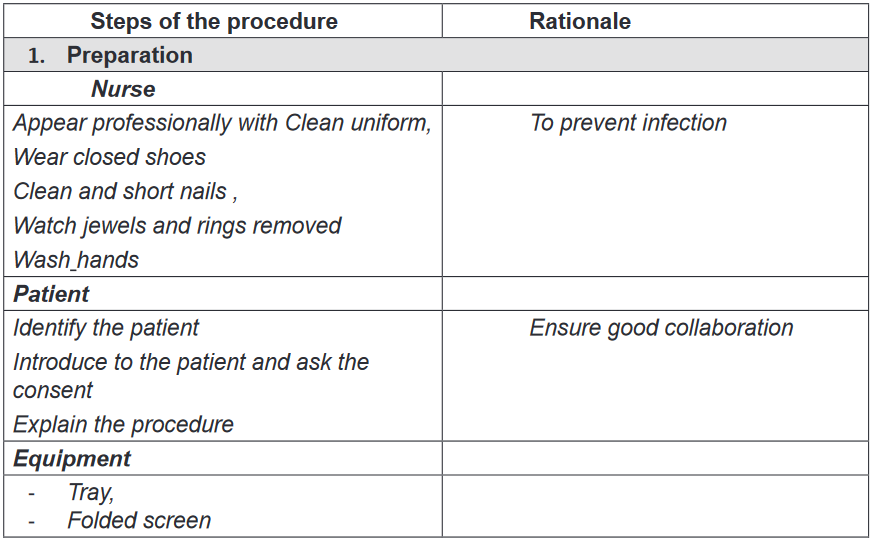
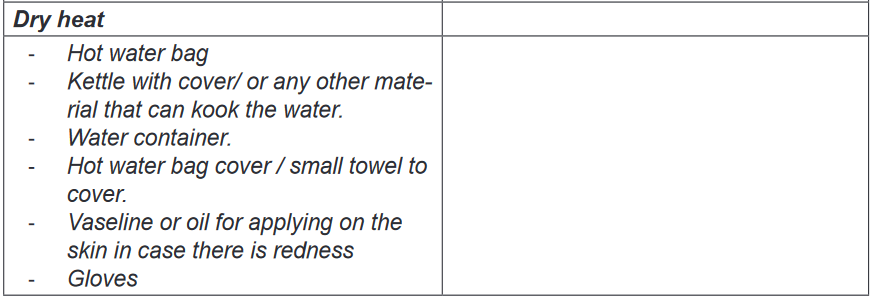
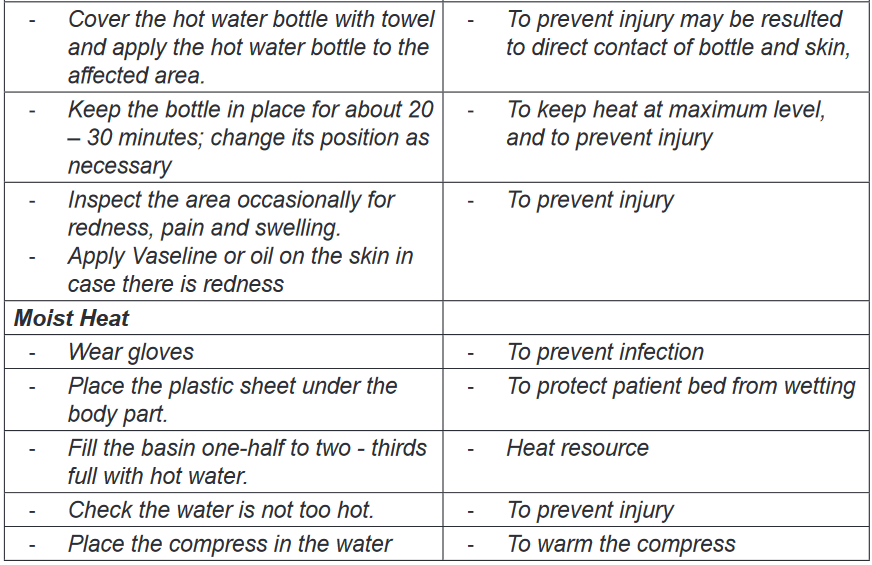
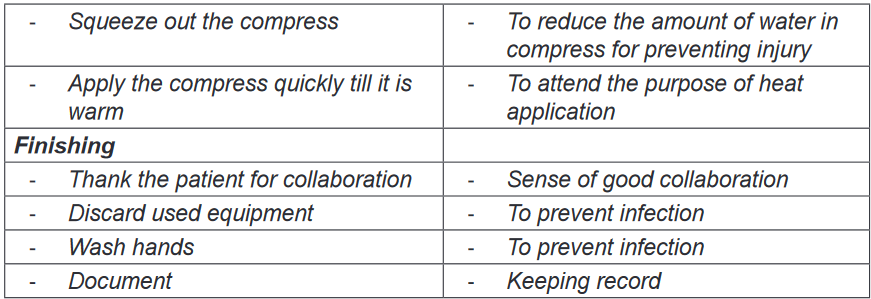
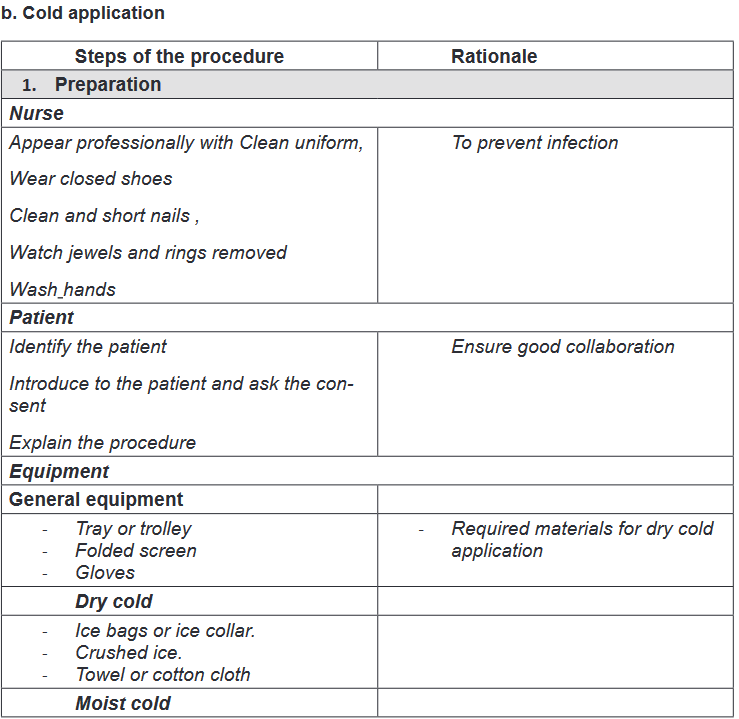
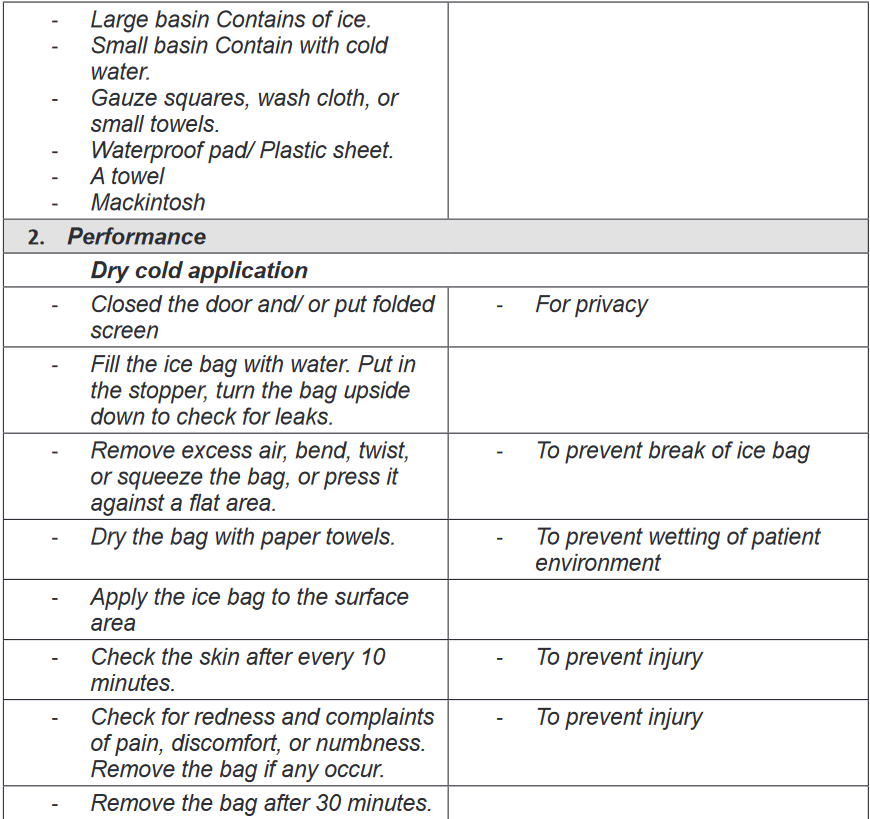
2.6.5. Techniques of local heat and cold application
Heat or cold should be applied after assessing the patient’s physical condition for
signs of potential intolerance to heat and cold. First observe the area to be treated.
