UNIT3:BARRIER AND PERMANENT FAMILY PLANNING
Key Unit Competence
Provide barrier and permanent family planning services
Introductory activity 3
Analyze the pictures above, and answer the questions below:
a) What are the messages conveyed by these pictures above?
b) What have you heard about the methods of family planning shown by the
above pictures?
c) In your opinion, under what circumstances should the family planningmethods shown in the above pictures can be indicated?
3.1 Introduction to barrier family planning methods
Learning activity 3.1
i. What do you know about barrier methods?ii. What are the types of barrier methods?
Barrier methods include either physical devices that prevent sperm from reaching
an egg or chemicals that kill or damage sperm in the vaginal canal. Barrier methods’
success is highly dependent on people’s ability to use them correctly every time
they do sexual intercourses. When used correctly, barrier methods can prevent
women from becoming pregnant and can also protect both the female and male
partners against sexually transmitted infections including HIV.
Barrier contraceptives are classified into two main types: mechanical barriers and
chemical barriers.
Mechanical barriers
They are devices that provide a physical barrier between the sperm and the egg.
Examples of mechanical barriers include the male condom, female condom,
diaphragm, cervical cap, and sponge.
Chemical barriers
Chemical barriers or spermicides are sperm-killing substances, available as foams,
creams, gels, films or suppositories, which are often used in female contraceptionin conjunction with mechanical barriers and other devices.
Self-assessment 3.1
i) How do barrier methods of family planning act?
ii) With examples, explain the two types of barrier family planning methods.iii) To what extent are barrier methods of family planning successful?
3.1.1 Male condom
Learning activity 3.1.1
i) What do you know about the male condom?
ii. In what situations can you advise individuals and couples to use male
condom?iii. Enumerate advantages and disadvantages of male Condom?
Introduction
A male condom is a covering that unrolls over a man’s erect penis and is usually
made of thin latex rubber. It keeps a man’s sperm from getting into a woman’s
vaginal canal. It can also prevent the partner from becoming infected with the
microorganisms that cause various Sexually Transmitted diseases (STIs) and
Human Immune Deficiency Virus (HIV).
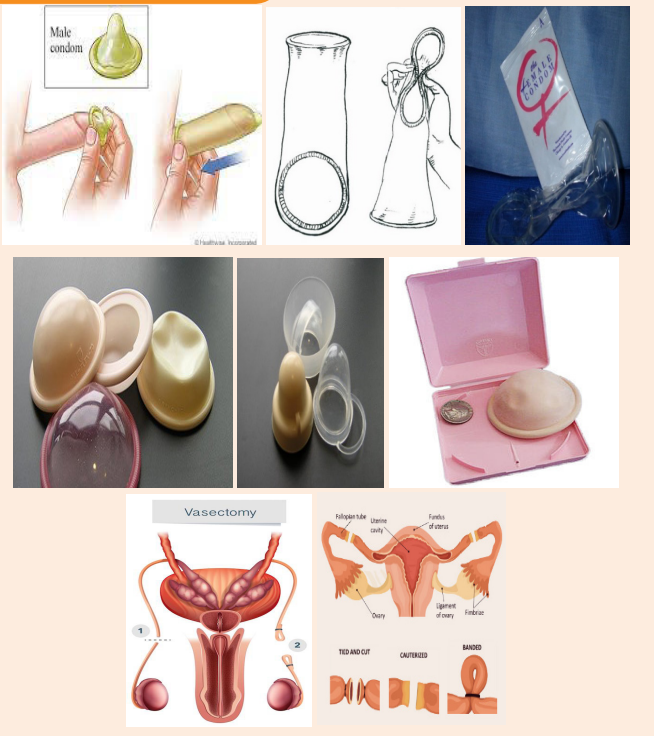
a) How to use a male condom
Watch the video demonstration on how to wear a male condom found on this link:
For each sex act, one new condom must be used. Before using a condom, the
package must be checked to see if the condom is not torn or damaged. Expired
condom should not be used. Other directions on the use of the condom are outlinedin the box below.
b) Indication
The male condom should be indicated as a family planning method of choice in the
following cases
• If the couple chooses that as their preferred,
• If an individual man or woman engages in occasional sexual intercourse,
• discordant couples,• If a man has premature ejaculation problems.
