UNIT 5: DISLOCATION AND FRACTURE
Key Unit competence
Take appropriate decision on dislocation and fracture
Introductory activity 5.0
Observe the pictures below and respond to the questions attached.
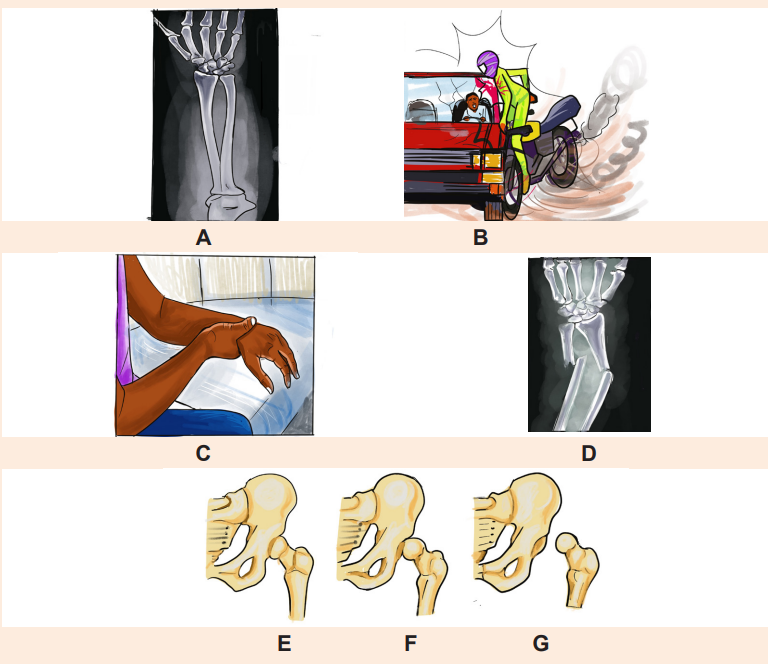
1. From the images mentioned above, which ones represent normal structure of bone?
2. What did happen to image D?
3. By observing the images above, what should be the possible cause of the problem observed in the image D?
4. What do you observe on the images F and G?
5. How image E differ from image G?
5.1. Description of dislocation
Learning Activity 5.1
The place where two or more bones in the body are connected is called a joint. A dislocation is a severe injury to the ligaments that surround a joint. It occurs when the bones in a joint become separated completely from their usual positions, when. Any joint in the body can become dislocated due to various factors. Read the following case study and answer the question below:
A 26 year old male presented to the emergency department of one tertiary hospital in Rwanda complaining with severe right shoulder pain that radiated down his humerus and into his elbow, right shoulder swelling and inability to move his right arm. He reported that he felt from the height of 6m, 40 minutes before arrival and used his arm to avoid complete fall down. Right shoulder dislocation was suspected clinically, x ray was taken and shoulder dislocation noted. Closed reduction was performed to correct this problem and better outcome was observed, patient was discharged at the same day. Previously he experienced shoulder dislocation three times which was reduced manually under local anaesthesia two month prior. She has no other current medical problem and no previous history of relevant surgery.
Questions related to the case study.
1. From the case study above, identifying the two risk factors that can be associated with shoulder dislocation.
2. What are the signs and symptoms of this condition highlighted in the case study?
3. What are the diagnostic measures used to confirm shoulder dislocation for this patient?
4. What is the surgical management done for this patient?
5. What is the outcome for this patient?
5.1. 1. Definition of dislocation concepts
Dislocation: is defined as complete separation of bone from the joint surface

Subluxation: is a partial or incomplete displacement of bone from the joint surface. The clinical manifestation of a subluxation are similar to those of dislocation but the severity are less.
5.1. 2. Causes of dislocation
Any trauma that forces a joint out of place causes a dislocation. The following are the common causes of dislocation: Accident, Falls, Contact sports such as football and basketball. Dislocations can also occur during regular activities when the muscles and tendons surrounding the joint are weak. These injuries happen more often in older people with weaker muscles and balance problems.
5.1. 3. Signs and symptoms of dislocation
Symptoms of a dislocation vary depending on the severity and location of the injury. The most common sign of dislocation is deformity of affected joint. Additional clinical manifestations include: local pain, tenderness, loss of function of injured part, swelling in the joint tissues, bruising, and instability of the joint.