Assess the skin, looking for any open areas such as alterations in skin integrity
(e.g., abrasions, open wounds, edema, bruising, and bleeding, or localized areas
of inflammation) that increase the patient’s risk of injury. The health care provider
commonly orders heat and cold applications for traumatized areas, the baseline
skin assessment provides a guide for evaluating skin changes that can occur
during therapy. Include in your assessment the neurological system for sensation
(to understand if the patient senses extremes of cold or heat) and the patient’s
mental status to be sure that he or she can correctly communicate any issues with
the hot or cold therapy.a) Heat application
Self-assessment 2.6.
1) Explain the indications and contraindications of the heat application
2) Explain the relationship between the following terms
a) Vasoconstriction and swelling
b) Vasodilatation and inflammation2.7. Assisting the patient to eliminate
Learning activity 2.7
Regular elimination of body waste products is essential for normal body
functioning; the body eliminates its waste mainly through the urinary and the
gastro-intestinal systems. The metabolic reactions and other homoeostatic
processes lead to wastes which should be evacuated and if not eliminated,
they can alter the homeostasis lead to body malfunctions. Patients who are not
able eliminate independently or not able to control it (for example in case of
incontinence) should be assisted.
1) With reference to the above text and the knowledge from biology, explain
different ways of human body waste elimination
2) Think about possible consequences that may arise if the gastro-intestinal
system elimination is disturbed
3) Think about the patient with urinary incontinence, what could be possible
the consequences2.7.1. Introduction
a) Bowel elimination
The digestive system has many functions; ingestion, mastication, deglutition,
digestion, absorption and elimination. Elimination of the waste products of
digestion is the passage of fecal material that remains in the colon following the
digestion and absorption of nutrients and fluids which are required for maintenance
of metabolic health. The excreted waste products are referred to as faces or stool.
Normal feces are characterized by: brown color, soft formed consistency, tubular
shape as in the rectum, tolerable odor depending on diet and normal fecal content.
The normal bowel elimination frequency is 1-3 times a day to 3 times a week.Many factors affect defecation such as different stages of life (new-born, infant,
toddler, preschool children and adolescent adult and elder adult), Diet, fluid intake
and intolerance, physical activity and psychological factors such as anxiety and
depression. Physical disability, certain medications, gastrointestinal infection and
disease processes can also affect defection. Nurses are frequently involved in
assisting people with elimination problems. These problems can be embarrassing
to the individual and can cause considerable discomfort.Most problems of elimination are: Constipation which is defined as fewer than
three bowel movements per week. This infers the passage of dry, hard stool or the
passage of no stool. Fecal impaction is a mass or collection of hardened faces in
the rectum. Impaction results from prolonged retention and accumulation of fecal
material. Diarrhea is a problem of elimination that refers to the passage of liquid
faces and an increased frequency of defection.Encopresis also called fecal incontinence is an elimination problem that refers
to the loss of voluntary ability to control fecal and gaseous discharges through the
anal sphincter. Flatulence is an elimination problem that consist of presence of
excessive gas in the intestines and leads to stretching and inflation of the intestines
(intestinal distention) If excessive gas cannot be expelled through the anus, it may
be necessary to insert a rectal tube to remove it.b) Urinary Elimination
The urinary tract system is made of kidney, ureters, bladder and urethra; the pathway
trough which urine flows and is eliminated from the body. Urinary elimination depends
on the effective functioning of the upper and lower urinary tract. Micturition or
voiding, or urination refer to the process of emptying the urinary bladder. Urine
collects in the bladder until pressure stimulates special sensory nerve endings in
the bladder wall called stretch receptors.
Fundamental of Nursing | Associate Nursing Program | Senior 4110
They are many factors that affect the volume and characteristics of the urine
produced and the manner in which it is excreted such as: developmental
factors(infant, preschooler, school age children, adult, older adult), psychosocial
factors that stimulate micturition reflex includes privacy, normal position, sufficient
time, occasional running water. Fluids and food intake affect voiding. Other factors
that affect voiding are medication, muscle tone, pathological conditions that affect
urinary tract system and surgical and diagnostic procedures.Altered urine production is characterized by Polyuria which is the production of
abnormally large amounts of urines by kidneys, often several liters more than the
person’s usual daily output. Oliguria and Anuria are used to describe urinary output.
Oliguria is low urine output usually less than 500ml a day. Anuria refers to a lack
of urine production.