c) Contraindications
The male condom should not be the family planning method of choice in the
following cases:
• If the individual male partner is allergic to latex manifested through swelling
or difficulty breathing,
• If the individual male partner cannot maintain erection,
• For some people (both male and female) who may develop a mild, local
irritation or a rash after using a male condom.
d) Effectiveness
When used correctly on every act of sexual intercourse, male condoms are 98%
effective in protecting the woman from getting pregnant. This means that only 2
out of 100 people will become pregnant in 1 year when male condoms are used as
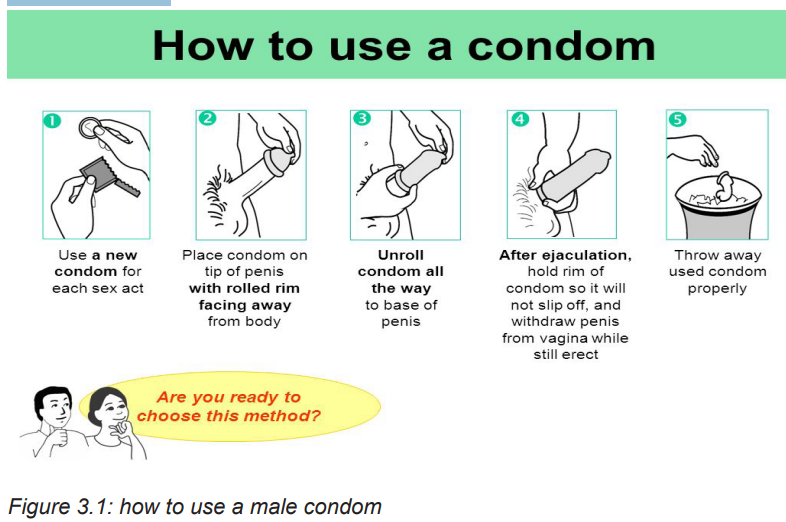
contraception.e) Advantages and disadvantages of male Condom use
Self-assessment 3.1.1
i) Who should use a male condom as a family planning method?
ii) Who should not use male condom as a family planning method?iii) Explain step by step how a condom is used.
3.1.2 Female condom
Learning activity 3.1.2
a) What do you know about the female condom?
b) Who should use the female condom as a family planning method?c) Who should not use female condom in family planning method?
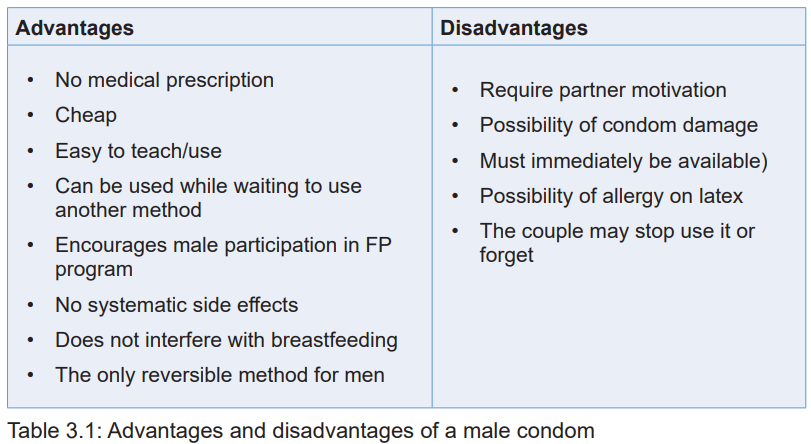
A female condom is a lubricated pouch made of thin, soft plastic that fits loosely
inside vagina used during sexual intercourse to reduce the probability of
pregnancy and/or sexually transmitted infections. A female condom can be put
into the vagina before sex, but make sure the penis does not come into contact
with the vagina before the condom has been inserted. Semen can still come out
of the penis even before a man has had an orgasm (fully ejaculated).
a) How to use a female condom
For each sex act, one new condom must be used. Before using a condom, the
package must be checked to see if the condom is not torn or damaged. Expired
condom should not be used.
• Open the packet and remove the female condom, taking care not to tear it.
• Squeeze the smaller ring at the closed end of the condom and put it into the
vagina.
• Make sure the large ring at the open end of the condom covers the area
around the opening of the vagina.
• Make sure the penis goes in the female condom, not between the condom
and the side of the vagina.
• After sex, remove the female condom immediately by gently pulling it out. You
can twist the large ring to prevent semen leaking out.
