Topic outline
UNIT1:GASTRODUODENAL ULCERS
Key Unit competence:Take appropriate decision on Gastro Duodenal Ulcers
Introductory activity 1.0
The image A and B illustrate the structures of stomach and duodenum. Observethem and respond to the attached questions.
1) Is there any difference between the two images (A&B)?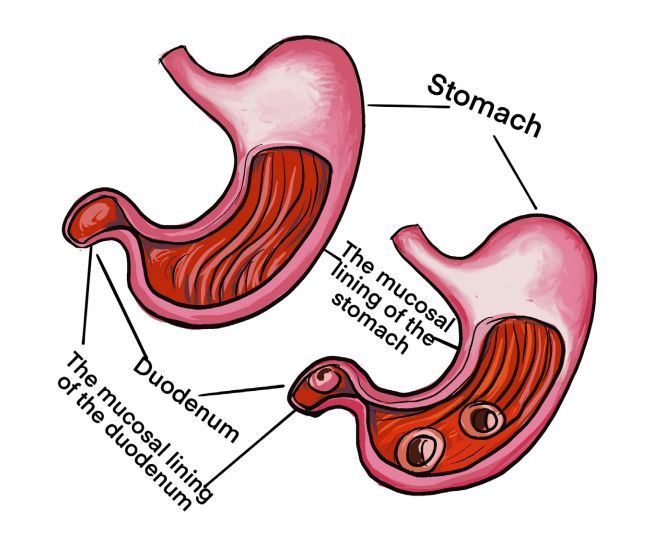
2) What explanations can you give to justify the abnormal structure of
stomach and duodenum?
3) What do you think can cause the modifications that you have observed?
4) What are the manifestations of such abnormalities in the human body?
5) How can health personnel identify or notice these abnormalities of
stomach and duodenum?6) How can these abnormalities be corrected?
1.1. Description of gastroduodenal ulcers
Learning Activity 1.1
S.D is a 47-year-old police officer who lives and works in urban area. Mr. S.D has
now been admitted to the hospital where you are allocated.
*In the past history, Mr. SD has had ‘heartburn’ and abdominal discomfort for
years, but he thought it went along with his job. Last year, after becoming weak,
light-headed and short of breath, he was found to be anemic. He said that he
took omeprazole and ferrous sulfate for 3 months before stopping both, saying
he had ‘never felt better in his life’.
*On today’s initial assessment, S.D is alert and oriented, though very worried
about his condition. Skin pale and cold; BP 136/78, P 98; his abdomen is
distended and tender with hyperactive bowel sounds; he has active upper GI
bleeding as manifested by 200 mL bright red blood obtained on nasogastric tube
that has been inserted.
* The medical doctor is now ordering different diagnostic measures and include
FBC, endoscopy and a biopsy taken from the stomach and duodenum.
*The results of FBC have indicated low Hemoglobin and low hematocrit. Tissue
biopsy obtained during endoscopy confirms the presence of H. pylori infection.
Questions related to the case study
1) Identify the biography of the patient described in the case study
2) What is the medical history of patient described in the case study?
3) Describe the signs and symptoms that the patient present and are
described in the case study
4) What are the aggravating and relieving factors?
5) What is the probable diagnostic method of this S.D?
Learning Activity 1.1
1.1.1. Definition and the Gastroduodenal ulcers
Gastroduodenal ulcers also known as Peptic ulcer (PU) disease is a condition in
which painful sores or ulcers develop in the lining of the stomach or the first part of
the small intestine (the duodenum).
1.1.2. Causes and pathophysiology of Gastroduodenal ulcers
Studies have revealed two main causes of peptic ulcers (PU): Helicobacter pylori
(H. pylori) bacteria and pain-relieving NSAID medications. There are other manyfactors of Peptic ulcers.
Risk factors for peptic ulcer disease
• H. pylori infection,
• Low socioeconomic status Crowded, unsanitary living conditions
• Unclean food or water
• Advanced age
• History of PUD
• Concurrent use of other drugs such as glucocorticoids or other NSAIDs
• Cigarette smoking
• Family history of PUD
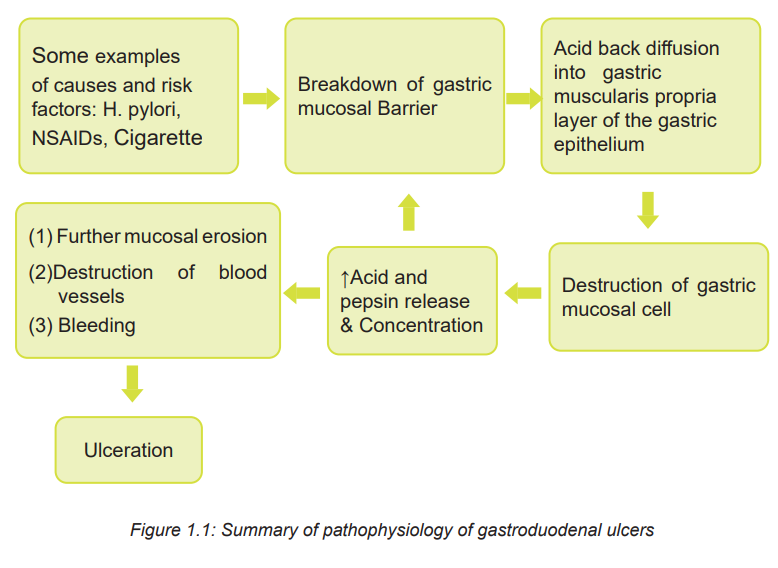
PU disease is characterized by discontinuation in the inner lining of the gastrointestinal
(GI) tract because of an increase in the concentration or activity of gastric acid or
pepsin. It extends into the muscularis propria layer of the gastric epithelium. Some
individuals have more rapid gastric emptying, which, combined with hypersecretion
of acid, creates a large amount of acid moving into the duodenum. As a result, peptic
ulcers occur more often in the duodenum. The Pathophysiology of gastroduodenalUlcer is summarized on the figure 1.1.
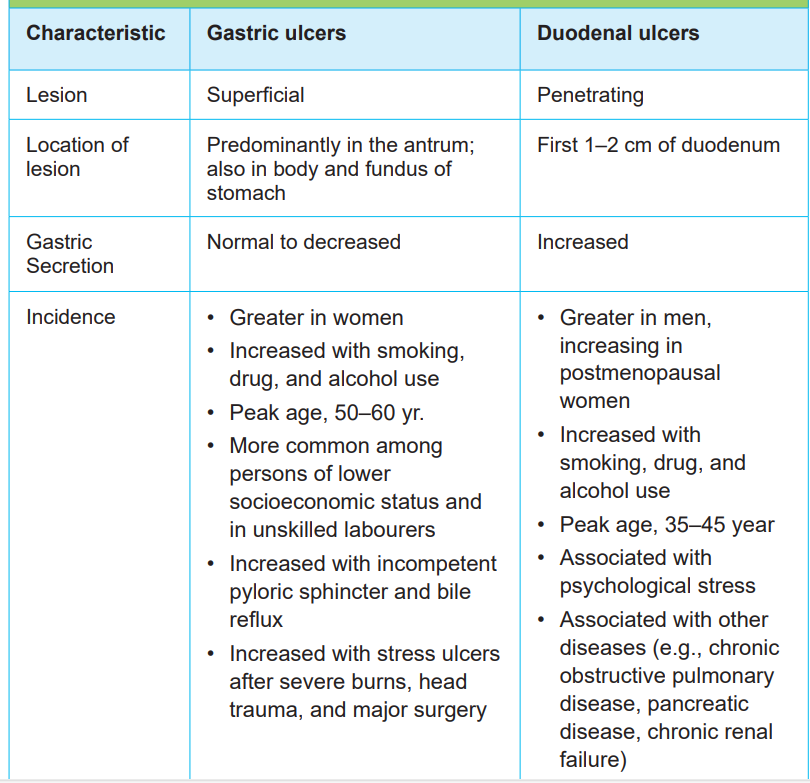
1.1.3. Signs and symptoms of Gastroduodenal ulcers
Some people with ulcers don’t experience any symptoms. But signs of a peptic
ulcer can include burning pain in the middle or upper stomach between meals or
at night. Pain that temporarily disappears if you eat something or take an antacid,
bloating, heartburn, nausea or vomiting.
In severe cases, symptoms can include dark or black stool (due to bleeding),
vomiting, weight loss, severe pain in the mid to upper abdomen. Table 1.1 comparesthe characteristics of duodenal and gastric ulcers
Table 1.1: COMPARISON OF GASTRIC AND DUODENAL ULCERS
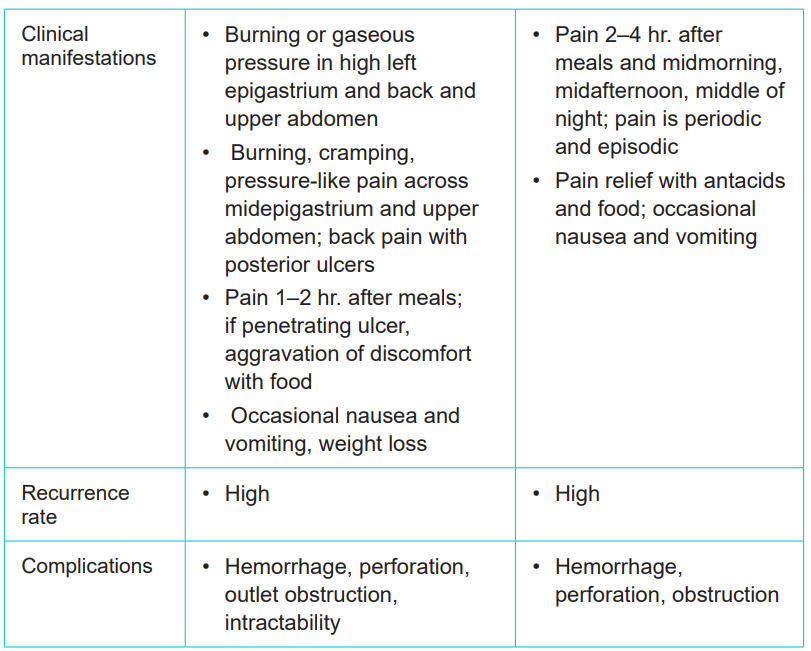
1.1.4. Diagnostic measures
The gastroduodenal ulcers can be diagnosed through a complete history, physical
examination, Complete Blood Cell Count (CBC), upper gastrointestinal endoscopy
with biopsy, Helicobacter pylori testing. Endoscopy is the most accurate diagnostic
procedure and allows for direct viewing of the gastric and duodenal mucosa
(Fig.1.2).
The Complete blood cell count may indicate low level of Hb and Ht due to chronic
bleeding. Helicobacter pylori results are referred to as positive or negative.
Differential diagnostic includes acute choleritiasis, cholique syndrome, myocardialinfection
Figure 1.2: Esophagogastroduodenoscopy (EGD) directly visualizes the mucosal lining of the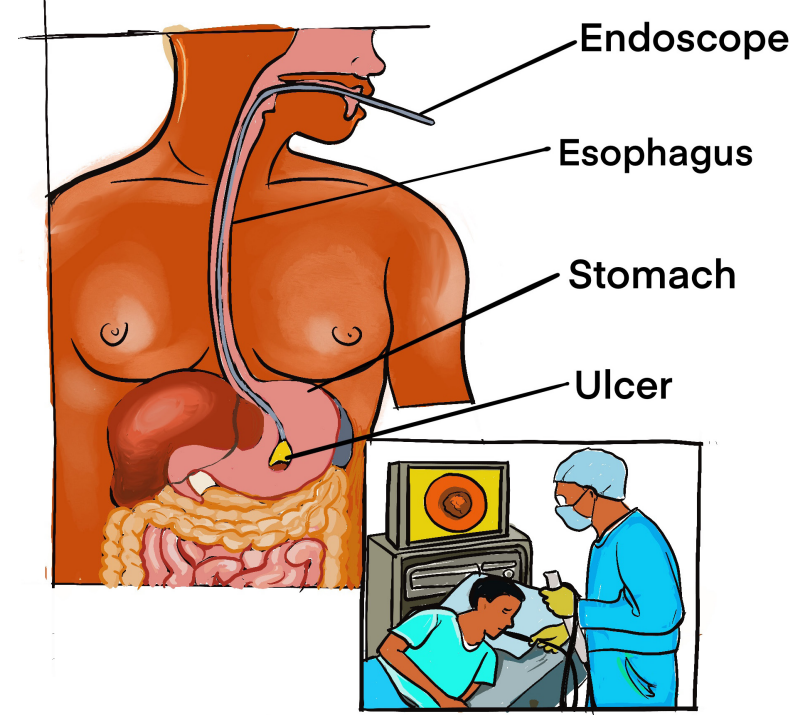
stomach with a flexible endoscope. Ulcers or tumors can be directly visualized and biopsies taken.(Lewis et.al 2012)
Self-assessment 1.1
Briefly explain the pathophysiology of gastroduodenal ulcers?
Identify other diseases that would mimic the symptoms of gastroduodenal ulcers?How would reduce the anxiety of the patient caused by the fear of endoscopy?
1.2. The management of gastroduodenal ulcers
Learning Activity 1.2
…Continuation of S.D case study
After different investigations, the medical doctor confirmed that the police officer
Mr. S.D is suffering from Gastroduodenal ulcers. Regarding the treatment,
Mr. S.D has received two units of packed RBCs and intravenous fluids. Oral
omeprazole (40 mg BID) was ordered and when he was in endoscopy they
managed to stop the bleeding.
Questions related to the case study
1) What is the surgical treatment plan adopted by the medical doctor for this
patient?
2) In group discuss the different medication prescribed to this patient3) List potential complications which may happen to this police officer
1.2.1. The treatment plan of Gastroduodenal ulcers
Medications to treat peptic ulcer include:
• Proton pump inhibitors (PPI): These drugs reduce acid, which allows the ulcer
to heal (e g: nexium).
• Histamine receptor blockers (H2 blockers): These drugs also reduce acid
production (e g: Tagamet).
• Antibiotics: These medications kill bacteria (e g:Amoxicillin).
• Protective medications: Like a liquid bandage, these medications cover the
ulcer in a protective layer to prevent further damage from digestive acids and
enzymes (e g: Carafate).
