UNIT 4 : ETHICAL ISSUES IN HEALTH CARE
Key Unit competence:
To demonstrate good descision making when facing an ethical issue in nursingpractice
4.0 Introductory activity
1. Ms.K. a 12-year-old, has been admitted to an acute care hospital for an
emergency appendectomy. Her parents have been given information about
the surgery and what to expect in the immediate postoperative period. Three
members of the nursing staff have also assured these anxious parents that
they will be notified as soon as K. is admitted to the post anaesthetic area
or sooner if there are complications with the procedure.
After the surgical intervention and while the client was in the recovery room,
the intravenous catheter was leaking fluid and blood out of the vein and the
client bed was dirty and wet . The care giver informs the nurse in charge
of the recovery room but the nurse doesn’t react. Thirty minutes after, the
client was agitated, sweeting and the monitor shows a low blood pressure.
While the nurse come later, she starts by blaming the mother to careless
about the child, she starts to insert a new catheter in the vein, the phone
rings and takes it, the catheter drains the blood in bed and when he resumes
the procedure , the catheter was obstructed . The client and her mother
refuse to be punctured again and complain to the in charge of surgical Unitabout being not being well cared.
In the following examples, identify the ethical principles that would be appropriate
for the nursing staff to employ:
1. Identify the ethical issues that may arise in the above scenario
2. Identify the ethical principles respected in this case3. Explain the ethical principles of nursing care violated
4.1. Ethical principles in nursing practice
Learning activity 4.1
Miss.J. is 16 and she comes in to the community health centre to ask for abortive
method. The nurse asks her about her sexual life and Joan admits that she is
having sexual relations with her father and her mother is not informed. The
nurse is a family friend of Joan’s family and is quite close to Joan’s mother.
Joan’s father is a policeman and is not easy to communicate with him. The
nurse is quite confused by this news and is not sure how to help Joan who is
very anxious and promise to do unsafe abortion before being discovered by her
mother or prefer to die
1. Explain how the nurse is going to apply ethical principles of autonomy,beneficence and non-maleficence for this client
4.1.1. Definition of Ethics
World Health Organization: “ethics is concerned with moral principles, values and
standards of conduct” (WHO, 2016). Ethical issues are event which occur when a
given decision, scenario or activity creates a conflict with a society moral principles.
This may arise with individuals or institution since any of their activities might be
put to question from an ethical point view, Ethics, is one of the cross-cutting themes
relevant and crucial component to all health care professionals (both in pre-service
& in-service).
The principles of ethics included respect for persons autonomy, beneficence, non
maleficence and justice.
The concept of autonomy is an important extension of this principle; acting
autonomously means that the actions are the result of the person’s own deliberation
and choices. The principle of beneficence is often simply stated as an obligation
to act in ways that promote good. The principle of non-maleficence states that we
should act in ways that do not inflict evil or cause harm to others. While a generalprinciple of justice requires that we act in ways that treat people equitably and fairly
4.1.2. Autonomy and Beneficence
Moral principles are useful in ethical decisions about which action is right or wrong
in a situation especially in health care
a) Autonomy: in health care, respect for autonomy refers to the commitment to
include patients in decisions about all aspects of care as a way of acknowledging
and protecting a patient’s independence. the promotion of independent choice,
self determination and freedom of action, the independence and ability to be
self-directed or Self-governance and self-determination in health care provision.
This means that clients are entitled to make decision about what will happen totheir body
Autonomy is a principle and notion of moral decision making which hold that
a rational person (defined by age and mental ability) has the capacity to make
informed and voluntary decisions. Such a person would need to duly consider and
comprehend the risks and benefits of each choice, based on clear informationand without any controlling influences (e.g., fear, coercion, bribery).
Autonomy is also the capability to have input into determining your own well
being (Purtilo & Doherty, 2016), or self-rule that is free from both controlling
interference by others and limitations that prevent meaningful choice’ (Beauchamp
& Childress p.101)
For example, when a patient faces surgery, the surgeon has an obligation to
review the surgical procedure, including risks and benefits, out of respect for
the patient’s autonomy. The consent that patients read and sign before surgery
documents this respect for client autonomy.
Upholding autonomy - Supporting self-determination in others and their
freedom to choose what constitutes a good quality of life for them (Sasson,2000)
b) Beneficence: Beneficence is doing or active promotion of good, refers to taking
positive actions to help others. The principle of beneficence is fundamental to
the practice of nursing and medicine and refer to all forms of action intended to
benefit others. This is done by providing health benefits to the clients, balancingthe benefits and risks of harm, considering how a client can be best helped.