Altered urinary elimination is characterized by: urinary frequency that refers to
voiding at frequent intervals; that is more than six times per day. Nocturia is a
condition where a person wakes more than once during the night to void. Urgency
is the sudden strong desire to void. There may or may not by a great deal of urine
in the bladder, but person feels a need to void immediately.Dysuria is altered urinary elimination characterized by voiding that is either painful
or difficult. Enuresis is involuntary urination in children beyond age when voluntary
bladder control is normally acquires usual by 5 years of age. Urinary incontinence
is involuntary urination. Urinary retention is when emptying the bladder is impaired,
urines accumulates and the bladder becomes over distended.Neurogenic bladder is an altered urinary elimination characterized by impaired
neurological function that interfere with the normal mechanisms of urine elimination
resulting in lack of perceiving bladder fullness and inability to control urinary
sphincters. The bladder may become flaccid and distended, or spastic, with frequent
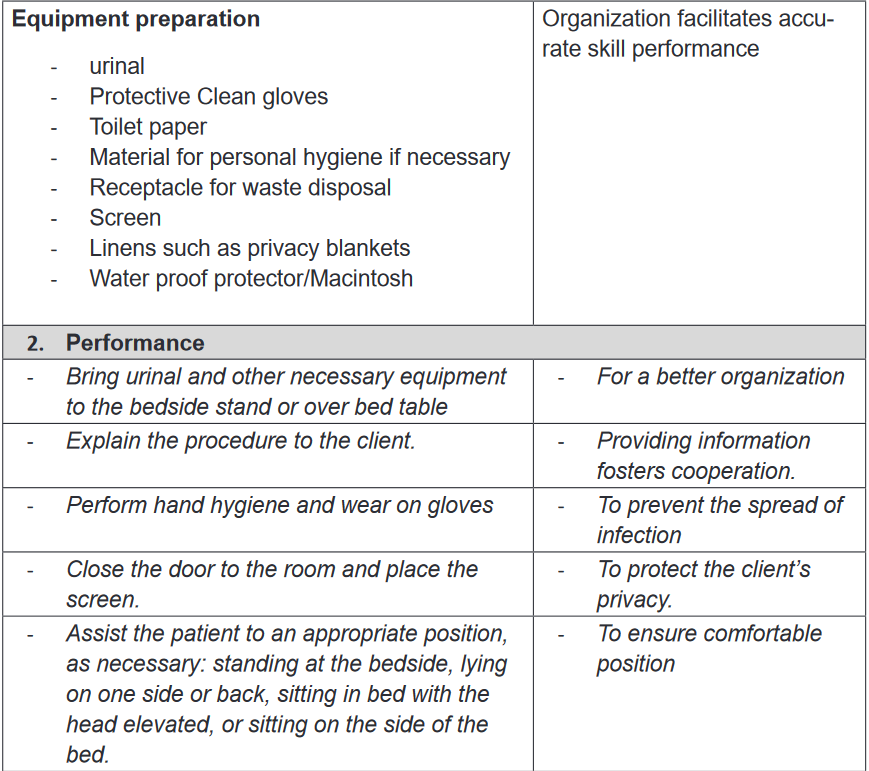
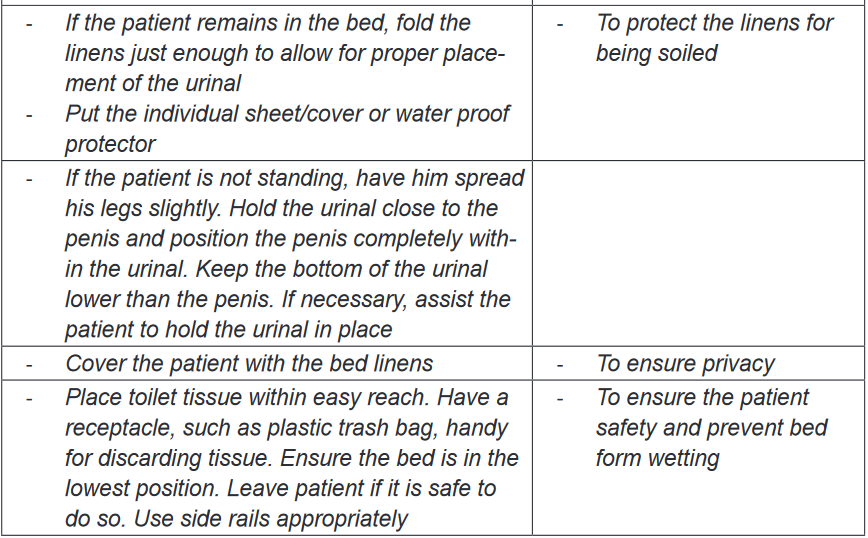
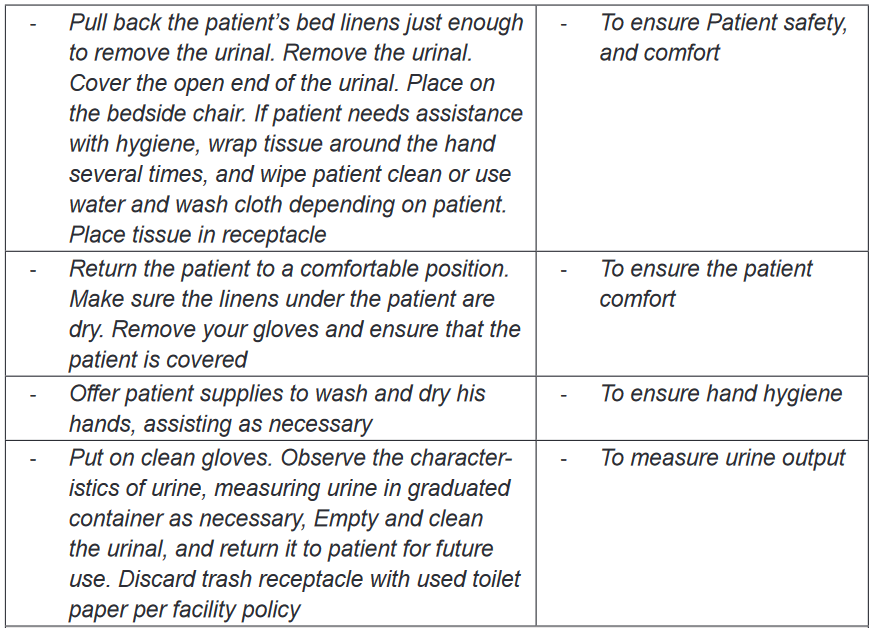
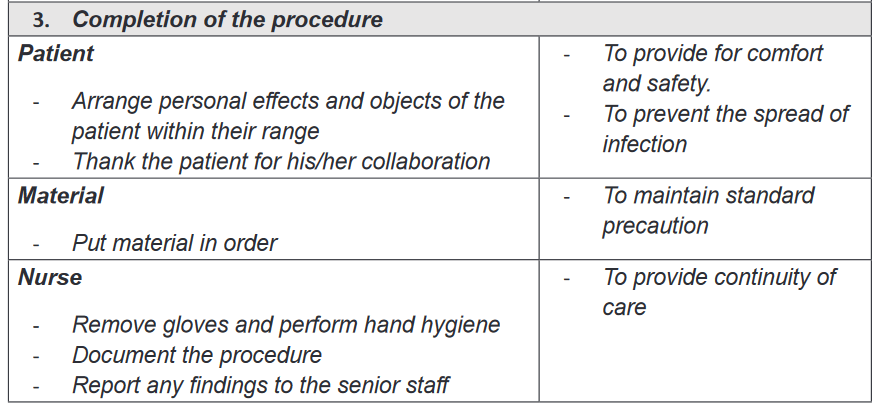
involuntary urination.2.7.2. Use of urinal
a) Indications and contraindications
In case patient cannot move of from the bed due to different conditions such as
lower limb fracture, or other conditions preventing him to move from the bed;
urinal, a device that help people to urinate while in bed, can be used to collect urine
while patient on bed. Urinals are indicated to people who have conscious control
of micturition and movement of their arms to urinate without the help of nurse.