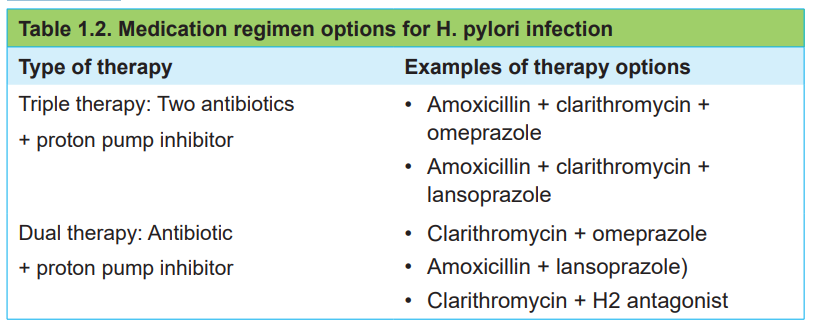
• Several treatment options are combined to cure H. pylori without recurrence.
Triple therapy has the best eradication rate
• Endoscopy procedure treatment:
• Doctor may treat peptic ulcers during an endoscopy procedure by injecting
medications
• Doctor can also use a clamp or cauterization (burning tissue) to seal it off and
stop the bleeding.
To eradicate the H pylori infection dual or triple therapy is recommended as indicatedin table 1.2.
1.2.2. Associate nurse decision making
In the hospital, the associate nurse will perform tasks that are delegated by
registered nurses. The primary focus of care for peptic ulcer disease is educating
patients. The teaching guide will include detail the following:
– Describe dietary modifications
– Explain the rationale for avoiding cigarettes
– Emphasize the need to reduce or eliminate alcohol ingestion
– Explain the rationale for avoiding OTC drugs unless approved by the
patient’s health care provider.
– Explain the rationale for not interchanging brands of antacids and
– H2-receptor blockers that can be purchased OTC without checking with
the health care provider Emphasize the need to take all medications as
prescribed
– Explain the importance of reporting any of the following:
– Describe the relationship between symptoms and stress. Stress reducing
activities and relaxation strategies are encouraged.
– Encourage patient and caregiver to share concerns about lifestyle changesand living with a chronic illness.
1.2.3. Complications of gastroduodenal ulcers
Perforation, abscess of the appendix, and peritonitis are major complications of
gastroduodenal ulcer. With perforation, the pain is severe, and temperature iselevated to at least 37.7°C.
Self-assessment 1.2
Mr. S.M a patient on your department unit, has a duodenal ulcer. His wife runs to
the nursing station and says that you need to help her husband, he is in terrible
pain. As you enter the room, you see Mr. SM bent knee-to-chest position on the
bed. He is crying and says he has excruciating abdominal pain.
1) What additional data would you gather?
2) What emotional support would you offer to Mrs. SM?
3) After orders are obtained, what actions will you anticipate implementingunder supervision
1.3 End unit assessment
End of unit assessment
1) What are the most frequent symptoms of Gastroduodenal ulcers?
2) What are the diagnostic measures of Gastroduodenal ulcers?
3) The nurse is teaching the client and her family about possible causes of
peptic ulcers. How does the nurse explain ulcer formation? Choose the
best answer.
a) Caused by a stressful lifestyle and other acid-producing factors such as
Helicobacter pylori
b) Inherited within families and reinforced by bacterial spread of
Staphylococcus aureus in childhood
c) Promoted by factors that tend to cause over secretion of acid, such as
excess dietary fats, smoking, and H. pylori
d) Promoted by a combination of possible factors that may result in erosion
of the gastric mucosa, including certain drugs and alcohol
4) Duodenal and gastric ulcers have similar as well as differentiating features.
What are characteristics unique to duodenal ulcers (select all that apply)?
a) Pain is relieved with eating food.
b) They have a high recurrence rate.
c) Increased gastric secretion occurs.
d) Associated with Helicobacter pylori infection.
e) Hemorrhage, perforation, and obstruction may result.
f) There is burning and cramping in the midepigastric area.
5) What are the dietary modifications would you recommend a patient withgastroduodenal ulcers?
UNIT2:APPENDICITIS
Key Unit competence:
Take appropriate decision on appendicitisIntroductory activity 2.0
Observe the images A and B below illustrating the structures of appendix inhuman body.
1) Is there any difference between two appendixes?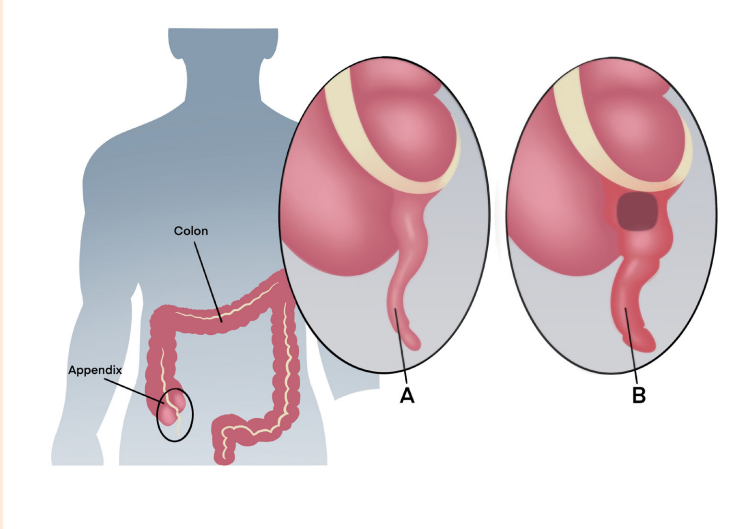
2) Which one of these two would reflect the normal structure of appendix in
the human body?
3) Describe the abnormalities that you have observed.
4) What do you think can cause the abnormalities that you have observed?
5) What are the manifestations of the observed abnormalities in the human
body?
6) How can health personnel identify these abnormalities?7) How can these abnormal structures be corrected?
2.1. Description of appendicitis
Learning Activity 2.1
M.H, a-13-year-old boy with history of constipation comes into the emergency
of referral hospital for severe abdominal pain. M.H reports that his abdomen
hurts for the past 24 hours. He notes that he initially suffered from mild pain
around his umbilicus last night and this morning he reported that the pain has
migrated to his right lower quadrant. He tells the nurse that the pain just keeps
getting worse and it is associated with nausea, vomiting and fever (39 degrees
Celsius). Upon physical assessment, M.H doesn’t allow anyone auscultate
or palpate his abdomen because of the pain. After 10 minutes he allowed the
nurse to do physical assessment. He is quite tender to mild palpation in the
right lower quadrant and he has muscle guarding. M.H prefers to lie still with the
right leg flexed. The medical doctor ordered blood sample to check the number
of WBCs. He also ordered ultrasound and CT scan. The blood test revealed
elevated WBC and neutrophil counts. An ultrasound and computed tomography
(CT) scan revealed an enlargement in the area of the cecum and appendicitis
was confirmed. Based on the case study narrated above, answer to the followingquestions.
Questions related to the case study
1) Identify the biography of M.H
2) What is the medical history of M.H?
3) Describe the signs and symptoms of M.H
4) What are the aggravating and relieving factors for M.H?5) What are the differential diagnosis M.H?
2.1.1. Definition of appendicitis
Appendicitis is inflammation of the appendix, a narrow blind tube that extends
from the inferior part of the cecum. Appendicitis, inflammation of the vermiform
appendix, is a common cause of acute abdominal pain and most common reason
for emergency abdominal surgery. It occurs at any age, but it is more common in
adolescents and young adults and slightly more common in males than females
2.1.2. Causes and pathophysiology of appendicitis
Because of the small size of the appendix, obstruction may occur, causing
inflammation and making it susceptible to infection. The obstruction is often caused
by a faecalith or hard mass of faeces. Other obstructive causes include a calculus
or stone, a foreign body, inflammation, a Tumor, parasites (e.g. pinworms) or
oedema of lymphoid tissue. Hereditary and family tendencies of appendicitis have
been noticed. Following obstruction, the appendix distends with fluid secreted by
its mucosa. As pressure within the lumen of the appendix increases, blood supply
is impaired, leading to inflammation, edema, ulceration and infection.
2.1.3. Signs and symptoms of appendicitis
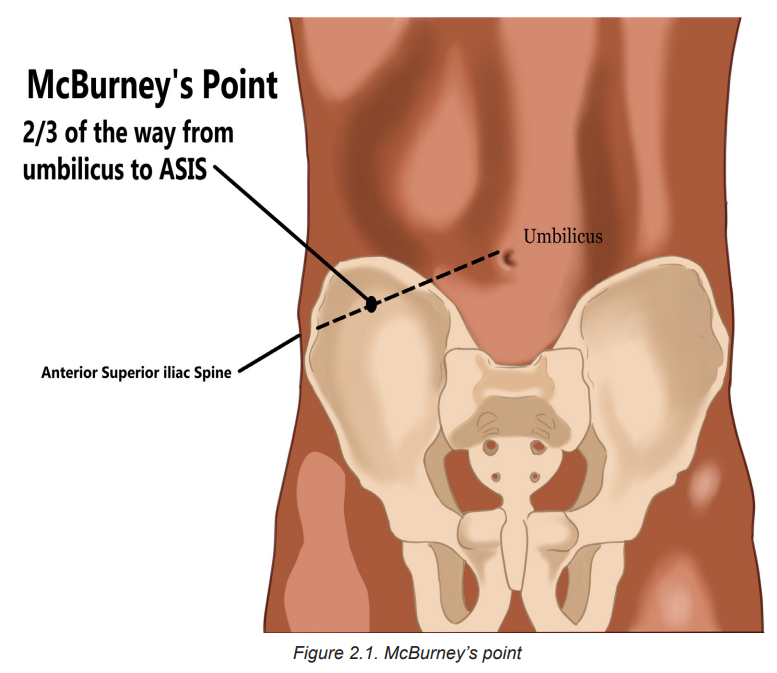
Signs and symptoms of appendicitis include fever, generalized pain in the upper
abdomen. Within hours of onset, the pain usually becomes localized starts on the
periumbilical area to the right lower quadrant at McBurney’s point, midway between
the umbilicus and the right iliac crest. This is one of the classic symptoms of
appendicitis. Nausea, vomiting, and anorexia are also usually associated. Physical
examination reveals slight abdominal muscular rigidity (guarding), normal bowel
sounds, and local rebound tenderness (intensification of pain when pressure is
released after palpation) in the right lower quadrant of the abdomen. The pain is
aggravated when patient straightens the leg, coughs, walks and makes any shaking
movement. The patient may keep the right leg flexed for comfort.
! Consideration for practice
• Sudden relief of preoperative pain may signal rupture of the distended and
edematous appendix.
• Assess abdominal status frequently, including distension, bowel sounds and
tenderness: Increasing generalized pain, a rigid, boardlike abdomen andabdominal distension may indicate developing peritonitis.
2.1.4. Diagnostic measures
The appendicitis can be diagnosed through a complete history, physical examination,
and a differential WBC count. The WBC count is mildly moderately elevated in most
cases. CT scan is the preferred diagnostic procedure, but ultrasound is also used. A
urinalysis is done to rule out genitourinary conditions that mimic the manifestations
of appendicitis. Other differential diagnostic includes intestinal obstruction,
inflammation and stones of gall bladder, stones in urinary organs such as ureter,
ruptured ovarian follicle, a ruptured tubal pregnancy, perforation of stomach orduodenal ulcer and inflammation of the right colon
Self-assessment 2.1
1) Who are people most likely to develop appendicitis?
2) Among the cells of WBC, which ones would increase in case ofappendicitis?
2.2. The management of appendicitis
Learning Activity 2.2
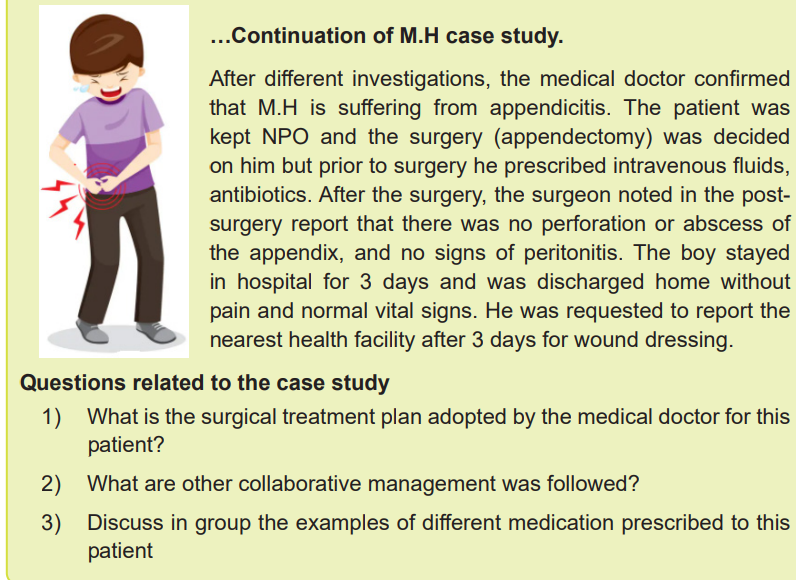
2.2.1. The treatment plan
The patient is kept NPO, and surgery (check appendectomy collaboration care in
box 2.1) is done immediately unless there is evidence of perforation or peritonitis.
Medications prior to surgery, intravenous fluids are given to restore or maintain
vascular volume and prevent electrolyte imbalance. Antibiotic therapy with a third
generation cephalosporin effective against many gram-negative bacteria, such as
cefotaxime (Cefotaxime Sandoz), ceftazidime (Fortum) or ceftriaxone (Rocephin)
is initiated prior to surgery. The antibiotic is repeated during surgery and continued
for at least 48 hours postoperatively. Post-operative analgesic medications are
administered as prescribed.
Following an uncomplicated appendectomy, the person is often discharged either
the day of, or the day following, surgery. Postoperative teaching includes:
• Wound or incision care, including hand hygiene and dressing change
procedures as indicated.
• Instructions to report fever, increased abdominal pain, swelling, redness,drainage, bleeding or warmth of the operative site to the doctor.
• Activity limitations (e.g. lifting, driving), if any.