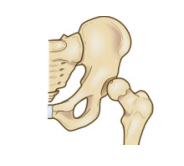
5.1.4. Adequate surgical diagnosis of dislocation
The history taking and physical examination are considered to be the most important tools that physician uses to diagnose a dislocation. The diagnosis of dislocation may be done by looking at the moving joint and asking about what caused the injury.
In some cases, an imaging test called an X-ray man be used to take a picture of the bones. The X-ray studies are performed to determine the extent of displacement of the involved structures. The joint may also be aspirated to assess for hemarthrosis or fat cells. Fat cells in the aspirate indicate a probable intraarticular fracture.
5.1.5 Nursing and collaborative management of dislocation
A dislocation requires prompt attention and is often considered an orthopaedic emergency. It may be associated with significant vascular injury. The longer the joint remains untreated, the greater the possibility of avascular necrosis. The hip joint is particularly susceptible to avascular necrosis .Compartment syndrome may also occur after a dislocation. Neurovascular assessment is critical.
The first goal of management is to realign the dislocated portion of the joint in its original anatomic position. This can be accomplished by a closed reduction, which may be performed under local or general anaesthesia depending on the severity of dislocation. Aesthesia is often necessary to relax the muscle so that the bones can be manipulated without causing pain to the patient.
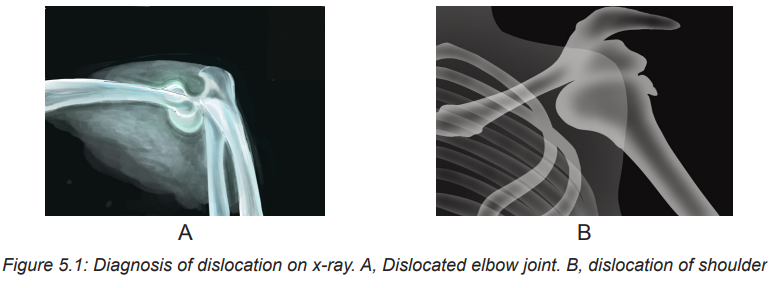
In some circumstances, surgical open reduction may be necessary. After reduction, the extremity is usually immobilized by bracing, splinting, taping, or using a sling to allow the damaged ligaments and capsular tissue time to heal. Nursing management of subluxation or dislocation is directed toward relief of pain and support and protection of the injured joint. After the joint has been reduced and immobilized, motion is usually restricted. A carefully monitored rehabilitation program can prevent fracture instability and joint dysfunction. Gentle range-of-motion (ROM) exercises may be recommended if the joint is stable and well supported. An exercise program slowly restores the joint to its original ROM without causing another dislocation.
Key components of dislocation management
– Treatment of any serious complications
– Pain relief
– Protection, rest, ice, compression, and elevation (PRICE)
– Realignment (reduction) of parts that are out of place
– Immobilization, usually with a splint or cast
– Sometimes surgery
Techniques for immobilizing a dislocated Joint
Differents technics can be used for managing disloction include:
– Sling technic
– Sling and swathe
– Finger splint
– Dynamic fingersplint
– Radialguttersplint
– Thumbspicasplint
– Posterior ankle splint
5.1.6 Complications and evolution of dislocation
5.1.6.1 Complications of dislocation
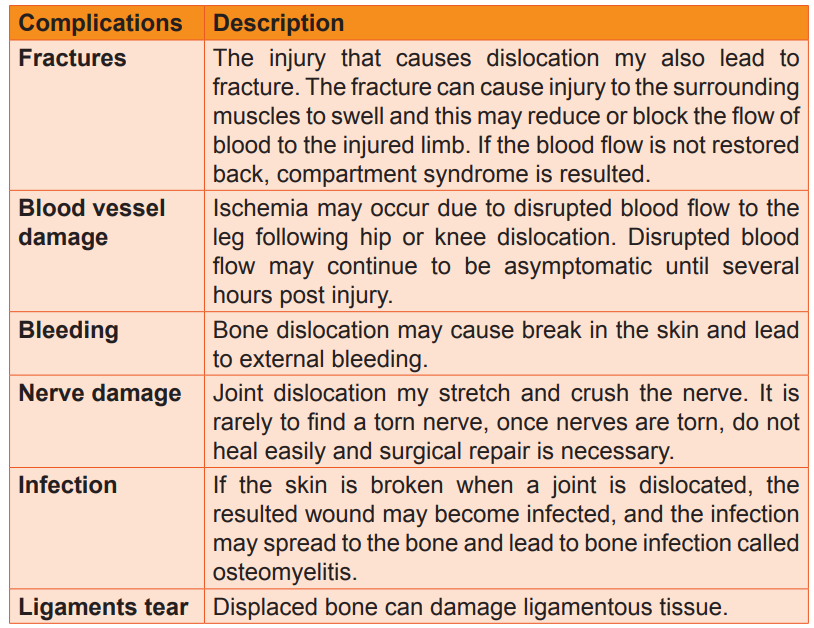
The following table summarizes the main complications related to dislocation
5.1.6.2 Evolution of dislocation
Many dislocations and related injuries heal well and result in few problems. However, some do not completely heal even though they are diagnosed and treated appropriately. How long an injury takes to heal varies from weeks to months depending on type of injury, location of the injury and the person’s age. For instance, very young people heal quickly than adults, and some disorders which impairs blood circulation such diabetes and peripheral vascular disease slow down the healing.