Example: a child
who has fever has a risk of developing seizures. And
respiratory arrest, if you reduce fever you prevent seizures and promote childhealth (doing good).
In the line of beneficence, Fundamental responsibilities of nurses are
1. To promote health
2. To prevent illness
3. To restore health
4. To alleviate suffering(ICN, 2012; Sezibera & Karugarama, 2011)
4.1.3. Non-maleficence and Justice
a) Non-maleficence: Maleficence refers to harm or hurt; thus no maleficence is
the avoidance of harm or hurt. In health care, ethical practice involves not only
the will to do good, but the equal commitment to do no harm to the client. The
health care professional tries to balance the risks and benefits of care while
striving at the same time to do the least harm possible. The nurse must weigh
the harm against the expected benefit and avoiding deliberated , risk of harm
that occurs during the performance of nursing actions.
Non-maleficence is a principle which holds that no intentional or predictable harm
or injury should be charged against a person, either through acts of commission
or omission. The concept of intention is important in an understanding of non
maleficence. It holds that if a person intended to not harm first, but the end result
was harmful, he/she did not act immoral. Non-maleficence is also intentionally
refraining from actions that contribute to harm (Beauchamp & Childress, 2013;
Purtilo & Doherty, 2016)
b) Justice: justice refers to fairness. Most often used in discussions about access
to health care resources, including the just distribution of resources. Justice is
the promotion of equity or fairness in every situation a nurse encounters. Care
must be fairly, justly, and equitably distributed among a group of patients as itcan be compared to fair distribution of goods in the society
Self-assessment 4.1
Mr.K. is a senior nurse working in Internal Medicine unit for more than 15 years.
He has acquired experience in caring different clients suffering for different
pathologies. A client suffering for hemiplegia (paralysis of one side of the body)
was admitted for further investigations and better management of hemiplegia.
The blood sample for laboratory investigations must be withdrawn, the client
gives consent for procedures but don’t consents for urinary catheter as she has
urinary incontinence. While the nurse has inserted a catheter in the vein, the
phone rings and takes it, the catheter drains the blood in bed and when he
resumes the procedure, the catheter was no longer draining out blood. The client
refuse to be punctured again and complain to the in charge of Unit about beingnot being well cared by the nurse
1. Enumerate the ethical principles what were not respected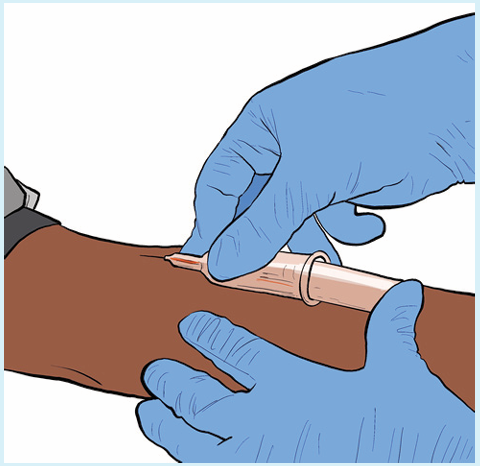
2. How can we qualify the behaviour of the nurse in the above scenario
3. Was the urinary catheter necessary for the client? If yes, how can weproceed to convince the client?
4.2. Ethical issues in nursing profession
Learning activity 4.2
Mrs N. a 50 years old male patient is admitted in surgical ward for post operative
care, he has a body temperature of 37.4 Celsius degrees, a heart rate of 96beats
per minute, SO2 of 98% and blood pressure of 102/62 mmHg. He undergone an
operation for removal of appendix which was infected and the surgical procedure
was successful. However, this patient has no health insurance, he was treated
due to the emergency situation and currently, the social agent discovered that
he is not able to pay for the surgical intervention as well as for other medicines
and procedures required after the operation.
1) What principle is challenged for that patient?
2) How can a nurse will intervene to respond to the needs of that patient
without compromising to the financial policy of the health care institution?
Ethics are essential to the integrity of the nursing profession as it helps ensure better
patient care. Nursing is a highly fast-paced job with new challenges arising daily
and nurse managers across the country all dealing with similar ethical dilemmas.
Many of these situations are rooted in protecting patients’ rights, adequate staffing,
advanced decision-making, and quality patient care.