• When it is appropriate to return to work.Summary of appendectomy care is indicated in table 2.1
2.2.2. Associate nurse decision making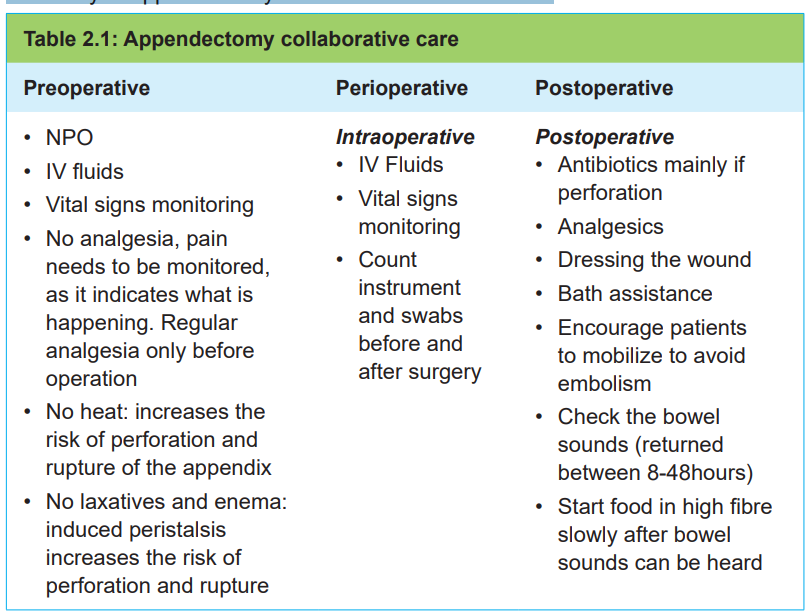
An associate nurse who receives a patient with signs and symptoms of appendicitis
must refer the case to the next level for adequate management. In the hospital, the
associate nurse works under supervision of registered nurses and they will discuss
the appropriate nursing care plan.
2.2.3. Complications of appendicitis
Most patients recover quickly after an appendectomy and frequently are discharged
from the hospital after few days. Preventing complications during the perioperative
period is a primary nursing care goal. Perforation and peritonitis are the most likely
preoperative complications. With perforation, the pain is severe, and temperature is
elevated to at least 37. 7°C. Postoperative complications include wound infection,abscess and possible peritonitis.
Self-assessment 2.2
1) What is the rationale of avoiding the use of warm/heating pads to relieve
the pain resulting from appendicitis?2) Explain the treatment options for a patient with appendicitis
2.3. End unit assessment
End of unit assessment
1) Within hours of onset, the pain of appendicitis usually becomes localized
starts on the ___________ area to the ___________ quadrant.
2) What are the diagnostic measures of appendicitis?
3) The patient has persistent and continuous pain at McBurney’s point. The
nursing assessment reveals rebound tenderness and muscle guarding
with the patient preferring to lie still with the right leg flexed. What should
the nursing interventions for this patient include? Choose the best answer
a) Laxatives to move the constipated bowel
b) NPO status in preparation for possible appendectomy
c) Parenteral fluids and antibiotic therapy for 6 hours before surgery
d) NG tube inserted to decompress the stomach and prevent aspiration
4) Appendicitis may occur:
a) After complications of an episode of flu
b) After complications of a viral infection of the digestive
c) After opening to the appendix becomes blocked by stool
d) After an enema to evacuate the stool
5) If you suspect the appendicitis, what type of medicine should you not
take?
a) Analgesics
b) Laxatives
c) Anti-inflammatory
d) Allergy medicines
6) BA 19-year-old student in her second year of a dental degree. BA arrives
at the emergency department at 0200hrs. She presents a general lower
abdominal pain which started the previous evening. She is also nauseated
and reports episodes of vomiting. The physical assessment reveals the
T 37. 8 o C, R 16, BP 110/70; abdomen flat and guarded. BA WBC was
14000/mm3
.
a) What are the missing characteristics/features of the abdominal pain to
confirm appendicitis?
b) What are the disturbed needs of BA?
c) Is appendectomy indicated for this patient? Justify your response7) List the complications of appendicitis
UNIT3:INTESTINAL OBSTRUCTION
Key Unit competence:
Take appropriate decision on intestinal obstruction
Introductory activity 3.0
Observe the segments of the intestines presented in figure A, B, C and D andrespond to the questions below.
1) What do you think is happening to these segments of the intestines?
2) Is there any difference between four figures? Describe the differences
observed.
3) Reference to what you leant in anatomy and physiology, what are the
implications of such structures on food digestion?
4) What are other manifestations of such structures to the human body?
5) How can health personnel identify these structures?6) How can these segments be corrected?
3.1. Description of intestinal obstruction
Learning Activity 3.1
L.A, a 59-year-old woman was brought to the hospital with a 3-day history of
complete constipation and faeculent vomiting. She had no other medical or
surgical history and was not taking any regular medications. She lived at home
with sister and required assistance with several activities of daily living, however,
she was able to eat oh her own. On examination, her abdomen was extended
and mildly tender in the right iliac fossa, but there was no guarding or peritonism.
Chest and cardiac examination revealed tachycardia (115bpm), BP 139/102
mmHg, RR 18, T0 37.10C and saturation 98% on room air. The medical doctor
prescribed the following investigations: blood sample, abdomen x-rays and CT
scan. The results showed an increase of WBCs, urea and creatinine. A relatively
gasless abdomen with few dilated loops of small bowel was observed in the
results of X-rays. The CT scan showed small bowel obstruction within the mid
small bowel loop with the possibility of ischaemia of the small bowel loop. Therewas no evidence of bowel operation.
Questions related to the case study
1) What is the intestinal obstruction?
2) Briefly describe the pathophysiology of intestinal obstructions
3) What are the key signs and symptoms of intestinal obstructions highlightedin the case study?
3.1.1. Definition of intestinal obstruction
Intestinal obstruction occurs when the contents of intestines fail to pass through the
bowel lumen. The obstruction may take place in both small or large intestines and
can be partial or complete.
3.1.2. Causes and pathophysiology of intestinal obstruction
The two types of intestinal obstruction are mechanical and non-mechanical.
Mechanical obstruction occurs when a blockage occurs within the intestine from
conditions causing pressure on the intestinal walls such as adhesions (B), twisting
or volvulus (C) of the bowel, intussusception (D), or strangulated hernia (A). Non
mechanical obstruction may result from a neuromuscular or vascular disorder.
Paralytic ileus (lack of intestinal peristalsis and bowel sounds) is the most common
form of non-mechanical obstruction.
When an obstruction occurs, fluid, gas, and intestinal contents accumulate proximal
to the obstruction, and the distal bowel collapses.
The proximal bowel becomes increasingly distended, and intraluminal bowel
pressure rises, leading to an increase in capillary permeability and extravasation of
fluids and electrolytes into the peritoneal cavity.
This accumulation of fluids in intestines and in peritoneal cavity causes a severe
reduction in circulating blood volume, hence hypotension, hypovolemic shock and
bowel ischemia.
When the distension is severe the segment of the bowel becomes gangrenous a
condition known as intestinal strangulation or intestinal infarction (figure 3.1)
If it is not corrected quickly, the bowel will rupture, leading to infection, septic shock,
and death. If the obstruction is below the proximal colon or in the large bowel which
is less common and not usually as dramatic as small-bowel obstruction, dehydration
occurs more slowly because of the colon’s ability to absorb fluid and distend well
beyond its normal full capacity.
If the blood supply to the colon is cut off, the patient’s life is in jeopardy because ofbowel strangulation and necrosis
3.1.3. Signs and symptoms of intestinal obstruction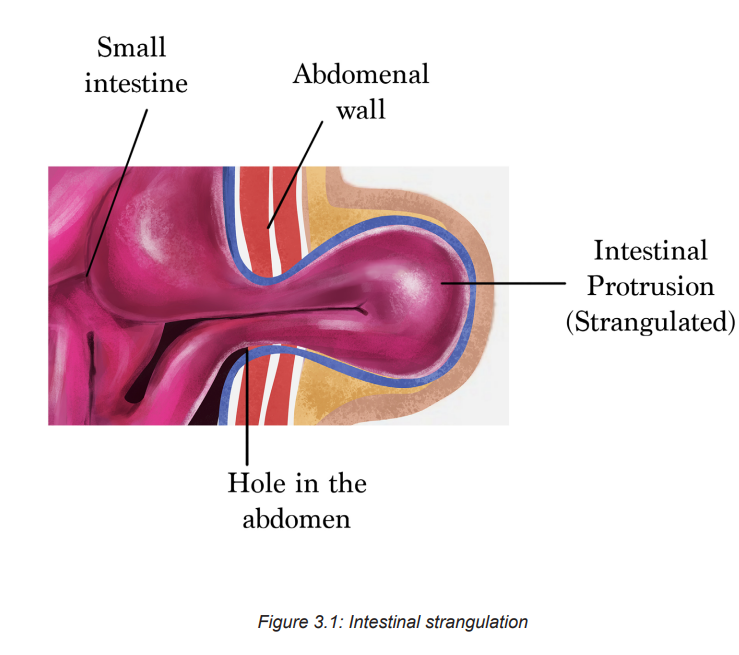
The clinical manifestations of intestinal obstruction vary, depending on its locationas displayed in table
! Consideration for practice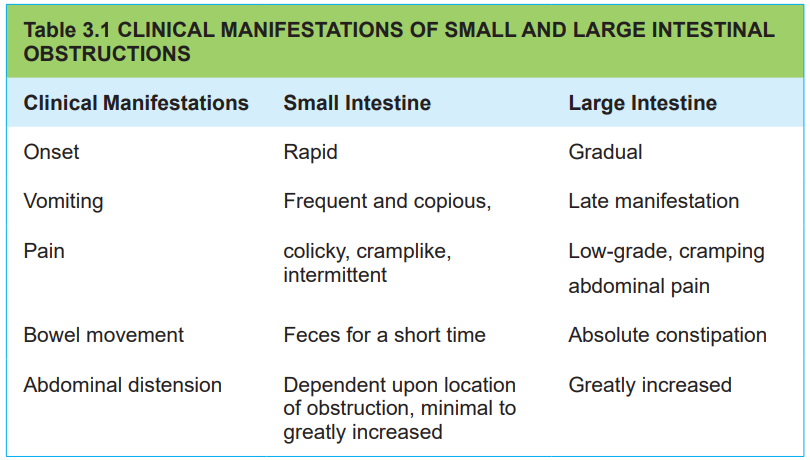
• Abdominal tenderness and rigidity are usually absent unless strangulation or
peritonitis has occurred.
• Auscultation of bowel sounds reveals high-pitched sounds above the area of
obstruction. Bowel sounds may also be absent.
• The patient often notes borborygmi (audible abdominal sounds produced by
hyperactive intestinal motility).
• The patient’s temperature rarely rises above 37.8° C unless strangulation or
peritonitis occurs.
• Promptly report any acute increase in abdominal, groin, perineal or scrotal
pain.
• An abrupt increase in the intensity of pain may indicate bowel ischaemia due
to strangulation.
3.1.4. Diagnostic measures of intestinal obstruction
A thorough history and physical examination. CT scans, abdominal x-rays,
Sigmoidoscopy or colonoscopy may provide direct visualization of an obstruction in
the colon. A FBC and blood chemistries may be performed. An elevated WBC count
may indicate strangulation or perforation. Elevated haematocrit values may reflect
hemoconcentration. Decreased hemoglobin and hematocrit values may indicate
bleeding from a neoplasm or strangulation with necrosis. Serum electrolytes, BUN,and creatinine are monitored frequently to assess the degree of dehydration.
Self-assessment 3.1
1) List different exams performed in order to diagnose intestinal obstruction
condition
2) What is the indication of frequent monitoring of electrolytes, BUN andcreatinine on patient suffering of intestinal obstruction?
3.2. The management of intestinal obstruction
Learning Activity 3.2
…Continuation of L.A case study
After different investigations, the medical doctor confirmed that LA is suffering
from intestinal obstruction. Intravenous catheter was inserted and IV fluids
administered; a decompressive nasal gastric tube was put in place and later
alone patient was taken to the theatre for surgery.
A laparotomy was performed and proved to be a single potato, measuring 4×3cm,
swallowed without chewing. The potato was extracted. In post-operative, the
medical doctor prescribed antibiotics, anti-emetics and pain control medications
and the patient was recovered well with no complications. The patient was
discharged with written letter to her sister regarding dietary advice. The patient
was subsequently followed up 8 weeks postoperatively and she was well.
Questions related to the case study1) What is the pre and post-operative treatment plan of Mrs. L.A?
3.2.1. The treatment plan of intestinal obstruction
The management of a bowel obstruction focuses on relieving the pressure and
obstruction and providing supportive care. The intestine is decompressed by NG
tube insertion and keeping the patient.Nothing by mouth (NPO), the dehydration
and electrolytes imbalances are corrected by administering fluid and electrolytes.
Surgery may be necessary to relieve a mechanical obstruction or if strangulation
is suspected. In post-surgery mouth care is performed, medications such as
antibiotics, antiemetics, and analgesics are administered. A teaching plan is also
elaborated.
Include the following topics when teaching a person with intestinal obstruction in
preparation for home care:
• Wound care
• Activity level,
• Return to work and any other recommended restrictions
• Recommended follow-up care
• Recurrent obstructions, explain their cause, early identification ofmanifestations and possible preventive measures.
3.2.2. Associate nurse decision making
An associate nurse who receives a patient with signs and symptoms of intestinal
obstruction must refer the case to the next level for adequate management. In the
hospital, the associate nurse works under supervision of registered nurses and
they will discuss the appropriate nursing care plan.
3.2.3. Complications of intestinal obstruction
Small intestines obstructions: Hypovolaemia and hypovolaemic shock with
multiple organ dysfunction is a significant complication of bowel obstruction and
can lead to death. Renal insufficiency from hypovolaemia leads to acute kidney
injury or dysfunction. Pulmonary ventilation may be impaired because abdominal
distension elevates the diaphragm, impeding respiratory processes. Strangulation
associated with incarcerated hernia or volvulus impairs the blood supply to the
bowel. Gangrene may rapidly result, causing bleeding into the bowel lumen and
peritoneal cavity and eventual perforation. With perforation, bacteria and toxins
from the strangulated intestine enter the peritoneum and, potentially, the circulation,
resulting in peritonitis and possible septic shock. Strangulation greatly increases
the risk of mortality.
Large intestines: If the ileocaecal valve between the small and large intestines is
competent, distension proximal to the obstruction is limited to the colon itself. This
is known as a closed-loop obstruction. It leads to massive colon dilation as the
ileum continues to empty gas and fluid into the colon. Increasing pressure within
the obstructed colon impairs circulation to the bowel wall. Gangrene and perforationare potential complications
Self-assessment 3.2
Mrs. LS is admitted for abdominal pain. She has a history of abdominal surgery.
Her abdomen is distended, firm, and tender to touch. She states that she feels
nauseated.
1) Is Mrs. L.S at risk for developing an intestinal obstruction?
2) How would the nurse know if Mrs. LS is at risk of developing a small bowel obstruction?
3.4. End of unit assessmentEnd of unit assessment
1) What are the common causes of intestinal obstruction?
2) What are the most common types of intestinal obstructions?3) What are the predicted complications on patient with intestinal obstruction?
UNIT4:HERNIAS
Key Unit competence:
Take appropriate decision on Hernia
The below images illustrate different structures including esophagus, stomach,
diaphragm (A, B, C) umbilicus (D) and inguinal area (E). Observe them andrespond to the questions attached.