However, it is contraindicated to people who are unconscious, not having control
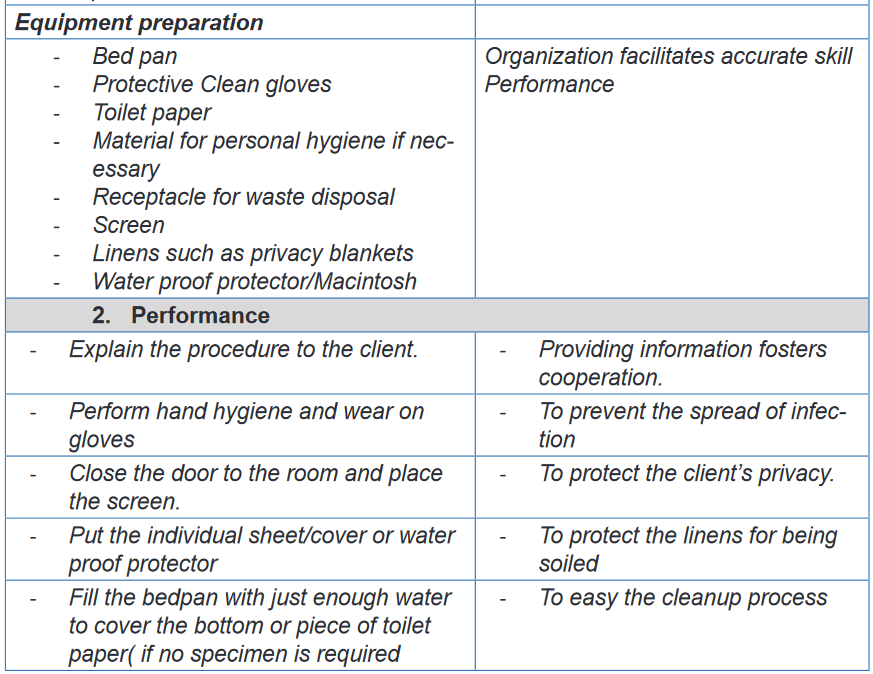
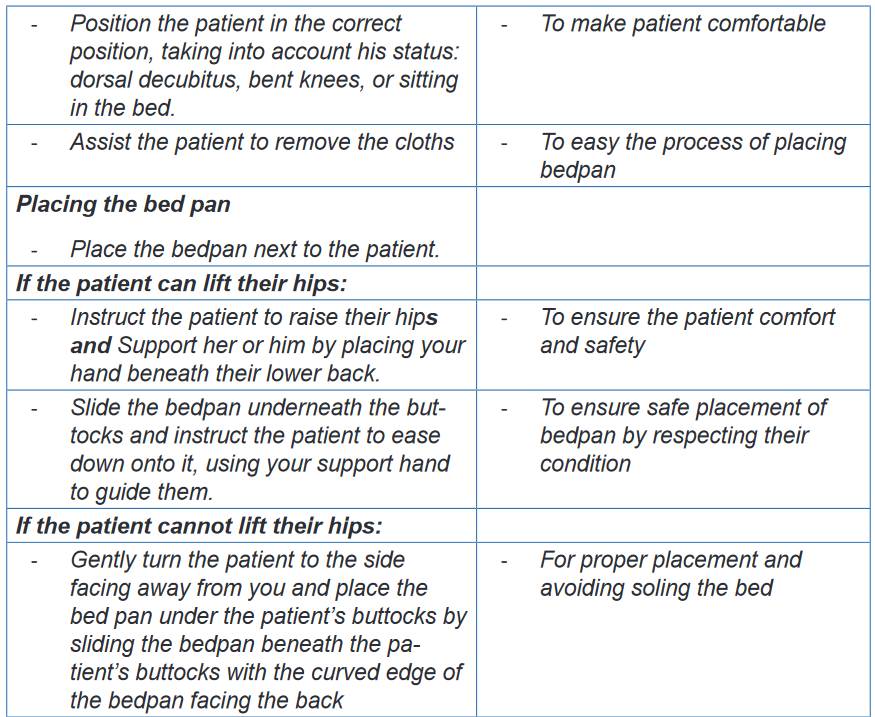
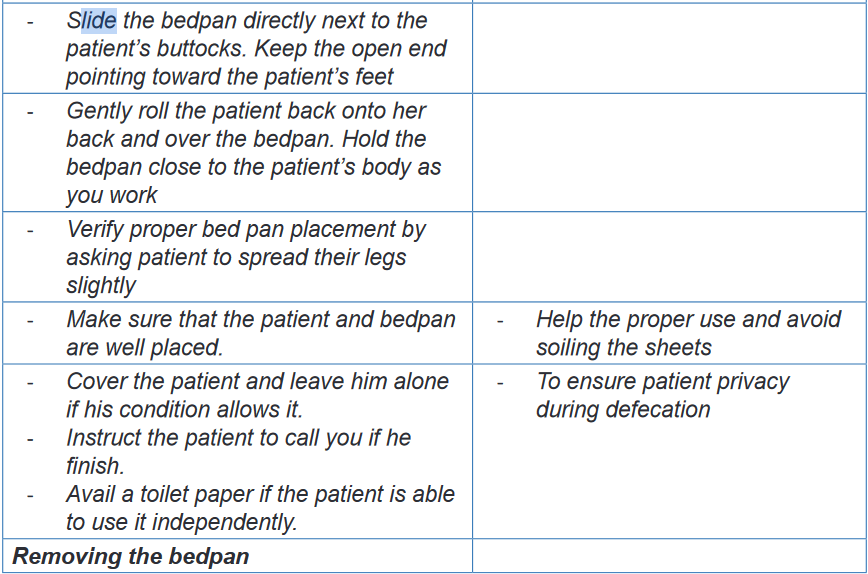
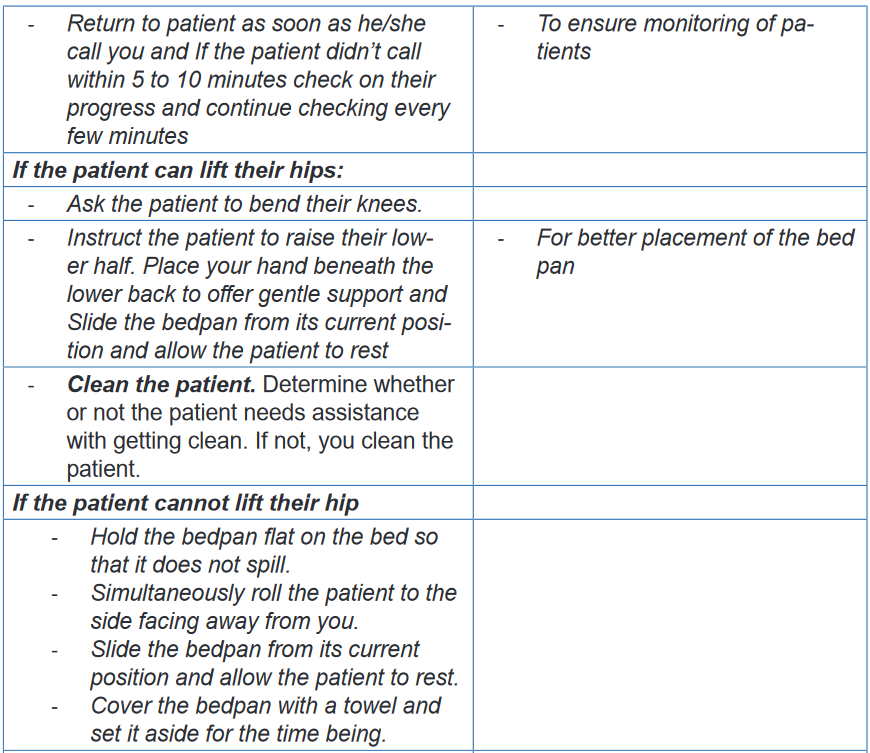
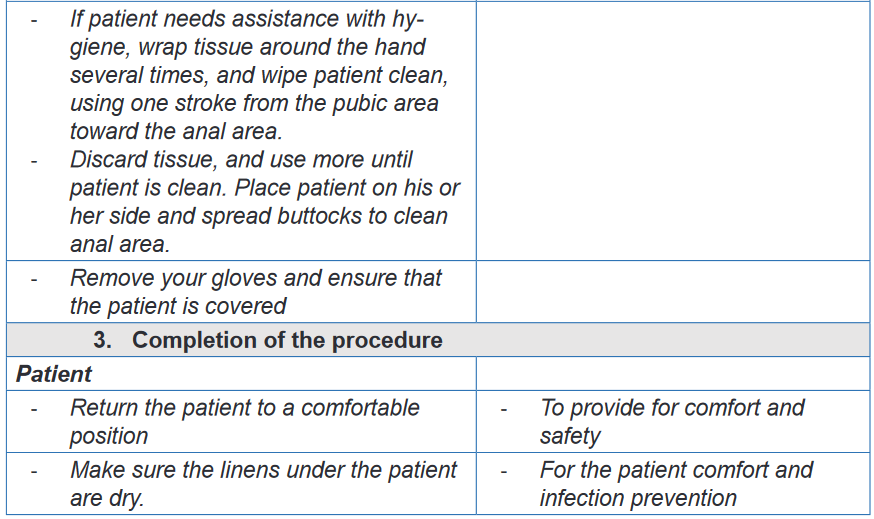
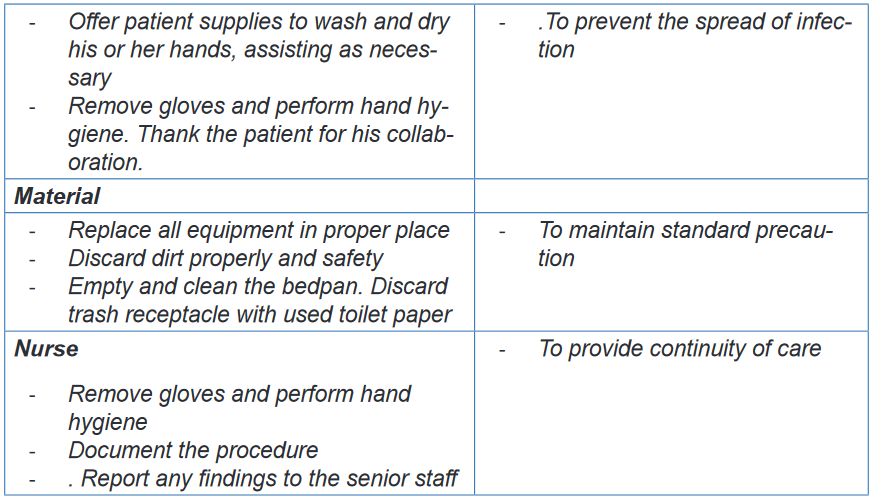
