UNIT 2: SKIN ULCERS AND STOMIES
Key Unit competence
Take appropriate decision on skin ulcers and stomies conditions
Introductory activity 2.0
Observe the images displayed below in box A and B, and answer to the questions below.
1. Reference to what you learned in anatomy and physiology, and the first
Unit of Surgical Pathology, which organ of human body is displayed by images in box A and in Box B?
2. What characteristics/elements would indicate the abnormalities in the structure of the affected organ, in Box A and Box B?
3. Describe the abnormalities that you have observed if any.
4. What do you think can cause the abnormalities that you have observed?
5. What are the manifestations of the observed abnormalities in the human body?
6. How can health personnel identify these abnormalities?
7. How can these abnormal structures be collected?
2.1 Description of Ulcers
Learning Activity 2.1
You are on day duty in surgical in-patient for females, and you are caring for Mrs. M.E, a 62 years old female patient. She is on 15th day of hospitalization for total hip replacement (following a left hip fracture secondary to road traffic accident by a motorcycle) and the discharge is planned in 3 days. She is 1, 65 meter and she weighs 85 kg, with a history of diabetes, and hypertension. Mrs. M.E. is only able to move with help and spends most of her time in bed or a wheelchair. In her documentation, it is also specified that she has stage. II pressure ulcer on her sacral area. You are doing discharge teaching with her daughter, who is her primary caregiver. You explain the importance of preventing further skin breakdown and further complication that she needs to reposition her mother every 2 hours.
Questions related to the case study:
1. What do you understand by pressure injury?
2. On which signs and symptoms do they base on to classify Mrs. M. E’s pressure ulcer as stage II?
3. From the case study above, identifying the risk factors that can be associated with Mrs. ME’s. skin ulcers /pressure injury
2.1.1 Definition of skin ulcers
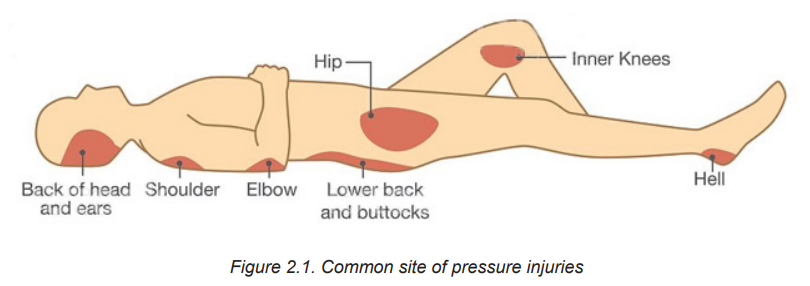
Skin ulcer is an open sore in the skin caused by poor blood flow. Skin ulcers mostly affect the legs, and can also show up on the feet, back, and hips. They are more common in older people and patients with peripheral vascular disease like those with diabetes. Pressure ulcers or injuries are example of most commonly occurring skin ulcers among hospitalized patients. The most common site of pressure injuries are shown on the figure below 2.1:
2.1.2 Types of skin ulcers, Signs and Symptom
Four types of skin ulcers exist. Each one has a different cause and slightly different symptoms. Skin ulcer types include:
Venous skin ulcers
Venous skin ulcers are caused by poor blood circulation in the leg veins. They usually affect the leg between the knee and ankle. Leg ulcers are mostly venous ulcers (80-90%).
Arterial skin ulcers
Arterial ulcers, or ischemic ulcers, happen when blocked arteries cause poor blood flow. These ulcers commonly form on the lower leg, feet, heels, toes, outer side of ankles. Arterial ulcers are usually very painful. Pain might get worse at night or when the legs aren’t moving.
Neuropathic skin ulcers
Neuropathic ulcers are caused by nerve damage and narrow arteries. They’re also called diabetic foot ulcers. These ulcers typically occur on the pressure points of the foot. This includes: heels, toes, and bottom of feet. Neuropathic foot ulcers affect about 15 percent of people with diabetes.
Decubitus (pressure) ulcers
Decubitus ulcer, pressure sore, pressure ulcer, pressure injury, bed sore, are the term used interchangeably. The use pressure injury as the best term, given that open ulceration is not always present.
It is defined as “A localized damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense pressure, prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue”. Pressure injuries usually affect the back, hips, buttocks, ankles, and heels.