1) Identify normal and abnormal structures among the images above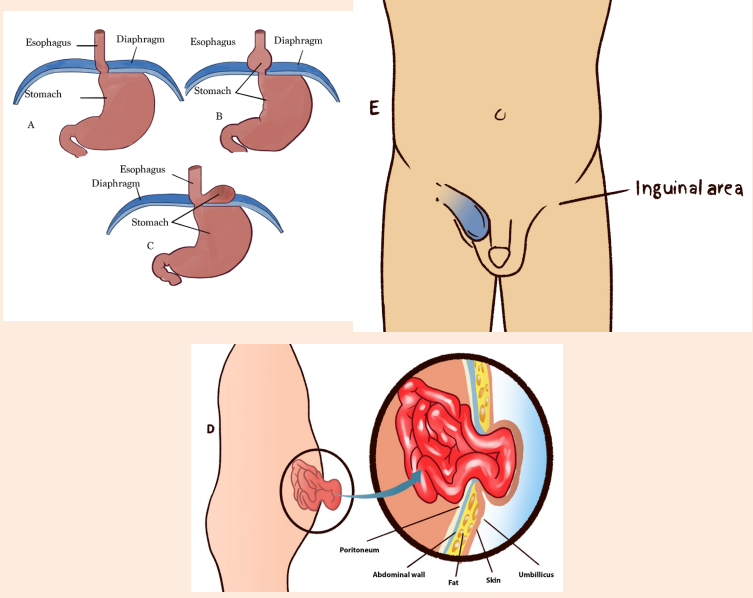
2) What is the common characteristic of the abnormal structures?
3) What could be the causes of such abnormalities?
4) What are the manifestations of such abnormalities in the human body?
5) How can health personnel identify or notice these abnormalities?6) How can these abnormalities be corrected?
4.1. Abdominal hernias
Learning Activity 4.1
Mr. Y.A. 65 years old male, a laborer in a sawmill with low socioeconomic status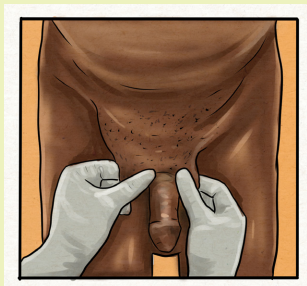
visits the hospital with chief complaints of swelling of about 10cm in right groin
since 3 years and pain in the right groin since 6 months. In the history, patient
was apparently well 3 years back, he noticed a swelling in right groin while
coughing which was initially small size (3cm) gradually increasing to present
size and reaching up to the scrotum. Mr. Y.A states that the swelling increases
when standing, coughing and lifting heavy weights. It decreases on lying down
and disappear on manipulation (pushing it using his fingers). Y.A has a history of
chronic cough with sputum since 20years but no history of chronic constipation
or urinary problems. Mr. Y.A is a known case of COPD on bronchodilators since
20 years, has habit of smoking, non-alcoholic, non-vegetarian diet, bowel and
bladder habits-regular. No history of similar history in his family. He regular takes
levasalbutamol inhaler since 20 years. No history of any allergy. On physical
examination; normal vital signs, a swelling of size 6x3cm is present above and
medial to the pubic tubercle extending into the scrotum up to upper pole of right
testis.
After taking history and performing physical exam, the health personnel confirmedinguinal hernia and planned a surgical treatment.
Questions related to the case study.
1) Based on the history of Y.A, what are the contributing factors of inguinal
hernia?
2) What are the signs and symptoms of inguinal hernia?
3) How inguinal hernia be diagnosed?4) What is the treatment adopted by the health personnel?
4.1.1 Definition of abdominal hernias
A hernia is an abnormal protrusion of an organ or structure through a weakness or
tear in the wall of the cavity normally containing it. Abdominal hernias are defined
as the abnormal protrusion of intra-abdominal contents through congenital/acquiredareas of weakness in the abdominal wall
4.1.2 Types of abdominal hernias
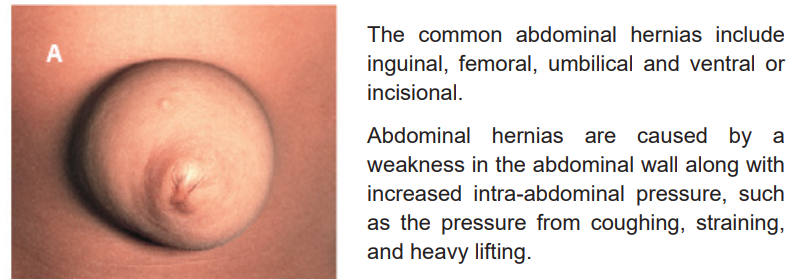
Ventral or incisional hernias are due to weakness of the abdominal wall at the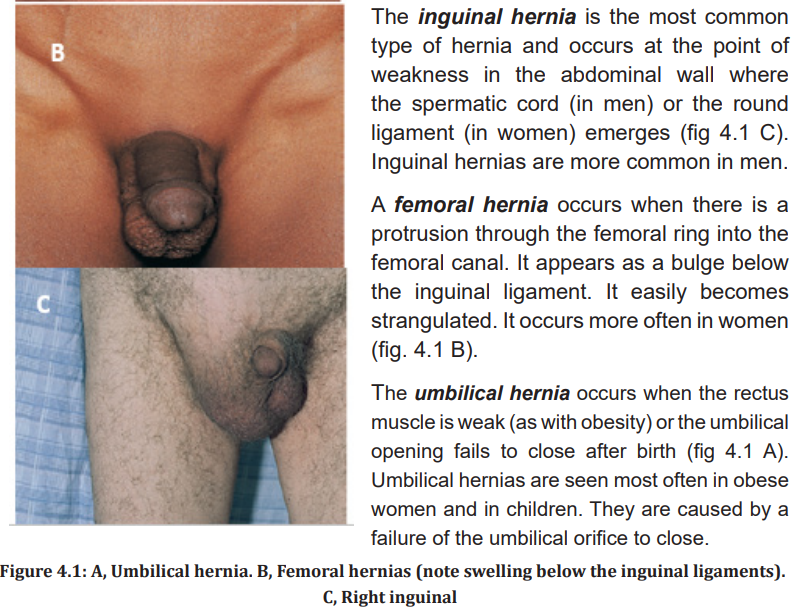
site of a previous incision (fig 4.2). They occur most commonly in patients who
are obese, have had multiple surgical procedures in the same area, or have hadinadequate wound healing because of poor nutrition or infection.
Hernias that easily return to the abdominal cavity are called reducible. The hernia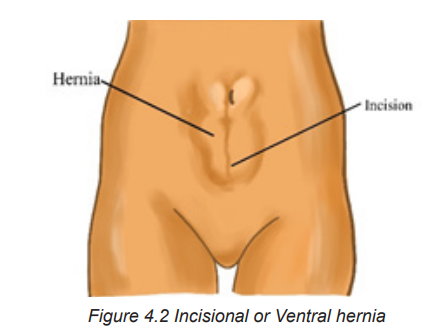
can be reduced manually or may reduce spontaneously when the person lies down.
If the hernia cannot be placed back into the abdominal cavity, it is known as irreducible
or incarcerated. In this situation the intestinal flow may be obstructed. When the
hernia is irreducible and the intestinal flow and blood supply are obstructed, the
hernia is strangulated. The result is an acute intestinal obstruction.
4.1.3 Clinical manifestations of abdominal hernias
An abdominal hernia may be readily visible; an abnormal bulging can be seen in
the affected area of the abdomen, especially when straining or coughing. There
may be some discomfort as a result of tension. If the hernia becomes strangulated,
the patient will have severe pain and symptoms of a bowel obstruction such as
vomiting, cramping abdominal pain, and distention. Strangulated hernias are painful
and inflamed hernias that cannot be reduced, they require emergency surgery.
4.1.4. Diagnostic measures
Abdominal hernias are mainly diagnosed based on history, physical examination
and ultrasound.
4.1.5 Therapeutic Measures
Treatment options include no treatment, observing the hernia, using short-term
support devices, or surgery to cure the hernia. A supportive truss or brief applies
pressure to keep the reduced hernia in place. Emergency surgery is needed for
strangulation or the threat of bowel obstruction. Surgical repair is recommended
for inguinal hernias. Surgical procedures are most often done laparoscopically
and include hernioplasty (open or laparoscopically) or herniorrhaphy (open hernia
repair).
Herniorrhaphy involves making an incision in the abdominal wall, replacing the
contents of the hernial sac, sewing the weakened tissue, and closing the opening.
Hernioplasty involves replacing the hernia into the abdomen and reinforcing the
weakened muscle wall with wire, fascia, or mesh. Bowel resection or a temporary
colostomy may be necessary if the hernia is strangulated.
Postoperative Care
Care following inguinal hernia repair is generally similar to any abdominal
postoperative care. Patients can perform deep breathing to keep lungs clear
postoperatively but should avoid coughing. Coughing increases abdominal
pressure and could affect the hernia repair. Teach patients to splint the incision
and keep their mouths open when coughing or sneezing are unavoidable. The
male patient may experience swelling of the scrotum. Ice packs and elevation of
the scrotum may be ordered to reduce the swelling. Because most patients are
discharged the same day of surgery, they are taught to change the dressing and
report difficulty urinating, bleeding, and signs and symptoms of infection, such as
redness, incisional drainage, fever, or severe pain. The patient is also instructed to
avoid lifting, driving, or sexual activities for 2 to 6 weeks. Most patients can return
to nonstrenuous work within 2 weeks.
After a hernia repair, the patient may have difficulty voiding. Measure intake and
output and observe for a distended bladder. Scrotal edema is a painful complication
after an inguinal hernia repair. A scrotal support with application of an ice bag mayhelp relieve pain and edema. Encourage deep breathing, but not coughing.
4.1.6 Associate nurse decision making
The associate nurse has to recognize the signs and symptoms of hernias and the
strangulated hernias for better referring. A post-operative teaching plan is also
important and includes the above measures mentioned in post-operative care.
4.1.8 Complications
An incarcerated hernia may become strangulated if the blood and intestinal flow are
completely cut off in the trapped loop of bowel. Strangulated hernias do not develop
in adults very often. Incarceration leads to an intestinal obstruction and possibly
gangrene and bowel perforation. Symptoms are pain at the site of the strangulation,nausea and vomiting, and colicky abdominal pain.
Self-assessment 4.1
1) What are the types of abdominal hernias?
2) Identify the common factors associated with abdominal hernia3) What are the signs and symptoms of a complicated hernia?
4.2 Hiatal hernia
Learning Activity 4.2
P.F, a 56-year-old male consults the health facility experiencing pain about 2-3cm
beneath his sternum and sharp pains in radiating towards his left shoulder. The
pain varies in intensity and is increased immediately after eating spicy foods.
After most meals, he suffers from mild heartburn. He said that the health
personnel initially prescribed a two week course of Omeprazole, which alleviated
the symptoms, but they returned after a few days.
The physical examination does not disclose any strong evidence. The patient is
obese, lacks regular physical activities and poor diet. All other findings are within
normal limits.
The medical doctor requested some diagnostic studies including an esophagram
(barium swallow) and an endoscopy to visualization the lower esophagus. The
results of these tests showed that there is a bulging mass in the low part of
the esophagus and confirmed that it was the stomach prolapsing through the
diaphragmatic esophageal hiatus i.e. hiatal hernia. Considering that omeprazole
did not act before, the medical doctor proposed a surgical treatment that was
scheduled in 2 weeks. While waiting for the surgical intervention, the patient was
taught to observe some conservative treatment including:
• Elevation of head of bed
• Avoid reflux-inducing foods (fatty foods, chocolate, peppermint)
• Avoid alcohol
• Reduce or avoid acidic pH beverages (red wine, orange juice)
• Antacids were prescribed (omeprazole)
Questions related to the case study.
1) Identify the biography of the patient described in the case study
2) What is the medical history of patient described in the case study?
3) Describe the signs and symptoms that the patient present and are
described in the case study
4) What are the diagnostic studies?5) What was the proposed management plan?
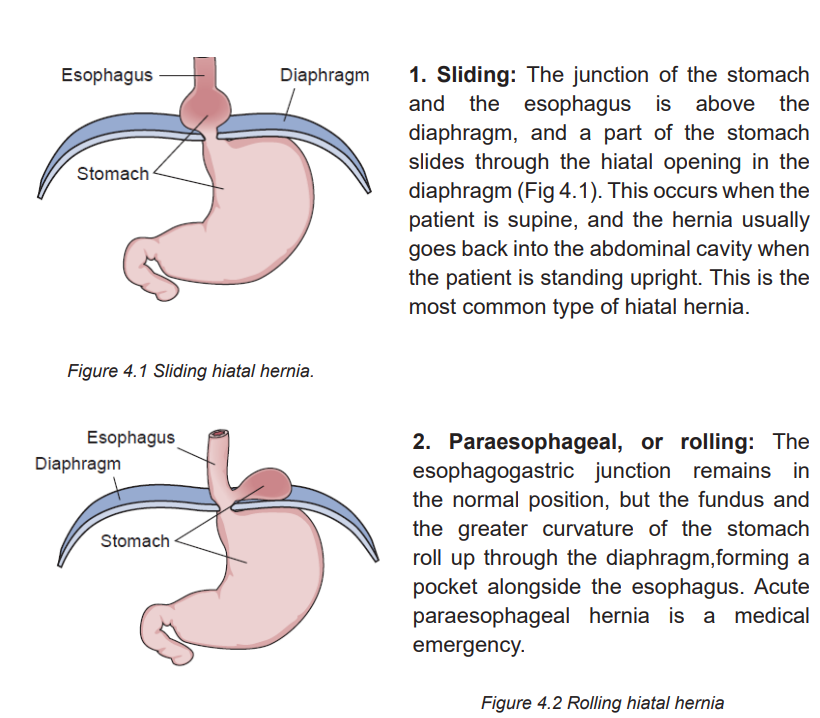
4.2.1 Definition of hiatal hernia
Hiatal hernia is a condition in which the stomach slides up through the hiatus of
the diaphragm into the thorax. It is also referred to as diaphragmatic hernia andesophageal hernia.
4.2.2 Causes and pathophysiology of Hernia
Many factors contribute to the development of hiatal hernia. Structural changes,
such as weakening of the muscles in the diaphragm around the esophagogastric
opening, occur with aging. Factors that increase intraabdominal pressure, including
obesity, pregnancy, ascites, tumors, intense physical exertion, and heavy lifting ona continual basis, may also predispose patients to development of a hiatal hernia
Hiatal hernias are classified into the following two types:
4.2.3 Signs and symptoms of Hernia
A small hernia may not produce any discomfort or require treatment. However, a
large hernia can cause pain, heartburn, a feeling of fullness, or reflux (regurgitation),
which can injure the esophagus with possible ulceration and bleeding.