• Informed Consent
Informed consent can sometimes be an ethical battle for nurses. There is a concern
as sometimes patients do not feel comfortable asking questions and giving consent
without fully realizing the implications of their treatment. If patients feel supported
and trust their doctors and nurses, they are more likely to follow a treatment plan and
experience better outcomes. Nurses should ensure that patients fully understand
all the facets of their treatment plans. The details include knowing all the risks
and the layout of how a procedure will take place or how certain medications
and treatments will affect them. Therefore, healthcare workers should take every
measure to assure their patients understand the treatment plan to obtain informedconsent securely.
• Protecting Patient Privacy and Confidentiality
Patient privacy and confidentiality are significant ethical issues faced by nurses. If not
done correctly, this can have legal ramifications and result in severe consequences
for healthcare professionals. Although nurses must protect their patient’s rights
and act in their best interest, they are still obligated to respect patient autonomy.
Patient autonomy, the right of patients to independently make decisions about their
care based on personal or cultural belief systems, is a prime principle of nursing
and should be respected by all healthcare professionals. With patient autonomy,
patients have the right to refuse medications, treatments, or procedures. Although
this may conflict with suggestions made by nurses and doctors, nurses will still
have to respect this decision and operate accordingly.
• Shared Patient Decision-Making
Shared decision-making is a far more ethical approach to patient care than years
ago when healthcare professionals fully controlled patient treatment. Share
patient decision-making extends patient autonomy where patients and healthcare
professionals work together to make the best decision possible regarding patient
care. With shared decision-making, patients and healthcare professionals have
open conversations about a patient’s background, values, beliefs, and culture,
building a trusting relationship between patient and doctor. A good relationship will
facilitate nurses and healthcare professionals to get patients to communicate and
cooperate properly. When patients are actively involved in decision-making, they
are more likely to be satisfied with their care and trust the doctor’s treatment plans.
• Addressing Advanced Care Planning
Advanced care planning is always a difficult conversation for healthcare professionals
to have, predominately when end-of-life care conversations surround it. These
conversations are between patients and doctors when they need to make plans
for their future health care if they pass away or are left too ill to make their own
decisions. Patients will explore, discuss, and document their personal preferences
regarding their healthcare. This process helps them identify their personal goals
and values about future medical treatment. They also will share who they would like
to make decisions on their health care if they can’t make decisions for themselves.
For example, an issue might be if a patient has asked not to be on a ventilator, but
their immediate family demands. Despite the problematic scenario, nurses mustput the needs and wants of patients first, especially in end-of-life care.
• Inadequate resources and staffing
When medical facilities have scarce resources, patients are at risk of not receiving
proper care leaving nurses to make difficult decisions. Hard decisions may also need
to be made when facilities are faced with inadequate staffing levels. When there is
not enough staff for patients, nurses do not have the time to do everything needed
for each patient. Patient needs can include recovery times or even addressing the
patient’s emotional and physical needs. A nurses’ moral obligations to patients are
compromised due to work restraints and stress overload. They are left with mentalstruggles trying to decipher where they should focus their priorities.
Self-assessment 4.2
1. What are the 5 common ethical issues in nursing practice?
2. Explain any possible 4 factors that may originate a conflict of interest may
occur in nursing practice.3. What should nurse do in case conflicts are occurring in healthcare?
4.3. Health System and Ethical Challenges
Learning activity 4.3
Mrs.T. aged 68 years old is admitted in Accident and Emergency unit ward for
pulmonary oedema and presents respiratory distress with dyspnoea SO2 65 %
and is in unconscious status. Mr C. the nurse on the shift has no enough bed and
is obliged to put the patient near the other patient who was treated from Covid 19
and tested negative with rapid test but yet the final result from a confirming test
is not yet found and is waited in two hours.
1) What are the ethical issues presented in this situation G.?2) Relate the ethical issue with the ethical principle challenged in this case?
a) Health system challenges
Health system policies or challenges can sometimes contribute to situations of
ethical challenges
Examples:
• Shortage of healthcare professionals
• Large number of patients
• Health insurance payment structure: patients’ lack of health insurance or
money, delays in payments to hospital
• Inequity in distribution of equipment and materials, etc.