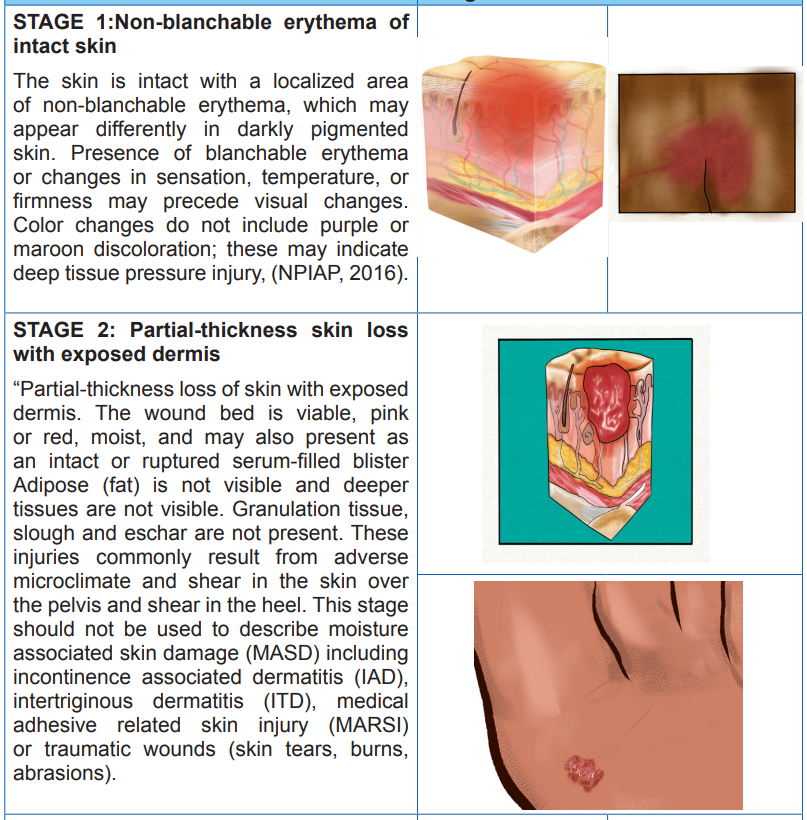
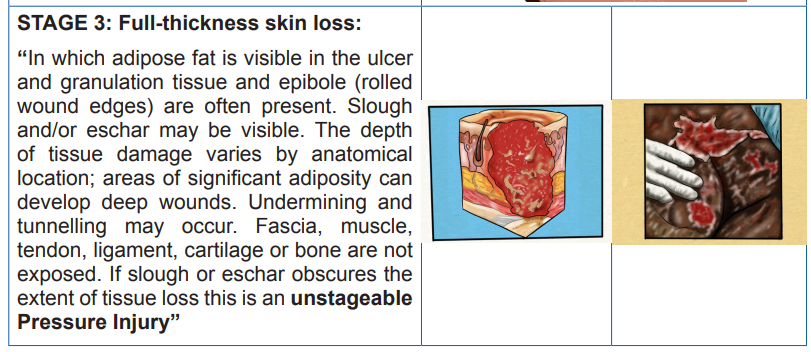
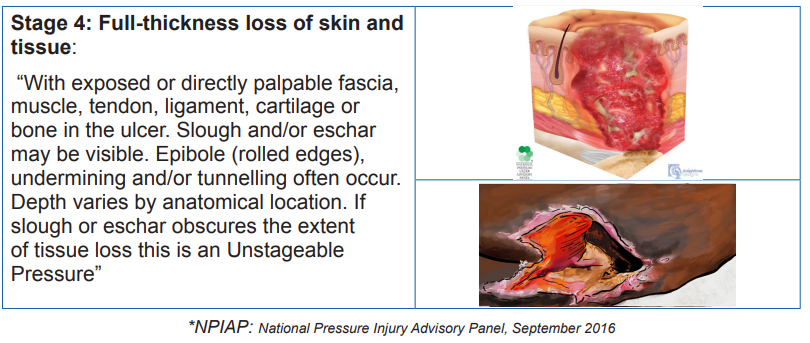
Table2.1. Stages of Decubitus /Pressure injuries/ ulcers
2.1.3 Common Signs and symptoms of a skin ulcer
Signs and symptoms depend on the types and the severity of the skin ulcer. A skin ulcer generally, looks like a round open sore in the skin. Its outer border might be raised and thick. Others signs and symptoms may include itchiness, skin discoloration (in early stage) pain, redness (for darker skin tone, it may look shiny or blue) swelling and tenderness around the ulcer. Additionally fever, bleeding, or pus (yellow or green pus due to an infection) draining from the ulcer may be noticed. The more the skin ulcer gets worse, the more it will look like a crater.