The chest pain can mimic angina and is described as burning; squeezing; or radiating
to the back, neck, jaw, or arms. Complaints of chest pain are more common in
older adults with hiatal hernia or gastro esophagus reflux (GERD) disease. Unlike
angina, hiatal hernia and GERD-related chest pain is relieved with antacids.
4.2.4 Diagnostic measures
An x-ray studies such as an esophagram (barium swallow) may show the protrusion
of gastric mucosa through the esophageal hiatus. Endoscopic visualization of the
lower esophagus provides information on the degree of mucosal inflammation or
other abnormalities.
4.2.5 The management of Hernia
Conservative treatment includes lifestyle changes to alleviate symptoms of hiatal
hernia; losing weight, taking antacids, eating small meals that pass easily, through
the esophagus, not reclining for 3 to 4 hours after eating, elevating the head of the
bed 6 to 12 inches to prevent reflux, and avoiding bedtime snacks, spicy foods,alcohol, caffeine, and smoking.
4.2.6. Complications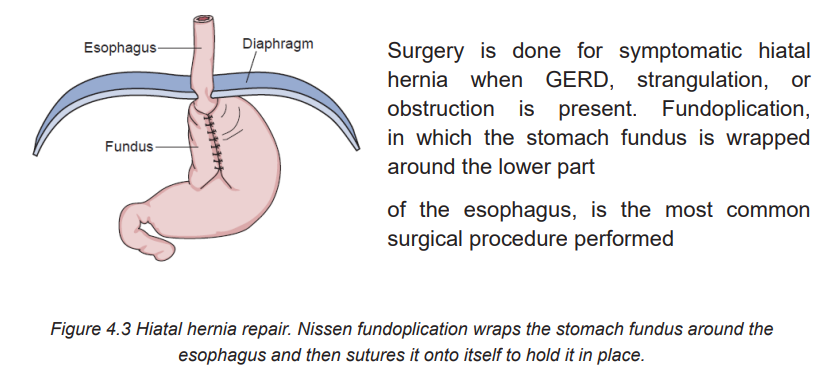
A paraesophageal hernia is rarer but serious as part of the stomach squeezesthrough the hiatus and is at risk for strangulation (blood supply is cut off).
4.2.7. Associate nurse decision making
In the hospital, the associate nurse will perform tasks that are delegated by registered
nurses. The primary focus of care for hiatal hernia disease is educating patients.
The teaching guide will include detail the following: The patient is taught lifestyle
interventions to reduce the symptoms of hiatal hernia. If the patient undergoes
surgery, general postoperative nursing care is provided. In addition,
following fundoplication, patients are assessed for dysphagia during their first
postoperative meal. If dysphagia occurs, the physician should be notified becausethe repair may be too tight, causing obstruction of the passage of food.
Self-assessment 4.2
1) Explain the types of hiatal hernia
2) What are other diseases that can mimic the signs and symptoms ofhiatal hernia?
4.3 End unit assessment
End of unit assessment
1) How should the nurse teach the patient with a hiatal hernia or GERD to
control symptoms?
a) Drink 295 to 355ml of water with each meal.
b) Space six small meals a day between breakfast and bedtime.
c) Sleep with the head of the bed elevated on 4- to 6-inch blocks
d) Perform daily exercises of toe-touching, sit-ups, and weight lifting.
2) The patient calls the clinic and describes a bump at the site of a previous
incision that disappears when he lies down. The nurse suspects that this
is which type of hernia (select all that apply)?
a) Ventral
b) Inguinal
c) Femoral
d) Reducible
e) Incarceratedf) Strangulated
3) The patient asks the nurse why she needs to have surgery for a femoral,
strangulated hernia. What is the best explanation the nurse can give the
patient?
a) The surgery will relieve her constipation.
b) The abnormal hernia must be replaced into the abdomen.
c) The surgery is needed to allow intestinal flow and prevent necrosis.
d) The hernia is because the umbilical opening did not close after birth as
it should have.
4) What are the most frequent symptoms of abdominal Hernia?
5) What are the diagnostic measures of hiatal hernia?
6) What are the do’s and don’ts after inguinal hernia surgery?UNIT5:HEMORRHOIDS
Key Unit competence:Take appropriate decision on Hemorrhoids
Introductory activity 5.0
The images below from A to E illustrate the structures of the cross section ofsigmoid and anus. Observe them and respond to the attached questions.
1) What are the physiological changes would reflect these changes in the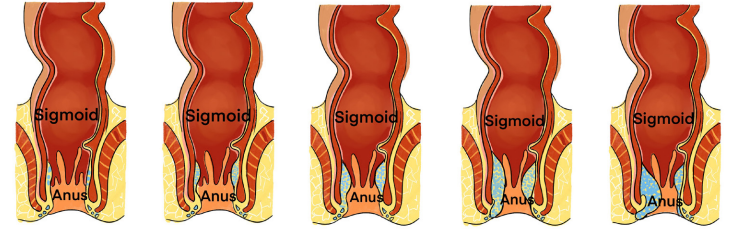
intestines?
2) What are the manifestations of such abnormalities in the human body?
3) How can health personnel identify or notice these abnormalities?4) How can these abnormalities be corrected?
5.1. Description of Hemorrhoids
Learning Activity 5.1
N.A is a 37-year-old pregnant woman consults the hospital with pain in the rectum
during and after passing stools. She said that he saw blood on the toilet paper
that she used. She also mentioned that she has been having hard stool since
some weeks and itching. The medical doctor put the patient on the left lateral
decubitus with the N. A’s knees flexed toward the chest, he inspected the anus
and performed anal digital examination. A bulging mucosa was observed duringinspection and palpated confirming external hemorrhoids.
Questions related to the case study
1) What is the medical history of N.A described in the case study?
2) Do you think that this history has something to do with the haemorrhoids?
Explain your response.3) Describe the signs and symptoms presented in the case study
5.1.1. Definition of Hemorrhoids
Hemorrhoids are a very common anorectal condition defined as the symptomatic
enlargement and distal displacement of the normal anal cushions.
5.1.2. Causes and pathophysiology of hemorrhoids
The exact pathophysiology of hemorrhoidal development is poorly understood.
For years the theory of varicose veins, which postulated that hemorrhoids were
caused by varicose veins in the anal canal, had been popular but now it is obsolete
because hemorrhoids and anorectal varices are proven to be distinct entities.
Today, the theory of sliding anal canal lining is widely accepted. This proposes that
hemorrhoids develop when the supporting tissues of the anal cushions disintegrate
or deteriorate. Hemorrhoids are therefore the pathological term to describe the
abnormal downward displacement of the anal cushions causing venous dilatation
and increase in pressure in the veins.
Some of the risk factors of hemorrhoids include pregnancy, prolonged sitting or
standing position, obesity and chronic constipation. Portal hypertension related to
liver disease may also be a factor.
5.1.3 Signs and symptoms of Hemorrhoids
Internal hemorrhoids (Fig 5.1) are usually not painful unless they prolapse. They
may bleed during bowel movements. External hemorrhoids (Fig 5.1) cause itching
and pain when inflamed and filled with blood (thrombosed). Inflammation and
edema occur with thrombosis, causing severe pain and possibly infarction of theskin and mucosa over the hemorrhoid
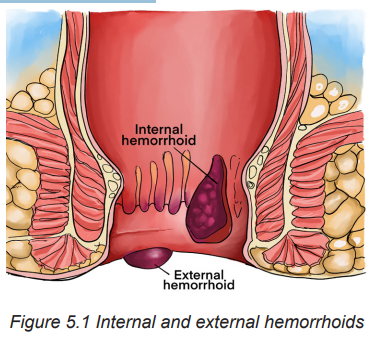
5.1.4 Diagnostic measures
The Hemorrhoids can be diagnosed through a complete history, physicalexamination; (lubricated finger, gently inserted into the anal canal while asking the
patient to bear down the resting tone of the anal canal). Internal hemorrhoids are
generally not palpable on digital examination, anoscopy is performed. Hemorrhoidal
bundles will appear as bulging mucosa and anoderm within the open portion of the
anoscope. Sigmoidoscopy and colonoscopy can also be used. A complete blood cell
(CBC) count may be useful as a marker for infection. Anemia due to hemorrhoidalbleeding is possible.
Self-assessment 5.1
1) Briefly explain the pathophysiology of Hemorrhoids?2) Identify other diseases that would mimic the symptoms of Hemorrhoids?
5.2. The management of Hemorrhoids
Learning Activity 5.2
…Continuation of N.A case study
After physical exam, the medical doctor confirmed that Madam N.A is suffering
from Hemorrhoids. Regarding the treatment, Mr. S.D has received antiinflammatory drugs and advice on how to change her lifestyle
Questions related to the case study.
1) What is the surgical treatment plan adopted by the medical doctor for this
patient?
2) In group, discuss the different medication prescribed to this patient.3) List potential complications which may happen to Madam N.A.
5.2.1. The treatment plan of Hemorrhoids
Treatment is aimed at preventing constipation, avoiding straining during
defecation, maintaining good personal hygiene, and making lifestyle changes to
relieve hemorrhoid symptoms and discomfort .Lifestyle modification use of anti
inflammatory and surgery are the treatment of hemorrhoids
5.2.2. Associate nurse decision making
In the hospital, the associate nurse will perform tasks that are delegated by
registered nurses. The primary focus of care for haemorrhoids disease is educatingpatients. Encourage patient and caregiver to share concerns about lifestyle.
5.2.3. Complications of Hemorrhoids
The most common and serious complications of haemorrhoids include perianal
thrombosis and incarcerated prolapsed internal haemorrhoids with subsequent
thrombosis. They are characterised by severe pain in the perianal region possibly
with bleeding. In a short history of the perianal thrombosis, acute surgical incisionor excision is indicated, which can result in rapid relief of the painful symptoms
Self-assessment 5.2
Mr. K.M a patient on your department unit, has a Hemorrhoids. His wife runs to
the nursing station and says that you need to help her husband, he is in pain.
4) What additional data would you gather to confirm the statement of her
wife?5) What emotional support would you offer to Mrs. SM?
5.3 End unit assessment
End of unit assessment
1) Following a hemorrhoidectomy, what should the nurse advise the patient
to do?
a) Use daily laxatives to facilitate bowel emptying.
b) Use ice packs to the perineum to prevent swelling.
c) Avoid having a bowel movement for several days until healing occurs.
d) Take warm sitz baths several times a day to promote comfort and
cleaning.
2) A patient is scheduled for a hemorrhoidectomy at an ambulatory day
surgery center. An advantage of performing surgery at an ambulatory
center is a decreased need for
a) laboratory tests and perioperative medications.
b) preoperative and postoperative teaching by the nurse.
c) psychologic support to alleviate fears of pain and discomfort.
d) preoperative nursing assessment related to possible risks and
complications.
3) Apart from digital examination, what are other diagnostic tests indicated
in the case of hemorrhoids?
4) Changing life style is one way to prevent and treat hemorrhoids. What
are the lifestyle modifications would you recommend a patient with
haemorrhoids?
5) What is the role of medications in the treatment of haemorrhoids?The
goals of pharmacotherapy are to reduce pain and constipation in patients
with haemorrhoids.
6) What is the role of pregnancy in the aetiology of haemorrhoids?Pregnancy
clearly predisposes women to symptoms from haemorrhoids, although
the aetiology is unknown. Notably, most patients revert to their previously
asymptomatic state after delivery. The relationship between pregnancy
and haemorrhoids lends credence to hormonal changes or direct pressure
as the culprit.
7) What is the role of blood studies in the workup of hemorrhoids? A complete
blood cell (CBC) count may be useful as a marker for infection. Anemia
due to hemorrhoidal bleeding is possible
8) What is the role of colonoscopy in the workup of hemorrhoids?
Colonoscopy, virtual colonoscopy, and barium enema are reserved forcases of bleeding without an identified anal source.
UNIT6:BALANITIS AND BALANOPOSTHITIS
Key Unit competence:Take appropriate decision on balanitis and balanoposthitis
Introductory activity 6.0
The Image A and B illustrate the structures of male reproductive organs. Observethem and respond to the attached questions.
1) Which one of these two figures (A&B) would reflect the normal or abnormal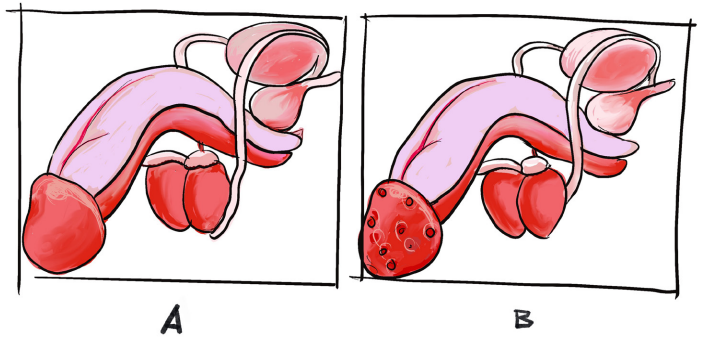
structure of the male reproductive organ in humans?
2) What explanations can you give to justify the abnormal structure of the
male reproductive organ you have found?
3) What do you think can cause the modifications that you have observed?
4) What are the manifestations of such abnormalities in the human body?
5) How can health personnel identify or notice these abnormalities of malereproductive organ in humans?
6.1. Description of Balanitis and Balanoposthitis
Learning Activity 6.1
You are at health center on day duty in consultation, you receive Mr. K C., a 26
year’s old uncircumcised male patient. He was complaining of urethral discharge
and painful urination. During history taking he reveals you that he had the same
signs and symptoms, 6 months ago and bought some drugs from the pharmacy
and symptoms disappeared. Once asked if he had sex in previous time, he
reveals you that he had it twice before developing the signs and symptoms and
he confirms that he did not told his girlfriend. During the physical exam of external
genitalia, you notice that the glans and the prepuce are inflamed, reddened, with
foul smell white discharge under the foreskin. At this stage, different diseases
are presumed including gonorrhea, balanitis, syphilis and candida. Urinalysis,
urethral opening swab and blood test were requested for better diagnosis.
Finally, the exams revealed a balanitis/ balanoposthitis caused by gonorrhea.
After confirming balanitis/ balanoposthitis. The treatment of gonorrhea was given
and KC was advised to have circumcision and to bring her girl friend to gettreatment as well.
Questions related to the case study:
1) What are possible risk factors which might probably exposed K.C to this
problem?