b) Challenges and Emerging Health Systems Issues in Rwanda
• Insufficiency of trained health care providers
• Lack of integration and accessibility of NCDs services at all levels of the
healthcare system,
• Specialized NCDs services,
• High NCDs costs and lack of funds mobilization frameworks at global, regional
and national levels,
• Lack of basic equipment and specialized infrastructure for NCDs,
• Essential drugs and advanced NCDs treatment, and
• Lack of proper NCDs data management
All of them they can indirectly contribute to ethical challenges (Yiika Sejdiu, 2018)
c) Dealing with Ethical Issues in Nursing
Every nurse should become familiar with the Code of Ethics for Nurses. The
hospital’s ethics committee, the hospital code of conduct or a variety of educational
resources. Some organizations have an ethics consultation service whose members
assist staff to discuss about any ethical issue that occurs.” Also, having a diverse
group of nurses allows an environment where conversations on ethical issues occur
within their units. These open dialogues will benefit the patients as they feel more
welcomed and recognized by their hospital staff. Example: Another ethical dilemma
for nurses is the refusal of medication and vaccinations from patients and their family
members. Vaccinations often become a high debate, especially when addressing
childhood vaccinations. Although it is a parent’s right to refuse immunization for
their child, healthcare professionals must share the health risks this poses for the
future of their child’s health. Nurses must provide them with accurate information
while also respecting boundaries.
MORAL model to address ethical issues
Usually, the MORAL model is used likely the easiest model to use in everyday
clinical practice site, consisting of similar constructs as the nursing process, the
MORAL model has five steps:
1) Massage the ethical issue: develop a full understanding of the ethical conflict
and gather information about the situation
2) Outline the options
3) Resolve the ethical issue
4) Act by applying the chosen option,
5) Look back and evaluate.
Health policy concerns the choices that a society or a part of society makes in
regard to the health and welfare of its citizens. Nurses are frequently involved in
health policy issues in everyday clinical settings.
E.g.: Insufficiency of nursing staff, limited prescription authority legalized abortion
Moral distress, defined as a painful state of imbalance seen when nurses make
a moral decision but are unable to implement the decision because of real or
perceived institutional constraints, can be positively addressed in the workplace.E.g.: patient who missed the oxygen due to high demands in period of COVID -19.
Self-assessment 4.3
1) What are the challenges occurring in health system that may lead to
ethical challenges in nursing?2) Provide 5 examples of issues in health system occurring in Rwanda
4.4. End unit assessment
A. MULTIPLE CHOICE QUESTIONS
1. The essence of doing justice refers to One among the following
a. Giving money to poor patients for buying drugs
b. Provide appropriate care without discrimination
c. Identify particular cases for social support
d. Bring to court the nurses who are unethical
2.The no maleficence principle is applied in One among the following actions
a. Avoid to give injection for not harming the patient
b. Check and verify the correct drug and dose before injection
c. Avoid to report a nurse who is unethical to the patient
d. Hiding the patient who is vulnerable to the drug abuse
3.The ethical issues are raised due to which among the following situations
a. Insufficient staff in nursing
b. Lack of support for professional development
c. Difficulties in Health system policy
d. All of the above
4. Ethical dilemma refers to one among the following
a. Informed consent
b. Disclosure of medical conditions
c. Incompetence among peers
d. All of the above
5. The principle of beneficence refers to One among the following nursing
activities
a. Communicate effectively and friendly to the colleagues
b. Performs the nursing care to the assigned patients
c. Provide support when the number of nursing staff is not sufficient
d. All of the above
6. The following actions are not respecting the principle of No maleficence Except
a. Absenteeism
b. Reporting to the doctor when there is error on the drug prescription of the
patient
c. Injecting the wrong dose to the patientd. Not documenting the data examined on the patient’s file
7. The principle of autonomy is applied in which One of the following situations?
a. Provide health education
b. Ensure patient privacy
c. Explain the informed consent formd. Provide the drug prescribed
8. Among the following reasons, One is Most appropriate to justify why nurses
should respect clients
a. Respect the culture
b. Religious customs
c. Inspire trust from the client and the publicd. Practice citizenship
B. SHORT ANSWER QUESTIONS
1. Define ethical issue in nursing?
2. Illustrate with an example an ethical issue
3. The challenges occurring in health system that may lead to ethicalchallenges in nursing?
C. Additional activities
1. Remedial activities
1. Explain briefly the meaning of ethics in health care
2. Enumerate 4 qualities / traits of good health professional that you would
like to see on the nurse who is caring a friend of yours
3. What are the primary moral principles of nursing practice?
2. Consolidation activities
a. According to what you have observed in health institution in which you
have been or what you have heard in discussing with your colleagues,
What must be the causes of unethical behaviour?
b. As a student in the program of associate nurse, after learning the ethical
issues which may arise during provision of nursing care, identify at least 4common ethical issues which may occur in working place.