• Throw away the condom in a bin, not the toilet.
b) Mode of Action
Female condom act by forming a barrier that keeps sperm out of the vagina,
preventing pregnancy.
c) Indications
Some indications of using female condom include the following:
• Individual’s or couple’s choice
• If an individual engages in occasional sexual intercourse,
• If the couple is discordant,
• Genital tract infection, including active sexually transmitted infection including
vaginitis under treatment,
• If the female partner desires assurance that semen was not released into her
vagina,
d) Contraindication
A female condom is contraindicated for females in the following cases:
• Being allergic to latex,
• When it is impossible for the female partner to maintain erection,
• Cannot be used as a replacement for the long-term methods of contraception,
• Women who have sex three or more times a week.
e) Effectiveness
If used correctly, female condoms are 95% effective to protect women against
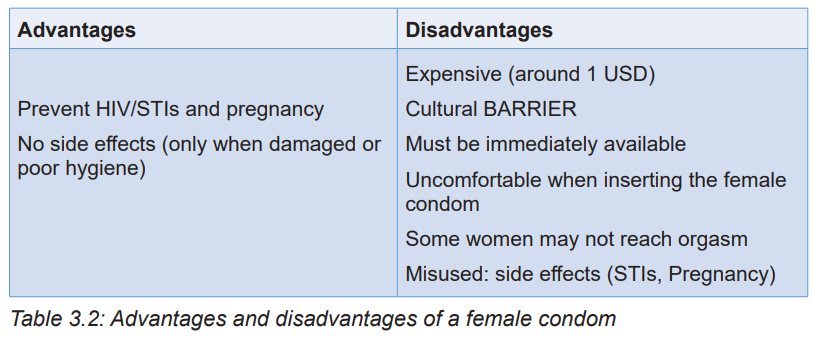
pregnancy and being infected by sexually transmitted infections.f) Advantages and disadvantages of female condom
Self-assessment 3.1.2
a) Briefly explain the female condom as a barrier family planning.b) Describe step by step how the female condom is used.
Homework 3.1
Go to the internet and search for diaphragm contraceptive and write down notesthat will be discussed in the classroom.
3.1.3 Diaphragm
Learning activity 3.1.3
a) Based on the information you have gathered on the internet, answer the
following questions:
b) What is a diaphragm?c) What are advantages of diaphragm as a barrier method of family planning?
Diaphragm is a dome-shaped bowl made of thin, flexible silicone that sits over
the cervix, it covers the cervix before sex and left in place of at least six hours
after sex and prevents sperm passing through the cervix so sperm can’t get in and
fertilize an egg. It is better to use it with a gel that kills sperm (spermicide) that’s whyit is a barrier method of birth control.
a) Indications
The use of diaphragm may be an appropriate method of contraception for women
who prefer an intercourse-related non-hormonal method of contraception and
desire a barrier method that can provide continuous protection for up to 24 hours.
b) Contraindications
Some contraindications to diaphragm use include of the following: allergy to
rubber or latex, repeated urinary tract infections, lack of personnel trained in fitting
diaphragms or of time for proper fitting and instruction, some physical abnormalities,
inability to understand the technique.
c) Advantages and disadvantages
There are the advantages of using diaphragm like when the user like only need to
use a diaphragm when she wants to have sex. She can put it in at a convenient
time before having sex (use extra spermicide if you have it in for more than 3
hours) there are usually no serious associated health risks or side effects.
As for the disadvantages, the diaphragm use has been criticized for the following
deficits:
• Not as effective as other types of contraception as it depends on how the
person using it remembers to use it and using it correctly.
• Does not provide reliable protection against STIs.
• It can also take a time to learn how to use it.
d) Possible side effects
There are some side effects that have been reported by the users including the
following:
• Irritation of the vagina and surrounding skin or an allergic reaction,
• strong odors or vaginal discharge if the diaphragm is left in too long,
• an allergic reaction to the material in the diaphragm,
• a higher risk for urinary tract infections (UTIs),• Risk of toxic shock syndrome if the diaphragm is left in too long.
Self-assessment 3.1.3
a) Who should not use the diaphragm?
b) What are the side effects associated with the use of diaphragm?
c) Mention at least two disadvantages of using diaphragm as a barriermethod?
Learning activity 3.1.4
Watch the video on this link:;
and answer these questions:
a) What is a cervical cap?
b) Under what circumstances should a cervical cap may not be used as a
contraceptive method?