2) Identify the signs and symptoms as described in the case study
3) Which statement by the patient indicates the most likely cause of the
recurrence of his infection?
a) “I took the Vibramycin twice a day for a week.”
b) “I haven’t told my girlfriend about my infection yet.”
c) “I had a couple of beers while I was taking the medication.”
d) “I ve only had sexual intercourse once since my medication”
4) Why blood tests were included in the diagnostic tests to find the diagnosis
of K.6.1.1. Definition and the Balanitis and Balanoposthitis
Balanitis is often confused with two similar conditions: phimosis, balanoposthitis
and prosthitis. All these conditions affect the penis. However, each condition affects
a different part of the penis.• Phimosis is a condition that makes it difficult to retract the foreskin.
• Balanitis is inflammation of the head (glans) of the penis.
• Balanoposthitis is inflammation of both the penis head (glans) and the foreskin.
• Prosthitis is the inflammation of the prepuce
6.1.2. Causes and pathophysiology of Balanitis and Balanoposthitis
Balanitis and Balanoposthitis are mostly caused by poor hygiene in uncircumcised
men. Other causes may include:
• Sexually transmitted diseases/infections(STDs/STIs) such as Gonorrhea,
chlamydia, trichomonas vaginalis, mycoplasma genitalium, genital helps,
human papilloma virus(HPV), syphilis
• Genital yeast infection (candidiasis).
• Diabetes
• Scabies (tiny burrowing parasite) infection.
• Skin conditions that cause itchy, dry, scaly skin (ex. In psoriasis and eczema
diseases conditions).
• Reactive arthritis, a type of arthritis that develops in response to an infection
somewhere in the body
• Reactive arthritis, a type of arthritis that develops in response to an infection
somewhere in the body.
Beside poor hygiene among uncircumcised men, other predisposing factor
include: over-the-counter (OTC) medications, and no- retraction of the foreskin.
Balanitis can be classified under different types
• Balanitis (also called Zoon’s balanitis):
– This is the main type of balanitis,
– usually affects uncircumcised, middle-aged men
– the head of penis is inflamed, painful, and reddened
• Circinate balanitis:
– This is the type of Balanitis which occurs as a result of reactive arthritis,
(an arthritis that develops in response to an infection in the body).
– Inflammation, redness, pain, and small lesions (sores) on the head of the
penis are present
• Pseudoepitheliomatous keratotic and micaceous balanitis:
– very rare form of balanitis
– It mostly affects men over 60– scaly warts on the glans is present
6.1.3 Signs and symptoms of Balanitis and Balanoposthitis
Generally, signs and symptoms of balanitis may appear suddenly or gradually.
They can include:
• Swelling
• Pain and irritation on the glans (head of the penis).
• Redness or red patches on the penis.
• Itching under the foreskin.
• Areas of shiny or white skin on the penis.
• White discharge (smegma) under the foreskin
• Foul smell.
• Painful urination.
• Sores or lesions on the glans (rare and specific to Pseudoepitheliomatouskeratotic and micaceous balanitis)
6.1.4 Diagnostic measures of Balanitis and Balanoposthitis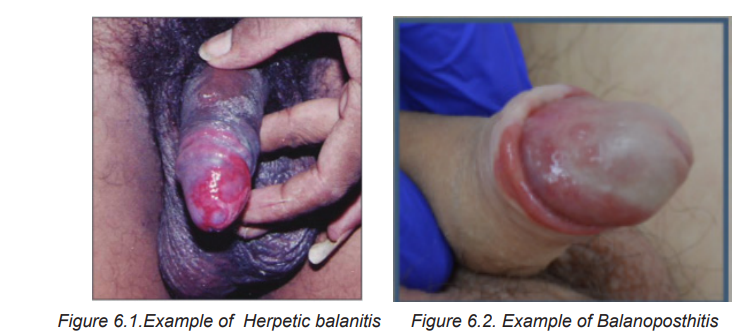
The Balanitis and Balanoposthitis can be diagnosed through a complete history,
physical examination as well as some diagnostic test to determine the underlying
cause like infection
• Urinalysis
• urethral opening swab
• blood test: glycaemia (to exclude Diabetes mellitus), full blood count (to
determine the type of infection)
NB: In people with recurrent balanitis and balanoposthitis, HIV test is advisableSelf-assessment 6.1
1) What are the signs and symptoms of balanitis and balanoposthitis?
2) Briefly explain the pathophysiology of Balanoposthitis?
3) All types of balanitis share almost the same signs and symptoms. What
is the specific sign and particular sign for circinate balanitis?4) List the treatment goals of Balanitis and Balanoposthitis
6.2.1 The treatment of Balanitis and Balanoposthitis
The treatment and management of balanitis depends on the underlying cause and
contributing factors. Whatever the treatment plan, the goal of treatment is to:
• Minimize sexual dysfunction
• Minimize urinary dysfunction
• Exclude penile cancer
• Treat premalignant disease
• Diagnose and treat sexually transmitted disease.
Depending on the cause, the treatments can include:
• Antibiotics: If a sexually transmitted infection (STI) is confirmed to be the
cause of balanitis, the antibiotics will be prescribed. The antibiotic will also
depend on the type of infection (Gonorrhoea, chlamydia, trichomonas vaginalis,
mycoplasma genitalium, genital helps, human papilloma virus(HPV), syphilis
• Circumcision: is a surgical procedure in which the foreskin covering the
penis is surgically removed. Circumcision is recommended in case of
recurring symptoms of balanitis in uncircumcised
• Antifungal creams: is prescribed if the yeast infection is the underlying
cause of balanitis. Antifungal like clotrimazole will be applied the glans (head
of the penis) and foreskin as prescribed.
• Diabetes management: If you have diabetes, your provider will show you
how to manage the condition.
• Improved hygiene: this consist of washing and drying under the penis’s
foreskin (glands) often to reduce the risk of reoccurrence of balanitis.
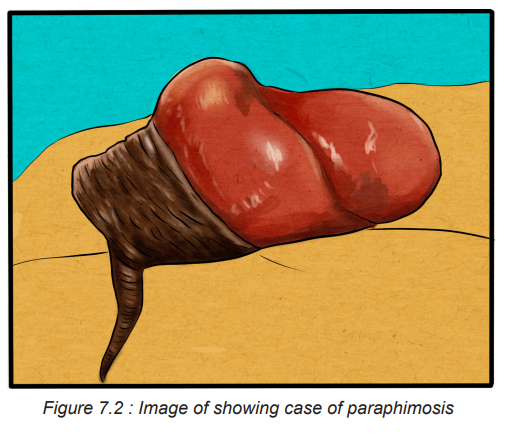
6.2.2. Evolution and complications of Balanitis and Balanoposthitis
Untreated balanoposthitis does not usually cause serious complication except
when its underlying cause are cancerous origin.Generally untreated inflammation of the glans of the penis (balanitis) is frequently
associated with a degree of the inflammation of the foreskin (posthitis), a situation
which can lead to the following:
• Phimosis: retraction of the penis’s foreskin. The foreskin may swell, cause
pain, and blockage during urinating. The swelling is typically described as
balloon-like swelling or ‘ballooning’).
• Paraphimotic: a surgical condition whereby the penis’ foreskin becomes
trapped behind the head of the penis, and cannot be pulled over the head
to its normal position. This is typically very painful and considered a medical
emergency. It must be treated as soon as possible, otherwise the blood flow
to the glans may be restricted, and complete circumcision will need to be
carried out in advanced cases.
• Structure of urethral meatus: the scarring around the opening of the
waterpipe, due to chronic inflammatory changes, can lead to the narrowing
of the water hole.
6.3 End unit assessment
End of unit assessment
1) An abnormal finding noted during physical assessment of the male
reproductive system is
a) Descended testes.
b) Symmetric scrotum.
c) Slight swollen and reddish glans of penis
d) The glans covered with prepuce.
2) List the complications of Balanitis and Balanoposthitis
3) What are the preventive measures for Balanitis/ Balanoposthitis?
4) How clotrimazole cream for balanitis is used?
5) What are the treatment modalities of Balanitis/ Balanoposthitis?UNIT 7:PHIMOSIS AND PARAPHIMOSIS
Key Unit competence:Take appropriate decision on phimosis and paraphimosis
Introductory activity 7.0
The Image A, B, C and D illustrate the structures of male reproductive organs.Observe them and respond to the attached questions
1) What do you think on the figure A, B, C&D?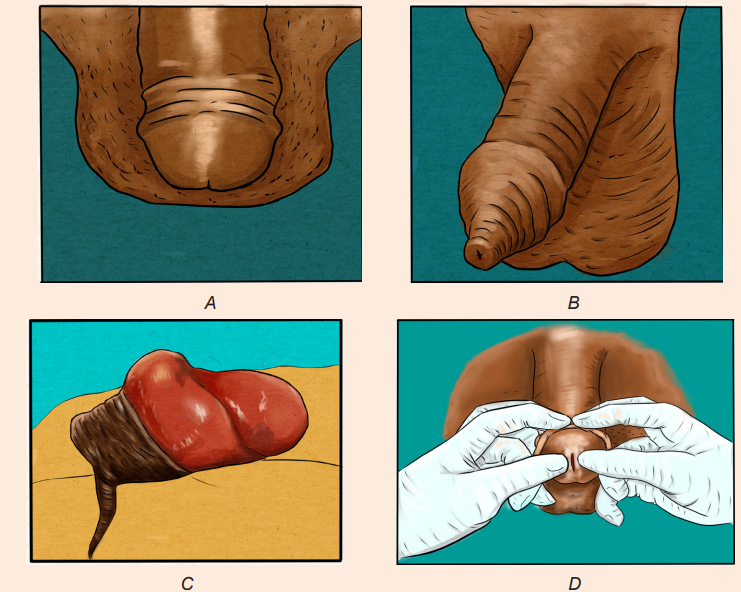
2) What are your observations on figures (A, B, C&D) would reflect the
abnormal structure of the male reproductive organ in humans?
3) What do you see in image B and C?
4) What is the difference between A and C?5) What do you think about that someone is doing in image D?
7.1. Description of Phimosis and Paraphimosis
Learning Activity 7.1
Miss D.K is associate nurse at one health facility in rural area of Rwanda.
During her night duty, she received Mr. M G, a 26 year’s old uncircumcised
male patient. He was complaining of foreskin scratching, painful urination and
painful erections. During history taking he reveals to nurse that he had inability
to pulldown the foreskin since birth and the same signs and symptom since 6
months ago. The nurse in charge of consultation examined him and a diagnosis
of phimosis was made and a rendez vous for circumcision was fixed on the
next 2 days. Arriving at home, he wanted to take shower before sleeping. While
performed genital hygiene, he tried to retract his prepuce for more visualization
but he failed to retract it back. Immediately he started to feel severe penile
pain and inability to pass urine as he felt something like a barrier to pass the
urine. During the physical exam of external genitalia, Nurse noticed that the
glans and the prepuce are inflamed, reddened. He is glans appears enlarged
and congested, with a collar of swollen foreskin around the coronal sulcus. At
this stage, the final diagnosis was made: patient was suffering from phimosis
complicated into paraphimosis. Finally, Nurse attempted the manual reduction
and failed. The decision for surgical treatment was made: Performance of sterile
circumsion under local anesthesia (emergency dorsal slit) and prescription ofpainkiller was done.
Questions related to the case study:
1) Basing on the case scenario, what are the causes and possible risk
factors which might probably exposed MG to this problem?
2) Identify the signs and symptoms Mr. MG presented at health facility
3) Why lab tests were not included in the diagnostic tests to find the diagnosis
of MG?
4) How nurse diagnosed the condition of Mr. MG?5) Which treatment did they provide to Mr. MG?
7.1.1 Definition and the Phimosis and Paraphimosis
Phimosis and paraphimosis are conditions that occur among uncircumcised male
clients when the opening of the foreskin is constricted. All these conditions affect
the penis foreskin.
Phimosis: is defined as the inability to retract the skin (foreskin or prepuce)
covering the head (glans) of the penis and leading to a tightness or constriction
of the foreskin around the head of the penis, making retraction difficult. Phimosis
may appear as a tight ring or “rubber band” of foreskin around the tip of the penis,preventing full retraction.
Physiologic VS Pathologic Phimosis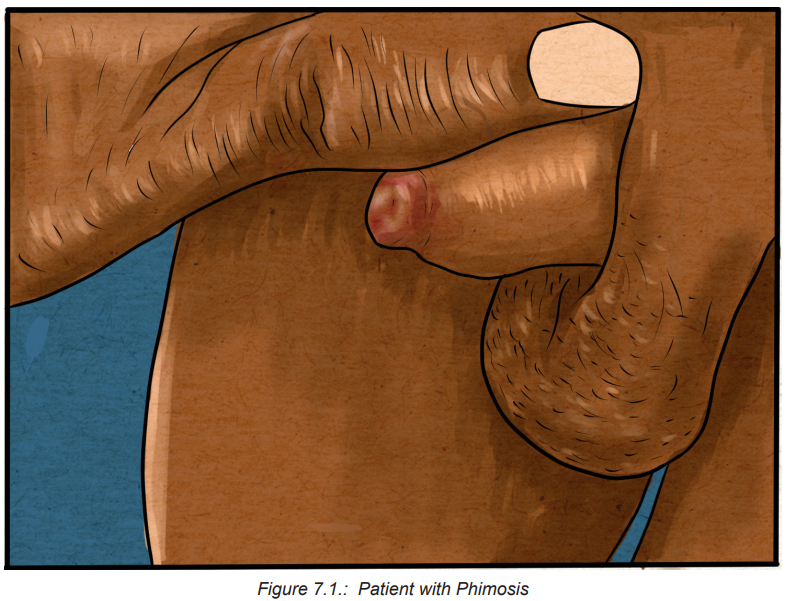
Depending on the situation, this condition may be considered either physiologic
or pathologic. Physiologic, or congenital, phimosis is a normal condition of the
newborn male and in children younger than 3 years of age, and may be a normal
finding up until the age of puberty while acquired (pathologic) phimosis is most
seen in post pubertal males, or in patients in whom scarring has developed from
chronic infection and inflammation (balanoposthitis), or as a result of repeated
forced retraction of congenital phimosis.
Smegma: is a collection of skin cells from the glans penis and inner foreskin that
is often noted with retraction of the foreskin. This natural skin shedding helps to
separate the foreskin from the head of the penis. Smegma may appear as white
pearls underneath the skin, which can easily be washed off once the foreskin is
retracted.