Self-assessment activity 5.1
1. What is the difference between dislocation and subluxation?
2. State four signs and symptoms of hip dislocation.
3. What are the causes and risks factors of dislocation in general?
4. List five key components of dislocation management.
5. Describe four complications of dislocation.
5.2 Description of fractures
Learning Activity 5.2
A 45 years old male admitted in accident and emergency with right thigh deformity, severe pain and profuse bleeding post road traffic accident. The physician performed immediate compressive dressing after giving pain killers and x-ray was of right thigh was ordered. The findings on x ray revealed right open Comminuted femur fracture, the wound was irrigated and cleaned using normal saline and dressed. Casts were used to immobilize the bone while waiting for open reduction and external fixation as final management.
Questions related to the case study.
1. From the case study above, identifying the three signs presented by the patient on arrival at emergency department.
2. Identify the type of fracture highlighted in the case of this patient.
3. What is the diagnostic test done to confirm this type of fracture?
4. What was the management done for this patient?
5.2.1 Definition of fracture
A fracture is a disruption or break in the continuity of the structure of bone. Although physical trauma related injuries account for the majority of fractures, some fractures are caused by disease process especially osteoporosis and cancer.
5.2.2 Classification of fractures
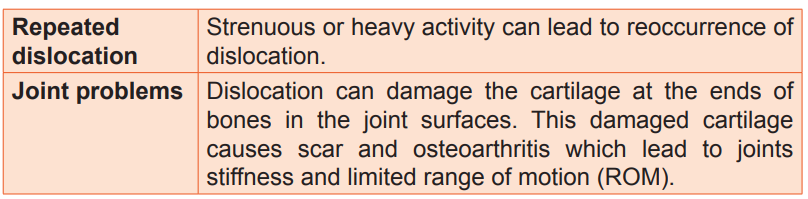
5.2.2.1 Classification of fracture according to the communication with external environment.
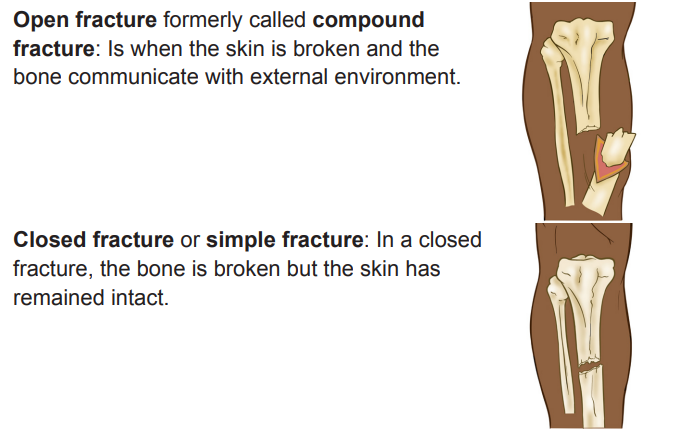
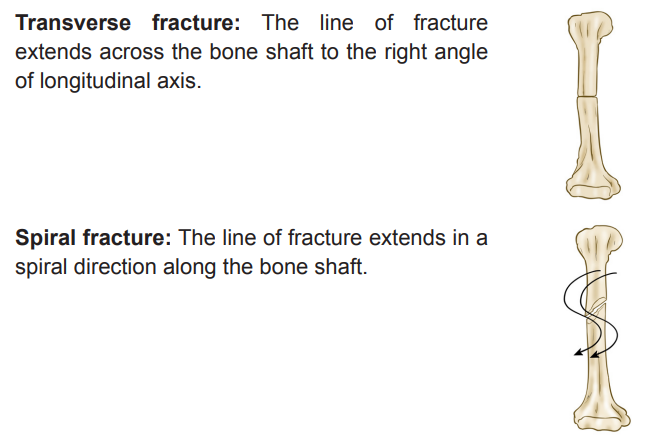
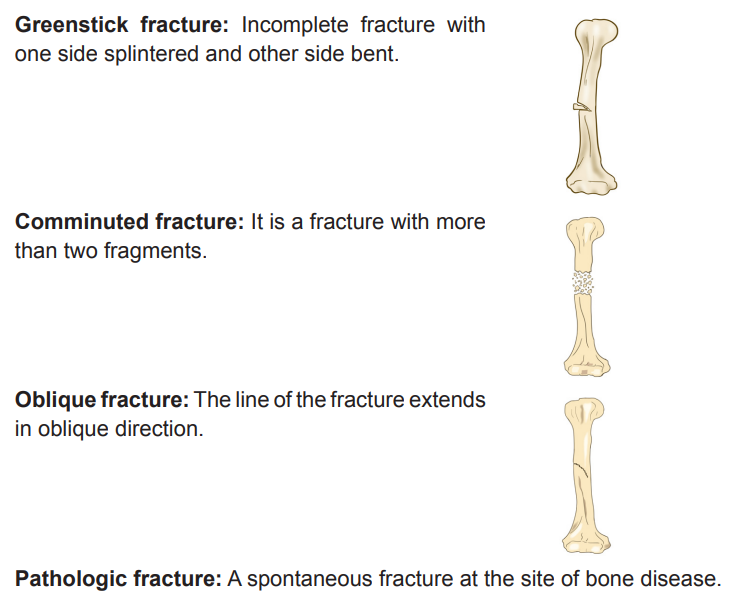
5.2.2.2 Classification of fracture according to the direction of fracture line
5.2.3 Signs and symptoms of fracture