The cervical cap is a one of the temporary birth controls (contraceptive) devices
that prevents sperm from entering the uterus. The cervical cap is a reusable, deep
silicone cap that is inserted into the vagina and fits tightly over the cervix. The
cervical cap is held in place by suction and has a tie to help with removal. It can
insert the cap ahead of time or just before sex and the cap should be left in place for
6 hours after sex. The cervical cap is effective at preventing pregnancy only when
used with spermicide.
c) Tips to inserting the cervical cap in the vagina
Before you use the cervical cap for the first time, practice inserting the cap and
checking its placement.
To use a cervical cap, a woman must:
• Check the position of her cervix before inserting the cervical cap. To
find the cervix, a woman inserts her finger deep into her vagina. The cervix
feels like the tip of your nose. Its position will vary according to the time of themonth and the woman’s body position.
• Apply spermicide. Fill the cervical cap’s bowl with about 1/4 teaspoon (1.25
milliliters) of spermicide. Spread a thin layer of spermicide on the brim of
the cervical cap that faces the cervix. Place 1/2 teaspoon (2.5 milliliters) of
spermicide in the groove between the rim and the dome of the cervical cap.
The woman should avoid removing the cap for at least six hours after the last
time she had sex.
• Insert the cervical cap. Insert the cervical cap into the vagina before sexual
arousal to ensure proper placement. Find a comfortable position, such as
squatting. Separate the labia with one hand. With the other hand, hold the
cervical cap with the bowl facing upward and squeeze the rim of the cervical
cap between your thumb and index finger.
• Slide the cervical cap into the vagina — making sure the taller brim of the
cervical cap enters the vagina first. Push the cervical cap along the rear wall
of the vagina as far as it will go. Use finger to locate the cervix and press the
rim of the cervical cap around the cervix until it is completely covered.
• Always check the cervical cap’s position before sex. Squat, bear down,
insert your finger into your vagina and press upward on the dome to make
sure your cervix is covered. If the cervical cap is not covering your cervix
completely, either push it onto the cervix or remove it and reinsert it.
• Gently remove the cervical cap. After sex, leave the cervical cap in place
for at least six hours and up to two days. To remove the cervical cap, squat,
bear down and rotate the cap. Relax your muscles and push up on the dome
of the cervical cap to break the seal.
• Grasp the removal strap and gently pull. Be careful not to scratch your
vagina. After removal, wash the cervical cap with mild soap and warm water
and let it air-dry. Store the cervical cap in its provided container.
b) Indication
Any woman without current pelvic or cervical infections can use cervical cap.
c) Contraindication
The care provider can discourage the use of cervical cap if the woman has the
following conditions:
• Current history of pelvic, cervical, vaginal, or urinary traction infection;
• intermenstrual bleeding;
• medical procedures to the cervix;
• breast feeding;
• Recently gave birth or had a miscarriage or an abortion
• Recently had cervical surgery
• Have a history of pelvic inflammatory disease, toxic shock syndrome, cervical
cancer, third-degree uterine prolapse, uterine tract infections, or vaginal or
cervical tissue tears
• Have vaginal or cervical abnormalities that interfere with the fit, placement or
retention of the cervical cap
• Are at high risk of pregnancy (women younger than age 30; women who
have sex three or more times a week; women who have had previous
contraceptive failure with vaginal barrier methods; or women who are not
likely to consistently use the cervical cap)
• Are allergic to spermicide or silicone.
d) Advantages and disadvantages
The advantages of using the cervical are the following, it does not affect future fertility
for either the woman or the man. It is used only at the time of sexual intercourse. It
is safe to use while breastfeeding. It is less expensive than hormonal methods of
birth control.
The cervical cap is more difficult for women to learn to insert and remove than the
diaphragm. If worn for more than two days (48 hours), you run the risk of toxic
shock syndrome or unpleasant vaginal odor and discharge.
e) Effectiveness
The cap is 80.4% effective according to the Pearl Index and 89% of the women
are satisfied with using the cap. There is a 51% continuation rate over a 1-year
period. The cervical cap appears to have a satisfactory rate of contraception when
compared with other barrier methods and women are adept at its use.
f) Side effects
The possible side effects may include: from the spermicide, irritation of the vagina
and surrounding skin or an allergic reaction, strong odors or vaginal discharge if the
cap is left in too long, an allergic reaction to the material in the cap and changes inthe cervix because of irritation
Self-assessment 3.1.4
a) Describe how a cervical cap is removed from the woman’s vagina after
sexual intercourse.
b) What are the possible side effects associated with using a cervical cap as
a contraceptive method?