3. Extended activity: You are working in health centre receiving clients I
suffering for different health problems which you have adults, middle ages
clients and under 15 years clients and you haven’t sufficient desk to give a
seat to everyone
a) Which clients are you going to select and according more respect?
b) What can you do to improve the working environment and the wellbeing
of clients?c) Which nurse’s value are you going to promote
References
• Elizabeth Manias, Fiona Geddes, Bernadette Watson, Dorothy Jones and Phillip
Della Perspectives of clinical handover processes: a multi-site survey across
different health professionals Journal of clinical nursing 2015 25, 80–91, Doi:
10.1111/jocn.12986
• Doreen M. Towsley-Cook Terese and A. Young 2007 Ethical and legal issues for
imaging professionals Mosby Elsevier Philadelphia US p.2-8
• Barbara Cherry Susan R. Jacob Contemporary nursing issues, trends, and
management pp.411
• Nico Nortjé Willem A. Ho mann Jo-Celene De Jongh Editors 2018 African
Perspectives on Ethics for Healthcare Professionals SPRINGER
• Sue West, Senior Nursing Education Adviser, 2019 Blog: https://www.nmc.org.
uk/news/news-and-updates/blog-whats-a-nursing-associate/
• https://www.google.com/
• https://pmi.edu/blog/march-2021/what-5-qualities-make-a-good-nursing
assistant
• Bandman Elsie L , ( 2004 ) Nursing Ethics Through the life span , 3rd edition ,
Stamford Connecticut
• Zane Wolf ( 2012) , Measure nursing: official journal of the Academy of Medical
Surgical Nurses, 21(1):16-22,6
• Doreen M.Towsley-Cook, Therese A. Young ( 2007 ) Ethical and Legal issues for
Imaging Professionals , Mosby, Inc affiliate Elsevier Inc.
• Ian E Thompson ; Kath M Melia et al (2006 ), Nursing Ethics, 5th Edition ,
Churchill, Livingstone Elsevier
• Rwandan regulatory body Nursing Council of Nurses and midwives (NCNM)
adopted by the constitution of the Republic of Rwanda of 04 June, 2003 and
the Law no 25/2008of 25/7/2008 establishing the National Council of Nurses and
Midwives and adopted by the cabinet in its session of 09/07/2010
• International Council of Nurses (ICN) in Sao Paulo (Brazil) in July 1953 and
revised by the same council in Frankfurt (West Germany) in June 1965.
• The NMBI (2014) Code of Professional Conduct and Ethics
• Bord Altranais agus(2007) Code of Professional conduct for Registered Nurses
and Registered Midwives , Nursing and Midwifery Board of Ireland13. Legal
Principles and the Limits of Law Joseph Raz in https://core.ac.uk/download/
pdf/160248327.pdf
• BASAVANTHAPPA , BT ( 2006) , Fundamentals of nursing, 2nd edition , pages
99- 121, JAYPEE BROTHERS MEDICAL PUBLISHERS, SAINT LOUIS USA
• Margaret Keatings, O’ Neil B. Smith ( 2000), Ethical and Legal Issues in
Canadian Nursing, 2 nd Edition, Saunders Elsevier
• Universal Declaration of Human Rights (United Nations, 1948) which proclaims
that the basis for freedom, justice and peace is founded on the recognition of
the inherent dignity and of the equal and of the absolute rights of human beings.
• The European Convention on Human Rights (Council of Europe, 1998), the
Irish Constitution (Government of Ireland,1937) and the Equal Status Acts
(Government of Ireland, 2000-2008)
• Bord Altranais agus(2007) Code of Professional conduct for Registered Nurses
and Registered Midwives , Nursing and Midwifery Board of Ireland
• ANA’s Principles for Nursing Documentation Guidance for Registered Nurses
2010
• The NMBI (2014) Code of Professional Conduct and Ethics in the Irish health
care context
• Code of Professional Conduct and Ethics for Registered Nurses and Registered
Midwives Draft October 2013
• Potter and Perry (2017) , Fundamentals of nursing , 8th edition, Elsevier, pages
287 -29
• American Nurses Association. (2015b). Nursing: Scope and standards of
practice (3rd ed.). Silver Spring.