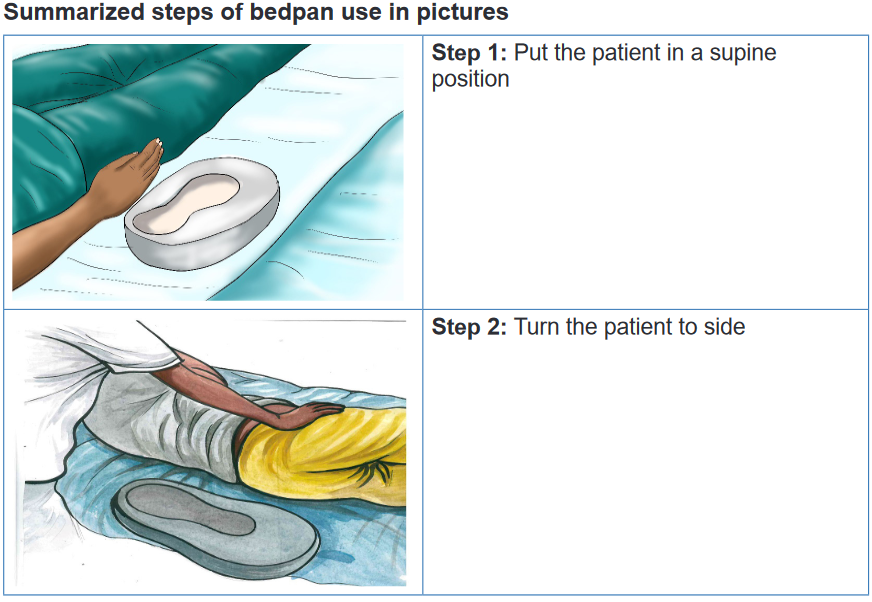
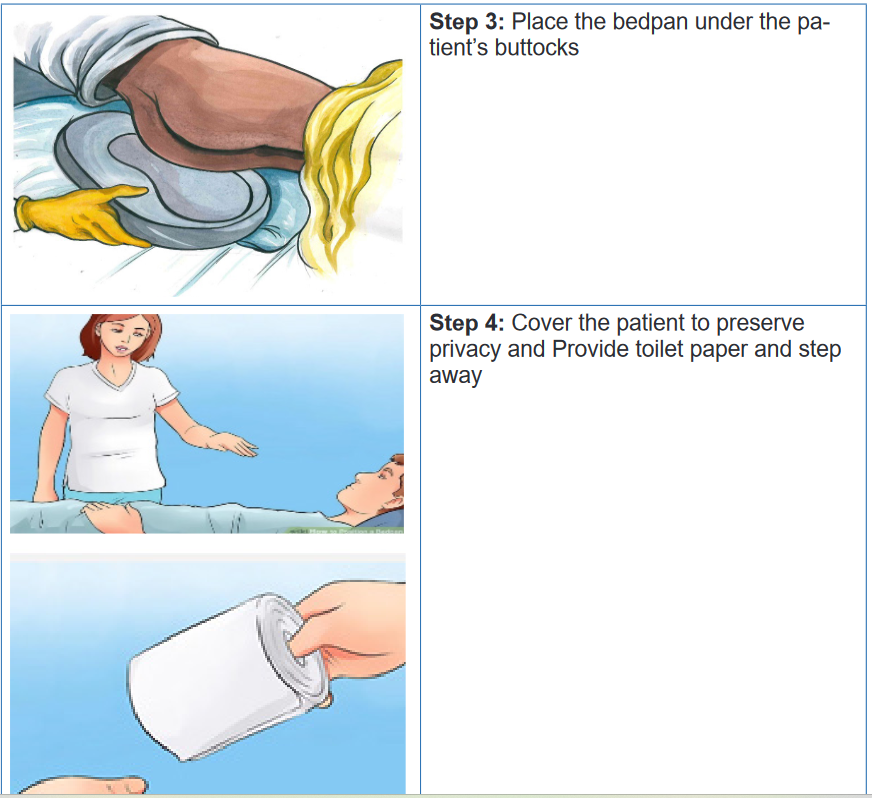
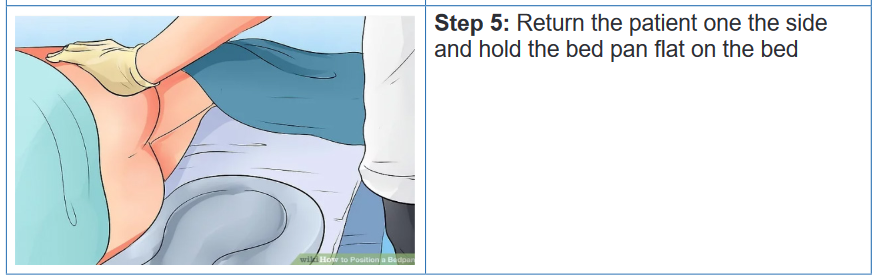
2.7.3. Use of bed pan
a) Definition of bed pan
A bed pan is a container used in hospital settings to assist bed ridden patient for
urination and defecation. A bed may be made in metal Stan steel or plastic material.
