Topic outline
UNIT 1: ABSCESS AND PHLEGMOM
Key Unit competence
Take appropriate decision on abscess and phlegmon conditions
Introductory activity 1.0
Observe skin structure displayed on image A, B and C below and answer to the questions below.
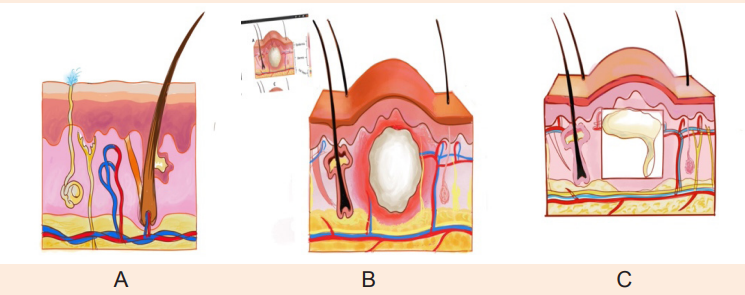
1. Reference to what you learned in anatomy and physiology, which one of the three images would reflect the normal structure of the skin in the human body?
2. What characteristics/elements would indicate the abnormalities in the structure of the skin? Describe the abnormalities that you have observed if any.
3. What do you think can cause the abnormalities that you have observed?
4. What are the manifestations of the observed abnormalities in the human body?
5. How can health personnel identify these abnormalities?
6. How can these abnormal structures be collected?
1.1. Description of Abscess and phlegmon
Learning Activity 1.1
K.A, a previously healthy 18-year-old young man presents with history of pain and swelling on his right thigh and in the left arm pit since 4 days. K.A reported that he was injured by his colleagues when playing football last month. K.A also reports that he normally has excessive sweat in the arm pit and has been shaving his axillary hair with same disposable razor for long time. Last night K.A had headache and fever.
After taking his vital signs, the nurse found that all vital signs are within normal limits, except the slight increase of the body temperature (37.8C). On examination, the health care provider found that there is a 3 x 3 cm confined fluctuant, warm, tender, and erythematous mass. There is no drainage or associated open wound. In addition to that another one unbounded small (1 x 2 cm) mass in the left arm pit was diagnosed. The health care provider requested to take blood sample of FBC that showed a slight increase of WBC.
The medical doctor concluded that the mass on the right leg was an abscess and that the one on the left arm pit is the phlegmon.
Questions related to the case study.
1. From the case study above, identify the risk factors that can be associated with abscess and phlegmon
2. Explain the pathophysiological mechanisms behind swelling, tenderness and local heat
3. Describe the signs and symptoms of K.A described in the case study.
4. From the signs described in the case study, what is the key characteristic that differentiates abscess from phlegmon?
1.1. 1. Definition of abscess and phlegmon
An abscess is accumulation of pus in soft tissues. It may be difficult to differentiate abscess from phlegmon but abscess is confined to the area of infection (image B, introductory activity 1.0) and phlegmon is unbounded and can keep spreading out along connective tissue and muscle fibre (image C introductory activity 1.0). Abscess and phlegmon can be internal or external. The most common site of external abscess and phlegmon include inguinal and axillary areas, anus, vaginal (Bartholin gland) and neck.
1.1.2. Causes and Pathophysiology of abscess and phlegmon
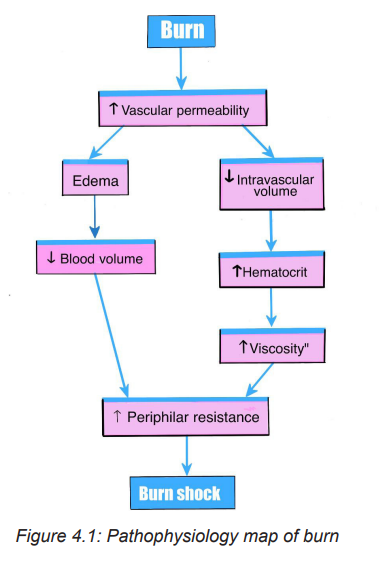
Abscess and Phlegmon are frequently caused by bacteria; most often group A streptococcus or Staphylococcus aureus. People with compromised immune system may be vulnerable to abscess and phlegm on formation. Bacteria may enter via a scratch, insect bite, or injury. It kills the local cell, resulting in the release of cytokines. Cytokines trigger an inflammatory response (figure 1.1); a large numbers of white blood cells migrates to the area then increases the regional blood flow.
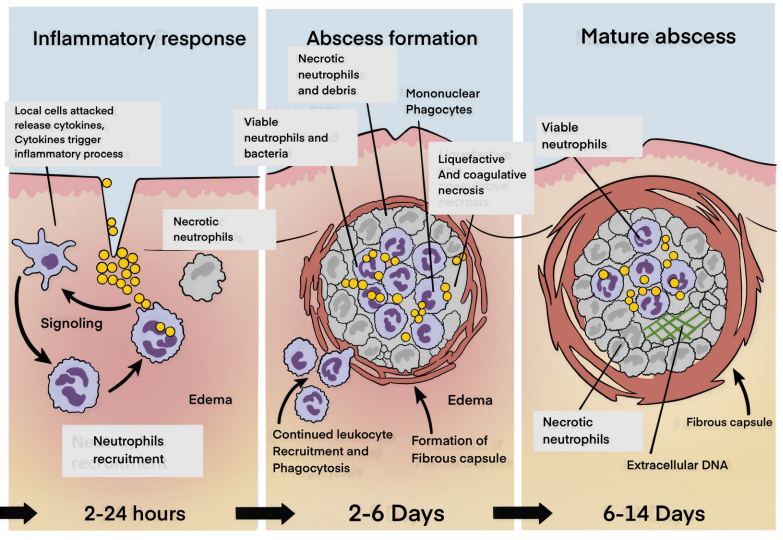
Figure 1.1. Pathophysiology of abscess
The increased blood supply leads to increased temperature of the area, pain, swelling and redness. The final structure of the abscess consists of the central cavity with pus and a surrounding wall, which is the pyogenic membrane. If the natural and acquired resistance of the host is adequate, the pyogenic membrane is rapidly replaced by granulation tissue which prevents the systemic invasion of bacteria (figure 1.2).
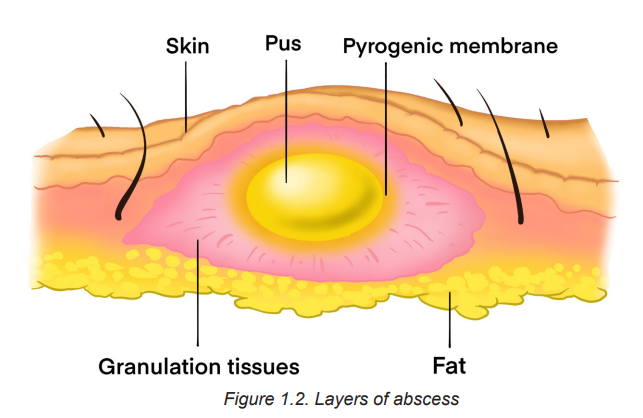
Pus is a viscous liquid that consists mostly of dead and dying neutrophils and bacteria, cellular debris, and fluid leaked from blood vessels. Because an abscess is virtually inaccessible to antibodies and antibiotics, it is very difficult to treat. Sometimes a surgical incision is necessary to drain and eliminate it. Some abscesses, can burst of their own accord. The abscess cavity then collapses, and the tissue is replaced through the process of repair.
1.1.3. Signs and symptoms of abscess and phlegmon
Signs and Symptoms of skin abscess and phlegmon vary, depending on the location and severity of the infection. If not treated, an infection can spread to deeper tissue and disable the limb or area involved. Local signs of skin abscess and phlegmon can be: heat, redness, sore, swelling and pain. A patient may also have systemic signs of a bacterial infection, such as swollen lymph glands, fatigue, fever and headache.
1.1.4. Diagnostic measures
Skin abscess and phlegmon are visible and can easily be diagnosed through inspection. Palpation on the area of pain can reveal lumps or tenderness. For internal abscess different laboratory and radiology tests can be ordered, which may include Full blood count (FBC), ultrasound, X-ray, MRI and CT scan. The results of FBC may show elevated WBCs mainly neutrophils.
Self-assessment activity 1.1
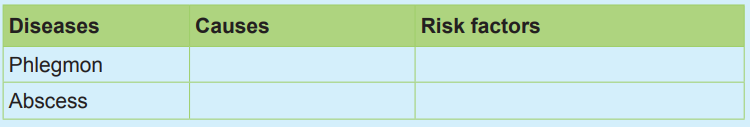
The following are the causes and risk factors of abscess and phlegmon, use them to complete the table below:
Staphylococcus area, injury, bite, scratch, excessive sweat, low immune system
1.2. The management of abscess and phlegmon
Learning Activity 1.2
After different investigations the health care provider decided to do the incision and drainage to evacuate pus and debris. In the post-incision report, the health care provider noted that
K.A will receive oral antibiotics and painkiller medications. K.A received his medications and was discharged home and given appointment after 3 days for wound dressing change.
Questions related to the case study.
1. What is the surgical treatment plan adopted by the health care provider for KA?
2. Discuss in group, different medical treatment prescribed to this patient and give an example of appropriate drug on each group of medication (antibiotics and painkiller).
1.2.1. The treatment plan of Abscess and phlegmon
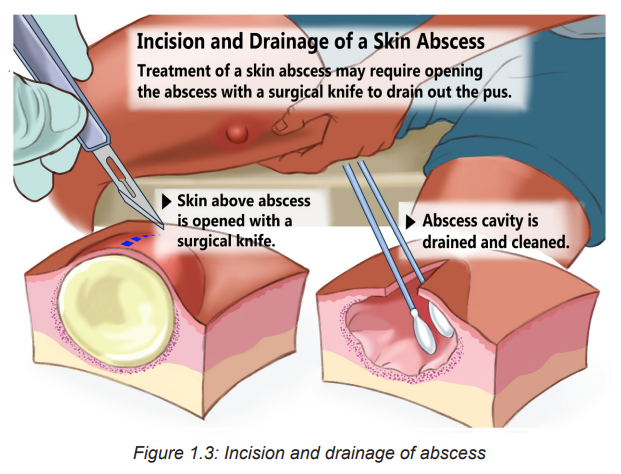
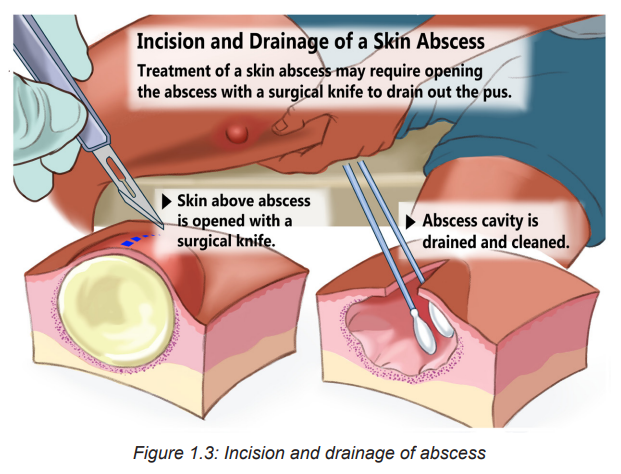
The treatment of Abscess and phlegmon is oriented by the level of severity. Minor phlegmon may be treated with oral antibiotics. But incision and drainage may be performed to clean dead tissues and prevent the spread of infection. Incision and drainage is the treatment of choice of abscess (figure 1.3). The site of incision and drainage is performed to evacuate pus and debris.
Antibiotics and pain killer medications are also prescribed to subside infection and relieve pain. The appropriate duration of antibiotics for treatment of skin and soft tissue infection depends on the nature of the clinical presentation, and the clinical response should guide duration of therapy.
! Consideration for practice
Antibiotics are not mandatory in the post abscess incision and drainage. Other clinical considerations may guide the decision of antibiotics such immune status, living conditions, size (≥2 cm), multiple lesions, systemic signs such as fever, inadequate response of incision and location of the abscess and phlegmon.
1.2.2. Evolution and complications of abscess and phlegmon
The untreated abscess and phlegmon can spread infection to the surrounding tissues and even into the bloodstream causing an infective endocarditis and a systemic infection (septicaemia). The reoccurrence of abscess and phlegmon may be possible.
Self-assessment activity 1.2
1. Do patients with abscess always receive antibiotics during post-incision and drainage? Justify your answer.
2. How can external and skin abscess and phlegmon be diagnosed?
1.3. End of unit assessment
End of unit assessment
1. Identify the common sites of abscess and phlegmon
2. Which one of the following is not a sign and symptom of an abscess and phlegmon (choose the best answer)?
a) Redness
b) Swelling
c) Nausea
d) Local heat
3. Incision and drainage is the best option for the treatment of abscess and phlegm. What are the pathophysiological reasons justifying this best option?
4. A forty-year-old woman presented with the chief complaint of redness, pain, swelling of left groin. She was previously treated with oral pain killer without improvement. The physical examination showed that there is a fluctuant, tender, and erythematous mass, and warm on touch on the left groin. The Health Care Provider (HCP) suspected an abscess.
a) What are the questions with regard to abscess, the HCP will ask to complete the history of this woman?
b) What are the disturbed needs of this patient?
c) Draw a teaching plan that will help this woman to prevent the complications of the abscess
UNIT 2: SKIN ULCERS AND STOMIES
Key Unit competence
Take appropriate decision on skin ulcers and stomies conditions
Introductory activity 2.0
Observe the images displayed below in box A and B, and answer to the questions below.
1. Reference to what you learned in anatomy and physiology, and the first
Unit of Surgical Pathology, which organ of human body is displayed by images in box A and in Box B?
2. What characteristics/elements would indicate the abnormalities in the structure of the affected organ, in Box A and Box B?
3. Describe the abnormalities that you have observed if any.
4. What do you think can cause the abnormalities that you have observed?
5. What are the manifestations of the observed abnormalities in the human body?
6. How can health personnel identify these abnormalities?
7. How can these abnormal structures be collected?
2.1 Description of Ulcers
Learning Activity 2.1
You are on day duty in surgical in-patient for females, and you are caring for Mrs. M.E, a 62 years old female patient. She is on 15th day of hospitalization for total hip replacement (following a left hip fracture secondary to road traffic accident by a motorcycle) and the discharge is planned in 3 days. She is 1, 65 meter and she weighs 85 kg, with a history of diabetes, and hypertension. Mrs. M.E. is only able to move with help and spends most of her time in bed or a wheelchair. In her documentation, it is also specified that she has stage. II pressure ulcer on her sacral area. You are doing discharge teaching with her daughter, who is her primary caregiver. You explain the importance of preventing further skin breakdown and further complication that she needs to reposition her mother every 2 hours.