Paraphimosis: is a strangulation of the glans penis from an inability to replace the
retracted foreskin. It is a urologic emergency, occurring in uncircumcised males, in
which the foreskin becomes trapped behind the corona and forms a tight band ofconstricting tissue
7.1.2 Causes and risks factors and the Phimosis and Paraphimosis
Phimosis is a tightness or constriction of the foreskin around the head of the penis,
making retraction difficult, is caused by edema or inflammation of the foreskin,
usually associated with poor hygiene techniques that allow bacterial and yeast
organisms to become trapped under the foreskin. Congenital phimosis is expected
in children younger than 3 years of age, and may be a normal finding up until the
age of puberty. These phimotic conditions often are caused by a congenitally small
foreskin; however, chronic inflammation at the glans penis and prepuce secondary
to poor hygiene or infection also are etiologic factors.
Beside poor hygiene in young children others various reasons may also contribute
to development of phimosis including:
• Skin conditions such as eczema, psoriasis, lichen planus and lichen sclerosus.
When it affects the penis, lichen sclerosis is known as penile lichen sclerosis
or balanitis xerotic obliterans (BXO).
• Preputial adhesions, or scar tissue, that keep the foreskin attached to the tip
(glans) of your penis.
• Injuries.
• Infections, including sexually transmitted infections (STIs).
The cause of paraphimosis is most often iatrogenic. The condition is frequently
occurring after penile examination, urethral catheterization or cystoscopy.
Paraphimosis typically occurs after Foley catheter placement. Rare causes of
paraphimosis include self-inflicted injury to the penis (such as piercing a penile ringinto the glans) and paraphimosis secondary to penile erections
7.1.3 Pathophysiology and Types of Phimosis and Paraphimosis
When the foreskin becomes trapped behind the corona for a prolonged time, it
may form a tight, constricting band of tissue. This circumferential ring of tissue can
impair the blood and lymphatic flow to and from the glans and prepuce. As a result
of penile ischemia and vascular engorgement, the glans and prepuce may become
swollen and edematous. If left untreated, penile gangrene and auto amputation
may follow in days or weeks. Phimosis is divided into two forms: physiologic and
pathologic phimosisis.
Physiologic phimosis: Children are born with tight foreskin at birth and separation
occurs naturally over time. Phimosis is normal for the uncircumcised infant/child
and usually resolves around 5-7 years of age, however the child may be older.
Pathologic phimosis: Phimosis that occurs due to scarring, infection or
inflammation. Forceful foreskin retraction can lead to bleeding, scarring, and
psychological trauma for the child and parent. If there is ballooning of the foreskin
during urination, difficulty with urination, or infection, then treatment may be
warranted.
7.2 Signs and Symptoms of Phimosis and Paraphimosis
Clients with phimosis report pain with erection and intercourse and difficulty cleaning
under the foreskin.
Clients with paraphimosis often presents with penile pain. However, pain may
not always be present. The glans appears enlarged and congested, with a collar
of swollen foreskin around the coronal sulcus. If the condition continues, severe
edema and urinary retention may occur. A tight, constricting band of tissue appearsimmediately behind the head of the penis as shown in the figure below.
The physical examination should focus on the penis, urethral catheter (if present)
and scrotum. The penis should be inspected for the presence of foreskin, the color
of the glans, the degree of constriction around the penile corona and turgor of the
prepuce. Absence of foreskin excludes the diagnosis of paraphimosis. A pink orsalmon hue to the glans indicates a good blood supply.
Self-assessment 7.1
1) What are the signs and symptoms of paraphimosis?
2) Briefly explain the pathophysiology of the paraphimosis?
3) Differentiate Physiologic phimosis from pathologic phimosis4) List the risks factors associated to paraphimosis?
7.4 Treatment plan of Phimosis and Paraphimosis
Treatments for phimosis and paraphimosis vary depending on the child and
severity of phimosis. It involves reducing the penile edema and restoring the
prepuce to its original position and may include: gentle daily manual retraction,
topical corticosteroid ointment and application or circumcision. Several noninvasive
or minimally invasive methods are used to reduce the penile swelling, but due to
extreme pain patients may require a penile nerve block or topical analgesic or oralnarcotics before penile manipulation.
• Manual reduction of phimosis and Paraphimosis:
The goal of treatment is to return the foreskin to its natural position over the glans
penis through manual reduction. Manual pressure may reduce edema. A gloved
hand is circled around the distal penis to apply circumferential pressure and disperse
the edema. One strategy involves pushing the glans back through the prepuce by
applying constant thumb pressure while the index fingers pull the prepuce
over the glans. Ice and/or hand compression on the foreskin, glans, and penis
may be done before this technique to reduce edema. Topical corticosteroid cream
applied two or three times daily to the exterior and interior of the tip of the foreskinmay also be effective.
Ice packs are also useful in reducing swelling of the penis and prepuce. The penis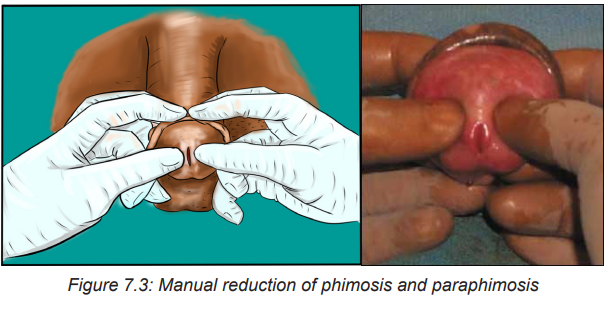
is first wrapped in plastic, with ice packs applied intermittently until the swelling
subsides .To reduce edema, a compressive elastic dressing is then wrapped
circumferentially around the penis from the glans to the base. This dressing
should be left in place for five to seven minutes, and the penis should be checked
periodically to monitor the resolution of swelling. Once the swelling has subsided,
the wrap should be removed.
• Pharmacologic therapy
Injection of hyaluronidase into the edematous prepuce is effective in resolving
edema and allowing the foreskin to be easily reduced. Degradation of hyaluronic
acid by hyaluronidase enhances diffusion of trapped fluid between the tissue planes
to decrease the preputial swelling. Hyaluronidase is well suited for use in infants
and children.
Granulated sugar has shown to be effective in the treatment of paraphimosis based
on the principle of fluid transfer occurring through osmotic gradient. Granulated
sugar is generously spread on the surface of the edematous prepuce and glans.
The hypotonic fluid from the edematous prepuce travels down the osmotic gradient
into the sugar, reducing the swelling and allowing for manual reduction. Both of the
procedures mentioned here should be performed by a physician experienced in
these techniques
• Minimally invasive therapy
The “puncture” technique is a minimally invasive therapy in which a hypodermic
needle is used to directly puncture the edematous prepuce. Puncture sites permit
safe and effective evacuation of the trapped fluid. External drainage of the trapped
fluid allows for manual reduction of paraphimosis.
Blood aspiration of the tourniqueted penis may be attempted .The base of the penis
is temporarily tied off with a rubber tourniquet. An 18-gauge needle is inserted
into the penis, and corporal blood is aspirated to reduce penile swelling. These
techniques should only be performed by a physician experienced in the procedures.
N.B: All of these techniques are geared toward reducing the swelling so that
manual reduction can be performed.
After the preputial swelling has subsided, paraphimosis is reduced .To reduce the
prepuce, the thumbs of both hands are placed on the glans and the fingers wrap
behind the prepuce. A gentle but steady and forceful pressure is applied to the glans
with the thumbs, and counter traction is applied to the foreskin with the fingers as
the prepuce is pulled down. When performed properly, the constricting band oftissue should come down distal to the glans with the prepuce.
• Surgical therapy
Severe constricting band of tissue precludes all forms of conservative or minimally
invasive therapy, an emergency circumcision dorsal slit type is recommended to
relieve these conditions permanently .This procedure should be performed with
the use of a local anesthetic by a physician or a trained health care personnel
experienced with the technique. Circumcision, a definitive therapy, should be
performed at a later date to prevent recurrent episodes, regardless of the methodof reduction used.
7.4 Evolution and complications of Phimosis and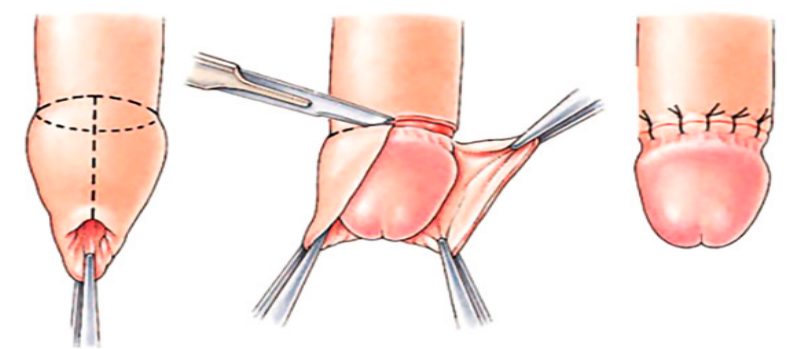
Paraphimosis
The prognosis for phimosis is usually very good. A small amount of bleeding can
occur as the skin is retracted but long term negative outcomes are very rare.
Complications of phimosis include balanitis, posthitis, paraphimosis, voiding
dysfunction, painful erection and penile carcinoma. Patients may present with
complaints of erythema, itching, discharge, or pain with sexual intercourse.
The prognosis for paraphimosis depends on the speed of diagnosis and reduction
constricting band of tissue. With prompt treatment, the outlook is excellent.
But without effective or delayed treatment, complications that can occur with
paraphimosis will range from mild to severe and life threatening condition. These
include pain, infection, and inflammation of the glans penis. If the condition is not
relieved in a sufficiently prompt timeframe, the distal penis can become ischemic
or necrotic. When this happens, paraphimosis can result in: a severe infection,
damage to the tip of the penis, gangrene, or tissue death, resulting in the loss of
the tip of the penis.
7.6 End unit assessment
1) Which patient is at the greatest risk for developing Paraphimosis
condition?
a) Circumsed Patient with chronic sexual transmitted diseases
b) Patient with urinary tract infection
c) A 17-year-old man with pre-existence congenital phimosis
d) A 65-year-old circumcised patient with urinary incontinence
2) What is the most important cause of the paraphimosis among the
following?
a) Skin conditions such as eczema, psoriasis and lichen planus
b) Iatrogenic cause like urethral catheterization or cystoscopy.
c) Injury to genital organ
d) Multiple Sexual activity
e) for cirumsed men
3) List the 4 components of treatment plan for phimosis and paraphimosis
4) Explain the importance of pain killer before manual reduction of
paraphimosis.
5) Explain the goal of manual reduction of phimosis and paraphimosis.
6) What can you do to reduce edema if you are called to care for patient with
paraphimosis?
7) When surgical therapy will be decided in case of paraphimosis?
8) What can be done to prevent complications to paraphimosis?9) List 4 complications of phimosis and paraphimosis?
UNIT8:HYDROCELE AND TESTICULAR TORSION
Key Unit competence:
Take appropriate decision on Hydrocele and Testicular torsion
Introductory activity 8.0
The image A, C and c illustrate the structures of testicle. Observe image A, B, C,D and E and answer the questions below.
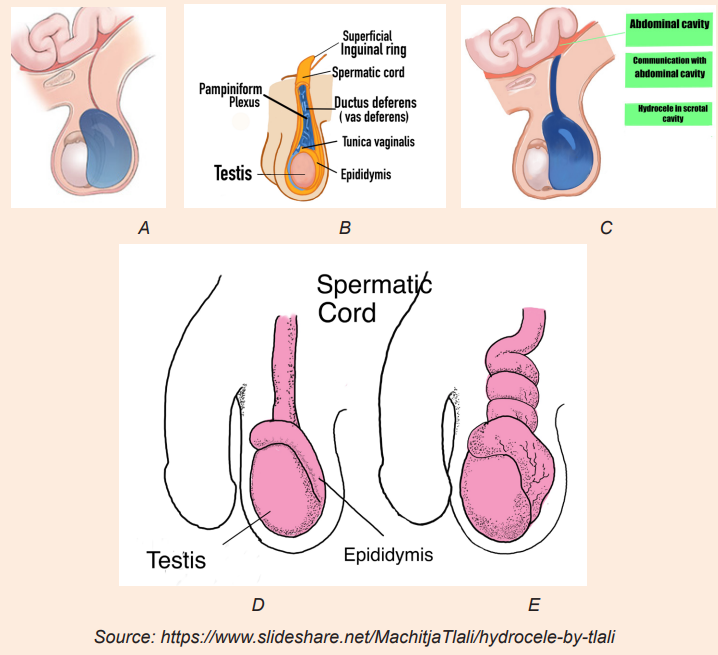
Draw the image without labels, and make image D in the black context
1) Which one of these three images (A, B, C, D) would reflect the normal
structure of testicle?
2) What is the difference between image A and B?
3) What is the difference between image A and C?
4) What is the difference between image D and E?5) How can these abnormalities be corrected?
8.1. Description of hydrocele
Learning Activity 8.1
H.K is a 5 years old boy was referred to the surgical OPD for urologist review on
20.5.2022 with swelling of right scrotum since 5 months. The mother complained
of swelling of right scrotum, which increased in size gradually. There was mild
pain when the swelling started. There was no history of fever or trauma when it
started. The physician performed trans-illumination test which become positive
and hydrocele was confirmed. The patient was scheduled for surgery to drain
the fluid accumulated in the scrotum under local anaesthesia using needle andsyringe.
Questions related to the case study
1) Identify the biography of the patient described in the case study.
2) What are the signs and symptoms described in the case study?
3) What is the probable surgical diagnosis of this H.K?
4) Which test performed to confirm surgical diagnosis described in the case
study?5) What was the management provided for this patient H.K?
8.1.1. Definition of hydrocele
A hydrocele is a non-tender, fluid-filled mass that results from interference with
lymphatic drainage of the scrotum and swelling of the tunica vaginalis that surrounds
the testis. Hydroceles vary greatly in size. Very large hydroceles are sometimesseen in elderly men and it might have been getting larger over a number of years.
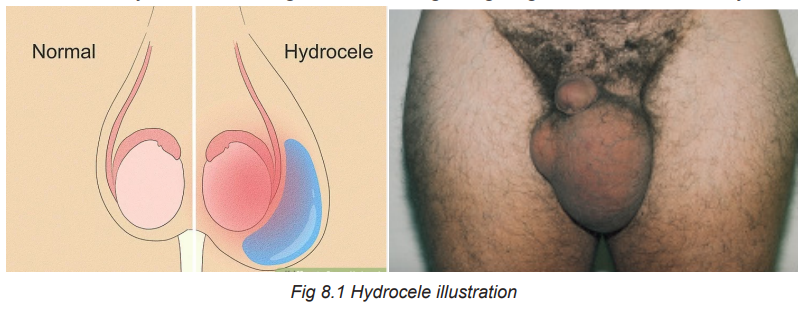
8.1.2. Causes of hydrocele
Most hydroceles occur in adults and are most common in men aged over 40 years.