Self-assessment activity 2.1
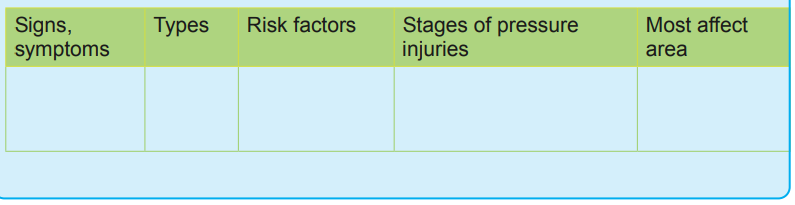
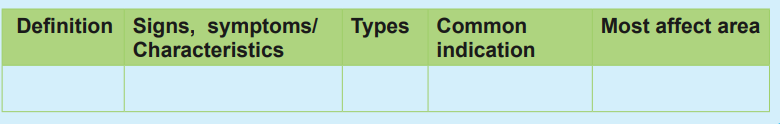
From your readings, please use the provided words to fill out the table below:
“Non-blanchable erythema of intact skin, Older age, Pain, Redness, Venous skin ulcers, Peripheral vascular disease, Round open sore with thick and raised outer border, Ankles, Heels, Decubitus ulcers, Poor blood supply , Tenderness around the sore, Back of The head(occiput) and ears, Itchiness, Skin discoloration , Swelling, Poor blood flow, Back, Neuropathic skin ulcers, hips, Buttocks, Partial thickness skin loss with exposed dermis, elbow, shoulders,
2.2. Causes, risk factors, overview on pathophysiology and diagnostic measures of skin ulcers
Learning Activity 2.2
… Continuation of M.E case study. The day prior discharge of Mrs. M.E, she was complaining of fever. The vital signs were To 380 C, Pulse 88 beats /min, BP 82/59, RR 20 resp/min. The full blood count was done and leucocytosis was noticed with decreased haemoglobin. The examination of pressure injury revealed a dirty dressing with foul smelling and pus discharge. Adipose fat in the wound was also visible but tendon, fascia, muscle, ligament, and cartilage were not visible. The care givers reported that after being home back to look for money (leaving her little sister with their mother), she came back and found out that their mother is no longer eating well, and is weak.
Questions related to the case study:
1. Identifying the risk factors that can be associated with Mrs. ME’s deteriorated health status?
2. What are the underlying cause of her hyperthermia and leucocytosis?
3. At which stage of pressure injury is her pressure now?
4. Briefly describe the pathophysiological mechanism behind her pressure injury
2.2.1 Causes and pathophysiology of ulcers
The skin ulcers develop when there is a lack or reduced blood circulation. Causes of poor blood flow include:
a) Diabetes: lack or insufficient insulin production by islet of Langerhans in the pancreas to metabolise the sugar lead to high blood sugar. Over time, high blood sugar lead to nerve damage, a situation called peripheral neuropathy. The last one lead to decrease or loss of sensitivity including in feet and legs. Unfelt pressure and pain will lead to unrecognized injury in feet or legs. Untreated injuries can easily turn into skin ulcers, and high blood sugar slows down the wound healing.
b) Atherosclerosis or arteriosclerosis: is a disease whereby the arteries become narrow due to fat build-up called plaque, a situation which hinder the blood circulation leading to poor blood supply to body organs particularly extremities. If left untreated, the body organ which are not well perfused the skin tissue will break down and a sore will be formed
c) Venous insufficiency: occurs when the veins cannot send blood from legs to the heart. Blood collects in the leg veins, which leads to swelling. If the swelling is severe, it can put pressure on skin and cause ulcers. (Causes of venous insufficiency include varicose veins and blood clots).
d) Pressure: Pressure ulcers /injuries begin when staying in one position for too long, the individual’s body weight exerts a downward constant force on the skin and subcutaneous tissue that lie between a bony prominence and an external surface (such as a mattress or wheelchair cushion). Sustained pressure from medical devices may also cause pressure injuries. It is generally thought that force that results in an external pressure more than the arterial capillary filling pressure, around 32 mm Hg, and more than the venous capillary outflow pressure, around 8 to 12 mm Hg, inhibits blood flow and results in local tissue hypoxia. Sustained external pressures above a threshold causes prolonged ischemia and sets the tissue down a path toward necrosis. Reperfusion injury, which occurs because of the return of blood supply after a period of ischemia, has been posited as an additional source of tissue damage leading to pressure ulcers/injury. The highest pressures often occur at the interface of bone and muscle, causing necrosis at this depth while leaving the skin relatively spared
NB: The following microbial (bacteria), also play a role in pressure injuries infections:
– Staphylococcus aureus
– Pseudomonas auruginosa
– Proteus mirabilis
– Enterococcus faecalis
2.2.3 Risk factors of skin ulcers/injuries
Risk factors of developing skin ulcers include:
– Increasing age: due to increased atherosclerosis and venous insufficiency.
– Limited mobility. Being bedridden, paralyzed, or using a wheelchair puts the skin under constant pressure, decreased blood perfusion to tissue, hypoxia and necrosis or open sore
– Cigarette smoking. Smoke hardens arteries and disrupts proper blood flow.