Questions related to the case study:
1. What do you understand by pressure injury?
2. On which signs and symptoms do they base on to classify Mrs. M. E’s pressure ulcer as stage II?
3. From the case study above, identifying the risk factors that can be associated with Mrs. ME’s. skin ulcers /pressure injury
2.1.1 Definition of skin ulcers
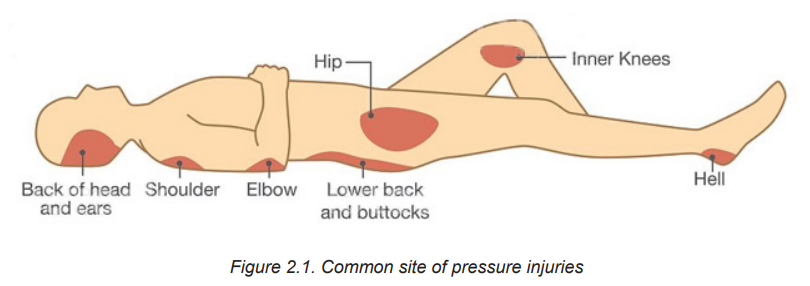
Skin ulcer is an open sore in the skin caused by poor blood flow. Skin ulcers mostly affect the legs, and can also show up on the feet, back, and hips. They are more common in older people and patients with peripheral vascular disease like those with diabetes. Pressure ulcers or injuries are example of most commonly occurring skin ulcers among hospitalized patients. The most common site of pressure injuries are shown on the figure below 2.1:
2.1.2 Types of skin ulcers, Signs and Symptom
Four types of skin ulcers exist. Each one has a different cause and slightly different symptoms. Skin ulcer types include:
Venous skin ulcers
Venous skin ulcers are caused by poor blood circulation in the leg veins. They usually affect the leg between the knee and ankle. Leg ulcers are mostly venous ulcers (80-90%).
Arterial skin ulcers
Arterial ulcers, or ischemic ulcers, happen when blocked arteries cause poor blood flow. These ulcers commonly form on the lower leg, feet, heels, toes, outer side of ankles. Arterial ulcers are usually very painful. Pain might get worse at night or when the legs aren’t moving.
Neuropathic skin ulcers
Neuropathic ulcers are caused by nerve damage and narrow arteries. They’re also called diabetic foot ulcers. These ulcers typically occur on the pressure points of the foot. This includes: heels, toes, and bottom of feet. Neuropathic foot ulcers affect about 15 percent of people with diabetes.
Decubitus (pressure) ulcers
Decubitus ulcer, pressure sore, pressure ulcer, pressure injury, bed sore, are the term used interchangeably. The use pressure injury as the best term, given that open ulceration is not always present.
It is defined as “A localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense pressure, prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue”. Pressure injuries usually affect the back, hips, buttocks, ankles, and heels.
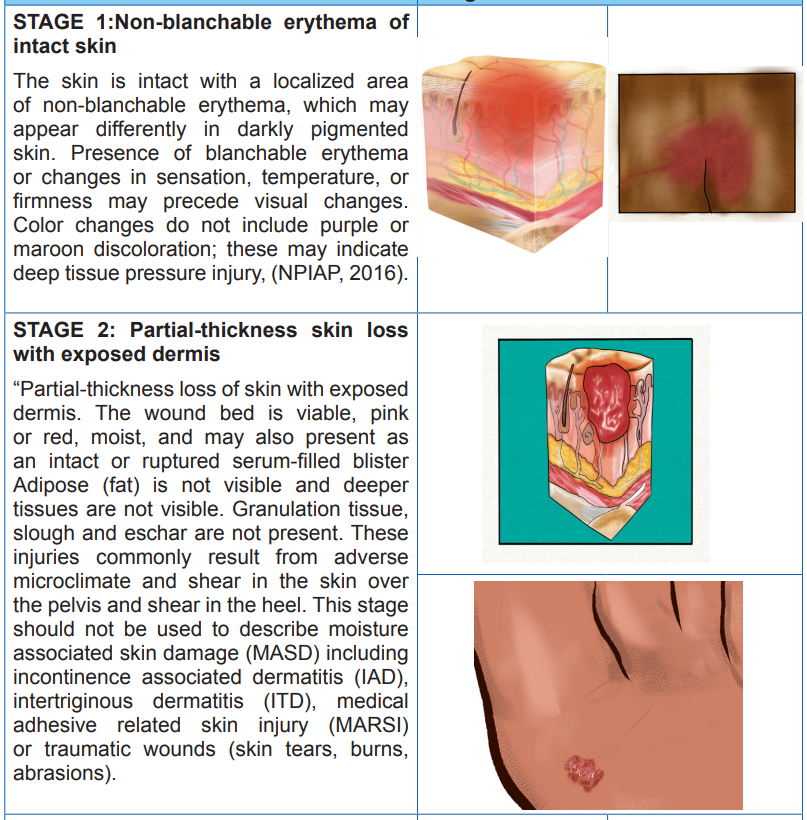
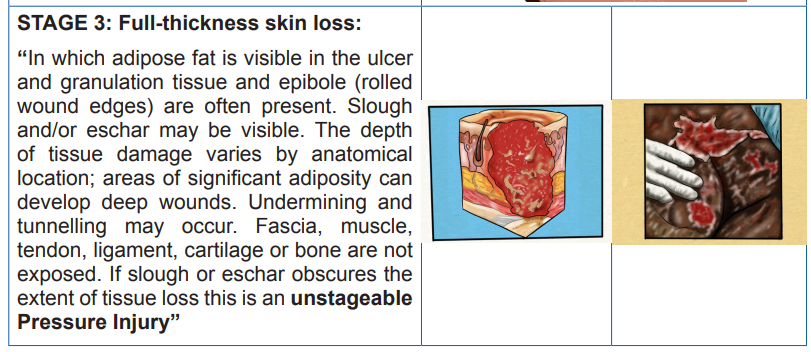
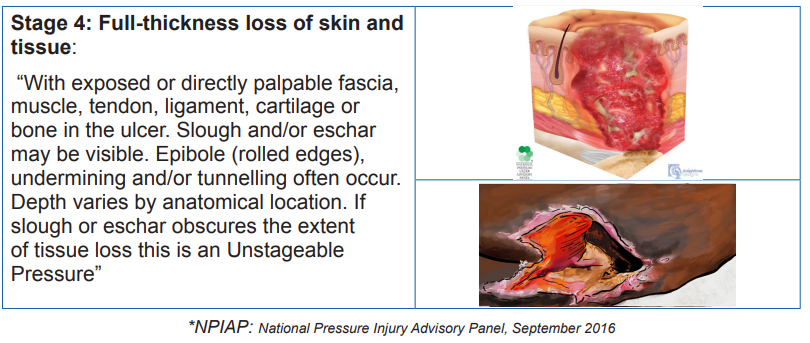
Table2.1. Stages of Decubitus /Pressure injuries/ ulcers
2.1.3 Common Signs and symptoms of a skin ulcer
Signs and symptoms depend on the types and the severity of the skin ulcer. A skin ulcer generally, looks like a round open sore in the skin. Its outer border might be raised and thick. Others signs and symptoms may include itchiness, skin discoloration (in early stage) pain, redness (for darker skin tone, it may look shiny or blue) swelling and tenderness around the ulcer. Additionally fever, bleeding, or pus (yellow or green pus due to an infection) draining from the ulcer may be noticed. The more the skin ulcer gets worse, the more it will look like a crater.
Self-assessment activity 2.1
From your readings, please use the provided words to fill out the table below:
“Non-blanchable erythema of intact skin, Older age, Pain, Redness, Venous skin ulcers, Peripheral vascular disease, Round open sore with thick and raised outer border, Ankles, Heels, Decubitus ulcers, Poor blood supply , Tenderness around the sore, Back of The head(occiput) and ears, Itchiness, Skin discoloration , Swelling, Poor blood flow, Back, Neuropathic skin ulcers, hips, Buttocks, Partial thickness skin loss with exposed dermis, elbow, shoulders,
2.2. Causes, risk factors, overview on pathophysiology and diagnostic measures of skin ulcers
Learning Activity 2.2
… Continuation of M.E case study. The day prior discharge of Mrs. M.E, she was complaining of fever. The vital signs were To 380 C, Pulse 88 beats /min, BP 82/59, RR 20 resp/min. The full blood count was done and leucocytosis was noticed with decreased haemoglobin. The examination of pressure injury revealed a dirty dressing with foul smelling and pus discharge. Adipose fat in the wound was also visible but tendon, fascia, muscle, ligament, and cartilage were not visible. The care givers reported that after being home back to look for money (leaving her little sister with their mother), she came back and found out that their mother is no longer eating well, and is weak.
Questions related to the case study:
1. Identifying the risk factors that can be associated with Mrs. ME’s deteriorated health status?
2. What are the underlying cause of her hyperthermia and leucocytosis?
3. At which stage of pressure injury is her pressure now?
4. Briefly describe the pathophysiological mechanism behind her pressure injury
2.2.1 Causes and pathophysiology of ulcers
The skin ulcers develop when there is a lack or reduced blood circulation. Causes of poor blood flow include:
a) Diabetes: lack or insufficient insulin production by islet of Langerhans in the pancreas to metabolise the sugar lead to high blood sugar. Over time, high blood sugar lead to nerve damage, a situation called peripheral neuropathy. The last one lead to decrease or loss of sensitivity including in feet and legs. Unfelt pressure and pain will lead to unrecognized injury in feet or legs. Untreated injuries can easily turn into skin ulcers, and high blood sugar slows down the wound healing.
b) Atherosclerosis or arteriosclerosis: is a disease whereby the arteries become narrow due to fat build-up called plaque, a situation which hinder the blood circulation leading to poor blood supply to body organs particularly extremities. If left untreated, the body organ which are not well perfused the skin tissue will break down and a sore will be formed
c) Venous insufficiency: occurs when the veins cannot send blood from legs to the heart. Blood collects in the leg veins, which leads to swelling. If the swelling is severe, it can put pressure on skin and cause ulcers. (Causes of venous insufficiency include varicose veins and blood clots).
d) Pressure: Pressure ulcers /injuries begin when staying in one position for too long, the individual’s body weight exerts a downward constant force on the skin and subcutaneous tissue that lie between a bony prominence and an external surface (such as a mattress or wheelchair cushion). Sustained pressure from medical devices may also cause pressure injuries. It is generally thought that force that results in an external pressure more than the arterial capillary filling pressure, around 32 mm Hg, and more than the venous capillary outflow pressure, around 8 to 12 mm Hg, inhibits blood flow and results in local tissue hypoxia. Sustained external pressures above a threshold causes prolonged ischemia and sets the tissue down a path toward necrosis. Reperfusion injury, which occurs because of the return of blood supply after a period of ischemia, has been posited as an additional source of tissue damage leading to pressure ulcers/injury. The highest pressures often occur at the interface of bone and muscle, causing necrosis at this depth while leaving the skin relatively spared
NB: The following microbial (bacteria), also play a role in pressure injuries infections:
– Staphylococcus aureus
– Pseudomonas auruginosa
– Proteus mirabilis
– Enterococcus faecalis
2.2.3 Risk factors of skin ulcers/injuries
Risk factors of developing skin ulcers include:
– Increasing age: due to increased atherosclerosis and venous insufficiency.
– Limited mobility. Being bedridden, paralyzed, or using a wheelchair puts the skin under constant pressure, decreased blood perfusion to tissue, hypoxia and necrosis or open sore
– Cigarette smoking. Smoke hardens arteries and disrupts proper blood flow.
– History of blood clots leading to blood flow issues, hypo perfusion of tissue, necrosis, and open sore
– High blood pressure. Hypertension damages the arteries and disrupts blood flow.
– High blood cholesterol: it increases narrowing and oxidative stress in the arteries, which disrupts blood flow.
– Obesity: raises the risk for diabetes, atherosclerosis, and increased pressure in leg veins.
– Pregnancy. During pregnancy, hormonal changes and increased blood volume may cause leg vein problems.
2.2.4 Adequate surgical diagnosis of skin ulcers
Skin ulcers are usually clinically diagnosed, however there is a series of test which can be performed to assist in the diagnostic process. These include:
– Medical history: The information provided can help to better understand the symptoms
– Physical exam: This reveals the size and depth of the patient’s sore/ulcer, and explore if any blood, fluid, or pus discharge.
– Blood test: in case of infected ulcer, a blood panel (complete Blood Count (CBC), haemoglobin (Hb), Haematocrit (Ht), Red blood cells can assist in determining the underlying cause of infection.
– Tissue or fluid culture. This test can also help in determining the kind of the bacteria causing the infection for the prescription of the right antibiotics.
– Imaging tests. An X-ray, CT scan, or MRI helps in visualizing the tissue and bone under the sore/ulcer, to take appropriate measures.
Self-assessment activity 2.2
1. How diabetic patient are more likely to develop pressure injury?
2. List specific microbes which are more likely to cause the infection of pressure injuries
3. What are the diagnostic measures of skin ulcers?
4. Briefly explain how obesity increase the risk of developing pressure injuries.
2.3 Management of skin ulcers
Learning Activity 2.3
Following the interpretation of Mrs. ME’s laboratory exams results, the physician decided to prescribe injectable antibiotics, oral analgesic and painkiller, as well as the Ringers lactate. He also prescribes twice daily wound cleaning with normal saline 0.9% and wet dressing. 5 days later Mrs. ME. reported to fill well, and the laboratory results were promising and the discharge was decided.
Questions related to the case study.
1. What is the goal of skin ulcer treatment and management?
2. What is the surgical treatment plan adopted by the physician for Mrs. ME.?
3. In your respective groups, discuss different medical treatment prescribed to Mrs. ME and give an example of appropriate drug on each group of medication (antibiotics, analgesic and painkiller).
4. Briefly describe specific supportive management needed for Mrs. ME.
5. What do you plan to include in the patient and care giver teaching plan prior discharge?
2.3.1 Treatment plan of ulcers
The goal of skin ulcer treatment is to heal the wound, reduce pain, and treat any infection. The treatment may include:
a) Wound/ sore/ulcer cleaning and Dressing: to protect the wound and keep it clean. This promotes healing and prevents infection. The type of dressing depends on type and cause of ulcer and the findings from examination findings. Examples include moist dressings, hydrogels, hydrocolloids, collagen wound dressings, dressing with honey, and antimicrobial dressings.
NB: Normal saline 0.9% is mostly used to clean skin ulcers. Always check on the prescribed cleansing solution, recommended dressing type and the frequency of dressing changes
b) Antibiotics: antibiotic ointment is prescribed for infected skin ulcers. Once the infection has reached deeper tissue or bone, oral antibiotics will be recommended. In some patients, skin ulcer may not be infected but the antibiotics are prescribed to reduce the risk of infection.
c) Pain medication: for painful skin ulcer, analgesics may be prescribed to control patient’s pain .This may include simple analgesic like Paracetamol, ibuprofen, diclofenac, or even strong analgesic like morphine.
NB: The choice of the analgesic, route and dosage depend on individual case basing on the severity of the skin ulcer, complication and other comorbidities.
d) Surgery: Surgery is the last treatment option and it is indicated in large sore/ ulcer which might need for example, a skin graft. This will close the wound and help proper healing. Surgery may also be done to remove pressure by shaving away bone.