The causes of hydrocele is unknown in most of cases. A few cases of hydroceles
occur when something is wrong testicles. For instance, infection, inflammation,
injury or tumours involving the testes may cause fluid be accumulated which leads
to hydrocele formation.
8.1.3. Types of hydrocele
Communicating hydrocele
In communicating hydrocele the opening does not close and fluid is able to go backbetween abdominal cavity and scrotal cavity.
Non-communicating hydrocele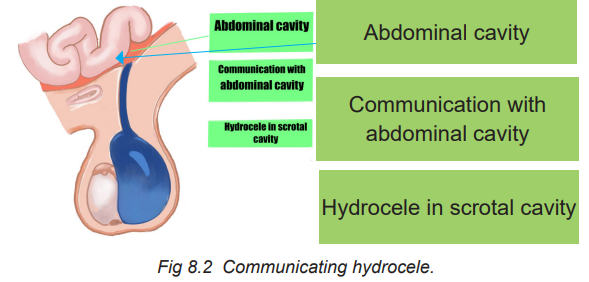
The open remains closed after the testicle is in the scrotum but there is fluid trapped
in the scrotum. This type is mostly found often in new-born and may take up to oneto resolve.
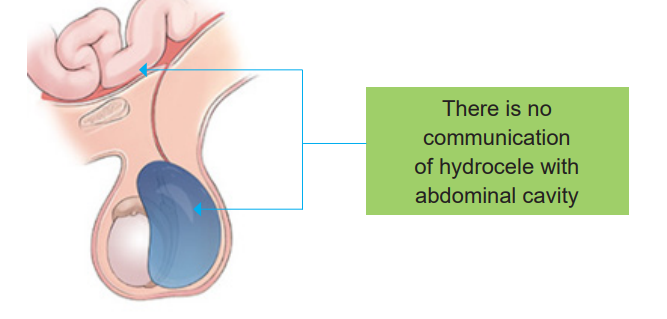
8.1.4. Signs and symptoms of hydrocele
Non-communicating hydrocele is characterized by a constant swelling.
On the other hand, in communicating hydrocele the swelling comes and goes
throughout the course of a day.Fluid around the testis does not usually cause pain or discomfort.
8.1.5. Diagnosis of hydrocele
Doctor uses the following modalities to diagnose hydrocele:
Doctors usually perform a physical examination for diagnosing Hydrocele. During
exam the doctor will not be able to feel the testicle well due to the presence of
fluid in the sac. Doctors will also check for tenderness in scrotum and shine a light
through the sac. This procedure is called “trans-illumination” and it allows the
doctor to determine presence of fluid. The scrotum will allow light transmission if
fluid is present. It will appear to light up with light passing through it. The light will
not shine through the scrotum if the swelling is due to solid mass. The doctor may
also perform an ultrasound to check for tumors, hernias or any other cause forswelling of the scrotum.
Ultrasound: This can help to check your testes to make sure if there aren’t otherunderlying causes of hydrocele.
8.1.6. Treatment plan of hydrocele
Two modalities of hydrocele management
A. Aspiration with needle and syringeB. Surgical management (hydrocelectomy)
A. Aspiration with needle and syringe
This procedure can be performed for non-communicating hydrocele once thescrotum become swollen.
B. Surgical management of hydrocele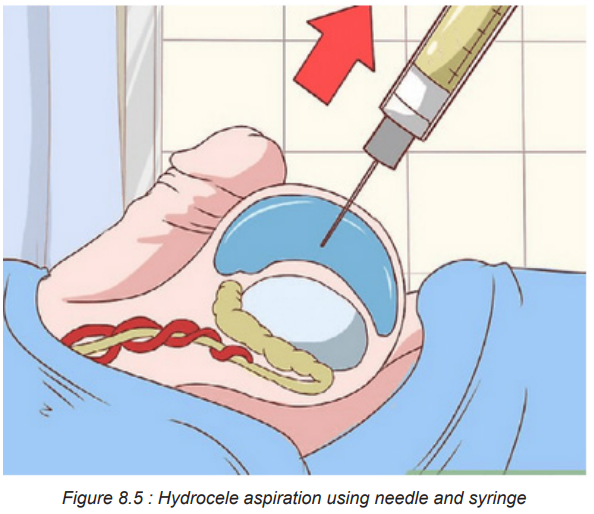
Non-communicating hydrocele: Normally resolve on its own over time and do not
require surgery. The surgery is required if swelling persists past 12 months of age.
Communicating hydrocele: This types, do not resolve on its own and it requires
surgery (hydrocelectomy). The surgery is recommended to decrease the chance of
a loop of bowel or abdominal contents getting stuck which could hurt the bowel and
the testicle. This surgery is done under anaesthesia and small incision is made inthe groin.

8.1.8. Complications and evolution of hydrocele
Left untreated Hydroceles can lead to infection of the fluid and testicular atrophy. A
large hydrocele may block the testicular blood supply leading to testicular atrophy
and subsequent impairment of fertility. Haemorrhage into the hydrocele can result
from testicular trauma. If a communicating hydrocele does not go away on its own
and is not treated, it can lead to an inguinal hernia. In this condition, part of the
intestine or intestinal fat pushes through an opening (inguinal canal) in the groin
area. The prognosis for congenital hydrocele is excellent. Most congenital cases
resolve by the end of the first year of life. Persistent congenital hydrocele is readily
corrected surgically.
Self-assessment 8.1
1) Define hydrocele
2) What are the signs and symptoms of hydrocele?
3) Differentiate communicating and non-communicating hydrocele.
4) How is trans-illumination test done?5) Outline three complications of hydrocele.
8.2. Description of Testicular torsion
Learning Activity 8.2
A 15 year-old male was admitted to the Emergency Department of a tertiary
Hospital presenting with a sudden and continuous pain in the left testicle. The
pain was progressive, radiated to the abdomen and left inguinal area, it was
accompanied with nausea and vomiting of more than 12 h since its onset. On
physical examination the left testicle was found to be larger in volume to the right
one, was painful, local temperature had risen and there was a negative Prehn
sign (exacerbation of pain upon elevation of the testicle on raising the affected
testicle). There was also an absence of the cremasteric reflex which is an
indicative of testicular torsion. Doppler ultrasound showed changes suggestive
of testicular torsion. Emergency surgery was performed on the day of admission
to correct this problem. This showed findings of a necrotic left testicle with a
360° rotation of the spermatic cord for which a left orchiectomy was performed.
The pathology study reported hemorrhagic testicular infarction. There were no
complications during recovery and the patient was discharged the day aftersurgery.
Questions related to the case study
1) Identify the biographic data of the patient from the case study above.
2) List the signs and symptoms presented by patient on his arrival to the
Emergency Department.
3) What are the findings identified by physician on physical examination?
4) What is the surgical diagnosis of this patient found on Doppler ultrasound?5) How was this surgical diagnosis corrected?
8.2.1. Definition of Testicular Torsion
Testicular torsion involves a twisting of the spermatic cord that supplies blood to thetestes and epididymis. It is most commonly seen in males younger than age 20.
8.2.2. Causes and pathophysiology of Testicular Torsion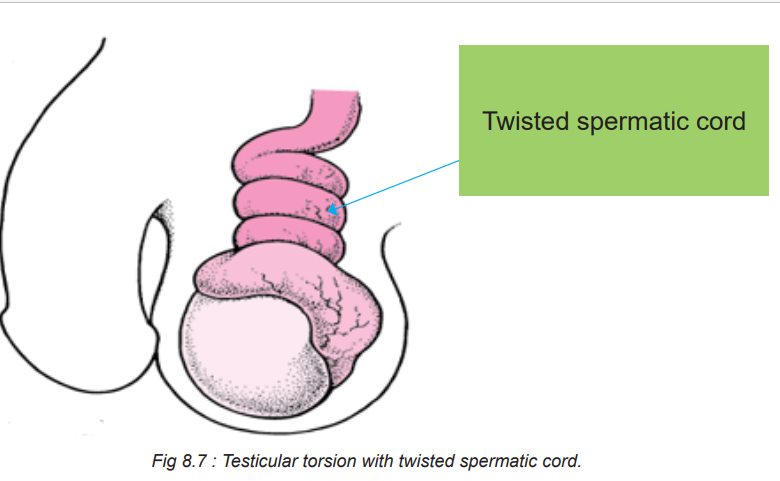
Testicular torsion can occur spontaneously, as a result of trauma, or as a result of
an anatomic abnormality. As the testicle twists around the spermatic cord, venous
blood flow is cut off, leading to venous congestion and ischemia of the testicle.
The testicle becomes tender, swollen, and possibly erythematous. As the testicle
further twists, the arterial blood supply is cut off which leads to further testicular
ischemia and eventually necrosis. In most individuals, the testicle rotates between
90-180 degrees and compromised blood flow. Complete torsion is rare and quickly
decreases the viability of the testes. The correction is possible if the torsion is lessthan 8 hours but rare if more than 24 hours have elapsed.
8.2.3. Signs and symptoms of Testicular Torsion
Signs and symptoms of testicular torsion include:
Unilateral scrotal pain: The pain may be constant or intermittent, but not positional.
Associated symptoms: Nausea and vomiting, abdominal pain and inguinal pain.
Scrotal swelling and erythematous.
The testicle may be in an abnormal or transverse lie and maybe in a high position.
Absence of cremasteric reflex (Stroking of the skin causes the cremaster muscle
to contract and pull up testicle toward the inguinal canal) but it is not reliable in
patients less than one year. In absence of cremasteric reflex, the stroke of skin willnot allow the pulling up of testicle towards inguinal canal.
The following chart summarizes the signs and symptoms of testicular torsion
8.2.4. Diagnosis of Testicular Torsion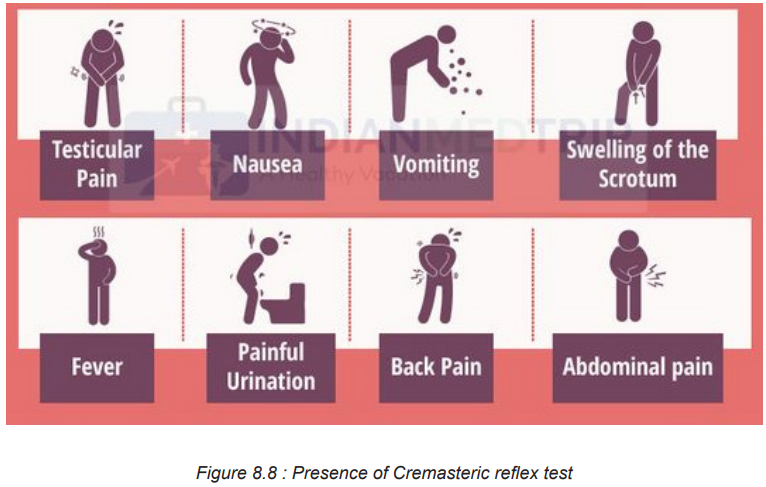
To diagnose testicular torsion, Doppler ultrasound is typically performed to assess
blood flow within the testicle. Decreased or absent blood flow confirms the diagnosis.
MRI and CT scan may also be performed. Although surgical exploration is invasive,
it remains the gold standard in the diagnosis of testicular torsion.
8.2.5. Treatment plan of Testicular Torsion
Manual detorsion
Manual detorsion was first described in 1893 to reverse ischemia and provide
instantaneous pain relief. This procedure may limit testicular infarction while
preparations are being made for surgical exploration. The procedure is done by
rotating the affected testicle at 180 degrees in clockwise direction. The procedure
may need to be repeated 2–4 times, as torsion can involve rotations of 180–720
degrees. Manual detorsion should be guided by instantaneous resolution of painand re-establishment of blood.
Surgical Exploration
Torsion constitutes a surgical emergency because, if the blood supply to the
affected testicle is not restored within 4 to 6 hours, ischemia to the testis will occur,
leading to necrosis and the possible need for removal. Unless the torsion resolves
spontaneously, surgery to untwist the cord and restore the blood supply must beperformed immediately

8.2.6. Complications and evolution of Testicular Torsion
The common complications of testicular torsion include the following:
• Loss of testis
• Infection
• Infertility
• Loss or diminished exocrine and endocrine function in men
Evolution of testicular torsion
Since many years ago there has been a markable improvement in the recovery of
the testes following torsion. However, poor results still occur especially in African
Americans, young patients, and those who lack health insurance. Better outcome
is obtained if the surgery is done within 8 hours. The outcomes of testicular torsion
depend on when the patient presents to the hospital and how quickly the diagnosis
is made and treatment is undertaken. Delays in diagnosis and treatment always
lead to testicular atrophy. About 20-40% of cases of testicular torsion result in an
orchiectomy. The risk of losing a testis is much higher among AfricanAmericans and
younger males. For those who present within the first 6 hours of symptoms, the
survival rate is nearly 100% but this number quickly drops to less than 50% if thedelay in seeking help is more than 12-24 hours.
8.3. End unit assessment
End of unit assessment
1) Define testicular torsion.
2) State two main causes of testicular torsion.
3) The following are the signs and symptoms of testicular torsion EXCEPT:
a) Scrotal pain
b) Nausea and vomiting
c) Scrotal swelling
d) Presence of cremasteric reflex
4) The following are complications of testicular torsion EXCEPT:
a) Loss of testis
b) Infection
c) Infertility
d) Increased exocrine and endocrine function in men
5) Identify which one among A and B is representing communicatinghydrocele and non-communicating hydrocele in the following illustrations:
6) What is the most common imaging study performed to diagnose a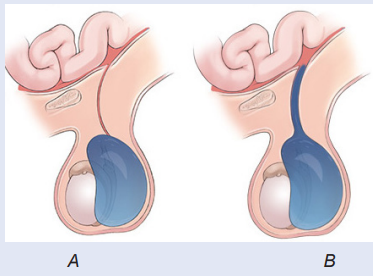
testicular torsion?
7) State two treatment modalities of hydrocele and testicular torsion foreach.
REFERENCES
1) Lewis, S. L., Dirksen, S. R., Heitkemer, M. M., & Linda Bucher. (2014).
MEDICAL-SURGICAL NURSING Assessment and mManagement of clinical
problems (NINTH). Canada: ELSEVIER MOSBY.
2) Williams, L. S., & Hopper, P. D. (2015). Understanding Medical Surgical
Nursing (Fifth edit). Philadelphia: F.A. Davis Company.
3) Hinkle, J. L., & Cheever, K. H. (2018). Brunner and Suddarth’s textbook of
medical-surgical nursing. Wolters kluwer india Pvt Ltd.
4) Winkelman, C. (2016). Medical-surgical nursing: Patient-centeredcollaborative care. Elsevier