– History of blood clots leading to blood flow issues, hypo perfusion of tissue, necrosis, and open sore
– High blood pressure. Hypertension damages the arteries and disrupts blood flow.
– High blood cholesterol: it increases narrowing and oxidative stress in the arteries, which disrupts blood flow.
– Obesity: raises the risk for diabetes, atherosclerosis, and increased pressure in leg veins.
– Pregnancy. During pregnancy, hormonal changes and increased blood volume may cause leg vein problems.
2.2.4 Adequate surgical diagnosis of skin ulcers
Skin ulcers are usually clinically diagnosed, however there is a series of test which can be performed to assist in the diagnostic process. These include:
– Medical history: The information provided can help to better understand the symptoms
– Physical exam: This reveals the size and depth of the patient’s sore/ulcer, and explore if any blood, fluid, or pus discharge.
– Blood test: in case of infected ulcer, a blood panel (complete Blood Count (CBC), haemoglobin (Hb), Haematocrit (Ht), Red blood cells can assist in determining the underlying cause of infection.
– Tissue or fluid culture. This test can also help in determining the kind of the bacteria causing the infection for the prescription of the right antibiotics.
– Imaging tests. An X-ray, CT scan, or MRI helps in visualizing the tissue and bone under the sore/ulcer, to take appropriate measures.
Self-assessment activity 2.2
1. How diabetic patient are more likely to develop pressure injury?
2. List specific microbes which are more likely to cause the infection of pressure injuries
3. What are the diagnostic measures of skin ulcers?
4. Briefly explain how obesity increase the risk of developing pressure injuries.
2.3 Management of skin ulcers
Learning Activity 2.3
Following the interpretation of Mrs. ME’s laboratory exams results, the physician decided to prescribe injectable antibiotics, oral analgesic and painkiller, as well as the Ringers lactate. He also prescribes twice daily wound cleaning with normal saline 0.9% and wet dressing. 5 days later Mrs. ME. reported to fill well, and the laboratory results were promising and the discharge was decided.
Questions related to the case study.
1. What is the goal of skin ulcer treatment and management?
2. What is the surgical treatment plan adopted by the physician for Mrs. ME.?
3. In your respective groups, discuss different medical treatment prescribed to Mrs. ME and give an example of appropriate drug on each group of medication (antibiotics, analgesic and painkiller).
4. Briefly describe specific supportive management needed for Mrs. ME.
5. What do you plan to include in the patient and care giver teaching plan prior discharge?
2.3.1 Treatment plan of ulcers
The goal of skin ulcer treatment is to heal the wound, reduce pain, and treat any infection. The treatment may include:
a) Wound/ sore/ulcer cleaning and Dressing: to protect the wound and keep it clean. This promotes healing and prevents infection. The type of dressing depends on type and cause of ulcer and the findings from examination findings. Examples include moist dressings, hydrogels, hydrocolloids, collagen wound dressings, dressing with honey, and antimicrobial dressings.
NB: Normal saline 0.9% is mostly used to clean skin ulcers. Always check on the prescribed cleansing solution, recommended dressing type and the frequency of dressing changes
b) Antibiotics: antibiotic ointment is prescribed for infected skin ulcers. Once the infection has reached deeper tissue or bone, oral antibiotics will be recommended. In some patients, skin ulcer may not be infected but the antibiotics are prescribed to reduce the risk of infection.
c) Pain medication: for painful skin ulcer, analgesics may be prescribed to control patient’s pain .This may include simple analgesic like Paracetamol, ibuprofen, diclofenac, or even strong analgesic like morphine.
NB: The choice of the analgesic, route and dosage depend on individual case basing on the severity of the skin ulcer, complication and other comorbidities.
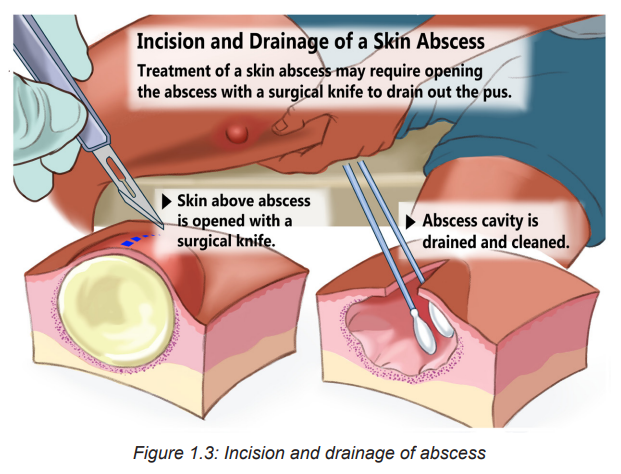
d) Surgery: Surgery is the last treatment option and it is indicated in large sore/ ulcer which might need for example, a skin graft. This will close the wound and help proper healing. Surgery may also be done to remove pressure by shaving away bone.