NB: For the management of skin ulcers/injuries, caused by pressure (called pressure injuries/ulcers) the treatment includes pressure reduction, friction avoidance and shearing forces, local care and sometimes skin graft as earlier discussed
e) Specific Supportive management
• Pressure relief over the affected or vulnerable area –turning the patient every 2 hours
• Rigorous skin care
– Keeping the skin clean and well hydrated to prevent skin erosions and lacerations
– Catheterization for patient with incontinence
– Advice caregivers to assess other areas at risk to identify early signs of pressure ulcer
• Nutrition
– Protein supplements
– Adequate nutrition and hydration in consultation with nutritionist
• Optimize management of comorbidities that may affect healing e.g. uncontrolled DM
• Ensure proper follow-up:
– The wound should be cleaned and freshly dressed regularly
– Repeated debridement might be necessary
• To use pressure injury risk assessment tool to identify individuals at risk of developing pressure injuries. They are five tools like Braden scale, Norton scale, Gosnell scale, the Knoll scale and the Waterlow scale. The most widely used is the Braden Scale for predicting injury developed by Barbara Braden and Nancy Bergstrom in 1988.This tool allows nurses and other healthcare providers to evaluate the patient’s risk for developing pressure injuries by examining six criteria:
– Sensory Perception: ability to respond meaningfully to pressure related discomfort (1–4)
– Moisture: degree to which skin is exposed to moisture (1–4)
– Activity: degree of physical activity (1–4)
– Mobility: ability to change and control body position (1–4)
– Nutrition: usual food intake pattern (1–4)
– Friction and Shear: amount of assistance needed to move, degree of sliding on beds or chairs (1–3)
The highest score is 23 while the lowest total score is 6 (NPUAP, 2014)
• A patient with A score of 15 to 18 has mild risk of developing pressure injury
• The one with a score of 13 to 14 has a moderate risk,
• A score of 10 to 12 indicate that the patient is at a high risk of developing pressure injury
• A score of 9 or less is an indication that the patient is at a very high risk
f) Patient’s Teaching for Simple Skin Ulcer Management Within Household:advise the patient to:
• Elevate the affected leg to improve blood flow. the leg is kept above the heart level, and cushions or pillows can be used for this purpose
• Use compressing socks to reduce leg swelling by improving blood flow back up to the heart.
• Apply high quality honey to a dressing, then apply the dressing on the skin. Honey has anti-inflammatory and antimicrobial benefits. (NB: Open sore should be managed in appropriate health setting with qualified health personnel and appropriate sterile materials)
2.3.2 Complications from skin ulcers
If left untreated, a skin ulcer may become infected, and the healing process will be prolonged. The infection can also spread to deeper tissue, bones, joints, and blood.
Self-assessment activity 2.3
1. In regards to predicting the risk of developing pressure injury among hospitalized patients,
a) Enumerate the existing tools serving for that specific purpose
b) Among them, which tool is mostly and widely used?
c) For the widely used, enumerate criteria based on to evaluate/score the patient’s risk of developing pressure injury/ulcer
2. What is the most used cleansing solution to clean pressure injuries
3. What is the most important preventive measure of skin ulcers?
4. What are the complication of untreated skin ulcers?
2.4. Description of Stomies
Learning Activity 2.4
Six weeks following Mrs. ME discharge, she has been readmitted, complaining of severe crampy abdominal pain, diarrhoea, mixed with blood, fatigue and weight loss. Following the complementary exams, the ulcerative colitis was confirmed and ileostomy was performed.
Questions related to the case study:
1. What do you understand by ileostomy?
2. What are characteristics of a normal stomy/ostomy?
3. List the types of stomies you know
4. What is the difference between ileostomy and colostomy?
2.4.1 Definition of stomy
The term comes from Greek. The suffix stoma means “mouth”, “opening”. According to Taber’s Medical Dictionary, stomy is defined as artificially and surgically produced opening into a specified part of the body or between body parts.
The term stomy and ostomy are used interchangeably, and by definition an ostomy is a surgical procedure that allows intestinal contents to pass from the bowel through an opening in the skin on the abdomen. The opening is called a stoma.
The stoma is created when the intestine is brought through the abdominal wall and sutured to the skin. The intestinal contents then empty through the hole on the surface of the abdomen rather than being eliminated through the anus. An ostomy is used when the normal elimination route is no longer possible. It should be clean, slightly pink, without ulcerations.
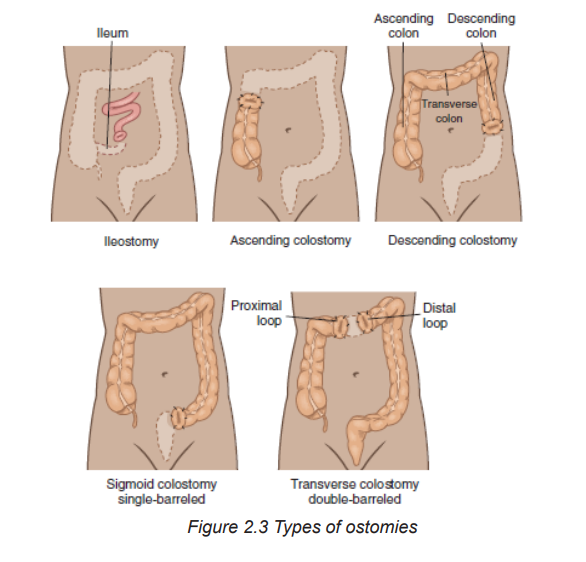
2.4.2 Types stomies
The stomy or ostomy is described and named according to the part of the body where it is produced and according to the type. A normal ostomy/stomy is pinkish-red and moist. It slightly sticks out from the skin, and it is normal to see a little mucus. Spots of bloodish mucus on stoma/ostoma is also normal. Below are examples of stomies:
• Tracheostomy: A tracheostomy is a surgically created stoma in the trachea to establish an airway. It is used to:
– Clear upper airway (bypass obstruction),
– Facilitate removal of secretions,
– Allow long-term mechanical ventilation.
• Esophagostomy: an ostomy produced at the level of esophagus
• Gastrostomy: an ostomy produced at the level of gastric
• Jejuniostomy: an ostomy produced at the level of jejunum
• Ileostomy: An ostomy made at the level of ileum. Output from an ileostomy has not entered the colon and thus is liquid. The ileostomy drains continuously, and the patient must constantly wear a bag to collect the drainage. In contrast, output from a sigmoid colostomy resembles normal formed stool, and some patients are able to regulate emptying time so they do not need to wear a collection bag (see table 1).
• Caecostomy: an ostomy produced at the level of caecum
• Colostomy: An ostomy in the colon. It is also named and characterized by its anatomic site such as ascending, transverse, descending and sigmoid colostomy. The more distal the ostomy, the more the intestinal contents resemble feces that are eliminated from an intact colon and rectum.
• Urostomy (urinary diversion): is a surgically created opening in the abdominal wall through which urine passes. An urostomy indicated when the bladder is either not functioning or has to be removed. Reasons for surgery includes: bladder cancer, spinal cord injuries, and malfunction (e.g. chronic infection of the bladder and birth defects such as spina bifida).
NB: Ostomies may be temporary or permanent. For example, the person with a draining fistula may need a temporary ostomy to prevent stool from reaching the diseased area. Patients who have trauma to the intestines (e.g., gunshot wound, stabbing) may need a temporary ostomy. Cancer involving the rectum requires a permanent ostomy because all bowel distal to the ostomy is removed. The major types of ostomies are end stoma, double-barreled, and loop ostomy
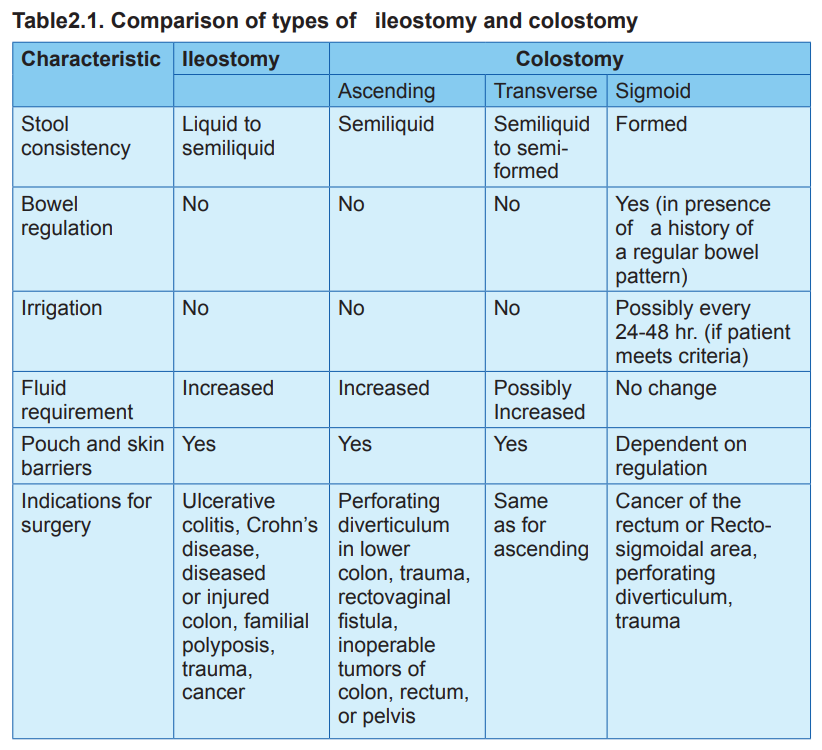
The table below summarizes the comparison of types of ileostomy and colostomy
Self-assessment activity 2.4
From your readings, please use the provided words to fill out the table below:
“injured colon, surgically produced opening into a specified part of the body, Esophagostomy, moist, familial polyposis, Presence of little mucus, Ileostomy, pinkish-red, Urostomy, slightly stick out from the skin, Tracheostomy, Spots of bloodish mucus, Ulcerative colitis, Crohn’s disease, trauma, cancer, Perforating diverticulum in lower colon”
2.5 Management of stomies
Learning Activity 2.5
It is on day 5 of Mrs. ME hospitalization post readmission. She is now feeling well, vital signs are within normal range and she regained appetite. She is only complains of her peristoma mucosal pain and irritation
Questions related to the case study:
1. What do you think has caused the reported irritation?
2. How would you best manage/treat this problem?
3. What are the possible complication to be prevented?
2.5.1 Treatment plan of stomies
The management of peristomal skin problems depends on the contributing factors. Generally, the management of stomies consists of regular cleaning, changing the puching bag, and or dressing where necessary Normal peristomal skin should be clean, dry, and intact and look like the skin on the rest of the abdomen or the skin where it is located. In case of deep infection, systemic antibiotics will be prescribed
2.5.2 Stoma Complications
Two categories exist: Early and late complication
– Early stomal complications occur within 30 days of surgery, and include: mucocutaneous separation, stoma necrosis, and stoma retraction.
– Late complications include stomal stenosis, stomal prolapsed, stomal trauma, and parastomal hernia. The Goals to prevent or decrease the incidence of stoma complications include weight reduction, promoting a healthy lifestyle, and proper ostomy management pre- and postoperatively.
Peristomal Complications
Peristomal skin issues are common and mostly occurs in eldest due to skin aging process. Immediate peristomal complication are caused by
a) Chemical (moisture-related injury from exposure to stoma effluent or stool leakage): Irritation of peristomal mucosal by digestive enzymes in the small intestine. if leaved untreated peristomal skin can become so damaged that the skin barrier will not adhere
b) Mechanical: results from skin stripping, abrasions or pressure injury due to the removal of skin barrier, tape or ostomy accessories.
c) Bacterial: Moist skin is more prone to overgrowth of fungi and bacteria.
Note: Beside, stoma and peristomal complications, patients with ostomies (Particular patients with ileostomy) are at risk of dehydration and electrolyte deficiency. This is due to the loss of the absorptive function of the large colon. Patients should be taught signs and symptoms of dehydration, how to prevent it, and when to report to the health facility.
Note: Patients with ileostomy should:
– Drink up to 2 l of fluid a day, and more if they are in hot weather or participating in outdoor activities
– Increase food intake high in sodium like canned vegetables, broth, and tomatoes, and in potassium, such as bananas, potatoes, and spinach.
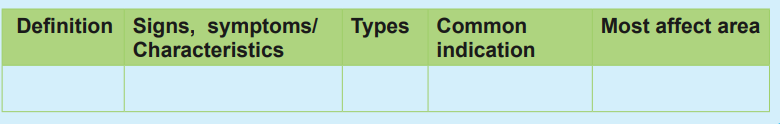
The table below summarize common peristomal complications and their management
Table 2.2: Summary of peristomal complications
2.5.3 Associate nurse decision making
An associate nurse who receives a patient with signs and symptoms of skin ulcer and stomy must be able to diagnose these conditions, manage simple skin ulcers and stomy and refer complicated cases to the next level for adequate management. In the hospital, the associate nurse works under supervision of registered nurses and they will discuss the appropriate nursing care plan. The associate nurse also helps the patient to comply with self-care:
Ostomy Self-Care
1. Explain what an ostomy is and how it functions.
2. Describe the underlying condition that resulted in the need for an ostomy.
3. Demonstrate and allow the patient and caregiver to practice the following activities:
– Remove the old skin barrier, cleanse the skin, and correctly apply new skin barriers.
– Apply, empty, clean, and remove the pouch.
– Empty the pouch before it is one-third full to prevent leakage.
– Irrigate the colostomy to regulate bowel elimination (optional).
4. Explain how to contact the wound, ostomy, and continence (WOC) nurse with questions.
5. Describe how to obtain additional ostomy supplies.
6. Explain dietary and fluid management.
– Identify a well-balanced diet and dietary supplements to prevent nutritional deficiencies.
– Identify foods to avoid to reduce diarrhea, gas, or obstruction (with ileostomy).
– Promote fluid intake of least 3000 mL/day to prevent dehydration (unless contraindicated).
– Increase fluid intake during hot weather, excessive perspiration, and diarrhea to replace losses and prevent dehydration.
– Describe symptoms of fluid and electrolyte imbalance.
– Explain how to contact the registered dietitian with questions.
– Explain how to recognize problems (fluid and electrolyte deficits, fever, diarrhea, skin irritation, stomal problems) and how to contact the appropriate health care provider.
7. Describe community resources to assist with emotional and psychologic adjustment to the ostomy.
8. Explain the importance of follow-up care.
9. Describe the ostomy’s potential effects on sexual activity social life, work, and recreation and strategies to manage these changes.
2.6 End unit assessment
End of unit assessment
1. Which patient is at the greatest risk for developing pressure injury?
a) A 42-year-old obese woman with type 2 diabetes
b) A 78-year-old man who is confused and malnourished
c) A 30-year-old man who is comatose following a head injury
d) A 65-year-old woman who has urge and stress incontinence
2. What is the most important nursing intervention for the prevention and treatment of pressure injury?
a) Using pressure-reduction devices
b) Massaging pressure areas with lotion
c) Repositioning the patient, a minimum of every 2 hours
d) Using lift sheets and trapeze bars to facilitate patient movement
3. The patient is being transferred from another health facility with the description of a sore on her sacrum that is deep enough to see the muscle. What stage of pressure injury does the nurse expect to see on admission?
a) Stage I
b) Stage II
c) Stage III
d) Stage IV
4. A Nurse coming on day duty is reading the patient’s file(records) and he found out that the patient has a stage III pressure injury on his right left hip. What should the nurse expect to find on assessment of the patient’s left hip?
a) Exposed bone, tendon, or muscle
b) An abrasion, blister, or shallow crater
c) Deep crater through subcutaneous tissue to fascia
d) Persistent redness (or bluish color in darker skin tones)
5. Which nursing interventions for a patient with a Stage IV sacral pressure injury are most appropriate to assign or delegate to a licensed practical nurse (select all that apply)?
a) Assess and document wound appearance.
b) Teach the patient pressure injury risk factors.
c) Choose the type of dressing to apply to the ulcer.
d) Measure the size (width, length, depth) of the ulcer.
e) Assist the patient to change positions at frequent intervals.