A client with or suspected to have a fracture will experience the following signs and symptoms including:
Edema and Swelling: due to disruption and penetration of bone through skin or soft tissues, or bleeding into surrounding tissues.
Pain and tenderness: Muscle spasm as a result of involuntary reflex actionof muscle, direct tissue trauma, increased pressure on nerves, movement of fracture parts.
Muscle Spasm: Irritation of tissues and protective response to injury and fracture.
Deformity: Abnormal loss of bony contours.Ecchymosis and contusion: Discoloration of skin as a result of extravasation of
blood in subcutaneous tissues.Loss of Function: due to disruption of bone or joint, preventing functional use of limb or part.
Crepitation: Grating or crunching together of bony fragments, producing palpable or audible crunching or popping sensation.
5.2.4 Stages of fracture healing
Bone healing goes through a complex multistage healing process that occurs in the following stages:
First stage: Formation of hematoma: When a fracture occurs, bleeding creates a hematoma, which surrounds the ends of the fragments. The hematoma is extravasated blood that changes from a liquid to a semisolid clot. This occurs in the initial 72 hours after injury.
Second stage: Granulation tissue: During this stage, active phagocytosis absorbs the products of local necrosis. The hematoma converts to granulation tissue. Granulation tissue (consisting of new blood vessels, fibroblasts, and osteoblasts) produces the basis for new bone substance called osteoid during days 3 to 14 post injury.
Third stage: Callus formation: minerals such as calcium, phosphorus and magnesium and new bone matrix are deposited in the osteoid, an unorganized network of bone is formed that is woven about the fracture parts. Callus is primarily composed of cartilage, osteoblasts, calcium, and phosphorus. This occurs at the end of second week after injury.