NB: For the management of skin ulcers/injuries, caused by pressure (called pressure injuries/ulcers) the treatment includes pressure reduction, friction avoidance and shearing forces, local care and sometimes skin graft as earlier discussed
e) Specific Supportive management
• Pressure relief over the affected or vulnerable area –turning the patient every 2 hours
• Rigorous skin care
– Keeping the skin clean and well hydrated to prevent skin erosions and lacerations
– Catheterization for patient with incontinence
– Advice caregivers to assess other areas at risk to identify early signs of pressure ulcer
• Nutrition
– Protein supplements
– Adequate nutrition and hydration in consultation with nutritionist
• Optimize management of comorbidities that may affect healing e.g. uncontrolled DM
• Ensure proper follow-up:
– The wound should be cleaned and freshly dressed regularly
– Repeated debridement might be necessary
• To use pressure injury risk assessment tool to identify individuals at risk of developing pressure injuries. They are five tools like Braden scale, Norton scale, Gosnell scale, the Knoll scale and the Waterlow scale. The most widely used is the Braden Scale for predicting injury developed by Barbara Braden and Nancy Bergstrom in 1988.This tool allows nurses and other healthcare providers to evaluate the patient’s risk for developing pressure injuries by examining six criteria:
– Sensory Perception: ability to respond meaningfully to pressure related discomfort (1–4)
– Moisture: degree to which skin is exposed to moisture (1–4)
– Activity: degree of physical activity (1–4)
– Mobility: ability to change and control body position (1–4)
– Nutrition: usual food intake pattern (1–4)
– Friction and Shear: amount of assistance needed to move, degree of sliding on beds or chairs (1–3)
The highest score is 23 while the lowest total score is 6 (NPUAP, 2014)
• A patient with A score of 15 to 18 has mild risk of developing pressure injury
• The one with a score of 13 to 14 has a moderate risk,
• A score of 10 to 12 indicate that the patient is at a high risk of developing pressure injury
• A score of 9 or less is an indication that the patient is at a very high risk
f) Patient’s Teaching for Simple Skin Ulcer Management Within Household:advise the patient to:
• Elevate the affected leg to improve blood flow. the leg is kept above the heart level, and cushions or pillows can be used for this purpose
• Use compressing socks to reduce leg swelling by improving blood flow back up to the heart.
• Apply high quality honey to a dressing, then apply the dressing on the skin. Honey has anti-inflammatory and antimicrobial benefits. (NB: Open sore should be managed in appropriate health setting with qualified health personnel and appropriate sterile materials)
2.3.2 Complications from skin ulcers
If left untreated, a skin ulcer may become infected, and the healing process will be prolonged. The infection can also spread to deeper tissue, bones, joints, and blood.
Self-assessment activity 2.3
1. In regards to predicting the risk of developing pressure injury among hospitalized patients,
a) Enumerate the existing tools serving for that specific purpose
b) Among them, which tool is mostly and widely used?
c) For the widely used, enumerate criteria based on to evaluate/score the patient’s risk of developing pressure injury/ulcer
2. What is the most used cleansing solution to clean pressure injuries
3. What is the most important preventive measure of skin ulcers?
4. What are the complication of untreated skin ulcers?
2.4. Description of Stomies
Learning Activity 2.4
Six weeks following Mrs. ME discharge, she has been readmitted, complaining of severe crampy abdominal pain, diarrhoea, mixed with blood, fatigue and weight loss. Following the complementary exams, the ulcerative colitis was confirmed and ileostomy was performed.
Questions related to the case study:
1. What do you understand by ileostomy?
2. What are characteristics of a normal stomy/ostomy?
3. List the types of stomies you know
4. What is the difference between ileostomy and colostomy?
2.4.1 Definition of stomy
The term comes from Greek. The suffix stoma means “mouth”, “opening”. According to Taber’s Medical Dictionary, stomy is defined as artificially and surgically produced opening into a specified part of the body or between body parts.
The term stomy and ostomy are used interchangeably, and by definition an ostomy is a surgical procedure that allows intestinal contents to pass from the bowel through an opening in the skin on the abdomen. The opening is called a stoma.
The stoma is created when the intestine is brought through the abdominal wall and sutured to the skin. The intestinal contents then empty through the hole on the surface of the abdomen rather than being eliminated through the anus. An ostomy is used when the normal elimination route is no longer possible. It should be clean, slightly pink, without ulcerations.