6. Of the following pressure injury predicting tool, what is the most widely used?
a) Braden scale
b) Gosnell scale
c) Waterlow scale
d) Norton scale
7. What do you understand by tracheostomy?
8. Identify the common sites of skin ulcers and ostomies
9. What are the risk factors that can be associated with pressure injury development?
10. Explain the pathophysiological mechanisms behind development of Pressure injury
UNIT 3: CONTUSIONS/SPRAINS
Key Unit competence
Take appropriate decision on contusions and sprains
Introductory activity 3.0
The below images (A,B) illustrate different normal and abnormal structures of ankles. Observe them and respond to the questions attached.
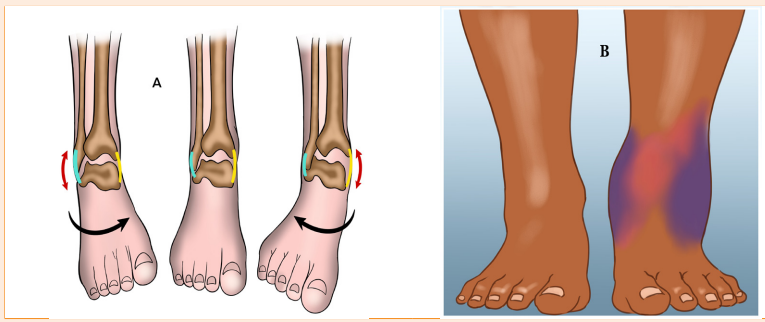
1. Describe the abnormal structures of ankle observed
2. What could be the causes of such abnormalities?
3. What are the manifestations of such abnormalities in the human body?
4. How can health personnel identify or notice these abnormalities?
5. How can these abnormalities be corrected
3.1. Contusions/ Sprains
Learning Activity 3.1
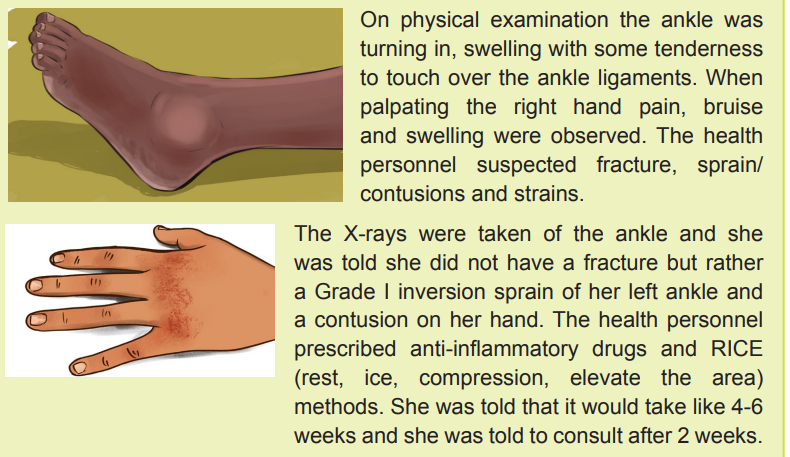
A 35-year-old woman attends the clinic after she was mopping the house causing her to slip on some water. She fell, rolling her right ankle to the side. She also used her right hand to support her during a fall and she is complaining pain at the same hand. She was able to get up and weight bear through her injured ankle, limping to the nearest hospital.
On inspection, her left ankle was pretty sore with some noticeable swelling of her ankle. She was not able to walk properly. On her right hand, a bruise and swelling were also observed.
Questions related to the case study
1. What is a sprained ankle/what is contusion?
2. What was done to reduce the swelling?
3. How long will it take to recover?
4. When can she resume her sport?
3.1.1 Definition of terms
A sprain is a stretching or tearing of ligaments, the tough bands of fibrous tissue that connect two bones together in the joints. The most common location for a sprain is in the ankle.
A contusion is an injury that causes bleeding and tissue damage underneath the skin, usually without breaking the skin. Any injury that puts pressure on an area repetitively can cause a contusion.
3.1.2 Causes and risk factors of contusions/sprains
A sprain occurs when there is an overextension or tear of a ligament while severely stressing a joint. Sprains often occur in the following circumstances:
– Ankle: Walking or exercising on an uneven surface, landing awkwardly from a jump Knee: Pivoting during an athletic activity
– Wrist: Landing on an outstretched hand during a fall
– Thumb: Skiing injury or overextension when playing racquet sports, such as tennis
Children have areas of softer tissue, called growth plates, near the ends of their bones. The ligaments around a joint are often stronger than these growth plates, so children are more likely to experience a fracture than a sprain.
Factors contributing to sprains include:
– Environmental conditions. Slippery or uneven surfaces can make people more prone to injury.
– Fatigue. Tired muscles are less likely to provide good support for the joints. When an individual is tired, she/he is also more likely to succumb to forces that could stress a joint.
– Poor equipment. Ill-fitting or poorly maintained footwear or other sporting equipment can contribute to the risk of a sprain.
Contusions also called bruise are black-and-blue spots. This happens when small blood vessels get torn and leak blood under the skin. But bones, muscles, and organs can also get bruised. This may damage deep tissues but not cause a bruise that can be seen.
a) Subcutaneous contusion
A subcutaneous contusion (fig. 3.1 A) is the bruise that most people are familiar with. A subcutaneous contusion is a bruise just beneath the skin. Almost everyone experiences a subcutaneous contusion at some point. Just as a cut bleeds from tiny blood vessels, injuries to tiny blood vessels under the skin cause most subcutaneous contusions. Areas that a person may land on or use to support themselves during a fall, such as the hands and knees, are particularly vulnerable.
Very rarely, a large bruise causes massive bleeding, from a vein or artery that is difficult to stop. This can be life-threatening without treatment.
b) Muscle contusion
The muscles are full of blood vessels that supply them with blood and oxygen. A bruise to a muscle is deeper than a subcutaneous contusion, and it can be very painful. A person with a muscle contusion may think that they have a sprain, strain, or broken bone.
c) Bone contusion
A bone contusion can feel similar to a break or fracture, and it may make it difficult to move the area of the injury.
d) Eye contusion
An eye contusion is a bruise on or around the eye. Contusions on the eyelid can be painful and may look swollen. However, they are rarely serious. A person may also bruise the cornea, which is the tissue inside the eye. This can be more serious, especially without treatment or if there are other eye injuries present.
e) Cartilage contusion
Cartilage is flexible but thick tissue that is harder than muscle but softer than bone. The outside of the ears and the tip of the nose both contain cartilage.
f) Organ contusion
Internal organs such as the kidneys, lungs and heart can develop bruises after a forceful blow or fall. Organ contusions damage the blood vessels and other soft tissue in organs. These injuries are dangerous, and they can be life-threatening. This is because they may interfere with the functioning of the organ. People with organ contusions may require hospitalization. For example, a person with a pulmonary contusion, or a bruise on the lungs, may need to use an artificial ventilator.
3.1.3 Clinical manifestations of contusions/sprains
Signs and symptoms of sprains will vary, depending on the severity of the injury, and may include; pain, swelling, bruising, limited ability to move the affected joint and hearing or feeling a “pop” in the joint at the time of injury. Depending on the junction or ligament affected, a turn in or out of the joint maybe observed.
As it was mentioned early, the most common location for a sprain is in the ankle, usually involving the foot and ankle turning inwards (inversion) and damaging at least one of the ligaments on the outside of the ankle. It is possible to twist the ankle outwards (eversion) but this is far less common (fig3.2).
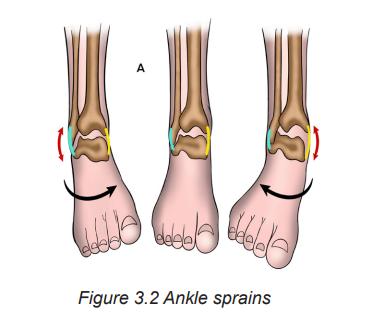
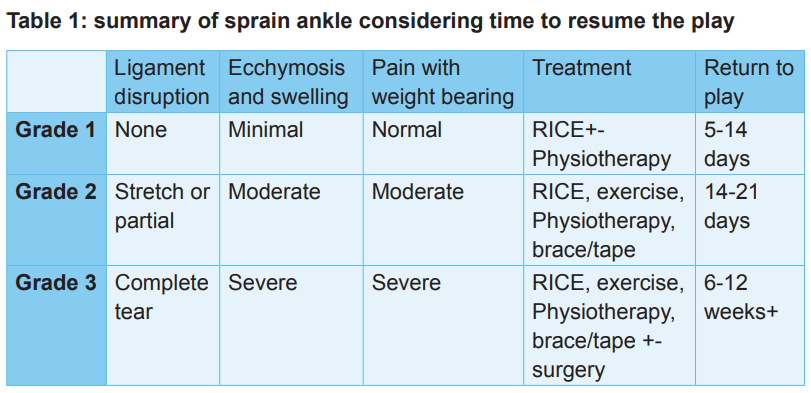
There are two different basic classifications of ankle sprains: Anatomic (the level severity of damage to tissues in the ankle) and functional (the level an injury affects a patient’s ability to walk or put weight on the ankle).
Anatomic Classifications
Grade I ankle sprain – lateral ligaments are strained (overstretched)
– Grade II ankle sprain – partial tearing of one or several of these ligaments
– Grade III ankle sprain – complete rupture (tear) one or more of the lateral ligaments
Functional Classifications
– Grade I injury – the patient is able to fully weight bear and walk
– Grade II injury – the patient walks with a noticeable limp
– Grade III – the patient is unable to walk
For most contusions, the main symptom is pain. The pain can be either mild or severe. Larger, deeper contusions, such as those affecting the bone or muscles, are typically more painful. If there is pain following a fall or blow, there may be a contusion. Some common symptoms of a contusion include:
– Red, blue, or black swelling near the injured area
– Throbbing or aching
– Difficulty moving the area
Contusions to organs can affect their ability to function. Following a hard blow to the stomach, back, or chest, a person should seek immediate medical treatment for pain, swelling, weakness, or any signs of illness. These could be signs of an organ contusion.
Difficulty breathing or changes in heart rate could be signs of a lung or heart contusion. These are medical emergencies that require immediate treatment.
3.1.4 Diagnostic measures of contusion/sprains
A physical exam is performed; touch the skin around the injury to check for points of tenderness. Ask the patient to move his/her foot to check the range of motion and to understand what positions cause discomfort or pain.
If the injury is severe, one or more of the following imaging scans are done to rule out a broken bone or to evaluate in more detail the extent of ligament damage:
– X-ray; during an X-ray, this test is good for ruling out bone fractures.
– Magnetic resonance imaging (MRI) good for soft internal structures of the ankle, including ligaments.
– CT scan; can reveal more detail about the bones of the joint.
– Ultrasound; may help to judge the condition of a ligament or tendon when the foot is in different positions.
3.1.5 Therapeutic Measures of contusions/sprains
Most contusions of bones, muscles, skin, and cartilage will not need medical treatment. Instead, using the RICE method at home can help with pain and swelling, as well as speed up recovery. Organ contusions may require more intensive treatment, surgery to repair an injury or stop the bleeding.
Treatment for a sprains depends on the severity of the injury. The treatment goals are to reduce pain and swelling, promote healing of the ligament, and restore function of the joint.
– Self-care: For self-care of an ankle sprain, R.I.C.E. approach is used for the first two or three days:
– Rest: Avoid activities that cause pain, swelling or discomfort.
– Ice: Use an ice pack or ice slush bath immediately for 15 to 20 minutes and repeat every two to three hours while. If a patient has vascular disease, diabetes or decreased sensation, she/he has to talk with the doctor before applying ice.
– Compression: To help stop swelling, compress the ankle with an elastic bandage until the swelling stops. Don’t hinder circulation by wrapping too tightly. Begin wrapping at the end farthest from your heart.
– Elevation: To reduce swelling, it is recommended to elevate the joint above the level of the heart, especially at night. Gravity helps reduce swelling by draining excess fluid.
– Medications: In most cases, over-the-counter pain relievers
— such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others) or acetaminophen (Tylenol, others)
— are enough to manage the pain of a sprained joint.
– Devices: Because walking or maintaining a normal position with a sprained joint might be painful, using crutches until the pain subsides is recommended. Depending on the severity of the sprain, an elastic bandage, sports tape or joint support brace to stabilize the joint are recommender. In the case of a severe sprain, a cast or walking boot may be necessary to immobilize the ankle or any other joint while it heals.
– Physiotherapy: Once the swelling and pain is lessened enough to resume movement, a series of exercises to restore the range of motion, strength, flexibility and stability may be recommended.
– Surgery: In rare cases, surgery is performed when the injury doesn’t heal or the joint remains unstable after a long period of physical therapy and rehabilitative exercise. Surgery may be performed to:
– Repair a ligament that won’t heal
– Reconstruct a ligament with tissue from a nearby ligament or tendon
3.1.6 Complications of contusions/sprains
Skin contusions most of the time do not have complications but organ contusions may have complications. For example, a person with a pulmonary contusion, or a bruise on the lungs, may need to use an artificial ventilator.
Sprains complications are:
– Chronic pain
– Chronic joint instability
– Arthritis in the joint
3.1.7 Associate nurse decision making
The associate nurse will help the patient to apply RICE methods to treat contusions/ sprains and teach the patients how to prevent the contusions/sprains.
Self-assessment activity 3.1
1. What is the difference between a sprain, strain and contusion?
2. Identify the common factors associated with sprain
3. What are the signs and symptoms of a contusions/sprain?
4. Explain the types of contusions
3.2 End unit assessment
End of unit assessment
1. If you have a sprain, it means you’ve injured a ligament.
a) True
b) False
c) The most common site of a sprain is the wrist
d) True
e) False
2. A typical sprain occurs when you misstep and land on the side of your foot.
a) True
b) False
c) Explain the pathophysiology of contusions?
d) What is the difference between inversion and eversion sprain of ankle?
e) Identify the diagnostic measures of sprains
3. The ICE method is commonly used for self-care of sprains and contusions. Explain this method.
4. Based on function classification of sprains of ankle, describes different stages of sprains.
UNIT 4: BURN CONDITIONS
Key Unit competence
Take appropriate decision on Burn conditions
Introductory activity 4.0
Observe carefully the following images and answer to the questions below.