3.2 Permanent contraceptive methods
Learning activity 3.2.1
a) Enumerate the types of permanent methods of family planning you know.
b) What is vasectomy as a permanent contraceptive method?
Permanent contraception involves making a person incapable of reproduction.
Disrupting the tubes that carry sperm or the egg ends the ability to reproduce.
This form of contraception should always be considered permanent, although
the procedures can sometimes be reversed. Normally, permanent contraceptive
methods can only be chosen for individuals and/or couples who have had children
and have decided that their family is complete. Permanent contraceptive methods
encompass vasectomy and tubal ligation. In the next sub-sections, each method isdiscussed in details.
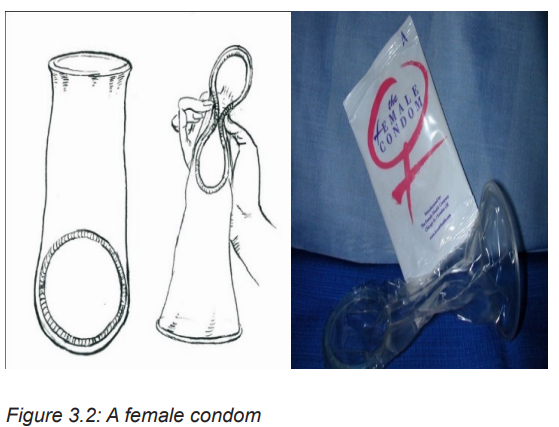
A vasectomy also called male sterilization or male surgical contraception, it is a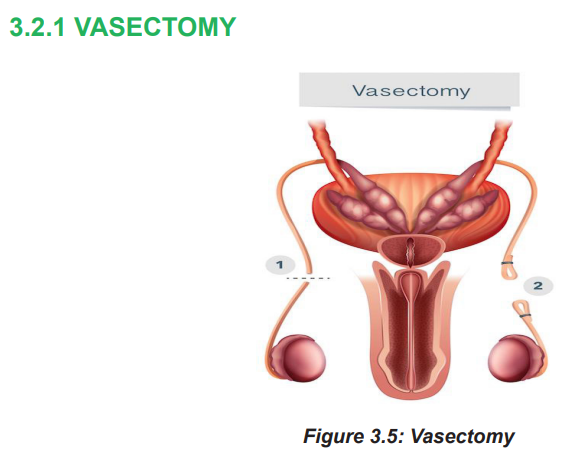
permanent family planning method which is irreversible, it is a simple surgery done
by a doctor in a hospital or clinic. The small tubes in the scrotum that carry sperm are
cut or blocked off, so sperm can’t leave the body and cause pregnancy. Theprocedure is very quick, and the client can go home the same day.
a) Mode of action
A vasectomy blocks or cuts each vas deferens tube, keeping sperm out of the
semen. Sperm cells stay in the testicles and are absorbed by the body. Starting
about 3 months after a vasectomy, the semen won’t contain any sperm, so it can’t
cause pregnancy. But a men will still have the same amount of semen that he did
before.
b) Indications
Some indications are: for men who do not want more children, transection and
occlusion of the vas deferens, no interference with sexual performance
c) Contraindications
There are some contra indications for vasectomy like active STIs, swollen and
tender testes, scrotal skin infection, and bilateral un-descended testes.
d) Advantages of Vasectomy
The following are the advantages of using vasectomy like Safer and more effective
than tubal ligation, Vasectomies don’t change the way having an orgasm or
ejaculating (cumming) feels, Failure is less than 1%.
e) Disadvantages of Vasectomy
The following are some of the disadvantages,
• Does not protect against sexually transmitted infections
• Need use of other contraceptives for 8-12weeks after operation.
• Does not use general Anesthesia.
• It’s non-reversible.
Reason for failure can be:
Unprotected intercourse soon (before azoospermia is documented – approx. 3
months)
Failure to occlude the vas (technical errors)
Recanalization
f) Effectiveness
A vasectomy is one of the most effective kinds of birth control. It’s almost 100%
effective at preventing pregnancy, it takes about 3 months for the semen to become
sperm free.