2.4.2 Types stomies
The stomy or ostomy is described and named according to the part of the body where it is produced and according to the type. A normal ostomy/stomy is pinkish-red and moist. It slightly sticks out from the skin, and it is normal to see a little mucus. Spots of bloodish mucus on stoma/ostoma is also normal. Below are examples of stomies:
• Tracheostomy: A tracheostomy is a surgically created stoma in the trachea to establish an airway. It is used to:
– Clear upper airway (bypass obstruction),
– Facilitate removal of secretions,
– Allow long-term mechanical ventilation.
• Esophagostomy: an ostomy produced at the level of esophagus
• Gastrostomy: an ostomy produced at the level of gastric
• Jejuniostomy: an ostomy produced at the level of jejunum
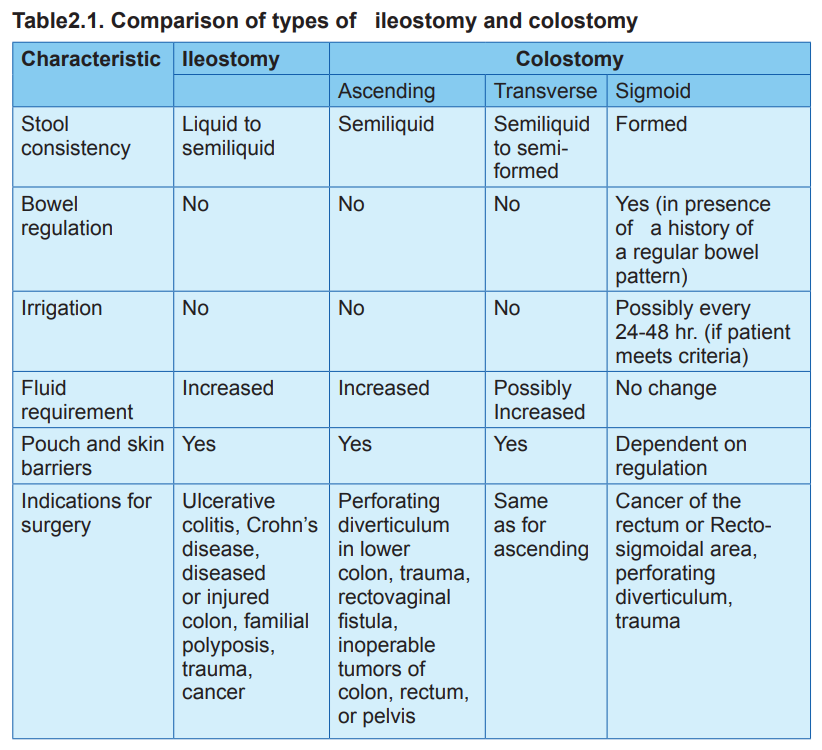
• Ileostomy: An ostomy made at the level of ileum. Output from an ileostomy has not entered the colon and thus is liquid. The ileostomy drains continuously, and the patient must constantly wear a bag to collect the drainage. In contrast, output from a sigmoid colostomy resembles normal formed stool, and some patients are able to regulate emptying time so they do not need to wear a collection bag (see table 1).
• Caecostomy: an ostomy produced at the level of caecum
• Colostomy: An ostomy in the colon. It is also named and characterized by its anatomic site such as ascending, transverse, descending and sigmoid colostomy. The more distal the ostomy, the more the intestinal contents resemble feces that are eliminated from an intact colon and rectum.
• Urostomy (urinary diversion): is a surgically created opening in the abdominal wall through which urine passes. An urostomy indicated when the bladder is either not functioning or has to be removed. Reasons for surgery includes: bladder cancer, spinal cord injuries, and malfunction (e.g. chronic infection of the bladder and birth defects such as spina bifida).