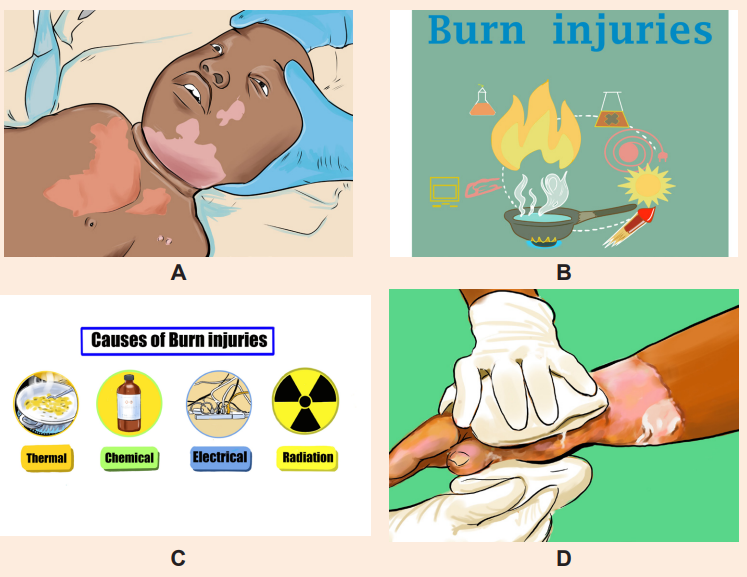
1. What do you think happened to this person in image A?
2. How do you call this condition in image A?
3. According the images above B and C, what do you think were the possible causes and risks factors that may contribute to this condition?
4. By analysing the image D, what do you think they are doing to this patient?
5. What do you think may be the complications for patient in image A?
4.1 Description of burn condition
Learning Activity 4.1
Judy A. is 32-year-old female, and she is an old case of epileptic condition on treatment at the nearest health center. He was cooking food for family in her kitchen when he turns on the bottle of cooking gas, she felt down. The entire house was engulfed in flames when the fire department arrived on scene. The neighbour called 911 when he smelt smoke. Judy was found conscious by the firefighters and was pulled out. She was burned on the anterior part of the chest with blisters formation which burst and involvement of the right upper limb. She was immediately stabilized on scene and was rushed to the nearest health center via ambulance. While enroute, the nurse started an 18-gauge IV with Ringer lactate and a dose of 5mg of Pethidine was given as pain killer. Upon arrival at the health center, Judy was found to have stage 2 burn wounds on his anterior part of the chest and entire right arm with stage 2 burns. Emergency treatment was provided: Local wound care with normal saline and aseptic dressing with Vaseline gauze was applied. Judy was at risk for smoke inhalation and a compromised airway as she presented a difficulty in breathing with tachypnea, so oxygen supplement with facial mask and fluid resuscitation was initiated before being transferred at the District hospital.
Questions related to the case study.
1. From the case study above, identify the risk factors that can be associated with burn injury
2. Explain the pathophysiological mechanisms behind blisters formation
3. List the signs and symptoms of burn as described in the case study.
4. From the signs described in the case study, why Judy is classified as stage 2 burn?
5. From the case scenario, what are the treatment offered to Judy before being transferred to District Hospital?
4.1. 1 Definition of Burn
Burn is a generic term used to describe cutaneous injury resulting from thermal, chemical, or electrical environmental causes. Pulmonary injury, both primary and secondary, is common and often necessitates ventilator support.
Burn is a tissue injury that results from thermal application (hot/ cold) and from application of physical or chemical energy urns disrupt the skin, which leads to increased fluid loss; infection; hypothermia; scarring; compromised immunity; and changes in body function, appearance, and body image.
It can lead to an increased morbidity and mortality rate in young children and the elderly when compared to other age groups with similar injuries.
4.1.2 Causes and Pathophysiology of Burn
Burns are caused by a transfer of energy from a heat source to the body. It may be caused several factors like dry heat, moist heat, cold injury, chemical burns, electrical burns, ionizing radiation and friction. The resulting effects are influenced by the temperature of the burning agent, duration of contact time, and type of injured tissue
It is a crucial to understand the pathophysiology of a burn injury for effective management. Causes lead to different injury patterns, which require different management. Pathophysiologically, burn injuries result in both local and systemic responses. In addition to cutaneous injury, burns are often associated with smoke inhalation injury or other traumatic injuries that aggravate the local and systemic problems of burns.
Local response: The three zones of a burn were described by Jackson in 1947.
– Zone of coagulation: This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins.
– Zone of stasis: The surrounding zone of stasis is characterized by decreased tissue perfusion. The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible. Additional insults such as prolonged hypotension, infection, or edema can convert this zone into an area of complete tissue loss.
– Zone of hyperaemia: In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypoperfusion.
These three zones of a burn are three dimensional, and loss of tissue in the zone of stasis will lead to the wound deepening as well as widening.
Systemic response: The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 30% of total body surface area. Cardiovascular changes like capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs.
4.1.3 Types of Burn Burn type is determined according to the causative agent:
– Thermal Burns: caused by flame, flash, scald, or contact with hot or high cold objets
– Chemical Burns : result of contact with acids, alkalis, and organic compound
– Electrical: result from the conversion of electrical energy into heat. Extent of injury depends on the type of current, the pathway of flow, local tissue resistance, and duration of contact
– Radiation: result from radiant energy being transferred to the body resulting in production of cellular toxins
– Smoke and Inhalation Injury: from breathing hot air or noxious chemicals
4.1.4: Signs and symptoms of burns
Symptoms range from a feeling of minor discomfort to a life-threatening emergency, depending on the size and depth (degree) of the burn. Clinical symptoms of burn may differ also depending on the causative agent.
The patient with severe burns is likely to be in shock from hypovolemia. Frequently the areas of full-thickness and deep partial-thickness burns are initially anesthetic because the nerve endings have been destroyed.
Superficial to moderate partial thickness burns are very painful. Blisters, filled with fluid and protein, are common in partial-thickness burns. The patient with a larger burn area may develop a paralytic ileus, with absent or decreased bowel sounds. Shivering may occur as a result of chilling that is caused by heat loss, anxiety, or pain. The patient may be alert and able to answer questions shortly after admission or until he or she is intubated (if there is an inhalation injury).
Patients are often frightened and benefit from a calm reassurances and simple explanations of what to expect as you provide care. Unconsciousness or altered mental status in a burn patient is usually not a result of the burn but of the hypoxia associated with smoke inhalation. Other possibilities include head trauma, substance abuse, or excessive amounts of sedation or pain medication.
4.1.5: Diagnostic modalities
Diagnosing burn injury is basically determined by the clinical symptoms a patient is presenting at time of admission. Basic laboratory studies should be obtained in patients with severe burns or concomitant trauma, including a complete blood count, blood type and cross match, chemistries electrolytes measurement, coagulation profiles, arterial blood gas measurement, and a pregnancy test, when appropriate.
Laboratory tests or changes in laboratory values such as erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level are of low yield in detecting or predicting burn infections because of the inflammatory response associated with the burn itself .Renal function tests like creatinine and albumin clearance should be carried out because burned patients are at high risks of renal complication resulting from hypovolemic shock.
4.2 Classification of burns injury
The treatment of burns is related to the severity of the injury .Severity of burn is determined by:
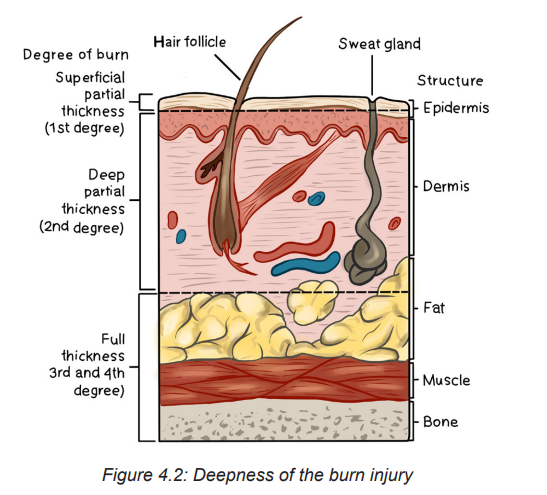
1. Depth of burn: Burn injury involves the destruction of the integumentary system (epidermis, dermis, and subcutaneous tissue). The depth of a burn injury depends on the type of injury, causative agent, temperature of the burn agent, duration of contact with the agent, and the skin thickness. Burns are classified according to the depth of tissue destruction.
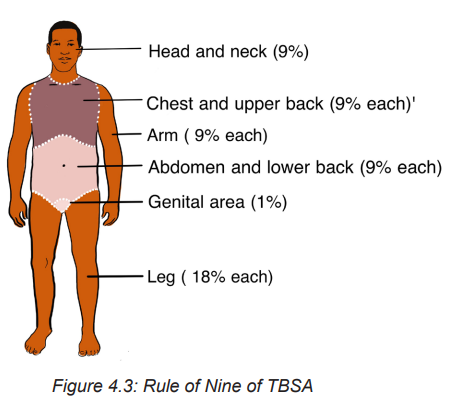
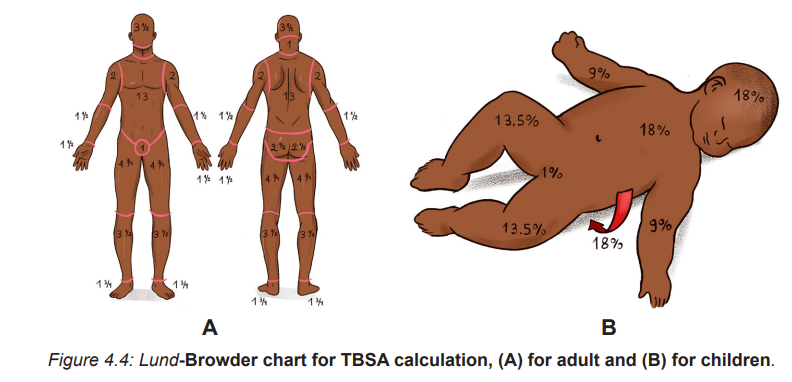
2. The extent of burn calculated in percent of total body surface area (TBSA): Two commonly used guides for determining the TBSA affected
Lund-Browder: more accurate because it considers the patient’s age in proportion to relative body-area size
The Rule of Nines: is often used for initial assessment of a burn patient because it is easy to remember.
Note: Depending to extent and deepness of injured tissue, burn is classified in 3 different stages
First-degree Burns or Superficial burns: involve only the first layer of the skin (epidermis) and characterized by redness, manifests with erythema and tenderness. Healing occurs naturally within a week.
– Second degree burn or partial thickness: This involves part of dermis. It manifests with blisters, edema, moist surface and pain at the affected site.
– Third-degree Burns or Full thickness: Third-degree burns involve all layers of the skin and may be some damage to the nerves, fat tissue, muscles and bones .The skin may vary from white and lifeless to black and charred. White or greyish and the surface is pain free
3. Location of burn: The severity of the burn injury is also determined by the location of the burn wound. Burns to the face and neck and circumferential burns to the chest or back may interfere with breathing as a result of mechanical obstruction from edema or leathery, devitalized burn tissue (eschar). These burns may also indicate possible inhalation injury and respiratory mucosal damage.
Burns to the hands, feet, joints, and eyes are of concern because they make self-care difficult and may jeopardize future function. Burns to the hands and feet are challenging to manage because of superficial vascular and nerve supply systems that need to be protected while the burn wounds are healing. Burns to the ears and the nose are susceptible to infection because of poor blood supply to the cartilage. Burns to the buttocks or perineum are highly susceptible to infection from urine or feces contamination
Circumferential burns to the extremities can cause circulation problems distal to the burn, with possible nerve damage to the affected extremity. Patients may also develop compartment syndrome from direct heat damage to the muscles, swelling, and/or pre-burn vascular problems
4. Patient risk factors (e.g., age, past medical history): patient with pre existing cardiovascular, respiratory, or renal disease has a poorer prognosis for recovery because of the tremendous demands placed on the body by a burn injury. The patient with diabetes mellitus or peripheral vascular disease is at high risk for poor wound healing, especially with foot and leg burns. General physical debilitation from any chronic disease, including alcoholism, drug abuse, or malnutrition, makes it challenging for the patient to fully recover from a burn injury. In addition, the burn patient who has also sustained fractures, head injuries, or other trauma has a more difficult time recovering.
4. 3 Calculation of the Total Body Surface Area (TBSA)
The TBSA is an other important factor to consider for effective management of burn injury. It is calculated by using two commonly used guides: (1) Lund-Browder: more accurate because it considers the patient’s age in proportion to relative body area size and (2) The Rule of Nines: often used for initial assessment of a burn patient because it is easy to remember.
4.3.1 The Rule of Nines or Wallace rule The size of a burn can be quickly estimated by using the “rule of nines.” This method divides the body’s surface area into percentages.
– The front and back of the head and neck equal 9% of the body’s surface area.
– The front and back of each arm and hand equal 9% of the body’s surface area.
– The chest equals 9% and the stomach equals 9% of the body’s surface area.
– The upper back equals 9% and the lower back equals 9% of the body’s surface area.
– The front and back of each leg and foot equal 18% of the body’s surface area.
– The genital area equals 1% of the body’s surface area.
4.3.2: Lund and Browder chart
The Lund and Browder chart is a tool useful in the management of burns for estimating the total body surface area affected. This chart takes into consideration of age of the person, with decreasing percentage Burned Surface Area (BSA) for the head and increasing percentage BSA for the legs as the child ages, making it more useful in paediatric burns.
Self-assessment activity 4.1
1. Basing on the stage of burn, describe the clinical symptoms of burn
2. What is the common and easiest clinical guides for calculating TBSA in burned patient?
3. Provide the difference among the 3 stages of burn injury.
4.4 Treatment and phases of burn management
Burn management can be organized chronologically into three phases: emergent (resuscitative), acute (wound healing), and rehabilitative (restorative). Overlap in care does exist. For example, the emergence phase begins at the time of the burn injury, and care often begins in the prehospital phase, depending on the skill level of providers at the scene. Planning for rehabilitation begins on the day of the burn injury or admission to the burn center. Formal rehabilitation begins as soon as functional assessments can be performed. Wound care is the primary focus of the acute phase, but wound care also takes place in both the emergent and rehabilitation phases.
The four major goals relating to burn management are (1) Prevention measures, (2) life-saving measures for the severely burned person (3) prevention of disability and disfigurement and (4) rehabilitation.
4.4.1 Prehospital care
At the scene of the injury, priority is given to removing the person from the source of the burn and stopping the burning process. Rescuers must also protect themselves from being injured. In the case of electrical and chemical injuries, initial management involves removal of the patient from contact with the electrical or chemical source.
Small thermal burns (10% or less of TBSA) should be covered with a clean, cool, tap water dampened towel for the patient’s comfort and protection until medical care is available. Cooling of the injured area (if small) within 1 minute helps minimize the depth of the injury. If the burn is large (greater than 10% TBSA) or an electrical or inhalation burn is suspected, first focus your attention on the ABCs:
– Airway: Check for patency, soot around nares and on the tongue, singed nasal hair, darkened oral or nasal membranes.
– Breathing: Check for adequacy of ventilation.
– Circulation: Check for presence and regularity of pulses, and elevate the burned limb(s) above the heart to decrease pain and swelling.
To prevent hypothermia, cool large burns for no more than 10 minutes. Do not immerse the burned body part in cool water because it may cause extensive heat loss. Never cover a burn with ice, since this can cause hypothermia and vasoconstriction of blood vessels, thus further reducing blood flow to the injury. Gently remove as much burned clothing as possible to prevent further tissue damage. Leave adherent clothing in place until the patient is transferred to a hospital. Wrap the patient in a dry, clean sheet or blanket to prevent further contamination of the wound and to provide warmth.