Fourth stage: Ossification: Ossification of the callus occurs from 3 weeks to 6 months after the fracture and continues until the fracture has healed.
Fifth stage: Consolidation: As callus continues to develop, the distance between bone fragments diminishes and eventually closes. During this stage ossification continues. This stage can occur up to 1 year after injury.
Sixth stage: Remodelling: Excess bone tissue is resorbed in the final stage of bone healing, and union is complete. Gradual return of the injured bone to its preinjury structural strength and shape occurs. New bone is deposited in sites subjected to stress and resorbed at areas where there is little stress. The summary of bone healing is shown in the images below:
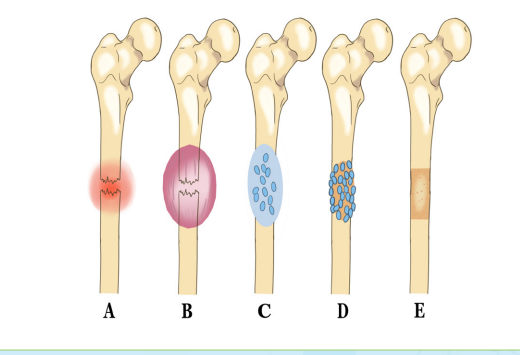
Fig: Bone healing. A, Bleeding at fractured ends of the bone with subsequent hematoma formation. B, Organization of hematoma into fibrous network C, Invasion of osteoblasts, lengthening of collagen strands, and deposition of calcium D, Callus formation: new boneis built up as osteoclasts destroy dead bone. E, Remodelling is accomplished as excess callus is resorbed and trabecular bone is laid down.
5.2.5 Diagnosis of fracture
– History and physical examination
– Radiographic test like X-ray,
– Computed tomography (CT) Scan
– Magnetic Resonance Imaging (MRI)
5.2.6 Treatment plan of fracture
The following are the overall goals of fracture treatment are
1. Anatomic realignment of bone fragments (reduction)
2. Immobilization to maintain realignment
3. Restoration of normal or near normal function of the injured part.
Fracture reduction
It consist of the following of:
– Closed reduction
– Open reduction
– Traction
Closed Reduction: Closed reduction is a nonsurgical, manual realignment of bone fragments to their previous anatomic position. Traction and counter-traction are manually applied to the bone fragments to restore position, length, and alignment. Closed reduction is usually performed while the patient is under local or general anaesthesia immobilize the injured part to maintain alignment until healing occurs.
Open Reduction: Open reduction is the correction of bone alignment through a surgical incision. It usually includes internal fixation of the fracture with wires, screws, pins, plates, intramedullary rods, or nails. The type and location of the fracture, patient age, and concurrent disease may influence the decision to use open reduction. The main disadvantages of this form of fracture management are the possibility of infection, complications associated with anaesthesia, and effect of pre-existing medical conditions (e.g., diabetes).
Traction: Traction is the application of a pulling force to an injured or diseased part of the body or an extremity. Counter-traction pulls in the opposite direction.
Advantages of traction
1. Prevent or reduce pain and muscle spasm associated with low back pain or cervical sprain.
2. Immobilize a joint or part of the body.
3. Reduce a fracture or dislocation.
4. Treat a pathologic joint condition (e.g., tumor, infection).
5. Provide immobilization to prevent soft tissue damage.
6. Promote active and passive exercise.
7. Expand a joint space during arthroscopic procedures.
8. Expand a joint space before major joint reconstruction.
The two most common types of traction
– Skin traction
– Skeletal traction
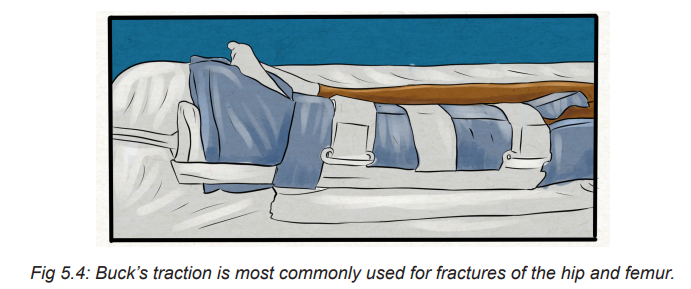
Skin traction: It is generally used for short-term treatment (48 to 72 hours) until skeletal traction or surgery is possible. Tape, boots, or splints are applied directly to the skin to maintain alignment, assist in reduction, and help diminish muscle spasms in the injured extremity.