• THOMSON Reuters (2021).Nursing and Midwifery Council: sanctions: https://
uk.practicallaw.thomsonreuters.com/w-003-7294?transitiontype=default&conte
xtdata=(sc.default)&firstpage=true
• STEFEN P.O Keef (2021), https://www.gomedmalohio.com/practice-areas/
medical-malpractice/hospital-or-nursing-negligence/
• http://www.nmbi.ie/Standards-Guidance/Code)
• http://www.nmbi.ie/Standards-Guidance/Code
• https://www.google.com/search?q=Role+of+the+regulatory+bodies+in
+nursing+profession+according+to+ICN&sxsrf=AOaemvLte5VkNKKS1_
3IH22boDuUpnKCeg%3A1631195576019&ei=uBE6YfBX1NSBBtWSpSA&oq
=Role+of+the+regulatory+bodies+in+nursing+profession+according
• https://www.slideshare.net/lindadevi1/legal-issues-in-nursing-ppt-11889901 ;
• https://www.google.com/search?q=meaning+of+bad+nursing+practice&biw=
1120&bih
• https://www.medleague.com/same-day-surgery-nursing-malpractice/
https://rnspeak.com/nursing-negligence
• https://www.google.com/search?q=what+is+the+meaning+of+nursing+practice
&oq=whait+is+the+meaning+of+nursing+practice&aqs=ch
&oq=
• https://www.google.com/search?q=what+is+the+meaning+of+nursing+practice
&oq=whait+is+the+meaning+of+nursing+practice&aqs=ch
• https://www.google.com/search?q=what+is+the+meaning+of+nursing+practice
• https://www.google.com/search?q=Role+of+the+regulatory+bodies+in+nursing+
profession+according+to+ICN&sxsrf=AOaemvLte5VkNKKS1_3IH22boDuUpnK
Ceg%3A1631195576019&ei=uBE6YfBX1NSBBtWSpSA&oq=Role+of+the+
regulatory+bodies+in+nursing+profession+according+to+ICN&gs_lcp=Cgdnd3
Mtd2l6EAw6BwgjELADECc6BwgAEEcQsAM6BwgjELACECc6BAgAEA06C
AghEBYQHRAeOgcIIRAKEKABOgQIIRAVSgQIQRgAUJBjWI_zAWDOjAJoA
XACeAGAAZIGiAH0iAGSAQozLTMuNi4xNy40mAEAoAEByAEJwAEB&
sclient=gws-wiz&ved=0ahUKEwjwk_iGhfLyAhVUasAKHVVJCQQQ4dUDCA4
• http://www.nmbi.ie/Standards-Guidance/Code ;
• https://www.google.com/search?q=RNMU&oq=RNMU&aqs=chrome..69i57.
6640j0j7&sourceid=chrome&ie=UTF-8
• https://journals.sagepub.com/doi/abs/10.1177/019394599101300407?journalC
ode=wjna
• UK NMC We regulate nursing associate 2020 https://www.nmc.org.uk/about-us
/our-role/who-we-regulate/nursing-associates/
• Standards of proficiency for nursing associates 2018 http://www.nmc.org.uk/ ;
• International Journal of Caring Sciences September-December 2015 Volume 8
| Issue 3| Page 830 www.internationaljournalofcaringsciences.org Review
Article Ethical Issues and Dilemmas Encountered in Nursing Practice in
Turkey Nevin Utkualp, PhD Lecturer Uludağ University.
• Basso-Musso L. Nursing and the resolution of ethical dilemmas. Invest Educ
Enferm. 2012;30(2):260-268
• Abeer M. Zakaria , Wafaa F. Sleem and Abeer Mohamed Seada, 2016.
Effectiveness of ethical issues teaching program on knowledge,
ethical behaviour and ethical stress among nurses, Journal of Nursing
Education and Practice 2016, Vol. 6, No. 7doi: 10.5430/jnep.v6n7p125http://
jnep.sciedupress.com
• American Nurses Association, 2010.Code of ethics for Nurses with interpretive
statement,
• https://www.princetonhcs.org//media/princeton/documentrepository/
documentrepository/nurses/code-of-ethics.pdf
• Saima Hamid, Rabia Kanwal, Mohammad Hamza Bajwa, Sadaf Khalid and
Henna Mubarak 2016. Ethical Issues Faced by Nurses during Nursing Practice
in District Layyah, Pakistan. Diversity and Equality in Health and Care 13(4)doi:10.21767/2049-5471.100068