Chemical burns are best treated by quickly removing any chemical particles or powder from the skin. Remove all clothing containing the chemical because the burning process continues while the chemical is in contact with the skin. Flush the affected area with copious amounts of water to irrigate the skin anywhere from 20 minutes to 2 hours post exposure. Tap water is acceptable for flushing eyes exposed to chemicals. Tissue destruction may continue for up to 72 hours after contact with some chemicals
Observe patients with inhalation injuries closely for signs of respiratory distress .These patients need to be treated quickly and efficiently if they are to survive. If CO poisoning is suspected, treat the patient with 100% humidified O2. Patients who have both body burns and an inhalation injury must be transferred to the nearest burn center.
Always remember that the burn patient may also have sustained other injuries that could take priority over the burn itself. Individuals involved in the prehospital phase of burn care must adequately communicate the circumstances of the injury to hospital providers. This is especially important when the patient’s injury involves being trapped in a closed space, exposure to hazardous chemicals or electricity or a possible traumatic injury.
4.4.2 Emergent phase/ Resuscitative phase
The emergent or resuscitative phase is the time required to resolve the immediate, life-threatening problems resulting from the burn injury. This phase usually lasts up to 72 hours from the time the burn occurred. The primary concerns are the onset of hypovolemic hock and edema formation. The emergent phase ends when fluid mobilization and diuresis begin.
In the emergent phase, the patient’s survival depends on rapid and thorough assessment and appropriate interventions. Usually the physician and you make an initial assessment of the depth and extent of the burn and coordinate the actions of others on the health care team. In a community hospital, determine whether the patient requires inpatient or outpatient care. In the case of inpatient care, decide whether the patient remains in the hospital or should be transferred to the closest burn center. Nursing and collaborative management predominantly consists of airway management, fluid therapy, and wound care. Patients often improve and worsen, unpredictably, on an almost daily basis. Physical and occupational therapy are important in both the acute and rehabilitation phases, proper positioning and splinting begin on the day of admission. Emotional support and teaching of patients and caregivers begin on admission.
• Airway management
Respiratory support with early endotracheal intubation if necessary in which ventilator support will be used with the delivered oxygen concentration based on Arterial Blood Gas (ABG) values. Escharotomies of the chest wall may be needed to relieve respiratory distress secondary to circumferential, fullthickness burns of the neck and trunk .When intubation is not performed, treatment of inhalation injury includes administration of 100% humidified O2 as needed.
Place the patient in a high Fowler’s position, unless contra indicated (e. g: spinal injury), and encourage deep breathing and coughing every hour. Reposition the patient every 1 to 2 hours and provide suctioning and chest physiotherapy (as ordered). When intubation is not performed, 100% humidified O2 as needed. The CO poisoning is treated by administering 100% O2until carboxyhemoglobin levels return to normal.
• Fluid therapy
The ideal resuscitation fluid should be one that produces a predictable and sustained increase in intravascular volume, has a chemical composition as close as possible to that of extracellular fluid, is metabolized and completely excreted without accumulation in tissues, does not produce adverse metabolic or systemic effects, and is cost-effective in terms of improving patient outcomes. Currently, there is no such fluid available for clinical use.
Establishing intravenous (IV) access is critical for fluid resuscitation and drug administration. At least two large-bore IV access sites must be in place for patients with burns that are 15% TBSA or more. It is critical to establish IV access that can handle large volumes of fluid. For patients with burns greater than 30% TBSA, consider a central line for fluid and drug administration and blood sampling .An arterial line is often placed if frequent ABGs or invasive BP
– Assess the extent of the burn wound using a standardized Chart
– Then use a standardized formula to estimate the patient‘s fluid ressuscitation requirements.
– Fluid replacement is achieved with crystalloid solutions usually lactated Ringer’s, colloids like albumin, or a combination of the two.
– All formulas are estimates, and fluids must be titrated based on the patient’s response (e.g., hourly urine output, vital signs).
– The Parkland (Baxter) formula for fluid replacement is the most Common formula used
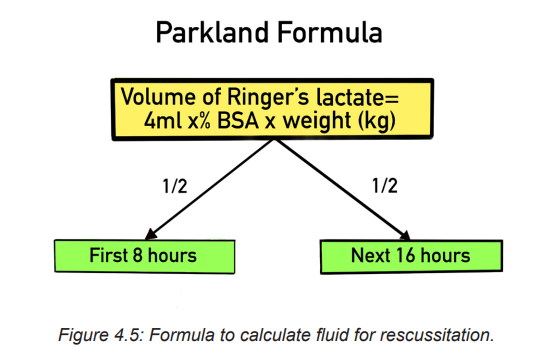
This formula was designed to help the healthcare provider determine the proper amount of fluids to administer to a patient following a burn. Parkland’s burn formula is most useful during the first twenty four hours of fluid resuscitation with second degree or greater burns. Ringers lactate is the fluid of choice and should be administered at 4 mL/kg of body weight per percentage of burn using total body surface area (TBSA) as a guide.
Administer ½ of fluid requirements in 1st 8 hours, then administer the 2nd half of fluid requirements over the next 16 hours.
For example :A person weighing 75 kg with burns to 20% of his or her body surface area would require 4 x 75 x 20 = 6,000 mL of fluid replacement within 24 hours. The first half of this amount is delivered within 8 hours from the burn incident, and the remaining fluid is delivered in the next 16 hours.
Children receive maintenance fluid in addition, at an hourly rate of:
– 4ml/kg for the first 10kg of body weight plus
– 2ml/kg for the second 10kg of body weight plus
– 1ml/kg for >20kg of body weight.
• Wound care
Once a patent airway, effective circulation, and adequate fluid replacement have been established, priority is given to care of the burn wound. Partial thickness burn wounds appear pink to cherry-red and are wet and shiny with serous exudate. In this principle, permanent skin coverage is the primary goal for burn wound care. Two approaches to burn wound treatment are (1) the open method and (2) the use of multiple dressing changes (closed method).
In the open method: the patient’s burn is covered with a topical antimicrobial and has no dressing over the wound.
In the multiple dressing change, or closed method, sterile gauze dressings are impregnated with or laid over a topical antimicrobial.
– These dressings are changed anywhere from every 12 to 24 hours to once every 14 days (depending on the product).
– Most burn centers support the concept of moist wound healing and use dressings to cover the burned areas, with the exception of facial burns.
– When the patient’s open burn wounds are exposed, always wear personal protective equipment (PPE) (e.g., disposable hats, masks, gowns, gloves).
– When removing contaminated dressings and washing the dirty wound, use nonsterile, disposable gloves.
– Use sterile gloves when applying ointments and sterile dressings
– In addition, prevent shivering by keeping the room warm (approximately 85° F [29.4° C]
– Perform thorough hand washing both before and after patient contact to prevent cross-contamination
– Permanent skin coverage is the primary goal for burn wound care: different forms of skin grafting will be used in case of needs.
• Drug therapy
– Provision of analgesics and sedatives: Promote the use of analgesics for the patient’s comfort. Early in the post burn period, IV pain medications should be given because (1) onset of action is fastest with this route; (2) oral medications have a slower onset of action and are not as effective when GI function is slowed or impaired because of shock or paralytic ileus; and (3) intramuscular (IM) injections will not be absorbed adequately in burned or oedematous areas, causing pooling of medications in the tissues. Analgesic requirements can vary widely from one patient to another, so consider a multimodal approach to pain management.
! Remember that the patient’s pain intensity may not directly correlate with the extent and depth of burn.
– Tetanus immunization: Tetanus toxoid is given routinely to all burn patients because of the likelihood of anaerobic burn wound contamination. If the patient has not received an active immunization within 10 years before the burn injury, tetanus immunoglobulin should be considered.
– Antimicrobial agents: After the wound is cleansed, topical antimicrobial agents may be applied and covered with a light dressing. Systemic antibiotics are not routinely used to control burn wound flora because the burn eschar has little or no blood supply and consequently little antibiotic is delivered to the wound. In addition, the routine use of systemic antibiotics increases the chance of developing multidrug resistant organisms.
– Some topical burn agents penetrate the eschar and inhibit bacterial invasion of the wound. Silver impregnated dressings (e.g. Acticoat, Silverlon, Aquacel AG) can be left in place from 3 to 14 days, depending on the patient’s clinical situation and the particular product. Silver sulfadiazine (Silvadene, Flamazine) and mafenide acetate (Sulfamylon) creams are also used.
SAFETY ALERT:
Check the patient for any allergies to sulfa, since many burn antimicrobial creams contain sulfa
– Venous thromboembolism prophylaxis (VTE): Burn patients are at risk for VTE. If there are no contraindications, it is recommended that low-molecular weight heparin or low-dose unfractionated heparin be started as soon as it is considered safe. For burn patients who have a high bleeding risk, VTE prophylaxis with sequential compression devices and/or graduated compression stockings are used until the bleeding
• Nutritional therapy
Once fluid replacement needs have been addressed, nutrition takes priority in the initial emergent phase. Early and aggressive nutritional support within several hours of the burn injury can decrease mortality risks and complications, optimize healing of the burn wound, and minimize the negative effects of hypermetabolism and catabolism. Enteral feedings (gastric or intestinal) have almost entirely replaced parenteral feeding. Early enteral feeding, usually with smaller-bore tubes, preserves GI function, increases intestinal blood flow, and promotes optimal conditions for wound healing
• Maintaining Normal Body Temperature
– Provide warm environment: use heat shield, space blanket, heat lights, or blankets.
– Assess body temperature frequently.
– Work quickly when dressing wounds to minimize heat loss from the wound
• Minimizing pain and anxiety
– Pain scale to assess pain and differentiate between restlessness due to pain and restlessness due to hypoxia.
– Administer analgesics as prescribed
– Provide emotional support, reassurance, and simple explanations about procedures.
– Assess patient and family understanding of burn injury
– Psychological interventions if necessary.
4.4.3. INTERMEDIATE PHASE
Begun from 48 to 72 hours after the burn injury and consist of:
– Routine care
– Restoring normal fluid balance
– Preventing Infection
– Maintaining adequate nutrition
– Promoting Skin Integrity
– Relieving pain and discomfort
– Promoting physical mobility
– Supporting patient and family processes
– Monitoring and managing potential complications
4.4.4 Rehabilitation phase
– Promoting activity tolerance
– Improving body image and self-concept
– Monitoring and managing potential complications
– Promoting activity tolerance
4. 5 Complications of burn
The three major organ systems most susceptible to complications during the emergent phase of burn injury are the cardiovascular, respiratory, and urinary systems.
Cardiovascular system complications: include dysrhythmias and hypovolemic shock, which, if untreated, may progress to irreversible shock. Circulation to the extremities can be severely impaired by deep circumferential burns and subsequent edema formation, which act like a tourniquet.
Respiratory system: is vulnerable to two types of injury: (1) upper airway burns and (2) lower airway injury. Upper airway distress may occur with or without smoke inhalation, and airway injury at either level may occur in the absence of burn injury to the skin. The patient may require a fiberoptic bronchoscopy and carboxyhemoglobin blood levels to confirm a suspected inhalation injury. Look in the prehospital notes to see if the patient was exposed to smoke or fumes.
Urinary System: The most common complication of the urinary system in the emergent phase is acute tubular necrosis (ATN). If patient becomes hypovolemic, blood flow to the kidneys is decreased, causing renal ischemia. If this continues, acute kidney injury may develop.
With full-thickness and major electrical burns, myoglobin (from muscle cell breakdown) and haemoglobin (from RBC breakdown) are released into the bloodstream and occlude renal tubules. Carefully monitor the adequacy of fluid replacement because this can counteract obstruction of the tubules.
Infection: The body’s first line of defense, the skin, is destroyed by a burn injury. The burn wound is now colonized with the person’s own organisms that were on the skin before the burn. Localized inflammation, induration, and sometimes suppuration can be seen at the burn wound margins. Partial-thickness burns can convert to full-thickness wounds when these organisms invade viable, adjacent, unburned tissue. Invasive wound infections may be treated with systemic antibiotics based on culture and sensitivity wound swab results.
Watch for signs and symptoms, including hypothermia or hyperthermia, increased heart and respiratory rate, decreased BP, and decreased urine output .The patient may have mild confusion, chills, malaise, and loss of appetite. The WBC count usually is between 10,000/µL (10 ×109/L) and 20,000/µL (20 ×109/L). The WBCs have functional defects and the patient remains immunosuppressed for many months after the burn injury
The causative organisms of sepsis are usually gram-negative bacteria (e.g., Pseudomonas, Proteus organisms), putting the patient at further risk for septic shock. When sepsis is suspected, immediately obtain cultures from all possible sources, including the burn wound, blood, urine, sputum, oropharynx and perineal regions, and IV site. Treatment immediately begins with antibiotics appropriate for the usual residual flora of the particular burn center. When the culture and sensitivity results are known, the antibiotic in use may be continued or changed based on the results. At this stage the patient’s condition is considered critical, requiring close monitoring of vital signs.
Skin and joint contractures and hypertrophic scarring: A contracture (an abnormal condition of a joint characterized by flexion and fixation) develops as a result of the shortening of scar tissue in the flexor tissues of a joint. Areas that are most susceptible to contracture formation include the anterior and lateral neck areas, axillae, antecubital fossae, fingers, groin areas, popliteal fossae, knees, and ankles.
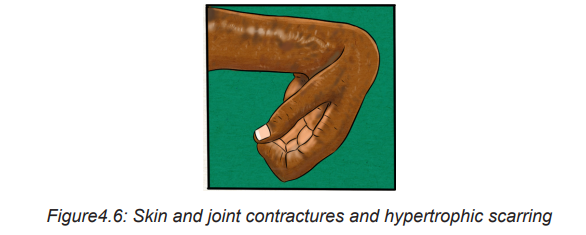
Self-assessment activity 4.3
1. List the four major goals relating to burn management
2. What are the components of nursing and collaborative management of pain?
3. How can you calculate an estimated fluid replacement for a patient with burn?
4. As associated nurse how will you provide fluid to the patient once it is calculated
4.6 End unit assessment
End of unit assessment
1. The injury that is least likely to result in a full-thickness burn is
a. Sunburn.
b. Scald injury.
c. Chemical burn.
d. Electrical injury
2. When assessing a patient with a partial-thickness burn, the nurse would expect to find
a. Blisters.
b. Exposed fascia.
c. Exposed muscles.
d. Intact nerve endings.
e. Red, shiny, wet appearance.
3. Which one of the following is not most important factors that influencing the resulting effects of burn?
a. Temperature of the burning agent
b. Duration of contact time
c. Age of the victim
d. Type of injured tissue
4. The patient is being admitted at health facility where you are working as student in clinical placement and with he is presenting with burn injury after gas explosion at home. Which type of burn injury does the nurse expect to see on admission?
a. Chemical burn injury
b. Thermal burn injury
c. Electrical burn injury
d. Smoke and inhalation injury
5. Which of the following clinical symptoms is likely to explain the full thickness/ third- degree burns?
a. Fluid-filled vesicles or blisters formation associated to sever pain caused by nerve injury.
b. Erythema blanching on pressure, pain and mild swelling, novesicles or blisters
c. Superficial epidermal damage with hyperemia where tactile and pain sensation is intact
d. All skin elements and local nerve endings are destroyed and coagulation necrosis present.