The traction weights are usually limited to 5 to 10 lb (2.3 to 4.5 kg). A Buck’s traction boot is a type of skin traction used to immobilize a fracture, prevent hip flexion contractures, and reduce muscle spasms. In skin traction, assessment of the skin is a priority, since pressure points and skin breakdown may occur quickly. Assess key pressure points every 2 to 4 hours.
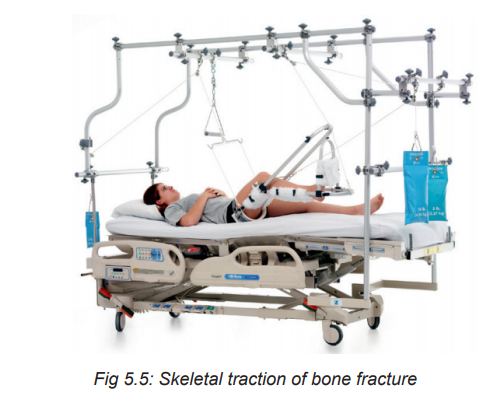
Skeletal traction: It is used to align injured bones and joints or to treat joint contractures and congenital hip dysplasia. It provides a long-term pull that keeps the injured bones and joints aligned. To apply skeletal traction, the physician inserts a pin or wire into the bone, either partially or completely, to align and immobilize the injured body part.
Fracture immobilization
– Casting
– External fixation
– Internal fixation
Casts: A cast is a temporary circumferential immobilization device. Casting is a common treatment following closed reduction. It allows the patient to perform many normal activities of daily living while providing sufficient immobilization to ensure stability.
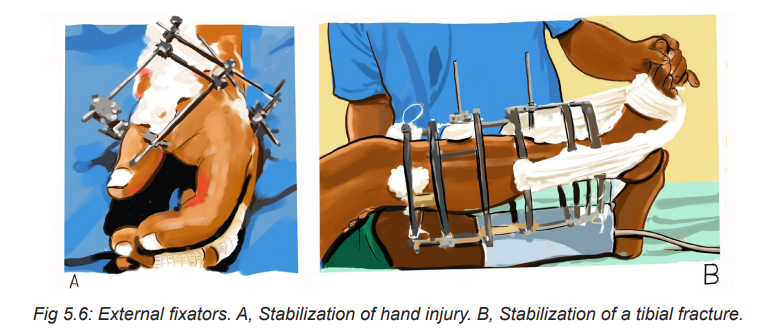
External Fixation: An external fixator is a metallic device composed of metal pins that are inserted into the bone and attached to external rods to stabilize the fracture while it heals. It can be used to apply traction or to compress fracture fragments and to immobilize reduced fragments when the use of a cast or other traction is not appropriate. Because the use of an external device is a long-term process, ongoing assessment for pin loosening and infection is critical. Infection signaled by exudate, erythema, tenderness, and pain may require removal of the device.
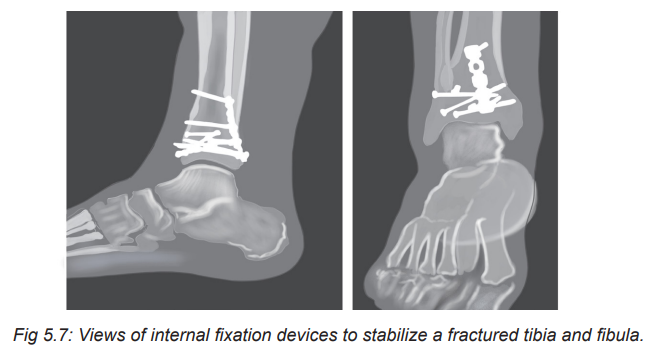
Internal Fixation: Internal fixation devices (pins, plates, intramedullary rods, and metal and bio-absorbable screws) are surgically inserted to realign and maintain bony fragments. These metal devices are biologically inert and made from stainless steel, vitallium, or titanium. Proper alignment is evaluated by x-ray studies at regular intervals.