They are two different types of bed pans: regular and fracture.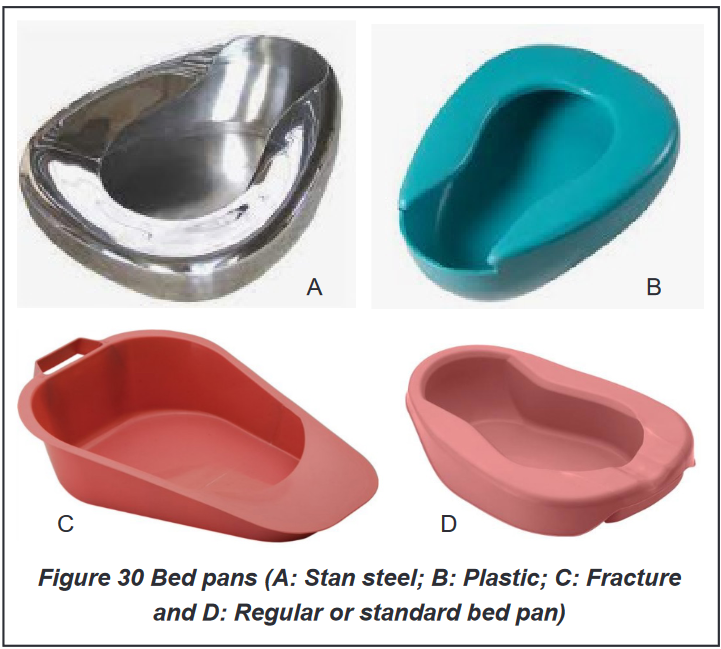
Indications of the bed pan use
Same as the urinal, bed pan can be used when client cannot walk to the bathroom;
patient with hip and lower extremity fracture, debilitating illness or profound fatigue,
high fall risk and increased injury potential, obstetrical and gynecological and patient
with fracture and patient who have had surgery that make them unable to move.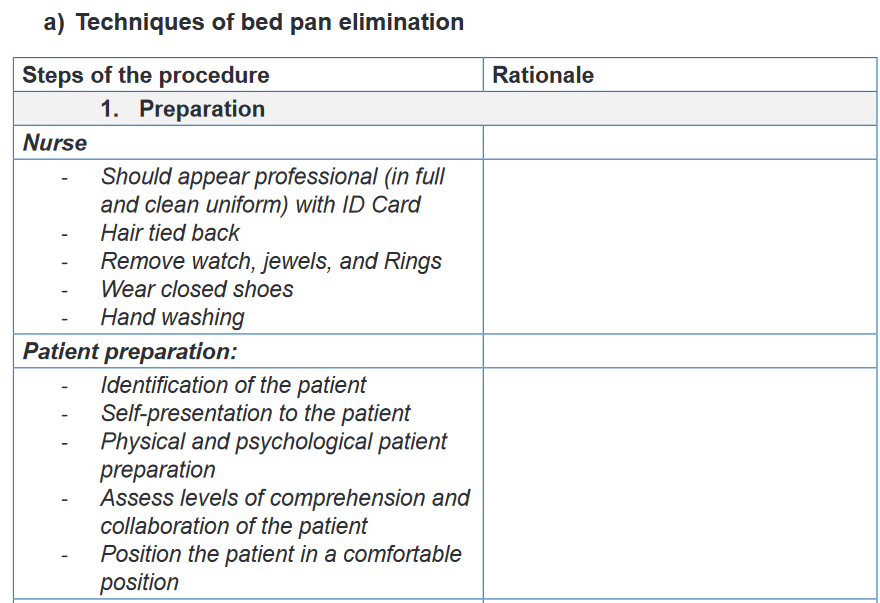
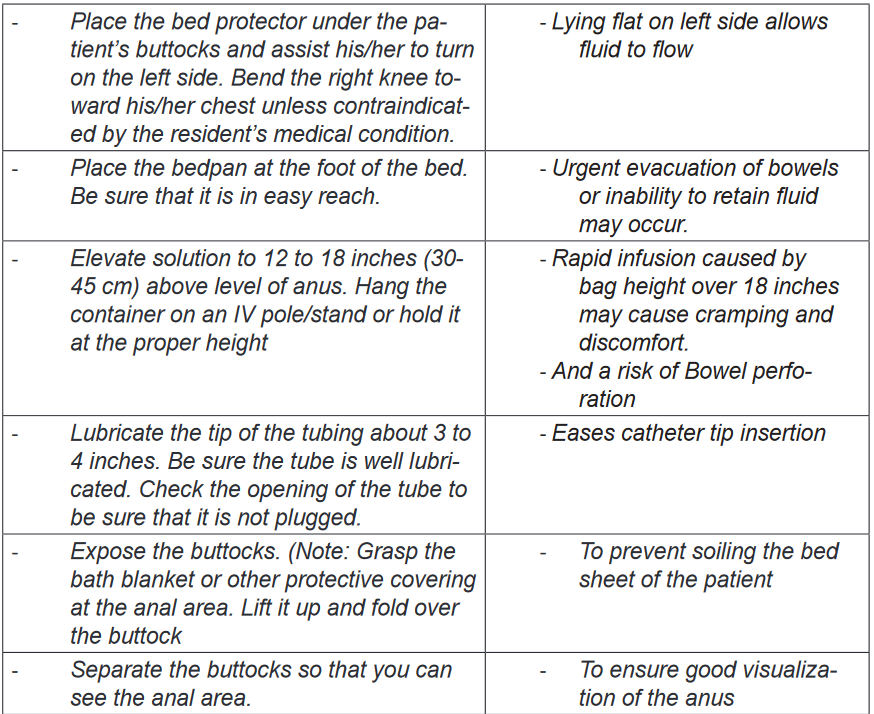
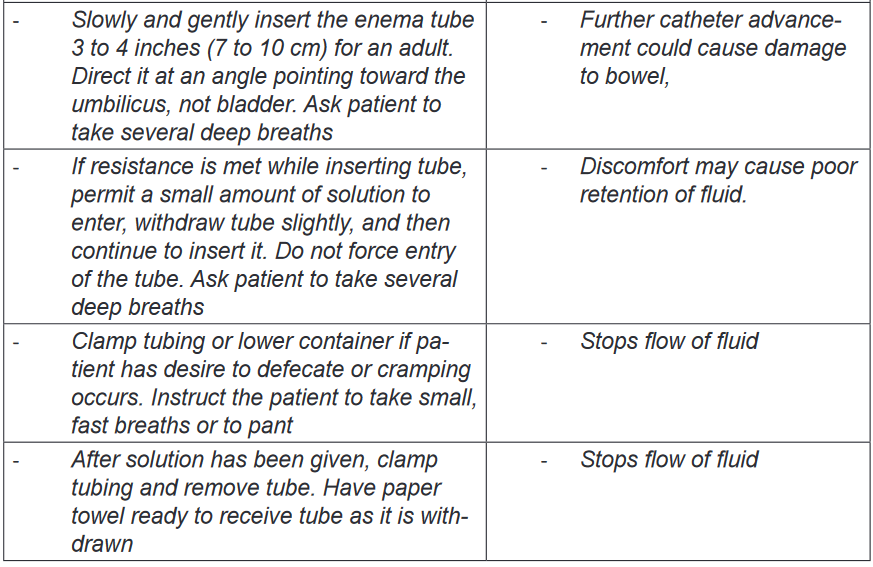
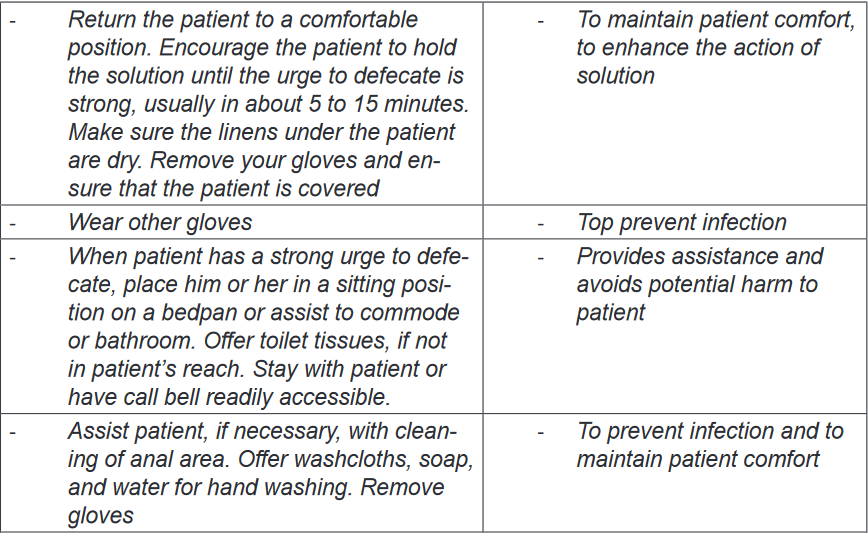
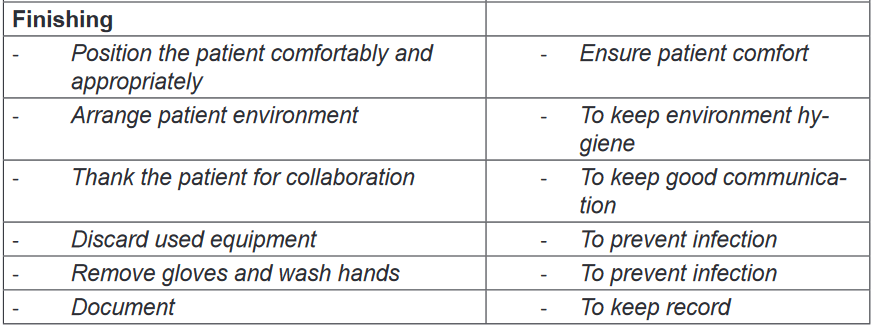
2.7.4. Enema
a) Definition and Types of enema
An enema is a a procedure in which liquid is injected into the rectum, to expel its
contents or to introduce drugs or permit X-ray imaging.. The purpose of an enema is to cleanse the lower bowel, to evacuate the stool
or flatus, or to instill medication. The enema solution should be at 37.7°C (100°F)
because a solution that is too cold or too hot is uncomfortable and causes cramping.