6. You are caring XY patient of 50year old male who has suffered second and third degree burns to the entire anterior thorax and abdomen, anterior right arm, and the anterior of the left upper leg. By using the Rules of Nine, which one of the following constitute the best answer about TBSA:
a. 9%
b. 18%
c. 27%
d. 36%
7. Identify the 4 common factors determining the severity of burn?
8. What do you understand by circumferential burn?
9. By using Parkland formula, calculate the fluid replacement to be administered to a XY patient with TBSA of 32%. Mr XY is a 45 years old man with 1.80m of height and 75kg of weight
10. List at least 5 complications related to burn injury
UNIT 5: DISLOCATION AND FRACTURE
Key Unit competence
Take appropriate decision on dislocation and fracture
Introductory activity 5.0
Observe the pictures below and respond to the questions attached.
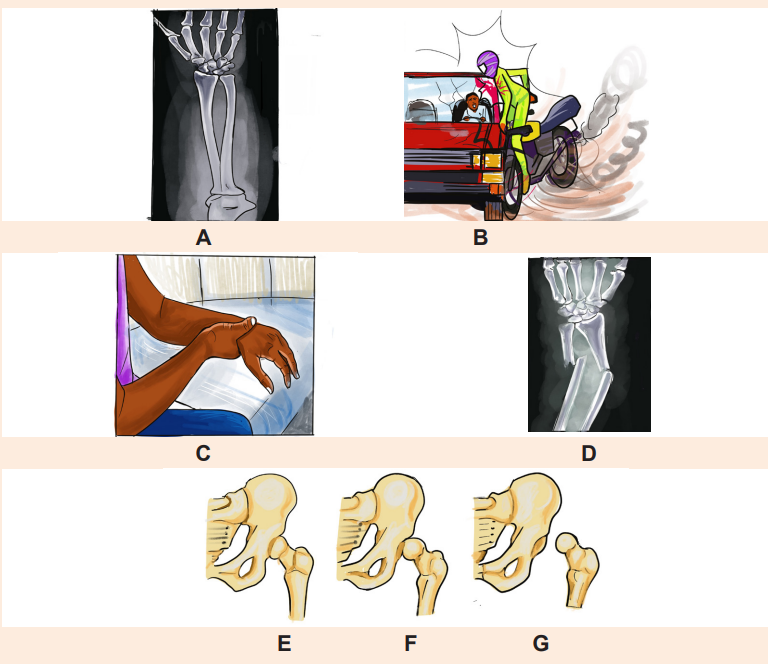
1. From the images mentioned above, which ones represent normal structure of bone?
2. What did happen to image D?
3. By observing the images above, what should be the possible cause of the problem observed in the image D?
4. What do you observe on the images F and G?
5. How image E differ from image G?
5.1. Description of dislocation
Learning Activity 5.1
The place where two or more bones in the body are connected is called a joint. A dislocation is a severe injury to the ligaments that surround a joint. It occurs when the bones in a joint become separated completely from their usual positions, when. Any joint in the body can become dislocated due to various factors. Read the following case study and answer the question below:
A 26 year old male presented to the emergency department of one tertiary hospital in Rwanda complaining with severe right shoulder pain that radiated down his humerus and into his elbow, right shoulder swelling and inability to move his right arm. He reported that he felt from the height of 6m, 40 minutes before arrival and used his arm to avoid complete fall down. Right shoulder dislocation was suspected clinically, x ray was taken and shoulder dislocation noted. Closed reduction was performed to correct this problem and better outcome was observed, patient was discharged at the same day. Previously he experienced shoulder dislocation three times which was reduced manually under local anaesthesia two month prior. She has no other current medical problem and no previous history of relevant surgery.
Questions related to the case study.
1. From the case study above, identifying the two risk factors that can be associated with shoulder dislocation.
2. What are the signs and symptoms of this condition highlighted in the case study?
3. What are the diagnostic measures used to confirm shoulder dislocation for this patient?
4. What is the surgical management done for this patient?
5. What is the outcome for this patient?
5.1. 1. Definition of dislocation concepts
Dislocation: is defined as complete separation of bone from the joint surface

Subluxation: is a partial or incomplete displacement of bone from the joint surface. The clinical manifestation of a subluxation are similar to those of dislocation but the severity are less.
5.1. 2. Causes of dislocation
Any trauma that forces a joint out of place causes a dislocation. The following are the common causes of dislocation: Accident, Falls, Contact sports such as football and basketball. Dislocations can also occur during regular activities when the muscles and tendons surrounding the joint are weak. These injuries happen more often in older people with weaker muscles and balance problems.
5.1. 3. Signs and symptoms of dislocation
Symptoms of a dislocation vary depending on the severity and location of the injury. The most common sign of dislocation is deformity of affected joint. Additional clinical manifestations include: local pain, tenderness, loss of function of injured part, swelling in the joint tissues, bruising, and instability of the joint.
5.1.4. Adequate surgical diagnosis of dislocation
The history taking and physical examination are considered to be the most important tools that physician uses to diagnose a dislocation. The diagnosis of dislocation may be done by looking at the moving joint and asking about what caused the injury.
In some cases, an imaging test called an X-ray man be used to take a picture of the bones. The X-ray studies are performed to determine the extent of displacement of the involved structures. The joint may also be aspirated to assess for hemarthrosis or fat cells. Fat cells in the aspirate indicate a probable intraarticular fracture.
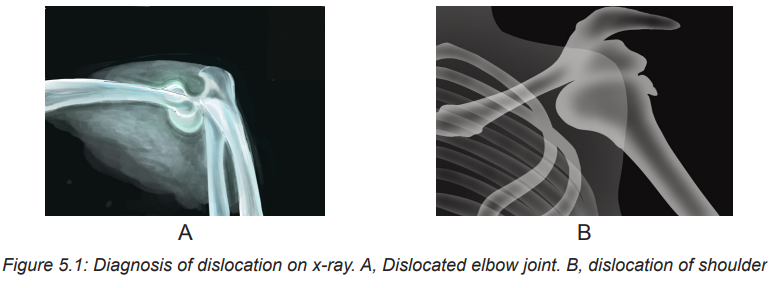
5.1.5 Nursing and collaborative management of dislocation
A dislocation requires prompt attention and is often considered an orthopaedic emergency. It may be associated with significant vascular injury. The longer the joint remains untreated, the greater the possibility of avascular necrosis. The hip joint is particularly susceptible to avascular necrosis .Compartment syndrome may also occur after a dislocation. Neurovascular assessment is critical.
The first goal of management is to realign the dislocated portion of the joint in its original anatomic position. This can be accomplished by a closed reduction, which may be performed under local or general anaesthesia depending on the severity of dislocation. Aesthesia is often necessary to relax the muscle so that the bones can be manipulated without causing pain to the patient.
In some circumstances, surgical open reduction may be necessary. After reduction, the extremity is usually immobilized by bracing, splinting, taping, or using a sling to allow the damaged ligaments and capsular tissue time to heal. Nursing management of subluxation or dislocation is directed toward relief of pain and support and protection of the injured joint. After the joint has been reduced and immobilized, motion is usually restricted. A carefully monitored rehabilitation program can prevent fracture instability and joint dysfunction. Gentle range-of-motion (ROM) exercises may be recommended if the joint is stable and well supported. An exercise program slowly restores the joint to its original ROM without causing another dislocation.
Key components of dislocation management
– Treatment of any serious complications
– Pain relief
– Protection, rest, ice, compression, and elevation (PRICE)
– Realignment (reduction) of parts that are out of place
– Immobilization, usually with a splint or cast
– Sometimes surgery
Techniques for immobilizing a dislocated Joint
Differents technics can be used for managing disloction include:
– Sling technic
– Sling and swathe
– Finger splint
– Dynamic fingersplint
– Radialguttersplint
– Thumbspicasplint
– Posterior ankle splint
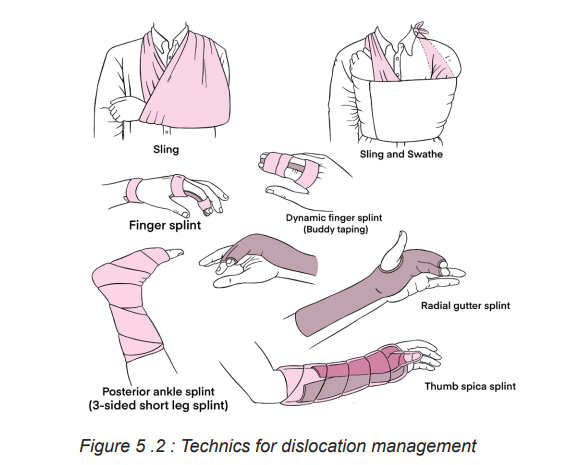
5.1.6 Complications and evolution of dislocation
5.1.6.1 Complications of dislocation
The following table summarizes the main complications related to dislocation
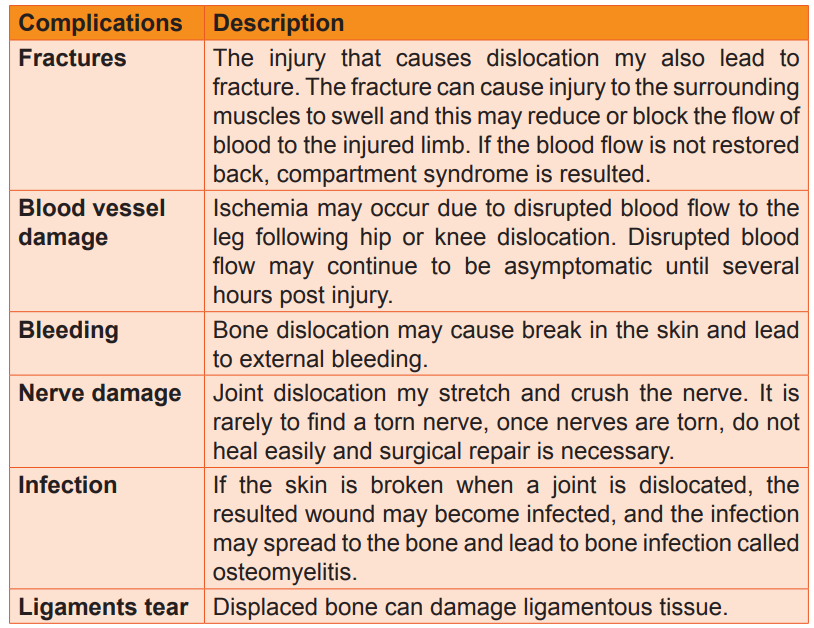
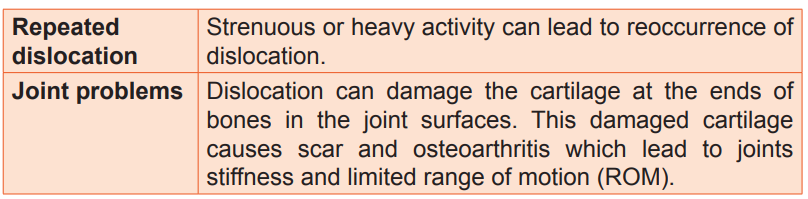
5.1.6.2 Evolution of dislocation
Many dislocations and related injuries heal well and result in few problems. However, some do not completely heal even though they are diagnosed and treated appropriately. How long an injury takes to heal varies from weeks to months depending on type of injury, location of the injury and the person’s age. For instance, very young people heal quickly than adults, and some disorders which impairs blood circulation such diabetes and peripheral vascular disease slow down the healing.
Self-assessment activity 5.1
1. What is the difference between dislocation and subluxation?
2. State four signs and symptoms of hip dislocation.
3. What are the causes and risks factors of dislocation in general?
4. List five key components of dislocation management.
5. Describe four complications of dislocation.
5.2 Description of fractures
Learning Activity 5.2
A 45 years old male admitted in accident and emergency with right thigh deformity, severe pain and profuse bleeding post road traffic accident. The physician performed immediate compressive dressing after giving pain killers and x-ray was of right thigh was ordered. The findings on x ray revealed right open Comminuted femur fracture, the wound was irrigated and cleaned using normal saline and dressed. Casts were used to immobilize the bone while waiting for open reduction and external fixation as final management.
Questions related to the case study.
1. From the case study above, identifying the three signs presented by the patient on arrival at emergency department.
2. Identify the type of fracture highlighted in the case of this patient.
3. What is the diagnostic test done to confirm this type of fracture?
4. What was the management done for this patient?
5.2.1 Definition of fracture
A fracture is a disruption or break in the continuity of the structure of bone. Although physical trauma related injuries account for the majority of fractures, some fractures are caused by disease process especially osteoporosis and cancer.
5.2.2 Classification of fractures
5.2.2.1 Classification of fracture according to the communication with external environment.
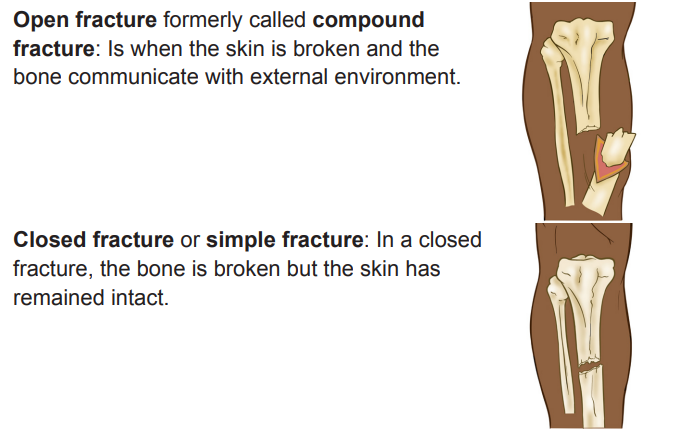
5.2.2.2 Classification of fracture according to the direction of fracture line
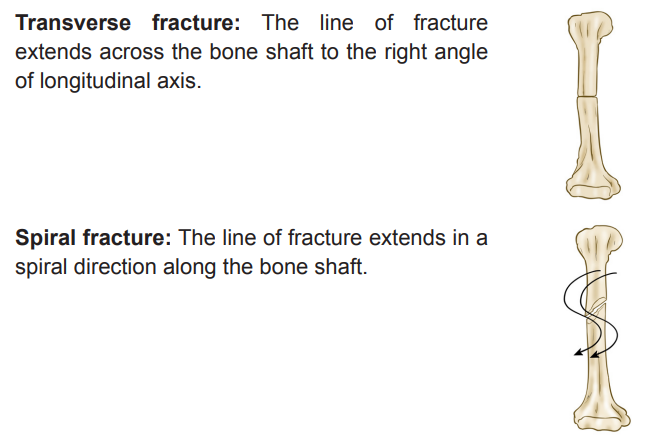
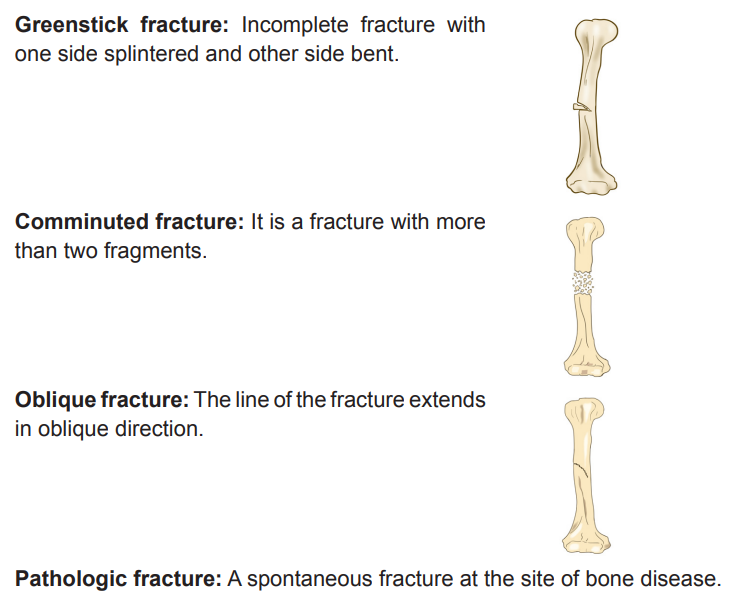
5.2.3 Signs and symptoms of fracture
A client with or suspected to have a fracture will experience the following signs and symptoms including:
Edema and Swelling: due to disruption and penetration of bone through skin or soft tissues, or bleeding into surrounding tissues.