Although a man can have intercourse two to three days following the procedure,
the vasectomy does not work right away. It takes roughly 3 months for semen to
be entirely clear of sperm. A man or his partner should use another type of family
planning, such as condoms, throughout these three months. Alternatively, if a
woman was already using a family planning method before her partner’s vasectomy,
she can keep using it for another three months before stopping it. A vasectomy isconsidered effective after three months.
Self-assessment 3.2.1
a) How vasectomy works as a permanent contraceptive method?
b) What are indication and contra indication of using the vasectomy?c) What are advantages of vasectomy?
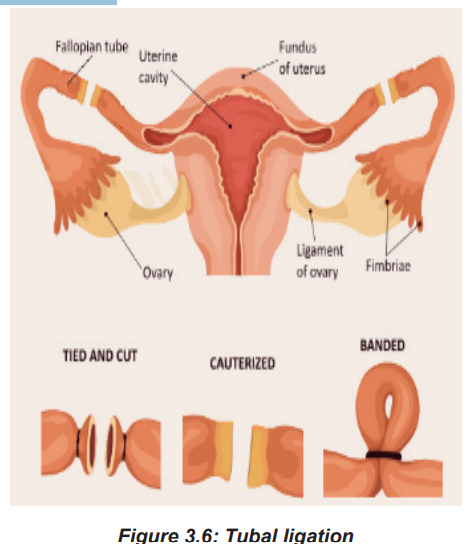
3.2.2 TUBAL LIGATION
Learning activity 3.2.2
a) What is a tubal ligation as a permanent contraceptive method?
b) Who should use the tubal ligation?c) What are advantages of tubal ligation?
A tubal ligation (also known as ‘having your tubes tied’) is a procedure to close bothfallopian tubes which means that sperm cannot get to an egg to fertilize it
a) Indication
The tubal ligation is indicated for women who want a permanent method of
contraception and are free of any gynaecologic pathology that would otherwise
dictate an alternate procedure. It is also indicated for women in whom a pregnancy
could represent a significant clinical and medical risk.
b) Contra indication
Contraindications include indecisive patients, very young age, incapable of making
a medical decision, the presence of gynecological malignancy, and morbidly obese
patient.
c) Side effects
Some women may experience long-term side effects like regret After Sterilization,
Sterilization Failure & Ectopic Pregnancy, Menstrual Cycle Changes, there is also
Post Tubal Ligation Syndrome (hot flashes, chronic fatigue, irregular or heavier
periods, loss of libido, increased depression and/or anxiety, achy, sore joints and/or
muscles, weight gain and memory lapse)
d) Advantages
Tubal ligation’ advantages are the following: permanently prevents pregnancy, so
she no longer need any type of birth control and it does not protect against sexually
transmitted infections. Tubal ligation may also decrease the risk of ovarian cancer,
especially if the fallopian tubes are removed.
e) Disadvantage
Some disadvantages of tubal ligation are the following; it is a permanent and
irreversible method, some people regret having it, especially if their circumstances
change. Tubal ligation does not protect against STIs. Using condoms is the best
way to prevent STIs.
f) The Benefits
Some benefits of tubal ligation are: It works immediately and can be performed
after childbirth, it doesn’t cause hormonal imbalance like other contraceptives,
Eliminates the need to monitor schedules for pills or cycles and it may lower therisk of ovarian cancer.
Self-assessment 3.2.2
a) How does tubal ligation work as a permanent contraceptive method?
b) Who should not use the tubal ligation?c) What are the disadvantages of tubal ligation
End unit assessment 3
I. True (T) or false (F) questions
1. Barrier methods exist only for males.
2. Condoms should be worn after ejaculation.
3. Barrier methods are safe and have no systemic effects.
II. Multiple-choice questions
Choose the correct answer
1. Which methods of birth control needs a prescription?
A. Birth control pill
B. Contraceptive patch
C. Cervical cap
D. all of the above
2. What do male condoms offer that other forms of birth control do not?
A. Least chance of failure
B. Best protection against STIs
C. Cheapest to use
D. All of the above
3. Which type of intrauterine device (IUD) IS available?
A. Copper
B. Titanium
C. Hormonal
D. A and C
4. Which of these methods of sterilization is permanent?
A. Tubal sterilization
B. Implants
C. Vasectomy
D. . A and C
III. Open questions
1. Who should use the male condom as a family planning method?
2. Enumerate advantages and disadvantages of male Condom?
3. Who should not use female condom in family planning method?
4. Enumerate advantages and disadvantages of female Condom?5. What is diaphragm as barrier method?