Enemas are classified into four groups: cleansing, carminative, retention, and
return-flow enemas.i. Cleansing enema
The goal of cleansing enemas is to remove feces. This type of enema is indicated in
case of constipation, patient preparation for surgery and some diagnostic test (i.e.,
colonoscopy). Normal saline is Isotonic considered as safe to use. Cleansing
enemas have two sub category: high or low. A high enema requires large volume
(i.e., 500 to 1,000 mL) for adult and is provided to cleanse as much as possible the
colon. The client changes the positions from the left lateral to the dorsal recumbent
and then to the right lateral position during administration so that the solution can
follow the large intestine. The low enema requires a small volume (90 to 120 mL)
and is used to clean the rectum and sigmoid colon only. The client maintains a left
lateral position during administration.ii. Carminative enema
A carminative enema is given mainly to expel flatus (intestinal gas). The solution
instilled into the rectum remove gas. For an adult, 60 to 80 mL of fluid is instillediii. Retention enema
A retention enema tends to introduce the oil or medication into the rectum and
sigmoid colon. The liquid is retained for a relatively long period for 1 to 3 hours. The
goal is to soften the faces, lubricate the rectum and anal canal, hence facilitating
passage of the fecesiv. Return-flow enemas
A return-flow enema, also called a Harris flush, is occasionally used to expel flatus.
Alternating flow of 100 to 200 mL of fluid into and out of the rectum and sigmoid
colon stimulates peristalsis. This process is repeated five or six times until the flatus
is removed and abdominal distention is relieved.
b) Indications and Contra-indications of enema
Enema is indicated to evacuate the bowel before surgery, X-ray or for bowel
examinations such as an endoscopy and to treat severe constipation. The enema
is contraindicated when phosphate or sodium is in high concentration in the blood,
or when calcium is low in the blood. Enema is also contraindicated in the following
condition: dehydration, anal cancer, Laceration or wounds on anus, Hemorrhoid,
Diarrhea, Intestinal occlusion or perforation and Appendicitisc) Complications of enema
A wrongly administered enema can damage tissue in the rectum/colon and
cause bowel perforation and, if the device is not well sterilized can cause the
infections. Long-term, regular use of enemas can cause electrolyte imbalances.
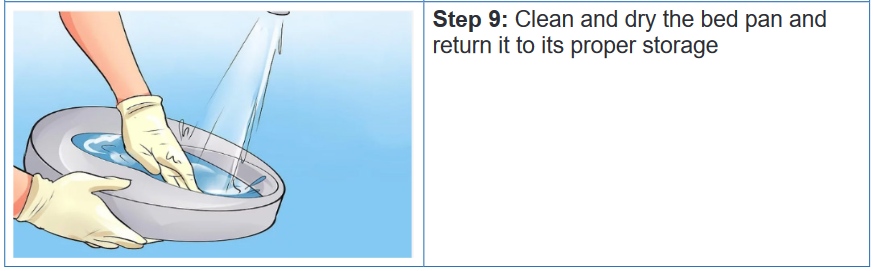
Other effect of enemas can include bloating and cramping.d) Administering enema (evacuating enema/return flow enema)
Nursing Alert
• During the procedure the pulse and blood pressure should be monitored.
If the pulse drops and/or the blood pressure rises, the procedure must be
stopped.
• Assess for presence of feces using Bristol stool score (Figure 31 Bristol
stool score) and record.
• In Scybala-type stool (hard, smaller lumps), remove a lump at a time until no
more fecal matter can be felt and place in receptacle.
• In a solid mass, push finger into the middle of the fecal mass and split it,
remove small sections until no more fecal matter can be felt and place in
receptacle. Do not attempt to hook and drag feces as this can damage the
bowel wall.
• If the fecal matter is more than 4cm in diameter and cannot be broken up,
then the procedure should be stopped and medical advice is required.
• If the feces are hard and dry, consider inserting two glycerin suppositories
30 minutes before commencing the procedure.
• If feces are too soft to remove effectively, consider leaving the patient for
another 24 hours to enable further re-absorption of water content and review
fiber content of diet or prescribe appropriate bulking agent.
• Stop the procedure if the patient complains of feeling unwell, having pain or
bleeding, or if patient asks you to discontinue.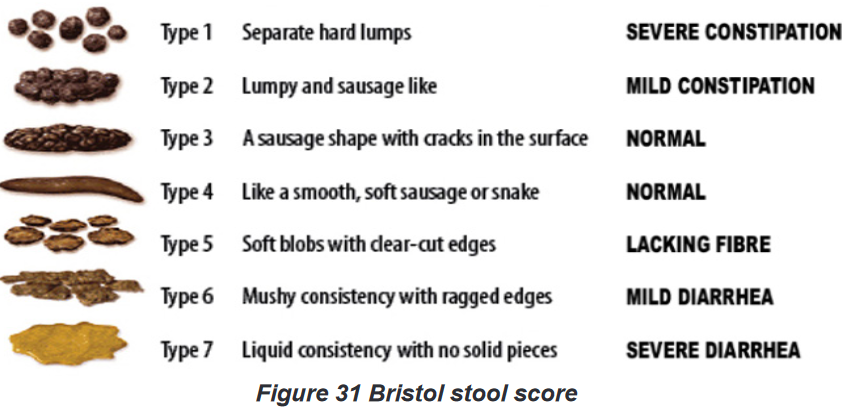