Pain and tenderness: Muscle spasm as a result of involuntary reflex actionof muscle, direct tissue trauma, increased pressure on nerves, movement of fracture parts.
Muscle Spasm: Irritation of tissues and protective response to injury and fracture.
Deformity: Abnormal loss of bony contours.Ecchymosis and contusion: Discoloration of skin as a result of extravasation of
blood in subcutaneous tissues.Loss of Function: due to disruption of bone or joint, preventing functional use of limb or part.
Crepitation: Grating or crunching together of bony fragments, producing palpable or audible crunching or popping sensation.
5.2.4 Stages of fracture healing
Bone healing goes through a complex multistage healing process that occurs in the following stages:
First stage: Formation of hematoma: When a fracture occurs, bleeding creates a hematoma, which surrounds the ends of the fragments. The hematoma is extravasated blood that changes from a liquid to a semisolid clot. This occurs in the initial 72 hours after injury.
Second stage: Granulation tissue: During this stage, active phagocytosis absorbs the products of local necrosis. The hematoma converts to granulation tissue. Granulation tissue (consisting of new blood vessels, fibroblasts, and osteoblasts) produces the basis for new bone substance called osteoid during days 3 to 14 post injury.
Third stage: Callus formation: minerals such as calcium, phosphorus and magnesium and new bone matrix are deposited in the osteoid, an unorganized network of bone is formed that is woven about the fracture parts. Callus is primarily composed of cartilage, osteoblasts, calcium, and phosphorus. This occurs at the end of second week after injury.
Fourth stage: Ossification: Ossification of the callus occurs from 3 weeks to 6 months after the fracture and continues until the fracture has healed.
Fifth stage: Consolidation: As callus continues to develop, the distance between bone fragments diminishes and eventually closes. During this stage ossification continues. This stage can occur up to 1 year after injury.
Sixth stage: Remodelling: Excess bone tissue is resorbed in the final stage of bone healing, and union is complete. Gradual return of the injured bone to its preinjury structural strength and shape occurs. New bone is deposited in sites subjected to stress and resorbed at areas where there is little stress. The summary of bone healing is shown in the images below:
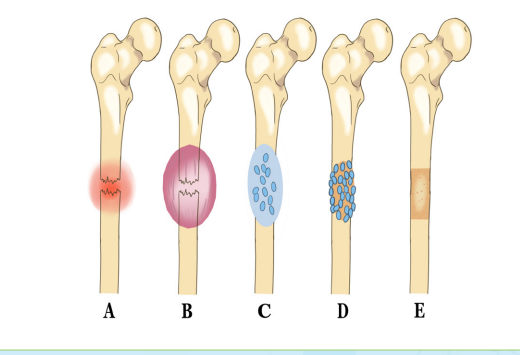
Fig: Bone healing. A, Bleeding at fractured ends of the bone with subsequent hematoma formation. B, Organization of hematoma into fibrous network C, Invasion of osteoblasts, lengthening of collagen strands, and deposition of calcium D, Callus formation: new boneis built up as osteoclasts destroy dead bone. E, Remodelling is accomplished as excess callus is resorbed and trabecular bone is laid down.
5.2.5 Diagnosis of fracture
– History and physical examination
– Radiographic test like X-ray,
– Computed tomography (CT) Scan
– Magnetic Resonance Imaging (MRI)
5.2.6 Treatment plan of fracture
The following are the overall goals of fracture treatment are
1. Anatomic realignment of bone fragments (reduction)
2. Immobilization to maintain realignment
3. Restoration of normal or near normal function of the injured part.
Fracture reduction
It consist of the following of:
– Closed reduction
– Open reduction
– Traction
Closed Reduction: Closed reduction is a nonsurgical, manual realignment of bone fragments to their previous anatomic position. Traction and counter-traction are manually applied to the bone fragments to restore position, length, and alignment. Closed reduction is usually performed while the patient is under local or general anaesthesia immobilize the injured part to maintain alignment until healing occurs.
Open Reduction: Open reduction is the correction of bone alignment through a surgical incision. It usually includes internal fixation of the fracture with wires, screws, pins, plates, intramedullary rods, or nails. The type and location of the fracture, patient age, and concurrent disease may influence the decision to use open reduction. The main disadvantages of this form of fracture management are the possibility of infection, complications associated with anaesthesia, and effect of pre-existing medical conditions (e.g., diabetes).
Traction: Traction is the application of a pulling force to an injured or diseased part of the body or an extremity. Counter-traction pulls in the opposite direction.
Advantages of traction
1. Prevent or reduce pain and muscle spasm associated with low back pain or cervical sprain.
2. Immobilize a joint or part of the body.
3. Reduce a fracture or dislocation.
4. Treat a pathologic joint condition (e.g., tumor, infection).
5. Provide immobilization to prevent soft tissue damage.
6. Promote active and passive exercise.
7. Expand a joint space during arthroscopic procedures.
8. Expand a joint space before major joint reconstruction.
The two most common types of traction
– Skin traction
– Skeletal traction
Skin traction: It is generally used for short-term treatment (48 to 72 hours) until skeletal traction or surgery is possible. Tape, boots, or splints are applied directly to the skin to maintain alignment, assist in reduction, and help diminish muscle spasms in the injured extremity.
The traction weights are usually limited to 5 to 10 lb (2.3 to 4.5 kg). A Buck’s traction boot is a type of skin traction used to immobilize a fracture, prevent hip flexion contractures, and reduce muscle spasms. In skin traction, assessment of the skin is a priority, since pressure points and skin breakdown may occur quickly. Assess key pressure points every 2 to 4 hours.
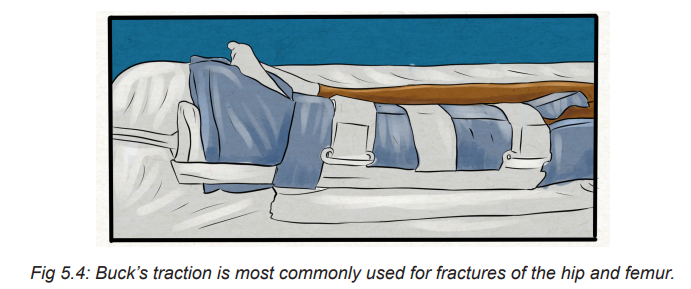
Skeletal traction: It is used to align injured bones and joints or to treat joint contractures and congenital hip dysplasia. It provides a long-term pull that keeps the injured bones and joints aligned. To apply skeletal traction, the physician inserts a pin or wire into the bone, either partially or completely, to align and immobilize the injured body part.
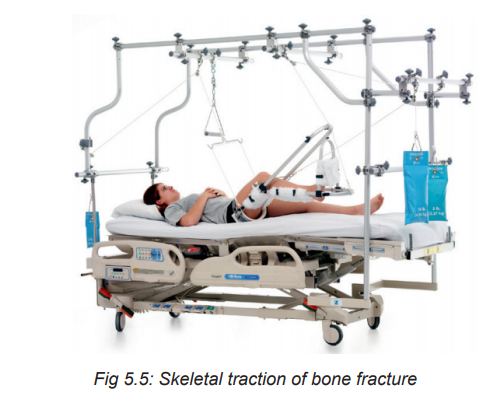
Fracture immobilization
– Casting
– External fixation
– Internal fixation
Casts: A cast is a temporary circumferential immobilization device. Casting is a common treatment following closed reduction. It allows the patient to perform many normal activities of daily living while providing sufficient immobilization to ensure stability.
External Fixation: An external fixator is a metallic device composed of metal pins that are inserted into the bone and attached to external rods to stabilize the fracture while it heals. It can be used to apply traction or to compress fracture fragments and to immobilize reduced fragments when the use of a cast or other traction is not appropriate. Because the use of an external device is a long-term process, ongoing assessment for pin loosening and infection is critical. Infection signaled by exudate, erythema, tenderness, and pain may require removal of the device.
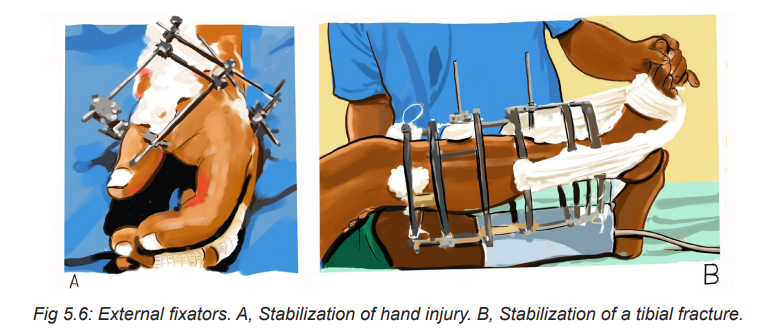
Internal Fixation: Internal fixation devices (pins, plates, intramedullary rods, and metal and bio-absorbable screws) are surgically inserted to realign and maintain bony fragments. These metal devices are biologically inert and made from stainless steel, vitallium, or titanium. Proper alignment is evaluated by x-ray studies at regular intervals.
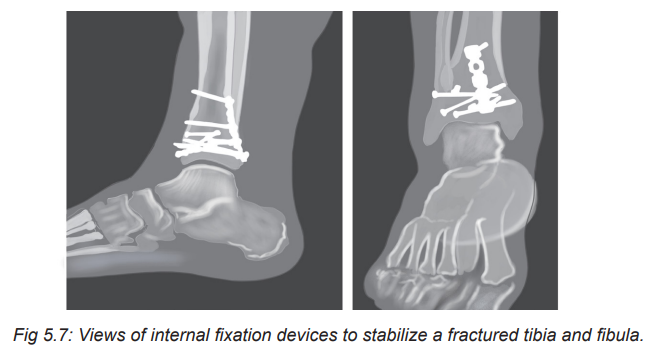
Open fracture management
– Surgical debridement and irrigation
– Tetanus immunization
– Prophylactic antibiotic therapy
– Immobilization
5.2.7 Complications and evolution of fracture
5.2.7.1 Complications of fracture
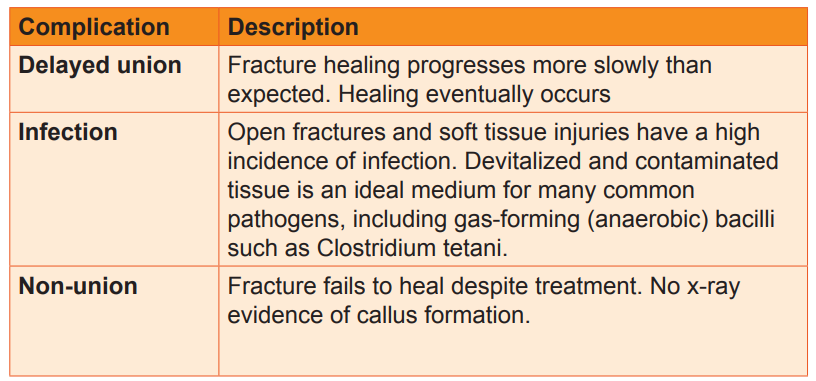
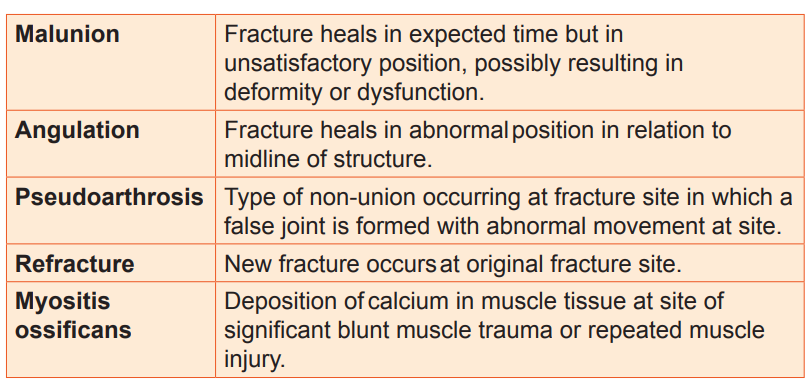
5.2.7.2 Evolution of fraction
The fractures heal well if adequate management is done timely.
5.3. End of unit assessment
1. Dislocation is defined as incomplete displacement of joint surface
– True
– False
2. The history taking and physical examination are considered to be the most important tools that physician uses to diagnose a dislocation
– True
– False
3. Describe the classification of fracture according to the direction of fracture line.
4. Enumerate four stages of bone healing fracture.
5. How a fracture is diagnosed?
6. State two modalities of fracture management.
7. List six complications of bone healing.
8. A 20 years old female patient admitted in emergency department with right femoral bone protrusion associate with bleeding post RTA. Vital signs were in normal range.
a. What type of fracture do you expect for this patient?
b. Which first aid can you give to this patient?
REFERENCES
1. Lewis, S. L., Dirksen, S. R., Heitkemer, M. M., & Linda Bucher. (2014). MEDICAL-SURGICAL NURSING Assessment and Management of clinical problems (NINTH). Canada: ELSEVIER MOSBY.
2. Williams, L. S., & Hopper, P. D. (2015). Understanding Medical Surgical Nursing (Fifth edit). Philadelphia: F.A. Davis Company.
3. Hinkle, J. L., & Cheever, K. H. (2018). Brunner and Suddarth’s textbook of medical-surgical nursing. Wolters kluwer india Pvt Ltd.
4. Winkelman, C. (2016). Medical-surgical nursing: Patient-centered collaborative care. Elsevier
5. https://www.google.com/search?q=dislocation&tbm=isch&ved=2ahUKEwiF5I6i3e33AhUH0YUKHR40DzwQ2-cCegQIABAA&oq=dislo&gs_lcp=CgNpbWcQ
6. https://www.msdmanuals.com/home/injuries-anpoisoning/dislocations/overview-of-dislocations
7. Medical surgical nursing book 9th edition.
8. https://www.google.com search?q=x+ray+of+dislocated+shoulder++&tbm=isch&ved= 2ahUKEwiNoIvatO73AhVCdBoKHaLSBOEQ2