NB: Ostomies may be temporary or permanent. For example, the person with a draining fistula may need a temporary ostomy to prevent stool from reaching the diseased area. Patients who have trauma to the intestines (e.g., gunshot wound, stabbing) may need a temporary ostomy. Cancer involving the rectum requires a permanent ostomy because all bowel distal to the ostomy is removed. The major types of ostomies are end stoma, double-barreled, and loop ostomy
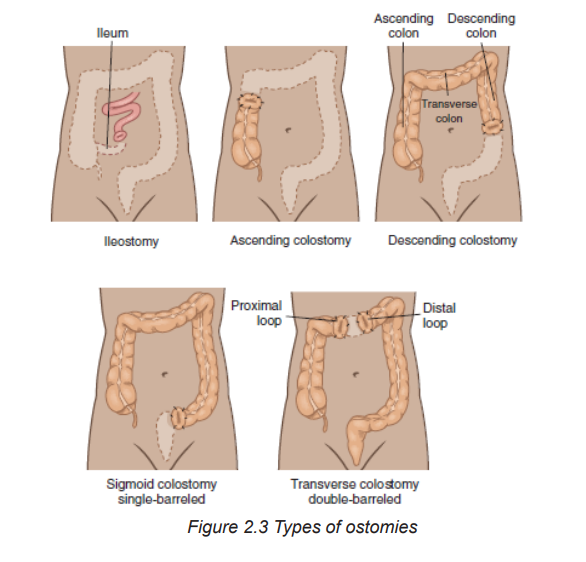
The table below summarizes the comparison of types of ileostomy and colostomy
Self-assessment activity 2.4
From your readings, please use the provided words to fill out the table below:
“injured colon, surgically produced opening into a specified part of the body, Esophagostomy, moist, familial polyposis, Presence of little mucus, Ileostomy, pinkish-red, Urostomy, slightly stick out from the skin, Tracheostomy, Spots of bloodish mucus, Ulcerative colitis, Crohn’s disease, trauma, cancer, Perforating diverticulum in lower colon”
2.5 Management of stomies
Learning Activity 2.5
It is on day 5 of Mrs. ME hospitalization post readmission. She is now feeling well, vital signs are within normal range and she regained appetite. She is only complains of her peristoma mucosal pain and irritation
Questions related to the case study:
1. What do you think has caused the reported irritation?
2. How would you best manage/treat this problem?
3. What are the possible complication to be prevented?
2.5.1 Treatment plan of stomies
The management of peristomal skin problems depends on the contributing factors. Generally, the management of stomies consists of regular cleaning, changing the puching bag, and or dressing where necessary Normal peristomal skin should be clean, dry, and intact and look like the skin on the rest of the abdomen or the skin where it is located. In case of deep infection, systemic antibiotics will be prescribed
2.5.2 Stoma Complications
Two categories exist: Early and late complication
– Early stomal complications occur within 30 days of surgery, and include: mucocutaneous separation, stoma necrosis, and stoma retraction.
– Late complications include stomal stenosis, stomal prolapsed, stomal trauma, and parastomal hernia. The Goals to prevent or decrease the incidence of stoma complications include weight reduction, promoting a healthy lifestyle, and proper ostomy management pre- and postoperatively.
Peristomal Complications
Peristomal skin issues are common and mostly occurs in eldest due to skin aging process. Immediate peristomal complication are caused by
a) Chemical (moisture-related injury from exposure to stoma effluent or stool leakage): Irritation of peristomal mucosal by digestive enzymes in the small intestine. if leaved untreated peristomal skin can become so damaged that the skin barrier will not adhere
b) Mechanical: results from skin stripping, abrasions or pressure injury due to the removal of skin barrier, tape or ostomy accessories.
c) Bacterial: Moist skin is more prone to overgrowth of fungi and bacteria.
Note: Beside, stoma and peristomal complications, patients with ostomies (Particular patients with ileostomy) are at risk of dehydration and electrolyte deficiency. This is due to the loss of the absorptive function of the large colon. Patients should be taught signs and symptoms of dehydration, how to prevent it, and when to report to the health facility.
Note: Patients with ileostomy should:
– Drink up to 2 l of fluid a day, and more if they are in hot weather or participating in outdoor activities
– Increase food intake high in sodium like canned vegetables, broth, and tomatoes, and in potassium, such as bananas, potatoes, and spinach.
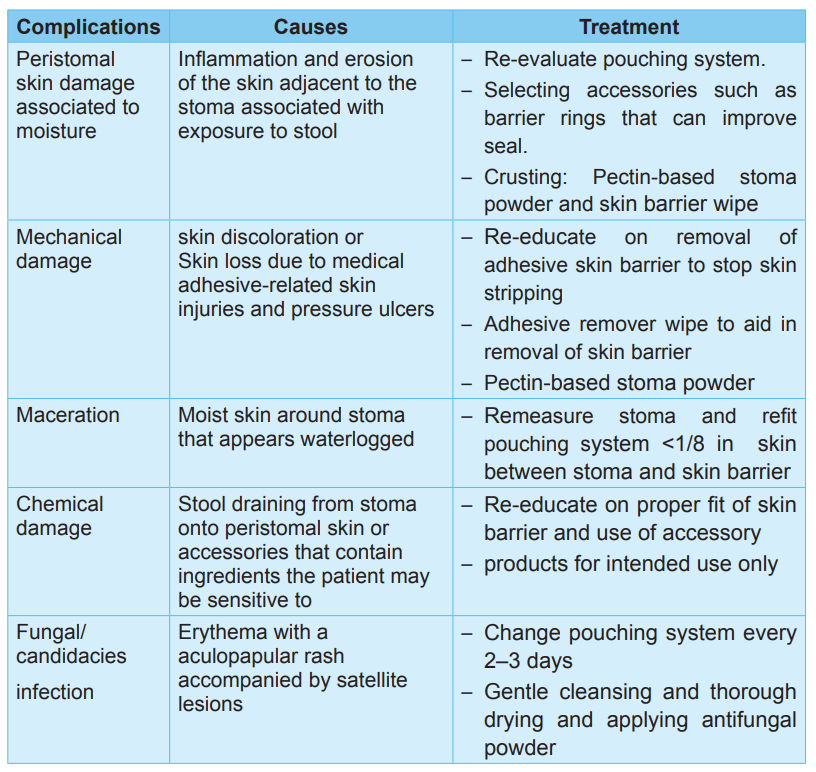
The table below summarize common peristomal complications and their management
Table 2.2: Summary of peristomal complications
2.5.3 Associate nurse decision making
An associate nurse who receives a patient with signs and symptoms of skin ulcer and stomy must be able to diagnose these conditions, manage simple skin ulcers and stomy and refer complicated cases to the next level for adequate management. In the hospital, the associate nurse works under supervision of registered nurses and they will discuss the appropriate nursing care plan. The associate nurse also helps the patient to comply with self-care:
Ostomy Self-Care
1. Explain what an ostomy is and how it functions.
2. Describe the underlying condition that resulted in the need for an ostomy.
3. Demonstrate and allow the patient and caregiver to practice the following activities:
– Remove the old skin barrier, cleanse the skin, and correctly apply new skin barriers.
– Apply, empty, clean, and remove the pouch.
– Empty the pouch before it is one-third full to prevent leakage.
– Irrigate the colostomy to regulate bowel elimination (optional).
4. Explain how to contact the wound, ostomy, and continence (WOC) nurse with questions.
5. Describe how to obtain additional ostomy supplies.
6. Explain dietary and fluid management.
– Identify a well-balanced diet and dietary supplements to prevent nutritional deficiencies.
– Identify foods to avoid to reduce diarrhea, gas, or obstruction (with ileostomy).
– Promote fluid intake of least 3000 mL/day to prevent dehydration (unless contraindicated).
– Increase fluid intake during hot weather, excessive perspiration, and diarrhea to replace losses and prevent dehydration.
– Describe symptoms of fluid and electrolyte imbalance.
– Explain how to contact the registered dietitian with questions.
– Explain how to recognize problems (fluid and electrolyte deficits, fever, diarrhea, skin irritation, stomal problems) and how to contact the appropriate health care provider.
7. Describe community resources to assist with emotional and psychologic adjustment to the ostomy.
8. Explain the importance of follow-up care.
9. Describe the ostomy’s potential effects on sexual activity social life, work, and recreation and strategies to manage these changes.
2.6 End unit assessment
End of unit assessment
1. Which patient is at the greatest risk for developing pressure injury?
a) A 42-year-old obese woman with type 2 diabetes
b) A 78-year-old man who is confused and malnourished
c) A 30-year-old man who is comatose following a head injury
d) A 65-year-old woman who has urge and stress incontinence
2. What is the most important nursing intervention for the prevention and treatment of pressure injury?
a) Using pressure-reduction devices
b) Massaging pressure areas with lotion
c) Repositioning the patient, a minimum of every 2 hours
d) Using lift sheets and trapeze bars to facilitate patient movement
3. The patient is being transferred from another health facility with the description of a sore on her sacrum that is deep enough to see the muscle. What stage of pressure injury does the nurse expect to see on admission?
a) Stage I
b) Stage II
c) Stage III
d) Stage IV
4. A Nurse coming on day duty is reading the patient’s file(records) and he found out that the patient has a stage III pressure injury on his right left hip. What should the nurse expect to find on assessment of the patient’s left hip?
a) Exposed bone, tendon, or muscle
b) An abrasion, blister, or shallow crater
c) Deep crater through subcutaneous tissue to fascia
d) Persistent redness (or bluish color in darker skin tones)
5. Which nursing interventions for a patient with a Stage IV sacral pressure injury are most appropriate to assign or delegate to a licensed practical nurse (select all that apply)?
a) Assess and document wound appearance.
b) Teach the patient pressure injury risk factors.
c) Choose the type of dressing to apply to the ulcer.
d) Measure the size (width, length, depth) of the ulcer.
e) Assist the patient to change positions at frequent intervals.
6. Of the following pressure injury predicting tool, what is the most widely used?
a) Braden scale
b) Gosnell scale
c) Waterlow scale
d) Norton scale
7. What do you understand by tracheostomy?
8. Identify the common sites of skin ulcers and ostomies
9. What are the risk factors that can be associated with pressure injury development?
10. Explain the pathophysiological mechanisms behind development of Pressure injury