2.7.7. Hygiene Care of ostomies (gastrostomy, ileostomy, colostomy).
A stomy (ostomy) is an opening for the gastrointestinal or urinary tract onto the skin
of the abdomen in the purpose of helping patient with elimination of urines or feces.there are many types of intestinal ostomies: A gastrostomy is an opening through
the abdominal wall into the stomach it is mainly indicated for the purpose of feeding
the patient; A jejunostomy opens through the abdominal wall into the jejunum;
an Ileostomy opens into the ileum; and A Colostomy is an opening through the
abdominal into the colon (ascending, descending or transverse).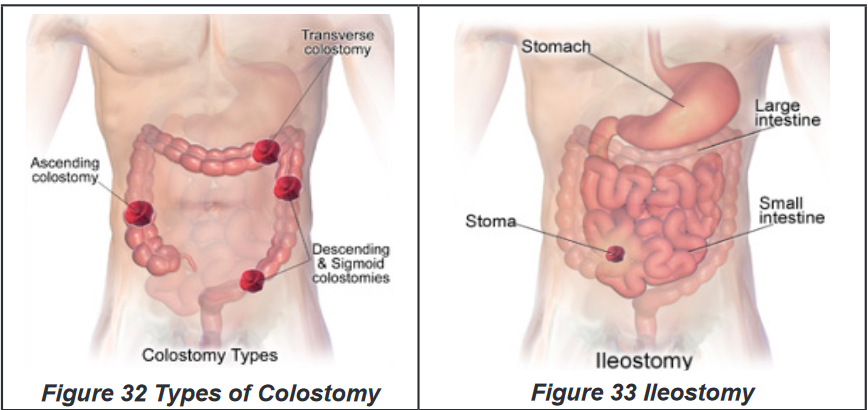
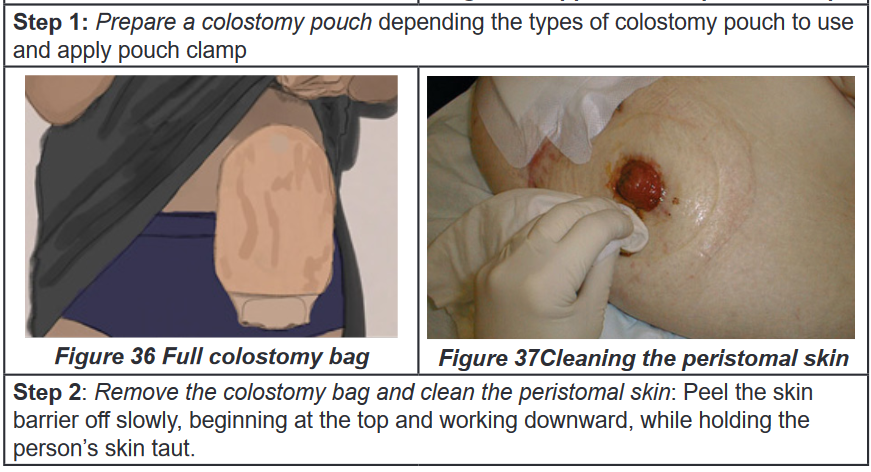
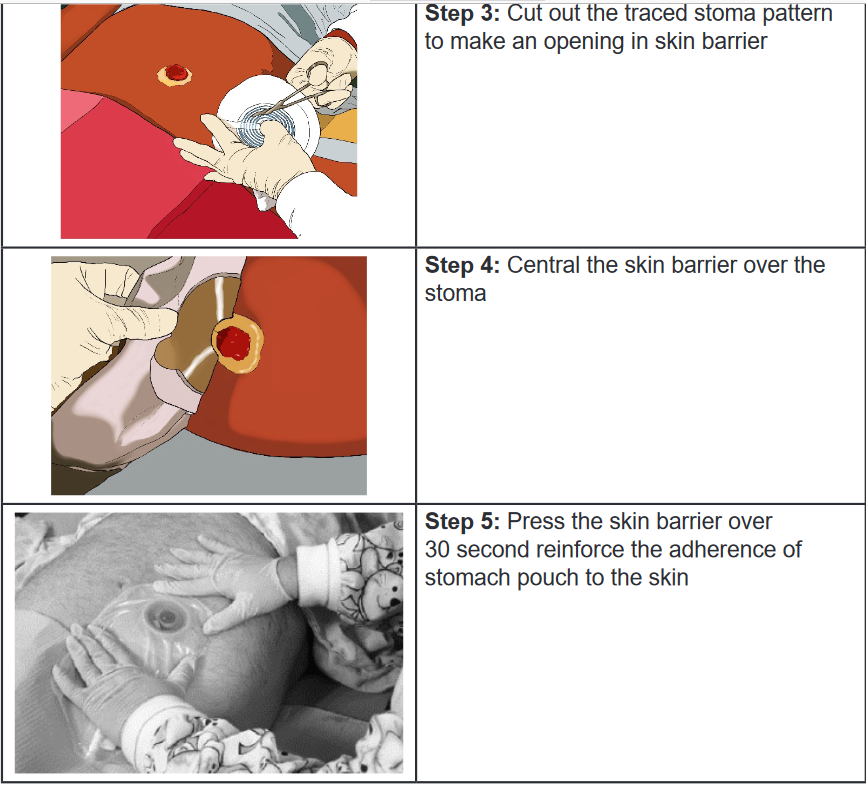
Techniques of providing hygienic care to colostomy or ileostomy: Changing
a colostomy bagPurpose and indications
This procedure is done for the purpose of hygiene and infection prevention of the
patient and is indicated to bedridden patient with colostomy and ileostomy.
Self-assessment 2.7.
1) When caring for male clients at the healthcare facility who require
assistance with urinary elimination, for which of the following clients
should the nurse use a urinal?
a) Clients who can ambulate
b) Clients who are weak
c) Clients who are unable to walk
d) Clients who are confined to bed2) A nurse is caring for a client with severe pain in the abdomen and
constipation resulting from fecal impaction. Which of the following
interventions should the nurse perform to facilitate easy insertion within
the rectum when removing the fecal impaction?
a) Lubricate the fore finger
b) Place the client in the Sims’ position
c) Lubricate the rectal tube
d) Warm the cleansing solution.3) A physician has ordered the nurse to administer an oil retention enema
to a client for easier expulsion. For how long should the nurse ask the
client to retain the cleansing solution within the large intestine?
a) At least 1 hour
b) At least 10 minutes
c) At least 5 minutes
d) At least half an hour.4) All of the following are devices for elimination except
a) Wheel chair
b) Urinal
c) Bed Pan
d) Diaper5) Define the following bowel diversions:
a) Stoma
b) Ileostomy
c) Colostomy6) list the complications of excessive rectal manipulation
7) Identify the primary action of enema
8) What is the purpose of using diaper for adult patients.
End unit assessment 2
Question I
Bathing is a hygienic practice during which a cleaning agent (such as soap) is used
to remove sweat, oil, dirt, and microorganisms from the skin. Answer the following
questions, which involve the nurse’s role in assisting clients with bathing.
A nurse is caring for an elderly client who has undergone rectal surgery. The
client is averse to bathing daily. The nurse needs to ensure that body areas
subject to greatest soiling or that are sources of body odors are cleaned and
infections do not occur
1) What kind of bath should the nurse suggest to the client?
2) What care should the nurse take when providing perineal care to the client?Question II
Many factors affect ventilation and, subsequently, respiration. Positioning and
teaching breathing techniques are two nursing interventions frequently used to
promote oxygenation. Answer the questions related to nursing intervention to
promote oxygenation.A nurse is caring for a client who is brought to the health care facility with
breathing difficulty. The client is diagnosed to have hypoxia.
In what position should the nurse place the client to promote better breathing?Question III
Nursing care activities such as positioning, moving, and transferring clients
reduce the potential for disuse syndrome. Nurses can become injured if they
fail to use good posture and body mechanics while performing these activities.
Answer the following questions, which involve the nurse’s role in preventing
work-related injuries.A nurse is caring for an elderly client with a fractured leg following a fall. When
caring for this client, the nurse should take precautions to prevent injuries to
him- or herself
1) What care should the nurse take before planning to turn and move the
client?
2) What should the nurse do as part of planning to move the client?
Question IV
Asepsis means practices to decrease or eliminate infectious agents, their
reservoirs, and vehicles for transmission. It is the major method for controlling
infection. Answer the following questions, which involve the various aspects of
asepsis that a nurse should follow while caring for clients.
A nurse practices medical and surgical asepsis to accomplish care for a client
suffering from an infection. There are other clients around who should be
protected from the spread of infection.
1) What are the principles or measures the nurse should follow to break the
chain of infection?
2) What are antimicrobial agents?
3) Which antimicrobial agents should the nurse use and why? Define the
role of each type of agentQuestion V
Heat and cold have various therapeutic uses and each can be used in several
ways. Examples include an ice bag, collar, chemical pack, compress, and
Aquathermia pad. Answer the following questions, which involve a nurse’s role
in the application of a compress.
A nurse is caring for a 2-year-old-client who is being treated for viral fever at the
health care facility. The nurse uses a cold compress for the child.
1) What is the purpose of a cold compress?
2) How should the nurse apply the compress to the client?Question VI
1) Identify the risk factors that predispose a patient to pressure ulcer
formation.
a)
b)
c)
d)
e)
2) Staging systems for pressure ulcers are based on the depth of tissue
destroyed. Briefly describe each stage
I.
II.
III.
IV.
V.