Open fracture management
– Surgical debridement and irrigation
– Tetanus immunization
– Prophylactic antibiotic therapy
– Immobilization
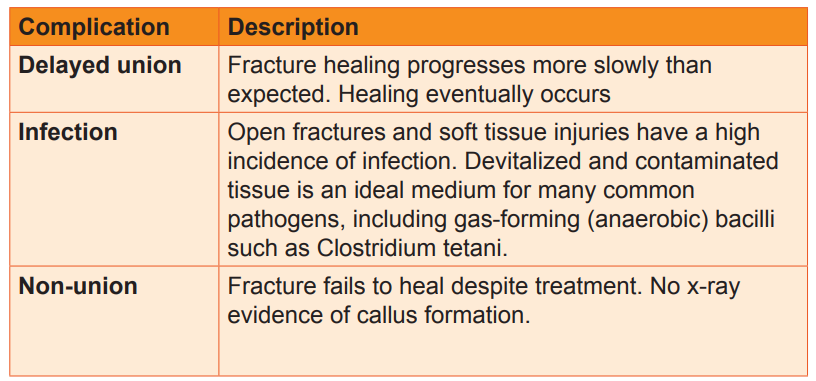
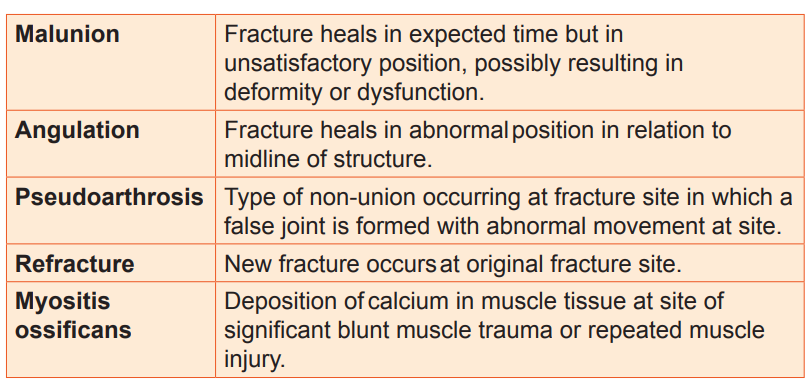
5.2.7 Complications and evolution of fracture
5.2.7.1 Complications of fracture
5.2.7.2 Evolution of fraction
The fractures heal well if adequate management is done timely.
5.3. End of unit assessment
1. Dislocation is defined as incomplete displacement of joint surface
– True
– False
2. The history taking and physical examination are considered to be the most important tools that physician uses to diagnose a dislocation
– True
– False
3. Describe the classification of fracture according to the direction of fracture line.
4. Enumerate four stages of bone healing fracture.
5. How a fracture is diagnosed?
6. State two modalities of fracture management.
7. List six complications of bone healing.
8. A 20 years old female patient admitted in emergency department with right femoral bone protrusion associate with bleeding post RTA. Vital signs were in normal range.
a. What type of fracture do you expect for this patient?
b. Which first aid can you give to this patient?
REFERENCES
1. Lewis, S. L., Dirksen, S. R., Heitkemer, M. M., & Linda Bucher. (2014). MEDICAL-SURGICAL NURSING Assessment and Management of clinical problems (NINTH). Canada: ELSEVIER MOSBY.
2. Williams, L. S., & Hopper, P. D. (2015). Understanding Medical Surgical Nursing (Fifth edit). Philadelphia: F.A. Davis Company.
3. Hinkle, J. L., & Cheever, K. H. (2018). Brunner and Suddarth’s textbook of medical-surgical nursing. Wolters kluwer india Pvt Ltd.
4. Winkelman, C. (2016). Medical-surgical nursing: Patient-centered collaborative care. Elsevier
5. https://www.google.com/search?q=dislocation&tbm=isch&ved=2ahUKEwiF5I6i3e33AhUH0YUKHR40DzwQ2-cCegQIABAA&oq=dislo&gs_lcp=CgNpbWcQ
6. https://www.msdmanuals.com/home/injuries-anpoisoning/dislocations/overview-of-dislocations
7. Medical surgical nursing book 9th edition.
8. https://www.google.com search?q=x+ray+of+dislocated+shoulder++&tbm=isch&ved= 2ahUKEwiNoIvatO73AhVCdBoKHaLSBOEQ2
